WINTER 2022-23 Trend Bending: TRACKING & BENDING TRENDS TO CREATE BETTER SOLUTIONS How the National Opioid Settlement Will Affect Berks County

The Response is published through funding from county and state dollars in concert with the Berks County Opioid Coalition under the guidance of the Council on Chemical Abuse. cocaberks.org • 610-376-8669
EDITORIAL BOARD
T.J. Huckleberry
Executive Officer, Berks County Medical Society


John Adams
District Attorney, County of Berks
Kevin S. Barnhardt Commissioner, County of Berks Marcia Goodman-Hinnershitz Director of Planning & Resource Development, Council on Chemical Abuse
Tracy Hoffmann Hoffmann Publishing Group

Lee Olsen
Olsen Design Group Architects, Inc. Stanley J. Papademetriou Executive Director, Council on Chemical Abuse

BERKS COUNTY’S OPIOID COALITION, SOS BERKS www.sosberks.com
BERKS OPIOID COALITION LEADERSHIP WITH SOS BERKS
Kevin S. Barnhardt and Stanley J. Papademetriou Coalition Co-chairs
COMMUNITY SAFETY COMMITTEE
John Adams and Yvonne Stroman Co-chairs
COMMUNITY AWARENESS COMMITTEE
Laura Catalano Chair
DATA COMMITTEE
Justin Loose and Kathy Noll Co-chairs
PREVENTION EDUCATION COMMITTEE
Cory Trevena and Jaclyn Steed Co-chairs
TREATMENT COMMITTEE
Amanda Miller and Bernice Hines-Corbit Co-chairs
OPIOID COALITION VISION
The opinions expressed in this publication are for general information only and are not intended to provide specific legal, medical or other advice or recommendations for any individuals.

All rights reserved. No portion of this publication may be reproduced electronically or in print without the expressed written consent of the publisher or editor.
BERKS COUNTY OPIOID COALITION
3
THE LATEST UPDATES BY
SOCIAL
FEATURES 4 Prevention & Recovery: A Team Effort 6 Becoming a Bendsetter 8 Diversity, Equity, and Inclusion (DEI): A Worthy Goal for SUD Treatment and Recovery 12 Diversity, Equity, and Inclusion in Substance Use Treatment 16 Employee Drug Test Positivity at Two-Decade High 19 How the National Opioid
Will Affect
County 24 Loss: Understanding the
to
Use 28 Post-Traumatic Stress Disorder, Trauma and Recovery: A Veteran’s Perspective
RECEIVE
FOLLOWING US ON
MEDIA
Settlement
Berks
Connection
Substance
Identify opportunities to remediate the opioid
through the
of evidence
strategies and resources.
crisis
provision
based/best practice
to
|
CONTENTS
OPIOID COALITION MISSION The mission of the coalition is
determine the extent to which Berks County is being affected by the non-prescriptive use of opioids and the use of heroin through the examination of its devastating effects, both personal and societal, and to set recommendations that address the prevention, intervention, treatment and recovery supports of local residents that suffer from opioid addiction. 2669 Shillington Road, Box #438 Sinking Spring, PA 19608
HoffPubs.com | (610) 685.0914 Designer | Kim Lewis FOR ADVERTISING INFO CONTACT: Alicia@hoffpubs.com, 610.685.0914, ext. 210 READ THE RESPONSE ONLINE AT Response.HoffmannPublishing.com
WINTER 2022-23
Prevention & Recovery: A Team Effort



The overdose crisis has not nor will not miraculously disappear. It requires a comprehensive and sustained effort to stem and subsequently turn the tide away from this crisis. To date, there have been numerous efforts to address the overdose issue in our community. While the overdose numbers remain high, it would NOT be accurate to believe that the efforts employed have been ineffective. Many lives have been saved and despair has turned into hope.
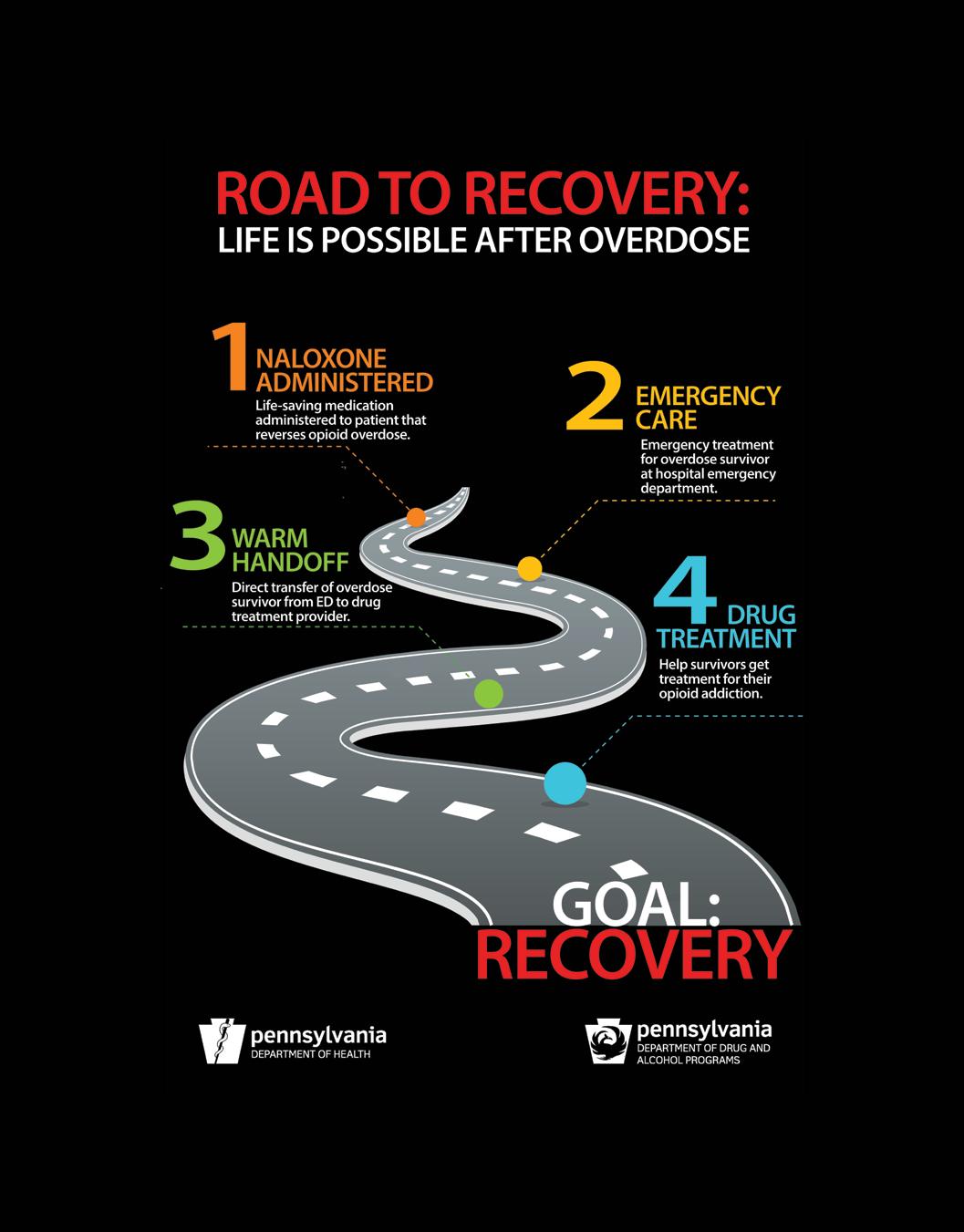
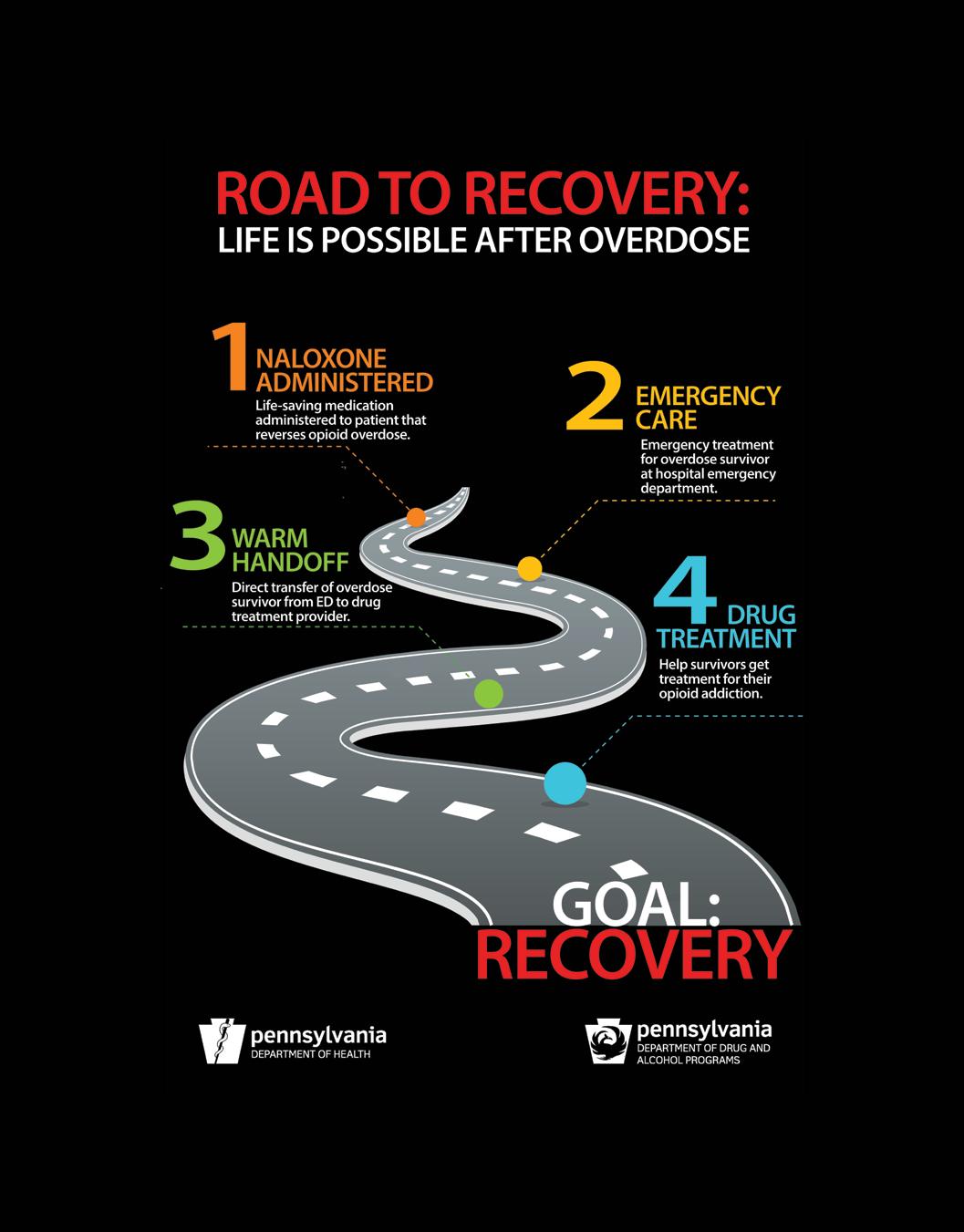
Emergency medical technicians (EMTs) and other first responders have, from the outset of the crisis, answered countless calls to revive overdose victims and subsequently have saved numerous lives.
These calls are distressing and many times instead of a heartfelt thank you, the EMTs are rebuked for “ruining a high.” Regardless, EMTs across the county continue to respond to overdose calls and save lives. Law enforcement personnel do what they have always done, employ efforts and strategies to disrupt the supply of illegal drugs into our community. Some of these drugs are the most dangerous and deadly substances we have seen locally. In response to the crisis, law enforcement personnel also now carry and administer life-saving naloxone. Law enforcement continues to work to keep our community as safe as possible.

THE RESPONSE // WINTER 2022-23 4 FROM THE COALITION
From the SOS Berks Chairpersons Coalition Co-Chairs: Kevin S. Barnhardt, Commissioner, County of Berks, and Stanley J. Papademetriou, Executive Director, Council on Chemical Abuse
Medical personnel, law enforcement and substance use professionals conduct community awareness forums to alert the public to the overdose crisis. As a result, there has been a sharp increase in the public’s knowledge regarding the problem. There is much more of an understanding of overdose issues in our community as well as the resources available to address opioid use disorders. There is also now a much keener appreciation by the public for the use of medications to address the problem.
As a result of the large number of overdose deaths in the past several years, harm reduction approaches have gained more attention both nationally and across the region. There is a broad array of harm reduction techniques, several of which have been employed in Berks County such as medication assisted treatment, enhanced naloxone availability and criminal justice diversion programs to name a few.
Addiction-related stigma continues to be a major barrier to individuals and families seeking much – needed help. Sometimes, stigma can affect the type of help someone receives. While this is an area that requires persistent attention, major progress has been made in the area in the past several years. More individuals now see substance use disorders for what it is - a brain disease. Also, there is more acceptance of specific medications as a means for some individuals to overcome certain addictions. The more stigma is reduced in our community, the more addiction recovery can take hold and flourish.
A personal note from Stan:
Over the past several years, the federal and the state government have provided specific funds to address overdoses and opioid use issues. These funds have been crucial in helping remove barriers from those in need of treatment and have enhanced access to medication assisted treatments. Additionally, these funds allowed for expansive local distribution of the lifesaving opioid overdose antidote – naloxone. Fortunately for our community, additional funds will be available through the National Opioid Settlement. (These settlement funds and their impact for Berks County is explained further on in this issue.)
The Opioid Settlement funds now offer us an opportunity to further develop and grow other innovative programs and activities that heretofore we would not be able to consider due to funding limitations.
These are but just some of the many local efforts to address the overdose crisis. This list will expand as other proven approaches and methods are identified and new strategies integrated into our local response. As we refine our responses to the opioid crisis, we must even more closely examine the root causes of the epidemic. This includes more effectively addressing issues related to trauma as well as assuring that matters associated to diversity, equity and inclusion are adequately addressed. Now, more than ever, it is time to redouble our efforts to overcome the tragic trends in overdoses.
I am retiring in December and as such I will be stepping down as co-chair of the SOS Berks Opioid Coalition. SOS Berks has been both a challenging and rewarding endeavor. Constant reminders of the death and devastation of the overdose crisis is overwhelming. Yet, the feelings of hope and optimism are energizing especially when working together with committed individuals seeking to improve our community. Not even a pandemic, which shut the world down for months, could stop this group from seeking ways to make a difference.
A big thank you to all the special and inspiring individuals – too numerous to mention – that I met and worked with on this journey. A most special thank you to my co-chair, Commissioner Kevin Barnhardt. Kevin is the heart and soul of SOS Berks. His “never say never” attitude is contagious and keeps us going through these challenging times. I know SOS Berks will continue the fight and leave no stone unturned in seeking to significantly reduce overdose deaths and ease the suffering that comes with addiction.
5
Becoming a Bendsetter

Crosby, Stills, and Nash began one of their most popular songs with, “It’s getting to the point where I’m no fun anymore.”
T.J. Huckleberry Executive Officer Berks County Medical Society

Well, this year, as I hobbled into my 40th year of existence, never has a lyric rung so true for me. For a while, I fooled myself into thinking that age was not catching up to me… until this year.
This year, I have caught myself uttering to packs of kids, who have already tuned me out, the same cliches and advice that my old coaches and teachers gave to me. I have endured hearing my 11-year-old son call me “bruh,” like he was some shrunken version of Jeff Spicoli. I have had my wife subtly and not so subtly tell me my wardrobe is a few election cycles out of fashion. And in my men’s basketball league the previous talk about who has the nicest sneakers has been replaced with who has the newest and most sensible knee and ankle braces.
I am putting it in writing. When it comes to what’s new and trendy, I think I am out of touch.

THE RESPONSE // WINTER 2022-23 6
Trendsetter: a person who can spot new trends early on and spreads these fads to new locations and social groups.
LETTER FROM THE EDITOR
And to be honest, I care about more important trends in my life. So, what, if don’t Instagram on tick tock or that I prefer Abraham Lincoln biographies over the Kardashians. Nowadays, as a parent and a community member, it’s the trends I see that affect all of us that seem to matter the most.
The alarming statistics concerning overdoses in our county, the rise in fentanyl use, and demographic and social inconsistencies in substance abuse; that has my attention. The data itself makes me want to explore the ways we can turn the rising numbers on a line graph and bend them back down to zero. I don’t need to be a trendsetter; I want to bend the negative trends we are facing. … I want to be a bendsetter.


in
Instead of focusing on the superficial and the popular; if we are acting as bendsetters, our mindset also needs to focus on those who are at times overlooked, taken for granted, or are in the minority. Those who are suffering in silence yet still in desperate need of our resources. That is the focus of this edition of The Response


The bendsetters highlighted in this edition are concentrating on our local veterans, our LGBTQ+ members, and those in trauma. Rest assured, in future articles we will continue to highlight those who are striving to bend the negative trends in our community and shed light on the individuals and organizations who demand our recognition.
On behalf of The Response, we hope you all find this edition to be totally rad, ehh super chill, maybe just gnarly… or whatever these kids are calling it nowadays.
So... let me get a pen to switch this around.
Trendsetter Bendsetter: a person who can spot new trends ^ early on and spreads these fads reach out to new locations and work with other social groups to create positive change.
7
their community
Diversity, Equity, and Inclusion (DEI):


A Worthy Goal for SUD Treatment and Recovery
Consider these scenarios:
A woman who uses a wheelchair is relieved to find out that the inpatient treatment facility to which she has been referred is accessible.

A non-binary member of a recovery group is pleasantly surprised that the facilitator honors their identity.


A teenager who was raised by his grandparents is thankful that the substance abuse prevention program at his school is inclusive of all kinds of families.

THE RESPONSE // WINTER 2022-23 8 FEATURE
A non-native English speaker is grateful to find an interpreter when she receives an assessment for a substance use disorder (SUD).
A Black man feels validated because his therapist understands the impacts of minority stress.
Danelle Bower, PhD, MSW
These examples highlight service providers and professionals who are following the principles of Diversity, Equity, and Inclusion (DEI). DEI is a top priority for many organizations. Businesses and non-profits recognize the importance of serving all of their clients in an equitable manner. DEI has three major principles.

The first major principle of DEI is a commitment to increasing diversity in its various forms. Diversity recognizes human differences with respect to race, ethnicity, sex, sexuality, gender/ gender identity, religion/spirituality, age, physical differences, social class, psychological development, and other aspects of one’s identity. People with different life experiences bring a variety of outlooks, which can spur innovation. Diversity enriches organizations and communities. Research shows that organizations with more diversity arrive at smarter decisions, make fewer errors in judgment, and demonstrate greater creativity and effectiveness in solving problems (Sommers, 2006; Nathan & Lee, 2015 & Levine et al., 2014).
Confronting bias and discrimination with the goal of equity in mind is a second principle of DEI. As humans, we all possess unconscious bias. While this is a natural part of the human condition, it is not inevitable. An awareness of our own biases is the first step. Then, through reflection and challenging our existing beliefs, we can practice what Patricia Devine (2012) calls “prejudice habit-breaking.” Research shows that individuals who have this level of awareness are more likely to speak up when they see discrimination in their workplaces and communities.
continued on next page
Definition of terms:
Ally
An individual who acknowledges their own privilege and stands up when they see discrimination
Ethnicity
One’s cultural heritage
Gender
Social rules and norms associated with being a girl/boy or woman/man
Gender Identity
An individual’s personal experience with gender
Non-binary
An individual whose gender identity is outside the gender binary (girl/boy, woman/man)
Race
A social construction that groups people based on physical characteristics
Sex
Physical differences as distinguished by chromosomes and genitalia
Sexuality
One’s sexual and/or romantic attraction
Sexual Minority Adults Refers to non-heterosexual individuals
Unconscious Bias
Subconscious stereotypes that individuals hold and can lead to discrimination
9
This principle also recognizes that the social experiences of groups are different. There are groups that are disproportionately impacted by social problems. For example, substance use rates are higher for sexual minority adults (SAMHSA, 2020). Minority stress, discrimination, harassment, stigma, and isolation are risk factors for SUD. Further, racial minorities are less likely to receive treatment for a SUD (SAMHSA, 2020). These disparities are a result of unequal resource distribution, unconscious bias on the part of providers and racism. The principles of DEI ask us to reflect and consider this discrimination. Equity is a necessary goal in order to address these disparities.
The aim of the final principle of DEI is to intentionally make spaces as inclusive, accessible, and welcoming as possible. A recent podcast from The Takeaway (WNYC Studios, 2021) reported on an organization, Music: Not Impossible, which used technology to create a type of vest (Haptic Suits) for use by Deaf individuals, which “translate music into vibrations that people can then feel throughout their entire body” (para. 1). The haptic suit is an accommodation which serves as an intentional inclusivity act for the Deaf. This example of music inclusivity can serve as a model for those engaged in reducing the stigma of SUD. Treatment providers, advocates and members of the recovery community can find their versions
of the Haptic Suit. Additionally, this third principle considers the voices that are heard and those that have been forgotten or misunderstood. There are many different configurations of families; however, some families are not represented as well as others. For example, an individual seeking drug and alcohol treatment might notice that a facility only has pictures of the traditional nuclear family on its brochures and posters. It may make this individual hesitant to seek treatment as the environment does not feel inclusive to someone whose family does not fit into this box. A non-binary individual seeking treatment for a SUD might feel invisible if the intake form they fill out does not leave room for their gender identity. A woman who has experienced trauma may be hesitant to return to an event at a recovery center because she felt trapped due to the placement of the furniture in the room.
Many DEI advocates have added a “B” to the acronym DEI for belongingness. Individuals and groups committed to serving anyone in need of SUD prevention, treatment and recovery should intentionally think about their spaces, materials, and methods to enhance a sense of belonging for all.
Some tips to enhance your commitment to DEI include the following: notice who is missing at the proverbial table; learn more about the populations you serve; examine your organization’s practices to see who is left out; be an ally and support the events of the communities you want to reach. Organizations that want to increase their commitment to diversity should view their processes through a critical lens.
They can ask questions such as:

• Are a variety of perspectives apparent at all levels of our organization?
• What groups do we need to hear from more?
• Do we understand the populations we serve and how can we learn more about them?
• How can we stand up and be an ally when members of various groups face discrimination?
• How can we ensure we do this even within our own organizations?
Most importantly, it is essential that we approach DEI work with grace and humility. We may fail sometimes, but it is important that we show compassion to ourselves and others, recognize our mistakes and work to do better.
THE RESPONSE // WINTER 2022-23 10 FEATURE S FI C UPP RTIVE ONCEPTS FOR AMILIES, NC. JOIN OUR TEAM & BE HAPPY - In-Home Caregivers $15+ No Experience Needed! - Paid training, begin your career in Health Services All shifts available - Pt & Ft, flexible schedules - $1,000 sign on bonus - $250 pt sign on bonus - $1,000 referral bonuses unlimited, refer your friends & make extra $$$$$$ unlimited - Assist individuals w/ Intellectual DisabilitiesVehicle provided while at work, spend your day making someone’s life better: Shopping ,outings, Dr Appts. attending day programs, and more! Some cooking, cleaning and personal care too. - Positions in most counties in Pa- Berks, Schuylkill, Lebanon, Lehigh, Allegheny, Juniata, Mifflin, Montgomery Providing compassionate care since 1993 #CareersInCaring Our
219 Noblestown Rd Carnegie, Pennsylvania 15106 120 Prospect St. Reading, PA 19606 SCAN TO APPLY
Locations

Diversity, Equity, and Inclusion in Substance Use Treatment
 Jolynn L. Haney, PhD
Jolynn L. Haney, PhD
LGBTQ+ refers to lesbian, gay, bisexual, transgender, queer, and questioning individuals. Although each of these groups has unique characteristics, one of the shared features across the LGBTQ+ community is that its members are at high risk for mental health and substance use disorders. Unfortunately, the stigma associated with having a substance use disorder, combined with the discrimination from being a member of a sexual minority, can be a barrier to getting treatment.

Understanding the Problem
Unfortunately, we do not have a clear idea of substance use disorder prevalence among the LGBTQ+ population. One of the reasons we lack this knowledge is because understanding prevalence depends on carefully constructed and conducted national studies that ask questions about sexuality. Until recently, few federally funded studies have asked about individuals’ sexuality. For example, the Survey on Drug Use and Health (NSDUH) did not include items about sexual orientation until 2015.1 The survey designers made these changes to identify health issues among sexual minorities and to track changes in these groups over time. By collecting this information, NSDUH researchers hoped to better understand the factors influencing substance use. In turn, this knowledge can help inform policies that support prevention, treatment, and recovery for the LGBTQ+ community.
Another issue that affects accurate statistics about LGBTQ+ individuals and substance use is openness in responding to survey questions. Survey participants, particularly those in older age groups or specific cultures, might be less likely to disclose information about their sexual orientation and preferences than younger age groups or other cultures.2 As a result, prevalence estimates on sexual orientation among those with substance use concerns could be underreported.
FEATURE
12
The Need for Specialty Services

In addition to needing better data on the LGBTQ+ population’s experiences with mental health and substance use treatment, we also need more services that offer specialty care. For example, in 2015, around 1.7 million sexual minority adults needed substance use treatment. Of these adults, however, only about 260,000 (10.6%) received treatment at a specialty facility.1 One critical reason we need specialized treatment and treatment choices is that these programs can improve access to services for the LGBTQ+ community. For instance, a 2021 study found that sexual minority adults were only half as likely to access treatment compared to non-sexual minority adults because they did not know where to go for treatment or could not find the treatment they needed.3
Consider the following facts to understand why improving substance use treatment access is essential for the LGBTQ+ community:
• Sexual minorities are almost three times more likely to experience a mental health condition than heterosexuals.1

• Transgender adults are almost four times more likely than cisgender adults to have mental health conditions.4

• The risk of suicide (thoughts attempts, completion) is three to six times greater for lesbian, gay, and bisexual adults than for heterosexual adults.5
• LGBTQ+ youth are more than four times as likely to attempt suicide than their peers.6 continued on next page

13
Illicit Drug or Alcohol Use Disorder Past Year by Age Group and Gender
Sexual Minority Sexual Majority
37.1% 32.5% 31.5%
35.6% 21.8% 12.4%
16.1% 11.0%
Ages 18-25 Ages 26+
Source: National Survey of Drug Use and Health, 2020, Public Use Data Analysis System https://pdas.samhsa.gov/#/survey/NSDUH 2020 DS0001. Sexual minority = lesbian, gay, or bisexual; sexual majority = heterosexual. Illicit drugs include marijuana, cocaine (including crack), heroin, hallucinogens, inhalants, methamphetamine, or prescription psychotherapeutics (i.e., pain relievers, tranquilizers, stimulants, and sedatives).
In addition, the LGBTQ+ community faces discrimination across different life domains: at home, at school, in the workplace, in the housing market (renting or buying), and in receiving healthcare, including life-saving medical care.6 “Minority stress” describes the chronic stress that marginalized groups experience when faced with long-term pervasive discrimination and stigma. This stress is intensified for sexual minorities who are also members of other minority groups (i.e., people of color who are sexual minorities).7
Deciding Where to Get Treatment
There are many things to consider when selecting a substance use treatment program. Although some treatment facilities offer specialty care for sexual minorities, one study found that 70% of these programs were no different from treatment programs that provided services to non-sexual minorities.8 A current Pennsylvania treatment facilities survey conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA) showed that 133 (22.0%) facilities offer specialized substance use treatment services for sexual minority adults.9 Compared to the percentage of programs in other states and nationally, Pennsylvania fell below the national average.
Although 22% is low, it is a notable improvement from 2010, when only 35 (less than 7%) of Pennsylvania facilities reported having specialty programming for sexual minorities.9
There are a few ways to find specialty care. For example, SAMHSA has a list of specialty programs on its website.9 Another free search tool is the Addiction Treatment Locator, Assessment, and Standards Platform (ATLAS.)10 As previously mentioned, some of these programs may offer sexual minority treatment services in name only. Therefore, the following questions may be helpful when deciding on an LGBTQ+affirming treatment program11:
• Does the facility have culturally diverse and competent therapists who can recognize and address the needs of individuals who identify as LGBTQ+?
• Does the facility distinguish between the clinical needs of individuals within the LGBTQ+ group to provide clientcentered care that differs for each sexual minority subgroup?
• Does the facility address relapse prevention in social contexts that apply to the LGBTQ+ community?
THE RESPONSE // WINTER 2022-23 14 FEATURE
Male Female
• Are stress management and other coping skills addressed to help clients who face discrimination and prejudice related to having a minority status?
• Does the facility help clients with self-acceptance and selfdisclosure issues concerning their sexual orientation or gender identity?
• Given the high rate of mental health distress among sexual minority populations, can the facility recognize and address co-occurring mental health concerns?
• Does the facility address the intersection between sexual orientation or gender identity and other specialty population needs, such as those members of the LGBTQ+ community who are people of color, women, pregnant or postpartum women, veterans, and older adults?
• Is the program trauma-informed? This question is critical because there is a high rate of trauma experienced by the LGBTQ+ population.
Final Thoughts
When we talk about diversity and diverse groups, it is important to remember that diversity also exists within these groups. Although the LGBTQ+ community shares sexual minority status, each group has distinct characteristics. Therefore, even though it is a common practice to use the LGBTQ+ acronym to refer to this group collectively, we need to keep in mind that each group is diverse. In other words, “one size does not fit all” in specialty care within the LGBTQ+ community.
The pathway to recovery is a complex process experienced differently by each person undertaking the journey. Cultural sensitivity and humility are core components of care that enhance the treatment experience, encourage engagement, and support treatment retention. Specialized services for minority populations need to demonstrate that they offer unique care and are not simply branding themselves as “LGBTQ+” services. As community members, we can help improve things by being aware of these issues and supporting advocacy efforts to provide better, more diverse services.
Sources:
1. Medley, G., Lipari, R. N., & Bose, J. (2016). Sexual orientation and estimates of adult substance use and mental health: Results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review, 10, 1–54. https://www.samhsa.gov/data/sites/ default/files/NSDUH-SexualOrientation-2015/NSDUH-SexualOrientation-2015/NSDUH-SexualOrientation-2015.pdf
2. Morgan, R. E., Dragon, C., Daus, G., Holzberg, J., Kaplan, R., Menne, H., & Spiegelman, M. (2020). Updates on terminology of sexual orientation and gender identity survey measures (FSCM 20-03). Federal Committee on Statistical Methodology. https:// nces.ed.gov/fcsm/pdf/FCSM_SOGI_Terminology_FY20_Report_FINAL.pdf
3. Haney, J. L. (2020). Sexual orientation, social determinants of health, and unmet substance use treatment need: Findings from a national survey. Substance Use & Misuse, 56(2), 205-213. https://doi.org/10.1080/10826084.2020.1853775
4. Wanta, J. W., Niforatos, J. D., Durbak, E., Viguera, A., & Altinay, M. (2019). Mental health diagnoses among transgender patients in the clinical setting: An all-payer electronic health record study. Transgender health, 4(1), 313-315. DOI:10.1089/trgh.2019.0029
5. Ramchand, R., Schuler, M. S., Schoenbaum, M., Colpe, L., & Ayer, L. (2021). Suicidality among sexual minority adults: Gender, age, and race/ethnicity differences. American Journal of Preventive Medicine, 62(2), 193-202. https://doi.org/10.1016/j. amepre.2021.07.012
6. Johns, M. M., Lowry, R., Haderxhanaj, L. T., et al. (2020). Trends in violence victimization and suicide risk by sexual identity among high school students — Youth Risk Behavior Survey, United States, 2015–2019. Morbidity and Mortality Weekly Report, 69, (Suppl-1):19–27.
7. Schuler, M. S., Rice, C. E., Evans-Polce, R. J., & Collins, R. L. (2018). Disparities in substance use behaviors and disorders among adult sexual minorities by age, gender, and sexual identity. Drug and Alcohol Dependence, 189, 139-146. https://doi.org/10.1016/j. drugalcdep.2018.05.008
8. Williams, N. D., & Fish, J. N. (2020). The availability of LGBT‐specific mental health and substance abuse treatment in the United States. Health Services Research, 55(6), 932-943. https://doi.org/10.1111/1475-6773.13559
9. Substance Abuse and Mental Health Services Administration. (n.d.). Behavioral health treatment services locator. https://www. samhsa.gov/find-treatment
10. Addiction Treatment Locator, Assessment, and Standards Platform. (n.d.). https://www.treatmentatlas.org/ 11.New York State Office of Addiction Services and Supports. (2022). LGBTQ-affirming program endorsement standards and guidance. https://oasas.ny.gov/system/files/documents/2022/06/lgbtq-affirming-program-endorsement.pdf
15
Employee
Positivity at
High
Albert Dallao, ARCpoint Labs of Reading, PA
We have more openings than applicants and we need people!” A commonly heard employer statement over the past two years. As employee shortages continue to challenge the business landscape, many employers are relaxing their hiring requirements. Changing or relaxing requirements to pass an employment drug test may be one way of bringing more employees through the door. But a change in your employee drug testing requirements comes with risks.
In its 2022 Annual Drug Testing Report and Industry Insights Report, Quest Diagnostics, a leading drug test provider, indicated the rate of positive drug test results reached its highest rate since 2001. The data is based on testing results completed through 2001. This report also indicated that positivity rates were up over 30% from an all-time low in 2010-2012.
Nearly One In 20 Test Positive



Nationwide workforce testing results reported by Quest Diagnostics in 2021 indicate a 4.6% positivity rate among employees tested. Several drug categories saw positivity rates increase year over year including Marijuana, up 8.9%, Amphetamine (including Methamphetamine), up 7.8%, and Cocaine, up 5.0%. Opiate and Oxycodone positivity rates continued to trend downward, decreasing 19% from 2020 to 2021 with an overall reduction of 56.4% over the past five years. (See chart below.)


THE RESPONSE // WINTER 2022-23 16 FEATURE
Drug
Test
Two-Decade
Positivity Rates From 2020-2021 *Nationwide Workforce Testing Results Marijuana Increase 8.9% Cocaine Increase 5.0% Amphetamine (including Methamphetamine) Increase 7.8% Opiate and Oxycodone Decrease 19% “
Should We Hire Them?
According to the same Quest Diagnostics report, preemployment positivity rates have increased 17% over the past 5 years. More alarming, the post-accident test (workplacerelated incidents) positivity rate increased nearly 42% during the same period. In 2021, post-accident positivity rates for Marijuana increased 63% and Cocaine rates increased 266.7% versus 2020. The growing rate of post-accident positive results suggests that more employers are opting to relax preemployment testing requirements and/or are willing to risk the higher costs related to more workplace accidents to gain employees.

Should Employers Stop Testing for Marijuana?

Local Trends – Berks County
Based on random employee testing performed by local test provider, ARCpoint Labs of Reading, PA, overall positivity rates during the 2019-2021 period ranged between 7.5% and 8.5%. During the first three quarters of 2022, the overall employee positivity rate jumped to 12%. Marijuana continues to be the major contributor to these rates…accounting for 75% of the positive tests in 2021 and 87% for positive test results in 2022 (to date). For both years, Amphetamine (including Methamphetamine) and Cocaine contributed to the majority of the non-marijuana related positivity rates.
A major contributing factor to the Marijuana positivity rate increase can be attributed to the emergence of Medical Marijuana access in Pennsylvania. In 2022, approximately 50% of local employees testing positive for Marijuana provided a valid Pennsylvania Medical Marijuana card.
In addition, many local employers are accommodating Medical Marijuana use in safety-sensitive job positions and/ or considering the elimination of Marijuana from their pre-employment drug test programs. While this may open opportunities for more candidates to be hired, the employer may ultimately incur more costs associated with post- accidentrelated incidents and increased encounters of “at risk” employee behaviors.

17
continued on next page
Protecting your Employees and Your Business

A typical workplace drug testing program includes preemployment testing, post-accident testing or “post-incident” testing and reasonable suspicion testing, also referred to as “for-cause” testing. An employer may also decide to include periodic testing, return-to-duty testing, and follow-up testing as part of their workplace testing program. Random testing is usually more effective at detecting and deterring drug use than pre-employment testing because employees do not know when they may be selected for testing.
Employers and employees agree that impaired workers are a threat to the workplace, the public, and other employees. All employers should have workplace policies established that include identification of impaired employees. Training programs are available for managers, supervisors, and employees which can help with establishing a formal process for identifying and documenting reasonable suspicion situations.
Also, employers need to understand the risks associated with accommodating Marijuana use. The Pennsylvania Medical Marijuana Act provides employers with certain rights when faced with accepting or denying Employee Medical Marijuana use. Know your employer rights under this act before you decide to accommodate Medical Marijuana card holders or decide to eliminate marijuana testing. Before making any changes to your Marijuana testing policy, consider reviewing the changes with your workman’s compensation provider.
Employee illicit drug use is trending on the rise! Once you make the decision to eliminate or change your drug testing requirements, it is nearly impossible to reverse that decision.


References:
Quest Diagnostics 2022 Drug Testing Index Report (www.questdiagnostics.com/business-solutions/employers/ drug-screening/knowledge-center/drug-testing-index) ARCpoint Labs of Reading PA (www.ARCpointLabs.com/Reading)

THE RESPONSE // WINTER 2022-23 18 FEATURE
610-375-4426 19 N 6TH ST, STE 300, READING, PA HOURS: 8 AM-4 PM • M-F Drug & Alcohol Assessments • Treatment Referrals • Peer-to-Peer Recovery Support for all Publicly Funded Berks County Residents NO INSURANCE? WE CAN HELP! VISIT WWW.BERKSTASC.ORG FOR DETAILS WALK-IN ASSESSMENTS & TREATMENT REFERRALS, 8 AM-4 PM DAILY. COMMERCIAL INSURANCES NOT ACCEPTED
The devastating effects of the opioid epidemic have been felt nationwide. Berks County, like most parts of the Country, has not been immune to the impact that the opioid epidemic has had on municipalities. Notably, in 2021, Berks County found its overdose death rate to exceed the national average. The difficulty in fighting the opioid epidemic has been compounded in recent years with the ever-growing prevalence of Fentanyl and the unique challenges posed by the COVID pandemic. Faced with these growing difficulties, many states and local political subdivisions decided to pursue litigation against opioid pharmaceutical distributors and manufacturers to secure some measure of relief against the unrelenting challenges posed by opioids on communities.
In what has collectively become known as the “National Opioid Settlement,” nationwide settlements have been reached to resolve all litigation against the three largest pharmaceutical distributors: McKesson, Cardinal Health, and AmerisourceBergen (“Distributors”) and manufacturer Janssen Pharmaceuticals, Inc., and its better-known parent company, Johnson & Johnson (“Manufacturers”). Berks County, as a political subdivision, was eligible for, and has agreed to
How the National Opioid Settlement Will Affect Berks County
Cody L. Kauffman, Esq.
participate in, the National Opioid Settlement. With money from the settlement beginning to flow through the County, this article aims to provide background on the litigation, the settlement, and, how the distributed money will be used to combat the opioid epidemic in Berks County.
As the name implies, the National Opioid Settlement is not specific to Berks County, nor to Pennsylvania for that matter. Rather, the settlement was a product of negotiations that involved a bipartisan group of State Attorney Generals. Prior to agreeing to the settlement, negotiations had been ongoing for many years. The settlement resolves over 4,000 claims of local and state governments throughout the Country.
While varied in nature, the underlying allegations of most of the lawsuits involve claims of deceptive marketing practices and/or overdistribution of opioids. The Manufacturers and Distributors agreed to pay a total of $26 Billion to resolve the litigation.

19 FEATURE
continued on next page
In addition to the significant monetary figure, the settlement also includes requirements for the companies to implement internal policy changes that are hoped to minimize the risk of future harm and prevent a recurrence of this public health crisis in the future. Among other things, the Distributors will be required to establish an independent clearinghouse that will provide the Distributors and regulators with data analytics that establish where the opioids are going and how often. Additionally, Johnson & Johnson has agreed to stop selling opioids for at least 10 years and to further not fund, promote, or lobby activities relating to opioids.
As mentioned, the total amount of the settlement is $26 Billion and is structured as follows. The Distributors will be required to pay a total of $21 Billion over a total of 18 years. Johnson & Johnson will be required to pay a total of $5 Billion over 9 years. The combined maximum value of the settlement for Pennsylvania was just over $1 Billion, specifically, $1,070,609,642. The term “maximum value” is used because the total settlement value is participation-based: i.e., the more political subdivisions that participate in the settlement, the higher the total settlement value for Pennsylvania. The Pennsylvania entities eligible to participate in the settlement include the State, Counties, municipalities with a population of 10,000 or more, and certain special districts that include large school districts and health/hospital districts. The settlement includes those entities which have previously pursued litigation against the manufacturers/distributors and also those who have not. All 67 Pennsylvania Counties have signed on to participate in the settlement.
In Berks County, the municipalities which were eligible to participate in the settlement include Amity Township, Cumru Township, Exeter Township, Muhlenberg Township, the City of Reading, Spring Township, and Wyomissing Borough.

Like the 67 counties, all seven eligible Berks County municipalities have joined the settlement. In short, Berks County has done its part to maximize the settlement proceeds flowing to the County. Additionally, District Attorney John Adams, by virtue of his previously filed litigation against the Distributors and Manufacturers, will be eligible to receive additional settlement proceeds for his Office. While the settlement proceeds will ultimately flow through the County and not directly to each eligible municipality, their participation plays a key role in ensuring the settlement dollars are maximized for Berks County. Those municipalities, like all others in Berks County, will realize the benefit of the settlement dollars when they are disbursed through the County.
Of the just over $1 billion that will be distributed to Pennsylvania, 70% of those proceeds will be going directly to the Counties. The intra-County allocation is determined by various opioid-related metrics. The metrics that determine the total allocation for each County include overdose deaths, overdose hospitalizations, Naloxone Administrations, and Morphine Milligram Equivalents (MME) adjustment. Based upon those metrics, Berks County has been determined
THE RESPONSE // WINTER 2022-23 20
FEATURE
to receive 1.88% of the Pennsylvania settlement proceeds earmarked for Counties. This equates to just over $13 million for Berks County, $13,153,973.96 to be exact. Of the remaining 30% of the settlement proceeds, 15% will be going to litigating entities (i.e., entities who have previously filed litigation against the Distributors/Manufactures), while the remaining 15% will be controlled by the Legislature.
The funds will be disbursed directly to the counties via the Pennsylvania Opioid Misuse and Addition Abatement Trust (“Trust”). The Trust was created by virtue of the Commonwealth Court formally entering the Consent Judgement Order, which formalized the settlements and formally created the Trust. The Trust will function as the overseer of the settlement proceeds both in distributing the funds and ensuring they are used properly. The trust is comprised of a chairperson appointed by the Governor, a secretary of one of Pennsylvania’s health & human services agencies, four legislative member trustees, and seven regional trustees. Berks County is a member of the Settlement’s Capital Region, which consists of Adams, Berks, Centre, Cumberland, Dauphin, Fulton, Franklin, Huntingdon, Juniata, Lancaster, Lebanon, Mifflin, Perry, Snyder, Union, and York Counties. Commissioner Robert Postal of Mifflin County has been selected as the Capital Regional trustee to serve on the Trust.
As mentioned, the Trust will oversee how the settlement dollars are spent to ensure they are used for permissible purposes. The opioid settlement differs from previous settlements, such as the tobacco settlement, in that the funds must be used for opioid remediation and future opioid abatement practices. The funds cannot be used for purposes unrelated to opioid remediation. The settlement specifically outlines agreed-upon usages of the funds, within “Exhibit E” to the settlement agreement. Exhibit E outlines the specific purposes for which the funds can be used. A key focus of the settlement was that the funds must be used to address the opioid epidemic and the structure of the settlement ensures that the monies can only be used for approved opioid remediation/abatement purposes. The
settlements include strict reporting requirements to ensure the funds are not improperly spent. The Trust will be establishing channels of communication so that Counties can confirm that intended usages of the funds are indeed eligible under the terms of the settlement.
Now that the Courts have signed off on the settlement agreements and the Trust has been formally created, Counties have begun to see the settlement proceeds. Berks County received its first payment of $538,130.62 from the Trust in early September 2022.
Recognizing the importance of ensuring the funds were administered in a way that maximized their impact, Berks County has contracted with the Council on Chemical Abuse (COCA) to administer the opioid settlement funds in Berks County. COCA, as the single county authority in Berks County, has been working to prevent substance use and promote treatment and recovery from addiction since 1971.

From the County’s perspective, having COCA administer the opioid settlement funds was a logical choice. COCA’s expertise in the field will ensure the opioid settlement funds are not just allocated but allocated effectively.


continued
Do you have unused or expired In Berks County, 49 percent of teens who PA Youth Survey claimed to have acquired help prevent misuse and protect our enviroment
on next page
How the funds will be distributed in Berks County will be guided by the “core abatement strategies” outlined within Exhibit E to the Settlement Agreement. Those core strategies are as follows:

• Expanding training, and increasing distribution, for the use of Naloxone or other approved drugs to reverse opioid overdoses.
• Increase distribution, provide education & awareness training, and provide treatment and recovery support services for Medication-Assisted Treatment (MAT) and other opioid-related treatment.
• Provide comprehensive evidence-based treatment and services, including expanding Screening, Brief Intervention, and Referral to Treatment (SBIRT) services, for pregnant & postpartum women with co-occurring Opioid Use Disorder (OUD) and other Substance Use Disorders (SUD).
• Expanding treatment, services, and recovery support for Neonatal Abstinence Syndrome.
• Expansion of warm hand-off programs and recovery services.
• Treatment for incarcerated populations to include treatment and recovery support to inmates and those transitioning out of the criminal justice system with OUD and co-occurring SUD/MH disorders.
• Funding for prevention programs to include media campaigns to prevent opioid use, school prevention programs, medical provider education for best practices, community drug disposal programs, and training for first responders to participate in services that connect at-risk individuals to behavioral health services/support.
• Expanding syringe service programs to include access to sterile syringes and linkage to care and treatment of infectious diseases.
• Data Collection and Research to analyze the effectiveness of the abatement strategies within the State.
In speaking at a Berks County operations meeting before the Berks County Board of Commissioners, COCA’s Executive Director, Stanley Papademetriou, outlined COCA’s overall strategy for administering the settlement funds in Berks County. In formulating the strategy, COCA and Papademetriou closely reviewed the parameters of Exhibit E and worked to create a strategy consistent with the core strategies outlined in the settlement agreement. Importantly, COCA acknowledged that the opioid crisis is not a geo-specific problem within the County, but rather, one that is ubiquitous and indiscriminate. Due to this, COCA’s implementation of the settlement funds will be focused on ensuring the funds are used to provide benefits countywide. To that end, COCA plans to utilize the valuable relationships they have fostered with local providers
to ensure the funds are getting to where they belong and are needed: the Berks County Community. Papademetriou outlined that the guiding principles for how the funds will be administered in Berks County include addressing existing service gaps, sustaining those services that have proven to be effective, and collaborative community efforts with organizations such as the SOS Berks Opioid Coalition.
COCA used these principles to create three main strategies for how the settlement funds will be utilized: Treatment (treating OUD, supporting those in treatment and recovery, and connecting those who need help to appropriate services), Prevention (prevention of opioid misuse, prevention of overdose deaths and other harms, and safe medication
THE RESPONSE // WINTER 2022-23 22 FEATURE
management), and miscellaneous strategies including support for first responders, training and workforce development, participation in research and evaluation. COCA’s plan will be reviewed and updated yearly to ensure progress is being made toward their goals and the funds are being maximized. As the needs of the Community evolve, so too will how the funds are administered. COCA has, and will continue to, work closely with Berks County’s leadership to ensure the funds are administered in a manner consistent with the core strategies outlined within Exhibit E that best maximize the settlement funds in Berks County.
While the opioid epidemic will undoubtedly continue to present challenges on a national and local level, the National Opioid Settlement funds are a welcome and valuable addition to the battle against opioids. Due to the cooperation of all eligible municipalities throughout the County and the County’s subsequent partnership with COCA to administer the funds, Berks County is in a strong position to ensure the impact and effectiveness of these funds are maximized. The opioid epidemic has not discriminated, with its impact being felt by all communities in Berks County. Through the use of these settlement funds, the County and COCA are committed to ensuring the dollars serve our communities, our residents, and those who work tirelessly to fight this battle. While disbursed directly to the County, these settlement dollars belong collectively to the County’s communities, residents, and providers. It is the County’s goal to remain as transparent as possible with how the settlement funds are administered. We welcome input from the Community regarding how the dollars should be spent. Administering these funds is a tremendous responsibility, which presents an equally tremendous opportunity to make a difference. It will take a collective effort to combat the evolving opioid crisis, but with the assistance of the settlement funds, the County and COCA are committed to ensuring Berks County realizes the full potential of these dollars.
We Have DailyPay


Sources:
https://nationalopioidsettlement.com/executive-summary/ https://www.wakegov.com/national-opioid-settlement https://www.naag.org/issues/opioids/ https://ncdoj.gov/attorney-general-josh-stein-national-opioid-settlement-finalized/ https://www.motleyrice.com/article/26-billion-settlement-opioid-distributors-jj https://www.doj.state.wi.us/news-releases/drug-distributors-and-johnson-johnson-commit-26-billion-opioid-agreement https://www.readingeagle.com/2022/03/29/berks-county-receive-16-million-opioid-settlement/

23 SCAN & A P P LY TO AY #CAREERSINCARING #FINDYOURPURPOSE #MAKEADIFFERENCE WWW.APISMGT.ORG/CAREERS We Offer: Sign On Bonuses Competitive Pay Flexible Hours Great Benefits PT & FT Positions Join Our AwardWinning Team!
Get Paid Everyday Apis Services, Inc. We support 32 highly successful businesses & non-profit organizations throughout the USA!
Loss: Understanding the Connection to Substance Use
 Dr. Ramona Roberts, Executive Director, Caron Outpatient Treatment Center Aliyah Dean, Kutztown University
Dr. Ramona Roberts, Executive Director, Caron Outpatient Treatment Center Aliyah Dean, Kutztown University
As human beings we stand at the precipice of conscious life in the natural world. Just as we make connections, so does the natural world around us. The question to ask, however, is what makes us different from other species in the natural world? The answer to that is not love itself, but how love is expressed. Love is one of the most powerful feelings that can be universally expressed and understood. What love does not exempt us from is the grief that we are given when we lose someone in our life.
A moment that sweeps us off our feet and stops our world instantaneously. Losing someone can be a traumatic experience for you, the person next to you, or the person in front of you. Grief can result from a multitude of experiences that can include death of a loved one or losses related to aging, miscarriage, retirement, death of a pet, moving from a house with a lot of fond memories, and even loss of life the way you envisioned it due to circumstances like a medical condition or a loved one’s
experience with substance use. It may be expressed in different ways based on the person, their culture, what was modeled to them, and their beliefs surrounding the loss and can show up as intellectualizing, guilt, shame, sadness, regret, longing, denial, helplessness, hopelessness, anger, numbness, fear, or maybe relief. What is imperative to remember during the grief process is that these feelings can easily be displaced.
Prolonged grief has been officially recognized in our newly updated DSM-5 TR (March 2022). Decades of studies on individuals experiencing grief outside of what has been normalized, highly influenced the need for this recent change. Additionally, rather than pathologizing grief, it serves to highlight how disabling grief can be and allow for more service delivery to assist those who are struggling. Prolonged grief can be diagnosed when symptoms persist, adversely causing a disruption in one’s life similarly to post-traumatic stress disorder (PTSD) where some losses may find themselves landing diagnostically.
FEATURE
THE RESPONSE // WINTER 2022-23 24
A person who is experiencing prolonged grief can experience the following symptoms:
• identity disruptions (feeling as if a part of you has died along with the deceased),
• feeling of disbelief about the death, avoiding any reminders that the person has passed,
• intense emotional pain,
• finding it difficult to reintegrate (difficulty engaging with friends/family, difficulty at work or holding work, pursuing interest, planning for the future),
• emotional numbness,
• feeling that life no longer has meaning,
• and intense feelings of loneliness.
PTSD symptoms may overlap here and additionally include intrusive recall/flashbacks/nightmares, arousal symptoms (sleep disturbance, irritability, problems concentrating, and hypervigilance), and changes around mood and thoughts.
Unfortunately, children are often coined the “resilient” group of grief likely due to the mindset that children do not fully understand finality, or the meaning of death itself. Consequently, this can leave children vulnerable to not receiving adequate attention or support during grief. Our youth’s experience with grief is impacted by a range of factors
such as family, their developmental stage, previous losses in their life, their temperament and even their culture or religion. Just like adults, grief shows up differently for each person, and internal and external elements play a crucial role. Children and adolescents can experience fluctuations of emotion, displayed as confusion, anger, sadness or increased worry.
Grief can also show up in their behavior through acting out, sleep disturbances, isolation (social withdrawal), change in eating habits, clinging to familiar adults, and regression to bedwetting or thumb sucking. Then we add the challenges for teens in expectations being placed on them to be able to problem solve and engage in autonomous thinking yet relying on their emotional part of the brain as their frontal lobes that are responsible for judgment, impulse control, and decision making are not fully formed until early to mid-twenties.
Our youth may have a challenging time accepting that their loved one is not coming back, may react with emotional outbursts that are intense and hard to regulate, and could be preoccupied with the details of the death. Guilt also ensues with them believing that they might’ve caused the death or were able to prevent it in some way, and this can also grow into anxiety that other important people in their life might have bad things happen to them too.

Recovery. Resiliency. Wellness.
Community Care, a nonprofit recovery-focused behavioral health managed care organization, manages mental health and substance use disorder services for individuals in Berks County’s HealthChoices program. Our goal is to improve the health and well-being of the communities we serve.
We offer substance use disorder services for adults, including:

• Withdrawal management
• Rehabilitation
• Medication-assisted treatment
• Certified recovery specialists
If you would like more information about services or help with your recovery, call Community Care at 1.866.292.7886.
25
continued on next page
Grief can also easily extend its hand and meet the firm grip of substance abuse as we see that youth often suppress their grief or cope with it in unhealthy ways that could involve self-injury, substance use, and isolation. This in turn can lead to increases in depression/anxiety, and a decline in academic performance.
In a 12-month period between September 2020 and September 2021, 104,000 Americans died due to a drug overdose. As of 2020, the National Survey on Drug Use and Health stated that 40.3 million people, from the ages of 12 years and older, had a past-year substance disorder.

Many try to escape grief via substances, and we have seen the connection in the literature between the two. One can understand how this emotional pain would want to be avoided, yet what we have learned in the trauma world is that avoidance does not actually make things go away, in fact it can make things worse. According to UCLA research, overdose deaths among U.S. teens nearly doubled in 2020 compared to the previous ten years, as well as increased another 20% in the first half of 2021. The National Center for Drug Abuse highlights that a fifth of eight graders have tried an illegal drug at least once and that almost half of teens report by grade 12 having used illegal drugs, and that about 62% of teens have abused alcohol by that same senior year.
It is common when having a conversation with someone who has a substance use disorder (SUD), that they disclose a loss of an individual in their life that sparked their usage (whether it is first time use or a relapse). Children who have dealt with a loss are at an elevated risk for substance misuse later in life, those who lost their parents between the ages of 6-18.
The conversation often becomes one that is tiptoed around and family and friends may back away just when we need them the most in fear that they do not know the right words to say. We encourage each reader to keep this in mind to help provide the needed support, normalization, and validation of someone’s experience. Allowing oneself to have and feel emotions is important as they all serve a purpose, and they can also spark action in us. Sadness (crying) may prompt reminiscing about your relationship or engaging in things that may honor the person who passed. Loneliness may lead you to start making new connections. Everyone grieves differently and we do not experience the same emotions or the same display of emotions. Vulnerability is strength, and not only helps the individual heal, but serves as a healthy model for others that may be grieving the loss as well.
THE RESPONSE // WINTER 2022-23 26 FEATURE
Grow Your Business in Berks! Restoring Passenger Rail Service to Berks General Elections 2022: What You Need to Know VETERAN SERVICES UPDATES Keeping You Connected Berks County, PA, Government News & Services For Advertising, Contact Tracy@Hoffpubs.com HoffmannPublishing.com • 610.685.0914x201 NEW INAUGURAL ISSUE! Reach 75% of All Berks County Adults… Advertise in Berks 1st Magazine The Official Berks County Government Magazine Sharing news about constituent services, events and timely and trending topics surrounding county services. Berks 1st will be mailed directly to 87,646 households (60% to 70% of every household within many municipalities), and into another 300+ high-traffic locations.
post-traumatic stress disorder, trauma and recovery:

FEATURE
THE RESPONSE // WINTER 2022-23 28
a veteran’s perspective
Walter Gensemer, Vietnam Combat Veteran, Mentor, Hospice Volunteer and Survivor
“I could have left Vietnam after one year, but voluntarily stayed for a second year. I didn’t recognize the damaging effects of my combat deployments until years later. While reading about post-traumatic stress disorder (PTSD) in a veteran’s newsletter, the signs -including irritability, emotional numbness, difficulty sleeping and trouble concentrating – hit home and I sought help. By this time, I was out of the Army for about 20 years before I was finally diagnosed with PTSD. PTSD affects 80% of all combat veterans. I always thought that was for the weaker soldiers. I was strong. I was tough. Over the years, I learned it doesn’t matter how tough you are,” Gensemer said.
PTSD is a mental health condition that can affect ANYONE; it is triggered by a terrifying event you have experienced or witnessed. Symptoms may include flashbacks, nightmares, severe anxiety, depression, and uncontrollable thoughts about the event.
The names for PTSD have changed over the years; Soldiers Heart (Civil War), Shell Shock (WWI), Combat Fatigue (WWII), Operational Exhaustion (Korea), and Post-Traumatic Stress Disorder (PTSD) (Vietnam and after). A few years ago, discussion began on changing its name again to post-traumatic stress injury (PTSI). Professionals felt changing it from disorder to injury would reduce the stigma that is related to this disorder.

14 common symptoms of ptsd:
1. Having unwanted nightmares, vivid memories, or flashbacks of the event that make you feel like it’s happening all over again.
2. Feeling upset by things that remind you of the event.
3. Feeling irritated or having uncontrollable, angry outbursts.
4. Avoiding people, places and/or things that remind you of the event.
5. Feeling emotionally cut off and distant from others.
6. Isolating yourself from family and friends.
7. Feeling numb and losing interest in things you once used to care about.
8. Constantly feeling on guard or hypervigilant.
9. Having difficulty sleeping.
10. Having trouble concentrating.
11. Being jumpy or easily startled.
12. Constant use of drugs or alcohol to numb the pain.
13. Considering harming yourself or others.
14. Overworking often to keep your mind off what happened.
29
continued on next page
Complete a PTSD screening with PTSD Screening Instruments - PTSD: National Center for PTSD (va.gov) and discuss the results with your doctor, a mental health specialist or a counselor. Talk to another veteran. Talk to a family member or friend.


There are two types of treatment that have been shown to be effective in treating PTSD: counseling and medications. Professional therapy or counseling can help you understand your thoughts and reactions and help you learn techniques to cope with those challenging thoughts. Medications can also be used to help reduce tension, irritability, and even help improve your sleep.
“We know that these freedoms were bought at a price … and we honor those who laid down their lives so that we can enjoy those freedoms,” said Gensemer.
If you are suffering from any disabilities you believe to be related to your active-duty military service, please reach out to a local Veterans Service Organization/Officer(VSO) OGC - Accreditation Search (va.gov) to support you and represent your claims into the Veterans Affairs. Advocacy services are free and could result in access to VA benefits such as VA Healthcare and monthly, tax free VA Compensation benefits (among other benefits).
If you are experiencing a Mental Health Emergency or are having suicidal ideations, please call 9-8-8 and Press 1 for veterans.
You can learn more about VA Benefits at www.va.gov or by calling 1-800-MYVA-411.
• Outpatient Substance Use Disorder Counseling
• Outpatient Mental Health Counseling
• Individual and/or group therapy
• Medication Assisted Treatment (MAT)
• Certified recovery/peer specialists
• Physical health and wellness services
• Genoa Pharmacy on site (for both you and your family)
Dr. Netaji, is board certified in Addiction Medicine and specializes in Medication Assisted Treatment (MAT). Dr. Netaji is a caring and compassionate physician who can help you on your road to recovery – always in a judgement-free zone.
Walter Gensemer is a Vietnam Combat Veteran, Purple Heart Recipient who earned three Bronze Stars and several commendations for Heroism. Walter is a Berk County Military Hall of Fame inductee-Class of 2010 and was a recipient of the 2021 American Red Cross Hero’s Award. 2021 American Red Cross Hero.
FEATURE
what can you do if you feel you have ptsd?
THE RESPONSE // WINTER 2022-23 30
645 Penn Street, 2nd Floor, Reading, PA 19601 • berkscounselingcenter.org Here are a few of the services we offer:
Learn how we can help you or someone you love by calling 610.373.4281 A Certified Community Behavioral Health Clinic/Integrated Community Wellness Center Integrated Counseling and Physical Health and Wellness Services serving Adults, Youth and Families.
Dr. NetajiMAT Specialist
Safe
Disposal Bags






Medication Storage and Disposal
The locking medicine case allows for organization and secure storage of medicines and medical supplies.
to
County residents while supplies last.
Medication Lock Boxes
Free
Berks
Bern Twp
Bethel Twp
your unused, expired medications (including pet) to one of the 29 drop boxes throughout
a list of accepted items and locations on the COCA website.
Drop Box Locations Take
Berks County. Find
unused
Do you have unused or expired medications?
teens who
prescription drugs
claimed to have acquired them
You can help prevent misuse and protect our enviroment by safely disposing of your medications. (610) 376-8669 I cocaberks.org/rxsafety About COCA Serving the community since 1971, the Council on Chemical Abuse (COCA) is the coordinating agency for publicly supported drug and alcohol programming in the county. COCA and its partners provide an array of prevention, intervention, treatment and recovery services. Paid for with Pennsylvania taxpayer dollars.
Dipose of
or expired medications safely at home! This disposal process works on pills, patches and liquids. The bag and its contents can then be safely disposed in a household trash can. Bags are available at no cost to Berks County residents.
In Berks County, 49 percent of
said they had misused
in the 2019 PA Youth Survey
“from someone living in my home.”
for affordable and accessible life-saving treatment.
Hoy hay esperanza para un tratamiento a bajo costo y accesible que salve vidas
When it comes to addiction, every second counts.
Today, there’s hope for saving a life with NARCAN®. Berks County residents have access to free NARCAN® opioid overdose reversal kits.
There’s hope for recovery, too. Residents have access to safe, affordable, and accessible drug and alcohol treatment options right here in Berks. Virtual telehealth options are also available.
Cuando se trata de adicción, cada segundo cuenta.
Hoy, existe la esperanza de salvar una vida con NARCAN®. Los residentes del condado de Berks tienen acceso a kits gratuitos de reversión de sobredosis de opioides NARCAN®.
También hay esperanza de recuperación. Los residentes tienen acceso a opciones de tratamiento de drogas y alcohol seguras, asequibles y accesibles aquí mismo en Berks. También se encuentran disponibles opciones de telesalud virtual.
HOPE TODAY THERE’S
for with PA taxpayer dollars.
.
Paid
To order a Narcan® kit, find treatment, and learn more, visit cocaberks.org/HOPE
Para pedir un kit Narcan®, buscar tratamiento y obtener más información, visite cocaberks.org/HOPE .


























 Jolynn L. Haney, PhD
Jolynn L. Haney, PhD


























 Dr. Ramona Roberts, Executive Director, Caron Outpatient Treatment Center Aliyah Dean, Kutztown University
Dr. Ramona Roberts, Executive Director, Caron Outpatient Treatment Center Aliyah Dean, Kutztown University