10 minute read
Adolescent and Adult Chlamydial Infections
Adolescent and Adult Chlamydial Infections and the Role of Pharmacists
By: Briana Williams, PharmD Candidate
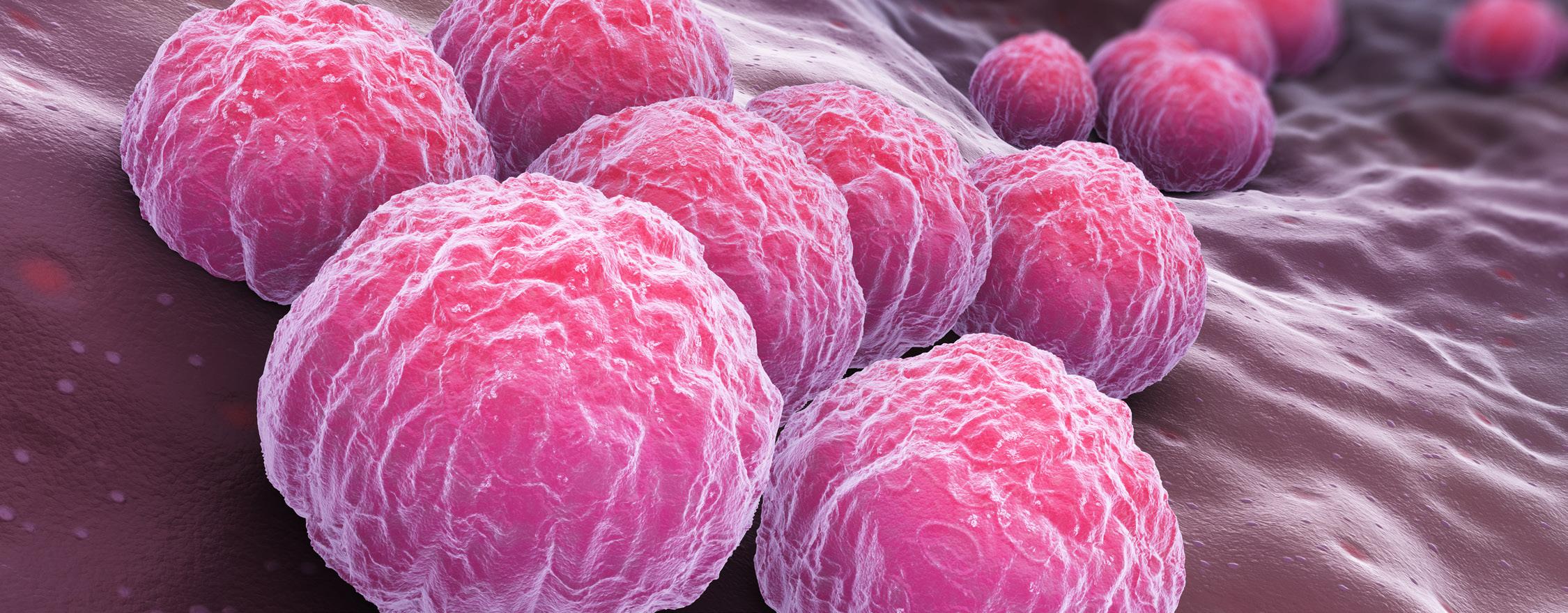
Chlamydia trachomatis, a Gram-negative bacterium, is the pathogen for the sexually transmitted infection (STI), commonly referred to as chlamydia. Chlamydia is transmitted through unprotected oral, anal, and vaginal sexual activities with an individual who has chlamydia, and infection can occur with or without the presence of ejaculate. Individuals who engage in unprotected sex are at greater risk of infection than men who have sex with men. (1) Chlamydia is the most common STI reported in the United States. In 2019, according to a Centers for Disease Control and Prevention report, North Carolina ranked sixth in the nation for the number of positive chlamydia screenings. (2)
Patients infected with C. trachomatis are often asymptomatic, making the incidence of chlamydia much higher than reported due to the lack of proactive screening programs. Untreated chlamydia can lead to complications such as cervicitis, urethritis, and proctitis. In gay, bisexual, and other identifying men who have sex with men, chlamydia-induced proctitis has been shown to have a higher incidence of lymphogranuloma venereum, a chronic infection of the genital lymphatic system. (1) In women with chlamydia, lack of treatment can lead to irreversible damage to the reproductive system with issues ranging from pelvic inflammatory disease, ectopic pregnancy, chronic pelvic pain, and infertility. In pregnant women, chlamydia infection can lead to premature birth. The infection can be transmitted from mother to baby during vaginal delivery, leading to complications such as pneumonia and ophthalmia neonatorum, a form of conjunctivitis that, if left untreated, can result in corneal perforation and blindness. (1)
Although chlamydia is often asymptomatic in both men and women, when symptoms are present, women typically experience vaginal discharge, painful intercourse, dysuria, pelvic pain, lower abdominal pain, and intermenstrual pain. Men can experience dysuria, urethral discharge, and scrotal pain and swelling. Symptoms in both men and women can appear several weeks after the initial exposure. (1)
Individuals aged 15-24 years also have a higher risk of chlamydia infection due to higher rates of risky sexual behaviors, such as multiple or frequent changes in sexual partners. (3) Health disparities also play a significant role in higher incidence rates of chlamydia. According to the CDC, in 2020, chlamydia rates were six times higher for African American/Black individuals than Whites. (2) Using condoms correctly each time an individual engages in sexual activity is the best way to dramatically reduce the risk of becoming infected or transmitting the infection to others. (1)
Patients testing positive for chlamydia should also be tested for other STIs (e.g., HIV, gonorrhea, and syphilis) since the risk of other STIs is high. Table 1 shows the first-line and alternative treatment regimens for chlamydial infection. Main counseling points for patients include:
• Both the patient and their sexual partner(s) should be treated to cure and prevent reinfection.
• Patients should take the entire course of therapy to cure chlamydia.
• If treated with a single-dose regimen, the patient should abstain from sexual activities for seven days. (1)
• If treated with a 7-day course, the patient should refrain from sexual activities until they have completed the entire duration of treatment and have no symptoms. (1)
Doxycycline and azithromycin appear to be equally efficacious in managing urogenital chlamydial infections; however, doxycycline seems more effective in treating rectal and oropharyngeal chlamydial infections for both men and women. (4-7) However, doxycycline is contraindicated in pregnant women during the second and third trimesters.
Historically, C. trachomatis has responded well to antibiotic treatment. Globally, chlamydia has been sensitive to macrolides, tetracyclines, and fluoroquinolones; however, in recent decades, there have been a number of reports of in vitro antimicrobial resistance. (8-11) In a 2000 case report by Somani et al., chlamydia displayed unusual antibiotic-resistance characteristics, and the authors suggested that C. trachomatis displays heterotypic resistance, meaning the chlamydial population contains both susceptible and resistant organisms. (11) Once the antibiotic is no longer present, resistant organisms continue to propagate. (11)
There is no clear treatment pathway for managing antibiotic-resistant chlamydia. In some cases, the pathogenic strain of C. trachomatis may be resistant to treatment or produce a relapse or latent symptom presentation. The patient may not have adhered to their treatment regimen or could be reinfected, presenting with a new infection.Therefore, if symptoms continue after treatment, the patient should be re-evaluated by their primary care provider. (1) If treatment resistance is suspected after evaluation, an antibiotic from the recommended alternative list should be tried. If the second round of treatment is unsuccessful, culture and sensitivity tests may be necessary to determine the next course of action. (11)
Access to care plays a major role in decreasing the rates of chlamydia in North Carolina. (12) As previously mentioned, disparities amongst certain populations leave patients vulnerable and unable to seek medical attention when needed. Affordability and accessibility of care are two key factors perpetuating the high incidence of chlamydia, making it a public health concern in the state. (3) Another attributable factor is acceptability, which refers to patient beliefs and how these translate to their comfort in seeking care and how welcome they feel when receiving care. Gender, sexual orientation, age, ethnicity, education, and socioeconomic characteristics can all influence the perceived patient-provider relationship. When coupled with a particularly sensitive healthcare need, such as an STI, patients may feel very uncomfortable seeking care in a timely manner. The limited availability and accommodation of medical appointments outside traditional medical practice hours further complicate access to care, particularly for disparate populations.
In the United States, there are an estimated 108 million people in which regular STI testing is appropriate. (13) Having efficient and highly accessible screening programs for STIs is essential for decreasing their spread. This is especially true for chlamydia due to the number of asymptomatic cases. In North Carolina, screening for chlamydia during pregnancy is required by law. (14) Sexually active females, 25 years of age or younger, and any individuals with STI risk factors should be screened for chlamydia at least annually. (1) Retesting three months after treatment for chlamydia infection is recommended for all infected individuals, even after successful treatment.(1) North Carolina currently funds local health departments and family planning facilities for chlamydia screening. (15) Yet, our state ranks well above the national average for chlamydia infections. (2)
Community pharmacists serve as a front-line approach for many health care issues, including a number of preventative care needs. What if pharmacists partnered with local health departments to help generate awareness
and assist with screening and treatment for STIs? Pharmacists would be ideal healthcare providers to offer point-of-care (POC) STI screening, risk-mitigation education, treatment, and referral due to their trusted role in their communities. If pharmacists were a more integral part of the screening and treatment initiation, they would have the information they need to help guide treatment adherence and encourage retesting when appropriate.(16-17)
In March 2021, the Food and Drug Administration granted Clinical Laboratory Improvement Amendments (CLIA) waiver for the first-ever molecular POC test and testing platform for chlamydia and gonorrhea. (18) This new technology, offered by Binx Health, provides a novel STI POC testing opportunity for innovative pharmacies that have applied for and received a CLIA waiver. According to an article in Fortune, the company plans to provide free rentals for theBinx io POC equipment, with single-use cartridges (Figure 1) that can provide test results within 30 minutes. (19)
Pharmacies not interested in purchasing, renting, or housing onsite testing equipment can still develop an STI service by partnering with a full-service lab company, such as Labcorp© or Mako Medical Laboratories. Pharmacies may carry, promote, and sell STI home test kits like the Everlywell Chlamydia & Gonorrhea Test (Figure 2).
Everlywell, HealthLabs, Personalabs, QuestDirect, and LetsGetChecked are just a handful of the companies offering STI at-home testing kits run by CLIA-approved laboratories. (20) These at-home tests are easily administered by the patient. Depending on the kit, and the tests to be run, the patient collects finger-stick blood, urine, and/or vaginal swab sample. The collected sample(s) is mailed to the lab, and once the lab processes the test, the patient is contacted directly with their test results.
For pharmacists to be able to sustain a pharmacy-based STI service, major policy advancements are needed. Becoming and staying involved with the North Carolina Association of Pharmacists (NCAP) is an effective way to advocate for policy change in the profession. In North Carolina, pharmacists are allowed to perform CLIA-waived POC tests. Gaining the authority for pharmacists to test and treat certain STIs could dramatically improve access to screening and treatment and should help produce a positive shift in managing this public health crisis. However, the challenge pharmacists and pharmacies face is that health plans typically do not recognize and pay pharmacists for screening and evaluation, nor do health plans reimburse for the test-related materials at an appropriate level.
In the next legislative session, NCAP will run a bill calling for fair reimbursement and test-andtreat authority for pharmacists. It would be advantageous to address chlamydia and other STIs if North Carolina pharmacies had access to state funding to help cover the cost of STI screening and care for uninsured or underinsured individuals.
Author: Briana Williams is a 2023 PharmD Candidate at Campbell University College of Pharmacy and Health Sciences.
References
1. Detailed STD Facts - Chlamydia. https://www.cdc.gov/std/chlamydia/ stdfact-chlamydia-detailed.htm. Updated 2022. Accessed Jun 15, 2022. 2. Sexually Transmitted Disease Surveillance 2019. Table 2. Chlamydia — Reported Cases and Rates of Reported Cases by State, Ranked by Rates, United States, 2019. CDC Web site. https://www.cdc.gov/std/statistics/2019/tables/2.htm. Updated 2022. Accessed Jun 15, 2022. 3. Cooksey CMJL, Berggren EK, Lee J. Chlamydia trachomatis Infection in Minority Adolescent Women: A Public Health Challenge. Obstetrical & Gynecological Survey. 2010;65(11):729-735. 4. Kong FY, Tabrizi SN, Law M, et al. Azithromycin versus doxycycline for the treatment of genital chlamydia infection: a meta-analysis of randomized controlled trials. Clin Infect Dis 2014;59:193–205. 5. Páez-Canro C, Alzate JP, González LM, Rubio-Romero JA, Lethaby A, Gaitán HG. Antibiotics for treating urogenital Chlamydia trachomatis infection in men and non-pregnant women. Cochrane Database Syst Rev 2019. 6. Dukers-Muijrers NHTM, Wolffs PFG, De Vries H, et Treatment effectiveness of azithromycin and doxycycline in uncomplicated rectal and vaginal Chlamydia trachomatis infections in women: a multicentre observational study (FemCure). Clin Infect Dis 2019;69:1946–54. 7. Dombrowski JC, Wierzbicki MR, Newman LM, et al. Doxycycline versus azithromycin for the treatment of rectal chlamydia in men who have sex with men: a randomized controlled trial. Clin Infect Dis 2021. 8. Mourad A, Sweet RL, Sugg N, Schachter J. Relative resistance to erythromycin in Chlamydia trachomatis. Antimicrob Agents Chemother. 1980;18:696–8. 9. Jones RB, DerPol BV, Johnson RB. Susceptibility of Chlamydia trachomatis to trovafloxacin. J Antimicrob Chemother. 1997;39(Suppl B):63–5.
10. Lefevre JC, Lepargneur JP, Guion
D, Bei S. Tetracycline-resistant
Chlamydia trachomatis in Toulouse,
France. Pathologie Biologie (Paris) 1997;45:376–8. 11. Somani J, Bhullar VB, Workowski
KA, Farshy CE, Black CM. Multiple drug-resistant Chlamydia trachomatis associated with clinical treatment failure. J Infect Dis. 2000;181:1421–7. 12. Wyszewianski L. Access to Care: Remembering Old Lessons. Health Serv
Res. 2002;37(6):1441-1443. \ 13. U.S. Preventative Services Task
Force. Chlamydia and Gonorrhea:
Screening. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/chlamydia-and-gonorrhea-screening. Updated 2021. Accessed July 18, 2022. 14. 10A NCAC 41A .0204. Control Measures - Sexually. http://reports.oah. state.nc.us/ncac/title%2010a%20 -%20health%20and%20human%20 services/chapter%2041%20-%20 epidemiology%20health/subchapter%20a/10a%20ncac%2041a%20 .0204.pdf. Accessed July 18, 2022. 15. North Carolina Department of
Health and Human Services.
Chlamydia in North Carolina, 2020. https://epi.dph.ncdhhs.gov/cd/ stds/figures/2020-Chlamydia-Factsheet-Final.pdf. Updated 2021. Accessed July 18, 2022. 16. Ross M. Three STDs Spreading: How
Pharmacists Can Help. Pharmacy Times 2015. https://www.pharmacytimes.com/view/3-stds-spreadinghow-pharmacists-can-help. Accessed
September 8, 2022. 17. Wood H, Gudka S. Pharmacist-led screening in sexually transmitted infections: current perspectives. IPRP. 2018;7:67-82. 18. U.S. Food and Drug Administration.
FDA Allows for First Point-of-Care
Chlamydia and Gonorrhea Test to be Used in More Near-Patient Care
Settings. https://www.fda.gov/ news-events/press-announcements/ fda-allows-first-point-care-chlamydia-and-gonorrhea-test-be-usedmore-near-patient-care-settings.
Updated 2021. Accessed July 18, 2022 19. Hay M. Binx aims to capture a milestone in STI testing technology. https://fortune.com/2020/04/21/ sti-testing-binx-io-clinics-pharmacy/.
Updated 2020. Accessed July 18, 2022. 20. Everlywell. Discreetly test for chlamydia and gonorrhea. https://www. everlywell.com/products/chlamyd-
ia-gonorrhea-test/. Updated 2022. Accessed July 18, 2022. 21. Workowski KA, Bachmann LH, Chan
PA, et al. Sexually Transmitted Infections Treatment Guidelines, 2021.
MMWR Recomm Rep. 2021;70(4):1187 22. Binx. CLIA-Waived, Point-of-Care
Testing. That’s the binx io; https:// mybinxhealth.com/point-of-care. Updated 2020. Accessed July 18, 2022.
Table 1. Centers for Disease Control and Prevention (CDC) 2021 treatment guideline on urethral, cervical, or rectal C. trachomatis infection21
Treatment Regimens for Non-Pregnant Adolescents and Adults
First-line Regimen Doxycycline 100 mg orally twice daily for 7 days
Alternative Regimens Azithromycin 1 g orally in a single dose or Levofloxacin 500 mg orally once daily for 7 days
Treatment Regimens for Pregnant Women
First-line Regimen Azithromycin 1 g orally in a single dose
Alternative Regimen Amoxicillin 500 mg orally 3 times/day for 7 days
Figure 1: Binx io Testing Platform for Chlamydia & Gonorrhea22
Figure 2: Everlywell Chlamydia & Gonorrhea Test Kit Components20











