j our nal e
Modifier 25 Policy
CignaDelays
Controversial Policy
Proper Coding For Tomosynthesis



CignaDelays
Controversial Policy
Proper Coding For Tomosynthesis


Quest ion:
We have been billing non-covered observation hours on our claims when applicable. All of them seem to be billing OK, with the exception of Traditional Medicare The non-covered observation hours are on a separate line with a modifier attached (G0378-GY). Could you please advise on this situation?

Answ er:
A Medicare beneficiary should not be charged for observation hours that exceed the Medically Unlikely Edit (MUE) of 72 hours Medicare cautions that there is a difference between non-covered and nonpayment and that Medicare covers all medically reasonable and necessary observation services.
Medicare Administrative Contractor Novit as suggests hospitals bill hours beyond the MUE under revenue code 0762 with no HCPCScode with charges in the non-covered fields.

The GYmodifier should only be appended to services or items statutorily excluded from Medicare coverage. Observation hours do not meet that definition.
Further, Medicare indicates that admitting or discharging an observation patient rarely takes over 48 hours. If the observation cases extend beyond that time, the patient possibly met the admission criteria

Chapter 4 of the Medicare Claims Processing Manual, states:

Referencing CMSChapter 6 of the Medicare Benefit Policy Manual, 20 6 (B Coverage of Outpatient Observation Services):


Although Observation patients receive a Medicare Outpatient Observation Notice (MOON), the Medicare Benefit Policy Manual further discusses observation services and the ABN for non-covered items or services.

Quest ion:
We understand we cannot use the facility charge of Q3014 anymore. Is this correct?Can we still bill the professional and facility levels associated with the telehealth visits?For example, 99201-99205 and 99211-992115 for a professional and a small facility charge to match?
Answ er:
Now that the Public Health Emergency (PHE) is over, hospitals may report Q3014 only if the patient comes to the facility to utilize HIPAA-compliant telehealth equipment while a distant site practitioner performs a telemedicine visit.
Although billing professionals may continue to bill Medicare for telehealth services (subject to Medicare?s ?List of Telehealth Servicesfor Calendar Year 2023?), hospitals may no longer report HCPCSQ3014 (Telehealth originating facility fee) to claim reimbursement for supporting a facility-based physician or non-physician practitioner performing a telemedicine service
In addition, telehealth equipment must be HIPAA compliant after 5/11/2023.
Remote services provided by facility staff (such as physical therapists, etc.) will no longer be covered by Medicare, except certain mental health or substance abuse disorder treatment reported with HCPCSC7900 ? C7902.)
An FAQ published by CMSoffers more guidance to billing after the PHEended. A link and an excerpt are provided for your review. I have also attached a paper that outlines the changes.
FAQs: CMSWaivers, Flexibilities, and the End of the COVID-19 Public Health Emergency

FAQs: CMSWaivers, Flexibilities, and the End of the COVID-19 Public Health Emergency

17. At the end of the PHE, when can hospitals bill for:
i The originating site facility fee (HCPCScode Q3014)?
ii The clinic visit (HCPCScode G0463)?
iii. Remote mental health services (HCPCScodes C7900 - C7902)?
Following the anticipated end of the PHE(May 11, 2023):
i Hospitals cannot bill for this code after the PHEunless the beneficiary is located within a hospital and the beneficiary receives a Medicare telehealth service from an eligible distant site practitioner Only in these cases can the hospital bill for the originating site facility fee (HCPCScode Q3014).
ii.If the beneficiary is within a hospital and receives a hospital outpatient clinic visit (including a mental/behavioral health visit) from a practitioner in the same physical location, then the hospital would bill for the clinic visit (HCPCScode G0463)
iii.If the beneficiary is in their home and receives a mental/behavioral health service from hospital staff through the use of telecommunications technology and no separate professional service can be billed, then the hospital would bill for the applicable HCPCS C-code describing this service (HCPCScodes C7900 - C7902).

Quest ion:
We are going live on June 1, 2023 with a new 3-D mammography machine. Are there any new codes we should be using for billing?We've looked at 77061, 7706 and 77063 for Breast Tomosynthesis Screening And Diagnostic, but we don't see a reimbursement. Can you provide some assistance?
Answ er:
Congratulations on your new equipment! That?s a wonderful enhancement to the hospital?s service to the community.
I have attached our coding matrix for mammography services, which was last updated in 2022; coding has not changed.
In summary, the codes you will need to report tomosynthesis are 77063 and G0279 for Medicare and MediCal (G0279 is diagnostic tomo, unilateral or bilateral). Not all commercial payers will accept G0279, they may require the hospital to report 77061 for a unilateral diagnostic or 77062 for bilateral diagnostic Medicare does not accept 77061 of 77062, it requires providers to report G0279 instead Both G0279 and 77063 are reimbursed by Medicare under the Medicare Physician Fee Schedule at $26.33 for the technical component.
Commercial payers who do not accept G-codes may prefer 77061-77062 for diagnostic tomosynthesis.

Like Medicare, Medi-Cal accepts/reimburses G0279 and 77063 for tomosynthesis Here are excerpts from the Medi-Cal fee schedule


Report the screening code 77063 under revenue code 0403 ? Other Imaging Services ? Screening Mammography.
Report the diagnostic code G0279 (or 77061-77062) under revenue code 0401 ? Other Imaging Services ?Diagnostic Mammography
On May 22, 2023, The Cigna Group added a banner to it?s controversial ?Modifier 25?

Reimbursement Policy website announcing that implementation of the policy will be delayed as they ?continue to review for future implementation?:

This is the second time Cigna has delayed this unpopular proposed policy The policy was first introduced in 2022, but Cigna delayed implementation, presumably due to physician opposition
In March of 2023, Cigna announced it would implement the policy in certain states on May 25, 2023, but again announced its delay on May 22, 2023 The policy requires professional fee providers to submit office notes (via email or fax) when billing office visit codes 99212-99215 with modifier 25. Modifier 25 indicates the E/M was a separate and distinct service performed during the same visit as another billable procedure
Under Cigna?s new policy, if office notes were not submitted by email or fax to support the claim, payment would be denied
A link and an excerpt from the policy is provided below:
https://static.cigna.com/assets/chcp/secure/pdf/resourceLibrary/clinReimPolsModifi ers/Notifications/Modifier 25 Significant Separately Identifiable Evaluation and M anagement pdf ?
? Cigna requires the submission of office notes with claims submitted with E/M CPT® codes 99212, 99213, 99214 and 99215, and modifier 25 when billed with a minor procedure. The E/M line will be denied if Cigna does not receive adequate documentation to support that a significant and separately identifiable service was performed The documentation should be submitted with a cover sheet indicating the office notes supports the use of modifier 25 appended to the E/M code.?
A number of physician organizations, including the American Medical Association (AMA), the American Academy of Family Physicians (AAFP), and several other major medical groups have unleashed public letter-writing campaigns to persuade Cigna not to implement the new policy.

CorroHealt h invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

New s
- COVID-19: Public Health Emergency Ended May 11
- End of COVID-19 Public Health Emergency FAQs
- Advancing Health Equity Through The CMSInnovation Center: First Year Progress And What?s To Come
- Power Seat Elevation Equipment on Power Wheelchairs: Coverage, Coding, & Payment
- Medicare Shared Savings Program: Apply for January 1 Start Date by June 15
- Inpatient Rehabilitation Facility Services: Review Choice Demonstration
- Women?s Health: Talk with Your Patients About Making their Health a Priority
Claim s, Pricers, & Codes
- COVID-19: Reporting CRModifier & DRCondition Code After Public Health Emergency ?
Reminder
Event s
- Skilled Nursing Facility: Minimum Data Set Resident Assessment
Instrument Training
Publicat ions
- Screening Pap Tests & Pelvic Exams ? Revised
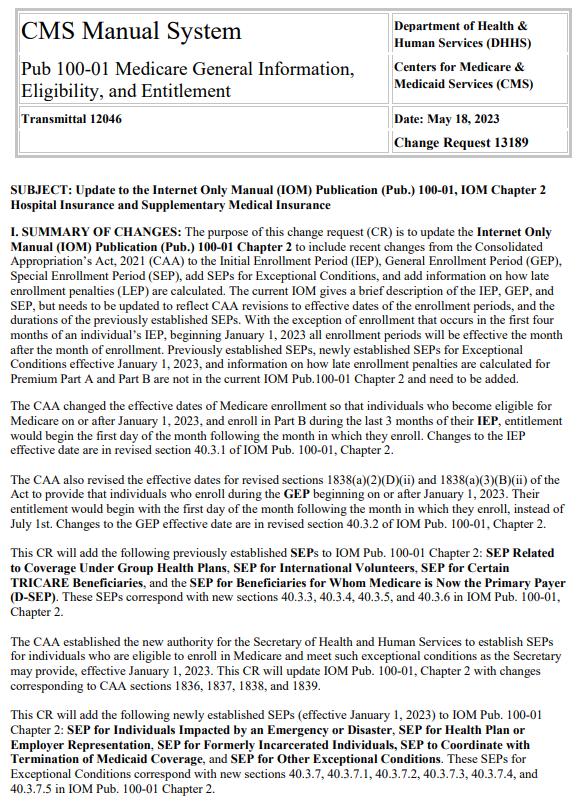
Therew ereSEVEN new or revised Transmittalsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.







Therew as1new or revised MedLearn released thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.


Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to thebest of CorroHealth'sknowledgeisaccurateat thetimeof distribution. However, due to the ever-changinglegal/regulatory landscape, thisinformation issubject to modification asstatutes, laws, regulations, and/or other updatesbecome available. Nothingherein constitutes, isintended to constitute, or should berelied on aslegal advice. CorroHealth expresslydisclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anything contained in thematerials, which areprovided on an "as-is"basisand should beindependentlyverified before beingapplied. You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability. The information in thisdocument isconfidential and proprietaryto CorroHealth and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduceor transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording, and broadcasting, or byanyinformation storageand retrieval system must beobtained in writingfrom CorroHealth. Request for permission should bedirected to Info@Corrohealth.com.

