
14 minute read
Familial hypercholesterolaemia 5
Navigating diabetes medications
By Dr Andrew Klimaitis, Physician, Duncraig
Recommendations on the use of hypoglycaemic medications are getting clearer. Metformin is still first-line. Gliflozins (SGLT2s) and gliptins (GLP1s) improve survival though the latter require injections. DPP4s are safer than sulphonylureas.
This is based on data showing mortality benefit with both SGLT2s and GLP1s, and increasing concern about hypoglycaemia, particularly in the elderly and patients with established vascular disease. Sulphonylureas are the ‘bad guys’ causing both hypoglycaemia and weight gain. DPP4s don’t prevent macrovascular complications, but don’t cause hypos or weight gain. Good diabetic control slows down microvascular complications so there is still a place for sulphonylureas and Acarbose, even without macrovascular benefits. Start with Metformin. There is some mortality benefit and possibly slowing-of-ageing properties.
With any suggestion of cardiac disease, especially heart failure, use an SGLT2. Studies show that gliflozins improve cardiac outcomes just as much in non-diabetics. Cardiologists prescribe them without PBS reimbursement. Gliflozins also preserve renal function in most forms of nephropathy. Their effectiveness with a GFR below 30 is less clear, but they seem to continue helping even without further glucose lowering. GLP1s sell themselves because of appetite suppression and weight loss. Not everyone tolerates them, but it is amazing how prepared patients are to self-inject if they might lose a few kilos. Gliptins reduce vascular complications, particularly strokes. This hasn’t yet been generalised to non-diabetics. Combining a GLP1 (PBS), SGLT2 (around $50 non-PBS), and Metformin maximises weight loss. DPP4s are the best-tolerated agents, particularly in the elderly, but don’t use them (or GLP1s) in patients with a past history of pancreatic disease.
Key messages
Good diabetes control slows microvascular complications Tailor medications to patient circumstances Beware overtreatment in the frail.
Most type 2s exhibit fasting hyperglycaemia. Toujeo (or Lantus) can be given once daily. Start with the same number of units as the average fasting sugar reading. Increase by two to four units weekly until the fasting sugars drop to single figures, eventually aiming for sixes and sevens. Ryzodeg can be used instead (once daily before biggest meal) if postprandial sugars are also elevated. This incorporates a short acting insulin into the regime.
Twice or three times daily regimes can be used later, but many type 2s are fine with once daily insulin. Dulaglutide (used weekly) is not PBS subsidised with insulin, though exenatide (used twice daily) is. GLP1s can mitigate insulin’s weight gain.
Bariatric surgery should be discussed and can have dramatic benefit. Most patients know someone who’s had the operation. Their enthusiasm will generally reflect how things went for that person.
Lastly, don’t overtreat the frail. A study of frail elderly living in the community, but requiring some form of home assistance, showed that maximal survival was at a HbA1c of 8.5%. Patients at 7.5% did worse, roughly equivalent to those at 9.5%. Tighter control presumably caused more hypos which then translated into falls, strokes, etc.
Author competing interests – nil
OBESITY MANAGEMENT (and COVID-19)
Obesity in this era of Covid-19 carries an even greater risk with an increase in hospital and ICU admissions.
Weight management is more important than ever and, as always, we are here to help with a number of surgical and medical options tailored to the individual. We are able to see patients either in person at our rooms at Subiaco, Murdoch, Booragoon or Mandurah, or via Telehealth.
FOR ENQUIRIES/BOOKINGS:
Ph (08) 9332 0066 Fax (08) 9463 6202 Mob 0401 809 255 (Dr Chandraratna) Mob 0413 149 758 (Dr Gong) Mob 0404 758 539 (Dr Kiyingi)
Diabetic CKD management
By Dr Mark Thomas, Nephrologist, RPH
There has been a quiet revolution in the management of diabetic chronic kidney disease (DKD) in the past five years with the advent of Sodium Glucose Linked Transport 2 Inhibitors (SGLT2i’s) and glucagon-like peptide receptor agonists (GLP1Ra’s) finally providing agents with cardiac and renal outcome benefits.
But powerful pills can have powerful side-effects, so patients and health-care professionals all need to know their use – and when to stop temporarily.
Australia-wide surveys historically showed 50% of T2DM patients had either albuminuria or GFR under 60, especially with Aboriginality, diabetic duration over 10 years, Hba1c above 7%, BMI above 30, BP greater than 140/90 and/or
Key messages
Historically 50% with T2DM have impaired renal function New diabetes medications provide renal and cardiac benefits Careful monitoring is important.
smoking. However, no strategies other than ACE inhibitors or Angiotensin Receptor Blockers (ARB) had shown cardio-renal protection in randomised controlled trials.
Between 2007-2013 there were neutral or negative outcomes from intensified diabetic control, combined ACEi/ARBs, endothelin antagonists, DPP4 inhibitors and other therapies. Positive RCT evidence for either SGLT2i’s or GLP1Ra’s has emerged every year since then.
SGLT2i’s prevent the renal proximal tubules recycling filtered urinary sodium and glucose back into the body. This allows overflow when blood sugar levels (BSLs) are raised, but avoids hypoglycaemia when BSLs fall, providing a steady loss of calories for the overweight, and additional sodium loss for the hypertensive.
The resultant salt-rich tubular urine effectively reverses the pathological hyperfiltration seen with diabetes or obesity with a predictable average 3-7ml/min fall in eGFR within two weeks of starting. GFR stabilisation follows, with 20-30% less likelihood of death, acute or chronic kidney

We are proud to announce the opening of Aurora Imaging providing comprehensive care
Obstetric and gynaecological ultrasound Maternal Fetal Medicine Reproductive Genetic Counselling
Our expert team comprises:
Professor Jan Dickinson Dr Scott White Dr Shin Lee Dr Winston Almeida Dr Heidi Hughes-D’Aeth Dr Chhaya Mehrotra Ms Karen Harrop
Our cohesive experienced on-site team are all specialist trained in women’s health and happy to provide telephone advice to our referring doctors.
disease or heart failure over the next five to seven years. Although the glycosuric effect falls when GFR under 45, the CV-renal benefit applies even as GFR falls, and is seen patients already on statins, ACEi or ARBs, and in all patient sub-categories.
There is a predictable risk of glycosuric bacterial or fungal sepsis in the first two months after initiation, as already applies in diabetics with poor control, suboptimal hygiene or uncircumcised. This is best treated with scrupulous groin and abdominal fold washing, drying and baby powder, and standing ready with pre-emptive cephalexin for dysuria plus clotrimazole for thrush.
The major risk of euglycaemic diabetic ketoacidosis occurs in T1DM (or long-standing T2DM with reduced beta-cell reserve) if SGLT2i’s are continued during reduced fluid or food intake, needing to be ceased three days prior to elective surgery. If not avoided, then it can be identified by pH below 7.3, HCO3 under 15, blood ketones above 0.6 and BSL less than usual expected 25 in conventional DKA and managed by insulin-dextrose infusion until ketones resolved.
A ‘sick day plan’ is needed for every diabetic CKD patient when unable to maintain adequate food and fluid intake: This includes self-monitored weight, BP and temperature; temporary reduction/omission of ACE, ARBs, diuretics, metformin, SGLT2i; check FBC, CRP, electrolytes, LFTs, VBGs, troponin & ketones, and hospitalisations for insulin/glucose infusion if not rapidly improving.
Author competing interests – nil
Now offering video and in person consultations for Neuro Spinal Surgical Services
Neurospine Institute is a multi-disciplinary specialist practice offering advice and treatment across the full range of spine and brain conditions.
Also offering: Spine Focused Physiotherapy Treatment Service for patients in need of treatment for back and neck pain, rehabilitation or recovery following injury or spinal surgery.
Dr Paul Taylor Spinal Surgeon Spine Surgeon
Dr Paul Taylor Spinal Surgeon Dr Andrew Miles Neurosurgeon
Dr Paul Taylor Spinal Surgeon Dr Michael Kern Neurosurgeon
Dr Paul Taylor Spinal Surgeon Dr Greg Cunningham Spine Surgeon
We welcome Dr Greg Cunningham to the team. Dr Cunningham utilises some of the most advanced techniques in spinal surgery available worldwide and is available now to see privately insured patients.
3 CONVENIENT LOCATIONS
Plus regional clinics in Mandurah, Vasse, Albany and Geraldton. Murdoch Suite 77, Level 4 Wexford Medical Centre 3 Barry Marshall Parade Murdoch WA 6150 Perth Suite 7, Level 4 140 Mounts Bay Road Perth WA 6000 Wembley Suite 10, First Floor 178 Cambridge Street Wembley WA 6014
1800 NEUROSPINE (1800 638 767) (08) 6147 8200 info@nsiwa.com.au nsiwa.com.au
Genea Hollywood Fertility provides a comprehensive individualised range of fertility treatments for Western Australians.
Our specialist team has up to 30 years’ experience in fertility treatments.

Our patients have access to Genea’s world leading science.
All patients have individualised assessment and treatment
Genetic testing is available where needed
Our treatment charges are transparent
Our clinicians, scientists and support staff are committed to achieving successful outcomes.
Dr Simon Turner MBBS, FRANZCOG, FRCOG
Prof Lincoln Brett BMedSc, BSc (Hon, MBBS, FRANZCOG
Dr Julia Barton MBBS, FRANZCOG, FRCOG
Dr Michael Allen MBBS (UWA), FRANZCOG, MRMed
Dr Joo P. Teoh FRANZCOG, MRCP (Ire), MRCOG, MBBCh, Msc (Lon), MD (Glasgow) Subspecialty Repromed (UK)
Genea Hollywood Fertility means high success rates, understanding staff and individual care.
Genea Hollywood Fertility
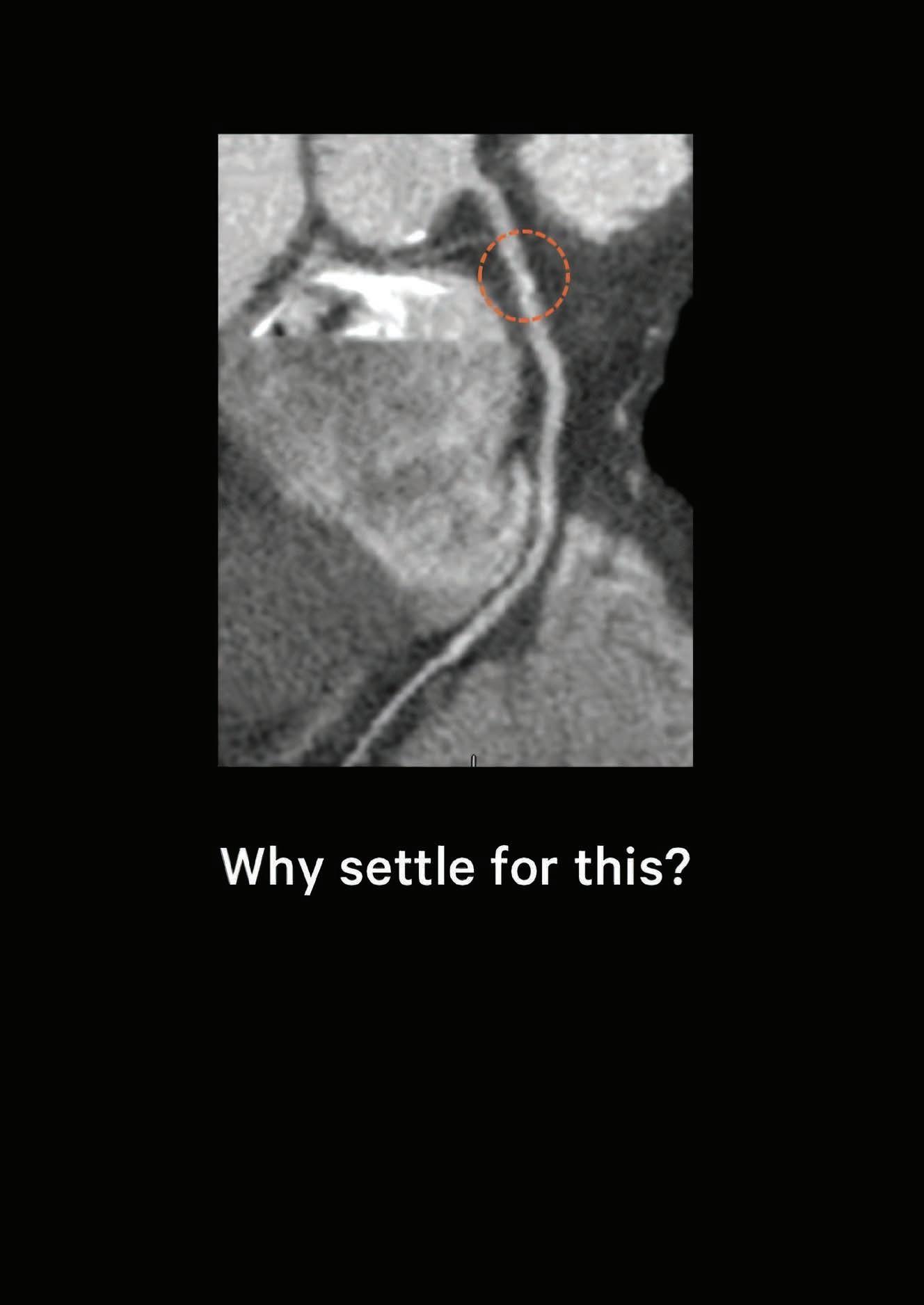
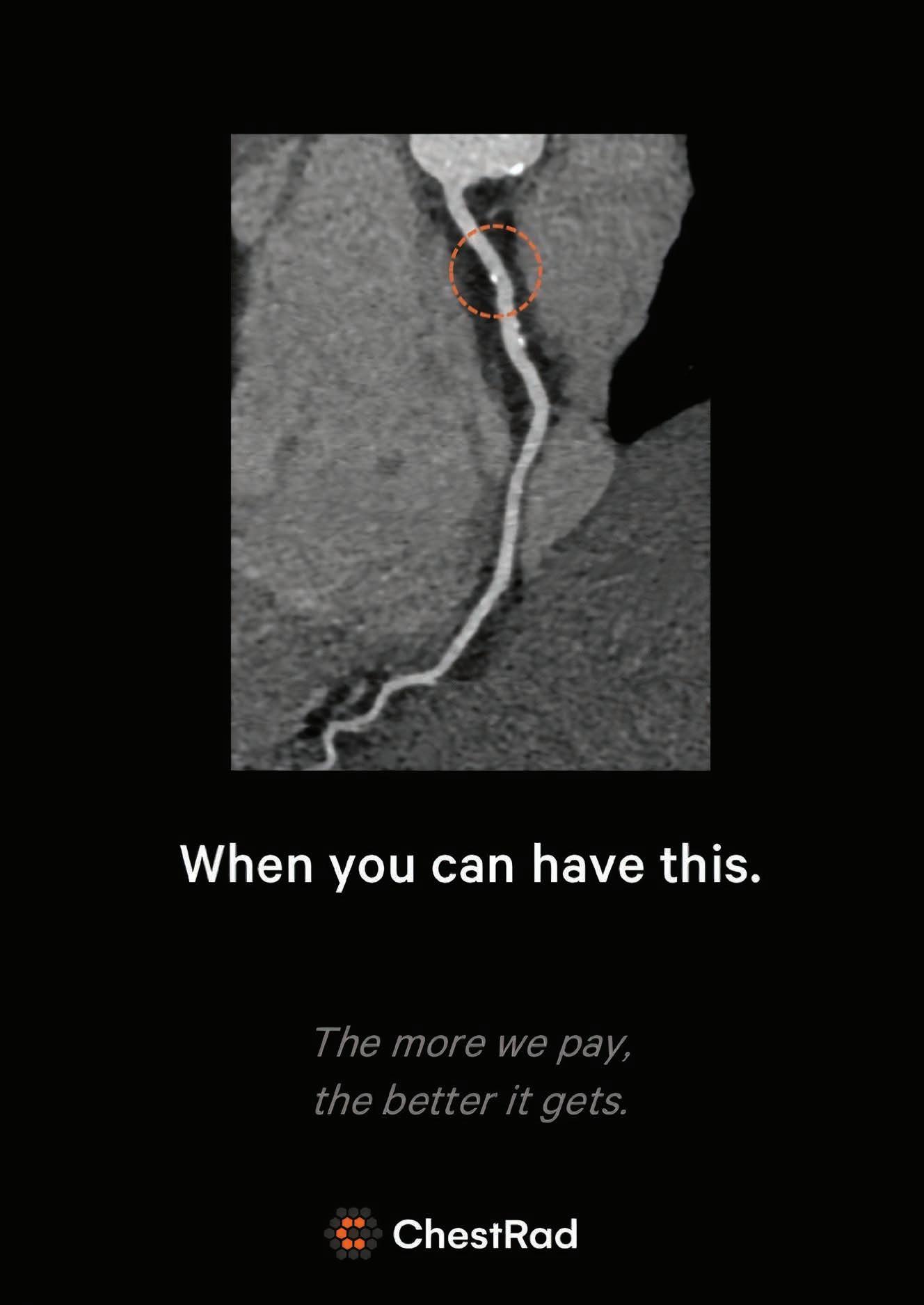
Calcium score and CTCA – which test when?
By Dr Lawrence Dembo, Cardiologist, Murdoch
The coronary calcium score is a powerful risk factor of a future cardiovascular event. Why? Because calcium is direct, visible evidence of coronary artery disease, while the standard risk factors are only risks of atherosclerosis.
An elderly patient with a full house of risk factors and a calcium score of zero has a very low risk. A young patient with no risk factors and a very high calcium score has an extremely high risk of future coronary artery disease. Atheroma occurs with inflammatory changes in the wall of the coronary artery. Over time, some of the inflamed ‘soft’ plaques heal. A byproduct of this chronic inflammation is calcium deposition analogous to a ‘scar’. While the calcium is inert and not dangerous, the amount of calcium correlates with the total burden of coronary atheroma and the risk of future coronary events.
Key messages Calcium score is a powerful risk prediction tool Coronary CT (CTCA) is for diagnosis of equivocal symptoms For symptoms, request CTCA not calcium score.
No IV contrast is required. Set-up takes less than five minutes and scan time is only a few seconds with minimal radiation exposure. The amount and density of calcium in the coronary artery walls is measured to derive a calcium score. Importantly, this test only quantifies coronary calcium and does not define any soft plaque or coronary artery narrowing.
In the asymptomatic, a calcium score of zero implies a very low risk in the short-to-medium term and generally provides reassurance, which is additive to standard risk scores. The risk profile of two thirds of patients will be reclassified from intermediate to low or high risk and may be used to guide the aggressiveness of risk factor management when compared to current risk scores. Up to 15% of intermediate risk patients have non-calcified atheroma despite a zero score which may provide false reassurance.
In symptomatic individuals, a calcium score alone is not indicated. A CT coronary angiogram (CTCA) is recommended as it will visualise non-calcified soft plaque or coronary artery stenosis. Many practices include a calcium score with a CTCA. CTCA is a diagnostic test allowing visualisation of the coronary artery lumen to rule out stenosis and define the presence of vulnerable, soft (noncalcified) atheroma. The amount of plaque seen is also a strong risk predictor. The more plaque seen, the higher the risk.
After sublingual GTN to dilate the coronary arteries, and IV contrast, ECG-guided CT images are acquired. The engineering of specifically designed cardiac imaging CT scanners is quite extraordinary. To minimise blur due to cardiac motion, scans need to be super-fast. Not all CT scanners are the same (a Toyota is not a Ferrari) with significant differences in spatial and temporal (blur) resolution. It’s important to do your homework before referring.
For chest pain that is indeterminate (equivocal chest discomfort) in a patient who is intermediate risk, then the investigation of choice is a CTCA. A normal CTCA effectively rules out coronary artery disease as a cause of the symptoms (specificity ~ 99.9%) and in 8% of cases, defines another cause for the symptoms e.g. lung cancer, pulmonary embolus, hiatus hernia, pneumonia, etc.
A Medicare rebate exists for some CTCAs referred by a specialist. There is no rebate yet for a calcium score.
The Panic of COVID-19 Pandemic
By Prof Sergio Starkstein, Psychiatrist, Fremantle
“It is fear what I fear most”, wrote Michel de Montaigne. Fear in the guise of anxiety or panic is recognised as the second major problem produced by the COVID-19 pandemic, after the infection itself.
While fear has a dramatic impact not only among infected individuals but among the population at large, including healthcare workers, it is still unclear how best to deal with this problem.
Suggestions to reduce anxiety include the consumption of media, keeping to healthy diet, exercise and sleep regimes, to practise mindfulness, and to reach out for support. However, this is putting the cart before the horse. For instance, who can advise on how much and which ‘media’ is safe to consume? Anxiety means to have fear about future events. To avoid future dangers and to appease this emotion most humans want as much information as possible.
One of the non-ethical strategies of some media is to instil fear by producing material with dramatic overtones becoming a magnet of attention. This creates a vicious circle of fearmongering resulting
Key messages
Fear pervades those infected, the ‘at risk’ population, and healthcare providers Simple measures, whilst helpful, are not always easy to implement.
in increased fear which stimulates more consumption of media. Secondly, healthy habits are easy to advise but difficult to implement in the context of high anxiety, especially during quarantine.
A healthy diet and a refreshing sleep are the first victims of this toxic combination. There is poor motivation (and sometimes no physical space) to exercise; and a mindful silent meditation may even increase the monsters of fear when the quarantine results in increasing boredom, a decreasing financial state, loneliness and domestic violence. Finally, reaching out for company is complex while in quarantine, and lonely people may become lonelier, many times ending in despair and sadness. What about fears among health
workers? A recent article in JAMA suggests reducing fear by increasing safety measures, such as those recommended by the Centre for Disease Control. These include wearing PPE (gown, gloves, N95 respirator, a face shield, and, if possible, a powered air-purifying respirator). Add to this careful hand hygiene, and cleaning of workspaces and equipment.
Nobody will argue against these recommendations, but extra measures may add to the exhaustion and frustration of healthcare workers. Conversely, knowing the relevance of PPE but lacking it may increase anxiety among healthcare workers in developing countries.
The psychological morbidity produced by fear cannot be exaggerated yet rational ways of dealing with it in the context of heterogeneous personalities, major differences in the access to material and human resources, and disparate professional abilities remains a matter for deep debate.
– References available on request
Author competing interests – nil
. Specialising in hip, knee, shoulder, foot and ankle . Consulting rooms at SJOG Murdoch Hospital and Mount Hospital . Privately insured, DVA, Workers Compensation and MVA patients welcomed . Medico Legal assessments




PROF PIERS YATES Hip, Knee & Trauma Primary & Revision Arthroplasty Hip Resurfacing A/PROF GARETH PROSSER Hip, Knee & Trauma Primary & Revision Young Adult Hip Hip Resurfacing
MR BENJAMIN WITTE Knee Surgery ACL & Sports Injuries Knee & Hip Replacement Medico Legal MR SATYEN GOHIL Knee & Shoulder ACL & Sports Injuries Arthroplasty & Trauma
MR THOMAS BUCHER Hip & Knee - Primary & Revision ACL and Trauma Gluteal Tendon Reconstruction MR BORIS BRANKOV Foot and Ankle Surger y Limb Deformities Bone Infection, Trauma
MR ANDREW MATTIN Shoulder, Elbow & Wrist Hip & Knee Sports injuries Arthroplasty & Trauma
MR SIMON WALL Hip & Knee-Primary & Revision ACL and Trauma Ilizarov Frames MR LI-ON LAM Knee, Shoulder & Hip Uni Compartmental Knee Knee and Shoulder Arthroscopy ACL and Trauma
MR CHRISTOPHER JONES Hip & Knee Replacement - Primary & Revision Computer assisted Surgery Hip Resurfacing Trauma










