YOUR COMMUNITY RESOURCE FOR WHAT’S HAPPENING IN HEALTH CARE SUMMER 2023 Published by Pennsylvania’s First Medical Society Brain Injury & Opioid Use Disorder: Information & Support For Professionals Burnout Defined Ticks… What You Need to Know p 4 p 6 p 8 Kristi Gilfillan p 18
OFFICERS 2023
President
David E. Bobman, MD
President Elect
Mahmoud K. Effat, MD
Vice President
Richard O. Oyelewu, MD Treasurer
Winslow W. Murdoch, MD Secretary
Christina J. VandePol, MD
Editor & Immediate Past President
Bruce A. Colley, DO
Board Members
Norman M. Callahan, III, DO
Heidar K. Jahromi, MD
Mian A. Jan, MD
John P. Maher, MD
Manjula K. Naik, MD
Sean V. Ryan, MD
Francis X. Speidel, MD
Lynne A. Stilley, MBA Executive Director
Chester County Medical Society 1050 Airport Road PO Box 5344
West Chester, PA 19380-5344
Website – www.chestercms.org
Email – OurCCMS@gmail.com
Telephone – (610) 425-9190
Chester County Medicine is a publication of the Chester County Medical Society (CCMS). The Chester County Medical Society’s mission has evolved to represent and serve all physicians of Chester County and their patients in order to preserve the doctorpatient relationship, maintain safe and quality care, advance the practice of medicine and enhance the role of medicine and health care within the community, Chester County and Pennsylvania.
The opinions expressed in these pages are those of the individual authors and not necessarily those of the Chester County Medical Society. The ad material is for the information and consideration of the reader. It does not necessarily represent an endorsement or recommendation by the Chester County Medical Society.

PUBLISHER: Hoffmann Publishing Group, Inc. 2669 Shillington Rd, Box #438, Reading, PA 19608 For Advertising Information & Opportunities Contact: Tracy Hoffmann 610.685.0914 x201 tracy@hoffpubs.com www.Hoffpubs.com Contents SUMMER 2023 Letters to the Editor: If you would like to respond to an item you read in Chester County Medicine, or suggest additional content, please submit a message to OurCCMS@gmail.com with “Letter to the Editor” as the subject. Your message will be read and considered by the editor, and may appear in a future issue of the magazine. Cover: “Springhouse” 9" x 12" Oil, Kristi Gilfillan Read more in The Art of Chester County on page 18. In Every Issue 3 President’s Message 18 The Art of Chester County 4 Brain Injury & Opioid Use Disorder: Information & Support For Professionals 6 Ticks… What You Need to Know 8 Burnout Defined 11 We’re Making Progress in Addressing Maternal Mortality But There’s Still Much More Work to Do 14 Regional Hospital Finance Challenges 22 Healthcare is Withering 24 The Detrimental Impact of the Venue Rule Change by Pennsylvania Supreme Court on Physician Shortage 25 Guest Column: A health care crisis is upon us, and this one is starting in courtrooms 26 Constituent, Voter, Patience, Tenacity, Ask, Engage, Clinical 28 Congenital Syphilis 30 Amazon Prime Vs. Etsy Features
David E. Bobman, MD President, Chester County Medical Society
 BY DAVID E. BOBMAN, MD PRESIDENT OF CHESTER COUNTY MEDICAL SOCIETY
BY DAVID E. BOBMAN, MD PRESIDENT OF CHESTER COUNTY MEDICAL SOCIETY

We asked. You answered. We heard you!
As I previously mentioned, we polled our members to see what they were looking for in the Chester County Medical Society. Several issues came up. First, political advocacy was a common concern. While there are many physician practice issues which need to be addressed on a political level, the most pressing issue revolves around the reversal of a decision 2 decades ago to limit medical liability to the venue in which the alleged malpractice occurred. (Please see my separate article in this issue addressing this matter.) Spearheaded by physician leadership of Paoli Hospital, along with members of the Chester County Medical Society Board, a working group has been established to attempt to tackle this rather difficult and complex issue. Look for more to come in subsequent publications of our newsletter.
Secondly, though the number of private physician practices has dwindled, they now, more than ever, need assistance with the many issues which arise during the running of their practice. To this end, we are in the process of putting together a list of businesses and services which have been recommended by our members. Our hope is to negotiate preferred pricing for our members as well. This is still a work in progress.
Lastly, many people felt there has been a loss of interaction between physicians as many have become isolated in their offices or are otherwise too busy to interact with their colleagues. We are in the process of arranging several fun social functions – ones that may include not only physicians, but also their spouses and children. Please check our website periodically for our upcoming events and to register online.
Fond Regards, David
What’s on your mind? Help us to learn more about emergent trends affecting your work! Write to us at: OurCCMS@gmail.com www. CHESTERCMS .org
Summer 2023 PRESIDENT’S MESSAGE
SUMMER 2023 | CHESTER COUNTY Medicine 3
BRAIN INJURY & OPIOID USE DISORDER: Information & Support

For Professionals
50% of those involved in substance abuse treatment have a history of brain injury, and this estimate is even higher among those who also have mental illness.1

In recent years, opioid misuse has become a significant public health challenge, with many unwanted consequences, including an intersection with brain injury. Opioid use disorder increases the risk for brain injury. Those who are addicted to opioids and/or survive overdose can experience brain damage because of lack of oxygen to the brain, which often happens repeatedly.2 Individuals who misuse substances are also more susceptible to brain injuries caused by falls and violence. Additionally, growing evidence suggests that individuals with brain injuries may be uniquely susceptible to opioid use disorder as a result of their struggles with chronic pain, pre- and post-injury addiction, neurobehavioral challenges, medication mismanagement, and difficulty accessing effective treatment.3

Brain injury impacts an individual’s ability to concentrate, remember, plan, problem-solve, and self-regulate. These neurocognitive challenges leave individuals with brain injury less equipped to participate in and benefit from conventional substance abuse treatment and more likely to experience treatment failures. In fact, research suggests that those with history of brain injury need adaptations to their treatment as well as long-term support in order to succeed. They also benefit from being connected to specialized brain injury services and resources.4
What are we doing?
The Pennsylvania Department of Health is partnering with the Brain Injury Association of Pennsylvania (BIAPA) to raise awareness of the intersection of brain injury and opioid misuse and provide training and consultation to substance abuse providers and professionals who work with individuals struggling with opioid misuse and/or addiction.
How will this help?
By increasing both knowledge and awareness of this issue, we hope to build the capacity of professionals who come into contact with individuals with both substance use disorder and brain injury to identify and treat both problems successfully. This program will also highlight statewide resources.
What will the program do?

• Raise awareness of the intersection of brain injury and substance misuse;

• Provide training to providers and professionals who work with individuals with substance abuse disorder and/or brain injury;
• Offer assistance to providers who want to develop their ability to identify, treat, and/or refer individuals with both brain injury and substance abuse disorder.
For more information
Contact: Tara DiGuilio 717-753-5619 diguilio@biapa.org.
1Dams-O’Connor, K., Cantor, J. B., Brown, M., Dijkers, M. P., Spielman, L. A., & Gordon, W. A. (2014). Screening for traumatic brain injury: Findings and public health implications. The Journal of Head Trauma Rehabilitation, 29(6), 479.
2Corrigan, J. & Sayko Adams, R. (2019). The intersection of lifetime history of traumatic brain injury and the opioid crisis. Addictive Behaviors; 90: 143-145.
3Adams, R. S., Corrigan, J. D., & Dams-O’Connor, K. (2020). Opioid use among individuals with traumatic brain injury: a perfect storm?. Journal of Neurotrauma, 37(1), 211-216.
4Lorenz, L. and Doonan, M. (2019). A Policy Analysis of Access to PostAcute Rehabilitation Services for People with Acquired Brain Injury in Massachusetts and Beyond. Massachusetts Health Policy Forum Issue Brief. This project was funded by the Pa. Department of Health’s Title V Maternal Child Health Services Block Grant.
4 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
Call the Brain Injury Resource Line 1-800-444-6443 This project was funded by the Pa Department of Health s T tle V Maternal Child Health Services Block Grant --
Built for Your Practice

We understand that starting, running, and expanding a practice is no small feat. Our team of Relationship Managers offers years of experience partnering with medical professionals to develop custom strategies that address your distinct healthcare business needs.


CitadelBanking.com/ Healthcare WELCOME TO BETTER
BUSINESS
BANKING
Citadel is recognized as a Forbes 2022 Best-in-State Credit Union. Federally Insured by NCUA.
Ticks… What You Need to Know
BY DR. ERUM ILYAS, BOARD CERTIFIED DERMATOLOGIST
Why do we worry so much about ticks?
Ticks are a worry as they can transmit various diseases. Ticks are tiny and can be frustrating simply because the initial bite can often be missed only to be followed by a number of concerning symptoms – either immediately or delayed.
What are the most common tick-borne illnesses?
The most common tick-borne illness in the US is Lyme Disease. It is endemic in various parts of the country. Ticks are the carrier for the bacteria that causes Lyme disease. They transmit it to humans through a bite and the bacteria can proceed to cause a rash and impact the heart, central nervous system, and the joints, as well as leading to significant fatigue. These symptoms can occur immediately or be delayed – even by months.
The range of other tick-borne illnesses include babesiosis, ehrlichiosis, Rocky Mountain Spotted Fever, anaplasmosis, Southern Tick-Associated Rash Illness, Tick-Borne Relapsing Fever, Tularemia, Colorado tick fever, and Q fever.
Are tick-related illnesses common?
Tick-borne illnesses are considered to be on the rise. However, in practice, I also suspect that they are increasingly recognized
in recent years given the nonspecific nature of the delayed symptoms. I routinely find ticks on patients when performing annual skin cancer screenings. They do not always have evidence of rashes or symptoms, however, there is an ongoing source of exposure in gardeners and others that enjoy outdoor recreation.
What is the best way to protect ourselves from tick-borne illnesses?
When returning indoors, especially if you live in an area endemic to Lyme disease, it is important to perform headto-toe tick checks. Start on the scalp and feel through the hair for any ticks. Feel with your fingers across your neck, face, back, chest, abdomen, arms, and legs. Feel through the folds of the arms and knees while paying special attention to the lower back and back of the neck. Ticks can be tiny – as small as a poppy seed. Feeling for them is better than just looking for them. Look for unexplained rashes. They do not always have symptoms. Some people expect them to feel like a mosquito bite when in fact many have no itching associated. If you have a persistent scab or bump that doesn’t seem to heal or you keep picking at it, it may be worth a check with your dermatologist to make sure a tick isn’t stuck!
It is true that identifying the tick can be helpful as specific ticks are more likely
to transmit specific diseases. However, we are learning more about co-infections and possible exposures to multiple ticks given outdoor activities that make this more likely. I strongly recommend focusing on the symptoms that you experience to guide treatment.

It is common to find that patients either did not have a rash or do not recall a rash. The rash is more a sign of exposure. However, the rash can disappear with or without treatment. If no treatment is undertaken, secondary and tertiary Lyme symptoms can occur where it impacts other organs in the body.
With rates on the rise, how can people protect themselves from ticks?
Pennsylvania routinely tops the list for Lyme diagnoses in the country. I routinely find ticks on patients presenting for routine annual skin cancer screenings and, at times, an incidental target-like rash from Lyme disease. These patients are often genuinely shocked to find out these ticks were feasting on them or that they had evidence of a Lyme infection.
The first line of defense against Lyme is still considered personal protective measures. These include:
• Wearing long sleeves, pants, socks
• Performing tick checks when returning indoors
6 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
PentaHealth is an independent, physician-led group of dedicated providers located throughout Southeastern Pennsylvania who proactively deliver seamless, high quality, and accessible care to all, one person at a time.














www.pentahealth.com








• Take a shower or bath after spending time outdoors
• Placing the clothes worn outdoors in the dryer (set the temperature at high heat) to kill off any ticks still present

• Use of insect repellents while outdoors
• Use of clothing treated with insect repellents
Evaluating your yard or outdoor area can also be helpful to reduce the tick populations in these regions. According to the CDC, it can be helpful to:
• Keep the lawn mowed and clear the brush
• Create barriers between the lawn or shrubs and outdoor recreational areas such as playgrounds. This can be achieved by the use of a 3-foot wide barrier made up of wood chips or rocks.
• Clear trash or unused lawn equipment to avoid hiding areas for ticks
And, of course, check your pets for ticks as well.
I also recommend consideration to Tick Tubes. These can be made at home with toilet paper roll holders, lint from the dryer, and permethrin spray. The lint is used by rodents to make their nests with the permethrin, reducing the volume of ticks in the region.
Do we need any legislation?
The main benefit legislation may serve with regard to Lyme disease would be increasing public awareness of Lyme as well as ensuring insurance coverage for diagnosis, treatment, and management of the disease.













Is it essential to identify the type of tick?

This is a great question. It is true that identifying the tick can be helpful as specific ticks are more likely to transmit specific diseases. However, we are learning more about co-infections and possible exposures to multiple ticks given outdoor
New patients always welcome Appointments available 7 days a week
















Our family caring for your family
Call us first, we are always available 610-423-8181
activities that make this more likely. I strongly recommend focusing on the symptoms that you experience to guide treatment.
Is it possible to have a tick bite without a rash?
It is common to find that patients either did not have a rash or do not recall a rash. The rash is more a sign of exposure. However, the rash can disappear with or without treatment. If no treatment is undertaken, secondary and tertiary Lyme symptoms can occur where it impacts other organs in the body.








SUMMER 2023 | CHESTER COUNTY Medicine 7 www. CHESTERCMS .org
Burnout Defined
BY ANEESHA
We know it is an honor and a privilege to be a physician. But, being a doctor has its pluses and minuses. Many of the stresses of our field can fall under the concepts of burnout and moral injury.

Burnout Defined
Burnout is a workplace syndrome that occurs when certain issues get in the way of a physician’s ability to provide care to his patient. It has three main elements: emotional exhaustion, depersonalization, and low personal accomplishment1. A 2022 Medscape survey of 13,000 doctors in 29 specialties found that 47% of physicians said they felt burnt out. This was up from 42% in 2021. Specialties with the highest numbers of burnout included emergency medicine and critical care. More women experienced burnout vs. men (56% vs. 41%)2
Many factors contribute to burnout. In the Medscape survey, 60% of doctors stated that bureaucratic tasks such as charting and paperwork were the main factor that led to their burnout. Other factors listed were:
• Misalignment of an individual doctor’s goals to the practice’s or organization’s goals
• Workplace violence
• Workload as it relates to hours worked and number of patients seen
• Lack of flexibility and autonomy2
Electronic health records can also be a significant source of burnout. A time-motion study by the American Medical Association showed that 50% of a physician’s workday is spent on data entry or other administrative desk work, and only 20% is spent on direct patient care. Lastly, a lack of professional fulfillment can have a large impact on burnout. This relates to doctors spending less than 20% of their time on the most meaningful aspects of their work.
The results of burnout divide into organizational and individual consequences. On an organizational level, multiple studies have shown that burnout leads to an increase in errors and patient safety events as well as an overuse of healthcare resources such as lab testing and imaging. Also, burnout will lead to a decrease in quality of care and patient satisfaction scores. Burnout threatens the achievement of the triple aim of healthcare – better care, improved population health, and lower healthcare costs3. On an individual level, burnout has numerous physical effects such as
• Lack of sleep
• Substance abuse
• Headaches
• Stress ulcers1
There are also severe mental health impacts of burnout on doctors. Studies show that burnout leads to a rise in mental health conditions such as depression, anxiety, and suicidal thoughts. In the 2022 Medscape survey, 1 out of 5 physicians described themselves as being clinically depressed2. Physician suicide is a tragedy affecting almost 400 U.S. physicians a year. Particularly
8 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
DHARGALKAR, MD, EMERGENCY MEDICINE & PHYSICIAN ADVISOR FOR CHESTER COUNTY HOSPITAL’S WELLNESS PROGRAM FOR PHYSICIANS & ADVANCE PRACTICE PROVIDERS
dangerous is the fact that doctors know exactly how to end their own lives and often have easy access to the means to do so. Therefore, suicide completion rates are 1.4-2.3x higher compared to the general population. Despite being at a greater risk for these conditions, the majority of physicians will not seek help when they need it. Reasons for this include the pervasive view that doctors can deal with their mental health issues on their own without help from a professional, concerns that it will affect state and hospital licensure, and the societal stigma that may occur if colleagues and the community learn about their condition.
The Role of Healthcare Systems
Another way to view the problem of burnout is through the lens of healthcare systems and organizations. This can be viewed as an imbalance of job demands and job resources3. Job demands include
• Excessive workload
• Unmanageable work schedules
• Administrative burdens
• Workflow interruptions and distractions
• Inefficient technology
• Time pressures
• Patient factors
• Moral distress
Job resources include
• Meaning and purpose in work
• Organizational culture
• Alignment of values and expectations
• Job control with flexibility and autonomy
• Professional relationships and social support
• Work-life integration1
Mounting system pressures have contributed to this imbalance where the demands of a clinician’s job are greater than the resources available to complete the job effectively. Internal system pressures include an increased push for performance improvement, technology that hinders rather than supports patient care, and practice policies that do not align with the professional values of doctors1. Factors external to individual healthcare organizations also play a major role in burnout. These factors include complex
legislation, rigid regulatory standards, as well as professional and societal expectations1
Wendy K. Dean, MD (president of the Moral Injury of Healthcare), summed it up best when she stated, “Conversations with hundreds of physicians have shown that the constraints in the system which prevent them from getting their patients the care they need – moral injury – is the primary source of distress. It’s time to stop holding individual clinicians responsible for the dysfunction in the U.S. healthcare system.”
Why Fix It?
Before we talk about the solutions available to address burnout, it is important to outline the argument as to why it is important to improve physician well-being. There is a moral argument to be made about decreasing burnout and improving the well-being of those in our community who care for the health of the rest of society. However, a strong financial argument can also be made.
Multiple studies have shown that implementing strategies to improve physician wellness saves money. It does this in multiple ways. First, retaining doctors and decreasing turnover rates can save a healthcare organization $500,000 to $1,000,000 a year per doctor4. Second, improving well-being can decrease malpractice risk which leads to less money going towards legal fees and settlements. Finally, a Mayo Clinic study of 2,500 physicians showed that in the 24 months after a 1-point rise in burnout or a 1-point drop in physician satisfaction, there was a 30-50% chance that physicians would reduce their professional work effort. By reducing burnout, healthcare institutions can increase productivity, thereby increasing revenue.
Multiple customizable online calculators are available for organizations to determine the cost of physician burnout. These calculators are based on a variety of objective data and can determine the return on investment of interventions taken to reduce burnout in doctors4.
Solutions
Before taking a deep dive into solutions to decrease burnout and improve well-being, we need to set up the foundational principle that individual-focused strategies can be an effective part of larger organizational efforts but do not sufficiently address clinician burnout on their own1. Addressing burnout requires improving the design and organization of the environments in which clinicians train and work. Casting this issue as a personal problem can lead individual doctors to pursue solutions that are beneficial to themselves personally, but detrimental to the
continued on next page >

SUMMER 2023 | CHESTER COUNTY Medicine 9 www. CHESTERCMS .org
Burnout Defined
continued from page 9
healthcare of society as a whole, such as reducing professional work effort. Also, physicians are often skeptical and resistant when individually focused offerings are not coupled with sincere efforts to address the system-based issues contributing to burnout. The Stanford Model of Well-Being shows the three primary factors needed to improve physician well-being:
As it relates to personal resilience, the 2022 Medscape survey showed that 54% of doctors cope with burnout through exercise and 41% of them talk with family members and friends or sleep more2. Physicians keep up with their happiness and mental health in much the same ways. However, the primary way we are going to make real improvements in physician burnout is through unit-level and systems-level changes.
At the unit level, one can use multiple strategies to maximize clinician well-being and mental health. For example, units can foster a positive work environment through clear communication expectations, recognition of employee accomplishments, and promotion of employee wellness programs. Units should implement structured debriefs to process difficult experiences and create peer support networks to promote resiliency and stress management. Lastly, unit leaders can work with their teams to develop meaningful professional connections among colleagues. This will help with learning and professional growth and can include networking events, mentoring programs, and other professional development opportunities5
Most importantly, systemic issues that impact clinician burnout and compassion fatigue need addressing. Leaders of the following groups must all work together to reduce clinician burnout and foster professional well-being.
• Healthcare organizations
• Health professions educational institutions
• Federal agencies
• Health information technology stakeholders
• State licensing boards
• Health system credentialing bodies3
The Clinician Well-Being National Plan, launched by the National Academy of Medicine in October 2022, focuses on the concept of collective action to strengthen health workforce wellbeing. They have outlined the following seven priorities:
• Create and sustain positive work and learning environments and culture
• Invest in measurement, assessment, strategies, and research
• Support mental health and reduce stigma
• Address compliance, regulatory and policy barriers for daily work
• Engage effective technology tools
• Institutionalize well-being as a long-term value
• Recruit and retain a diverse and inclusive health workforce4
A Wellness Program for Physicians and Advanced Practice Providers has been established at Chester County Hospital. Through this program, we strive to eliminate burnout, reduce suffering and promote a culture of wellness for our community by raising awareness, improving understanding, and creating and implementing programs and initiatives. We acknowledge the good work of our physicians through National Women’s Physician Day and Doctor’s Day activities. In addition, reducing stigma around mental health and suicide is a key part of our mission. We do this by organizing an event every September on National Physician Suicide Awareness Day. Finally, we are an integral part of numerous hospital-wide initiatives focused on improving the well-being of all Chester County Hospital staff such as WeCare, a peer support network.
In conclusion, physician burnout is a serious problem that will require collaboration between the national health system, healthcare organizations, hospitals, practices, and clinics as well as the doctors themselves to fix. It may seem daunting but the consequences are too devastating if we are not successful. Even one small step towards improving physician well-being is a step in the right direction.
References
1. National Academy of Medicine. 2019. Taking Action Against Clinician Burnout: A Systems Approach to Supporting Professional Well-Being. Consensus Study Report – Highlights. Washington DC: The National Academies Press. https://nam.edu/wp-content/uploads/2019/10/CR-reporthighlights-brief-final.pdf
2. Kane, Leslie A. Physician Burnout & Depression Report 2022: Stress, Anger, and Anxiety. Medscape.com. https://www.medscape.com/ slideshow/2022-lifestyle-burnout-6014664. Published 2022 January 21. Accessed 2023 July 12.
3. National Academy of Medicine. 2019. Taking Action Against Clinician Burnout: A Systems Approach to Supporting Professional Well-Being. Consensus Study Report – Key Messages. Washington DC: The National Academies Press. https://nap.nationalacademies.org/resource/25521/CR%20 report%20key%20messages%20final.pdf
4. National Academy of Medicine. 2022. National Plan for Health Workforce Well-Being – Highlights. Washington DC: The National Academies Press. https://nam.edu/wp-content/uploads/2022/09/CWBnational-plan-highlights-4-pager-9.27.22.pdf
5. Well-Being Index Team. Unit-level Strategies for Maximizing Clinician Well-Being and Mental Health. mywellbeingindex.org. https://www. mywellbeingindex.org/blog/unit-level-strategies-for-maximizing-clinician-wellbeing-and-mental-health#:~:text=This%20blog%20will%20discuss%20 six,connections%20with%20colleagues%3B%20encouraging%20self%2D. Published 2023 April 19. Accessed 2023 July 10.
10 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
We’re Making Progress in Addressing Maternal Mortality But There’s Still Much More Work to Do
BY STATE SENATOR CAROLYN COMITTA
The birth of a child should be a special time – a joyous occasion for mothers and families. Tragically, too many mothers in Pennsylvania and America face serious and sometimes fatal health consequences due to pregnancy and childbirth-related complications.
We already know that among affluent nations, the U.S. is one of the least-safe countries to have a baby. Sadly, and shamefully, maternal mortality rates continue to trend upward. According to the Centers for Disease Control and Prevention, there were 32.9 deaths per 100,000 live births in 2021, the highest rate in the nation since 1965. Overall, in 2021, 1,205 women died during childbirth or in the six weeks afterward, an increase from 861 in 2020 and 754 in 2019.
Furthermore, this growing crisis is disproportionally impacting women and communities of color. A new study published in the Journal of the American Medical Association shows that the maternal mortality rate in the U.S. more than doubled between 1999 and 2019, with Black mothers consistently bearing the highest burden. Nationally, the maternal mortality rate is two to four times higher for Black mothers than their white counterparts.
While Pennsylvania fared better than some of our neighbors, we still showed a more than 30 percent increase in Black mortality rates during those two decades. A 2022 report from the Pennsylvania Maternal Mortality Review Committee, which reviews all maternal deaths in the Commonwealth, found that
Pennsylvania had an overall pregnancy-associated mortality ratio (PAMR) of 82 deaths per 100,000 live births. Non-Hispanic Blacks had the highest PAMR of 163 per 100,000 live births. In addition, recent national studies are showing significant increases – as much as 44 percent – in maternal mortality for Hispanic women.
In Pennsylvania, we continue to take steps to save lives, provide enhanced care, and support all healthy mothers, babies, and families:
• This summer, the governor signed Act 5 into law, requiring more detailed tracking of the health issues that mothers experience during pregnancy and birth. In addition, Philadelphia is taking steps to require hospitals to share detailed information about pregnancy, delivery, and the parent’s health for patients who experience serious childbirth complications. Knowledge is power and with more information and enhanced data gathering we will be better equipped to save lives.
• In September 2021, I was joined by my friends on the Pennsylvania Women’s Health Caucus and doctors from Chester County Hospital in kicking off our campaign to extend Medicaid coverage from 60 days to one year postpartum for all Pennsylvanians. We succeeded and thanks to federal funding from the American Rescue Plan Act, all mothers in Pennsylvania can now access coverage for up to one year following the birth of a baby.
continued on next page >

SUMMER 2023 | CHESTER COUNTY Medicine 11 www. CHESTERCMS .org
Senator Comitta (right) with Senator Judy Schwank, co-chair of the Pennsylvania Women’s Health Caucus (left), and Pennsylvania Speaker of the House Joanna McClinton (center).
We’re Making Progress in Addressing Maternal Mortality
continued from page 11
Senator Comitta applauds the Pennsylvania Department of Human Services’ decision to opt in our Medicaid program for postpartum individuals at a press conference at Phoenixville Hospital. The change extends Medicaid coverage for postpartum individuals from 60 days to one year following the birth of a child. Pictured on right is Stuart Brilliant,
This is especially important because more than half of the cases of maternal death between 2013 and 2018 impacted mothers enrolled in Medical Assistance when they delivered. And nearly 60 percent of maternal mortality deaths occurred between 42 and 365 days of delivery, many well beyond the standard 60 days of Medical Assistance coverage for pregnant women.
• And although it is currently being delayed, this year’s budget spending plan allocates $2.3 million to expand maternal health programming, including implementing prevention strategies to reduce maternal mortality and morbidity.

Still, we have much more work to do. In a nation and region where medical technology and professionals are worldrenowned, we can lead the way in providing exceptional care for new moms and newborns.
A big part of that challenge is bridging the gap in access to resources, accurate information, and quality care. According to CDC data, about 84 percent of pregnancy-related deaths in the U.S. are preventable. Improving wellness services, access to nutritional support, counseling and exercise, increased screenings for behavioral health and postpartum depression, more home-based and visiting services, breastfeeding support, substance use disorder treatment, childcare service, and access to family planning can greatly improve maternal health outcomes.
In addition, it’s important to meet expectant mothers where they are – literally and figuratively – in terms of prepartum and postpartum services. More than 193,000 Pennsylvanians live in maternity care deserts where a lack of obstetricians, hospitals with delivery units, or birth centers raise the risk of poor maternal and infant health outcomes.

I am a co-sponsor of Senate Bill 355, legislation introduced by state Senator Judy Schwank, that calls for extending Medicaid coverage to doulas. While not clinicians, doulas are trained professionals who can provide emotional, physical and educational support during pregnancy, birth, and postpartum. And there is strong evidence that they can reduce childbirth complications and improve care coordination. Furthermore, community-integrated doulas can be effective in helping reduce racial disparities and bridge cultural gaps in communities of color. At a time when we’re facing a shortage of doctors and nurses, empowering doulas may be an effective strategy for reducing maternal mortality.
Finally, I must emphasize that ongoing attacks on reproductive freedom only threaten to roll back and limit access to reproductive care. While abortion remains safe and legal in Pennsylvania, states that heavily restrict access to abortion have some of the highest maternal mortality rates. Some of the very same procedures outlawed through abortion bans include safe treatment of those who experience ectopic pregnancies, safe and legal fertility treatment, safe procedures for those who suffer miscarriages, and safe and accessible postpartum and birthing care. The bottom line is reproductive health and maternal health are deeply connected with reproductive choice. Like all healthcare choices, these must remain between patients and healthcare professionals. Doctors must be free to do their jobs effectively and all Pennsylvanians must feel safe accessing the full scope of reproductive, perinatal, and maternal health care.
12 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
M.D.
Senator Comitta (right) honors Pam Bryer (left), the first executive director of the Maternal and Child Health Consortium of Chester County, at the organization’s gala event. Bryer gave nearly two decades of service to the nonprofit organization, which works to address maternal and child health disparities in our region.
IT’S YOUR #1 DEFENSE AGAINST ONE OF THE MOST LETHAL CANCERS.
It’s fast. It’s painless. Most insurance will cover it for patients 45 or older. And it could save their lives.

Colon cancer can be deadly when it’s not caught early. But it can be completely eradicated through early detection by colonoscopy. Now, thanks to a GI Genius™-enabled colonoscopy, technology aided by artificial intelligence, doctors at Main Line Gastroenterology Associates can diagnose colon cancer with unprecedented accuracy.

DON’T PUT IT OFF. REFER YOUR PATIENTS FOR A COLONOSCOPY TODAY.
COLONOSCOPY CANCER
Call USDH at 610-644-6755 or schedule online at usdigestivehealth.com.
Recently, my family was blessed with another grandchild – a beautiful, healthy baby girl. We were fortunate that my daughter and granddaughter had access to quality prepartum and postpartum care, as well as a strong family support structure. As I watched them bond over their first days together, I was filled with gratitude for the care they received and the doctors, nurses, and medical workers who all helped ensure a safe and healthy delivery and follow-up care.
And yet, at the same time, I was also painfully aware that for too many Pennsylvanians and Americans those moments are consumed by grief in the loss of a mother – a loss that can echo through an entire family and community.
In Pennsylvania, we can do better and we are working to support healthy mothers, babies, and families. I thank all the doctors, nurses, and medical staff who are vital to that effort. And I look forward to continuing to work with you and all our healthcare professionals to develop innovative strategies and solutions to reduce maternal mortality and save lives.
SUMMER 2023 | CHESTER COUNTY Medicine 13 www. CHESTERCMS .org
Line Gastroenterology Associates
Line Gastroenterology Associates
Carolyn T. Comitta of West Chester serves as State Senator for Pennsylvania’s 19th District and is a member of the Pennsylvania Women’s Health Caucus.
Main
Main
It could be the choice of your patient’s life.
Senator Comitta (left) and U.S. Rep. Chrissy Houlahan (center) talk with doctors and nurses at Paoli Hospital. Comitta worked with fellow state legislators to direct nearly $2.1 million in federal grant funding to the hospital to expand its emergency department.


14 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
Regional Hospital Finance Challenges

 BY JAMES PARADIS, PRESIDENT, PAOLI HOSPITAL, MAIN LINE HEALTH
BY JAMES PARADIS, PRESIDENT, PAOLI HOSPITAL, MAIN LINE HEALTH
The Winter 2023 edition of Chester County Medicine included “Crisis of Healthcare Financing in America” in which Sean V. Ryan, MD, MBA, provided an excellent review of the current financial crisis facing our nation’s healthcare industry and its impact on patients, hospitals, and physicians. Dr. Ryan provided a valuable history of the Medicare and Medicaid system’s development of payment models and the serious financial challenges they create for patients and providers. I would like to add my perspective on our regional hospital industry that reinforces Dr. Ryan’s national cry of alarm.
At the highest level, the financial dilemma facing hospitals is that governmental payors (i.e., Medicare and Medicaid) pay hospitals less than what it costs to provide care to the patients covered by those programs. In our region, Medicare pays approximately 75% and Medicaid pays approximately 60% of the cost of care, respectively. This is neither new nor surprising. Traditionally, hospitals have recognized this underpayment problem and managed it by negotiating payments from commercial insurers that exceeded the cost of care. The higher revenues from commercial insurers offset the losses from governmental payors. This cross-subsidization of governmental payers by private payers allowed Medicare and Medicaid to pay below-cost rates, limited federal and state spending on healthcare, and kept hospitals financially viable. The commercial insurers in turn, passed it on to employers and individual
insurance plan participants in the form of higher premiums, deductibles, and co-payments and limitations of coverage. This implicit social welfare policy meant that employers and their employees subsidized the cost of care for older and poorer Americans. As employers across all industries strive to protect their finances, they have pushed back on insurers to reduce their coverage expenses, and insurers have then resisted increasing payments to hospitals.
Hospitals’ loss of traditional cross-subsidies from commercial insurers creates an increasing financial risk as the senior (i.e., 65+) population in our region grows. The total population in Chester and Delaware Counties has grown only slightly in recent years, but there has been a significant increase in the senior population. Seniors comprise 25% of the population but utilize over 50% of inpatient hospital days. Medicaid patients represent another 16.5% of hospital days; hence, government payers account for two-thirds of hospital days in our region. The senior population is expected to grow by 16.5% over the next 5 years while the rest of the population remains flat. As a result, the portion of hospital services represented by governmental payers is projected to increase to 70-75%. That means that hospitals will attempt to make up for the losses they incur on a larger portion of their patients from a smaller portion of commercially insured patients.
continued on next page >
SUMMER 2023 | CHESTER COUNTY Medicine 15 www. CHESTERCMS .org
Regional Hospital Finance Challenges

continued from page 15
The impact of these financial pressures is apparent in our region. The past three years have seen the closures of Delaware County Memorial and Springfield Hospitals in Delaware County and Brandywine and Jennersville Hospitals in Chester County resulting in a loss of 16% of the inpatient beds in Delaware County and 25% of inpatient beds in Chester County.
In many industries, the closure of businesses in the market would have a positive impact on the remaining players as competition is reduced and demand for their services is increased. However, in this case, the facilities that closed had cared for a disproportionately higher percentage of Medicare and Medicaid patients which contributed to their financial struggles and ultimate closure. As those same patients now seek care from the remaining hospitals in our region, the financial burden shifts to those facilities. To compound the problem,
the remaining hospitals were already busy and did not have adequate facilities or workforce to easily accommodate the new patients. The hospitals were forced to quickly expand Emergency Departments, inpatient units, and staff, further increasing cost pressures.
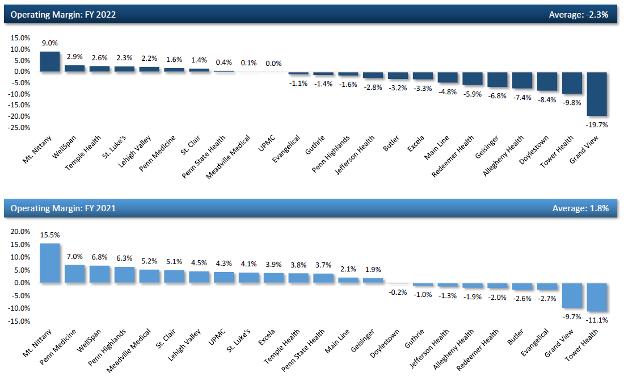
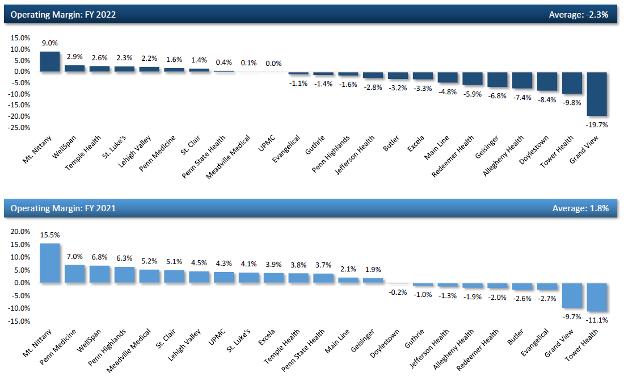
Despite significant cost-cutting initiatives, the economic situation for the majority of health systems in our region remains dire. The table above, from ECHO Financial 2022 Pennsylvania Health System Peer Comparison, shows that the operating margins for Pennsylvania health systems eroded significantly during fiscal 2022 to an average operating income of negative 2.3%. That loss occurred despite most providers still receiving funding from the CARES Act and FEMA related to the pandemic response.
16 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
Learn & Earn with Quality Insights: EARN FREE CMEs/CEs
No-Cost Education Series: Evidence-Based Prescribing: Tools You Can Use to Fight the Opioid Epidemic
The Pennsylvania Department of Health and Quality Insights have partnered to provide LIVE and VIRTUAL education sessions for healthcare professionals.

REGISTRATION IS NOW OPEN: Scan the QR code to visit the Quality Insights website for session dates and registration.

Each module in this training series can be applied to the NEW required eight training hours on the treatment and management of patients with opioid or other substance use disorders, as mandated under the Consolidated Appropriations Act of 2023 for all Drug Enforcement Administration (DEA)-registered practitioners.
This is clearly not a sustainable situation. Most health systems can withstand short-term losses, but they cannot operate in the red for the long term. Our region, unlike areas with robust public hospital systems, relies exclusively on the private sector to provide hospital care. As we witnessed during the height of the pandemic, when there is a major health care crisis our community turns to local hospitals for help. Our medical and hospital professional organizations must continue to work with public officials to help them understand the severity of the current financial crisis and to advocate for changes to the health care funding model at the state and federal level.
Sources:
Pennsylvania Department of Health Inpatient utilization reports

Pennsylvania Health Care Cost Containment Council data

ESRI population demographics FY22-27
ECHO Financial 2022 Pennsylvania Health System Peer Comparison
SUMMER 2023 | CHESTER COUNTY Medicine 17 www. CHESTERCMS .org
Developed by Quality Insights on August 1, 2023. Publication number PADOH-PDMP-080123-GK REGISTER NOW
Kristi Gilfillan
BY BRUCE A. COLLEY, DO
Iam delighted to introduce you to our featured artist for our journal’s summer edition. I was fortunate to spend an hour with her and tour the studio, a well-lit upper floor of an out-building at her beautiful farm in central Chester County. Kristi Gilfillan was born and raised in Chester County and like all the previous artists and craftsmen we have been privileged to feature, she describes an inborn knowledge of a propensity to create. Their media may vary – sculpture, ceramic, painting, cabinet making, photography and such – but they all remember from an early age of 4 or 5 that they could see, hear, and interpret their surroundings, possibly a bit differently from others, then create a rendering of the world as they know it.

Kristi remembers sketching and painting from at least age 4 and describes her paternal grandmother, who lived to 103 and was creating art well into her 90s, as constantly encouraging her. Her grandmom’s art and pastel box are still among Kriti’s most prized possessions. Kristi’s mom, Joan Spillman, still paints regularly with Kristi and continues to be her teacher, critic, and most energetic and admiring advocate. A bit of devil in her as a child, Kristi admits to faking illness so she could skip school and join her mother and grandmom in their plein air art class. Amazingly, some of the members of the original group still paint together in what is now known as “The Artist Circle” and since Kristi is not playing hooky anymore, she is now Co-Chair.

www. CHESTERCMS .org 18 CHESTER COUNTY Medicine | SUMMER 2023
“SPRINGHOUSE” 9"x 12" Oil
“FARM AT THE BEND” 12" x 24" Oil



www. CHESTERCMS .org SUMMER 2023 | CHESTER COUNTY Medicine 19
“ACE” 12" x 12" Oil
“FEELING COOPED UP” 16" x 16" Oil
“SUNFLOWERS” 9" x 12" Oil
The Art of Chester County continued from page 19

Off to Bucknell for college, Kristi majored in math and fine art. Of note, Kristi is the second Bucknell artist we have featured in our journal (see: Gwenn Knapp-Summer 2018 at our website). Moreover, Gwenn was also a math major (I will forgo a paint by numbers joke), but apparently something at Bucknell allows math to equate to art. Not sure how to reconcile her math degree and love of art, Kristi continued her training at Drexel University and earned a master’s in interior design, thus allowing her to use both right and left cerebral hemispheres. Kristi then worked 12 years for interior design and architectural firms, then as an independent consultant until her youngest started school. She then returned to her passion, oil painting mostly full time, but still, she does part time design consulting.

Kristi works primarily with oil paint. Her oeuvres include landscapes, architecture, plein air, still life and animal portraits. She takes inspiration from her many Chester County artist colleagues whom she holds in high regard. Still, her most precious time is spent painting with her mother, and a special mentor, Chester County artist Elise Phillips. Please take time to enjoy Kristi’s art. Perhaps, and only perhaps, you will see intimations of other Chester County artists you know rendered in Kriti’s unique style and accomplished technical skill. Joan, how proud you must be of your daughter, what talent!

20 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
“WELL, ARE YOU COMING?” 16" x 20" Oil
“BOAT DOCK” 24" x 36" Oil
“HARBORVIEW” 30" x 40" Oil
Artist Bio
Kristi graduated from Bucknell University with majors in Studio Art and Mathematics. Continuing on to earn a M.S. in Interior Design from Drexel University, she focused her creative eye on the three-dimensional design of interior spaces. After many years of working full time as an Interior Designer, Kristi redirected her creative focus to oil painting.
Kristi does numerous commissioned pieces each year, especially dog portraits. Over the past seven years she has gotten involved in Plein Air painting events and competitions. Kristi is currently the Chair of The Artists Circle Fine Art Group, a group of 20 female artists, and a member of MAPAPA. Much of her inspiration, both plein air and in the studio, is drawn from the Chester County countryside, Martha’s Vineyard and Nantucket.

Kristi shows her work at Gallery222 in Malvern, Yellow Springs Art Show, The Devon Horse Show, The Artists Circle Art Show, other local shows and at her private studio.

Artist Statement
“I have always loved to draw and paint, but it was not until I had children that I realized the immense gratification I feel from oil painting. Each new piece creates new challenges and sense of accomplishment. Transforming a blank white canvas into a stirring memory, a peaceful landscape, a special place or even an old furry friend is the magic I feel as a painter. The ability art has to transform and enliven a space, is enhanced by my background in both art and interior design.
In a world where so much is constantly moving, may we find tranquility in the presence of art.
My goal is to create pieces that people will feel an emotional connection to and want to enjoy in their own environment. ”
www. CHESTERCMS .org SUMMER 2023 | CHESTER COUNTY Medicine 21 KRISTI GILFILLAN Fine Artist 610.952.7635 kgilfillan2@yahoo.com www.kgilfillanart.com
“CHIP” 9" x 12" Oil
HEALTHCARE
IS WITHERING
BY FRANK SPEIDEL, MD
Hospitals continue to close because they are not financially viable under the current system. Medical research has vastly improved our ability to prevent and treat serious illness; however, the payment for improved services has not kept pace with the interventions. While our doctors and hospitals can provide the gold standard of care, they receive copper for compensation.
The response has been both reflexive and whimsical. Hire consultants with no knowledge of health care, pass legislation increasing closure notification to Pennsylvania Department of Health from 90–180 days. Establish yet another agency to bring greater “accountability to both for profit and nonprofit health care profiteers.”
To be sure, venture capitalists can be involved in the demise of hospitals. One can buy a failing hospital and manage it in a way that optimizes their short-time financial reporting. One can defer maintenance, cut service lines, short inventory, shrink employee benefits. Cutting operating expenses will enhance the income statement and the failing hospital has been turned around. It can then be bundled with other turned-around hospitals, and sold for a profit.
In 2017, Community Health Systems (CHS), which is traded on the New York Stock Exchange, sold five hospitals in southeastern Pennsylvania to Tower Health for $418 million. Before their acquisition by CHS, Brandywine and Jennersville had been independent.
Why have long-standing, essential community assets become prey for predatory acquisition? Because operating as an ongoing hospital costs more than the income they generate from operating as a hospital.
Beyond the turning of the provision of health care into a commodity to be bundled, brokered and speculated, there are other drivers of the contraction of health care in the US. The compensation for providing care has not kept pace with the cost of the care.
Almost all the Philadelphia area health systems have negative operating margins, as reported by Harold Brubaker of the Philadelphia Inquirer. Only the Penn Health System and the Children’s Hospital of Philadelphia have positive operating margins of two percent and eight percent respectively.
Hospitals are closing because they lose money operating. Yet, paradoxically, we are spending more every year on health care. In
the period 2009–2019, national per capita expenditure in constant dollars percentage increase ranged from 3.4 percent in 2015 to 4.3 percent in 2009, according to the CDC. We have become comfortable with and accepted the idea that we are spending too much on health care and we need to limit the increase.
In 1980, the increase in per capita spending was twelve percent. So how can we spend even more per capita, yet hospitals are closing for lack of funds? Is this simply bad management?
The magical thinking that we can drive a Lamborghini at Kia prices leads to increasing bureaucracy, price fixing, and regulatory burden.
One reason is payer mix. The insurance mix of Medicare, Medicaid, private insurance and self-pay of the patients treated by the hospital is a complicated system. Federal and state programs, Medicare and Medicaid set and decide how much to pay for the health care provided. This is a political decision, and the consensus is we are paying too much for health care.
Medicare only pays 84 cents for every dollar of care provided and Medicaid reimburses only 88 cents for every dollar spent, according to the American Hospital Association. Hospitals make up the shortfall of government payment for services by private insurance billing. For a hospital to survive, every Medicare patient seen and treated for a loss of sixteen cents must be balanced by a private patient providing a sixteen-cent profit. The payer mix of the catchment area of the hospital is critical to survival. Areas with higher Medicaid, Medicare and self-pay populations are challenged to stay open.
A more significant reason for the operating loss is the change in services provided, commonly referred to as the “market basket of goods” by economists.
In order to make a diagnosis, patients will frequently get an image such as an x-ray. In the 1970s, to image a patient’s brain, we inserted a needle into the carotid arteries, injected contrast dye, and took a rapid series of x-rays. The procedure was painful, noisy, dripped with complications, and provided sparse information. (Think of the scene in The Exorcist where Meagan has the study.) We now can image the brain and entire body using CT and MRI scans harvesting a tsunami of information all with an order of magnitude and less risk
22 CHESTER COUNTY Medicine | SUMMER 2023
www. CHESTERCMS .org
Article originally published in Broad and Liberty.
and complications. The cost of the now ubiquitous CTs and MRIs dwarf the expenditures for the needles, dye, and x-rays.
In the 1980s, a heart attack was treated with morphine, oxygen, and drugs for irregular heartbeats. It was not very effective, but it was not very expensive. Today, the standard of care for the acute heart attack is percutaneous angioplasty within 90 minutes. Consider the cost to build, equip, maintain, and staff with on-call, high professional personnel the catheterization lab. The ongoing expense to provide this care seismically dwarfs our 1980s best-of-care. The results are equally dramatic.
In Jan. 2017, Circulation Research published an article documenting the continuing decline in cardiovascular mortality in the US seen below.

We can coordinate everything for a complete home look including room, walls and windows or just give you a few ideas.




Stop in or call for an appointment:
717-354-2233
Monday - Friday 10 a.m. - 5 p.m. Saturday 10 a.m. - 2 p.m.
Analogously, we buy a car for transportation as we purchase health care for our well-being. With cars, we may purchase a Kia or we may purchase a Lamborghini. I think it is unreasonable for us to assume we can drive a Lamborghini at Kia prices. In buying a Lambo over a Kia, we are choosing a different “market basket of goods.” Compared to the health care we had in the 1970s, we are roaring along in a Lambo.
We may choose to flatten the rising expenditures for the improving market basket of health care goods by setting Medicare and Medicaid reimbursements below the cost of services. If we choose to do so, as we have, we may expect shortages, wait lines, arbitrage and black markets. The shortages may range from cancer drugs to hospitals. The magical thinking that we can drive a Lamborghini at Kia prices leads to increasing bureaucracy, price fixing, and regulatory burden.
This approach, while having the virtue of being simple, easy, and signaling care, solves no problems. It only accelerates the mismatch expense and compensation for care provided. Solving the problem starts with understanding the problem — understanding based in economics, not whimsy.
Dr. Frank Speidel is a former emergency physician, US Navy Flight Surgeon and recovering hospital administrator (CEO). He is currently a producer and host of “The Doctor Is In” for MLTV 21.
SUMMER 2023 | CHESTER COUNTY Medicine 23
www. CHESTERCMS .org S pecializinginWindowTreatments&HomeDecor! VALANCES • DRAPERIES • SHEERS • BLINDS • SHADES • BED ENSEMBLES • PILLOWS
1064 East Main St. (Rt. 23) | New Holland, PA
www.HeritageDesignInteriors.com
The Detrimental Impact of the Venue Rule Change by Pennsylvania Supreme Court on Physician Shortage
BY DAVID BOBMAN, M.D.
The recent move by the Pennsylvania Supreme Court to change a long-standing venue rule has stirred apprehension within the state’s medical community. The rule, established in 2003, mandates that medical malpractice lawsuits must be filed in the county where the alleged malpractice took place. The proposed change in this rule threatens to escalate an already critical physician shortage in Pennsylvania.

The venue rule was initially introduced to deter “venue shopping,” a practice in which plaintiffs would file lawsuits in counties perceived to be more favorable to their cause, irrespective of where the supposed malpractice occurred. Before the rule, Philadelphia, known for its plaintiff-friendly juries and substantial verdicts, was a common choice for such lawsuits. This led to a malpractice insurance crisis, resulting in soaring premiums that forced many physicians to reduce services, leave the state, or retire prematurely.
The potential change in this rule has sparked fears of a return to the pre-2003 crisis. The Pennsylvania Medical Society and other stakeholders have voiced their concerns that this shift could lead to a dramatic increase in malpractice insurance premiums, pushing physicians, especially those in high-risk specialties like neurosurgery and obstetrics, out of Pennsylvania. This could further intensify the physician shortage in a state already grappling
with an aging physician workforce and a rural population with limited access to healthcare services.
While some argue that the change would enhance patient rights, allowing those affected by medical negligence to seek justice in any county, the potential harm to Pennsylvania’s healthcare system is severe. The state is already experiencing a significant physician shortage. According to the Association of American Medical Colleges, the U.S. could face a shortage of up to 139,000 physicians by 2033, and Pennsylvania, with its aging population and vast rural areas, is expected to be disproportionately affected.
The reversal in the venue rule also threatens to compromise the quality of healthcare services in the state. With fewer physicians, patients may face longer wait times for appointments, reduced access to specialty care, and increased travel times to receive medical care. This could particularly impact rural and underserved communities, exacerbating existing health disparities.
In conclusion, the repeal of the venue rule poses a significant threat to the healthcare system in Pennsylvania given its potential harm to the state’s healthcare infrastructure and the accessibility of care for patients. The theoretical benefits to patients seeking justice in medical malpractice cases must be carefully balanced against the worrisome risk of exacerbating the physician shortage and widening health disparities in the state.
24 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
COLUMN: A health care crisis is upon us, and this one is starting in courtrooms
BY CURT SCHRODER
In the six months since the medical malpractice venue rule went into effect, a staggeringly high number of medical malpractice verdicts are setting off alarm bells around the commonwealth that the state is once again hurtling towards a health care crisis.
The data is clear, the number of medical malpractice cases filed in Philadelphia’s notoriously verdict friendly Court of Common Pleas has sharply increased, as have the number of “nuclear” verdicts.
Not surprisingly, Philadelphia’s notoriously verdict-generous Court of Common Pleas has been a hotbed of activity.
In the first six months of 2023, 300 medical malpractice cases have been filed, surpassing the total of 275 filed for the entirety of 2022.
Meanwhile, regional health systems, including the Hospital of the University of Pennsylvania ($182 million verdict), and Temple University Health System ($25 million verdict), have borne the brunt of these verdicts.
Unfortunately, other parts of the state have not been spared from these negative actions.
In February, a jury returned a $16 million verdict in a Beaver County case, and in Chester County, a jury awarded a plaintiff $19 million in a case.
The trajectory of these verdicts and the frequency is raising alarm bells, leading to comparisons to the late 1990s-early 2000s Pennsylvania medical malpractice crisis.
Skyrocketing jury verdicts often bear no relationship to reasonable
compensation for associated harm.
And often, it’s the plaintiffs’ attorneys who financially benefit the most from these lucrative verdicts.
The ramifications of these verdicts are far-reaching and can lead to increased medical malpractice premiums to cover the costs of these substantial verdicts; defensive medicine and overutilization of tests, procedures or treatments by medical practitioners to protect against potential litigation; a reduction in health care affordability and accessibility; and a shortage of high-risk specialty care as it becomes too risky to practice specialized medicine in the Commonwealth.
Action needs to be taken now before we are in a full-blown healthcare crisis.
The legislature needs to re-examine the concept of caps on noneconomic damages, which was last discussed in the early 2000s.
Attorney contingency fees should be capped, which will allow the injured person to take home more of the award. In the interim, more immediate steps that should be considered include:
• Trial judges should consider granting post-trial motions seeking relief from these verdicts. In 99% of the cases, trial judges do not award any relief at the post-trial stage. Judicial decisions impact not only the immediate parties to a trial but also the entire health care system.
• Judges with medical malpractice experience should be assigned to hear these cases. Medical liability cases are becoming more complicated. Therefore, it is better for the court, the
clients, and the lawyers, to have a trial judge familiar with the issues that arise in these cases preside over them.
• Post-trial evidentiary hearings should be scheduled to address whether the amounts of damages awarded are necessary to compensate victims. The “life care plans” plaintiffs submit — one of which estimated the cost of life care for a single patient to be $100 million — are often unrealistic and bear no resemblance to what the patients, most of whom can obtain insurance to cover the costs, will pay.
• Institute additional rules or guidelines on appeal for determining whether a verdict is “excessive” or “shocks the conscience.”
• Explore the efficacy of setting up a no-fault birth injury fund in Pennsylvania to guarantee medical payments for neurologically injured infants and their families, as an alternative to the jury trial system.
While it is obvious that there will be no “quick fix” to this burgeoning crisis, steps must be taken now to avoid a system collapse.
Anything short of immediate action stands to threaten patient safety, endanger critical healthcare advancements, and risk again, reduction in healthcare in the commonwealth, leaving all its citizens at risk.
SUMMER 2023 | CHESTER COUNTY Medicine 25 www. CHESTERCMS .org
Curt Schroder is the Executive Director of the Pennsylvania Coalition for Civil Justice Reform.
GUEST
DAILY TIMES PUBLISHED: JULY 10, 2023 AT 2:10 P.M. | UPDATED: JULY 10, 2023 AT 8:36 P.M.
Constituent Voter Patience Tenacity Ask Engage Clinical
BY LARRY L. LIGHT RETIRED PAMED LOBBYIST

Do you remember the building blocks you probably played with as a child? If that goes back just a little bit too far, then you might recall the building blocks used by your children or grandchildren. Very likely the building blocks were passed down from one generation to the next. It was commonly accepted that playing with those building blocks was an important, if not vital, element of every child’s early age development.

There are building blocks, essential elements of a political relationship between a policy-making politician and a physician, that are just as significant. And, you’re now at an age where you can understand the role that they play. With the state General Assembly and the Congress having started a 2-year legislative session at the beginning of the year, it’s a perfect time to either start building relationships with your legislators or to take some steps to rejuvenate a relationship that already exists. Here are some of the key building block elements to keep in mind.
Constituents and Voters are important to legislators. The pool of constituents in their district in a sense serves as the committee of the whole in determining whether they are doing a good enough job to be elected. Of course, the boundary lines blur with media coverage in the
newspapers, television news and radio reports, but a responsible legislator will be focused on addressing the interests of his or her constituents, the residents of the legislative district or the entire state for a US Senator. There are immense outside influences on every legislator, from special interests to social media activists, who are not constituents and can easily influence issues and policy decisions. When you want to meet or communicate with a legislator to express your opinion, support or oppose a legislative bill or call attention to a problem, being identified as a constituent and registered voter is an important factor.
Patience and Tenacity are two important characteristics for physicians seeking to build a useful relationship with their legislator. It will become quickly apparent that the legislative process does not move with dispatch. Your patients who are upset at long waits in scheduling appointments and procedures would find the long process of committee and floor amendments and votes in both the House and Senate to be even more daunting. Legislation passes into law only when every box has been checked, from introduction and committee approval to signature by the Governor.
Those immersed daily in the legislative process understand that if you oppose a bill, you only must win one of the multiple votes to derail the proposal. The process
26 CHESTER COUNTY Medicine | SUMMER 2023 www. CHESTERCMS .org
Politics & Medicine
Larry Light is a retired PAMED senior staff responsible for advocacy, governmental relations and political affairs.
is designed to assure that the legislation will have a thorough vetting and to allow each and every member of the legislative body to have input in the final product. The net effect is to provide numerous opportunities to dilute the language through amendments or to win the vote that will bury the bill in committee and effectively kill the legislation. Once a vote is lost, it is almost impossible to recover and reverse the action, so great deliberative care is taken to make certain all of the legislative procedural steps can be completed. Only about 10% of the thousands of bills introduced in a 2-year session are brought up for votes on the Senate and House floor. The process discourages hasty decisions at every turn. It’s not an easy process for physicians to embrace.
Whether you are writing a letter or email to express your support (or opposition) on a legislative issue or meeting personally with the legislator, a guiding principle should always be to Ask for help in addressing the issue rather than telling the legislator what must be done. Having considered the problem at length, physicians and other individuals often fall into the trap of asserting their commitment to a single policy remedy. Legislators soon find that every policy change has multiple implications and
many different invested interests. The key is to focus on addressing the health care problem and working with legislators to achieve a viable resolution to that problem.

If you are seeking to build and maintain a relationship with a legislator, the kind of relationship that will help bring results in the political universe, it will probably help considerably if you find ways to Engage in the political process. Candidates have political campaigns to win elections. The election winners are the ones who decide how the local, state or national government will deal with your issue. Hold a fund raiser to bring together your like-minded professional and personal friends to help the candidate win the election. Take an active part in the campaign by writing a letter to the editor supporting a candidate, or promote the candidate on social media. If the candidate is someone likely to support your position or issue or already has done so, then you’re making an investment as a citizen in the political process. This is how those who are not running for office have input into the political process.
When physicians engage in the political process their Clinical expertise brings a unique skill set to the debate. That also applies to political relationships.
As the relationship develops you can expect to be the go-to contact for the legislator, asked to provide insight on an extremely wide vista of health care issues. Your accessibility to connect and respond will certainly be a positive factor when issues of direct concern to you are on the table. From another perspective, your ability to bring into focus key clinical aspects of a health care issue will make your arguments pro or con even more effective. Your clinical training and experience are widely recognized as credible resources.
These are certainly unusual times in the political universe, particularly at the state and national levels. Political candidates often find themselves fighting more desperately to satisfy their political base than to attack their opponent. Campaigns are often driven by social media generated by sources not directly affiliated with the candidate. The same forces are at play in the legislative process as the primary element framing legislative issues has drifted from solving problems to forcing the other party to make “bad votes.” In that milieu it becomes even more important for physicians to seek opportunities to develop political relationships that will facilitate addressing health care issues that are important to your patients and your practice.
SUMMER 2023 | CHESTER COUNTY Medicine 27 www. CHESTERCMS .org
Congenital Syphilis
BY WILLIAM F. KRAMER, D.O., CHESTER COUNTY PUBLIC HEALTH PHYSICIAN
Congenital syphilis occurs when the spirochete Treponema pallidum is transmitted from a pregnant woman to the fetus. Infection can result in stillbirth, prematurity, or a broad spectrum of clinical manifestations. Only the most severe clinical cases are apparent at birth.
Incidence
Congenital syphilis is a significant public health problem, affecting approximately one million pregnancies per year worldwide. Most cases occur because the mother received no prenatal care or insufficient treatment for syphilis before or during pregnancy. Among women with untreated early syphilis, 40 percent of pregnancies result in spontaneous abortion. Rates of congenital syphilis in the USA have risen sharply since 2012. This increase parallels increases in primary and secondary syphilis among women during this period. The 2020 case rate, 57 cases per 100,000 live births, is the highest reported rate since 1991.
Risk Factors
Maternal risk factors for syphilis during pregnancy include sex with multiple partners, sex in conjunction with drug use or transactional sex, late entry into prenatal care (first visit during the second trimester or later) or no prenatal care, methamphetamine or heroin use, incarceration of the woman or her partner, and unstable housing or homelessness.
Poor access to prenatal care is an important risk factor for congenital syphilis. The CDC reports at least one-quarter of
reported cases received no prenatal care. Among cases in which the mother received prenatal care, roughly 40 percent received no treatment for syphilis during pregnancy, and more than 30 percent received inadequate treatment. The most common missed opportunity for prevention of congenital syphilis is the lack of adequate maternal treatment despite timely diagnosis.
The rate of congenital syphilis is increased among infants born to mothers with HIV infection. The rate of congenital syphilis is generally low among children adopted internationally; however, it is increased among those adopted from Africa. Screening all international adoptees for congenital syphilis is recommended, regardless of country of origin.
Clinical Manifestations
Clinical manifestations before two years of age are consistent with early congenital syphilis. Clinical findings of untreated infants usually appear by three months of age, most often by five weeks. Live born neonates with congenital syphilis are asymptomatic at birth in 60-90 percent of cases. The presence of signs at birth depends on the timing of intrauterine infection and treatment. The most common findings in symptomatic infants include hepatomegaly, jaundice, nasal discharge (snuffles), rash, generalized lymphadenopathy, and skeletal abnormalities (pseudoparalysis of Parrot, Wimberger sign).
Clinical manifestations after two years of age are consistent with late congenital syphilis. Late congenital syphilis develops in approximately 40 percent of infants born to women with untreated syphilis during pregnancy. Most manifestations are

www. CHESTERCMS .org 28 CHESTER COUNTY Medicine | SUMMER 2023
prevented by appropriate treatment of the mother during pregnancy or treatment of the infant within the first three months of life. Manifestations include facial features (frontal bossing, saddle nose), ophthalmologic (interstitial keratitis), hearing (sensorineural hearing loss), oropharynx (Hutchinson teeth), cutaneous (rhagades), neurologic, skeletal, and hematologic.
Evaluation and Diagnosis
The CDC and the American Academy of Pediatrics, AAP, provide guidelines for the evaluation and management of congenital syphilis. The CDC guidance details evaluation and treatment of neonates born to mothers with syphilis. Four scenarios are offered, from confirmed congenital syphilis to congenital syphilis unlikely, with detailed work up and treatment recommendations required for each scenario.
After treating a pregnant woman for syphilis at the Chester County Health Department, a letter detailing the evaluation and treatment of the patient is sent to her Ob/Gyn along with a copy of the CDC guidance to be referenced in the care of the newborn.
Testing
The PADOH recommends that all pregnant women be tested for syphilis at the first prenatal visit, at the third trimester of pregnancy, and at the delivery of the child, or at the delivery of a stillborn child. Pennsylvania law requires the attending physician to offer the woman a test for syphilis at the time of the first examination.
Any woman who has a fetal death after 20 weeks’ gestation should be tested for syphilis. No mother or neonate should leave the hospital without maternal serologic status having been documented at least once during pregnancy.
The PADOH recommends that all patients of childbearing age presenting with any of the following should be tested for syphilis: macular/popular rash of hands or soles, generalized macular, popular rash, lesion of genital, rectal, oral area, moth eaten scalp alopecia, loss of eyelashes, lateral third of eyebrows, generalized lymphadenopathy, malaise, or recent positive test for another STD.
Treatment
Syphilis can be treated effectively with a penicillin regimen that is both appropriate for the stage of syphilis and initiated 30 days or more before delivery. Pregnant women diagnosed with syphilis should be treated immediately. Their sex partner(s) should also receive treatment to prevent the mother from becoming reinfected and to improve the health of her partner. Infants exposed to syphilis during pregnancy must be thoroughly evaluated at birth, as described above, and receive effective penicillin treatment if indicated. These infants should also be closely followed post-delivery, regardless of initial evaluation or treatment, because infants with congenital syphilis may not have any initial symptoms at birth
but later develop symptoms of congenital syphilis if not treated appropriately. Infants with congenital syphilis who are not treated within the first three months of life are more likely to have lifelong complications of congenital syphilis such as blindness, deafness, and intellectual disability.
Summary

Congenital syphilis is a preventable disease that is on the rise for multiple reasons. Women of childbearing age are the fastest growing group of syphilis patients in the USA. Multiple risk factors are present. Some patients may have been infected in the distant past and don’t recall any symptoms or had symptoms that resolved without testing or treatment. Early testing of women at risk with prompt treatment will prevent congenital syphilis and avoid complications or death of neonates.
Information is referenced from CDC and PADOH guidance, and UpToDate.
William F. Kramer, D.O., Chester County Public Health Physician wkramer@chesco.org (610)-344-6230
www. CHESTERCMS .org SUMMER 2023 | CHESTER COUNTY Medicine 29
BY CHRISTINE MEYER, M.D.
The other day, I spent way too much time trying to dry some lettuce leaves for a salad (yes, I know, this is the Chester County Medical Society publication – stick with me). Anyway, after having the thought and failing to act on it MANY times, I decided I HAD to have a salad spinner.
Given my menopause brain (attention span: zero), I grabbed my phone, opened my Amazon app and ordered the highest rated salad spinner.
None of this is earth shattering information. What was, is that the package arrived on my door step two hours later.
I had a need and through an app on my phone, it was met in just a few hours.
That is the beauty and genius of Amazon Prime. If you need something and are willing to take the most available brand or color or size, you can have it in less time than it would take to drive to a retailer.

Nearly 19 years after starting it, sometimes, my practice feels like Amazon Prime. If you call or text in the morning, there is a very, very high likelihood you will get an appointment within a few hours – as long as you are willing to see the next available provider and aren’t too particular about the time of the appointment. You can be seen on a Sunday, early in the morning, or late at night. If you don’t necessarily want to sit on the phone, you can send a message directly to your provider via the patient portal and get a response, usually the same day. If you
want to pay your bill instantly, you can head to our website and do so in moments.
These conveniences are huge selling points for our practice. And, I am proud of the level of accessibility we have been able to achieve.
The thing is, even though I use Amazon many times per week, I actually LOVE Etsy.
When I want something personalized and made JUST for me, whether it is a pile of t-shirts for a family trip, or a unique piece of jewelry for a gift, I don’t go to Amazon, I go to Etsy. You can find “exquisite,” “customizeable,” “personalized,” and “one of a kind” items. BUT, you have to be willing to wait. You have to plan ahead. If you need your thing fast or now or immediately, Etsy will let you down.
Nearly 19 years ago, when I started my practice, it was more Etsy than Amazon. It was just me for 5 years. I was the only clinician in the office, was on call every night, every weekend, and every holiday. In turn, I knew every single patient intimately. I knew their stories, their medical history, and their families. Seeing my patients at the grocery store or on the trail or at a restaurant was a treat for me. I felt connected. I felt seen. I felt like my community chose me for me. NOT for my immediate and constant availability.

As the practice grew, my team grew along with our availability. In the last several years, I have come to spend less

www. CHESTERCMS .org 30 CHESTER COUNTY Medicine | SUMMER 2023
time seeing patients myself and more time managing the practice of 20+ clinicians. If I am recognized in the store or at a restaurant now, it is by the picture on my website or Facebook or Instagram. People are still, for the most part, kind and appreciative. But they also say things like “Oh! You ARE real!” or “I’ve gone to your practice for years but have never met you!” or “Huh. I thought you were just the name on the door.”

Hearing these things chips away at me. I carry those tiny comments around. Sometimes, I brush them off as “the cost of doing business.” Many times, I find myself questioning many of my life choices.
When I started out, I was like that Etsy artist. I intended to give every patient exactly what they needed from ME. I saw them in the office and in the hospital. I called them back myself at all hours and did so happily. But, the price for that was so high. I was a young solo practitioner with small kids. Taking those patient calls interrupted dinner times. Running over to the hospital meant missing recitals and T-ball games and family gatherings.
Now, our patients get what they need more often from people other than me. I still see patients three days per week but I don’t go to the hospital anymore and very rarely take calls.
My practice has become more Amazon than Etsy and I absolutely regret the lost personal connections I had with patients.

But, at 51 years old, my LIFE has become more ETSY than Amazon. I have much more time for my family and my passions. I drive my youngest daughter to school every day and am there when she gets home most days. I get to see her face and know how her day was. I NEVER miss a single event and can’t remember the last time my dinner conversation was interrupted by a patient call. The thing is that I have THREE kids. My older two are out of the house and will never get to experience THAT version of me. And I absolutely regret the lost connections I could have had with my older two.
I never set out to build an Amazon practice but a lifelong Etsy practice was just not sustainable for me. When I think about my career and life, I do have some regret but I also have mountains of pride. My older kids appreciate the work, determination and grit it took to build a successful small business. My youngest daughter appreciates our morning rides and the uninterrupted dinners –dinners I make nearly every night from scratch. I still work a lot but I also do a lot of living my life.
So, would I rather have Etsy or Amazon?
The truth is, there are times for both. The trick is recognizing and then embracing them.
Christine Meyer and Associates 750 W. Lincoln Highway Exton, PA 19341

Christinemeyermd.com

Reach Your Audience... Reach 35,000+ Engaged Consumers Plus, 3,500+ Physicians, Dentists & Practice Managers Throughout Chester County www.Hoffpubs.com Advertise in YOUR COMMUNITY RESOURCE FOR WHAT’S HAPPENING IN HEALTH CARE SUMMER2023 Published by Pennsylvania’s First Medical Society OpioidBrainInjury& InformationUseDisorder: &Support For Professionals Burnout Defined WhatTicks… You Need to Know p4 6 8 Kristi Gilfillan p18 Reach out to us today! Tracy Hoffmann 610-685-0914 x201
www. CHESTERCMS .org SUMMER 2023 | CHESTER COUNTY Medicine 31
When it comes to MRI providers, there is a difference.
MRI Group has a long tradition of excellence: Accurate image reading. Collaborative, highly trained physicians. Exceptional patient experience. Affordable rates.
• Images read by local radiologists
• Radiologists available 24 hours a day, year round, to read images and provide consultation
• All MRI Group locations are ACR accredited
• All radiologists are board certified by American Board of Radiology
• Experts in various radiology specialties including cardiovascular, interventional, neuroradiology, vascular, musculoskeletal, and pediatric imaging
• Evening appointments available
MRI scans performed at our Parkesburg location
• Abdomen
• Brain
• Chest
• Extremity
• Joint
• Magnetic Resonance
Angiography (MRA)
• Pelvis
• Spine
Phone: 717-291-1016
Fax: 717-509-8642
MRIGroup.com
Several locations in Lancaster County and Chester County
CHESTER COUNTY LOCATION: 950 S. Octorara Trail, Parkesburg (Intersection of Routes 30 and 10)
We are located at the Penn Medicine Lancaster General Health Parkesburg outpatient facility.



 BY DAVID E. BOBMAN, MD PRESIDENT OF CHESTER COUNTY MEDICAL SOCIETY
BY DAVID E. BOBMAN, MD PRESIDENT OF CHESTER COUNTY MEDICAL SOCIETY


















































































 BY JAMES PARADIS, PRESIDENT, PAOLI HOSPITAL, MAIN LINE HEALTH
BY JAMES PARADIS, PRESIDENT, PAOLI HOSPITAL, MAIN LINE HEALTH