3 minute read
Paediatric IBD –Crohn’s and colitis
By Dr Ajay Sharma, Paediatric Gastroenterologist, Perth
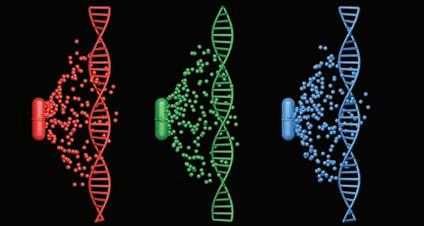
The incidence of Crohn’s disease (CD) and ulcerative colitis (UC), is increasing among children and impinges upon their growth, education and social wellbeing. Because high rates of IBD onset occur in childhood and adolescence, monitoring the incidence of paediatric IBD may reflect changing trends in IBD demographics. Environmental triggers, (e.g. dietary antigens, infections) combined with specific IBD genes (most are polygenic), can lead to a chronic activation of the mucosal immune system, recognised clinically as CD or UC.
Growth failure, common in children and adolescents with CD, may be the only presenting symptom. The pathogenesis of growth failure in IBD includes malabsorption, increased caloric needs, suboptimal intake due to anorexia, and gastrointestinal losses. This affects growth. However, delayed puberty, corticosteroids, and proinflammatory cytokines such as TNFα and interleukin 6 are also responsible for growth failure in this patient population. IBD involving the colon (UC or CD) most commonly presents with diarrhoea and rectal bleeding. CD involving the ileum and/or cecum tends to present more subtly, with abdominal pain, weight loss, fatigue, and fever. Perianal fistulae and infections are seen in CD, but not UC. Extraintestinal Key messages
The incidence of IBD is increasing in children Symptoms may be non-specific Treatment aims to optimise growth and quality of life.
manifestations (e.g. erythema nodosum, arthritis) are seen in both. Definitive diagnosis of IBD is established by a combination of radiography, endoscopy, and histology. Differentiating CD from UC can be difficult, especially if the IBD is limited to the colon.
Over time, the natural history of the two diseases differs. Patients with CD will frequently develop complications such as strictures, abdominal abscesses, or perianal fistulae, whereas patients with UC continue to have bloody diarrhea as their principal manifestation. Treatment goals are to maximise therapeutic response, adherence and psychological support, minimise toxicity, improve quality of life, promote physical growth and prevent complications. Improved growth and development, without the side effects of steroid therapy, make exclusive enteral nutrition (EEN) a better first-line therapy in children with active CD. With mild-to-moderate levels of disease activity, therapy includes 5 ASA (amino salicylates), antibiotic therapy, corticosteroids and enteral nutrition.
Immunomodulators (e.g. Azathioprine, methotrexate) have a role in maintenance. Biologics (e.g. Anti TNF-Infliximab, and adalimumab) are approved for treatment of CD in children. Indications for surgery in CD include failure of medical therapy, intestinal complications (e.g. obstruction, perforation, intraabdominal abscess, fistula) growth failure in children, and carcinoma. 5-ASA therapy is beneficial in inducing remission in UC and can be used in maintenance. AZA is effective maintenance therapy for those who have failed or cannot tolerate 5 ASA and those requiring repeated courses of steroids. Biologics are used in moderate to severe UC or failed steroids and AZA. Approximately third of patients with UC undergo surgery within the first 10 years of their illness.
Attention to emotional and family implications of chronic illness, and maximising the growth and nutrition, is an integral part of the long-term care of the paediatric patient.
Author competing interests – nil
N E W A D D R E SS & N A M E P r e v i o u s l y “ M a y l a nd s C o m p o u n d i n g ”
‘Problem Solvers’ of Pharmaceuticals We specialise in customised, compounded medicines
Enquire about our Pick-up point pharmacies, all around the Metro area
BioHRT .Dental .Dermatology .Hospice .Nutrition .Paediatric .Pain .Sports www.clinicarecompounding.com.au MAYLANDS 245 Guildford Road, Maylands P: (08) 9370 4410 F: (08) 9471 7115 E: maylands@clinicarecompounding.com.au BALDIVIS Unit 1/7 Minden Lane, Baldivis (opp. Stockland Baldivis) P: (08) 9523 2274 E: baldivis@clinicarecompounding.com.au