2 minute read
Implications for Outcomes
perceptions about telemedicine among underserved urban African American and Latino populations. Telemedicine has been advanced as a vehicle to increase access to specialty care among the urban underserved, yet little is known about its acceptability among these populations. George et al. (2009) found that concerns about telemedicine varied between the two racial/ethnic groups. These findings have implications for important issues such as the adoption of telemedicine, patient satisfaction, and doctor-patient interactions. It will be critical to consider perceptions of this healthcare innovation in the development of strategies to market and implement telemedicine among underserved urban African American and Latino populations.
One of the greatest challenges facing people in underserved neighborhoods is the access to consultants. Nijland et al. (2009) address the role of e-consultation in this regard. The patients’ motivations to use e-consultation strongly depended on demands being satisfied, such as getting a quick response. When analyzing socio-demographic and health-related characteristics, it turned out that certain patient groups—the elderly, the less educated, chronic medication users, and frequent general practitioner visitors—were more motivated than other patient groups to use e-consultation services, but also were more demanding. Less-educated patients, for example, more strongly demanded instructions regarding e-consultation use than highly educated patients.
Advertisement
Sicker patients with greater care needs are being discharged to their homes to assume responsibility for their own care with fewer nurses available to aid them. This situation brings with it a host of human factors and ergonomic (HFE) concerns, both for the home care nurse and the home dwelling patient, that can affect quality of care and patient safety (Or et al., 2009). Many of these concerns relate to critical home care tasks concerning information access, communication, and patient self-monitoring, equitability, and self-management.
Outcome measures reflect the result of care, from a clinical or patient perspective. Although mortality is by far the most commonly used measure, other outcomes that could be used as quality indicators include complications of care, hospital admission or readmission, visits to the emergency room, and a variety of patient-centered and staff-based measures of satisfaction, health status, or utility. Outcomes can also be defined in the context of patients’ and staff experiences.
Ramaekers et al. (2009) conducted a study on telemonitoring aimed at assessing its short-term impact on patients’ disease-specific knowledge, adherence, and depression. The improved adherence rates within the three-month study period underscored the potential of telemonitoring to enhance selfmanagement among heart failure patients and its potential impact on other outcomes. Longer-term results will enable solid conclusions to be reached concerning the relationship between telemonitoring and patients’ adherence.
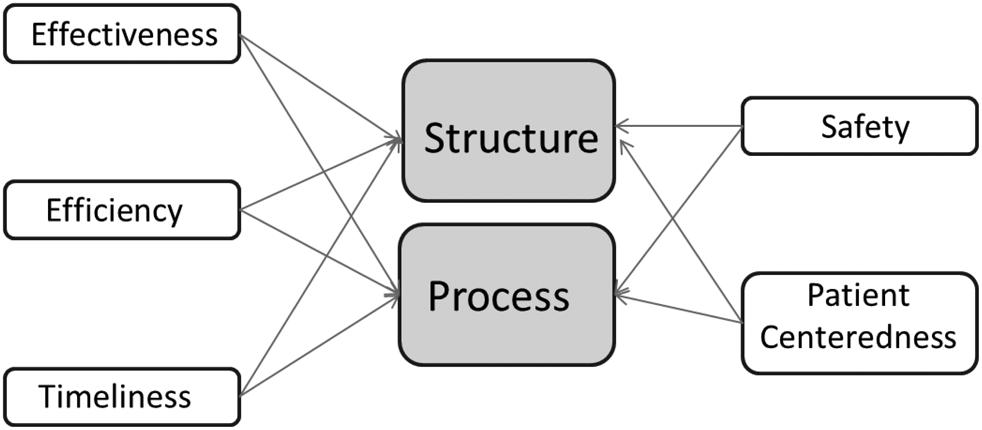
Figure 9.2 shows the interaction between the variables that drive structure and process and telemedicine quality. In this framework, telemedicine quality manifests in two ways—patient satisfaction and provider satisfaction—with vital implications for clinical outcomes.
Any attempt to understand quality in telemedicine must account for the following key variables:
◾ Access to care by patients ◾ Access to service providers ◾ Patient safety ◾ Diagnostic accuracy ◾ Clinical effectiveness (communication among care providers, documentation and records, outcomes, reliability of interpreted data at remote locations, etc.) ◾ Confidentiality of health records ◾ Patient satisfaction, patient perception, and acceptability ◾ Provider satisfaction ◾ Structure—(technology, facility, transmission, efficiency of care delivery, costs, etc.)