






The NSA?s intent is to provide transparency in healthcare costs and prevent balance billing, and to meet those objectives NSA documents must communicate informative estimates and clearly explain the patient?s rights under the NSA Join us as we review the CMStemplates of required NSA documents and demonstrate how to properly utilize these documents for the patient?s greatest benefit.
CorroHealth?s ?No Surprises Act and Price Transparency, a New Monthly Series?was created to provide attendees with clarity around No Surprises Act, to answer questions, and get you on the best path for success. The series also clarifies payers?increased role in the process, the status of impactful legislation, and the processes providers should follow to comply
Leading the series is CorroHealth?s resident subject matter expert, Barbara Johnson, BSN, RN ?Senior Revenue Consultant
As a registered nurse Johnson worked in emergency medicine before transitioning into nursing administration She entered the specialty of Revenue Integrity as a nurse auditor where she expanded her knowledge of coding and revenue cycle compliance through membership in AAPCand HFMA Today, she is CorroHealth?s leading subject matter expert on NSA
Quest ion:
A patient (21-month-old child) was seen in the hospital, and the physician ordered an Entire L Lower Limb due to child limping There has been many e-mails and a meeting on which code or codes should be used. Our lead coder states XRFemur and XRTibia & Fibula 2 view and to add a modifier 52. Is this correct?

Answ er:
We agree that the professional fees for 73552/73590 should NOT have modifier 52 appended, because the work of interpretingthe two examinations is not reduced or diminished by having the tib/fib and femur on the same image for each view. The facilit y/ t echnical fees for 73552/73590 SHOULD have modifier 52 appended, because only two total exposures were performed instead of four.
According to CPT®Assistant (November 2017, page 10-11):

Quest ion:
Our facility is performing pain procedures and we are receiving rejections from Medicare on 64484 and 64483 from indicating we can only bill quantity of (1) for surgical CPT®s We are only billing one 64483 and 64484, however on of each under the facility and one under professional.

We have attempted to remove the anatomical modifier, XU, and 50 on the ones for 50. Do you have any suggestions as to why we are seeing this rejection, or if we are billing appropriately?Had you had other facilities inquire about the same rejection issue?

Answ er:
The solution offered in the message you shared from NGSis to roll up all the charges onto one line for revenue code 0761.

An LCA published by NGSsupports that requirement. A link and excerpt are provided for your review
Article - Billing and Coding: Epidural Steroid Injections for Pain Management (A58745) (cms gov)

When reporting CPT® codes 64479 through 64484 for a unilateral procedure, use one line with one unit of service For bilateral procedures regarding these same codes, use one line and append the modifier-50.
We reviewed CMSclaims for a market hospital and discovered that 64483 was getting paid on that one line with modifiers 50, LT, and RT. We suggest that you roll the charges onto the one line and continue to use the appropriate modifier

Legislation has been re-introduced to both chambers of the 118th United States Congress to amend Medicare rules which require certain lab test providers to report commercial payer payment rates to Medicare every three years.
The proposed legislation has the support of many healthcare organizations, including the American Hospital Association, the American Clinical Laboratory Association, the Association of American Medical Colleges, the American Association for Clinical Chemistry.
The goal of the proposed legislation is to improve the accuracy of market-based Medicare payment for clinical diagnostic laboratory services, and to reduce administrative burdens in the collection of data
Medicare?s laboratory rate-setting procedure, which was changed by the Protecting Access to Medicare Act (PAMA) of 2014, have been beset by legal challenges and repeated delays PAMA required Medicare to set payment rates on the Clinical Laboratory Fee Schedule to the median rate paid by commercial payers for the same lab test
The procedure in obtaining the rate payment data, which CMSmust collect from providers to correctly set the median payment rates, is burdensome and arguably inaccurate In 2016, the first data collection under the new process resulted in draconian reductions in the 2018 Clinical Lab Fee Schedule payment rates for many common lab tests, which in turn resulted in a legal battle In fact, the USCourt of Appeals for the District of Columbia characterized the CMS process as ?arbitrary and capricious?in its decision in favor of the American Clinical Laboratory Association on July 15, 2022

Congress has repeatedly issued eleventh hour delays to the data reporting deadline for 2019 payment data, which requirement applied to hundreds of hospitals nationwide The initial deadline of January 1, 2020 has been delayed by Congress four years running, with the current reporting deadline for 2019 data set for January through March 2024.
In an attempt to fix the problematic procedure, bipartisan legislation was introduced in 2022 called the ?Saving Access to Laboratory Services Act?, or SALSA, but the 117th Congress failed to act by year-end The beginning of a new session of Congress required the proposed legislation to be reintroduced. Consequently, on March 28, 2023, twin bills were introduced to each chamber of the 118th Congress
The text of these bills are available at the following links:
Senate Bill S. 1000 ?Saving Access t o Laborat ory Services Act
Sponsor: Brown, Sherrod [Sen.-D-OH](Introduced 03/28/2023)
Cosponsors: (1)
Com m it t ees: Senate ? Finance
Lat est Act ion: Senate - 03/28/2023 Read twice and referred to the Committee on Finance.
House Bill H.R. 2377 ?Saving Access t o Laborat ory Services Act
Sponsor: Hudson, Richard [Rep.-R-NC-9] (Introduced 03/29/2023)
Cosponsors:( 25)
Com m it t ees: House - Energy and Commerce; Ways and Means
Lat est Act ion: House - 04/07/2023 Referred to the Subcommittee on Health
Highlight s of t he bills include t he follow ing provisions:
- Directs CMSto select providers required to report using a valid statistical sampling method, rather than requiring all ?applicable laboratories?to report
- Delays the next data collection period to begin on or after January 1, 2026, with reporting due in 2027
- Provides for data collection every 4 years, rather than every three years as previously required
- Authorizes Medicare to permit providers to exclude manual remittances from the data reported, if manual remittances represent less than 10%of the lab?s claims
- Removes the confusing and pointless ?Majority of Medicare Revenues?test
- Caps reductions in reimbursement to 2.5%in 2025, and 5%for subsequent years
- Excludes Medicaid Managed Care payer rates of reimbursement from the data collection requirements

On 4/7/2023, the House referred HR1835 to the Subcommittee on Health under the Committee on Energy and Commerce, and to the House Ways and Means Committee
As of this writing, no hearings are yet scheduled for these bills within the committee/subcommittee calendars published at https://docs.house.gov/Committee/Committees.aspx?Code=WM00#

Officially, the United States Department of Human Services ended the federal Public Health Emergency (PHE) on May 11, 2023.
CMShas published a Frequently Asked Questions document covering many of the issues related to healthcare providers following the end of the PHE An excerpt of some of those questions appears here
Many of t he flexibilit ies and w aivers in place are t ied t o em ergency declarat ions, legislat ive act ions by Congress, and regulat ory act ions across governm ent . Can t he Cent ers for Medicare & Medicaid Services (CMS) ext end Medicare, Medicaid, and Market place flexibilit ies beyond May 11, 2023, w hen t he Adm inist rat ion is planning t o end t he PHE?
Thanks to the Administration?s whole-of-government approach to combatting the virus, we are in a better place in our response than we were three years ago, and we can transition away from an emergency phase
The emergency declarations, legislative actions by Congress, and regulatory actions across government, including by CMS, allowed for changes to many aspects of health care delivery during the COVID-19 PHE. Health care providers received maximum flexibility to streamline delivery and allow access to care during the PHE
While some of these changes will be permanent or have been extended due to Congressional action, some waivers and flexibilities will expire, as they were intended to respond to the rapidly evolving pandemic, not to permanently replace standing rules.
CMShas released several documents that identify when waivers and flexibilities will end, as well as which waivers and flexibilities have been extended or will remain beyond the end of the PHE
To help individuals served by our programs know what to expect when the COVID-19 PHE ends, CMSreleased a fact sheet that highlights major impacts CMSalso released provider-specific fact sheets that will help the health care sector transition to non-emergency operations when the PHEends
In addition, CMSdeveloped a roadmap for the eventual end of the COVID-19 PHEand is sharing information on what health care facilities and providers can do to prepare for future emergencies
Additionally, CMSis offering technical assistance to States overseeing Medicaid and CHIP programs and engaging in public education about the necessary steps to prepare for the end of the PHE, including guidance on the end of the Medicaid continuous enrollment condition and the expiration of many other temporary authorities adopted by states during the COVID-19 PHE For additional information, visit CMSgov
People with Medicare coverage will continue to have access to COVID-19 vaccinations without out-of-pocket costs after the end of the PHE. Once the federal government is no longer purchasing or distributing COVID-19 vaccines, people with Traditional Medicare pay nothing for a COVID-19 vaccination if their doctor or other qualified health care provider accepts assignment for giving the shot Those with Medicare Advantage (MA) plans should contact their plan for details about payment for COVID-19 vaccines, but MA beneficiaries will pay nothing for a COVID-19 vaccination if they receive their vaccinations from an in-network provider
How m uch w ill CMS pay healt h care providers t o adm inist er COVID-19 vaccines t hrough t he end of t he 2023 calendar year?
Under the Medicare Part B preventive vaccine benefit, CMSwill continue to pay approximately $40 per dose for administering COVID-19 vaccines through the end of the calendar year in which the Secretary ends the Emergency Use Authorization (EUA) declaration for drugs and biologicals with respect to COVID-19 The COVID-19 EUA declaration has not ended Note: The COVID-19 EUA declaration is distinct from, and not dependent on, the federal PHEfor COVID-19, expected to expire on May 11, 2023, or the COVID-19 National Emergency that ended April 10, 2023
Effective January 1 of the year following the year in which the EUA declaration ends, CMSwill set the payment rate for administering COVID-19 vaccines to align with the payment rate for administering other Part B preventive vaccines, which is currently approximately $30 per dose 5/5/2023 These payment rates do not apply in settings that are paid at reasonable cost for preventive vaccines and their administration (for example, Federally Qualified Health Centers and Rural Health Clinics).
If someone is enrolled in an MA plan, the provider should submit claims for vaccine administration to the MA plan, and the amount the provider is paid for the vaccine administration service is determined by the contract between the MA plan and the provider if there is a contract If there is no contract in place for COVID-19 vaccinations covered by the MA plan, the Medicare payment rate would apply.
After the PHE, will the additional payment for at-home COVID-19 vaccinations continue?
Medicare will continue to pay an additional amount of about $36 in addition to regular administration fees for the administration of COVID-19 vaccines at home This additional Medicare payment for at-home COVID-19 vaccinations will continue through the end of calendar year 2023
For individuals enrolled in a MA plan, provider payment rates are determined by the contract between the MA plan and the provider when such a contract is in place and may or may not include additional payments for at-home COVID-19 vaccinations. If there is no contract in place for vaccinations covered by the MA plan, the Medicare payment rate would apply
When w ill t he enforcem ent discret ion end t hat allow s m ass im m unizers t o bill direct ly t o Part B for vaccines furnished t o Skilled-Nursing Facilit y (SNF) pat ient s in a Medicare-covered st ay?
Anticipating the end of the COVID-19 PHEon May 11, 2023, the enforcement discretion associated with this policy would end on June 30, 2023. Beginning on July 1, 2023, SNFs will be responsible for billing for vaccines furnished to SNFpatients in a Part A stay. Third-party suppliers furnishing these vaccines under arrangement with the SNFwould be required to seek payment from the SNFfor their services, consistent with SNFConsolidated Billing regulations
Will Medicare cont inue t o cover t reat m ent (s) for pat ient s w it h
Yes There is no change in Medicare coverage of treatments for those exposed to COVID-19 once the PHEends, and in cases where cost sharing and deductibles apply now, they will continue to apply Generally, the end of the COVID-19 PHEdoes not change access to oral antivirals, such as Paxlovid and Lagevrio For individuals enrolled in a MA plan, the plans must cover treatments that Traditional Medicare covers, but they may require the individual to see a provider who is in the MA plan?s network and may have different cost sharing than Traditional Medicare.
Those with Traditional Medicare can continue to receive COVID-19 PCRand antigen tests with no cost-sharing when the test is ordered by a physician or certain other health care providers, such as physician assistants and certain registered nurses, and performed by a laboratory.
People enrolled in MA plans can continue to receive COVID-19 PCRand antigen tests when the test is covered by Medicare, but their cost-sharing may change. Through the end of the COVID-19 PHE, Medicare covered and paid for over-the-counter (OTC) COVID-19 tests at no cost to people with Medicare Part B, including those with MA plans. The demonstration that allowed coverage and payment for OTCtests will ended when the PHEended on May 11th. Medicare Advantage plans may continue to cover the tests, so check with your plan for details.
Will t he w aiver of t he t hree-day hospit al st ay requirem ent prior t o a SNF st ay cont inue, or w ill it end w it h t he PHE?
Many flexibilities, including the waiver of the Medicare three-day qualifying hospital stay (QHS) requirement prior to a Medicare-covered SNFstay, are no longer be in effect for the Medicare fee-for-service program
For any Medicare Part A-covered SNFstay which begins on or prior to May 11, 2023, without a QHS, that stay can continue for as long as the beneficiary has Part A SNFbenefit days available and for as long as the beneficiary continues to meet the SNFlevel of care criteria (e g , requiring daily skilled care)
For any new Medicare Part A-covered SNFstay which begins after May 11, 2023, (including stays which experience a break in Part A coverage that exceeds three consecutive calendar days before resuming SNFcoverage), these stays will require a QHS. However, a doctor or other provider who is part of an Accountable Care Organization (ACO) may still be able to send their patients for a Medicare-covered SNFstay even if they have not stayed as an inpatient in a hospital for at least three consecutive days first.
For someone to qualify for this benefit, the doctor or other provider has to decide that SNF care is needed and certain other eligibility requirements are met. Additionally, MA plans may elect to furnish coverage of post-hospital SNFcare in the absence of the prior qualifying hospital stay as part of their Medicare-covered services. MA enrollees should check their Evidence of Coverage document for coverage requirements related to SNFcare
Aft er t he PHE, w hen can hospit als bill for:
1 The originat ing sit e facilit y fee (HCPCS code Q3014)?
2 The clinic visit (HCPCS code G0463)?
3. Rem ot e m ent al healt h services (HCPCS codes C7900 - C7902)?
Following the anticipated end of the PHE:
1 Hospitals cannot bill for this code after the PHEunless the beneficiary is located within a hospital and the beneficiary receives a Medicare telehealth service from an eligible distant site practitioner Only in these cases can the hospital would bill for the originating site facility fee (HCPCScode Q3014)
2 If the beneficiary is within a hospital and receives a hospital outpatient clinic visit (including a mental/behavioral health visit) from a practitioner in the same physical location, then the hospital would bill for the clinic visit (HCPCScode G0463)
3. If the beneficiary is in their home and receives a mental/behavioral health service from hospital staff through the use of telecommunications technology and no separate professional service can be billed, then the hospital would bill for the applicable HCPCS Ccode describing this service (HCPCScodes C7900 - C7902).
Aft er t he end of t he PHE, can hospit als bill for t he originat ing sit e facilit y fee (HCPCS code Q3014) w hen a beneficiary is not in t he hospit al but a hospit al-based out pat ient depart m ent physician furnishes a Medicare t elehealt h service and t he hospit al provides adm inist rat ive and clinical support ?
No Following the end of the PHE, hospitals will no longer be able to bill HCPCScode Q3014 to account for the resources associated with administrative support for a professional Medicare telehealth service.
Follow ing t he end of t he PHE, can hospit als bill for out pat ient physical/ occupat ional t herapy services provided t o beneficiaries in t heir hom es t hrough t elecom m unicat ion t echnology by hospit al em ployed physical t herapist s, occupat ional t herapist s, and speech language pat hologist s?
The waivers that currently allow for these flexibilities were under the CMSHospitals Without Walls Initiative expired at the end of the PHE.
During the PHE, under these waivers, a subset of counseling, therapy, and educational services have been eligible to be provided remotely by the hospital clinical staff, as long as they were are furnished to a patient in the hospital, which may have included the patient?s home, if the home was considered a provider-based department of to the hospital during the PHE.
In context of the anticipated end of the PHE, CMShas received a number of inquiries from interested parties regarding the expiration of this policy, including questions about whether policies other than the expiring waivers are relevant The questions are currently under review.

There are many more FAQs in the document You can download the complete 11-page document from CMSby clicking the icon below.

CorroHealt h invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

Thursday, June 1, 2023
New s
-
CMSAnnounces Plan to Ensure Availability of New Alzheimer?s Drugs
- COVID-19 Health Care Staff Vaccination Final Rule
- Medicare Secondary Payer Accident-Related Diagnosis Codes: How to Get Paid
- Hospitals: New Payment Adjustments for Domestic N95 Respirators
- Expanded Home Health Value-Based Purchasing Model: May Newsletter
- Improve Cognitive Health: Medicare Covers Services
MLN Mat t ers® Art icles
- Ambulatory Surgical Center Payment System: July 2023 Update
-
HCPCSCodes Used for Skilled Nursing Facility Consolidated Billing
Enforcement: July 2023 Quarterly Update
-
Updating Medicare Manual with Policy Changes in the CY2020 & CY2021
Final Rules
Publicat ions
- Medicare Preventive Services ? Revised
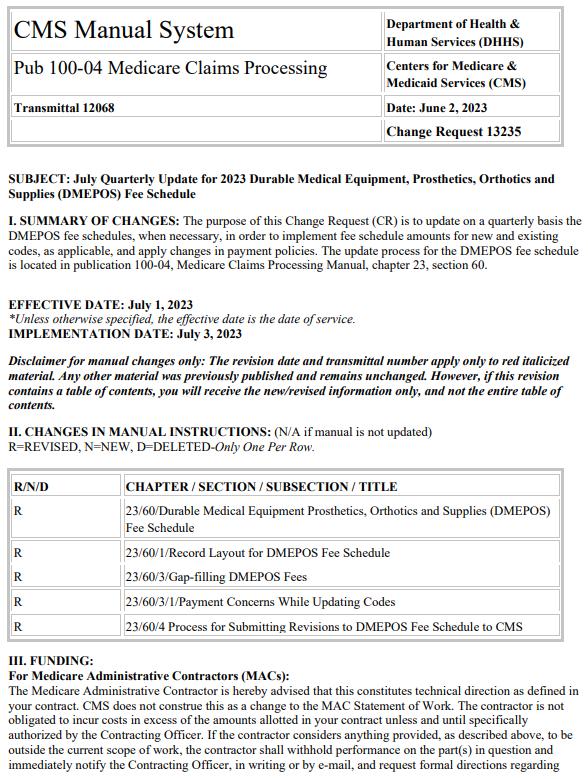
Therew ereSEVEN new or revised Transmittalsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.





Therew as1new or revised MedLearn released thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.





Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to thebest of CorroHealth'sknowledgeisaccurateat thetimeof distribution. However, due to the ever-changinglegal/regulatory landscape, thisinformation issubject to modification asstatutes, laws, regulations, and/or other updatesbecome available. Nothingherein constitutes, isintended to constitute, or should berelied on aslegal advice. CorroHealth expresslydisclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anything contained in thematerials, which areprovided on an "as-is"basisand should beindependentlyverified before beingapplied. You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability. The information in thisdocument isconfidential and proprietaryto CorroHealth and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduceor transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording, and broadcasting, or byanyinformation storageand retrieval system must beobtained in writingfrom CorroHealth. Request for permission should bedirected to Info@Corrohealth.com.

