j our nal e
Changes







DHShas released its first annual report on how the No Surprises Act is impacting health care markets, and the results are both surprising and expected.
Among the crucial findings are the decrease and concentration of out-of-network billing, both claims and the total amount associated with those claims; trends regarding changes in hospital ownership; and horizontal consolidation and pass-through costs to consumers
Join us as we analyze the findings and what they mean to the industry going forward We will also discuss the key factors that play a role in the DHS?evaluation of NSA and what they might mean for market trends, consolidation, and out-of-network billing.

Leading the series is CorroHealth?s resident subject matter expert, Barbara Johnson, BSN, RN ? Senior Revenue Consultant. As a registered nurse Johnson worked in emergency medicine before transitioning into nursing administration She entered the specialty of Revenue Integrity as a nurse auditor where she expanded her knowledge of coding and revenue cycle compliance through membership in AAPCand HFMA Today, she is CorroHealth?s leading subject matter expert on NSA.

You can cat ch up here!
CorroHealth?s ?No Surprises Act and Price Transparency, a New Monthly Series?was created to provide attendees with clarity around No Surprises Act, to answer questions, and get you on the best path for success The series also clarifies payers?increased role in the process, the status of impactful legislation, and the processes providers should follow to comply


Contact Your State's Account Executive.




Quest ion:
We need some information regarding billing for xylocaine with epinephrine in the physician office setting Specifically, are charges based on units or volume, and can xylocaine w/epi be charged in conjunction with an in-office surgical procedure?

It was our understanding that local anesthetic use is an inherent surgical procedure component, which is not separately billable Are there any circumstances in which it is separately billable in the office setting?

Answ er:
First, there are different reimbursement rules for a freestanding physician clinic than a provider-based clinic/outpatient department of a hospital.
Whether the clinic is freestanding or provider-based, the administration of the local anesthetic is indeed ?integral to?the surgical procedure. The provider should not charge 96372THERAPEUTIC, PROPHYLACTIC, ORDIAGNOSTICINJECTION (SPECIFYSUBSTANCEORDRUG); SUBCUTANEOUSORINTRAMUSCULAR.
A provider-based clinic (reporting facility fees on the UB/837i claim form) can report the pharmacy charge, but lidocaine with epinephrine will be low cost, ergo status N under OPPS. Under OPPS, Medicare and managed Medicare payers will not pay a facility fee for status N drugs, payment is packaged to the other payable lines on the same facility fee claim Pharmacy charges without a HCPCSare reported under rev code 0250 (Of course, a CAH gets paid for every line item that is a covered service, even low cost drugs or supplies, on the CMScost-based reimbursement methodology.)
A freestanding clinic may opt to report a pharmacy charge for the anesthetic drug itself on a separate line of the 837p professional fee claim form. However, it?s not always worth it to go to the trouble. Low cost drugs like lidocaine are more trouble to bill than they?re worth in reimbursement on a professional fee claim
Under MPFS, Medicare pays a professional fee claim 837p for drugs with HCPCSaccording to the rules set forth in Chapter 17 of the Medicare Claims Processing Manual (MCPM)
Attached a PDFdocument which provides the pertinent excerpt from that chapter
Unlike a UB04/837i, a pro fee claim 1500/837p must report a HCPCSor CPT® code on each and every charge line For drugs without a HCPCS, professional fee claims may report the Unclassified Drug HCPCSJ3490, but the claim must indicate the dose and NDCof the drug in the remarks field on the pro fee claim. The MACwill evaluate the note and decide whether/what to pay on that line
Lidocaine is assigned J2001, and epinephrine is J0171 ? and although the combination of the two drugs is available as an SUVinjectable, I didn? t find a HCPCSassigned for the combination medication. You could offer to double-check if CarolinaEast can provide an NDC.

You can find the reimbursement rates under Part B for physician claims for the two HCPCS J2001 and J0171 on the Calculator using the Medicare Part B Drug Payment Allowance report


Neither Lidocaine nor epinephrine are going to yield much in payment:

Bottom line, a lot of drugs are more trouble to bill than they?re worth in reimbursement on a professional fee claim

Many facilities bill diagnostic vascular ultrasound services from the referring physician?s order as an automated process, without any review by a coding professional This practice can result in an inaccurate code if the interpreting professional fails to meet the specific documentation requirements for vascular ultrasound examinations.
The radiology report serves as the documentation for both the professional and technical portions of the examination The documentation within the medical record must support the exam that was performed--both for the professional fee (the radiologist?s interpretation) and the technical fee (the technologist?s work of performing the exam). It is the reading radiologist?s responsibility to ensure the components of each diagnostic ultrasound exam performed are documented appropriately in the radiology report
The CPT® guidelines state that all diagnostic ultrasound studies require the following:
- Permanently recorded images with measurements (when such measurements are clinically indicated)
- A final, written report to be issued for inclusion in the patient?s medical record
Per CPT® , ?Use of ult rasound, w it hout t horough evaluat ion of organ(s) or anat om ic region, im age docum ent at ion, and final, w rit t en report , is not separat ely report able.?
Duplex and Doppler scans can be perplexing due to redundant terminology and lack of necessary documentation.
Both non-invasive vascular studies and duplex scans use Doppler ultrasound to evaluate blood flow in the vessels.

The CPT® manual specifies two required capabilities for Doppler units:
- Producing hard copy output (printable waveforms)
- Allowing bidirectional flow analysis (some handheld Doppler units are able to identify a blood vessel by verifying the presence of flow, but cannot assess the direction)
Doppler exams performed without these characteristics are considered part of the patient's physical exam and should not be reported separately.
A duplex scan is a vascular ultrasound that examines the characteristics (such as speed and direction) of blood flow in a vein and/or artery. It merges real-time imaging (2D B-mode ultrasound) with two modes of Doppler ultrasound: spectral Doppler and color Doppler. Color Doppler produces a color image of the vessel overlaid on a B-mode ultrasound image, showing both structure and blood flow velocity and direction

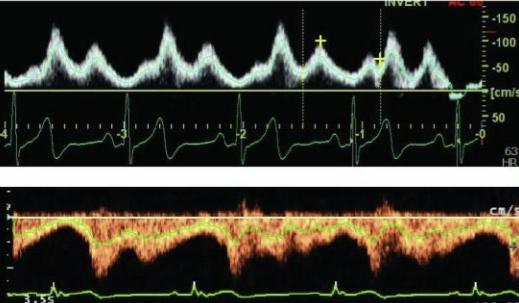
Spectral Doppler presents a graphic display of Doppler data, with jagged vertical lines called waveforms representing flow velocity The vertical axis shows flow velocity in centimeters per second. Higher spikes represent more rapid within blood flow in the vessel. Spectral and color Doppler must both be performed and documented to substantiate a duplex code.
Per the CPT® manual, a duplex scan requires ?real-time images integrating B-mode two dimensional vascular structure, Doppler spectral analysis, and color flow Doppler imaging.? Per Clinical Examplesin Radiology(Winter 2015), when color Doppler is performed alone (without spectral Doppler) to visualize anatomic structures with concurrent real-time ultrasound, it is included in the non-vascular ultrasound code
For example, if the technologist quickly turns on the color Doppler to evaluate for flow in the scrotal arteries during a testicular ultrasound, only the testicular UScode (76870) should be reported According to CPT® Assistant, March 2015, a duplex scan may be reported in addition to a non-vascular diagnostic ultrasound of the same anatomic site (e g , 93975 with 76700) when both services are performed and documented appropriately.
Duplex scanning should not be regularly performed on every patient who receives a diagnostic ultrasound study According to Clinical Examplesin Radiology(Winter 2013), if there is no order from the referring physician for a duplex scan, there must be ?a detailed explanation by the radiologist in [their] report as to why the Doppler was medically necessary.?
The radiologist should detail the exam protocol in their documentation to facilitate correct billing and prevent complications in the event of an audit. As indicated in Clinical Examplesin Radiology(Spring 2012):
?At the very minimum, the technique part of the report should state that ?AduplexDoppler studywasperformed.?Ideally, it should state, for example, ?AduplexDoppler studywas performed, consistingof integrated two-dimensional (2D) real-timeimaging, color flowDoppler, and Doppler spectral analysisutilizing5.0 MHz and 7.0MHz linear arrayprobes.?The body of the report should optimally describe that normal flow, compressibility, and augmentation were demonstrated on Doppler spectral analysis.?
If the radiologist explicitly says that a duplex study was done, the performance of a B-mode 2D US, color Doppler, and spectral Doppler is inferred. If the physician does not indicate performance of a duplex study, both color flow and spectral Doppler must be clearly documented in the report
Clinical Examplesin Radiology(Spring 2012) indicates that documentation of color Doppler without mention of spectral Doppler does not adequately support the assignment of a duplex code Additionally, Clinical Examplesin Radiology(Spring 2007 and Spring 2008) contain detailed examples of how to appropriately document interpretation of these studies within the radiology report.
The American College of Radiology Ultrasound CodingUser?sGuide identifies examples of terminology that would support performance of a Doppler examination:
- Analog velocity
- Bandwidth broadening
- Monophasic
- Peak systolic velocity
- Phasicity
- Power Doppler
- Pulsed Doppler
- Pulsatility
- Resistive index
- Spectral analysis
- Spectral broadening
- Spectral Doppler
- Tardus parvus waveforms
- Triphasic
- Velocity
- Duplex Doppler
Vascular ultrasound, as with other diagnostic USstudies, requires that permanent images be obtained and archived in the medical record or PACS. It is not required that the report document that permanent images were acquired. However, it is recommended that the provider or facility document this information
The technique must support the performance of a duplex exam, but the report must also identify the presence, absence, or other characteristics of blood flow in the vessels being assessed Per Clinical Examplesin Radiology(Spring 2020), specific information pertaining to the flow parameters, waveforms, velocities, or resistive indices may be recorded when the interpreting physician deems them significant.
There are specific CPT® codes for non-invasive vascular ultrasound of certain anatomic areas. These include the cerebrovascular arteries (93875-93888), extremity arteries (93922- 93931), extremity veins (93965-93971), visceral arterial inflow and venous outflow (93975- 93981), and hemodialysis access scanning (93990)
If a limited bilateral non-invasive vascular ultrasound study of the extremities is performed, choose the appropriate code from the ?unilateral or limited study?codes (93926, 93931, 93971) These codes correspond to unilateral (or limited unilateral) studies, but also to limited bilateral studies When both the upper and lower extremities are evaluated, two units of the
If a limited bilateral non-invasive vascular ultrasound study of the extremities is performed, choose the appropriate code from the ?unilateral or limited study?codes (93926, 93931, 93971) These codes correspond to unilateral (or limited unilateral) studies, but also to limited bilateral studies When both the upper and lower extremities are evaluated, two units of the appropriate code should be reported
If both non-vascular diagnostic ultrasound and duplex are performed, both must be medically necessary and meet CPT® documentation requirements for the technique and structures identified. It is recommended that the radiologist dictate separate reports for the two studies, or at least describe the two studies under separate headings / paragraphs within the same report If a combined report is issued, the content of the documentation for each USshould align with the typical documentation for when they are performed as stand-alone exams.
Under National Correct Coding Initiative (NCCI) edits, certain non-vascular diagnostic ultrasound codes are bundled into the duplex study code for the same anatomic area. Append modifier -59 or -XU to the non-vascular ultrasound code when a complete, separate, medically necessary study is performed and documented The National Correct Coding Policy Manual, Chapter 9 states:
?Abdominal ultrasound examinations (CPT® codes 76700-76775) and abdominal duplex examinations (CPT® codes 93975, 93976) are generally performed for different clinical scenarios, although there are some instances where both types of procedures are medically reasonable and necessary. In the latter case, the abdominal ultrasound procedure CPT® code should be reported with an NCCI PTP-associated modifier.?
Clinical Examplesin Radiology(Summer 2012) dictates that while a duplex study falls under the "test design" exception to Medicare?s regulations for ordering diagnostic tests (and thus does not require a physician order), it is essential to review individual payer policies, as not all will align with this explanation

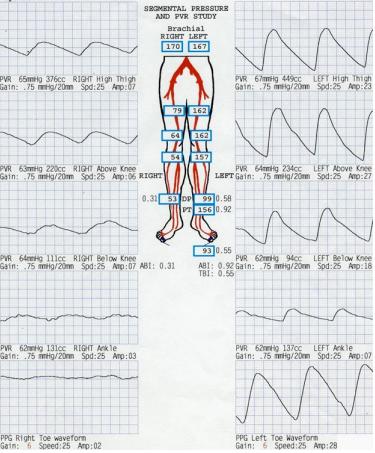
Non-invasive physiologic studies (NIPS) are functional measurement studies that examine and confirm vascular insufficiency and occlusive disease without imaging These studies include ankle-brachial index (ABI), Doppler analysis, plethysmography, and oxygen tension measurements. The ABI evaluates circulation in the extremities using a blood pressure cuff and a handheld Doppler unit. Blood pressure measurements are taken at various arterial sites, and the ABI is calculated based on the systolic pressure readings ABIs performed alone without any other physiologic studies are not separately reportable, as CPT® includes them in the provider's evaluation and management service.
Many Medicare contractors have released Local Coverage Determinations (LCDs) and/or Supplemental Instruction Articles for vascular ultrasound, which include instructions on coverage and billing for each MAC. Prior to billing for these services, it is essential to review local policy
Most insurance providers do not allow reimbursement for both a duplex scan and a noninvasive physiologic study on the same anatomic area. Some payers have expressly indicated that physiologic testing will not be covered if a duplex study has already been conducted
For example, Cigna?s policy appears on the next page:


Having a clear understanding of the technology and terminology associated with duplex and Doppler exams is vital for ensuring appropriate documentation, charging, and billing for these services

For additional information, please see the following PARA Papers, also available in the Advisor tab of the PARA Data Editor.
Q&A: Upper and Lower Extremity Venous Duplex
Q&A: Duplex Ultrasound
Q&A: Duplex Scan
Ultrasound Documentation Requirements: Complete vs Limited
Ultrasound Guidance in the Hospital Setting


On July 13, 2023, the Centers for Medicare & Medicaid Services (CMS) proposed Medicare payment rates for hospital outpatient and Ambulatory Surgical Center (ASC) services. The Calendar Year (CY) 2024 Hospital Outpatient Prospective Payment System (OPPS) and ASC Payment System Proposed Rule is published annually and will have a 60-day comment period, which will end on September 11, 2023 The final rule will be issued in early November
In addition to proposing payment rates, this year?s rule includes proposed policies that align with several key goals of the Administration, including promoting health equity, expanding access to behavioral health care, improving transparency in the health system, promoting safe, effective, and patient-centered care, and addressing medical product shortages. The proposed rule advances the Agency?s commitment to strengthening Medicare and uses the lessons learned from the COVID-19 PHEto inform the approach to quality measurement, focusing on changes that will help address health inequities It also seeks comment on potential payment adjustments to hospitals for the additional costs of establishing and maintaining a buffer stock of essential medicines in order to help curtail shortages of these medicines in the future
These proposed payment policies will affect approximately 3,500 hospitals and approximately 6,000 ASCs. The hospital price transparency proposed policies impact over 7,000 institutions that are licensed as hospitals As with other rules, CMSis publishing this proposed rule to meet the legal requirements to update Medicare payment policies for OPPShospitals and ASCs annually.

This fact sheet discusses the major provisions of the proposed rule (CMS-1786-P), which can be downloaded at:
https://www federalregister gov/public-inspection/2023-14768/medicare-program-hospital -outpatient-prospective-payment-and-ambulatory-surgical-center-payment

Quest ion:
In Physical Therapy, the Physical Therapists and Physical Therapy Assistants are required to dcoument pain levels in their notes Is this also true for Speech Therapists as well?
Answ er:
Pain level is generally not a standard requirement for a speech therapy assessment; however, providing relevant information on pain or discomfort observed during speech or related activities is essential

The following website can provide more detailed guidance and information
https://www asha org/

Transitional Care Management (TCM) services play a crucial role in ensuring smooth and successful care transitions for patients moving from an inpatient hospital setting to their home or a community-based care facility. These services focus on coordinating and managing the patient's healthcare following a critical period after discharge. The aim of TCM is to reduce complications, improve outcomes, and enhance patient satisfaction Proper coordination and management of patients during the immediate post-discharge period may also reduce readmissions
KeyComponentsof TCM:
- Face-to-Face Visit
Following a patient's discharge from an inpatient hospital stay, a face-to-face visit is conducted within 7 or 14 days, depending on the complexity of the medical decision-making involved. During this visit, the physician evaluates the patient's medical condition, reviews the discharge summary, reconciles medications, and develops a comprehensive care plan.
- Communication and Care Coordination:
TCM services involve substantial communication and coordination between the physician, patient, and other healthcare providers This includes arranging necessary follow-up appointments, collaborating with specialists, and facilitating communication between the hospital and post-discharge care settings
An important aspect of TCM is reconciling and managing medications during the transition This involves reviewing the patient's medication list, addressing discrepancies, providing education on medication usage, and addressing any potential adverse effects or interactions


The physician, in collaboration with the patient and other members of the healthcare team, develops a comprehensive care plan tailored to the patient's specific needs and goals This plan includes instructions for follow-up care, self-management strategies, and coordination of additional services.
It is important to ensure accurate coding and documentation to support the services provided Here are some key considerations:
- Eligibility: TCM services are typically eligible for Medicare reimbursement Ensure that the patient meets the specific criteria set by Medicare or other payers for TCM services, including a face-to-face visit within the specified timeframes
- Documentation: Accurate and detailed documentation is essential to support the medical necessity of TCM services. Documentation must include the complexity of medical decision-making, the coordination efforts involved, medication reconciliation, and the development of a comprehensive care plan Reimbursement: TCM services are typically reimbursed separately from the Evaluation and Management (E/M) services provided during the face-to-face visit Ensure that the appropriate TCM codes are billed separately from any E/M codes to avoid duplication of services See CorroHealth TCM, CCM, RPM, PCM Table.
- Reimbursement: TCM services are typically reimbursed separately from the Evaluation and Management (E/M) services provided during the face-to-face visit Ensure that the appropriate TCM codes are billed separately from any E/M codes to avoid duplication of services See CorroHealth TCM, CCM, RPM, PCM Table
- Reporting:
- Transitional Care Codes 99495 (TCM? within 14 calendar days of discharge) or 99496 (TCM? within 7 days of discharge) may be reported by the same practitioner during the 30-day TCM service period as Chronic Care Management codes 99487 (CCM? multiple? first 60 minutes of clinical staff time directed by a physician or other qualified healthcare professional), 99489 (CCM? multiple? first 30 minutes of clinical staff time directed by a physician or other qualified healthcare professional) or 99490 (CCM? multiple? first 20 minutes of clinical staff time directed by a physician or other qualified healthcare professional)
- An RHCand FQHCmay bill TCM services and general care services for the same patient during the same service period if they are reported following the requirements for the code(s) billed.
- Shared or Incident-to-Billing: When performed in a clinic setting, some TCM services may be billed under the supervising physician or as incident-to-services. Understand the billing guidelines applicable to the practice and ensure compliance with the relevant regulations
- Consent: Obtain written consent from the patient for TCM services, explaining the scope and nature of the services, as well as any associated cost-sharing requirements.
Remote Physiologic (or Patient) Monitoring (RPM) services have emerged as a powerful tool in healthcare, enabling the continuous monitoring of patients?health status and providing timely interventions RPM is a collection and analysis of physiologic data transmitted from the patient electronically to the healthcare provider for assessment RPM allows real-time opportunities for assessment and the ability to view trends over periods of time.
KeyComponentsof RPM:
- Remote Monitoring Devices:


RPM services rely on the use of remote monitoring devices that collect and transmit patient health data. These devices can include blood pressure monitors, glucose meters, pulse oximeters, weight scales, and wearable devices The data collected from these devices is securely transmitted to healthcare providers, allowing for continuous monitoring and assessment
- Data Transmission and Analysis:
RPM services involve the transmission of patient data from remote monitoring devices to healthcare providers or a designated monitoring center. Healthcare professionals review and analyze the data to identify trends, deviations, or any potential health concerns This allows for early intervention and proactive management of the patient's condition
- Care Coordination and Interventions: RPM services enable healthcare providers to coordinate care effectively and provide timely interventions. They can communicate with patients remotely, provide education on self-management, adjust treatment plans as needed, and address any concerns or questions raised by patients The goal is to optimize patient care and improve health outcomes

Consent: Obtain written consent from the patient for RPM services, explaining the scope and nature of the services, as well as any associated cost-sharing requirements
- Eligibility: RPM services are typically eligible for reimbursement from Medicare and some private payers Ensure that the patient meets the specific eligibility criteria defined by the payer, which may include having chronic conditions that require ongoing monitoring and management.
- Time-Based Billing: RPM services are billed based on the total time spent on care management activities during a calendar month This includes the time spent by clinical staff, physicians, or other qualified healthcare professionals in monitoring, reviewing data, and providing interventions. See CorroHealth TCM, CCM, RPM, PCM Table for more information
- Documentation: Accurate documentation is crucial to support the medical necessity of RPM services Document the time spent on care management activities, including review and analysis of data, patient interactions, and interventions provided. Additionally, maintain records of the types of monitoring devices used and the patient's consent for remote monitoring
- Reporting services:
Most RPM services will be billed under service codes 99453/99454 and time-based codes 99457/99458
99453 (remote monitoring of physiologic parameter? .initial setup and patient education on use of equipment) may only be billed one time per patient
A provider may only bill 99454 (remote monitoring of physiologic parameters) one time per month regardless of how many devices are monitored. Reporting 99454 requires transmission and reading performed at least 16 days during the month

99458 (remote physiologic monitoring treatment management services? each additional 20 minutes) may be reported up to two times per month (once at 40 minutes, next at 60 minutes) after 99457 (remote physiologic monitoring treatment management services? each first 20 minutes) has been billed RPM codes may be reported during the same service period as CCM (99487-99490), TCM (99495-99496)

- Communication and Interactivity: To bill for RPM services, there must be interactive communication between the patient or caregiver and the healthcare provider This may include phone calls, video visits, or secure messaging platforms. Ensure that these interactions are properly documented.
Chronic Care Management (CCM) services play a vital role in providing comprehensive and coordinated care for patients with chronic conditions These services aim to improve patient outcomes, enhance patient engagement, and reduce healthcare costs associated with managing chronic illnesses.
KeyComponentsof CCM:
- Care Planning and Coordination: CCM services involve the development of a personalized care plan tailored to the patient's chronic conditions. This plan encompasses an assessment of the patient's health needs, the establishment of goals, and the coordination of care across multiple healthcare providers Care coordination may include regular communication, scheduling appointments, and sharing health information to ensure a seamless healthcare experience
- Communication and Remote Patient Monitoring (RPM):
Effective communication between healthcare providers and patients is crucial for successful chronic disease management CCM services often involve regular telephone or electronic communication between the patient and the healthcare team Additionally, the use of remote patient monitoring devices, such as blood pressure monitors or glucose meters, can provide valuable data to assess the patient's condition remotely
Ensuring proper medication management is essential in chronic care CCM services may include medication reconciliation, monitoring adherence, and providing education to patients about their prescribed medications This component helps optimize medication regimens, minimize adverse effects, and improve treatment outcomes.



CCM services aim to provide patients with increased access to care and enhance continuity. This includes same-day or next-day appointments for urgent needs, extended office hours, and 24/7 access to healthcare providers for urgent issues
Timely access to care helps manage exacerbations, address concerns, and prevent unnecessary emergency department visits.
- Eligibility: CCM services are typically eligible for Medicare reimbursement. Ensure that the patient meets the specific criteria outlined by Medicare or other payers for CCM services, such as having two or more chronic conditions that are expected to last at least 12 months An initiating visit is required for patients who have not seen the billing practitioner within the past 12 months
- Time-Based Billing: CCM services are billed based on the total time spent on care management activities during a calendar month. This includes both the time spent by the physician or other qualified healthcare professional and the clinical staff. CCM services are not typically face-to-face but require a minimum of 20 minutes of services before billing. See CorroHealth TCM, CCM, RPM, PCM Table for more information.
- Documentation: Accurate and detailed documentation is crucial to support the medical necessity of CCM services. Document the time spent on care management activities, details of care coordination efforts, medication management, and patient communication
- Reporting Services:
- CCM initial visit may be a Face-to-face evaluation and management visit, an Annual Wellness Visit (AWV), or an Initial Preventative Physical Exam (IPPE) for a patient the billing practitioner has not seen in the previous 12 months The practitioner must discuss the CCM with the patient If the initiating visit requires a comprehensive assessment and care planning, G0506 (Comprehensive assessment of and care planning by the physician or other qualified health care practitioner for patients requiring CCM services (billed separately from monthly care management services) (Add-on code, list separately in addition to primary service) may be billed as part of the initiating visit
- Both complex and non-complex CCM services cannot be reported for the same patient during the same calendar month 99491 (CCM? multiple? first 30 minutes provided personally by a physician or other healthcare professional) may not be reported in the same calendar month as 99487 (CCM? multiple? first 60 minutes of clinical staff time directed by a physician or other qualified healthcare professional), 99489 (CCM? multiple? first 30 minutes of clinical staff time directed by a physician or other qualified healthcare professional) or 99490 (CCM? multiple? first 20 minutes of clinical staff time directed by a physician or other qualified healthcare professional)
- Time included in a CCM service cannot be counted towards other billed time-based codes
- Transitional Care Codes 99495 (TCM? within 14 calendar days of discharge) or 99496 (TCM? within 7 days of discharge) may be reported by the same practitioner during the 30-day TCM service period as Chronic Care Management codes 99487 (CCM? multiple? first 60 minutes of clinical staff time directed by a physician or other qualified healthcare professional), 99489 (CCM? multiple? first 30 minutes of clinical staff time directed by a physician or other qualified healthcare professional) or 99490 (CCM? multiple? first 20 minutes of clinical staff time directed by a physician or other qualified healthcare professional)

- RHCs & FQHCs may report general care management once per month using G0511 for 20 minutes or more of clinical staff time devoted to TCM, CCM, PCM, chronic pain management (CPM) or Behavioral Health Integration (BHI) services provided by a qualified healthcare professional
- Consent:
Obtain written consent from the patient for CCM services, explaining the scope and nature of the services, that only one practitioner (per month) may furnish and bill the CCM services The patient should be notified of cost-sharing requirements
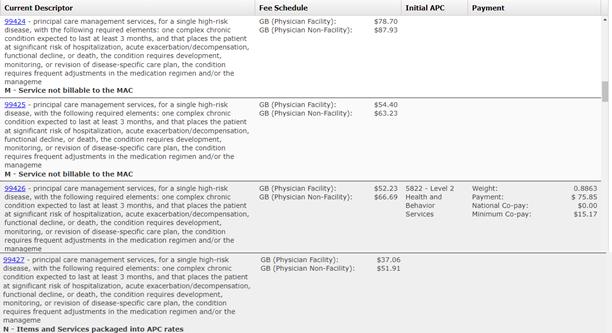
Principal Care Management (PCM) services are designed to furnish care to CCM patients who may have one or more chronic conditions with a focus on improving a single high-risk condition. PCM services involve the coordination and management of a patient's healthcare needs across multiple providers, ensuring continuity and seamless transitions between different care settings
KeyComponentsof PCM:
- Care Coordination:
PCM services involve coordinating and integrating healthcare services across different providers and settings. This includes facilitating communication between healthcare professionals, scheduling appointments, arranging necessary tests or procedures, and ensuring the timely exchange of medical information Effective care coordination enhances patient safety, reduces duplicative tests or treatments, and promotes the delivery of appropriate and timely care
- Patient Education and Self-Management Support:

PCM services emphasize patient education and self-management support to empower patients in managing their health conditions This component includes providing education on medication adherence, lifestyle modifications, symptom management, and self-monitoring techniques. By equipping patients with the knowledge and skills to actively participate in their own care, PCM services promote better health outcomes and improved quality of life
- Care Plan Development and Review:

PCM services involve the development and regular review of a comprehensive care plan tailored to the patient's specific needs and goals. The care plan includes a summary of the patient's health conditions, treatment goals, medication list, and recommended interventions. Regular review and updates to the care plan ensure that it remains relevant and aligned with the patient's evolving healthcare needs.
- Medication Management:
Effective medication management is a critical aspect of patient care management PCM services include medication reconciliation, assessment of medication adherence, monitoring for potential drug interactions or side effects, and providing education to patients on proper medication use. Optimizing medication regimens improves patient safety, reduces adverse events, and enhances treatment effectiveness
- Consent:
Obtain written consent from the patient for PCM services, explaining the scope and nature of the services, as well as any associated cost-sharing requirements.
- Eligibility: PCM services are typically eligible for reimbursement from Medicare and some private payers. Ensure that the patient meets the specific eligibility criteria defined by the payer, which may include having chronic conditions that require ongoing care management.
- Time-Based Billing: PCM services are billed based on the total time spent on care management activities during a calendar month. This includes both the time spent by clinical staff and the physician or other qualified healthcare professional PCM services require a minimum of 30 minutes before billing. See CorroHealth TCM, CCM, RPM, PCM Table for more information.
- Documentation: Accurate and detailed documentation is crucial to support the medical necessity of PCM services. Document the time spent on care management activities, care coordination efforts, patient education, medication management, and care plan development or review.
- Reporting Services:
- 99497 (advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate) is a stand-alone billable RHCvisit
- Shared or Incident-to-Billing: When performed in a clinic setting, some PCM services may be billed under the supervising physician or as incident-to-services Understand the billing guidelines applicable to the practice and ensure compliance with the relevant regulations
CorroHealt h invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

Thursday, July 13, 2023
New s
- Hospital Outpatient Prospective Payment System: Remedy for the 340B-Acquired Drug Payment Policy for Calendar Years 2018-2022
- National Coverage Determination: Pre-exposure Prophylaxis Using Antiretroviral Drugs to Prevent HIVInfection
- Medicare Dental Services: Learn What?s Covered
Claim s, Pricers, & Codes
- Institutional Providers: Resubmit Audiology Claims Returned with Reason Code 34963
- Inpatient Prospective Payment System-Excluded Hospitals: Correcting Issue with Excluded Units
- ICD-10-CM Diagnosis Codes: FY2024 Coding Guidelines & Conversion Table
Event s
- Expanded Home Health Value-Based Purchasing Model: Overview of the Interim Performance Report Webcast ? July 27
MLN Mat t ers®Art icles
- ICD-10 & Other Coding Revisions to Laboratory National Coverage Determinations: October 2023 Update
- Ambulatory Surgical Center Payment System: July 2023 Update ? Revised
- New Fiscal Intermediary Shared System Edit to Validate Attending Provider NPI ? Revised
Publicat ions & Mult im edia
- Period of Enhanced Oversight for New Hospices in Arizona, California, Nevada, & Texas
- Expanded Home Health Value-Based Purchasing Model: New Resources
Therew asONEnew or revised Transmittal released thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.


Therew ereNOnew or revised MedLearnsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.



Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to thebest of CorroHealth'sknowledgeisaccurateat thetimeof distribution. However, due to the ever-changinglegal/regulatory landscape, thisinformation issubject to modification asstatutes, laws, regulations, and/or other updatesbecome available. Nothingherein constitutes, isintended to constitute, or should berelied on aslegal advice. CorroHealth expresslydisclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anything contained in thematerials, which areprovided on an "as-is"basisand should beindependentlyverified before beingapplied. You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability. The information in thisdocument isconfidential and proprietaryto CorroHealth and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduceor transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording, and broadcasting, or byanyinformation storageand retrieval system must beobtained in writingfrom CorroHealth. Request for permission should bedirected to Info@Corrohealth.com.

