8 minute read
Dimensions of Quality Measurement in Telemedicine
it is not yet clear in what situations, if any, the potential benefits might be realized. Early studies, each performed at a single center and comparing care before and after the implementation of a tele-ICU system, documented decreases in length of stay (LOS), mortality, and cost, first in an academicaffiliated community hospital and subsequently in a tertiary-care hospital (Rosenfeld et al., 2000; Breslow et al., 2004).
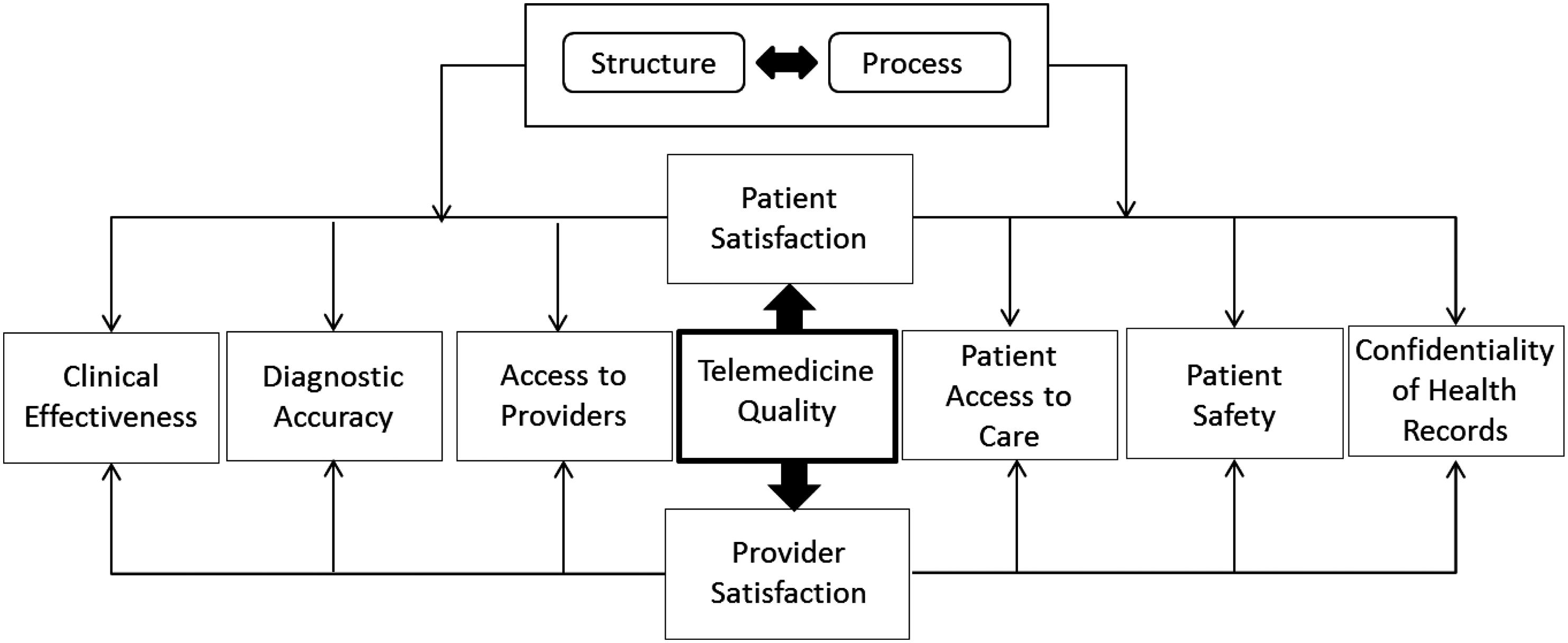
In this chapter, we propose a merger between Donabedian’s model (structure and process), and the IOM model to identify 12 dimensions for evaluating quality in telemedicine (Table 9.1). In Table 9.2, we explain the intersections between the two models (Figure 9.1).
Advertisement
Dimensions of Quality Measurement in Telemedicine
Using the combination of the models from the IOM and Donabedian, we arrive at a confluence of powerful ideas that make it possible to evaluate quality in telemedicine. This combination presents 12 dimensions for evaluating quality, as shown in Tables 9.1 and 9.2, above. The following is a brief description of the dimensions and the corresponding research questions:
Safety and Structure: Safety addresses how to avoid injuries to patients from the care intended to help them. Structure refers to the attributes of the settings in which providers deliver healthcare, including material resources (e.g. EHRs), human resources (e.g. staff expertise), and organizational structure (e.g. hospitals vs. clinics). The healthcare structure reflects the setting or system in which care is delivered. The research question is: Does the structure of the telemedicine application help
Table 9.1 Twelve Dimensions of Quality Telemedicine
Institute of Medicine Model
Safety Effectiveness
Patient-Centered
Timely Efficient
Equitable Donabedian’s Partial Model
Structure Process
1 2
3
5
7
9
11 4
6
8
10
12
Table 9.2 Explanation of Intersections between Donabedian’s Model and IOM Model
Institute of Medicine Model Donabedian’s Process/Structure
Structure Process
Safety How is safety affected by the structure of TM?
Effectiveness How does the structure of TM affect effectiveness?
Patient-Centered What is the impact of the structure of TM on patient-centeredness?
Timely How does the structure of TM affect timeliness?
Efficient How does the structure of TM affect efficiency? Equitable Does the structure of TM make it possible to deliver services in an equitable manner? How is safety affected by the TM process? How effective is the process used in delivering TM? Is the TM process as patientcentered as it needs to be?
How does the process affect the timeliness of TM?
How does the process affect the efficiency of TM? What is the impact of the process on the equitable delivery of care?
avoid or prevent injuries to the patients from the care intended to help them? According to the Telemedicine Research Center (TRC), a nonprofit public research organization based in Portland, Oregon, two types of technology are used in most telemedicine applications. The first type stores and sends digital images taken with a digital camera from one location to another. The most common application of this kind of telemedicine is teleradiology—sending X-rays, computerized tomography (CT) scans, or MRIs from one facility to another. The other type of technology described by the TRC is two-way interactive television
Figure 9.1 Framework of intersections between models.
(IATV), which uses video-teleconferencing equipment to create a meeting between a patient and primary care physician in one location and a physician specialist elsewhere when a face-to-face consultation is not feasible because of time or distance. Peripheral equipment even enables the consulting physician specialist to perform a virtual physical examination and hear the patient’s heart sounds through a stethoscope.
The availability of desktop videoconferencing has expanded this form of telemedicine from a novelty found exclusively in urban, university teaching hospitals to a valuable tool for patients and physicians in rural areas who were previously underserved and unable to access specialists readily. The same technology may be used to send slides or images from the pathology laboratory to another physician or laboratory for a second opinion.
Another example of the use of digital image transfer is the rural primary care physician who, miles from the nearest dermatologist can send a photograph of a patient’s rash or lesion and receive an immediate, long-distance consultation from the dermatologist. There are significant safety challenges posed by locations in rural areas, especially regarding technology, power supply, and qualified personnel.
One application of telemedicine that uses only the standard telephone line in a patient’s home is transtelephonic pacemaker monitoring. Cardiac technicians at the other end of the telephone can check the implanted cardiac pacemaker’s functions, including the status of its battery. Transtelephonic pacemaker monitoring can identify early signs of possible pacemaker failure and detect potential pacemaker system abnormalities, thereby reducing the number of emergency replacements.
It can also send an electrocardiogram ( ECG) rhythm strip to a patient’s cardiologist. Additionally, some of the communities that would benefit most from telemedicine do not have the telecommunications equipment necessary to deliver the bandwidth for telemedicine (http://www.libraryi ndex.com/pages/1866/Change-Challenges-Innovation-in-Health-Care-D elivery-INFORMATION-COMMUNICATION-TECHNOLOGY.html, 2009). Safety and Process: Safety addresses how to avoid injuries to patients from the care intended to help them. Processes of care are the clinical interventions and services provided to patients. Process of care denotes what is actually done to the patient in the giving and receiving of care. The risk factors vary depending on the particular application of telemedicine. Teleradiology, for example, involves sending X-rays, CT scans, or
MRIs from one facility to another. The same technology may be used to
send slides or images from the pathology laboratory to another physician or laboratory for a second opinion. There is no independent way to verify the qualifications of the individuals interpreting the images or ascertain the quality of the images. Varghese and Phillips (372009) studied how advanced practice nurses (APNs) cared for their telehealth patients. According to Varghese, they did so by (1) being with them, (2) personifying the images, and (3) possessing certain attributes. The major constructs that emerged from the data together formed a model of how APNs conveyed caring in telehealth.
As the menu of telehealth services (telesurgery, telecardiology, telerehabilitation, teledermatology, teledentistry, telehomehealth, teleassessment, telepathology, etc.) grows, it is imperative to evaluate the point of convergence between safety and process. According to Lee et al. (2010), parents reported positive perceptions about telemedical retinopathy of prematurity (ROP) diagnoses, but expressed a preference for face-toface care. Thus, telemedicine has the potential to alter the nature of the patient-physician relationship. The resulting research question is: What are the safety issues involved in the widely divergent scope of applications in the field of telemedicine? Are the risk factors significantly different from process to process for each application? Does the absence of a face-to-face interaction predispose certain patients to safety concerns? Does the departure from traditional physician-patient communication create possible safety issues?
Sandberg et al. (2009) conducted a study to better understand the experiences of providers and the factors they perceive contribute to the success of telehealth interventions and their own satisfaction. Face-toface or telephone interviews were conducted with 10 diabetes educators (nurses and dietitians) who served as providers of a telemedicine case management intervention for older adults who have diabetes. Qualitative analyses revealed that providers were very satisfied with their experience and felt their efforts with patients were generally successful. Providers also identified several unique benefits to telehealth interventions. These included opportunities for more frequent contact with patients, greater relaxation and information due to the ability to interact with the patients in their own homes, increased ability to reach the underserved, more timely and accurate medical monitoring, and improved data management. The primary disadvantages of telehealth they identified were technology problems and a concern about the lack of physical contact with patients.
Effectiveness and Structure: Effectiveness is determined in the context of providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (avoiding underuse and overuse, respectively). Structure refers to the attributes of the settings in which providers deliver healthcare, including material resources (e.g. EHRs), human resources (e.g. staff expertise), and organizational structure (e.g. hospitals vs. clinics). Healthcare structure reflects the setting or system in which care is delivered. Two important questions arise, as follows: i) Does the structure of a telemedicine application support the quest for effectiveness? and ii) Is effectiveness compatible with the structure of a telemedicine program?
Despite the promise of telemedicine, several obstacles prevent
Americans from realizing all its potential benefits. As of July 2004, many states in the United States did not permit physicians who are not licensed in their states to practice telemedicine, and the Centers for
Medicare and Medicaid Services will reimburse for interactive teleconference services but not digital image transfer. Although insurance coverage is rapidly widening, some private insurers are reluctant to pay for telemedicine, and some physicians fear additional liability (i.e., medical malpractice suits or other litigation) arising from telemedicine.
Warshaw et al. (2009) investigated the diagnostic and management effectiveness of teledermatology. They noted that, in general, the diagnostic accuracy of teledermatology was inferior, whereas the management of teledermatology was equivalent to a clinic’s dermatology.
However, for the important subgroup of malignant pigmented lesions, both the diagnostic and management accuracy of teledermatology was generally inferior to a clinic’s dermatology and up to seven of thirtysix index melanomas would have been mismanaged via teledermatology. They advised that teledermatology and teledermatoscopy should be used with caution for patients with suspected malignant pigmented lesions.
A study conducted by the Mayo Clinic, Rochester, Minnesota, and the
University of California, San Diego, California, shows the benefit of telemedicine in stroke diagnosis. Six rural hospitals were connected to specialists at two primary stroke centers using a video feed from a mobile robotic telemedicine camera system positioned near the patients’ beds.
Subsequently, 276 patients with stroke symptoms at their respective emergency departments were randomly assigned to telephone consultations versus two-way telemedicine consultations. Using telemedicine,