206 ◾ Healthcare Value Proposition
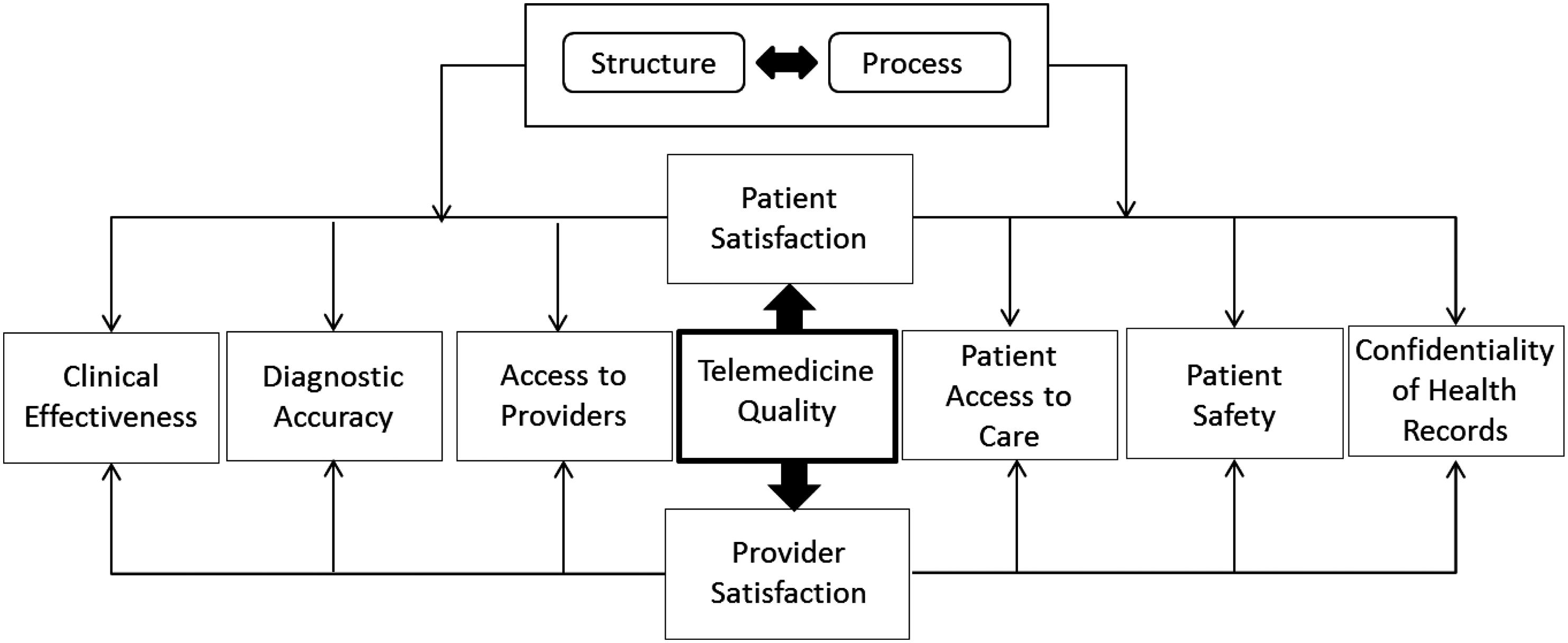
it is not yet clear in what situations, if any, the potential benefits might be realized. Early studies, each performed at a single center and comparing care before and after the implementation of a tele-ICU system, documented decreases in length of stay (LOS), mortality, and cost, first in an academicaffiliated community hospital and subsequently in a tertiary-care hospital (Rosenfeld et al., 2000; Breslow et al., 2004). In this chapter, we propose a merger between Donabedian’s model (structure and process), and the IOM model to identify 12 dimensions for evaluating quality in telemedicine (Table 9.1). In Table 9.2, we explain the intersections between the two models (Figure 9.1).
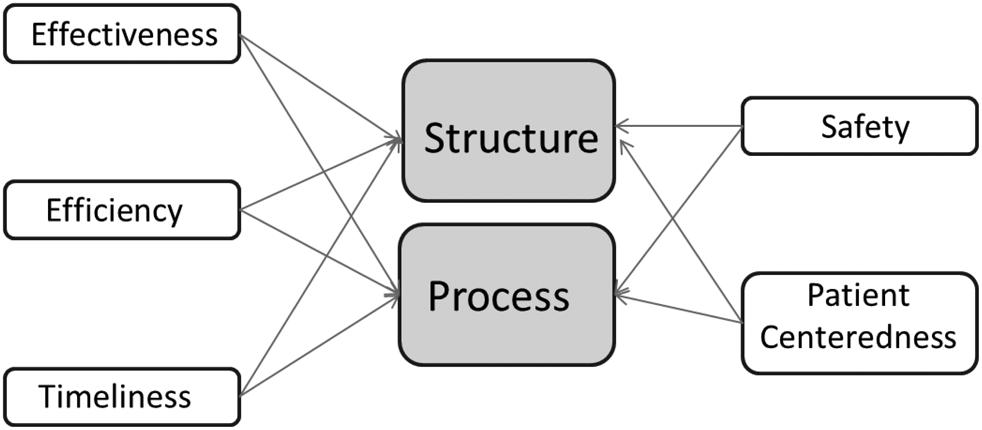
Dimensions of Quality Measurement in Telemedicine Using the combination of the models from the IOM and Donabedian, we arrive at a confluence of powerful ideas that make it possible to evaluate quality in telemedicine. This combination presents 12 dimensions for evaluating quality, as shown in Tables 9.1 and 9.2, above. The following is a brief description of the dimensions and the corresponding research questions: Safety and Structure: Safety addresses how to avoid injuries to patients from the care intended to help them. Structure refers to the attributes of the settings in which providers deliver healthcare, including material resources (e.g. EHRs), human resources (e.g. staff expertise), and organizational structure (e.g. hospitals vs. clinics). The healthcare structure reflects the setting or system in which care is delivered. The research question is: Does the structure of the telemedicine application help Table 9.1 Twelve Dimensions of Quality Telemedicine Donabedian’s Partial Model Institute of Medicine Model
Structure
Process
Safety
1
2
Effectiveness
3
4
Patient-Centered
5
6
Timely
7
8
Efficient
9
10
Equitable
11
12