Living With Diabetes
www.healthawareness.co.uk


Kate Gerrard, Content Manager, JDRF UK
Page 06
Professor Andrew Boulton, President, International Diabetes Federation
Page 08
I am hoping that by sharing my experience of being diagnosed with prediabetes and what I did to get my blood sugars back to the normal range, I can inspire and help others.
Read more on Page 2

Q4 2022 | A promotional supplement distributed on behalf of Mediaplanet, which takes sole responsibility for its content
“For the first time, we have statistical insight into what can make the most impact across the world.”
“Education can help stop the rise of diabetes and prevent its complications.”
Image provided by Diabetes UK
Craig Rowe
TV Presenter on Channel 4’s A Place In The Sun, Diabetes UK supporter
The importance of checking if you are at risk of type 2 diabetes
Craig Rowe was diagnosed with prediabetes. Prediabetes means that blood sugars are higher than normal but not high enough to be diagnosed with type 2 diabetes. It also means there is a high risk of developing type 2 diabetes but does not always mean it will lead to type 2 diabetes.
Q: How did you find out about your diagnosis?
I had gone for blood tests because I was getting terrible night sweats, and the GP suggested that we run some tests. The results came back with a diagnosis of prediabetes.
Q: How much did you know about prediabetes?
I will be honest. I knew very little about diabetes in general, even though I heard it runs in my family. It felt to me, at the time, that I was being told I was knocking on the door of developing type 2 diabetes. Being given this diagnosis was a huge wake-up call, and I knew I had to find out more and take positive action towards getting my blood sugar down. But as someone who is fairly optimistic, I also knew that it was a good thing I found out because at least I could do something about it.
Know your risk of type 2 diabetes — even if you’re under 40
Increasing numbers of people under 40 are being diagnosed with type 2 diabetes. It is one of the most common — and serious — health conditions we face in the UK.
Casesof type 2 diabetes are rising rapidly and, until recently, it was considered quite rare in people under the age of 40. That common belief, however, is shifting after new statistics revealed an alarming acceleration of diagnoses in younger age groups across the UK.
of health conditions — including obesity and type 2 diabetes. As a result, people who are at increased risk of type 2 diabetes are often less likely to be able to benefit from support to manage it.
Q: Why have you chosen to share what you’ve been through?
I am beyond excited to be working with Diabetes UK. I am hoping that by sharing my experience of being diagnosed with prediabetes and what I did to get my blood sugars back to the normal range, I can inspire and help others. I also feel that as a Black man, it is my duty to share with my Black and Asian brothers how much more susceptible we are to type 2 diabetes and to have discussions about the warning signs, getting tested and taking action.


Q: What are your feelings about the future?
I am feeling really positive! The more I learn about prediabetes, the more I can adapt my lifestyle and, in particular, how I can balance the demands of being a busy TV presenter with what my body needs to keep itself healthy.
It felt to me, at the time, that I was being told I was knocking on the door of developing type 2 diabetes. To
Serious complications
Analysis of NHS data, carried out by Diabetes UK and our long-standing partner Tesco, has shown that cases of type 2 diabetes are now rising at a faster rate among those under 40 than in those over 40. Registered cases of type 2 in this age group are up 23% in just five years.
It is important to remember that the numbers of under-40s with type 2 diabetes remain a small proportion of total cases. But this trend of rapidly increasing, early-onset type 2 diabetes is incredibly troubling. The condition is known to have more severe and acute consequences in people under 40 and, without the right treatment and support, it can lead to serious complications that include kidney failure and heart disease.
Knowing the factors
While type 2 diabetes is often stigmatised as a condition that people bring on themselves, the risk factors are multiple and complex. They include genetics, family history and ethnicity, as well as living with obesity or being overweight, among other factors.
Social deprivation is also an issue. Factors such as income, education, housing, access to healthy food and poorer access to healthcare, have been strongly linked to an increased risk of developing a number
Registered cases of type 2 in this age group are up 23% in just five years.
How to check your risk
To mark World Diabetes Day 2022, Diabetes UK and Tesco have launched a campaign to drive a million people to check their individual risk of type 2 diabetes by using our free online ‘Know Your Risk’ tool or by visiting their local Tesco pharmacy. Anyone who completes an assessment will be directed to free advice and information regarding the help and support available to manage their risk.
02 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
WRITTEN BY Douglas Twenefour Head of Care at Diabetes UK
INTERVIEW WITH Craig Rowe TV Presenter on Channel 4’s A Place In The Sun, Diabetes UK supporter
to use the free
can be
@HealthawarenessUK @MediaplanetUK Please recycle
Manager:
Klingen caroline.klingen@mediaplanet.com Business Development Manager:
Managing Director:
Williams Head of Business
|
Content Editor:
|
Digital
Paid
find out more, go to diabetes.org.uk/riskscore WRITTEN BY John McKie Most people over 18 are eligible
‘Know Your Risk’ tool which
found at: riskscore.diabetes.org.uk/c/tesco To find your nearest Tesco Pharmacy, visit tesco.com or take an online assessment at: tesco.com/pharmacy
Project
Caroline
Emma-Jean Edwards
Alex
Development: Ellie McGregor
Head of Print & Design: Thomas Kent Designer: Aimee Rayment
Angelica Hackett O’Toole
Head of
Operations: Harvey O’Donnell
Media Strategist: Jonni Asfaha Social & Web Editor: Henry Phillips Digital Assistant: Carolina Galbraith Duarte | All images supplied by Gettyimages, unless otherwise specified | Contact information: uk.info@mediaplanet.com or +44 (0) 203 642 0737
Helping the rising number of people with diabetes through education
Improving care for diabetes requires education and knowledge sharing among patients and healthcare providers.
Rightnow, 10% of adults — more than 500 million people — are living with diabetes. That number is expected to grow to almost 800 million within the next 25 years.
Knowing your diabetes needs
WRITTEN BY Henry Anhalt, D.O. Paediatric Endocrinologist and Chief Medical Officer, embecta
As prevalence continues to rise, the care continuum continues to evolve, creating a significant need to provide new and ongoing education. At embecta, our primary focus has been to collaborate with the global diabetes community to elevate the standard of diabetes care via education and equipping healthcare professionals and those they treat with the necessary tools to help people manage their diabetes.
Living with diabetes can be overwhelming, whether someone has been newly diagnosed or is making a change to their treatment plan (e.g. adding insulin injections). Learning more about the available treatment options can be empowering, helping individuals feel in control as they work with their care team to manage their diabetes.
Expanding access to educational resources
One of the best ways to help people manage this condition is through expanded access to education, which has been a hallmark of our company. We reach people with diabetes, doctors, pharmacists, caregivers and other healthcare professionals in over 100 countries, providing support to more than 30 million patients.
We engage directly with people with diabetes through our BD™ Diabetes Care app — an educational and lifestyle tool designed to provide each person with an experience based on their journey. Through adaptive learning and AI, the app gives people with diabetes lifestyle content tailored to their individual, emotional and functional needs. It extends the efforts of healthcare providers by connecting patients to in-home support and education.
Advancing injection therapy
We work with healthcare providers and pharmacists to advance injection therapy. We want to ensure those prescribing and dispensing injection products have a strong understanding of the benefits of shorter needles, injection site rotation and singleuse needles for the amount of insulin prescribed.
People living with diabetes need access to ongoing education to understand their condition and carry out the daily self-care which is essential to staying healthy and avoiding complications.
We offer offices and pharmacies educational resources and tools for their patients. This includes injection how-to guides to educate about proper injection technique and ‘Getting Started’ booklets and toolboxes to support those beginning insulin therapy.
Providing these to everyone involved in the diabetes management ecosystem can help manage the burden of those living with diabetes.
Addressing patient burden
Organisations around the world are working to develop new treatments, devices or products aiming to improve diabetes care. But we cannot take our eyes off the patient while we focus on innovation. People living with diabetes need access to ongoing education to understand their condition and carry out the daily self-care which is essential to staying healthy and avoiding complications.
The reality of diabetes is that people on an insulin therapy protocol need to monitor their glucose and administer insulin accordingly. It can be challenging, as many individuals on insulin therapy may feel embarrassed, isolated or misunderstood.
With the right support and guidance from the moment of diagnosis, we can help reassure people with diabetes that they are not alone on their journey and provide educational resources to help them manage their diabetes.

Improving diabetes care standards
We, at embecta, will continue to work to improve the standard of care for those living with diabetes. Innovative products are part of the solution; access to educational resources is another. Everyone deserves to live a life unlimited by diabetes, and increasing access to educational tools and resources is a great place to start.

A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 03MEDIAPLANET
Paid for by embecta Find out more at embecta.com
Imageprovidedbyembecta
“Why I’m rocking my diabetes tech — and feel so proud of it!”


Diabetes doesn’t need to have a detrimental effect on your body positivity. The secret is to view it in a different, empowering way.
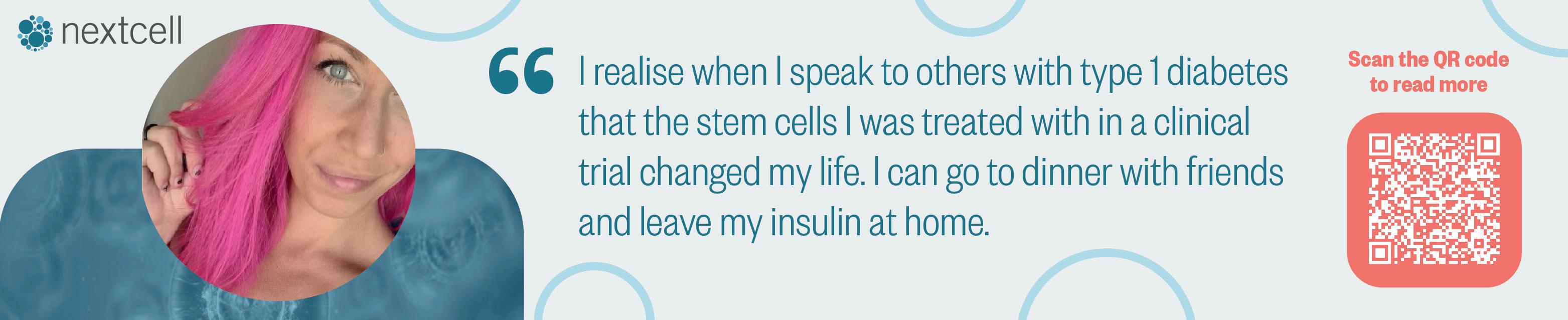
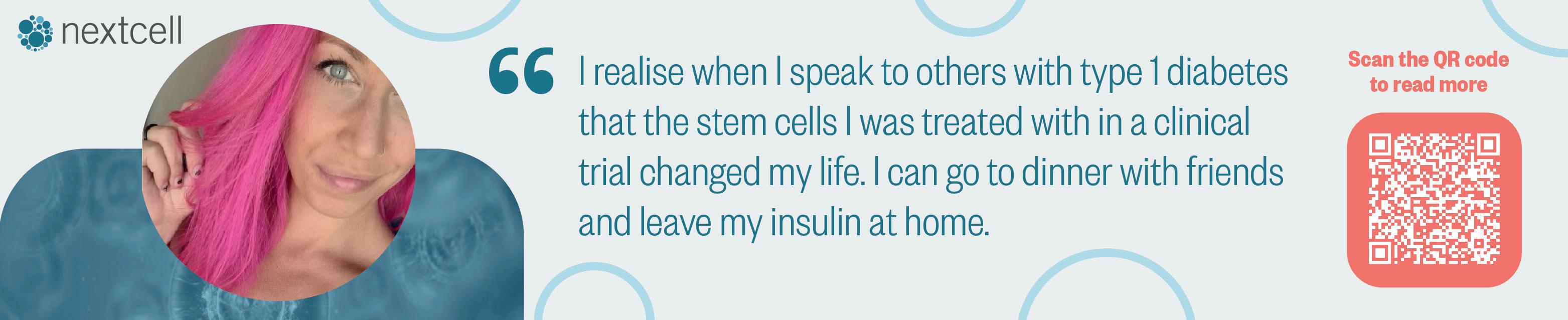
When she was 12, content creator Jasmine Jaffar discovered she had type 1 diabetes — a diagnosis she found overwhelming at first. “I thought: This is out of my control, and I can’t change it. But I do have control over how I think about it.” So, she began to view her diabetes in a more positive and empowering way.
Life-changing way to monitor glucose Nowadays, Jasmine, 25, posts regularly about thriving with diabetes and emotional wellbeing. She’s also a passionate advocate for body positivity and proudly displays the glucose monitoring sensor attached to the back of her upper arm.

Jasmine scans it with her mobile phone to get an accurate reading of her current glucose levels. If these
are too high or too low, she can then take steps to get them back in range. “When I was first diagnosed, I’d fingerprick to test my glucose levels, which meant it was hard to be flexible and proactive with my management,” she says. “When I was introduced to this tech, I thought: This is life-changing. It truly transformed my diabetes management.”
Embracing your diabetes
Jasmine is aware that type 1 diabetes can impact self-image and body positivity.
“That sensor on your arm makes an invisible condition visible to others,” she admits. “But when you embrace your diabetes, it can be so empowering. It’s not something that should be hidden, because it’s part of you and enables you to be your most authentic self. I feel as though the technology I wear is a symbol of my
experiences. It has taught me about my body and my health. I’m rocking it — and I feel proud of it!”
A freeing experience
Jasmine reflects a positive attitude in her social media posts. “People tell me that coming across my platforms has given them hope that they can still thrive with diabetes, or how comforting it is to see positive energy around it. That means so much to me because I want people to feel empowered with their diabetes.”
Jasmine doesn’t want to downplay the condition. “Diabetes can be hard, and there will be challenging times,” she says. “But if you embrace it, you can live a beautiful, happy, healthy life. And if one person sees my posts and thinks: ‘Right — I am going to wear that dress, even if my sensor is showing!’ then that’s a huge win for them...and me.”
04 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK Be seen for who you are, not your diabetes. Images are for illustrative purposes only. Not actual patient or data. 1. Data on file. Abbott Diabetes Care. 2. Data based on the number of users worldwide for FreeStyle Libre family of personal CGMs compared to the number of users for other leading personal CGM brands and based on CGM sales dollars compared to other leading personal CGM brands. © 2022 Abbott. FreeStyle, Libre, and related brand marks are marks of Abbott. ADC-66217 v1.0 11/22.
Find Jasmine Jaffar on Instagram and TikTok at @thetypethat
INTERVIEW WITH Jasmine Jaffar Content Creator, FreeStyle Libre Ambassador
WRITTEN BY Tony Greenway
How to improve your emotional wellbeing and deal with stigma





Diabetes isn’t just a physical condition. Its challenges can also take a toll on your emotional wellbeing, so it’s okay to be honest and open if you are struggling.
Ifyou struggle with your emotional wellbeing because of your diabetes, that shouldn’t come as a surprise, says Deborah Christie, Professor of Paediatric and Adolescent Psychology and Consultant Clinical Psychologist at University College London Hospital’s NHS Foundation Trust. “Managing diabetes can be intrusive and burdensome,” she explains. “That can result in a low mood, anxiety, lack of self-care and, eventually, significant burnout.”
Deborah Christie Professor of Paediatric and Adolescent Psychology, Consultant Clinical Psychologist


Stigma is created by a lack of knowledge and a fear of the unknown.



Accepting realities
Professor Christie emphasises that these types of feelings shouldn’t be considered mental health issues. “I prefer the term ‘emotional distress,’ because these are reasonable emotional reactions to a challenging condition,” she says. “You have to come to terms with your reality. But you might need help to get there.”
The answer is to keep talking, says Professor Christie. “Talk to your healthcare team. Talk to your family or, if you’re in a relationship, talk to your partner, and tell them what you are going through. Talk to a clinical health psychologist who has experience with helping people through the challenges of chronic illness. Find someone who can help you think things through. Follow positive role models on social media who will give you messages of hope and encouragement.”




Facing stigma
Understand that you will face stigma, consciously or unconsciously, from society, institutions and even healthcare professionals in some instances — and know how best to deal with it. “Stigma is created by a lack of knowledge and a fear of the unknown,” says Professor Christie.

“When human beings see something they don’t understand or perceive as scary, they can react negatively. Unfortunately, it can mean that people with diabetes don’t get equal access to treatment or are faced with barriers to services and needs. For example, schools might not let children with diabetes go on school trips.”
Seeking help
Your emotional wellbeing can be affected by your diabetes — it’s okay to be honest and acknowledge it. You’re not being weak or unreasonable. “The struggle is a real and normal part of living with diabetes,” says Professor Christie. “It doesn’t have to always be that way, so ask for help — and keep asking until you get the right help. Don’t give up.”
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 05MEDIAPLANET Diabetes shouldn’t define you. Manage your diabetes the easy way with the FreeStyle Libre 2 system –the #1 sensor-based glucose monitoring system worldwide1,2 Now You Know Visit Sample.FreeStyle.Abbott to start your FREE trial
INTERVIEW WITH Professor
WRITTEN BY Tony Greenway
WRITTEN BY Kate Gerrard Content Manager, JDRF UK

Alleviating the global burden of type 1 diabetes: driving change with data
Calorie restriction programme can lead to remission of type 2 diabetes
Diabetes is increasing worldwide, with 4.41 million people in the UK currently diagnosed with type 2 diabetes and another 13.6 million at increased risk of developing it.
Type 1 diabetes is one of the fastest-growing chronic health conditions worldwide, impacting nearly 9 million people.
Ourresearch programme at JDRF is on a global scale, bringing together the best minds from across the world to drive research into treatments and cures. Now, the Type 1 Diabetes Global Index gives us first-of-itskind global data to help identify the specific interventions needed to tackle the type 1 crisis.
Global picture of type 1
What we haven’t had — until now — is a global picture of the type 1 diabetes crisis. The Type 1 Diabetes Global Index, led by JDRF in partnership with other global type 1 organisations, uses data modelling to show the prevalence and impact of type 1 in every country. It gives us the most accurate picture of the global state of the crisis.
It highlights the ‘missing people’ — the number of people who would still be alive if they had not died early due to complications from type 1 and ‘healthy years lost’ — time lost to ill health, disability or early death from living with type 1 diabetes.
Globally, the index indicates that there are 3.86 million ‘missing people.’ The average number of ‘healthy years lost’ to type 1 diabetes per person, worldwide, is 32 years (if diagnosed at age 10).
Leveraging data for action
The data gives us leverage to call for specific interventions at a country level, including timely diagnosis, access to affordable insulin, glucose testing and the prospect of cellular cures.
Take Rwanda, for example, where an estimated 3,651 people live with type 1 and lose an average of 50 healthy years. JDRF has partnered with an international charity, Life for A Child, which will use the data from the index to map and understand the needs of people with type 1 in Rwanda and support the clinical provision of insulin and blood glucose testing. These interventions can help us restore some of those 50 years lost — and save lives.
In the UK, the index shows us that the average number of healthy years lost to treatment and care is 3.3 years.
What could this mean for the UK?
In the UK, the index shows us that the average number of healthy years lost to treatment and care is 3.3 years. It also shows us that if everyone had access to technology that automates insulin delivery and glucose monitoring, we could give people back nearly three years of their life, drastically minimising the burden of type 1.
For the first time, we have statistical insight into what can make the most impact across the world.
Approximately850,000 people have type 2 diabetes in the UK but are not diagnosed yet. Diabetes leads to 185 amputations, 30 incidents of serious vision loss and 700 premature deaths every week, in addition to other complications like heart attack and stroke. The NHS spends 1 billion every year (10% of its budget) on diabetes.
Physical activity and sustained weight loss can reduce the risk of diabetes by about 50%, and people with diabetes can achieve sustained remission.
Reversing diabetes in overweight people
The Diabetes Remission Clinical Trial (DiRECT) research shows that with a structured low-calorie diet (800 calories) programme — supplied by a total diet replacement programme, followed by structured weight loss maintenance — 50% of people with diabetes can achieve remission.

Almost 9 out of 10 can succeed if they lose 15 kg or more in the first year. Results show that 36% of people were still in remission two years later. These results were associated with a reduction of fat around the liver and pancreas, with improved morphology and function of the pancreas, among other benefits.
In addition to the health benefits, the DiRECT approach to diabetes results in financial savings of about £1,337 per person over their lifetime.
Weight reduction in people with normal weight
Although most people with type 2 diabetes are overweight, about 10% are of normal weight. Recent results of the ReTUNEing type 2 diabetes remission (ReTUNE) trial in participants who had normal weight (BMI <27) show exciting results with a low-calorie diet (800 Kcal per day) for two to four weeks. It is followed by a four to six-week weight loss maintenance period, gradually returning to normal food. These cycles were repeated until the participants had lost 10–15% of their original body weight. The research shows that this approach reduced the average BMI from 24.8 kg/m2 to 22.4 kg/m2 — with 70% of participants achieving diabetes remission.
How does weight loss help?
It appears that beta cells in the pancreas which secrete insulin are not dead but just asleep in people with type 2 diabetes. They can wake up and start functioning normally with enough weight loss.
These recent developments offer hope to millions. They can reverse, or at least delay, the development of type 2 diabetes and its complications with attention to diet and weight loss irrespective of their initial weight.
06 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
WRITTEN BY Dr Umesh Dashora Consultant, Endocrinology and Diabetes at Conquest Hospital, Hastings and meeting secretary, Association of British Clinical Diabetologists





A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 07MEDIAPLANET ww w.glucomen.co.uk Now available on prescription Actual Real-time data Provides a glucose value every minute for better treatment decisions and hypo/hyper avoidance Needle-free Insertion is completely needle-free for a reduced risk of pain or bleeding Eco-friendly Reusable applicator, transmitter and needle-free insertion reduces CGM waste by up to 93% Reduced site reactions Free from isobornyl acrylate; the allergen responsible for the majority of site reactions GlucoMen Day® CGM provides a new glucose value every minute for actual real time alarms, plus needle-free application helps it to be the most eco-friendly system on the market. myglucomen@menarinidiag co uk0800 085 220 4
living
diabetes
access to education
can
People
with
need better
so they
have the confidence to manage their condition and avoid
or delay life-threatening complications.
~Professor Andrew Boulton, President, International Diabetes Federation
Could our eyes hold the key to pain-free glucose monitoring?
A simple scan of the eye could hold the answer to pain-free and non-invasive glucose testing.
Withthe number of people living with type 2 diabetes increasing each year, former Apple industrial designer Daniele De Iuliis suggests that a ‘pain-free, 21st-century solution’ to glucose testing is ‘long overdue’ and has his sights set on using the eye to help deliver it.
The eye: a window to your health?

After 27 years working in Apple’s industrial design team, De Iuliis became a founding investor in Occuity, a Reading-based startup developing an optical device to non-invasively measure glucose levels via the eye. The device will work by safely shining a light into the eye to measure subtle changes and determine glucose levels within the aqueous humour, which has been demonstrated to closely match glucose in the bloodstream.

De Iuliis describes the concept of the ‘Occuity Indigo’ as a pen-like device that is both easy to carry and use, highlighting that it will need no consumables and can be used without the stigma associated with current finger stick devices. “Having witnessed existing finger stick testing firsthand, the idea that you can easily take a pain-free glucose measurement from yourself or a loved one — young or old — is most definitely a game-changer,” says De Iuliis.
Community support
The team behind the device is building a community of people who share an interest in diabetes. Already over 8,000 strong, the community is given the opportunity to share their views on the technology and design. They will also be able to support its development through surveys, clinical trials, product testing and even buying shares in the company through its Seedrs crowdfunding campaign.
As De Iuliis concludes: “Diabetes is a very personal condition, and of course, once you have it, it’s likely with you for the rest of your life. We know people want a non-invasive solution, and we thought giving those same people the opportunity to become shareholders in our business is a great way to enable them in joining us on this journey to try to improve their lives and millions more across the globe.”
Investing in diabetes education can help WHO reach its targets
Accordingto the latest research from the International Diabetes Federation (IDF), more than half a billion people globally (537 million) are living with diabetes — a number that’s expected to exceed 640 million by 2030. To curb this rise, the Member States of the World Health Organization (WHO) have agreed on a set of ambitious, global diabetes targets to be achieved by 2030. These include ensuring that 80% of people living with diabetes worldwide are diagnosed and have good control of blood glucose and blood pressure.
Severe global situation
To achieve these goals, diabetes education must be made a priority. Current estimates show nearly half of adults living with diabetes are undiagnosed. If the condition remains undetected or is inadequately treated, it can lead to serious complications including blindness, heart attack, kidney failure, lower-limb amputation and stroke. In fact, according to Dr Thedros Adhanom Ghebreyesus, Director-General of WHO, diabetes is now the only major non-communicable disease for which the risk of dying early is continuing to rise.
People living with diabetes need better access to education so they can have the confidence to manage their condition and avoid or delay life-threatening complications.
It is equally important that healthcare professionals have access to ongoing training to provide the best possible diabetes treatment, care and advice.
Consultation time is limited, with the average person with diabetes spending less than three hours per year with a healthcare professional. Therefore, it is imperative that healthcare professionals can make the most of the time they have available.
Education today to protect tomorrow
Education can help stop the rise of diabetes and prevent its complications. This World Diabetes Day, IDF is campaigning for improved education and training for people with diabetes and healthcare professionals.
IDF is also asking members of the public and the diabetes community to send a letter to their health minister to request that sufficient human and financial resources be dedicated to diabetes education. In order to help achieve the WHO diabetes targets, we need education today to protect tomorrow.
08 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
Investing in diabetes education is growing in importance as the number of people around the world with diabetes continues to rise.
Consultation time is limited, with the average person with diabetes spending less than three hours per year with a healthcare professional.
WRITTEN BY Professor Andrew Boulton President, International Diabetes Federation
Paid for by Occuity Learn more at occuity.com/jodc
INTERVIEW WITH Daniele De Iuliis Design Director, Occuity
WRITTEN BY Richard Kadri-Langford