j our nal e
Newborn Diagnosis

Proper CodingWhenTransferring






The NSA?s intent is to provide transparency in healthcare costs and prevent balance billing, and to meet those objectives NSA documents must communicate informative estimates and clearly explain the patient?s rights under the NSA Join us as we review the CMStemplates of required NSA documents and demonstrate how to properly utilize these documents for the patient?s greatest benefit.
CorroHealth?s ?No Surprises Act and Price Transparency, a New Monthly Series?was created to provide attendees with clarity around No Surprises Act, to answer questions, and get you on the best path for success. The series also clarifies payers?increased role in the process, the status of impactful legislation, and the processes providers should follow to comply
Leading the series is CorroHealth?s resident subject matter expert, Barbara Johnson, BSN, RN ?Senior Revenue Consultant
As a registered nurse Johnson worked in emergency medicine before transitioning into nursing administration She entered the specialty of Revenue Integrity as a nurse auditor where she expanded her knowledge of coding and revenue cycle compliance through membership in AAPCand HFMA Today, she is CorroHealth?s leading subject matter expert on NSA

Quest ion:
We have twins who were born at another facility and tansferred to our facility. The insurance company is stating that we need to bill with a diagnosis in the range of Z38 00 - Z38 8 However, CMSguidelines state that a code from category Z38 is only assigned at the time of birth.
If a newborn is transferred to another institution, a code from category Z38 should not be used at the receiving hospital We have tried appealing the claims with records and the coding guidelines to show we were the receiving hospital for these twins But the appeal was denied, still stating that there is a conflict with the type of bill and/or diagnosis code. What can you recommend?
Answ er:
When a newborn is transferred from another hospital immediately following birth, the correct Admission Type to be reported by the receiving hospital on a UB claim is "1" (Emergency)

The Special Point of Origin Code (FL 15) of "6" appropriately indicates that the infant was admitted as a transfer from another healthcare facility for specialized or higher-level care related to the childbirth process

As you pointed out, the ICD-10 Official Coding Guidelines, Chapter 16 ,Z38 codes may not be reported by Onslow as the receiving hospital of the transferred infants.

Quest ion:
This is a new elective procedure we would like to start performing. Can you review if this procedure can be charged out on a case level basis like we do for all the other main OR procedures?
Billing codes and reimbursement -- HIFU 55880, aspiration of bladder / SP cath 51102, foley cath 51702, some (but not all) will require cysto 52000 and/or transurethral resection of the prostate (TURP) 52601

Here is some information from the vendor: We mobilize our Sonablate HIFU technology with experienced technicians and FDA mandated disposables on a per-click basis making it possible for hospitals like yours to integrate HIFU (for localized prostate cancer) without the capital purchase of equipment and service contracts.
With the recent change in reimbursement, we are seeking to transition all our nationwide cases to hospitals in 2023 CMSannounced the 2023 OPPSPreliminary Rates recently and reassigned HIFU (55880; Abltj mal prst8 tiss hifu) to Level 6 which reimburses at $8,711 09 (and close to $10,700 in this market). Additionally, we have been told by the hospitals we are already working with that they are receiving reimbursement from commercial carriers already.
What should we expect to get reimbursed from this procedure?
Answ er:
Medicare covers CPT® 55880, OPPSreimbursement for your facility would amount to a total allowed of $9,978.76:
Yes, the hospital surgery department may use one of its time- and acuity-based surgical ?level? charges. The level charge selected should take into account the extra expense incurred for the HIFU equipment vendor. It is inappropriate to charge separate supply charges for re-usable equipment, even if it is rented ? that expense should be captured within the charges for the use of the operating room

Alternately, if the duration of this procedure is fairly predictable, the hospital could opt to create a special hard-coded charge for 55880 In general, we recommend using ?level?charges
Level charges should take into consideration three factors:
- Surgery suite set-up time
- The number of hospital staff required to attend the procedure (excluding professionals that bill separately for their services), and
Please note that there are a number of CCI edits that will prevent reporting all of the codes mentioned in your question for the same encounter Some of the code pairs are not billable on the same claim, and no modifier will permit it
If both the ablation and a TURPare performed in the same session, the ablation code 55880 will require a modifier indicating that it is separate and distinct from a TURP52601:

Many facilities bill diagnostic ultrasound services from the referring physician?s order as an automated process, without any review by a coding professional This practice is discouraged because when charging for complete diagnostic ultrasounds, the CPT® Manual outlines very specific documentation requirements for these examinations.
The radiology report serves as the documentation for both the professional and technical portions of the examination The documentation within the medical record must support the exam that was performed--both for the professional fee (the radiologist?s interpretation) and the technical fee (the technologist?s work of performing the exam).
It is the reading radiologist?s responsibility to ensure the components of each diagnostic ultrasound exam performed are documented appropriately in the radiology report. The CPT® guidelines for diagnostic ultrasound state that all diagnostic ultrasound studies require the following:
- Permanently recorded images with measurements (when such measurements are clinically indicated)
- A final, written report to be issued for inclusion in the patient?s medical record
Per CPT® , ?Use of ultrasound, without thorough evaluation of organ(s) or anatomic region, image documentation, and final, written report, is not separately reportable.?
Com plet e vs Lim it ed Ult rasound
CPT® instructions pertaining to coding a complete vs. a limited ultrasound are as follows: ?For those anatomic regions that have ?complete?and ?limited?ultrasound codes, note the elements that comprise a ?complete?exam The report should contain a description of these elements or the reason that an element could not be visualized (eg, obscured by bowel gas, surgically absent).
If less than the required elements for a ?complete?exam are reported (eg, limited number of organs or limited portion of region evaluated), the ?limited?code for that anatomic region should be used once per patient exam session A ?limited?exam of an anatomic region should not be reported for the same exam session as a ?complete?exam of that same region ?
Complete diagnostic ultrasound of the unilateral breast requires evaluation and documentation of the following:
- All four quadrants of the breast
- Retroareolar region
- Axilla, if performed
If a focused assessment of one or more, but not all, of these elements are evaluated and documented, the limited code 76642 should be reported
Complete diagnostic ultrasound of the abdomen requires real-time evaluation and documentation of the following:
- Liver
- Gallbladder
- Common bile duct
- Pancreas
- Spleen
- Kidneys
- Upper abdominal aorta
- Inferior vena cava
If less t han t he required elem ent s for a com plet e exam are perform ed and docum ent ed, code 76705 should be report ed.
Complete diagnostic ultrasound of the retroperitoneum requires real-time evaluation and documentation of the following:
- Kidneys
- Abdominal aorta
- Common iliac artery origins
- Inferior vena cava
OR If clinical history suggests urinary tract pathology, complete evaluation of the kidneys and urinary bladder also comprises a complete retroperitoneal ultrasound.
If less than the required elements for a complete exam as described in the previous page are documented, the exam should be reported using limited code 76775.
Complete first trimester (<14 weeks 0 days gestation) OB ultrasound evaluation requires real-time evaluation and documentation of the following:
- Determination of number of gestational sacs and fetuses
- Gestational sac/fetal measurements appropriate for gestational age
- Survey of fetal visible fetal and placental anatomic structure
- Qualitative assessment of amniotic fluid volume and gestational sac shape
- Examination of the maternal uterus and adnexa
If less than the required elements for a complete exam are performed and documented, code 76815 should be reported.
Complete OB ultrasound evaluation after the first trimester (> or = 14 weeks 0 days gestation) requires real-time evaluation and documentation of the following:
- Determination of number of fetuses and amniotic/chorionic sacs
- Measurements appropriate for fetal age
- Survey of intracranial, spinal, and abdominal anatomy
- 4-chambered heart
- Umbilical cord insertion site
- Placenta location
- Amniotic fluid assessment
- Examination of the maternal adnexa
If less t han t he required elem ent s for a com plet e exam are perform ed and docum ent ed, code 76815 should be report ed.
Obst et rical Ult rasound ? Det ailed Fet al Anat om ic Eval
Complete OB ultrasound with detailed fetal anatomic evaluation requires real-time evaluation and documentation of the following:
- All the elements required for code 76805/76810, plus
- Fetal brain/ventricles
- Face
- Heart/outflow tracts and chest anatomy
- Abdominal organ specific anatomy
- Number, length, and architecture of limbs
- Detailed evaluation of umbilical cord and placenta
- Other fetal anatomy as clinically indicated
The imaging report should document the results of the evaluation of each element described above or the reason for non-visualization
If less t han t he required elem ent s for a com plet e exam are perform ed and docum ent ed, code 76815 should be report ed
Code 76817 describes obstetrical ultrasound evaluation via a transvaginal approach. Per CPT® Assistant, November 2011, this code includes evaluation of:
- Embryo(s) and gestational sac(s)
- Maternal uterus, adnexa, and/or cervix
76817 may be reported in addition to a follow-up transabdominal approach OB US(76816) when necessary to adequately view the structures.
Complete non-obstetric ultrasound of the female pelvic anatomy requires real-time evaluation and documentation of the following:
- Description and measurements of the uterus and adnexal structures (i e , fallopian tubes and ovaries)
- Measurement of the endometrium
- Measurement of the bladder (when applicable)
- Description of any pelvic pathology (e g , ovarian cysts, uterine leiomyomata, free pelvic fluid)
76857 should be reported
If less t han t he required elem ent s for a com plet e exam are perform ed and docum ent ed, code 76857 should be report ed.
According to the American College of Radiology (ACR) Ultrasound Coding User?s Guide, a complete non-OB transvaginal ultrasound includes evaluation of:
- Uterus
- Endometrium
- Ovaries
- Adnexa (e g , ovaries, fallopian tubes, and uterine ligaments)
Clinical Examplesin Radiology(Winter 2016) indicates that while the adnexa must be evaluated and documented, the fallopian tubes do not need to specifically be mentioned. If evaluation of the uterus is not performed or documented, modifier 52 should be applied to code 76830 to indicate reduced services
It is appropriate to report 76856 or 76857 with 76830 when both are performed together However, the practice of performing and reporting both studies for every patient is discouraged Per Clinical Examplesin Radiology(Spring 2020), when transabdominal and transvaginal pelvic ultrasound are performed together, the transvaginal ultrasound is considered a specialized, problem-focused exam and should be performed only when medically necessary
Complete ultrasound of the male pelvic anatomy requires real-time evaluation and documentation of the following:
- Evaluation and measurement (when applicable) of the urinary bladder
- Prostate and seminal vesicles (to the extent visualized transabdominally)
- Any pelvic pathology (e.g., bladder tumor, enlarged prostate, free pelvic fluid, pelvic abscess)
If less t han t he required elem ent s for a com plet e exam are perform ed and docum ent ed, code 76857 should be report ed.
Complete ultrasound of a specific joint within an extremity requires real-time evaluation and documentation of the following:
- Joint space (e.g., effusion)
- Peri-articular soft tissue structures surrounding the joint (muscles, tendons, other soft-tissue structures)
- Any identifiable abnormality
The imaging report should document the results of the evaluation of each element described above or the reason for non-visualization
If less t han t he required elem ent s for a com plet e exam are perform ed and docum ent ed, code 76882 should be report ed
Accurate and complete documentation is essential when reporting ultrasound guidance. The documentation should clearly indicate the type of procedure, the specific anatomical location of the images, the specific anatomic structures visualized, and a documented description of the localization process. This information is critical to ensure that the service is accurately reported.
The CPT® Manual states the following:
?Ultrasound guidance procedures also require permanently recorded images of the site to be localized, as well as a documented description of the localization process, either separately or within the report of the procedure for which the guidance is utilized. Use of ultrasound, without thorough evaluation of organ(s) or anatomic region, image documentation, and final, written report, is not separately reportable ?
For additional information regarding accurate documentation and reporting of ultrasound guidance, please see the link to the PARA paper located in the PARA Dat a Edit or:
Ultrasound Guidance in the Hospital Setting
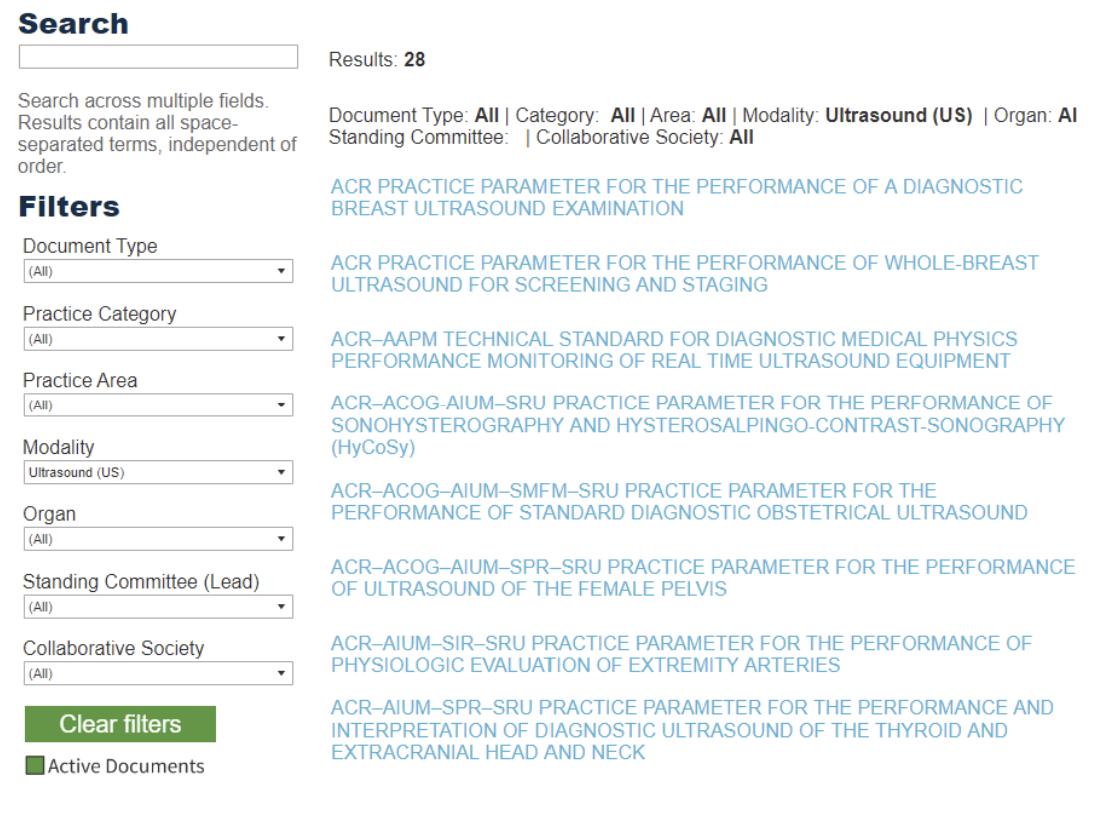
The American College of Radiology (ACR) offers specific parameters for the performance and interpretation of various types of imaging exams, including ultrasound:
https://www.acr.org/Clinical-Resources/Practice-Parameters-and-TechnicalStandards
Below is an example of a radiology report for a complete abdominal ultrasound Does this documentation meet the criteria for reporting a complete exam of the abdomen?

Answ er: No, this report does not meet the documentation criteria for reporting a complete abdominal ultrasound. There is no documentation of evaluation of the inferior vena cava (IVC), which is a component of a complete abdominal US. If the IVCwas evaluated, the radiologist should include this documentation in the report to support a complete study In this instance, an amended or corrected report could be issued to support charging a complete study
Code selection for diagnostic ultrasound is based on a variety of very specific documentation requirements. Clear documentation is extremely important to ensure proper coding and reimbursement Code descriptions and documentation should be reviewed carefully, and when unclear, the provider should be queried
CorroHealt h invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

Thursday, June 8, 2023
New s
- CMSAnnounces Resources and Flexibilities to Assist with the Public Health Emergency in the Territory of Guam Due to Recent Typhoon
- CMSRoundup (June 2, 2023)
- Gender-Specific Services: Billing Correctly and Usage of the Condition Code/Modifier
- Medicare Shared Savings Program: Apply for January 1 Start Date by June 15
- Skilled Nursing Facility Value-Based Purchasing Program: June Feedback Report
- Short-Term Acute Care Hospitals: Program for Evaluating Payment Patterns Electronic Reports
- Medicare Providers: Deadlines for Joining an Accountable Care Organization
- Help Address Disparities in the LGBTQI+ Community
Claim s, Pricers, & Codes
- National Correct Coding Initiative: July Update
- Integrated Outpatient Code Editor: Version 24.2
MLN Mat t ers®Art icles
- Allowing Audiologists to Provide Certain Diagnostic Tests Without a Physician Order
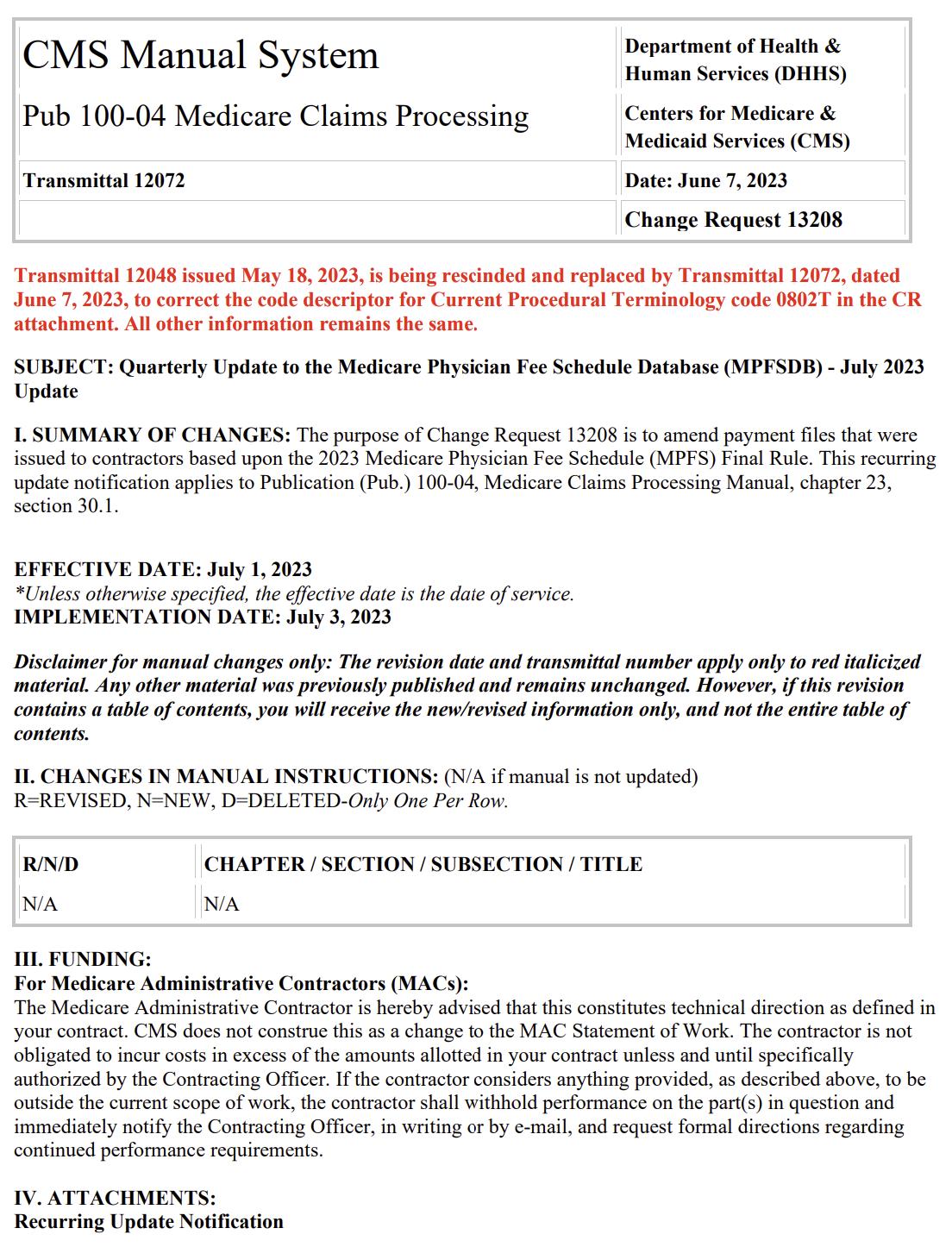
Therew ereTHREEnew or revised Transmittalsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.



Therew ereno new or revised MedLearn released thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.

Contact the expert in your state and discover the difference CorroHealth can make on your bottom line


Does Your Payer Pricing St rat egy Deliver The Highest Reim bursem ent ?
- Opt im ized reim bursem ent rat es
If not, we can help.
The Revenue Int egrit y Program Is Just One St rat egy Making A Difference.
- Reduced adm inist rat ive burden of m aint aining a pricing st rat egy
- Three m ont h ROI from net revenue im pact
Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to thebest of CorroHealth'sknowledgeisaccurateat thetimeof distribution. However, due to the ever-changinglegal/regulatory landscape, thisinformation issubject to modification asstatutes, laws, regulations, and/or other updatesbecome available. Nothingherein constitutes, isintended to constitute, or should berelied on aslegal advice. CorroHealth expresslydisclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anything contained in thematerials, which areprovided on an "as-is"basisand should beindependentlyverified before beingapplied. You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability. The information in thisdocument isconfidential and proprietaryto CorroHealth and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduceor transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording, and broadcasting, or byanyinformation storageand retrieval system must beobtained in writingfrom CorroHealth. Request for permission should bedirected to Info@Corrohealth.com.

