
59 minute read
What we have achieved in 2019/20
PART 3
1. What we have achieved in 2019/20
Advertisement
Progress against the quality priorities that we set for 2019/2020
This section describes the Trust’s progress against the quality priorities that we set for 2019/20 The Trust had nine quality priorities for the year.
Priorities for improvement in 2019/20
PATIENT SAFETY
Priority 1
Priority 2
Priority 3
PATIENT EXPERIENCE Achievement
Promote safe and therapeutic ward environments by preventing violence Strengthen further Risk Management and Care Planning including overall risk issues in acute ward patient groups Improve service user safety and staff wellbeing in communitybased teams
Priority 4
Building a just and learning Culture
Priority 5
Agree and Implement a revised patient experience strategy Priority 6 Improve signposting for welfare support for service users
CLINICAL EFFECTIVENESS
Priority 7 Priority 8 Priority 9
Improve dementia care Continue progress with Patient flow Improve Service Users’ physical health care
PATIENT SAFETY
Description of the quality issue and rationale for prioritising
Safe and therapeutic ward environments with prevention of violence, reduction in restraints and responsive support for service users and staff post-incident are Trust priorities. While progress has been made within this area, further achievements are required.
Incidents of violence and aggression may also affect the perception by staff of services and service users in a manner that has a strong negative impact on the overall experience of care (De Benedictis et al., 2011 cited by NICE, 2015)
A safe environment has an impact on how therapeutic and safe our service users, staff and visitors feel; service users and staff experience can be negatively impacted if the environment is perceived to be unsafe.
Evidence tells us that challenging behaviours, such as aggression and violence, are relatively common in mental health settings, with potential serious consequences that can negatively affect not only the health and safety of staff, service users and carers, but can impact on the recovery of service users (NICE Guideline 10, 2015; Mental Health Act Code of Practice, 2015).
The Trust is therefore committed to safe clinical environments for all staff, service users and visitors and has committed resources and engaged in evidence-based interventions to tackle this issue.
Dedicated Specialist
The Trust has employed a dedicated Violence Reduction Specialist/Reducing Restrictive Practice (RRP) Lead who started in post in February 2020. They are focusing specifically on reducing aggressive and violent incidents, supporting staff to understand conflicts and containment patterns, and are key to our reducing restrictive practice goals. They have been working with colleagues across the Trust to embed a culture of identification and prevention, as well as promoting less restrictive environments with early feedback from staff being very positive.
Implementing SafeWards
This is an evidence-based, non-pharmacological clinical model known to reduce violence and aggression in mental health inpatient settings. The SafeWard Model also places an emphasis of psychologically-informed communication, structured activity and service user participation in the day to day operation of wards. We have incorporated safe ward training as part of our induction and into various training programmes. The Trust worked with Bright Charity to provide staff training and support on implementation. We hope to continue to work with SafeWards experts over the coming 12 months to continue to embed the 10 identified interventions on all our wards.
Policy review, development and Implementation
Covid-19 restrictive intervention protocol
The Coronavirus pandemic brought an additional challenge across the globe but a more unique challenge for mental health inpatient health care
providers. There were concerns that restrictive interventions will increase across care due to implementing government guidance for people in inpatient services.
We developed a Covid-19 restrictive intervention protocol that reflects a least restrictive approach and that also ensures that people’s human rights were not impacted while in care and gives a balance that promotes the health and safety of staff and other people.
Other guidance
We have updated our seclusion policy in line with the current evidence-based and legal framework to promote the use of least restrictive principles and a human right-based approach that we hope would impact positively in the reduction of the use of seclusion and the service users experience when this intervention is needed.
We continue to monitor and review all use of restrictive intervention via our monthly positive and proactive care group.
Reducing Restrictive Practice (RRP) Training
There is a vast amount of available evidence that indicates a restrictive, overbearing and controlling culture in inpatient settings can itself increase service user frustration, gives rise to flash points, cause conflict and lead to more containment (Bowers et al., 2014).
Our RRP Lead is delivering a bespoke training to staff that is focused on a human right based approach that will support staff understanding and create an extensive awareness of the impact of a restrictive environment and culture, with the aim of reducing conflict and containment and so reducing restrictions and prompting a least restrictive approach.
External Post-Restraint Debrief
Nice Guidelines 10 recommends a post restraint incident debrief following the use of restrictive intervention. They also recommend that an independent debrief takes place within 72 hours, this is a unique intervention that is quite challenging to implement.
Our Trust have experts by experience who are working as volunteers, facilitating post restraint intervention debriefs. This is a unique project that has received positive feedback across the country.
Prevention and Management of Violence and Aggression Training Standard
From April 2021, it will become compulsory for all NHS Trust to ensure that the training staff are receiving, conforms to the Restraint Reduction Network’s (RRN) training standards. This requirement will be made mandatory and regulated by the Care Quality Commission. Among other aspects, the standard is aimed at ensuring all training syllabuses across the country meet the same criteria with the overall aim of focusing on reducing the use of restrictive interventions. C&I has engaged with, and are currently working with, a provider who has been assessed and certified in line with the RRN standards via the BILD Association of Certified Training. As part of the standard, and in line with other best practice guidance, the Trust is now providing refresher/update training to staff, in line with Covid IPC guidance and use of appropriate PPE.
Implementing team Safety Huddles
Safety huddles continue to be embedded across our inpatient teams as one of our interventions in identifying, preventing and managing violence and aggression. The safety huddle is a short briefing that takes place on the wards during the course of a shift involving all staff; its focus is to quickly discuss potential escalating behaviour or risk that needs addressing and attend to it in order to prevent a potential conflict situation escalating. It is also used to feedback outcomes
of interventions with service users and celebrate positive interactions during a shift.
Body Cam Pilot
The Trust is also planning a body cam pilot as part of its violence and aggression reduction strategy. A research article on the feasibility of using body worn camera in an inpatient mental health setting carried out by Northamptonshire NHS Foundation Trust reported a reduction in complaints and incidents following the introduction of body cams in an inpatient ward. The project is led by the QI team with input from our RRP lead, nurses, medical staff, OTs, psychologists and service users. The pilot will start with 2 inpatient acute wards in the Autumn
We now have an established police liaison team across the boroughs of Camden and Islington and the officers visit both the St Pancras site and Highgate sites weekly. They are supporting staff and service users with any concerns or questions and helping with problem solving any major issues regarding incidents of violence and aggression.
Violence and Aggression Data Collection
All violence and aggression data is captured via our online incident reporting system DATIX. The Positive and Safe Group, held monthly and chaired by Deputy Director of Nursing, reviews and analyses violence and aggression data regularly and discusses themes from incidents in monthly meetings with wider Trust team. All learning from incidents, suggestions on how to reduce incidents are discussed and solutions disseminated to staff on the wards and various departments via the Acute and Rehab Quality forums.
The next 12 months’ key priorities
With services responding to the global pandemic, this response will be the main focus over the coming six months. However, we need to continue to ensure that service users and staff are working together to keep environments safe, reduce the levels of violence and aggression and continue to identify and reduce restrictive interventions.
• Development of a Promoting Safe and
Therapeutic services strategy with targets including agreed % reductions in restraints, seclusion and restrictive interventions
• Decrease in staff assaults and increased support for staff when an assault has happened.
• To have an Increase in staff and service user positive feedback on their experiences whilst an inpatient or working on the ward
• Embedding of the Relational Security model and using this to review incidents.
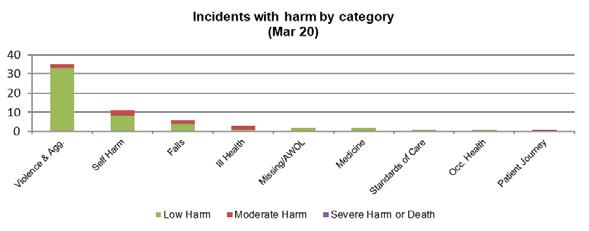
Incidents resulting in harm up to March 2020
The overall trend on the number of incidents suggests continuing reduction in incidents of violence and aggression against staff and service users.
This data shows that the proportion of restraints that are prone restraints are being kept to a minimum.

Identified area for improvement
• Quality and timeliness of risk information
• Review and development of Risk
Management Policy
• Review and development of Risk
Management training
• Review and development of risk assessment documentation, including risk history summaries with the Trust’s electronic recode system.
• Increased co-production of safety plans / care planning with service users, carers and families
• Review and development of a comprehensive evaluation framework
What we have achieved
This work has progressed significantly via the Trust Risk Management and Suicide Prevention Task and Finish Group, which has Trustwide divisional representation and service user and carer input. A core training programme has been drafted which will include a trauma-informed approach, a strong focus on therapeutic rapport, co-production, formulation, documentation and communication. This will be supplemented by core training for managers to ensure that staff are supported with complex risk assessment and management, clinical supervision and appropriate lessons learnt process post incident. Clinical safety and staff wellbeing will be integral to this training. The current documentation template is under review, via the Digital Connections Forum. It is agreed that a new Risk Chronology / History template will be added to the EPR, reflecting evidence that previous risk is an important indicator of future risk. The current risk assessment and management plan EPR template is being developed with significant feedback from clinicians and service users. The safety plan will be aligned with the Dialog + new care plan / recovery plan and be based on additional consultation with the service user representatives. This work is closely aligned with the suicide prevention workstream, which is supported by external stakeholder groups pan London and with Camden and Islington Public Health Department’s development of a local Suicide Prevention Strategy. A draft Suicide Prevention Plan will be taken to the Trust’s Quality and Safety Programme Board in November 2020 and will include Training options.
The finalisation and development of Risk Management and Suicide Prevention Training has been identified as a high priority in the Trusts’ Health Education England Registered Nurse and Allied Health Professional Training Plan. This enables a dedicated training resource to progress this work and recruitment to this role is planned for late 2020, (subject to the impact of the C19 pandemic).
The Task and Finish group has achieved initial policy review and identified documentation and training requirements and is aligning this work with an STP-wide suicide prevention initiative.
The Trust was in the midst of a trial of a new approach to care planning that was developed with active service user and carer input when the Covid 19 pandemic lockdown happened. The trials were in Islington SAMH CMHT, SAMH HTT and EIS, but were suspended as teams were restricting frequency and duration of face-to-face reviews and the Care Planning
process devised was reliant on in-person contact. We are now adapting approaches in each team and responding to new team working practices so that the pilot can conclude, and an implementation plan developed
Next steps/future challenges
• Completion of the multi-disciplinary Task and Finish group review • A structured implementation plan with the completion of the review
• Development and implementation of a revised, virtual / online training programme with a dedicated resource
• A revised evaluation and ongoing governance framework
Description of the quality issue and rationale for prioritising
There has been considerable improvement in the completion of core skills training over the past 12 months, with overall compliance reaching 88%. There are, however, some skills areas where we have not reached target levels. The critical importance of core skills training was highlighted by the CQC as part of its inspection. Core skills/mandatory training supports staff to provide safe and effective care to service users and is at the core of safe care.
Identified areas for improvement
• Increase accessibility for Breakaway training
• Increase the number of days available for, and % of staff completing, CPR and ILS training
• Plan dates well in advance to accommodate all staff and increase uptake
• Reduce number of non-attendance
What we have achieved
Zoning Meetings
Following the audit over the summer the R&R Division has now revised the Zoning Protocol to strengthen the section on clients of concern and in particular maintaining the safety of clients awaiting MHAs and will re-audit practice against the revised protocol.
The zoning meetings are now business as usual and have been vital during the COVID-19 situation. This is because teams are now working from the office and remotely so the function of staff checking in through these meetings has also become very important. In addition, the meetings are used to prioritise clients of concern as well as those shielding and to decide who will receive a phone call or a face to face contact. The importance of having, and properly using IT is central to this.
With the lone working we are also in a changing situation; we are revising how lone working works in practice.
Description of the quality issue and rationale for prioritising
Service users’ needs are varied and can be complex. To meet those needs, the Trust is continuously thinking of new ways to evaluate the needs of patients and to deliver personalised care. One way to identify gaps in meeting service users’ needs relates to the issue of clinical risk management and how this can be dynamic in nature. To address this, community teams in the Rehab and Recovery Division have implemented daily MDT meetings. Attended by all professionals, these daily meetings provide staff with an opportunity to discuss clients of concern, urgent clinical issues and ensure critical pieces of work are not missed by the team. The meetings adopt a Clinical Zoning structured approach to support the wider MDT decide on the resources required to safely carry out the interventions required. As an outcome service users’ needs are met in a timely manner and staff feel greater support when facing issues relating to clinical risk.
Current picture
Daily MDT meetings are currently taking place across many Recovery and Rehabilitation community teams, apart from a few who hold meetings two to three times a week due to the operation capacity of the teams. Through benchmarking best practice, the Trust developed and implemented a protocol to ensure that these meetings are undertaken in a structured, standardised and consistent way to facilitate the delivery of targeted mental health, physical health and social interventions whilst enhancing collaborative and effective multi-disciplinary work to support service users in their recovery and managing difficult time and crisis. We have undertaken some audits to measure compliance against the protocol
Identified areas for improvement
• Early intervention in crisis to improve outcomes and service user experience
• Input from all multi-disciplinary professionals
• Recording system to track all actions, from day to day
• Recording of actions and outcomes on
Carenotes
• Improved communication with inpatient services to expedite discharges
• Efficient use of resources through joint working with crisis teams
• Improved Crisis planning in relation to high intensity users
How we will improve
• Effectiveness of Clinical Zoning –
Consistency in standards implementation
• Effective systems for managing concerns and gaps identified
• Improved patient experience
• Improved staff experience
• Joint quality improvement initiatives between Recovery & the Crisis Team
How we will measure success
• Compliance audit
• Regular review and evaluation of systems
• Monitor rates of inpatient admission
• Monitor rate of repeated re-admissions under the Mental Health Act
• Measure service user experience of the service responsiveness
• Measure staff experience
Core Skills
Description of the quality issue and rationale for prioritising
Core skills/mandatory training supports staff to provide safe and effective care to service users and is at the heart of safe care. The critical importance of core skills training was highlighted by the CQC as part of its inspection and commended the Trust on the changes that we had made because there had been a considerable improvement in the completion of core skills training over the past 12 months, with overall compliance reaching 88%. However, due to the COVID-19 pandemic most of the faceto-face training was suspended for a period to minimise cross infection risk. This meant our overall compliance figures dropped, making it challenging for the Trust to reach target levels as shown below.
Core Skills Target Compliance 31st March 2020 Compliance 30th September 2020 Movement From Jan-Sep
NHS | CSTF | Fire Safety
NHS | CSTF | Fire Warden
NHS | CSTF | MH NHS | CSTF | Infection Prevention and Control Level 1 - 3 Years NHS | CSTF | Infection Prevention and Control - Level 2 - 2 Years NHS | CSTF | Moving and Handling - Level 1 - 3 Years NHS | CSTF | Information Governance - 1 Year NHS | CSTF | Equality, Diversity and Human Rights - 3 Years NHS | CSTF | NHS Conflict Resolution (England - 2 Years | (Breakaway) Conflict Resolution - Physical Intervention Skills - 2 Years | (PMVA) NHS | CSTF | Resuscitation - Level 2 - Adult Basic Life Support - 1 Year | CPR Intermediate Life Support 80% 83.2% 79.21% -4%
80% 89.6% 80.61% -9%
80% 88.4% 85.28% -3.1%
80% 94.1% 87.97% -6.1%
80% 87.6% 84.80% -2.8%
80% 88.4% 85.28% 3.1%
95% 89.5% 93.35% +3.9%
80% 89.4% 86.31% -3.1%
80% 94.2% 90.98% -3.3%
80% 73.70% 66.81% -6.9%
80% 89.3% 86.73% -2.6%
80% 65.34% 54.83% -10.5%
80% 74.48% 69.44% -5.0%
Safeguarding Adults Level 1 80% 89.9% 85.02% -4.9%
Safeguarding Adults Level 2 80% 91.5% 86.65% -4.8%
Safeguarding Adults Level 3 80% 87.5% 74.72% -12.7%
Safeguarding Children Level 1 80% 89.6% 85.71% -3.9%
Safeguarding Children Level 2 80% 90.8% 86.21% -4.6%
Safeguarding Children Level 3 80% 91.1% 75.22% -15.9%
Prevent 1-2 85% 93.7% 92.41% -1.3%
WRAP 85% 95.2% 94.84% -0.3%
MCA 80% 80.7% 80.03% -0.7%
Identified areas for improvement
• Increase accessibility of virtual training during the COVID-19 pandemic
• Plan dates well in advance to accommodate all staff and increase uptake
• Reduce number of non-attendance
What we have achieved
Most of the core skills have maintained the target 80% compliance level, despite the pandemic. The increase in the number of days available for virtual Information Governance training made a huge difference. Last year’s compliance rate was 86.2% and the current figure is 93.5%, well-placed to reach the 95% required level
Actions that have been put in place for improvement:
• Additional CPR and ILS social distance compliant training sessions have been made available during the COVID-19 pandemic in order to meet uplift in demand.
• Monthly Core Skills report will continue to be published on the intranet
• Weekly reporting will continue to enable managers to monitor trajectories at a local level and help to plan for required release of staff to attend core skills training as necessary
• Trajectories will continue to form part of this reporting in order to highlight pinch points and to manage supply and demand for face-to-face programmes
• Post-pandemic commissioning of courses will aim to flatten ‘spikes’ caused by periods of concentrated high demand
• Core skills completion is now a requirement under the new Agenda for Change pay deal and will therefore form part of decisionmaking on whether a member of staff will progress to the next pay point.
• Maintaining the level of completion will require managers to forward plan the release of staff at a more measured pace in order to avoid spikes in demand and dropoff in completion levels. Divisions need to support their managers to work through levelling out the spikes which tend to occur between November and March.
Lone Working Device
Description of the quality issue and rationale for prioritising
Where employees work alone, personal safety is a priority consideration for the Trust. The Trust has therefore implemented policies and guidance on how to manage this risk. In addition to carrying a mobile phone, the lone workers have also been issued with lone working devices which are remotely monitored to enable a quick response when summoning emergency services on activation. With these additional safety devices, the risks that lone workers face should be reduced to an acceptable level. The Trust recognises that the implementation of safe working arrangements will largely depend on robust local circumstances, local procedures and protocols which should provide staff with specific guidance in relation to lone working and associated risk reduction techniques. Lone working devices are one element of how the Trust protects the safety of staff in combination with effective risk assessments, management plans, checking in after visits and teams undertaking joint visits were applicable.
Current Picture
The Trust has identified over 800 communitybased staff as lone workers and are currently leasing 580 devices. These devices are either a pooled device where two or more staff use it occasionally, or a dedicated device for sole use by a member of staff. Since implementation there has been a notable increase month-on-month of the number of staff using the devices. There are still issues with staff undertaking the training to use the device, and as a result, all staff identified as a lone worker have now had the training added to their core skills training making it mandatory. This will also allow training to notify managers of staff that are non-compliant and will ensure that new starters get this within their first week at the Trust. The Trust is also now in the process of rolling the lone working devices out to all wards for staff to carry when escorting patients outside on Section, to ensure their safety and the welfare of the service users when off-site. Identified areas for improvement • Reach the target training compliance level
• Improved access to a device for all staff
How we will improve
• Effective systems for managing concerns and gaps identified
• Act on feedback received from the Lone working Device monitoring agency
• Ensure all lone workers have access to a device when lone working
How we will measure success
• Undertake a compliance audit of staff carrying a lone working device
• Regular review and evaluation of systems
• Monitor rates of incidents were the lone working devices have been activated
• Measure staff experience
PATIENT EXPERIENCE
Priority 4: Building a just and learning culture
Identified areas for improvement
• Implement the local suicide prevention strategy
• Set up a group to specifically look at reducing self-harm and suicide
What we have achieved:
C&I’s cultural vision is working towards creating an increasingly more compassionate, collaborative, connected and responsive culture where staff and service users are valued, empowered and safe. We reported last time that one of the ways of embracing this was via a cultural collaborative where we met with other local Trusts and shared experiences and ideas of how to develop the culture. This initiative due to COVID-19 restrictions has been put temporarily paused until 2021.
In line with being responsive and compassionate, OD has been working closely with wellbeing to focus on supporting leadership and staff. Throughout the first wave of COVID-19, all managers and leaders were offered some oneto-one support. Many responded positively to this. Several teams were also offered reflective spaces where the emotional impact of COVID-19 was considered and it gave participants an opportunity to talk openly and safely while supporting one another. OD is also leading on a cross-Trust project team to create these reflective spaces for all teams.
Mentoring and coaching has continued during this period. A group of experienced external coaches and mentors offered their coaching expertise to all staff affected by COVID-19. Over 70 of our staff have been part of this and are finding this very helpful. The Fair and Just Culture programme run by Mersey Care continues to be put on hold due to COVID-19 and we hope to take this forward in the Spring of 2021. This programme offers insights into how to create an environment where staff feel supported and empowered to learn when things do not go as expected, rather than feeling blamed.
Description of the quality issue and rationale for prioritising
The Trust aims to deliver improved patient experience. We are revising the patient experience strategy, and its delivery/implementation plan. The current strategy has four over-arching principles:
• always listening,
• understanding what we are told,
• collaboration and co-production, and,
• communication, transparency and accountability.
Identified areas for improvement
• Increase the level of engagement and involvement of service users
• Finalise and launch a clear patient experience strategy
• Increase FFT response rates, a range of feedback mechanisms and the volume of responses
• Increase participation in co-producing care plans and collaborative working in delivering quality and service improvement
• Compliance with the accessible information standard
• Improve patient access and experience for people with characteristics protected by the Equality Act 2010
What we have achieved
As described earlier, the Trust engaged with Leeds University to provide support in delivering a strategy fit-for-purpose. Engagement with Care Opinion for partnership working has also commenced
Service User and Carer Involvement
The Trust is committed to promoting service user and carer involvement in all aspects of its work. Service user representation is now integral to a number of key Trust committees including the Finance Programme and Quality Boards. Operational Divisions are expected to have service user representation at Divisional Management meetings and Quality Forums
Managers undertaking recruitment are expected to involve a service user representative in the interview panel both in face to face and MS Teams based recruitment.

A monthly service user alliance meeting provides a “critical friend forum” for managers to present proposed changes with the Trust and to seek feedback. In recent months, this group has taken presentations on the St Pancras re development, the Trusts response to COVID and the use of peer coaching in C&I.
Next steps/challenge:
• Integration of experience and involvement
• Triangulation of patient, carer and staff feedback
• Executive champion to provide leadership and consistency
• Emphasis on data capture and analysis
• Invest in people with lived experience
Description of the quality issue and rationale for prioritizing
The Trust has received feedback from service users that there is insufficient support and guidance on welfare rights. They have told us that this gap is a factor in not coping with their illness
Identified areas for improvement what we have achieved:
• Improving signposting for welfare of service users.
Islington Council and the Trust
Islington Council and Camden and Islington Mental Health NHS Trust are committed to working in partnership to improve the offer available for our service users.
We aim to do this by:
The Fairer Together Partnership, which has been established to bring together a range of organisations in Islington to confront the challenges local people are facing and provide equal access to services. We are aware that statutory services have a role to play for the most vulnerable, but we cannot do it alone. The community of Islington, 3rd party services, providers, religious settings and voluntary networks etc. are all highly important in supporting our service users to improve their quality of life.
The Islington Directory, which aims to bring all the contact details of services in Islington into one place. We are at the start of this journey and continuing to strive to make the directory the place service users and carers go to, to find out about local community services and support networks.
The Making Every Contact Count (MECC), is an approach to ensure that every service user we come into contact with has an aim of improving their health and wellbeing. The MECC ensures that each service user is supported to take action to improve their own lifestyle by eating well, maintaining a healthy weight, drinking alcohol sensibly, exercising regularly, not smoking and looking after their wellbeing and mental health. This will include signposting and working in partnership with GPs, nurses, pharmacists and other specialist services.
The Strength Based Approach Model, which is used in assessments and reviews with individuals at both the Trust and London Borough of Islington. There is evidence that the use of a strengths-based approach can improve social
networks and enhance wellbeing for service users. A strengths-based approach within mental health, concentrates on the assets of individuals, families, groups and community organisations, which can allow service users to obtain a more personalised service which focuses on prevention and building resilience in individuals by signposting and using community resources. There are also three welfare rights advisors employed by the Trust. One is in the Community Mental Health Division representing the nonpsychosis service line. The other two are in Rehabilitation and Recovery, specifically in the South and North Camden R&R teams.
Camden Council and the Trust
Camden adult social care is working closely with C&I to implement What Matters – Camden’s strengths-based approach. What Matters is about working in partnership with people, focusing on what they want to achieve, looking together at their strengths, connecting them to informal support networks and community assets, and any formal support that is needed. A main thread of What Matters is the importance of relational practice and taking the time to connect people to community support rather than just signposting them. This may involve going with the person to an activity the first time, or phoning them to see how they got on.
COVID-19 has presented huge challenges, one of which is ensuring that all those who need support receive it. The VCS, C&I and the local authority have worked closely together to develop a single point of access for voluntary sector support. This support has in some instances replaced formal care support to free up care capacity. The SPA is working well and is an area we want to further develop.
CLINICAL EFFECTIVENESS
Priority 7: Improve Dementia Care
Description of the quality issue and rationale for prioritising
The Trust aims to further enhance our postdiagnosis offer for patients diagnosed with dementia. Our Services for Ageing and Mental Health are keen to implement a wider range of clinical interventions to improve clinical effectiveness.
Identified areas for improvement
• Introduction of additional clinical interventions
• Set up a research and innovation group
What we have achieved
The merger of the Islington Memory Service and Dementia Navigator model is now complete and a new Team Manager and lead Consultant in post. The team is now realigning to work in an integrated way with the Primary Care Networks. Our memory services continue to promote and support earlier diagnosis Both boroughs remain in the top three best performing CCGs for dementia diagnosis prevalence across London. Following diagnosis, all our patients with dementia are offered an ongoing service. This provides a single point of contact for the service user and their carer(s) and a regular review. This allows medication and care to be adjusted and means that the services user doesn’t have to continually re-tell their story as their illness progresses.
Next steps/future challenges:
Across our services working with people living with dementia we continue to work to enhance our post-diagnosis services
In Camden Memory Service, we are introducing a formal frailty scoring at contact points within care pathway, such as at assessment and at review. This will inform physical health advice provided by practitioners and referrals to other services. We are also piloting a “recovery” planning tool which more formally identifies opportunities to undertake life story work and advance care planning with service users with dementia, and to talk about physical. Also, in Camden, our non-medical prescriber can offer service users living with dementia and their carers, intensive, and importantly ongoing support, with taking dementia medication managing its side effects and interaction with other drugs.
In Islington, the Care Home Liaison Service is expanding with occupational therapy partly funded by North PCN – part of this role will be to improve dementia well-eing and reduce behavioural symptoms of dementia in care homes through enhanced occupation and upskilling of activity coordinators.
In order to improve the care of people living with dementia across all services, jointly with Whittington Health NHS Trust, we offer Tier 2 Dementia training accessible to all C&I staff and colleagues from Whittington Health, LBI and voluntary sector services and care homes in Islington
Priority 8: Continue progress with patient flow
Description of the quality issue and rationale for prioritising
The Trust aims to improve timely access to our services, ensure that patients are assessed and receive appropriate treatment and support in the right clinical and care settings, and are able to be stepped down to suitable services when they need less intensive, or in some cases restrictive, care and treatment.
As examples, we want to ensure that services users and local people having a mental health crisis can be rapidly assessed, ideally in the community.
If they attend local Accident and Emergency Departments, we want to ensure their waiting times are minimised.
If they need an inpatient admission, we want to ensure there is a bed available straight away, and when they are clinically ready for discharge from hospital, ensure they have the right support in the community to enable that discharge to happen quickly and safely.
Patient flow involves the clinical care, physical resources and internal systems needed to get service users from the point of referral/admission to the point of discharge/transfer, ensuring comprehensive high-quality clinical treatment, care and support is offered.
The aim of the Patient Flow Programme is, by July 2021, to achieve bed occupancy of 85%, reduce our length of stay for acute beds to 32 days and eliminate the need for out-of-area placements.
The Trust current status – We have seen a gradual reduction in bed occupancy in 2020, with it dropping 90% after the summer of 2020. Our length of stay for 2019/20 was 41 days and the Patient Flow programme aims to reduce this further, through a series of workstreams. A programme of activities and projects are underway to help achieve our aim, including:
• Pilot of enhanced OT/psychology input on acute wards
• Male psychiatric inpatient care unit QI project to reduce internal referrals
• Developing standard operating procedures in the acute pathway to reduce variation
• A Consultant Lead for patient flow has been appointed in July 2020
• Collaboration with a third sector organisation to enhance the discharge team
Identified areas for improvement • Eliminating long waits in A&E
• Reducing inappropriately long lengths of inpatient stay
• Reducing re-admission rates and patients with high numbers of admissions to acute inpatient care
What we have achieved
Work to improve patient flow continues; the MADE (Multi Agency Discharge Events) are now business as usual and bring together the acute staff, community teams, local authorities and CCG’ (Clinical Commissioning Groups) to help with discharging patients from our wards. This multi-agency work has helped to reduce the number of long stayers onwards, and also the length of time these patients stay on the wards.
The reduction in the number of long stayers was maintained and the work supporting frequently-admitted patients, which paused at the beginning of the Covid-19 period is now recommencing
The next key areas of focus are on supporting frequently-presenting patients, the early identification of deteriorating patients and
alternatives to admissions (where clinically appropriate).
The projects to address these key areas of focus are being undertaken with a QI (Quality Improvement) methodology and see the Delivery Improvement team working alongside the QI team to support front line clinical staff and managers.
Risk stratification of patients
The work to improve patient flow changed emphasis during the height of the pandemic, with attention switched to managing the changing demand on C&I’s acute wards and a focus on discharging and freeing up beds.
Ways of working changed during this period; a Mental Health Assessment Centre was set up divert activity away from acute trusts’ emergency departments. This was well-received and a business case has been submitted to make this more permanent. The discharge team focused on all discharges, not just those without a care co-ordinator and this increased discharges at the beginning of the COVID-19 period.
Crisis Houses took step-down patients rather than just trying to prevent admissions, which helped improve discharges. All projects relating to patient flow and experience are monitored and reviewed in the monthly patient flow meeting, which reports into the Clinical Strategy Programme Board.
Description of the quality issue and rationale for prioritising
• The Trust prioritises integrating physical health and mental health care and has made significant progress in this area as described above
• The revised Physical Health Screening Tool (PHST) is now accessible on our electronic patient record system (Carenotes)
• While there has been an increase in the number of patients being screened and treated, this remains a Trust priority.
• The appointment of a physical health lead is significantly improving systems, policies and processes to ensure physical health care is routinely and consistently assessed and monitored.
• In 2019/20 the Trust further increased use of data to improve the quality of care delivery and outcomes for service users
• The Integrated Practice Unit (IPU) continues to develop structured services for the seriously mentally ill (SMI) population in partnership with primary care and other agencies, with a focus on chronic disease management.
• The IPU will capture additional intelligence to further understand morbidity and mortality rates and interventions offered
The Trust developed its first dedicated Physical Health Lead in 2018. Key outcomes from this role were:
• Embedding the National Early Warning
Score (NEWS) that determines the degree of illness of a patient. The development and implementation of medical devices competencies
• Review and development of the physical health screening tool
• Further implementation and development of smoking cessation policy and practice
• Review and development of physical health policy and clinical protocols, including the management of Venous Thrombosis
inpatient services as part of the Trust’s smoking cessation protocol
Identified areas for improvements
• Implement the clinical dashboard to improve the governance of physical health interventions, including screening / assessment and signposting to treatment options
• Continued training of staff to ensure required competence is supported and monitored
• Improved use of data to improve practice and outcomes
• Further alignment of the Integrated Practice Unit providing physical health interventions for the seriously mental ill population with the Trust’s broader physical health agenda
What we have achieved:
Training to promote understanding of, and be able to use, the physical health dashboard is underway and a presentation took place at the Executive Seminar in February 2020. In the meantime, the dashboard continues to be promoted and Divisions are being supported to access physical health screening data to support practice and improved screening performance, currently provided in a report format. The physical health team continue in partnership with IT to improve methodologies for capturing physical health data, for both screening and successive interventions.
Monthly Physical Health incident data will be reported to Divisional Performance Meetings via the Physical Health and Nutrition Group. Trends, themes and learning will then be cascaded.
The NEWS2 is now digitally available and will be piloted on Dunkley and Rosewood wards before making it available Trust wide early in 2020. NEWS2 training is now incorporated into the ILS/CPR training with our new provider.
The physical health team are represented at the Pan London Physical Health Network and have extensively contributed to the new standards. The physical health team are also contributing to developing the Trust Clinical Strategy led by the Medical Director.
Next steps/future challenges
• Review methodology for CQUIN data collection; to include the process for validation
• Weekly monitoring of completeness of data capture through automated reports and regular audits.
• Development of training for patient-facing staff, level 1 & 2 Smoking /Alcohol
• Launch Physical Health Dashboard and associated training
Numbers of Physical Health Assessment undertaken April 2019 to Mar 2020
Division Number of PH Screening Tool recorded
Acute Community Mental Health Recovery & Rehabilitation Services for Ageing & Mental Health Substance Misuse & Forensics Not Recorded 1305 53 917 425 1 83
How were these priorities monitored to ensure achievement?
The quality priorities for 2019/20 were monitored via our governance framework within the Trust. Each Divisional Quality/ Governance Forum monitors activities for each priority at operational level. The overview of the achievement of these was through the Divisional leadership arrangements with oversight being monitored through the Quality and Safety
Programme Board chaired by the Director of Nursing and Quality.
The overall assurance for the achievement of the quality priorities was assured through the Quality Committee which is a sub-committee of the Trust Board. Any risks to the achievement of the quality priorities will be reported via the divisional and corporate governance arrangements within the Trust.
QUALITY IMPROVEMENT
CQC report November 2019
Staff had been engaged in various ways to learn, improve and innovate and were given time to do this in their day to day roles. The Trust was committed to delivering a Quality Improvement (QI) programme and had invested in this across the organisation. The QI programme had flourished since the last inspection and was well embedded across the trust
Quality Priorities and Improvement
The development of Quality Improvement methodology (QI) has been part of the C&I strategy since 2016, aiming to develop a culture of continuous improvement, with strong frontline service user and carer involvement in improvement work at the Trust. A QI team provides training in QI and supports the improvement work across the organisation
The QI approach continuous to be further embedded in the Trust culture, with wider training of staff and the methodology has been incorporated into divisional business and quality agendas.
A number Quality Improvement projects led by frontline services aligned with the Quality Priorities 1-9.
Acute Wards Violence and Aggression Reduction Collaborative

Acute ward Coral began a QI project on reducing violence and aggression in September 2018, which has seen impressive reductions in incidents with physical violence down by 83% and verbal aggression down by 64%.
We know that safety huddles are an effective way to reduce violence. When we launched the
Violence & Aggression Reduction Collaborative, teams implementing Safety Huddles first before moving on to focusing on other causes of violence.
The collaborative gives teams a chance to reflect together about what has been working well and learn from each other how to overcome problems they have faced along the way.
QI projects included
• Improving care plans and compassionate care using life story on Garnet Ward, an older adult ward
• For 100% service users to have their dual diagnosis needs recorded in their care plans in six months
• For service users on Malachite ward to know what a care plan is, be aware of its contents and satisfied that their needs have been identified.
• Improving crisis care plans in North Camden
R&R
• Improving the efficiency of compiling and implementing a treatment plan informed by extended medication history on acute wards.
• Improving staff awareness and skill of minimising risk of falls.
• Development of a clear, safe and effective discharge protocol for clients within cluster 11 from secondary care to primary care,
South Camden Recovery Team.
• Improving informal carers identification in the personality disorder service
• Implementing a
‘Leaving Summary’ at the Camden
Acute Day Unit.
Camden Acute Day Unit
After implementation of new leaving summary days between day of discharge and discharge summary being sent to GP reduced to a range of 0-10 days, with a mean of 2.9 days)
25
20
Mean no. of days between discharge and summary production
15
10
5
0
12 34 56 78 91 01 11 2 Week 1-6: Before new summary 7-12: After new summary
Surveys from team members working on QI projects suggest that they can experience better team working, an increase in psychological safety and an increase in confidence and pride. Taking part in QI work can therefore, in itself, improve wellbeing
Also, the QI team have supported several projects that had the explicit aim to improve wellbeing of the teams including several separate projects in iCope.
Priority 4 Building a just and learning culture
A QI project is focusing on decreasing the likelihood of BAME staff going through formal disciplinary procedures across the Trust. Key change ideas have included appointing a WRES lead, reviewing the disciplinary policy, using data from pan London Disciplinary procedure analysis, creating a poster on micro aggression and BAME staff career journey. BAME staff have been offered coaching and ‘Unconscious Bias training’ is available for all trust staff.
Quality Improvement Hub Strategy
By co-producing QI projects with service users and their families, we will make improvements that are important to them and that align with the wider healthcare service they experience. Involvement with a ‘little i’ means getting service users’ ideas and feedback at certain stages of a project. Involvement with a ‘bit I’ means that service users are a fundamental part of the team throughout the project. In partnership with service users and carers the QI Hub aims to:
Projects with Service User Involvement (2019)
40
30
20
10
0
Build Co-production 2022-2024
• Encourage staff to use their lived experience.
• Encourage staff to ‘refer’ to QI coproduction as a treatment option.
• Encourage teams to coproduce solely with people who have used their services within the last 6 months.
• Encourage staff to take a lead for coproduction in their team.
Build the Processes 2020-2021
• Co-produce guidelines on how to match service users to QI projects according to their strengths.
• Attend service user forums to understand and offer the QI support people need.
• Offer co-produced QI training from the QI Hub, Recovery College and Trust induction.
• Create pamphlet for service users describing benefits of QI and different roles and support available.
• Develop a QI induction for service users.
• Nominate a QI service user lead who helps to make judgements on which projects can be registered.
• Gain service users’ feedback on quality of QI projects in their service during project and at debrief.
• Measure impact of service user involvement on staff wellbeing.
• Focus on how Co-production can Help People Recover from Mental Illness 2018-2019
• Celebrate ‘early wins’ in coproduction.
• Create a service user agreement template.
• Monitor which teams are paying service users for their involvement in QI.
• Partner with Service User Involvement Facilitator to share QI projects with service users.
• Invite service user to QI Hub meetings where appropriate.
• Create a service user involvement page in QI resource pack.
• Encourage project teams to involve service users. Discuss at QI training and share examples of how they have been fundamental to projects.
• Agree on and write guidance for payment of service users in QI projects and inform project teams.
• Develop a tool to measure the level of co-production in projects and services.
Priority 7: Improve Dementia Care
Several QI projects are underway in the memory service focusing on ensuring a timely and safe service for service users. These include reducing the length of time between referral and diagnosis, improving Client Satisfaction Questionnaire feedback, improving the multidisciplinary disciplinary team meeting and improving dementia navigators’ clinical time management. One project has been completed which has focused on ‘Remodelling the follow-up procedures of patients with mild cognitive impairment.’ This has led to 87 fewer overdue reviews.
Priority 8: Patient Flow
The QI team is working closely with the Patient Flow and Experience group on the projects described earlier in the report and this will be a priority workstream for the QI team in the coming year. Current projects include work on reducing referrals to our psychiatric inpatient ward through outreach work, and a weekly “Big Room” event that brings team members together from across community and acute teams to work out how to improve the pathway across all quality dimensions.
Priority 9: Improving health care: Examples of projects
Several services developed physical health focused projects mapping out their own process to understand where changes need to be made then either using the Trust physical health dashboard or devising their own method of measurement so that they can track the effectiveness of the change they are implementing.
For example, the Assertive Outreach Team have focused on training staff how to complete the health check and using the MDT meeting to problem solve booking in difficult-to-engage service users.
Services that worked on improving physical heath through QI projects include:
• Complex Depression, Anxiety and
Trauma team
• South Camden R&R
• Islington Learning Disabilities Partnership
• Sapphire ward
• Islington Early Intervention Service.
• Assertive Outreach Team
• Ruby Ward developing a strong organisational culture of continuous improvement.
• Planning for the development of a Quality
Management System (QMS), bringing together quality planning and QI. The Board agreed to pursue this approach in 2019
• The QI teams, with Board approval, have already begun work on integration with project managers and the C&I
Organisational Development (OD) team.
• The QI team continued to support many projects across the organisation and delivered training in QI methodology, as well as working more closely with divisions on their improvement priorities.
Some important milestones in the QI journey 2019/2020
• In 2019/2020 the Executive agreed to strengthen the Quality Improvement team including creating a Head of QI position.
The ambition was to further support
March 2020, more than 500 staff had taken up the offer of QI training. There were 131 registered QI projects on our online platform, and these projects which will also be available on the QI website by the end of 2020.
The 2019 Staff Survey shows that nearly two thirds of the workforce feel able to make improvements happen in their area of work, which is at the higher end of national benchmarking. This is one of the main outcome measures for the QI programme
Recruitment to the enhanced QI team model was delayed by the pandemic and much of the QI work was paused or disrupted in the beginning of 2020 to support the organisation through the early phases of the pandemic, but the QI team have now re-started and adapted its work, continuing to focus on supporting frontline staff and service users lead improvement work.
Next steps on the QI Journey
• Support delivery of the Clinical Strategy and 2020/21 Quality Priorities • Continue to build QI capability and capacity and celebrate the contribution of service users, carers and frontline teams
Develop a Quality Management System that creates local, divisional and organisational learning systems and better co-ordinates the work between governance, improvement and transformation teams within the organisation
The QI team and their work are accountable to and supported by the Medical Director and the Quality & Safety Programme Board.
“C&I staff along with service-users know at times smoking becomes a personal thinking friend, a comfort zone, especially at times of feeling lonely, isolated, pressured, confused and the thinking of so many thoughts. Do we really believe that smoking helsp us with our mental health wellbeing? But together we can STOP is being an unhealthy controlling HABIT by way of the individual Cessation Plan.” Paul Ware, Service User Governor

STATEMENTS OF ASSURANCE FROM THE BOARD
During 2019-20, Camden and Islington NHS Foundation Trust provided and/or sub-contracted the following NHS services across approximately 30 Trust sites in Camden, Islington and Kingston; together with presence in GP practices for IAPT and practice-based mental health in all three local authorities
Camden and Islington NHS Foundation Trust Divisions
• Acute Adult Mental Health
• Community Adult Mental Health
• Services for Ageing and Mental Health(SAMH)
• Recovery and Rehabilitation
• Substance Misuse Services
Camden and Islington NHS Foundation Trust has reviewed all the data available to it on the quality of care in each of these NHS services.
The income generated by the NHS services reviewed in 2019/20 represents 100% of the total income generated from the provision of NHS services by Camden and Islington NHS Foundation Trust for 2019/20’
AN OVERVIEW OF THE QUALITY OF CARE OFFERED BY THE NHS FOUNDATION TRUST: KEY INDICATORS OF SAFETY, EFFECTIVENESS AND PATIENT EXPERIENCE
Patient Safety
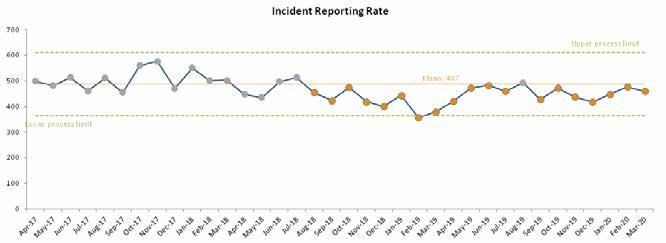
The Trust uses Datix to report incidents. All staff are provided with an introduction to incident reporting at induction. There are online resources to support staff with incident reporting and management. The incident reporting policy was updated in June 2019 and included clarification for staff and managers of the Trust’s minimum standards for incident reporting and management. 5467 incidents were reported over the year. The Trust continues to promote an open reporting culture. The Trust has maintained a steady rate of incident reporting over the year,however there has been an overall decline in the numbers of incidents reported over the past two years. To correspond with this trend, there has been an even more dramatic decrease over the past two years in the numbers of incidents resulting in harm
Incidents all categories by level of harm:

Patient safety incidents and the percentage that resulted in severe harm or death
The proportion of incidents resulting in no/low harm has remained consistently high over the past three years, accounting for on average 96% of all incidents reported. This supports evidence of a good safety culture within the organisation, indicating staff willingness to continue to report low level issues and not just the more serious incidents. The proportion of incidents resulting in severe harm has remained consistently low over the past three years, accounting for on average 0.5% of all incidents reported.
Risk management
The Trust has an established process for managing risk and detecting and responding to quality concerns. The risk management strategy is reviewed annually, with the Audit and Risk Committee having oversight of this process.
Each Division has a risk register that is monitored regularly to ensure risks are being managed. The most recent internal audit of risk management concluded that the Trust has a well-designed process for the addition and review of divisional risks. Over the past two years this process has been enhanced through the establishment of risk registers for corporate teams and the migration of risk data to the Datix online system. A Divisional and Corporate Department Risk Scrutiny Group (DRSG) is established, attended by each of the divisions and heads of corporate departments. This group meets on a quarterly basis to review each of the divisional and departmental risk registers in parallel. Following this, an Executive Risk Scrutiny Group is held on a quarterly basis to review all risks scored 15 and above and is attended by Executive Directors. This process supports consistency of reporting and risk-scoring, as well as ensuring appropriate challenge is applied across all risk registers.
Through this process, high level risks are routinely escalated and reported to the Audit and Risk Committee and Board. The Audit and
Risk Committee also undertakes regular “deep dive” analysis into key areas of risk concern, to enable scrutiny of risk trajectories and whether appropriate mitigating actions have been identified to manage the risk.
In addition, the Board Assurance Framework (BAF) provides the Board with a clear and comprehensive method for the effective and focused management of the strategic risks that could affect the delivery of its principal objectives and strategic priorities. The BAF is reviewed quarterly and a narrative report to the Audit and Risk Committee provides assurance of the continued risk management processes and to highlight any concerns or areas of progress.
Incidents (all categories) Apr19 May19 Jun19 Jul19 Aug19 Sep19 Oct19 Nov19 Dec19 Jan20 Feb20
Mar20
No harm 354 409 409 397 444 377 420 385 361 404 417 392 Low harm 57 51 56 42 37 35 42 38 45 35 47 55 Moderate harm 9 10 15 18 10 13 8 14 10 8 11 9 Severe harm 0 2 3 3 1 3 2 1 2 1 2 3 or death

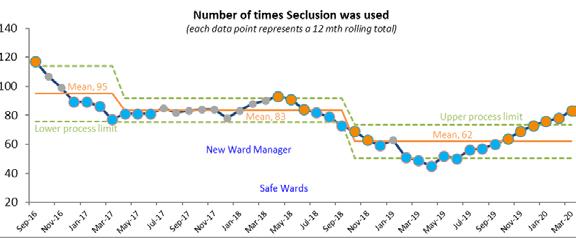
Seclusion:
The use of seclusion continues to decline and demonstrates the Trust is achieving least restrictive practice in this area. In May 2019, another White Ribbon training event was held entitled ‘Sexual Safety and the launch of the Pathfinder Project: Embedding Trauma-informed Practice’. The day included the launch of the Sexual Safety Policy and Poster.
Falls:
There is a Falls Prevention Policy in place to support staff with reporting falls. There is a Falls Lead and a Falls Group where falls are reviewed.

Number of falls incidents by harm
(Trust 24 Hour Bedded Units & Day Centres)
20
15
10
5
0
Apr-18 May-18 Jun-18 Jul-18 Aug-18 Sep-18 Oct-18 Nov-18 Dec-18 Jan-19 Feb-19 Mar-19 Apr-19 May-19 Jun-19 Jul-19 Aug-19 Sep-19 Oct-19 Nov-19 Dec-19 Jan-20 Feb-20 Mar-20 No Harm Low Harm Moderate Harm Severe Harm or Death
PATIENT EXPERIENCE INDICATORS
We continue to meet the 20% response rate for our Family & Friends Test and patients recommending their service have also remained above 90%. The Trust is currently reviewing how to improve response rates; a survey is being carried out to identify issues and best practice relating to obtaining and inputting the information on to the Trust system (Meridian).
FFT 2018/19 – 2019/20
Financial Year 2018/19 2019/20
Quarter Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 FFT Responses 951 670 578 454 448 878 511 501 % Recommended 82% 90% 92% 93% 91% 87% 95% 92%
Community Mental Health Service User Survey
Survey Year 2016 2017 2018 2019
Overall Experience Score 68% 72% 69% 70%
Every year, the Trust participates in the National Community Mental Health Survey. The purpose of the survey is to understand, monitor and improve service users’ experience of NHS community mental health service. Data is used by the CQC and other organizations for assessment, improvement, governance and regulatory purposes.
This year, a sample of 1,250 CPA and Non-CPA community mental health service users seen by someone face-to-face at the trust between 1 September and 30 November 2019 was generated at random. The survey was carried out from February to June this year.
Results
• With 255 surveys returned completed, the
Trust had a response rate of 21%, down from 24% in 2019.
• The Trust average score has improved to 70 from 66 in 2019.
• The Trust scored in the top 20% of Trusts on 11 questions, the bottom 20% of Trusts on 0 questions. The Trust scored in the middle 60% on the remaining 17 questions.
• Four questions scored significantly better than 2019 and one question significantly worse.
• C&I’s average score was higher than the
London average and better than six of the nine other Trusts
What we are doing well (the top 20% of Trusts)
• Seeing people often enough and service users feeling staff understand how mental health needs affect other areas of life
• joint decision making
• knowing who to contact in a crisis
• understanding medicine and side effects
• organizing care and services well and support with physical health needs; financial advice or benefits; finding or keeping work or joining a group/ taking part in an activity
Where we are getting better compared with last year (four questions where the Trust scored significantly better than 2019)
• Explaining treatments and therapies in an understandable way and
• Joint decision making and involving service users in deciding what treatments or therapies to use?
• Providing NHS therapies that have helped
Identified areas for improvement
• Asking people for their views on the quality of care they have received (1 question where the Trust scored significantly worse than 2019)
• Holding a specific meeting to discuss how your care is working at least once a year (low score compared with other London
Trusts)
How we will improve
• We know having a strong response to the survey is important to get the most meaningful data. We will ensure service users are encouraged and supported to complete the survey in 2021
• We will continue our work with Leeds
Beckett University on our Patient Experience
Strategy which will include regular experience feedback mechanisms
We will work with teams to ensure all service users have an annual review.
COMPLAINTS –
Numbers and Themes Arising
The Trust received 138 formal complaints this year, so almost the same as in the previous business year when 136 were received. In addition, 219 concerns received via the Advice and Complaints Service were resolved informally, (against 235 in the previous year). Of course, this only represents a proportion of the issues that staff resolve directly with service users daily. The Acute Division received the most complaints, followed by Community Mental Health. Complaint numbers in substance misuse services and services for older people remain low.
Although complaint numbers appear fairly consistent year-on-year, the feeling is that they are increasing in complexity – number of issues raised, scope of issues raised and the difficulty of trying to resolve issues where resolution may already have been attempted without success by the time that formal process begins.
The complaints received cover a wide variety of issues often quite specific to the individual’s care or experience and it is not always possible to identify common themes. However, the following issues have been noted to recur this year:
In Community Mental Health Division, some services continue to have long waiting lists due to mismatch between demand for the service and available resources. Also noted in this Division is the challenge of providing support to a cohort of people who, while having significant mental health needs, do not meet the criteria for any services that the Trust is currently able to offer. There are ongoing discussions with our commissioners as to how to address both these issues.
Across the Trust, and particularly in the Acute Division, issues regarding communication with service users and their carers/relatives are noted. In Recovery and Rehabilitation services, managing both service user and carer expectations about the level of input that the Trust can provide remains challenging.
Learning from Complaints
This business year, around 59% of complaints responded to, were either fully or partially upheld, which is a very similar figure to the previous business year. Generally, we see around half of all complaints being upheld. It may be that as we continue to get better at resolving concerns informally, only the more serious and valid matters are going through formal process. The Trust is committed to using the feedback we receive through complaints to improve our services. All teams have a regular slot at their team meetings where any complaints can be discussed and reflected on.
Complaints which are either partially or fully upheld, will have an action plan to ensure that recommendations are implemented. Action plans are discussed and reviewed at divisional quality forums.
Below are some examples of improvements made in the last year as the result of feedback from complaints:
• Although respecting patients’ wishes and their confidentiality lies at the heart of our
care planning, there is often a delicate and dynamic balance between respecting these and also ensuring that all appropriate partners in care, (such as the community team and the family in this case), are appropriately informed and able to contribute to the care the patient receives.
• The Trust will aim to ensure that our soft service provider who is responsible for catering, is routinely invited to the ward community meetings and that feedback from these is documented and circulated.
• A renewed focus on search training to reduce the possibility of items being brought onto the ward which can be used to self-harm.
• A review of the audio equipment used within iCope to determine if there is any opportunity to improve the background sound-cancelling quality of existing equipment (e.g. improved microphones on headsets) or to make changes to the environment to reduce the impact of background noise in shared offices. Also, regular reminders to go out to all iCope staff members encouraging them to be mindful of the noise levels in the room when colleagues are on the phone.
• All clients with booked telephone assessments to receive an appointment letter or some acknowledgement of their appointment in good time before their telephone assessment. The appointment/ acknowledgement letter should contain information about what to expect from a telephone assessment and what to do if individuals need urgent crisis support for mental health difficulties while waiting to be seen.
Meeting Deadlines
The Trust target is for 80% or more of complaints to be responded to within the timeframe. This target has remained challenging this year, with around 60% of complaints meeting deadlines*. We have been successful in making short term improvements but sustaining improvement longer term remains difficult.
Meetings have taken place with Divisional Leads to discuss these challenges and possible solutions. Investigator resource is an ongoing issue for the divisions, especially those that receive greater numbers of complaints. A review of the complaints policy has been undertaken, specifically with a view to ensuring that divisional management has clear oversight of their open complaints and of any obstacles to completion that managers are dealing with. Additional management resource was also brought into the Complaints Team on a temporary basis, to support process improvement.
The Complaints Team continues to offer support to investigators on an individual basis and have also provided group training to staff.
We have continued to encourage prompt informal resolution of concerns at team level wherever possible.
Survey Year
Number of complaints 2016/ 17 2017/ 18 2018/ 19 2019/ 20
172 127 136 138
Clinical effectiveness
National data indicates that bed occupancy in acute mental health NHS facilities is often close to 100%. As an organisation, we have achieved an average of 96% each year over the past two years. Although this figure is high, it has allowed us to ensure service users are admitted to their local services, keeping links with family, friends and the local community. Our organisational aim is to reduce bed occupancy to 85% or below over the next 12 months.
Financial Year 2018/19 2019/20
Quarter Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Bed Occupancy 97.1% 98.1% 96.5% 95.6% 95.3% 97.0% 95.6% 93%
Average LOS for Acute Wards:
We are aware that a person’s length of stay (LOS) in our inpatient services is a key driver in inpatient bed occupancy rates. Predicting length of stay for a person can be a challenge, as multiple factors need to be considered; these include the person’s primary diagnosis, physical health, any substance misuse concerns, housing, relationship and employment status, functional and social impairment. Other organisational factors could be the persons experiences whilst in the inpatient services and the therapeutic environment of the ward. The Trust completed a focused piece of work on expediting discharges with the involvement of both the Discharge facilitation and Home Treatment teams. The Trust has worked proactively, establishing an expected date of discharge soon after admission to ensure that service users are receiving safe and effective care, shaping their journey to make every day count and giving tangible hope at a time when they are acutely unwell. Having this expected date of discharge facilitates shared decisionmaking conversations with the service user, family and carers and supports the wider patient flow and bed management systems.
The NHS Mental Health Improvement Plan indicates that the average time for a person to be in an inpatient service is 32 days. For 201920, our average length of stay was 41 days.
Acute ALOS excl leave
78
UCL
68
58
48
38
28
18
LCL
Apr-18 May-18 Jun-18 Jul-18 Aug-18 Sep-18 Oct-18 Mean 45
Nov-18 Dec-18 Jan-19 Feb-19 Mar-19 Apr-19 May-19 Jun-19 Jul-19 Aug-19 Sep-19 Oct-19 Nov-19 Dec-19 Jan-20 Feb-20 Mar-20
Emergency Psychiatric Re-admission (30 days) Area Target 2019/20 Q1 Q2 Q3 Q4
Emergency Psychiatric Re-admission (90 days) Area Target 2019/20 Q1 Q2 Q3 Q4
Trust 8% 10.6% 6.8% 10.0% 8.0%
Trust 15% 18.5% 20.8% 20.0% 19.0%
As an organisation, we have undertaken a focused piece of work to identify those people who use our inpatient services on a frequent basis i.e. three or more admissions in three years This piece of work has led to the formulation of advanced care and crisis plans, which are multi agency led, to meet the needs of these identified service users. This work also includes several projects to help reduce re-admissions at both 30 and 90 days and the early signs are this work is having a positive impact It will be supported, in the future, by the enhanced Crisis Team services, peer-support workers and strengthened community services which aim to reduce re-admissions into hospital through intensive community support.





