60 minute read
Data quality
The Data Quality Policy has been updated during the year, and with the reestablishment of Data Quality Improvement Group (DQIG), the Information ,eam – along with the Data Warehouse and Clinical Applications teams – continue to work closely to monitor and improve the quality of data across the Trust. This includes identifying root causes of several data quality issues and is in the process of embedding these within the recording process, working closely with the Divisions and the Business Performance Teams while addressing the data quality. As part of this process, several new data quality dashboards and reports have been built and are being used widely across the Trust by different teams.
The Information Team is conducting ongoing work to continue improving the data quality through collaborative working with Operational/ Clinical teams and Contracts and Costing teams.
Advertisement
Some of the data quality improvement activities include:
• A new version (v4) of Mental Health
Services Data Sets (MHSDS) submission criteria has been implemented. MHSDS and improving access to psychological therapies (IAPT) submissions provide a wide range of quantitative and qualitative information about the services that the Trust offers, and data quality reports are generated to identify any anomalies.
• The introduction of data quality reports and investigations across data quality has resulted in reduction of the number of data quality issues pertaining to MHSDS submission (from around 15,000 to 1500 in the last 8 months). The latest NHS Digital published data quality maturity index (DQMI) score for the Trust is 97.4% (February 2020), compared to 85.5 in April 2019.
• The Data Quality Improvement Group meetings are held monthly currently focussing on improving data quality across the Trust. All the relevant stakeholders are included in this group ranging from Finance,
Contracts, Clinical Applications, Costing, etc., to ensure all data quality issues are captured and addressed effectively in a timely manner.
• The Trust is promoting a data driven culture where several dashboards, including data quality reports, are being built by the
Information Team to ensure data is available to the Trust teams on a near real-time basis to monitor their team performance and data quality.
Information Governance Toolkit
Information Governance (IG) is about how NHS and social care organisations and individuals handle information.
The Information Governance Toolkit is a performance tool produced by NHS Digital. It draws together the regulations and central guidance related to information governance and presents them as one set of information governance requirements. NHSI have stated that the 2018/19 assessments are “rolling standards”, so will be assessed based on the Trust’s ability to regularly attain, update and publish defined standards on the NHSI toolkit website.
The Trust continually reviews its information governance framework to ensure all personal and medical information is managed, handled and disclosed in accordance with the law and best practice. The Trust is also in the process of ensuring General Data Protection Regulation compliance and has updated its fair processing notice.
In addition, we attach great importance to training, data quality and clinical records management. As a result, we have seen improvements in several aspects across the Trust.
Improving Information Governance is a key NHS priority. This is reflected in national standards set out in the Data Security and Protection Toolkit (DSPT) which the Trust is required to complete and submit before end of March 2020 for this reporting period.
In March 2019, the Trust’s status for DSPT was standards met. The next DSPT will be submitted before 31 March 2020 and the trust is aiming to achieve standard met again.
Completion of DSPT demonstrates that the organisation is compliant with the following: • Compliance with the expected data security standards for health and social care for holding, processing or sharing personal data.
• Readiness to access secure health and care digital methods of information sharing, such as NHSmail and Summary Care Records
• Good data security to the CQC as part of the Key lines of Enquiry (KLOEs).
The Data Security and Protection Toolkit is an online self-assessment tool that enables organisations to measure and publish their performance against the National Data Guardian’s ten data security standards.
The Trust is measuring performance against the National Data Guardian’s 10 data security standards. These are:
1. Personal Confidential Data
2. Staff Responsibilities
3. Training
4. Managing Data Access
5. Process Reviews
6. Responding to incidents
7. Continuity Planning
8. Unsupported systems
9. IT Protection
In addition, the Trust has identified Information Asset Owners (IAO) to embed effective information risk management activities across the Trust by embedding these responsibilities in day-to-day activities. Project has been initiated to update the Information Asset register which will then be inputted into the Information Asset Management (IAM) tool. The IAM tool will be intuitive for IAOs to use and regularly update their assets and report any risks to the SIRO.
Cyber Security
A cyber security programme is in place and progressing well with five workstreams:
Leadership and Governance: The Information asset management work is vital to information flow mapping and risk management. The Information Asset Management and Compliance Manager is in post and will deliver the Information Asset Management programme within 6 months working with Asset Owners across the Trust, set up support working groups and ensure training and awareness for all relevant staff is completed.
Operational: The email system has now been migrated to 365, the organisation currently have both NHS mail and CANDI Mail. The plan is for NHS Mail to be switched off and CANDI email will be used as the secure email domain. This is currently in progress. Communication: Office 365 training has commenced, and Yammer was used to communicate the courses to staff. Yammer is a collaborative tool. There are 18 Yammer groups set up and an IG Yammer working group. A digital newsletter is sent on a regular basis which features Information governance and cyber security updates.
Clinical Workstream: The recruitment of Chief Nursing Information Officer (CNIO) role has been in the job matching process. The cyber security clinical work will be well supported following recruitment to this post.
Procurement: Despite the contract amnesty the contracts team has made really good progress and 69% of the contracts over 50K have been logged. There is further work to be done to review contracts which are processing personal information. Both Contracts and Procurement are working collaboratively on this.
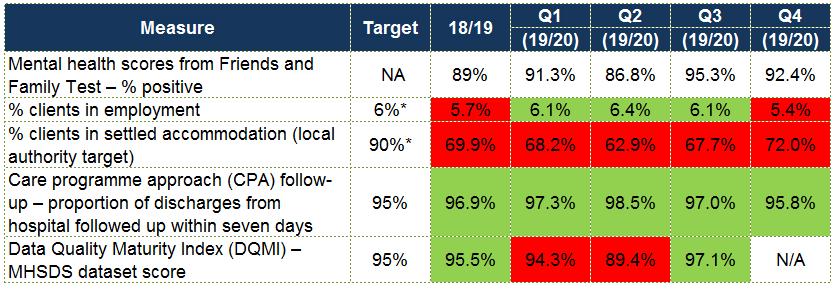
REPORTING AGAINST CORE INDICATORS
Since 2012/13, NHS foundation trusts have been required to report performance against a core set of indicators using data made available to the trust by NHS Digital.
7 Day Follow-Up CPA inpatient discharges followed up within 7 days (Face to face and telephone) 97.3% 98.5% 96.1% 95.8%
Gatekeeping Proportion of admissions gatekept by Crisis Resolution Teams 97.9% 98.4% 98.7% 99.1%
Q1 Q2 Q3 Q4
Measure
Mental health scores from Friends and Family Test – % positive
% clients in employment
% clients in settled accommodation (local authority target) Care programme approach (CPA) follow-up – proportion of discharges from hospital followed up within seven days Data Quality Maturity Index (DQMI) – MHSDS dataset score
Target 18/19 Q1 Q2 Q3
(19/20) (19/20) (19/20)
NA 89% 91.5% 86.7% 95.6%
6%* 5.7% 6.1% 6.4% 6.1%
90% 69.9% 68.2% 62.9% 67.7%
95% 96.9% 97.3% 98.5% 97.0%
95% 95.5% 94.3% 89.4% 97.4% (provisional)
Proportion of people experiencing a first episode of psychosis treated with a NICE approved care package within two weeks of referral
Target 18/19 Apr-19 May-19 Jun-19 Jul-19 Aug-19 Sep-19 Oct-19 Nov-19 Dec-19 Jan-20
People with a first episode of psychosis begin treatment with a NICE recommended care package within two weeks of referral 56% 75% 81% 87% 75% 87% 87% 94% 94% 89% 91% Not published
Patient Experience of Community Mental Health 2019:
The Annual Community Survey results were published in November 2019 and showed the Trust had made several improvements on last year’s results. This survey is published by CQC and is the national survey that all mental health trusts participate in.
The survey report uses standardised data to generate a score for each question asking the respondent to rate the service they received.
This score is then used to benchmark the Trust’s position in relation to all other responding organisations. Most of our scores are in the intermediate 60% range and some are in the top 20% of all trusts surveyed;
Summary of results
• There is a general improvement in results since 2018.
• Most scores are in the intermediate range.
• Six scores are in the top performing category.
• Just four scores remain in the bottom category.
• NHS Therapies needs urgent attention.
• The overall rating of care has improved.
• But do remember – sample sizes are small, and some changes can be hard to explain.
Actions CARE AND TREATMENT
Continue excellent work on ensuring service users are seen often enough for their needs.
ORGANISING CARE
Seek to understand why some service users don’t feel their care is organised effectively. Drill down into data.
REVIEWING CARE
Continue excellent work on ensuring all service users are being offered a formal review meeting and that this is made explicit.
CRISIS CARE
Work to ensure service users know who to contact when in crisis. Investigate the range and level of support provided by the out of hours service.
NHS THERAPIES
Scores have dropped significantly. Seek to understand why: focus on ensuring service users are involved in decisions.
SUPPORT AND WELLBEING
There are some positive results here. Focus on involving family members and signposting service users to sources of peer support.
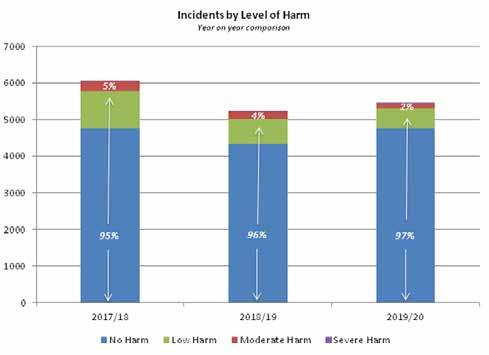
Patient safety incidents and the percentage that resulted in severe harm or death
Camden and Islington consider the data to be as described due to the following reasons - the data for this indicator is derived from Datix our internal patient safety software. The majority between 72 – 85% of patient safety incidents reported result in no harm and only a small fraction (less than 1%) of patient safety incidents resulted in severe harm. The Trust is committed to learning from serious incidents.
The proportion of incidents resulting in no/low harm has remained consistently high over the past three years, accounting for, on average, 96% of all incidents reported. This supports evidence of a good safety culture within the organisation, indicating staff’s willingness to continue to report low level issues and not just the more serious incidents. The proportion of incidents resulting in severe harm has remained consistently low over the past three years, accounting for on average 0.5% of all incidents reported.
Total Incidents by harm
Risk management
The Trust has an established process for managing risk and detecting, and responding to, quality concerns. The risk management strategy is reviewed annually, with the Audit and Risk Committee having oversight of this process.
Each Division has a risk register that is monitored regularly to ensure risks are being managed. The most recent internal audit of risk management concluded that the Trust has a well-designed process for the addition and review of divisional risks. Over the past two years this process has been enhanced through the establishment of risk registers for corporate teams and the migration of risk data to the Datix online system.
A Divisional and Corporate Department Risk Scrutiny Group (DRSG) is established, attended by each of the Divisions and Heads of Corporate Departments. This group meets on a quarterly basis to review each of the Divisional and Departmental risk registers in parallel. Following this an Executive Risk Scrutiny Group is held on a quarterly basis to review all risks scored 15 and above. Executive Directors attend the meeting.
This process supports consistency of reporting and risk scoring as well as ensuring appropriate challenge is applied across all risk registers.
Through this process high level risks are routinely escalated and reported to the Audit and Risk Committee and Board. The Audit and Risk
Committee also undertakes regular “deep dive” analysis into key areas of risk concern to enable scrutiny of risk trajectories and whether appropriate mitigating actions have been identified to manage the risk.
In addition, the Board Assurance Framework (BAF) provides the Board with a clear and comprehensive method for the effective and focused management of strategic risks that could affect the delivery of its principal objectives and strategic priorities. The BAF is reviewed quarterly and a narrative report to the Audit and Risk Committee provides assurance of the continued risk management processes and highlights any concerns or areas of progress.
COMPLAINTS
Numbers and Themes Arising
The Trust received 132 formal complaints this year, which is similar to the previous business year, when 136 were received. In addition, 185 concerns received via the Advice and Complaints Service were resolved informally (there were 235 in the previous year). Of course, this only represents a proportion of the issues that staff resolve directly with service users daily. * The Acute Division received the most complaints, followed by Community Mental Health. Complaint numbers in substance misuse services and services for older people remain low.
Although complaint numbers appear fairly consistent year-on-year, the feeling is that they are increasing in complexity – that is the number of issues raised, the scope of the issues raised and the difficulty of trying to resolve issues where resolution may already have been attempted without success by the time that formal process begins.
The complaints received cover a wide variety of issues and are often quite specific to the individual’s care or experience; it is not always possible to identify common themes. However, the following issues have been noted to recur this year:
In the Community Mental Health Division, some services continue to have long waiting lists due to a mismatch between demand for the service and available resources. Also noted in this Division is the challenge of providing support to a cohort of people who, whilst having significant mental health needs, do not meet the criteria for any services that the Trust is currently able to offer. There are ongoing discussions with our commissioners as to how to address both these issues.
Across the Trust, and particularly in the Acute Division, issues regarding communication with service users and their carers/relatives are noted. In Recovery and Rehabilitation services, managing both service user and carer expectations about the level of input that the Trust can provide remains challenging.
Learning from Complaints
This business year around 59% of complaints responded to, were either fully or partially upheld, which is a very similar figure to the previous business year. Generally, we see around half of complaints being upheld. It may be that as we continue to get better at resolving concerns informally, only the more serious and valid matters are going through formal process. The Trust is committed to using the feedback we receive through complaints to improve our services. All staff have a regular slot at their team meetings where any complaints can be discussed and reflected on. Complaints which are either partially or fully upheld will have an action plan to ensure that recommendations are implemented. Action plans are discussed and reviewed at divisional quality forums.
Below are some examples of improvements made in the last year as the result of feedback from complaints:
- Although respecting patients’ wishes and their confidentiality lies at the heart of our care planning, there is often a delicate and dynamic balance between respecting these and also ensuring that all appropriate partners in care (such as the community team and the family) are appropriately informed and able to contribute to the care the patient receives.
- The Trust will aim to ensure that our service provider, who is responsible for the catering is routinely invited to the ward community meetings and that feedback from these is documented and circulated.
- A renewed focus on search training to reduce the possibility of items being brought onto the ward which could be used to self-harm.
- A review of the audio equipment used within iCope to determine whether there is any opportunity to improve the background sound-cancelling quality of existing equipment (e.g. improved microphones on headsets) or to make changes to the environment to reduce the impact of background sounds in shared offices. Also, regular reminders to go out to all iCope staff members encouraging them to be mindful of the noise levels in the room when clinicians when colleagues are on the phone.
- All clients with booked telephone assessments to receive an appointment letter or some acknowledgement of their appointment in good time before their telephone assessment. The appointment/ acknowledgement letter should contain information about what to expect from a telephone assessment and what to do if individuals need urgent crisis support for mental health difficulties while waiting to be seen.
Meeting Deadlines
The Trust target is for 80% or more of complaints to be responded to within timeframe. This target has remained challenging this year because of priorities and resources during the pandemic, with around 60% of complaints meeting deadlines. We have been successful in making short-term improvements but sustaining improvement longer-term remains difficult.
Meetings have taken place with Divisional Leads to discuss these challenges and possible solutions. Investigator resource is an ongoing issue for the divisions, especially those that receive greater numbers of complaints. A review of the complaints policy is being undertaken,
specifically with a view to ensuring that divisional management has clear oversight of their open complaints and of any obstacles to completion that managers are dealing with. Additional management resource has also been brought into the complaints team on a temporary basis, to support process improvement.
The Complaints Team continue to offer support to investigators on an individual basis and have also provided group training to staff.
We have continued to encourage prompt informal resolution of concerns at team level wherever possible
Compliments
Whilst we are always conscious of the need to learn and improve where we could have done better, we know that there is a lot of excellent practice within the Trust, and this is reflected in some of the positive feedback that we receive. Here are some examples received by a range of services across the Trust:
• Following a course of CBT, a service user wrote to say that it had transformed his life for the better. He wrote “It is as if a mighty stone of pain and misery has been lifted from my heart.”
• Feedback for the crisis team: the service user was incredibly impressed by the whole service, he reported that everyone was genuine and caring and not at all patronising.
• The crisis call centre was complimented by a caller for responding immediately, professionally and efficiently.
• Thanks to Garnet Ward from the daughter of a service user for their care and kindness towards her father. She said: “He could not have been in a better place.”
NICE Guidelines
The table below provides the details and status of NICE (National Institute for Health and Care Excellence) guidelines and Quality Standards applicable to the Trust.
Guidance
Division Outstanding Baseline assessments Partially Implemented
Acute 0 R&R 0 CMH 0 SAMH 0 SMS 0 Trust 1 Total 1 0 0 0 0 0 5 5
Quality Standards
The table below shows the detail of the Quality Standards that are in progress or baseline assessments that are due to be completed.
Quality Standards
Division Outstanding Baseline assessments Partially Implemented
Acute 0 R&R 0 CMH 0 SAMH 0 SMS 0 Trust 4 Total 4 0 0 0 0 0 2 2
KEY QUALITY INITIATIVES IN 2019/20
Quality Improvement
Measurement for Improvement
the most important single change in the NHS… would be for it to become, more than ever before, a system devoted to continual learning and improvement of patient care, top to bottom and end to end
Berwick Report: “A promise to learn: a commitment to act” (2013)
Overview and Milestones
• 2018/19 marked a significant acceleration of the QI programme with QI work becoming more widespread in teams driven by the establishment of a larger QI teamvIn 2019/2020 the Executive agreed to strengthen the Quality Improvement team including creating a Head of QI position. The ambition was to further support developing a strong organisational culture of continuous improvement.
• A key part of reaching this work lies in the co-creation of a Quality Management
System (QMS), bringing Quality Assurance (QA), Quality Control (QC), Quality Planning (QP) and QI closer together. The Board agreed to pursue this approach in 2019
• The QI team, with Board approval, have already begun work on integration with project managers and the C&I Organisation
Development (OD) team

• The QI team continued to support many projects across the organisation and deliver training in QI methodology as well as work more closely with divisions on their improvement priorities
• Recruitment to the enhanced QI team model was delayed by the Covid pandemic and much of the QI work was paused or disrupted in the beginning of 2020
Engaging, encouraging and inspiring
• Monthly Senior Leadership Team meeting –
QI project presented by team
• Website under development- Will increase the profile of QI at C&I, publish stories about QI work, celebrate achievements and share learning to complement training. This is due to launch shortly
• @candi_QI enabled us to collaborate and share learning with other QI teams and experts across the world.
• Spotlight – the QI Newsletter has been sent out to all staff monthly, updating on QI stories and projects
• QI Celebration - planning had started in
January 2020, but was put on hold due to
COVID
Developing improvement skills
The QI Hub continued to offer a variety of training opportunities to all staff and offered training and skill development to service users and carers
Graph 1. Numbers of attendees to intro to QI/ QI Lab
600
400
200
0
Apr19 May 19 Jun19 Jul-19 Aug 19 Sep 19 Oct19 Nov19 Dec19 Jan20 Feb20 Mar20
Graph 2. Numbers of projects coached
250
200
150
100
50
0
Apr19 May 19 Jun19 Jul-19 Aug 19 Sep 19 Oct19 Nov19 Dec19 Jan20 Feb20 Mar20
Measurement for Improvement
Performance Measures Review Group
The quality of Statistical Process Control (SPC) reporting is critical, leading to a group forming in February to have oversight on the following key issues
• To support the development of one main tool, and present data in a uniform manner
• To agree rules on how data is communicated. For example, confidence when resetting control limits and the language used to describe the charts, including icons and colours
• To review arising performance measures to understand the most appropriate method to visually present data. For example, is an SPC chart suitable, is there a simpler way?
Embedding into daily work
• Membership includes professionals from
Governance, Informatics, HR and the QI hub.
We have worked closely with the OD team to develop a training pathway for all staff at C&I to access QI knowledge and development at all levels.
• Improvement Technician Apprenticeship: 8 staff from grades 5-7 enrolled in Sept 2020

• Managers essentials: 10 managers attended
• Leadership for Improvement: 20 Senior leaders attended the first day in February 2020
Embedding into daily work
Our CQC report said:
Staff had been engaged in various ways to learn, improve and innovate and were given time to do this in their day to day roles. The trust was committed to delivering a Quality Improvement (QI) programme and had invested in this across the organisation. The QI programme had flourished since the last inspection and was well embedded across the Trust
https://www.cqc.org.uk/provider/TAF/reports

PRIORITIES
Staff Wellbeing. ‘What Matters to You?’
At all initial project meetings, when talking about the problem staff wanted to improve, QI coaches asked: ‘What matters to you?’ and were curious about their wellbeing. This helped judge readiness. Over the course of the last year we had 9 teams sign up for the ‘pure approach’ and 139 projects ran with well-being as a key driver
Violence Reduction Collaborative
The collaborative is now focused on bringing together the different initiatives including Safe Wards, testing body cameras for staff and peer debrief volunteers to outline a standard process on how the acute wards respond to violent and aggressive incidents, with a key focus on empowering staff.
Digital Connections Forum
The forum continued to support front line teams make changes to clinical applications to enhance their everyday working. It trialled its first ‘Clinical Hacks Event’ which was a huge success with crisis teams making use of the assist tab functions and launching their “Reducing the number of clicks QI project”.
Length of Stay
For 2019/20 average length of stay remained unchanged at 41 days. The QI team have supported the work to reduce this time and have worked on a careful analysis on the contributing factors to patient flow problems. Improvement has been made in the number of those who have stayed for more than 50 days.
The Clozapine Services and Pathway
Formed with multidisciplinary membership, the group has developed clear processes and standards of clozapine care. The staff involved in this group have started to use QI methodology to support eight key areas of improvement. The key outcome measure is the number of days that patients continue to adhere to clozapine.
Physical Health
Significant progress has been made in increasing the number of physical health assessments completed. Key barriers to assessing the effectiveness is the functionality of the physical health screening tool which is currently being upgraded. Factors that increase screenings include having an identified physical health lead, full involvement from the team, the use of a dashboard and psycho-education and training for staff.
ACHIEVEMENTS AND MEASURING PROGRESS

Next Steps
• Development of a Quality Management System at C&I
• Co-producing improvement – improving service user feedback systems, involvement and experience
• Developing a QI Coach Programme at C&I
• Working with Barnet, Enfield and Haringey QI team. Sharing learning between teams, sharing our QI method and training, collaborating on celebratory events.

Key programmes we are supporting:
• Patient Flow
• Enhancing our community services and
Integrated Care Systems (including physical health of our service users) • Supporting Delivery of Digital Strategy, including video consultation
• Staff Wellbeing
• Reducing Inequalities
Completed Projects
Care
• Joint working on Acute Wards - to enhance dual-diagnosis care in C&I
• Safeguarding Children - Improving Drs admission clerking Doc of service users’ contact with children
Discharge and Recovery
• Dunkley Ward - Discharge medication counselling
• Discharge medication counselling - A nurseled QI project
• Increase the number of Trust staff teaching at The Recovery College
Group Programme
• Increase attendance in groups in Camden
Drugs Service
• Improving the group programme at the
Margarete Centre
• Focus on me - Group Programme - Better
Lives Family Service
Physical Health
• Sapphire Ward: Improving Ward Rounds -
An emphasis on Physical Health
• Camden Acute Day unit: Physical health screening
• Improving Physical Healthcare for Psychiatric inpatients: Sapphire PH
Process and Procedure
• Clozapine Programme at C&I
• Focus Assessment Process
• Improving induction for Foundation Drs
• Using QI methodology to implement a
‘leaving summary ‘at the Camden Acute
Day Unit
• Remodelling the follow-up procedures of patients with mild cognitive impairment in
Islington Memory Service
• Improving the Dementia pathway in Camden learning disability service
• Daffodil Unit Assay Project
• Close Observations
• Substance Misuse Division.
• Building the Will
• Reduce the time spent by clinicians on email requests
• Improving service users’ feedback at
Islington learning disability partnership
QI Survey. Everyone that completes a project is asked to complete a survey. In 2019/20, 42 people responded.
1. How much impact has QI had on your confidence to affect change in the Trust?
Overall Meridian score for this question: 86.90% (based on 42 responses)
100
80
60
40
10
0
57.14%
33.33%
Positive impact Slight positive impact
9.52%
0.00% 0.00%
No impact
Slight negative impact Negative impact
2. What impact has QI had on your wellbeing at work?
Overall Meridian score for this question: 77.38% (based on 42 responses)
100
80
60
40
10
0
40.48%
30.95% 26.19%
Positive impact Slight positive impact
2.38% 0.00%
No impact
Slight negative impact Negative impact
3. What impact has QI had on teamwork in your service?
Overall Meridian score for this question: 87.50% (based on 42 responses)
100
80
60
40
10
0
57.14%
35.71%
Positive impact Slight positive impact
7.14% 0.00% 0.00%
No impact
Slight negative impact Negative impact
4. How likely are you to recommend C&I to friends and family as a place to work?
Overall Meridian score for this question: 77.40% (based on 42 responses)
100
80
60
40
10
0
40.48% 35.71%
19.05%
2.38% 2.38%
Positive impact Slight positive impact
No impact
Slight negative impact Negative impact

Key Focus 2020/2021
On 4 March 2020 NHS England declared a level four incident due to the COVID-19 pandemic. All QI projects were paused due to the need for services to focus on the crisis. As the Trust moves into the recovery phase, the QI hub is supporting services with localised changes specifically focused on: • Infection control and social distancing
• Equality
• Physical health
• Digital
• Integrated care
• Patient flow
Recovery College
The C&I Recovery College continues to offer public courses on mental health and wellbeing to build the population’s self-care skills and improve self-management of health conditions. We treat everyone coming through our door holistically, understanding that life has its ups and downs, challenges and happy moments. Recovery, to the college, is an ongoing journey where we try to increase our resilience by having a toolbox with several different tools available, discovering which tool works best, when and in what situation. We use the social model of disability and use co-production to learn all from each other.
New courses are prepared from scratch through partnership working e.g. Green prescription (Castlehaven Community Centre), Building connections in the community (Mind in Camden), Making the most of your memory (Trust Occupational Therapist), Dealing with Debt (Mary Ward Legal Centre), Living well with a long term condition (Whittington Health Clinician) and Men’s Space (Jules Thorne Clinician).
The college works with other organisations to access space for running the courses and without these we would not be able to do what we are doing. To name a few: Birkbeck University, Kentish Town Community Centre, Kings Place Music Foundation, Crowndale Centre, Islington Town Hall and Sapphire Independent Training Resource Centre.
We were surprised last year to be asked to provide consultancy for Recovery College Berlin as they were at the early stages of their start-up. Another organisation, Changing Lives, purchased our Men and Masculinity course materials together with two rounds of tutor preparation courses as they want to use it within their supported housing accommodation services for veterans.
We started to provide training to Newly Qualified Nurses with ‘Co-production and Shared Decision Making’ and ‘Motivational Interviewing’ CPD events. A QI project commenced to extract the benefits of tutoring at the college as a lot of trust employees seemed to use their learning for enhancing their career prospects.
Mental Health Matters events
Our “Mental Health Matters” events are a series of informal quarterly meetings for Trust members, service users and staff to discuss issues relating to mental health. Members of the public are also invited to attend.
ADDITIONAL INFORMATION AS STIPULATED BY NHS ENGLAND
Equality and Diversity, Staff Engagement and Organisational Development
Staff Survey
Each year our staff members are invited to take part in the national annual Staff Survey. It gathers views on their experience at work around key areas including on development opportunities, health and wellbeing, staff engagement, and feeling able to raise concerns.
1.1 C&I Staff Survey 2019 Response Rate
Trust Score 2018 Trust Score 2019 National 2019 average for mental health Trust Improvement/ Deterioation Ranking compared with all mental health trusts 2018
49% 59.7% 54% Improvement of 10.7 percentage points Above Average
The Trust’s 2019 staff survey response rate was 59.7%, an increase of 10.7% from last year and above the national average for mental health trusts of 54%. This is the highest response rate for Camden and Islington Foundation Trust.
1.2 Overall staff engagement
The Trust recorded a score of 7.0 (on a scale of 1-10) against a national average of 7.0 for mental health trusts.
The tables below show the top and bottom five ranking scores and how we compared to last year’s results as well as to other mental health trusts in England.
1.3 C&I Top Five Ranking Scores 2019
Trust Score 2018 Trust Score 2019 National 2018 average for mental health Trust Improvement/ Deterioration
Senior managers try to involve staff in important decisions Communication between senior management and staff is effective Senior managers act on staff feedback Appraisal/review definitely helped me improve how I do my job Able to make improvements happen in my area of work
42% 47% 38% 5% improvement Above average
46% 51% 42% 6% improvement Above average
39% 43% 36% 4% improvement Above average
33% 31% 24% 2% deterioration Above average
66% 64% 59% 2% deterioration Above average
In addition to the above top five ranking question scores, Camden and Islington scores have remained consistently above average (since 2015) for appraisals that agree clear objectives and remains the top-ranking Trust for appraisals that improve how staff do their job.
In terms of ‘Theme’ scores there has been a statistically significant improvement since last year in positive responses to questions indicating staff perception of an environment safe from violence. Meanwhile, scores in the theme relation to Quality of Care also now demonstrate above average performance.
In the themes of Equality, Diversity and Inclusion, Health and Wellbeing, Morale, and Bullying and Harassment, overall scores are significantly below average. There have been improvements in scores for some questions where the Trust was previously ranked lowest amongst mental health trusts; however, scores remain below average in those areas. See table below for bottom five ranking scores
Ranking compared with all mental health trusts 2018
1.4 C&I Bottom Five Ranking Scores 2019
I am unlikely to look for a job at a new organisation in the next 12 months Appraisal/ review: organisational values definitely discussed Not experienced discrimination from patients/service users, their relatives or other members of the public Had appraisal/KSF review in the last 12 months Not experienced harassment, bullying or abuse from patients/service users, their relatives or other members of the public Trust Score 2018 Trust Score 2019 National 2019 average for mental health Trust Improvement/ Deterioration
46% 43% 51% 3% deterioration Below average
Ranking compared with all mental health trusts 2019
32% 34% 40% 2% improvement Below average
83% 84% 90% 1% improvement Below average
88% 84% 89% 4% deterioration Below average
61% 62% 67% 1% improvement Below average
The Trust has identified the following key themes to focus on as areas for improvement in 2020/21
• Equality of opportunity and fairness
• Experience of bullying and harassment from service users and the public
• Health and wellbeing of staff
• Morale (covering questions around autonomy and agency, relationships at work, intention to stay)
• Increase in staff experiencing violence from colleagues
• Number of staff having appraisals and their subsequent access to learning and development opportunities The New Workforce Strategy has an associated delivery plan which includes actions and timeframes to be monitored by the Workforce and Culture Programme Board.
Actions include
• Engagement with staff at a local level to facilitate ownership of action plans to tackle key issues raised in the Staff Survey
• ‘You said, we did’ campaign throughout the year to increase the visibility of the impact of actions
• Workforce Race Equality Standards (WRES) and Workforce Disability Standards (WDES) action plans to raise awareness of challenges, increase representation at higher bands and to support adjustments that enable staff to access opportunities.
• Improving information on wellbeing offerings through the intranet
• Promoting the revised Trauma at Work
Pathway,
• Increase the profile of opportunities available to gain apprenticeship qualifications
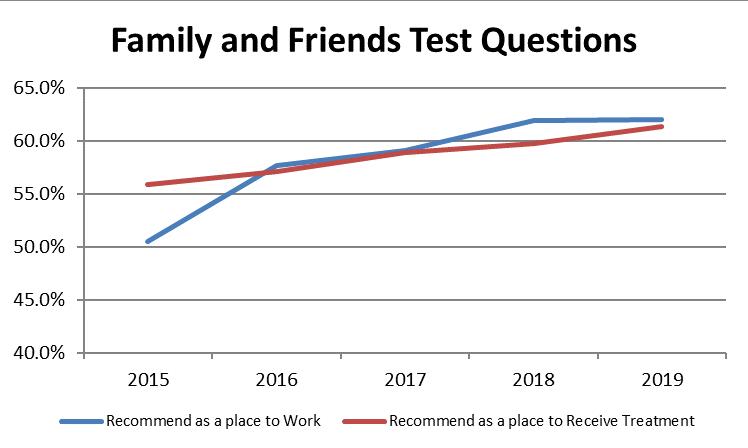
1.5 Engagement score through Friends and Family Test (FFT)
The Friends and Family questions continue to be sent out using the CandiConnect platform.
Two questions are asked in the Family and Friends test:
• How likely are you to recommend Camden and Islington NHS Foundation Trust to friends and family if they needed care or treatment?
• How likely are you to recommend Camden and Islington NHS Foundation Trust to friends and family as a place to work?
A response between “Very Likely” and “Very Unlikely” is required by the survey and an opportunity is given to explain the reason for one’s answer. Answers of “Very Likely” and
“Likely” are considered positive scores.
FFT Q4 shows 69% positive for the first question (treatment). This represents a 2% improvement on the same period in 2019. The positive responses for the second question (work) showed a drop of 4% on the same period last year at 63%.
In free text responses relating to recommending the Trust as a place to receive treatment, there were positive comments about the professionalism, empathy and dedication of colleagues with some services highlighted as being exceptional. However, less positive comments refer to perceived under-resourcing, high caseloads and long waiting lists for services.
Likely to recommend for Care of Treatment

Likely to recommend as a place of work
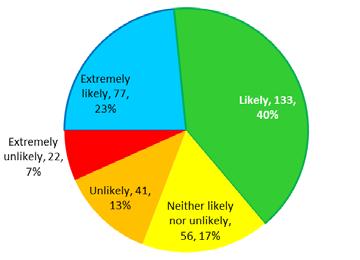
Positive free text comments recommending the Trust as a place to work refer to opportunities for development and progression, co-production with staff and service users, and a friendliness of colleagues. Less positive remarks are around experiencing a lack of equality of opportunity, poor working environments, high workloads, bullying behaviours and hierarchical management. Replies to the same questions as part of the Staff Survey are consistently 5-10% lower than in the standalone FFT online survey, which has a considerably lower sample size / response rate. This implies that there is likely to be a positive bias in the standalone FFT surveys. The Staff Survey results still show an upward trend since 2015, although recommending as a place to work has only risen marginally since the 2018 survey.
1.6 Friends and family test questions in the staff survey
Our commitment to ensuring Equality, Diversity and Inclusion
A fundamental and unique aspect of this Trust is the diverse community we serve and our diverse workforce. This year we have further developed The Our Staff First Project. This has been very effective in retaining and developing the Trust’s own staff since it was launched in 2017. Almost a fifth of bands 8a and 9 roles are now filled by BAME staff – a rise of 4.5% on the previous year.
Our Staff Survey and WRES results tell us that despite introducing Our Staff First we need to think differently and look at other ways of supporting fairness and discrimination. This will be a key strategic priority in our refreshed Workforce Strategy and a focus of our refreshed Equality and Diversity Strategy.
To further increase the numbers of BAME staff at 8a and above, we have added a new intervention to our recruitment process and this is overseen by the Director of HR & OD who will be advised prior to offer of any decision not to recruit a BAME member of staff if the scoring is three points or less, different to non-BAME candidate.
In conjunction with Our Staff First and our Workforce Race Equality Standard (WRES) Action Plan, the role of the WRES Expert has been further developed to support the equality, diversity and inclusion work for BAME and is working closely with the Employee Relations Team to ensure fairness in the disciplinary process and how it is applied.
The BAME staff group, Network for Change, continues to contribute to the Our Staff First strategy and hosted a successful Strength in Diversity Conference in October, with keynote speakers including C&I’s Human Resources and Organisational Development Director and the Director of the WRES NHS England.
The Disability+ Staff Network is extremely active and has co-produced material with the Equality, Diversity and Inclusion Lead, including the Supporting Staff with Disabilities and Long Term Conditions (physical and mental health conditions) reviewed the Equality, Diversity and Inclusion Policy and supported the renewed membership of the Disability Confident Scheme, and are supporting the Trust in achieving the next level in the scheme.
The Rainbow LGBT+ Staff Network is now fully established and is making headway with their membership of the Stonewall Diversity Champion Programme and, for the second year running, was due to attend the London Pride Parade. The C&I rainbow lanyards continue to be a popular way of showing both staff and service users that we are an open and inclusive organisation. In addition, the C&I Recovery College and the Equality and Diversity Lead have further developed the range of equality and diversity courses and we now have a LGBT+ Course. All courses are co-produced and copresented with service users.
Organisational Development
In 2018/9 there were 16 apprenticeship starts, undertaking qualifications in Business Administration, Trainee Nurse Associate, Senior Leadership and Human Resources. This represents a new way of addressing learning needs and alternative career pathways for new staff and existing staff.
The Trust has entered a collaborative with colleagues in other Trusts to examine our organisational culture and to build a culture of collaborative leadership. We will be working with The Whittington Hospital, Moorfields Eye Hospital and Newham Hospital. This initiative is due to last 18 months and includes a Discovery, Design and Delivery phase. During this time, staff from across bands, professions and services will be invited to be involved in the work and decision making.
The OD Manager has been working with the London Leadership Academy and the Estate Transformation project team to plan ways to engage staff in the design and reconfiguration of services to be housed in the proposed Integrated Community Mental Health Centres (formerly known as community hubs).
ENSURING EQUALITY AND TACKLING INEQUALITIES
Camden and Islington NHS Foundation Trust recognises the importance of ensuring its services are fair and equitable to all. The diversity of staff, service users, partners and any visitors to our services is celebrated. We expect everyone who visits any of the sites, or who come into contact with any Trust services, or work for the Trust, to be able to participate fully and achieve their full potential in a safe and supportive environment. The organisation welcomes all service users and members of staff irrespective of race, disability, sex, sexual orientation, gender reassignment, marriage and civil partnership, pregnancy and maternity, age, religion or belief.
The Trust meets all its requirements from within the Public Sector Equality Duty (which forms part of the Equality Act 2010). The requirements and how these are met is detailed opposite.
2.1 Stonewall Membership
The Trust is in its first year of being a Stonewall Diversity Champion. Stonewall is the UKs leading lesbian, gay, bisexual and transgender (LGBT) equality charity and has been
instrumental in changing the national legislative environment for people who consider
themselves to be LGBT+ and taking forward the agenda. The Trust is aspiring to reaching the Top 100 in the Stonewall Workplace Equality Index. The Stonewall rating is often seen as an indicator of an organisation’s approach to equality and inclusion overall and can further increase all diversity in the workplace.
Part of the Trust’s work for LGBT+ equality has included planning for our involvement in the London Pride parade for the second year.
2.2 Staff Networks
The staff networks provide a platform for staff to voice their opinions and support the Trust to improve working practices and services. It has been an invaluable resource that has had several positive outcomes. There are currently four active staff networks:
• Network for Change (Black, Asian and minority ethnic) and allies staff network.
Disability+ (mental and physical lived experience) carer’s allies’ disability staff network.Rainbow+ (lesbian, gay, bisexual and transgender) and allies staffWomen (all who identify as women) and allied staff
Each staff network has an executive sponsor, whereby an executive director has committed
to championing that group at Board level. They attend at least one meeting a year to understand the issues being raised by the group.
2.3 Equality and Diversity Training
In 2018/19 the Trust’s compliance rate for mandatory equality and diversity training was 91.0%. Training in equality and diversity is a mandatory e-learning module for all staff and a key component of the new staff induction process. Following a review of all mandatory training, staff will do equality and diversity refresher training every three years, ensuring that
all employees are equipped with the appropriate knowledge and awareness to provide consistently fair treatment towards colleagues and patients/service users alike. In addition, workshop sessions are offered by the Equality, Diversity and Inclusion Lead for services and staff members who would like further information and training around inclusion.
Requirement
Public Sector Equality Duty (introduced 2011
Employers and employees in the public sector, and in private or voluntary organisations carrying out work on behalf of a public sector employer, have a legal duty in the workplace to:
General duty
1. Prevent and eliminate discrimination, harassment and victimisation. 2. Establish and promote equality and equal opportunities. 3. Foster good relations. • Collection of equality monitoring information for service users/ staff.
• Equality analysis process in place.
• Equality staff networks.
Specific duty
1. Publish information to demonstrate compliance with the general equality duty.
2. Prepare and publish one or more equality objectives to achieve any of the things from the general equality duty. • Equality Annual Report.
• Analyse and publish staff and patient equality monitoring data annually.
• Published equality objectives.
• Carry out equality analysis on key decisions.
NHS Standard Contract Equality Delivery System 2 (EDS2)
Workforce Race Equality Standard (WRES)
Workforce Disability Equality Standard (WDES) Evidence
• Equality Delivery System 2 review of grading and actions on an annual basis.
• Implementation of actions
• Results collated and submitted to NHS England annually.
• Action plan in place and being implemented. • Results collated and submitted to NHS England annually.
• Action plan in place and being implemented.
Organisational Development (OD)
There are currently 31 staff undertaking apprenticeships in Business Administration, Improvement Technician, Trainee Nurse Associate, Masters in Leadership and Data Analyst qualifications. The Trust continues to explore ways to optimise use of the Apprenticeship Levy funds in order to create new career pathways. This offers opportunities for staff to progress and for the Trust to explore alternative skills mix.
The Trust continues to work in a learning collaboration between The Whittington Hospital, Moorfields Eye Hospital, and Newham Hospital in order to examine our organisational culture and to build a culture of collaborative and compassionate leadership.
Staff from across bands, professions and services have been invited to be involved in the work as we progress through the Diagnostic, Design and Delivery phases over the coming year OD priorities for the coming year:
• Equality and Fairness
• Service Transformation
• Embedding the Cultural Pillars
The OD team also works in close collaboration with the Trust Wellbeing Lead, the Quality Improvement team and the Equality, Diversity and Inclusion and WRES Leads.
Recruitment and Retention
In 2019/20 we have recruited 232 new non-medical staff to the Trust excluding trainee positions, we recruited 20 to band 8a and above roles and 30% of these appointments have been BAME Staff.
There has been a key focus on improving the number of BAME staff we employ and ensuring that the recruitment process is fair and transparent. We have worked in partnership with BEH, to re-launch our BAME reps’ initiative and re-branded this under Equality Champions. We have implemented joint training for Equality Champions across both organisations and we are working to set up an automated process to share Equality Champions across both trusts. We have worked with the Ministry of Defence to achieve the Employer Recognition Scheme Silver award for the work we have been doing with the armed forces in recognition of the Trust putting in place forces-friendly initiative such as our Employing staff in the armed forces policy.
We are working closely with the divisions to improve recruitment levels especially in our nursing roles and plan to attend The Times Nurses and Midwifery recruitment fair in March.
Learning from Death
There is a Learning from Deaths process at the Trust. There are weekly Mortality Review Meetings Group meetings where all deaths are subject to case review. Quarterly Learning from deaths reports are presented at the Board.
Item Prescribed information Comments
27.1 The number of its patients who have died during the reporting period, including a quarterly breakdown of the annual figure.
27.2 The number of deaths included in item 27.1 which the provider has subjected to a local 72-hour investigation or Serious Incident Investigation. Including a quarterly breakdown of the annual figure.
27.3 Of the deaths reported in item 27.2, all were investigated to determine avoidability of death in terms of provider care. The avoidability scale scores from 1-6 with scores. Scores 1-3 confirm that the investigator and review panels (SI and MRG) agreed that the death was definitely avoidable, strong evidence of avoidability or probably avoidable. Total 185 Q1- 102 Q2- 112 Q3 – 101 Q4 - 129 72 Hour investigation Q1 - 28 Q2 - 35 Q3 – 37 Q4 - 42
SI investigation Q1- 8 Q2- 7 Q3 - 1 Q4 - 9 Q1- 0 death scored as <=3
Q2- 0 deaths scored as <=3
Q3-4 not available
27.4 A summary of what the provider has learnt from case record reviews and investigations conducted in relation to the deaths identified in item 27.3:
Learning:
• Poor physical health is a key theme in the deaths reported during Quarter 1. Action Plans to address these issues include; training for new staff on the Physical Health
Screening Tool and addressing health issues in the service user care plan.
Learning continued:
• Service users who present with diagnostic uncertainty may not be receiving the care they need at a time they need it. This occurred in two of the investigations where service users experienced delays in accessing the care they required due to them being referred to an inappropriate service, or decisions about referral to an appropriate service were delayed due to diagnostic uncertainty. • Incomplete documentation continues to be a theme in Serious Incident Reviews. Although direct causal relationships are not clear. • The option to “create a new” risk assessment function on Carenotes, means that historically important information in the previous risk assessment is not carried forward into the most upto-date report. There is a risk of information getting lost. • There appears to be gaps in engaging carers of service users and fulfilling the requirements under The Care Act 2014 including undertaking formal carers’ assessments. • Delays in Mental Health Act assessments and how to support services users during the delays emerged again this quarter.
Learning:
Key themes identified from the serious incident investigations undertaken into service user deaths in the Trust. • Expected natural deaths, are the highest cause of death for this population. Many are the result of many years of poor lifestyle, diet, smoking, sedentary lifestyle and substance misuse. • The need for prompt engagement by services after a service user death was an area of improvement from one of the reports. Families felt they were not contacted quickly enough, or offered the right support following the death of a loved one. The Being Open and Duty of
Candour Policy (2015) outlined the expected timeframes to contact families after the death of a service user. There could be improvement in teams responding as outlined in the Trust Policy. • Communication and interface within the organisation (between teams), and with external providers (other NHS Trusts, GPs) has been a concern repeated in a number of the deaths’ reviews from this quarter. Investigations evidence that not all necessary information was shared as would be expected. None has been directly linked to the cause of the death; however, this is a key learning point from these investigations. • The need for joint investigations into care was highlighted with the first recorded service user death from the Specialist Perinatal Mental Health Service (SPMHS). The SPMHS was formed in November 2017, to work across the five North East London Boroughs, (Camden, Islington,
Barnet, Enfield, and Haringey). This was an unexpected unnatural death, which found at
Inquest that the care provided by the SPMHS was good and the death could not have been prevented. • NHS England have completed their substantial piece of work to provide literature for services, and families/carers affected by a homicide by a service user with a mental health diagnosis.
These can be obtained online at https://www.england.nhs.uk/london/our-work/mhsupport/.
This is in addition to the “helping hand” booklet, for families and carers of persons who end their life through suicide. The latter has been shared Trustwide. The Homicide literature will be shared accordingly.
• The reviews of these deaths also brought up issues regarding the planning and discharge process from inpatient units. This includes referral onto community teams in a timely way, with understanding of the triage processes and response time of the receiving team. Also, to ensure discharge plans are communicated clearly with the service user, family, and other C&I and non-
C&I providers. • During this period, one patient death occurred on the ward. This was recorded as a natural death, however learning from the review detailed gaps in physical health management, including ECG and VTE assessments as per the Physical Health and Wellbeing Policy. 27.5 A description of the actions which the provider has taken in the reporting period, and proposes to take following the reporting period, in consequence of what the provider has learnt during the reporting period (see item 27.4). As stated above 27.6 An assessment of the impact of the actions described in item 27.5 which were taken by the provider during the reporting period. As stated above 27.7 The number of case record reviews or investigations finished in 0 the reporting period which related to deaths during the previous reporting period but were not included in item 27.2 in the relevant document for that previous reporting period. 27.8 An estimate of the number of deaths included in item 27.7 which the provider judges as a result of the review or investigation were more likely than not to have been due to problems in the care provided to the patient, with an explanation of the methods used to assess this. N/A 27.9 A revised estimate of the number of deaths during the previous N/A reporting period stated in item 27.3 of the relevant document for that previous reporting period, taking account of the deaths referred to in item 27.8.
LEARNING FROM DEATHS AND SERIOUS INCIDENTS
Description of the quality issue and rationale for prioritising
The 2017 Care Quality Commission (CQC) review of the way NHS trusts review and investigate the deaths of patients in England found that learning from deaths was not being given enough priority in some organisations and consequently valuable opportunities for improvements were being missed.
Identified areas for improvement
• To ensure that all data related to deaths is standardised into the Trust’s approved
QI process, using various charts this will allow for better detection of special cause variance within a service.
• For a singular Trust Suicide Prevention
Strategy to be developed that draws on the learning from suicides within the Trust
• The Governance structure around the scrutiny of Action Plans related to Serious
Incidents required improvement in order to make the process more robust and transparent.
What we have achieved
• The Trust has a Mortality Review Group (MRG) that meets on a weekly basis to review all deaths.
The MRG is attended by the Medical Director, Nursing Director and Chief Operating Officer.
When deaths are reviewed in the MRG, the views and concerns of the family are considered as part of the process.
• The Trust produces quarterly and an annual ‘Learning from Deaths’ reports that are heard at the public Board meetings.
• The Learning from Deaths report includes data for all deaths of Trust service users and draws together the common themes in a thematic review (Please see Chart 1 as an example)
• The data for deaths is broken down into several categories that meet the MAZARS Framework, in addition several other categories are produced that further identify if there are any specific concerns within a certain Division or Team. The categories are as follows:
o Expected Natural (Broken down into “When Expected or Earlier than Expected)
o Unexpected Natural (Broken down into “Sudden Natural Cause or “Natural Cause but didn’t need to be”)
o Expected Unnatural (Expected, but not from the cause that was expected)
o Unexpected Unnatural (Suicides and Homicides)
o Total Deaths
o Deaths by division
o Time between Inpatient deaths
o Time between deaths caused by self-harm
• The Trust has now developed a suicide reduction strategy that develops and reviews large Trust
Wide projects targeted towards the reduction of suicide. These Trust wide projects are developed in response to learning from Serious Incident Investigations following the suicide of a patient.
• To date these projects include:
o Improving the Care Plan Process
o A complete review of the entire Risk Assessment process including:
• The reviewing and updating of the Risk Assessment template
• Introducing and Risk Event Chronology
• Reviewing and commissioning new training
• Introducing Risk Assessment as a core competency for clinical staff
o Improving access to bereavement counselling for relatives and careers of patients that have committed suicide
o Improved data sharing with Public Health England
• The Action Plans for Serious Investigations have been fully migrated over to Datix, this will allow for a more transparent view of the completion of Action Plans and how effective they have been at improving patient safety
• 72 Hour Reports have been moved over to Datix, this will allow for more timely responses to incidents of concern that require further enquiry
Next steps/future challenges:
• Introducing quarterly surveillance groups related to the key learning from deaths, these will include the Divisional Leads
• Reviewing current divisional Governance structures to ensure that the completion of Action
Plans related to Serious Incidents have been sufficiently scrutinised
• Developing a strategy that aligns the Trust to the New National Patient Safety Strategy (July 2019)
Total Number of Deaths (Chart 1)
70 65 60 55 50 45 40 35 30 25 20 10 5 0
Apr-17 Jun-17 Aug-17 Oct-17 Dec-17 Feb-18 Apr-18 Jun-18 Aug-18 Oct-18 Dec-18 Feb-19 Aug-19 Jun-19 Aug-19 Oct-19 Dec-19 Feb-20 Total Number of Deaths
Mean
Lower process limit
Upper process limit
Common Cause
Special Cause Concern
0.0 0.2 0.4 0.6 0.8 1.0
NHS IMPROVEMENT TARGETS
In 2018/19 the Trust continued to be assessed on a quarterly basis to meet selected national standards for access and outcomes.
NHS Improvement Single Oversight Framework
Camden and Islington NHS FT considers this data is as described due to the following reasons - the data for these indicators is derived from our internal performance systems. Camden and Islington NHS FT has taken the following actions to make further improvements on these indicators even though the indicators are on target, and so the quality of its services, by reviewing the data to identify gaps and taking appropriate actions.
Proportion of people experiencing a first episode of psychosis treated with a NICE approved care package within two weeks of referral
Target 18/19 Apr-19 May-19 Jun-19 Jul-19 Aug-19 Sep-19 Oct-19 Nov-19 Dec-19 Jan-20 Feb-20 Mar-20
People with a first episode of psychosis begin treatment with a NICE recommended care package within two weeks of referral 56% 75% 81% 87% 75% 87% 87% 94% 94% 89% 91% 67% 79% Not Published
Improving access to psychological therapies (IAPT):
a) proportion of people completing treatment who move to recovery (from IAPT dataset)
b) waiting time to begin treatment (from IAPT minimum dataset):
Camden and Islington NHS FT considers this data is as described due to the following reasons - the data for these indicators is derived from our internal performance systems. Camden and Islington NHS FT has taken the following actions to make further improvements on these indicators and particularly those relating to ‘proportion of people completing treatment who move to recovery’, and to the quality of its services by close review with improvement plans in place.

Inappropriate out-of-area placements for adult mental health services:
NB: Figures include Acute/PICU OAP placements:
Camden and Islington NHS FT considers this data is as described due to the following reasons - the data for this indicator are derived from our internal performance system. Camden and Islington NHS FT has taken the following actions to improve this indicator, and so the quality of its services by:
1. Focusing on long-stayers (over 50 days) on our acute wards, with a set of actions being developed and implemented following the recent long-stayer audit 2. The development of plans to reduce admissions
3. Analysis of demand for male PICU, with an appraisal of options to develop additional
C&I capacity to treat all men who need intensive care locally
Inappropriate out-of-area placements for adult mental health services (Occupied Bed days) 219 697 340 331
Q1 19/20 Q2 19/20 Q3 19/20 Q4 19/20
Ensure that cardio-metabolic assessment and treatment for people with psychosis is delivered routinely in the following service areas:
The Trust’s physical health screening tool enables staff to screen all patients and ensure that they are assessed appropriately. The physical health policy has been revised and there are several physical health initiatives at present to provide further support for staff in all service areas.
Admissions to adult facilities of patients under 16 years old
No patients <16 within C&I
Freedom to speak up
The Trust has commissioned the Guardian Service, an independent and confidential service established to support NHS employees at all levels and in all roles, to discuss any matter relating to patient care, patient safety and work-related concerns. The service was designed in response to The Francis report. The Guardian Service fills a much-needed gap for both NHS organisations and staff by providing an independent and confidential reporting liaison service. The Guardian Service covers patient care and safety, whistle blowing, harassment, bullying, and work grievances. Today GSL supports nine NHS organizations employing approximately 65,000 staff.
The service provides information and emotional support in a strictly confidential, non-judgmental manner and in an off-the-record discussion. The one-to-one nature of the service is a fundamental foundation of the service providing personal contact in contrast to an online, email or drop box approach.
Initial contact with the Guardian Service is normally by telephone and this is answered by an appointed Guardian to any given organisation. The call may initially go to the voice mail service of an appointed Guardian and will be responded to within the same working day. The Guardian Service is unique in that all contact is on a personal basis and only via email where this is the preference of a contacting employee. A unique and dedicated number is commissioned for each Trust.
The service is focused on the individual, helping them to articulate their concern and decide what action they wish to take. They do not offer advice, legal or otherwise and their purpose is to help the individual articulate their concerns, understand what options exist in resolving their concern and helping them reach their own decision as what to do. Self-determination by a contact on what actions to take is a fundamental principle of GSL. With the agreement of the staff member, the service escalates the issue in line with agreed parameters, bringing the issue to the attention of the appropriate Executive or management team member.
On Initial contact service users are informed that instances of patient safety will be reported following the meeting. The meeting takes place with this caveat. Reporting can be anonymous, or with the staff members permission, include their name.
For many individuals, the opportunity to speak about their concerns in a safe environment with a neutral and understanding person can be an end in itself. Experience to date has demonstrated that the initial subject matter raised by an individual is often a symptom of a deeper held concern. The role of a Guardian in surfacing these deeper held issues is critical and supports the individual to rationalise their concerns to a point where they can decide for themselves to take further action or recognise their current reaction as an emotional response.
PATIENT BENEFITS
Potential patient safety issues identified immediately
Improved staff experience reflected in improved patient experience ORGANISATION BENEFITS
Surfaces issues that otherwise might have been unknown
Improves performance levels in reducing the number of employees experiencing stressful environment
Reduces the number of serious grievances and potential litigation EMPLOYEE BENEFITS
Independent and confidential support
Help in articulating their concerns
Feeling of being listened to
The Guardian Service:
• Allows individuals to seek impartial assistance without formalising their issue, in a confidential manner
• Assists issues to be resolved at an early stage
• Provides facilitation of meetings to resolve issues
• Reduces the number of formal grievances raised in an organization
• Reduces the number of grievances becoming litigious
• Protects working relationships between parties to a complaint
• Surfaces issues for the organisation that might otherwise be unknown
• Ensures action is taken in a timely manner
• Reduces organisational time and resources in handling complaints, grievances etc.
STAKEHOLDER INVOLVEMENT IN QUALITY REPORTS
The Trust’s quality goals are co-developed with stakeholders and communicated within the Trust and the community it serves.
In order to finalise the selected Quality Priorities for 2019/20, the Trust carried out a survey to gather the views of patients, staff, volunteers, trust members and governors and other stakeholders, on what they feel the Trust needs to focus on to ensure ongoing improvements in delivering quality of care. The information from this survey is used to inform the development of the Quality Report.
A “long list” of potential priorities was developed using a range of sources including quality and safety dashboards, various reports and feedback from trust governance groups and patient groups.
Sources of information included:
• Governance and management leads and groups
• Feedback received through user forums
• Commissioners and local authorities’ feedback
• Stakeholder consultation
STAKEHOLDER STATEMENTS
Commissioners’ Statement
North Central London Clinical Commissioning Group (CCG) is responsible for the commissioning of mental health services from Camden and Islington NHS Foundation Trust on behalf of the population of Islington and all associate CCGs. In its capacity as lead co-ordinating commissioner, the CCG welcomes the opportunity to provide a statement for the Camden and Islington NHS Foundation Trust Quality Account. The 2019/20 Quality Account has been reviewed within the CCG and by colleagues in NHS North East London Commissioning Support Unit.
Prior to the first wave of the Covid-19 pandemic, the CCG met monthly with the Trust at its Clinical Quality Review Group meetings (CQRG). This forum is where the commissioners are provided with assurance regarding the quality of care and services provided by the Trust. Throughout the pandemic, CQRGs have been paused. However, the CCG has maintained an open and ongoing dialogue with the Trust during this time. Commissioners look forward to attending the Trust’s internal Quality and Safety meetings next year to obtain the required assurance about quality of care.
The CCG has reviewed the information contained within the draft Quality Account (provided to the CCG in November 2020). We confirm that the document received complies with the required content as set out by the Department of Health, or where the information is not yet available, place holders have been inserted for their inclusion in the final Account.
The CCG is delighted to see the wealth of Quality Improvement (QI) projects in place across the priority areas and a number of these demonstrate the benefit they have provided for patients and service users, for example, an increase in service user involvement in QI projects and reduction in verbal aggression. The CCG would be keen to support ongoing and future QI initiatives, especially with a focus on improvement of care and experience across pathways within integrated care.
The Trust fully achieved four of the nine priorities for 2019/20 and partially achieved the others. Although the priorities not fully achieved are not priorities for 2020/21, we were pleased to see the Trust will continue to work on these over the coming year.
The Care Quality Commission (CQC) inspected the Trusts’ core services in October and November 2020. The CQC rated the Trust as ‘Good’ overall. Due to the hard work and dedication of the Trust and staff, the Trust was rated as ‘outstanding’ for Effectiveness. The safe domain was rated at ‘requires improvement’ and the Quality Account would benefit from the inclusion of key actions the Trust is taking to address the issues identified.
The CCG supports the six quality priorities identified by the Trust for 2020/21, which focus on:
• Patient Safety: Reducing violence and aggression
• Suicide prevention
• Patient Experience Service user and carer experience
• Expanding the peer workforce
• Clinical Effectiveness Refreshed clinical strategy
• Improving physical health care
The CCG looks forward to hearing of progress against the Trust’s chosen priorities for 2020/21 and the difference they make for our residents. The CCG will continue to foster an excellent supportive working relationship with the Trust and will continue to work towards greater collaboration, providing both support and constructive challenge where required.
7th December 2020 Comments from Camden Council Health and Adult Social Care Scrutiny Committee
No comments received.
Comments from Islington Council Health and Adult Social Care
No comments received.
Comments from Healthwatch Camden
Healthwatch Camden will not be commenting on any of the Quality Accounts this year.
We look forward to continuing to build upon our work with C&I as part of Camden’s Integrated Care Partnership in the year ahead.
Matthew Parris
Director
Healthwatch Camden
Received 9 December 2020
Comments from Healthwatch Islington
During 2019/20 Healthwatch Islington carried out research with BAME communities into their awareness of a range of mental health support available to residents. Despite those we spoke to having an acknowledged need, there were very low levels of awareness of statutory services. Furthermore, those working in Black and Minority Ethnic-led organisations felt that the Trust needed to reach out into the community more, to enable more people to access support. We are pleased that during the year members of the Trust including [the Head of Business Partnerships (who champions equality within the Trust, and we look forward to seeing more integrated, cross-sector ways of working develop. We know that the Trust continues its work on developing the estates and look forward to working with the Trust to shape that in a way that is as accessible and inclusive as possible. We know it’s been an extremely challenging year for colleagues working in the health and care sectors and we want to give thanks for the way that they have adapted over the year.
Emma Whitby Chief Executive
Healthwatch Islington
Received 7 December 2020
Response to Stakeholder Statements
The Trust would like to thank stakeholders for their comments. We look forward to working with stakeholders in the forthcoming year to achieve our priorities.





