Summer


INSIDE: Dean Linda S. Weglicki’s Next Step

2023




MUSC COLLEGE OF NURSING Front Matter n Dean’s Welcome Message 03 Innovation n Game ON n Bridging the Gap n Design Thinking n On Call n Faculty Recognitions n Federal Grants n 2022-2023 Publications 09 Around the College n Our CONStrong Community 04 Table of Contents
On the front cover: Dean Linda S. Weglicki, Ph.D., R.N. looks back on nearly a half century of service as a nurse.

On the back cover: MUSC College of Nursing Faculty and Staff.
Photos by Josh Goodwin.
Lifelines
A publication of the Medical University of South Carolina College of Nursing

VOLUME XV // ISSUE � // ���3
Executive Editor
Linda S. Weglicki, Ph.D., R.N. Professor & Dean
Editor
Jennifer A. Turner
Director of Communications & Marketing
Photographer
Josh Goodwin
Multimedia Content Developer
Graphic Designer
Christopher Berge
Berge Design | bergedesign.com
MUSC Writers
Bryce Donovan
Harrison Huntley
Melissa Varner
Barry Waldman
Alex Walters
MUSC Photographers
Nancy Carney
Zheng Chia
Jonathan Coultas
Sarah Pack
PUBLISHED BY
nursing.musc.edu

SEND COMMENTS TO:
Lifelines Editor MUSC College of Nursing 99 Jonathan Lucas Street, MSC 160 Charleston, SC 29425-1600
turnerja@musc.edu
POSTMASTER: Send corrections to Lifelines, MUSC College of Nursing, 99 Jonathan Lucas Street, MSC 160, Charleston, SC 29425-1600.
© Copyright 2023 by the Medical University of South Carolina College of Nursing. All rights reserved. No part of this publication can be reproduced without permission from the Medical University of South Carolina College of Nursing.
Impact
A Culture of Belonging n Empowering Global Health n Advocacy for the Profession n Student Scholarships n Opening Doors n Philanthropy & Engagement n Innovation in Action n R ipple Effect 39
Shot
#CONSTRONG 54 Inspiration n n n The Next Step Love Connection From Suits to Scrubs 27
n
Parting
n





 Special moments from the College of Nursing 2022-2023 Convocation and Pinning ceremonies.
Special moments from the College of Nursing 2022-2023 Convocation and Pinning ceremonies.
�
COLLEGE OF NURSING
Photos by Josh Goodwin.
MUSC
DEAN’S WELCOME MESSAGE
It has been a privilege of a lifetime to serve as the 7th dean of the MUSC College of Nursing at this remarkable institution, and I will be eternally grateful for the many meaningful moments and outstanding, dedicated people – our leaders, faculty, staff, students, alumni, and donors – who have helped shape my time as dean. I am incredibly proud of our college, and this issue of Lifelines is just a snapshot of some of the many outstanding happenings and accomplishments this past year as well as a glimpse into the exciting future.
This issue introduces Dr. Teresa Kelechi, who steps into the interim dean position on July 1st. Dr. Kelechi brings a rich history and leadership within MUSC to the College of Nursing and will provide stability during this time of transition. The executive leadership team will be joined by Dr. Terri Fowler, newly appointed associate dean for practice, innovative partnerships, and advocacy who will focus on growth in faculty practice opportunities, community engagement, and advocacy work.
In addition to providing an update on the college’s national and international leadership in advancing palliative care education, research, and practice, we also highlight and pay tribute to Pat Coyne, who retired this spring as MUSC’s Director of Palliative Care but continues to partner with the college in advancing our palliative care footprint.
We are excited about the opportunities that will be created as we begin renovation of the first floor of the College of Nursing building this fall, with the aims of supporting planned growth in student enrollment;
providing a much-needed, welcoming area to build a sense of community and gathering for students, staff, faculty, and guests; and creating flexible, multifunctional spaces for our research and practice priorities.
The stories on the future of nursing simulation, telehealth, and design thinking highlight our faculty’s expansive commitment to innovation, including envisioning new student educational experiences, embedding telehealth into the curriculum, and providing care to various patient populations we serve in Charleston, South Carolina, and beyond.
As I end my tenure as dean of the college, my story shares some of the amazing opportunities and influential nurse leaders who have been instrumental in shaping my career and trajectory in nursing over the past 48 years. In addition, the advocacy for nursing editorial represents my view of the importance of individually and collectively informing policy and engaging in actions that elevate topics important to nursing, nursing education, research, practice, and the profession.
I hope you enjoy the many spotlights and stories throughout this issue of Lifelines that share a few of the important impacts, innovations, philanthropic activities, and accomplishments being spearheaded by our students, faculty and staff, alumni, and development board and donors. I am inspired and proud of all their wonderful achievements and work. The future is bright, and I look forward to following the college’s successes in the years ahead.
As I look forward to what comes next, I’m inspired by the incomparable Ann Darlington Edwards, whose love for nursing never wavered even as she stepped into new roles as first lady of South Carolina as well as MUSC. She always found a way to connect with nursing, whether through advocacy for the nurses of our state and beyond or philanthropy in supporting MUSC College of Nursing and the future of nursing practice, research, and education. Like her, I deeply love the profession I chose and how it has shaped my life, and I look with anticipation toward what comes next.
Thank you for being part of my incredible journey and for your continued support of the College of Nursing.
In-service and respectfully,
Linda S. Weglicki, Ph.D., R.N. Dean and professor

3 LIFELINES MAGAZINE
Former First Lady Ann Edwards with Dean Linda S. Weglicki during a reception in May.
23rd in the Nation!
US News & World Report names
Associate Professor Terri Fowler, DNP, APRN, FNP-C, will assume the position of Associate Dean for Practice, Innovative Partnerships, and Advocacy for MUSC College of Nursing on August 1. In this role, she will foster sustainable relationships in the community and beyond through clinical and entrepreneurial partnerships with the college and champion innovative programs that are responsive to current and emerging healthcare needs and challenges.

“I am honored to continue to serve MUSC and the College of Nursing in advancing nursing practice, patient care, and student education through partnerships, community engagement, and advocacy. I look forward to working with the outstanding CON faculty and staff to expand the reach of nursing practice and advocacy efforts to improve the health of the communities served.”
—Dr. Terri Fowler
MUSC College of Nursing 23rd in the nation (and 1st in SC) for Best Graduate Nursing SchoolsDNP Programs! ��%
100%

RN-BSN
US News & World
ABSN
US News & World
NCLEX-RN First Time Pass Rate, 2022 #4
Online Program
Report #3�
Program
Report
ANCC
RANKINGS
Pass Rates, 2022
2022-2023
AROUND THE COLLEGE 4 MUSC COLLEGE OF NURSING
Photos by Josh Goodwin.
Interim Dean
Teresa J. Kelechi, Ph.D., R.N., FAAN, will assume the position of Interim Dean for MUSC College of Nursing on July 1. Since 2019, she has served as the Associate Dean for Research and Ph.D. Studies and is the holder of the David and Margaret Clare Endowed Chair and a tenured professor. Kelechi received a Bachelor of Science in Nursing from Kent State University, a Master of Science in Gerontological Nursing from Case Western Reserve University, and Doctor of Philosophy from the University of South Carolina.

As a certified wound care nurse and gerontological clinical nurse specialist, her research interests include lower extremity ulcer prevention and management interventions (cooling therapy, physical activity, palliative wound powder, self-monitoring with infrared thermometry, artificial
intelligence for bioburden detection), symptom self-management (pain/ loneliness therapies), and caregiver stress reduction (mindfulness/ breathing). Kelechi has received funding to support her research from various agencies and organizations such as the National Institutes of Health/National Institute of Nursing Research, American Nurses Foundation, Marine Polymer Technologies, Inc. and Firststring Research, Inc. She currently teaches in the Ph.D. program as a senior scholar and mentor.
Joining MUSC in 1987 and the College of Nursing in 2001, Kelechi has participated in and held numerous intramural and extramural leadership roles over almost four decades of service, including directorships of the college’s Symptom Self-Management Center and the university’s Recruitment
MUSC College of Nursing Faculty Appointments

Core for the South Carolina Clinical and Translational Research Institute/ Clinical and Translational Science Awards Program.
Her son Thomas is a 2018 graduate of the ABSN program and now works in Arizona, and she and her husband Jim, a golf professional, reside on James Island with their two dogs, rescues dachshund Femmy and beagle Chaco.
Director, Community Engagement: Simone Chinnis, DNP, MBA, FNP-C, AE-C
Director, Advocacy and Policy: Amy Williams, DNP, APRN, CPNP-PC
Faculty during the May 2023 Convocation.
5 LIFELINES MAGAZINE
Leaders in Palliative Care
In November, MUSC College of Nursing was honored to host internationally renowned palliative care expert and End-of-Life Nursing Education Consortium (ELNEC) principal investigator Betty Ferrell, R.N., Ph.D., MA, CHPN, FAAN, FPCN for Nursing Grand Rounds “The Future of Palliative Care: After the Storm” and the Palliative Care Showcase: All that is PC at MUSC and Beyond. The event brought together faculty members, clinical practitioners, researchers and graduate students in a wide-ranging dialogue revolving around impactful outcomes, the many areas that compassion and palliative care touch and the exciting work being done in the clinical practice, education, research and policy arenas.


Did you Know?
In 2022, MUSC College of Nursing was designated as one of six Regional Centers for Palliative Care Nursing Education in the United States by the End-of-Life Nursing Education Consortium (ELNEC) project. Carrie Cormack, DNP, APRN, CPNP, associate professor and lead faculty for the college’s Palliative Care program, is the regional co-chair. In this role, she serves as an expert and leader for other schools in the region seeking information and direction on expanding palliative care education.



AROUND THE COLLEGE
MUSC faculty members, clinical practitioners, researchers and graduate students joined Dr. Betty Ferrell for the Palliative Care Showcase.
6 MUSC COLLEGE OF NURSING
Photos by Josh Goodwin.
PAT COYNE RETIRES
College of Nursing faculty member Pat Coyne, MSN, ACHPN, ACNS-BC, FAAN, FPCN, retired this spring from his position as MUSC’s Director of Palliative Care.
Instrumental in advancing palliative care through his groundbreaking and decades-spanning work, Coyne was recently honored by Dr. Betty Ferrell in “A Tribute,” which appears in the April issue of the Journal of Hospice & Palliative Nursing. While paying homage to his unwavering commitment to health equity, compassionate care and mentorship, Ferrell credited Coyne as a trailblazer of nurse leadership in palliative care. Thank you Pat, for your leadership in advancing palliative care.
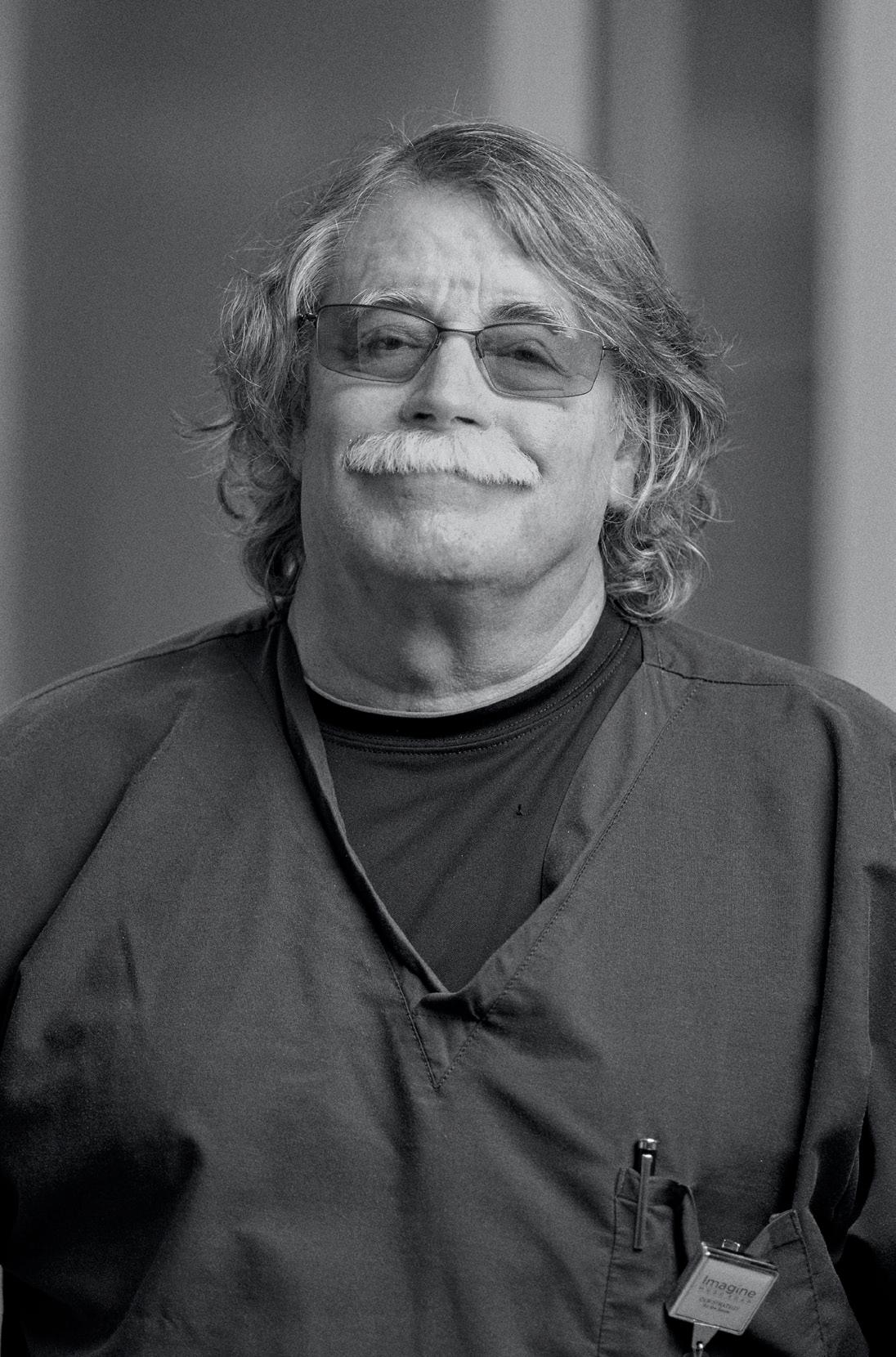
International Palliative Care Training
Last fall, MUSC College of Nursing faculty members Carrie Cormack, DNP, APRN, CPNP, and Pat Coyne, MSN, ACHPN, ACNS-BC, FAAN, FPCN, taught End-of-Life Nursing Education Consortium (ELNEC) training in Salzburg, Austria. Supported by the Open Medical Institute, an international initiative for medical professionals that aims to improve health care on a global scale, the experience featured 33 nursing professionals from Eastern European countries (including Albania, Armenia, Hungary, Kazakhstan, Romania and Ukraine) who attended the week-long training as fellows to further develop their skills and knowledge in palliative and end-of-life care.
“As faculty with ELNEC, I led the pediatric content,” said Cormack. “The fellows were all invested in improving the quality of life for their patients and families and learning how to provide palliative care despite the significant barriers that exist for them and their patients.” In addition to didactic sessions, the fellows worked through interactive role playing and case studies to deepen their understanding. They also took part in interactive “self-care” sessions, one of which highlighted the benefits of art therapy. As a capstone, they divided into groups based on their country of origin and planned a project that could be implemented upon their return home.
“At the end of the week, the projects were presented to the group for questions and feedback,” shared Cormack. “The aim of the training is for each participant to return and share the information learned, with the goal to expand and improve health care globally. It is an honor and privilege to be part of this experience. Sharing with and learning from passionate nurses from around the world is life changing.”
Cormack and Coyne’s international ELNEC training work continues throughout 2023.
7 LIFELINES MAGAZINE
AROUND THE COLLEGE
Building for the Future
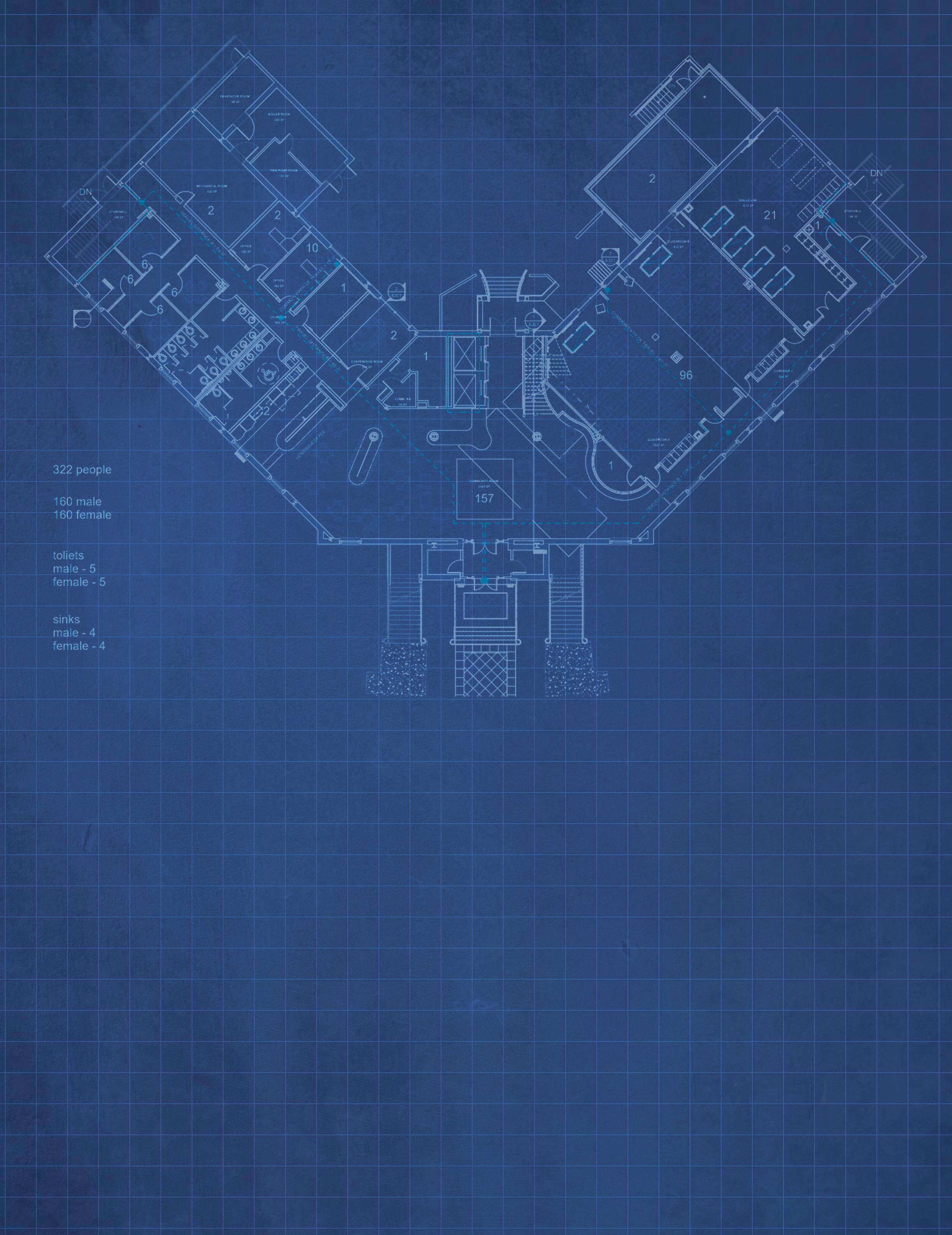 by Linda S. Weglicki, Ph.D., R.N., Dean and Professor
by Linda S. Weglicki, Ph.D., R.N., Dean and Professor
Now that all the approvals are complete, we look with great anticipation to the renovation of the first floor of the College of Nursing building. The college reacquired the first floor this past spring when the MUSC Simulation Center moved to its new location in the James W. Colbert Education Center and Library.
The renovation will accommodate planned growth in student enrollment, particularly in our on-campus Accelerated Bachelor of Science in Nursing (ABSN) program; help us meet American Association of Colleges of Nursing (AACN) and Commission on Collegiate Nursing Education (CCNE) nursing education requirements; and ultimately support the increased need for qualified nurses in South Carolina—all through innovative, competency-based training in a modern learning environment. It is imperative that our college strategically expands the utilization of space within
our current building. Addressing these key objectives is critical to our continued growth and sustainability and to offset the predicted growing nursing workforce shortage in South Carolina.
This project primarily includes renovation of the existing ground floor of the College of Nursing to create flexible multi-functional, student-centric education and community spaces along with collaborative research and practice hub conference spaces designed to support the college’s tripartite mission. Specifically, the first floor renovation consists of approximately 11,000 gross square feet and will include a new accessible entry and lobby from Jonathan Lucas Street at ground level and a new interior stair for expanded access to the second floor. A skills lab on the third floor is planned to be relocated to the first floor, and the existing space will then be repurposed to support faculty, staff, and student engagement and
activities. The first floor main lobby will feature collaborative gathering areas for the entire college as well as serve as pre-function space in support of the classroom and lecture spaces and can be used during break-out sessions.
The renovation will provide a 1,700 square foot lecture-type hall with flexibility to be subdivided into smaller lecture rooms or opened for a larger classroom. It will also include a 600 square foot sub-dividable research hub, and a 1,200 square foot multifunctional common area adjacent to a kitchen to support College of Nursing workforce and student community engagement, workshops, conferences, and professional meetings. The renovation will include offices for Student Services and state-of-the-art AV systems and technologies to support in-person and remote instruction. We expect the renovation to be completed by fall 2024 with planned increased enrollment in our ABSN program in spring 2025.
8 MUSC COLLEGE OF NURSING
INNOVATION
GAME ON THE FUTURE OF NURSING SIMULATION
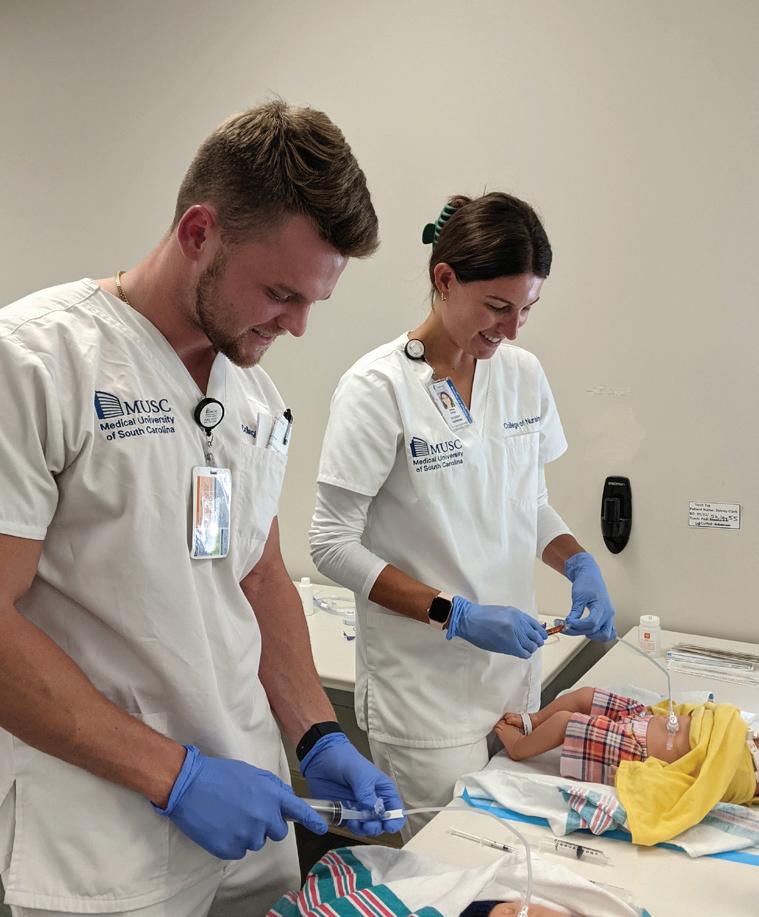
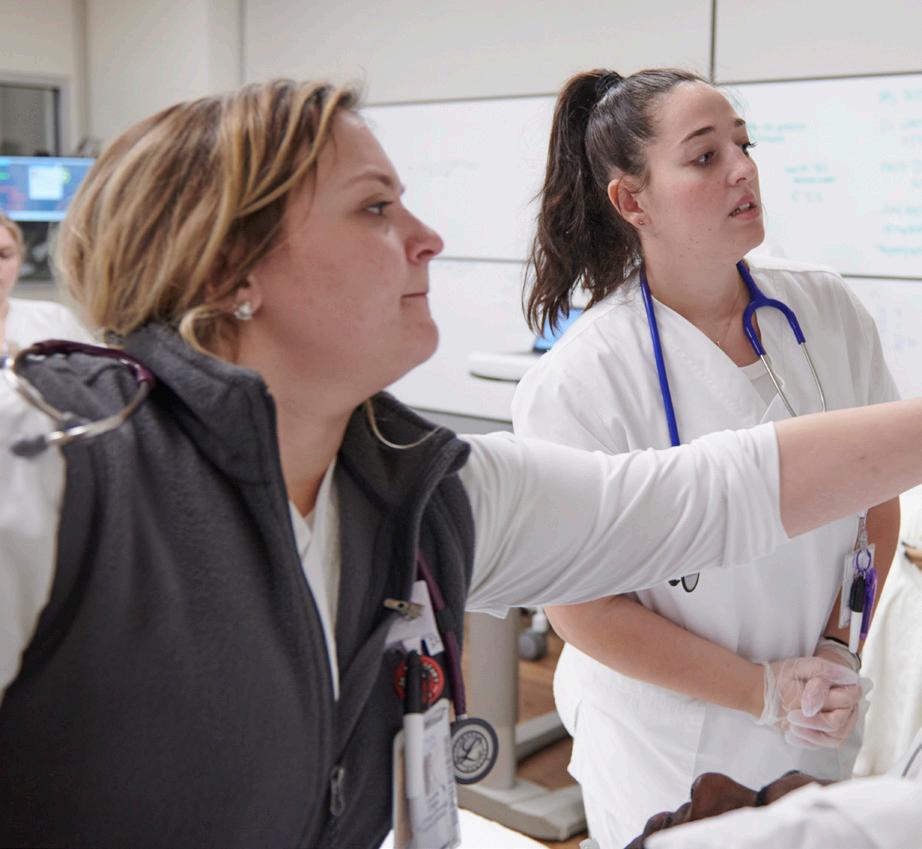
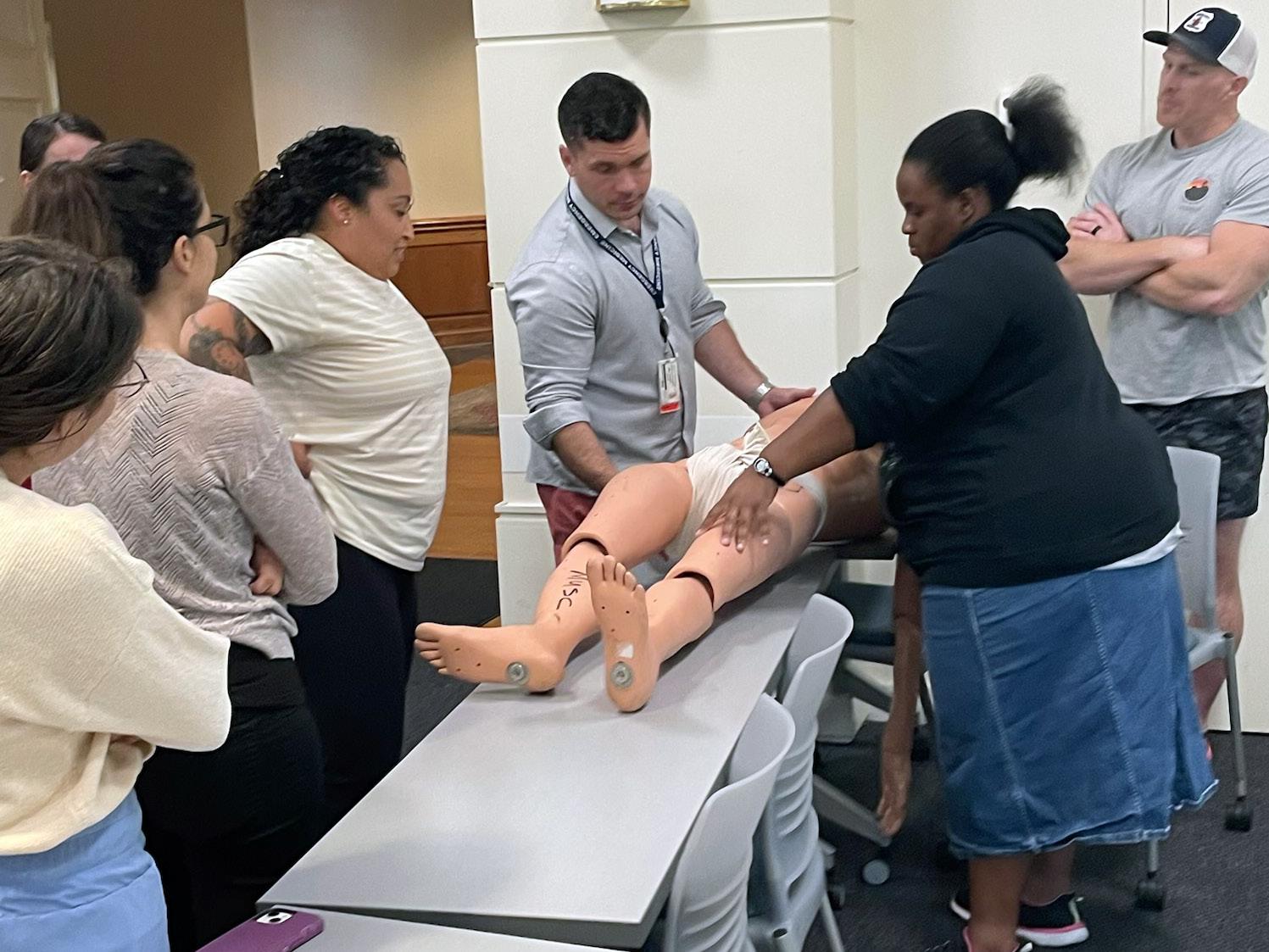
With the opening of MUSC’s new Simulation Center, the College of Nursing’s simulation team spotlights current immersive learning experiences and previews the innovations to come in nursing simulation education.
 From left: Jennifer Ciccone, Dr. Kristen Poston, and Alexis Williams work together to steer CON’s simulation education.
From left: Jennifer Ciccone, Dr. Kristen Poston, and Alexis Williams work together to steer CON’s simulation education.
9 LIFELINES MAGAZINE
Photos by Josh Goodwin.
INNOVATION
One of the priority areas I am currently focused on is developing and strengthening our academic and hospital workforce collaborations to inform our new simulation opportunities. We are also using these collaborations to increase clinical judgment skills as we prepare students for the Next Generation NCLEXRN exam (NGN). Specifically, by collaborating with our content experts on the hospital side, we can identify the gaps they’re seeing in care delivery at the bedside, and we can then take that information into our courses to develop simulation opportunities that build clinical judgment skills in our Accelerated BSN students.

Recently, we collaborated with MUSC certified wound and ostomy nurse Glenda Brunette, MSN, R.N., CWON, who brought her expertise in wound care and skin assessment to help inform us of wound care challenges that new nurses were encountering, and we brought our expertise in developing simulation and NGN clinical judgment questions. We were able to increase student confidence in assessing diverse skin tones and wounds, increase student confidence in managing atypical wound care incidents, and demonstrate improved performance on NGN style clinical judgment test questions. Ultimately, this strengthens our graduates when they sit for board licensure and certification and also strengthens the workforce at our hospital downstream when these graduates encounter these issues at the bedside as practicing nurses.
Considering the next horizon is so exciting because there are so many incredible things happening in simulation. With the increased emphasis on demonstration of competence within nursing curriculums, I think we will see a push for development of simulation modalities that can help us more directly observe and measure nursing student competence. For
example, I think we will see a push for implementation of simulation programs across curriculums that map actual or modified quality of nursing care indicators from the hospital side (quality indicators). I think to some degree we already have some of the equipment and technology we need to do this, but developing these programs will take manpower investment to develop, map and manage simulations and to train and compensate standardized patients (so the funding need is really in those areas). I think investment to support this level of mapping makes good sense though, as again, it is likely mutually beneficial across academic and hospital entities. Additionally, I think expansion of nursing specific opportunities and interprofessional education opportunities to address critical safety issues and teamwork development will continue to evolve. Exploration of more flexible methods, such as virtual reality simulations or online asynchronous game worlds, that can overcome scheduling and location challenges while still meeting learning objectives, will likely grow.”
Kristen M. Poston, DNP, APRN, FNP-C, CHSE, Assistant Professor and Lead Faculty for
Undergraduate Programs
“The College of Nursing is using simulation education in many ways to add a realistic learning experience for our students in a safe environment. Students also have the opportunity to practice nursing skills as well as work through patient scenarios using high fidelity mannequins. We have the ability to change the high fidelity mannequins’ heart sounds, lung sounds, etc., which creates a more realistic learning experience. Recently, we developed a new hybrid simulation that is used in the Medical-Surgical Nursing course which utilizes a standardized patient (trained actor) wearing a catheter
trainer so that students can practice communication skills along with nursing skills.
The future of nursing simulation includes more realistic mannequins with more humanistic features and ways to simulate real patient scenarios. Also, virtual reality simulation offers a new way to train nursing students. The benefits include access to learning from anywhere at any time in a 3D realistic health care setting, and access to hundreds of different patient scenarios which can promote critical thinking skills without causing harm to a patient.”
—Jennifer Ciccone, MSN, RN, CHSE Simulation Lab Instructor
�� MUSC COLLEGE OF NURSING
“We’re incorporating advanced technology using high fidelity mannequins and devices to allow students to gain a hands-on student-patient experience before they go into the clinical unit. What’s next? Virtual and augmented reality to make the student’s experience feel even more authentic than it already is.” Alexis Williams

 , Simulation Assistant
, Simulation Assistant

Located in the newly renovated James W. Colbert Education Center and Library, the new MUSC Healthcare Simulation Center boasts 12,000 square feet of cutting-edge spaces and technology to support immersive learning, including high fidelity scenarios, for students. The center's inventory of simulators includes 30+ mid to high fidelity manikins and over 100 task trainers to support a broad range of simulationbased educational objectives.



�� LIFELINES MAGAZINE
BRIDGING THE GAP
PREPARING COLLEGE NURSING STUDENTS FOR TELEHEALTH ENCOUNTERS
by Alex Walters, MUSC Instructional Design Manager MUSC Office of Instructional Technology & Faculty Resources
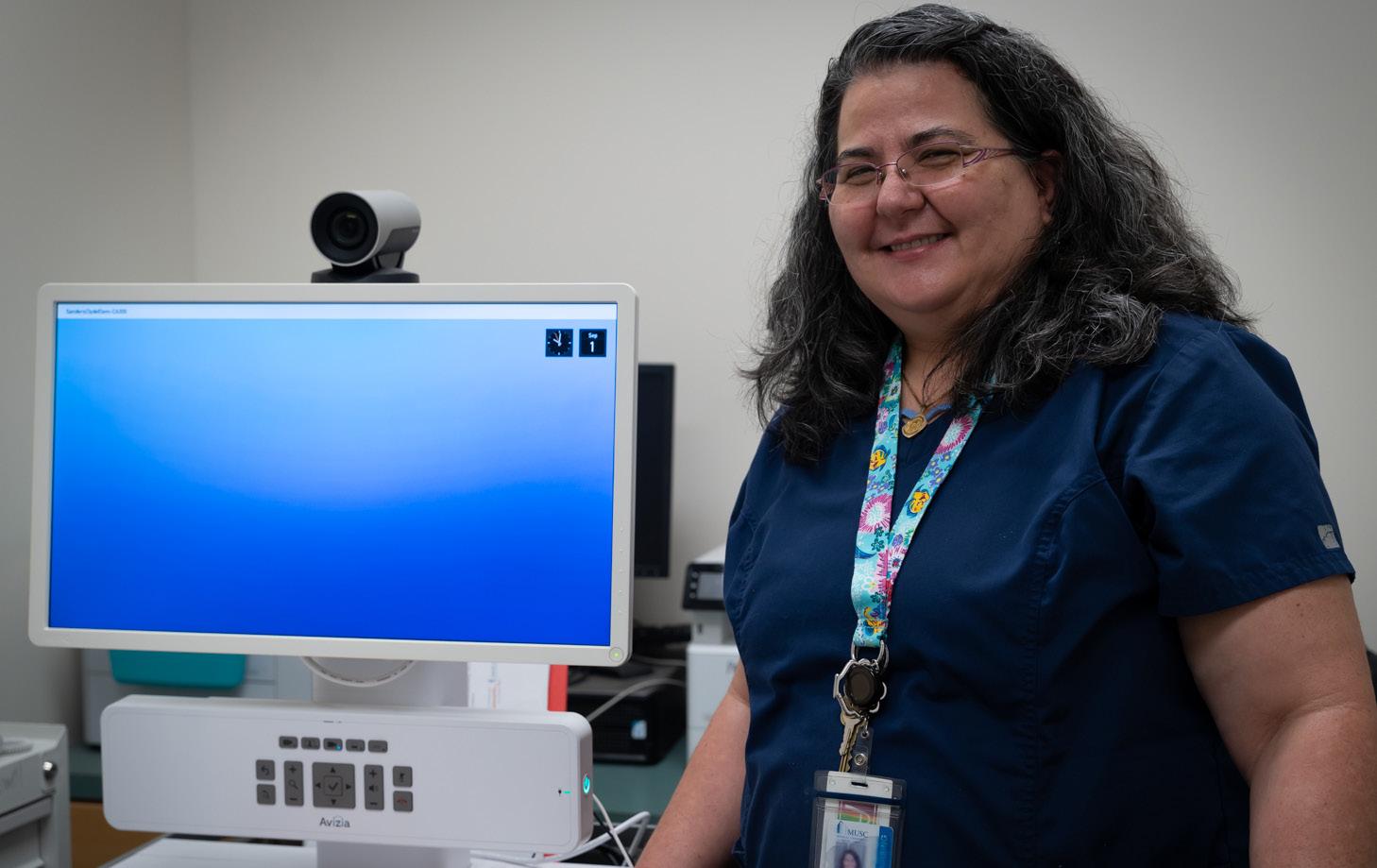
Assistant Professor Katherine Chike-Harris, DNP, APRN, CPNP-PC, FNP-BC, CNE has always embraced the importance of preparing MUSC College of Nursing students for the variety of situations that they will encounter during practice, with telehealth being at the forefront of her work. Now, her forward-thinking project expands the possibilities of telehealth education not only for the College of Nursing but also for the entirety of MUSC.
Last fall, Chike-Harris was named an awardee for the 2022-23 MUSC Education Innovation Fund, which seeks out innovative educational approaches, techniques and programs to provide one-time funding for piloting or further evaluation. Her plan is to provide a scope, curriculum and actionable ways for embedding the work
of telehealth into the College of Nursing’s courses, with an emphasis on scenarios and experiential learning. ChikeHarris stressed the need for undergraduate students to become comfortable with these interactions, especially with the recent and rapid acceleration of telehealth and the demand for students to be proficient in this area.


INNOVATION
Photos by Josh Goodwin.
�� MUSC COLLEGE OF NURSING
“I wanted to develop a simulated visit where our Bachelor of Science in Nursing students will have the experience of working with the telehealth cart, troubleshooting the cart and then presenting patients to our Doctor of Nursing Practice students,” she noted.


Exposing students to these scenarios is key to making sure that they are equipped for practice and ready to take on any situation that they encounter. “Being exposed to this education will prepare students to help practices integrate,” she explained. “Especially for the undergraduate students, having that experience in the classroom will translate to postgraduation, because telehealth is here to stay.”
Chike-Harris’s efforts to create a rich, embedded curriculum on telehealth has provided numerous opportunities for the project to evolve. Considering what the project looks like moving forward, Chike-Harris provided this insight: “I’m using this as a pilot study, so I’m currently developing the cases, the scenarios and the workflow, and I’m hopeful that once that is solidified, I can open up the project to more colleges on campus as an interprofessional education initiative. This spring, we’ve had great success introducing the joint simulation
to our BSN and DNP students, and within the next year, I’m going to try to invite the other colleges on the MUSC campus to participate in this interprofessional simulate telehealth activity.”
Chike-Harris’ excitement is palpable when envisioning the long-range impact of telehealth. “I love telehealth,” she enthused. “You know telehealth is my end game. I think it is critical that everybody be exposed to it, especially learners. If students become comfortable with it, then they will adopt it after graduation. My main love with telehealth is that we are reaching populations that we typically cannot reach due to a number of healthcare barriers.”
Equitable access to healthcare has always been a passion for Chike-Harris. “My mother was a firstgeneration immigrant to the United States, and even though my father was military and American, my mother still had language barriers, and at that time a lot of discrimination,” she said. “There was also the challenge of navigating the complex healthcare network of the United States. So, growing up with those challenges gave me a better appreciation of those underserved populations that need help.”
� 3 LIFELINES MAGAZINE
Scenes from one of Dr. Chike-Harris’ recent simulated telehealth visits involving ABSN and DNP students interacting with a standardized patient.

� 4 MUSC COLLEGE OF NURSING
INNOVATION
In addition to her work as a College of Nursing faculty member, Chike-Harris serves as a provider for South Carolina’s schoolbased telehealth program, which helps to deliver medical care to children in underserved areas through more than 100 school-based clinics across 23 counties. Each school participating in the program receives a specialized telehealth cart (with attached peripherals such as an electronic stethoscope, otoscope and lens) which allows the school nurse to telepresent children to remote providers, who are able to see and hear the examination results in real time. “So instead of children missing a part or a whole day of school, we can provide them with care,” said Chike-Harris. “Nine times out of 10, they are back in class within 15 to 30 minutes, increasing their seat time and education.”

Chike-Harris also uses the school-based telehealth program as a clinical precepting opportunity for her Doctor of Nursing Practice students, who can join her physical location or connect through one of the other supported school-based clinics located around the state. It is an innovative approach to both clinical training and care delivery.



“It’s called the teleprecepting model, which is something that not a lot of people are doing in the United States with pediatric or family nurse practitioner students—or at least not reporting on,” Chike-Harris explained. “I haven’t found much documentation where people say they are using nurse practitioner students in this model. We’re unique in the way we can provide a whole exam with the carts and the peripherals.” The teleprecepting model can potentially provide more pediatric clinical opportunities for nurse practitioner students, which is currently a major challenge for many nurse practitioner programs in the United States. Several students can be placed within the school-based clinics and telepresent patients to one provider, thus increasing the traditional 1:1 studentpreceptor ratio. Additionally, the teleprecepting model offers nurse practitioner students the opportunity to intimately experience the health care challenges underserved populations face and how telehealth can improve their access to quality health care.
 Dr. Katherine Chike-Harris.
Dr. Katherine Chike-Harris.
� 5 LIFELINES MAGAZINE
Photo by Nancy Carney.
DESIGN THINKING
With Smartphone Application, Patients with Sickle Cell Disease Can Better Care for Themselves or Loved Ones
by Barry Waldman, Progressnotes muschealth.org/health-professionals/progressnotes
When Associate Professor Shannon Phillips, Ph.D., R.N., was a registered nurse in the pediatric ICU, she cared for children with a host of complex chronic diseases and was perplexed by the disparity in grant funding for research and disease-modifying therapies for sickle cell disease. Focusing her research on the under-resourced battle against it, Phillips today is at the forefront of producing technology to enhance the ability of children and adolescents with sickle cell disease to self-manage their own health.

Hard, sticky, short-lived and misshaped red blood cells invade the blood stream of people with sickle cell disease. These crescent-shaped, or sickle, red blood cells cause abnormal hemoglobin as part of a genetic disease primarily affecting those whose ancestors came from sub-Saharan Africa. Roughly 100,000 Americans are currently afflicted with this painful and debilitating disease according to the Centers for Disease Control and Prevention.
Individuals with sickle cell disease, particularly those who suffer from sickle cell anemia, endure pain and vulnerability to infection. With their bow shapes, sickle cells clog blood flow and die early, leaving those with this kind of anemia constantly short of red blood cells
and the oxygen they carry. To prevent a sickle cell crisis, afflicted individuals must avoid dehydration, overheating, exposure to high altitudes and taxing athletic endeavors. There are a handful of pharmaceutical therapies that help manage sickle cell disease, but they expose patients to an array of side effects including lowered white blood cell and platelet count which increases the risk of infection. The only current cure right now is a bone marrow or stem cell transplant, but gene replacement therapy is showing encouraging results in early clinical trials.
Without a cure, sickle cell patients have a life expectancy 20 years less than the general population. Those with sickle cell anemia live, on average, about
Dr. Shannon Phillips. Photo by Josh Goodwin.
INNOVATION
� 6 MUSC COLLEGE OF NURSING
Photo by Josh Goodwin.
30 years less. And even these numbers are a vast improvement over just 50 years ago, when most individuals with sickle cell didn’t survive to adulthood.
With increased life expectancy has come another challenge: the transition from childhood to adulthood with sickle cell disease is fraught with difficulties even beyond the norm. First, because sickle cell disease was primarily a childhood disease in the past, most services are aimed at children. Those who age out of pediatric services encounter a serious dearth of specialists, case managers, insurance coverage and access to health care, and they must suddenly take the lead in tracking and coordinating their own care.
Second is the stigma that comes with the diagnosis of sickle cell disease, which generally presents as excruciating pain. Because suffering individuals require ongoing pain medication, health care professionals may view them as med-shopping and deny them pain relief, particularly now in the shadow of the opioid crisis. This breakdown in communication may be exacerbated when patients are suffering corollary issues like depression or cognitive impairment.
Advocates for individuals with sickle cell disease say race also presents a challenge. Research shows Black Americans already face more barriers to care and have worse outcomes than the rest of the population. And patients who have had negative experiences in the ED or with their assigned health care practitioners may be reluctant to seek care and struggle to manage their condition. This can be life-threatening in the face of a disease that requires constant attention.
Phillips' app, currently dubbed Voice Crisis Alert (v.2), helps children up to age 17 follow treatment regimens, attend clinic appointments and generally improve the management of their care.
Preliminary testing has demonstrated that the app is useful for adolescents moving from parent-led management to self-management. Patients and their parents liked the app and found that it aided their efforts to stay current with their regimens and keep pain at bay.
The kid-friendly interface allows users to customize their avatar with hair and clothes and to earn points for achieving benchmarks that will allow them to upgrade their virtual selves to having a virtual dog, for example.
The “I’m in Pain” button allows users to indicate where
on their body they hurt and to indicate the severity according to validated pain-rating scales. The app-based pain history helps them delve into behaviors that might be indicators of emerging pain.
In post-testing during feasibility studies, parents told Phillips and her team that they found their children were hiding their pain prior to using the app, but were less reluctant to share with the app. “The idea is to help people start to see if there are patterns or triggers to their pain,” Phillips said.
The app includes the user’s sickle-cell related health history, including their type of sickle cell disease, their white blood cell count, blood type, medications they take and the dose and much more. The app also reminds them when to take their meds.
The app not only helps patients and their parents understand their disease but also aids communication with teachers, school nurses and others who need to know. One user employed the app to help her teacher understand why it was so important that she stay hydrated.
Phillips says the reminder can eliminate doubt about whether a patient is abusing pain relief. “If you’re in a pain crisis and don’t remember when you took your last Percocet, you can just look at the app and find out,” she said.
In addition, the app supplies organized, authoritative information about sickle cell disease care, which Philips and her team discovered was desperately needed. “We heard from a lot of people that they just Googled the subject and looked at reviews,” Phillips said. The app also links to the MyChart health portal, which provides patients a plethora of information and facilitates communication with caregivers.
Voice Crisis (v.2) has been in development for a couple of years and has demonstrated measurable outcomes reducing fatigue, anxiety and pain as well as improving health-related quality of life for children over the age of eight and developing self-management skills that will aid in the transition to adulthood.
Phillips knows the app doesn’t solve many of the issues facing children and teens with sickle cell disease but is optimistic about the future. “It’s very promising, which is why we’re working hard to get to the next stage of [largescale] testing.”
� 7 LIFELINES MAGAZINE
ON CALL: SOUTH CAROLINA PUBLIC HEALTH PREPAREDNESS STUDENT CORP
by Kasey Jordan, Ph.D., R.N Assistant Professor, ABSN Program
Participants in the inaugural MUSC cohort of the South Carolina Public Health Preparedness Student Corp (SCPHPSC) have completed their training and are ready to meet Lowcountry health needs if disaster occurs.
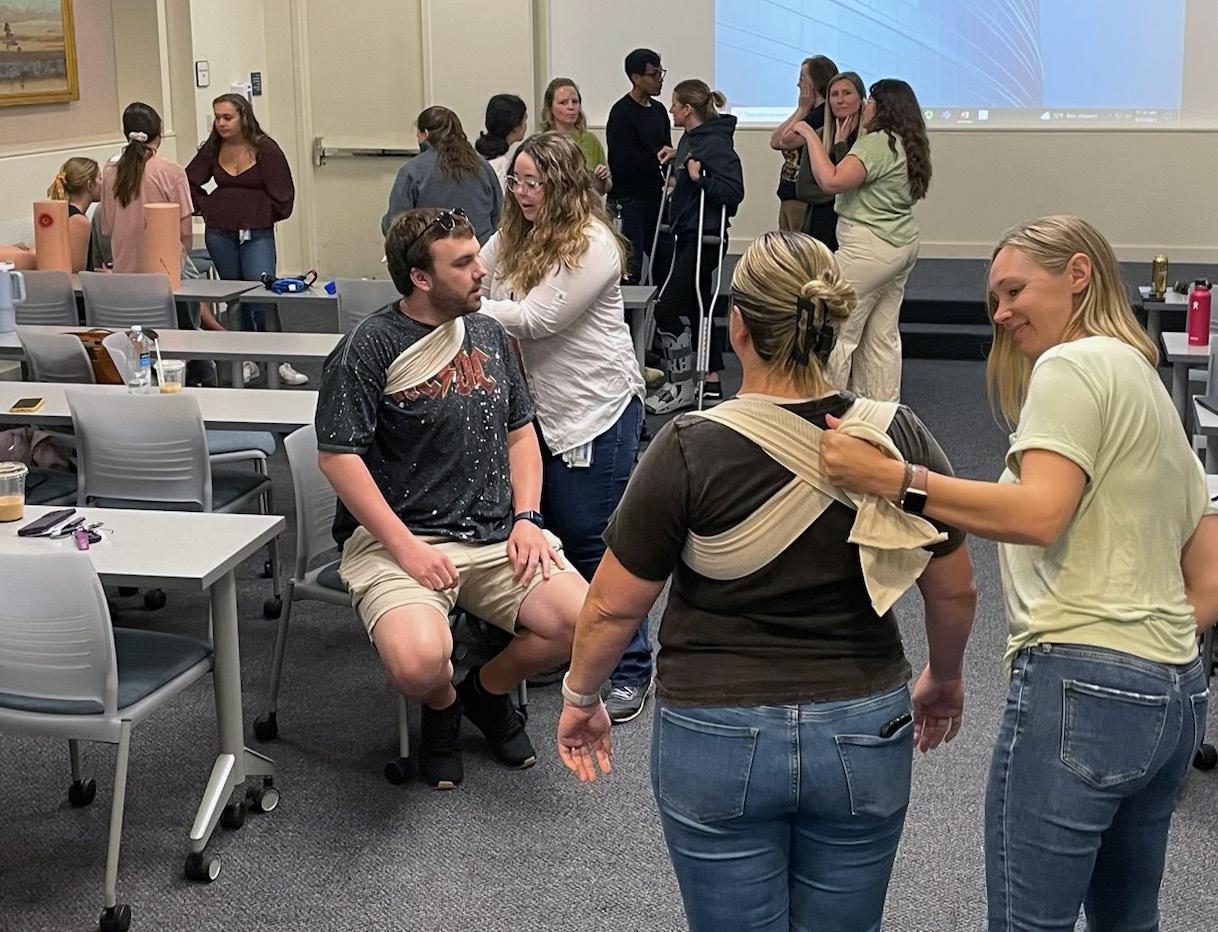
SCPHPSC is a statewide initiative to increase the number of health care professionals available to respond to a disaster. Spearheaded by Dr. Shirley Timmons of Clemson University with funding from South Carolina Department of Health and Environmental Control, the program supports disaster preparedness training throughout South Carolina.
As the MUSC SCPHPSC project director, I partnered with College of Medicine assistant professor Dr. Dustin LeBlanc, who also serves as MUSC’s Medical Director for Emergency Preparedness, to lead the first group of MUSC participants in the program. Over the course of the spring semester, fifty Accelerated BSN students engaged in equity-focused disaster response training in order to join a statewide registry of professionals ready to be called in the event of a disaster. Students completed activities above and beyond their traditional coursework, including training in contact tracing, incident command structure and social determinants of health in disaster. Two required courses, IS-100.C: Introduction to the Incident Command System and IS-700.B: An Introduction to the National Incident
Management System, were completed online through FEMA’s Emergency Management Institute.
The experience culminated in an April summit that gave students the opportunity to apply the knowledge they had gained throughout the program. Dr. LeBlanc coordinated advanced hemorrhage control skills stations, which were also supported by emergency medicine residents Dr. Parker Lewis, Dr. Gabrielle Beam and Dr. Colleen Hagopian. Dr. DaNine Fleming, MUSC Office of Equity’s Associate Chief Officer for Inclusive Excellence, engaged students in a dynamic conversation about barriers to disaster resilience in Charleston. The event culminated with a mass casualty tabletop exercise developed for this group by Lt. Bryan Wood from the MUSC Office of Public Safety. This fall, we hope to welcome a new, interprofessional cohort of MUSC SCPHPSC students from both the College of Nursing and College of Medicine.
INNOVATION
Students applied their knowledge during a Saturday morning April summit held on MUSC’s campus.
� 8 MUSC COLLEGE OF NURSING
Photos by Kasey Jordan.
National and International Faculty Recognitions
n Dr. Elizabeth Bear (Professor Emerita) Dorothea M. Lang Pioneer Award American College of Nurse-Midwives

n Dr. Carrie Cormack Fellow in Palliative Care Nursing Hospice and Palliative Nurses Association
Award of Excellence
End-of-Life-Nursing Education Consortium
Leah Harrison Excellence in Clinical Writing Award Journal of Pediatric Health Care
n Dr. Carolyn Jenkins (Professor Emerita) Benjamin Osuntokun Award for Outstanding Contributions to Stroke Research in Africa African Stroke Organization Conference
n Dr. Teresa Kelechi
International Nurse Researcher Hall of Fame Sigma Theta Tau International Honor Society of Nursing
n Dr. Joy Lauerer Award for Excellence in Practice – APRN American Psychiatric Nurses Association






n Dr. Leigh Ridings mHealth Scholar mHealth Training Institute
n Dr. Martha Sylvia 2nd place, Informatics Book of the Year American Journal of Nursing
n Dr. Gigi Smith Outstanding Publication award Association for Educational Communications & Technology

n Dr. Janelle Wagner Outstanding Publication award Association for Educational Communications & Technology
 Dr. Elizabeth Bear
Dr. Carolyn Jenkins
Dr. Joy Lauerer
Dr. Martha Sylvia
Dr. Janelle Wagner
Dr. Carrie Cormack
Dr. Teresa Kelechi
Dr. Leigh Ridings
Dr. Elizabeth Bear
Dr. Carolyn Jenkins
Dr. Joy Lauerer
Dr. Martha Sylvia
Dr. Janelle Wagner
Dr. Carrie Cormack
Dr. Teresa Kelechi
Dr. Leigh Ridings
� 9 LIFELINES MAGAZINE
Dr. Gigi Smith
College of Nursing Newly Funded Federal Grants
Self-Management for Youth Living with Sickle Cell Disease (SMYLS)
PI: Shannon Phillips, PhD, RN
Sponsor: NIH/NINR
Performance Period: 04/21/2023 –01/31/2028
Total Award: $2,558,419
Augmenting Suicide Prevention Interventions for Service members (ASPIS)
PI: Tracy Stecker, PhD
Sponsor: Ohio State University/DOD
Performance Period: 09/30/2022 –09/29/2026
Total Award: $90,176
Nurse Faculty Loan Program
PI: Susan D. Newman, PhD, RN, CRRN
Sponsor: HRSA
Performance Period: 07/01/2022 –06/30/2023
Total Award: $143,289
Cognitive Behavioral Therapy for Treatment Seeking Patients (CBTTS) as an Approach to Increasing Engagement with MOUD Treatment
PI: Tracy Stecker, PhD
Sponsor: Sub. University of Rochester/ HRSA
Performance Period: 09/01/2022 –08/31/2023
Total Award: $93,941
Recruitment and Engagement in Care to Impact Practice Enhancement (RECIPE) for Sickle Cell Disease
PI: Shannon Phillips, PhD, RN
Sponsor: Sub. University of Alabama at Birmingham/NIH
Performance Period: 08/15/2022 –07/31/2027
Total Award: $146,115
Improving the Collaborative Health of Minority COVID-19 Survivor & Carepartner Dyads Through Interventions Targeting Social and Structural Health Inequities
PI: Martina Mueller, PhD
Sponsor: University of South Carolina/ NIH/NINR
Performance Period: 08/01/2022 –06/30/2026
Total Award: $120,642
South Carolina Public Health
Preparedness - Student Corp (SCPHPSC)
PI: Kasey Jordan, PhD, RN

Sponsor: Clemson University/CDC
Performance Period: 11/01/2022 –06/30/2023
Total Award: $208,474
Mobilizing Behavior Change to Promote Occupational Health and Wellness Among Firefighters
PI: Tatiana M. Davidson, PhD
Sponsor: Department of Homeland Security / Federal Emergency Management Agency Grant (FEMA)
Performance Period: 09/09/202209/08/2024
Total Award: $484,658
Preparing PHOENIX to Fly: Building Capacity for Research on Spinal Cord Injury Peer Mentoring
PI: Susan D. Newman, PhD, RN, CRRN
Sponsor: ACL/NIDILRR
Performance Period: 09/01/2022 –08/31/2025
Total Award: $599,951
A Scalable mHealth Resource to Facilitate Behavioral and Emotional Recovery after Pediatric Traumatic Injury – Supplement
PI: Leigh E. Ridings, PhD
Sponsor: NIH/NICHD
Performance Period: 12/01/202206/30/2023
Total Award: $53,982
INNOVATION
Named the 2022 Peggy Schachte Research Mentor last fall, Dr. Ken Ruggiero celebrated with his team, including (L-R) Dr. Hannah Espeleta, Tonya Hazelton, and Dr. Tatiana Davidson.
�� MUSC COLLEGE OF NURSING
Photo by Jennifer Turner.
Faculty Publications: January 2022-May 2023
Books and Chapters
Dubose-Morris, R. A., Chike-Harris, K. E., Garber, K., Schimek, A. M., & Stroud, K. (2022). Telehealth: Reaching out to patients and providers. In Nursing informatics. Health informatics (pp. 321–337). Springer Nature.
Johnson, E. E., & Sylvia, M. L. (2022). Secondary data collection. In Clinical Analytics and Data Management for the DNP (No. 3rd) (pp. 61–86). Springer.
Vigil, I. M., & Sylvia, M. L. (2023). Real-world population health analytics in community, public, and medical health systems. In Medicine and Public Health Together (pp. 79–106). Telemachus Press.
Sylvia, M. L., & Terhaar, M. F., Eds. (2024). Clinical Analytics and Data Management for the DNP (No. 3rd). Springer.
Wagner, J. L., & Smith, G. (2023). Self-management programs for children with epilepsy and their families. In Epilepsy: A comprehensive textbook (No. 3rd). Lippincott: Wolters Kluwer Health (in Press).
Articles
Broome, S. B., Williams, K. W., & Hendrix, K. (2022). App providing psychosocial and educational supports benefits caregivers of children with newly diagnosed food allergies. Journal of Food Allergy, 4, 163–171.
Chandler, J., Christon, L. M., Benfield, K., Pairet, S., Hoffman, M., Treiber, F., Mueller, M., & James, W. E. (2023). Design and rationale of a pilot randomized clinical trial investigating the use of a mHealth app for sarcoidosis-associated fatigue. Contemporary Clinical Trials Communications, 32, 101062.
Christon, L. M., Chandler, J. L., Benfield, K., Pairet, S., Hoffman, M., Treiber, F. A., & James, W. E. (2023). Perceptions of the fatigue experience and a breathing awareness meditation-integrated mHealth App for fatigue and stress in patients with sarcoidosis. Fatigue: Biomedicine, Health & Behavior, 11(1), 14-34.
Chike-Harris, K. E., Snyder, E., & Conner, R. S. (2022). Educating APRN students about telehealth credentialing, licensing & billing. Journal of Nursing Education, 61(7), 413-416.
Chike-Harris, K. E., Lauerer, J. A., Powers, A. R., & Stanley, A. Y. (2022). Telehealth professionalism education for APRN students. Nursing Education Perspectives, 43(6), 382-383.
Stanley, A. Y., Chike-Harris, K. E., Chinnis, S. P., & Durham, C. O. (2023). Adolescent contraception management: A review of medical options. The Journal for Nurse Practitioners (in Press).
Garber, K., Chike-Harris, K., Vetter, M. J., Kobeissi, M., Heidesch, T., Arends, R., Teall, A., & Rutledge, C. (2023). Telehealth policy and the advanced practice nurse (APRN). The Journal for Nurse Practitioners (in Press).
Bowen, F. R., & Chinnis, S. (2022). Multidisciplinary intervention highly effective in decreasing restraint use in paediatric acute care. Evidence-Based Nursing, 25, 58.
Chinnis, S. P., & Stanley, A. (2022). A new model of care: Pediatric asthma management. Online Journal of Rural Nursing and Health Care (in Press).
Dodds, C. B., Kerr, L. K., Cormack, C. L., Kascak, K. L. W., Mulrenin, B., & Hiester, B. (2022). Eye spy: Improving nonverbal communication and interprofessional learning perceptions in health science students. Journal of Humanities in Rehabilitation, April, digital issue.
Cormack, C. L., & Dahlin, C. (2022). The pediatric palliative APRN leader. Journal of Pediatric Health Care, 36, 381–387.
Conner, R. S., Cormack, C. L., Fowler, T. O., & Durham, C. O. (2023). Enhancing DNP student diagnostic and clinical reasoning skills. Journal of Nursing Education, 62, 109–111.
Bernard, D. L., O’Loughlin, K., Davidson, T. M., Rothbaum, A., Anton, M. T., Ridings, L. E., Cooley, J. L., Gavrilova, Y., Hink, A. B., & Ruggiero, K. J. (2022). Differences in mental health engagement and follow-up among black and white patients after traumatic injury. The Journal of Trauma and Acute Care Surgery, 94(1), 117-124
Davidson, T. M., Haws, J., Laifer, L., Acosta, L., Ralston, A., Ruggiero, K., & Andrews, A. (2023). A distinction without a difference? A multimethod approach to understanding PTSD and depression symptom overlap among disaster-exposed adolescents. Research on Child and Adolescent Psychopathology (in Press).
Cordoba, O., Andrews, A., Davidson, T. M., Galea, S., & Ruggiero, K. (2023). Longitudinal and bidirectional associations of post-traumatic stress disorder and emotional support among disaster-affected men and women. Journal of Traumatic Stress (in Press).
Durham, C. O., Lauerer, J. A., & Smith, W. A. (2023). An innovative approach to a multi-track advance practice registered nurse program: The integration of behavioral health and primary care cohorts. Nursing Education Perspectives, 44(2), 130–131.
�� LIFELINES MAGAZINE
Fisher, R. S., Espeleta, H. C., Baskin, L. S., Buchanan, C. L., Chan, Y.-M., … Wisniewski, A. B. (2022). Decisional regret about surgical and nonsurgical issues after genitoplasty among caregivers of female infants with CAH. Journal of Pediatric Urology, 18, 27–33.
Fisher, R. S., Dattilo, T. M., Sharkey, C. M., Traino, K. A., Espeleta, H. C., … Mullins, L. L. L. (2022). Sleep patterns related to emotion dysregulation among adolescents and young adults. Journal of Pediatric Psychology, 47, 111–120.
Espeleta, H. C., Peer, S. O., Are, F., & Hanson, R. F. (2022). Therapists’ perceived competence in trauma-focused cognitive behavioral therapy and client outcomes: Findings from a community-based learning collaborative. Child Maltreatment, 27, 455–465.
Traino, K. A., Espeleta, H. C., Dattilo, T. M., Fisher, R. S., & Mullins, L. L. (2023). Childhood adversity and illness appraisals as predictors of health anxiety in emerging adults with a chronic illness. Journal of Clinical Psychology in Medical Settings, 30, 143–152.
Bakula, D. M., Traino, K. A., Dattilo, T. M., Davis, M. P., Sharkey, C. M., Espeleta, H. C., … Mullins, L. L. L. (2023). Parent psychosocial adjustment to inpatient pediatric rehabilitation, and the role of uncertainty and self-care. Rehabilitation Psychology, 68(2),146-154.
Brier, Z., Hidalgo, J., Espeleta, H., Davidson, T. M., Ruggiero, K., & Price, M. (2023). Assessment of traumatic stress symptoms during the acute post-trauma period. FOCUS: The Journal of Lifelong Learning in Psychiatry (in Press).
Espeleta, H. C., Bakula, D. M., Cherry, A., Lees, J., Shropshire, D., Ruggiero, K. J., Domm, K., Mullins, L. L., & Gillaspy, S. (2023). Caregiver perceptions of the pediatric medical home model to address the health services needs of youth in foster care: A qualitative examination. Children and Youth Services Review (in Press).
Fowler, T. O., Sterrett, J. J., Smith, W. A., Bailey, J. R., & Cartmell, K. (2023). Building the healthcare workforce to serve the underserved. Journal of Interprofessional Education and Practice (in Press).
Fowler, T. O., Sterrett, J. J., Smith, W. A., Bailey, J. R., & Cartmell, K. (2023). Establishing interprofessional clinical learning experiences in primary care safety-net sites. Journal of Interprofessional Care (in Press).
Gulledge, A. M., Miller, S. N., Newman, S. D., Christon, L. M., & Flume, P. A. (2022). Living with cystic fibrosis: The experience of social isolation. International Journal of Nursing and Health Care Science, 02, 13.
Gulledge, A. M., Miller, S. N., Newman, S. D., Mueller, M., Christon, L. M., & Flume, P. A. (2023). Social isolation among adults
living with cystic fibrosis in the United States: A single-center experience. Journal of Nurse Practitioners, 19, 104585.
Guille, C., Johnson, E. E., Douglas, E., Aujla, S. J., Boyars, L. M., Kruis, R., Beeks, R., Cristaldi, K. K., Ford, D. W., & Sterba, K. R. (2022). A pilot study examining access to and satisfaction with maternal mental health and substance use disorder treatment via telemedicine. Telemedicine Reports, 3, 24–29.
Sterba, K. R., Johnson, E. E., Douglas, E., Aujla, R., Boyars, L. M., Kruis, R., Beeks, R., Grater, R., Cristaldi, K. K., Ford, D. W., & Guille, C. (2023). Implementation of a women’s reproductive behavioral health telemedicine program: A qualitative study of barriers and facilitators. BMC Pregnancy and Childbirth, 23, 167.
Kirkland, E. B., Johnson, E. E., Chloe, C., Marsden, J., Verdin, R., Ford, D. W., Cristaldi, K. K., & Sterba, K. R. (2023). Diabetes remote monitoring program implementation: A mixed methods analysis of delivery strategies, barriers and facilitators. Telemedicine Reports (in Press).
Jordan, K., Harris, H. S., Broderick, C., Reese, K., & Jordan, A. (2022). School nurse perceptions of continuing education: Identifying the process of engagement. Journal of Continuing Education in Nursing, 53, 35–41.
Bonham, P. A., Brunette, G., Crestodina, L., Droste, L. R., Gonzalez, A., Kelechi, T. J., Ratliff, C. R., & Varnado, M. F. (2022). 2021 guideline for management of patients with lower-extremity wounds due to diabetes mellitus and/or neuropathic disease: An executive summary. Journal of Wound, Ostomy and Continence Nursing, 49(3), 267-285.
Kelechi, T. J., Hernandez-Tejada, M. A., Balasubramanian, S., Bian, J., Madisetti, M., & Nagel, A. (2022). Addressing physical, functional, and physiological outcomes in older adults using an integrated mHealth intervention “Active for Life”: A Pilot randomized controlled trial. International Journal of Nursing and Health Care Research, 5, Article 3.
Kelechi, T. J., Madisetti, M., Prentice, M., & Mueller, M. (2022). Cooling intervention (MUSTCOOL) for prevention of lower extremity ulcer recurrence: A randomized controlled trial. Journal of Wound, Ostomy, and Continence Nursing, 48, 203–210.
Kelechi, T. J., Mueller, M., Madisetti, M., & Prentice, M. (2023). Efficacy of a self-managed cooling intervention for pain and physical activity in individuals with recently healed chronic venous leg and diabetic foot ulcers: A randomized controlled trial. Journal of Wound, Ostomy, and Continence Nursing, 49, 365–372.
Gainey, S., Muzzy, W., Dooley, M., Lauerer, J., Pelic, C., Rheingold, A. A. A., Holmes-Maybank, K., & Smith, G. (2022). Outcomes and
INNOVATION
�� MUSC COLLEGE OF NURSING
lessons learned from an interprofessional student training program in Screening, Brief Intervention, and Referral to Treatment (SBIRT) at an academic health sciences center. Nurse Education Today, 111, 105323.
York, J. A., Valvano, M., Hughes, F., Sternke, L. M., Lauerer, J. A., Baker, J. A., Edlund, B., Reich, K., & Pope, C. (2023). Nursing leadership and influence in practice domains at a Veterans Affairs Health Care System. Nursing Outlook, 71, 101937.
Hudgins, T., Layne, D., Kusch, C. E., & Lounsbury, K. (2022). Disruptive academic behaviors: The dance between emotional intelligence and academic incivility. Journal of Academic Ethics, 1–21.
Hudgins, T., Brown, K. D., Layne, D., & Maggard Stephens, T. (2022). The effect of academic nurse leaders’ toxic behaviors. The Journal of Nursing Education, 61, 88–92.
Ambrose, J. W., Layne, D. M., Nemeth, L. S., & Nichols, M. G. (2022). A systematic concept analysis of healthcare team resilience in times of disaster and pandemic. Nursing Forum, 57, 671–680.
Hudgins, T. A., Layne, D. M., Kusch, C. E., & Lounsbury, K. (2023). An analysis of the perceptions of incivility in higher education. Journal of Academic Ethics, 21, 177–191.
Stephens, T., & Layne, D. M. (2023). A national survey of nursing faculty resilience, moral courage, and purpose. Journal of Nursing Education (in Press).
Goobie, G. C., Carlsten, C., Johannson, K. A., Khalil, N., Marcoux, V., … Lindell, K. O., … Nouraie, S. M. (2022). Association of particulate matter exposure with lung function and mortality among patients with fibrotic interstitial lung disease. JAMA Internal Medicine, 182, 1248–1259.
Goobie, G. C., Ryerson, C. J., Johannson, K. A., Keil, S., Schikowski, E., … Lindell, K. O., & Nouraie, S. M. (2022). Neighbourhood disadvantage impacts on pulmonary function in patients with sarcoidosis. ERJ Open Research, 8(4), 357-2022.
Goobie, G. C., Ryerson, C. J., Johannson, K. A., Schikowski, E., Zou, R. H., … Lindell, K. O., & Nouraie, S. M. (2022). Neighborhood-level disadvantage impacts on patients with fibrotic interstitial lung disease. American Journal of Respiratory and Critical Care Medicine, 205, 459–467.
Sullivan, D. R., Iyer, A. S., Enguidanos, S., Cox, C. E., Farquhar, M., Janssen, D. J. A., Lindell, K. O., … Reinke, L. F. (2022). Palliative care early in the care continuum among patients with serious respiratory illness: An official ATS/AAHPM/HPNA/SWHPN policy statement. American Journal of Respiratory and Critical Care Medicine, 206, e44–e69.
Goobie, G. C., Li, X., Ryerson, C. J., Carlsten, C., Johannson, K. A., Fabisiak, J. P., Lindell, K. O., … Zhang, Y. (2023). PM and constituent component impacts on global DNA methylation in patients with idiopathic pulmonary fibrosis. Environmental Pollution, 318, 120942.
Madiraca, J., Lindell, K., Coyne, P., & Miller, S. (2023). Palliative care interventions in advanced chronic obstructive pulmonary disease: An integrative review. Journal of Palliative Medicine (in Press).
Gilmore, J., McClendon, J., Madisetti, M., & Kelechi, T. J. (2022). Predictive chronic wound monitoring protocol for healing assessment via intelligent biosensing technology and machine learning. Biomed J Sci & Tech Res., 46(5), 37963-37972.
Lopez, C. M., Baker, N. L., Moreland-Johnson, A. D., Slick, N., Eckard, A. R., Madisetti, M., Resick, P., Safrin, S., & Danielson, C. K. (2023). Development and feasibility testing of an integrated PTSD and adherence intervention Cognitive Processing Therapy-Life Steps (CPT-L) to improve HIV outcomes: Trial Protocol. SSRN (in Press).
Miller, S., Teufel, R., Nichols, M., Davenport, P., Mueller, M., Silverman, E., Madisetti, M., Pittman, M., Kelechi, T., & Strange, C. (2022). Feasibility of RESP-FIT: Technology-enhanced selfmanagement intervention for adults with COPD. International Journal of Chronic Obstructive Pulmonary Disease, 16, 3263–3273.
Dahne, J., Player, M. S., Strange, C., Carpenter, M. J., Ford, D. W., King, K., Miller, S., Kruis, R., Hawes, E., Hidalgo, J. E., & Diaz, V. A. (2022). Proactive electronic visits for smoking cessation and chronic obstructive pulmonary disease screening in primary care: Randomized controlled trial of feasibility, acceptability, and efficacy. Journal of Medical Internet Research, 24, e38663.
Croft, K., Miller, S. N., & Plowman, E. (2023). Provision of oral care in the cardiothoracic ICU: A survey of nursing staff. Journal of Nursing Education (in Press).
Parker, L. A., Bendixen, M., Sullivan, S., Cacho, N., & Mueller, M. (2022). Antepartum breast pump education for mothers and their support person: Effect on time to first expression and lactation outcomes-a randomized controlled pilot study. Breastfeeding Medicine, 17, 437–445.
Stafford, L., Valcarce, V., Henry, M., Neu, J., Parker, L., Mueller, M., … Larkin, J. (2022). Detection of SARS-CoV-2 IgA and IgG in human milk and breastfeeding infant stool 6 months after maternal COVID-19 vaccination. Research Square, digital issue.
Kanter, J., Schlenz, A. M., Mueller, M., Humphrey, D., Sirline, L. P., Stevens, J., Melvin, C. L., Adams, R. J., & Phillips, S. (2022). Dissemination and implementation of stroke prevention looking at the care environment (DISPLACE) study evaluates novel interventions to
� 3 LIFELINES MAGAZINE
improve TCD (Sickle Stroke Screening) implementation. Blood, 140, 5009–5010.
Lisanby, S. H., McClintock, S. M., McCall, W. V., Knapp, R. G., Cullum, C. M., Mueller, M., … Prolonging Remission in Depressed Elderly (PRIDE) Work Group. (2022). Longitudinal neurocognitive effects of combined Electroconvulsive Therapy (ECT) and pharmacotherapy in major depressive disorder in older adults: Phase 2 of the PRIDE study. The American Journal of Geriatric Psychiatry, 30, 15–28.
Parker, L. A., Cacho, N., Bendixen, M. M. M., Sullivan, S., Magãlhaes, M., Krueger, C., & Mueller, M. (2022). Measures of lactation outcomes in women delivering preterm infants. Nursing Research, 70, 193–199.
McManus, K. R., Lapid, M. I., Forester, B. P., Mueller, M., … Johnson, E. K., & Petrides, G. (2022). Simulated electroconvulsive therapy: A novel approach to a control group in clinical trials. The Journal of ECT, 38(3), 165–170.
Haviland, K., Mueller, M., Walters, C. B., & Kelechi, T. J. (2023). Disparities in cancer screening in sexual and gender minority populations: A secondary analysis of the Behavioral Risk Factor Surveillance System data. Oncology Nursing Forum, 50, 157–167.
Stafford, L. S., Valcarce, V., Henry, M., Neu, J., Parker, L., Mueller, M., … Larkin, J. (2023). Editorial response to Cosentino and Marino RE: detection of SARS-CoV-2 IgA and IgG in human milk and breastfeeding infant stool 6 months after maternal COVID-19 vaccination. Journal of Perinatology, 1–2.
Stafford, L. S., Valcarce, V., Henry, M., Neu, J., Parker, L., Mueller, M., … Larkin, J. (2023). Detection of SARS-CoV-2 IgA and IgG in human milk and breastfeeding infant stool 6 months after maternal COVID-19 vaccination. Journal of Perinatology (in Press).
Tejada-Hernandez, M., Balasubramanian, S., Nagel, A., Madisetti, M., & Kelechi, T. J. (2022). Feasibility trial of an integrated treatment “Activate for Life” for physical and mental well-being in older adults. Pilot and Feasibility Studies, 8, 38.
Calvo-Schimmel, A., Newman, S. D., Sterba, K. R., Miaskowski, C., & Qanungo, S. (2022). Barriers and facilitators to supportive care implementation in advanced disease prostate cancer survivors: A theory-informed scoping review. Cancer Nursing, 45, E782–E800.
Logan, C.-S., Newman, S. D., Robert, S., & Nichols, M. G. (2022). Describing South Carolina public school administrators’ perceptions and experiences related to school-based interventions and strategies to promote health physical activity and eating behaviors: A qualitative study. Journal of School Health, 92(6), 581-593.
Camp-Spivey, L. J., Newman, S. D., Stevens, R. N., & Nichols,
M. (2022). Survey of South Carolina public school personnel perspectives on barriers and facilitators to regular physical activity and healthy eating behaviors in schools. The Journal of School Health, 92, 1062–1073.
Calvo-Schimmel, A., Newman, S. D., Sterba, K. R., Mueller, M., Miaskowski, C., & Qanungo, S. (2022). Unmet supportive care needs in prostate cancer survivors with advanced disease: A mixed-methods exploration. Canadian Oncology Nursing Journal, 32, 512–525.
Newman, S. D., Toatley, S., Rodgers, M. D., Qanungo, S., Mueller, M., Denny, B., & Rodriguez, A. (2023). Feasibility of a communitybased, online, peer-supported spinal cord injury self-management intervention: Protocol for a pilot wait-listed randomized trial. JMIR Research Protocols, 12, e42688.
Singh, A., Arulogun, O., Akinyemi, J., Nichols, M. G., Calys-Tagoe, B., Ojebuyi, B., Jenkins, C. M., … Akinyemi, R. (2022). Biological sample donation and informed consent for neurobiobanking: Evidence from a community survey in Ghana and Nigeria. PLoS ONE 17(8): e0267705.
Uvere, E., Nichols, M. G., Ojebuyi, B. R., Yahaya, I. S., Calys-Tagoe, B., Jenkins, C. M., … Akinyemi, R. (2022). Capacity-building for stroke genomic research data collection: The African-Neurobiobank ELSI Project experience. Biopreservation and Biobanking, 21(2), 158-165.
Nichols, M. G., Arulogun, O., Singh, A., Olorunsogbon, O., Uvere, E., Melikam, S., Akinyemi, J., Jenkins, C., Owolabi, M., Ovbiagela, B., & Akinyemi, R. (2022). Community insight on the ethical, legal, and social implications of stroke genomic and biobanking research in Sub-Sharan Africa. Journal of Stroke and Cerebrovascular Diseases, 31(4), 106356.
Nichols, M. G., Magwood, G. S., Woodbury, M. L., Brown, K., Jenkins, C. M., & Owolabi, M. (2022). Crafting community-based participatory research stroke interventions. Stroke, 53, 680–688.
Adigun, M., Ojebuyi, B. R., Akinyemi, J., Wahab, K., Akpalu, A., … Nichols, M. G., Jenkins, C. M., … Akinyemi, R. (2022). Human rights implications of stroke biobanking and genomics research in SubSaharan Africa. International Human Rights Law Review, 11, 112–137.
Bedeker, A., Nichols, M. G., Allie, T., Tamuhla, T., van Heusden, P., Olorunsogbon, O., & Tiffin, N. (2022). A framework for the promotion of ethical benefit sharing in health research. BMJ Global Health, 7(2), e008096.
Adigun, M., Ojebuyi, B. R., Akinyemi, J., Wahab, K., Akpalu, A., Nichols, M. G., Jenkins, C. M., … Akinyemi, R. (2022). Legal implications of stroke biobanking and genomics research in SubSaharan Africa. Journal of Legal Medicine, 29(2), 579-598.
INNOVATION � 4 MUSC COLLEGE OF NURSING
Adigun, M., Ojebuyi, B., Akinyemi, J., Wahab, K., Akpalu, A., … Nichols, M. G., Jenkins, C., … Akinyemi, R. (2022). Symbolic legislation and the regulation of stroke biobanking and genomics research in Sub-Saharan Africa. The Theory and Practice of Legislation, 9, 404-424.
Arulogun, O., Nichols, M. G., Jenkins, C. M., Fakunle, A., Akpa, O., … Owolabi, M. (2023). Are there differences in perceptions, preferences, and attitudes towards disclosure of genetic testing for stroke? A qualitative study among stroke-free SIREN-SIBS Genomics study participants. Journal of Stroke and Cerebrovascular Diseases, 32(3), 106978
Sarfo, F. S., Nichols, M. G., Opare-Addo, P., & Ovbiagele, B. (2023). Polypill programs to prevent stroke and cut costs in low-income countries: Moving from clinical efficacy to pragmatic implementation. Stroke, 54, 407–414.
Sarfo, F. S., Akinyemi, J., Obiako, R., Nichols, M. G., Fakunle, A., Adusei, N., Ampofo, M. M., Arulogun, O., Jenkins, C. M., … Owolabi, M. (2023). Effect on an educational intervention for primary stroke risk reduction in West Africa: A pilot RCT. Stroke (in Press).
Chargualaf, K., Bourgault, A., Torkildson, C., Graham-Clark, C., Nuñez, S., … Nichols, M. G. (2023). Learning from the COVID-19 pandemic to retain new graduate nurses in the workforce. Nursing Management (in Press).
Sumpter, I., Phillips, S., & Magwood, G. S. (2022). Approaches to reducing fragmented care in systemic lupus erythematosus (SLE) and other multimorbid conditions: A realist review. International Journal of Care Coordination, 25(4), 103–114.
Schlenz, A. M., Phillips, S. M., Mueller, M., Melvin, C. L., Adams, R. J., & Kanter, J. (2022). Barriers and facilitators to chronic red cell transfusion therapy in pediatric sickle cell anemia. Journal of Pediatric Hematology/Oncology Nursing, 39, 209–220.
Shady, K., Phillips, S., & Newman, S. D. (2022). Barriers and facilitators to healthcare access in adults with intellectual and developmental disorders and communication difficulties: an integrative review. Review Journal of Autism and Developmental Disorders, digital issue.
Phillips, S., Chen, Y., Masese, R., Noisette, L., Jordan, K., Jacobs, S., Hsu, L. L. L., Melvin, C. L., Treadwell, M., Shah, N., Tanabe, P., & Kanter, J. (2022). Perspectives of individuals with sickle cell disease on barriers to care. PloS One, 17, e0265342.
Galandanci, N. A., Phillips, S., Schlenz, A. M., & Kanter, J. (2022). Variation in newborn screening follow up processes for sickle cell disease. Blood, 140, 11120–11121.
Phillips, S., Schlenz, A. M., D’Alton, S. V., Johnson, M., & Kanter, J. (2023). Patient and family opioid decision making for pain management in sickle cell disease: a qualitative study. Journal of Pain (in Press).
Schlenz, A. M., Phillips, S., Mueller, M., & Kanter, J. (2023). Practice patterns for addressing developmental-behavioral concerns in sickle cell specialty care. Clinical Psychology and Psychotherapy (in Press).
Poston, K. M., Brunette, G., & Ciccone, J. (2023). Collaborative strategies to improve clinical judgment and address bedside care challenges. Teaching and Learning in Nursing (in Press).
Cartmell, K. B., Kenneson, S. A., Roy, R., Bhattacharjee, G., Panda, N., Kumar, G., & Qanungo, S. (2022). Feasibility of a palliative care intervention utilizing community health workers to facilitate delivery of home-based palliative care in India. Indian Journal of Palliative Care, 28, 21–27.
Powell, R. A., Ali, Z., Gikaara, N., Qanungo, S., Melikam, S. E., & Cartmell, K. (2022). Research attitudes, practice and literacy among Kenyan palliative care healthcare professionals: An observational, cross-sectional online survey. BMJ Supportive and Palliative Care, 21(1), 206.
Helms, J., & Reinbeck, D. (2022). Improving rates of pneumococcal vaccination in a skilled nursing facility. Journal of Gerontological Nursing, 48, 52–56.
Jackson, H. J., Reneau, M. G., & Hande, K. (2022). A scoping review of measures utilized to assess patient satisfaction with acupuncture treatments within randomized controlled trials. Medical Acupuncture, 34, 308–315.
Hink, A. B., Killings, X., Bhatt, A., Ridings, L. E., & Andrews, A. L. (2022). Adolescent suicide-Understanding unique risks and opportunities for trauma centers to recognize, intervene, and prevent a leading cause of death. Current Trauma Reports, 1–13.
Ridings, L. E., Espeleta, H. C., Streck, C. J., Davidson, T. M., Litvitskiy, N., Bravoco, O., Kassam-Adams, N., & Ruggiero, K. J. (2022). Assessing service quality and access in trauma centers through behavioral health screening, education, and treatment after pediatric injury. Journal of Pediatric Surgery, 57, 632–636.
Dalton, S. V., Ridings, L., Williams, C. S. P., & Phillips, S. (2022). The bereavement experiences of children following sibling death: an integrative review. Journal of Pediatric Nursing, 66, e82–e99.
Ridings, L. E., Davidson, T. M., Walker, J., Winkelmann, J., Anton, M. T., Espeleta, H. C., Nemeth, L. S., Streck, C. J., & Ruggiero, K. J. (2022). Caregivers’ and young children’s emotional health needs
� 5 LIFELINES MAGAZINE
INNOVATION
after pediatric traumatic injury. Clinical Pediatrics, 61, 560–569.
Gilmore, A. K., Mosley, E. A., Oesterle, D. W., Ridings, L. E., … Ruggiero, K., Kaysen, D., Danielson, C. K., & Self-Brown, S. (2023). Teen Well Check : An e-health prevention program for substance use, sexual assault, and sexual risk behaviors for adolescents in primary care. European Journal of Psychotraumatology, 14, 2157933.
Cusack, S., Ridings, L., Davidson, T. M., Espeleta, H., Wilson, D., & Ruggiero, K. (2023). Social support in relation to PTSD symptoms among patients with violent vs. non-violent Injury. Psychological Trauma: Theory, Research, Practice, and Policy (in Press).
Ruggiero, K. J., Anton, M. T., Davidson, T. M., deRoon-Cassini, T. A., & Hink, A. B. (2022). It is time to prioritize complete trauma care. The Journal of Trauma and Acute Care Surgery, 92, e18–e21.
Shanholtz, C., Ruggiero, K., Hanson, R., Anton, M., Ridings, L., Espeleta, H., Saunders, B., & Davidson, T. M. (2023). A comparison of the readiness of youth service agencies to implement a technology-based toolkit to support treatment delivery. Community Mental Health Journal (in Press).
Lesher, A., McDuffie, L., Smith, T., Foster, A., Ruggiero, K., Barroso, J., & Gavrilova, Y. (2023). Optimizing an outpatient mHealth intervention for children with burns: A convergent mixed-methods study. Journal of Burn Care and Research (in Press).
Smith, W., Lauerer, J., & Durham, C. O. (2022). An innovative approach to a multitrack advance practice registered nurse program: The integration of psychiatric mental health and primary care cohorts. Nursing Education Perspectives, Nursing Education Perspectives, 44, 130–131.
Smith, W. A., & Davila, N. M. (2023). Updates and clinical pearls from the 2021 American College of Gastroenterology (ACG) Gastroesophageal Reflux Disease Clinical Guideline. The Nurse Practitioner (in Press).
Terzulli, D. M. (2022). Development of an autonomic dysreflexia simulation. Teaching and Learning in Nursing, 17, 494–497.
Terzulli, D. M., Smith, A., & Klein, A. M. (2022). An innovative approach to teaching dosage calculations using mirror technology. Nurse Educator, 48(1), 42.
Terzulli, D. M. (2023). Using dating profiles to teach pathopharmacology. Journal of Nursing Education, 61(12), 725.

Wagner, J. L., Brothers, S. L., Guilfoyle, S. M., Modi, A. C., Smith, G., & Clifford, L. M. (2022). Behavioral health screening in pediatric epilepsy: Which measures commonly used in the United States are “good enough”? Epilepsy & Behavior, 134, 108818.
Wagner, J. L., Bhatia, S., Marquis, B. O., Vetter, I., Beatty, C. W., … Skjei, K. (2023). Health disparities in pediatric epilepsy: Methods and lessons learned. Journal of Clinical Psychology in Medical Settings, 30(2), 251–260.
Schmidt, M., Glaser, N., Riedy, T., Rietta, C., Huszti, H., Wagner, J., Smith, G., … Modi, A. C. (2022). Learning experience design of an mHealth intervention for parents of children with epilepsy. International Journal of Medical Informatics, 160, 104671.
Mitchell, J., Wagner, J. L., Jobst, B., Sajatovic, M., & Berg, A. T. (2023). Beyond seizures: Tapping into the community. Epilepsy Currents (in Press).
Sumneangsanor, T., Ruchiwit, M., & Weglicki, L. (2022). The effects of a biofeedback and music training programme in reducing stress in Thai patients living with cancer receiving palliative care. International Journal of Palliative Nursing, 28(10), 453–463.
Fawcett, S., Williams, A. A., Johnson, E. E., & Ramsey, K. (2022). Improving treatment of chlamydia and gonorrhea infections during the COVID-19 pandemic: A quality improvement study utilizing provisional Centers for Disease Control guidance. Journal of the American Association of Nurse Practitioners, 34, 373–380.
Scan the QR code or visit bit.ly/3NiTNgs to learn more about the research interests of MUSC College of Nursing faculty. � 6 MUSC COLLEGE OF NURSING
INSPIRATION
THE NEXT STEP
After 48 years in nursing, Dean Linda S. Weglicki, Ph.D., R.N., is transitioning into retirement to intentionally prioritize family and the next phase of life beyond the many competing demands and challenges as MUSC’s top academic nurse leader. While reflecting on some of the highlights of her illustrious career, Dean Weglicki credits the people and life experiences that have shaped her as a nurse and leader and reveals why she has always worked hard to be one step ahead.

� 7 LIFELINES MAGAZINE
Photo by Zheng Chia.
INSPIRATION
What first inspired you to pursue a nursing career?
This will not sound strange to those who grew up as part of the baby boomer generation: My formal introduction to nursing began in high school. As a ninth grader, I worked as a candy striper at our local hospital and belonged to the Future Nurses Club, and in my senior year, instead of attending classes, I worked as a nurse tech in my high school-sponsored health care program.

My mother, who attended nursing school when I was young, was a great influence and role model in my decision to pursue a career in nursing. At that time, she was raising four young children, studying, and then serving as part of the nursing workforce in our community hospital. Two years after I finished high school I graduated from Harper Hospital School of Nursing, a Detroit hospital-based diploma program, and my first position as a new graduate nurse was in the
ICU at the Detroit Medical Center, where I quickly advanced my clinical knowledge and skills.
Even as a new nurse, it seems you were looking ahead to the next step. What motivated that focus on self-improvement and growth?
During my early developmental years in nursing, I realized that my calling and passion were in education and mentoring. I sought out clinical and leadership opportunities in these areas by challenging myself within the profession in many roles, including as a nurse manager, in-serviceinstructor, hospital nursing supervisor, clinical specialist in oncology, and then nurse recruiter for a multi-hospital system during the 1980 nursing workforce shortage. However, I realized that in order to have a greater impact in nursing education, I had to advance my own education and did so by completing my BSN, MSN, and certification in teaching and
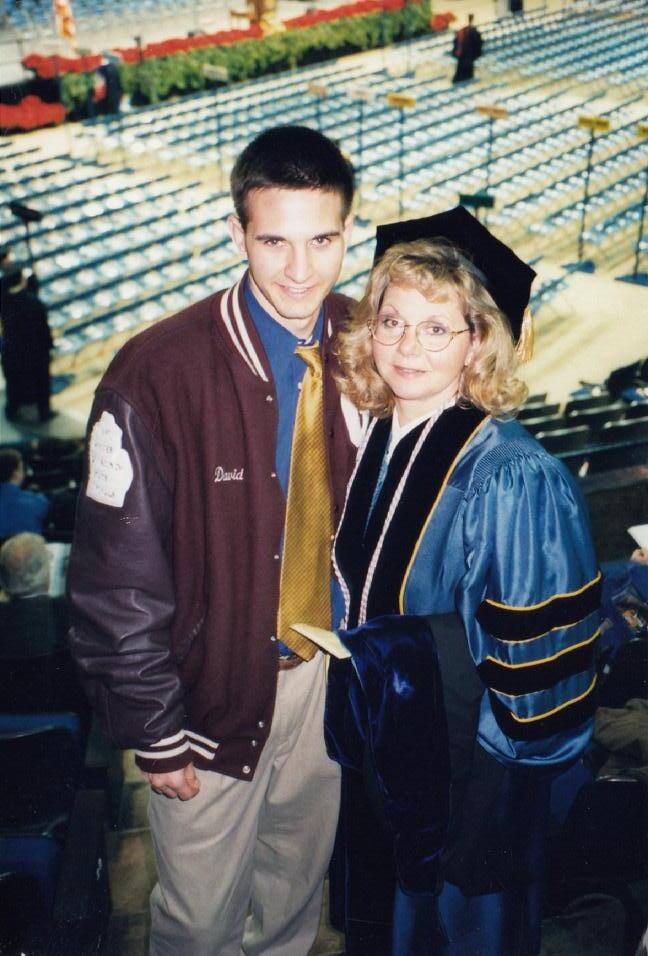
education at Wayne State University (WSU) and then my Ph.D. in Nursing Science from the University of Michigan (U-M).
Both universities were such rich environments for learning the value of nursing theory to guide practice and research, the principles of a strong teaching philosophy and pedagogy, the importance of mentorship at all levels and colleagueship, and how to be successful as an academician. Over the course of my 18 years at WSU, I learned, collaborated and worked with esteemed nurse leaders and trailblazers such as Gloria Smith, Ada Jacox, Madeleine Leininger, Marjorie Eisenberg, Jackie Campbell, Edythe Hough, Virginal Hill Rice, Marilyn Oermann, Virginia McBride, and Barbara Redman. During my Ph.D. program at U-M, my nursing career as a researcher was keenly shaped by Shake Ketefian, Ada Sue Henshaw, Nola Pender, Richard Redman, Carolyn Sampsell, Carol Loveland-Cherry, and Sally Lusk—many of whom
Above: Inspired by her mother to enter nursing, Weglicki has always viewed her family as an integral part of her nursing career.
� 8 MUSC COLLEGE OF NURSING
Photos by Josh Goodwin and provided.
are now Living Legends in the American Academy of Nursing. As role models, they inspired me that a nurse’s education is never finished. Who were some of the most influential people on your journey to becoming a dean?
That’s a tough question, because I have been so fortunate to have many important people shape my career and who I am today. My mother Janice first, not only because she pursued a career as a nurse in the early 1960s, but also because she taught me that I could achieve any goal in life if I worked hard and sought opportunities to grow. Specific to nursing, a few significant people immediately come to mind. Dr. Fredricka Shea, WSU professor and my master’s thesis advisor, taught me the value of finding your voice and asserting yourself, particularly when continuing to search for different answers when no new answers appear to exist, no matter how many ways you analyze the problem or data. Freddie kept asking me to run one more analysis of my data. One day I remember walking into her office and saying, Dr. Shea, no matter how many new analyses I run, I am not finding anything new. At that moment she smiled at me and said, “Congratulations, you have finished with your master’s thesis.”
Dr. Marilyn Oermann, a professor at WSU at the time and a prolific author in nursing education, had a tremendous impact on my professional development and journey. She not only challenged me in so many ways but was that person who said, “You are capable of doing so much more, and these
are the tools you need to develop to be the leader that I see and that you are meant to be.” Marilyn was my mentor and cheerleader at several pivotal points early in my career trajectory. Dr. Nola Pender, U-M professor and author of Pender’s Health Promotion Model, inspired and taught me the importance of being bold, thinking big, and setting goals and then giving everything I can to achieve them. Nola is a woman with such grace and kindness in her interactions with everyone and modeled for me the value of showing empathy, no matter how difficult the situation.
Dr. Mary Kerr, Deputy Director, National Institute of Nursing Research, was an excellent role model as a leader. Her mentorship provided me with the opportunity to grow my own leadership skills supported by participating in a number of federal leadership training programs, including a year-long NIH Executive Mentored Leadership Training program. I have used many of the principles and skills from that leadership training program in my dean’s role every day. Finally, Dr. Marlaine Smith, Florida Atlantic University (FAU) College of Nursing Dean, is well-known
for advancing unitary and caring perspectives in nursing and nursing science. Marlaine epitomized caring and actualized its tenets within her role as dean. I met her at a time when I was reflecting about what was on the horizon for the last years of my career in nursing. Through working with Marlaine, I knew that I wanted to emulate the nuances of caring she demonstrated in all aspects of her leadership.
How did mentorship play a role in preparing you to become a dean?
I figured out a long time ago that you cannot effect change nor create opportunities that will be supported if you don’t garner support from others and work as a team. I believe that as a leader, you are likely to be more effective if you create an environment—a culture really— where you don’t work against one another but instead embrace a common shared vision and goals. For me personally, I dedicated time and sought out as many leadership training opportunities as I could, first as a student, then as a young instructor and assistant professor, while at the National Institutes of Health, in professional organizations such as Sigma Theta
 Weglicki with MUSC ABSN nursing students.
Weglicki with MUSC ABSN nursing students.
� 9 LIFELINES MAGAZINE
INSPIRATION
Tau, through my local chapter and at the international level, at Midwest Nursing Research Society, the Council of Advanced Nursing Science, as an ambassador to the Friends of the National Institute of Nursing Research, and the American Association of Colleges of Nursing. Sometimes I took risks and detours, but for each path that I chose, I looked to leaders who held similar positions for their insight, mentorship, brainstorming, and consultation. I have been very fortunate in having dedicated, caring, and nurturing mentors along the way as I have challenged myself throughout my career to seek new and different paths where I could grow and cultivate the skills, characteristics, and requisites to prepare me for the complexity of being a dean during a time of continual change and persistent challenges. As a new dean at MUSC in 2018, I was fortunate to work with three experienced deans of fellow colleges of nursing in brainstorming, strategizing, and learning from their past experiences as I encountered new and demanding situations in my role.
Of what are you most proud from your tenure as Dean of MUSC College of Nursing?
Since becoming the dean in summer of 2018, there have certainly been many challenges that I believe we have successfully navigated and of which I am proud. Some of the ‘points of pride’ that immediately come to mind are:
1. Building a national and international reputation and designation as leaders in palliative care education and practice
2. Enhancing our working and collaborative academic-practice partnerships and relationship with MUSC Health-Charleston as well as all our new MUSC Regional Health Networks, Roper Saint Francis, and others
3. Successfully navigating the COVID 19 pandemic with our students being well-prepared as they graduated on time and entered the nursing workforce practiceready;
4. Increasing our ABSN graduate first time annualized NCLEX-RN
pass rates from ~91% (2018) to 99% (2022) and DNP specialty track certification first time pass rates to 100%
5. Enhancing and growing donor support of scholarships to support our students across all programs, reducing their student debt, and strategically increasing support to our doctoral students
6. Reorganizing the college’s leadership model so that assistant deans fully understand, appreciate, and support the developmental needs, expertise, work, and accomplishments of each faculty member teaching in their respective programs
7. Building out and implementing the Responsibility Center Management (RCM) budget model within the college so that it aligns with the university RCM budget model, which enables us to strategically plan, forecast, and manage costs of all our offices and individual programs—critical to effectively managing revenue and expenditures, especially when primary traditional revenue streams are challenged
8. Supporting growth of infrastructure in the Offices of Finance and Administration, Research, Academics, Practice, and our Nursing Technology Center in order to improve customer service as well as provide the expertise required to effectively support each of our programs
L-R: Weglicki joined MUSC HealthCharleston CNO Dr. Patti Hart and MUSC First Lady Kathy Cole at the 2022 Celebrating Wisdom Reception, which paid tribute to nurses with 25+ years of MUSC-Health service.

3 � MUSC COLLEGE OF NURSING
9. Providing opportunities to learn and grow through critical and challenging conversations in a respectful environment that honors each person for their diversity, uniqueness, talents, and gifts with the goal of enhancing belonging and inclusiveness
10. Advocating and lobbying for nursing, growth in nursing education programs and research, nursing and faculty workforce enhancement, and removal of barriers to nursing care and access provided by APRNs by permitting them to practice to the full extent of their clinical training and education at the state and federal level.
What do you believe are the most pressing challenges facing academic nursing today?


Unfortunately, we are encountering many complex factors influencing nursing today that we must, as academic leaders, educators, advocates, and influencers, be bold enough to address concomitantly. For example, some of the most pervasive multifaceted challenges are: a) the increasing shortages in the nursing workforce (including new graduates entering the workforce as well as faculty and researchers), b) limitations to professional practice where we cannot practice to the full extent
of clinical training and education, particularly in rural and underserved areas where access to care is so limited, c) changing health care delivery models which limit nursepatient contact and may impact quality of care, d) nurse staffing shortages and frequent turnover, e)evolving challenges for colleges and schools of nursing in securing clinical placements and preceptors, f)post COVID-19 pandemic new stressors that have resulted in workrelated burnout, increases in patient as well as peer horizontal violence, higher nurse turnover and turnover intention, and g) perceived or real lack of ability to decompress and disconnect from a virtual workplace, whether nurses work at a hospital bedside, community or clinic setting, or in colleges and schools of nursing. Over time, these complex challenges take a toll and negatively impact our mental and physical health, wellbeing, and ability to be resilient. In my opinion, these cumulative and sustained effects are creating the most pressing challenges facing academic nursing and can impact the care that we provide to our patients, families, communities, and societies that we serve.
Looking ahead, what’s next?
For me personally, I see a quieter and more relaxing time when I
will be able to disconnect and just enjoy all the blessings around me, especially quality time with my family and friends. I really haven’t had a lot of time over the past several years to savor the day without being mindful of upcoming deadlines or not having “just one more email to respond to,” (a standing joke in my family). I am overjoyed that I will be reuniting and living under the same roof as Larry, my husband of 47 years; I want to sit quietly and have an unrushed cup of coffee in the mornings as the sun comes up—we are both early risers and love that special time together as the day begins. I appreciate working outdoors in the yard and in my garden and taking walks, and I will finally have leisure time to enjoy with my daughter Michelle. I also look forward to driving rather than flying to Michigan, stopping at some of the beautiful places along the way, and spending the summer with my mother, my son David and daughter-in-law Kathleen, and brother and sisters who live in Michigan. It really is about having the time and spending it with those I love, and that is the next step I look forward to most.
L: Weglicki's leadership was instrumental in CON's continuing operations during the COVID-19 pandemic. R: Weglicki and her husband of 47 years, Larry.
3 � LIFELINES MAGAZINE
MILESTONES OF A 48-YEAR NURSING CAREER

� Expansion of the 1975 Nurse Training Act; ANA published Standards for Nursing Education, Accreditation of Continuing Education in Nursing, and Programs for Preparing Nurses for Advanced Roles
� Elimination of the nurse’s cap and traditional white uniform, white hose, and shoes
� Changes in models of care delivery and length of stay for hospitalized patients
� Transfer of patient record keeping and nurses’ notes to electronic health records

� AIDS and HIV epidemic resulted in changes in infection control practices, early 1980s
� Changes in autonomy of practice, including shift in traditional 8-hour workdays to 12-hour and flex schedules; Greater opportunities to practice in a diversity of health care settings
� National standardization of RN licensure overseen by National Council of State Boards of Nursing; nursing licensure compact available in many states
� Accreditation of nursing education programs required and overseen by Commission on Collegiate Nursing Education and Accreditation Commission for Education in Nursing

� Proliferation of nursing education programs1st Ph.D. in Nursing Science (~1975); Launch of DNP (1979) and specialty and certification programs
� ANA endorsed “Nursing: A Social Policy Statement” which defines nursing and its scope of practice, 1980
� New generation of high-fidelity simulators replaced Mrs. Chase dolls and became mainstay in nursing classrooms and skills labs
INSPIRATION
3 � MUSC COLLEGE OF NURSING
Weglicki with CON students during Convocation.
� National Center for Nursing Research at NIH established in 1986; was named the National Institute of Nursing Research (NINR) in 1993
� Following the naming and expansion of NINR, growth and respect of nursing science to inform evidence-based practice increased and new nursing research journals emerged

� The focus of nursing research evolved from patients and patient behavior (1980s) to clinical research, practice research utilization, and evidenced-based practice (1990s), and effectiveness of nursing interventions, quality and cost-effectiveness and health promotion, disease prevention, and symptom management (mid 1990 – 2000s)
� Total number of nursing colleges/universities grew to over 2600 in 2022
� First RN (Texas) elected to Congress, 1992
� Consensus Model for APRN Regulation: Licensure, Accreditation, Certification & Education, 2008
� Institute of Medicine released Future of Nursing report, 2010

� Worldwide COVID-19 pandemic transformed nursing; resulted in nurses being on the frontlines of care, stress, and burnout in the workforce
� Nurses now make up the largest workforce in health care, and one of the fastest growing industries in the US
� Slow increases in diversity within the profession, including men
� Nurses ranked #1 in honesty and ethical standards for 21 years in a row by US Gallup Poll
From her days as a new nursing student (left) to serving as the Dean of MUSC College of Nursing, Weglicki has built a legacy spanning a half century in nursing. In May, she joined her fellow MUSC college deans during Commencement.
33 LIFELINES MAGAZINE
Photo by Zheng Chia.
LOVE CONNECTION
College of Nursing Equips Students with Palliative Care Training
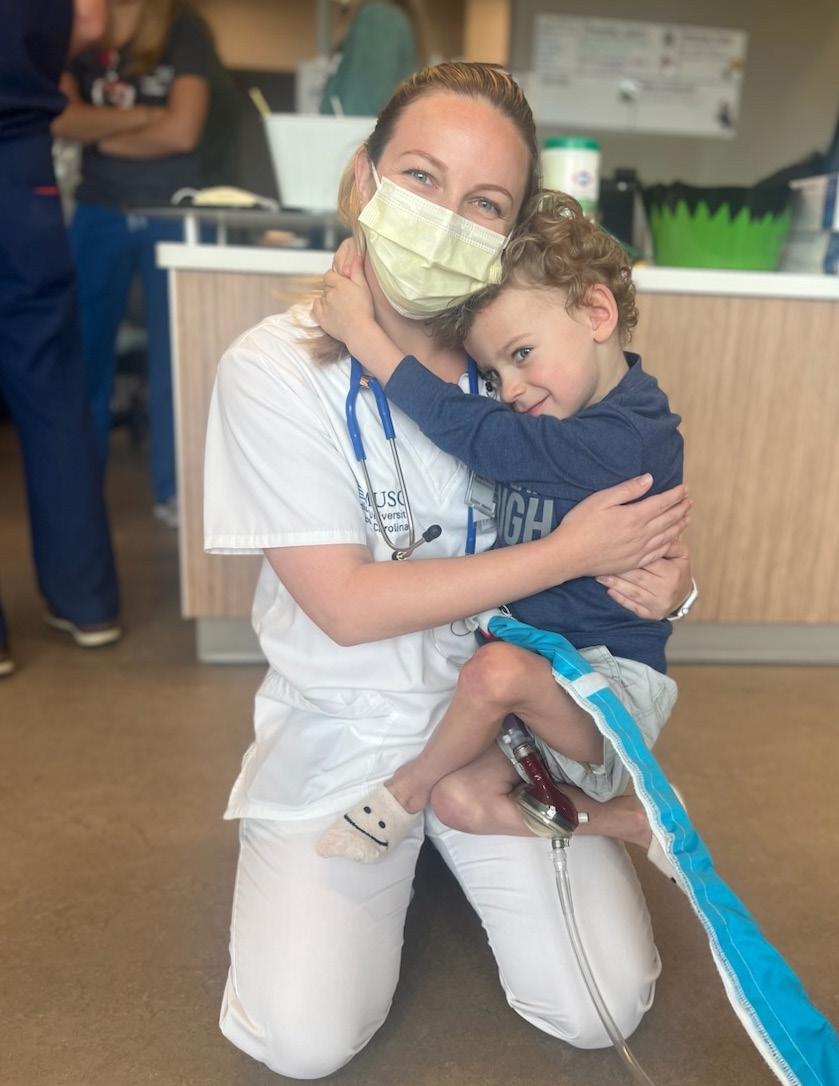 by Harrison Huntley, MUSC Catalyst News Office of Public Affairs and Media Relations
by Harrison Huntley, MUSC Catalyst News Office of Public Affairs and Media Relations

web.musc.edu/about/news-center
November is National Hospice and Palliative Care Month, and while many may be familiar with hospice care, palliative care is a lesser-known term outside of the medical field. However, with help from Kathleen Lindell, Ph.D., R.N., ATSF, FAAN, Associate Professor and the Mary Swain Endowed Chair in Palliative Care Health, and Carrie Cormack, DNP, APRN, CPNP, the lead faculty in palliative care education, it is now an integral part of the curriculum at
MUSC College of Nursing (CON).
To explain palliative care, Lindell points to the World Health Organization’s definition, which describes it as care that “improves the quality of life of patients and that of their families who are facing challenges associated with lifethreatening illness, whether physical, psychological, social or spiritual.” While it’s often associated with hospice care, Lindell is quick to point out that the two are different.
“Palliative care is an extra layer of support to help patients who have a serious illness across the patient’s lifespan,” she explained. “Hospice is offered ideally within the last six months of life and is focused on comfort. Palliative care can be offered alongside curative care, for instance, while patients are undergoing chemotherapy, being evaluated for a transplant or receiving dialysis, to name a few. When patients receive hospice, the focus is on comfort care,
INSPIRATION
v 34 MUSC COLLEGE OF NURSING
Wilson with Luke in the cardiac unit of the MUSC Shawn Jenkins Children’s Hospital.
not curative care.”
Linda S. Weglicki, Ph.D., R.N., dean of MUSC’s College of Nursing, Cormack and Lindell have created an environment where all of the graduate and undergraduate students receive palliative care education through the End-of-Life Nursing Education Consortium (ELNEC) curriculum. These ELNEC online modules provide all CON students with palliative care certification. This certification—combined with embedded clinical experiences and projects—helps students to care for patients dealing with life-threatening illnesses more effectually. “Ultimately, what happens is that patients with serious illnesses get better care. You improve the quality of life for individuals with serious illnesses and their families,” said Lindell.
Karoline Fossell knows this firsthand. CON students, as part of
their clinical rotations, worked with her young son, Luke Fossell, when he was a patient at Shawn Jenkins Children’s Hospital and waiting for a heart transplant. During his 5-month hospital stay, he engaged in growth and development activities with some third-semester students. Lindell said that the students experienced palliative care in action with the Fossells while Luke was waiting for his new heart. “In those situations, patients and families are scared. And so palliative care is this extra layer of attention to help to address their fears,” Lindell explained.
Karoline Fossell values what the MUSC palliative care team is able to offer to families. “Our lives had been turned upside down, but palliative care at MUSC ensured that not only was Luke taken care of, but that we, as his parents, were as well,” she said. “The palliative care team members at
MUSC collaborated with all of those involved in Luke’s care and really helped to make sure that every aspect of his care was well coordinated.”

In December, Luke received a heart transplant at the children’s hospital and is now enjoying life back home with his family. “Watching Luke live life with the happiness and energy that a little boy should is remarkable,” his mother shared. “We can never thank the medical staff at MUSC enough not only for saving Luke’s life, but also for being there for our family. It’s easy to want to push all that Luke went through to the back of our memory. But the truth is, there is also a lot we never want to forget. The cardiac staff became a part of our family, and we made it through our six-month stay with ease because of them. We can’t wait to see all that Luke accomplishes in life with his brand-new heart!”

w
v
Luke Fossell hugs ABSN nursing students Jenna Wilson, left, and Vivian Sayavong. All College of Nursing students get extensive training in palliative care.
Luke at home today.
35 LIFELINES MAGAZINE
Photos by Karoline Fossell and provided.
While still working in finance, Boden volunteered with the Goose Creek Fire Department. Ironically, he responded to exactly zero fires during the year or so he worked there – but the job was life-changing nonetheless.
Josh Goodwin.
FROM SUITS TO SCRUBS
How One Nursing Grad Made the Bold Move to Change Careers Completely
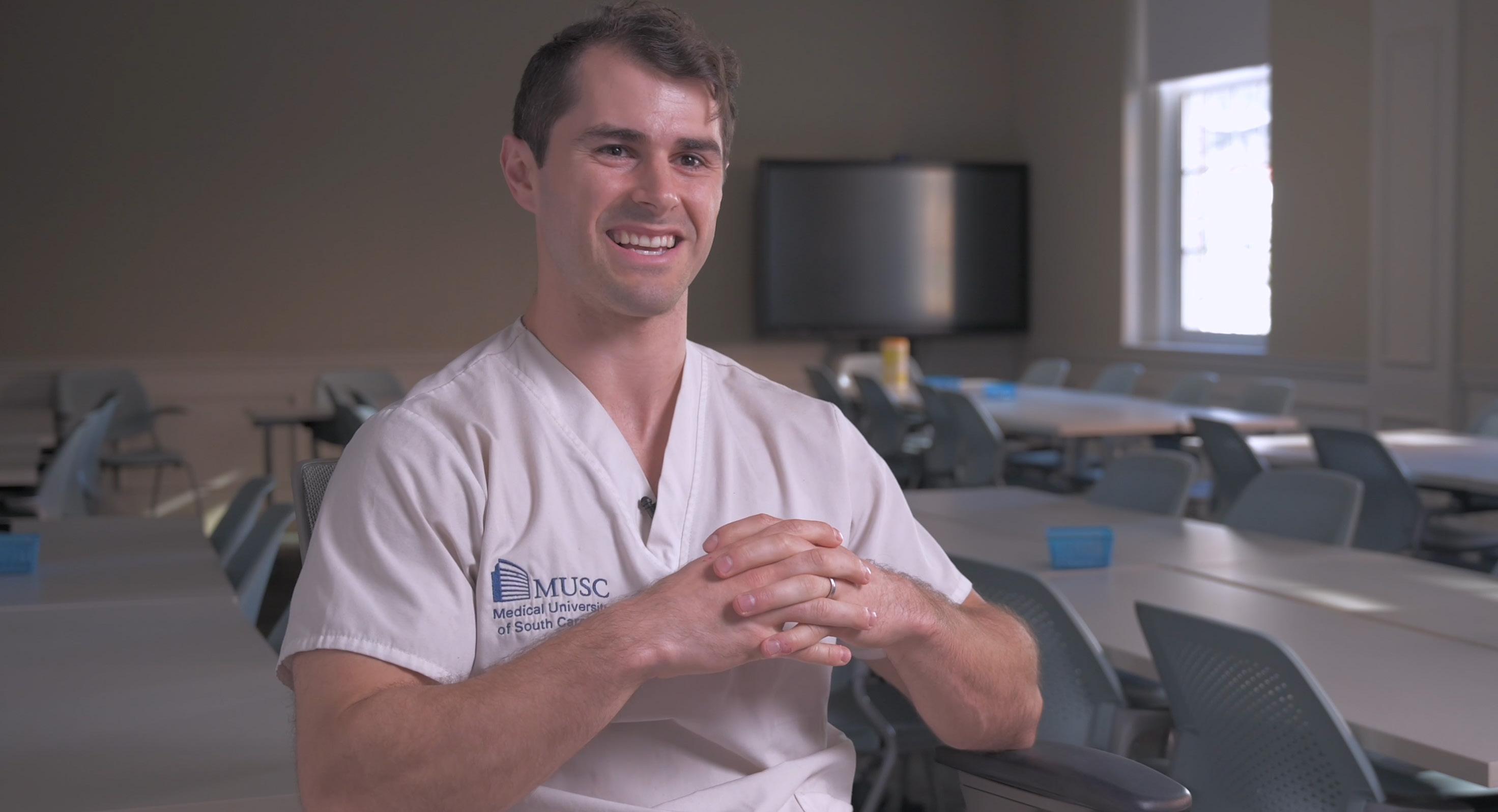 by Bryce Donovan, MUSC Catalyst News, Office of Public Affairs and Media Relations
by Bryce Donovan, MUSC Catalyst News, Office of Public Affairs and Media Relations
web.musc.edu/about/news-center
Thespreadsheets never stood a chance. It was 2021, and Zach Boden was up late, crunching numbers on corporate tax returns. “I just remember looking at the clock – it was, like, 3 a.m. – and I thought, ‘What am I doing with my life? I don’t want to do this anymore,’” Boden said. It was a feeling that had been slowly building for the financial analyst of more than five years, finally boiling over that early morning in the glow of his computer screen. Ironically, a few months later, while rescuing a woman – wearing no clothes and wielding a butter knife – from a tree, the 28-year-old with a master’s in business had a completely different feeling. He knew he was finally on the right track.
INSPIRATION
Photo by
36 MUSC COLLEGE OF NURSING
"What am I doing with my life?"
Road less traveled
In May, Zach Boden officially became a registered nurse when he graduated from MUSC’s College of Nursing. How he got there – his path, if you will – isn’t the same-old “I just always had a fascination for health care” journey. A career in medicine was never really on the Atlanta native’s radar
“To be honest, I never really knew what I wanted to do when I grew up,” he said. That wanderlust attitude, that lack of gravitation to any one particular subject or vocation, left him open to any and all possibilities. As a result, Boden seemed to go all-in on everything he did – from science to English to sports –on the off chance it ended up being his thing.
Eventually, football and baseball won out. It was the academic part – more specifically, the answer to the question: “What will I do for a living?” – that Boden still hadn’t figured out. Though he might not have had a clear direction on his occupational compass, Boden did well in school. So well, in fact, one of the places that offered him a scholarship was Harvard University.
“I want to be clear here,” he said with a selfdeprecating laugh. “I totally wouldn’t have gotten into Harvard if not for sports.” Sure, Harvard recruited him to play on its football and baseball teams, but his academic record was nothing to sneeze at. Couple
that with the kind of personality that makes others feel special – Boden has a way of clicking with people he’s just met, like he’s known them for years – that no doubt resonated with the prestigious Ivy League school.
Less than a year into his time at Harvard, things took a sad turn when his baseball coach had a heart attack and died during Boden’s freshman year. Two weeks later, the team’s running backs coach – the man most instrumental in recruiting Boden to Cambridge – took the head coaching job at Yale.

Understandably, Boden went through a few things. He started thinking. Reflecting. “I was just like, ‘I don’t know. I’m from Atlanta. Nothing is really keeping me up here besides athletics.’ So much had changed so quickly for me, you know? I just wanted to go. To leave,” he said.
And so, this time he rushed to a different end zone, 700 miles south to Duke University. It would be the first of several mature-beyond-his-years decisions Boden would make. And it would be that fearlessness to make big changes – the instinct to zag when others zig, to take the chance and the road less traveled –that would be one of his most defining traits in life.
Though he didn’t replicate his success on the football field in Durham, North Carolina (“We got our butts kicked every week – but at least it was on
 L-R: Boden and HomeGrown Lifting business partner, Will Whitman. Photo provided. Boden celebrates a big play for the Duke Blue Devils. Photo provided by Duke University Athletics.
L-R: Boden and HomeGrown Lifting business partner, Will Whitman. Photo provided. Boden celebrates a big play for the Duke Blue Devils. Photo provided by Duke University Athletics.
37 LIFELINES MAGAZINE
national TV, right?”), he did make lifelong friendships and even met his future wife, thanks to a spur-ofthe-moment weekend road trip to visit some pals at Davidson College.
Finding his own way
There came a point in time at Duke when Boden couldn’t hedge any longer. He needed to choose a path, to declare a major that would hopefully relate to his future career. With no real clear path in front of him, he opted for the logical choice: to follow in his father’s footsteps and join the family business – real estate finance.
“My old man really wanted me to do it, so I gave it a crack,” Boden said. Slight pause. “And it sucked.” In Boden’s defense, he came to that conclusion honestly, after five long years working in finance – even spending a year post-graduate earning his Master of Management Studies (MMS) from Duke’s Fuqua School of Business. He gave number crunching his all.
“I’m not trying to bang on finance,” he said. “You’ve got to find the balance between paying the bills and being happy. It did fine in the pay-the-bills department. It just didn’t make me happy enough.”
What it did do, though, was provide Boden with the seed money – and more importantly, the confidence – to start his own business with one of his former Harvard football teammates. In 2019, the two launched HomeGrown Lifting, a company that manufactures and sells fitness equipment. Thanks to COVID (said no one, ever) and a new wave of people looking to work out at home, not in a crowded gym, HomeGrown took off in a big way. That successful foray, coupled with a wild hair – his wife, Katy, a cardiothoracic nurse, whose sense of purpose not only inspired Zach but also piqued his interest in health care – led him to volunteer for the City of Goose Creek Fire Department as a firefighter/EMT.

It was during those weekend shifts – answering calls to help people who had overdosed, fallen off a ladder, gotten stuck in a tree naked – that a fire was
lit. (Ironically, he never once responded to an actual fire.) And his passion for patient care blossomed.
And so there he was, the human dichotomy: By week, he was MBA Zach, keeping things in the black; by weekend, he was volunteer firefighter/EMT Zach, keeping people on the ground (and in their clothes).
And he loved it.
More specifically, he loved the time he spent with patients. Helping them with their wounds. Riding with them to the Emergency Department. Sitting with them at the hospital.
So it was inevitable. In the summer of 2021, Boden was accepted into the MUSC College of Nursing’s Accelerated Bachelor of Science in Nursing (ABSN) program. During the 16 months that followed, he was named Student Government Association president, shadowed Katy for several weeks and even randomly got the call to be a bone marrow donor (he plans to meet the 5-year-old recipient this summer). In May, he began a new job –trading in his suit for scrubs – as he works as an R.N. for Roper Hospital in its ED.
“I’m really excited,” he said. “I’m gonna be raw, but man, am I excited to get up in the morning and do a job I’m passionate about.”
INSPIRATION
Scan the QR code or visit bit.ly/3WDfbBg to hear Boden share more about his experience as an Accelerated BSN student at MUSC College of Nursing.
38 MUSC COLLEGE OF NURSING
Boden and his wife Katy, a cardiothoracic nurse. Photo by Silver and Chalk Images.
IMPACT
“This year we had the honor of welcoming, conversing and learning from Dr. Phoenix Matthews for the 12th annual Janelle Othersen Visiting Professorship Lecture. Dr. Matthews, a professor in the Department of Population Health Nursing Science and Associate Dean for Equity and Inclusion at the University of Illinois, Chicago, presented a thought-provoking and idea-generating talk entitled, ‘It takes a village: Creating a safe and inclusive learning environment.’ Many in the college benefited from one-on-one and small group dialogues with Dr. Matthews during their visit to MUSC and the college. We look forward to future discussions on how we integrate many of the strategies outlined by Dr. Matthews to enhance a culture of belonging which more clearly delineates our college-wide commitment to focused strategic priorities for inclusivity, equity, diversity, and belonging.” —Dean Linda S.
 Weglicki
Photo by Josh Goodwin.
Weglicki
Photo by Josh Goodwin.
A CULTURE OF BELONGING 39 LIFELINES MAGAZINE
Diversity, Equity, Inclusion and Belonging Highlights
A respected leader in the field of advancing inclusivity and belonging, Dr. Rumay Alexander visited CON in the fall and again in early spring at the invitation of Dean Linda S.Weglicki to facilitate and engage staff and faculty in an open conversation focused on “Courageous Dialogues: Building Trust and Excellence through Inclusivity.”
vIn November, the Student Nurses' Association sponsored a Friendsgiving Cultural Feast to celebrate the season of gratitude with delicious foods inspired by the diverse cultures and customs of the CON community.

Launched in May, the inaugural MUSC College of Nursing Summer Scholars program offered nine undergraduate students an introduction to scholarly activities and research, with in-person and virtual sessions on professional development, foundations of research, and the structural and social determinants of health and health disparities.


IMPACT w
w
4 � MUSC COLLEGE OF NURSING
Photos by Josh Goodwin.
Empowering Global Health
patients
DNP student Tammy Halladay embarked on a medical mission trip in the Galápagos Islands in October to gain global health experience working with an under-served population. “Our small team of 39 miraculously helped 2,231 patients with their medical, dental and vision needs in our four-day clinic,” Halladay shared. “In addition to the support of the local church, we were invited by the mayor and his wife who also hosted our team and worked alongside the local government and community helpers. At the end of the week, the mayor and his wife personally gave each one of us a special gift and exchanged hugs as he emotionally thanked us for changing lives in the local community. It was beautiful to witness an area that suffered greatly from the pandemic overcome hardships as we all came together as a body of believers, the church, government and international humanitarian group. Mutual respect, a simple genuine smile and sharing God’s unconditional love goes a long way into edifying and empowering communities.”

Falk-Griffin Endowment funds helped support Halladay’s trip, which was the first MUSC College of Nursing in-person global health experience made possible by the funds.
 Halladay and her team helped 2,231
with their medical, dental and vision needs over the span of four days.
Halladay and her team helped 2,231
with their medical, dental and vision needs over the span of four days.
4 � LIFELINES MAGAZINE
H H
ADVOCACY FOR THE PROFESSION
by Linda S. Weglicki, Ph.D., R.N., Dean and Professor
As the Dean of the College of Nursing, I engage in many activities as the chief administrative, executive, and coordinating officer of the college. One of my most important responsibilities is advocacy for MUSC, our college, and nurses and the nursing profession. Advocacy, which comes from the Latin word advocatus, meaning “a pleader on one’s behalf” or “one called to aid,” is an umbrella term defined as an activity by an individual or group that aims to influence decisions within political, economic, and social institutions (MerriamWebster). To be an advocate is to publicly support, defend, promote, recommend, or plead a particular cause or policy—generally with great passion and voice.
Over the course of my career, and particularly as an academic dean, I have always believed that nothing is more important or powerful than informed people (nurses) coming together— declaring from a shared voice—to help inform policy that affects our practice, engagement, and position, and which ultimately affects the patients, families, and communities
we serve. As individual nurses, as professional organizations, as a collective, we have a responsibility to be aware, perhaps today more than ever before in our history, due to our current multifaceted challenges, current policies, laws and regulations, and the current political landscape that affect and impact the work that we do—in clinical practice, in education, in research, and in being integral members of interprofessional health care teams.
It’s hard to say how much time I spend in advocacy work for MUSC and the College of Nursing, for nursing in SC, with the State Board of Nursing in advancing our State Practice Act, and at the federal level. In addition to keeping our state and federal legislators and senators, along with staffers, informed through regular communications of issues important to nursing (practice, workforce, education, faculty workforce, research, and faculty and student scholarships, loans, and loan forgiveness), I provided testimony to the SC House Education Committee in response to a proposed bill that would have authorized SC technical colleges
to begin providing accelerated BSN degree completion. I co-led the SC initiative to request state funds to support efforts to counter the nursing and faculty workforce shortage (resulting in $10 million in FY23 state appropriated funding for the Nursing Initiative focused on faculty retention and growth). I work with our MUSC legislative liaisons to keep appraised of and advocate for topics important to nursing and visit and communicate with our legislative representatives and their staffers, in their offices in Columbia and in Washington, DC.
I also serve as one of 30 elected national ambassadors to the Friends of the National Institute of Nursing Research (FNINR). As an FNINR ambassador I focus on educating
IMPACT
4 � MUSC COLLEGE OF NURSING
H
Congressional leaders about the true impact of nursing science with the ultimate goal of increasing research funding that will lead to scientific breakthroughs, improve health outcomes, promote health equity, and impact our nation’s more pressing and persistent health challenges, as well as support the training of nurse scientists made possible by the NINR. As a FNINR ambassador, my visits to Capitol Hill each year are as an advocate on behalf of the state of South Carolina, providing Congressional leaders with information about health issues important in the state, and the pressing needs to increase research funding to address them. I encourage you to intentionally seek ways to increase your advocacy about policy topics and issues important to nursing, nursing education, research, practice, and the profession.
• Send messages to your federal legislators and senators to ask Congress to support academic nursing, advance higher education, pursue transformative research, develop a robust workforce, and advance sustainable models of care that lead to a healthier nation.
• Support Title VIII Nursing Workforce Development Programs (of the Public Health Services Act [42 U.S.C. 296 et seq.]) which addresses all aspects of the nursing workforce including education, practice, recruitment, and retention and was reauthorized during the
• Champion the American Nurses Association Enterprise 2023 –2025 Strategic Plan which focuses on “One Vision, One Mission” to elevate, evolve, and ensure the success of the 4.4 million American registered nurses and our profession.

A Final Note: Legislators are often skeptical about too much data and research because special interest groups have been known to skew numbers to serve their own agenda, so balance your advocacy efforts with authentic stories that highlight the impact of your cause. Told in straightforward language, such stories build connection and inspire others to share their message.
In March, Ph.D. student Danielle Edmonds, Dean Linda S. Weglicki, and DNP student Krista Coppola visited SC State Legislative Offices in Washington, DC and advocated to address the critical need to have bipartisan federal funding for key bills to support Title VIII, the National Institute of Nursing Research appropriations, the FAAN Act and student loans and scholarships. Opposite: Weglicki met with Governor Henry McMaster as part of her advocacy work for nursing in South Carolina.
COVID-19 pandemic in 2020.
43 LIFELINES MAGAZINE
Scholarship Announcements
Fall 2022- Spring 2023
Thank you for Being the Difference!
Our donors help ease the financial burden of our students so that they can attend nursing school without undue financial hardship. Scholarships also help us recruit and educate nurses at the doctoral level to offset the national shortage of nurse educators. To learn more about establishing a scholarship and being the difference in a nurse’s life, contact Lilia Correa, Director of Development, at 843-792-8421 and correal@musc.edu
Undergraduate
125th Anniversary Endowed Scholarship
Jenna Wilson
Caroline W. Davis RN Scholarship
Virginia Britt
Christina Burnley
Jessica Claborn
Reedy DeRienzo
Emily Kozma
Elizabeth Mathis
Edna Zheng
Dorothy Johnson Crews Endowed Scholarship
Hannah Caudill
Anna Layman
Abigail Smith
Kenadee Tanney-Cadieux
Gretchen Wanning
Dr. Heidar A. Modaresi Nursing Scholarship
Olivia Forrest
Dr. J.W. Thurmond Endowed Scholarship
Ericka Prokop-Gryson
Edith Dority Lucas ’58 Endowed Scholarship
Madison Hodges
Exchange Club of Charleston Award (Nursing)

Shelby Turner
Jenna Wilson
Graduate Incentive Award-Nursing
Myoshia Baskin
Danielle Edwards
Helene Fuld Health Trust Endowment
Lorelei Dimmel
Caroline Durham
Mary Heustess
Carina Marotto
Henry T. Finch Jr. Nursing Scholarship
Jordan Eaddy
Jean P. Wilson College of Nursing Endowed Scholarship
Alexis Carter
Morgan Downing
Hannah McCarter
Olivia Phillips
Caitlyn Reilly
Vaida Shelley
Jill and Richard Almeida Nursing Endowed Scholarship
Olivia Forrest
Joan K. Rigter Nursing Scholarship
Sarah Blakely
Joseph H. and Terese T. Williams Endowed Nursing Scholarship
Kendall Hormel
Vanessa Varbanova
Julie & Anthony Lanzone Scholarship
Makayla Hartley
Lettie Pate Whitehead Foundation Scholarship
Kara Allen
Hale Alston
Kayla Baus
Rachel Casteel
Hannah Caudill
Oakley Cole
Emily Cope
Casey Dickson
Morgan Downing
Isabel Edwards
Caitlin Fields
Megan Glennon
Ashley Hoffman
Noa Hubara
Myra Ingraham
Johari Johnson
Elizabeth Jourdain
Madison Jrolf
Kelly Kesterson
Anna Layman
Anna Lee
Malashia Nesbitt
Zakiya Overton
Olivia Phillips
Laarni Sanders
Mekenzie Scardo
Ryan Weatherford
Kaylee West
Edna Zheng
Margaret Ann Kerr Endowed Scholarship
Megan Henson
Marianna Stuart Mason Endowed
Memorial Scholarship
Alexandra Marshall
L-R: PH.D. student Kesia Levesque, the recipient of the Marianne T. Chitty Memorial Scholarship, & Dr. Kay Chitty.
IMPACT
44 MUSC COLLEGE OF NURSING
Photos by Josh Goodwin.
Marie LePrince Farmer Nursing Scholarship
Kourtney Dobmeier
Johari Johnson
Kendall Silvers
Martha Halliday Wrobleski Memorial Scholarship
Jenny Nankoua
Marvin and Cleo T. McAlhany CON Endowed Scholarship
Caitlyn Reilly
MUSC College of Nursing Board Scholarship

Bianca Garsys
MUSC Provost Scholarship
Ezinne Agim
Sierra Ancrum
Rachel Casteel
Malia Davis
Darien Dean
Christopher Dunn
Isabel Edwards
Alexis Gontz
Brianna Hildret
Malashia Nesbitt
Amy Tamblyn
Morgan Washington
Olivette Garr Smith Scholarship
Ashleigh Baker
Lucas Hess
Patrick and Maureen Marr Endowed Scholarship
Kala Steward
Reba Carter O’Keeffe
Endowed Scholarship
Danielle Edwards
Ariel Sullivan
Roper St. Francis Healthcare Patron Nursing Scholarship
Brionna Bright
Christian Chassereau
Rose and Ted Levin Nursing Scholarship
Danielle Mashburn
Ruth Chamberlin Scholarship
Courtney Hughes
Samuel Steinberg Endowed Scholarship
Brianna Hildreth
Sandra Hayes Poulnot Nursing Scholarship
Lucy Downs
Kendall Silvers
For Mekenzie Scardo, a scholarship to attend the ABSN program made it possible to expand her horizons while working as an aeromedical evacuation technician in the Air Force Reserves: “It has been a difficult path at times, but I am truly humbled, knowing that the hard work and dedication through the years are validated by your confidence in my abilities to award me a scholarship. You have not only provided me with financial relief but also motivated me to continue on this journey.”

Profile photos provided.
Ted and Joan Halkyard Nursing Endowed Scholarship
Myra Ingraham
Renata Menezes
Thomas J. Wiscarz Memorial Nursing Endowed Scholarship
Christian Chassereau
Rendol Williams
The Provost’s Scholars join Dean Linda S. Weglicki during the Dean’s Annual Scholarship Reception.
45 LIFELINES MAGAZINE
Vanette Schultz Forbes ‘47 Nursing Scholarship
Alexis Gontz
Virginia Lawton Harper Scholarship Fund
Courtney Hughes
Women Inspired Through Stories
Shelby Baker
Graduate
125th Anniversary Endowed Scholarship
Tiffany Connor
135th Anniversary Scholarship
Imani Sumpter
1883 College of Nursing Scholarship
Mary Prybylo
Megan Wayne
Andell Endowed Scholarship
Bethany Ghent
Madison Morris
Annie K. Norton Endowed Scholarship
Hannah Boyd
Barbara Sutton Pace

Endowed Nursing Scholarship
Marie Vestal
Betty C. Kelchner Endowed Scholarship
April Ratley
Betty Murray Brundage
Kinard Endowed Scholarship
Abby Kent
Captain Robert Wilkens Palliative Care Scholarship
Polly Boynton
Jacquelyn Robins
Charleston County Medical Society Alliance

Shenae Long
CVS Health Foundation Scholarship
Kiara Baylock
Hannah Boyd
Johntoria Dargan
Sabrina Dingle
Tammy Halladay
Dorothy Johnson Crews Endowed Scholarship
Emily Askew
Dr. Deborah C. Williamson Nursing Scholarship
Rikayla Boone
Dr. James B. Edwards Nursing Scholarship
Emily Stump
Dr. Sekou Dakarai Nursing Scholarship
Maggie Long
Elsie Morgan Endowed Nursing Scholarship
Onyiyechi Ajukwa
Susan McCabe
Lindsay Pugh
Gail W. Stuart Endowed Scholarship
Jonah Burrell
Jean P. Wilson College of Nursing Endowed Scholarship
Matthew Reeves
Kelley Westbrook
For Ph.D. student Angela Lentini-Rivera, R.N., MA, CPNP, a scholarship has made possible her lifelong goal to obtain a Ph.D. and help childhood cancer survivors: “I have worked at Memorial Sloan Kettering Cancer Center for 25 years, and supporting parents and caring for children with cancer have been my life’s passion. After completing my Ph.D. in Nursing Science, I aim to bridge the gaps in care that young childhood cancer survivors experience. I look forward to the day when I can pay this gift forward to another student!”
Izant Family Foundation Scholarship
Shenae Long
Lettie Pate Whitehead Foundation Scholarship
Lakara Alston
Tamra Atkins
Rikayla Boone
L-R: ABSN student Jordan Eaddy, the recipient of the Henry T. Finch, Jr. Nursing Scholarship, & Dr. Nancy Finch.
46 MUSC COLLEGE OF NURSING
IMPACT
Katherine Chike-Harris
Johntoria Dargan
Danielle Edmonds
Krysta Falls
Georgia Garrett
Bethany Ghent
Heather Kellis
Lillian Kendinger
Mary MacGregor
Essence McClary
Stephanie Neary
Kylie Newsom
Doris Owusu Amoah
Tonya Palmer
Ji Hyun Ru
Meera Shah
Cecilia Tallo
Haley Wren
Marianne T. Chitty Endowed Nursing Scholarship
Kesha Levesque
Mary Swain Endowment
Ifeoma Onyeike
Beth Williams
Mason Scholars
Angela Lentini-Rivera
Maude Callen Endowed Memorial Scholarship
Essence McClary
MUSC Provost Scholarship
Meghan Ames
Tamra Atkins
Dave Balbarada
Hannah Brown
Katherine Chike-Harris
Suzanne Hakeos
Heather Kellis
Tonya Palmer
KellyAnn Reese
Theresa Skojec
Denise Smalls
Rachel Torlay
Courtney Wages
Taylor Wait
Bianca Wallace
L-R: CON Development Board Chair

Patrick Marr & ABSN student Kala Steward, recipient of the Patrick & Maureen Marr Endowed Scholarship.

Nina Smith Nursing Scholarship
Lakara Alston
Katherine Chike-Harris
Alyssa Davis
Ashley Efremov
Elizabeth Kelly
Olympia “Bia” Vallis Nursing Scholarship
Shannon D’Alton
Yulia Lopez
Ruth P. and Stephen Stewart Endowed Scholarship
Jennifer Huggins
Sara Piechnik Endowed Scholarship
Stacy Harris
Ursula Caton Endowed Memorial Scholarship
Tammy Halladay
L-R: Dr. Cathy Durham, DNP student

Jonah Burrell, recipient of the Gail W. Stuart Endowed Scholarship, & Ray Burrell.
A scholarship has opened the door to ABSN student Shelby Baker’s ultimate goal: serving those most in need. “The didactic and clinical education at the institution is unmatched, and I am excited to put what I have learned into practice. My ultimate goal is to become a certified registered nurse anesthetist that practices anesthesia in a rural or underserved community. I would like to bridge some of the healthcare gaps experienced by those who live in underserved areas.”
47 LIFELINES MAGAZINE
OPENING DOORS
by Melissa Varner Public Information Director Institutional Advancement
Laarni Sanders wakes up by 4:30 a.m. during the school week. She gets herself ready and then starts making and packing lunches for her three children. “That way it’s less chaos for my husband when he drops them off,” she explains. She’s out the door by 5:30 a.m., headed north from her home in Beaufort, South Carolina, to the MUSC College of Nursing in downtown Charleston. Laarni is a student in the college’s Accelerated Bachelor of Science in Nursing (ABSN) program. It’s a fast-track option for students like Laarni, who already have 60 or more hours of college credit. Through the ABSN program, she will earn a bachelor’s degree in nursing in 16 months instead of the traditional four years.
Classes are held on-campus, so Laarni makes the two-hour commute twice a day, Monday through Thursday. “Four hours on the road is very hard,” Laarni said. “I try to do as much work as I can on campus. On my way home, I’m usually listening to recordings from lectures to use my time wisely.” When she gets home, she’s still on the go, picking her children up from sports or honor society and then juggling dinner duties with her husband, Shedrick.
Shedrick is in school for biblical studies, Laarni says. “I’m so thankful for him because he also works two to three jobs so I could stop working and go to school. And so, when I saw that I received the Lettie Pate Whitehead scholarship, it was such a huge blessing and lifted a financial burden off us.”
The Lettie Pate Whitehead scholarship supports female students with financial need in nine Southeastern states. Laarni is one of 49 MUSC nursing students who received a Lettie Pate Whitehead scholarship for the 2022-23 school year. Over the past 30-plus years, the foundation has given more than $3.4 million in scholarship funding to the MUSC College of Nursing.
Laarni has also benefited from the SEED program, which is supported by the Duke Endowment. SEED stands for Supporting Educational Excellence and Diversity for South Carolina Nursing. The program helps train diverse students to fill an urgent need for skilled nurses in South Carolina’s rural and medically underserved communities.
Laarni, a Filipino American, developed a heart for service at a young age. “My dad was military, so I moved around my
whole life,” she explained. “Being exposed to other cultures really helped me understand what people receive or how different it is, even in different parts of the United States. That inspired me to pursue a field in health care.”
Laarni started her career as a medical assistant, eventually transitioning into administrative work. But she knew it wasn’t what she was meant to be doing. At nearly 40, Laarni decided to go back to school. “I decided to just trust in what God had planned,” she said. “I applied to MUSC, and seeing all the doors open through donors and scholarships just solidified the path I’m supposed to go on.”
Laarni has a year to go until graduation – another year of four-hour commutes at least four times a week. And although it’s hard now, she knows it’s only temporary. “I’m passionate about this. I know the end result will be worth it.”
She and Shedrick are also proud of the example they’re setting for their three children: 14-year-old Syleia, 11-yearold Shraja and 9-year-old Shedaveon. “I always tell my kids, ‘Whenever people help you, you do what you can. And when you’re able to step on your own two feet, you pay it forward.’ I am looking forward to the day where I’ve graduated and stable and we can give generously as well … I think that’s very important. It shows that, ‘Hey, I’m not just here to receive I want to give back.’”
Until then, she remains grateful to the donors who have made this path possible. “Thank you for being a part of this journey,” Laarni said. “By giving, you’re not just making a difference in my life, but the lives of all the patients I’ll help in the future.”
“MUSC College of Nursing, along with all of our students who have been fortunate to receive a Lettie Pate Whitehead Foundation scholarship, are so appreciative of the years of support. These scholarships make a significant difference to our students as they pursue their goals and dreams of becoming a nurse.”
 –Linda S. Weglicki, Ph.D., R.N., Dean of the MUSC College of Nursing
–Linda S. Weglicki, Ph.D., R.N., Dean of the MUSC College of Nursing
IMPACT
Sanders after her Stethoscope and White Coat Ceremony last fall.
48 MUSC COLLEGE OF NURSING
Student Philanthropy & Community Engagement




MUSC College of Nursing students are passionate about shining a light on the needs of the surrounding community and then stepping up to help fulfill them. Often led by the college’s Student Government Association and Student Nurses’ Association, these initiatives benefit everyone from children to seniors and foster both leadership and compassionate care. Here are just a few of the efforts that students supported this past year: Backpack Buddies, Be the Match, CARES Pediatric Prevention Clinic, Charleston Hispanic Association, Envision MUSC, Father to Father, James Island High School Health Science Program, Lowcountry Orphan Relief, One80 Place, Partners in Healthcare/East Cooper Community Outreach, Shawn Jenkins Children’s Hospital, SC Department on Aging, and Wings for Kids.

49 LIFELINES MAGAZINE
Photos by Josh Goodwin, Jennifer A. Turner and provided.
Innovation in Action: Endowed Faculty Chairs in Nursing
By Lilia Correa, Director of Development
L-R: Dr. Kathleen Lindell, Mary Swain, Dr. Linda S. Weglicki, and Lilia Correa during November’s MUSC Palliative Care Showcase: All that is PC at MUSC and Beyond Dr. Lindell is the Mary Swain Endowed Chair in Palliative Care Health.

IMPACT
5 �
Photo by Josh Goodwin.
MUSC COLLEGE OF NURSING
An endowed faculty chair in nursing is a prestigious position that is typically awarded to a distinguished nursing scholar or researcher who has made significant contributions to his or her field. The position is usually funded through an endowment, which provides financial support for the holder of the chair’s research and teaching activities.
WHY ARE ENDOWED FACULTY CHAIRS IMPORTANT?
The importance of an endowed faculty chair in nursing lies in an institution’s ability to attract and retain top talent in the field of nursing. The position provides a platform to conduct cutting-edge research, develop innovative teaching strategies and engage in community outreach activities that can have a significant impact on the nursing profession and health care in general.
An endowed faculty chair in nursing can also serve as a catalyst for collaboration and interdisciplinary research, as the holder of the chair can bring together scholars and practitioners from different fields to work on complex health care issues. The holder can also help to elevate the status of the institution and increase public awareness of the critical role that nurses play in promoting health and wellness.
Overall, an endowed faculty chair in nursing is an important investment in the future of the nursing profession, as it helps to ensure that nursing research and education remain at the forefront of health care innovation and excellence.
WHAT IS THE PROCESS OF CREATING AN ENDOWED FACULTY CHAIR?
When an individual or organization donates to a university, they may specify that the funds be used to create an endowed faculty chair. This allows the university to attract and retain highly accomplished scholars, researchers or educators in a particular field of study by providing a competitive salary and other resources to support their work. Typically, endowed faculty chairs are named after the donor or another individual or organization who is being honored.
The terms of each endowed faculty chair may vary, but they generally provide a stable source of funding for the position and allow the university to support important academic work in perpetuity. Endowed faculty chairs are highly regarded in academia, and such a position can enhance the
reputation and prestige of the university and the individual who holds the chair.
WHAT INSPIRES DONORS TO CREATE AN ENDOWED FACULTY CHAIR?
One excellent example is Mary Watcher Swain, an alumna from the Class of 1980, and her husband David, who created the Mary Watcher Swain Endowed Chair in Nursing in 2016. “David and I are convinced that nurses, who are often the ‘voice’ of needy patients, must continue to lead the charge to improve clinical outcomes and enhance quality of care. This can only be accomplished as the best minds and most compassionate health care providers closely work together to develop and implement creative and innovative solutions. We have seen firsthand how our own parents have benefitted directly as a result of these innovations as they have dealt with various health challenges in recent years.”
INNOVATION AND EXCELLENCE ARE POSSIBLE WITH YOUR SUPPORT.
Endowing faculty chairs can enhance the nursing profession and make a lasting impact by naming them after you, your loved ones, friends, colleagues or a favorite professor. The MUSC Foundation permanently invests the endowment to ensure the funds are paid in perpetuity, and a portion of the earnings is allocated to the endowed faculty chair position at the College of Nursing. An endowed faculty chair can be created by pledging $1,000,000 over a five-year period, with gift payments made over time.
Want to learn more? Please call (843) 792-8421 or email correal@musc.edu
MUSC COLLEGE OF NURSING ENDOWED CHAIRS
Ann Darlington Edwards Endowed Chair in Nursing
David & Margaret Clare Endowed Chair: Dr. Teresa Kelechi
Mary Swain Endowed Chair in Palliative Care: Dr. Kathleen Lindell
SmartState Endowed Chair of the Technology Applications Center for Healthful Lifestyles
(TACHL): Dr. Ken Ruggiero
5 � LIFELINES MAGAZINE
College of Nursing Development Board

2022-2023







The board is committed to raising the margin of excellence of the MUSC College of Nursing and is uniquely positioned to make a significant impact on the future of nursing and health care. Board members support and advance the work of the college through advocacy, education, philanthropy, community engagement and fundraising. Thank you to our board members for their service!

 Patrick Marr Board Chair WSR Realty
Nancy Finch Community Volunteer
Wade Boals Saltwater Cowboys
Bob Mason Community Volunteer
Cas Danielowski Millenia Medical Staffing
Frank Pugliese Principal Financial
Connor Danielowski Chronic Care Staffing
Victor Rivera Bank of America
Catie Meehan Steinberg Law Firm Rinne Sade Community Volunteer
Patrick Marr Board Chair WSR Realty
Nancy Finch Community Volunteer
Wade Boals Saltwater Cowboys
Bob Mason Community Volunteer
Cas Danielowski Millenia Medical Staffing
Frank Pugliese Principal Financial
Connor Danielowski Chronic Care Staffing
Victor Rivera Bank of America
Catie Meehan Steinberg Law Firm Rinne Sade Community Volunteer
IMPACT 5 � MUSC COLLEGE OF NURSING
RIPPLE EFFECT
By Jennifer A. Turner Director of Communications and Marketing
CON alumnus Sekou Dakarai, DNP, PMHNP-BC, Class of 2015, recently shared what inspires his passion for the psychiatric mental health nurse practitioner field and why he’s committed to paying it forward.

What inspired you to pursue nursing? What led you to MUSC?
I was inspired to pursue nursing based on two reasons: my love for helping others and the flexibility and stability that the nursing field provides. What led me to MUSC was the fact that I am originally from Charleston and was actually born at MUSC 40 years ago. So it seemed symbolic in a way that I would be able to be educated and groomed to be a professional in the place where it all literally began for me.
What do you value most about your experience at the College of Nursing? How did it prepare you for your specialty area of nursing practice?
What I valued most about my experience at MUSC was the relationship that I established with former professors who are now my peers. The professors at the CON were always approachable and never made me feel intimidated. With regards to how the CON prepared me for my specialty area of nursing, I would say that having excellent faculty with decades of clinical experience along with the breadth of the program’s clinical exposure prepared me well. The professors in the CON were also very encouraging and offered sound career advice as I prepared to transition into the workforce as a mental health provider.
As a DNP, what do you love most about your work?
The thing I love most about my work is being able to make a positive impact in the lives of those who are struggling with their mental health as well as the ability to manage my own patients. What inspired you to create a scholarship for CON DNP students interested in a career in the area of psychiatry/mental health? What impact would you like to see?

I was inspired to create a scholarship for CON DNP
students interested in Psych MH largely because of the stigma associated with mental health, especially in minorities. Growing up, I watched countless family members struggle silently with mental health concerns for a variety of reasons. Some of it was pride, some of it was based on cultural belief that you should be strong enough to handle it on your own, partly because of a lack of trust for medical professionals. The ultimate impact that I hope this scholarship brings is to increase the number of minority mental health providers which ultimately leads to increased trust and more minorities seeking help for mental health problems.
As a recent alumnus, why do you believe it is important to give back to CON and support the next generation of nursing students?
MUSC is the community that gave me an opportunity to pursue my dream. Their faith in me has afforded me the opportunity to help people who are struggling with their mental health. It is my hope that by giving back, the psychiatric mental health nurse practitioner (PMHNP) field will continue to grow which will increase access to mental health providers for those who need it.
Fun fact about you: I enjoy acting. Actually, I hold a BA in theatre and have worked as a stand-in for a professional actor in a motion picture film and have also appeared as an extra in multiple films.
53 LIFELINES MAGAZINE
To our incredible students: We are so proud of your commitment to the nursing profession and your impact as the next generation of nurse leaders. We are honored to be part of your journey!





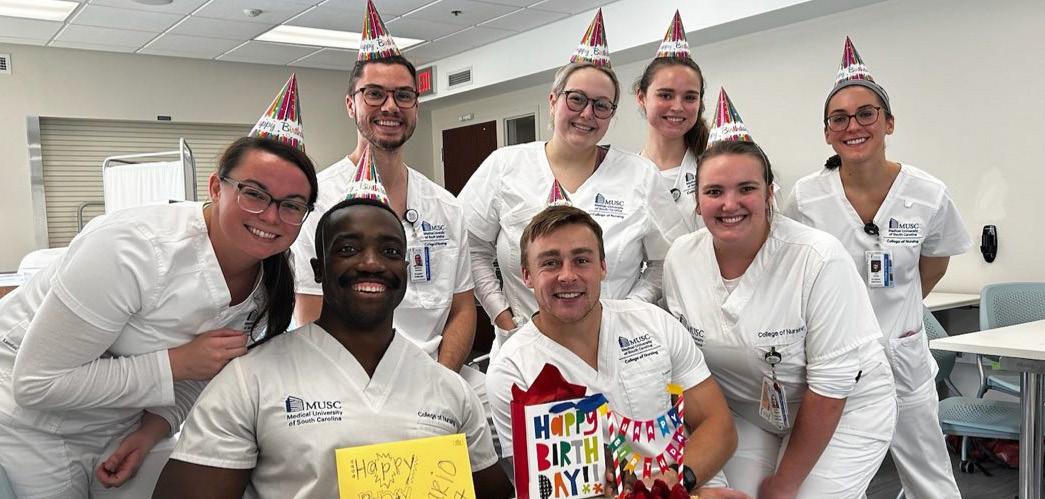
 Photos provided and by Josh Goodwin.
Photos provided and by Josh Goodwin.









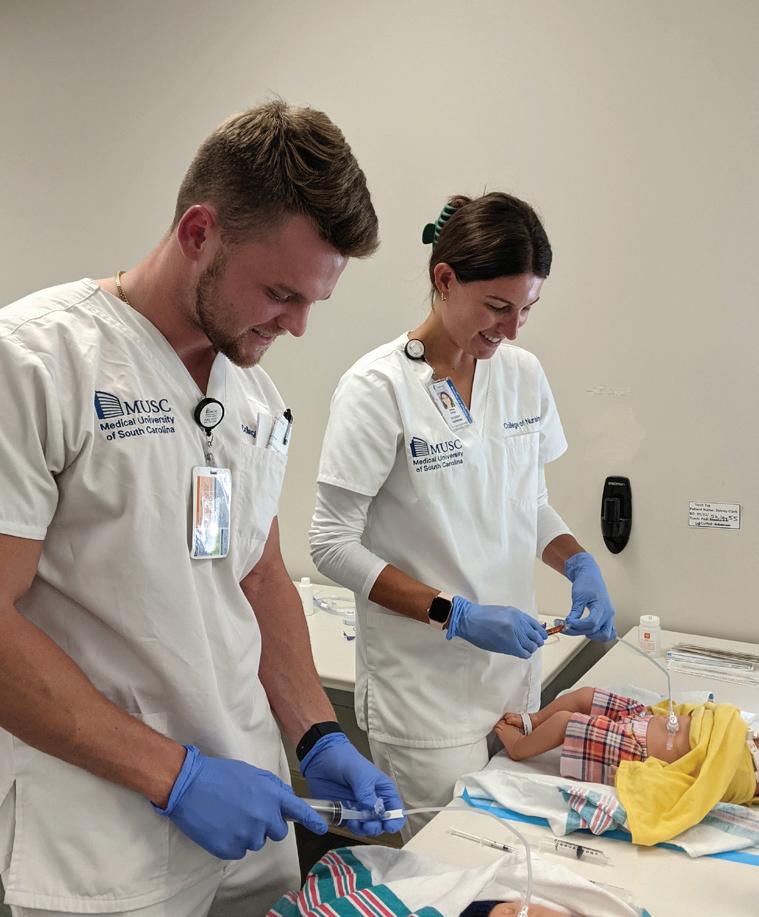


#CONSTRONG

Non-Profit US Postage PAID Permit # ��� Charleston, SC
99 Jonathan Lucas Street MSC 160 Charleston, SC 29425-1600










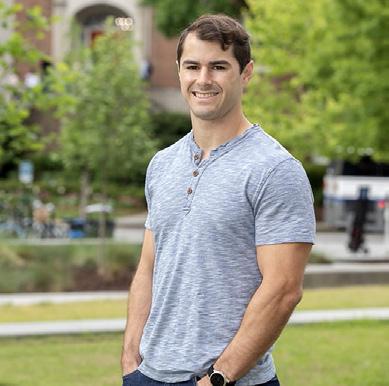





 Special moments from the College of Nursing 2022-2023 Convocation and Pinning ceremonies.
Special moments from the College of Nursing 2022-2023 Convocation and Pinning ceremonies.











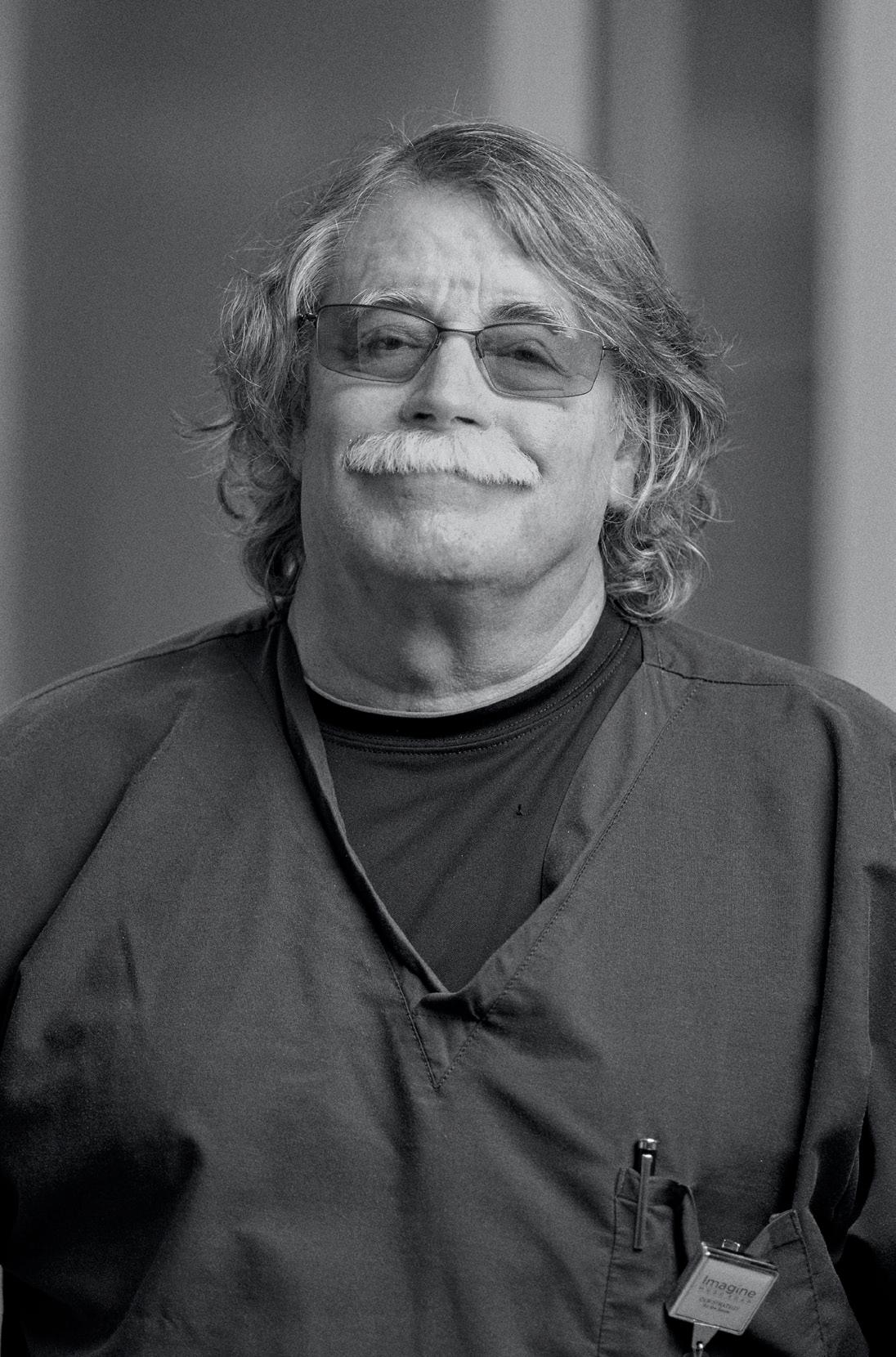
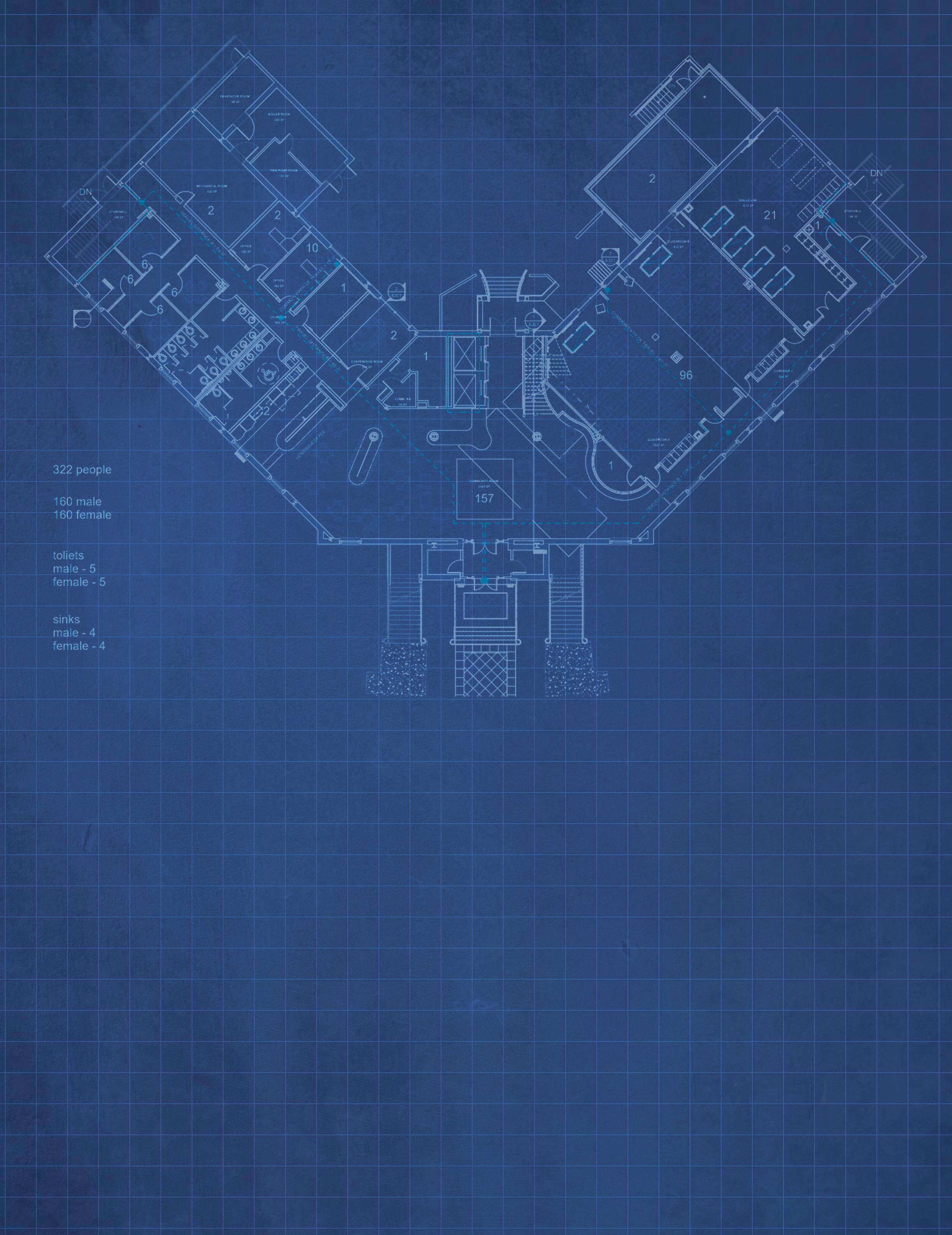 by Linda S. Weglicki, Ph.D., R.N., Dean and Professor
by Linda S. Weglicki, Ph.D., R.N., Dean and Professor
 From left: Jennifer Ciccone, Dr. Kristen Poston, and Alexis Williams work together to steer CON’s simulation education.
From left: Jennifer Ciccone, Dr. Kristen Poston, and Alexis Williams work together to steer CON’s simulation education.

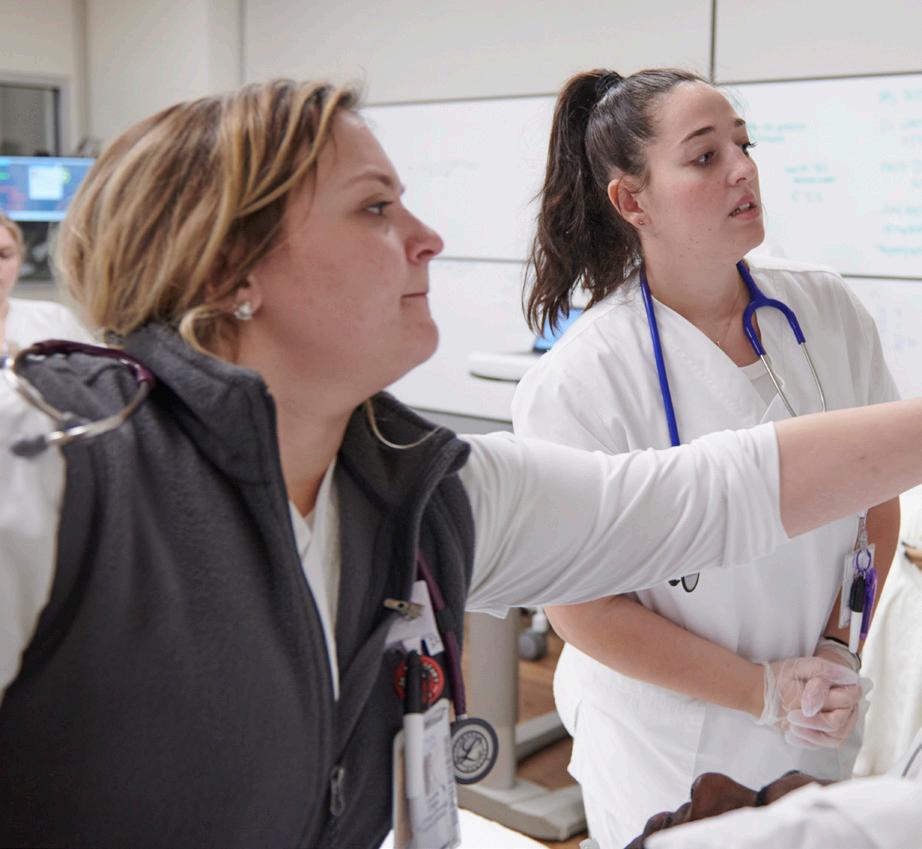

 , Simulation Assistant
, Simulation Assistant










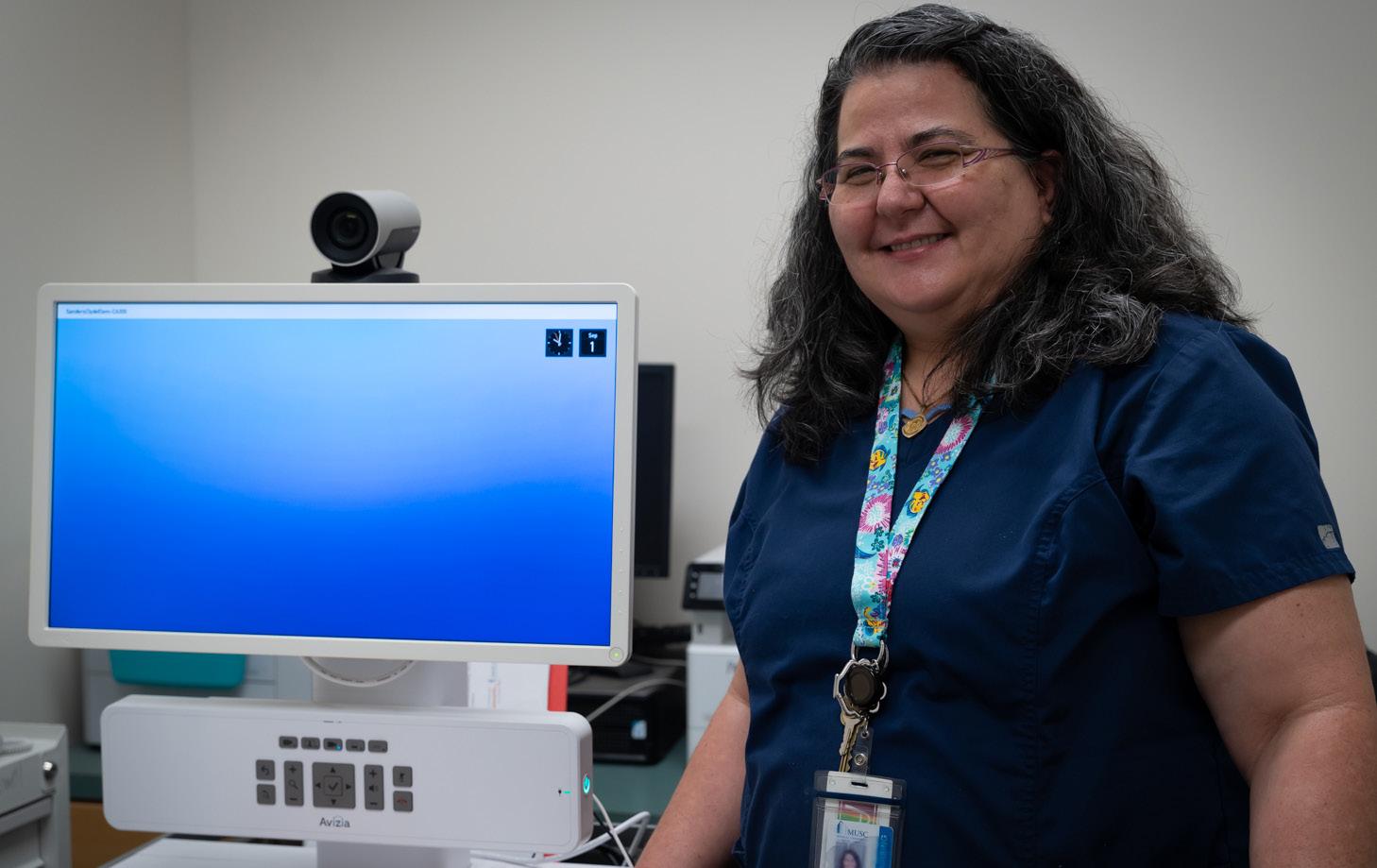



 Dr. Katherine Chike-Harris.
Dr. Katherine Chike-Harris.

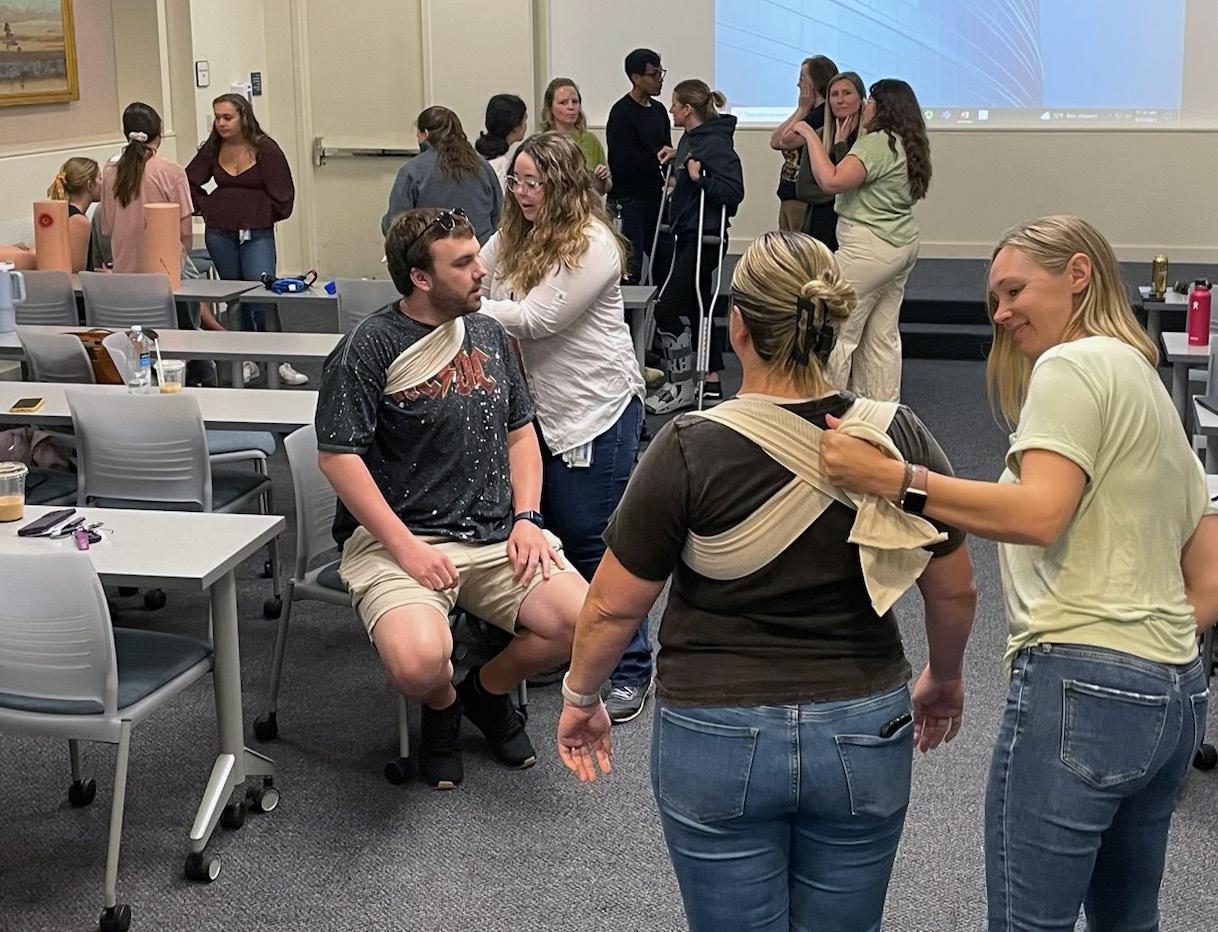
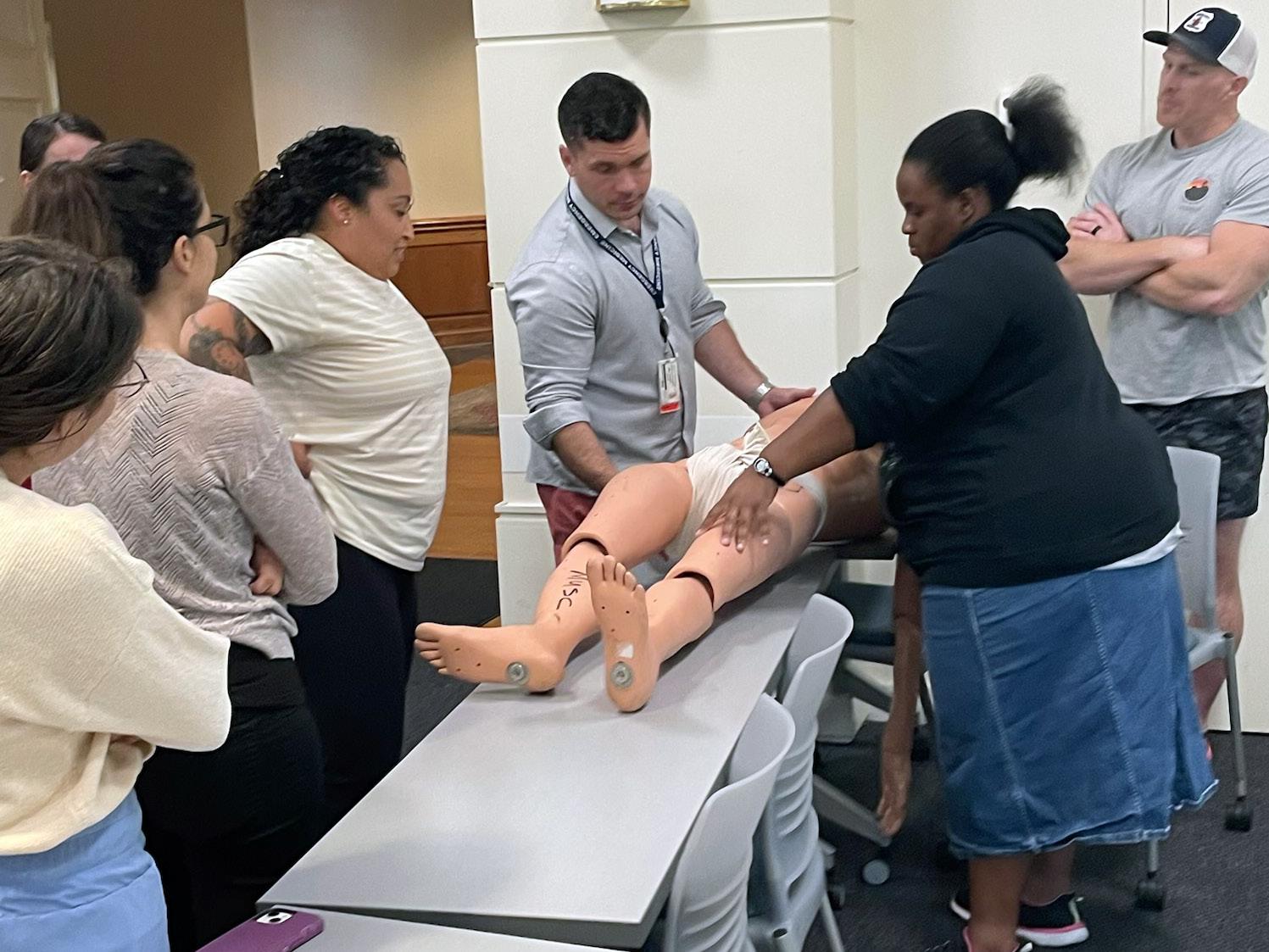








 Dr. Elizabeth Bear
Dr. Carolyn Jenkins
Dr. Joy Lauerer
Dr. Martha Sylvia
Dr. Janelle Wagner
Dr. Carrie Cormack
Dr. Teresa Kelechi
Dr. Leigh Ridings
Dr. Elizabeth Bear
Dr. Carolyn Jenkins
Dr. Joy Lauerer
Dr. Martha Sylvia
Dr. Janelle Wagner
Dr. Carrie Cormack
Dr. Teresa Kelechi
Dr. Leigh Ridings




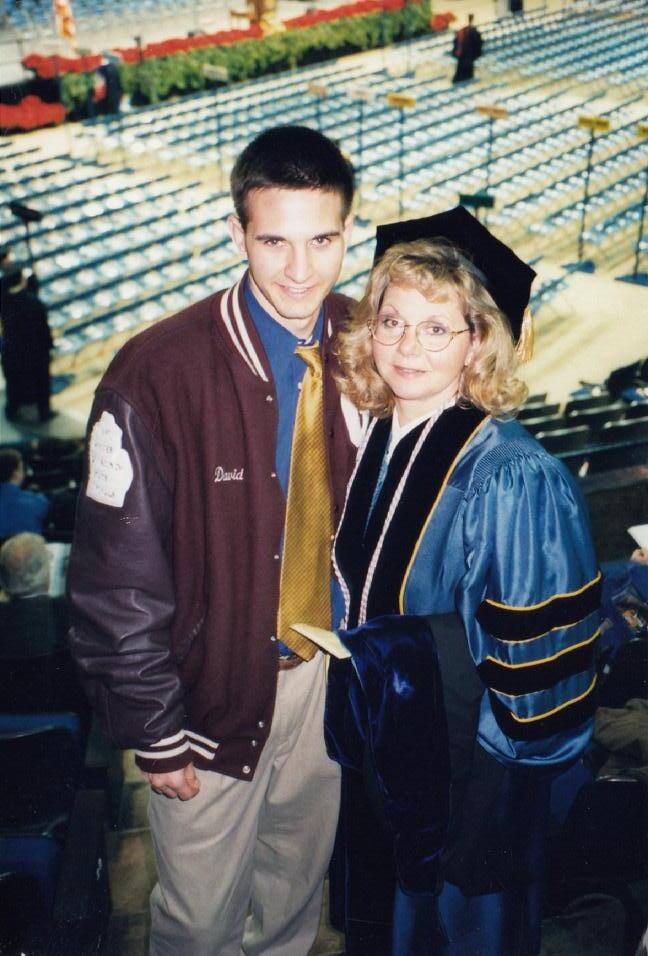
 Weglicki with MUSC ABSN nursing students.
Weglicki with MUSC ABSN nursing students.








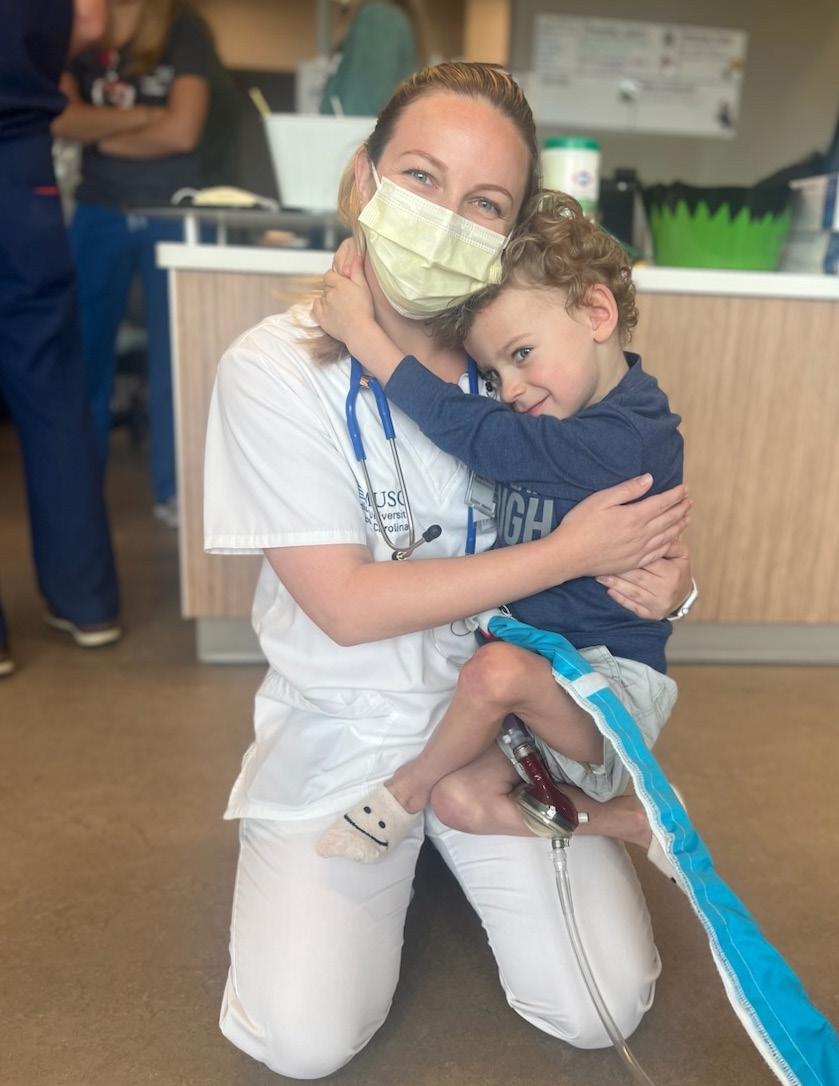 by Harrison Huntley, MUSC Catalyst News Office of Public Affairs and Media Relations
by Harrison Huntley, MUSC Catalyst News Office of Public Affairs and Media Relations



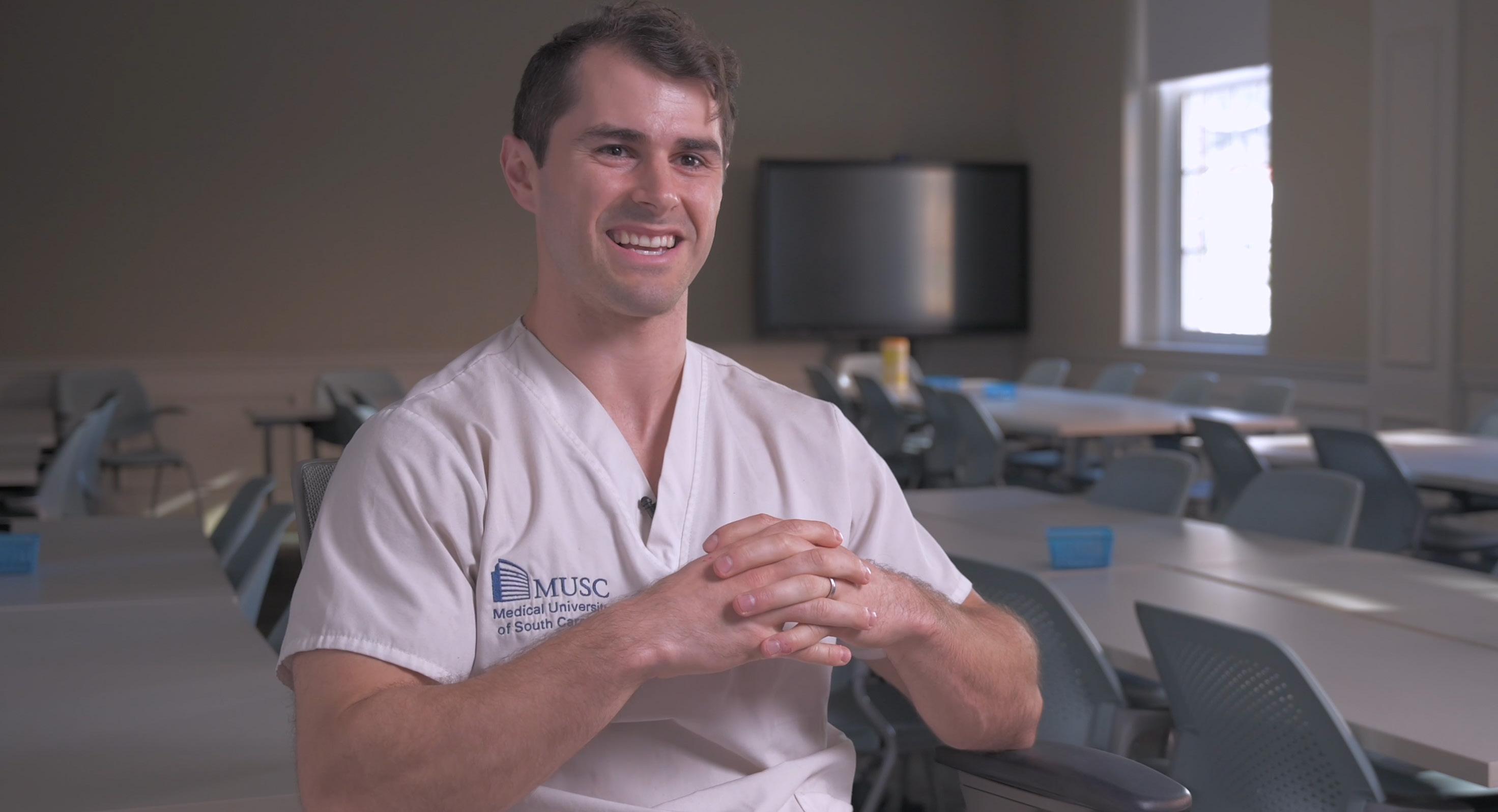 by Bryce Donovan, MUSC Catalyst News, Office of Public Affairs and Media Relations
by Bryce Donovan, MUSC Catalyst News, Office of Public Affairs and Media Relations

 L-R: Boden and HomeGrown Lifting business partner, Will Whitman. Photo provided. Boden celebrates a big play for the Duke Blue Devils. Photo provided by Duke University Athletics.
L-R: Boden and HomeGrown Lifting business partner, Will Whitman. Photo provided. Boden celebrates a big play for the Duke Blue Devils. Photo provided by Duke University Athletics.

 Weglicki
Photo by Josh Goodwin.
Weglicki
Photo by Josh Goodwin.




 Halladay and her team helped 2,231
with their medical, dental and vision needs over the span of four days.
Halladay and her team helped 2,231
with their medical, dental and vision needs over the span of four days.
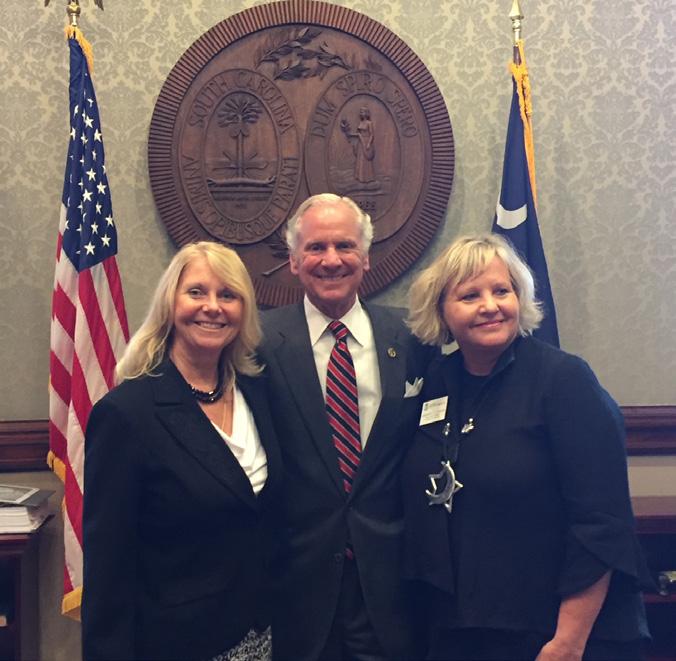









 –Linda S. Weglicki, Ph.D., R.N., Dean of the MUSC College of Nursing
–Linda S. Weglicki, Ph.D., R.N., Dean of the MUSC College of Nursing















 Patrick Marr Board Chair WSR Realty
Nancy Finch Community Volunteer
Wade Boals Saltwater Cowboys
Bob Mason Community Volunteer
Cas Danielowski Millenia Medical Staffing
Frank Pugliese Principal Financial
Connor Danielowski Chronic Care Staffing
Victor Rivera Bank of America
Catie Meehan Steinberg Law Firm Rinne Sade Community Volunteer
Patrick Marr Board Chair WSR Realty
Nancy Finch Community Volunteer
Wade Boals Saltwater Cowboys
Bob Mason Community Volunteer
Cas Danielowski Millenia Medical Staffing
Frank Pugliese Principal Financial
Connor Danielowski Chronic Care Staffing
Victor Rivera Bank of America
Catie Meehan Steinberg Law Firm Rinne Sade Community Volunteer







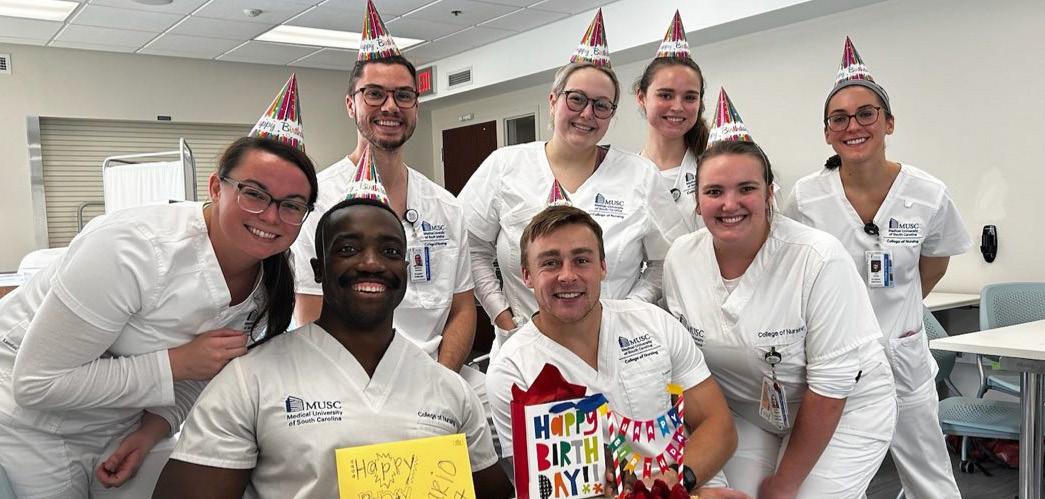
 Photos provided and by Josh Goodwin.
Photos provided and by Josh Goodwin.