
13 minute read
The COVID long haul
As we all have a break from the intensity of pandemic disaster response, doctor health and wellbeing has never been more important, Dr Sarah Newman writes.
The COVID-19 outbreak remains a once in a 100-year phenomenon, the likes for which doctors and the community were unprepared. We have been living and working in pandemic conditions for some time now, and mostly have assimilated and accepted the necessary actions which have seen successful containment of the disease in Australia (so far).
The psychological impact on health care workers has been profound. Initially, feelings of fear, anxiety and panic, a ‘pre-traumatic’ stress were experienced as we watched the uncontrolled viral spread ravage other countries.
High levels of stress for doctors were created by a range of factors including lack of PPE, financial worries, profound changes to our work practice, and loss of social contact.
Fortunately, the flood of cases we were anticipating did not eventuate. Now, with limited levels of community transmission and relaxation of restrictions, we are taking a breath and looking to the recovery and reconstruction phase of a pandemic. But what psychological implications can we expect in this next phase?
Eventual recovery is likely to be prolonged, especially given real disease control with vaccination is realistically many months if not years away. We are simultaneously needing to look beyond COVID, while being primed to move back into disaster management at a moment’s notice.
better equipped and primed health system to deal with any future waves of disease.
We need to acknowledge as a profession the psychological impact this momentous time has had on us as frontline workers, and not simply dismiss it and return to ‘business as usual’. The psychological impact includes burnout, anxiety, depression and post-traumatic stress. These issues may develop long past the acute period as people are finally able to reflect on their experiences.
Talking about our experiences, for some but not all, can be useful to deal with emotion, possible feelings of shame, guilt and moral injury experienced.
What can we do to be psychologically ready for this period? This is very much a marathon – we, ourselves, need to prepare for the long-term by enacting realistic and sustainable strategies for maximising our resilience and burnout prevention. We also need to support our family, friends and staff members who will also be psychologically vulnerable (even if they appear fine on the surface). At work we need to return to managing our patients’ chronic conditions.
It is important that we stay abreast with reliable, timely information and avoid the toxic influence of social media. Our mindset is important; we are seen as community leaders; our outlook should encourage measured and informed action and instil hope in our patients.
There are silver linings. Many of us will have learnt more about ourselves and our work colleagues, and come closer together as a team. Some work practice changes will have long-term benefits such as telemedicine on a grand scale, which will hopefully advance the way we deliver and service our patients.
The future of COVID remains unknown, and we will only know the outcomes as they unfold. This can leave a feeling of powerlessness, but if we focus on what we can do, manage the situations as they arise, look after ourselves and our colleagues, seek help when needed and have hope for the future, then we are better placed to face new challenges.
If you are experiencing any issues please contact: • Doctors Health Advisory Service 24/7 Advisory Line: 9321 3098 • Lifeline: 13 11 14
See www.dhaswa.com.au for the latest COVID-19 wellbeing resources
The federal government has recently provided funding for improvements in the detection and management of familial hypercholesterolaemia (FH). It heralds an exciting time for the application of precision genomic medicine through collaboration between the laboratory, primary and secondary care. FH is a common inherited disorder of low-density lipoprotein cholesterol (LDL-c) catabolism, leading to increased lifetime LDL-c exposure and premature atherosclerotic cardiovascular disease (asCVD).
FH occurs in 1:250 people, thus there are ~100,000 people with FH in Australia. However, currently less than 10% of these people are diagnosed, with ~90,000 people undiagnosed and under treated. People with untreated FH have a prevalence of asCVD of ~50% in men by age 50 years and ~30% in women by age 60 years. There is strong evidence that early treatment reduces the excess cardiovascular risk associated with this genetic condition.
We currently have very good methods to diagnose and treat people with FH – but the largest challenge in FH management worldwide is to increase awareness and detection of people with FH. A healthy lifestyle including lowfat diet and regular exercise along with lipid lowering with statins and ezetimibe are the cornerstones of therapy. Lipid lowering therapy dramatically reduces the risk of asCVD, and is currently recommended from age of 10 for children with FH.
Genetic testing is the gold standard for diagnosing patients with FH and is additionally important as patients with genetically confirmed FH have a significantly higher risk of asCVD than patients without a pathogenic variant for any given LDL-c, thus allowing personalised treatment. Furthermore, the relatives of a patient with a pathogenic variant are at risk of inheriting the variant. Genetic testing for FH makes cascade testing more accurate and has been demonstrated to be cost effective.
Genetic testing for the initial member of a kindred identified at risk of FH (index case) is funded if requested by a specialist and family cascade testing for the variant in first (50% risk per person) and second (25% risk per person) degree family members will be rebated by Medicare when requested by primary and secondary care clinicians.
Medicare Criteria 73352 Characterisation of germline variants causing familial hypercholesterolaemia, requested by a specialist or consultant physician for a patient for whom no familial variant has been found; and who has any of the following:
Dutch Lipid Network Criteria Score of at least 6, An LDL-cholesterol or 6.5 mmol/L or more in the absence of secondary causes, An LDL-cholesterol of between 5.0 and 6.5 mmol/L with signs of premature or accelerated atherogenesis. 73353 Detection of a familial mutation for a patient who has a first or second degree relative with a documented pathogenic germline gene variant for familial hypercholesterolaemia.
Before the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors were released, the minority of patients with formally
A/Prof Damon Bell MB ChB, PhD, FRCPA, FFSc, FRACP Chemical Pathologist and Endocrinologist
About the Author
A/Prof Bell has expertise in the diagnosis and management of inherited and acquired lipid disorders.
diagnosed FH were able to achieve the desired LDL-c targets (LDL-c <2.6 mmol/L without asCVD or <1.8 mmol/L with asCVD) with statin and ezetimibe therapy.
However, PCSK9 inhibitors can reduce LDL-c by over 50% in addition to statins and ezetimibe, and are available on the PBS for people with FH who meet LDL-c and clinical criteria. The PBS criteria for Evolocumab (Repatha) were revised as of the May 1, 2020, lowering the LDL-c level to >2.6 mmol/L from 3.3 mmol/L for people with FH on maximally tolerated therapy and symptomatic asCVD. Criteria have also been introduced for non-FH patients with symptomatic asCVD and an LDL-c level of >2.6 mmol/L on maximally tolerated therapy, with a streamlined specialist application process and reapplications from all medical practitioners.
Clinipath Pathology and Sonic Genetics have a comprehensive FH service to assist specialists and general practitioners with FH detection, including highlighting patients at risk of FH based on their LDL-c concentrations, offering FH genetic testing incorporating professional pre- and post-test genetic counselling and assistance identifying family members for cascade testing.
References on request


Main Laboratory: 310 Selby St North, Osborne Park
General Enquires: 9371 4200 Patient Results: 9371 4340 For information on our extensive network of Collection Centres, as well as other clinical information please visit our website at www.clinipathpathology.com.au
Burning out
Researchers from UNSW’s School of Psychiatry and Black Dog Institute, led by Prof Gordon Parker, have carried out studies into burnout – one has mapped personality styles which could predispose certain people to burning out and the other has developed a check-list of signs and symptoms by people experiencing it.
While burnout is not currently recognised as a standalone clinical diagnosis, the World Health Organisation officially listed burnout as an occupational syndrome, which can have severe impacts on sufferers’ mental and physical health, while the financial impact of burnout is huge, with stress-related work absenteeism and presenteeism costing Australia $14.81 billion per year.
In one of UNSW’s new studies, the responses from 1,019 people who completed a questionnaire indicated nine other factors commonly affecting people experiencing burnout. These included: anxiety/stress; depression and low mood; irritability and anger; sleep disturbances; lack of motivation or passion; lack of concentration, memory loss or brain fog; withdrawal from others; and physical

symptoms such as aches, headaches, nausea and low libido; and emotional fragility.
Participants included managers, students, teachers, home/child carers, nurses and midwives. While it was open to both males and females, 75% were female.
“The other study also raises intriguing questions about whether more carefree and easy-going people might be less likely to develop burnout due to a ‘protective’ personality style. Perfectionistic and work-focused traits have also been discovered to be the biggest red flags for those developing burnout.
Opioids and Australia
The social and economic costs of extra-medical opioid use to Australia in 2015-2016 was estimated to be 2203 deaths and $15.7 billion, according to a report published by the National Drug Research Institute (NDRI) at Curtin University. The researchers defined extramedical opioid use as the misuse of pharmaceutical opioids and illegal opioids such as heroin.
In the March edition of Medical Forum, we explored extra-medical opioid use and found, much like the NDRI, that it is an issue that runs deep into the community.
How deep? According to the NDRI, 645,260 Australians were misusing pharmaceutical and illegal opioids, while 104,000 were classified as dependent.
Economically, the tangible costs of extra-medical opioid use were reported to be $5.63 billion with $1.08b in healthcare costs, $936m in drug-related crime, $481m in road traffic accidents, $2.48b in premature death, $459m in workplace costs and $194m in a non-defined category including prevention programs. The breakdown of the costs to the healthcare sector were $311m for pharmaceutical treatments, $127m specialist drug treatments, $249m for inpatient hospital treatment, $235m for primary healthcare treatment, $41m in ambulance and emergency presentations, $31m for outpatient services and $85m in other costs.
The authors say the intangible cost of extra-media use of opioids is $10.13b based on the reported deaths.
Flu vax monitored
A pilot program led by UWA, Dr Alan Leeb’s SmartVax, MedAdvisor and the QUT will be monitoring the effects of flu vaccines administered by pharmacists this flu season. When the novel COVID-19 vaccine becomes available, the program could monitor its effects as well.
Supported by a $40,000 grant from the JM O’Hara Research Fund of the Pharmaceutical Society of WA, the program aims to fill a void where no surveillance program exists to monitor the effects of immunisation from in-pharmacy vaccinations.
Central to the project is active vaccine surveillance, which is particularly important for vaccines that change such as the flu vaccine, and for new vaccines. For the first time worldwide, a four-strain flu vaccine specifically formulated for people 65 years and older is available, which will be monitored.
Alan said the project was a gateway to being able to monitor adverse events for any new vaccine at the population level. Patients who receive immunisations at participating pharmacies will automatically be sent text messages to monitor adverse events following immunisation. Pharmacists will then be able to provide support when needed.
BCG and newborns
Telethon Kids Institute researchers working with a global team have identified the mechanism behind one of science’s most enduring mysteries: what makes the 100-yearold tuberculosis (TB) vaccine, BCG, so effective at preventing newborn deaths from diseases other than TB.
Telethon Kids researchers Professor Tobias Kollmann and Dr Nelly Amenyogbe identified a dramatic and rapid increase in neutrophils in mice and babies within three days of BCG vaccination. They first witnessed the phenomenon – known as emergency granulopoiesis (EG) –
in mice, with their global team later validating it in blood samples from newborn babies in West Africa and Papua New Guinea. “It’s been known for a very long time that neutrophils play a very important role in managing sepsis, but until now nobody understood the role of BCG in initiating this critical process,” Dr Amenyogbe said. “It was actually thought to be biologically implausible, however, we’ve not only shown how BCG is involved, but that it kicks off this process almost instantly following vaccination – far more quickly than anticipated.”
Testing Dr Google
With about 80% of Australians searching the internet for health advice and 34% of people attending emergency departments having looked up online their symptoms online, just how clinically effective is the internet?
To answer this question Australian researchers have tested the effectiveness of online symptom checkers and their clinical abilities to accurately diagnose and triage. For the purposes of the research, symptom checkers (SCs) are programs, apps and websites that provide probable diagnoses and triage advice. Researchers tested the diagnostic and triage abilities of 36 SCs on 48 simple non-co-morbid patient vignettes. Ten provided diagnostic and triage advice, while 17 provided purely diagnostic advice and nine were limited to triage advice. Healthdirect was the only Australianspecific SC.
The findings suggest the limited abilities of SCs, with 36% of the patient vignettes correctly diagnosed. SCs were more accurate triaging, with 49% of the patient vignettes receiving appropriate advice, however, the researchers found this advice was particularly risk-averse, frequently suggesting urgent care when not appropriate.
Patient downturn
Figures from the Medicare Benefits Schedule (MBS) reveal what has been suspected for weeks – there
Shoulder tension

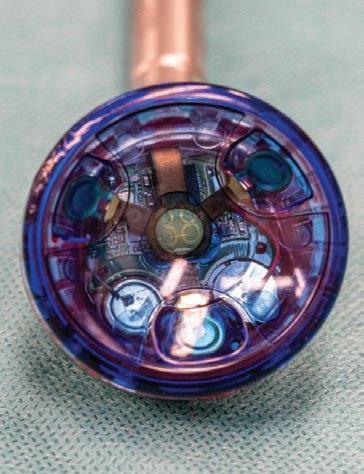
Orthopaedic surgeon Dr Sven Goebel oversaw the first Australian joint replacement shoulder surgery using a computer-aided load balancing sensor recently at Bethesda Hospital. A reverse total shoulder arthroplasty was performed using technology that can intra-operatively quantify joint tension in the shoulder. Once the information is provided by the sensor, it is discarded and the sensor is not permanently implanted in the patient. was a 10% drop in GP visits for the management of chronic disease in March, equating to 96,000 less visits compared to the same time last year. Alongside the impact of COVID-19 on this decline, pathology data from NSW reveal a 28% drop in cholesterol tests being processed in March compared with February.
Heart Foundation Chief Medical Adviser, cardiologist Professor Garry Jennings, said the data also showed an 18% drop in Aboriginal and Torres Strait Islander health checks in March compared to the same time last year.
“A doubling of the number of calls to our Helpline compared to the same time last year tells us that many Australians living with heart disease are worried about their risk of COVID-19 complications, especially as restrictions ease,” he said.
And while GPs claimed more than one million telehealth items in March, only a small proportion of GP visits for the management of chronic disease were delivered via Telehealth. The data also showed an increase in shorter GP visits of less than 20 minutes, compared to the same time last year, which is likely a reflection of increased flu vaccinations.
Telehealth has helped slightly to bridge the gap for longer GP consults of more than 20 minutes, which saw a 9% drop from March last year.
Curtin grants
Curtin University has been awarded $1.29 million in NHMRC grants to develop strategies to predict stillbirth and to investigate ways to eliminate tuberculosis in high-risk countries.
Dr Gizachew Tessema from Curtin’s School of Public Health will develop a strategy to predict the risk of stillbirth, preterm birth and low birth weight by analysing data from more than four million births in WA, NSW, South Australia and the Northern Territory. Dr Kefyalew Alene from Curtin’s School of Public Health and Telethon Kids Institute leads the second research project, which aims to design and implement an innovative approach for eliminating tuberculosis in high-burden countries such as Ethiopia and China.










