




Hard to believe, however, after more than a year and half since the NSA became law, we are still looking for a quick and fair resolution to disputes The challenge is, providers are initially underpaid and then often wait up to six months for a resolution from a process that has increased in cost Recent reports on the IDRprocess show outcomes have been favorable for providers, but are frequently too little, too late. Meanwhile, providers are also tasked with defending additional charges not included on Good Faith Estimates when a patient chooses to dispute charges that exceed the GFEby $400
In this episode, we define the dispute processes, offer suggestions to avoid disputes, and demonstrate how to access disputes when needed


CorroHealth?s ?No Surprises Act and Price Transparency, a New Monthly Series?was created to provide attendees with clarity around No Surprises Act, to answer questions, and get you on the best path for success. The series also clarifies payers?increased role in the process, the status of impactful legislation, and the processes providers should follow to comply
About Barbara Johnson, BSN, RN ?Senior Revenue Cycle Consultant
Leading the series is CorroHealth?s resident subject matter expert, Barbara Johnson, BSN, RN ?Senior Revenue Consultant
As a registered nurse Johnson worked in emergency medicine before transitioning into nursing administration She entered the specialty of Revenue Integrity as a nurse auditor where she expanded her knowledge of coding and revenue cycle compliance through membership in AAPCand HFMA Today, she is CorroHealth?s leading subject matter expert on NSA








We have a provider who is a Physician Assistant (PA) doing ultrasounds in the ERsetting. He is not running a report to show that he has done this, and there is no CPT®code for this service at this time. But if he is a certified ultrasound tech, runs the ultrasound report and we have the radiologist read the report and get a CPT®code for the ultrasound, then is this billable service?

Answ er:
Charging for Point-of-Care (POC) ultrasound in the ERcan be complicated
The CPT® manual states that ALL ultrasound requires image documentation and a final, written report, which some hand-held portable POCUSdevices are not capable of providing:

?Use of ult rasound, w it hout t horough evaluat ion of organ(s) or anat om ic region, im age docum ent at ion, and final, w rit t en report , is not separat ely report able.?
If permanent images from the POCultrasound are obtained and stored, and a radiologist interprets the images and generates a written report, then this would be a billable service
For POCultrasound, if there is no written report generated and there is no interpretation by a radiologist, there is no technical fee since this does not meet the CPT® requirements for reporting ultrasound studies. There is also no professional fee since no professional services were rendered If the radiologist reads the images from the POCUSand generates a report, they will bill for the professional fee for the interpretation of the USimages. The American College of Emergency Physicians (ACEP) offers the following guidance for non-radiologist interpretations of ultrasound exams in the ED:
https://www acep org/patient-care/policy-statements/interpretation-of-imaging-diagnostic-tests


?Interpretation of critical testing must be available 24 hours per day, 7 days per week Int erpret at ion should be com plet ed by a provider w ho m eet s or exceeds t he requirem ent s of t he inst it ut ion in w hich t he pat ient is receiving care.Off-site interpretation may be utilized, provided the process follows institutional and American College of Radiology (ACR) guidelines. It is preferred that off-site radiologists be credentialed by the hospital medical staff where the studies are performed Cont em poraneous int erpret at ion m ay be done by t heem ergency m edicine providers or by anot her specialist w it hin t he lim it s of t he t raining, experience, and com pet ence of t hat physician. Qualit y assurance of non-radiology int erpret at ions should follow inst it ut ional guidelines
Per U S Centers for Medicare & Medicaid Services (CMS) guidance, the provider performing contemporaneous interpretations of diagnostic studies is entitled to reimbursement for such interpretations. Interpretations should be available immediately to the ordering provider or their designee in accordance with institutional guidelines.
If the emergency physician believes that an urgent consultation with a radiologist is needed for the interpretation of a diagnostic study, that consultant must be immediately available for discussion and/or consultation with the treating physician.
?Whether the consultation is provided from a hospital staff physician or by an external contracted consultant, this physician should be board certified in radiology and licensed in the state where the images are obtained and should meet or exceed the credentialing requirements for physicians credentialed by the local health care facility
There are two additional issues of concern with charging for POCultrasound in the ER:

1)Most diagnostic ultrasound studies have very specific documentation requirements that must be met in order to bill for a complete ultrasound study CPT® code selection for the point-of-care ultrasound should be based on the specific documentation from the radiologist?s final, written report for the service. The radiology report serves as the documentation for both the professional and technical components of the procedure The below CorroHealth paper contains specific information about the documentation required for certain diagnostic USexams
Ultrasound Documentation Requirements: Complete vs. Limited

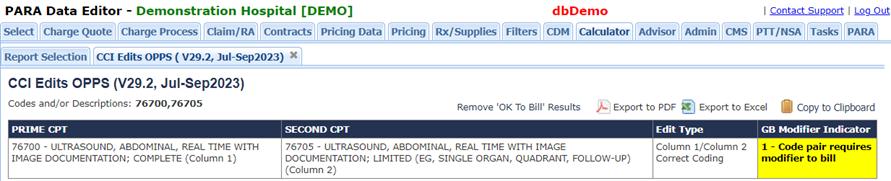
If the POCUSexam does not support the documentation/performance requirements for a complete ultrasound, it must be billed as a limited study This could become an issue if the patient goes on to have a second, more complete diagnostic ultrasound of the same anatomic site in the imaging department during an ED visit
Charging for both USstudies could potentially be appropriate if both are truly medically necessary, but the limited ultrasound would require a modifier in order to bypass NCCI edits for complete & limited studies billed on the same claim/same date of service (see example below). Charging for both ultrasounds would likely result in denials
Small balance revenue recoveries have emerged as a critical solution for healthcare organizations grappling with the challenges of uncollected accounts receivables (AR). With rising costs and limited resources, hospitals and healthcare providers often face the difficult decision of either abandoning revenue tied up in small balance accounts or expending significant efforts and administrative costs to recoup them. However, innovative solutions like CorroHealth's REVIVEplatform are transforming the process with an effective path to reclaiming valuable revenue

CorroHealth, a trusted leader in healthcare revenue recovery, understands healthcare organizations' challenges in managing small balance accounts Their advanced technology, analytics, and expertise provide a comprehensive automated solution that allows hospitals to address small balance accounts effectively. By partnering with CorroHealth, hospitals can leverage their expertise and technology to maximize returns without overwhelming existing billing staff

Small balance ARaccounts for a mere one to five percent of revenue, yet, they can consume a significant portion of an organization's ARdepartment's workload? 55 to 60 percent. These accounts typically remain unworked, and the root causes of delays are left unaddressed due to limited staff availability As a result, hospitals risk losing revenue that could be collected with the right approach and support.
Jon Guiliani, Senior Vice President Revenue Cycle Management at CorroHealth, emphasizes the impact of small balance revenue recoveries on financial health: "Small balance accounts may seem insignificant individually, but collectively, they represent a substantial amount of revenue that healthcare organizations often overlook. By implementing an efficient and automated system like CorroHealth's, hospitals can significantly improve their financial performance and enhance the quality of care they provide."
The financial challenges faced by hospitals are staggering. Annually, hospitals face initial denials of approximately $270 billion in claims, leading to high administrative costs of over $9 billion Even more alarming is that more than 65 percent of these denials are never reworked, even though over 90 percent of them could have been prevented in the first place.
In addition to these challenges, healthcare organizations struggle to find, train and retain affordable staff to manage small balance accounts. The complexity of the task can be daunting, with over 3,500 possible combinations of codes that may need to be addressed
The CorroHealth REVIVEplatform integrates seamlessly with a client's existing electronic medical records (EMR) system Through proprietary technology and automated decision-making, CorroHealth's team identifies root causes of delays and applies customized workflows to resolve them. By automating tasks such as claim notation, data gathering, and payer behavior analysis, CorroHealth streamlines revenue recovery, saving time and reducing administrative costs.CorroHealth consistently boosts clients' collections by over 30 percent, lowering costs by 30 percent and decreasing ARdays by 25 percent.
Jon Guiliani, Senior Vice President Revenue Cycle Management at CorroHealth, explains how their solution simplifies the recovery process: "Our platform combines robotic process automation, machine learning, a robust process flow system, and advanced analytics to optimize small balance claim resolution By automating repetitive tasks and providing consistent guidance, healthcare organizations can recoup revenue efficiently and redirect their resources to areas that truly matter."
CorroHealth's successful partnership with a non-profit hospital demonstrates the tangible impact of its small balance revenue recovery approach. Facing a backlog of aged accounts left by a previous vendor, the hospital turned to CorroHealth for assistance. By acting as an extension of the hospital's team, CorroHealth identified the root causes of delays and provided data-driven recommendations to improve its revenue cycle processes
Over the course of a decade, CorroHealth helped the hospital recover a staggering $116 million in aged small balance accounts Through the implementation of their technology-enabled solutions, the hospital achieved a 100 percent resolution rate on assigned claims, decreased the average account balance by 45 percent, and significantly reduced the number of aged accounts.
By aut om at ing repet it ive t asks and providing consist ent guidance, healt hcare organizat ions can recoup revenue efficient ly and redirect t heir resources t o areas t hat t ruly m at t er.
Small balance revenue recoveries substantially impact the financial well-being of healthcare organizations However, hospitals can strengthen their revenue streams by effectively addressing these accounts, enhancing patient care, and strategically allocating resources
As the healthcare industry evolves, CorroHealth remains committed to empowering healthcare organizations to overcome financial challenges and achieve sustainable success. Their innovative solutions, combined with advanced technology and industry expertise, position them as a trusted partner in navigating the complex landscape of revenue recovery.
About CorroHealt h:CorroHealth is the leading provider of clinically led healthcare analytics and technology-driven solutions dedicated to positively impacting the financial performance of hospitals and health systems. With over 8,500 employees worldwide, CorroHealth delivers integrated solutions, proven expertise, intelligent technology, and scalability to address needs across the entire revenue cycle.
For more information, please visitwww.corrohealth.com.
Quest ion:
For compression garments such as sleeves for arm, hand and knee, and bras for mastectomy, our research shows they are not DMEand the HCPCScould be A6549 These are not covered by Medicare. If we supply them to the patient, can we report them on the claim?If so, what is the correct revenue code and HCPCScode, and what would the cost be non-covered and non-collectable from the patient?
Answ er:
Many compression garments are non-covered, however below-the-knee compression stockings prescribed for venous statis ulcers of the legs are status N under OPPS, which means that they are covered, but not separately paid (see HCPCSA6531, A6532, and A6545 below ) Of course, a Critical Access Hospital will be paid on a cost-reimbursement basis for all covered charges on a facility fee claim

When used as medically necessary dressing immediately following surgery, some facilities include the cost of the initial post-surgical compression garment within the charge for the surgical procedure, or as an un-coded supply charge, rather than charging post-op patients for the compression garment as a non-covered item.
Hospitals may charge non-covered compression garments on a facility fee claim by reporting the appropriate HCPCSunder revenue code 0274 (MEDICAL/SURGICAL SUPPLIESAND DEVICES (ALSO SEE062X, AN EXTENSION OF027X). If an ABN was issued to transfer potential financial liability to the beneficiary for non-covered items, the hospital should append modifier GA (Waiver of liability statement issued as required by payer policy, individual case) to the HCPCS The ABN must be delivered far enough in advance that the patient has time to consider other options, such as purchasing from a pharmacy at a lesser cost
There are several HCPCSlisted in the PDEfor compression stockings, but only one (A6549) that includes the word ?sleeve?in the description


Some health plans may cover compression garments for conditions other than venous statis ulcers as will some Medicare Advantage plans Its important to check with each plan to verify coverage
Compression garments for breast prostheses are covered under Part B or Part A depending on the setting as indicated on this Medicare page: Breast Prosthesis Coverage (medicare.gov)


There is good news for 2024! The Lymphedema Treatment Act was passed by Congress on December 23, 2022, which will add compression garments as a billable item effective January 1, 2024 I have provided a link to read about the efforts of a few to make compression garments a covered item


On November 23, 2022, the FDA cleared the use of ?EchoGo Heart Failure 1.0,?a cloud-based automated machine learning-based diagnostic aid for patients undergoing routine echocardiography When utilized by an interpreting physician, this cloud-based system analyzes an echocardiographic Apical 4-Chamber loop to provide information that may be useful in detecting heart failure with preserved ejection fraction (HFpEF).

Following FDA clearance, the manufacturer applied to CMSfor a HCPCSto facilitate reporting the use of this diagnostic aid.Effective July 1, 2023, CMSestablished a new HCPCScode, C9786, to enable providers to claim reimbursement for the use of this new technology.
C9786 - ECHOCARDIOGRAPHYIMAGEPOST PROCESSING FORCOMPUTERAIDED DETECTION OFHEART FAILUREWITH PRESERVED EJECTION FRACTION, INCLUDING INTERPRETATION AND REPORT
The new code will be reimbursed by Medicare at $99.81 (national un-adjusted OPPSrate.)
The EchoGo Heart Failure 1 0 system uses Artificial Intelligence (AI) to more accurately interpret echocardiograms.The system was developed by echocardiography and AI experts from Ultromics, a spin-off of the UK?s University of Oxford, in collaboration with Mayo Clinic. The device uses AI to accurately detect heart failure with preserved ejection fraction (HFpEF) from a single echocardiogram image
HFpEFaccounts for 50%of the 64 million cases of heart failure worldwide and has overtaken heart failure with reduced ejection fraction (HFrEF) as the most prevalent form of the deadly disease.
CMSlisted C9786 in its OPPSAddendum B for July 2023 ? here is an excerpt:
According to the Ultromics website, ?The technology detects disease earlier and more consistently, alleviating the need for more costly and invasive procedures.?

CorroHealt h invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

Thursday, June 29, 2023
New s
- CY2024 ESRD Prospective Payment System Proposed Rule
- Transforming Medicare Coverage: A New Medicare Coverage Pathway for Emerging Technologies and Revamped Evidence Development Framework
- New Details of Plan to Cover New Alzheimer?s Drugs
- Model Participants for the Enhancing Oncology Model
- Hospital Price Transparency: Volunteer for Machine-Readable File Validator Testing
Claim s, Pricers, & Codes
- RARCs, CARCs, Medicare Remit Easy Print, & PCPrint: July Update
Event s
- Hospital Price Transparency Machine-Readable File Sample Format Webinar ? July 26
MLN Mat t ers®Art icles
- Ambulatory Surgical Center Payment System: July 2023 Update ? Revised
From Our Federal Part ners
- Locally-Acquired Malaria Cases Identified in U.S.
- Measles Guidance for the Summer Travel Season
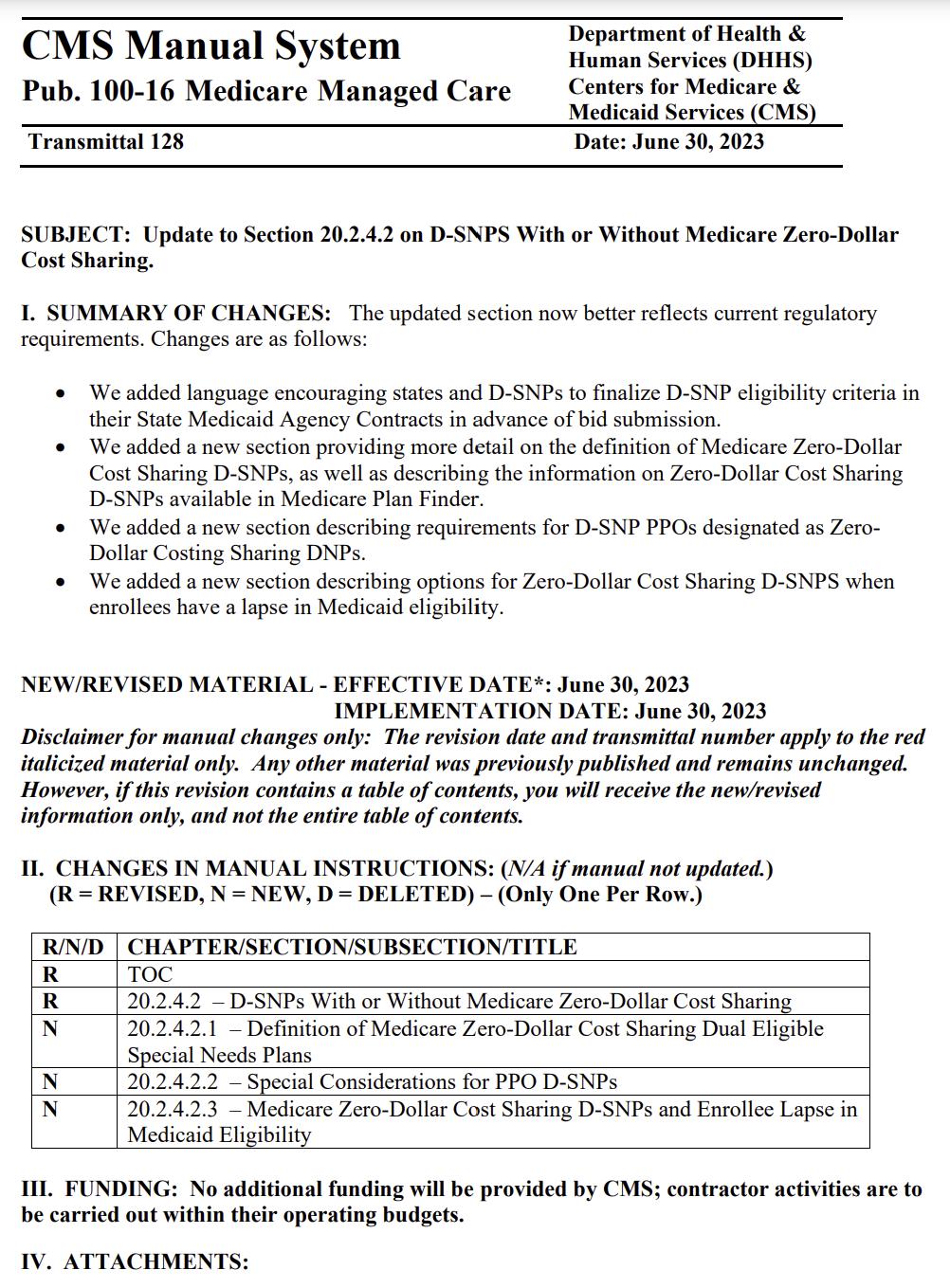
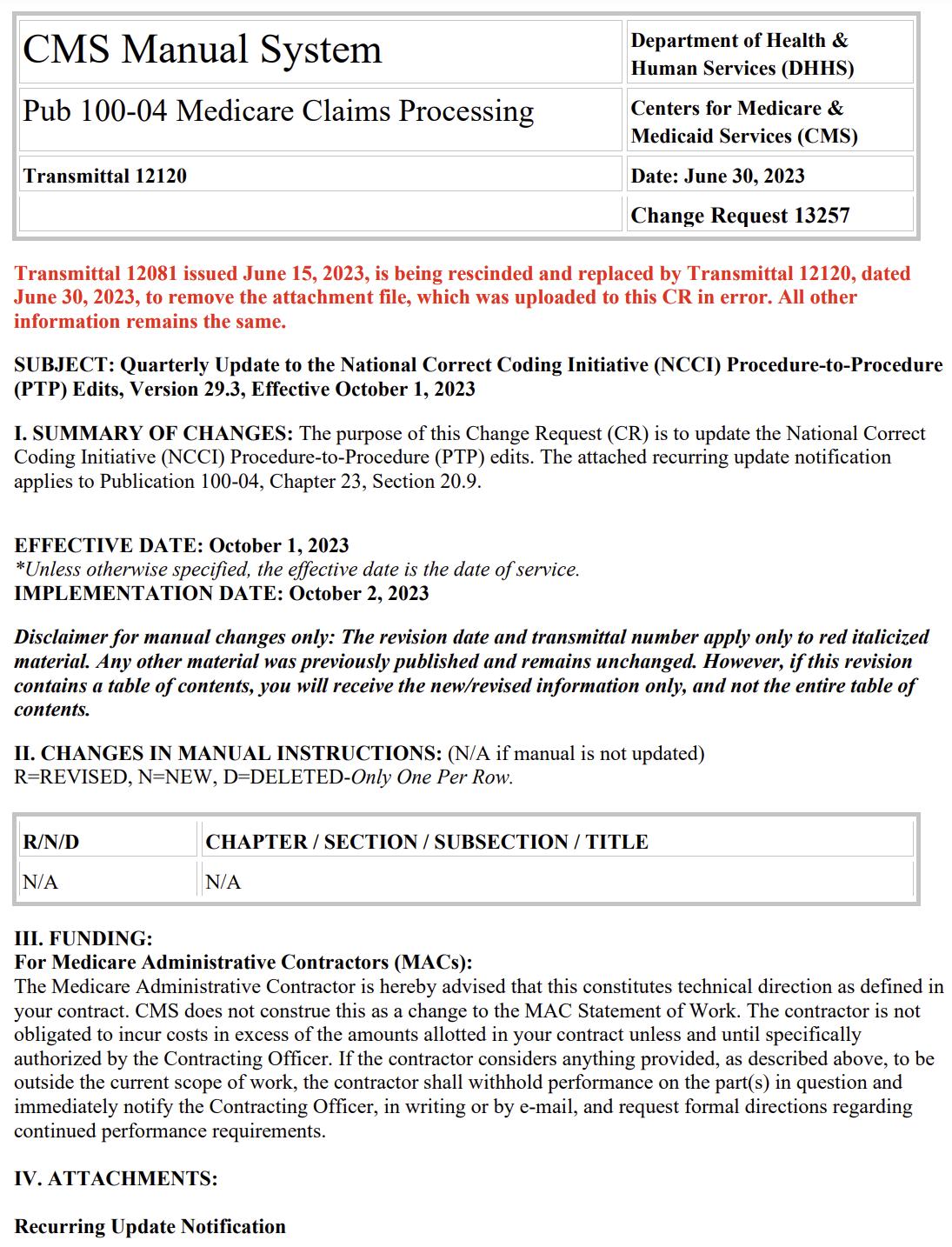
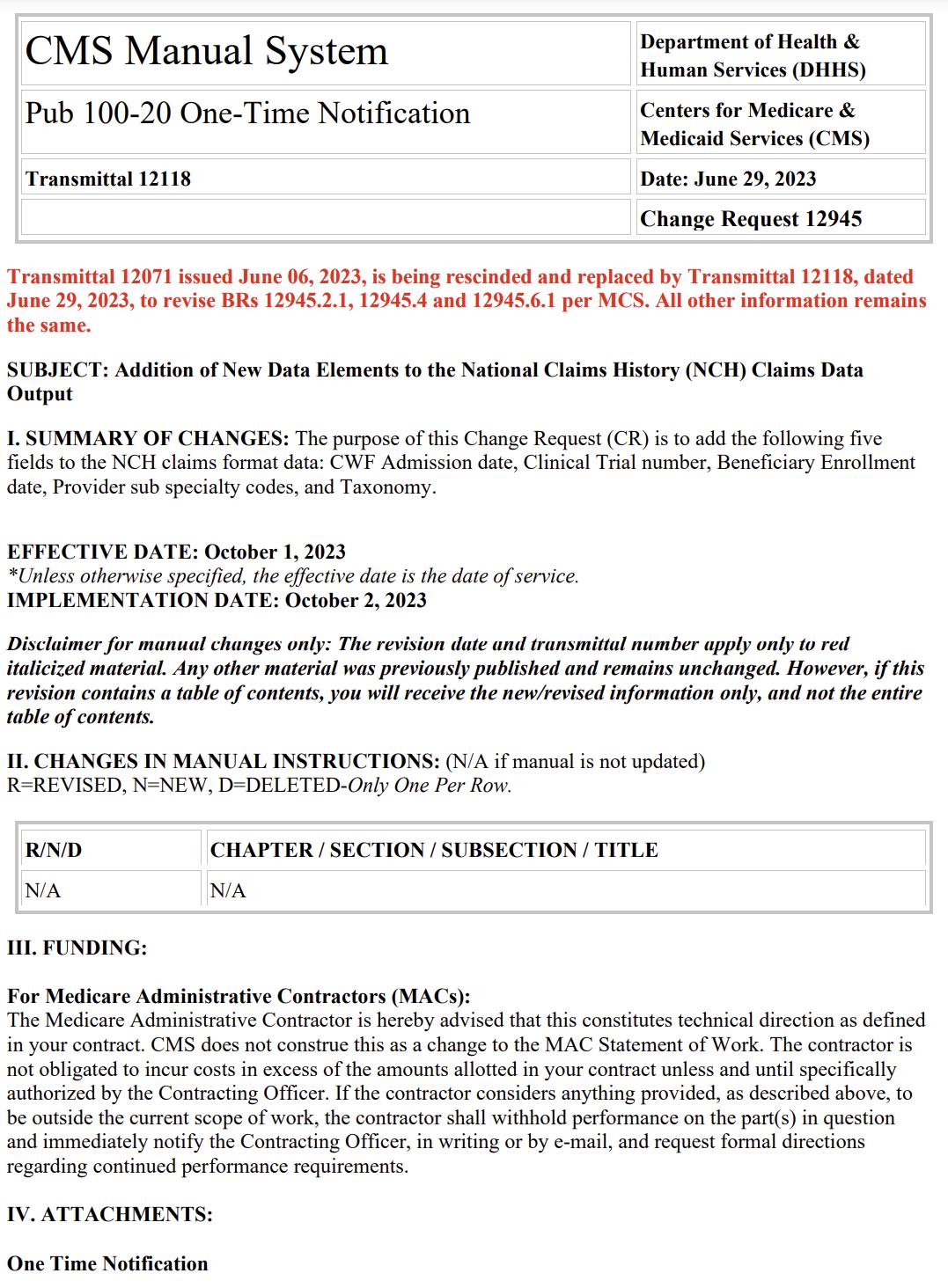
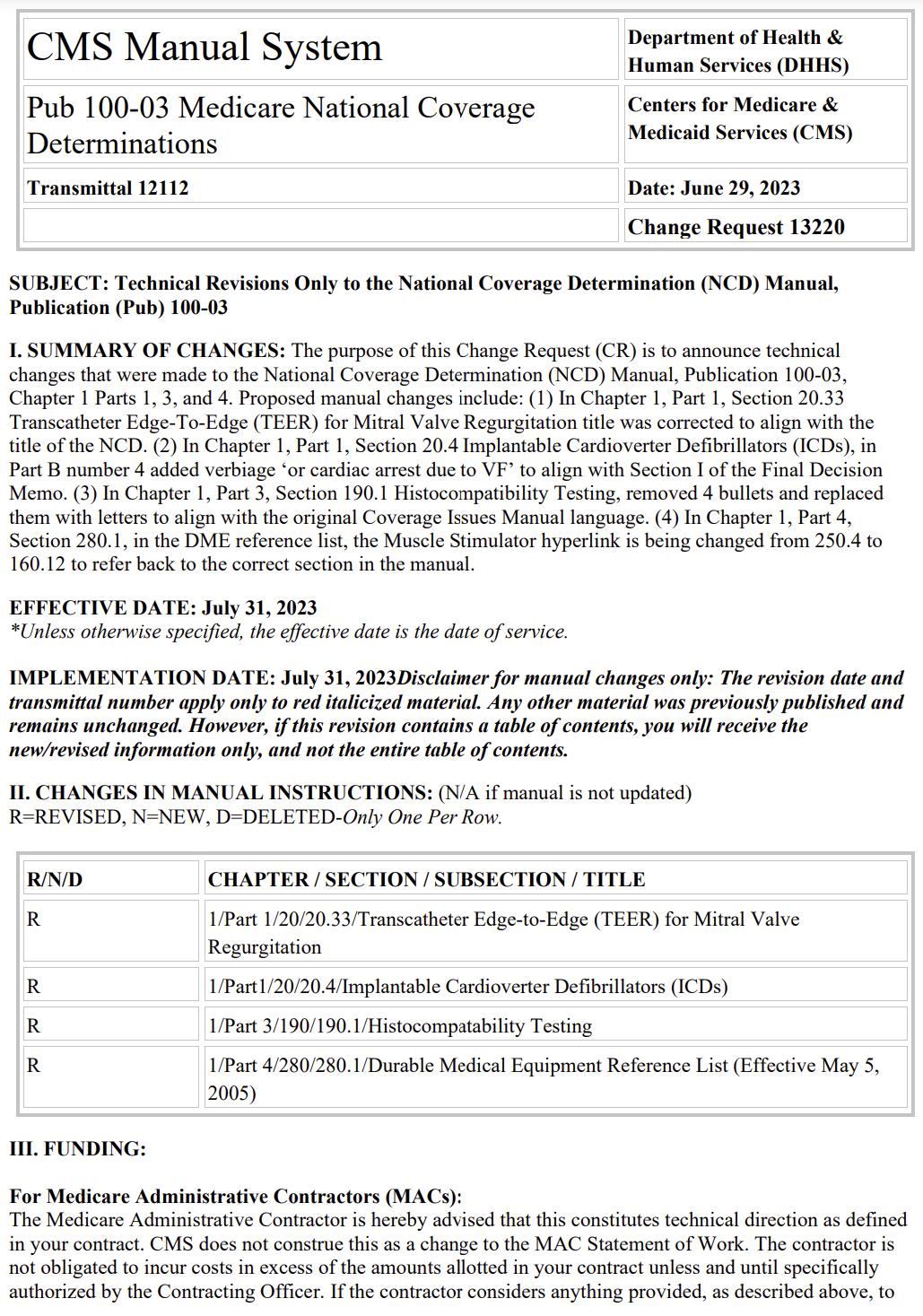
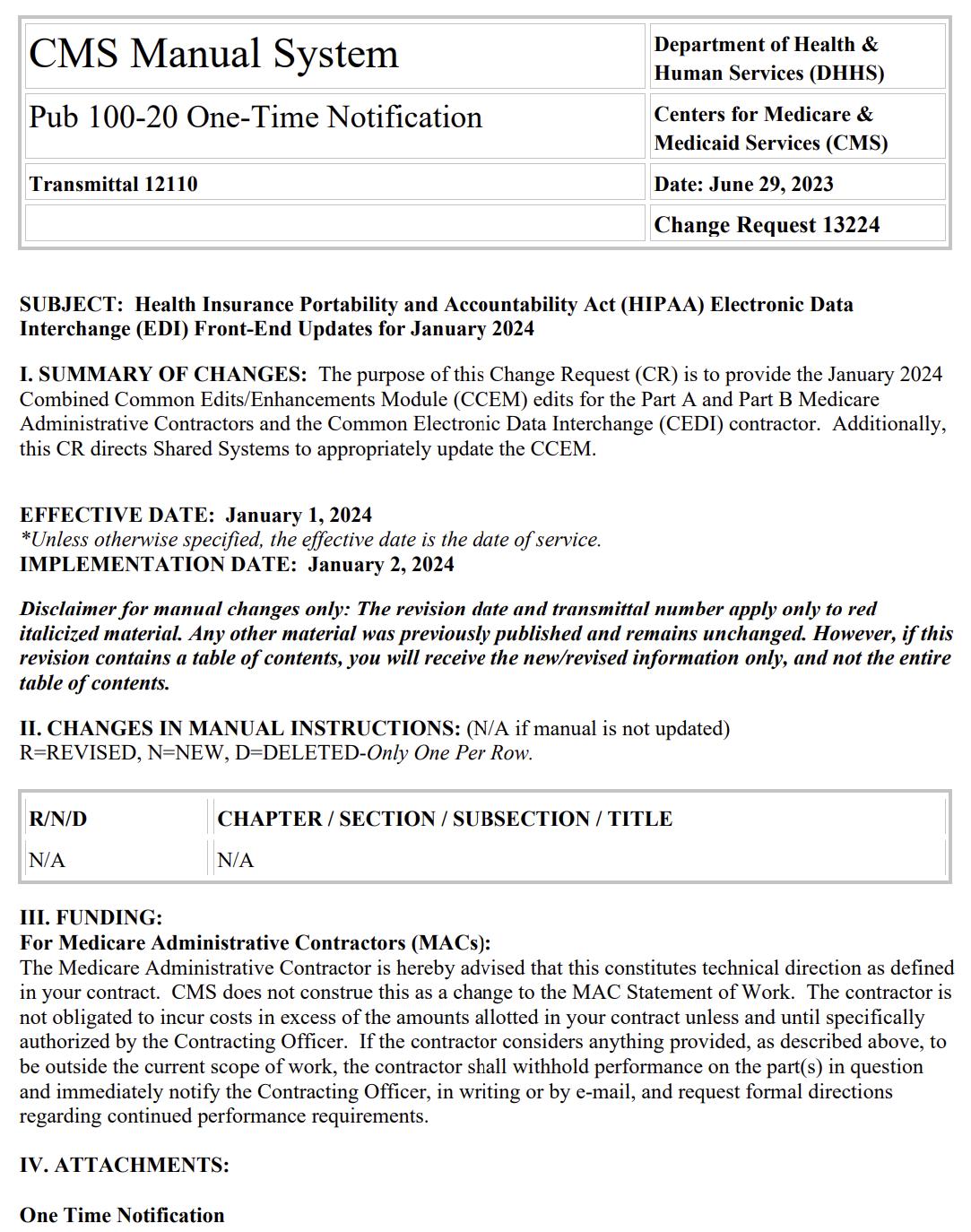
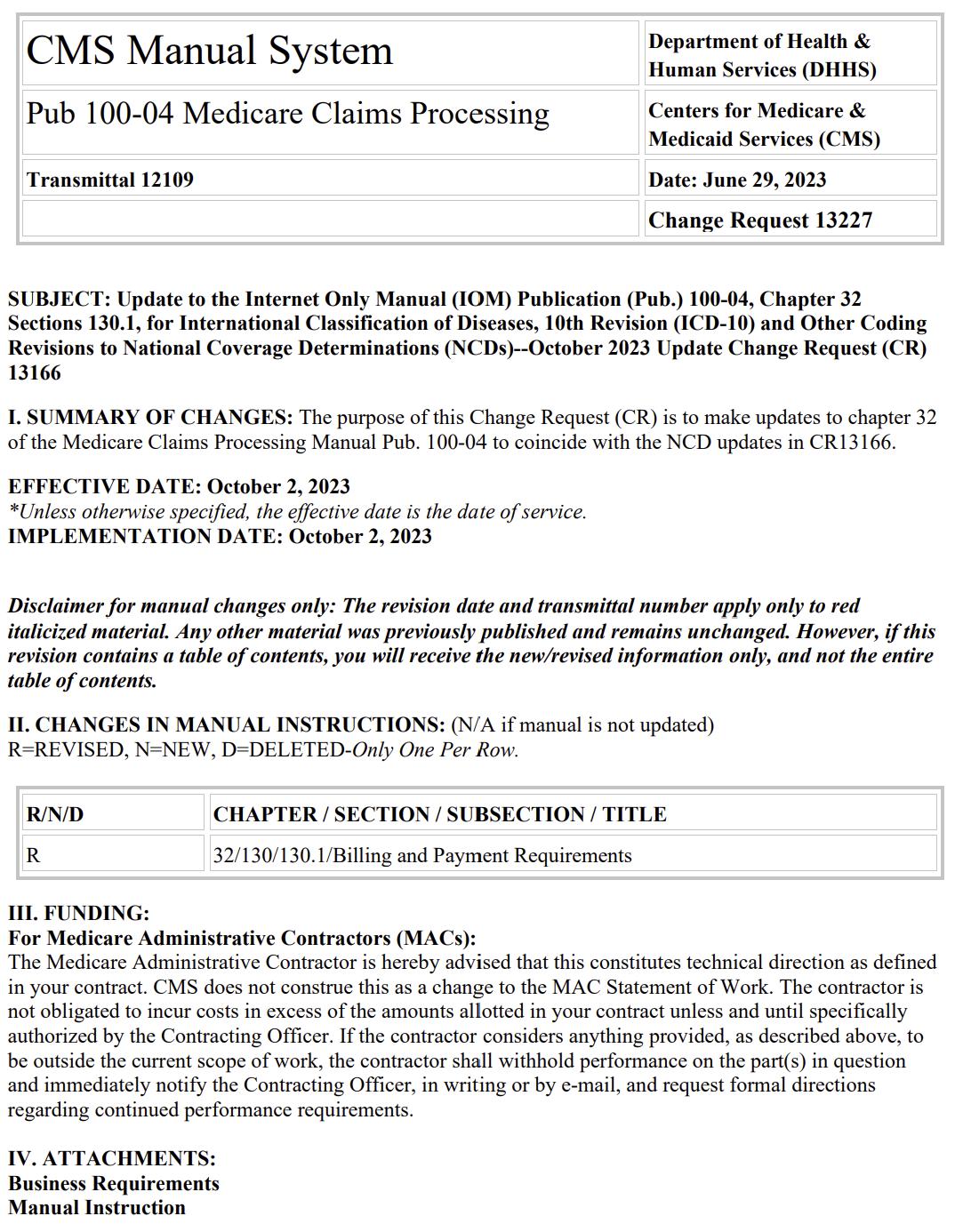
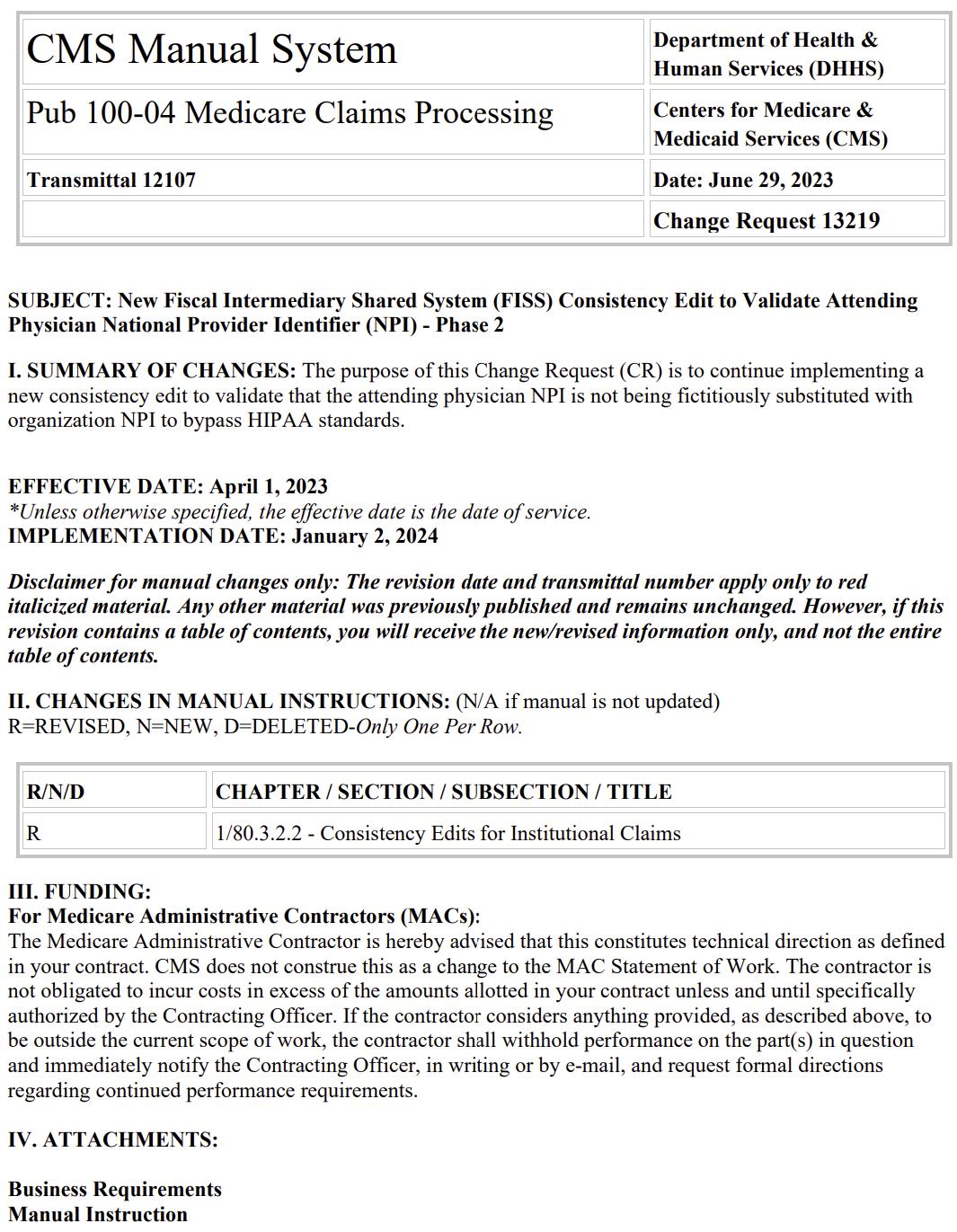
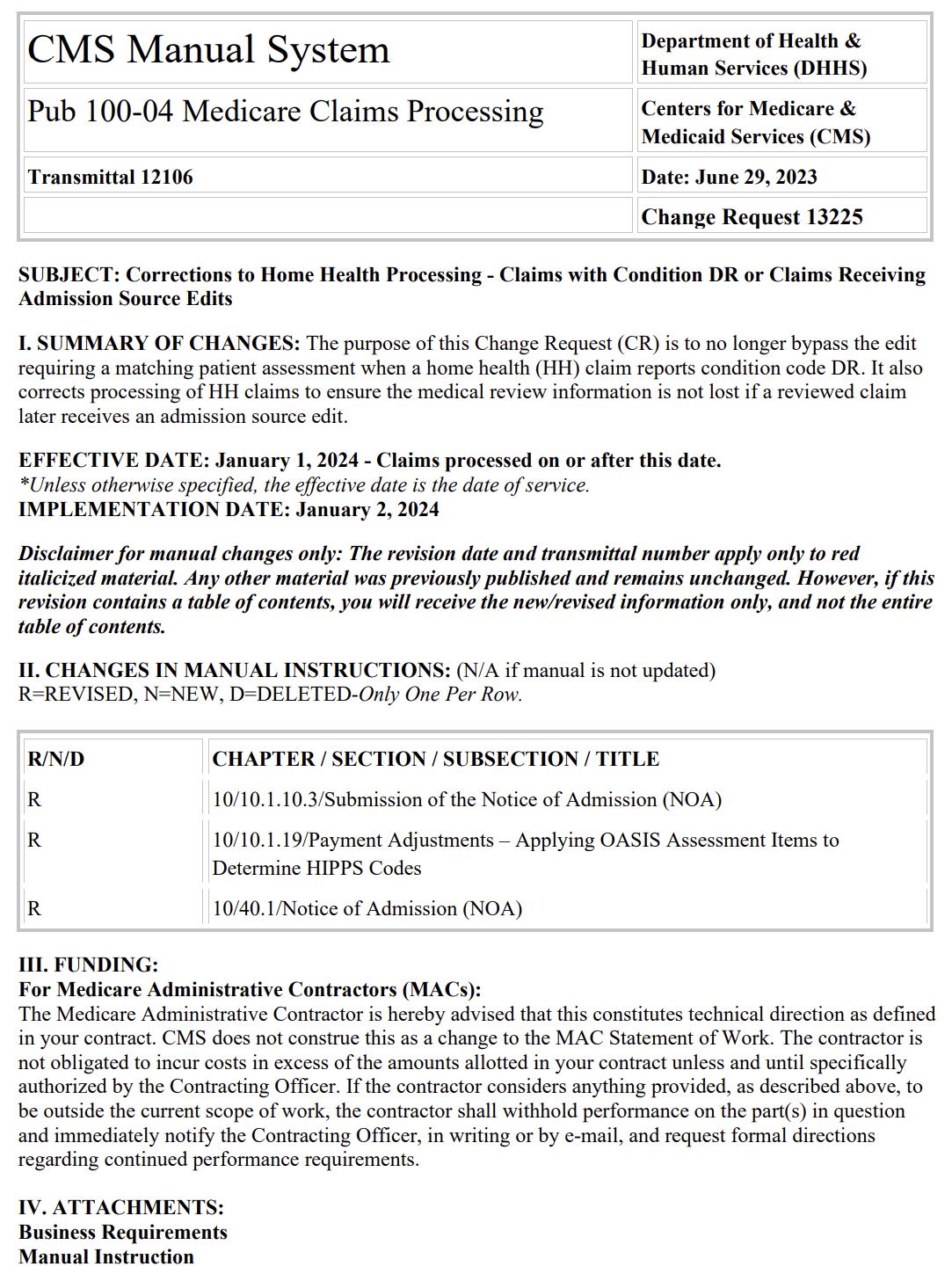
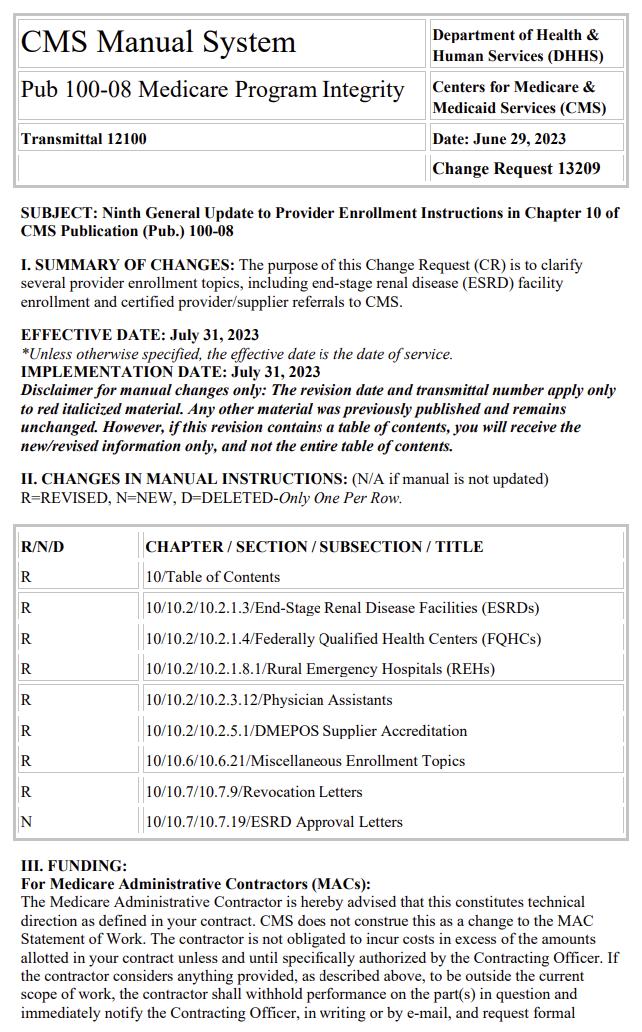
Therew ereFIFTEEN new or revised Transmittalsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.



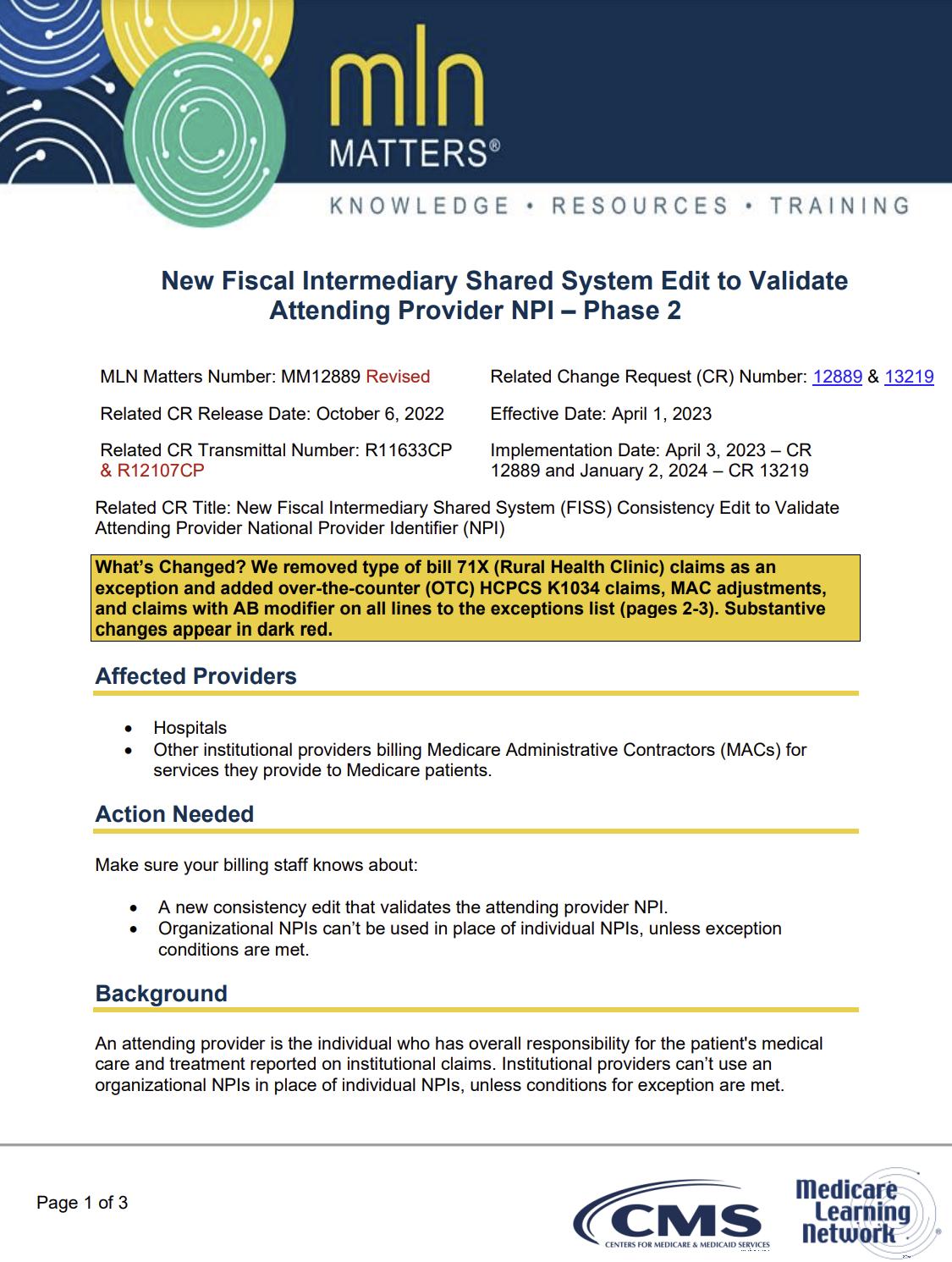
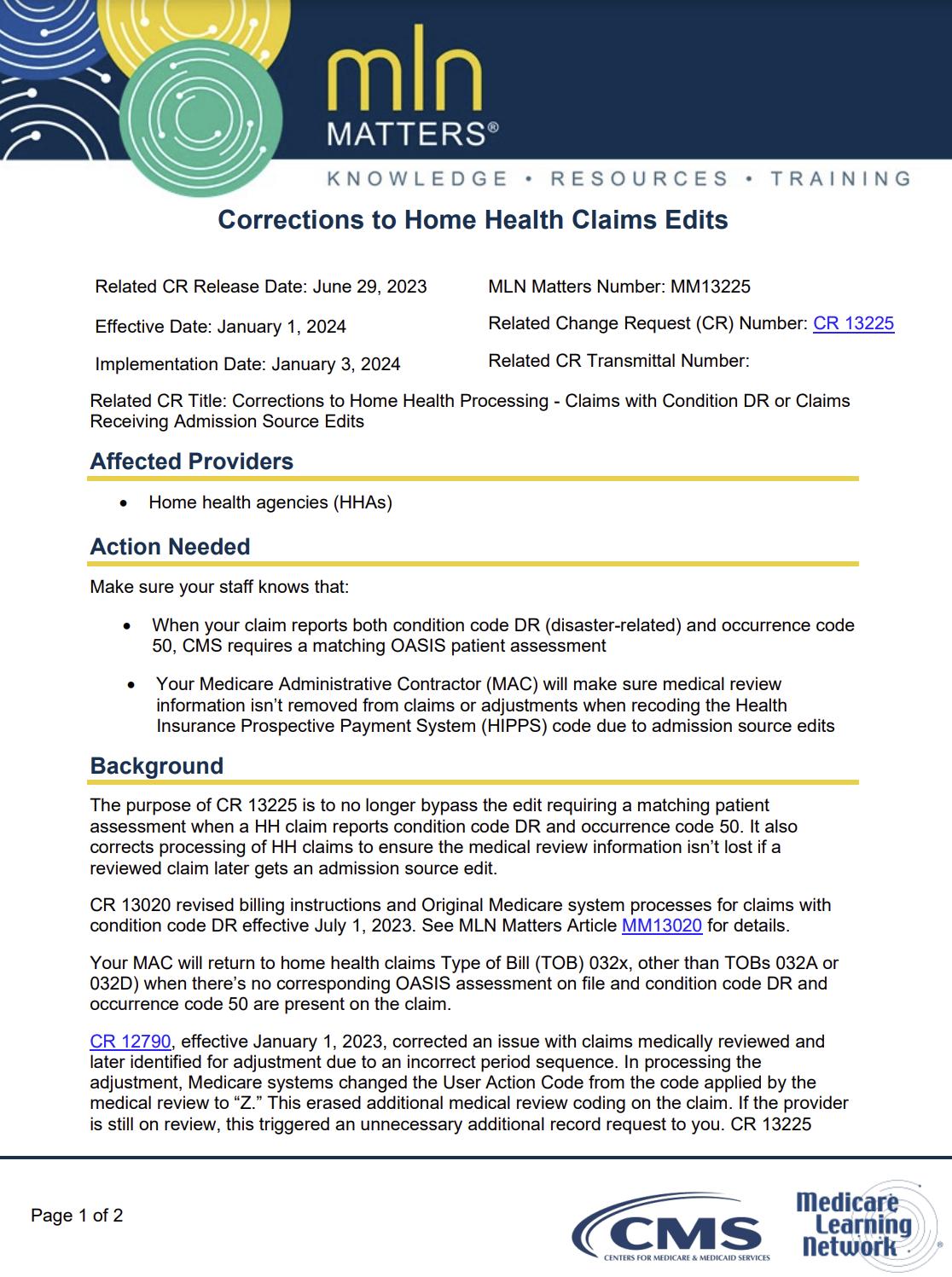
Therew ereFOUR new or revised MedLearnsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.


Contact the expert in your state and discover the difference CorroHealth can make on your bottom line


Does Your Payer Pricing St rat egy Deliver The Highest Reim bursem ent ?
- Opt im ized reim bursem ent rat es
If not, we can help.
The Revenue Int egrit y Program Is Just One St rat egy Making A Difference.
- Reduced adm inist rat ive burden of m aint aining a pricing st rat egy
- Three m ont h ROI from net revenue im pact
Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to thebest of CorroHealth'sknowledgeisaccurateat thetimeof distribution. However, due to the ever-changinglegal/regulatory landscape, thisinformation issubject to modification asstatutes, laws, regulations, and/or other updatesbecome available. Nothingherein constitutes, isintended to constitute, or should berelied on aslegal advice. CorroHealth expresslydisclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anything contained in thematerials, which areprovided on an "as-is"basisand should beindependentlyverified before beingapplied. You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability. The information in thisdocument isconfidential and proprietaryto CorroHealth and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduceor transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording, and broadcasting, or byanyinformation storageand retrieval system must beobtained in writingfrom CorroHealth. Request for permission should bedirected to Info@Corrohealth.com.

