THE EXECUTIVE CONNECTION
OF NORTH TEXAS









Amanda Brummitt, FACHE
Sarah Sentmore
Kean Villarta
Bert Witherspoon
Audrianne Schneider, FACHE
Kean Villarta
Mike Belkin, FACHE
Tom Peck, L-FACHE
Mark A. Riordan
Bert Witherspoon
Sarah Sentmore
Amanda Brummitt, FACHE
info@achentx.org
ACHE of North Texas
Editorial Office, c/o Executive Connection
PO Box 224732
Dallas, TX 75222-4732
p: 972.413.8144
e: info@achentx.org
w: achentx.org
OFFICERS
President
Aaron Bujnowski, FACHE
Managing Director, Health Industry Group | Health Systems Practice, Alvarez & Marsal Holdings, LLC
President-Elect
Ajith Pai, FACHE (Foundation Liaison)
President, Texas Health Harris Methodist Hospital Southwest Fort Worth
Immediate Past President
Felixia Colón, FACHE
Sr. Vice President & Group Operations Officer
SCP Health
Treasurer
Patrick Brown, FACHE
Senior Vice President-Operations, National Group Surgery Partners
Secretary
Joseph Clayton Lawrence, FACHE
Regional President of Operations Sound Physicians
Diversity, Equity & Inclusion Officer
Kris Sanders FACHE (Membership Liaison)
SVP Northern Market Growth & Development Children’s Health
The ACHE of North Texas e-magazine, The Executive Connection, is published triannually and includes information on the latest regulatory and legislative developments, as well as the quality improvement and leadership trends that are shaping and influencing the healthcare industry. Readers get indepth reporting on the issues and challenges facing hospital and health system leaders today. We make it our job to tell you about the great things the organization and Chapter are doing every day to ensure the health of our community. If you have any news and updates that you want to share with other members, please e-mail your items to info@northtexas.ache.org. Microsoft Word or compatible format is preferable. If you have a graphic or picture that you'd like to include, please send it as a separate file. The following are the types of information that our members shared in past ACHE of North Texas magazines, Advocacy Issues, Legislative Issues, Educational Opportunities, Awards / Achievements, Promotions (Members On the Move), Committee Updates, journal submissions, conference submissions, and workshop participations, sharing

Dr. Jim Allard, DNP, RN, NEA-BC, FACHE
ACHE Regent-at-Large, District 4 Chief Nursing Officer, Medical City Arlington
Timothy Bowen, FACHE (Sponsorship Liaison) President, Baylor Scott White - McKinney
Crystal Brown (Foundation Liaison) Vice President Operations/COO Methodist Mansfield Medical Center
Noreen Butte, MD (Physician Advisory Chair/Liaison) Pediatrician
Jared Lange (Networking Liaison) Director, Business Sustainability & Development Parkland Health
Christina Mathis, MHA (Sponsorship Liaison) Chief Operating Officer/Ethics & Compliance Officer, Medical City Plano
Angela Vincent Michael, FACHE (Education Chair/Liaison)
Director, Performance Improvement Methodist Health System
Trinette K. Pierre, DHA, RN, NEA-BC, FACHE (Through March 2024)
ACHE Texas – North Regent Executive Consultant/Advisor, Career Consultant, Professor, TRImani Consulting, LLC
Cassandra Self, FACHE (DE&I Liaison) Program Director, Texas Health Resources
Jared Shelton, FACHE (As of April 2024)
ACHE Texas – North Regent
President, Texas Health Harris Methodist Hospital Hurst-Euless-Bedford
Michael Talley, RRT, FACHE (Mentorship Liaison)
VP of Clinical Operations & Virtual Care, CHRISTUS Health
Keith Thurgood, PhD (Student Council Liaison) Clinical Professor & Program Director, MS Healthcare Leadership and Management, University of Texas at Dallas
Toya White, FACHE (Advancement Liaison)
Chief Operating Officer & Chief Nursing Officer, Texas Health Resources
Corey Wilson, FACHE (Communications Liaison)
Chief Operating Officer, Texas Health Harris Methodist Fort Worth
Timothy Wilson (DE&I Liaison)
SVP, Population Health Management, P3 Health Partners

Welcome to the New Year! It’s hard to believe that we’re already in 2024. We are launching forward to build off the great accomplishments of last year and ACCELERATE — which is our strategic theme for this year.
We received the exciting news that ACHE North Texas was given the Award of Merit as part of ACHE’s 2024 Chapter Management and Awards Program. Our chapter achieved the “Net Membership Growth” performance standard. Net membership growth is measured by the percentage difference between the total number of ACHE-affiliated chapter members in all membership categories at the beginning of the year and at the end of the year. Thanks to all who helped our membership grow last year. We recently went over 1,900 members — a new high for our chapter — and we are working towards the 2k mark!
As part of our Accelerate strategy, you will see some new and exciting educational and networking opportunities throughout the year. As these events are announced, we encourage you to attend and take advantage of the tremendous programming our committees have curated for you. In addition, we are taking another significant step forward with our ACHE of North Texas Foundation. This year, we will select our first local non-profit organization to sponsor and create a scholarship program to assist high school students from disadvantaged areas to pursue healthcare careers. These efforts will help us fulfill the foundation’s mission “to champion educational opportunities, develop current and future healthcare leaders, and promote health equity in our community.”
We encourage you to continue finding ways to engage with ACHENTX in 2024. We need you! We welcome your involvement, your ideas, and your talents. The strength of a chapter lies in the strength of its members. Our chapter is strong and vibrant because of you. So, thank you!
Let’s ACCELERATE into 2024 together!






Since 2021, I have had the honor of serving as your Regent. I cannot tell you of all of the accounts of new friends, strong relationships, and key insights that I have been blessed to gain as the Regent of ACHE of North Texas. Every event, every encounter, and every embrace has left me more determined to be a better leader than I was before our paths crossed. I am so grateful to each member of ACHE of North Texas who supported me, uplifted me, patted me on the shoulder when I needed encouragement, and loved on me non-stop during my time in this role. I pray I have done the same for you.
Throughout my time as Regent, I have had the pleasure of watching the amazing membership of ACHENTX navigate very trying and difficult times in healthcare. I have felt the kindness and support of all of you, our faithful colleagues and members of ACHENTX. You have shown me how to be a stronger leader. You’ve modeled courage when things were scary. You’ve shown grace when situations called for blaming. Although you stayed up late nights pacing the floor, you put on a smile and walked into your organizations with the “we will overcome” spirit that makes healthcare as a profession secondto-none. You’ve optimistically stepped forward and given of yourselves when others shook their heads and stepped back. You’ve shown strength even when you felt weak. You did not pretend that it wasn’t difficult. You faced the harsh reality, and then you changed that reality and made it face you. That is what leaders do. That is what you will be remembered for. That is your legacy.
When I think of the experiences that we’ve had over the past few years, I am reminded of something I’ve always believed in my heart: Leadership is not synonymous with management. It’s so much more than that. Leaders show up even when it’s difficult to do so. Leaders may not have an office key or a fancy title, yet leaders have heart. Leaders do not wear “leadership” for eight or 12 or 16-hours a day, but the mark of a leader follows that leader all day, every day. Leaders are more than just “workers.” Leaders are exceptionally gifted with the ability to positively influence everyone who gets close enough to experience their spark. Leaders are moved by a challenge and they readily face those challenges with strong determination. Leaders are both on the frontline in our healthcare organizations and on committees in our communities. Leaders are strong enough to influence the influential yet compassionate enough to give of themselves in community service venues. Leaders don’t have to
convince others by saying “I’m a leader” because others who respect those leaders will say it without reservation. With that definition stated, please allow me to say what I have felt throughout my years with ACHENTX: You, ACHENTX, are leaders. Keep leading!
It has been my pleasure to work alongside our amazing boards, Mr. John Whittemore, and the members of ACHE Texas Northern Division during my time in this role. I’ve had the support of Mr. Ken Hutchenrider, our past Texas Northern Regent, throughout this journey and I appreciate his leadership and expertise. Each member of our phenomenal chapter has influenced me in a tremendous way. It has been a blessing to serve you all in this capacity and more of a blessing to have learned from you. I am very thankful and grateful for your trust and your support.
As my term and Regent ends in March 2024, I want to welcome Jared Shelton, Regent-Elect for Texas Northern Division. He is an amazing individual and a leader whose reputation precedes him. I am excited to continue to work alongside Jared and all of our amazing Texas Northern Division colleagues as we continue to make Texas Northern the division everyone wants to join! If you have not already done so, please send love to Jared, and congratulate your new Regent-elect. I am confident that you will support him as he takes on this role.

Be blessed. Be safe. Keep smiling. Keep leading.
Much love to you all,
Trin
We are excited to announce another convenient way for members to keep up with their dues payments. In addition to auto-renewal of full dues, we are now offering the opportunity to pay ACHE dues in three installments.
After you make your first installment, ACHE will email you in advance of the second and third payments before credit/debit cards are charged. Additionally, once you sign up for the installment payment plan, your membership will automatically renew each year under the plan. ACHE will continue to keep you informed before processing future payments.
If you have any questions about the installment payment plan, contact ACHE’s Customer Service Center at contact@ache.org or call (312) 424-9400, Monday through Friday, from 8 a.m. to 5 p.m. Central time.
We are pleased to offer members three free online communities for physician executives, Asian healthcare leaders and LGBTQ+ healthcare leaders. The communities’ platform makes it easier than ever for peers to connect in real time, tackle issues together and ask important career-related questions. Members can participate in discussion threads, share resources and best practices, and crowdsource innovative ideas and solutions.
If you have any questions, please contact ACHE’s Customer Service Center at contact@ache.org or call (312) 424-9400, Monday through Friday, from 8 a.m. to 5 p.m. Central time.
Fellows can check on their progress by logging into My ACHE and viewing the FACHE Recertification Progress Tool. There is no need to wait until Dec. 31 to recertify. Fellows should recertify early, pending all requirements have been met, so that they may start earning continuing education and volunteer activities toward their next recertification cycle.
Fellows over the age of 60 that plan to retire within the next five years may be eligible for a one-time only five-year recertification waiver. Fellows in good standing who are retired from healthcare management may transfer to Retired or Life Fellow Status.
ACHE’s 2023–2024 Nominating Committee is calling for applications for service beginning in 2024. ACHE Fellows are eligible for the ChairElect and Governor vacancies and are eligible for the Nominating Committee vacancies within their districts. Those interested in pursuing applications should review the candidate guidelines for the competencies and qualifications required for these important roles. Open positions on the slate include:
• Nominating Committee Member, District 1 two-year term ending in 2026
• Nominating Committee Member, District 4 two-year term ending in 2026
• Nominating Committee Member, District 5 two-year term ending in 2026
• Four Governors three-year terms ending in 2027
• Chair-Elect.
Please refer to the following district designations for the open positions:
• District 1: Canada, Connecticut, Delaware, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont.
• District 4: Alabama, Arkansas, Kansas, Louisiana, Mississippi, Missouri, New Mexico, Oklahoma, Tennessee, Texas.
• District 5: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, Oregon, Utah, Washington, Wyoming.
Candidates for Chair-Elect and Governor should submit an application to serve that includes a copy of their resume and up to 10 letters of support. For details, please review the Candidate Guidelines, including guidance from the Board of Governors to the Nominating Committee regarding the personal competencies of Chair-Elect and Governor candidates and the composition of the Board of Governors.
Candidates for the Nominating Committee should only submit a letter of self-nomination and a copy of their resume.
Applications to serve and self-nominations must be submitted electronically to krock@ache.org and must be received by July 28. All correspondence should be addressed to Carrie Owen Plietz, FACHE, chair, Nominating Committee, c/o Kim Rock, American College of Healthcare Executives, 300 S. Riverside Plaza, Ste. 1900, Chicago, IL 60606-6698.
The first meeting of ACHE’s 2023–2024 Nominating Committee will be held March 21 during the 2023 Congress on Healthcare Leadership in Chicago. The committee will be in open session at 2:45 p.m. Central time. During the meeting, an orientation session will be conducted for potential candidates, giving them the opportunity to ask questions regarding the nominating process. Immediately following the orientation, an open forum will be provided for ACHE members to present and discuss their views of ACHE leadership needs.
Following the July 28 submission deadline, the committee may meet to determine which candidates for Chair-Elect and Governor will be interviewed. All candidates will be notified of the committee’s decision no later than Sept. 29, and candidates for Chair-Elect and Governor will be interviewed in person Oct. 19.
To review the Candidate Guidelines, visit ache.org/CandidateGuidelines. If you have any questions, please contact Kim Rock at (312) 424-9494 or krock@ache.org.
This year, we are extremely proud and deeply appreciative to have five of the industry’s leading companies as our 2023 Premier Corporate Partners:
• Change Healthcare
• Exact Sciences
• Intuitive
• LeanTaaS
• Quest Diagnostics
ACHE’s Premier Corporate Partners play a vital role in supporting our mission of advancing healthcare leadership and the field of healthcare management excellence. These relationships help ACHE support our educational programs and national events, such as the Congress on Healthcare Leadership, and they offer complimentary resources to members, such as on-demand content, white papers and articles, to help address critical issues in your organization.
In return, we offer our partners exclusive opportunities to engage with ACHE members to advance their key initiatives.
We hope you’ll join us in offering a warm welcome to each of our 2023 Premier Corporate Partners. We look forward to their partnership and support in the year ahead.

What are you doing now?
I am currently leading a team project to serve one of the largest healthcare systems in the NYC area. My team is placing advanced practice providers (APPs), and I have placed over 70 candidates in less than one year.
How long have you been a member of ACHE?
I have been a member of the ACHE for about three (3) years.
In your opinion, what is the most important issue facing healthcare today?
I believe that the provider shortage is the biggest challenge healthcare leaders face today. There has been a shortage of doctors for many years. Now, there is also a shortage of APPs and therapists.
Why is being a member important to you? Has ACHE membership been a benefit to you in your career?
I found that membership in ACHE has provided me with a great opportunity to network with other healthcare leaders. I have been exposed to a variety of healthcare professionals.
What advice would you give early careerists or those considering membership?
My advice to early careerists is to be open-minded about your career and try new things. I believe that exploring various professional opportunities is critical to personal and professional growth.
Tell us one thing that people don’t know about you. I am an avid gardener.

What are you doing now?
I am currently serving as a director with AMN Physicians. I work with clients to place permanent healthcare providers, primarily physicians. I also lead a team of three (3) recruiters, who are also placing permanent providers.
How long have you been a member of ACHE?
I have been a member of ACHE for about four (4) years.
In your opinion, what is the most important issue facing healthcare today?
I believe that healthcare disparity is one of the biggest challenges healthcare leaders need to address today. Socioeconomic determinants dictate health more than what is acceptable. We need to improve access to care for all US residents.
Why is being a member important to you? Has ACHE membership been a benefit to you in your career?
I found the biggest advantages of my ACHE membership to be both learning about the most current trends in the healthcare space and the opportunities to grow personally and professionally by networking with other healthcare leaders.
What advice would you give early careerists or those considering membership?
My advice to early careerists is to set high goals and work towards them. I believe that we can achieve so much if we challenge ourselves to be better.
Tell us one thing that people don’t know about you.
I am an adrenaline enthusiast and have bungee jumped off the highest bridge in Europe, located in Switzerland.

I currently lead the Enterprise Analytics team for GI Alliance, which is the largest gastroenterology practice network in the nation with more than 800 providers across 15 states. I am responsible for ensuring that decision makers across the organization are supported with highly useful, relevant and actionable information, which includes managing a team of analysts and overseeing the ongoing development of the company’s data infrastructure.
How long have you been a member of ACHE?
I joined ACHE in 2019 and was active in the Middle Tennessee (Nashville) Chapter until relocating back to the DFW area in 2021 (I grew up in Arlington).
In general, I think the most important issue is how to effectively manage the increased demand for healthcare services resulting from an aging population. Most Baby Boomers have now reached their seventies, and many of the issues we hear a lot about lately—workforce shortages, increasing costs, potential shortfalls in Medicare and Social Security, and several others—are either directly related to or exacerbated by this demographic trend. Meeting this surge in demand while continuing to focus on providing high-quality care at a reduced cost poses a significant challenge.
When I first got into healthcare in 2015, I remember being overwhelmed with the sheer complexity of the industry. While years of experience have certainly contributed a great deal to my understanding, joining ACHE really helped bring it all together and has introduced me to people, concepts and issues that I may not have encountered otherwise. As I’ve continued to progress in my healthcare career, the relationships, knowledge and support I’ve gained through being an active member have been invaluable.



To submit your update, milestone, award or accomplishment, CLICK HERE.
TIANDRA CAESAR accepted a new role as a Compensation Analyst, Associate at Cook Children’s Health Care System.
SAMAN AZIZ, MD, MHPE, MPH, CDIP received the Certified Documentation Integrity Practitioner (CDIP) certification.
SUSAN MERRITT graduated in July 2023 with her Bachelor’s in Healthcare Administration and was recently promoted to Administrative Supervisor for a rehabilitation hospital.
CASSANDRA SELF AND DEEPHA BALAJI completed the Dolan Career Accelerator Program through ACHE.
STEVEN HUNTER was promoted to Regional Director of Advanced Practice Professional Operations - East Region for Baylor Scott & White Health.
CRISTAL RETANA LULE was promoted to Community Relations Officer at Children’s Health.
REA OWENS-BYERLY was promoted to Sourcing Director at Vizient, with oversight of the Cleveland Clinic Cardiovascular Service Line.
WARREN POQUIZ has once again been selected as one of the winners of the 2024 RIchard J. Stull Essay Competition by ACHE National. He won 2nd Place in the Graduate Division of the contest on behalf of Texas Woman’s University and ACHENTX for his paper titled, ‘Navigating the Risks of AI Foundation Models in Healthcare: How Health Systems Can Respond.’ He will be presenting his paper at the ACHE Congress on Healthcare Leadership in Chicago on Wednesday, March 27, 2024.
MIKE BELKIN joined Curative Clinical, an executive search firm specializing in the permanent placement of physicians and advanced practice providers, as SVP. He is celebrating his 20th year in this career.
STEPHANIE MADRID has returned to the DFW Market after an 8 year stint as a district leader for Kindred Healthcare in Houston, TX and markets throughout Florida. She was recently promoted to SVP, Specialty Hospital Operations for ScionHealth where she has responsibility for 21 specialty hospitals and 5 acute rehabilitation units in TX, OK, NM, and AZ.


Why did you join the American College of Healthcare Executives (ACHE)? Maybe it was for industry-leading education. Or, for unrivaled networking opportunities. Maybe it was a way for you to give back to the industry and to the community. Resources offered by ACHE North Texas to its members are some of the best in the country. In fact, the chapter has been recognized for its diversity, communications, and mentoring initiatives.
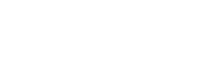
However, there is a resource that few know about – the Life Fellows and Retirees Committee. These dedicated healthcare professionals have devoted decades to their careers and to improving healthcare services to their communities. This is the first in a series of articles that will introduce you to members of this esteemed group. We hope you enjoy getting to know them and learn from their experience and insight.
Phil Wentworth. Jim Berg. Dresdene Flynn-White. Phil Prescott.
Each has left his or her mark on the north Texas healthcare community. We asked each of them to answer questions about their career, the path it followed, the advice they got from mentors and colleagues, and the advice they would give to young healthcare professionals.
Phil’s 50-year healthcare career began in the Army at Fort Sam Houston when he served as a Medical Field Service Officer. He worked for an officer who would later become the first chairman of the Trinity University Healthcare Program. It was at his urging that Phil enrolled at Trinity where he earned two degrees – Bachelor of Science and Master of Health Care Administration. He calls it the best decision of his life.
He spent five decades working primarily with nonprofit, faith-based healthcare organizations in the public and private sectors as well as senior care. He spent more than 30 years with the Presbyterian Healthcare System (now Texas Health Resources), 16 of those years as President of Presbyterian Hospital of Plano. In 2009, he received the Dean Duce Award given annually to a graduate of the Trinity University Program in Healthcare Administration, recognizing his outstanding leadership and significant contribution to the healthcare field.
What are the biggest changes you’ve seen over your career in healthcare?
Phil: The growth of the for-profit sector and the emergence of managed care companies. I’ve also seen significant advances in care, diagnosis, and treatment of diseases. I was in the field when Medicare was implemented. It was supposed to be the end of healthcare in the U.S. as we knew it.
What’s the best advice you received from a colleague, mentor or friend, that helped you in your career endeavors?
Phil: I have been fortunate to have wonderful mentors. My first boss and mentor at the New York City Health and Hospital Corporation, the public health system in New York, always stressed to make nice. Treat everyone the same, whether they were housekeepers, clerks, or professional staff. More recently, a mentor stressed the importance of putting the patient first.
When did you join ACHE and why?
Phil: I joined ACHE in 1975 and achieved Fellow in 1979. I joined because the organization adds credibility to an individual ‘s career and demonstrates his/ her commitment to the profession. It was a ticket to advancement.
Why have you remained a member of ACHE? What value do you receive from your ACHE membership at this point in your career?
Phil: As a Life Fellow I have been able to stay current with our profession through networking, interacting with young professionals, attending educational sessions, and participating in the chapter’s Mentor/ Mentee program.
What one piece of advice would you give to a new MHA graduate or young healthcare professional?
Phil: Don’t worry about the title, but look for organizations that have a mission, vision, and values that you can relate to and embrace. Work hard at your job but balance your work life with your personal life.
Are you optimistic or pessimistic about healthcare’s future?
Phil: I’m very optimistic. The young leaders I have met have prepared well to meet the challenges of the future. Healthcare leaders have always met the challenges and developed creative ways to solve challenges.
What healthcare activities are you currently pursuing?
Phil: I am still involved with ACHENTX as a Life Fellow. I chaired the Life Fellows and Retirees committee and I participate in the Mentor/Mentee program. I also serve on numerous non-profit boards in the healthcare field.

Jim Berg’s 48-year healthcare career was shaped in large part by his 24 years of service in the United States Air Force as a Medical Service Corps Officer. He attended Saint Louis University on an Air Force ROTC scholarship where he majored in Management Science with a focus on Operations Research.
One of his professors was a noted author on hospital management and a member of the St. Louis-based SSM Healthcare System board of trustees. At the professor’s urging, he set his sights on hospital administration as a career. His parents both had healthcare careers and his first “W-2” job, as he calls it, was as a hospital central services tech for $1/hour at age 16. In 1972, he was accepted to the St. Louis University MHA program with a full scholarship. “I made a great decision,” Jim says, “and the rest is history.”
He spent 12 years at Texas Health Presbyterian Hospital of Dallas retiring as President. His career has taken him to senior healthcare leadership positions spanning eight states from Utah to Texas to South Carolina and the upper Midwest. Throughout his career, he has been able to “do good and save money.”
What are the biggest changes you’ve seen over your career in healthcare?
Jim: I’ve seen changes at all levels. The most significant change is the care delivery continuum from prevention/ wellness to inpatient to ambulatory/outpatient to skilled/home care and hospice. Relevant data points: 7.4 hospital beds per thousand people in 1972 compared to 2.4 beds today.
What’s the best advice you received from a colleague, mentor or friend, that helped you in your career endeavors?
Jim: Several come to mind. Relationships are the “secret sauce.” The right culture can be magical. Continuously unpack processes to reduce redundancy, rework, and unnecessary activity.
When did you join ACHE and why?
Jim: I became an ACHE student associate in 1972, a member in 1974, and achieved Fellowship. I transitioned to Life Fellow in 2019. ACHE was considered the professional credential for healthcare leaders and a “must have” for job searches. The Air Force strongly encouraged ACHE membership for Medical Service Corp officers.
Why have you remained a member of ACHE? What value do you receive from your ACHE membership at this point in your career?
Jim: I have a personal commitment to pass it forward to younger colleagues. Previous generations of healthcare leaders mentored me to grow, be successful, and make a difference. ACHE provides a framework to encourage mentoring, networking, growth, learning, and development.
What one piece of advice would you give to a new MHA graduate or young healthcare professional?
Jim: Leaders make a difference in other people’s lives by communicating, clarifying, and modeling the organization’s mission, vision, and values. Leadership “must haves” include culture, vision, the ability to manage weaknesses, and mastering the art of compromise. Each of these is comprised of several components with emotional intelligence and social/ situational awareness most critical.
Are you optimistic or pessimistic about healthcare’s future?
Jim: Optimistic. Prior generations of healthcare leaders have met challenges with innovation and success. Future generations have more resources and technology and will be successful. AI will have a positive impact on healthcare delivery and could be a disruptor.
What healthcare activities are you currently pursuing?
Jim: I quasi-retired (for the second time) at the end of 2020 after serving as President/CEO of Roper St. Francis Healthcare System in Charleston, SC. I chaired the ACHENTX Life Fellows and Retirees committee in 2022 and I continue to serve as a mentor and guest lecturer. I also consult with individuals and private organizations on labor analytics, process improvement, and sustaining a culture of excellence.

Helping others is in Dresdene Flynn-White’s DNA. She began as a social worker and educator and was drawn to healthcare where she saw a critical need that cut across all situations. “I knew I was not physician material, but I understood people, organizations, and management,” Dresdene says.
Her 30-year career began at the University of California, San Diego, and ended with JPS Health Network in Fort Worth. She spent a significant part of her career with Kaiser Permanente. She earned a Bachelor of Arts in Sociology degree from Lincoln University and a Master of Arts in Higher Education degree from Columbia University. She was president of the ACHENTX chapter in 2016 and she received the Regent’s Lifetime of Service Award from ACHE in 2021. She serves on many community and state boards including Baylor Scott & White All Saints Medical Center – Fort Worth, Governor’s Health Care Information Council, and others.
What are the biggest changes you’ve seen over your career in healthcare?
Dresdene: Two areas stand out. First, the public accountability of healthcare providers via vehicles such as HEFIS, NCQA accreditation, patient experience data, and more that resulted in consumerism on the part of patients and families. Second, the expansion of the roles of healthcare providers such as nurse practitioners (NPs) and physician assistants (PAs).
What’s the best advice you received from a colleague, mentor or friend, that helped you in your career endeavors?
Dresdene: Remember who you are here for…it’s about the patient. Even though I didn’t provide hands-on care, my job was to make sure we had the best people who did. I supported them so they could do their best.
When did you join ACHE and why?
Dresdene: I joined ACHE in 2011. In my early career, I was an HR professional, so I focused on that education and certification. As my career evolved, I realized if I wanted to have a broader understanding of healthcare and more opportunities, ACHE membership and certification was what I needed.
Why have you remained a member of ACHE? What value do you receive from your ACHE membership at this point in your career?
Dresdene: Even though I’m retired, my brain still functions! I enjoy keeping up with the issues and challenges. While there are new issues to deal with, some are not so new. How we treat a diverse patient and employee population is not new, neither are mergers and acquisitions. Certainly, the rising cost of healthcare is not new. But how AI will impact care delivery is a new and fascinating dilemma.
What one piece of advice would you give to a new MHA graduate or young healthcare professional?
Dresdene: Teamwork is critical. Anyone who impacts patient care is a member of your team so treat them like it. There is no hierarchy, just different roles.
Are you optimistic or pessimistic about healthcare’s future?
Dresdene: I am very optimistic. I see organizations tackling hard issues, I see patients requiring a better response. I see more options being offered. Hopefully consolidations will not limit healthcare’s future.
What healthcare activities are you currently pursuing?
Dresdene: I am fulfilling speaking requests, pursue teaching opportunities, and I continue to participate in the ACHENTX Life Fellows and Retirees committee.

Phil Prosser has been involved in healthcare for more than 45 years. His executive healthcare experience spans the industry, from integrated delivery systems, to managed care organizations and postacute healthcare corporations. His expertise and insight have been honed through involvement in strategic planning and plan execution, operations, finance, payor negotiations, and marketing in both the managed care and hospital sectors.
For ten years he served in various senior management roles with the Presbyterian Healthcare System (now Texas Health Resources). Subsequent to that he was the Chief Managed Care Officer for LifeCare Hospitals, a multi-state post-acute care corporation.
Phil has a Bachelor of Science degree from Oklahoma Christian University, and a Master of Health Administration and Planning degree from Washington University in St. Louis. He has served on many boards including the Collin County Planning Board, the Mental Health Association of Collin County, and Circle Ten Scouting. He is the past chairman of the ACHENTX Life Fellows and Retirees committee.
What are the biggest changes you’ve seen over your career in healthcare?
Phil: I’ve witnessed the advancement of health care in ways that have improved our quality of life significantly. I’ve seen the growth of private equity and venture capital opportunities with the concomitant emphasis on the bottom line. I wish many of my colleagues would have had the opportunity to work in a faith-based environment where patient care is the priority. I have also seen how managed care organizations have throttled health care organizations with aggressive reimbursement schemes and intruded into the actual delivery of care under the guise of “medical management.”
What’s the best advice you received from a colleague, mentor or friend, that helped you in your career endeavors?
Phil: Bloom where you’re planted!
When did you join ACHE and why?
Phil: I joined ACHE in 1979 and progressed from Affiliate to Certification to Fellowship in relatively short order. I attribute this to the constant encouragement from my mentors, Joe Gunn and Phil Wentworth.
Why have you remained a member of ACHE? What value do you receive from your ACHE membership at this point in your career?
Phil: I see the ACHE credential as a very significant indication of my commitment to professional growth. It brings on a certain degree of credibility as I interact with other healthcare professionals and organizations.
What one piece of advice would you give to a new MHA graduate or young healthcare professional?
Phil: Maintain a degree of longevity and a progression of professional growth preferably within a reputable healthcare organization. Think carefully and seek counsel before transitioning from a current leadership role in a stable organization. Establish meaningful relationships with seasoned and respected healthcare executives. Coupled with your ACHE credential, this will strengthen your resume significantly.
Are you optimistic or pessimistic about healthcare’s future?
Phil: I want to be optimistic, however I am also uncertain which forces will prevail -those that focus on quality patient care or those that focus on the bottom line.
What healthcare activities are you currently pursuing?
Phil: I currently have a consulting practice and I am fortunate to have eight clients. I also have served as an ACHENTX mentor, chairman of the Life Fellows and Retirees committee and I currently oversee the committee’s Guest Faculty Program where we provide speakers and panelists for our regional health care administration programs on a wide array of topics.
You can achieve anything you put your mind to. The power to crush any goal is in all of us. Let’s set it free.


Dane Peterson thinks a lot about operational excellence. He continually seeks ways to drive results and performance, a product of his formative years as an engineer and two decades of experience leading hospital systems and academic health institutions. For the new Chief Operating Officer of Children’s HealthSM, operational successes in health care are not just about promoting process and efficiency. They’re also about fostering an environment for compassionate care.
Dane joined Children’s Health last August after serving as Interim Chief Executive Officer at Emory Healthcare in Atlanta. Recognizing the importance of firsthand understanding, he spent over 90 hours in his first few months shadowing care teams across ambulatory and inpatient settings, delving into the intricacies of patient care and connecting with team members systemwide. He spent an overnight shift in the Emergency Department (ED) and joined shifts in the Pediatric Intensive Care Unit (PICU) and Neonatal Intensive Care Unit (NICU) at Children’s Medical Center Dallas. He joined the ED, PICU and Perioperative teams, as well as the team at the Center for Pediatric Eating Disorders at

Children’s Medical Center Plano, among other shadowing experiences.
“You can sit there and hear anecdotal stories or look at spreadsheets and processes,” he says. “But when you’re on the hospital floor alongside the people on the front lines, that’s where you can soak in everything from a process and health care quality perspective. If you don’t do it early in your tenure,” he adds, “you lose the opportunity to learn – and to be able to add value – fast.”
Dane’s belief in the power of immersive leadership stems from his broad experiences leading successful teams at for-profit and notfor-profit academic health care systems. He spent more than 15 years at Emory Healthcare. He also served in leadership positions at Medical City Dallas Hospital and Creighton University Medical Center in Omaha, Nebraska.
Before entering the field of health care, he discovered his penchant for simplifying complex processes as a product engineer at Ford Motor Company. “What I liked was working with the folks on the floor of the plants, doing the value-added and the process-improvement work. Knowing that I was working with a team that was going to make better products for our customers – that’s what I loved.”
He sensed that operational excellence and process improvement could benefit teams in any industry or organization. Drawn to missiondriven care, he left Ford and pursued a MBA at Stanford, where he developed his strategic approach to health care leadership. “Whatever the complexity is, the less complex you can make it operationally, the better you can execute, and the higher quality and better efficiency you can have,” he says.
He views his role at Children’s Health as helping teams stay aligned to their goals as they work to deliver consistent, comprehensive care systemwide while also fulfilling the organization’s mission: to make life better for children.
“Our mission doesn’t change, but how we meet that mission can change as we get better and more efficient, and especially as we grow,” he says. “My job is to align our goals and processes to our mission across the organization, so we have the ability to implement and execute them to provide the highest-quality care possible to patients and their families across this rapidly growing region.”
Health care is a team sport, Dane notes, so alignment starts with investing in team members.
“Children’s Health is investing in recruiting and retaining the talent to care for our patients and their families,” he says. “Our leaders have worked hard and intentionally to cultivate the incredibly high employee engagement that we see across the system. When you have a well-functioning team, you can achieve anything.”
Alignment also means continuing to invest in crucial relationships such as the more than 60-year affiliation between Children’s Health and its academic partner, UT Southwestern.
Dane works closely with UT Southwestern to deepen collaboration through the Joint Pediatric Enterprise, which was created to support the
“Our mission doesn’t change, but how we meet that mission can change as we get better and more efficient, and especially as we grow.”
delivery of the highest quality pediatric care and to increase access to world-renowned faculty, biomedical research and clinical trials to children in North Texas and beyond.
“Our partnership with UT Southwestern allows us to provide absolutely unparalleled, excellent care,” he says. “We provide a great teaching environment for this generation of providers, and we support groundbreaking research that improves outcomes for the patients we serve. Not only do we have the vision for true excellence. We also have the ability to get there.”
In mission-driven pediatric health care, alignment also means putting service above self and caring for the family as well as the child, he says. He sees regular evidence of both during his many visits with Children’s Health care teams.
While visiting with a PICU team several weeks ago, he watched the team’s compassionate response to a family agitated by their child’s diagnosis. “It was a very challenging situation,” he recalls. “There is often a lot of emotion when your child is in the hospital, and even when things are going well, the emotion, concern and stress still pop up. The team lead, nurse, physician and social worker all came together as a group. They went around the circle to talk individually about how to respond, and each started with empathy around how difficult a situation this must be for the parents.
Continued on page 26
Continued from page 25

“It was incredible,” he says. “I know that happens in the adult world too, but it’s different caring for kids. It’s care that is both patient- and family-centered, provided by a team that comes together to find solutions and support parents and their children and our caregivers, that really makes an impact in the pediatric world.”
As Children’s Health continues to keep pace with the rapidly growing population it serves across North Texas, the system remains committed to ensuring that its culture is rooted in patient- and
Children’s HealthSM is the leading pediatric health care system in North Texas and has long been recognized as a leader in pediatric health. Children’s Health campuses include Children’s Medical Center Dallas, Children’s Medical Center Plano, and multiple Children’s Health Specialty Centers. With its academic partner, UT Southwestern, Children’s Medical Center Dallas is consistently ranked #1 children’s hospital in North Texas and among the nation’s best pediatric hospitals by U.S. News & World Report. Its commitment to excellence and providing outstanding care across all aspects of pediatrics has resulted in 10 out of 10 specialty programs being ranked among the best for six consecutive years, including Cancer, Cardiology & Heart Surgery, Diabetes & Endocrinology, Gastroenterology & GI Surgery, Neonatology, Nephrology, Neurology & Neurosurgery, Orthopedics, Pulmonology, and Urology.
In addition, Children’s Health nurses have received the Magnet® designation for the past 13 years, the highest honor for nursing excellence, and it has been named one of the 150 Best Places to Work in Healthcare by Becker’s Hospital Review for 10 consecutive years.
For more information and to support Children’s Health, visit Childrens.com; like Children’s Health on Facebook; follow Children’s Health on X, Instagram, Threads and LinkedIn; and subscribe to its YouTube channel.
family-centered care, its team members are heard and valued and its processes are efficient and effective, says Dane.
“It’s much easier to grow, grow, grow and allow yourself to have a successful business through growth,” he says. “It’s harder to do growth, efficiency and effectiveness together. But that is the key to success in your core operations. As much as we need to grow, we also need to remain affordable for the patients and communities we serve, and you can’t do that if you’re not efficient and effective.”
It’s a big challenge, says Dane, but one he is excited for.
“Through our collaboration with UT Southwestern, I believe we are on track to be one of the best children’s hospitals in the country, if not the world,” he says. “We have the vision, the ability, plus a fantastic team. That is our future.”
In today’s healthcare environment, different is good. We are a 100% physician-owned partnership, and we’ve been that way since day one.
Ownership creates stability.
Stability creates engaged physicians.
Engaged physicians make better decisions. Explore the difference at vituity.com/healthcare-services


Needs push us to innovate. What are the challenges your patients are facing today? What are the needs that are pressing you and/or your facility? What can you invent or what has already been invented and just needs to be harnessed? Be unafraid to innovate, change, and partner with others who are unafraid of the same. If you do, you can turn challenges into very rewarding and fulfilling successes solving ageold problems.
Embarking on the path of healthcare management has been a transformative journey for me, marked by a profound realization that needs serve as the driving force for innovation. I have navigated the intricate landscape of healthcare, particularly in the realm of telemedicine, finding inspiration in challenges, and deriving fulfillment from the relentless pursuit of inventive solutions. As I reflect on my experiences, I extend an invitation to fellow healthcare professionals to delve into their challenges, embrace innovation fearlessly, and usher in a new era of patient-centric care.
My journey unfolds in a small rural hospital in Sulphur Springs, Texas in 2013. They regularly received critical care patients that could be initially cared for by us during normal working hours, but coverage was inconsistent after hours and on weekends. The hospital was forced to transfer these patients to other facilities, often two to three hours away. This was extremely disruptive to the continuity of care for the patients as well as to the comfort and convenience of their families.
It was also a financial loss for the hospital. The hospital needed a way to provide consistent, daily critical care services for their patients thereby keeping both the care and their families local.
It was in the face of these challenges that a crucial question emerged between Dr. Christopher Gallagher and I: "What if we did something different?" Our training taught us the importance of always striving for excellence in clinical care and to think outside the box. This inquiry became the genesis of a telemedicine platform designed to seamlessly integrate virtual critical care into the hospital. Rather than waiting for others to find a solution, we decided to create the solution.
Breaking through the virtual barrier became a focal point, ensuring that telemedicine wasn't
 Dr. Chris Gallagher
Dr. Chris Gallagher
a detached experience for the patient, but a genuine extension of the medical team. We wanted to create an environment that replicated the experience of in-person, bed-side care as seamlessly as possible.

We were intentional in seeking to create a care delivery model and a culture that sought to integrate into the fabric of the local medical community to create clinical partnerships. Yes, we have a cart that can be rolled around with all the bells and whistles, but it’s also about the clinicians being consistently and readily available when needed and interacting with the on-site medical staff in a collaborative and collegial way –becoming a true extension of the medical team.
The platform has evolved tremendously since 2013, embracing technological advancements, integrating seamlessly with EMRs, and expanding to eight specialties. But all of this has occurred while aligning with our original vision of service - to reimagine the experience of virtual specialty care while creating lasting clinical partnerships.
Continuing with the theme of innovation and change, I realized early on in my career that I had a real passion for teaching the next generation of clinicians the knowledge and lore of how to care for patients. After completing my Fellowship in Pulmonary and Critical Care, I immediately got on the educational track as an assistant professor of medicine with a focus on interstitial lung disease and pulmonary hypertension.
However, as our telemedicine practice started to develop and mature, my ability to lead clinical teams on teaching rounds diminished more and more. I still had the passion, but it had to evolve. Thankfully, my role with Access TeleCare enabled me to still pursue educating others in a slightly different way, with potentially even more impact. Now, I get the privilege of guiding client hospitals and their clinical departments on how to better take care of their patients by leveraging the latest technological and care delivery design innovations. I get to enjoy the experience of implementing a new tech-enabled care delivery program that a hospital has never had before and watch it save and change lives.
Thus, in an unexpected manner, a career in business development and clinical leadership followed naturally from my career in clinical practice and education at an academic center. The joy and passion for education remains albeit in a different venue. Moving into an administrative leadership position allowed me to teach and to mentor future clinical leaders on how to model their clinical practices, to deliver clinical excellence, and to continue advancing and innovating. To do so in parallel to advising client hospitals on how to model their services for there to be a seamless integration of their services with ours all the while ensuring that they are getting a return on their investment with us, provides me with a lot of professional satisfaction and fulfills my desire to educate others. I think the day I stop being able to teach others is the day you’ll see me sign off and start traveling the world!
I’m continually motivated by the changes I can see occurring in the communities that we serve. As we introduce tech-enabled care, it elevates hospitals’ ability to provide access to high-quality
specialty providers who are delivering timely clinical care grounded in excellence. It is truly special to watch a community get revitalized because of their ability to provide this kind of care to their families, allowing us to help them keep care local and mitigate the disruptive forces of transfers.
As the healthcare landscape continues to evolve, the call to innovate becomes more imperative than ever. By reflecting on challenges, embracing change, and fostering collaboration, we can collectively pave the way for future innovations.
I’ve found my path, I’ve enjoyed the ride, and I look forward to what the future holds. I’ll leave where I started. "Needs always push us to innovate." This mantra becomes a rallying cry, urging healthcare professionals to reflect on their current challenges and needs. I extend an invitation to explore inventive solutions and embrace change fearlessly. In doing so, healthcare leaders can usher in a new era of healthcare delivery, addressing age-old problems and ensuring a more resilient, patient-friendly future.

Pritam Ghosh, MD is board-certified in internal, pulmonary, and critical care medicine. He completed a fellowship in adult pulmonary and critical care at The University of Texas Southwestern Medical Center in Dallas and currently serves as part-time volunteer faculty supervising residents and fellows. He serves as the Chief Medical Officer & Medical Group President for Access TeleCare.



September 19, 2023
Guest speaker: Patrick Brown, FACHE – Senior Vice President, Surgery Partners
The Fall Networking Blitz kicked off with a fun ice breaker involving Starburst. Based on the Sstarburst color chosen at check in, each person stood up and answered a simple ice breaker question like have you worked in another industry other than healthcare? Is this your first ACHE event? Is your commute to work an hour?
These various questions allowed all 50 plus attendees an opportunity to introduce themselves. Afterwards, Dr. J Alexander encouraged all attendees to network and make LinkedIn connections with at least two other attendees. This allowed attendees to engage in casual conversations with someone new and put into practice networking.
While eating the dinner provided, John Whittemore provided an overview of the ACHE North Texas chapter committees and how to get involved. He also emphasized the importance of networking at events, meeting new people, and asking for input and opinions that may lead to strong professional connections.
Lastly, Patrick Brown, the keynote speaker for the night, concluded this event with an overview of his career journey and his networking advice. Patrick’s healthcare career began in human resources and over the years he’s held leadership roles in supply chain management, strategy, and operations. While

his roles changed and his scope of work provided new challenges, he mentioned the importance of learning and staying curious because “Curiosity becomes experience.” The new opportunities and projects offered to him throughout his career led him to learn and grow professionally while gaining valuable experiences.
Beyond his work experiences and career journey, Patrick highlighted the importance of relationships. He reflected that he wants his impact to be known for how he made people feel. This is a reminder that “People will forget what you said, people will forget what you did, but people will never forget how you made them feel.” – Maya Angelou.
Patrick also discussed the impact ACHE has had on his career and the importance of networking at events. When thinking about networking, he offered the following advice:
• Be intentional in how you cultivate your network.
• Ask how you can provide value and help the person with whom you are trying to develop a professional relationship.
• Attend ACHE events because this helps organically grow your network and professional connections.
• Always be open to learn in your personal and professional lives.
The Fall Networking Blitz provided a fun, informal, and engaging opportunity for new and current ACHE members to build professional relationships with individuals across many organizations. Lessons learned were to be curious, adaptable, and be intentional by adding value to the relationships formed along one’s career journey.
Thank you to Medical City Heart & Spine for hosting this event and thank you to the ACHE leaders and speakers for facilitating a fantastic networking event for all attendees.




September 20, 2023
Methodist Dallas Medical Center
• Tirzah Brown, MPA, Director of Programs, Unbound Now North
• Sheyla Camacho, Public Health Educator, Victim Intervention Program (VIP)/Rape Crisis Center, Parkland Health
• Carrie Shiratom RN,MSN,FNP-C,ACNP-C, Co-Founder, Reclaim611
• Andrew Smith, FACHE, (Moderator) Strategy Leader for the Scheduling Customer Journey, Baylor Scott & White Health
The closing panel began with a powerful and vulnerable story from Whitney, a survivor of human trafficking. Her story set the tone for this educational and important topic.
The panelists defined what is human trafficking and provided information on the differences between adult sex trafficking, child trafficking, and labor trafficking. Adult sex trafficking is the purchase, transportation, and seeking of a person’s body for something of value (e.g., drugs, clothes, housing, etc.). Additionally, there has to be proof of force, fraud or coercion. Child trafficking is a form of child abuse involving a person under 18 years of age. In child
trafficking, there is an exchange of value like in adult sex tracking but with child trafficking, there does not need to be proof of force, fraud or coercion. Labor trafficking involves involuntary service through the use of force, fraud, or coercion.
Some may think their community may not experience human trafficking. However, the panelists emphasized we all have vulnerabilities because we are all human. There are some individuals that may be more at risk due to higher vulnerabilities such as homelessness, personal or parental drug addiction, lack of community, broken families, low self-esteem, or parents working at night. “Trauma doesn’t discriminate.”
Knowing the signs of human trafficking is important in healthcare. In a healthcare setting, there are opportunities to serve a victim due to the fact that the majority of victims see a healthcare provider. As Carrie stated, “Once you’re educated, you’ll see it.” Additionally, it’s essential for healthcare systems to have a protocol response when human trafficking is suspected. Suggested best practices for training and education included the following:
• Provide official education to staff and providers.
• Utilize resources from human trafficking organizations.
• Use universal screening questions for all patients.
• Create badge cards so staff know who to page.
• Trust your gut.
If a human trafficking is suspected or identified, having a protocol response helps protect the victim. The panelists did note that healthcare settings and providers are not there to save. Partnering with victim service agencies, task forces, and law enforcement agencies who have received trauma informed training can help serve potential victims. Encountering someone involved in human trafficking is a complicated and potentially dangerous situation. Therefore, having the appropriate education, training, and resources helps provide safety for all involved.
The panelists mentioned there are national resources such as the National Center of Missing & Exploited Children that provide education and services, in addition to local agencies like Traffic911, Unbound Now, and Reclaim611. There is no simple solution to preventing human trafficking, but as Whitney reminded us all, “Be compassionate and nonjudgmental.” Victims of human trafficking are humans regardless of their current situation. Healthcare organizations can help by knowing the signs, providing appropriate responses to the situation, and directing victims to appropriate resources in their community.




















On Tuesday, October 23, 2023, ACHE of North Texas gathered for one of the most coveted events of the year. The event, titled “Paving the Way from Clinician to Healthcare Executive,” took place in Fort Worth at The PalmWood.
Against the backdrop of breathtaking views of a western sunset, combined with spectacular food and beverages, the cozy crowd of new and seasoned members were able to network among each other before they witnessed the panelists engaged in insightful discussions about the unique challenges clinicians face when transitioning into executive roles.
Daniel L. Beckles, MD, PhD, FACS, FACC, FCCP, shared his journey from Cardiothoracic Surgeon to Adjunct Clinical Professor, emphasizing how his combined expertise in clinical practice and academia laid a strong foundation for executive leadership. Dr. Beckles’ remarks were his reflections on the evolving landscape of healthcare administration.
Dr. Noreen Butte, a pediatrician and trailblazer in Healthcare Informatics and Biopharmaceuticals, spoke passionately about her transition into executive roles driven by a desire to leverage technology for improved patient care. Dr. Butte’s insights highlighted the importance of innovation in shaping the future of healthcare leadership.
Stephanie Copeland, MD, MBA, CPHQ, FAAP, CPXP, shared her journey from clinical practice to Regional Medical Director, emphasizing the significance of additional qualifications and

certifications in driving organizational change. Dr. Copeland’s remarks enhanced the discussion by lending tips for effective strategies for clinician-executives.
Dr. John Marcucci, SVP Chief Medical Officer, discussed how his background as a clinician informed his approach to executive leadership reminding attendees about the importance of patient-centered care and organizational improvement.
Dr. Rob Nelson, VP & Head of Healthcare Transformation & Innovation, expertly moderated the discussion, guiding the panelists through thoughtful conversations.
Overall, the Cocktails with the Chiefs event at The PalmWood provided a perfect setting for exploring the complexities of transitioning from clinical practice to healthcare leadership, with the spectacular food and scenic views adding an extra dimension to the insightful discussions.

October 13, 2023
Sheraton Arlington Hotel
The positive energy was palpable as the room filled for the annual ACHENTX Women’s Breakfast. From students to seasoned professionals, the theme, Paving the Way to Personal Growth & Success, provided a platform for the three panelists to share experiences, advice and perspective. Moderated by Winjie Miao, SEVP & COO, Texas Health Resources, the panel of three included Karen “KJ” Johnson, Executive Director, Dress for Success, Traci Shortt, VP & Group Operations Officer, SCP Health and Becky Tucker, System SVP, Channel Integration, Texas Health Resources.
The discussion began with the question, “How do you define success?”. This looks different for each person, but common themes included seeing transformation in others and making a lasting impact. The panelists shared contributors to their success, which include support from family, friends, mentors and colleagues, being authentic and blocking time for learning and growth.
Panelists shared some advice, including:
• Be curious – align with your passion.
• The importance of learning boundaries. You can say “no” without an explanation – if you never say “no,” you delete the power of your “yes.”

• Have the courage to make tough decisions.
• Know that you deserve a seat at the table –and take it.
The conversation moved to goals not yet achieved:
• Losing weight (KJ)
• Saying “no” and being OK with it (Tracy)
• Work-life harmony vs work-life balance (Becky)
Secrets to staying motivated include staying focused on your passion, surrounding yourself with people that give back to you and making a difference. Becky also emphasized that it’s important to be generous with your appreciation.
An attendee asked, “Looking back on your career, was there a failure that helped you succeed?”
• It’s OK if you don’t get the job – something else is better aligned. (Becky)
• Just keep going. I know my worth. Make them tell you “no.” (Tracy)
• I was laid off – it was the trajectory to get me where I am today. Ask yourself – “Am I truly operating in my gifts?” Stay with it. Apply anyway. (KJ)

The time flew by and at the end of the discussion, Deepthi Michael, chair, Women’s Healthcare Executive Network, thanked the panelists and noted that donations were made in their honor to the ACHE North Texas Leadership Legacy Fund. She also announced that Tanya Stinson, Founder, Leaning Towards Change, is the incoming chair.











Junior League of Fort Worth Diaper Bank
Accepted by: Danielle Dollahite and Jennifer Hurd
Pictured with Senior Leader of the Year Award recipient Pamela Stoyanoff, MBA, CPA, FACHE
Exiting Board Members
Dustin Anthamatten, MBA, MA, CPA, FACHE
Fraser Hay, FACHE
Trinette K. Pierre, DHA, RN, NEA-BC, FACHE
Benton Sprayberry, FACHE
Exiting President
Felixia Colón, FACHE



Trinette K. Pierre DHA, RN, NEA-BC, FACHE ACHE National Award
Recipient





Seetha Modi 2023 Emerging Leader
Regent’s Award
Dr. Richard Greenhill 2023 Change Ambassador
Regent’s Award
Pat Driscoll 2023 Legacy Leader
Regent’s Award
Crystal Brown 2023 Executive Servant Leader
Regent’s Award
Tanya Stinson 2023 NTX Chapter Connector
Regent’s Award
Lenetra King 2023 Leadership Leverage


Charlene Kesee, DBA, FACHE
James R. Allard, DNP, RN, NEA-BC, FACHE
David T. Berry, FACHE





Nov. 3, 2023
Scottish Rite for Children Orthopedic and Sports Medicine Center
Scottish Rite for Children Orthopedic and Sports Medicine Center in Frisco hosted ACHENTX’s 4th Quarter Education Event on Thursday, Nov. 3. Attendees heard from two panels of experts, one focused on the “State of Healthcare: Industry Leaders’ Perspectives,” and the other addressing “Crisis Management: Strategies to Effectively Manage a Healthcare Organization.” Highly informative and interactive, attendees gained new knowledge and insight on these two timely topics.
on reimbursement, increasing pressure of supply and labor costs which could be a catalyst for innovation, and the entrance of private equity firms interested in investing in the most profitable areas. Bryant explained that COVID put a spotlight on the critical importance of the supply chain. She went on to share how she and her team work daily to get product into the hospitals and clinics to support patient care. She said her department is still dealing with a “substitute for the substitute for the substitute.” She also pointed out cybersecurity as a big concern. Hay said he expects a continued push for value for cost with a transition to value-based relationships. A key question he asked was “How do we reduce cost and not take away access?”
• W. Stephen Love (Moderator), President & CEO, Dallas-Fort Worth Hospital Council
• Aaron Bujnowski, FACHE, Managing Director, Health Industry Group/Health Systems Practice, Alvarez & Marsal Holdings, -
• Fraser Hay, FACHE, President, Texas Health Presbyterian Hospital Plano
• Pamela Bryant, SVP/Chief Supply Chain Officer, Parkland Health
Love asked the panelists to address the biggest issues facing their areas of expertise. Bujnowski listed disruption caused by new, non-traditional competitors, downward pressure
In terms of the future of mergers and acquisitions, Bujnowski sees in the short-term continued consolidation among those entities who are struggling. In the long-term, because of the pressure on pricing and the need to find additional revenue, organizations will have to take bold, decisive action, asking tough questions and perhaps shedding assets they no longer need to sustain their current and future business. Vertical integration will gain momentum with new entrants looking for the best care in the most effective way to claim more of the premium dollar.
Love asked Bryant what Parkland had done to reach out to the communities it serves. She listed many accomplishments including the new hospital and developing world-class maternal care and burn centers. “We’ve built lots of community clinics to provide access closer to home as we strive to reduce some ER visits. We really focus on building relationships with our
communities. From a supply chain perspective, as we look at our zips, for those who have food deserts, we make sure we work with our partners to provide farm stands to get those we serve fresh fruits and vegetables.”
Love asked Hay about technology’s impact on the patient experience. He called what’s being developed fantastic and unnerving. Will the technology add value? Is it going to improve processes that will improve the care we provide to patients? These are key questions that need to be answered when considering investing in new technology.
Wrapping up the session, Bujnowski said providers must reimagine care delivery to provide the highest outcomes at the lowest per unit cost. That will require next level thinking. Bryant noted Parkland has begun the journey to become a High Reliability Organization (zero defects). Morning huddles now include a daily safety story to reinforce the importance of safety. Hay highlighted Texas Health Connect, an initiative aimed at developing a navigational platform to help guide patients through their healthcare journey with the organization. If you receive care at any Texas Health facility, he said, it should be the same standard of care and experience you would receive at any other Texas Health facility.
• Christi Nguyen, FACHE (Moderator), Associate Chief Nursing Officer of Nursing Excellence, UT Southwestern Medical Center
• Lance Lynch, Consultant, Adaptiv Consulting Solutions
• Hollis Mignogno, Vice President
• Rob Monaghan, System Director, Business Continuity and Emergency Management, Baylor Scott & White Health
A common thread ran through this panel’s remarks – COVID-19. The panel addressed how a wide range of unplanned crisis situations – the pandemic, natural disasters, labor actions including strikes, can take a toll on the entire team adding physical, emotional, and psychological stress for employees, patients, and the communities served. As healthcare leaders, it’s important to understand and plan for needs in terms of crisis management in these situations. Knowing who to contact in your organization in case of emergencies is critical.
Nguyen asks each panelist to define crisis management and challenges they have faced. Lynch said resilience, incidence management, crisis management terms are used interchangeably. It starts when something becomes big enough to threaten your brand’s integrity and reputation such as delayed care, cybersecurity attacks, etc. Monaghan added it was anything that impacts an organization’s ability to provide care. Mignogno presented from the supplier’s point of view. Think about all economic and social challenges – mental health, shortages of products and people, how to deal with labor actions, etc. What is the impact you’re seeing within the organization, what do you need to think through, and how can you mitigate the situation?
All panel members addressed the critical importance of communications during a crisis. This includes internal communications – keeping employees, physicians, and
Continued on page 48
Fourth Quarter Educational Event Continued volunteers informed about what’s going on, as well as external communications to the public including current and future patients. The RAC (Regional Advisory Council) is the point at which information dissemination, collaboration, and communication occurs among all healthcare organizations in the area. The RAC also collects data, provides information, and can set up emergency care units if needed. Panelists agreed the Teams app provides an excellent automated communications platform for internal audiences. All panelists said their communications and PR teams are critical components of their crisis management teams. Collaboration to develop a scenario playbook is very helpful. Planning is important, but it is important not to get bogged down in anticipating every possible scenario. Annual training and exercises with mock scenarios is important. The panel listed these key takeaways for session attendees:
• Proactive Activation: Act swiftly in a crisis; delay can be costly. It’s wiser to activate early and adjust as needed, rather than trying to catch up once you’re behind.
• Plan, Organize, Orient, Equip, Test, and Evaluate: This systematic approach lays the groundwork for effective crisis management, regardless of the nature of the threat.
• Strategic Networking: Forge connections with community partners such as local, state, federal agencies, and Regional Advisory Councils well before a crisis hits. This ensures they recognize your organization when you reach out during an event.
• Get Involved with Your EM Teams: Executive Leadership isn’t only an explicit accreditation requirement but is associated with successful programs. Get involved

with internal training and exercises, to their regular meetings to learn about current threats and mitigation, etc.
• Invite EM Leaders to the Table: This ensures that organizational resilience planning is considered within every layer of the organization.
• Support Your EM Teams’ Needs: Their goal is to drive effective organizational resilience for the operation. Eliminating barriers to their success is key.
• Use Your Plans: When a crisis happens,don’t forget to pull out your plans and use them. They were built/vetted for a reason.
• Know Your Supply Chain: Who are your customers, who are your suppliers, who are your vendors.what are their plans, where do they operate, etc.?
• Keep Your Plan Simple: Focus on what really happened. Try not to plan for every issue that could occur. Planning for loss of facility, loss of power, loss of workforce, disruption in the supply chain, and disruption in technology is critical.

Your path is unique, and so is our support.
Grow, learn and evolve with CHRISTUS Health, where your career is nurtured every step of the way. Find your unique career path at CHRISTUScareers.org
Thursday, October 26, 2023
Irving Convention Center at Las Colinas
If you attended the ACHE of North Texas Summit and Convocation in October, you likely noticed the new format. That was no accident. Incoming President Aaron Bujnowski, FACHE, Managing Director, Alvarez and Marsal wanted to make the meeting more than the installation of new officers, he wanted the meeting to have impact and relevance for members and ample opportunity to make new connections and deepen existing ones.
By the most important measure, the event was a rousing success: people stayed until the end.
“This year, we saw the energy in the room around healthy leadership, that was relevant to people,” Bujnowski said.
To get people more engaged, Bujnowski said, “We got rid of the chairs and had people standing at high top tables. It encouraged them to move around and connect with more people between the different presentations.”
And they were different. Instead of a panel discussion, there were three Ted-like Talks delivered by handpicked and engaging speakers. Each of the talks focused on a different topic that North Texas health leaders could use to improve their own leadership skills. Instead of grouping them all together, they were spread out to give members ample time for networking.
“Everyone loves a good Ted-like Talk,” Bujnowski said. “They’re pithy, they keep people’s attention, and they spark ideas and conversation.”

The speakers were Lenetra King, FACHE, founder of Watch Me EXCEL, Lee Colan and Julie Davis. Bujnowski said they were selected because each could share practical, useable insights for leaders looking to improve.
In addition to ditching the chairs, food stations were interspersed throughout to create movement.
“We really wanted to create an environment where people could feel comfortable talking to people they didn’t know, people from different organizations,” he said. “That environment of connection was very dynamic.”
All good leaders build upon those who came before. Last year’s convocation was led by Immediate Past President Felixia Colón, FACHE, Sr. Vice President & Group Operations Officer, SCP Health, who brought equity and inclusiveness as a theme to her term.
“I appreciate Aaron for saying let’s do this differently,” Colón said. “It also highlights how important it is to have a succession plan that puts in people who are motivated to see the chapter move forward and has nothing to do with maintaining the same old way.”
Colón credits her predecessor as president, Dustin Anthamatten, FACHE, VP, Operations, Corporate Methodist Health, with really bringing new ways of approaching events.
“It really started changing with Dustin,” Colón said. “Dustin was always very visible as a leader,” she said. “He was always, always doing stuff. He always showed up and you know, we just have kind of taken on his same approach.”
As if riffing from the presenters, Colón said good leaders need to be comfortable with change and they need to be ready to consider equity and inclusion in the decisions they make and the way they lead.
“You’ve got to be comfortable with change, and then you can just block chain change on top of that, and then block chain again,” she added.
Both Bujnowski and Colón have challenged President-Elect Ajith Pai, PharmD, FACHE, President of Texas Health Southwest to continue innovating to keep members engaged and to help continue their journeys to improve as healthcare leaders.
“Of course, I accept that challenge and I’m looking forward to building on their great tenures as leaders. We are blessed to have such an active chapter and so many dedicated members. I learned so much from Felixia, and I’m enjoying working with Aaron to promote his agenda as president,” said Pai. “I’m committed to continuing their efforts around impact, relevance and connectivity.”
See Award Recipient photos starting on page 40











November 10, 2023
Toyota Stadium
The session commenced with a warm welcome from Immediate Past President Felixia Colón, who joyfully announced our chapter’s prestigious achievement—the 2023 Regent-at-Large Award for Accomplishments in Diversity. And, Colón proudly shared that we are the second largest chapter in the country. We’re coming for you, New York City chapter!
Passing the torch to President Aaron Bujnowski, the day unfolded with engaging introductions and a glimpse into the agenda. A delightful array of fun facts about board members emerged, revealing a diverse tapestry that includes a Texas Peace Officer, distiller, sailor, collegiate athlete, and two musicians.
Bujnowski guided us through the current chapter landscape, highlighting unprecedented success with a record number of platinum sponsors, paving the way for robust financial reserves. With a thriving membership of 1820, the chapter boasts unprecedented diversity, growth, and engagement. The leadership team stands as a powerful and diverse force, steering the ship with unwavering commitment. Strong programs and committees underscore the chapter’s vibrancy.
In a strategic discourse on charting the course for 2024, Bujnowski posed a compelling question: What’s the next step when everything is going well? The resounding answer: accelerate! Energized by this vision, the committees delved
into breakout sessions, setting the stage for an invigorating discussion about the path ahead.
As the meeting concluded, each committee provided a glimpse into their plans for 2024. One of the most exciting ideas is an ACHE North Texas Mini-Congress! We’re excited to accelerate into 2024!







In the early hours of Tuesday, November 14, 2023, the healthcare landscape resonated with purpose as 30 esteemed healthcare leaders from across the Metroplex converged at Cook Children’s Medical Center Prosper to meet their Vice President and Administrator, Kevin Greene. The occasion, aptly named ‘Breakfast with the President,’ unfolded between 7:30 am and 9:00 am, leaving an indelible mark on those who attended.
The event commenced with a shared meal, a symphony of flavors featuring Chick-fil-A chicken biscuit sandwiches, hashbrowns, and a selection of invigorating juices and coffee. Amidst this culinary backdrop, Greene, a native of Ft. Worth and a luminary in the healthcare arena, engaged in candid conversations with the attendees, fostering a sense of camaraderie.
Kiante Blakely, MHA, Project Manager for Children’s Health System, orchestrated the proceedings, extending gratitude to sponsors and committee members. With finesse, Blakely introducedGreene, who embarked on a reflective journey through his healthcare career.
Born at Texas Health Harris Hospital, Greene’s trajectory began as an intern, inspired by his mother, a Labor and Delivery nurse. From his early days as an IT Project Coordinator to his current role, Greene emphasized Cook’s unwavering commitment to investing in its people. A Trinity University graduate with a Master of Healthcare Administration degree,

Greene recounted his tenure in Austin with CHS before returning to the Cook Children’s Health System fold.
Greene’s narrative took a poignant turn as he shared a personal connection to Cook’s – both of his children are patients there. A heartfelt account of his son’s medical journey underscored the evolving service lines at Cook Children’s.
The audience was then treated to a visual journey through Cook Children’s Health System via a compelling video, encapsulating a century-long commitment to “The Promise.” This promise, Greene explained, revolves around providing exceptional care to sick and injured children, a legacy upheld for the past 100 years and projected into the future.
Acknowledging the Prosper campus team, Greene introduced the Chief Nurse Executive and Dr. Aanani. The floor was opened to questions, fostering an interactive dialogue.
Post-event, attendees were offered a tour of the state-of-the-art facility, a testament to Cook’s dedication to patient-centric care. The facility, just over a year old, boasts a captivating live LED-lit mural at the main entry, reflecting the seasons and hospital events. The design, with floors resembling a baseball, invites children of all ages into the hospital, while whimsical ceiling decor adds a touch of artistry. Technological innovations enhance the patient experience, with spacious rooms equipped for telehealth and seamless communication between providers and facilities.
In essence, ‘Breakfast with the President’ transcended a mere networking event; it was a journey through the past, present, and future of healthcare at Cook Children’s Medical Center Prosper – a beacon of hope, innovation, and unwavering commitment to “The Promise.”








November 16, 2023
SpinSci Technologies LLC






November 16, 2023
Moderator: Jonathan Sell
Founder and CEO, Innovative Solutions Management
Panelists:
• Serena Bumpus DNP, RN, NEA-BC Chief Executive Officer, Texas Nurses Association
• Dr. William Hooks, MD, MBA Chief of Anesthesiology/Medical Director, Perioperative & Procedural Services, Titus Regional Medical Center
• Kenneth Hutchenrider, Jr., FACHE President, Methodist Richardson Medical Center
The session commenced with moderator
Jonathan Sell initiating a discussion on crisis definition, prompting panelists to offer diverse perspectives. Scenarios like weather events, pandemics, labor strikes, mass casualties, power outages, and civil disturbances were explored. Serena Bumpus, DNP, RN, NEA-BC, emphasized, “Our patients are our greatest responsibility.” And she went on to explain that in a true crisis, “we have to make decisions that challenge our morals and ethics.”
The ensuing dialogue focused on proactive measures for unforeseen circumstances, emphasizing communication, supplies, staff, and security.
The importance of comprehensive communication plans, both formal and informal, encompassing internal and external stakeholders, was underscored. William Hooks, MD, MBA, advocated for clarity around incomplete information and honesty about the fluidity of the situation.
Innovative procurement and managing organizational resources, such as medical supplies and staff is a must. Ken Hutchenrider, Jr., FACHE shared a story from an ice storm where he and another executive shoveled snow when their engineering department couldn’t get to the facility. He said, “In a time of crisis, title doesn’t matter.” The person that needs to do the job is the person that is most able regardless of title.
Dr. Hooks elaborated on investments in security personnel and technology, as well as conflict resolution training. Workplace violence mitigation, involving risk assessment and implementation of measures like metal detectors, zero-tolerance policies, and reporting mechanisms, was addressed.
The panelists then discussed continuous improvement of emergency preparedness plans
through regular evaluations and drills. They highlighted the importance of regional advisory councils and state-level communication, emphasizing mental health support for teams pre and post-crisis.
In concluding remarks, leadership insights were shared. Hutchenrider advised maintaining calm and transparency, Bumpus advocated for postcrisis vulnerability, Hooks emphasized humility and seeking help from fellow leaders, and Sell stressed the importance of decisiveness in crisis leadership.

 Mihir Patel, MD Regional Chief Medical Officer
Mihir Patel, MD Regional Chief Medical Officer
November 30, 2023
Moderator: Aaron Bujnowski, FACHE, Director and Integrated Delivery Network
Segment Lead, Alvarez & Marsal
Panelists:
• Brad Prugh, Chief Executive Officer, Care Continuity
• Leslie Wainwright, PhD, Chief Funding and Innovation Officer, Parkland Center for Clinical Innovation
• Stormee Williams, MD, MBA, Vice President & Chief Health Equity Officer, Children’s Health System
a greater number of unknowns in higher reward risks. Know your leadership team and what they have the tolerance for when deciding the level of disruptive innovation. Fast fail and learn fast to refine strategy were common themes throughout the conversation of growth and innovation.
Pediatrician Dr. Williams reminded us that the innovations actually have to work clinically! Test them out before getting excited and rolling them out to the clinical team. She also encouraged people to be open to putting in the effort to learn about new technology that may help patients. Just say yes to learning and trying!
Examples of disruptive innovations that panelists shared success around:
• Use of telemedicine (specialty visits and school-based)
• Remote patient monitoring
Disruptive innovation leverages technology to help focus on making products and services more accessible and affordable. Disruptive innovations have the potential to decrease costs while improving both the quality and accessibility of care. “Disruptive Innovation in Healthcare Delivery” was moderated by Aaron Bujnowski, FACHE and the impressive panel was composed of Brad Prugh, Dr. Leslie Wainwright, and Dr. Stormee Williams.
To set the organization up for successful innovation, it should be a high reliability organization with strong leadership and culture. The organization must be willing to take an appropriate level of risk to achieve an appropriate level of award. Safer bets are likely going to be smaller and more incremental changes. There are
• Hospital at home
• Advanced data analytics
Panelists also discussed financial and reimbursement challenges with some of these innovations. Figuring out how to make these innovative care models financially viable will be key in their sustainability.
In closing, disruptive innovation in healthcare, exemplified by technologies like telemedicine and remote patient monitoring, holds promise for enhancing accessibility and affordability. However, to ensure success, organizations must foster a culture of high reliability, embrace calculated risks, and navigate financial challenges for sustainable implementation, as emphasized by this insightful panel.
November 30, 2023
Moderator: Paula Turicchi, FACHE, Chief Strategy Officer, Parkland Community Health Plan
Panelists:
• Monica Anderson, MS, CPXP, Valued Base Consultant, Customer Experience Leader, Baylor Scott and White Health TexasEast Region
• Aaron Davis, MSHA, FACHE, CPXP, Vice President & Chief Experience Officer, UMC Health System
• Brandi Jaco, Director of Patient Experience, CHRISTUS Trinity Clinic
“Reinventing Customer Service in Healthcare: Lessons Learned from the Best” kicked off with Moderator Paula Turicchi, FACHE asking what consumers want from a healthcare organization. Monica Anderson, MS, CPXP, Aaron Davis, MSHA, FACHE, CPXP, and Brandi Jaco shared that patients expect excellent clinical care, accessibility, affordability, and convenience. Patients also want to feel heard. We have listening opportunities during scheduling, during actual care, and through post-care surveys. They also want compassionate care and empathy through every step of the journey.
Panelists went on to share that providing compassion and empathy is free! Every healthcare organization can do it. And, patient compliance and outcomes improve when they
feel that healthcare providers truly care.
Multiple tools were discussed that can aid in improving patient experience including:
• Technology (online scheduling, visible wait times, online check-in, virtual visits, data capture, simulation labs)
• Reducing friction points
• Caring and positive language and communications
• Learning and managing expectations
• Rounding by non-clinicians
• Capturing non-clinical information for engagement and connection
• Training and recognition for clinical and nonclinical staff
• Surveys during and after care
• Post-discharge nurse calls
• Service recovery
In conclusion, “Reinventing Customer Service in Healthcare: Lessons Learned from the Best” delivered a comprehensive exploration of patient expectations and strategies to enhance healthcare experiences. The panelists illuminated that patients seek not only fundamental aspects like excellent clinical care, accessibility, affordability, and convenience but also the intangible yet crucial elements of feeling heard, valued, and understood throughout their healthcare journey. Ultimately, the discussion offered actionable insights to inspire positive transformations in the delivery of healthcare services, emphasizing the profound impact of empathy and strategic tools in shaping a patientcentric future.
December 7, 2023
This year’s annual holiday event took place at BowlGames in Dallas, TX. Attendees enjoyed an evening of networking, dinner, games such as darts, cornhole, and football, and an ugly sweater contest.





December 8, 2023




January 30, 2024
Texas Health Allen Hospital
Speaker: Amanda Thrash
In a recent gathering of the ACHE North Texas Chapter at Texas Health Allen Hospital, healthcare professionals convened for an enlightening session titled “Breakfast with the President.” Laura Parsons-Yanez, emceeing the event, extended her gratitude to sponsors, recognizing Texas Health Allen for hosting the gathering. After introducing new attendees, fellows, and board members, Laura set the stage for the featured speaker, Amanda Thrash, FACHE, the President of Texas Health Allen.
Amanda Thrash assumed her role as the hospital’s president in July 2022, overseeing daily operations and steering the 88-bed facility’s annual operating plan. Her extensive journey within the Texas Health system, starting as an administrative resident in 2009, reflects a deep commitment to healthcare leadership. Amanda’s accomplishments include significant contributions to market strategy, physician relationships, and operational efficiency improvements.
Sharing insights from her career, Amanda highlighted her success in enhancing EMS traffic, optimizing perioperative processes, and expanding cardiovascular and robotic service lines. Beyond her professional achievements, Amanda offered a glimpse into her personal life, emphasizing the importance of family, football, and hospitality.
With a Master of Healthcare Administration from Trinity University, Amanda traced her career
trajectory through various Texas Health facilities, emphasizing the role of faith and e organization’s “Promise.” She unveiled a map illustrating the extensive service areas covered by Texas Health Allen, which opened in 2000 and underwent a $70 million expansion in 2020.
Looking forward, Amanda outlined her vision for the hospital’s growth, aiming for 150 beds and an on-campus Ambulatory Surgical Center (ASC). She highlighted the current array of service lines at Texas Health Allen and delved into anticipated healthcare trends. Notably, she emphasized an expansionist mindset, catering to educated patient-consumers, a shift to outpatient services, and strategic workforce planning for the DFW area.
Amanda concluded her talk with valuable advice, urging professionals to take a seat at the table, embrace authenticity, learn from mistakes, seek mentors, and actively engage with industry associations like ACHENTX. Her words resonated as guidance for aspiring healthcare leaders navigating an ever-evolving landscape. The event provided a unique opportunity for ACHE North Texas Chapter members to glean insights from a seasoned professional dedicated to shaping the future of healthcare in the region.

Many other ACHENTX Events are in the works. Please monitor achentx.org/events or the weekly announcements for more details to be announced soon.
Date Event
Friday, March 22, 2024
March 25-28, 2024
Tuesday, April 2, 2024
Tuesday, April 16, 2024
Saturday, April 20, 2024
Thursday, April 25, 2024
May 9-10, 2024
July 8-19, 2024
Community Event: Ft Worth Botanic Garden
ACHE Congress
After Hours Event: Maple Branch Brewery
"Physicians in Healthcare Leaders (A Physicians Only Event)"
Lean Six Sigma Yellow Belt Certification Course
"Q2 In Person Education Event
Panel 1: Sustainable Strategies to Support Well Being for Healthcare Professionals
Panel 2: Financial Sustainability of Healthcare Organizations: A Plan of Action"
Two-Day Multi-Chapter Education & Networking Event
Lean Six Sigma Green Belt Certification Course
Jay D. Barnett
Andrew Born
Ingrid bowling, MS, CCC-SLP
Nadeem Chauhan, MBBS, MHA
Rehan Dharani
Mandida K. Dzikiti
Keesha Eguia, BSN
Julia Esparza
Robert R. Feldbauer, DBA, FACHE
Anessa D. Flores
Emma Foreman, MHA
Andrew Galpin, MBA
Tyson Garfield, DO
Viji George, DNP
Bonnie Hess
Saliyat Hussain, MHA
Sara Ibrahim
Nadia Khan
Maria Kuhn
Jennifer Ledbetter, MSN
Gustavo Lopez
John A. Majors
Peyton Marshall
Patrick J. McKeon, MS
Marilyn L. Moore, BS
Varatharaj Mounasamy, MD, MBA
Gabriel J. Okpagu, MD, MBA
Dane C. Peterson
Gary B. Pillans, MHA
Dajah Ponder
Reenie S. Regi
Teauna D. Rembert
Alyssa Riley
Paris L. Robinson
Allison Roden, MBA, MSN, RN
Laura Stapleton
Brady Taylor
Betsy Thomas, BS
Katherine Trungale, MBA
Manuel Villarreal Garcia, MD, MBA, MS
Dejia Vitatoe
DeVontae Warren, EdD
Amy L. Weaver, MHA
Ashley Whitlatch, DNP, MBA
Shawn Williams
Stephanie Abrams, DO
Ayesha Bashir
Cherish Burford
Rahel Charikar, BDS, MHA
Christine Chasse, JD, RN
Karen I. Chavez
Lara Cline
Kelsey Craig
Yadira Curtiss, BS, MHA
Lydia Danton
Chaz B. England, MS
Adrienne Frazior, JD
Aaron Fuller
Anjila N. Gautam
Denise M. Gomez
Nakeea Hill
Whitney Holloway
Nancy M. Houston
Stephanie U. Ikediobi
Sabrina Johnson
Sudhakar Karlapudi, MBBS
Lexi Kennedy
Naveed Khan, PharmD, MHA
Ryan Kivett
Daniel J. Lempa, BSc
Joseph I. Lemus
Kailey Marshall
Yaziri Y. Orrostieta
Elizabeth Ortiz
Kelcey Parks
Joshua Pierce
Leigh Ann Ray
Ashley Ridgeway-Washington, JD
Jalyn A. Smith
Lisa Smith
Lisa K. Smith, MSN
Gloria A. Spiritas
Melissa A. Stewart, APRN, NP
Sneha Sutaria
Daphne Tam
Sandra Torres, MBA
Alani Torres
Anna A. Tran
Misti M. Varnell, MSN, RN
Jan Vicary
Kimberly N. Walker, RN, BSN
Rhonda Y. Williams
Manisha R. Youngblood
Stephen Angelette, JD
Beau Benson
Nithu Bharthepudy
Zach Bush
Jay M. Crutchfield, MD
Ododo Enabulele
Elkan Gbadebo
Laura Gonzalez
Sheila J. Guinn
Jennifer Hattaway
Muhammad W. Khan, MBA, HCM
Sarah Mueller
Michelle Ng
Sonia Pathirajamudali
Rob Scott
Abby Shimon, PharmD
Edwin A. Shivers, II
Ashayla Stephens, MHA
Nikolas J. Swiderski
Doug Todes
Yasmin Vellani
Jana R. Voege, MBA, MS, FACHE
Matthew Vuckovich
Brian Wagers, MD
Kendra R. Walker, BS
Landon D. Welch, MHA
Jimmy L. White, MBA, EMT-P
Adam Wisler
Katherine Carter
David Darrigan, DO
Cullen Epley, MHA
Heather Farmakis, PhD
Mariah Fletcher
Shovendra Gautam, MD, MBA, Barbara Hayes
Bridgette L. Hunter
CPT Bradley Hurt
Gurbinder Jassar
Ashley S. Jones, MBA
Margie Kirkling-Ezenwa
Amy McCarthy, DNP, MSN, RN
Kendall J. McGhee
Michael Minks
Marcos Pesquera
Jason Plumley
Subrahmanya Venkateswara Rao
Kotamraju
Nancy J. Reed, LFACHE
Alex Rodriguez, BS
Audrianne Z. Schneider, FACHE
Salomeh P. Sheridan
Billy Smith
Cescilly O. Smith-Jenkins, PhD
Maj James Stafford, III
Amanda Villarreal
Monica F. Ward
Peter Yacoub
McKenzie R. Adams
Sandra Allen
Jordan Anderson, MHA
Cassandra M. Arellano
Jennifer Arnouville, DO
Capt Don Brathwaite, MBA, MPH
Courtney Busby
Peter Castro
Kihoon J. Cho, PharmD, BCPS, MBA
Robyn Cobb, MHA
Kate Costello
Michelle K. Davis
Tara Davis
Gerardo De Leon
James d’Etienne, MD
Curran Eigelberger, MHA
Tricia Elliott, MD
Victoria Feather
Christa Forrestal
Brittany Freiden
Chirag Gosai
Vishal Gottumukkala
Gregory L. Haralson, FACHE
Charles Huggins, MD
Elise M. Hulsebos, MPH, FACHE
Kimberly Jackson
Candice Johnson
Jay Johnson
Nicole L. Kindred
Jessica Kirby, DO
Heidi Knowles, MD
Michael Leary
CW2 Joshua Lewis, BS
Malachi Mack
Stephanie Madrid
Walt Massey
Dean S. Mazdai, BS, MHA
Casey McMullin
Jiye Moon
Hoyt Nichols
D. Andy North, FACHE
Dennis Okindo
Alisha Patel
Monali Patel
Maheen Pervaiz
Michael Rice
Dominique M. Salas-Garfias
Jesus Salazar , III
Emily A. Sander
Apinya Sangarunsilp
Veronica Singleton
Andrew B. Smith, FACHE
Astrid Sobotka
Michael Sullivan
Rasheika M. Swain
Cynthia L. Tamez
Anissa Vasquez
Alexis G. Villegas, Jr.
Brittany N. Wall, DNP, RN, APRN
Chris C. York, FACHE


























