2 minute read
Non-invasive prenatal testing (NIPT
By Dr Adeline Tan, Gynaepathologist, Perth
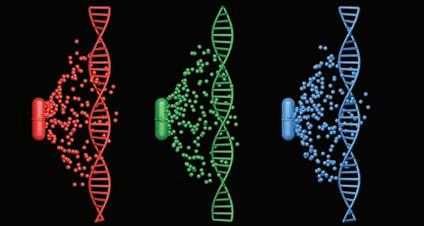
In recent years, there have been many advances in medical technology and women’s health. The connection between baby and mother begins from the very onset of conception, where fetal circulating free DNA (cfDNA) can be derived from the fetus and placenta within the maternal circulation.
The ability to analyse the likelihood of a number of genetic disorders by ‘simply’ detecting fetal DNA or, more accurately, fetal fraction (the proportion of cfDNA) within maternal blood with non-invasive prenatal testing (NIPT) has been a welcomed addition in providing more information for patient management. NIPT is performed between 10 and 14 weeks of gestation, when there is sufficient fetal cfDNA in the maternal circulation for analysis (as early as 10 weeks of completed gestation). The test can assess the chance of Trisomy 21 (Down syndrome), Trisomy 18 (Edwards syndrome) and Trisomy 13 (Patau syndrome), plus 22q11.2 deletion (DiGeorge syndrome) and sex chromosome abnormalities. Key messages
NIPT is performed between weeks 10 and 14 It is not a replacement for conventional screening Specific chromosomal abnormalities can be detected with NIPT.
While many genetic conditions are familial, these conditions can occur in any pregnancy and its probability increases with age. If there is sufficient fetal DNA in the sample, NIPT can either confirm that the proportion of fragments is as expected (low-risk result) or detect a change in proportion (indicating that the fetal cfDNA is high risk for an abnormality). Any abnormal result will be correlated with ultrasound and other first trimester screening results. Referral to genetic counselling and further testing such as rapid FISH for aneupoloidy of chromosomes 13, 18, 21, X, Y or karyotyping on amniotic fluid and chorionic villous sampling (CVS) is required for confirmation. Should a woman have conventional first trimester screening and ultrasound as well as NIPT testing? While NIPT is more accurate than conventional first trimester screening, conventional screening still has a place in patient care. It is important to note that NIPT is an optional screening test and not a diagnostic test. False positive and false negative results, although rare, can occur.
NIPT is not able to test for fetal viability and may provide a valid result despite fetal demise (based on the analysis of any residual fetal DNA). Hence, an early ultrasound at 8-11 weeks is still required for dating and checking viability of the fetus (or detecting multiple gestation). The two tests measure two different things: NIPT evaluates cfDNA from specific chromosomes, while first trimester screening assesses anatomy and biochemical function. However, NIPT is highly accurate and may preclude the need for more invasive testing by minimising the risk of a false positive result.
Author competing interest – nil
MBBS FRCS AMC FRACS
South Perth Hospital is pleased to advise Professor Richard Naunton Morgan, General Surgeon, has commenced a General Surgical service.