
Ban on Noncompetes at the Pennsylvania and Federal Level: How Will They Relate? p 6


Ban on Noncompetes at the Pennsylvania and Federal Level: How Will They Relate? p 6

Medical Emergency Response in Chester County: Physician Observations and Recommendations from the Covid Pandemic p 9
Falls: A Leading Cause of Accidental Death p 12





















































President
David E. Bobman, MD
President Elect
Mahmoud K. Effat, MD
Vice President
Richard O. Oyelewu, MD
Treasurer
Winslow W. Murdoch, MD
Secretary
Christina J. VandePol, MD
Editor & Immediate Past President
Bruce A. Colley, DO
Board Members
Norman M. Callahan, III, DO
Heidar K. Jahromi, MD
Mian A. Jan, MD
Manjula K. Naik, MD
Lynne A. Stilley, MBA
Executive Director
Chester County Medical Society 1050 Airport Road PO Box 5344 West Chester, PA 19380-5344
Website – www.CCMS.org Email – chestercomedsoc@gmail.com
Telephone – 610.389.4222
Chester County Medicine is a publication of the Chester County Medical Society (CCMS). The Chester County Medical Society’s mission has evolved to represent and serve all physicians of Chester County and their patients in order to preserve the doctorpatient relationship, maintain safe and quality care, advance the practice of medicine and enhance the role of medicine and health care within the community, Chester County and Pennsylvania.
The opinions expressed in these pages are those of the individual authors and not necessarily those of the Chester County Medical Society. The ad material is for the information and consideration of the reader. It does not necessarily represent an endorsement or recommendation by the Chester County Medical Society.

BY DAVID E. BOBMAN, MD PRESIDENT OF CHESTER COUNTY MEDICAL SOCIETY

David E. Bobman, MD, FACP, AGAF President, Chester County Medical Society
Artificial intelligence. This is a term that conjures up a plethora of ideas and emotions. To some, this evokes sci-fi images, at times unnerving, similar to HAL in 2001: A Space Odyssey, or of Arnold Schwarzenegger’s role in the Terminator movies. Others may see this in a more hopeful light, as the technology of the future, helping and improving our abilities in a variety of areas.
In an excellent article by Jesse Corn of Forbes Business Counsel, he writes, “From predictive and personalized treatment plans to models for early diagnosis, AI is already transforming the healthcare sector in unprecedented ways.” However, as with any technology, there are pros and cons. We are seeing this appear in many areas including glucose monitors, smart watches, EKG interpretation, and assisting in reading mammography, to name a few. Another important area includes monitoring for prescription drug interactions or contraindications. AI also may improve efficiency in our offices by assisting in scheduling, billing, and voice recognition software.
On the other hand, using artificial intelligence raises many concerns. Among them includes patient privacy and security of records. While artificial intelligence does amazing things (eg. Chat GPT) the accuracy of its content is not always correct. This may lead to diagnostic mistakes if its results are not well vetted. Furthermore, this creates a legal dilemma as to who, or what, is responsible for these errors. Additionally, artificial intelligence may lead to a loss of jobs, not only in medicine, but also in many fields of employment. These issues are illustrated by a recent nursing protest in California (Kaiser Permanente - San Francisco) which occurred over these concerns – both accuracy of its results and loss of nursing jobs.
Like it or not, incorporation of artificial intelligence technology into medical care is here to stay. As with any new technology, we need to proceed slowly and carefully to see that appropriate safeguards are in place. As many of us, myself included, are relative neophytes to this technology, the Chester County Medical Society will be hosting Dr. Kevin B. Johnson, MD, at our annual physician dinner on September 19. His degrees and accolades are too numerous to mention here, though he is VP for Applied Informatics in the University of Pennsylvania Health System. He will be speaking on “Utilizing AI to help Doctors Doctor: Opportunities and Challenges.” We expect this will be a terrific presentation and encourage anyone interested to attend.
Fond Regards, David



BY VASILIOS J. KALOGREDIS, ESQ., AND SONAL PAREKH, ESQ.


On April 17, 2024, House Bill 1633 (“HB 1633”) was passed by the Pennsylvania House of Representatives (the “House”) and referred to the Senate. Introduced on August 29, 2023, HB 1633 (as amended) prohibits the enforcement of certain noncompete covenants entered into by health care practitioners and employers. If passed, this will be the first Pennsylvania law expressly limiting noncompetes in the health care industry.
A noncompete covenant, or restrictive covenant, generally prohibits a former employee from competing against his/ her former employer within a particular geographic area for a specified period of time. When used in the health care field, these covenants are often onerous in both geography and duration, which can result in significant negative impacts such as forcing patients to break long-term relationships with their health care providers and/or exacerbating the ongoing staffing shortage in the health care industry.
Consolidated hospital systems increasingly stretch over broad geographic regions, meaning that a network’s noncompete clause can prevent healthcare practitioners from practicing in large areas of the Commonwealth, well beyond their initial employment location. Given that seventy-five percent of

PentaHealth is an independent, physician-led group of dedicated providers located throughout Southeastern Pennsylvania who proactively deliver seamless, high quality, and accessible care to all, one person at a time.
www.pentahealth.com







































physicians are employed by hospitals, health care systems or corporate entities, noncompete covenants in healthcare (i) inhibit competition that benefits employees and patients and (ii) can deter needed healthcare practitioners from wanting to practice within the Commonwealth. It is the position of the House that continuity of care is a fundamental public policy goal and therefore the Commonwealth cannot afford to continue losing health care practitioners to surrounding states and patients should not lose their local doctors.
Accordingly, pursuant to HB 1633, the Fair Contracting for Health Care Practitioners Act (the “Act”) provides that a noncompete covenant entered into or amended prior to the effective date of the Act is void and unenforceable upon the renewal of a health care practitioner’s license, registration or certification within the Commonwealth. A noncompete covenant entered into or amended after the effective date will be deemed contrary to public policy and void and unenforceable by an employer. The Act provides an exception to this rule if: (i) the primary health care facility or office where the health care practitioner is employed is located in a county of the sixth, seventh, or eighth class1; (ii) the geographic restriction is less than a 45-mile radius from the primary health care facility or office; and (iii) the length of the noncompete covenant is no




















more than two years. The Act makes it clear that its provisions do not prohibit the enforcement of a contract provision that allows an employer to recover reasonable expenses from a health care practitioner, subject to certain conditions.
Additionally, within ninety (90) days of a health practitioner’s departure from an employer, the Act requires an employer to notify the health care practitioner’s patients (that were seen within the past year) of: (i) where the health care practitioner will be rendering services in the future (if known); and (ii) how the patient may continue as a patient of the health care practitioner, or be assigned with a new health care practitioner within the existing employer. The notification requirement is to apply to a physician, certified registered nurse practitioner (“CRNP”), or physician assistant (“PA”) with an ongoing outpatient relationship with the patient.
If passed, the Act will take effect immediately with the notification requirement to take effect 30 days thereafter.
Interestingly, one week after HB 1633 was passed by the Pennsylvania House of Representatives, on April 23, 2024, the Federal Trade Commission (“FTC”) approved a final rule broadly banning all employee noncompete clauses, subject to a few exceptions, to be effective September 4, 2024. Specifically, continued on next page >
continued from page 7
the final rule will not apply to noncompete agreements for senior executives (i.e., workers earning more than $151,164 annually who are in a “policy-making position”) that are already in existence. The final rule will also not apply to noncompetes (i) entered into pursuant to a bona fide sale of a business entity, (ii) by a franchisor and franchisee, or (iii) restricting a worker’s ability to compete outside of the United States. The final rule will not affect trade secret laws, non-solicitation agreements or non-disclosure agreements which may serve as alternatives to noncompetes. Further, the rule will not apply to nonprofit companies outside of the FTC’s jurisdiction, which includes many of the hospitals and some of the biggest health insurers in the United States. Though the final rule is already facing numerous challenges, with more expected to come, if not overturned, the final rule will preempt HB 1633.
A physician may be considered to be a senior executive only in limited circumstances. A policy-making position means a business entity’s president, chief executive officer or the equivalent, or other person who has the ability to make decisions that control a significant aspect of the business entity. Here, a physician owner of a medical practice may be considered to be a senior executive only if he or she serves in these identified roles or has policy-making authority over the entire business (as opposed to a specific division or department). Therefore, whether a physician will be considered to be a senior executive will require a deeper legal analysis.
Further, a non-competition clause may be enforceable if it relates to a scenario where a physician owner sells his or her ownership to an independent physician practice because it is pursuant to a “bona fide sale of a business entity, of the person’s ownership interest in a business entity, or of all or substantially all of a business entity’s operating assets.”
Regardless of the exceptions enumerated by the FTC, the FTC has taken the position that if a noncompete clause is so broad that it effectively functions to prevent a worker from seeking or accepting work or operating a competing business in the United States after the conclusion of employment, the clause may be unenforceable under other laws, including antitrust, even if it would be exempt from the FTC’s final rule.
With regard to the applicability to nonprofits, the FTC has stated that it has no jurisdiction over most nonprofits, and therefore a nonprofit health system may still be able to enforce its noncompetes with physicians and other employees. However, it is currently unclear which entities and/or nonprofits will fall within and outside of the FTC’s jurisdiction. Because both judicial decisions and FTC precedent recognize that not all entities claiming tax-exempt status as nonprofits fall outside the
FTC’s jurisdiction, the FTC left open the possibility of enforcing the final rule against some tax-exempt entities that effectively operate as for-profit enterprises in the future. This may include hospitals and/or health systems. Until this is explicitly clarified as otherwise, these entities may remain immune from the noncompete ban.
However, if Pennsylvania passes HB 1633, it will permit for a stronger ban on noncompetes in Pennsylvania. Because HB 1633 is narrower (or stricter) in scope, it will not be preempted as it relates to nonprofit hospitals and health systems. Given that the General Assembly noted its intent to have the noncompete covenant apply to hospitals and health care systems with overly broad geographic regions, it may be possible to expand the reach of the FTC’s noncompetes to include such health systems and hospitals within the Commonwealth of Pennsylvania. Whether or not HB 1633 is passed, employers should be sure to adhere to required obligations, such as providing notice to covered workers, under the FTC’s final rule.
Stay tuned!
*This article is for educational purposes only and is not intended to be legal advice. All information provided in this article is current through May 15, 2024. Should you require legal advice on this topic or any other health law topic, or have any questions or concerns, please contact Vasilios J. (Bill) Kalogredis, Esq., or Sonal Parekh, Esq.
Vasilios J. (Bill) Kalogredis, Esq., has been advising physicians, dentists, and other health care professionals and their businesses as to contractual, regulatory and transactional matters for 50 years. He is Chairman of Lamb McErlane PC’s Health Law Department. Bill can be reached by email at bkalogredis@lambmcerlane.com or by phone at 610-701-4402.
Sonal Parekh, Esq., is an associate at Lamb McErlane PC who focuses on health care transactional matters and a broad range of health care regulatory-related issues on behalf of health care systems, physicians, dentists, and other health care providers, and is a pharmacist by education and training. Sonal can be reached by email at sparekh@lambmcerlane.com or by phone at 610-7014416.
1 A summary of each Pennsylvania County Class can be found on the Pennsylvania Courts website at https://www.pacourts.us/news-and-statistics/ research-and-statistics/dashboard-table-of-contents/resources/WebHelp/ General_Information/County_Classes.htm.
BY FRANK SPEIDEL, M.D., AND BRUCE A. COLLEY, D.O.

Beginning in 2020 our country and county were devastated by a novel respiratory pathogen, the SARS CoV-2 virus. We saw over a million Americans die, the economy derail and education crater.
Curiously, there have been few analyses of the pandemic and the response to it by any organization, agency, or municipality. In 2021 there was a majority staff report of the Senate Committee on Homeland Security and Governmental Affairs. And In 2022 CDC Director Rochelle Walensky, MD, ordered a review of the CDC’s performance during the pandemic.
Because there have been few critiques, in September 2022, the authors and a volunteer group of our physician colleagues began a review of the pandemic. This group, the Medical Emergency Response Workgroup (the Committee), endeavored to review and understand the pandemic and the response on the national, state and mostly the county level. The intent is to improve our future response to adverse events.
In this undertaking, the Committee surveyed municipalities, organizations, agencies and individuals in Chester County and surrounds. The written survey asked broad questions, regarding what we did well, what we could have done better, and what improvements to the overall mitigation strategies to the COVID pandemic the respondents thought would have been beneficial. We also asked respondents to share their thoughts and concerns, and to make suggestions as to how Chester County’s medical community and government entities might have improved their attempts to mitigate the COVID pandemic. We also invited general comments as to how Chester County can prepare for
future health or safety challenges. The committee allowed for anonymous and verbal responses.
In addition to surveying widely, the Committee reviewed published literature, both lay and scientific. The surveys and literature were used by the Committee to identify issues and drivers of the pandemic. The following is a summary of the Medical Emergency Response Workgroup’s findings (observations) and recommendations.
The Committee thought the global response to the pandemic exceeded expectations in two areas, clinical care at the bedside and the rapid vaccine development.
Some might see the comments about clinical care as being self-serving. Not so. Consider the December 2022 Homeland Security & Governmental Affairs (HSGA) report Historically Unprepared, Examination of the Federal Government’s Pandemic Preparedness and Initial COVID-19 Response. On page 9 of the of the report’s Executive Summary the authors write, “In addition, the tireless and ongoing work of frontline health care workers and officials fully engaged in the response saved countless lives.”
continued on next page >
continued from page 9

The rapid vaccine development is also recognized in this report. The authors wrote, “Operation Warp Speed swiftly and successfully coordinated with the private sector to develop a vaccine for the novel COVID-19 virus in record time, building on years of prior federal investments in scientific research, and was widely considered to be a resounding success.”
The Committee identified five opportunities for improvement: leadership, decision process, communication, review, and preparedness.
In leadership, the Committee noted an absence of meaningful preparedness and response. Misinformation and contradictions abounded; directions were frequently opaque and authoritarian. Leadership must always be anchored in honesty and act to identify the goals and the value of those goals. Moreover, leadership must embrace the understanding of the mission and actions needed to achieve the goals and to communicate the mission to the team. This was rare in the pandemic response. Frequently the goals were not identified or they changed without explanation.
The Committee sensed directives were issued in the absence of evidence, despite the growing body of evolving clinical evidence regarding the transmission, diagnosis, and treatment of COVID. In some circumstances decisions arose from citing authorities, not science. Moreover, in too many cases, the decision process ignored collateral effects and was indifferent to balance and proportion. In general, at every level the decision process suffered from a “silo effect” where a closed group makes decisions without diverse input.
In the Committee’s opinion, communication from the controlling governmental authorities was inconsistent, contradictory, and lacking precision and nuance. Communication at times was unidirectional, authoritative, and dismissive of dialogue. The Committee also noted the media prioritized ratings over “getting it right,” embracing the sensational over content. This detracted from an effective pandemic response.
The Committee noted the absence of publicized review at many levels. There were a few exceptions. On the national level in April 2022, Dr. Rochelle Walensky directed a review of the CDC’s response. The aforementioned HSGA report of December 2022 looked widely at the pandemic and our response.
At the county level there has been a Brown, McGarry, and Nimeroff law firm report on Antibody testing and a Health Department commissioned report by the Drexel University Dornsife School of Public Health on public health risks in Chester County.
At all levels preparedness was absent and evident. The Pennsylvania Department of Health Influenza Pandemic plan we found to be dated 2005 and all pages were watermarked “DRAFT.” Published Emergency Operations Plans were incomplete and unreviewed. The HSGA December 2022 report documents the extensive failure of preparedness.
In reviewing the missed opportunities in leadership, decision process, communication, review and preparedness, a telling example was the failure early on in delivering the COVID vaccine to Chester County’s most vulnerable citizens. The difficulty arose due to the complexity of obtaining and administering the vaccine by front line physicians in the wider community.
In a Disaster Utilize All Resources, Both Public and Private, Near and Distant
Chester County is the wealthiest county in the Commonwealth. Our economic power is a propitious asset, but the real wealth is in the people. We have massive human resources, chemists, physicists, infectious disease specialists,
veterinarians, etc. When things go bad, know where to find them and use them all.
Communications Reinvented and Exercised
Communication is in all directions and barrier free. Silothinking is the enemy of effective response to problems.
Tools to evaluate effectiveness of communication should be developed and used. Consider adopting and teaching Crew Resource Management (CRM).
Regular periodic exchanges among stakeholders should be scheduled. The mechanisms and procedures to have emergency on-need-basis interactions among the medical community, academia, government, industry, and the public at large should be well-established. Communication beyond usual operations should be regularly exercised and evaluated. Agree to disagree.
Identify and work together to address shared issues of concern with all stakeholders in Chester County, such as:
• Access to Healthcare is contracting, as such, the available state-of-the-art care that was typically found in Chester County is cratering. This would be an obvious initial joint endeavor. Most obviously, the reopening of Brandywine and Southern Chester Chester County Hospitals.
• Opiate misuse
• Disaster response planning is another (National Disaster Life Support Courses)
Stakeholders’ Initiation Meeting
Invite Chester County governance, directors, agencies, institutions, NGOs and professional societies to participate in a day-long working seminar to explore, plan and actualize recommendations one, two, and three.
The COVID-19 epidemic began as a disease and health care event. The response, however, was distinctly non-physician lead. Apart from our Chester County Health Department, which
was, as we must remember, pressed into service to manage the COVID crisis in both Chester and Delaware County; there was shockingly little direction from the CDC, state health department, the national medical specialty academies, or major university medical centers.
When addressing sudden, unforeseen crisis events that place people in harm’s way, especially medical crises, there must be a balance among harms and benefits. And though this was mostly a mass population event, in the end disease is always personal and patient-specific. Because of this rapidly spreading lethal virus, the action plan was initially confusing and disjointed; perhaps understandably, but it unfortunately remained so. The response was then driven by irrational inertia with the front-line clinicians mostly excluded from the advice and consent process. As is the nature of disease and treatment, in the end it is always the physician and the patient as a team, who alone must decide on the medical therapies in a co-operative attempt to avoid that “good night” (1). As such, the physicians of Chester County, entrusted to be the guardians of our fellow citizens’ health, must endeavor to optimize the medical care available to them, and ensure that it is of the highest quality. We must never be sidelined during a medical crisis again. We hope this report, prepared by the Committee, will, at least in some small way, lead to a more effective response to any future medical crises or public health challenges.
Moreover, it is our sincere hope that there will be an ongoing conversation among physicians, academia, industry, government, and the wider community about the response to COVID and our preparedness for future epidemics and mass public safety events. We invite and encourage comments and suggestions by all parties noted. They may be submitted to this journal’s editor. As well, the authors would be pleased to meet, present, discuss and answer questions about this report and disaster response and preparedness in general with any interested parties.
Respectfully,
Frank Speidel, M.D.
Bruce A. Colley, D.O. May 2024
1. “Do Not Go Gentle Into That Good Night” by Dylan Thomas





BY CHRISTINA VANDEPOL, M.D.
(reprinted from christinavandepol.com by permission of the author)
Anne (not her real name) was lying at the bottom of the stairs, unconscious, face bloodied, when EMS responded to her boyfriend’s 9-1-1 call. Anne had a history of alcoholism and depression. Police confirmed she was also the victim of previous domestic violence incidents. On admission to the hospital, she had multiple facial fractures, brain swelling, and a very high blood alcohol level. The boyfriend claimed he’d found her like that. Anne’s family insisted it was murder. It was up to the coroner – me – to decide. Was this fall an accidental death or a homicide?
A body at the bottom of a staircase. It’s a crime fiction trope for a reason. Falls are a leading cause of accidental death, but excluding homicide can be a challenge. Even sophisticated forensic analysis of injuries and blood spatter don’t always provide an answer. Investigators can’t always relay on interviews of someone on the scene or close to the victim. If alcohol or drugs are involved, as is often the case, both the cause and manner of death become more difficult to determine.
Netflix’ true crime docuseries The Staircase is about a fall-related death. The series covers years of investigation and two criminal trials that ended in hung juries. The director of the docuseries admitted that even he wasn’t sure if the husband, who happened to be a crime novelist, was guilty or innocent of murder.
Anne’s death was just as puzzling. After extensive studies, there wasn’t enough evidence to decide between accident or homicide. I ruled the manner of death undetermined. Meanwhile, the boyfriend who’d called 9-1-1 was nowhere to be found – rumor had it that he’d left the state. Because I had not ruled the manner of death a homicide, the police dropped the case.
Do a search using the term “fatal falls” and you’ll get endless hits for a video game featuring falls from “the sheer cliffs of the island’s coast.” Sounds terrifying, but at least you can play the game and walk away. The same wasn’t


PA 19355 610-644-6755
true for the 351 workers who died in a fatal construction site fall in 2020.
Falls are the leading cause of accidental death in the construction industry. Coroners call the local Occupational Safety and Health Administration (OSHA) for any workplace death. OSHA is very transparent with its data. Decedent names, locations, company names, and descriptions of each fatal event are on its user-friendly workplace fatalities website. Using what it learns from these tragic events, OSHA puts extensive effort into industry-specific fall prevention programs.
More than 42,000 people in the US died from a fall-related death in 2020. More than 86% of them were 65 years or older.
Falls are the leading cause of accidental death in the elderly. They are also the least likely to get a full medicolegal death investigation.
In 2020, just as many people died from falls as from drug overdose deaths in Chester County, PA. There were 108 drug intoxication deaths, a 4% increase from 2019. Most of those were in the 25-54 age groups. But there were also 107 fall deaths, a whopping 40% increase from 2019.
Long-term care facilities almost certainly under-report fall-related deaths. Nursing home physicians (usually medical
It could be the choice of your patient’s life.
Colon cancer can be lethal if undetected.
Colonoscopy has long been considered the Gold Standard in colon cancer detection and treatment. But today, US Digestive Health has set a higher standard in the detection and removal of cancerous polyps.
Introducing The Platinum Standard®
Combining an advanced AI-enabled technology with the experience of our gastroenterologists, USDH can now detect and remove more dangerous polyps and save more lives than ever before.
directors employed by the facility) may sign death certificates for deceased residents without seeing the body. They may not even have seen the patient for a month or longer and may rely on information provided by nursing staff to certify the cause of death. Unless a funeral director sees something of concern on the body, or the family reports a recent trauma, most care facility deaths are certified as due to natural causes. As a result, fallrelated deaths are often missed.
In 2019, Pennsylvania state legislators introduced bills mandating reporting of every nursing home death to the county coroner. That year Scott Grim, former Lehigh County coroner and currently Executive Director of the PSCA, was quoted as saying, “I’m a firm believer that all nursing home deaths and assisted living facility deaths – whether they are natural or not –are reported to the coroner’s office just to make sure everything is appropriate.” Despite bipartisan support, the bills never got out of committee. They should be re-introduced.
Christina VandePol is a physician, former coroner, writer, and speaker. The creator of Cause & Manner, a medicolegal death investigation blog (christinavandepol.com), Dr. VandePol is currently working on a book about her experiences as Chester County Coroner.


BY ASARE B. CHRISTIAN, MD, MPH
Chronic pain is a pervasive public health issue affecting millions worldwide. It is not merely a symptom but a complex condition that can profoundly impact an individual’s quality of life, mental health, and ability to perform daily activities. Chronic pain leads to significant healthcare utilization, economic burden due to lost productivity, and an increased risk of disability. Addressing chronic pain effectively requires a multifaceted approach that considers its biopsychosocial dimensions.
The opioid crisis has highlighted the limitations and risks of using opioid medications for pain management. While opioids can be effective for acute pain, their long-term use for chronic pain is fraught with dangers, including addiction, overdose, and death. The economic costs of the opioid crisis are staggering, encompassing healthcare expenses, lost productivity, addiction treatment, and criminal justice involvement. There is an urgent need to develop safer, more effective pain management strategies. Many current medications for pain management, such as nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and antidepressants, have significant limitations and potential side effects. NSAIDs, for instance, can cause gastrointestinal bleeding and cardiovascular problems, while acetaminophen can lead to liver damage. Additionally, these medications often fail to address the multifaceted nature of chronic pain, leading to suboptimal outcomes.
A major gap in effective pain management is the insufficient education provided to patients about their condition and treatment options. Many patients do not fully understand the chronic nature of their pain, the potential side effects of their medications, or the benefits of non-pharmacological treatments. Improved patient education can empower individuals to take a more active role in managing their pain and make informed decisions about their care.
The biopsychosocial model of pain emphasizes that pain is not solely a physical phenomenon but is influenced by biological, psychological, and social factors. This model advocates for a holistic approach to pain management that includes addressing nutritional factors, sleep quality, stress levels, and physical activity. Nutrition plays a critical role in modulating inflammation and pain, while adequate sleep and stress management are essential for overall health and pain control.
Integrative pain management combines pharmacotherapy with non-pharmacological approaches to provide comprehensive care. Evidence-based therapies such as cognitive-behavioral therapy (CBT), physical therapy, acupuncture, chiropractic care, and the use of supplements can enhance the effectiveness of traditional treatments while minimizing side effects. Such an approach not only addresses the symptoms of pain but also its underlying causes.

The overutilization of unsafe practices, including excessive imaging and surgeries, can lead to unnecessary risks and costs without improving patient outcomes. It is crucial to base treatment decisions on evidence and to prioritize safer, less invasive options whenever possible. Healthcare providers should be judicious in recommending surgeries and imaging studies, ensuring they are truly warranted.
Effective pain management requires a deep understanding of the underlying and perpetuating factors of pain, including gut microbiome dysfunction, HPA axis dysfunction, psychological stressors and trauma, metabolic dysfunction, HPG axis and hormonal imbalances, neuroplasticity, neuroinflammation, neurogenic inflammation, glial cell activation, epigenetic changes, and neurotransmitter imbalances. Addressing these factors is crucial in developing comprehensive and individualized treatment plans.
Complementary and alternative medicine (CAM) therapies can play a vital role in an integrative pain management approach. Supplements such as omega-3 fatty acids, vitamin D, magnesium, and turmeric have shown promise in reducing inflammation and pain. Physical therapy, tailored exercise programs, and techniques like acupuncture and chiropractic care can relieve musculoskeletal pain and improve mobility. Emerging evidence supports the use of cannabinoids in managing certain types of pain.
An integrative approach to pain management recognizes the complexity of chronic pain and the need for a multifaceted treatment strategy. By combining pharmacological treatments with non-pharmacological therapies, addressing the biopsychosocial aspects of pain, and focusing on patient education, healthcare providers can offer more effective and safer pain management solutions. Understanding and addressing the underlying factors of pain, from gut microbiome dysfunction to neuroinflammation, is crucial in developing comprehensive and individualized treatment plans. The ultimate goal is to improve the quality of life for those suffering from chronic pain while minimizing the risks associated with traditional pain management practices.
Asare B. Christian MD, MPH
Integrative & Regenerative Pain Management Specialist
Founder, Aether Medicine www.aethermedicine.com achristian@aethermedicine.com 565 E. Swedesford Rd, #315 Wayne, PA 19087


BY JOHN VENTURA, SENIOR VICE PRESIDENT, SENIOR PRIVATE BANKING RELATIONSHIP MANAGER FOR WSFS WEALTH PRIVATE BANKING AND BRYN MAWR TRUST, A DIVISION OF WSFS BANK
In the realm of financial planning, the traditional approach often focused on achieving specific financial milestones or accumulating a predetermined sum of money. However, as the dynamics of personal finance continue to evolve, a more holistic and personalized strategy has emerged – goals-based investment planning. This method shifts the emphasis from merely accumulating wealth to aligning investments with individual aspirations and life objectives.
In this article, we will delve into what goals-based investment planning entails and explore the values it brings to the forefront of financial decision-making.
Goals-based investment planning is a strategic approach that tailors investment portfolios to meet the unique and specific objectives of an individual or a family. Rather than fixating on arbitrary benchmarks or market indices, this method centers around identifying and prioritizing personal financial goals. These goals may encompass a wide range of aspirations, such as purchasing a home, funding education, securing a comfortable retirement, or even supporting philanthropic endeavors.
1. Goal Identification – The process begins with a comprehensive assessment of an individual’s or family’s
financial goals. This involves a detailed discussion about shortterm and long-term objectives, risk tolerance, time horizons and liquidity needs.
2. Customized Portfolios – Unlike traditional investment strategies, goals-based planning results in portfolios that are tailored to specific goals. This customization allows for a more efficient allocation of assets and ensures that the investment strategy aligns with the intended outcomes.
3. Risk Management – Rather than focusing solely on market risk, goals-based investment planning also considers the risk associated with failing to meet specific objectives. This comprehensive risk assessment helps in creating a more robust investment strategy.
4. Dynamic Adjustments – Life is dynamic, and financial goals may change over time due to various factors such as career shifts, family dynamics or unexpected life events. Goals-based investment planning is adaptable, allowing for adjustments to the investment strategy to accommodate evolving objectives.
1. Personalization and Individuality – One of the primary values of goals-based investment planning is its emphasis on individual aspirations. By acknowledging that each person’s financial journey is unique, this approach ensures that

Cheryl M. Vaughan
Senior Relationship
Manager
investment strategies are aligned with personal values and life objectives.
2. Emotional Well-Being – Traditional investment strategies often induce anxiety and stress due to their focus on market fluctuations. Goals-based planning, on the other hand, provides a more stable emotional anchor, as it centers on achieving specific life goals rather than chasing market trends.
3. Long-Term Perspective – Goals-based investment planning encourages a long-term mindset. Instead of being swayed by short-term market fluctuations, individuals are encouraged to stay focused on the enduring objectives that matter most to them.
4. Accountability and Discipline – Aligning investments with personal goals instills a sense of accountability and discipline in financial decision-making. This can lead to more prudent choices and a greater likelihood of successfully achieving longterm objectives.
Goals-based investment planning represents a paradigm shift in the world of financial management. By placing personal goals at the forefront, this approach not only enhances the potential for financial success but also brings values such as personalization, emotional well-being, a long-term perspective and accountability to the forefront of financial decision-making.
As individuals increasingly seek a more meaningful and purposeful approach to wealth management, goals-based investment planning stands out as a compass guiding them toward a future aligned with their unique aspirations.
Our Advisors serve individuals, families and business owners in developing deeply personalized strategies.
Providing customized wealth management solutions to individuals and families.
Learn more by contacting:
Cheryl M. Vaughan
NMLS #732568
Senior Relationship Manager
WSFS Wealth Center
3801 Kennett Pike, Suite C200 | Greenville, DE 19807 M: 302.379.9647 | O: 302.571.7210


r. Cissy van den Berg-Wolf retired from practicing internal medicine shortly before the COVID-19 pandemic, and quickly realized she was not ready to stop helping others through medicine. After hearing about Community Volunteers in Medicine (CVIM) from a Temple University colleague, Dr. van den Berg-Wolf began to share her passion and expertise at CVIM.

Community Volunteers in Medicine (CVIM), a local nonprofit full-service health care center that provides free, highquality healthcare to low-income, uninsured area individuals and families, relies on an army of volunteers like Dr. van den Berg-Wolf to serve more than 4,000 patients annually.
CVIM provides medical, dental, and behavioral health services at its main West Chester health center and small satellite facilities throughout the region. Most patient care, plus office work and interpreting, is performed by a dedicated fleet of 325 volunteers who donate approximately 38,000 hours of their time each year. CVIM offers extensive primary care services and a myriad of specialties. From endocrinologists to dermatologists to podiatrists, CVIM offers more than twenty specialties to truly care for the whole patient.
“It’ll change your life,” Dr. van den Berg-Wolf said. “It’s so positive here. You see the effects of what you do directly, and you get other people involved too.”
Dr. Gary Newman knew he wanted to continue doing something in the gastroenterology field in retirement. A clinical gastroenterologist in the Philadelphia area for about 40 years and head of the GI fellowship at Lankenau Medical Center for about 10 years before retiring in 2021, Dr. Newman volunteers at CVIM once a week.
Dr. Newman says CVIM has been “a tremendous experience,” noting the genuine camaraderie between patients, doctors, nurses, and staff. Indeed, CVIM has become part of Dr. Newman’s family; his brother-in-law, urologist Dr. Robert Schnall, is a CVIM volunteer, and Dr. Newman’s wife, hematologist/oncologist Dr. Sandra Schnall, is also becoming a CVIM volunteer.
They are far from the only ones! Many CVIM volunteers find that they can’t stop talking about CVIM and sooner or later they recruit a spouse, sibling, or neighbor to join them.


Community Volunteers in Medicine (CVIM), a free nonprofit health care center for low-income working people, is looking for volunteers.
We need current or retired providers to volunteer in our West Chester location Most providers work a four-hour shift, either weekly or biweekly
Recent experience in direct patient care required, preferably within the last two years.
MDs, DOs and CRNPs with active PA licenses

Primary care practitioners and specialists needed
Nurses, interpreters, and drivers also welcome!


The collegial atmosphere at CVIM is often cited by volunteers as one of their favorite parts of their role. Repeatedly, volunteers mention how much they enjoy the ability to work across departments as a true team; for example, a general practitioner working with an endocrinologist, pharmacist, and diabetes educator, all under one roof, to help a patient with diabetes manage their condition.
CVIM volunteers describe this ability to work together and prioritize patient care as “medicine the way it ought to be practiced.” Without the time limitations imposed by insurance billing requirements, providers can truly care for patients and often build strong bonds with those they serve. In return, CVM volunteers report that the gratitude they receive from their patients is worth its weight in gold: “I get back more than I give” is a familiar refrain.
Dr. Carl Giombetti joined CVIM three years ago after retiring from practicing pediatrics at Children’s Hospital of Philadelphia, volunteering twice monthly. His favorite part about it is the people. “Besides the patients – who I think are very appreciative – all the staff is on the same page. They are all just lovely people reaching out to help,” Dr. Giombetti said, “and they work together.”
Here’s what our volunteers say:

“IT WILL CHANGE YOUR LIFE”
“THE BEST WAY TO SPEND FOUR HOURS A WEEK!”
Dr. Giombetti encourages others to volunteer for CVIM. “If you have the time, and you want to do something fulfilling, why not? It’s not, ‘why should I?’ It’s, ‘why shouldn’t I?’”
CVIM recently saw a record increase in new patients, and the need for expanded access to healthcare in our community continues to grow. Meeting that need requires ongoing volunteer recruitment. From doctors and nurses to dentists, interpreters, volunteer drivers, and pharmacists, there is always a need for more help.
CVIM’s Medical Director Dr. Janet Jacapraro is effusive in her appreciation for those who donate their time to CVIM. “I know I speak for the CVIM staff and patients when I say that we are deeply grateful for the compassion and commitment demonstrated every day by our volunteer medical team. If patients are the heart of our mission, then surely our volunteers are the soul.”
If you or anyone you know is looking to give back and has some time – perhaps a recent retiree, or a part-time clinician, or anyone else, please learn more at cvim.org/volunteer.
BY WINSLOW W. MURDOCH, M.D., TOTAL ACCESS MEDICAL, LLC

Each individual clinician can amplify their voice and collaborate on solutions by engaging in organized medicine through County, State and Federal organizations. You do not have to be a member of PAMED (Pennsylvania Medical Society) to engage in this process, but if you want to make comments about or be a voting member on adoption of solutions, you need to be enrolled in your County and State Medical Society, or, conversely, ask for the support of a delegate from your County Medical Society to lobby for your hot button issue.

As a physician in the community, if you are enthusiastic about a hot button issue that is impacting your patients’ care or your practice, you can reach out to your County (CCMS) or State (PAMED) Medical Society member colleagues.
The process is fairly straightforward.
Below is a theoretical attempt at getting collaboration for a hot button issue that you feel passionate about.
Identify your hot button issue in a title: “Ending prior authorizations of Migraine medications”
“No added hidden fees for covered screening colonoscopies”
“Need for better patient education from public health in proper use of infant and child car seats,” etc.
Once you have identified and labeled your issue, share it with your County Medical Society executive or board members, and they will run it up the flagpole to see if there is already existing policy with PAMED or the AMA, and provide you with updates of movement around that policy if already adopted and being worked on.
If your hot button issue is not something currently in progress, or if you feel that the current level of attention needs to be increased, then, you can work on putting together an actual resolution for your state organization to cocreate, lobby and provide action to the request for change or improvement assuming it is adopted at the next house of delegates of PAMED in late October.
The next step is to create a list of reasons why this issue is important: for instance, how it is harmful to patients or practice by stating a series of:
“Whereas; Prior authorizations delay needed care”
“Whereas; Insurance benefits for coverage of USPTF screening services should include all fees”
“Whereas; proper infant and child car seat use saves lives”
If you can cite sources or references this is a bonus.
If you can ballpark an estimate for actual cost to implement, that is also a bonus if it applies. PAMED staffing can certainly help in this regard.
The final step is to create a resolution.
A resolution is a stand-alone request for discrete action or several related actions from PAMED or the PAMED delegation to the AMA to collaborate in communicating, organizing, structuring, and ultimately problem solving as per the resolution.
You should use the collective knowledge of your County Medical Society’s executive, as well as the volunteer board members at CCMS, to fine-tune and craft the resolution so that it has the highest likelihood of being adopted at the annual house of delegates of PAMED to become the work of PAMED or AMA in the upcoming year(s). If you are not a member of your County and State Medical Society, you will have to ask a member who is a delegate to the house of delegates of PAMED to sponsor your resolution. Our county board will assist. Conversely, if you are a member of your County and State Medical Society, you may also volunteer to attend remotely or in person the annual House of Delegates in late October as a delegate of your County.
CCMS will then assist you with submitting your resolution for review and comment. PAMED will then assign it to a volunteer PAMED reference committee of 4 or 5 physician peers and administrative support staff at PAMED.
Resolutions proposed are then posted for about 4 weeks to allow comment and discussion on a virtual site for any and all PAMED members who are engaged, allowing a healthy debate about specific resolutions proposed for that year. The smartest person in the room is the collective room, and the Pennsylvania Medical Society (PAMED) is a pretty big room.
All comments are then reviewed by the reference committee, and a recommendation to adopt, modify, send to the Board of Directors at PAMED for further study, for action after study, or not adopt will be made. There is no sausage making at the house of delegates. Resolutions stand or fall on their own merits, though wordsmithing sometimes does come into play.
If you and other PAMED members disagree with the recommendation of the reference committee, further debate and final voting can take place at the House of Delegates meeting in late October.





BY DR. DAVID W. STEPANSKY, MD, CURRENTLY EMPLOYED BY ZYNX HEALTH
Some might believe that modern evidence-based practice (EBP) in healthcare has a long and rich history. The truth is that evidence-based practice, clinical outcomes research, and certainly the use of order sets, are quite modern constructs. In fact, when it comes to evidence-based practice, the dissemination of credible medical knowledge has often been hindered by physicians who were stubbornly unwilling to deviate from their established beliefs and practices.
Consider the case of Ignaz Semmelweis. In 1847 this Hungarian doctor proposed that puerperal fever (or childbed fever), an infection in women following childbirth or miscarriage, was caused by a contagious process. He further proposed that the physicians of the day were responsible for spreading the contagion and made the heretical suggestion that they should wash their hands before engaging in such procedures. Dr. Semmelweis was aggressive and insulting to those with different viewpoints. His views were generally ridiculed by his superiors. To physicians of his day, the very idea that they, themselves, were responsible for causing illness in their patients, was unthinkable and abhorrent.
Dr. Semmelweis’s behavior became increasingly erratic, and he was eventually committed to an insane asylum where he passed away, likely from sepsis. His handwashing practices were enacted at his insistence by his medical students and junior physicians in 1850, but surgeons did not begin to regularly scrub before their procedures until the 1870s! From our modern perspective, it is very hard to believe that something as simple and basic as handwashing was so strongly opposed for many years.
One of the earliest examples of evidence-based medical practice is attributed to James Lind, a Scottish physician. In 1753, utilizing a process that would later be known as the “scientific method,” Dr. Lind discovered that eating fresh oranges and lemons could prevent and cure scurvy in British sailors. But the evidence-based practice movement was not formally introduced for another 230 years when, in 1981 (the year that I went into medical practice in Chester County!), a group of clinical epidemiologists at McMaster University in Canada, led by David Sackett, published a series of articles advising physicians how to appraise the medical literature. In fact, the term

“evidence-based medicine” did not appear in the medical literature until 1992 when the term was coined by Gordon Guyatt and then appeared in a series of articles in JAMA.
One may ask whether evidence-based medical practice has been shown to improve clinical outcomes. In a fascinating study, Emparanza, et al looked at the effects of establishing an evidence-based practice unit in a hospital. The physicians and nurses practicing in this unit were given special training on how to critically appraise the medical literature and were required to attend regular multidisciplinary meetings to discuss patient management utilizing the latest evidence-based practices. Clinical outcomes for the EBP unit versus the standard practice unit were followed from 2004 to 2011. The results were striking. The mortality of patients being treated by EBP doctors compared with their previous performance dropped from 7.4% to 6.3% and length of stay dropped from 9.15 to 6.01 days – both reductions being statistically significant. There were no similar outcome improvements for doctors continued on next page >

who practiced in the standard practice unit.
The value of EBP, including its ability to improve clinical outcomes, has been clearly demonstrated in many studies. Here are just a few examples:
The use of external cooling blankets for certain patients with sepsis has been shown to significantly reduce mortality.
The provision of high-protein oral nutritional supplements in hospitalized, malnourished COPD patients ≥ 65 significantly reduces 30-, 60-, and 90day mortality rates.
The continuation of hydroxyurea for hospitalized patients with sickle cell disease significantly reduces the incidence of acute chest syndrome and lowers the overall mortality rate.
Consultation to Cardiac Rehabilitation significantly reduces readmission rates for patients admitted with heart failure.
Indeed, the medical literature is replete with EBP research. A recent extensive review of the EBP literature concluded that, “…EBPs improve patient outcomes and yield a positive return on investment for hospitals and healthcare systems.”
Embedding current evidence-based practices into the order sets of our electronic health records is a very efficient way of encouraging the most current effective practices. This is obviously a relatively recent method for disseminating medical knowledge and encouraging its application, so it is reasonable to ask whether this approach has proven valuable. In fact, several studies have demonstrated the effectiveness of disease-specific order sets. Here are just a few examples:
Krive et al (2014) found that the use of evidence-based order sets for patients admitted with congestive heart failure significantly reduced both mortality and length of stay without effect on readmissions.
Kitchlu et al (2015) demonstrated that the use of evidence-based order sets for patients admitted with COPD exacerbations resulted in improved medical management and reduced lengths of stay.
Dale et al (2023), in a large retrospective cohort study, found that the use of an evidence-based order set in the management of sepsis was independently associated with lower
hospital mortality. The authors of the study concluded that, “Order sets can impact large-scale quality improvement efforts.”

The dissemination of medical knowledge and the tools that enable us to do so have obviously advanced considerably in recent years. The delivery of evidencebased practice by doctors and nurses is rightly the expectation of our patients. The use of evidence-based order sets in our electronic health records has been shown to improve patient care and so encouraging healthcare providers to utilize these order sets is of great importance.
To learn more about methods for disseminating evidence-based practices, contact David Stepansky, MD, at dwstepansky@gmail.com.
References
i Emparanza JI, Cabello JB, Burls AJ. Does evidence-based practice improve patient outcomes? An analysis of a natural experiment in a Spanish hospital. J Eval Clin Pract. 2015;21(6):1059-1065. doi:10.1111/ jep.12460
ii Schortgen F, Clabault K, Katsahian S, et al. Fever control using external cooling in septic shock: a randomized controlled trial. Am J Respir Crit Care Med. 2012;185(10):10881095. doi:10.1164/rccm.201110-1820OC
iii https://goldcopd.org/wp-content/ uploads/2023/03/GOLD-2023-ver-1.317Feb2023_WMV.pdf
iv https://www.nhlbi.nih.gov/sites/default/ files/media/docs/sickle-cell-disease-report%20 020816_0.pdf
v Gao Y, Wang N, Zhang L, Liu N. Effectiveness of home-based cardiac telerehabilitation in patients with heart failure: A systematic review and meta-analysis of randomised controlled trials [published online ahead of print, 2023 Apr 16]. J Clin Nurs. 2023;10.1111/jocn.16726. doi:10.1111/ jocn.16726
vi Connor L, Dean J, McNett M, et al. Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews Evid Based Nurs. 2023;20(1):615. doi:10.1111/wvn.12621
vii Krive J, Shoolin JS, Zink SD. Effectiveness of Evidence-Based Congestive Heart Failure (CHF) CPOE Order Sets Measured by Health Outcomes. AMIA Annu Symp Proc. 2014;2014:815-824. Published 2014 Nov 14.
viii Kitchlu A, Abdelshaheed T, Tullis E, Gupta S. Gaps in the inpatient management of chronic obstructive pulmonary disease exacerbation and impact of an evidence-based order set. Can Respir J. 2015;22(3):157-162. doi:10.1155/2015/587026
ix Dale CR, Schoepflin Sanders S, Chang SC, et al. Order Set Usage is Associated With Lower Hospital Mortality in Patients With Sepsis. Crit Care Explor. 2023;5(5):e0918. Published 2023 May 16. doi:10.1097/ CCE.0000000000000918


SageLife communities are designed to meet aging seniors wherever they are in their journey — giving them the power to be their best, most vibrant self. Our mission is to encourage, empower and celebrate successful aging.
Each of our communities reflect priorities that ma er most: dynamic lifestyle, adaptable care, and sophisticated amenities. We go where our residents lead us — allowing them to find their purpose and live their best life on their own terms.
That’s the SageLife difference.
AMBLER, PA 215-461-4880 The501.com
INDEPENDENT LIVING ASSISTED LIVING MEMORY CARE
MALVERN, PA 484-568-4777 LivingAtEchoLake.com
INDEPENDENT LIVING ASSISTED LIVING MEMORY CARE
WALLINGFORD, PA 610-690-1630 PlushMills.com
INDEPENDENT LIVING PERSONAL CARE
PAOLI, PA 610-640-4000 DaylesfordCrossing.com
PERSONAL CARE MEMORY CARE
Living to the power of you.
Dr. Stepansky is currently employed by Zynx Health, an organization that provides evidence-based solutions for the healthcare industry. Dr. Stepansky is a board certified internist with an extensive background in clinical informatics, quality, and utilizing evidence based practices. At Zynx, he is a Clinical Solutions Strategist who applies his knowledge in
this area and in performance improvement science to improve clinical outcomes at hospitals and clinics.

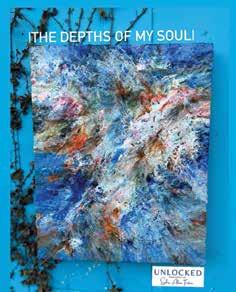
BY BRUCE A. COLLEY, DO


Whimsical Love
Each issue of our journal I find another artist with unique talents with a distinctive approach to their art. The variety of media and styles seem infinite. This should not surprise me as I have been a spectator of the flourishing art community in Chester County since I was a child. But with each artist I encounter I am once again surprised and delighted.
Sophia was introduced to me by a few other Chester County artists who told me her art was especially unique and her story more so. For sure, growing up with the “Chester County” school of art (Wyeths, Sculthorpe, Jamison, etc.), abstract art, though done by many local artists, is a bit off my radar and I had little natural inclination to appreciate it. Having the good fortune to meet Sophia, see her art and hear her motivations and descriptions of her techniques, I believe I have at least an intimation of the content of abstract renderings.
Sophia, growing up in central Pennsylvania then becoming an ordained minister, now works as a hospice chaplain and a part time minister in West Chester. When I meet with our featured artist in their studios, a question I always have and am most curious about is when they recognize their talent. Nearly all appreciate that their artistic talent was special and innate at a very early age. A very few, however, come to realize and use their talents as adults. Such is the case with Sophia who had no formal training in art but came to realize her talent as an artist in what I can best describe as a flashpoint moment. Though Sophia, for many years did use photography to tell her story, a paint date with her now fiancé unlocked her inborn talent as an artist even though never trained for or practiced fine art. Moreover, it unlocked her being and inner self; allowing her to come out to the wider community. Sophia’s artist statement gives a beautiful

This piece is a dream come true.
Artistically, it is a style that I’ve envisioned and hoped to create for several months, and it was birthed after several days in the new studio.
I added circles and texture, but something was missing.
I got a vision of a rainbow flair.
Because, I mean, when is a rainbow flair ever a bad idea?
It was exactly what it needed.
It needed love. It needed color. It needed movement.
As I stepped back from it, I felt a sense of wonder, awe and gratitude.
A style I’d dreaded and admired in others I somehow created myself.
Anything is possible.
When I looked at this piece to speak to me for its title…
I saw a city – a city of love.
I also dream about cities of love.
Places where justice is really for |all| and we honor humanity in one another. Places where we don’t destroy others and ourselves over what we believe. Places where love wins and we all can get along, or at least sit at the same table.
Yes, even evangelicals and the rest of the world.
Even donkeys and elephants.
Even white people and black and brown people. Even all of us.
This piece is a prayer and petition for all of us, that nothing is impossible, from a new art creation to a new way of living, and yes, even to a city of love.
I hope that the city of your own soul is filled with love, because I believe love starts at the home within our own selves and can ooze out to those in our little corner of the world.
It all matters.
Everything we do matters.
I will do my best to be a city of love...
Will you join me in reimagining and creating cities of love? Sending love, justice and possibility to you today.



The Art of Chester County continued from page 26
accounting of her unlocking experience. Unique to her artistic renderings is that she couples the painting with a story or poem. A true intersection of visual and literary arts. I think it is best to just share Sophia’s art and a few of her stories rather than struggling to summarize her special form of art. Pondering our discussion after we met, I wondered if it was the art that unlocks that spirit, or the spirit that unlocks the art. I suspect that it is both forces acting together. Please take a moment to enjoy Sophia’s unlocked art and self.


Contrary to popular belief, everyone is welcome at the table. Over this last year I’ve heard story after story of churches, families and friends rejecting those who are LGBTQ+.
It’s heartbreaking.
It’s foolish.
It’s the antithesis of what the table represents. There’s a better way.
The way of love is the way that leads to life.
However we identify, we are all welcome at the table.
If anyone has told you different, it’s a lie and rooted in someone else’s homophobia and systemic oppression.
If you are in need of a church that is inclusive and has a wide open table, check out my church: Cornerstone Christian Fellowship in downtown West Chester or www. cornerstonewestchester.com; you are fully welcome at our table.
Come to the table, eat and drink and be loved, because we are.


BY KEVIN B. O’REILLY, SENIOR NEWS EDITOR

For the last two years, the U.S. Congress has failed to stop in their entirety repeated across-the-board pay cuts that further threaten Medicare access to high-quality physician care, especially for patients in rural, underserved or economically marginalized areas.
In 2023, it was a 2% pay cut that took effect. And this year, physicians are seeing another 1.68% pay cut. The cuts come after the peak of the COVID-19 pandemic, amid physician and health worker shortages and rising inflation, and as the Change Healthcare cyber outage poses huge disruptions to the medical claims-processing systems.
“The need to stop the annual cycle of pay cuts and patches and enact permanent Medicare payment reforms could not be more clear,” AMA President Jesse M. Ehrenfeld, MD, MPH, said last month following the House vote on the government-funding deal that reduced the 2024 Medicare pay cut by about half.
While the AMA is working relentlessly to build understanding on Capitol Hill about the unsustainable path the Medicare payment system is on, preventing further cuts means getting to the root causes of what’s wrong with Medicare physician payment.
That is why the AMA created the Medicare Basics series, which provides an in-depth look at important aspects of the Medicare physician payment system. With these six straightforward explainers, policymakers and physician advocates can learn about key elements of the payment system and why they are in need of reform.
1. Medicare physician payment adequacy— Budget neutrality
As one of the few Medicare providers without a payment update tied to inflation, physicians have watched their inflation-adjusted payments fall dramatically since 2001. Physician payments are further eroded by frequent and large payment redistributions caused by budget-neutrality adjustments.
2. Merit-based Incentive Payment System (MIPS)
Although MIPS is well-intentioned, its reporting requirements are burdensome to physician practices and often appear to be clinically irrelevant. Congress must step in and act to prevent unsustainable penalties, invest in and enable the move to value-based care, and increase transparency and oversight in the program.
3. The Medicare Economic Index (MEI)
Since 1992, the role of the MEI in shaping Medicare physician payment has diminished dramatically, first under the sustainable-growth rate (SGR) and then under the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015. Physicians need an annual inflationary update, which will allow practices to better absorb other payment redistributions triggered by budgetneutrality rules and performance adjustments, as well as periods of high inflation and rising staffing costs.
4. Advancing value-based care with alternative payment models
Alternative payment models (APMs) are a key approach to achieving value-based
care by providing incentive payments to deliver high-quality and cost-efficient care for a clinical condition, a care episode or a patient population.
5. Transitioning to value-based care: Clinical data registries
The Centers for Medicare & Medicaid Services’ (CMS) clinical data registry approval process under the MIPS program is complex and cumbersome, and the lack of accessible cost data inhibits progress toward true value-based care. As a result, physicians’ ability to leverage their participation in these quality improvement efforts for MIPS and engage in continuous learning has been limited.
Value-based care relies on data. To be successful, physicians in MIPS need access to a wide range of information on a timely basis to understand gaps in care and identify opportunities to improve health outcomes, reduce variations in care delivery or eliminate avoidable services—all steps that can lower costs for patients and the Medicare program.
Leading the charge to reform Medicare pay is the first pillar of the AMA Recovery Plan for America’s Physicians.
The AMA has challenged Congress to work on systemic reforms and make Medicare work better for you and your patients. Our work will continue, fighting tirelessly against future cuts—and against all barriers to patient care.

BY SONIA BISACCIA, MD
Ialways knew I wanted to be a family doctor. In college I began envisioning practicing in a small town, where I could live above my office and if someone was late with a bill, I would happily accept fresh eggs from their chickens. Fast forward through years of school and training and instead I found myself working long hours, trying to care for 3000 patients with appointments every 15 minutes. I was exhausted, my patients needed me, and I knew I had to find a better way to use my years of training. And then I was introduced to the concept of Direct Primary Care.
Direct Primary Care is an innovative model of healthcare delivery that is gaining in popularity throughout the United States. By cutting insurance out of the patient-doctor relationship and using a subscription-based model, a physician can keep their practice small and personal, resulting in increased time and access for their patients. The Direct Primary Care (DPC) model allows physicians to provide healthcare at a more affordable rate and enables them to focus more on delivering quality care to their patients rather than navigating complex insurance requirements.
Talk to any primary care physician working for a healthcare system these days and they will tell you — they’re frustrated by the quantity of work they do outside of seeing patients and they’re frustrated by the little amount of time they’re given to see each patient. The DPC model inverts these numbers. Instead of carrying the typical 2500-3000 patients, DPC physicians often carry 300600 patients. Less patients means more time with each patient and less time spent clicking through refills and messages. Patients are also feeling the crunch of corporate healthcare — more and more they are turning to urgent care centers when they are ill because
they are unable to get an appointment with their primary physician. And when they do see their PCP, they often have a list of issues to discuss, but are unable to cover it all in a 15- or 20- minute visit. Having a DPC doctor means no co-pays, improved access, longer appointment times, and same or next day visits and patients really appreciate this.
The DPC movement represents a paradigm shift away from the traditional model of generating revenue through insurance reimbursements. This serves both physicians and patients. When insurance companies are removed from the equation, the overhead for a PCP practice dramatically decreases, eliminating the need for coders, billing companies, and an administrative presence. DPC often saves patients money as well. Besides decreasing the need for urgent care and ER use and eliminating the co-pay burden, many DPC practices are able to offer reduced rates on labs and imaging. For example, if a patient were to have a Complete Blood Count (CBC) at a popular neighborhood lab and insurance feels the test was not warranted they will refuse to pay for it, leaving the patient with a bill for $198, for just that CBC. Using what’s known as Client Billing, a DPC practice can obtain that same CBC at the same laboratory for just $2 and insurance is no longer dictating care. Removing insurance from the equation really can save everyone money. Most DPC physicians would agree that patients still need to have insurance, for catastrophic events, etc., however, removing it from the patient-PCP relationship can financially benefit everyone.
As healthcare in the US has become more and more expensive, finding ways to provide affordable high-quality primary care has proven elusive. The Direct Primary Care movement is providing one remedy to a current national problem and making patients and doctors happy at the same time.
BY DAVID BOBMAN, PRESIDENT, CHESTER COUNTY MEDICAL SOCIETY

Recently, Lynne Stilley, our administrative executive, was asked about physician unions by one of our members. This in turn led to contemplation about what their role and benefit is to physicians, particularly as it pertains to various local, state and national medical societies.
Through the years, there has been an enormous change in our medical system. Whereas most physicians were previously self-employed small business owners, this segment of the medical community is now only a small proportion of practicing physicians. Many physicians are now employed by hospital systems, private equity, insurance companies, or pharmaceutical companies, among others.
There has been disillusionment among physicians, and for a number of reasons membership in medical societies has fallen dramatically. For instance, in the 1950s approximately 75% of physicians belonged to the AMA. That number had fallen to about 15% as of 2011. (CMAJ. 2011 Aug 9; 183(11): E713–E714) The strategy of “divide and conquer” dates back millennia – as early as the ancient Babylonians. Intentionally or not, this has become the outcome of our current medical system. There is little solidarity in pursuing issues relevant to the medical community. Hence, our political influence has waned as we do not speak with a unified voice.
In an ideal world, physician unions would be unnecessary. However, this is perceived by many to not be the case. I think the main impetus for consideration of physician unionization is a sense of lack of control and bargaining power in dealing with these employers. Unions are an effective means of levelling the playing field in negotiations between employees and employers. They may help achieve an improvement in the dwindling physician reimbursements, hours worked, patient
care ratios, etc. They are likely to be more effective in achieving these means than a medical society alone can.
In the past, most physicians as private practitioners were considered supervisors or business owners, and therefore unable to unionize under the National Labor Relations Act. Times have changed and now nearly 75% of physicians are considered employees, making unionization possible for this sector of the physician population.
While these issues make physician unionization attractive, their focus tends to be more on the financial aspects of medicine and working conditions. However, physicians have many other issues that would not typically be addressed by unions. For instance, malpractice litigation weighs heavily on many physicians, especially those working in Southeastern Pennsylvania or those with ties to Philadelphia, where juries are liberal in awarding verdicts which at times are exorbitant in amount. Risk of criminal prosecution over medical care, often seen in maternity settings, is another increasingly important legal concern.
Other issues include dealing with onerous pre-certification processes, inability to prescribe the best medicines for a patient’s particular malady, frequent rule changes such as those for documentation requirements, and purchase and upkeep on expensive EMR systems, among others. These all add to wasted physician time, higher expenses, worse patient care, and increased physician frustration. This last issue is particularly important since Covid-19 where physician burnout has become epidemic.
These issues illustrate the need for a strong presence of medical societies on a local, state, and federal level. This is not where we are today. If county medical societies truly had membership
that equated to most of the doctors in a county, and all 62 county societies worked collaboratively in advocacy for doctors and patients, and they united in their issues within the State Society, which then works with the AMA on a federal level, doctors could and would have much more power and bargaining clout. This is the way the medical society system is supposed to work, and maybe did years ago. It is just as needed now, and probably more now than ever.
Membership is where it starts. All physicians need to join their Societies, as they would a union. Leadership is next. The individual boards of each society should have all recognized or emerging leaders involved on them. The same goes for the State Society.
Physicians are not aware of the benefits of belonging to a strong organization, or maybe the CCMS and other societies are not viewed that way, or are not visible enough. But they could be. All doctors need to sign up and, demonstrating a unified front, flex our collective muscles to achieve necessary change. A strong membership not only allows a louder collective voice, but also helps pay for the work that is being done and needs to be done for all physicians. No one but physicians have a stronger vested interest in medicine and the future. And they are the experts. They can bring awareness and solve problems. With increased physician participation, activism, and financial support of the medical societies and their PACS, we can bring more doctors into the general assembly in the State and on a federal level. Then life for physicians could and would be different and better than it is today.
I can picture a brighter future for doctors and society in general with strong, well-led physician medical societies in conjunction with physician unions.

BY JACK LYNCH, PRESIDENT AND CEO, MAIN LINE HEALTH
Main Line Health is facing unprecedented financial challenges, losing more than $225 million over the last two fiscal years. These deficits are significantly impacting funds available for reinvestment in new technologies, additional beds to address the closures of hospitals in our service area and information technology. These issues are not exclusive to Main Line Health — hospitals and health systems across the country are experiencing historic losses.
Through our Performance Excellence initiatives, we are working carefully to reduce the total cost of care, decrease length of stay and eliminate excess days by improving care coordination across the system, all while improving safety, quality and equity.
Founded in 1985, Main Line Health is a not-for-profit health system serving the Philadelphia region and beyond. Main Line Health consists of five hospitals, six health centers, 40+ offices, hundreds of clinical practices, 2,000+ physicians and more than 13,000 employees.
Main Line Health has experienced significant increases in costs associated with delivering safe, high-quality equitable and affordable care to our patients and the communities we serve.
Labor Pharmaceuticals Supplies



* Cost increases noted are since 2019
Main Line Health lost more than $300 million on Medicare patients over the last two fiscal years.
There are a number of factors contributing to this financial situation and challenging the system’s ability to deliver on its budgeted financial plan:
• Cost of care
• Insufficient payor reimbursements:
• Medicare: 73 cents on the dollar
• Medicaid: 57 cents on the dollar
• Private: Rates negotiated prepandemic
• Changing patient population
• Salary expenses
• Agency staff
• Inflation
• Drug cost increases
• Supply chain issues
• Increased length of stay
• Fairly reimburse hospitals for patients covered under government-funded programs
• Prevent all Medicare and Medicaid cuts for hospitals
• Prevent hospital cuts stemming from site-neutral policies
When health systems in this country have financial struggles, access to care becomes impacted.
- Jack Lynch III, FACHE President and CEO, Main

BY JANET HALIDAY, JANET HALIDAY CONSULTING
nstagram, Facebook, TikTok, and YouTube are some of the social media platforms that your medical practice should be utilizing to reach new potential patients. Even a simple social media business page with your contact information, images of your practice, and information about your services can provide excellent search engine information. Practices with multiple locations can benefit from individual business pages with their phone, email, and address map and can be managed under one admin umbrella. Social media platforms are great tools to meet your patients where they are online, searching for medical information, because search engines such as Google feature your social media posts. Even Google My Business can feature your social media pages.
Instead of solely having a website where search engines can gleam information, you now have 4 additional sources pointing to your website with even more opportunities to highlight your medical services. In Google search results, for example, each social media account is often listed separately under your website listing, therefore bumping your competition down the page on the Google search results.
All social media platforms use computer programs, referred to as algorithms, to show your content to people using their platform. When publishing to social media, quick 5 to 11-second videos combined with trending songs and hashtags work the best with the algorithms. Although the algorithms change constantly, a rule of thumb is to post at the same time daily based on your followers and when they are online, 5-6 times per week, and share to your page as a post, a reel, and a story. Hashtags such as #doctor #location #disease tell the algorithms what your content is about and platforms show it to those people searching for the hashtag word or following the hashtag. Social media posts without hashtags are like throwing a book into a library filled with other random books and hoping someone will find it. The difference can take an account from reaching a few hundred people per post to a few hundred million per post, aka “Going Viral.”
Some great ideas for your practice to share on social media may be;
• Physician Research News
• Medical News Updates in their specialty
• Local Disease Alerts
• Practice News
• Inclement Weather Closing
• Patient Success Stories
• New Procedure Offerings
• New Grants Earned
• New Staff or Retirement News
• Physician Awards
There are also a few rules when sharing on social media for physicians. Platforms such as Facebook won’t allow images of needles, medical procedures, or discussions using the word “Covid” or “cannabis.” Posts are not permitted to preface with questions such as “Do you suffer from…” or make a platform user uncomfortable about a medical condition. These posts will be flagged, removed, or even cause your account to be banned.
Hiring a professional social media management company is the best way a physician’s practice can ensure that they have a social media presence and meet the requirements of each platform. The combination of a great Google My Business page, with excellent social media business pages, helps medical practices show up in search engines and therefore result in more appointments. Better social media companies know the daily algorithms and are experts in each platform with several staff members who work solely in social media. They provide social media calendars and work with content creators to create, schedule and monitor the results of your online campaigns.
JanetHalidayConsulting@gmail.com
www.JanetHaliday.com


MRI Group has a long tradition of excellence: Accurate image reading. Collaborative, highly trained physicians. Exceptional patient experience. Affordable rates.
• Images read by local radiologists
• Radiologists available 24 hours a day, year round, to read images and provide consultation
• All MRI Group locations are ACR accredited
• All radiologists are board certified by American Board of Radiology
• Experts in various radiology specialties including cardiovascular, interventional, neuroradiology, vascular, musculoskeletal, and pediatric imaging
• Evening appointments available
CHESTER COUNTY LOCATION: 950 S. Octorara Trail, Parkesburg (Intersection of Routes 30 and 10)
We are located at the Penn Medicine Lancaster General Health Parkesburg outpatient facility.
MRI scans performed at our Parkesburg location
• Abdomen
• Brain
• Chest
• Extremity
• Joint
• Magnetic Resonance Angiography (MRA)
• Pelvis
• Spine
Phone: 717-291-1016
Fax: 717-509-8642 MRIGroup.com
Several locations in Lancaster County and Chester County