
34 minute read
Dr. Katherine Johnson: What is a cataract?
What is a cataract?
By Dr. Katherine Johnson A cataract is the clouding of your natural lens. The lens is located behind the pupil and helps to focus light onto the back part of the eye, the retina. As we get older, the lens thickens and will be able to focus less and less. This is the main reason most of us need reading glasses in our 40s or 50s. Eventually, the lens will become hard and yellow, possibly even white, and will change enough that your vision will become blurry and cause glare from bright lights.
Advertisement
Glasses cannot the vision loss due to cataracts, because the light is passing through a cloudy lens, like looking through a dirty window. When this occurs, the only way to improve your vision is to have the cataract removed. Unfortunately, this is a natural aging process and no drops or pills will fix it. The good news is that cataract surgery is one of the most successful and lowest risk surgeries we have in modern medicine and with current technology can be almost as accurate as LASIK.
The cataract, which is just the cloudy lens, needs to be removed from the eye and replaced with an artificial lens. The artificial lens is acrylic and causes no limitations or problems in the future. Modern cataract surgery is performed by breaking the lens up with an ultrasound and removing it through a tiny incision in the side of the eye. The surgery is usually very fast and typically done with only local anesthesia and a little relaxing medicine (happy juice). The wound is selfsealing, and the recovery time is often as little as one day. Cataract surgery is performed in a sterile operating room by an ophthalmologist. An ophthalmologist is a doctor specializing in disease and surgery of the eye. There have been some very exciting advances in cataract surgery in recent years, specifically with improvements in the artificial intraocular lens that takes the place of the old cataract lens. This lens will focus the light onto the retina, just like your old lens, but often even better. We can calculate which lens to use and many times can put your glasses prescription inside the new lens.
There is an additional option to take extra measurements of the eye during surgery to improve this accuracy and even fix your astigmatism. Recently, new lens technology has allowed us to put trifocal and progressive lenses inside the eye as well to limit your need for reading and computer glasses. These lenses, called multifocal lenses, will give you back as much youthful vision as modern
medicine allows. Imagine not needing glasses for anything anymore!
How do you know if you have cataracts? The symptoms of cataracts often develop slowly but include blurry vision, glare from headlights, difficulty seeing in dim lights, shadow images, and trouble reading fine print. Typically, cataracts develop in your 60s or 70s, but some people develop them earlier and others later.
If you notice these symptoms, contact an eye doctor, either an optometrist or ophthalmologist, for an evaluation and we can help you decide if you are ready for surgery. The surgery is typically covered by your medical insurance, not vision insurance. The premium multifocal lenses are not covered by insurance and cost extra out of pocket. Cataract surgery is only done once per lifetime, and the lens you choose will last for the rest of your life.
Everyone will eventually get a cataract, if we live long enough. The time to take the cataract out is when the symptoms of the cataract bother you enough to have the minor surgery to remove them. Because the surgery is so successful and so low risk, you don’t need to wait until “they are ripe” anymore. Luckily, in Alaska, we have incredible surgeons to help you and offer the very best in modern cataract surgery.
Dr. Katherine Johnson, M.D., FACS, is an ophthalmologist at Mountain View Eye Center in Fairbanks.
The One Health concept: Health care professionals, scientists and researchers who’ve embraced the One Health concept depend on community members for information about changes in the environment in their area and how it affects wildlife and other food sources. Courtesy of Local Environmental Observer Network
A new way of thinking
One Health is the idea that health of Alaskans is linked to the condition of animals and the environment
By Tim Ellis F or years, the western Alaska city of Bethel was overrun by stray dogs – hordes of mutts that had gone feral and overrun the town and surrounding Yukon-Kuskokwim Delta. The overpopulation created the usual assortment of nuisances, like strays knocking over garbage cans, raiding dumpsters and snuffling around in sewage. And that, in turn created a serious threat to human health.
“Dogs that live outside and have a meat-based diet are very likely to have parasites, and a lot of these parasites are transferable to people,” Brian Berube, an environmental health consultant with Alaska Native Tribal Health Consortium, told a local radio station reporter. That, combined with the problem of people being bitten by the strays, created a serious health threat — the spread of rabies and other diseases. In early 2017, nearly a thousand dog bites had been reported over the previous decade, mostly by strays. Most of the victims were children under age 10.
“Rabies is rampant over there,” says Arleigh Reynolds, an associate professor of veterinary medicine at the University of Alaska Fairbanks. “Every year, several people get treated for exposure to rabies.”
In response to the problem, experts with the Tribal Health Consortium, along with local, state and tribal officials, launched a series of measures that included bringing a full-time veterinarian to Bethel. They ramped up spay and
neuter programs and instituted humane means of reducing the stray dog population. They also launched research projects on diseases and other public health challenges created by canine overpopulation.
The multifaceted response was conducted using the principles of a relatively new approach to public health called One Health, says Reynolds, who directs UAF’s Center for One Health Research. “It isn’t a term that everybody knows yet, but I think it’s getting a foothold” among members of the general public, he said.
What is One Health? The One Health concept recognizes that the health of people is connected to the health of animals and the environment. The concept applies a holistic, multidisciplinary approach to studying, understanding and managing human health threats that arise from environmental, human or animal causes.
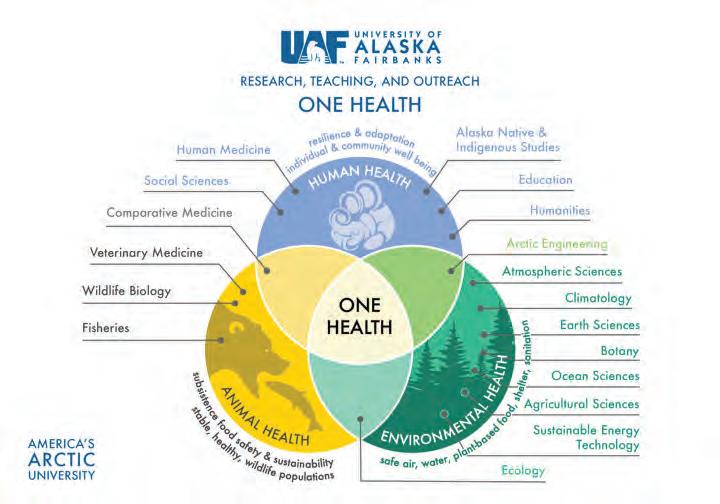
Veterinarians came up with the term One Health to explain the causes and solutions to diseases that spread from animals to humans — so-called zoonotic diseases. Reynolds says One Health takes into consideration human, animal and environmental factors in seeking solutions to the root causes of disease, instead of just treating the symptoms. He says an increasingly common environmental factor related to the spread of rabies and parasite-borne diseases in Alaska and elsewhere around the circumpolar north is climate change. The warming climate is more hospitable for disease-causing vectors, like the rabies and parasites that were being spread by Bethel’s feral dogs. And it enables wildlife like deer and elk to range farther north, bringing more and different diseases.
Reynolds says 70 percent of the world’s emerging diseases come from animals. And because the circumpolar north is warming more than twice as Mike Brubaker is director of Community Environment and Health for the Alaska Native Tribal Health Consortium. Courtesy of ANT HC

fast as the rest of the planet, there’s growing concern over tick-borne diseases brought into Alaska by those invasive animal species.
Other human health threats from climate change include harmful algal blooms offshore in areas where shellfish
Scientists believe warmer sea surface temperatures around Alaska are promoting large toxic algal blooms like this in the Bering Sea, which contaminates shellfish, an important subsistence food source for people who live along coastal areas. Courtesy of Local Environmental Observer Network
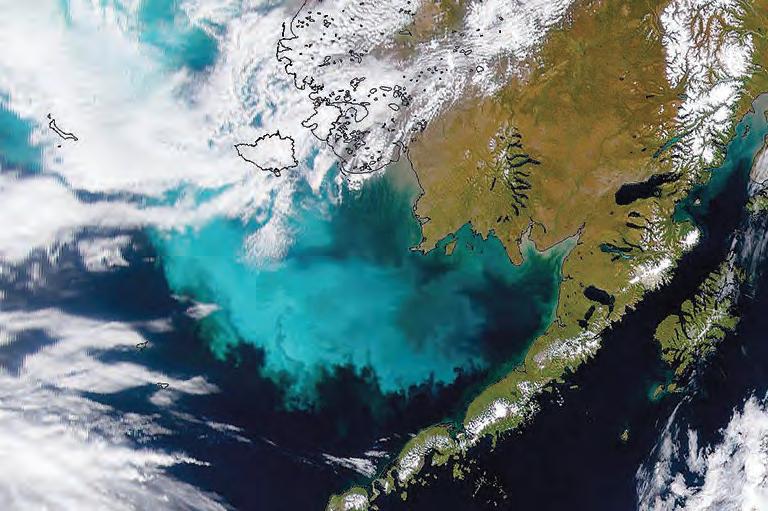
are harvested, and outbreaks of foodborne illnesses from spoiled meat in underground caches that no longer stay cool enough to keep the meat frozen. “This is really important when there are concerns about problems with a subsistence food source,” Reynolds said.
An approach for the Arctic Michael Brubaker, director of community environment and health for the Alaska Native Tribal Health Consortium, says applying the collaborative One Health works especially well in communities of indigenous peoples.
“It’s been gaining a lot of traction in the Arctic in particular, because of the people who live so close to the land,” said Brubaker, who’s worked with Reynolds and others to integrate One Health into his work.
“It’s an ecosystem approach to health,
so it resonates strongly in the Arctic and its indigenous peoples,” he said. Reynolds adds that indigenous peoples are keen observers of the land and its wildlife, and they also possess knowledge that’s passed down from their elders over millennia. He says that knowledge is hugely helpful for public health workers, along with scientists and researchers – and that’s an essential component of the One Health approach.
“We feel that a lot of the information we need to work on these problems exists among members of the community,” he said. “We build a relationship with the community, and then ask them what they see, help them build a data source and help them interpret that information so we can figure out a plan to mitigate the problem, or adapt to it.” He says One Health challenges health-care professionals and members of the scientific community to listen and talk with people.
“Traditionally,” Reynolds said, “what we health-care professionals have done when we look at these problems,” like the health threats posed by a feral dog overpopulation, “is typically send scientists and researchers into communities with a predisposed idea of what the problem is. And that’s what they’ll look at — which is often not what the community is actually experiencing.
“We feel that a lot of the information we need to work on these problems exists among members of the community,” he said, “but scientists maybe haven’t been taught how to listen to them, and how to talk in plain language the community members can understand.”
Tim Ellis is a freelance writer living in Delta Junction. Comments about this story? Email editor@newsminer. com.
‘One Health, One Future’ conference set for March at University of Alaska Fairbanks campus
Alaska Pulse T he University of Alaska Fairbanks Center for One Health Research and the U.S. State Department will jointly host an international conference in March that is expected to be the largest circumpolar One Health conference held in the United States in the coming year.
The “One Health, One Future” conference, to be held on the UAF campus March 11-14, will bring together public health officials, scientists and researchers from around the circumpolar north. Officials with the Arctic Council’s Sustainable Development Working Group and other international organizations
also will participate.
This event is part of the U.S. contribution to “One Arctic, One Health,” a five-year Arctic Council project that seeks to develop a circumpolar network of One Health experts to can share knowledge, conduct exercises and initiate collaborative investigations of One Health issues.
Adapted from

Courtesy of NVision Architecture

Long-awaited clinic coming to Tok
By Kyrie Long Alaska pulse C onstruction on a new health clinic is underway in Tok, with plans for Tanana Chiefs Conference to open the location this summer and expand health care services in the Upper Tanana subregion.
TCC, an Alaska Native nonprofit that provides health and social services, does have some services available in Tok.
In 2011-12, according to TCC Chief and Chairman Victor Joseph, it opened a subregional clinic in the Upper Tanana area at the request of the organization’s Upper Tanana board. Then, in 2014, it took over behavioral health services in the same area.
The nonprofit announced in May this year that it would be opening a new clinic in the area, with construction slated to start this year as well.
It hit a bit of a hiccup along the way: The clinic and Fort Greely shared the same contractor, with the military installation taking priority, so the construction ran a bit behind schedule. Nevertheless, TCC kept at it and the last of the beams for the hospital were slated to go up in December.
“So we’re doing well,” Joseph said. “Construction is moving along and we’re not expecting any problems. We’re still planning on opening next summer.” There are a few health care options available in Tok at present.
“Right now we’re operating out of three locations,” Joseph said.
The existing locations include two clinics and a behavioral health services facility. Together they can provide behavioral health and dental services, emergency care and primary care.
However, serving larger numbers of people can be difficult with the current clinic locations.
Joseph said the new clinic will allow TCC to meet the needs of people in the area when there is a “multi-person encounter.” For example, if there is a multivehicle accident, it’s hard for the existing clinics to meet the needs of multiple people with injuries.
“In our present locations ... when we have that happen, we’re having to use space that wasn’t designed for it,” he said. The new clinic will offer the full array of services out of a single facility.
“So we’ll have trauma care rooms, family practice rooms and we’ll also have behavioral health and dental services,” he said.
There are also plans for the clinic to have a pharmacy.
Joseph said TCC is making sure it can provide “good, solid medical care in a state-of-the art facility, one where they’re going to have a little bit more elbow room.”
Step by step by step Homer-area resident Louise Eskes (left) enjoys a walk with Dr. Paula Godfrey (center), an emergency room doctor at South Peninsula Hospital, and Godfrey’s daughter, Grace. Courtesy of South Peninsula Hospital

Homer’s Walk with a Doc aimed at community wellbeing
By McKibben Jackinsky B onita Banks, the health and wellness educator at South Peninsula Hospital in Homer, was searching for ways to improve the wellbeing of southern Kenai Peninsula residents when she heard about the Walk with a Doc program.
“Homer doesn’t have a mall. We don’t have an outdoor park. We needed someplace accessible to everyone,” said Banks, a registered nurse.
Walk with a Doc was started in 2005 by Dr. David Sabgir, a cardiologist from Columbus, Ohio, who improved his effectiveness in encouraging patients to make behavioral changes when he moved from a clinical setting to the informal atmosphere of a community walk. The approach has since spread worldwide with more than 500 chapters, including Walk with a Future Doc chapters led by medical students. The idea is to provide a comfortable setting in which participants ask health-related questions of local medical providers.
South Peninsula Hospital offers Walk with a Doc twice a month. The events are free to community members of all ages and all abilities.
Funding for the program comes from the hospital, with additional support from South Peninsula Hospital Foundation.
“The Walk with a Doc program is totally awesome,” said walker Barb Brodowski, who has taken advantage of the program since it began in Homer in 2017. “I can’t thank South Peninsula Hospital and the SPH Foundation for allowing the program to be held at no cost to participants.”
As perfect as the program appeared to be for Homer, Banks recognized a crucial missing piece — a good location.
The timing couldn’t have been better. Construction of the South Peninsula Athletic and Recreation Center was nearing completion. The $550,000 project, led by the Homer Soccer Association with Daniel Zatz at the helm, added a 12,000-square-foot fabric building designed by Alaska Dreams of Anchorage to the Homer landscape. It has a steel framework, a shape that sheds snow, and a floor made for sports activities.
“It was the perfect indoor place. Safe, out of the elements and fully accessible to everyone,” Banks said.
Having solved that problem, Banks
Board certified in OB/GYN, Dr. Katie Ostrom (left) and Health and Wellness Educator Bonita Banks (second from left), both of South Peninsula Hospital in Homer, give a short presentation to participants of Walk with a Doc. Courtesy of South Peninsula Hospital.

took her idea to Homer medical providers. She pointed out that in 2015, Vivek H. Murthy, the United States surgeon general, said, “Walking for better health may seem simplistic, but sometimes the most important things we can do are also the easiest and most obvious.” As she envisioned it, Homer’s program would be held at the rec center two times a month, begin with a 10-minute presentation by a doctor or other health care provider, be followed by a 45-minute walk led by the presenter, and offer fruit, water, coffee and blood-pressure checks.
Walk with a Doc fit the findings of Homer’s 2016 Community Health Needs Assessment: the community’s age demographic, concerns about obesity, heart disease and cancer as leading causes of death, and provided an avenue for family well-being. It also would strengthen relationships between the general population and the health-care community, Banks pointed out.
To get started, a physician was needed as lead doctor and spokesperson.
The first to raise his hand was Dr. Rob Downey, a general practitioner whose specialty is functional medicine and is a self-professed “big walker.” Banks and Downey recruited additional doctors, nurse practitioners, physician assistants, midwives, mental health professionals, physical therapists and others, giving walkers the opportunity to meet and ask questions of a wide range of medical professionals. Paula Godfrey, an emergency room doctor at South Peninsula Hospital, brought a touch of reality to her presentation on what days in the ER are like when one of her two daughters surprised walkers by faking a collapse and Godfrey’s other daughter provided immediate assistance.
“Different topics draw different people. It’s a really simple opportunity to answer questions that are a conundrum to them,” Downey said.
If questions indicate the need for medical follow-up, Downey encourages

seeing a doctor.
“This is an opportunity to be helpful,” he said. Of the program’s many benefits, Downey has observed it leaves participants feeling empowered for having had their questions answered and learning about resources available.
Banks said the value is widespread. “We have a core group of regulars who try to come to every walk — families, kids with trikes, three generations walking together — and we always have new people,” she said. “When you see people come together every other week and know they’re there for the social
Opposite page, bottom, Dr. Neil Schott (left), a physical therapist at South Peninsula Hospital, teaches walker Willy Dunne (right) exercises to address chronic pain. Right, using a rolling walker, Bonnie Boigvert is able to take advantage of Walk with a Doc, a twice-a-month community walk in Homer. Photos courtesy of South Peninsula Hospital


connection, it’s so rewarding. And then when you talk to people that showed up and did a quarter mile, and months later did a half mile and now they’re jogging, it’s great.”
Homer’s Walk with a Doc begins in October and wraps up in May, coinciding with the finish of a monthlong, communitywide walking challenge.
Not limiting her walking to the twice-a-month event,
Brodowski also walks at the rec center 2 miles a day, five days a week with friends. She remains one of Walk with a Doc’s biggest fans, setting two alarm clocks to ensure she doesn’t miss the Saturday morning event. “Every time I go, I learn another bit of information. It may not be pertinent to me at the moment, but, hey, one never knows,” she said.
A Valdez chapter of Walk with a Doc was begun in 2016 by Dr. Angela Alfaro in partnership with the city’s Parks and Recreation Department. The chapter is currently being reorganized, In Fairbanks, a chapter of Walk with a Future Doc is in the pre-planning stages for Foundation Health Partners, according to Kelly Atlee, the foundation’s senior director of communications and public relations. It is being spearheaded by Travis Kinane, a Pacific Northwest University third-year medical student currently placed at the Fairbanks Memorial Hospital and Tanana Valley Clinic. Kinane discovered the program while looking for a way to meet the needs of Fairbanks-area residents who “didn’t have a gym membership and needed some motivation and accountability.”
Dates, times and location are yet to be decided, but Atlee anticipates it will be “a fantastic program.” McKibben Jackinsky is a freelance writer living in Homer. For more information: • Walk with a Doc: walkwithadoc.org/ • Walk with a Doc, Homer: sphosp.org/ resources/community-education-events/ walk-with-a-doc/
With the help of two walking sticks, Homer-area resident Kat Stroup is off and walking at Walk with a Doc.





Accepting new patients of all ages, our team of providers specializes in cataract surgery, including premium lenses, ocular disease treatment, including diabetes, glaucoma and macular degeneration, ocular lasers, glasses and contact lens prescriptions, and annual eye exams!
TEXT or call us for an appointment today! 907-328-2920





Same day glasses possible for many prescriptions! Saturday appointments are available!
2555 Phillips Field Road | Fairbanks Alaska 99709
www.mountainvieweyes.com

Recipient Curt Whalen, right, with donor Dan Hauer after the kidney transplant. Donating a kidney to a friend in need was a no-brainer, according to Hauer. Courtesy of Dan Hauer
— Curt Whalen
Making a connection
Years after kidney donation, Fairbanks men remain close
By Kris Capps Alaska Pulse
Curt Whalen and Dan Hauer share a strange and wonderful connection. Back in 2014, both men worked as biomedical technicians at Fairbanks Memorial Hospital and had been friends for more than 10 years. So Dan knew that Curt suffered from polycystic kidney disease, an inherited disorder that occurs when clusters of cysts develop in the kidneys. Over the years, the disease progressively worsened.
By 2014, Curt knew he needed to get on the kidney transplant list. He wasn’t surprised. Both his siblings suffered the same condition and both underwent kidney transplants.
But he was surprised when Dan, who had become his boss, offered to donate one of his kidneys.
“It wasn’t even a thing where I had to ask for it,” Curt said. “He just offered.” Dan Hauer gave this little Grover figure to his wife in college. She later handed it down to their kids, who gave it back to their dad to watch over and comfort him during the transplant surgery. Courtesy Dan Hauer

“Now he’s gone and I’m still here and he didn’t take his kidney with him,” he added with a laugh.
Dan and his family moved to Kentucky in 2018. The friends still stay in touch and Curt contacts him on the anniversary of the transplant every year. Curt still works at Fairbanks Memorial Hospital.
For Dan, offering the kidney was a no-brainer.
His wife is a surgical nurse, so she was well aware of the procedure and totally supported the donation. His kids were a little nervous at first, he said, but once they learned more about it, they supported his decision.
Both men had a common friend who was on dialysis, and Dan didn’t want Curt to have to go through that.
“I knew at some point it would progress to the point he was going to need it and I was happy to offer it,” he said. “So I got tested and it ended up working out.”
The result has been that nearly six years later, both men are healthy and
rarely think about the surgery that changed Curt’s life.
“I try to just live life to the fullest and take each day as it’s given to me,” Curt said.
However, if that transplant had not happened, he said, “we wouldn’t be having this conversation. It definitely gave me a new lease on life.”
It also made him realize he is thankful for everything he already has.
“You reach a point in life where things you thought were important things in your youth … in the grand scheme, they don’t amount to much,” he said.

Although Dan Hauer moved out of state, the two remain friends. They share another connection: In 2016, Dan ruptured his patella tendon. A year to the day later, Curt ruptured his. Exactly another year later, Dan ruptured his other patella tendon.

Courtesy of Dan Hauer
So he embraces life every day and looks forward to his quarterly health reports. That motivates him to stay healthy.
Dan doesn’t think about it much either all these years later. He remains healthy and active, he said.
“It was something that had to be done at the moment. And it had to be done for someone I cared about, so I didn’t think twice about doing it,” he said. “But I don’t think back on it often. It was just something that had to be done.”
He said he wishes donating kidneys was more commonplace.
“It is major surgery,” he said. “But if you’re healthy and hydrating and taking care of yourself, you’re in the best position to be able to do it. And there are very few reasons to say you won’t do it.” The two friends have another medical connection. In 2016, Dan ruptured his patella tendon. A year later, to the day, Curt ruptured his patella tendon. Curt says it was a year later, again to the day, that Dan then suffered the same injury to his other leg.
“I told him, you better mark your calendar,” Dan said. “But he made it through last year without doing his other knee.”
The two remain good friends. They text each other once in awhile and Curt always gets in touch on the anniversary of the transplant.
“We’re guys. So we stay in touch the way guys stay in touch,” Dan laughed. “Just a quick ‘How’s it going?’”
Reach columnist/community editor Kris Capps at 459- 7546.
David James poses with an owl during a 1996 trip to Georgetown, Malaysia. Be prepared with the proper vaccinations and medications for problems that might crop up while traveling.
By David James
Know before you go
My wife was taking a medical librarianship class in the months before she and I left on a trip to Southeast Asia in the mid-1990s. As she learned of various rare diseases found in the tropics, she came home every night with a new and different story of some hideous affliction we might get exposed to. Then she described in graphic detail the way that illness could slowly and painfully kill us. Having having spent about a year all told traveling parts of Asia and Latin America before meeting her, and doing so without serious ailment, I calmly responded, “If we die, it will be in a bus crash.”
According to Dennis Rogers, a physician assistant at Tanana Valley Clinic in Fairbanks who has done travel consultations for 35 years, I was more or less correct. In a recent email exchange he told me that the “most important advice for travelers is safety. The leading cause of death when traveling is accidental trauma. Slow down, be safe.” Like many Alaskans, I’ve been known to flee the state during the winter. Which is why, in advance of an impending return visit to India this year, I made a recent appointment with Rogers to be sure I was medically prepared.
Getting sound medical advice and making sure you’re up to date on immunizations is important before heading off to parts of the world where illnesses unfamiliar to Americans can lurk. Trauma might be the most common cause of traveler deaths, but diseases like typhoid Check with a medical professional to update vaccines, medicines

and malaria can result in prolonged misery, even if you survive. But unlike trauma, there are steps you can take before you leave to avoid many ailments.
Alaska PULSE

2020 Make eye health a priority this year
North Pole facility collects, redistributes glasses ‘One Health’ in rural Alaska Walk with a Doc in Homer Kidney donation strengthens friendship See a medical professional before traveling Sitka’s holistic focus on community health Music as a healing force for teens Fairbanks sleep lab promotes zzzz’s Blood donation may have saved Healy man’s life
January 2020 Vol. 1, No. 1 FREE
Get your ad in this new full-color, glossy magazine about everything health in Alaska.
Call (907) 459-7548 or email advertising@newsminer.com
Preparing for my trip to India Practitioners who specialize in travel medicine can be found in most of Alaska’s larger communities, but even smaller clinics can help with needed immunizations, prescriptions and advice. So when should you consider a consultation? Rogers said, “It’s a good idea for most developing countries. But it’s always worth checking health-related issues for any country you’re traveling to.”
This is why your first stop before scheduling an appointment should be the Traveler’s Health page maintained by the U.S. Centers for Disease Control and Prevention (https:// wwwnc.cdc.gov/travel). Here you can find notification of current disease outbreaks across the globe, advice on the best pre-travel medical options, and tools for locating travel clinics and places that offer vaccinations. Best of all, the main page has a drop-down menu where you can click on the country or countries you plan on visiting and get the most up-to-date information.
Some of what’s found is self-evident. If you’re going to Iceland, bring a warm jacket and rain gear. If Indonesia is your destination, be sure you’re up on all vaccines and have a medical professional prescribe malaria pills and other needed medicines.
I pulled up the page for India to see what was advised. I’ve been fully protected against measles since college and had gotten this year’s flu shot, so those immunizations weren’t needed. Among other routine vaccinations, Rogers recommended I get a second hepatitis A injection (I’d only had one previously), as well as the jab for hepatitis B. While this form of hepatitis can only be acquired through bodily fluid exchanges, Rogers told me there have been rare occasions of travelers being bitten by infected people. Although this seemed unlikely, I decided to get the shot anyway.
Rogers also prescribed malaria prophylactics, which the CDC advises, and went over a map of India with me to let me know where the disease is most prevalent. I was surprised to learn that in the tropical south, where I had presumed the risk would be highest, it was in fact far less common than in northern cities on the Gangetic Plain. We discussed ways to avoid getting bit by mosquitoes, the first and most important line of defense against the parasite that the insects have carried to many countries.
Malaria is not something to be taken lightly. Years ago a coworker of mine came down with it shortly after returning from the tropics. He was a highly athletic marathon runner and weight lifter, but his body was reduced to a near skeletal state in a very short time. Had he not been in such good condition to begin with, his chances of survival would likely have been much slimmer.
Author David James and a young friend in Nebaj, Guatemala in 1991.

Among other routine vaccinations, Rogers recommended I get Other concerns for my destination include Japanese encephalitis, typhoid and rabies. Rogers said my likelihood of contracting encephalitis in the places I would be visiting was outweighed by the possible negative reactions to the vaccine. So we skipped that one. Typhoid, on the other hand was something I had never been vaccinated for. In the 1990s, when I spent a lot of time in developing nations, the typhoid vaccine was known to cause so many ill side effects that even specialty travel clinics advised against it unless someone was traveling directly into an outbreak. These days there’s a safe oral vaccine that consists of four pills taken over seven days. So I got a prescription for that along with the malaria medicine.
Rabies is more difficult. I’ve always said the one thing in India that truly frightened me during my first visit was dogs. They’re feral and aggressive. Rogers felt that a vaccination was unnecessary but did offer detailed instructions on what to do if I am bitten.
Food safety was another area of discussion. As a veteran traveler, I’m probably not as cautious as I should be. I like to eat and I often try strange foods. Still, there are certain things you should avoid, which the CDC page also details. Rogers told me that while stomach bugs frequently strike travelers in developing nations, often the cause is not food but failure of the traveler to eat with clean hands. So carrying antiseptic hand wipes isn’t a bad idea. He also prescribed a powerful antibiotic for if I do get sick. In his email, Rogers mentioned that many travelers engage in reckless sexual behavior, a point the CDC raises as well. And while some might think that avoiding sex workers will eliminate the risk, you don’t actually know the full history of that instant crush from Australia who you just met.
“So when I talk about safety,” Rogers said, “it includes putting on your seat belt, helmet and condom!”
Preparing for your own trip Since he’s been offering travel consultations for so long and is an avid traveler himself, I asked Rogers if he had been surprised by anything he’s encountered as a professional over the years.
He told me, “The most alarming thing I deal with is parents who still do not believe in vaccines and do not vaccinate their kids. Then when they come in for a travel consult to the developing world, these young folks have to do these intense catch-up schedules on vaccines. I don’t believe in the tooth fairy, but I do believe in the value and protection vaccines can offer.”
This is sound advice even for nontravelers. The recent and unwanted outbreaks of measles in America, a country where the disease was considered eliminated two decades ago, offer a
— Dennis Rogers, physician assistant at Tanana Valley Clinic
solemn reminder of why vaccines are necessary and just how much damage can be done by those who shun them based on medically unfounded claims of their dangers.
Monitoring your health after returning from overseas is as important as a pre-travel consultation and exercising safe practices while abroad. Rogers said the things to look out for are “Top of the list: fever, especially if traveling in a malaria endemic area.” I remembered my coworker who developed malaria in the ‘90s. He knew what signs to look for and sought medical help as soon as he noticed them.
Rogers said returning travelers should also seek prompt medical attention if they experience “persistent diarrhea or gastrointestinal symptoms, especially bloody stools.” Then, being the traveler he is, he added that he’d happily meet with “anyone with really great photos and experiences.”
I was sent home from my appointment with a small book called “The Pocket Doctor,” which is packed with information on health risks for travelers and how to identify and find help for them and which will go in my bag. It includes a suggested medical kit to pack along. The CDC site has a similar list of items, as well as specialty pages listing what might be needed for every foreign country, even Iceland.
I’m not a hypochondriac, but over the course of my varied overseas excursions I’ve had my share of stomach ailments, bloody injuries and (fortunately benign) bug bites. In Indonesia I developed an extremely high fever one day and was considering going to a hospital when it broke as quickly as it came on. I’ve never known the cause.
On a trip to Central America I found myself lacking antibiotics for severe stomach issues and wound up making an unplanned visit to a doctor in Honduras. It probably could have been avoided if I’d had my own supply of pills. So now I carry them when traveling in countries where Montezuma or Shiva might be eyeballing my intestinal tract.
But in the end, the advice I gave my wife years ago on what was most likely David James on Mount Bromo, island of Java, Indonesia.

to kill us is borne out by the CDC page for India.
The longest section of warnings and recommendations is labeled “Select safe transportation.” The first sentence of this section says, in boldface, “Motor vehicle crashes are the #1 killer of healthy US citizens in foreign countries.” These include pedestrian mishaps, motorcycle wrecks, getting in a vehicle operated by a drunk driver, and, yes, bus crashes.
And most importantly, the CDC and Rogers both advise getting medical evacuation insurance. These policies are inexpensive but invaluable if you find yourself needing immediate assistance in a remote location. You might come home sooner than intended on a medical flight, but it will be paid for, and it beats getting flown home in a box.
For those considering overseas ventures, Rogers said, “People need to plan weeks to months in advance of their travels for possible medical needs, vaccines, meds for malaria, and individual country recommendations and requirements.”
Check the CDC website regardless of how safe the country you will be visiting might be, schedule an appointment with your doctor if vaccinations and/or prescriptions are advised, and go forth armed with knowledge and the proper preventive measures in place. Happy travels.

Caring for your skin is what we do!
Dr. Nicole Soto, M.D. Dr. Maren Gaul, D.O.






