“Family
Paul Edwards, Director of Clinical Services, Dementia UK Page
“Approximately




















































































 Paola Barbarino, Chief Executive
Paola Barbarino, Chief Executive
Understanding Dementia www.healthawareness.co.uk Q3 2023 | A promotional supplement distributed on behalf of Mediaplanet, which takes sole responsibility for its content
and friends are the most common source of support for people with dementia.”
04
55.6 million cases of dementia globally could be delayed or reduced.”
Officer,
Disease International
Alzheimer’s
Page 06
Why we need to make dementia the priority it should be
There’s no way to sugarcoat it – dementia devastates lives. One in three people born in the UK today will get dementia, and it’s the UK’s biggest killer.
There are currently 900,000 people living with the condition and that number is set to rise to 1.6 million by 2040.
Dementia care crisis
WRITTEN BY Kate Lee CEO, Alzheimer’s Society

Dementia diagnosis rates hit a five-year low during the pandemic and have stagnated ever since, leaving tens of thousands of people unable to access the support they need. There are currently no treatments available to slow down the progression of Alzheimer’s disease, which is the most common form of dementia. This is causing immense stress and anxiety for family carers, who are often the primary caregivers for people with dementia. It is no wonder that people over 50 say that dementia is the condition they are most concerned about.
Tackling dementia head-on
The picture of dementia may seem bleak, but we cannot bury our heads in the sand. This colossal challenge will not go away on its own. We must make dementia a priority and tackle it head-on. We need to get everyone talking about this major health issue.
Alzheimer’s Society is at the forefront of this fight. We are making progress and believe we are on the cusp of better outcomes for people affected by dementia. We need to continue to invest in research, raise awareness, and provide support to those affected. Together, we can make a difference.
Government action
The Government has recognised the scale of the dementia problem and has included it in its Major Conditions
Project Manager: Rebecca Herbert rebecca.herbert@mediaplanet.com

Strategy. Alzheimer’s Society is working with policymakers to ensure that the plans are ambitious and that people living with dementia have a voice.
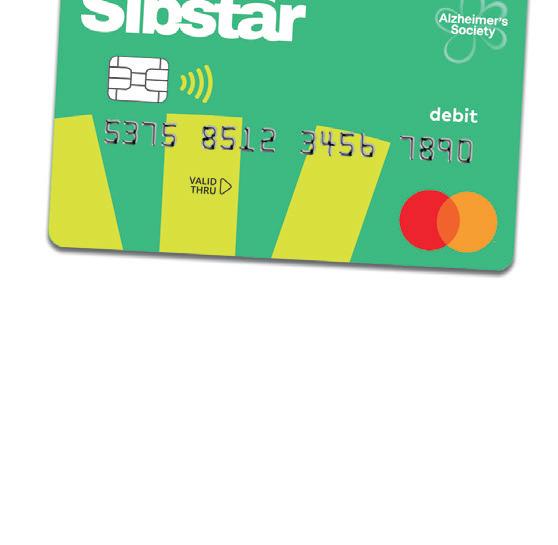
Thanks to a £5 million award from the players of People’s Postcode Lottery, Alzheimer’s Society, along with Alzheimer’s Research UK and the NIHR, have launched the Blood Biomarker Challenge. This will gather the information needed to introduce a blood test for dementia into UK healthcare systems. A blood test would be a crucial step in speeding up diagnosis and early intervention.
Hope for Alzheimer’s patients

After 20 years without any new Alzheimer’s disease drugs approved in the UK, two potential drugs, lecanemab and donanemab, have shown promise in slowing the progression of the disease. These drugs work by targeting amyloid plaques, which are thought to be a key factor in Alzheimer’s development. If approved, these drugs could represent a major breakthrough in the fight against Alzheimer’s.
We vow not to rest until we have a world where dementia no longer devastates lives.
Please help by donating to Alzheimer’s Society this World Alzheimer’s Month so we can carry on this crucial fight. Visit: alzheimers.org.uk
Business Development Manager: Chloe Leedham Managing Director: Alex Williams Country Manager UK: Ellie McGregor |
Head of Print & Design: Thomas Kent Designer: Aimee Rayment Content Editor: Angelica Hackett O’Toole | Head of Digital Operations: Harvey O’Donnell Paid Media Strategist: Jonni Asfaha Social & Web
Editor: Henry Phillips Digital Assistant: Carolina Galbraith Duarte | All images supplied by Gettyimages, unless otherwise specified
02 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
@HealthawarenessUK Contact information: uk.info@mediaplanet.com or +44 (0) 203 642 0737 @MediaplanetUK Please recycle
We are making progress and believe we are on the cusp of better outcomes for people a ected by dementia.
How to help people with dementia manage their money safely through an app
Do you work with dementia organisations?

My idea, written on a piece of paper in a café, won the Alzheimer’s Society accelerator programme. They, and Mastercard, are now important partners. That partnership enabled us to research and co-create our product with people living with dementia and their carers by looking at functionality, brand, tone and the app. We are continually talking to people with dementia to improve our product.
What sort of feedback have you received?
Carers say it has helped their loved ones retain their independence and has taken away much of the administrative worry. One lady with dementia told us, ‘Sibstar helps me to help myself.’ With overall positive feedback, we’re currently seeking funding for our second round, and we have some exciting TV appearances lined up for next year.
What is special about the app?

What inspired this app for people with dementia?
The idea came from my own lived experience of caring for my mum June and my dad Peter, who both have dementia. As my mum’s condition progressed, she struggled to understand her everyday money; she was falling victim to scams over the phone, making multiple cashpoint withdrawals and massively overspending on things she didn’t need.
What options did you look at?
We tried placing limits on her High Street bank account, scratching out the CVV on her card and taking her chequebook away; but nothing worked. We thought there must be a better way of enabling people with dementia to remain financially independent and financially safe.
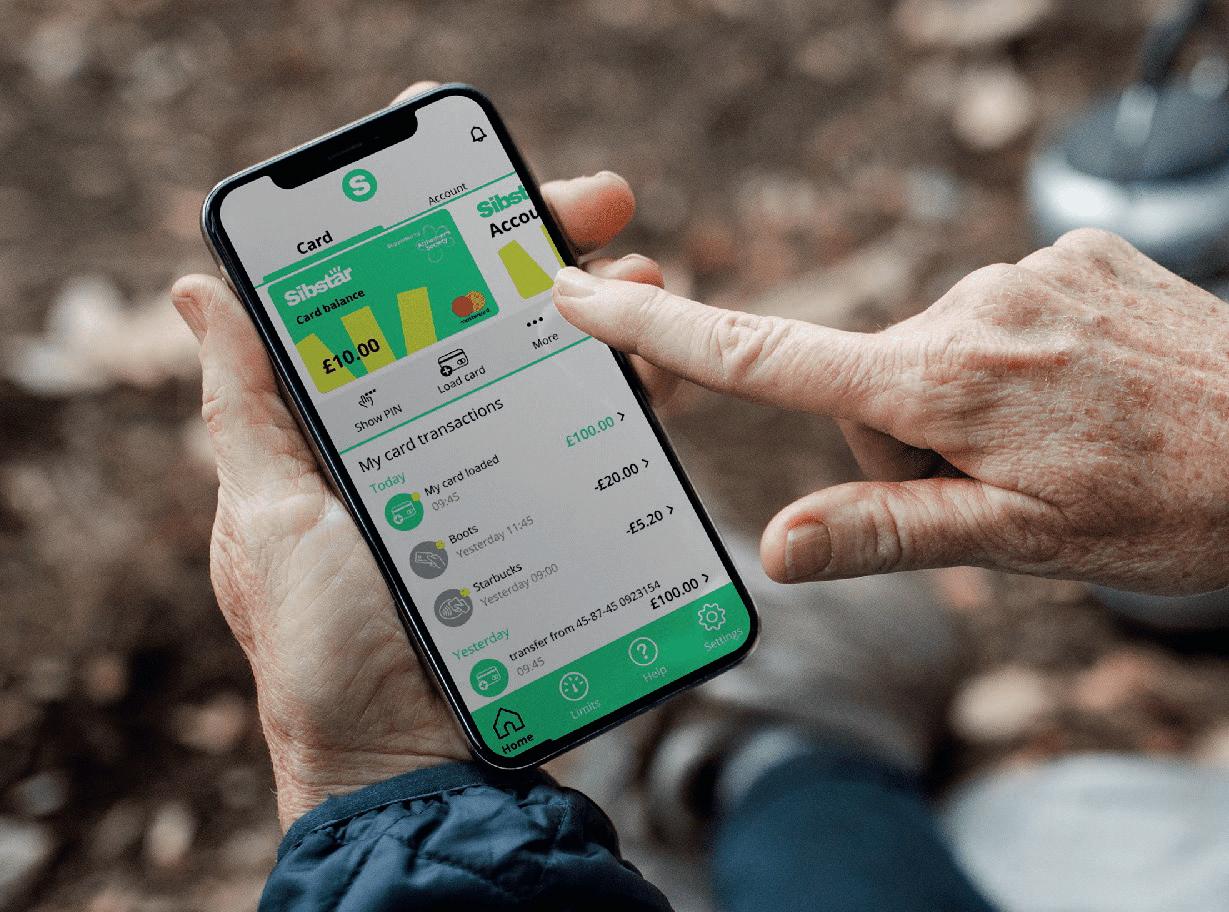
How does this finance solution work?
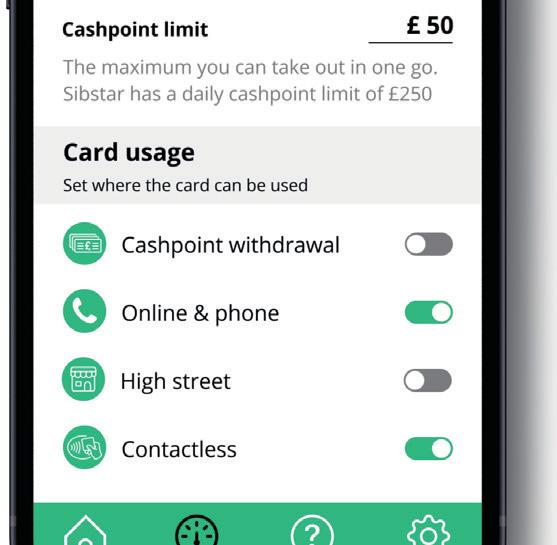
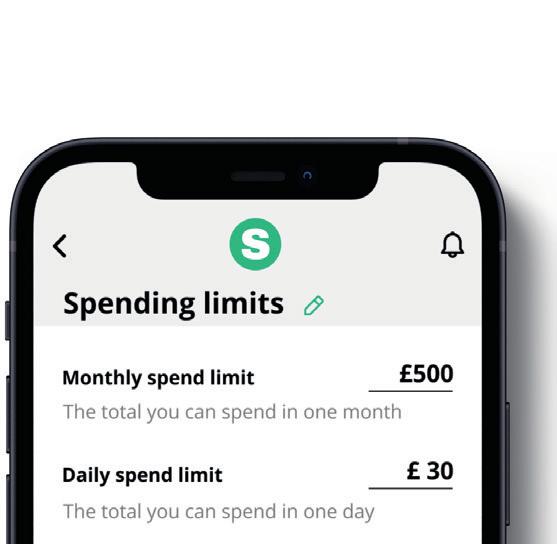
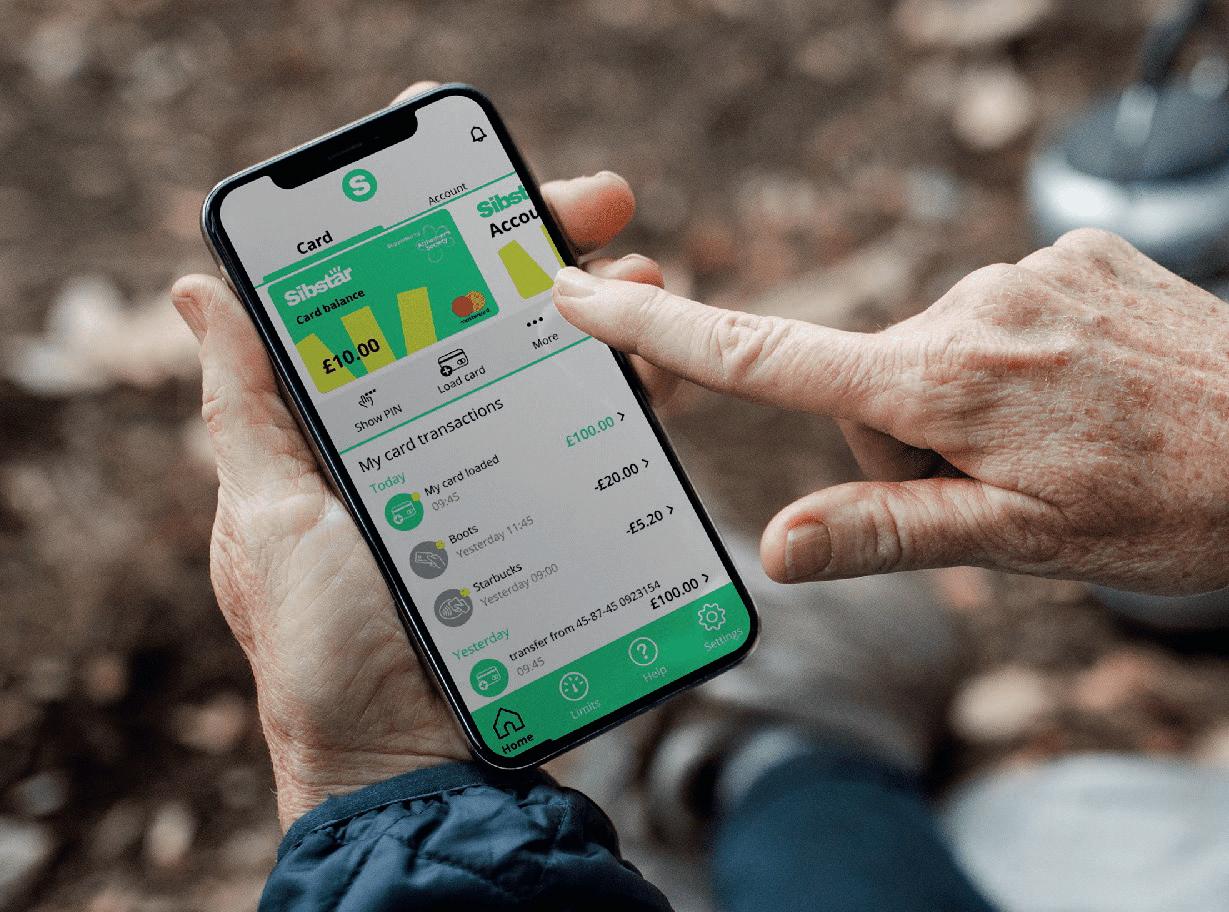
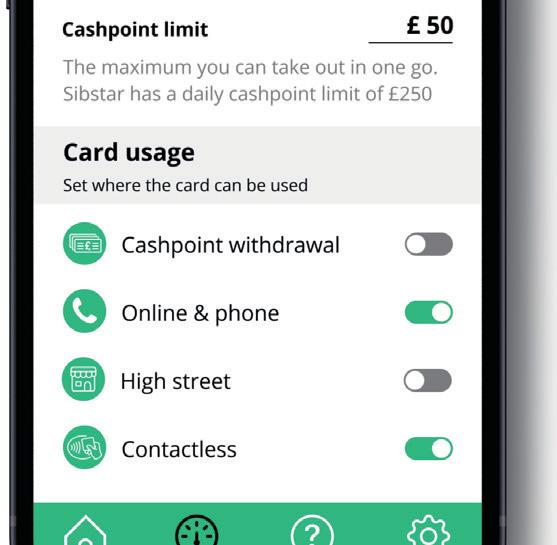
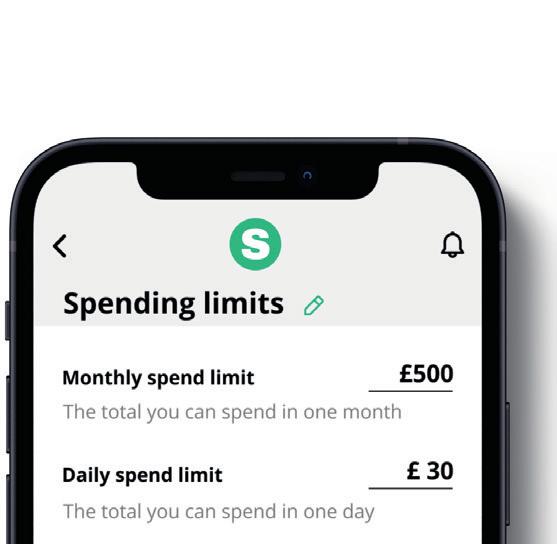
Load the Sibstar card with your chosen amount of money, then manage how and where that money can be used on the Sibstar app. Our app offers a wide range of functionality to help keep your money safe and can be adjusted instantly at any time. For instance, you can set monthly or daily spending limits, establish a cashpoint withdrawal limit, toggle cashpoint withdrawals or online and phone purchases on or off altogether. If a person with dementia has someone supporting them through Sibstar, their supporter will receive notifications each time

the card is used. This feature assists them in keeping an eye on their loved ones without being overly intrusive or overbearing. It also serves as a conversation starter.
Who are your customers?
They are mainly family carers: husbands; wives; sons; daughters; grandchildren; but anyone can have a Sibstar card. We receive calls from parents with adult children with learning disabilities or gambling addictions, but our present focus is on people with dementia because that is my lived experience and the basis of our startup.

How do people apply?
They can download the Sibstar app from the App Store or Google Play and sign up within the app. As with any financial product, identity checks are conducted on the person with dementia and their supporter. Additionally, if there is a lasting power of attorney in place, we review that as well. Once these checks are completed, the debit card is sent by mail.

Who uses the debit card?
It depends on where you are with your dementia journey. If someone has dementia but understands everyday money, they have a card and app on their phone. For those unable to understand, they have a debit card, and a supporter manages the money for them via the app.
As far as I am aware, we are the only financial solution enabling vulnerable adults to have a ring-fenced amount of money sitting on a card that can be managed safely. We are not in competition with banks, and I do not have a finance background; we are a service layer on top of what banks already provide.
I believe it can make a big difference; by retaining your financial independence you can continue living life the way that you choose.
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 03 MEDIAPLANET
Jayne Sibley, co-founder and CEO of Sibstar, talks about the debit card and app designed for people living with dementia and their family carers.
INTERVIEW WITH Jayne Sibley Co-Founder, Sibstar
Paid for by Sibstar Scan the QR code or find out more at sibstar.co.uk Advertorial
WRITTEN BY Mark Nicholls
Images provided by Sibstar
Why we shouldn’t forget about the carers who support people with dementia
A diagnosis of dementia can change everything. As a specialist dementia nursing charity, we know that families need tailored support to help them care for loved ones living with the condition.
There are many subtypes of dementia, which progress in different ways and display different symptoms. However, people who contact our helpline or attend our clinics, tell us that they are not given enough or sometimes any guidance following diagnosis and have no idea where to turn for help.
People unaware of dementia support
We recently conducted research, which shows that only 53% of people who know or knew someone with a diagnosis of dementia are aware of ‘all or most of the types of support available for people living with dementia’ in the UK.1
This lack of knowledge can be attributed to disjointed post-diagnostic care from health services; dementia has long been overlooked when it comes to health and social care provision despite being recognised as the leading cause of death in the UK.2

Affecting carers involved
With well-documented shortages in the health and social care workforce, caring responsibilities often fall to loved ones. Our research showed that family and friends are the most common source of support for people with dementia, with 45% of people who know someone with a diagnosis saying the person is, or was, supported by family and friends compared to just 33% receiving support from a GP and 24% from social services.1
This is putting pressure on family members who need support, too. A diagnosis of dementia impacts the whole family — not just the person with the diagnosis. It’s important for carers to seek out support for themselves as the caring role can be huge and requires time, adaptability and also forgiveness.
Forms of support for dementia
It’s clear that more specialist support is urgently needed to help with this huge and growing health crisis. In addition to addressing the gulf between health and social care services, we also need to see more specialist dementia nurses, improved local support services and greater access to at-home care options. These three things were identified as the most beneficial forms of support for people impacted by dementia.
WRITTEN BY Paul Edwards Director of Clinical Services, Dementia UK

04 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
References 1.Data taken from a survey of 3,008 adults conducted by Censuswide in July 2023 2.ONS data published 11th April 2023
If you need advice or support on living with dementia, contact the free Admiral Nurse Dementia Helpline on 0800 888 6678 or email helpline@dementiauk.org You can also book a free video or phone appointment to get expert dementia support from an Admiral Nurse. Find out more at dementiauk.org/book-an-appointment
Family and friends are the most common source of support for people with dementia.
How a new support system could enrich the lives of people with dementia
A model of personalised support could improve life for people with dementia and their carers by empowering them to make the best choices for their own care needs.
In this country, there is a concerning gap in dementia support, notes Dr Tomasina Oh, Associate Professor, Dementia Care Programme Lead at the University of Plymouth. “Some people living with dementia are falling between the cracks,” she says.



“They have received a diagnosis but are not yet in need of a care home or input from specialists. Worryingly, these individuals and their carers — who are usually spouses or family members — are often left without suitable support to face a range of daunting challenges.”
Personalised support for dementia patients and carers
Challenges can include social isolation, despair and frailty due to combined physical and cognitive decline. However, a five-year collaborative research project including the Universities of Plymouth and Manchester — established in 2018 and funded by the National Institute for Health and Care Research — aims to remedy this neglect by evaluating a system for dementia support they have developed.
Dementia PersonAlised Care Team (D-PACT) proposes improving the lives of people living with dementia — and their carers — with personalised emotional and practical support from an appropriately trained Dementia Support Worker. The support worker, supervised by specialists,

spends time understanding the individual’s particular situation and then empowers them and their carers to make the best choices for their own needs. Crucially, they are not there to tell them what to do.
Trusted point of contact offering proactive support
“The Support Worker becomes a trusted point of contact who can spot potential problems before they escalate into crises,” says Professor Richard Byng, Professor in Primary Care Research at the University of Plymouth. “It’s a model that helps the individual and their carers function and stay together.”

The study, which was conducted in a range of settings, shows potential value and has been well-received by those who took part. “People have described a step change in their support,” says Professor Byng. “They say they feel listened to and treated as a person, getting reassurance and relief — particularly carers — that they are doing things right and someone is alongside them.”
Our team is available 9am—5pm Monday to Friday to answer any questions you might have.
+44 (0)1752 764879; +44 (0)7458 052113; D-PACT@plymouth.ac.uk
Ways to make air travel a positive experience for people with dementia
Air travel can be a problematic experience for people living with dementia. A new research-informed booklet outlines the barriers they face — and how to overcome them.
People with dementia want to continue living life, their way, for as long as possible,” explains Ian Sherriff, BEM, Academic Partnership Lead for Dementia, University of Plymouth. “That’s why issues, such as accessible air travel, have become ever more important.”

Air travel challenges for people with dementia
Unfortunately, for some people with dementia, their experience of airports and air travel can be so unpleasant that they, and their carers, vow never to fly again. But now, a new researchinformed document aims to change that.
‘Improving the Accessibility of UK Air Travel for Passengers with Dementia and Other Non-Visible Disabilities,’ was produced by Sherriff and occupational therapists Dr Kate Turner and Dr Alison Warren from the
University of Plymouth — outlining the challenges that people with hidden disabilities may face when flying. These include being publicly embarrassed and disrespected; being offered a generic wheelchair service for assistance; and struggling to interpret signage.
Better staff education and awareness
As Chair of Prime Minister’s Dementia Air Transport Group (PMDATG), Sherriff has collaborated with the Civil Aviation Authority (CAA), the aviation industry, researchers and people with dementia to introduce guidelines — now implemented by all UK airports and airlines — for assisting passengers with hidden disabilities.
The document builds on the work of PMDATG and covers five areas: poor societal expectations; individual rights; physical barriers; aviation staff unawareness; actively including people living with dementia. It also
includes positive steps that can improve air travel accessibility.
Travel experiences can be ruined because a person’s condition has not been understood by airport workers and cabin crew. “Aviation staff may question if someone with dementia is even able to board an aeroplane,” says Sherriff. “The answer: yes, they can — and they have the absolute right to do so. It’s a matter of understanding their needs to make their experience a positive one.”
There is evidence that the research has made a difference. “This work made the impossible possible,” insists Dorothy Tudor, former carer of a person living with dementia. “We started flying to our holiday destinations again.”
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 05 MEDIAPLANET
PAGE WRITTEN BY Tony Greenway
Paid for by University of Plymouth
INTERVIEW WITH Professor Richard Byng Professor in Primary Care Research/PenARC Deputy Director, University of Plymouth
INTERVIEW WITH Dr Tomasina Oh Associate Professor, Dementia Care Programme Lead (Research), University of Plymouth
INTERVIEW WITH Ian Sherriff BEM, Academic Partnership Lead for Dementia, University of Plymouth.
INTERVIEW WITH Dr Alison Warren Associate Professor of Occupational Therapy, University of Plymouth
“ Scan the QR code to
more.
INTERVIEW WITH Dr Kate Turner Lecturer in Occupational Therapy, University of Plymouth.
find out
CONTRIBUTION FROM Hannah Wheat Senior Research Fellow, Philosophy of Medicine (sociology) PhD, University of Plymouth
How greater awareness can reduce the risk of dementia
Approximately 55.6 million cases of dementia globally could be delayed or reduced. Alzheimer’s Disease International describes ways to reduce your risk of developing dementia through its World Alzheimer Report.
The global impact of dementia
World Alzheimer Report 2023
BY
Dementia is now the 7th leading cause of death globally and the leading cause of death in the United Kingdom. Globally, 55 million people are living with the condition, a number set to increase to 139 million by 2050. This broadly translates to one person developing the condition every 3 seconds. Increasing evidence is suggesting that by addressing 12 common risk factors, up to 40% of the cases of dementia could be delayed or prevented equating to 55.6 million cases globally by 2050. This is by no means insignificant. Through increased awareness, it is possible for everyone to have an impact and potentially delay or reduce their chances of developing the condition. Of course, governments must play their part too.
World Alzheimer’s month
Every September, Alzheimer’s Disease
International and its global federation of over 120 members, organise the global awareness raising campaign, World Alzheimer’s Month. This year’s campaign aims to raise awareness and to challenge the stigma and discrimination which still surrounds the condition, with a key focus on the often small lifestyle changes that can have a significant impact on living longer, healthy lives.
While knowing the risk factors for dementia is important, the broader question remains on what tangible steps can be taken to reduce risk. While there is no magic bullet for dementia, there are steps that individuals can take to reduce their risk, including slowing down condition progression, following a diagnosis.

Evidence from the World Alzheimer Report 2023 has shown that exercise such as walking, bike riding, even dancing can help to reduce your risk of developing dementia. Just as it is important to maintain physical health, both social and mental stimulation are other ways we can reduce risk, including by maintaining social connections, learning a new language or challenging yourself with crosswords.
From a public health perspective, there are active ways in which governments must intervene with risk-reduction strategies. Increasing evidence suggests that providing hearing aids, for those with hearing loss, is a cost-effective measure to reduce a person’s risk of developing dementia. Other risk factors such as air pollution and low education are less simple to tackle, and governments and policymakers must do more to protect their constituents.
This World Alzheimer’s Month, we hope that all individuals will feel empowered to #ReduceRiskNow and to know that it is #NeverTooEarly or #NeverTooLate to start.
Stopping memory loss: how to use AI to diagnose and treat dementia early
Molecular and cellular changes to the brain are known to start decades before symptoms are apparent. One of these first steps is the overproduction and deposition of the amyloidpeptide in the brain. We are currently focused on advancing an amyloid- –an oral drug candidate, PK051, that can break up deposits of amyloid- .
Various forms of dementia
Dementia is the end result of many different diseases, such as Lewy body dementia, Parkinson’s and, most importantly, AD. By differentiating these, we can give the right treatments to the right patients. Memory tests, brain scans or analysing cerebrospinal fluid from a painful lumbar puncture struggle to differentiate between these forms of dementia.
Measuring biomarkers and patient information



Our novel dementia diagnostic measures levels of various biomarker proteins in blood, including amyloid- and forms of Tau, a second key protein in the progression of AD. Measuring just one or two of these biomarkers is inadequate for diagnosis.
However, when multiple measurements are combined with patient information — such as age, sex, ethnicity and genetics — using artificial intelligence (AI), we can accurately distinguish between different types of dementia and determine the severity of the disease. All that is needed is a drop of blood from a fingerpick.






Determining appropriate treatment and dosage
AI can also identify which biomarkers are most important for diagnosis. If we know what the culprits of the disease are, we can precisely target the disease with the right drug and dosage. This would enable large cost reductions for health providers and eliminate the need for invasive procedures, such as cerebrospinal fluid collection, to determine appropriate treatment.
We now know that it is crucial to look at a range of proteins on red blood cells to give an accurate Alzheimer’s diagnostic. If we do this, we may be able to use the new drugs that are now becoming available to head off dementia before it even starts.
“The results from the biomarker study indicate that it is not only possible to differentiate patients based on Amyloid positivity but also on the level of disease severity,” says Dr Bob Smith, Clinical Director of PharmaKure. AI-generated algorithms can be used as a ‘MOT test’ every five years from our 40s to monitor these biomarkers and treat patients in the early stages of the disease.


06 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
WRITTEN
Paola Barbarino Chief Executive Offi cer, Alzheimer’s Disease International
Find out more at pharmakure.com Paid for by PharmaKure
While there is no magic bullet for dementia, there are steps that individuals can take to reduce their risk.
Diagnosing and treating Alzheimer’s disease (AD) at its earliest stages is critical to stop the disease before severe memory loss takes place.
WRITTEN BY Dr Farid Khan Founder, PharmaKure
WRITTEN BY Professor Andrew Doig Co-Founder, PharmaKure; Professor of Biochemistry, The University of Manchester
advancing
Circadian lighting system explores ways to keep people with dementia safe and happy
Trials are underway to discover the extent to which circadian lighting systems can reduce levels of anxiety, stress and agitation in people with dementia.

Circadian lighting, which aligns the body to natural daily cycles, helps reduce anxiety and stress and can offset a condition referred to as ‘sundowning.’ While undergoing trials, early evidence suggests a positive impact of this lighting approach, also known as human-centric lighting.
Benefits of circadian lighting approach
Circadian lighting systems follow the natural sleep/wake cycles of the circadian rhythm — our 24-hour internal clock. The Society of Light and Lighting defines it as ‘lighting systems, which adapt to the changing needs of an individual throughout the day to allow them to receive the varied spectrum and quantity of light in relation to their natural circadian rhythm.’
In humans, signals from the eyes tell the hypothalamus part of the brain when it is day and night and control the amount of melatonin and serotonin released to correlate sleepiness with darkness and alertness with light. Dementia design expert Dr Pamela Topping says a balanced cycle reduces stress and anxiety, leading to greater contentment.
Reduced sundowning and improved staff environment
Circadian lighting can also reduce ‘sundowning,’ where care home residents may become agitated and restless as evening approaches. Altering the early evening light makes residents much calmer, insists Topping, which creates a calmer working environment for staff. “Residential homes have a high percentage of staff turnover, and it can be difficult to keep staff in positions, as dementia is a very challenging condition,” she adds.
The pioneering system is easily installed in all areas of a property, such as bedrooms, day rooms, bathrooms and nurse stations, as well as communal areas. Batteryless, kinetic switches on the walls connect to lighting via Bluetooth without cabling. “Nurses and caring staff are very much the focus of the lighting as well,” says Topping.
Three elements of the lighting system
Her co-founder, Lloyd Crawford, is an established lighting expert in Northern Ireland, specialising in industrial, commercial, exterior and healthcare sector lighting.


Topping trained as a nurse, then studied 3D design, and obtained a master’s in design and a PhD in design for dementia.
As Fellow of the Society of Light and Lighting, Crawford states that the three elements of the Skyjoy system are: (1) circadian lighting, (2) intelligent sensing and (3) cloud-based artificial intelligence (AI).

The innovation is about better replicating daylight in locations, such as nursing homes and care facilities, where people may spend time away from daylight. “It has been demonstrated that circadian lighting improves wellbeing, reduces anxiety and stress; and that has a knock-on benefit on staff and families of people with dementia,” he explains.
Lynne Green of Belfast Central Mission, manager of Kirk House, agrees: “In the relatively short time the lights have been installed, we can already see improvements in the wellbeing of the residents.”
Intelligent and discreet sensors
The intelligent sensors within every lighting do not record images but sense residents’ movements and collect data on patterns of behaviour. Data gathered from the sensors can provide research value for care homes as well as for academics, clinicians and architects who are designing nursing homes. Through its AI component, it will improve the performance of the circadian lighting and even has the potential to recognise falls and alert carers.
Lighting system based on evidence
Crawford says one trial in a nursing home in Northern Ireland is now moving into a longer-term assessment while another has started in a sheltered dwelling scheme. Skyjoy is working with Ulster University to produce evidence-based research with the system undergoing a qualitative and quantitative assessment.
The company has been shortlisted for the Longitude prize on Dementia and received a SHAPES award – a Europe-wide project supporting innovative technologies for smart and health ageing. While acknowledging there is still further research required, such as how people react to daylight in different parts of the world, Crawford believes circadian lighting systems will improve the lives of people with dementia by optimising their environment.
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 07 MEDIAPLANET
Find out more at skyjoy.co.uk
Paid for by Skyjoy
INTERVIEW WITH Dr Pamela Topping Co-Founder, Skyjoy
INTERVIEW WITH Lloyd Crawford Co-Founder, Skyjoy
WRITTEN BY Mark Nicholls
Carers need more support to weather the cost of living crisis
Caring for a loved one who has dementia can cause fi nancial hardship. However, there is support available that may help.
Managing the current cost of living crisis is especially difficult for unpaid carers supporting loved ones. Carers UK research reveals that one in six unpaid carers are in debt because of caring; the proportion unable to afford their utility bills has doubled in a year.
benefits or receiving the right support. Carers may be eligible for benefits such as Carer’s Allowance for themselves; Attendance Allowance on behalf of the person they care for; Carer’s Credit to count towards their pension; or other types of support.
BY
Increasing costs of being a carer
Carers often have heightened expenses as a result of their caring role. For example, increased heating bills to keep a relative with dementia warm and safe or transport costs taking them to medical appointments.
Those who care for family members with dementia may also face expenses related to nutrition and supporting the person they care for to maintain a healthy weight. Often caring for many hours — sometimes around the clock — some find it difficult to stay in paid work. In the UK, 600 people a day leave the workforce to care. Given the pressures, it’s essential that carers know where to look for support when it’s available.
Where carers can find support
Carers Week 2023 research revealed that 73% of those who have provided unpaid care did not identify themselves as carers. This means carers may not be claiming relevant
A Carer’s assessment by the local authority could help a family member supporting a relative with dementia identify practical support for them, looking at the impact caring has on their life and what support or services they could benefit from.
Ways to balance life and caring
While rewarding, caring for a family member with dementia can be physically and emotionally draining. Breaks are essential to prevent carer burnout and enable carers to be able to fulfil their caring duties safely. It’s also important that carers, where possible, try to dedicate some time to looking after their own wellbeing — whether that’s getting out for some fresh air or reading a book.
It’s worth carers in employment checking whether their employer has carer-friendly policies in place to help them manage work and care, including flexible working.
Employees in the UK are set to benefit from The Carers Leave Act which, when in force, will provide a statutory right to up to five days of unpaid carer’s leave.

08 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
More information about benefits and support for carers can be found at carersuk.org/ help-and-advice/
WRITTEN
Helen Walker Chief Executive, Carers UK
While rewarding, caring for a family member with dementia can be physically and emotionally draining.
In the UK, 600 people a day leave the workforce to care.
Two breakthroughs in dementia research that could lead to an improved patient experience
Scientists and researchers are making big steps forward in dementia diagnosis and treatment. Their findings could positively impact the lives of people with the condition.
For Professor Claude Wischik — Co-Founder, Chairman and Chief Executive of TauRx Pharmaceuticals, global leader in tau-based Alzheimer’s disease research — there is now hope for people living with dementia. “The question now is how long it will take to open the door, and we’ll work with regulators to achieve this.”

Digital breakthrough in dementia diagnosis

Two advances could revolutionise dementia diagnosis and treatment. First is the use of digital diagnostic tools to streamline the patient experience. Second is a new treatment, which can slow progression of brain damage caused by the disease. Together, these breakthroughs hold potential to improve outcomes and reduce the
burden on the health system.
“Modern technology, such as phones and tablets, can support diagnosis in the comfort of people’s homes,” explains Professor Bjoern Schelter, CEO of GT Diagnostics and Chief Analytics Officer at TauRx.


“For example, GT Diagnostics has developed a wellbeing app that reveals people’s cognitive health status in minutes. This can be connected to technologies used by healthcare professionals and, with other data, support a more timely diagnosis.”
Blood-based biomarkers enabling early personalised treatment

The second breakthrough is a new drug in development that has shown an effect on readily accessible blood-based biomarkers, which aid the detection and diagnosis of
Alzheimer’s disease and monitoring of its progression. Because biomarkers provide evidence of an individual’s neurodegeneration, treatment can be personalised and therefore more effective.
In people with Alzheimer’s disease, increased amounts of one such biomarker in the blood — Neurofilament Light Chain (NfL) — measure how much damage has been done in the brain and corresponds to decreased cognition and function.
“We are testing a drug targeting the tau pathology of Alzheimer’s. This has now been shown to reduce the increase of NfL levels in the blood in people with the disease, which means we’ve been successful in slowing disease progression,” says Professor Wischik, noting that his company is now in discussions with regulators about the treatment.



Earlier detection for better outcomes
Research in this field is generating a huge amount of hope and enthusiasm, says Dr Sonya Miller, Head of Medical Affairs at TauRx.

“Companies investigating different aspects of dementia treatment are now seeing their work come to fruition,” she notes. “That’s extremely positive because, like all diseases, several treatment approaches will be needed. On our part, we hope that by identifying people early enough in the process and treating the underlying tau pathology, we can positively impact people’s lives.”
and calculates a score between 0–100. The test, which accounts for age and sex, also shows a ‘healthy’ reference range, which is 55–80, to help users judge their performance.
Removing barriers to seeking assessment
A mobile app to test for cognitive decline could help streamline the process of diagnosing people who may have Alzheimer’s or dementia.
Results from five-minute home tests may highlight deteriorating cognitive health and enable healthcare professionals to make an early assessment.

Dementia detection with an app


Dr Linda Sommerlade, Head of Operations at GT Diagnostics, says home monitoring adds an important dimension to dementia assessment. “Cognitive decline happens slowly; and if there is no way to measure it, it takes longer to realise that something has changed,” she explains. Measuring subtle changes in brain health via a mobile app can facilitate an early identification of memory problems, leading to timely treatment.

Memory test for cognitive changes


GT Diagnostics, which aims to transfer research in Alzheimer’s and dementia diagnosis into clinical practice, has created a cognitive health app called HiPAL. It is a memory test to measure a person’s cognitive health status. “It is about remembering objects and their locations,” Sommerlade explains. “It is designed to be difficult, so even a healthy person will have trouble getting everything correct.”
The test captures and measures small changes in memory performance. “If the test is too easy, and half the population always get a full score, you won’t notice if something changes.” The test is selfadministered and can be started at any time. An algorithm checks the answers


Implementation into clinical practice is expected early next year in the UK, and a version for medical professionals is already available in America. However, Sommerlade notes that there can be stigma around memory loss that may delay an individual seeking help, and many people still believe memory problems are part of normal ageing. Doing the test at home reduces the hurdle of deciding when to go to the doctor.






Offering reassurance and remote monitoring




Patients, clinicians and healthcare systems can benefit from home monitoring of cognitive deterioration at a time of growing incidence of dementia. It can offer reassurance to people if the score is good or lead them to seek an earlier appointment if scores are not so good. “For healthcare systems, it will streamline the process,” Sommerlade insists. “If patients have data to hand, it enables doctors to form an opinion more quickly and decide on the next step.” After diagnosis, the app enables patients to track progress and cognitive changes.

A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 09 MEDIAPLANET Find out more at gtdiag.com
Paid for by GT Diagnostics
A simple mobile app can help people monitor changes and detect dementia
WRITTEN BY Mark Nicholls
INTERVIEW WITH Dr Linda Sommerlade Head of Operations, GT Diagnostics
INTERVIEW WITH
Professor Claude Wischik Co-Founder, Chairman and Chief Executive, TauRx Pharmaceuticals
INTERVIEW WITH Professor Bjoern Schelter CEO, GT Diagnostics and Chief Analytics Offi cer, TauRx Pharmaceuticals
INTERVIEW WITH Dr Sonya Miller Head of Medical Affairs, TauRx Pharmaceuticals
Find out more at taurx.com Paid for by TauRx
WRITTEN BY Tony Greenway
Pioneering a new era for dementia care
Every three seconds, someone, somewhere is diagnosed with dementia. Until recently, no treatments were available that could slow, let alone arrest, these cruel conditions. Now, we appear to be entering a new era for dementia care.
Accelerating development of dementia treatments
Laurence Barker, PhD Partner, Dementia Discovery Fund




Three new drugs — aducanumab, lecanemab and donanemab — have shown real potential in phase 3 clinical trials to delay cognitive deterioration in early-stage Alzheimer’s. However, these drugs are not cures for dementia. Though aducanumab and lecanemab were recently approved for sale in the US, their clinical impact is modest. Nevertheless, they demonstrate that meaningful progress is being made in the battle against Alzheimer’s disease. Launched in 2015 in the UK, the Dementia Discovery Fund (DDF) is the world’s largest family of dementiafocused venture capital funds, with over $500 million in committed capital. We aim to accelerate the arrival of a new wave of innovative dementia treatments. We have now made our first investment out of our second global impact fund, as we continue to invest in and create early-stage biotech companies seeking to revolutionise treatments for dementia.

A collaborative approach targetting impact and returns
Our approach is both ‘deep’ and ‘diverse.’ We draw insights from the leading edge of scientific enquiry and work with government entities, pharmaceutical companies, advocacy organisations, philanthropists and charities to transform knowledge into real-world impact. Our 17 active portfolio companies bring state-of-the-art technology to bear on Alzheimer’s disease and other dementias.
Rejecting the perceived trade-off between social impact and financial returns, we pursue a ‘dual bottom line,’ adding rigorous impact criteria to strict investment criteria. Given the immense unmet demand, any impactful therapy should generate both significant returns and societal benefits. We believe that two lessons — both core to DDF strategy — must now be applied to dementia.
Lesson 1: precision medicine
Technological advances (eg. in genomics, biomarkers and AI) enable pinpoint diagnosis and treatments tailored to specific patient groups. Dementia drug developers must now put these powerful new capabilities into action. In the past, trial patients were selected solely based on symptoms, ignoring dementia’s diverse causes. As a result, clinical trials were often expensive and prone to fail.
DDF portfolio company Therini Bio take a more precise approach. Their novel drug targets fibrin — a blood protein that causes inflammation when it escapes into the brain, a hallmark of Alzheimer’s. By measuring fibrin levels in brain fluid, Therini focus their trials on patients likely to benefit from treatment.
Lesson 2: no cure in a single drug
Potent, single therapies for other diseases, including specific cancers (eg. immunotherapies) and cardiovascular disease (eg. cholesterol or blood pressure medicines) can be transformative for some patients but do not serve the majority. Much
of the broader progress in treatment has come from prescribing several therapies in combination.
A similarly multi-pronged approach is crucial for dementia. Lecanemab, aducanumab and donanemab target ‘toxic amyloid plaques’ in Alzheimer’s disease brains. Clinical trial results suggest that clearing amyloid plaques alone is insufficient, however. But combining these drugs with those addressing other facets of disease, such as Therini’s brain inflammation drug, should deliver more substantial benefits. We seek complementary approaches and synergies throughout our portfolio.
Pioneering investment in dementia
Dementia research and development was underfunded and underachieving for too long. Thankfully, that is changing, as additional capital is invested in this problem. New Alzheimer’s drugs provide firm evidence that the dementia riddle can be solved. It’s time to usher in a flurry of innovative solutions for what’s arguably the most pressing health challenge of our age. Together, we can reimagine dementia care and enhance life for millions worldwide.
10 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK Find out more at ddf.vc
Paid for by Dementia Discovery Fund
Given the immense unmet demand, any impactful therapy should generate both significant returns and societal benefits.
Jonathan Behr, PhD Partner, Dementia Discovery Fund
Christian Jung, PhD Partner, Dementia Discovery Fund
The glasses use algorithms to recognise the faces of family members and friends, as well as objects in the user’s environment.
People with dementia can live well each day with smart assistive technology
People with dementia could be supported to live more independently for longer with their condition, with the help of an innovative pair of smart glasses.
Ateam from Khalifa University of Science and Technology in Abu Dhabi has designed unique intelligent modular adaptive glasses with high interoperability and comfort (iMAGIC) for people with dementia. They have sensors, a recognition system for familiar faces and objects, a fall detection system and alerts and reminder functions. They can also monitor vital signs including heart rate, body temperature and sleep patterns.
Hands-free solution for dementia
iMAGIC was recently named a semifinalist Discovery Award winner for the coveted Longitude Prize on Dementia. Project leader Professor Mohamed Seghier, Director of the university’s Healthcare Engineering Innovation Centre, says: “People living with dementia can struggle with their environment, so we wanted to create something familiar and hands-free to help them.”
The glasses combine different modules and functionalities with a camera for navigation. It can recognise faces and objects and has sensors that can detect falls and alert caregivers or families. “The glasses can be adapted, depending on the stage of dementia an individual is at,” he adds. “Someone with early signs may be able to live independently compared to someone at a higher stage of dementia where more support is needed.”
Benefits of the smart glasses
Professor Leontios Hadjileontiadis, Chair of the university’s Biomedical Engineering Department, explains that the smart glasses also work when the user is not wearing them. “Even when a person is sleeping, the glasses are awake and provide information about temperature, weather, pollution and aspects that relate to the environment someone is living in,” he explains.
The glasses use algorithms to recognise the faces of family members and friends, as well as objects in the user’s environment. It relays that information in a display before their eyes or orally via a headset. They also have a reminder system, such as when to take medication or contact a caregiver. He adds that the glasses demand very little from the user but provide a lot of benefits.
Helping people with dementia socially Physiological data, collected via sensors around the ear, can be directed to physicians and can identify possible falls. The glasses are a familiar item that a dementia patient could wear naturally. Yet, it reminds wearers of who they are with and where they are while providing important social context.
“It means people with dementia are not isolated but can communicate with people because they use this technology to assist them in their social expression. So, socially and physically, it helps them to keep their quality of life,” says Hadjileontiadis.
Next stage of technology
The Longitude Prize, funded by the Alzheimer’s Society and UK innovation agency Innovate UK, aims to encourage the development of technologies that can help people with dementia retain their independence.
The Discovery Award has given the Khalifa University team an £80,000 grant to design and develop their solution and submit the technology to the next stage of the prize in 2024. Going forward, the prototype smart glasses will be tested on people living with dementia in the UAE; and their feedback will be incorporated into the design.


Retaining independence for longer
The university team — which also includes Dr Aamna AlShehhi, Dr Naoufel Werghi, Dr Hamdan Hamdan and Rayyah Alkhanjari — wants to work with external companies and investors to further develop the smart glasses.
With an estimated 46.8 million people living with dementia worldwide, and this number predicted to double every 20 years, Seghier says it is crucial to find solutions that can help them live independently for longer. “Our main motivation was to develop a hands-free assistive device to make a difference in the lives of people with dementia. On a more personal note, some team members have relatives who are already living with dementia, and this was another driver to start this project.”
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 11 MEDIAPLANET Find out more at ku.ac.ae
Paid for by Khalifa University
INTERVIEW WITH Professor Mohamed Seghier Director, University’s Healthcare Engineering Innovation Centre, Khalifa University
INTERVIEW WITH Professor Leontios Hadjileontiadis Chair, Biomedical Engineering Department, Khalifa University
WRITTEN BY Mark Nicholls





12 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
We vow not to rest until we have a world where dementia no longer devastates lives.
~Kate Lee, CEO, Alzheimer’s Society


































































 Paola Barbarino, Chief Executive
Paola Barbarino, Chief Executive