*Implantable Cardioverter Defibrillator









Implant date: _________
☐ Pacemaker
☐ ICD Company:
☐ Abbott ☐ Biotronik ☐ Boston Scientific
☐ Medtronic ☐ MicroPort ☐ __________
MRI Conditionally Approved: ☐ Yes ☐ No
See summary in back for details and resources.
Order this book from :
PRITCHETT & HULL ASSOCIATES, INC.
3440 OAKCLIFF RD NE STE 126 ATLANTA GA 30340-3006 or call toll free: 800-241-4925
Copyright© 2023 by Pritchett & Hull Associates, Inc.
All rights reserved. No part of this book may be photocopied, reprinted or otherwise reproduced without written permission from Pritchett & Hull Associates, Inc.
Throughout this book, where Pritchett & Hull Associates, Inc. was aware of names of products for which a trademark has been claimed, such names have been printed in initial capital letters (e.g., MedicAlert).
Published and distributed by: Pritchett & Hull Associates, Inc.
Printed in the U.S.A.
 by Barbara Johnston Fletcher, RN, MN, FAAN
Julia Ann Purcell, RN, MN, FAAN (Author Emerita)
by Barbara Johnston Fletcher, RN, MN, FAAN
Julia Ann Purcell, RN, MN, FAAN (Author Emerita)
This book is to help you understand your pacemaker and/or ICD and what you can or can’t do when you have one. Do not use the book to replace your healthcare team’s advice or treatment.
*ImplantableBarbara Johnston Fletcher,
RN, MN, FAAN
Clinical Associate Professor
Brooks College of Health, School of Nursing
University of North Florida
Jacksonville, FL (previous)
Julia Ann Purcell, RN, MN, FAAN (Author Emerita)
Clinical Nursing Specialist, Cardiology 1968-1996
Emory University Hospital*
Atlanta, GA
John R Ferrante, RN, CCDS, CEPS, FHRS
Cardiac Device Specialist
Northside Hospital Heart Institute
Lawrenceville, GA
Our thanks to previous reviewers:
• Jonathan J. Langberg, MD
• Angel R. Leon, MD
*www.emoryhealthcare.org
We want this book to help put you at ease with your heart’s pacemaker and/or ICD by explaining what it can do for you. It may take a little time getting used to having a pacemaker and/or ICD, but you will find you can do most of what you want. Best of all, you will have the confidence that any symptom of an abnormal heart rhythm will be recognized and treated if necessary.
This book will explain:
• how pacemakers and ICDs work

• where these devices are placed in the body
• the usual surgery and recovery
• routine device checks
Your device manufacturer also has information about pacemakers and ICDs. Often you can read patient/family stories about life with a pacemaker or an ICD on their internet websites. After surgery, you will receive an ID card with the name of the company that made your device. Always carry this card in your wallet.
A pacemaker is a small electrical device put inside the body to control how your heart beats. Pacemakers look like this and fit just under your skin – most often in the shoulder area.
actual size
fits here
Pacemakers have 2 parts:
a pulse generator containing batteries
one or more lead wires that carry electrical signals to and from the heart
The pulse generator is a metal case that holds the energy that runs the pacemaker computer circuits. The pacemaker times how often the small electrical signals are sent to your heart. We will call the pulse generator, “pacemaker” from now on. The pacemaker lead wires carry signals from the pacemaker to the heart, causing it to beat. If your heart starts its own beat in time, these same leads carry the signal back to the pacemaker, putting it in standby mode.
A leadless pacemaker is available (single & dual chamber). It is small enough to be guided through a large vein and secured to the inside of the heart. Since the pacemaker touches heart tissue, lead wires are not needed to carry the electrical signals back and forth.
A pacemaker does for your heart what your heart’s electrical system cannot do on its own. Your healthcare team can check which of these created your need for a pacemaker:
Heart cells (S-A node) start a normal heartbeat but send out less than the usual 60-100 heartbeats per minute. This is called sinus bradycardia or sinus arrest.

The heartbeat goes from being too slow at times to being too fast. This is called bradycardia/tachycardia or sick sinus syndrome.
Upper heart cells that start a normal heartbeat (S-A node)
Cells between the upper and lower chambers (A-V node) that pass signals from the top of the heart to the bottom
Right bundle branch

Cells in the upper right heart (S-A node) send out the usual signals, but they get blocked between the upper and lower heart chambers in the AV node or bundle branches. This is called heart block.
NOTE: Heart block can happen on its own or as a result of a procedure to control a fast heartbeat that doesn’t respond to drugs (A-V node/His bundle ablation).
Delayed contractions between the lower heart chambers. One chamber contracts a little later than the other (a delay often seen in a weak heart.)
There are 4 main types of pacemakers.
Single chamber pacemaker (electrical signals going to a single heart chamber)
Dual chamber pacemaker (2 leads going to 2 heart chambers)
Biventricular pacemaker (2 leads carrying signals to both the right and left lower heart chambers and sometimes a lead to the upper right chamber)
Leadless pacemaker (single & dual chamber)
A single chamber pacemaker sends signals to either the upper or lower heart chamber to prevent a slow heartbeat. This kind of pacemaker sends out signals for a heartbeat only when needed.
lead to lower chamber (ventricle)


If your heart beats faster than the rate of the pacemaker, the single chamber pacemaker will remain on “standby” until needed. Single chamber pacemakers last 10 -12 years or longer, even if the pacemaker starts all of your heartbeats.
Some single chamber pacemakers do not need a lead wire. A tiny 'leadless' pacemaker can be guided through a vein into the heart and secured to the lower chamber.
'leadless' pacemaker
A dual chamber pacemaker makes sure that the upper chambers (atria) beat just before the lower chambers (ventricles) like in a normal heartbeat. A typical dual chamber pacemaker involves passing a lead through a vein to the upper right heart chamber and another lead to the lower right chamber. They now make a dual chamber leadless pacemaker.
lead to upper chamber (atrium)
lead to lower chamber (ventricle)
Sending and receiving signals in 2 or more heart chambers may use more pacemaker battery power. Battery replacement is often needed every 7-8 years.
A biventricular pacemaker has an extra lead passed inside the right atrium and into a vein on the outside of the left lower chamber. Signals through this extra lead can correct delays in contraction so the lower right and left chambers can beat together. This is known as cardiac resynchronization therapy (CRT).
extra lead insures that lower chambers beat at the same time
When the heart is weak (heart failure), one of the lower chambers often contracts a little later than the other. Biventricular pacing corrects this delay and insures that both chambers contract at the same time. Many people with heart failure notice a higher energy level and fewer heart failure symptoms with biventricular pacing over time.
Many pacemakers can speed up or slow down to meet the body’s demands. They watch for:
body movement
breathing patterns
heart response
Having your pacemaker go a little faster when needed often makes it easier to be more active.

The pacemaker settings may need to be changed as you return to your normal routine. This is to be sure the pacemaker responds just the right amount to your body’s need for more heartbeats. Let your healthcare team know if you notice unusual fatigue or if you think your heartbeat is speeding up when it doesn’t need to.
Some pacemakers can sense and treat fast heart rhythms (tachycardias). These pacemakers can send out short bursts of electrical signals to try and stop these fast rhythms. This is called anti-tachycardia pacing (ATP). Your doctor or nurse will let you know if your pacemaker has this feature. Drugs can be given to control or prevent fast heartbeats when needed.
If your cardiac device only does pacing, you can skip pages 11–12.
Just like a pacemaker, an ICD (or defibrillator) has a pulse generator –a metal container with electrical energy and circuits. In addition, most ICD's have one or more leads that carry electrical signals to and from the heart. The pulse generator of an ICD is slightly larger than a pacemaker.
The electricity needed to start a heartbeat is so small you cannot feel when pacing causes a heartbeat. When an ICD gives a shock, a much larger electrical signal is needed. An ICD is always on standby until a shock is needed to stop an abnormal heart rhythm. ICDs are used for fast heart rhythms, such as ventricular tachycardia and/or ventricular fibrillation. These rhythms are life-threatening and impair or stop blood flow. The ICD shock stops the abnormal rhythm and allows the return of a normal heart rhythm.
Drugs called “anti-arrhythmics” are usually given to prevent life-threatening heart rhythms. An ICD is needed to stop these rhythms if drugs don’t prevent them. You may feel dizzy when an abnormal rhythm starts, but the ICD works within seconds, often before serious symptoms can occur.
All of today's ICDs can provide back-up pacing after a shock as well as longterm pacing. Many ICDs also have the option of fast rate pacing (ATP) [page 10]. If rapid pacing signals do not stop a fast heartbeat, the ICD stands ready to deliver one or more shocks. Ask your healthcare team about your ICD settings.
It may take some time to adjust to having an ICD. The goal of having a device is to allow you to return to a normal life. If an abnormal rhythm happens, the ICD stands ready to deliver fast rate pacing and/or a shock. In some instances, medications may be needed to work with the ICD to control rhythms.
Tips to follow:
If you are feeling light-headed or dizzy, always sit down.
If you receive a single shock, report this to your healthcare team or device clinic. If you receive more than 1 shock in 24 hours and it's after hours, leave a message for your doctor or device clinic AND have someone take you to the ER or call 911.
If you are not feeling well after any shock, call 911.
Sometimes a subcutaneous ICD or S-ICD is placed under the skin on the lower left chest. The lead is threaded under the skin near the heart. S-ICDs offer short-term pacing through the chest muscles (transthoracic) if there is a slow heart rhythm after a shock.
Most pacemakers and ICDs are placed under the skin in the upper chest.
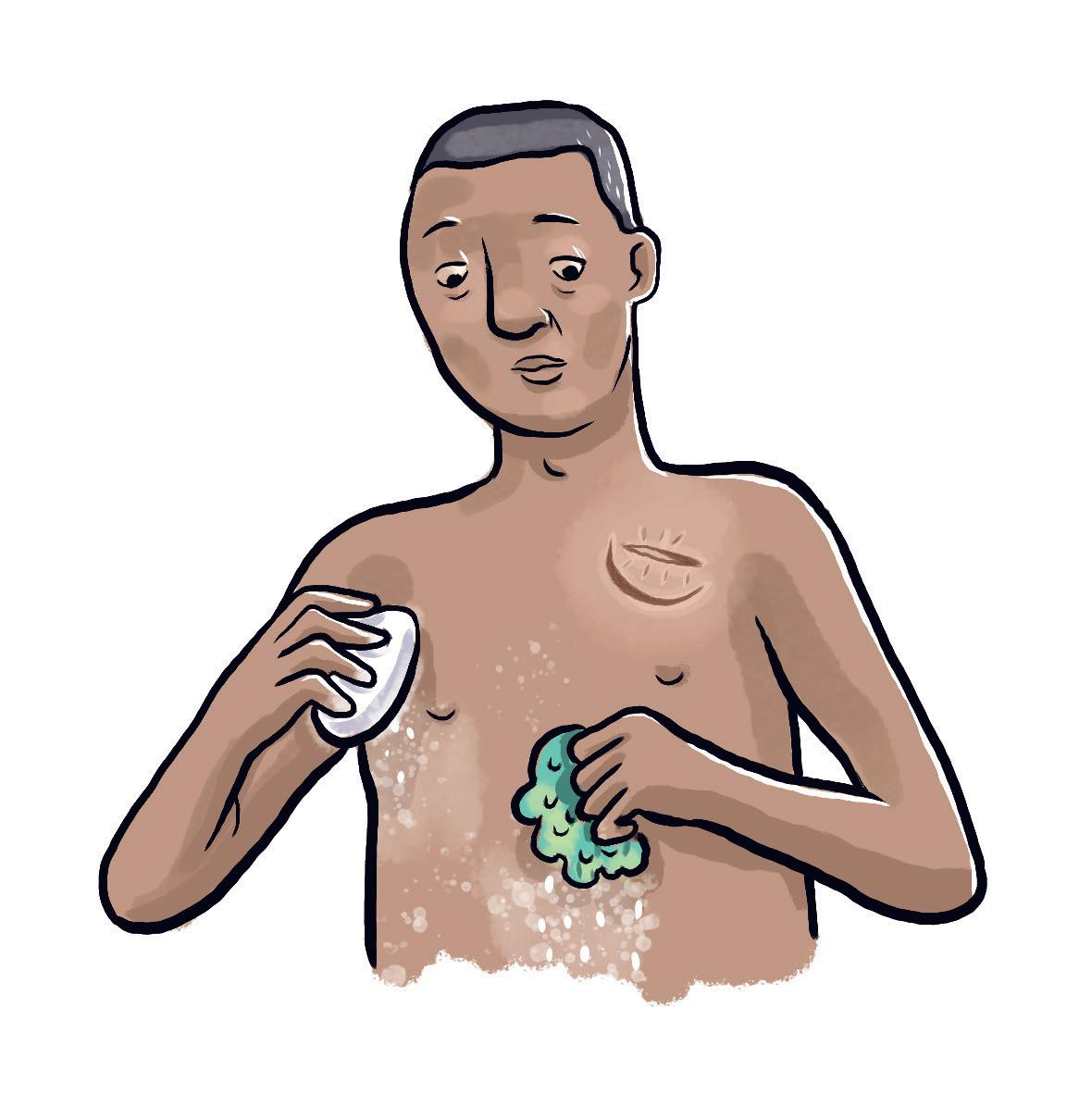
You are asked not to eat or drink for a number of hours before surgery. Your chest will be washed with a special soap and, if needed, any hair will be removed. You will get medicine in your vein to relax you and the skin will be numbed to prevent pain. Most people are sedated and it only takes an hour or two for the surgery.
An ICD is slightly larger than a pacemaker, and the surgery might take a little longer. If a test shock is necessary during ICD surgery, patients are sedated so they are not aware of the test shock.

For pacemaker and/or ICD surgery, an incision is made under the collarbone, often on the left side of the chest. A little pocket is made under the skin, over a vein. The doctor guides the lead(s) through a vein into a heart chamber(s) while watching an X-ray picture. The lead(s) must be in good contact with the heart so the electrical signals can go back and forth between the heart and the device. When the lead(s) are in place, the device is attached to them and placed in the pocket that was made under your skin.
Having a leadless pacemaker inserted is much like a heart cath procedure. A tiny pacemaker is implanted using a small nick in a leg vein. Using x-ray, your doctor uses a sheath to thread the small device to the desired location inside your heart. Recovery from this includes bedrest immediately after the procedure.
The area around the incision will be sore for a few days. Most incisions are sutured or closed with glue and a bandage isn't needed. Your incision will be closed in the best way for your surgery. In the recovery area, a nurse will check your pulse, blood pressure and incision. ECG monitoring is often used to see how your pacemaker or ICD is working.
Most people getting a device eat normal foods and are out of bed right away.

Your doctor has chosen the best method to close your incision. You may have skin adhesive (glue), tiny strips of tape, or stitches with Steristrips™ , or staples.
Please follow your instructions for incision care. Every patient and situation is different.
Most doctors ask that the incision be kept dry after surgery. (This can be from 1-12 days.)
Do not expose your wound to bright sunlight or tanning lamps during the first several weeks after surgery. Also, do not apply any liquids, ointment or any other product to the wound that is not ordered by your doctor.
You will be told when to have any stitches (or staples) removed. You can remove Steri-strips™ or skin adhesive when instructed by your doctor or clinic. Do not scratch, rub or pick at the skin adhesive, Steristrips™, stitches or staples used to close your wound.
Call a member of your healthcare team immediately if:
the incision is red, swollen or draining
the incision is warmer than nearby skin or is very tender
you have a fever over 100°F/37.8°C
Protect your incision from water until you are told you can get it wet.
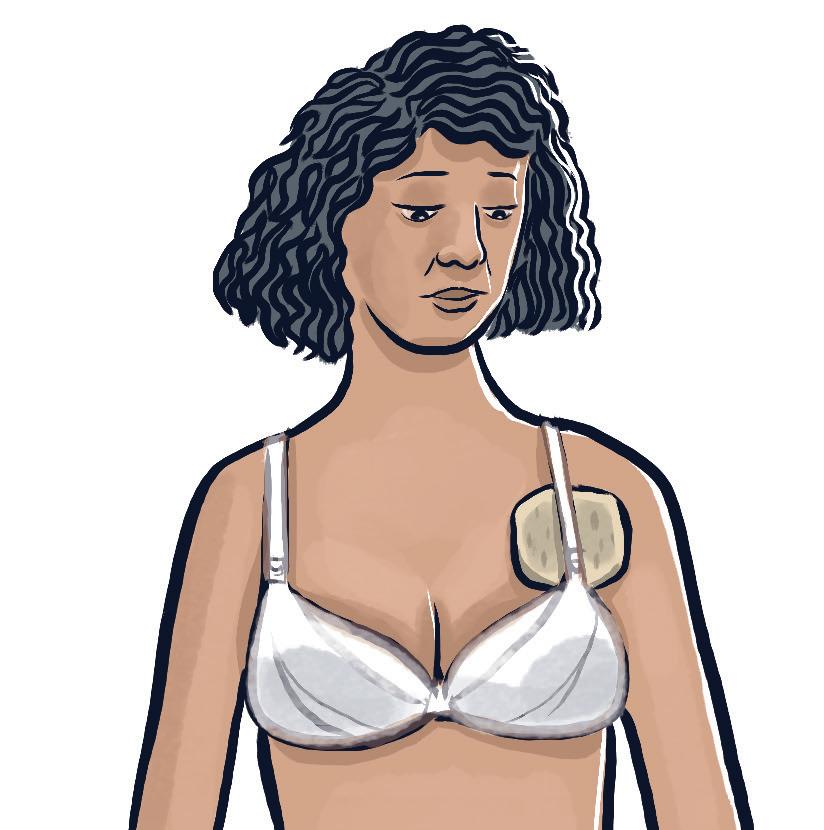
Clothing with elastic (such as bras) will not hurt the device, but, at first, loose clothing may feel better over the incision. Women may find that placing a pad over the incision makes a bra strap more comfortable until the soreness is gone. A pad may also help if your car seatbelt rubs the incision.
Antibiotics are given by vein during pacemaker or ICD surgery to prevent infection. If any fever or increase in swelling develops in the first few weeks, call your healthcare team to see if further antibiotics are needed.
Other medicines may also be needed to help prevent fast rhythms (anti-arrhythmics) or to make your heart pump better. A pill organizer box or electric pill dispenser may help you in taking your medicines as prescribed.

Most people recovering from pacemaker or ICD surgery can return to normal activity when the soreness around their incision goes away. Resume sexual activity when you feel comfortable. Follow your healthcare team’s advice about when to drive and return to work. Refrain from driving if on pain medication. If you pass out from your abnormal heart rhythm before the ICD can stop it or have several shocks in a short period of time, your doctor will ask you not to drive for the time being.
Once you are told it’s OK, you can return to activities like yard work, normal exercise and group sports without full body contact. If you like to lift weights, start with lighter weights and increase gradually. How much activity you can do is based on your overall physical condition, not the fact that you have a cardiac device. After the incision is healed, the device is not disturbed by water contact with things like swimming, taking a bath or shower.
Don’t do anything that might cause you to get a heavy blow to the skin over the device. If you hunt, never seat the gun against the shoulder closest to the device. Protect the area over your device from sharp blows or trauma.

Since it often takes a few weeks for any wire(s) to become secure in the heart, some caution is needed at first. Do not lift weights or do hard arm exercise for about 6 weeks or until your healthcare team says it is OK. During this time, do not lift more than 5-10 lbs and wait for things like tennis and golf that involve strong arm activity.
It's best not to lift your arm more than 90 degrees for 6 weeks.
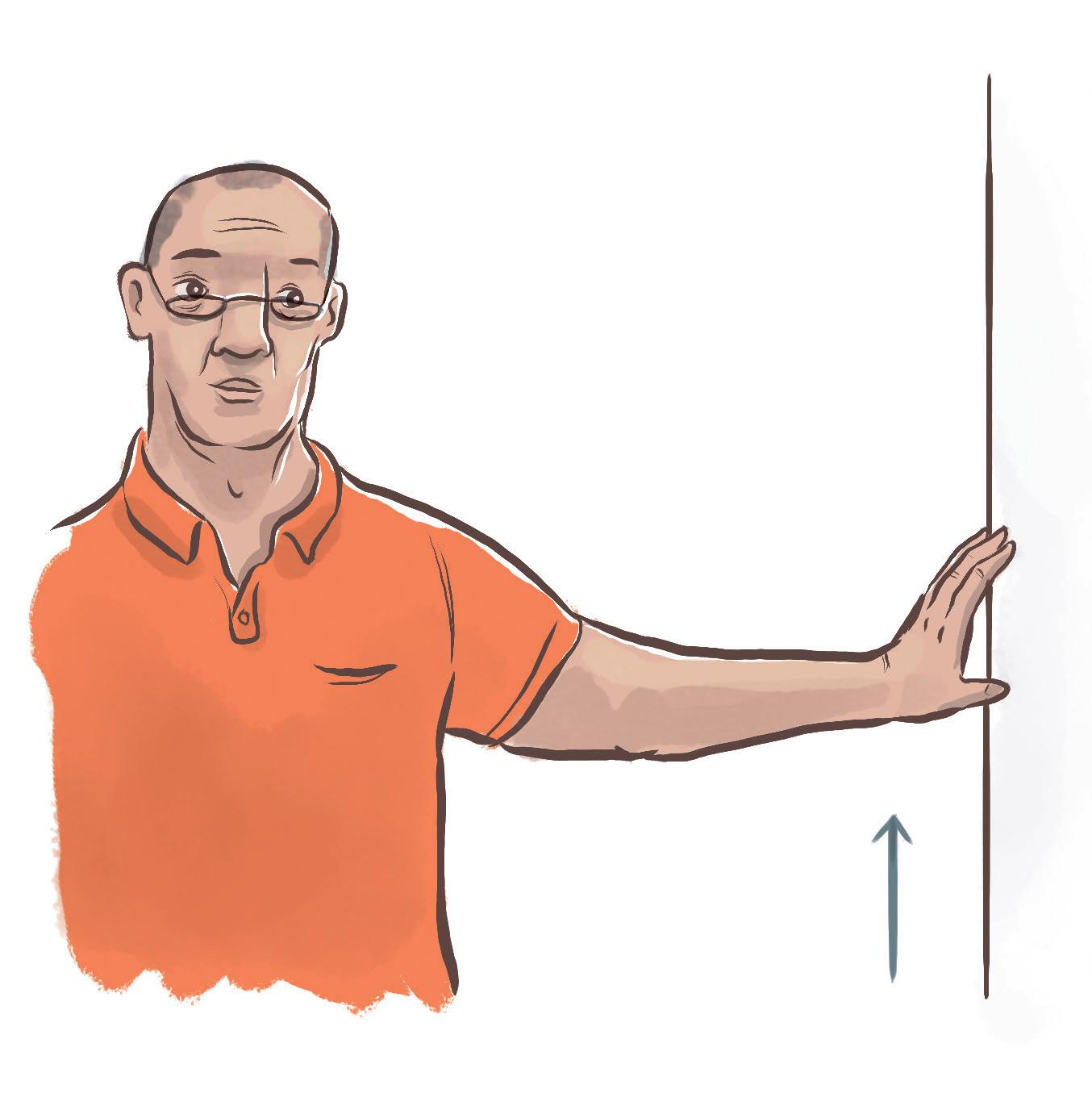
Unless you are told to wait longer, start doing small, slow arm circles after surgery. Use both arms but start with circles that are comfortable for the arm closest to the device. Gradually build up larger and larger arm circles. This helps the soreness go away, but don’t take it to the point of pain for your arm nearest the device. Some doctors suggest gradually “walking” your hands up a nearby wall over a period of days or weeks until you reach full range of motion in the shoulder nearest the device.
Although both a leadless pacemaker and all device lead(s) get secure inside the heart with time, using heavy equipment with strong vibrations (i.e., a jackhammer) may not be OK for someone with a pacemaker or an ICD. Check with your healthcare team before using this type of equipment.
If you wish to do endurance exercise, ask your healthcare team what kind you can do, how often to do it and for how long. Your warm-up before exercise can include a slow walk or slow peddling on a stationary bike. It can also include some stretching exercises like these:
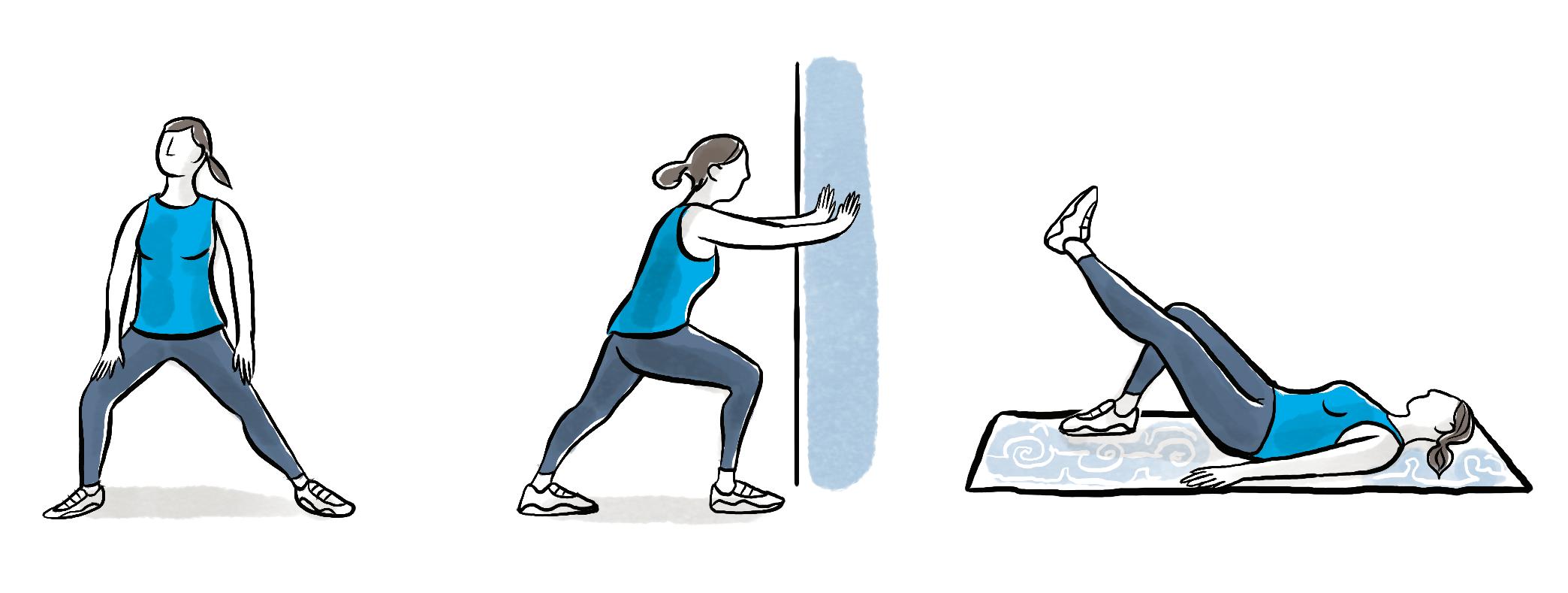
Your healthcare team will likely tell you to avoid extreme stretching or bending of the upper body for a number of weeks after cardiac device surgery. Some doctors say wait two weeks and others up to six weeks.
Your pacemaker may speed up as you increase body movement or breathing. Your heart may then be able to pump more blood with each beat and still meet your body’s needs. In all cases, your exercise should match what your heart can do and how you feel.
It is very unlikely that your cardiac device will be affected by electronic equipment in your home or while doing a hobby. However, it is always a good idea to:
Only use electrical items that are in good repair and
Avoid holding any electronic equipment directly over your cardiac device (see pages 22-23).
You can use common electronics found around the house. These include:
Large household appliances: washers, dryers, refrigerators, freezers,dishwashers, gas and most electric cooktops* or ovens, portable space heaters, sewing machines or sergers, vacuum cleaners and electric brooms
TVs and VCRs/DVDs, CD players, electronic games, all remote controls, CB radios
LAN, cordless and cell phones, pagers, walkie-talkies, electronic calendars, patient alert devices, OnStar by GM™ and/or GPS (global positioning system)
Smartphones and smartwatches and other electronic devices may interfere with implanted heart devices especially when held close to the device. Keep at least 6 inches between the device and phone or watch.
Ask your healthcare team and/or device company about induction cooktops in your kitchen. Most people are told to stay 2 feet away from the heating zone when it is turned on.

Some devices also have magnets inside which can trigger the magnet effects if held over the device. With pacemakers this can trigger the magnet rate. With ICDs, this can temporarily inhibit the ICD therapy. Magnets and devices with magnets should keep at least 6 inches away from any pacemaker or ICD.*
*https://www.heart.org/en/health-topics/arrhythmia/prevention--treatment-of-arrhythmia/ devices-that-may-interfere-with-icds-and-pacemakers
Microwave Ovens: You may still see warning signs near microwave ovens, but these relate to pacemakers made in the 70’s. Today’s microwaves are safe for people with a pacemaker or an ICD. You don’t need to be concerned about them.

Small Appliances: toasters, blenders, electric knives, electric can openers and food processors
Computers (hand-held, laptop and other), printers, scanners, copy and fax machines
Other: curling irons, shavers, electric blankets, heating pads (if not placed directly over the device), pest control or home security systems, tanning beds, golf carts, electric vehicle chargers or electric wheelchairs, treadmills, air purifiers, electric invisible fences, small magnetic pain therapy products (Ex: bracelets, slippers, shoe insoles and chair pads)
If you have questions about appliances, tools or other electrical devices, you can ask your healthcare team or call your device company at the telephone number shown on your device ID card. Ask for technical support.
Anything that uses electricity, batteries and/or contains magnets has an electromagnetic field. Most household appliances have very weak electromagnetic fields so almost none of them affect a cardiac device.
Your pacemaker or ICD is likely to ignore weak electronic fields. But just to be sure, avoid holding all electronics directly over your pacemaker or ICD. These suggestions may be helpful tips about keeping electronics away from your device:
Hold power tools so that they aren’t in direct contact with your pacemaker or ICD. (Examples: electric or cordless drill, electric screwdriver, soldering gun, jigsaw, radial arm and table saws, and electric hedge clipper.)

Place massagers or heating pads anywhere on the body as long as you avoid the area directly over the cardiac device.
Do not lean closely over spark-ignited motors when turned ‘on’, such as in a car, lawnmower, leaf or snow blower, tractor or boat.

The metal case of a pacemaker or ICD can trigger an alarm as you walk through a security detector. Keep your device ID card with you when shopping or going through security systems like in an airport, store, government building or school. Ask your healthcare team if it's ok to go through a security detector.
Walking through the electromagnetic field of a security detector or having a handheld wand waved briefly over your body will not damage or reset your device. It's best to keep wand 6-12 inches from the device. However, do not stand or lean against the outside or inside of a security detector for any length of time.
Electromagnetic interference (EMI) can affect the operation of your device, especially an ICD. Long periods of EMI can cause you to feel dizzy or notice your heart is beating too fast. Some devices give off beeping tones or vibrations when you are near a magnetic field. Moving away from the equipment is often all that’s needed. Usually, any symptoms go away and the device tones or vibrations stop. Let the device clinic staff know. In some cases, strong and long-lasting EMI might change the device settings or rarely, damage the device.
EMI can occur if you are very near any of these:
power plants, large generators and power transmission lines and buildings
restricted access areas of radar or radio/TV broadcasting antennas
strong magnets (i.e., junkyard magnets used to lift cars)
Magnetic resonance imaging (MRI or MRA*) is possible in patients with either a pacemaker or an ICD. Newer cardiac devices ARE approved for MRI as long as they are paired with a suitable lead system.
Ask your healthcare team if your device and the leads are OK for MRI. Show your device ID card and pass on what you are told to any doctor you see, especially in an emergency situation if MRI is mentioned. Any doctor can follow up with the company as needed 24/7.
If your device and lead system are NOT OK for MRI, many hospitals will not do the MRI. If an MRI is crucial at some point, your doctor may ask you to see an electrophysiologist (EP doctor). Sometimes they can make device changes and supervise an MRI procedure to reduce the risk of MRI to the device. These MD's have a lot of experience with MRI in patients with devices. Research continues to see if MRI or MRA can be done safely in more cardiac devices.

Some device companies suggest you also avoid abdominal stimulators, electric body fat scales and magnetic mattresses, chairs, pillows, and TENS machines.
Check with your healthcare team and/or device company before operating chain saws, electric arc welders or heavy industrial equipment.* Some device companies also say to keep at least 3 feet away from residential transformers and avoid using a jackhammer.
Since the thermal cautery in many medical and dental procedures can interfere with your pacemaker or ICD, always tell any doctor and dentist that you have a pacemaker or an ICD.
* Examples of heavy industrial equipment include dielectric heaters (used to bend plastic), electric steel furnaces, induction furnaces (such as kilns) and any large industrial magnets.

You can live a normal life and enjoy the benefits of having a pacemaker and/or ICD.

Keep all appliances and electrical equipment you use in good repair.
Your pacemaker and/or ICD can ignore the weak electromagnetic fields of most household and everyday electronics. But it’s a good idea NOT to hold electronics directly over your cardiac device.
Many pacemakers and ICD's ARE ok for MRI as long as they are paired with a suitable lead system. Ask if your system is MRI safe.
When you have a question about electronics and cardiac devices, ask your doctor and/or device manufacturer. Use the device manufacturer’s website (list on inside back cover) or call the customer service number on the back of your device ID card.
They can modify these instructions or tell you what precautions you need to take.
Your cardiac device is expected to last many years before replacement is needed. Pacemakers often last longer than ICD’s. Replacing a device that is under the skin often means removing the old one and slipping a new device in the same pocket. The leads can often be left in place as they last much longer than the pacemaker or ICD. Most pacemaker and ICD guidelines require some type of in-person or remote system evaluation every 3 months.
How often you need medical follow-up depends on:

your medical condition
routines set by your doctor or clinic
the length of time the device has been in place
Each cardiac device company has a programmer for its pacemakers and ICDs. During surgery, your doctor uses it to turn on your cardiac device and make the initial settings.
The programmer is used during follow-up visits to get information from your device. (This is often called “interrogating” your device.) The programmer can do one or more of these:

check device and lead functions (including the remaining ‘battery’ life)
change the settings (speed, energy, timing of signals between chambers, etc.)
retrieve stored heart rate data and electrograms (a type of ECG) that show how the device has been working
Using the programmer does not cause any pain and gives data about your heart's activity and device responses. Sometimes changes in the settings help your device work better for you and/or make it last even longer.

Doctor or clinic visits are still needed after someone gets a cardiac device. However, home monitoring of your pacemaker and/or ICD is often done between visits to keep up with how your device is working. This may allow fewer trips to the doctor’s office or clinic. Data from today's pacemakers and ICDs is often sent through the internet to be downloaded to your doctor's office or device clinic.
All devices implanted have the ability to be monitored remotely. Remote monitoring can be performed by either a special monitor the company will provide you or through your internet connected smart phone. If your device can connect to a smart phone, you will be instructed how to install the application on your phone and connect to your device. Instructions for connecting are fairly easy for the first connection (pairing). Once that is done, transmissions are sent automatically. Remote monitoring is not continuous monitoring. The transmitter will transmit at a certain time.
There are some devices that do not transmit automatically. You will need to transmit as instructed by your healthcare team or clinic.
phone line, cellular or internet connector
phone line, cellular or internet connector
If your pacemaker or ICD has the wireless feature, all you have to do is be within a few feet of the transmitter during the night when the cardiac device ‘wakes up’ for the transmission.
If your cardiac device does not have the wireless feature, you will need to hold a disc-shaped antenna (often called a wand) over the device during transmission.
Cellular adaptors or built-in cellphone technology will transmit if you do not have a physical phone line.
to
Your healthcare team can view the data on the company’s secure website and download a full report. Internet-based device data cannot be accessed by anyone but your doctor or device clinic. Your doctor’s office has to verify their user name and password to get the information.
Some people who have a pacemaker and/or ICD also have a chronic heart problem (Ex: heart failure). Trends in this data may allow a physician or nurse to intervene early and delay or prevent hospitalization.
Pacemaker and ICD patients usually can travel as they wish. Be sure to take the medicines you will need, plus some extra, in case of a travel delay. You may want to take your home monitoring equipment with you when traveling.

Keep your Medical Device Patient Card with you at all times while traveling. This card explains the fact that your device may trigger an alarm at airport security. Show your device ID card before going through security. A body search is best, but a brief walk through the upright unit or a brief waving of the hand-held wand over your device will not be a problem. The device companies have seen no problems with the new body scanner machines. Avoid periods of standing inside a walkthrough security device or leaning against the outside of it.
ICD patients traveling outside the US should look on the website or contact their device company for a list of doctors/hospitals using their products in other countries.
Contact your healthcare team if you have other travel questions. Visit your device company website for more information on travel.
Carry the device ID card with you at all times.
This names the company that made your pacemaker or ICD. If you have to go to the hospital, have any surgery or change doctors or dentists, tell the person treating you about your device. Updating your device company records with any changes in doctor name or your address is also a good idea.

Get an ID bracelet or necklace to make it easier for health providers to find out you have a cardiac device. Pick a bracelet or necklace with enough space to list the cardiac device and any other important items. (Be sure telephone service is available 24/7 if everything doesn't fit on the item your choose.)
See inside back cover of this booklet for resources.
Getting used to a pacemaker is often easier than to an ICD. With an ICD, you have to deal with knowing you could get an electrical shock if needed. While drugs often prevent abnormal heart rhythms, those who have had shocks describe them as unpleasant, but brief. People may feel dizzy or weak when a fast rhythm comes on, and should sit down if they notice this.
Although most people can resume normal daily activities after full recovery from ICD surgery, your doctor will say when you should drive. If you lost consciousness before your ICD rescued you (or if you have several shocks in a short period of time), your doctor will ask you not to drive for the time being. Be sure to follow your healtcare team’s advice about driving, since there are legal risks if you have a car accident when driving against the doctor’s advice.

Since an ICD shock is often a surprise, your doctor may ask that you look for ways to prevent serious falls. It is a good idea to have someone with you during things like swimming, diving, using a ladder or hiking. Warm-up and cool-down exercises along with limiting your intensity can help avoid abnormal heart rhythms. Driving may be restricted up to 6 months.
Learning more about your pacemaker or ICD can be very helpful. Some people go to an ICD support group to find out what to expect and how to adjust to the device. Others enjoy reading patient or family interviews or newsletters from their device company.
Knowing that your ICD is likely to stop a life-threatening heart rhythm can be a huge comfort. Some people never need a shock from their ICD but enjoy the protection it offers. With an ICD, you have protection that no one else has against sudden cardiac arrest. Since drugs often prevent abnormal heart rhythms, people with an ICD should take extra care not to miss a dose. Many find a daily or an electronic pillbox helpful.

Yes, both pacemakers and ICDs are under the skin and often visible. The leads from the device to the heart are very thin and often can’t be felt once the incision has healed. There is plenty of extra lead for body movement. But don’t “twirl” your device around in the skin pocket. Twirling would move the lead(s) away from contact with the heart. Leadless pacemakers are placed through a vein inside the heart and do not require a chest incision. They do show up on a chest x-ray.
The company that made your device will mail you a permanent ID card within 6-8 weeks. Call your doctor's office or device clinic if you don't receive your card after 8 weeks. You will receive a temporary ID card before leaving the hospital. This names the company making your device along with serial numbers for both your device and lead(s). Carry the card with you at all times.

Always follow the advice of your healthcare team and device manufacturer. Some cardiac devices ARE MRI-compatible but many are not. But most devices are not affected by routine tests like mammography, X-rays, CT scans and ultrasound. During some surgery and radiation therapy, settings on your device may need to be changed. If a TENS unit is needed for pain control, your doctor may test to see if the TENS unit affects your device. Once the TENS unit settings and electrode placements are made, do not change them without your doctor’s OK.

Small electrical signals (pacing) prompt the heart to beat and/or try and stop a fast rhythm. ICD’s send large electrical signals (shocks) to stop dangerous heart rhythms and allow the return of a normal heartbeat. When the heart no longer responds to these signals from the pacemaker/ICD, it stops pumping blood and a natural death occurs. A pacemaker or ICD can be removed or left in place before burial. It does NOT need to be turned off if left in place. Cardiac devices must be removed before cremation. Turning off an ICD prior to funeral home personnel removing it helps prevent accidental shocks.
Pacemakers and ICDs should last between 7-12 years. Each device company has a warranty period for their device. Devices last longer or shorter due to the amount of pacing or shocks necessary. Follow your healthcare team and device company’s advice for checking your ICD (usually every 3 months). The device programmer and remote home monitoring can tell when the battery power starts to drop.
Why do I have an ICD? What makes my doctor so sure I have a heart problem?

If you have an ICD, your doctor has found that you are prone to life-threatening abnormal heart rhythms. Sometimes an electrophysiology test (EP study) is used to see if life-threatening rhythms are likely. Many times drugs can prevent fast abnormal heart rhythms. When drugs don’t work, an ICD can often stop the abnormal rhythm and allow the return of a normal heartbeat.
What happens to anyone touching me if my ICD goes off during exercise or sex?
If your ICD does deliver a shock while you are touching someone else, they may get a minor tingling sensation. They would not feel the same impact of a shock that you do.
An abnormal rhythm can occur at any time. It’s rare for an ICD to deliver an unneeded shock to a fast, natural heart rhythm. Your doctor considered that in choosing the ICD rate settings. Often your doctor will use the programmer to learn about the heart rhythm at the time of a shock. If the rhythm leading to the shock was a fast, normal heartbeat, the ICD settings or your medicines may be changed.
Every device company has a point in the life of the device when the battery power reaches what’s called the ERI (Elective Replacement Indicator) or RRT (Recommended Replacement Time). It is not until this is reached that replacements will be scheduled. At this point there is at least 3-months of battery life left. You and your health care team can schedule a good time to replace your Pacemaker or ICD while it is still working properly.
Some devices send out beeping tones to alert you about a nearby large magnetic field. Some devices send out beeping tones or vibrations to alert you about a low battery status or possible lead or battery problems. In either case, let your device clinic know.

As with most things, the fear of getting the first shock usually goes away as you return to usual activity. Some people dream that they’ve gotten a shock and later learn from their doctor that the device didn’t go off. Some even get angry at the ICD. Negative feelings toward the ICD may also include sadness about having a heart problem. Some people have trouble sleeping, eating or getting back to normal activity. Most have emotions like fear, anger and sadness, at times doubting if the ICD is really needed. Handling your feelings and getting your confidence back often takes time. Most learn over time to think of their ICD as an important security measure.
Find ways to cope that have helped you in the past. Some people use humor to reduce stress – things like giving their ICD a funny name or making jokes about being the “Ever-ready bunny” or “a bionic man or woman.” Others cope well with this stress by taking long walks, exercising, getting a massage, as well as sharing feelings with family, friends or a professional. It also may help to read and learn more about life with an ICD and think about the device in a positive way.
A support group or reading about others’ experiences with an ICD can be very helpful as you discover you are not alone. With time, most people stop being afraid of having a shock and find comfort in knowing that an ICD will intervene if there is a life-threatening heart rhythm. Keep your doctor aware of any strong emotions about an ICD, especially if they last longer than the first few months.
Use this space to ask the questions you need from your doctor or nurse:
What company made my device?
Abbott Biotronik Boston Scientific
Medtronic MicroPort Other:
What type of device do I have?
Pacemaker
Leadless: Single: Dual:
Single chamber: right atrium right ventricle
Dual chamber: right atrium right ventricle
left ventricle HIS conduction system
Biventricular: right atrium right ventricle
left ventricle HIS conduction system
ICD
Single chamber: right ventricle
Dual chamber: right atrium right ventricle
left ventricle HIS conduction system
Biventricular: right atrium right ventricle
left ventricle HIS conduction system
Subcutaneous ICD (S-ICD):
Rate responsive sensors:
Heart sensing:
Breathing:
Body movement:
What to do if the ICD delivers a shock? Call
Dial 911 if you feel dizzy after a shock.
Can I have an MRI? (See page 25.)
What type of follow-up monitoring will I need?
Internet-based remote home monitoring:
Telephone transmission (some pacemakers):
How will I get the monitoring equipment?
Office/clinic visits:
Incision care:
Arm activities in the first few weeks:
First provider/doctor appointment:
Return to work/driving:
Other:
You can find more information about your device by looking at your pacemaker and ICD company web sites. Look on the back of your device ID card to identify which company made your device.
Biotronik
www.biotronik.com
(800) 547-0394
Boston Scientific www.bostonscientific.com
(800) 227-3422
MicroPort (Sorin, LivaNova)
www.microport.com
(312) 635-6602
General information is also available at www.hrspatients.org.
Medtronic www.medtronic.com
(800) 633-8766
Abbott (St. Jude Medical) www.abbott.com
(651) 756-5400
Ask your doctor about local ICD support groups. Consider purchasing medical ID jewelry like offered by MedicAlert, www.medicalert.org, 1-888-432-5378.



