5 minute read
3 The Patient Experience
Chapter 3 The Patient Experience
The battle line in the quest for excellence in healthcare goes through the patients’ experience. The patient experience is no longer an afterthought but the very essence of healthcare organizations’ existence. Excellence in patients’ experience is inextricably linked to excellence in employee experience, and patient experience suffers when staff morale is low. Of the many factors responsible for low staff morale, the most compelling have to do with management’s failure to strike the right balance between the workload demand and the organization’s capacity. When the staff is visibly overwhelmed, it is unrealistic to expect them to care much about the patient experience. Without careful monitoring of the available resources and staff’s capacity (in terms of time, equipment, processes, competencies, and skills), the patient experience will remain a distant concern for employees.
Advertisement
There will always be employees who give of themselves regardless of the morale in the unit or department. However, they are the exception. Unless there is a wholesale retooling of the employee experience, employees that are unengaged can only produce sporadic evidence of successes. Patient experience survey results are up for two months, then down for three, then up for one, etc. These organizations are perpetually in pursuit of the elusive top box score, and the employees are forever confounded by their lack of sustainable progress. Many of these survey “warriors” are unwilling cast members in a theatre of anguish fueled by a recalcitrant organizational culture.
The Beryl Institute defines the patient experience as the sum of all interactions shaped by an organization’s culture that influence patient
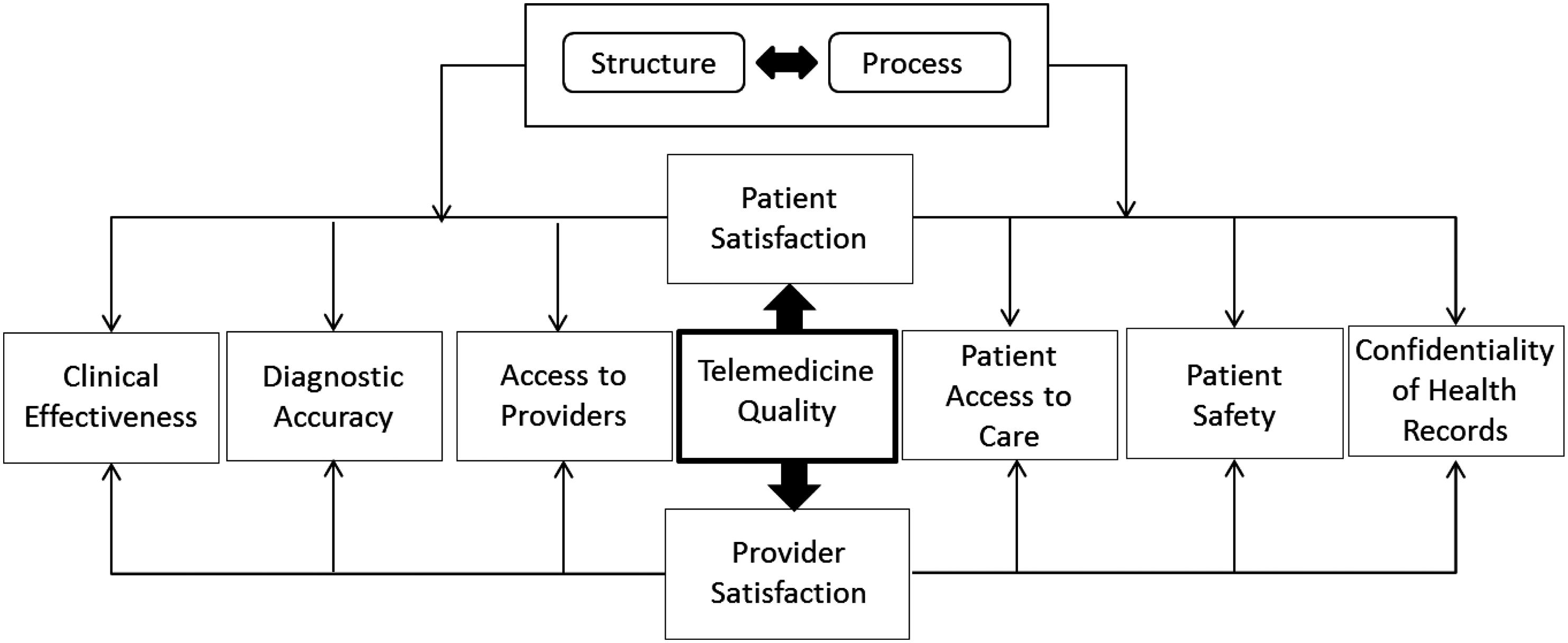
perceptions across the continuum of care (Beryl Institute, 2013). There are two key components of the patient experience—clinical excellence and service excellence. Most patients do not understand the clinical aspects of the services they receive; however, there are certain experiences that would cause them to lose trust in clinical services. The most significant determinants of patients’ erosion of trust is a failure in patient safety, failure to reduce patient suffering, and failure to show caring, empathy, and compassion. If a patient falls ill from a hospital-acquired infection or does not receive effective care that follows proven protocol, trust is eroded, and patients’ experience will suffer. Ensuring patient safety and quality care is the first step to creating a positive patient experience.
Providers can reduce patient suffering by being more attentive to the latter’s needs. Checking in on call buttons or determining if a patient needs help reaching an item or using the bathroom can help protect patients from falls or other harms, reducing preventable suffering. As patients have more choice and healthcare decisions impact their wallets more, they will increasingly compare their healthcare experience to their expectations in other aspects of their lives. As patients bear more out-of-pocket healthcare expenses, they will become choosier and more critical in their evaluation of services. Healthcare organizations will need to live up to the realities of a new service expectation to continue to win the business of their servicesavvy customers.
While critical acclaim and business accolades such as “the Best Hospitals,” or the “Number One Hospital” are essential to business success, the greatest measure of leadership success is the degree to which excellence in non-clinical aspects of the service match or exceed the excellence in clinical outcomes. Neither by itself is sufficient. There are four critical areas of concern for patients, as follows:
1. Engaged Staff with a Pleasant Disposition: A patient in a vulnerable state would prefer to deal with a healthcare provider (nurse, physician, or other staff) with an overall pleasant disposition. Patients often perceive a person with a pleasant disposition as being more approachable.
A provider who seems overwhelmed, in a hurry, or otherwise frustrated sends out signals that suggest he/she does not want to be bothered or, worse, does not want to be there. The message to the patient is: Limit the number of questions you might have, speak fast, and get straight to the point. A patient’s nightmare scenario is to deal with an angry nurse
or physician. In that situation, the patient’s concern is that he/she might exacerbate whatever is causing the provider to be angry. Some patients might even wonder if they are the target of the anger. Management must ensure that workload and staffing ratios allow providers sufficient time to provide the needed services. While the goal of a “happy staff” may be unrealistic, it is within the purview of good management to ensure providers have a reasonable chance of being successful at their responsibilities. 2. Connection with the Patient: When a caregiver connects with the patient, it speaks to how much respect he/she has for the patient.
When a provider connects personally with the patient, it acknowledges the patient is an individual worthy of respect and courtesy. This goes against conventional thinking about the need for providers to remain objective and unemotional. By connecting with the patient, a provider builds trust and increases the likelihood of a successful encounter. 3. Teamwork Among Caregivers: When patients perceive a lack of teamwork among providers, it shatters their trust in the process. The best evidence of a lack of teamwork is in communication breakdowns or failures. The perceived lack of communication between the doctor and the nurse leads some patients to conclude that they are receiving an inferior level of care. 4. Empathy Deficit: It takes a gifted clinician to demonstrate the ability to put themselves in the shoes of patients (and their family members) while providing a service to them. Most patients can perceive a caregiver’s indifference. Empathy enables providers to listen to the concerns of patients, understand their feelings and fears, and explain the choices and options caregivers are making and why. Patients value displays of concern and caring, especially in the emergency room. 5. Keeping Patients Informed: Providers often underestimate patients’ desire for information. Patients seek information about any and everything connected to their condition or the process for addressing it. This includes information about delays, options, and self-care at home.
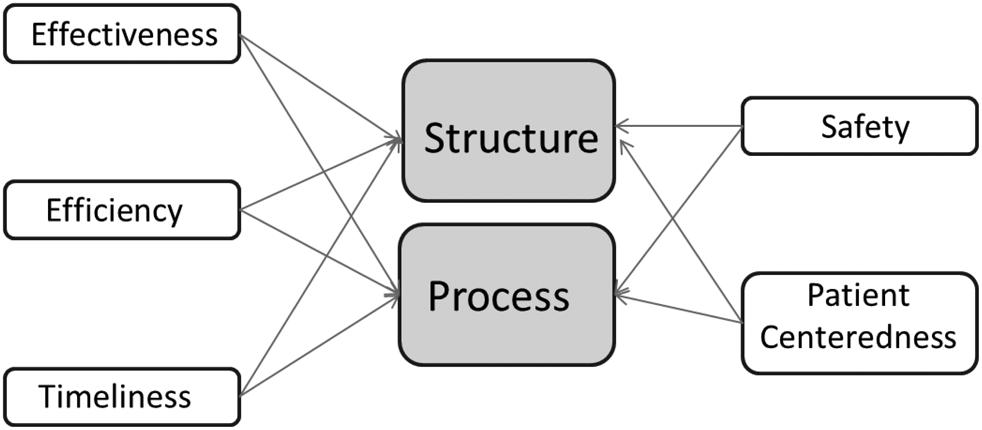
By focusing on care quality and safety as parts of the patient experience, as well as using patient-centered care approaches to drive patient satisfaction and access, healthcare leaders can achieve a better patient experience. To reduce negative patient experiences, healthcare providers must focus on better patient-provider communications. If health systems want to improve