Medical record


FALL 2022 BERKS COUNTY MEDICAL SOCIETY Your Community Resource for What’s Happening in Healthcare The BCMS Pat Sharma President’s Scholarship How to Become an Optimist Street Medicine – Reborn in Berks SCAN TO READ ONLINE INSIDE:
Exceptional heart and vascular surgical care is about access to highly skilled surgeons and leading-edge technology. And, it’s about timely, compassionate care close to home and your support system. When you choose Penn State Health for heart and vascular surgery, we’ll schedule your surgical consultation within five days. From advanced surgical treatment to emergency interventions to our growing team of expert heart and vascular surgeons, your heart is in the right place at Penn State Health.


STJ-19117-22-189275-0922
Call 610-378-2676 to schedule an appointment within five days.
heart and vascular surgeons, seeing you now in Berks.
Expert
Medical record
A Quarterly Publication
To provide news and opinion to support professional growth and personal connections within the Berks County Medical Society community.
Berks County Medical Society MEDICAL RECORD
Raymond C. Truex, Jr., MD, FACS, FAANS, Co-Editor
Lucy J. Cairns, MD, Co-Editor
Editorial Board
D. Michael Baxter, MD Shannon Marie Foster, MD, FACS
Jillian Ventuzelo, DO
T. J. Huckleberry, MPA
William Santoro, MD, FASAM, DABAM
Raymond C. Truex Jr., MD, FAANS, FACS

Contents
Features

Berks County Medical Society Officers
Jillian Ventuzelo, DO President
William Santoro, MD President Elect Kristen Sandel, MD Chair, Executive Council
Ankit Shah, MD Treasurer Jin Xu, MD Secretary Michael L. Haas, MD Immediate Past President T. J. Huckleberry, MPA Executive Director
Berks County Medical Society
Phone: 610.375.6555 | Fax: 610.375.6535 Email: info@berkscms.org www.berkscms.org
The opinions expressed in these pages are those of the individual authors and not necessarily those of the Berks County Medical Society. The ad material is for the information and consideration of the reader. It does not necessarily represent an endorsement or recommendation by the Berks County Medical Society.
Manuscripts offered for publication and other correspondence should be sent to 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501. The editorial board reserves the right to reject and/or alter submitted material before publication.
The Berks County Medical Record (ISSN #0736-7333) is published four times a year by the Berks County Medical Society, 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501. Subscription $50.00 per year. Periodicals postage paid at Reading, PA, and at additional mailing offices.
POSTMASTER: Please send address changes to the Berks County Medical Record, 2669 Shillington Rd, Sinking Spring, PA 19608, Ste 501.
14 The BCMS Pat Sharma President’s Scholarship – How to Become an Optimist 16 Determining Antibiotic Resistance in the Berks County Environmental and Clinical Settings 22 Efficacy of a Substance Abuse Program in a Regional Emergency Department 23 Reading Hospital/Tower Health Student Summer Research Projects
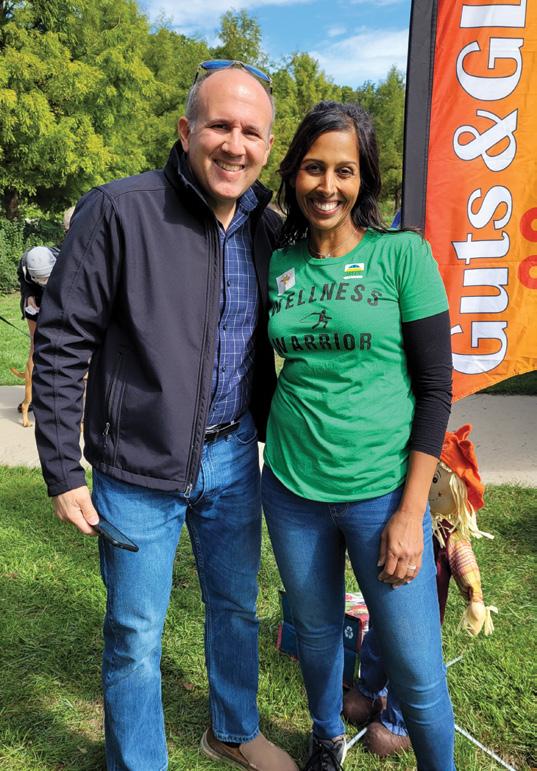
28 Street Medicine – Reborn in Berks 29 BCMS Night at the “Reading Fightin’ Phils” 30 A Night of Physician Storytelling 31 Polio. It’s happened again, right here in the US. 32 9th Annual Digestive Expo A Shining Success at a New Location 34 Reading Hospital Family Medicine Residency Program 50th Anniversary Celebration
Berks County Medical Society BECOME A MEMBER TODAY! Go to our website at www.berkscms.org and click on “Join Now”

Content Submission: Medical Record magazine welcomes recommendations for editorial content focusing on medical practice and management issues, and health and wellness topics that impact our community. However, we only accept articles from members of the Berks County Medical Society. Submissions can be photo(s), opinion piece or article. Typed manuscripts should be submitted as Word documents (8.5 x 11) and photos should be high resolution (300dpi at 100% size used in publication). Email your submission to info@berkscms.org for review by the Editorial Board. Thank YOU!
Hoffmann Publishing Group, Inc., 2669 Shillington Road, #438, Sinking Spring, PA 19608
www.Hoffpubs.com
For Advertising Information & Opportunities Contact: Alicia Lee 610-685-0914 x210 Alicia@Hoffpubs.com Sherry Bolinger 610-685-0914 x202 Sherry@Hoffpubs.com
FALL 2022
BERKS COUNTY MEDICAL SOCIETY
5 President’s Message 6 Compass Points 8 Editor’s Comments in every issue 10 Like Father, Like Son... and Daughter
Family is foundational, and having a perfect home for your family means everything. Having Peter Heim by your side to help you navigate through the multiple steps of buying or selling is key. Born and raised in Berks county, Peter is an award-winning Real Estate Broker with more than 35 years of experience.

A family man, Peter has been married to his wife Michele for more than 30 years. They have seven children and two grandchildren. Pete and his family are involved with many Berks County organizations.

This seasoned professional brings his hardworking yet fun personality to every interaction. Now Peter is proud to welcome his son Christopher onto his real estate team. Chris brings his unbridled enthusiasm, on-line savvy, and banking experience to the team. Let the Heim Team do the best job for you!
Peter specializes in customer service.
Whether listing or selling residential or commercial real estate, Peter is dedicated to helping his clients. His personal attention to every aspect of the business has garnered him more than 200 five-out-of-five Gold Star independent reviews.
“I have personally known Pete for close to two decades, and he is one of most conscientious, caring and outgoing people I know. He truly cares about his clients, and works harder than any other realtor I know. I highly recommend that you work with Pete.” – Dave R
“Pete is attentive to every detail. He made a hard journey of selling my mom’s house easier not just because he is a skilled realtor but in how much he cares about the story and people behind the sale.” – Cathleen P.
“Always a great experience working with Pete and now his son Chris as well.” – Michael S.
Peter K. Heim, CRS, GRI Associate-Broker



office: 610-898-1441 cell: 610-745-3378 email: pheim@kw.com www.peterheimrealtor.com



“Now more than ever HOME is important!”
Peter K. Heim, CRS, GRI
Christopher Heim







P resident ’ s M essage
Dear BCMS Member, Doctoberfest is almost here! Enjoy a night out with colleagues and their families at Saucony Creek Franklin Station Brewpub on Thursday, November 3! Reserve your spot today by emailing TJ at tjhuckleberry@berkscms.org FALL 2022 | 5
Jillian Ventuzelo, DO President
T.J. Huckleberry, MPA Executive Director

Parrots: A Political Problem

Hypothetical question? Let’s say in every observation room in your practice, a talking parrot has been placed in the corner. A regular parrot, with no formal medical education, of course. But these parrots are colorful and entertaining and their squawking appeals to most of your patients. And let’s say, hypothetically these talking parrots start to contradict your medical opinion to your patients. And let’s just say somehow, some of your patients start to really listen to these talking parrots. Moreover, these parrots are becoming increasingly louder and more distracting to you and your staff.
Clearly, these parrots are damaging the level of trust between you and your patients and undermining the integrity of your practice.
How would you react?
Well, you would try to get rid of the parrots, right?
So, you call the shopkeeper, and not only does he tell you that he will NOT remove them from your office but is planning to add MORE; and the only way you could get rid of these parrots is if you paid, per bird, to remove them.
So, the question is, how much of yourself are you willing to invest in order to save your practice and protect your patients from these outside influences?

One of the easiest and most tangible ways is through a PAMPAC donation.
No matter what your opinions of political action committees are, it is the game being played on the field. Until then, not supporting PAMPAC is essentially dumping truckloads of parrots into your practice and your colleagues’ practices. And I gotta tell ya…there are a lot of loud parrots coming out of the shoppe this year.

In all seriousness, there is a dire need for PAMPAC support this year. We need to strengthen and recruit more champions to our cause. Our general assembly hasn’t seen a physician elected to its ranks since 1960 and now more than ever we need to be heard. This could be the year that streak ends; Dr. Arvind Venkat, an Emergency Medicine physician from Alleghany County, is running for an open seat. Supporting candidates like him and others is how we maintain and build our influence at the Capitol.
So, no matter the party affiliation or district location, to have your voices heard over the din of political pandering, your action in our political system and your support for PAMPAC are essential.
If not you, then who?
6 | www.berkscms.org
c o MP ass P oints





FALL 2022 | 7
Our long-term perspective and counseled insight provide the confidence investors need in today’s challenging environment. As a registered investment advisor, our fiduciary responsibility is only to you and the best interests of your investments. Count on our qualified professionals for the trust, tenure and talent you can take
for the long term. If so, they may be suffering from TMJ Dysfunction and/or Sleep Disordered Breathing, such as snoring and obstructive sleep apnea. We offer comprehensive diagnosis and treatment. Our many years of experience have resulted in a high rate of successful outcomes. Our philosophy involves a conservative, non-surgical, non-pharmaceutical approach to management with an emphasis on multidisciplinary care. • Ear Pain without infection • Insomnia • Anxiety / Depression • Headache • Tinnitus Tammy Balatgek, DDS, MS Diplomate, American Board of Dental Sleep Medicine Diplomate, American Academy of Craniofacial Pain 2433 Morgantown Road (Route 10), Suite 200, Reading, PA 19607 www.TMJSleepCenter.com • 610.796.2835 Challenging Cases? We Can Help... SCAN & A P P LY TO AY #CAREERSINCARING #FINDYOURPURPOSE #MAKEADIFFERENCE WWW.APISMGT.ORG/CAREERS We Offer: Sign On Bonuses Competitive Pay Flexible Hours Great Benefits PT & FT Positions Join Our AwardWinning Team! We Have DailyPay Get Paid Everyday Apis Services, Inc. We support 32 highly successful businesses & non-profit organizations throughout the USA!
Integrity, Service, Performance. 610-376-7418 • connorsinvestor.com
Confidence
AN EDITOR’S SWAN SONG (SORT OF)
by Lucy J. Cairns, MD, Editor

Ireally really meant to work on this piece yesterday, but yesterday was the first dry day following passage of a cold front in mid-September, so I could not resist the call of the mountain … Hawk Mountain Sanctuary, that is. I am somewhat anxious each year, now that I am in my 70s, that this will be the year when the rocky uphill hike to the North Lookout starts to elicit complaints from knees or hips, or even end in a spill involving an ignominious return trip via improvised stretcher. Not this year!!! Just a trickle of birds went by the lookout during the hour I spent with binoculars glued to my face, but it was enough to raise the thrill I always feel when witnessing the natural phenomenon that marks a major transition in the lives of a multitude of birds as the seasons change once more and the passage of time becomes visible to us all.

The onset of autumn provokes reflection on how far we have come, and how far we still have to go. For the Medical Record, this autumn edition marks the transition from my decade of editorship to a period in which I will play a lesser role. I am delighted to announce that, as of the winter edition, Dr. Mike Baxter will assume the editorial mantle. Considering Mike’s longtime work for the magazine on the editorial board, and the many articles and editorials he has written over the years, I’d say

8 | www.berkscms.org e dito R ’ s c o MM ents
that he’s had the mantle in his closet for some time already! The future of the Medical Record looks bright under Mike’s leadership, but there is no denying that both Mike and myself are part of the ‘old guard’ of the BCMS. New voices on the editorial board are vital to our mission of reflecting the interests of the entire BCMS membership. Any member with an interest in joining the Record editorial board – or in contributing an occasional article –is encouraged to contact one of us or TJ Huckleberry.
In 2012, the year I took over as editor from Dr. Chuck Barbera, Dr. Bill Finneran was sworn in as the BCMS President. The challenges facing Pennsylvania physicians that year included the introduction of the ‘Meaningful Use’ initiative by CMS and drastic cuts by Gov. Tom Corbett’s administration to financial support for Medical Assistance, medical education, Maternal and Child Health, and hospital programs including OB, Neonatal Services, Burn Centers, Critical Access Hospitals, Trauma Centers, and Uncompensated Care. On the flip side, a major improvement in access to health care in Berks County was achieved with the June opening of the first office of the Berks Community Health Center, a Federally Qualified Health Center to care for patients regardless of ability to pay. Dr. Mike Baxter was the BCMS champion on this issue, working to improve access to care for our underserved community members for many years leading up to this great event.
I don’t have to tell you that in 2022 physicians in Berks County, the State of Pennsylvania, and around the country continue to face threats to their ability to provide the care they know their patients need and deserve. The forces attempting to control medical practice are powerful and cannot be fought one-on-one. Supporting organized medicine, including your county and state societies, is the only option to ensure you have a place ‘at the table’ rather than ‘on the table.’ In terms of public policy that adversely affects medical practice, state legislatures are the principal offenders. It is this fact that makes state medical societies so important to the profession, especially the only organization that combines the voices of physicians in all the specialties – PAMED.
The Berks County Medical Society has produced many leaders who have taken on influential roles with PAMED. The best recent example is the present PAMED Vice President, Dr. Kristen Sandel. Kristen was active in the BCMS during her entire tenure in Berks County, most recently serving as Chair of the Executive Council. The role of county societies is unique, since local concerns take priority for these groups. Being a member of your county society provides opportunities to work with like-minded
Pick Something Extraordinary!
Lisa Tiger is that rare combination of passion for her business, sales skill, marketing professional and unwavering care for her clients.

The ultimate professional, Lisa is the Top Producing Century 21 Agent in the State of PA, consistently ranked in the Top 100 in the US., but proudest of her premier ranking in Berks County. Lisa cares about the communities she serves, and it shows in her commitment to others.

In these challenging times, Lisa never waivers in her objective to help her clients reach their objective. It is always about YOU.
When you are ready to buy or sell, Team up with the Tiger!
Gold

Direct: 610-207-6186 Office: 610-779-2500 LisaTigerHomes.com
colleagues on issues affecting the physicians you work with and creates a valuable resource for community leaders trying to address public health issues. In recent years, this phenomenon is illustrated by the BCMS’s pivotal role in the creation of the Opioid Task Force in 2016 and the local response to the COVID-19 pandemic, including the Berks County Government COVID-19 Health Advisory Panel in July 2020.
During my time as editor, the Medical Record has documented a string of achievements on the part of BCMS members and has explored a wide variety of issues affecting our profession. We have indeed come a long way, but like the birds now on the wing we still have a long journey ahead of us. To our present BCMS members: thank you for your support! To any current non-members, I encourage you to join forces with us so we can all soar a little further and faster.
FALL 2022 | 9
Extraordinary Homes Deserve Extraordinary Attention
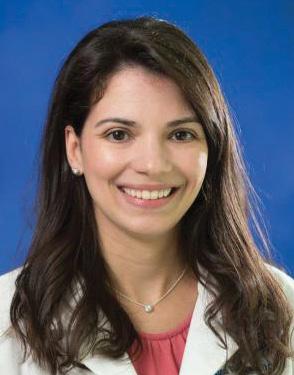
Like Father, Like Son… and Daughter
 by D. Michael Baxter, MD
by D. Michael Baxter, MD
How would you like to work for your father or at least be his partner? That is the choice that presented to our Berks County physicians featured in this Fall edition of the Medical Record. Laila Muallem, MD, and Greg Emkey, MD, finished their residencies in Obstetrics and Gynecology and Rheumatology, respectively, and had many options for their future medical practices. Both chose to come home and join their fathers providing care to the patients of Berks County. Many young physicians have followed parents into the practice of medicine; however, few go the next step and become partners in their parent’s private practice. This article also recognizes those parent physicians, Ron Emkey, MD, for his 50th year of practice in Berks County, and Nabil Muallem, MD, for his 35 years of caring for the women of Berks County.
Ron Emkey grew up in the small Northeastern PA town of Nanticoke where a local physician inspired his interest in medicine. He graduated from Dickinson College and Hahnemann Medical College followed by a tour of duty with a B-52 squadron in the US Air Force. He returned to Hahnemann and then the University of Pennsylvania to complete his residency in Internal Medicine. The Chief of Rheumatology at Penn encouraged him to pursue a Rheumatology Fellowship which he did at Harvard University/ Massachusetts General Hospital. Ron had already developed a strong interest in research early in his career and was encouraged to stay at Harvard after completing his Fellowship. However, he also had a very strong interest in direct patient care. As he explored his post Fellowship practice opportunities on a trip to Pennsylvania, he learned about a Rheumatology opportunity through Reading Hospital and was impressed by the reputation of the then-Chair of Internal Medicine, Pat Hildreth, MD. A visit to Reading convinced him that this was the opportunity for both patient care and research that he desired and 50 years later he remains committed to both of those objectives.

10 | www.berkscms.org M edical R eco R d c ove R s to R y
Ron is well known locally for his excellent patient care and his research interests; however, he is also recognized internationally for his pioneering research work particularly in the area of osteoporosis and bone density. When Merck introduced the bisphosphonate alendronate in 1995 at a medical conference in San Francisco, Ron was there with the research team. He continues to pursue his academic interests in research and teaching as well as treating thousands of local patients. He remains a great asset as well to his many admiring colleagues near and far, who continue to seek his advice.
Perhaps it is not surprising that Greg Emkey followed his father into medicine as he says, “growing up in a medical family,” he always wanted to be a doctor. One of seven children, Greg deeply appreciates his father and his mother, Judy, for their parental skills as well as professional attributes. A graduate of Swarthmore College, where he was an All-American tennis player, Greg then completed his medical school training at the Penn State College of Medicine followed by his Internal Medicine residency at Beth Israel Hospital. Although he completed a two-year research externship in Orthopedic Surgery, he ultimately was drawn to the field of Rheumatology and followed in his father’s footsteps by completing his Fellowship at the Harvard/Massachusetts General Hospital program. As his Fellowship neared its completion, like his father again, he was offered the opportunity to stay on at Harvard for a career in research; however, he too was committed to the direct care of patients. As he looked at opportunities to combine both his research and patient care interests, it became obvious that no practice offered more opportunity than back home with his father in Berks County. It is one of those classic Berks County stories that when
Great care for your patient starts with a strong team.

Adam J. Altman, MD
Angela Au Barbera, MD
Helga S. Barrett, OD
Jennifer H. Cho, OD, FAAO
Christine Gieringer, OD
David S. Goldberg, MD, FAAP
Marion J. Haligowski III, OD
Dawn Hornberger, OD, MS
Y. Katherine Hu, MD, MS
Lucinda A. Kauffman, OD
Christina M. Lippe, MD
Barry C. Malloy, MD
Michael A. Malstrom, MD
Mehul H. Nagarsheth, MD
Abhishek K. Nemani, MD
Tapan P. Patel, MD, PhD
Jonathan D. Primack, MD
Kevin J. Shah, MD
Michael Smith, MD
Anastasia Traband, MD
Monica Wang, OD
Denis Wenders, OD
Linda A. Whitaker, OD, MS
With 20+
Pennsylvania is the leading eye care practice in the region. Our doctors are always available for consults and referrals on eye issues, and our entire practice is committed to cooperative management of your patient. That means that we communicate and consult 360°. We share information, and we provide direct cell numbers to our partner physicians. And ultimately, it means better care and outcomes for your patients.
For consultations and referrals, call 610-378-1344.
Greg subsequently applied for privileges at Reading Hospital, the Chief Medical Officer who interviewed him was the same doctor who delivered him almost 30 years before, Gerald Malick, MD, eminent Berks County Obstetrician Gynecologist.
Ron and Greg have continued to combine research with their busy medical practice at
the Emkey Arthritis and Osteoporosis Clinic in Spring Ridge, Wyomissing. They both note that being in practice together may not be for everyone and the likelihood of success rests largely on the “pre-practice” relationship that exists for years before any professional relationship begins. There can be some “ego” issues when a patient prefers one Emkey
FALL 2022 | 11
Offices in Wyomissing, Pottsville, Pottstown, Lebanon and Blandon
EyeConsultantsOfPA.com
Adult Strabismus | Cataract Surgery & Intraocular Lenses | Comprehensive Ophthalmology & Optometry | Contact Lenses Cornea and External Diseases | Cosmetic & Reconstructive Eyelid Surgery | Cosmetic Botox‑Latisse | Diabetic Eye Care Glaucoma | Laser Vision Correction (Including Bladeless LASIK) | Low Vision | Macular Degeneration | Neuro Ophthalmology Oculoplastics | Orthoptic Therapy | Pediatric Ophthalmology & Optometry | Vitreo – Retinal Surgery
eye care specialists, Eye Consultants of
continued on next page >
Like Father, Like Son... And Daughter
over the other (Greg says he long ago accepted the fact that to many he will always be “the second-best rheumatology Emkey doctor” in Berks County) but in general the benefits far outweigh any drawbacks. Greg greatly admires his father and finds it an amazing opportunity to practice with and learn from him. Greg emphasizes that he thinks his father’s generation is better clinicians than his; but on the other hand, Ron recognizes unique skills that Greg and his generation have acquired. The two readily share “second opinions” with each other and deeply respect one another’s knowledge and abilities. Together they have written articles and co-authored book chapters on Vitamin D effects and Calcium metabolism. In addition, Ron feels that the opportunity to share this experience with his son has extended his own “practice-life” affording him the energy and desire to continue to do what he loves – care for patients and develop new knowledge and treatments to improve that care.
Anyone familiar with Nabil Muallem, MD, knows that he frequently has a broad smile on his face and that smile has grown even bigger since his daughter Laila joined his Obstetrics and Gynecology practice in Wyomissing this past year. Nabil was born in Nazareth, Galilee, the son of a priest in the Eastern Rite Catholic Church. His father encouraged him to pursue his education in the U.S. and he graduated from Allentown College of St. Francis de Sales. He completed his medical degree at the University of St. Tomas School of Medicine in the Philippines and came to Reading at the recommendation of his good friend, the legendary Dick Caron, founder of the Caron Foundation, who was a trustee at the Allentown College of St. Francis de Sales. Nabil completed his OB/GYN Residency at Reading Hospital in 1987 and initially joined Alex Massengale, MD, before starting his own practice, Nabil S. Muallem, MD, PC, in Wyomissing two years later. Since then, he has delivered and cared for thousands of women in Berks County and been recognized as an outstanding teacher of both OB/GYN and Family Medicine residents at Reading Hospital.
Laila completed an accelerated six-year undergraduate/ medical school curriculum at Penn State University and the Sidney Kimmel Medical College of Thomas Jefferson University. She considered a variety of medical careers
12 | www.berkscms.org
continued from page 11
but following a medical student rotation with the OB/GYN Department at Reading Hospital she decided her father’s choice was also hers. She finished her OB/GYN residency at Penn State Health Hershey Medical Center and considered her options. It became clear that joining her father back home in Wyomissing was an ideal choice.



Laila grew up in a very academic as well as medical family. Her mother Najla is a PhD economist and her brother Samer is a cardiology fellow at the Milton S. Hershey Medical Center. Laila has always seen her father as a great role model and appreciates that in many ways he is “old school” with skills no longer taught in medical school. On the other hand, Nabil appreciates Laila’s newer surgical skills, e.g., robotics and advanced level laparoscopy, as well as her strict adherence to principles of evidence-based medicine. Both of them bring different perspectives to complement each other and ensure the best care is delivered to their patients. Nabil also appreciates how easily his daughter has been accepted and trusted by even his longstanding patients as well as his younger ones, many who he delivered as babies.
The recently married Laila has learned from her overworked father (20 years in solo OB/GYN practice prior to Heidi Strieb, DO, joining him 13 years ago) the importance of keeping a balance in one’s medical life. And of course, joining her father as an additional trusted colleague has given Nabil some additional “free time” as well.
One opinion that both the Emkeys and the Muallems clearly share is the value that a lifelong relationship of trust and deep respect brings to any partnership. Practicing medicine with your parent can have a few challenges; however, the opportunity to share a professional as well as a personal familial bond is a reward that few are able to experience. These two families represent the very best of how such a relationship can enhance one’s life and patient care.






Congratulations to these outstanding clinicians and honored colleagues especially as they celebrate 50 and 35 years of care to the patients of our community.

FALL 2022 | 13 continued on next page 301 S 7th Ave Suite 145, West Reading, PA 19611 610-376-6542 Managing your medications has never been easier. Your medications come
dose you
tear
package off
roll and your pills are there. That’s all there is to it. an m b Just add Just water. Organized by date and time Securely sealed Clearly labeled Easy to open Ideal for travel and everyday NO EXTRA CHARGE FOR THIS SERVICE! FREE DELIVERY (10 MILE RADIUS)
organized by date and time, securely sealed in individual easy-open packages. So when it’s time to take your next
just
the
the
The BCMS Pat Sharma President’s Scholarship

How to Become an Optimist
Reasons to feel pessimistic about the future bombard us on a daily basis, so when I discover an antidote to gloom I hold on with both hands and stay with it! Such an antidote can be found in the BCMS summer student research program, the Pat Sharma President’s Scholarship. The stated purpose of this 6-week paid internship, now in its ninth year, is to encourage bright young people with a connection to our community to pursue careers in health care. With luck, some of them will return to our area and contribute to our own wellbeing, so this project is not entirely altruistic!
In this edition of the Medical Record, we are proud to publish the research reports written by the 2022 Pat Sharma President’s Scholarship recipients: Kirill Popovich and Safitaj Sindhar. Kirill is currently in his third year as a pre-med student at UNC Chapel Hill. Born in Moldova, Kirill holds dual US/ Moldovan citizenship and in April this year he was moved to participate in a mission trip to a Ukrainian refugee camp. His captivating description of that trip was published in the summer Medical Record. Safi Sindhar is a pre-med student on track to graduate from Penn State Berks in December. She was born and raised in rural India, where access to medical care is difficult and


where Safi and her family did not always receive competent care. These early experiences have set Safi on a path to improve access to quality healthcare for underserved communities in India and around the world. When our 2021 interns, Jasmine Slusser and Layla Abousaab, invited me to a catch-up lunch this summer I invited Safi to join us because her interests closely mesh with those of Jasmine and Layla. After two hours of wide-ranging conversation, I believe the three of them will stay in touch for years to come.
In other good news, after a 2-year hiatus due to the pandemic, the Reading Hospital revived the summer student internship we had been privileged to coordinate with in the past, and our relationship has been reestablished. Therefore, we are delighted to once again publish abstracts submitted by the hospital student interns – showcasing research projects in the participating hospital departments. The BCMS is thankful to Mr. Francisco Hernandez, System Director GME in the Reading Hospital/Tower Health Academic Affairs office, for his aid in reviving the association between the two summer programs.

M edical R eco R d F eatu R e
14 | www.berkscms.org
The BCMS Pat Sharma
President’s Scholarship
The bright, hardworking, and compassionate young people I have had the privilege of working with as the coordinator of this BCMS program always lift my spirits and give me hope for the future. I’m sure that all the other physicians (and community leaders) who help to make this program a success by spending time mentoring and/or allowing clinical shadowing reap the same rewards that I do. There are too many such helpers to thank them all here individually, but each played a vital role. This year, special thanks are due to Safi’s main project mentor, Dr. Deb Powell, and Kirill’s project mentor, Dr. Adam Sigal. Dr. Daniel Edwards (Center for Urologic Care of Berks County) provided invaluable assistance by coordinating the clinical shadowing experiences from which Kirill and Safi gained immense benefit.
This program would not exist if not for the generosity of BCMS member Pat Sharma, MD, who in 2018 endowed the BCMS Educational Trust with a fund to support the student stipend and other educational programs. From the program’s inception in 2014 through the summer of 2018, we were able to accept a single student, but for the past few years we have been able to bring on a second student thanks to gifts from Ray Truex, MD. The Trust’s only source of additional funds is the generosity of members like Pat and Ray, who see great value in extending a helping hand to the next generation of physicians. Please consider joining them in their philanthropy by contacting our Executive Director, Mr. T.J. Huckleberry, about making a contribution to the Educational Trust. Practice optimism and you will be rewarded!




FALL 2022 | 15
Michael J. Dinan, CFP® michael.dinan@domaniwealth.com Thomas K. Williams CFP®, CPA tom.williams@domaniwealth.com
Wealth, LLC (“Domani”) is an SEC registered investment adviser with its principal place of business in Lancaster, Pennsylvania. Domani and its representatives may only transact business in states where they are appropriately notice-filed and registered, respectively, or exempt from such requirements. For information pertaining to the registration status of Domani,
SEC
state securities regulators for those states in which Domani maintains a notice-filing. Wyomissing Office | 610.927.4685 domaniwealth.com Assurance in the Face of Change. Find it with a Domani Wealth Advisor.
Domani
please contact the
or the
Determining Antibiotic Resistance in the Berks County Environmental and Clinical Settings
by Safitaj Sindhar, BCMS Pat Sharma President’s Scholarship Recipient
Infectious Diseases,
This article has been shortened for publication in hard-copy form. The complete version, including the list of references, can be found in the digital publication available at www.berkscms.org/medical-record
INTRODUCTION
Antibiotic resistance (AR) refers to a phenomenon where pathogens, such as bacteria, become resistant to the effects of drugs and chemicals due to repeated exposure (Antibiotic Resistance, 2020). AR occurs as a natural process in which traits that improve survival, such as resistance to antibiotics, are selected for over time. Bacteria gain resistance through beneficial mutations, and/ or the incorporation of resistant genes in their genomes (Martinez & Baquero, 2000). The overuse of antibiotics in clinical and agricultural settings accelerates this natural process of AR in bacteria (Antibiotic Resistance, 2020).
IMPLICATIONS OF ANTIBIOTIC RESISTANCE
Frieri et al., 2017 found that liberal and unnecessary use of broad-spectrum antibiotics results in AR and is associated with high morbidity and mortality. When early detection of causative bacteria is lacking, infection control practices are poor, and/or the treatment regimen is left incomplete, AR in bacteria accelerates. This might be because antibiotic-resistant genes (ARG) of the pathogens are present in a reservoir called the resistome, from where pathogenic bacteria can acquire resistance via horizontal gene transfer (HGT) (Frieri et al., 2017).
In their 2016 study, Friedman et al. discussed that infections caused by antibiotic-resistant bacteria (ARB) have around a two-fold higher rate of adverse outcomes, both clinical and economic. Clinical adverse outcomes include complications, treatment failure, or death, and economic adverse outcomes include increased costs of care and longer stays in hospitals. The authors also discussed that primary reasons for treatment failure linked with infections caused by ARB include delayed treatment, lack of effective therapy, bacterial fitness, and more severe illness (Friedman et al., 2016).
PATHOGENS THAT BECOME RESISTANT
Although many pathogens can become resistant to the effects of antibiotics, certain bacteria cause human disease much more commonly than others in the environment and clinical settings. These include Escherichia coli (E. coli), Enterococci species, and Staphylococcus aureus (S. aureus). A discussion of resistance in these bacteria can be found in the digital (full) version of this article.
ANTIBIOTICS TO WHICH PATHOGENS BECOME RESISTANT
In recent years, many pathogens have become resistant to the effects of drugs such as penicillin, tetracycline, and nitrofurantoin. The project focuses primarily on these antibiotics, which are discussed in detail in the digital (full) version of this article.
MY BENCH RESEARCH IN A MICROBIOLOGY LAB AT PSU
I. Background
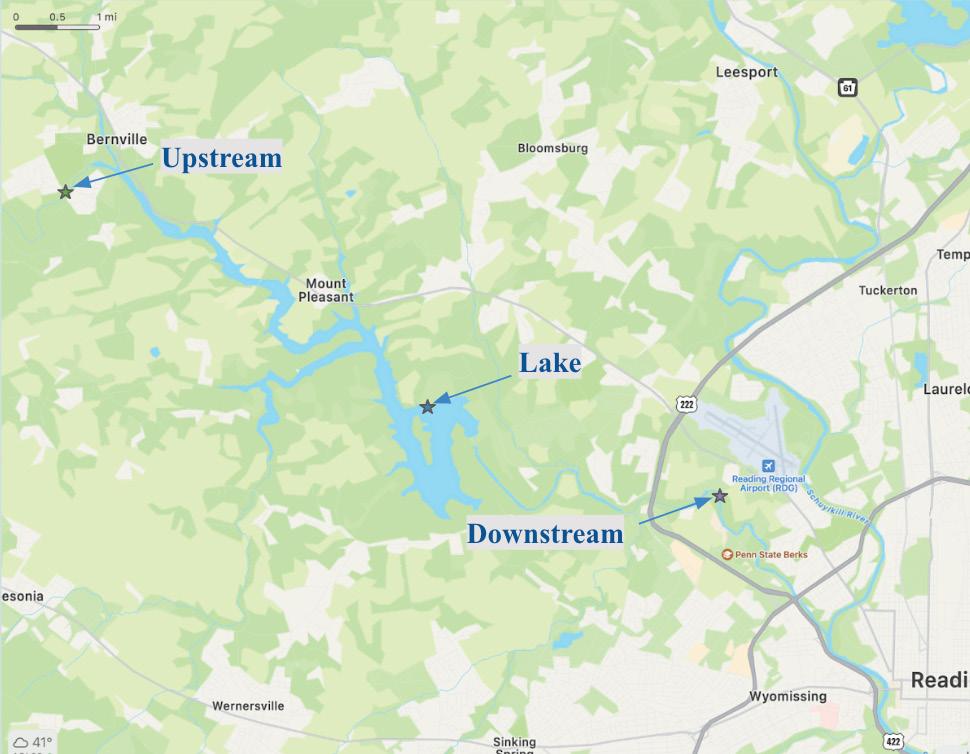
In my three years of study at Pennsylvania State University (PSU), Berks Campus, I have been engaged in a laboratory study with Dr. Tami Mysliwiec and Prof. Jill Felker. The study focuses on the presence of antibiotic resistance in bacteria found in the Blue Marsh Lake Watershed. Three sampling locations were chosen throughout the watershed. The first, henceforth called the ‘upstream’ site, is in close proximity to an agricultural area and therefore receives agricultural runoff. Next, the Blue Marsh Lake (‘lake’) is the recipient of pollutants from the human population that uses the area for recreational purposes. Finally, the ‘downstream’ site is surrounded by businesses and prone to industrial discharge. Figure 5 depicts the location of the sites relative to one another in Berks County, PA, and Figures 6-8 show images of individual sample sites.
16 | www.berkscms.org
Preceptors: Debra L. Powell, MD, Chief, Division of
Reading Hospital; Tami Mysliwiec, Ph.D., Associate Professor of Biology, Penn State Berks; Jill Felker, M.S., Lecturer in Chemistry, Penn State Berks; Lucy J. Cains, MD, Berks County Medical Society
The BCMS Pat Sharma
President’s Scholarship
Figure 5: The location of the upstream, lake, and downstream sites relative to one another.
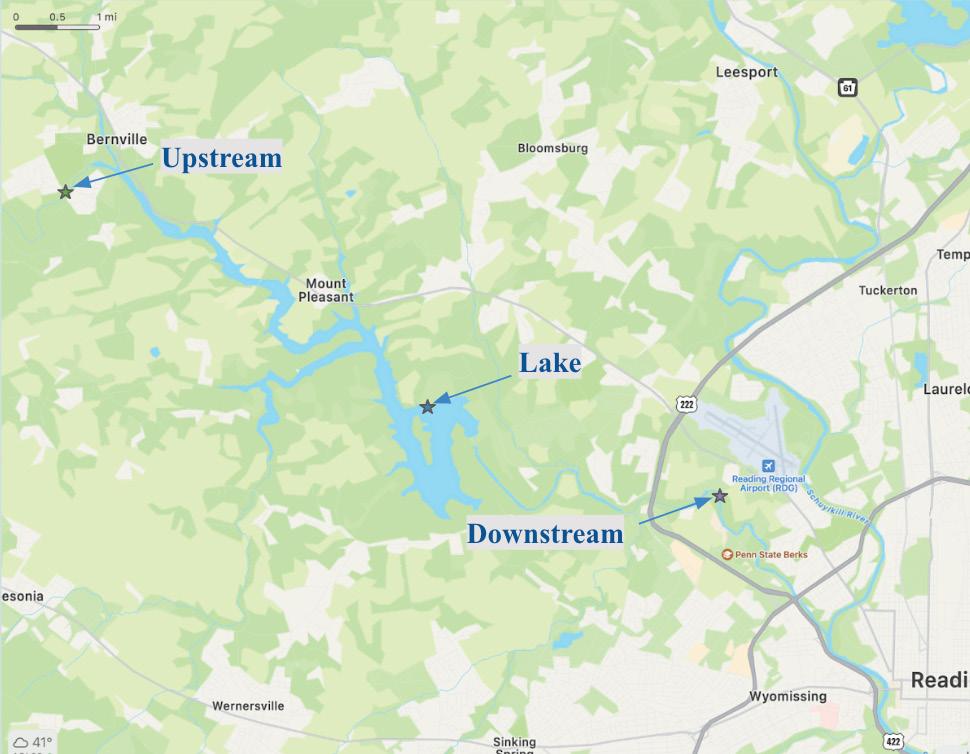
Figure 7: The lake site that is used for recreational purposes (40.384559, -76.042395). Because humans use this site for boating, swimming, or fishing, many contaminants (chemicals, metals, and plastics) can be found here.


Figure 6: The upstream site that is close to the agricultural region (40.422280, -76.124502). Because of its proximity to farmland, the area receives many pollutants from the agricultural runoff including fertilizers, organic matter, and nutrients. continued on next page >
Figure 8: The site that is downstream from the industrial region (40.369511, -75.975224). The chemical and industrial waste from the hospitals and factories near this region often ends up at this site.

FALL 2022 | 17
HOPE TODAY THERE’S Hoy hay esperanza para un tratamiento a bajo costo y accesible que salve vidas To order a Narcan® kit, find treatment, and learn more, visit cocaberks.org/HOPE Para pedir un kit Narcan®, buscar tratamiento y obtener más información, visite cocaberks .org/HOPE Paid for with PA taxpayer dollars
Determining Antibiotic Resistance in the Berks County Environmental and Clinical Settings
II. Methodology
Every month, water and sediment samples were collected for chemical and microbiological testing. Sampling and testing followed EPA-established protocols for recreational water. Escherichia coli and Enterococci spp. counts were collected using membrane filtration procedures, following the manufacturer’s recommendations. Kirby Bauer disk diffusion methodology was used to determine the antibiotic susceptibility to six classes of antibiotics in approximately 10% of the isolated colonies from collected samples. Genomic DNA was isolated from sediment samples. Total gDNA was analyzed for antibiotic-resistant genes using PCR analysis. qPCR was employed to quantitate antibiotic-resistance genes in the microbiome of the sediment samples.
III. Results
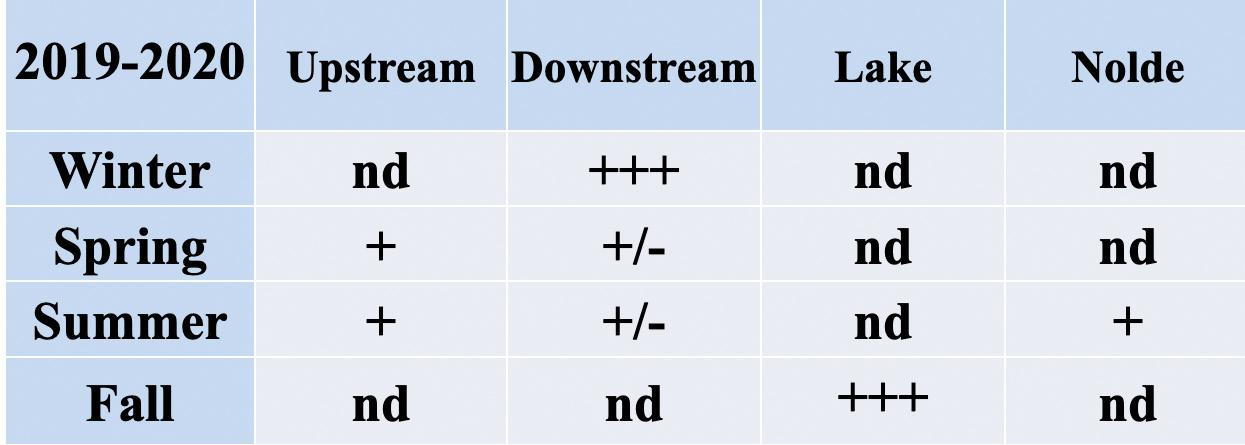
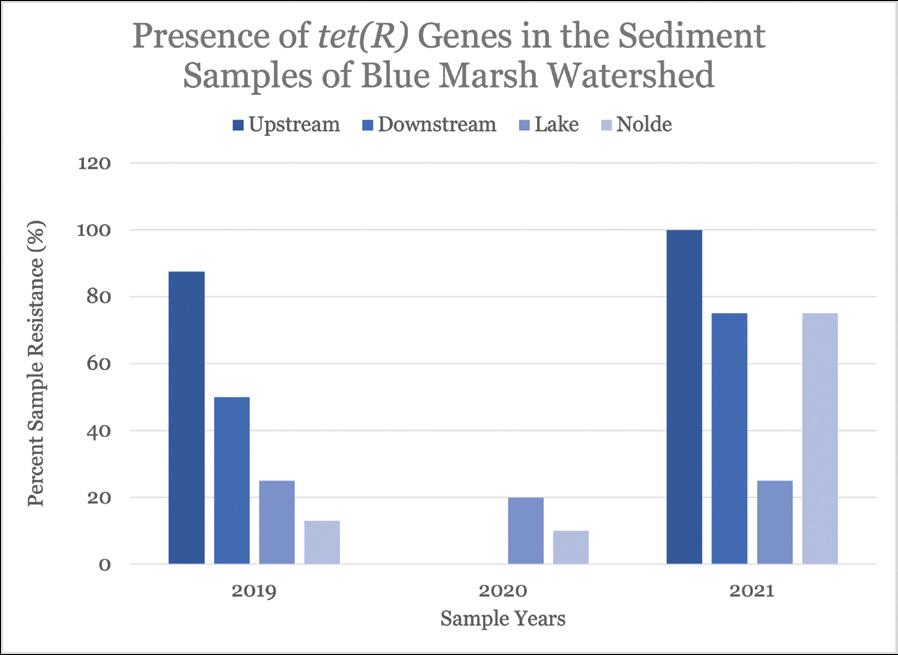
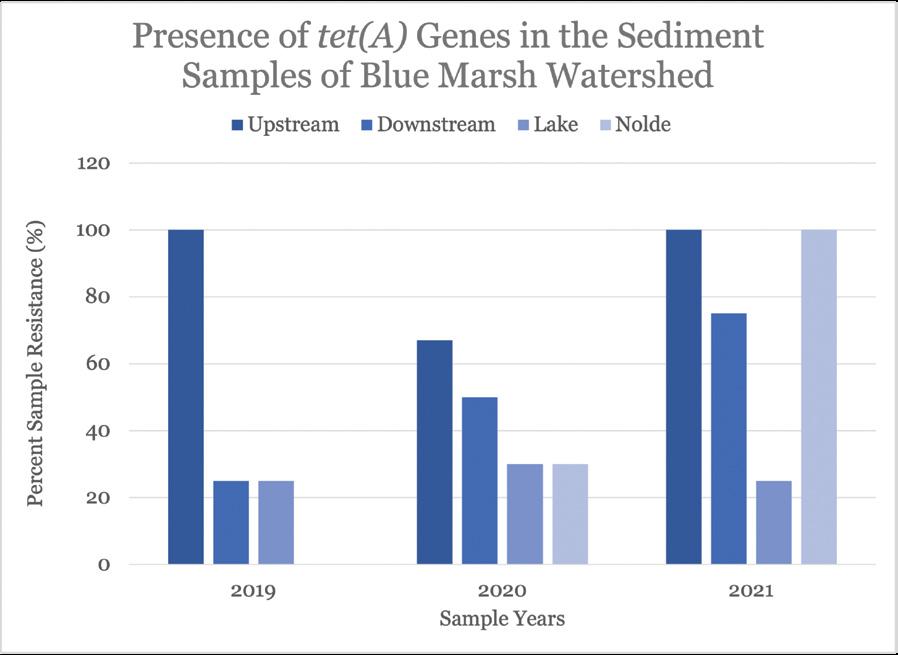
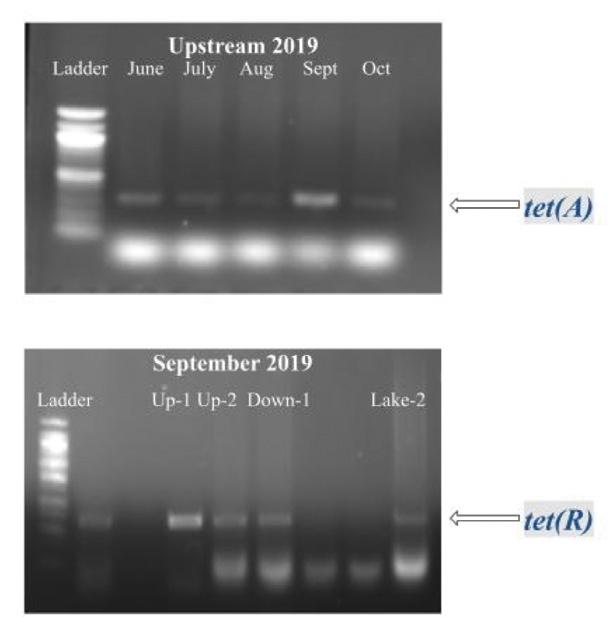
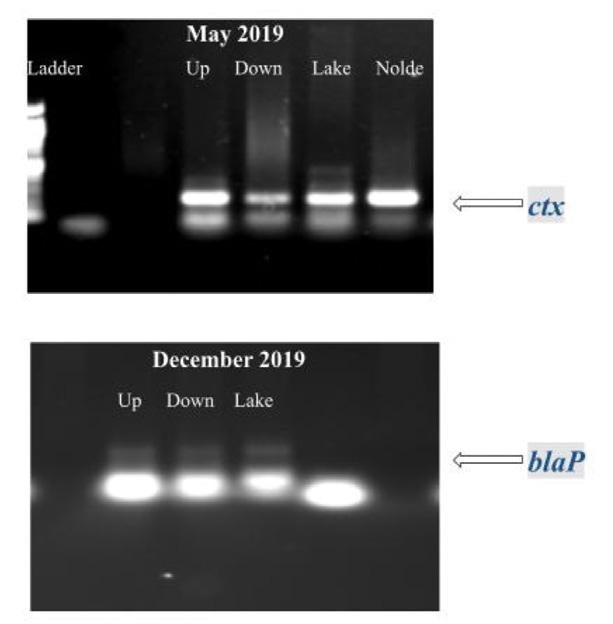
Figure 9. PCR amplification and gel electrophoresis of genomic DNA from sediment samples detected tetracycline-resistant genes. In the gDNA, the primers specific to the tet(A) gene identified a 405 bp fragment, and the tet(R) gene identified a 379 bp fragment.
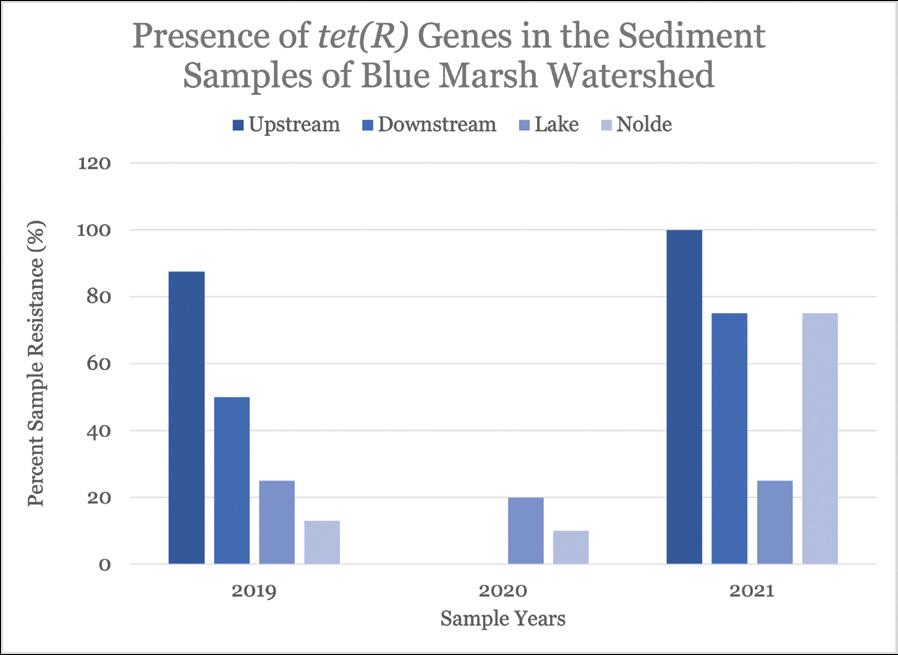
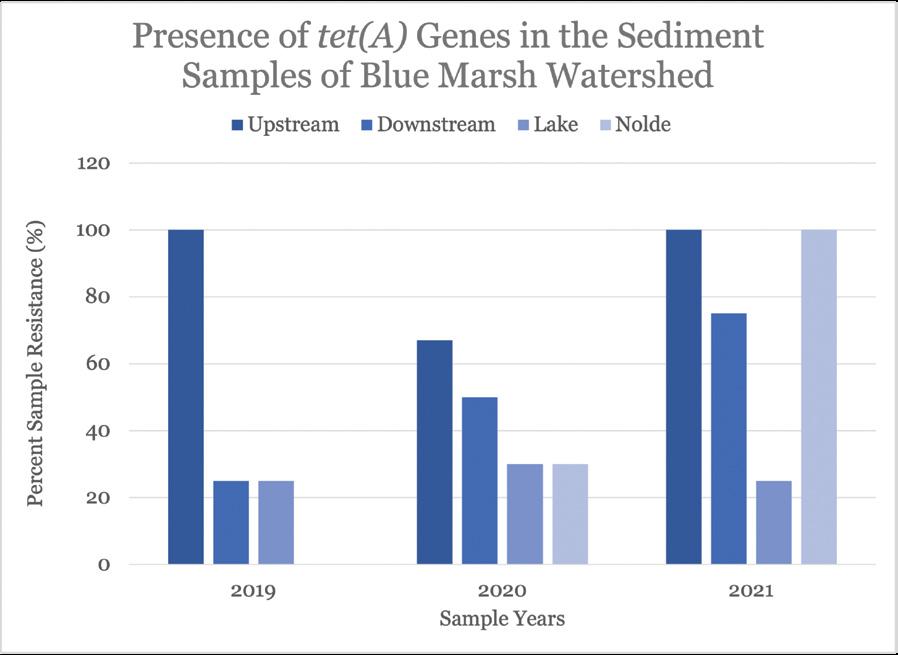
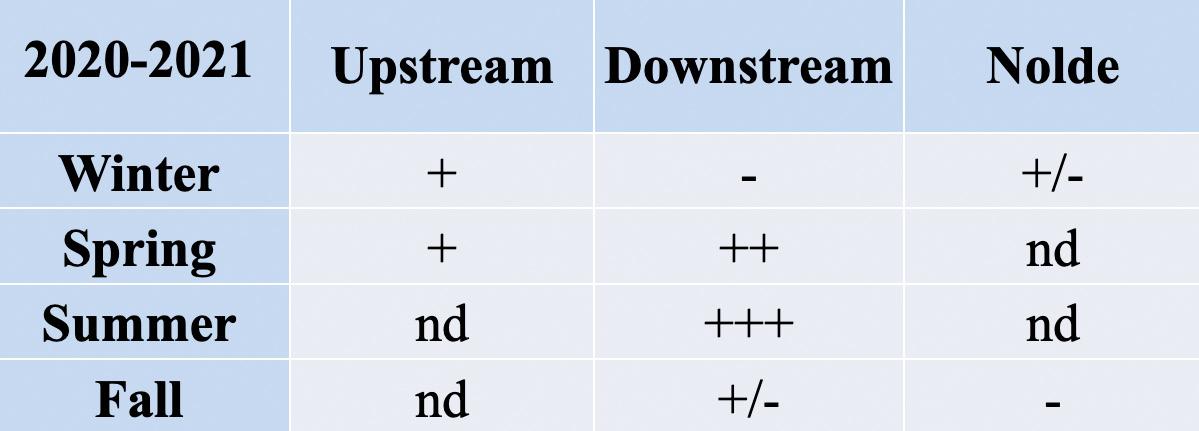
Figure 11. Quantification of the detection and prevalence of antibiotic-resistance gene tet(A) in the samples analyzed.
Figure 10. PCR amplification and gel electrophoresis of genomic DNA from sediment samples detected ampicillin-resistant genes. In the gDNA, the primers specific to the ctx gene identified an approximately 200 bp fragment, and the blaP gene identified an approximately 300 bp fragment.
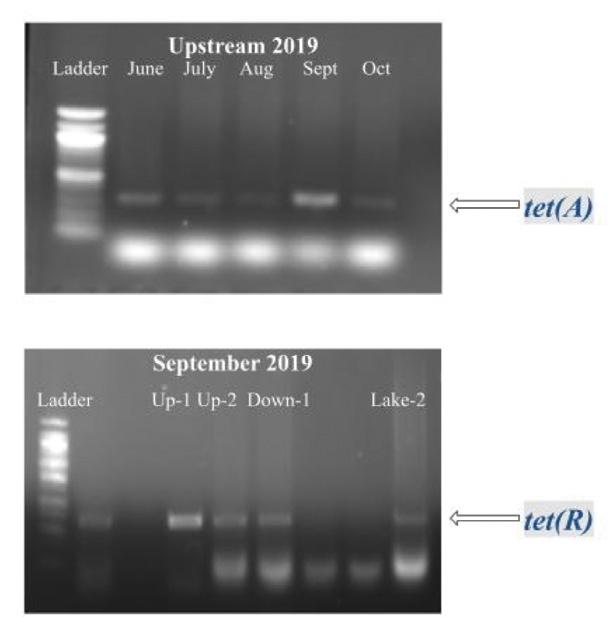
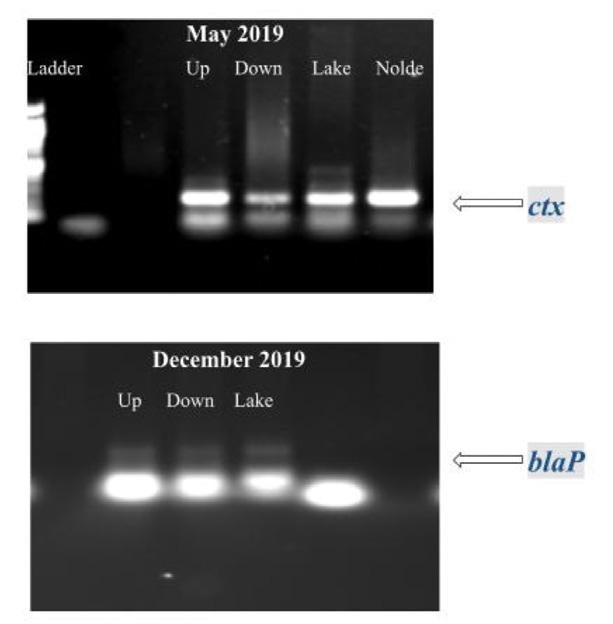
Figure 12. Quantification of the detection and prevalence of antibiotic-resistance gene tet(R) in the samples analyzed.
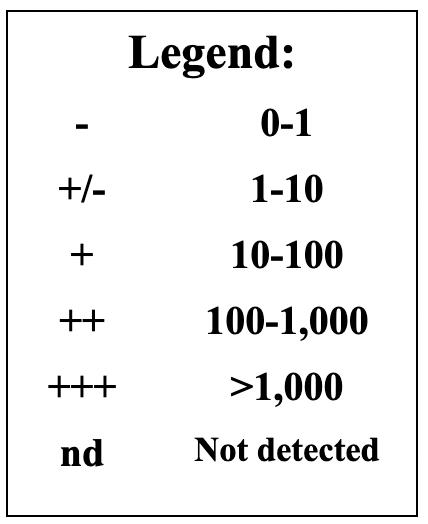
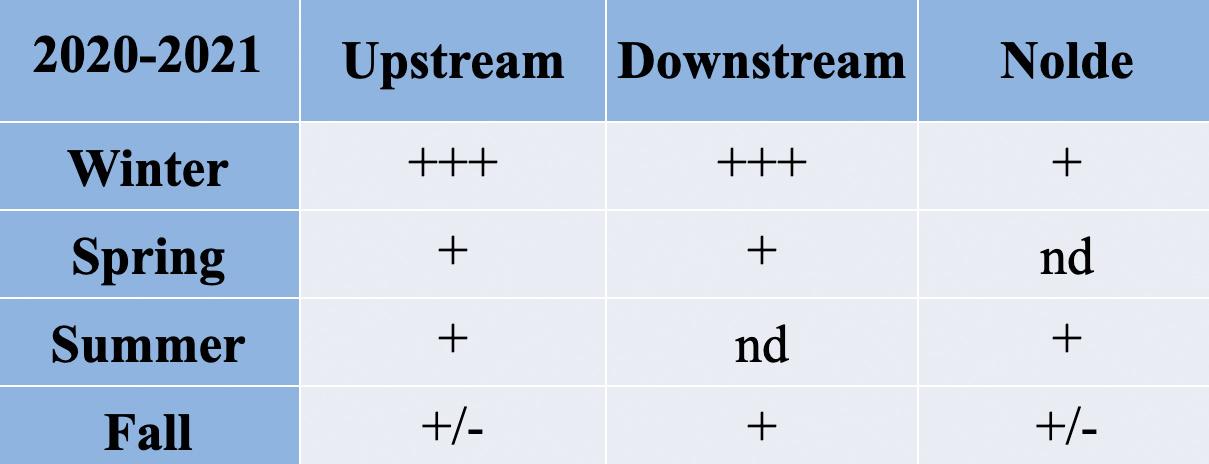
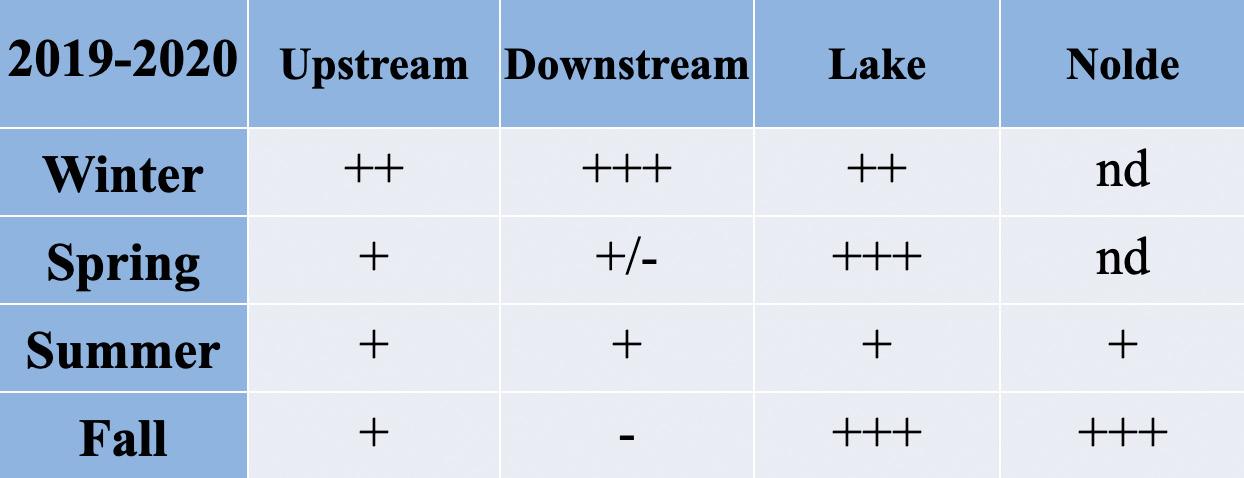
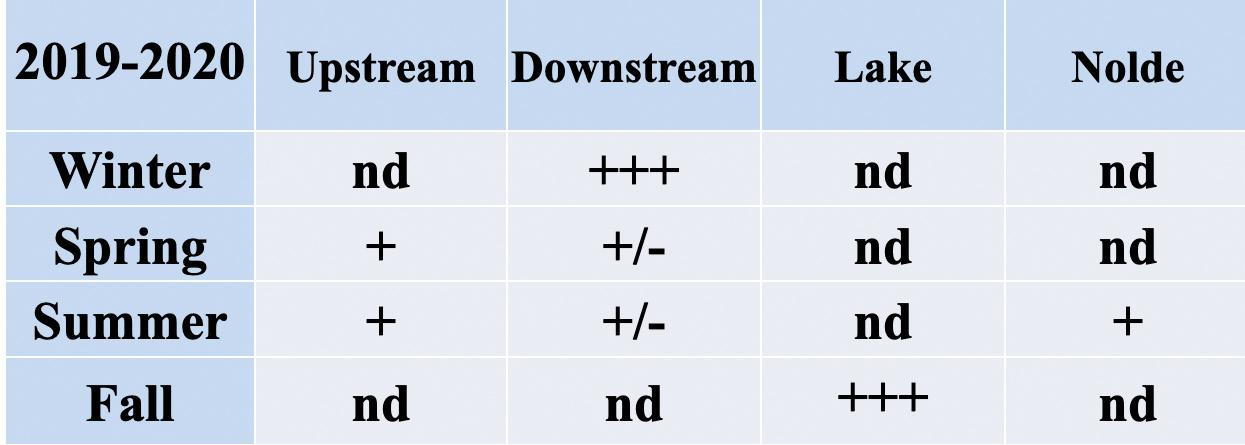
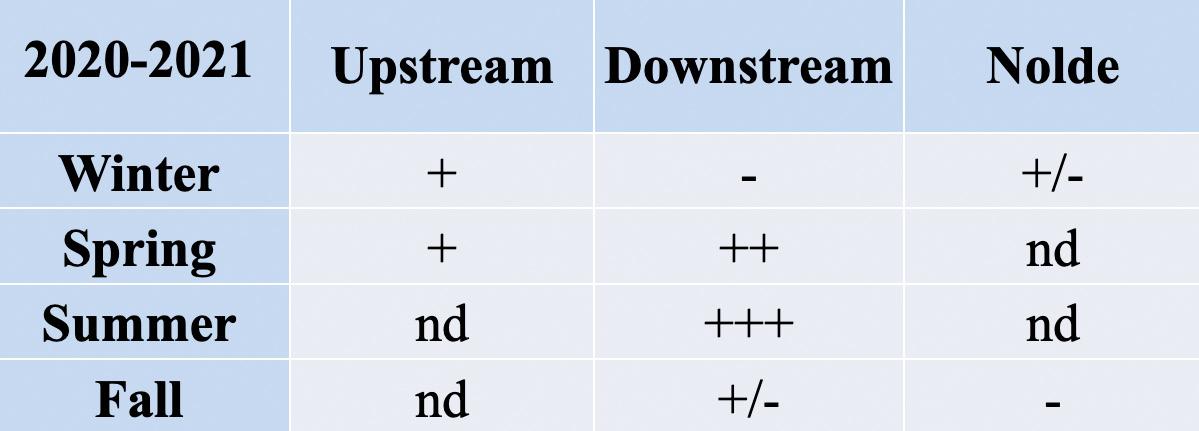
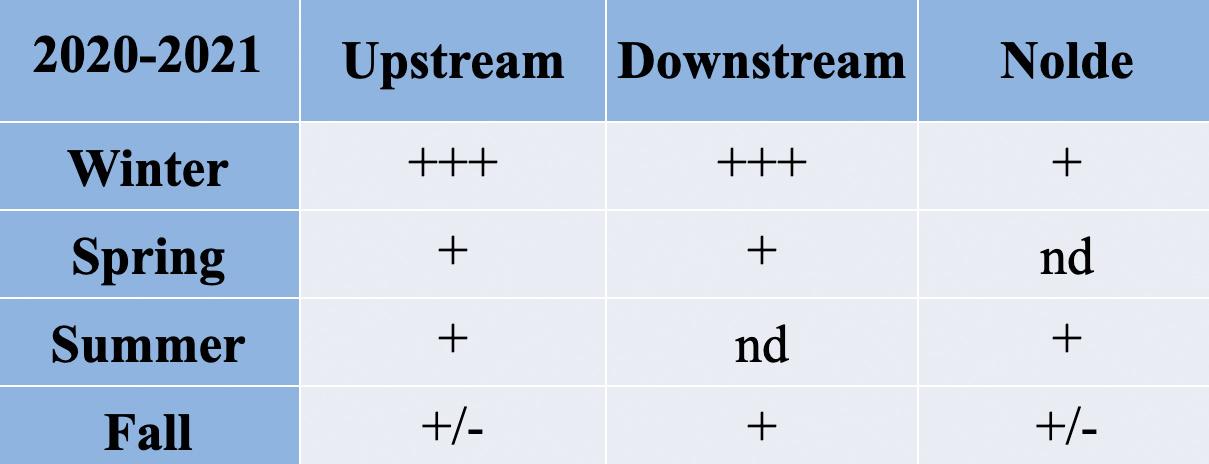
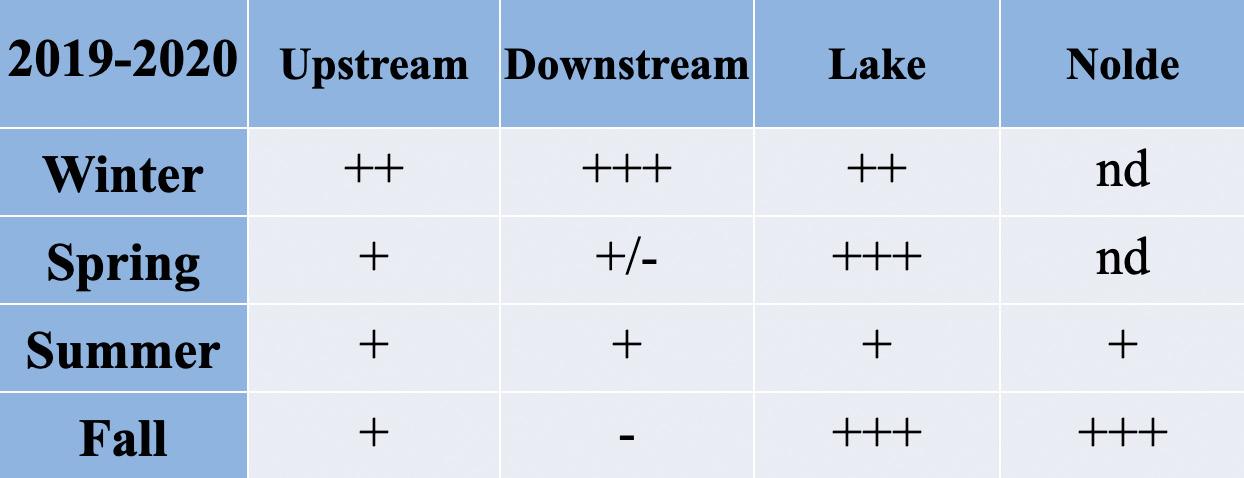
Table 1. Fold-changes in Enterococcus tetracycline-resistance gene tet(A) from 2019 to 2020.
Table 2. Fold-changes in Enterococcus tetracycline-resistance gene tet(A) from 2020 to 2021.
18 | www.berkscms.org
continued from page 17
The BCMS Pat Sharma
President’s Scholarship
Table 3. Fold-changes in Enterococcus tetracycline-resistance gene tet(R) from 2019 to 2020.
ANTIBIOTIC RESISTANCE IN BERKS COUNTY
I. Background
The microbiology laboratory at the Reading Hospital receives specimens from in-patient and out-patient settings for microbial identification and antibiotic susceptibility testing. For the purposes of this study, Dr. Debra Powell, the infectious disease specialist at Tower Health, provided me with these data sets on antibiotic resistance found in the clinical settings locally.
II. Methodology
Table 4. Fold-changes in Enterococcus tetracycline-resistance gene tet(R) from 2020 to 2021.
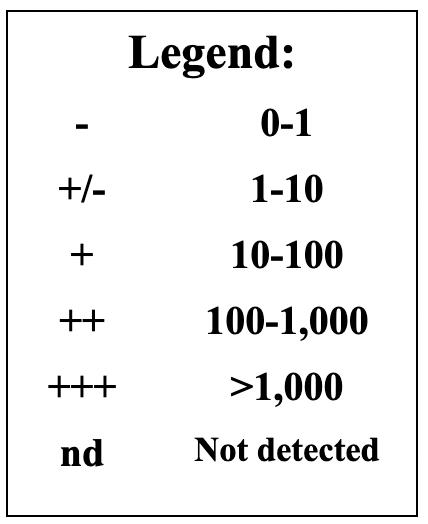
13: Legend to read the fold changes in Tables 1-4
The following data analysis is conducted on the isolates that came from various body parts of adult patients; duplicates of isolates from the same patient were excluded. The antibiogram data from the hospital shows the percentage of isolates that are “susceptible” to specific antibiotics since identifying antibiotics likely to treat an infection successfully is the most clinically relevant information for healthcare providers. Since my bench research was focused on monitoring the presence of genes conferring antibiotic resistance, in my search for correlations with this clinical data, I derived a figure for the percent of cultured isolates categorized as resistant. I did this by subtracting the percentage of susceptible isolates from 100. The percentage of resistant isolates thus derived is inflated to some extent because it includes those isolates classified as ‘intermediate’ by the clinical lab. The intermediate classification is applied to isolates whose response to a specific antibiotic indicates that the organism might not be successfully treated with the antibiotic at the dosages normally used. In the hospital lab data analyzed for this study, the number of isolates classified as an intermediate was close to zero for those tested against tetracycline and ampicillin. The numbers were higher for nitrofurantoin.
III. Results
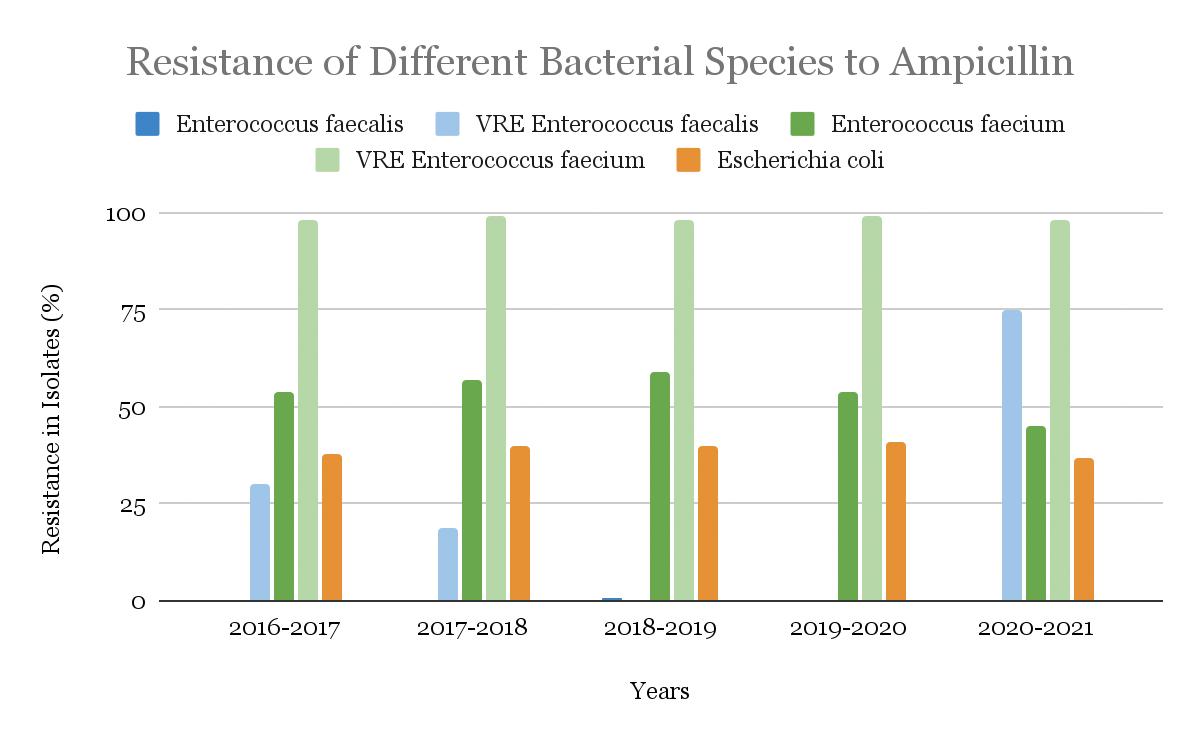
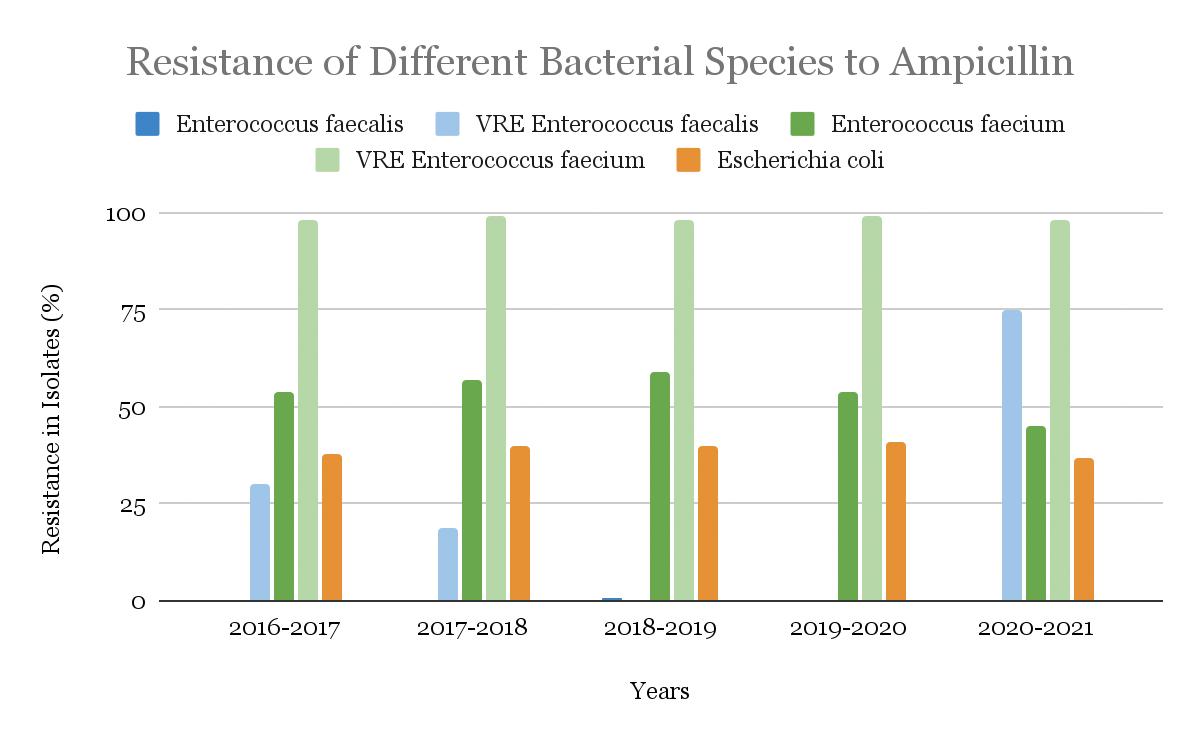
A. Ampicillin
IV. Conclusion
Chemical and microbial analysis of sediment samples, performed by other students in our laboratory, revealed significant seasonal variability for levels of certain pollutants. Nitrate and phosphate levels were elevated for all sites in fall and spring, and the sites had E. coli and Enterococci counts higher than the EPA recommended criteria about 36% of the time. Additionally, more than 80% of E. coli and 60% of Enterococci spp. were resistant to at least one antibiotic. PCR analysis revealed that the genome of the microorganisms in the upstream and downstream sample sites contain tetracycline-resistant genes, tet(A) and tet(R), as well as ampicillin-resistant genes, ctx, oxa and blaP. Tetracycline- and ampicillin- resistance was found—55.3% of tet(A), 42.7% of tet(R), and 91.7% of ctx resistance were found in all samples analyzed.
Between the years 2016-2021, the percentage of bacterial isolates classified as resistant to ampicillin was higher compared with other antibiotics. During the same time period, an average of 0.2% of the tested isolates were resistant to ampicillin in Enterococcus faecalis, and an average of 24.8% of resistance was found among the isolates of Vancomycin-resistant, or VRE, strains of Enterococcus faecalis. In Escherichia coli, resistance hovered around 39.2% of the isolates. Finally, while the average resistance in Enterococcus faecium isolates was 53.8%, in VRE Enterococcus faecium, the resistance was significantly higher, with an average of 98.4%. The trends over the years of ampicillin resistance in different bacterial species are shown in Figure 14.
FALL 2022 | 19
Figure
Determining Antibiotic Resistance in the Berks County Environmental and Clinical Settings
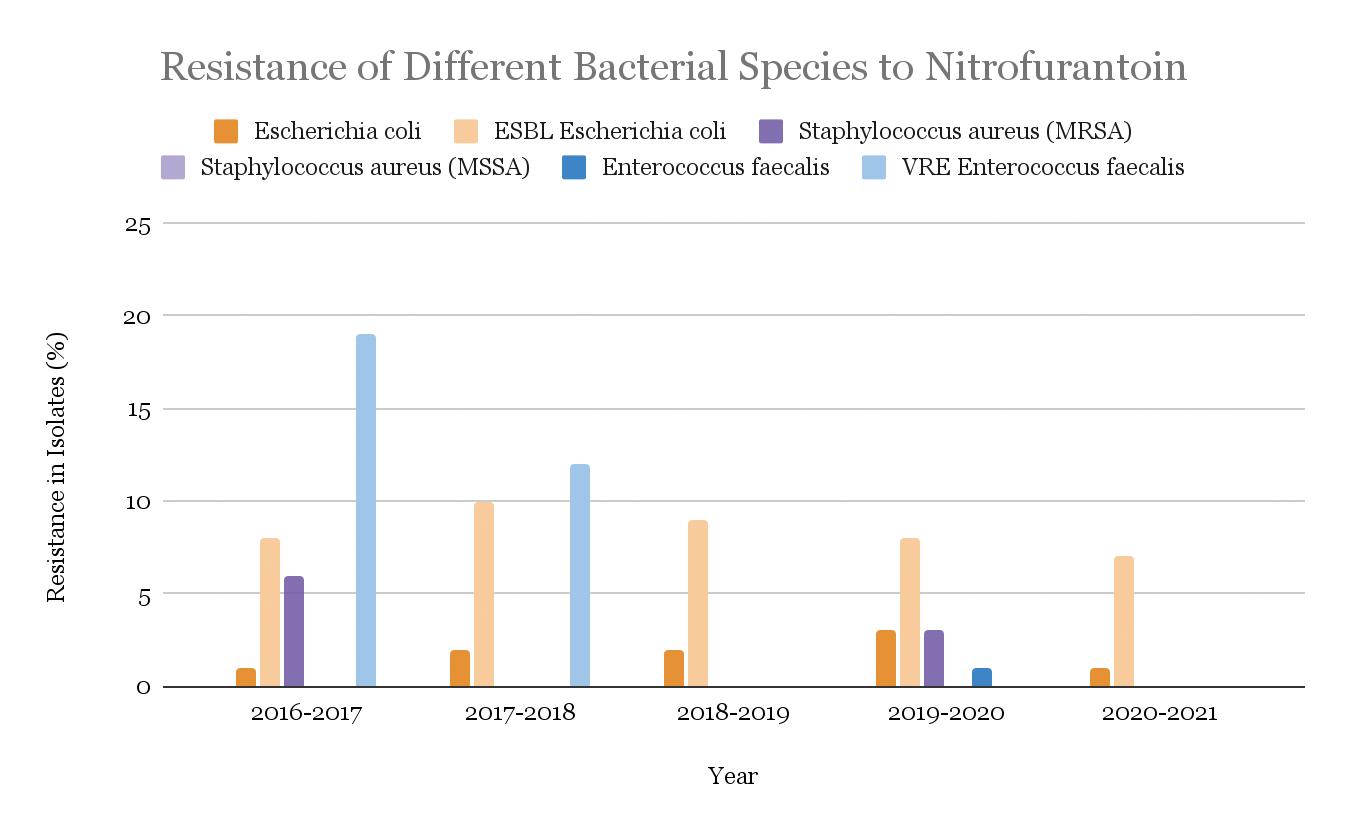
C. Nitrofurantoin
Nitrofurantoin resistance was found to be significantly lower in bacterial isolates when compared to other antibiotics. Between 2016 and 2021, an average of 1.8% of the Escherichia coli and 8.4% of (ESBL)-producing Escherichia coli showed resistance. The Methicillin-sensitive Staphylococcus aureus (MSSA) isolates had no resistance, while only 2.3% of the Methicillin-resistant Staphylococcus aureus (MRSA) isolates were found to have resistance to nitrofurantoin. Finally, Enterococcus faecalis and VRE Enterococcus faecalis had resistance in 0.3% and 7.8% of isolates, respectively. No statistical difference was found between the two. The trends over the years of nitrofurantoin resistance in these different bacterial species are shown in Fig. 16.
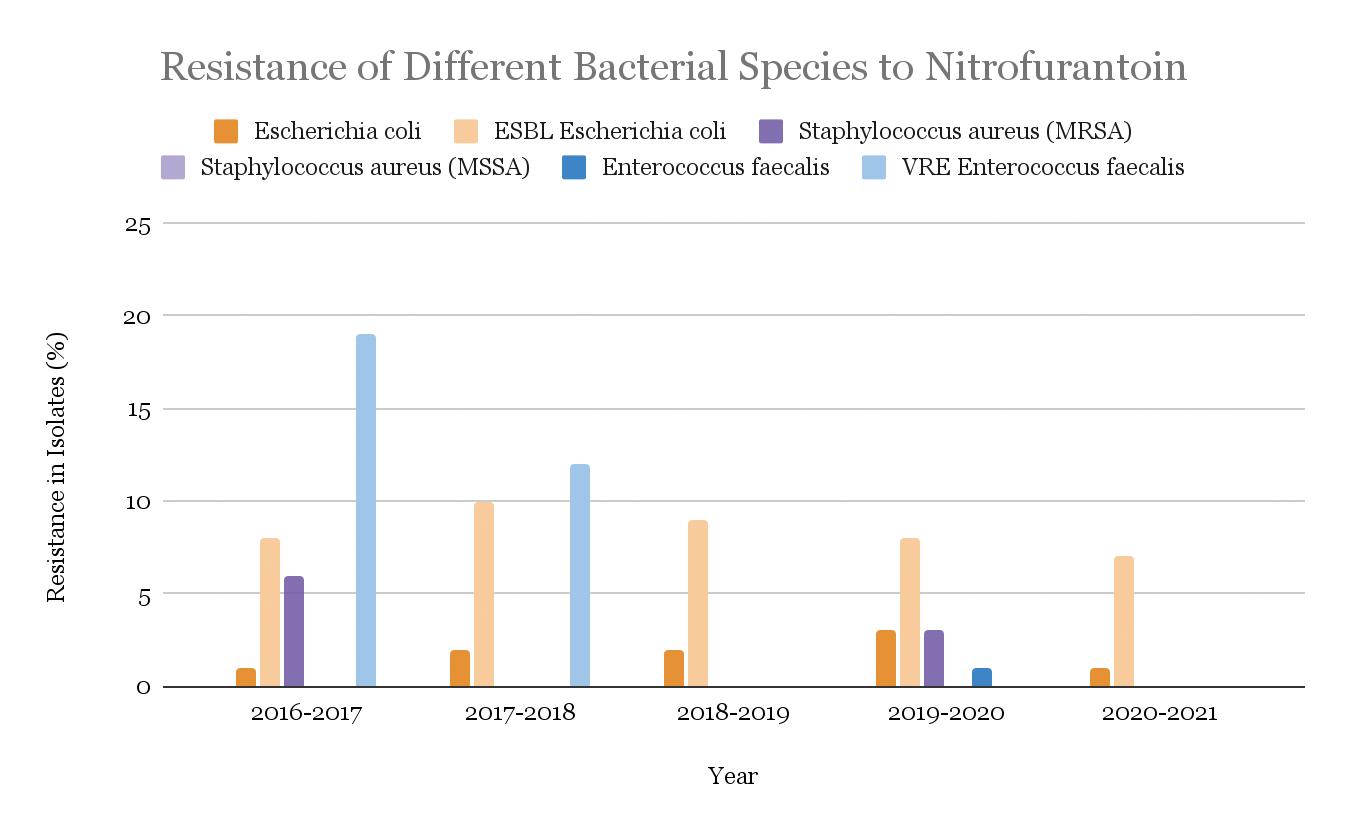
Figure 14: Ampicillin-resistance in isolates of five bacterial strains, Enterococcus faecalis, Vancomycin-Resistant (VRE) Enterococcus faecalis, Escherichia coli, Enterococcus faecium, and VRE Enterococcus faecium from years 2016 to 2021.
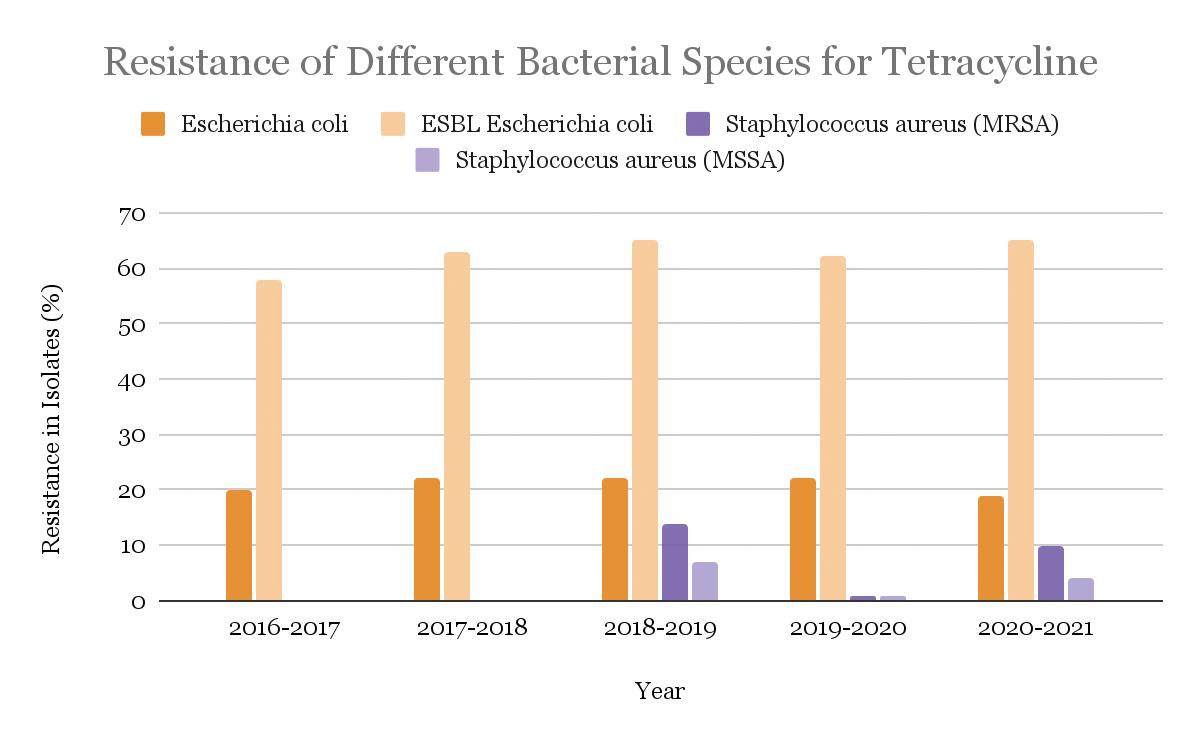
B. Tetracycline
For tetracycline, resistance in once-susceptible bacteria is high. In 21.0% of isolates of Escherichia coli, resistance was detected. Significantly higher resistance (in about 62.6% of the isolates) was found in Extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli. Next, methicillin-resistant Staphylococcus aureus (MRSA) demonstrated resistance in about 5.0% of the isolates, while methicillin-sensitive Staphylococcus aureus (MSSA) had about 3.0% of the isolates showed resistance. The trends over the years of tetracycline resistance in these different bacterial species are shown in Fig. 15.
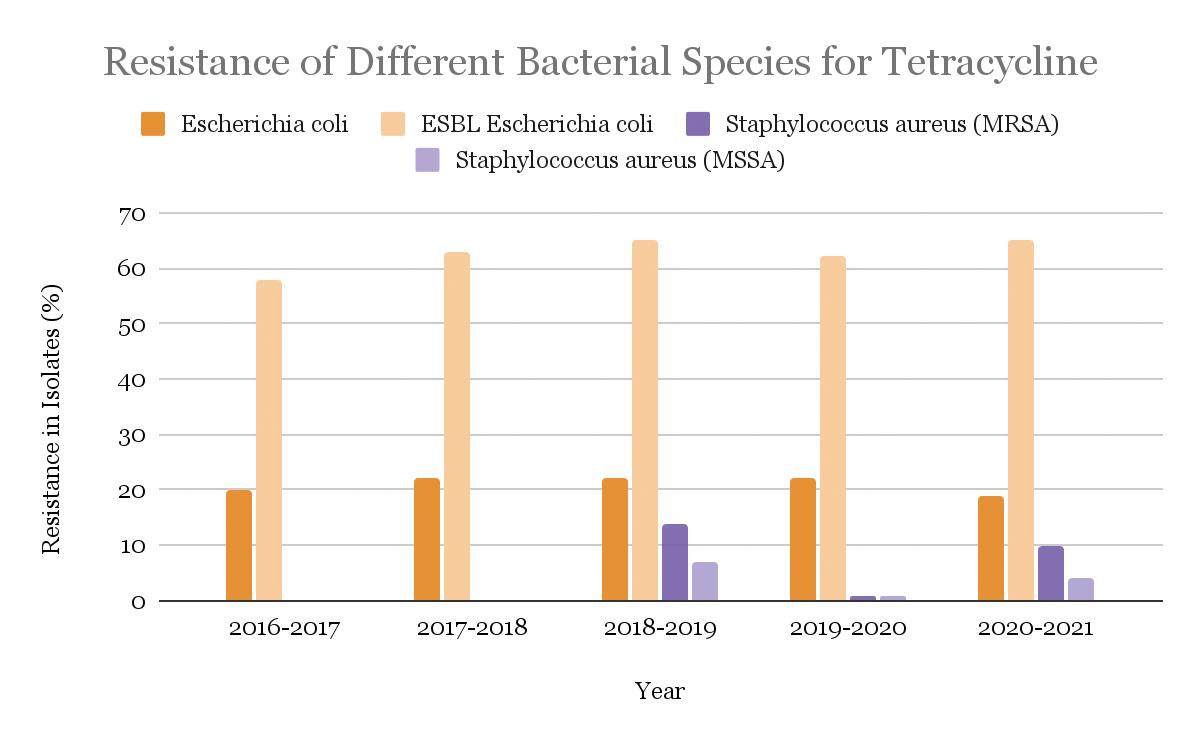
Figure 15: Tetracycline-resistance in isolates of four bacterial strains, Escherichia coli, Extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli, Methicillin-Resistant Staphylococcus aureus (MRSA), and Methicillin-Sensitive Staphylococcus aureus (MSSA) from years 2016 to 2021.
Figure 16: Nitrofurantoin-resistance in isolates of four bacterial strains, Escherichia coli, ESBL-producing Escherichia coli, Staphylococcus aureus (MRSA), and Staphylococcus aureus (MSSA), Enterococcus faecium, and VRE Enterococcus faecium from years 2016 to 2021.
IV. Conclusion:
As noted earlier, the research on environmental isolates in the Blue Marsh Watershed showed an increase in the prevalence of antibiotic-resistant genes since 2019. However, susceptibility (and therefore resistance) patterns over the last few years in the clinical setting at Reading Hospital have been relatively stable. This stability suggests that the Antibiotic Stewardship Program (ASP) at the Reading Hospital is having a beneficial effect on the prevalence of resistant infections in the Reading Hospital patient population. Also, the isolates for each year are dependent upon the number of patients with bacterial infections, so the variability of resistance from year to year may be explained by the unequal number of isolates collected and tested each year.
20 | www.berkscms.org
continued
from page 19
The BCMS Pat Sharma
President’s Scholarship
DISCUSSION:
In conclusion, the increasing prevalence of ARB is a serious global and public-health threat. According to the World Health Organization (WHO), AR negatively impacts the ability of physicians and medical professionals to treat common infections, which in turn leads to an increased infection rate, longer duration of illness, expensive and scarce treatment options, and poorer outcomes (Antibiotic Resistance, 2020). Therefore, the WHO has declared AR one of the most pressing public health issues of the 21st century. Some studies have estimated that by 2050 over 10 million people will die each year worldwide due to drug-resistant infections (Walsh, 2014).



As multidrug resistance patterns are on the rise, Frieri et al. (2017) prompted actions to devise antibiotic stewardship programs in clinical settings and the development of novel therapies that bypass the use of antibiotics altogether. Similarly, Friedman et al. (2016) proposed several changes, such as improving infection control precautions, broadening the antibacterial therapies, using combination therapy, primary source control, and expediting the microbiological test result reporting (Friedman et al., 2016). Finally, both Swami (2014) and Grossman (2016) agreed that because bacteria have increasingly acquired resistance to the older forms of these antibiotics, the only viable way to keep using tetracyclines and ampicillins is through the continued development of new synthetic variants. It is unclear how long this approach can be sustained, and therefore ways to directly disable the antibioticresistant mechanism need to be explored. It can be hypothesized that a reduction in the use of antibiotics in clinical and agricultural settings, without withholding treatment when appropriate, could relieve the selective pressure for mutants with resistance, resulting in the re-establishment of the sensitivity to these antibiotics (Grossman, 2016; Swami, 2014). Finally, Antibiotic Stewardship Programs, such as the one implemented at Reading Hospital, are a vital tool for controlling antibiotic resistance and should continue to be supported and promoted.
Safitaj Sindhar will graduate from Penn State Berks in December 2022 as a biology major with a minor in psychology. She is applying to medical schools this year, with a long-term goal of working internationally to improve access to quality healthcare.

Tomp

FALL 2022 | 21
kins
Building Healthcare Practices, Together Healthcare professionals are crucial to the strength of our communities When planning your financial strategy, work toward building your practice For Doctors, Dentists and Veterinarians 2607 Keiser Blvd, Suite 200, Wyomissing, PA 19610 484-509-0840 Specializing in the diagnosis and treatment of ALL neck and back disorders. • Pain Management • Physical Therapy • Epidural Injections • Spinal Surgery Compassionate. Personalized. Optimum Spine Care. Steven M. Evans, DO Director of Non-operative Spinal Care Stephen P. Banco, MD Fellowship-Trained Spinal Surgeon Steven M. Presciutti, MD Fellowship-Trained Spinal Surgeon ALL SURGERY PERFORMED IN BERKS COUNTY
Healthc are S er vices Suite
Efficacy of a Substance Abuse Program in a Regional Emergency Department

INTRODUCTION: Drug and alcohol abuse can be considered a widespread epidemic in the US. In an attempt to not only treat patients with acute substance intoxication, but also to cure their chronic use, the Reading Tower Health Hospital Emergency Department (ED) implemented a handoff program named the “Warm Handoff” (WHO). This program allows physicians to offer care outside of the ED by “handing off” a patient diagnosed with substance abuse to an appropriate acute detoxification/ rehabilitation facility. This study attempts to determine the efficacy and utilization of WHO, as well as provide data that will be used to modify and improve the program’s implementation.
METHODS: The study was conducted in a retrospective fashion. Patient records were retrieved based on an HIM code screening which selected any patient that presented to the ED with acute intoxication or an issue in which substance abuse played a major role. The patients were deidentified using the REDCap software database, and a form was filled out for every patient based on their history. It was important to determine whether WHO was offered/ not offered, whether the patient accepted/declined, and whether they presented to the ED with substance abuse at a later period in time, usually in the span of two years. Different statistical methods were performed to determine the outcome of the multiple related variables.
RESULTS: The working sample size consisted of 2027 subjects. Of those, only 888 (43.8%) had a WHO consult offered, and 544 (26.8%) accepted the WHO consult. Of those accepting a WHO consult, only 421 (20.8%) accepted treatment, 305 (15.0%) subjects were referred to inpatient treatment, and 116 (5.7%) were referred to outpatient treatment. Of the 544 subjects who accepted treatment, 18 subjects (3.3%) came back due to substance abuse in 72 hours, 36 subjects (6.6%) came back between 72 hours and 30 days, 28 subjects (5.15%) came back between 30 and 60 days, 147 subjects (27.0%) came back between 60 days and 1 year, and 130 subjects (23.9%) came back between 1 year and 2 years.
CONCLUSION: Based on the data, the WHO program is only offered 44% of the time. It is accepted with an even lower rate and even fewer people accept and attend treatment. Providers cannot force a patient to attend treatment, but the rate of WHO offerings must increase for a greater efficacy. In the early phases of the program, a patient could refuse a WHO consult. The process was later changed to automatically order a consult without patient approval to increase compliance. Therefore, out of the patients to whom a consult was offered, only 61% accepted. Some of the limitations of the study can be attributed to the lack of data in the case that a patient did not return to the ED for a substance abuse issue. Hence, it is impossible to know what exactly happened to the patient and whether they fully recovered or are currently under the influence of substance abuse.

22 | www.berkscms.org
by Kirill Popovich, University of North Carolina at Chapel Hill; Amanda Hill, Alvernia University; Christian Brito, Millersville University; Erica Tait, Alvernia University; Joaquim Diego Santos, Pennsylvania State University; Alexis Schoener, Pennsylvania State University; McKenna Brower, Syracuse University; Adam Sigal, MD; Traci S. Deaner, MSN, RN; Megan Reed; Monisha Bindra, DO; Charles Barbera, MD
The BCMS Pat Sharma President’s
Scholarship
Trends and Outcomes of ST-Segment-Elevation Myocardial Infarction in Hospitalized Patients Without Standard Modifiable Cardiovascular Risk Factors
by Baotram Nguyen; Biraj Shrestha, MD; Amar Suwal, MD; Rebecca DeBoer, DO; Laura Kane, RN; Anthony Donato, MD, Department of Internal Medicine, Reading Hospital, Reading, PA

INTRODUCTION: Standard Modifiable Cardiovascular Risk Factors (SMuRFs) include hypertension, diabetes, hyperlipidemia, and smoking, all of which increase the risk of developing heart disease. However, newer research has observed that in patients experiencing their first episode of ST-segment-elevation myocardial infarction (STEMI), patients without SMuRFs tend to have worse in-hospital outcomes for unclear reasons. We sought to better understand the impact of patient and physician preferences that could explain these differences.
METHODS: A retrospective chart review was performed on patients presenting to the Reading Hospital Emergency Department with the first STEMI episode from January 2019 to April 2022. Patients with past medical histories of STEMI, stent placements, or coronary artery bypass grafts were excluded in order to capture only first events. The study population was divided into two comparative cohorts, SMuRFs and SMuRFless STEMI, based on the history of hypertension, diabetes, hyperlipidemia, or smoking in the patients’ past medical records from EPIC. In addition, demographics and inhospital outcomes were assessed.
RESULTS: 356 first-time STEMI patients were identified, of which 36 (10.11%) were SMuRFless. SMuRFless patients were more likely to be younger (58.77 vs. 64.47 years) and male (74 vs. 65%).

SMuRFless patients were more likely to present to the emergency department as walk-ins (54.28 versus 39.25%), took longer to arrive after symptom onset (6.70 versus 5.15 hours), have higher initial troponin values (3.90 versus 2.70 ng/mL), had to wait longer for cardiac catheterization from arrival (69.96 versus 47.48 minutes) and were less likely to receive PCI overall (80.00 versus 89.09%). Furthermore, SMuRFless patients were more likely to have higher inhospital mortality (17.14 versus 8.72%), cardiogenic shock (14.70 versus 6.47), acute heart failure (5.88 versus 2.27%), bleeding requiring transfusion (8.82 versus 1.92%) and overall complications (25.71 versus 21.50%). At discharge, SMuRFless patients also received less guideline-directed medical therapy (GDMT) than patients with SMuRFs.
CONCLUSION: SMuRFless patients make up a considerable proportion of first-time STEMI patients at Reading Hospital, have higher mortality and complications, and undergo fewer procedures. Whether there are patient or physician preferences that may have influenced these outcomes is a matter of ongoing study for this project. Sample size in this interim analysis is too small to make statistical conclusions, but the work is ongoing.
FALL 2022 | 23
Student Summer Research Projects Reading Hospital/Tower Health
A Quality Improvement Project to Decrease the Number of No-Show Patients
by Cassiopeia Roychowdhury, MD, Dept. of Family Medicine, Reading Hospital, Reading, PA; Katie Rudzenski, DO, Dept. of Family Medicine PGY-3, Reading Hospital, Reading, PA; Emma Miller, Millersville University, Millersville, PA
INTRODUCTION: Patients’ attendance to their appointments is essential for maintaining their health and for the clinic’s productivity. However, doctors’ offices are noticing anywhere from 10-40% of their patients do not show up for their appointments and they do not cancel ahead of time. There are many different factors that can affect a patient’s ability to attend an appointment, whether it be transportation or forgetfulness. This study attempts to understand why patients are missing their appointments and to form possible interventions that could be used to reduce the number of no-shows. By reducing the percent of patient no-shows, it helps ensure that patients are receiving the care that they need, and the clinic is not losing revenue.
METHODS: Patients from the Family Health Care Center at Reading Hospital that have missed over 3-4 appointments were chosen at random and voluntarily surveyed over the telephone. A translator was used for patients that did not speak English. The survey included questions focusing on transportation, childcare, and if the patient was receiving reminders. The purpose of our survey was to explore common barriers patients face and create a targeted intervention for a future study. However, the data from the survey will be used to create targeted interventions in the future. Seven patients participated in the survey and results were analyzed with pie charts.
RESULTS: Based on the survey, most patients (40%) miss their appointments because they forgot despite 86% indicating they received at least one reminder. Other patients gave reasons such as being sick, needing childcare, being called into work, etc. When asked if the patients knew how to cancel the appointments, 71% reported that they did. 57% reported that they never tried to cancel the appointment. However, it should be noted that most of the patients we attempted to contact, did not answer their phone or the number called was inactive. Indicating patients might not be receiving reminders, especially if the inactive phone number is all the office has. Patients were also asked if they had reliable transportation and 28% reported that they did not.
CONCLUSION: This survey provided helpful insights on why patients are not showing to their appointments. For future interventions, patients could be given an appointment reminder on their primary care providers (PCP) business card. This study had planned to try the business cards as the intervention but due to time constrictions it did not get started until this week. The interventions’ effectiveness will not be seen for another week, but patients have already given feedback. Many patients thought seeing the PCP picture with their appointment made a personal connection and it was a smaller, more convenient option to the after-visit summaries. Other ideas would be to limit number of follow-ups and have patients call for appointments as needed. It would be helpful to confirm at check-out if the number on file is accurate. We can also ask patients for their preferred method of reminders such as a phone call, mychart, etc. A future recommendation for completing clinical surveys is to give them to qualifying patients in the office or allow the survey more time and send them in the mail. Most patients that were called did not answer or the phone number was inactive, and it made it not the most effective method. Overall, an intervention should be implemented to help improve the consistency of patient care and productivity in the office.
Resources
Claveau, J., Authier, M., Rodrigues, I., & Crevier-Tousignant, M. (2020, May). Patients’ missed appointments in academic family practices in Quebec. Canadian family physician Medecin de famille canadien. Retrieved July 14, 2022, from https://www.ncbi.nlm.nih. gov/pmc/articles/PMC7219803/

Jain, S. H. (2021, December 10). Missed appointments, missed opportunities: Tackling the patient no-show problem. Forbes. Retrieved July 14, 2022, from https://www.forbes.com/sites/ sachinjain/2019/10/06/missed-appointments-missed-opportunitiestackling-the-patient-no-show-problem/?sh=145cd2d7573b
Marbouh, D., Khaleel, I., Al Shanqiti, K., Al Tamimi, M., Simsekler, M. C., Ellahham, S., Alibazoglu, D., & Alibazoglu, H. (2020). evaluating the impact of patient no-shows on service quality. Risk Management and Healthcare Policy, Volume 13, 509–517. https://doi.org/10.2147/rmhp.s232114
24 | www.berkscms.org M edical R eco R d F eatu R e
The BCMS Pat Sharma
Reading Hospital/Tower Health
President’s
Scholarship Student Summer Research Projects
Solutionreach. (n.d.). Everything you need to know about no-shows in your practice. Everything You Need to Know About No-Shows In Your Practice. Retrieved July 14, 2022, from https://www. solutionreach.com/guide/reduce-no-shows-and-cancellations-inyour-practice?source_url=https%3A%2F%2Fwww.solutionreach. com%2Fguide%2Freduce-no-shows-and-cancellations-in-yourpractice%23%3A~%3Atext%3DNo-shows%2520are%252C%2520u nfortunately%252C%2520pretty%2520common.%2520No-how%25
20rates%2520have%2Cspecialty%2520and%2520here%2520to%25 20calculate%2520your%2520no-show%2520rate%2529

Toland, B. (2013, February 24). No-shows cost health care system billions. Gazette. Retrieved July 14, 2022, from https://www.postgazette.com/business/businessnews/2013/02/24/No-shows-cost-healthcare-system-billions/stories/201302240381
Mortality and Comorbidities Associated with COVID-19 Infection in Psychiatric Patients from a State Hospital
by Nicole Villa1, Matthew Driben2, Regina Reed2, Maria Ruiza Yee2, Eduardo D. Espiridion2 Drexel College of Medicine, Tower Health Campus1, Reading Hospital, Tower Health2
ABSTRACT
INTRODUCTION: As dangerous as COVID-19 has been for the general population, it has been even more severe in psychiatric wards. A state hospital is a particularly transmissible location for COVID-19, and the medications that psychiatric patients typically utilize may contribute to the incidence of comorbidities including obesity, hypertension, diabetes, chronic kidney disease, chronic obstructive pulmonary disease, heart failure, and cancer. Studies have found that patients with preexisting mental health disorders and comorbidities tend to have worse COVID-19 outcomes, including death.
METHODS: We performed a retrospective study on 24 patients (13 males, 11 females) in a psychiatric state hospital who were at least 18 years old, tested positive for COVID-19, and experienced symptoms severe enough to be admitted to Reading Hospital between April 1, 2020 to June 30, 2022. Patients with multiple COVID-19 admissions to the hospital during this period were counted only once if the period between admissions was less than two weeks.
RESULTS: The patient population had an average (IQR) age of 57.75 (48-64) and 2.12 (2-3) comorbidities (IQR). The most common psychiatric disorders were schizoaffective disorder (70.8%), schizophrenia (29.2%), and delirium (29.2%). For comorbidities, patients most commonly presented with hypertension (54.2%), chronic kidney disease (41.2%), diabetes (33.3%), and obesity (33.3%) upon admission. The most common psychiatric medications patients were taking as of their admission for COVID-19 were antipsychotics (83.3%), mood stabilizers (54.2%), antidepressants (54.2%), and benzodiazepines (41.7%).
CONCLUSION: Though our study was descriptive in nature, it was meant to shed light on what conditions precipitate the worsening of COVID-19 infection in psychiatric patients that results in hospitalization. We recommend additional studies in order to make a conclusion about the extent to which psychiatric medications result in worse COVID-19 outcomes due to worse comorbidities.

FALL 2022 | 25
Cardiac Arrest Resuscitation Excellence Project
by Adam Sigal, MD; Allison Atkinson, MS-1 Department of Emergency Medicine, Reading Hospital – Tower Health, West Reading, Pennsylvania

INTRODUCTION: Cardiac arrest throughout the country has a significantly low survival rate and is responsible for the death of over 300,000 people in the United States every year.1,2 Therefore, it is of interest to evaluate the resuscitation methods performed within Reading Hospital and the community to determine variables that impact cardiac arrest outcomes. This can promote discovering ways in which we can improve our quality of care.
METHODS: Retrospective chart reviews were performed looking at patients from Reading Hospital starting in January 2020 to May 2022 who experienced an out of hospital cardiac arrest or cardiac arrest within the emergency department. The charts were selected using a reporting system that collects the data directly after a code narrator is started in the emergency department. Additional data was collected manually and stored in REDCap. Variables investigated included, but were not limited to, whether the arrest was witnessed, presence or absence of bystander CPR, location of cardiac arrest, treatment performed by emergency medical services and the emergency department, survival to hospital admission, survival to hospital discharge, and neurological function status post cardiac arrest. Preliminary data analysis was performed on SAP/Webi BI Tool and Social Science Statistics.
RESULTS: 453 patients who experienced cardiac arrest under the conditions stated above were evaluated. Of these patients, 28.9% survived to admission from the emergency department and a total of 6.2% survived to discharge from the hospital. The percentage of patients who received bystander CPR was calculated to be 33% and some preliminary statistical analysis was performed to further evaluate components within this variable. Chi-square testing was used to compare the survival rates of patients who had witnessed cardiac arrests and received bystander CPR to those who had unwitnessed arrests and did not obtain CPR until the arrival of EMS. Chi-square calculations comparing these variables showed X2 (1, N=143) = 3.2149, p=.07297 (p>.05).3 Lastly, while the etiology of cardiac arrest can be broad, over 50% of the cardiac arrests that occurred within our data collection had cardiac etiology.
CONCLUSION: Given the ongoing nature of this project, we will continue to expand our registry to improve statistical power and will look at individual variables to determine if there are system or process changes that we can make to increase survival to hospital discharge. Potential areas of improvement include incorporating the latest research into our resuscitation research and methods in the emergency department as well as conducting community outreach on the importance of bystander-initiated CPR and AED use.
1. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2022 update: A report from the American Heart Association. Circulation. 2022;145(8). doi:10.1161/ cir.0000000000001052
2. Sudden cardiac arrest: Causes & symptoms. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17522-sudden-cardiacdeath-sudden-cardiac-arrest. Published June 6, 2022. Accessed July 10, 2022.
3. Chi-Square Test Calculator. Social Science Statistics. https://www. socscistatistics.com/tests/chisquare2/default2.aspx. Published 2022. Accessed July 10, 2022.
26 | www.berkscms.org
M edical R eco R d F eatu R e Student Summer Research Projects Reading Hospital/Tower Health
The
BCMS Pat Sharma President’s Scholarship
The Prospective Association Between Breast Arterial Calcifications on Routine Mammography Screening with Coronary Artery Disease and Stroke, A 17-Year Follow-Up
by Jenna Ehlert (MD Candidate, 2025); Matthew Nudy, M.D., Xuezhi Jiang, M.D., and Peter F. Schnatz, DO

Drexel University College of Medicine, West Reading, PA Department of OBGYN, Reading Hospital, Reading, PA
INTRODUCTION: The leading cause of death in women in 2018 was cardiovascular disease (CVD).1 However, the current clinical tools used to assess if a woman is high risk underestimate this true value. Incidental findings of breast arterial calcifications (BAC) on mammography screening may be utilized as a tool to routinely assess for risk of CVD. This study aims to determine if this tool is adequate in evaluating the risk after 17 years of prospective follow-up.
METHODS: The prospective cohort consists of women recruited during routine mammography screening between June and August 2004 at one of four radiology practices in Hartford, CT. The only exclusion criterium is male gender. Baseline data was collected about history of CVD and various risk factors including hypertension, hyperlipidemia, diabetes, tobacco use, exercise habits, and family history of CVD. Participants were contacted 17 years after this initial screening for follow-up with a similar risk questionnaire and to determine if they had developed coronary artery disease (CAD) or stroke. This data is currently being collected via mail, email, and phone calls. It will subsequently be correlated with the baseline mammograms that were analyzed for breast arterial calcifications (BAC) in 2004 by one of 21 radiologists who were standardized and blinded to the study.
RESULTS: Of the 1,995 participants who were enrolled at baseline, 334 have completed the 17-year follow-up survey, 57 are deceased, and 22 have declined to or were excluded from participating (male gender, transgender). Results are therefore still pending. The previously reported 10-year prospective study collected follow-up data on 1,039 individuals, 10.1% being BAC positive and 89.9% were BAC negative at baseline. Controlling for age and risk factors, BAC positive women were more likely to develop CAD after 10 years compared to BAC negative women (Odds Ratio [OR] 3.76, 95% Confidence Interval [CI] 1.94-7.28, p < 0.001). Additionally, controlling only for age, BAC positive women were more likely to have a stroke after 10 years (OR 5.10, 95% CI 1.82-14.30).

CONCLUSION: The 10-year prospective study showed a significant association between the presence of BAC on routine mammography with an increased risk of developing CAD and stroke. This data was consistent with the 5-year follow-up data from the same cohort. Continued collection and subsequent analyzation of data for the 17-year follow-up will allow us to determine if this correlation has continued.
1 Heron, M., Ph.D. (2021). Deaths: Leading Causes for 2018. National Vital Statistics Reports, 70(4). <https://www.cdc.gov/nchs/data/ nvsr/nvsr70/nvsr70-04-508.pdf>
FALL 2022 | 27
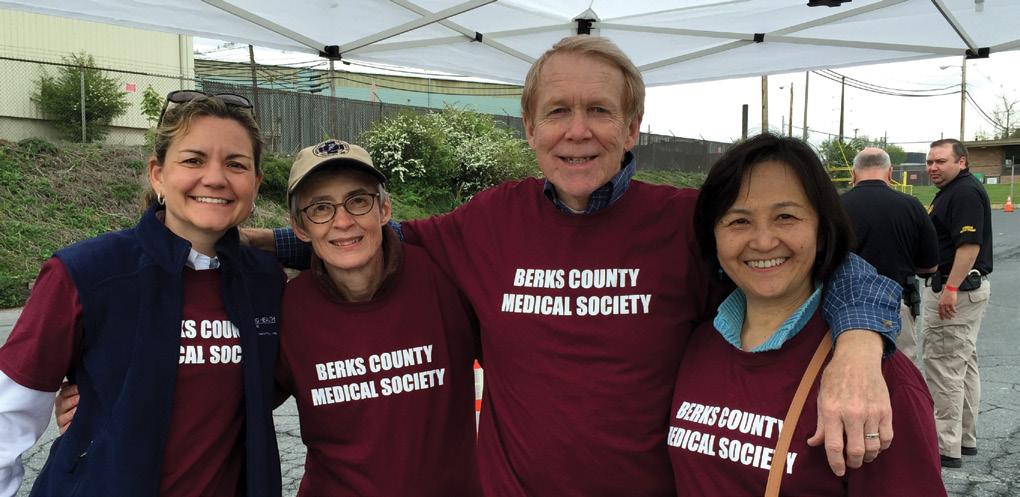
STREET MEDICINE – Reborn in Berks
by William Santoro, MD
Street Medicine can be considered the very first specialty in medicine. There were days in medicine when house calls were not only made but were commonplace. Along with house calls came the treatment of patients who could not afford care. This care was delivered either where the patients were, or the patients came to the doctor’s office and were treated at a discounted fee or at no charge. Although the days of house calls are long gone, I still believe that most physicians chose the field of medicine for reasons other than monetary.
In 1986, a homeless shelter in Berks County traveled from one church basement to another each week. A local family physician, armed with only a stethoscope, arrived at a church one evening and offered to see any person who had a medical question, free of charge. The word quickly spread and when the homeless shelter found a permanent place to reside, six physicians volunteered their time. These physicians rotated coverage at the homeless shelter delivering primary care medicine to any resident free of charge. Each physician donated not only their time, but equipment, supplies, and medication as well.
This program grew to become a full clinic supported by The Reading Hospital & Medical Center and staffed by attendings, interns and residents. It grew to the point of delivering primary care medicine; employing counselors and social workers to help people staying at the shelter in any way that was necessary. The program continued for many years… until it didn’t.
The 2016 Berks County Community Health Needs identified access to care as a key priority. Populations within the community that struggled the most with accessing quality healthcare were those who were homeless or who were at risk of becoming homeless. This became the impetus for the rebirth of Street Medicine in Berks County.
This modern Street Medicine was designed to deliver high quality patient-centered primary and preventive care as well as acute healthcare services to homeless individuals. Street Medicine aimed to increase accessibility and continuity of care by connecting patients to healthcare services through tele-health as well as providing patient case management services. The goal was to educate the patients on the available community services and resources.
The Street Medicine Team now provides primary and several limited specialty care services to patients. Different specialists such as diabetes management, podiatry, addiction medicine, and psychiatry, also volunteer their time and expertise and are considered part of the Street Medicine Team.
As an organized force, the Street Medicine Team has partnered with several community facilities including City Light Ministry, Hope Rescue Mission, New Journey Community Outreach, and the
YMCA of Reading-Berks County. The Street Medicine Team has set scheduled times when patients are seen at each of these facilities, but to truly be called Street Medicine, the team arranges to meet the patient where the patient is. The Street Medicine Team routinely visits locations such as encampments, parks, under bridges, along the Schuylkill River, in the mountains, and anywhere else in the County where people might be located who need help and/or medical care.
Street medicine has arranged to have several specialty clinics for patients.
The Eye Screening Clinic provides screening eye examinations and facilitates access to follow-up care. Screening exams include color blindness screening, field of vision screening, glaucoma screening, visualization of the retinas, and visual acuity changes.
The Pulmonary Screening Clinic provides for the evaluation and education of patients with breathing disorders including screening for sleep apnea, evaluation for low-dose CT lung cancer screening, tobacco cessation education, respiratory disease management and education on disease states such as COPD (Chronic Obstructive Pulmonary Disease), asthma and OSA.
Psychiatry and Addiction Medicine work together as many patients are dual diagnosed with illnesses in each specialty. A psychiatrist and addiction medicine specialist volunteer their time on a regular basis to help patients initiate, continue, or receive a bridge prescription along with a referral for a formal visit with a specialist in the field.
In 2022 the Street Medicine Team took the next step in helping this population by creating a tele-health kiosk at the Hope Rescue Mission. This kiosk allows a healthcare provider to meet virtually with patients who have an immediate need or require a follow-up from a prior visit. The tele-health kiosk allows much more flexibility for the provider and increased access for the patient. Moving forward, the Street Medicine Team has dreams of kiosks in other partnering facilities.
While Street Medicine counts their successes one patient at a time, they have amassed over 4,000 documented encounters and medical visits in just the past two years.
The Street Medicine Team
Founders:
Eugene York, MD, and Sarah Luber, DO
Primary Participating Physicians:
Pavani Pagolu, MD
Susmita Paladugu, MD
Anthony Donato, MD
Case Manager: Darla Harris, RN
Program Manager: Yomari Salvador-Rivera

28 | www.berkscms.org
M edical R eco R d F eatu R e
BCMS Night at the “Reading Fightin’ Phils” August 18, 2022



A spirited group of Drexel/Tower Medical School Students joined members for the annual outing at the “Reading Fightin’ Phils.” MS 2 students Maggie Vacchiano, and Danielle (Dani) Kessler had the honor of throwing out first pitches before the game. Drexel students enjoyed the Right Field swimming pool and it was hard to tell them apart from all of the tenyear-olds who joined them in the pool.





A great time was had by all!!

FALL 2022 | 29
M edical R eco R d F eatu R e
A Night of Physician Storytelling
by Raymond C. Truex, Jr., MD
humanities curriculum at Reading Hospital, intended to reduce burnout, improve communication skills, increase empathy, and improve ability to deal with the unknown. Narrative medicine is but one branch of the humanities curriculum, which also includes medical ethics, medical professionalism, communication, diversity, equity and inclusion, public health, theology and faith, history of medicine, and art in medicine.
When Dr. Caitlin Moss came to Reading Hospital as an academic hospitalist, she brought with her a concept that she had been introduced to at Beth Israel Hospital in Boston during her residency training. It wasn’t a diagnostic or therapeutic concept, but rather one related to the medical humanities.
On Thursday evening, September 8, 2022, the Reading Hospital Department of Medicine sponsored Our Stories, a Night of Physician Storytelling at the DoubleTree Hotel. This dinner event came together over seven to eight months through the collaborative efforts of Dr. Moss and Dr. Andy Donato, with the financial and venue support of Kate Thornton and the Reading Hospital Foundation. Those invited to the dinner included current and emeritus Reading physicians, residents, and Drexel medical students. Over 120 positive RSVPs were received.
The purpose of the dinner was physician communication, so younger physicians might hear how their older and more experienced peers managed their most difficult cases and dealt with the associated psychological stress; as Dr. Donato put it, “unpacking the burdens of being a practicing physician.”
The dinner was one part of the new medical
The dinner was highlighted by three guest speakers, Dr. Usama Nasir, Dr. Sarah Luber, and Dr. Erik Rupard, each of whom delivered poignant personal stories of medical stress and how they responded. Further, the seating arrangements at each table included a moderator and
a combination of house staff and more senior physicians who interacted with their own personal stories of challenging medical situations and their response to them.


Participants at all levels of medical experience found this dinner to be a success at many levels, and at the conclusion, there was a definite aura of camaraderie in the air. From early indications, this event may become an annual affair.


30 | www.berkscms.org M edical R eco R d F eatu R e
Polio.
It’s happened again, right here in
by Carol Ferguson, Founder, PA Polio Survivors Network - www.papolionetwork.org
The July announcement of a 20-year-old man from Rockland County, NY, paralyzed by the poliovirus, brings back memories of the fear, disability and death that came each summer with the polio epidemics. How can polio be happening here? We have had an injectable polio vaccine (IPV) that is 99% effective available to all children in the US since 2000. Vaccines can’t do their job if people don’t take them, and the young man from New York was not vaccinated. That’s why polio is happening again.
Initial reports indicate that his paralysis was caused by a mutation of the oral Type 2 poliovirus vaccine (OPV), a mutation that occasionally causes the vaccine to result in paralysis. The oral polio vaccines have not been given in the US since 2000, suggesting that the chain of transmission of this contagious disease began abroad. The CDC and WHO have reported the virus that infected him is genetically related to the vaccine-derived poliovirus recently found in London and Israeli sewage (like the US, they are countries that have seen the eradication of polio). The paralyzed man must have come in close contact with someone who had received the oral Type 2 polio vaccine outside the US.
As polio survivors, this case in NY is horribly sad and deeply personal. Sad because the injectable polio vaccine, the only vaccine given in the US, is 99% effective in its protection against all three types of polio. If only he had been vaccinated, the man who was paralyzed never would have become ill at all. Even sadder is that he will have to live with a disability and chances are high that he will experience and become even more disabled as a result of Polio Syndrome (PPS) – the late effects of polio – as he ages.
Why is one case of polio deeply personal? Because lack of vaccination has added one more preventable case of polio paralysis to the WHO estimated 20 million polio survivors, 75%+ of whom will develop PPS. Survivors of this disease will always remember:
• Those who died.
• The terror that came with being so sick.
• Lonely months and years of hospitalization, surgeries and painful rehabilitation all while separated from parents and siblings.
• The frightening reality of an iron lung.
• The sorrow that came with discovering wheelchairs, leg braces and crutches were ours for life.
• The loneliness that came as we returned home, and were forced to accept that everyone around us knew that it was the home of a “cripple,” and parents kept their children away.
• The shock that has come with the reality of the long-haul effects of polio (PPS), when those of us who thought we escaped or recovered from paralysis find ourselves with new weakness, fatigue and pain as we age.
“In Our Own Words” is a page on our website that features brief stories and videos of the realities of this terrible disease.
Yes, the story of this young man’s suffering is sad and deeply personal. Even one unvaccinated person with polio is one too many. His pain is completely unnecessary. The miracle of the polio vaccines came too late for us and for the millions of others who are living with polio’s effects.
We celebrate Rotary International’s focus on disease prevention and the Global Polio Eradication Initiative for their determined efforts to rid the world of polio and educate parents about the gift of modern vaccines.
In spite of these determined eradication efforts overseas, polio is happening in the US.
Please help your patients make the choice to vaccinate. No one needs to suffer from the effects of polio, ever again.
The foreign origin of the poliovirus that paralyzed the unvaccinated man in New York is a painful reminder that polio (and many vaccine preventable diseases) are only a plane ride away.
Some words from Berks County Medical Society:
While our more recent attention has been focused on COVID-19 vaccinations and boosters, the previous article is a clear reminder that all clinicians must continue to emphasize the necessity of completing all recommended childhood immunizations and subsequent boosters to prevent such devastating diseases and promote public health.

FALL 2022 | 31 M edical R eco R d F eatu R e
the US.
9th Annual Digestive Expo A Shining Success at a New Location
On September 24th, My Gut Instinct, Inc., a 501 c (3) non-profit organization in Berks County, hosted its 9th Annual Guts & Glory Digestive & Wellness Expo at a new location, the beautiful Perkins Plaza Event Lawn of the Penn State Berks Campus.
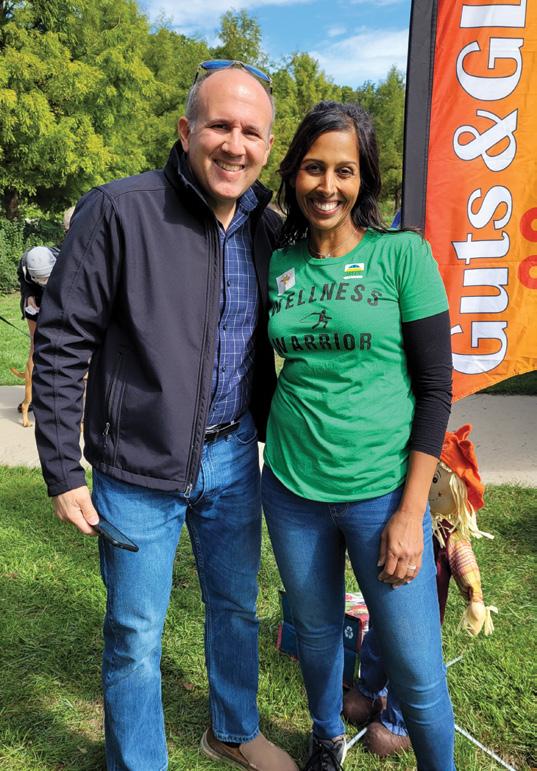


Aparna Mele, MD., created this public educational health expo for our community to inspire and embolden individuals to embrace their own power over their health and to find inspiration in the wonderful offerings in our community to energize their efforts to carve out their own journey to better wellness.
Each year, Guts & Glory aims to emphasize the importance of good digestion and health nutrition, educating community members about symptoms that warrant medical attention, encouraging a proactive and preventive approach to wellness, celebrating health and empowering individuals to take action to live healthier lives. In short, we want people to take charge to become beautiful from the inside out, because we believe that beauty starts on the inside. Take better care of your insides with better nutrition and better performance, and outside health and beauty then follow!
The ninth annual event didn’t disappoint and was a shining success. The overall theme this year was “Embrace Your Wellness.” The day brought hundreds of visitors of all ages on a beautiful and warm sunny fall day. There were about one hundred vendors in attendance that covered the many dimensions of wellness including emotional, physical, occupational, social, spiritual, intellectual, environmental, and financial. There were also martial arts demonstrations, yoga,
Native American dances, massage therapy, informational booths, Latin Flair Salsa demonstration, and of course the MEGA colon exhibit. The attendees were able to step through a large-scale model of the human colon which highlighted common disease conditions. It provided an interactive and educational experience. Free health screenings and biometric testing were offered by We Shine Healthcare Resources. We were also proud to welcome Senator Judy Schwank, a loyal supporter since our inception, and our County Commissioners Christian Leinbach and Michael Rivera. In addition, we welcomed state troopers and EMS to forge strong relations with the community.
Our visitors memorialized their visit by snapping selfies with our mascot, GUTSY GIRL, and made a commitment to improve their own health by signing our Pledge Wall with our 2022 pledge as follows:
HOW WILL I BE A WELLNESS WARRIOR?

The whole day delivered a full sensory experience, showcasing the sights, smells, tastes, sounds, and feel of health – a true health celebration and exciting journey of wellness education, nutrition

M edical R eco R d F eatu R e www.mygutinstinct.org 32 | www.berkscms.org
awareness, and health consciousness for all community members!


This event would not have been made possible without the tireless support of our title sponsor and number one fan, Penn State Health/St. Joseph Medical Center, and the generosity of Penn State Berks for donating their beautiful campus and their hardworking staff. Thank you to our loyal, knowledgeable, dedicated vendors, our tireless, energetic, and devoted volunteers, and our conscious and curious community members for helping make Guts & Glory 2022 the best year yet. The Youth Volunteer Corps of Reading, a team-based service-learning program, sent a team to stuff the event swag bags.
The goal of My Gut Instinct, Inc. is to promote community awareness of health and wellness through preventative health care and holistic well-being. The organization aims to increase public understanding of preventable diseases impacting community health by preventing avoidable diseases, motivating the community to make healthy choices, promoting cancer screenings, and raising awareness of health concerns.

The organization was founded by Dr. Aparna Mele, a local gastroenterologist, who stated, “We aim to provide people with health knowledge and empower them to take action to live healthier lives and become beautiful from the inside out, because we believe beauty starts on the inside. We want to show the community that eating and living healthy is not only easy to do, but it can also be fun and delicious too.”

Guts & Glory is an annual digestive and wellness expo happening in the fall, so spread the word, join our email list to enjoy monthly health-based articles and recipes all year in our e-newsletters entitled DIGEST, follow us, and share your pictures and stories on Facebook, Instagram, and Twitter. Mark your calendars each year and come out and celebrate healthy living with us!
Save the date for our special 10-year anniversary on Saturday, September 23rd, 2023.



FALL 2022 | 33
Reading Hospital Family Medicine Residency Program


50th Anniversary Celebration
DoubleTree Hotel, September 17, 2022
Approximately 120 graduates, former and current residency faculty, current residents, nurses, staff, spouses, and friends, attended the 50th Anniversary of the Reading Hospital Family Medicine Residency Program on September 17th.






Founded in 1972 by longtime Reading/Berks Family Physician, John “Jack” Wagner, the program has graduated over 250 Family Physicians and provided care for thousands of Berks County residents. While graduates live and practice from Washington State to Florida and Hawaii to Maine, many have stayed and practiced (some their entire careers) in Berks County. The first graduate, William Bennett, MD, from Maine, reminisced with local colleagues about their memories of those early days.
Events started with a morning CME program highlighting the work and skills of graduates Corey Keller, DO (Director of Sports Medicine at Temple University), Andrew Lutzkanin, MD (Associate Professor of Family and Community Medicine at PSU Hershey Medical School), Bill Santoro, MD (Director of Addiction Medicine, Tower Health), and Jeanne Manubay, MD, (Assistant Professor of Psychiatry and Family Medicine at Columbia University School of Medicine). In addition, a presentation by former Program Director and former Department Chair Michael Baxter, MD and a Panel Discussion with Tower Health Family Physicians Ivan Bubb, MD, Brian Kane, MD, and current Residency faculty member, Jacqueline Storer, DO, rounded out the morning topics.
The evening gala included soft music, dinner, and a program at the DoubleTree, and was a time of sharing memories, renewing friendships, and catching up on busy lives. John Franko, MD, Chair of the Department of Family and Community Medicine, welcomed guests and introduced evening speakers, including Chuck Barbera, MD, President and CEO of Reading Hospital, who congratulated and thanked all of those graduates and staff who have contributed to the success of the Program and the care of our local community. Dr. Baxter spoke of past memories and accomplishments, and John Sheffield, MD, current Residency Program Director, updated everyone on the present status of the program, and Dr. Storer spoke about her optimistic view of the future of the Residency and of opportunities ahead for Family Medicine.
It was quite a nostalgic evening and reminded everyone of the many friendships formed and good times shared over those many years. However, it was especially a reminder of the success achieved training such wellqualified physicians and the great care they have provided to thousands of patients near and far.
Past, Present and Future—A proud tradition continues.
34 | www.berkscms.org M edical R eco R d F eatu R e
Nationally ranked for heart care by U.S. News & World Report.

Right here – close to home.
Kaedan was born with life-threatening heart defects and had his first open-heart surgery at just four days old. He’s had many surgeries since — all right here in Central PA from a team whose surgical outcomes are among the best in the country. Today, he’s 18 and in college studying criminal justice.

CHI-17383-22 189310
Kaeden | LANCASTER
we can...
At BERKS EYE PHYSICIANS AND SURGEONS, we are happy to offer state-of-the-art and efficient care. Our doctors provide appropriate diagnosis and treatment, and fast feedback to you. Whether your patient has a sudden change in vision, cataracts, diabetes impacting vision, or even has a family history of glaucoma or macular degeneration, we would be honored to monitor and react to issues related to your patient’s eye health.

Domenic C. Izzo, Jr., MD
Cataract Surgeon Advanced Technology Lens Specialist Laser Vision Correction – LASIK Glaucoma and Dry Eye Treatment Comprehensive Ophthalmology
Francisco L. Tellez, MD, FACS
Glaucoma Specialist Glaucoma Surgery & Treatment Cataract Surgery Advanced Technology Lens Specialist Comprehensive Ophthalmology
Kasey L. Pierson, MD
Cornea Specialist Cornea Surgery Cataract Surgery Glaucoma and Dry Eye Treatment Comprehensive Ophthalmology
Peter D. Calder, MD
Cataract Surgery Advanced Technology Lens Specialist Glaucoma Treatment Dry Eye Treatment Comprehensive Ophthalmology
MD
Specializing in Diseases & Surgery of the Retina and Vitreous

610-372-0712 | berkseye.com | 1802 Paper Mill Road, Wyomissing, PA 19610 |
YES,
SEE YOUR PATIENTS SAME DAY FOR EMERGENCIES AND OFTEN SAME WEEK FOR CONSULTS.
Guri Bronner,




































 by D. Michael Baxter, MD
by D. Michael Baxter, MD