CONGRESSDELAYSLAB PAMA REPORTINGTO 2024

Within the Consolidated Appropriations Act of 2023 on December 23, 2022, Congress once again delayed the reporting period for private payer payment data on non-patient lab services. However, the data collection period remains January 1, 2019 through June 30, 2019.

In addition, Congress delayed cuts to lab test reimbursement that would have kicked in on January 1, 2023.
The private payer payment rate reporting requirement applies to ?applicable laboratories?, which includes hospitals which received more than $12,500 in Medicare reimbursement for non-patient lab services (billed on a 14XType of Bill) in the period January-June 2019.(There are additional requirements that define an ?applicable laboratory?, but most are met by hospitals with ?outreach?laboratory services )
The announcement is on the CMSPAMA Regulations webpage: https://www cms gov/medicare/medicare-fee-for-service-payment/ clinicallabfeesched/pama-regulations
ParaRev offers assistance to organizations which meet Medicare?s definition of an ?Applicable Laboratory?definition in preparing Lab PAMA reports. To learn more about which organizations are required to submit the report, or ParaRev's solution to assist with this burdensome project, please reach out to a ParaRev Account Execut ives ? Violet Archuleta-Chiu (violet.archuleta-chiu@corrohealth.com) or Sandra LaPlace (Sandra.laplace@corrohealth.com).
4 PARA Weekly eJournal: January
2023
18
NO SURPRISESACTIDRDISPUTEFEEINCREASED BY 700% IN 2023
The administrative fee for the Independent Dispute Resolution (IDR) process has increased by 700%in 2023 The administrative fee to participate in a dispute related to the No Surprises Act (NSA) ban on balance billing jumped from $50 to $350. Given the significant increase in the fee, many providers may find that disputes are not worth the burden and forgo the process. With the volume of disputes filed in a five-month window exceeding the anticipated yearly volume, one can speculate that CMSis using the fee to alleviate some of the backlog.
In addition to the administrative fee hike, the threshold for the IDRarbitrators?fixed fee was increased to $700 in 2023, an increase of $200 over the 2022 rates. For batched cases, the maximum allowed fee increased from $670 in 2022 to $938 in 2023

Last year was the first year balance billing was banned under the NSA with respect to the following services:
- Emergency services

- Non-emergency items or services furnished by out-of-network (OON) providers at certain in-network health care facilities, and
- Air ambulance services furnished by OON providers of air ambulance services
The OON facilities and providers found themselves disputing reimbursement with health plans rather than balance billing patients The law created a process for providers and insurers to resolve payment disputes by entering into a baseball-style arbitration. When they couldn? t negotiate between themselves, they turned to certified IDRentities to resolve the dispute
The first report published by HHS, DOL, and the Treasury Department reported that over 90,000 disputes were submitted to the federal IDRportal between April 15 and September 30. The report provides some interesting data indicating how the system was overloaded Over 80%of the disputes originated from emergency department visits Only ten provider groups accounted for 75%of the disputes. United Healthcare was involved in 25%of the disputes followed by Aetna with 14% The complete report can be found at this link:
Initial Report on the Independent Dispute Resolution (IDR) Process (cms gov)
5 PARA Weekly eJournal: January 18, 2023
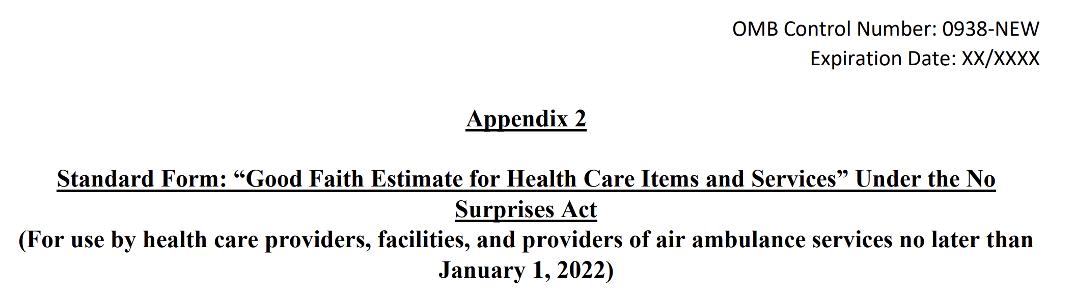
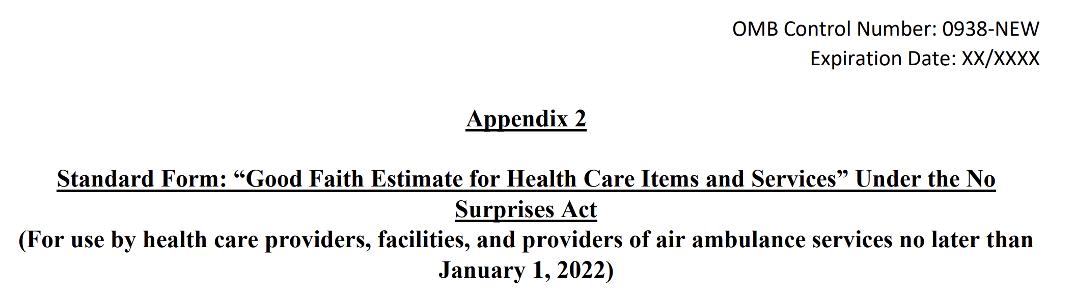
SHOPPINGAROUND: WHATCONSUMERS SEEIN GOOD FAITH ESTIMATES
What t o expect from a good fait h est im at e
Providers and facilities must give you:
- Your good faith estimate before an item or service is provided, within certain time frames

- An itemized list with specific details and expected charges for items and services related to your care
- Your good faith estimate in writing (paper or electronic) Note: A provider or facility can discuss the information included in the estimate over the phone or in person if you ask
- Your estimate in a way that?s accessible to you
Need help?View an example of what a good faith estimate may include (PDF) or a detailed explainer on the good faith estimate (PDF)
Disput ing charges higher t han t he est im at e
Once you get your good faith estimate from your provider or facility, keep it in a safe place so you can compare it to bills you get later
If you get the bill and the charges are at least $400 above the good faith estimate, you may be eligible to start a patient-provider dispute Learn more about the patient-provider dispute resolution process, including eligibility requirements View examples of good faith estimates that do and don't qualify for the dispute process. (PDF)
Insurance ID cards
Starting in 2022, new pricing information will be shown on any physical or electronic insurance identification card (ID) provided to you. This will include:
- Applicable deductibles
- Applicable out-of-pocket maximum limits
- A telephone number and website where you can get help or more information
A health plan may provide additional information on their website that you can access through a Quick Response code (commonly referred to as a QRcode) on a physical ID card, or through a hyperlink on a digital ID card.
9 PARA Weekly eJournal: January 18, 2023
SHOPPINGAROUND: WHATISA GOOD FAITH ESTIMATE?
what t heconsumer sees r egar dinggoodfait hest imat es
If you don? t have health insurance or you plan to pay for health care bills yourself, generally, health care providers and facilities must give you an estimate of expected charges when you schedule an appointment for a health care item or service, or if you ask for an estimate.

This is called a ?good faith estimate.?A good faith estimate isn? t a bill The good faith estimate shows the list of expected charges for items or services from your provider or facility. Because the good faith estimate is based on information known at the time your provider or facility creates the estimate, it won? t include any unknown or unexpected costs that may be added during your treatment.
Generally, the good faith estimate must include expected charges for:
- The primary item or service
- Any other items or services you?re reasonably expected to get as part of the primary item or service for that period of care
The estimate might not include every item or service you get from another provider or facility, even if some items or services may seem connected to the same service For example, if you?re getting surgery, the good faith estimate could include the cost of the surgery, anesthesia, any lab services, or tests In some cases, items or services related to the surgery that are scheduled separately, like certain pre-surgery appointments or physical therapy in the weeks after the surgery, might not be included in the good faith estimate. You?ll get a separate good faith estimate when you schedule those items or services with the provider or facility, or if you ask for it.
- After you schedule a health care item or service If you schedule an item or service at least 3 business days before the date you?ll get the item or service, the provider must give you a good faith estimate no later than 1 business day after scheduling If you schedule the item or service ORask for cost information about it at least 10 business days before the date you get the item or service, the provider or facility must give you a good faith estimate no later than 3 business days after you schedule or ask for the estimate
- That includes a list of each item or service (with the provider or facility), and specific details, like the health care service code
- In a way that?s accessible to you, like in large print, Braille, audio files, or other forms of communication
10 PARA Weekly eJournal: January 18 2023
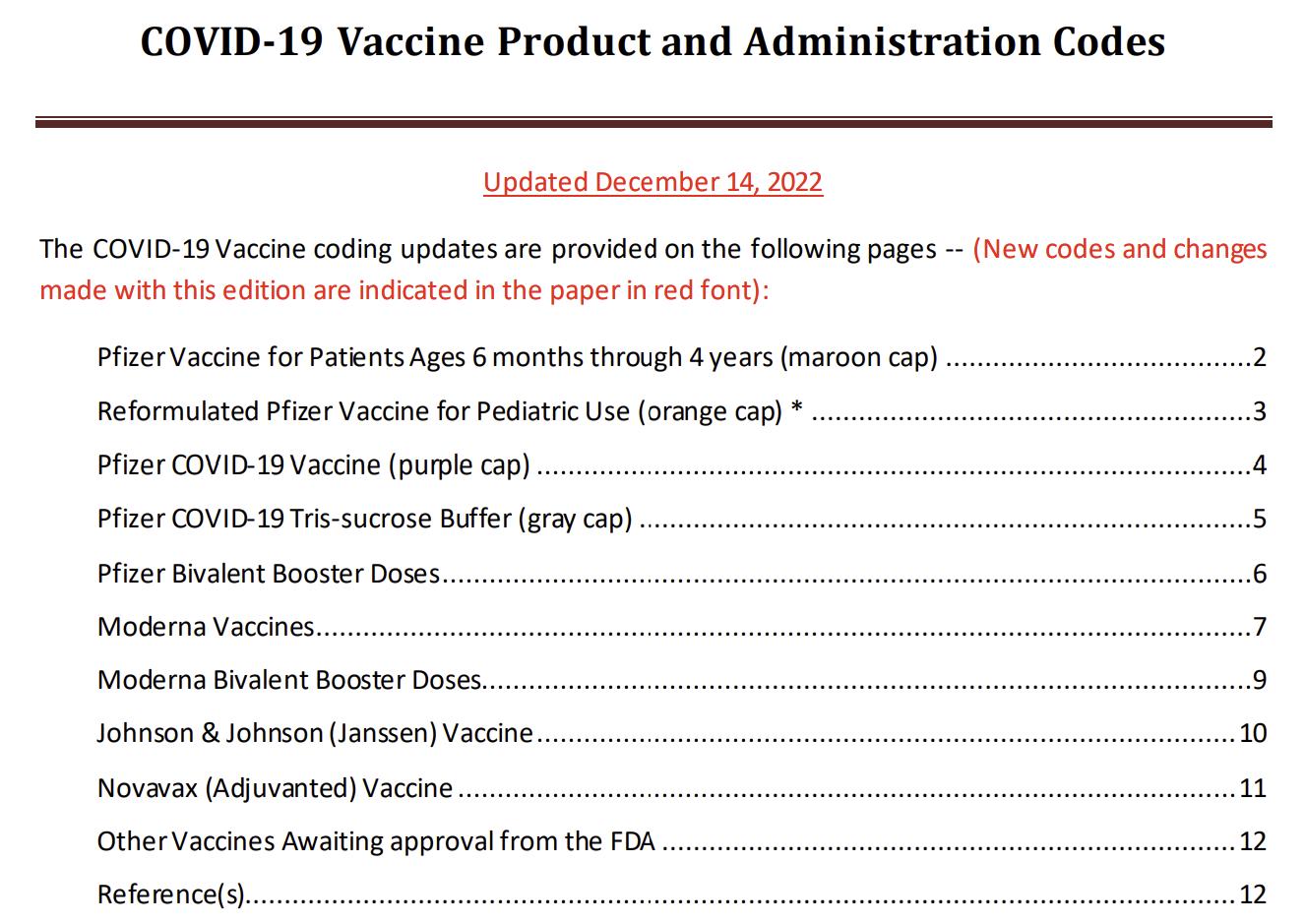
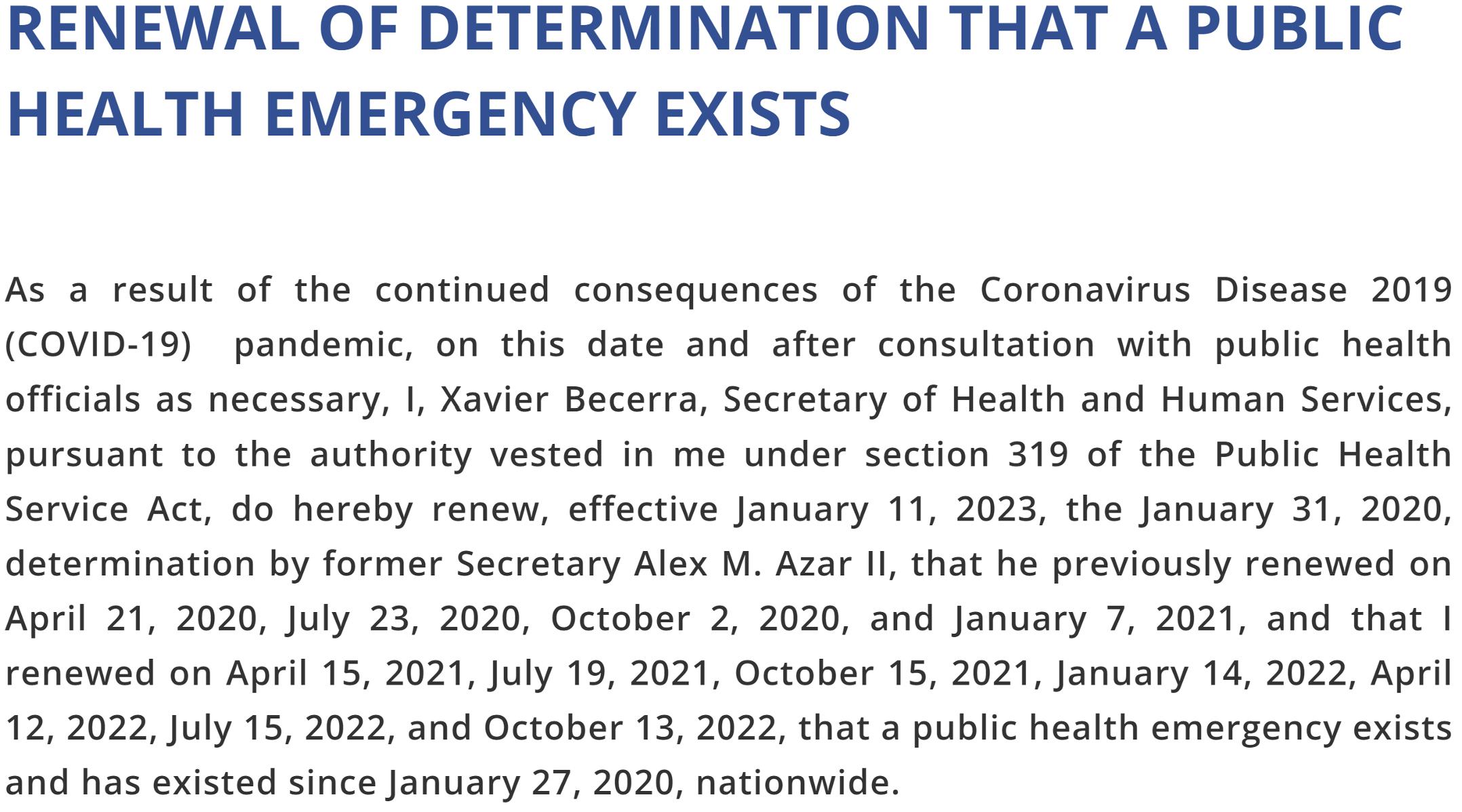
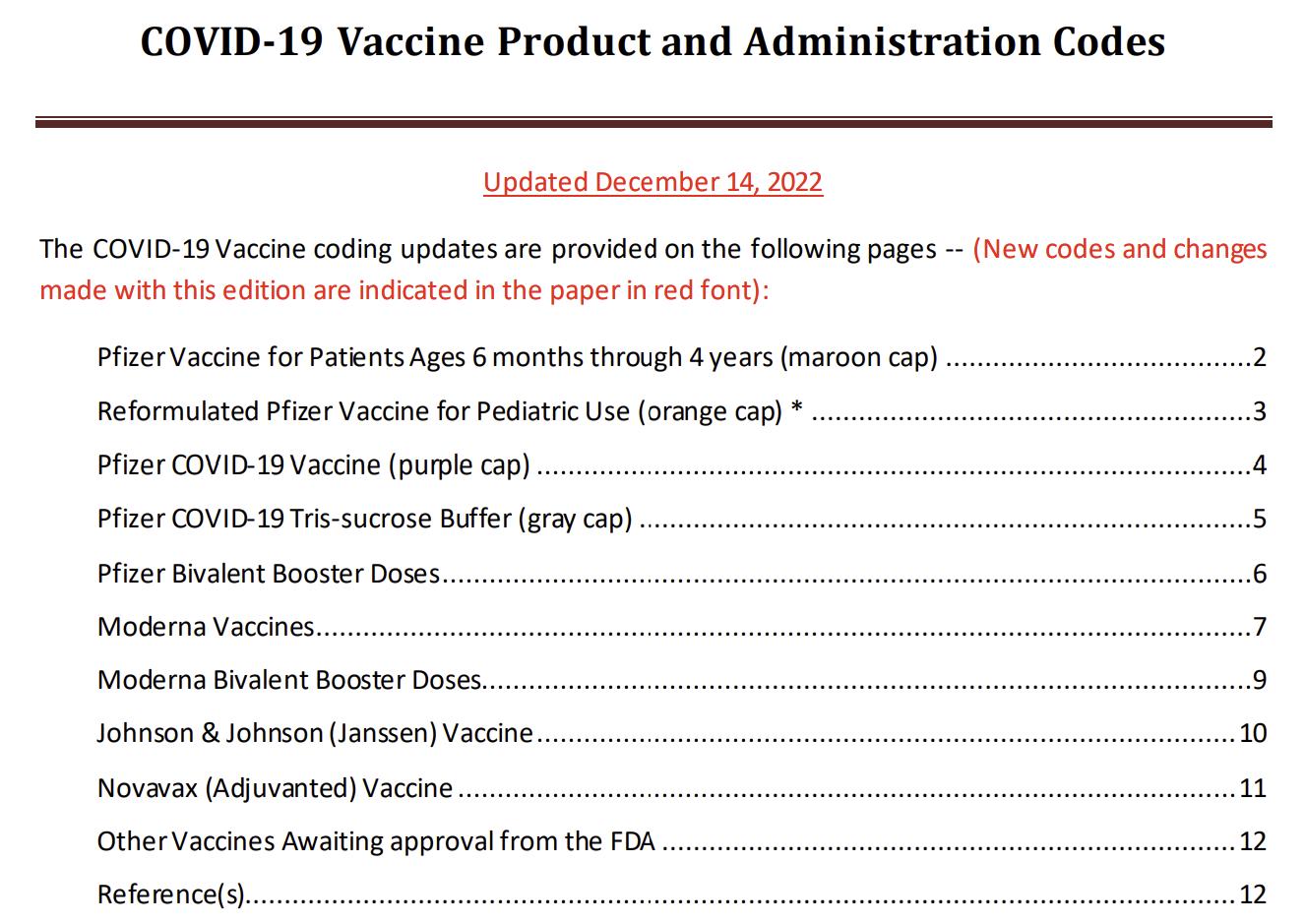
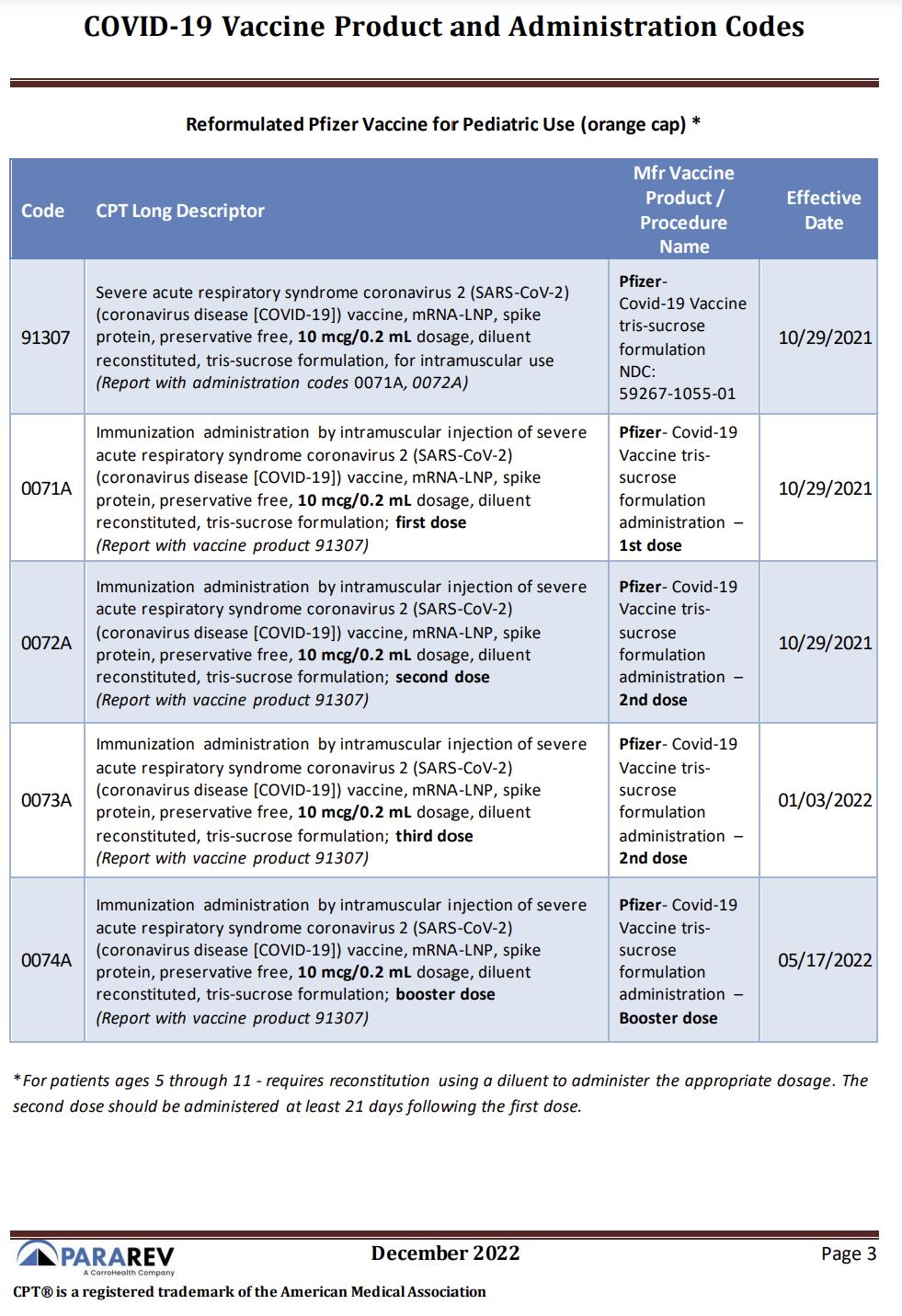
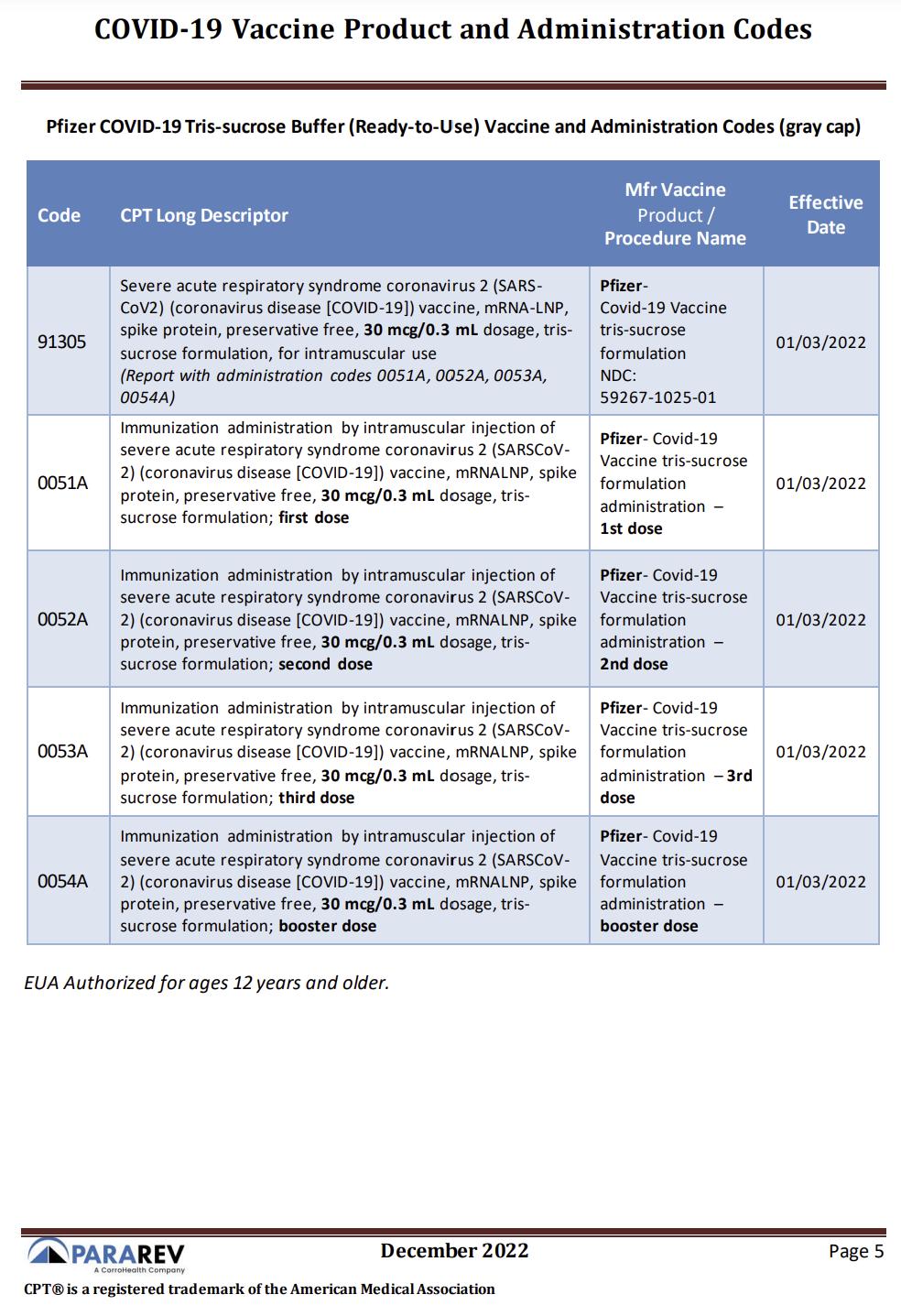
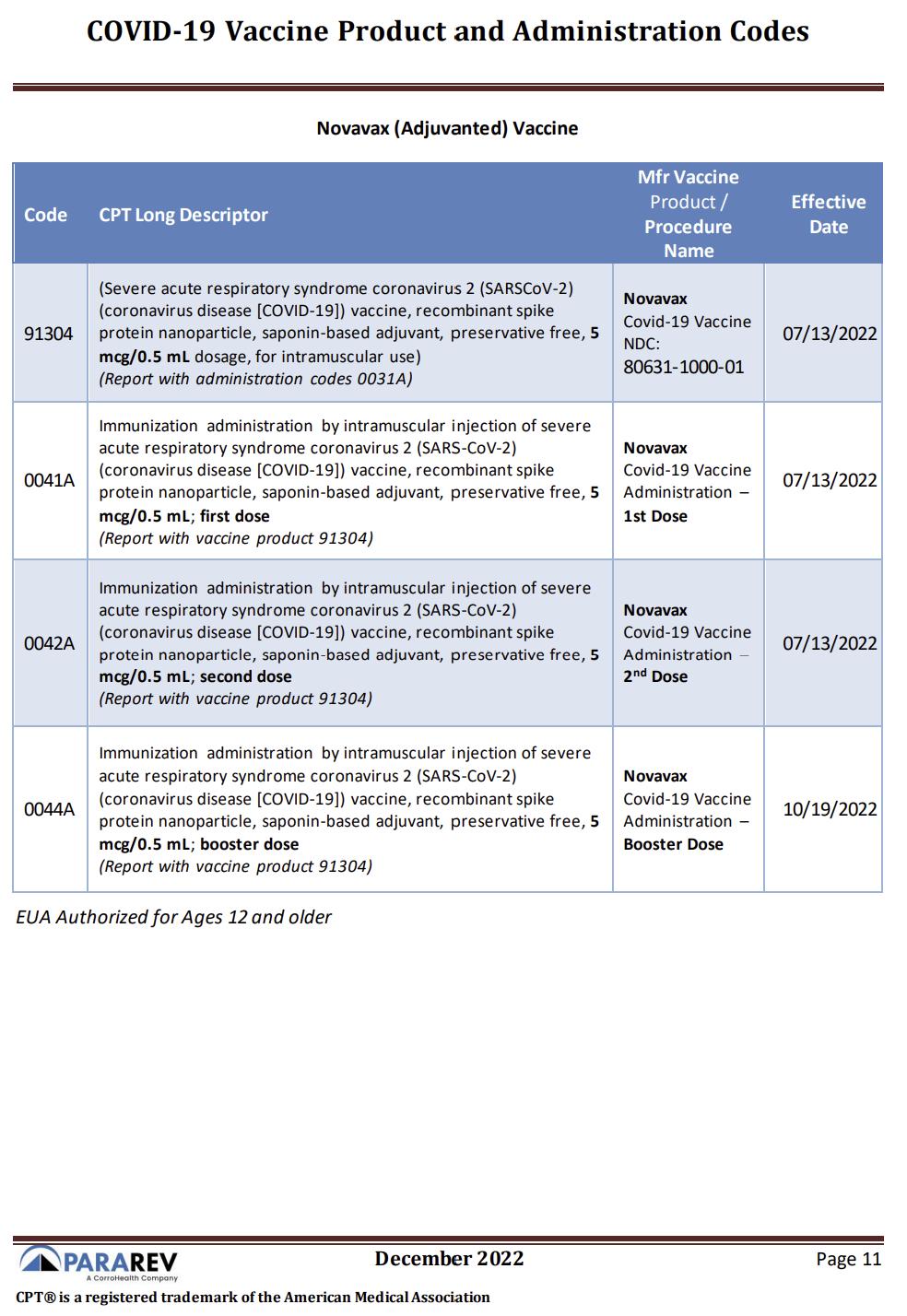
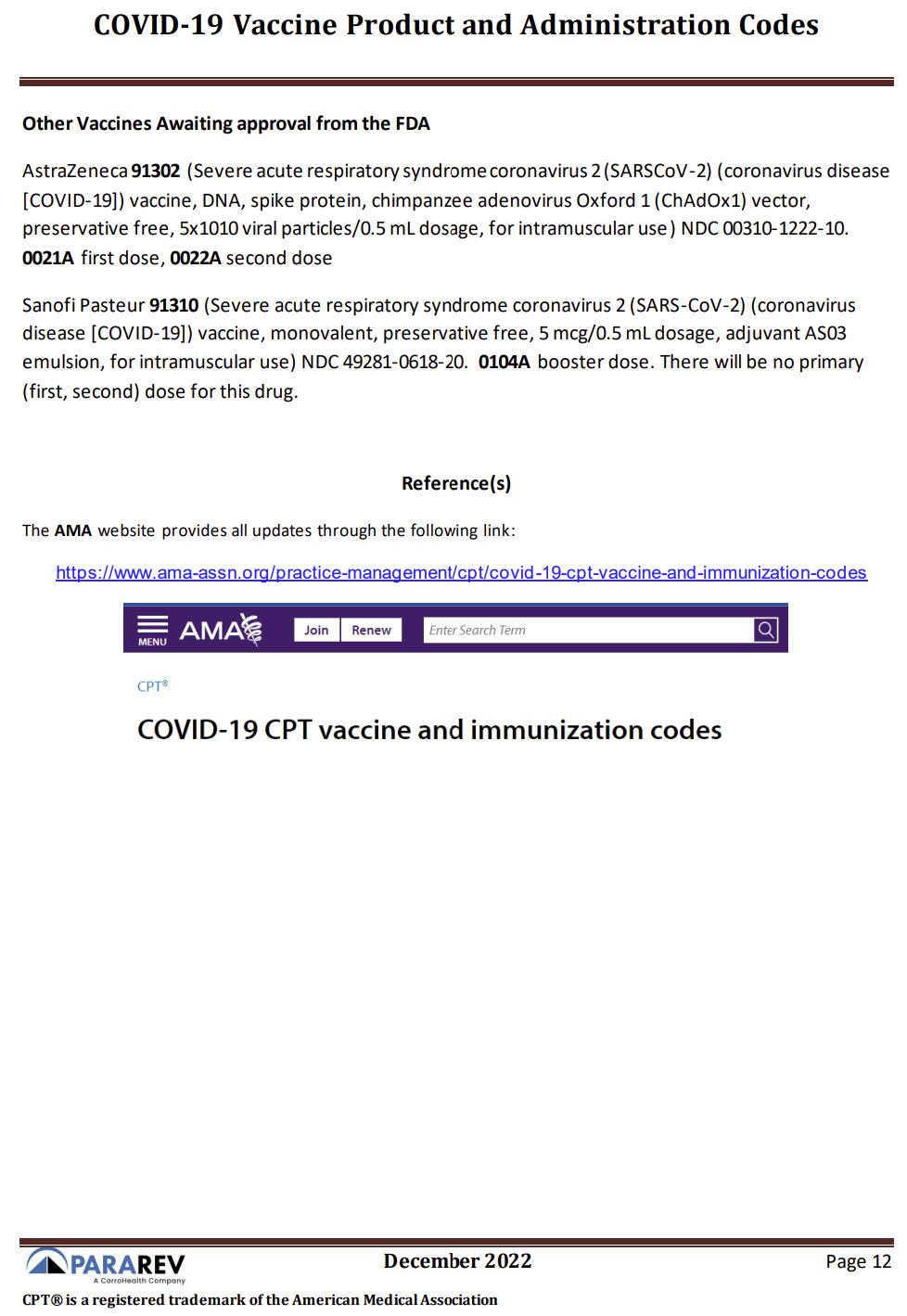
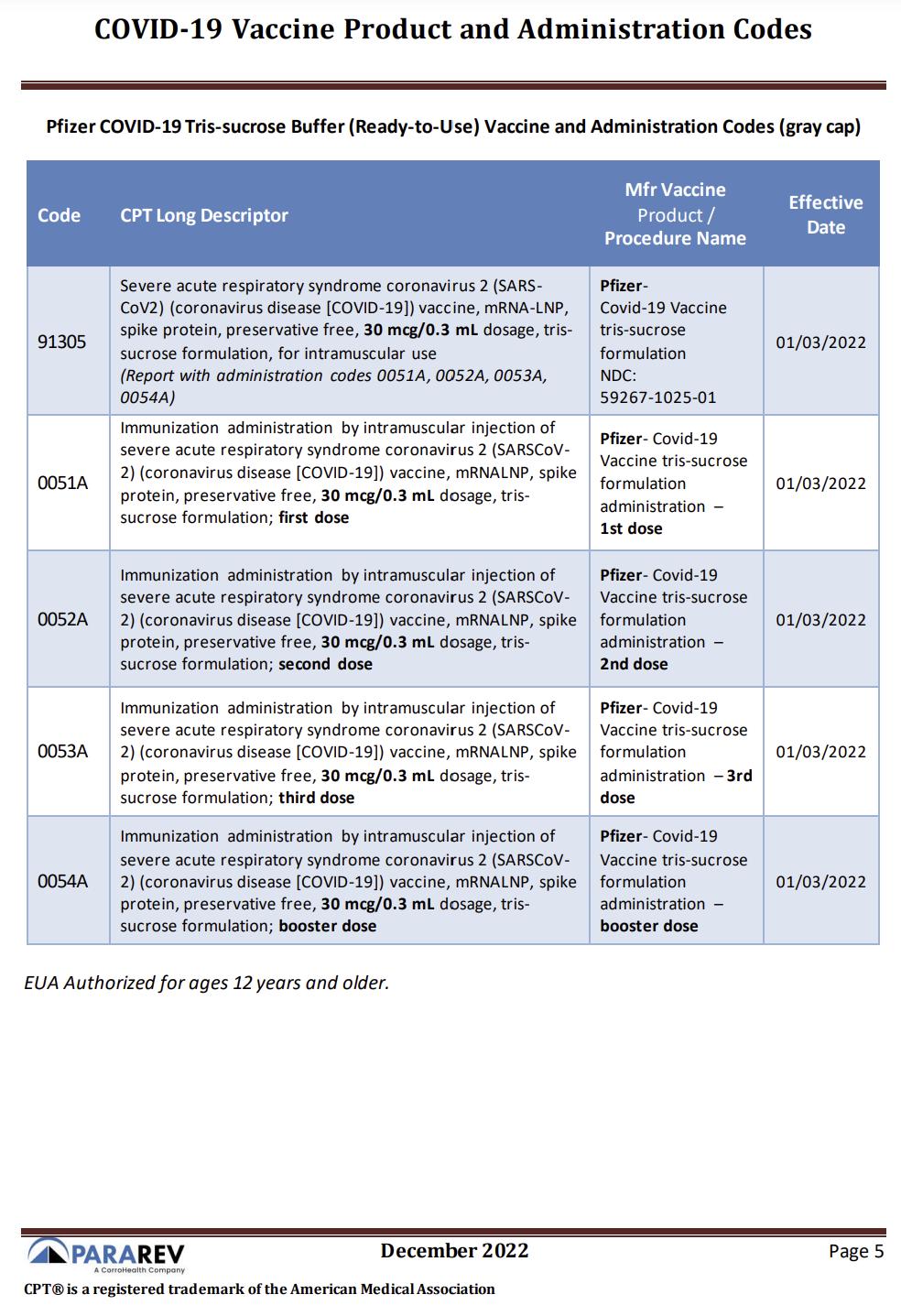
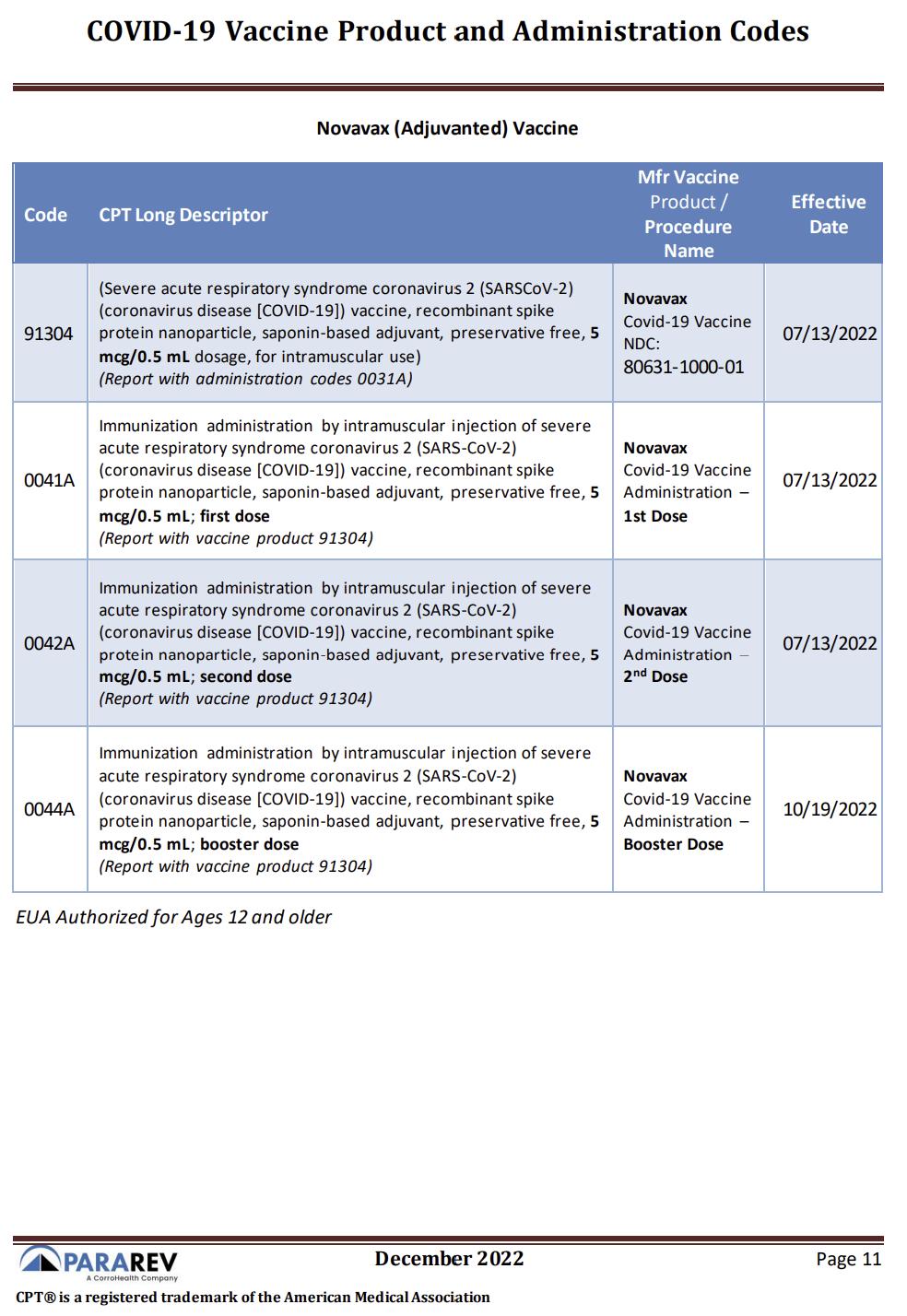
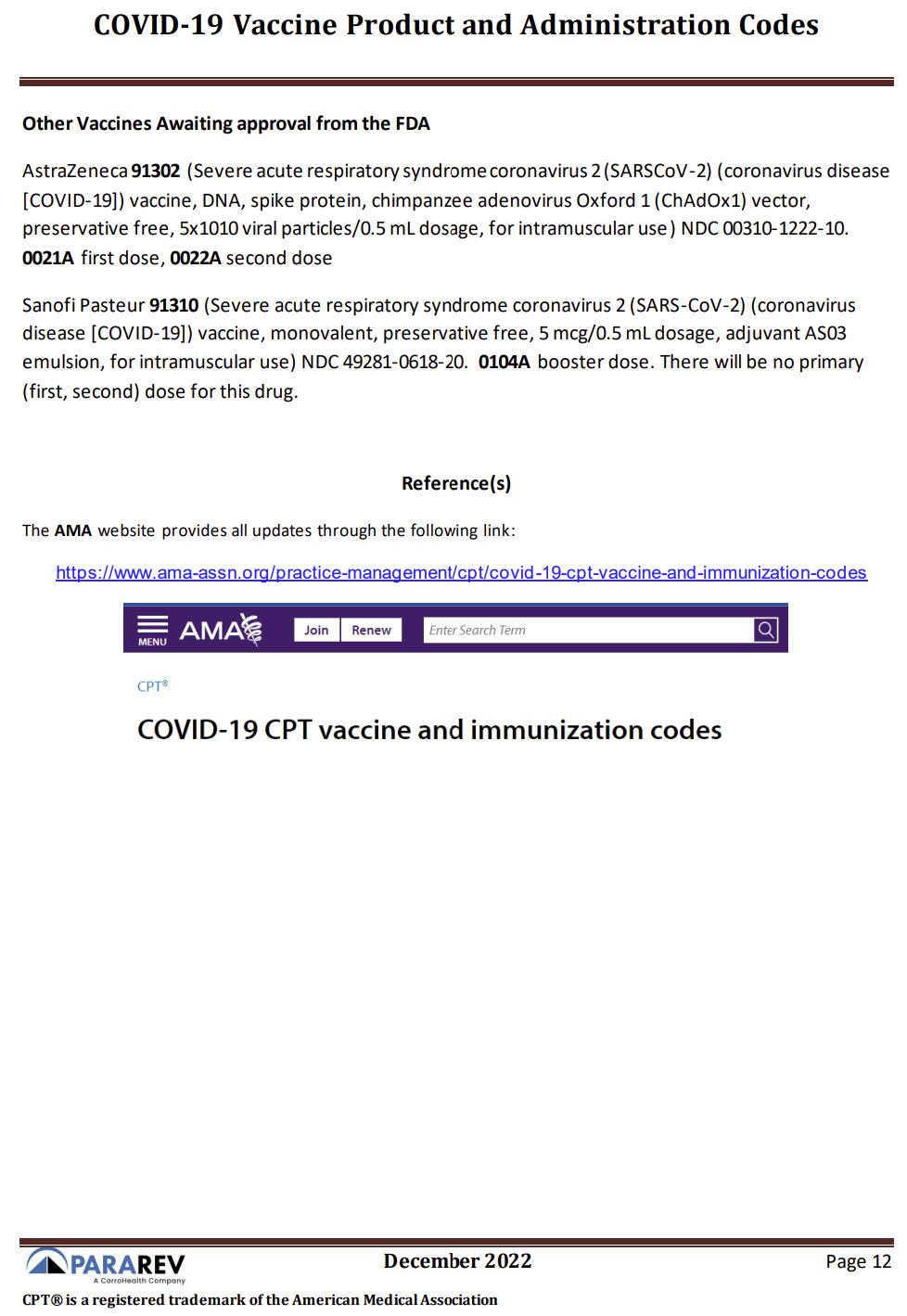
11 PARA Weekly eJournal: January 18, 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES

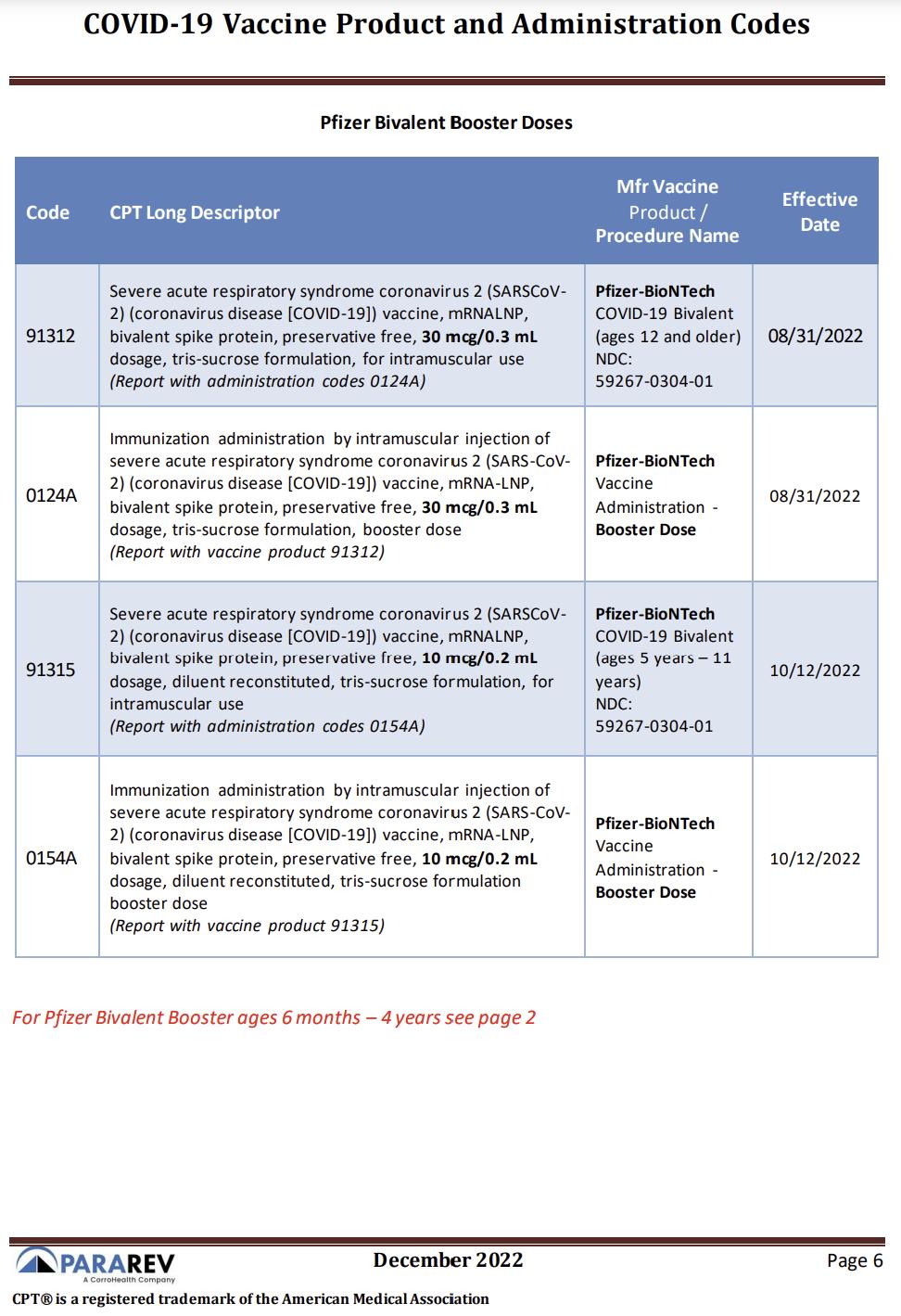
12 PARA Weekly eJournal: January 18 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES
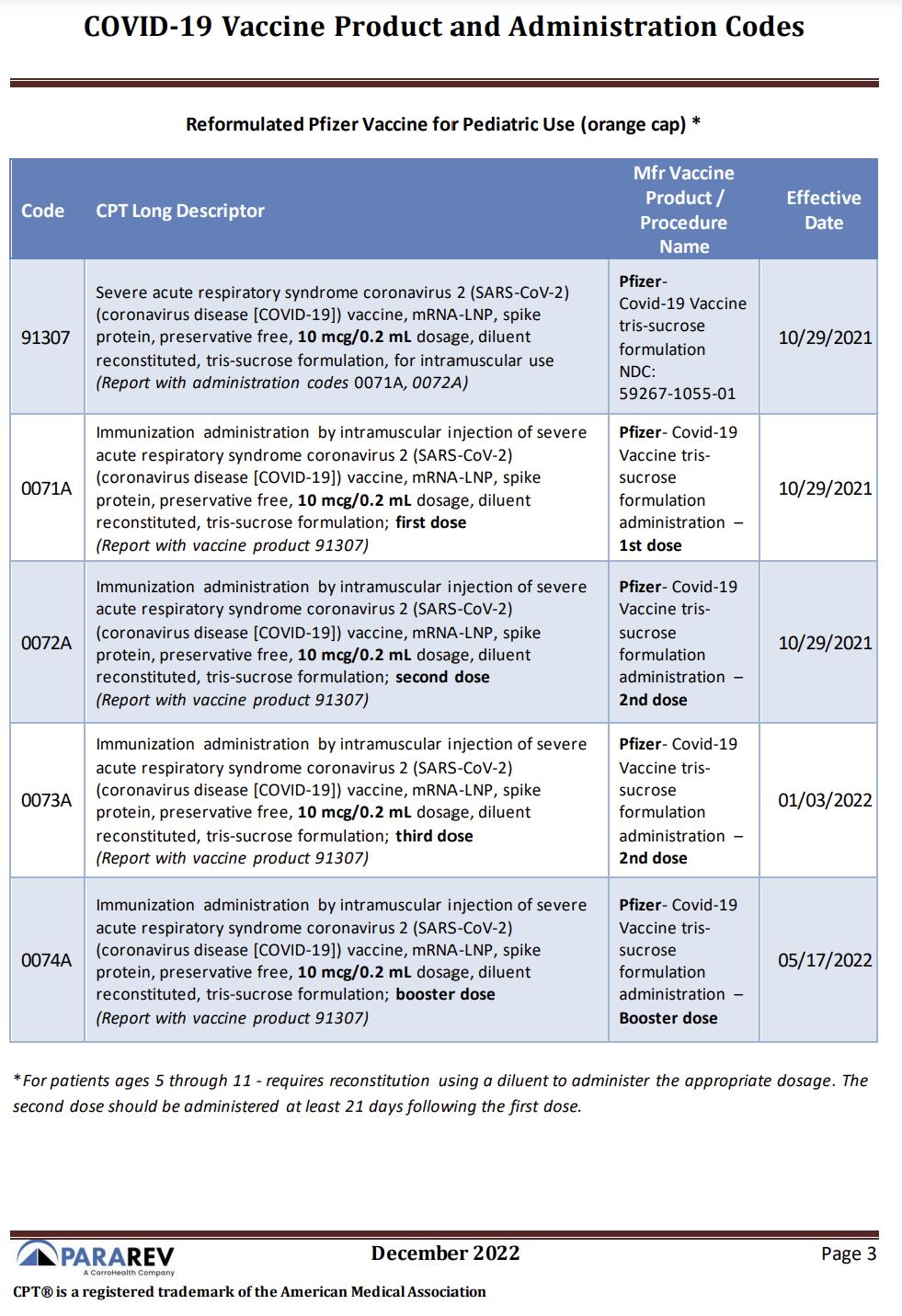
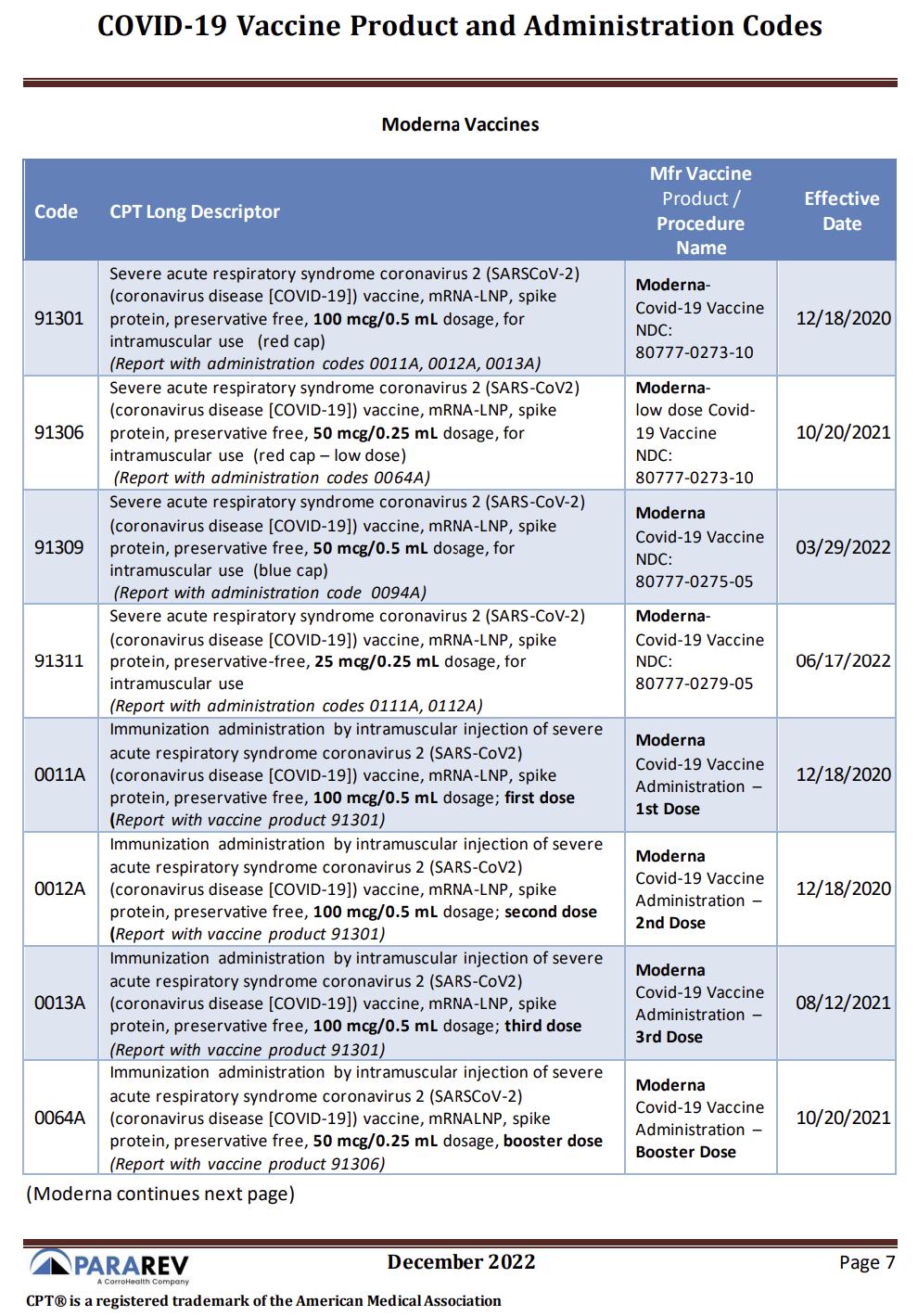
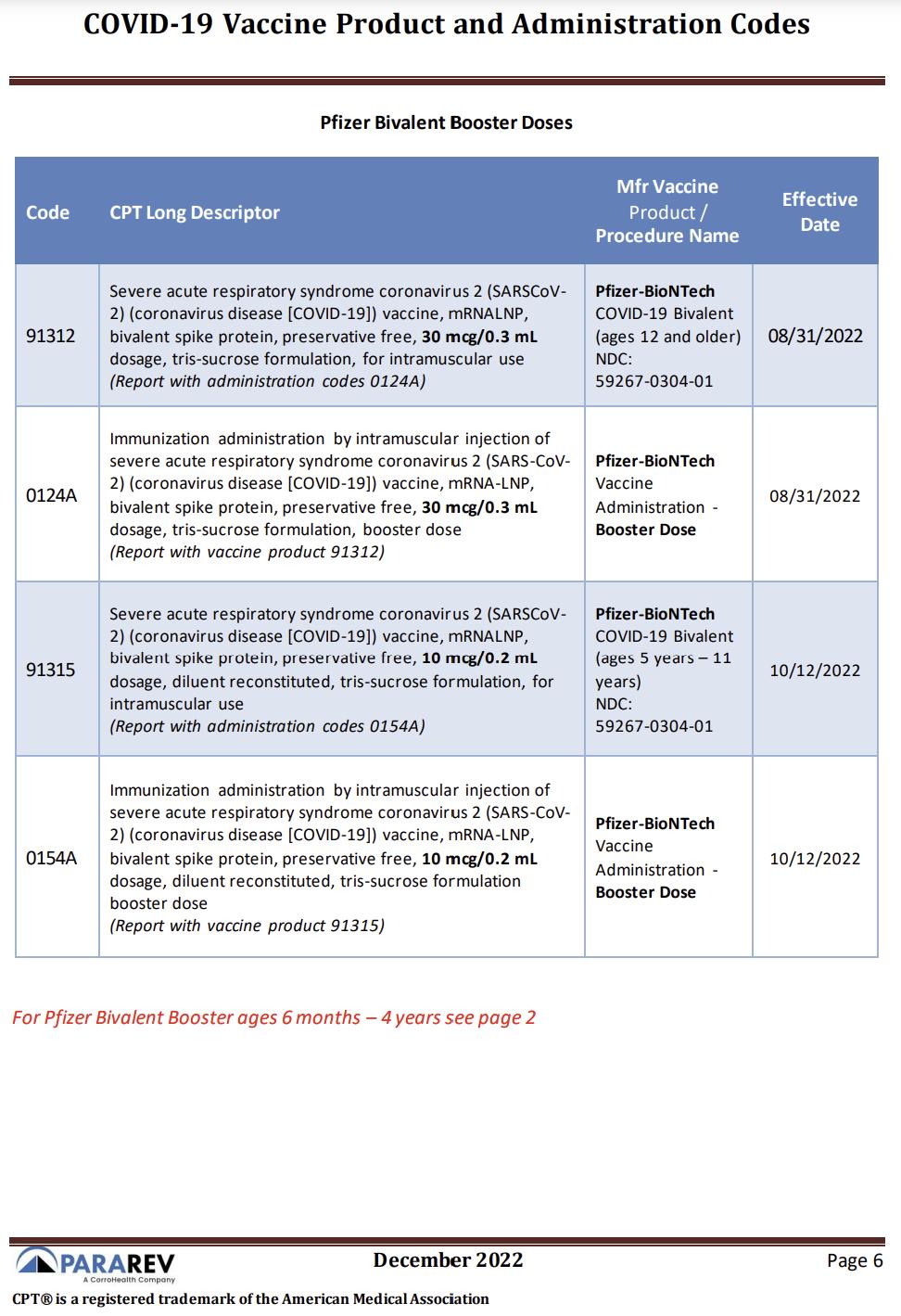
13 PARA Weekly eJournal: January 18, 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES

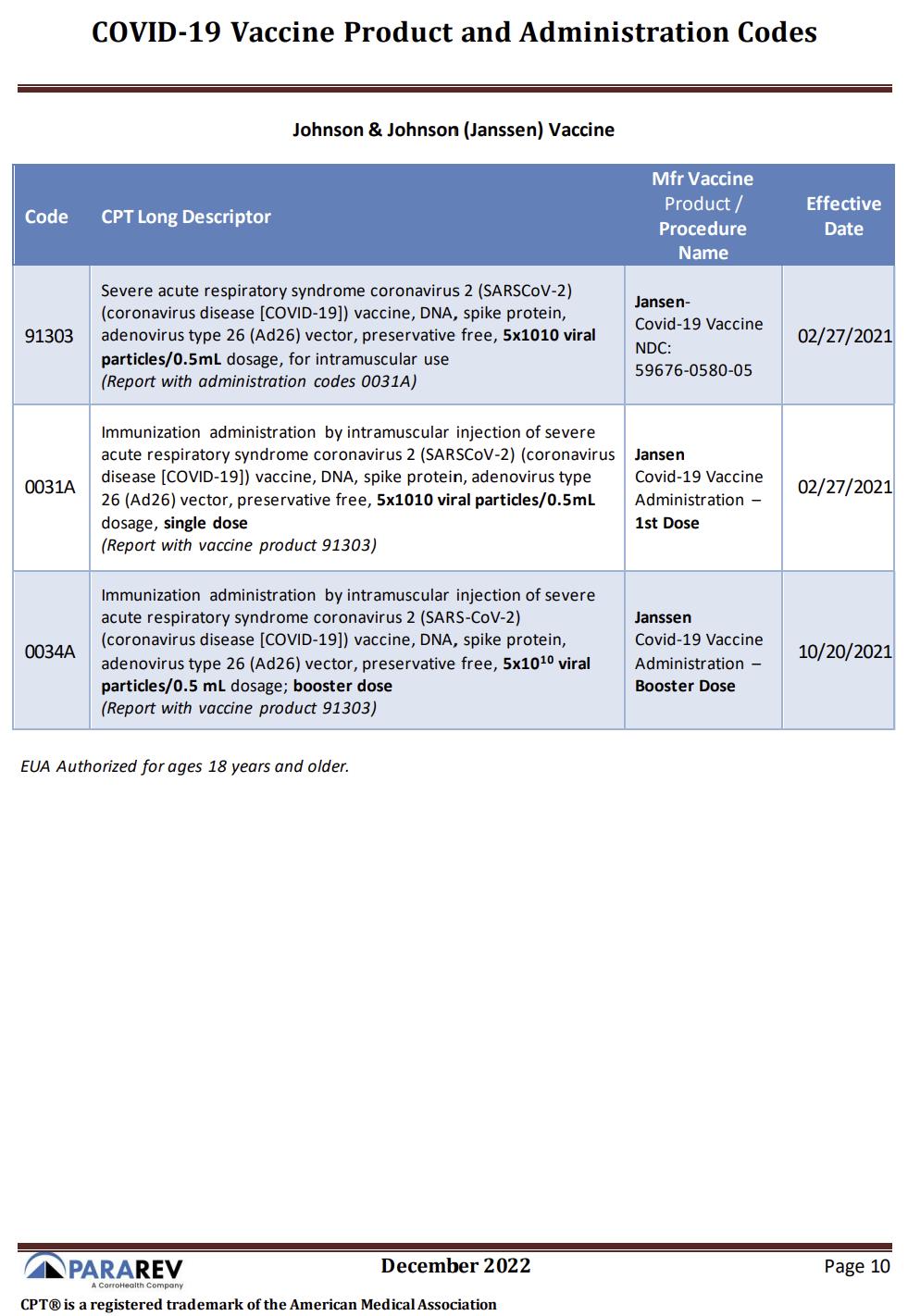
14 PARA Weekly eJournal: January 18 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES
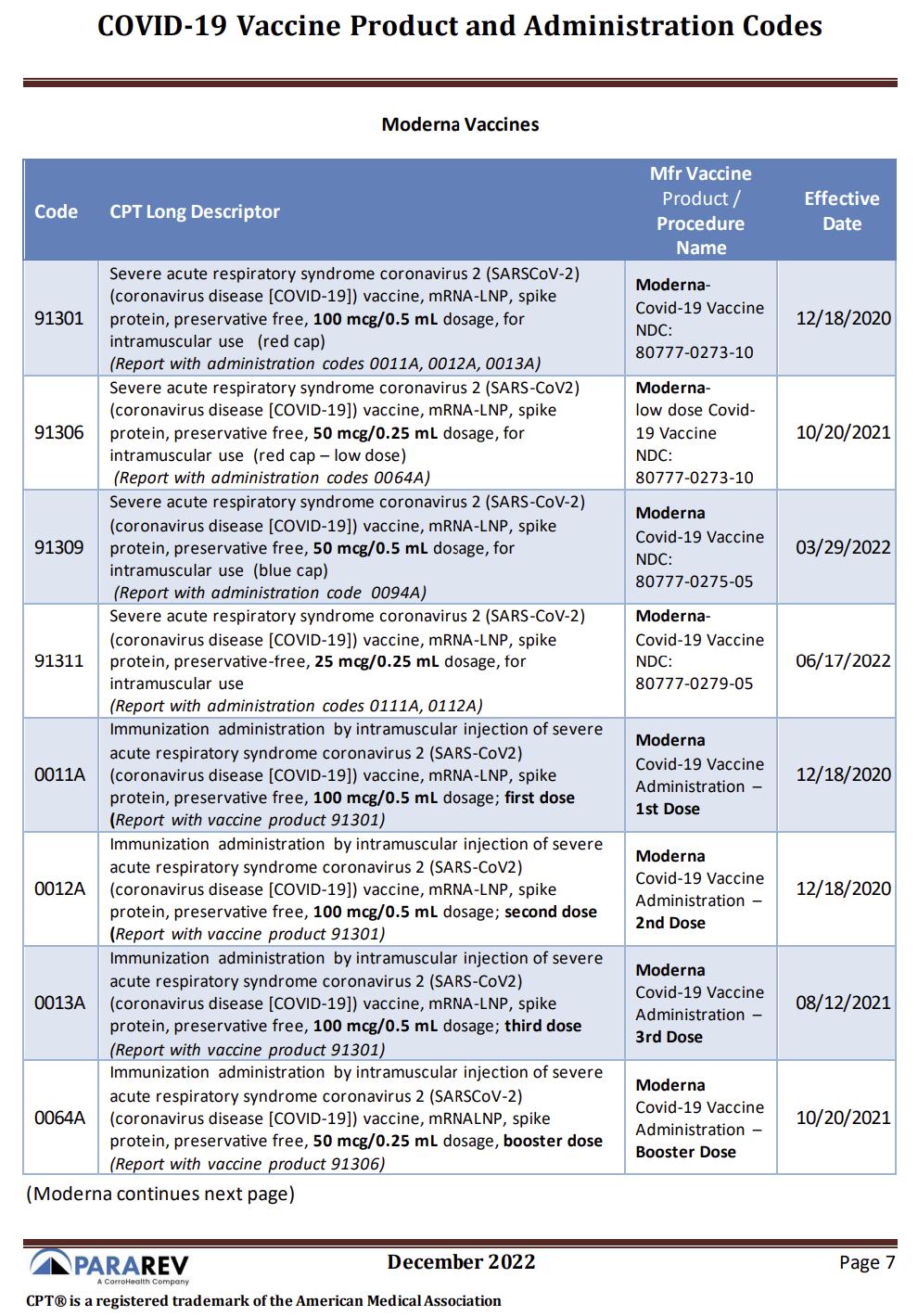
15 PARA Weekly eJournal: January 18, 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES
16 PARA Weekly eJournal: January 18 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES
17 PARA Weekly eJournal: January 18, 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES

18 PARA Weekly eJournal: January 18 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES

19 PARA Weekly eJournal: January 18, 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES
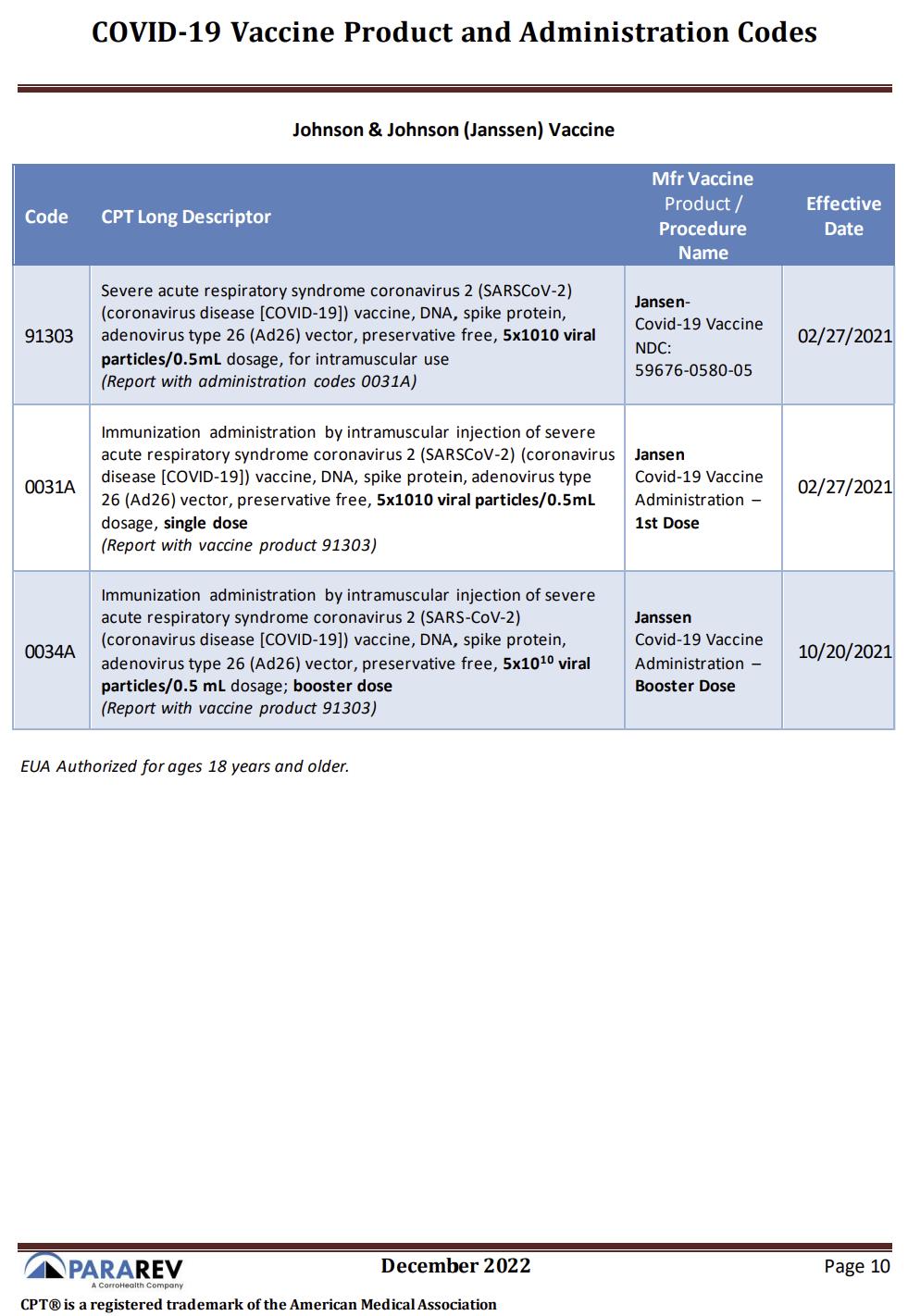
20 PARA Weekly eJournal: January 18 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES
21 PARA Weekly eJournal: January 18, 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES

22 PARA Weekly eJournal: January 18 2023 COVID-19 VACCINEPRODUCTAND ADMINISTRATION CODES
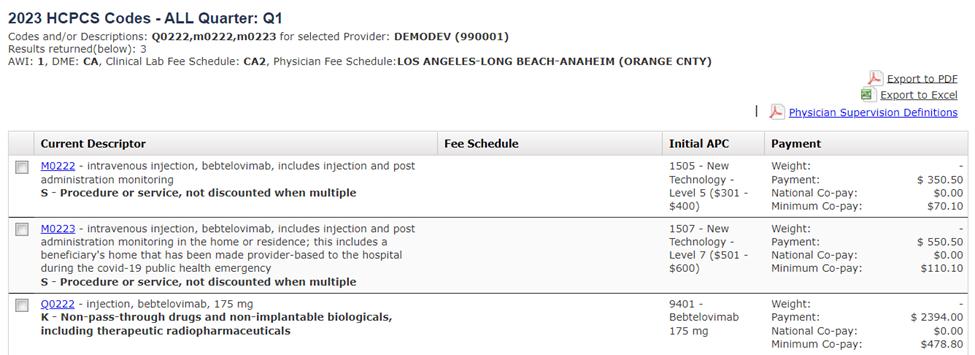
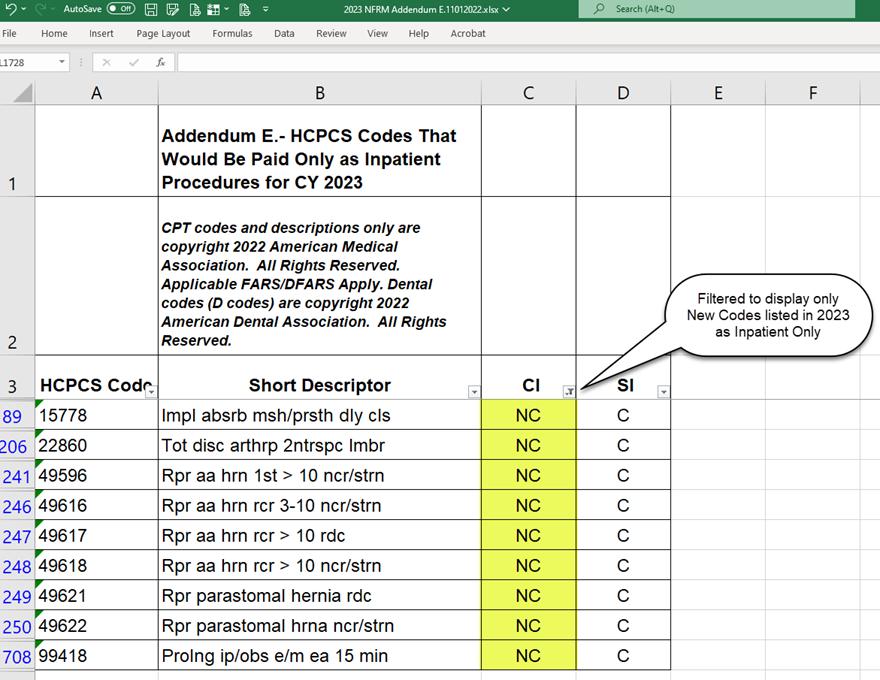
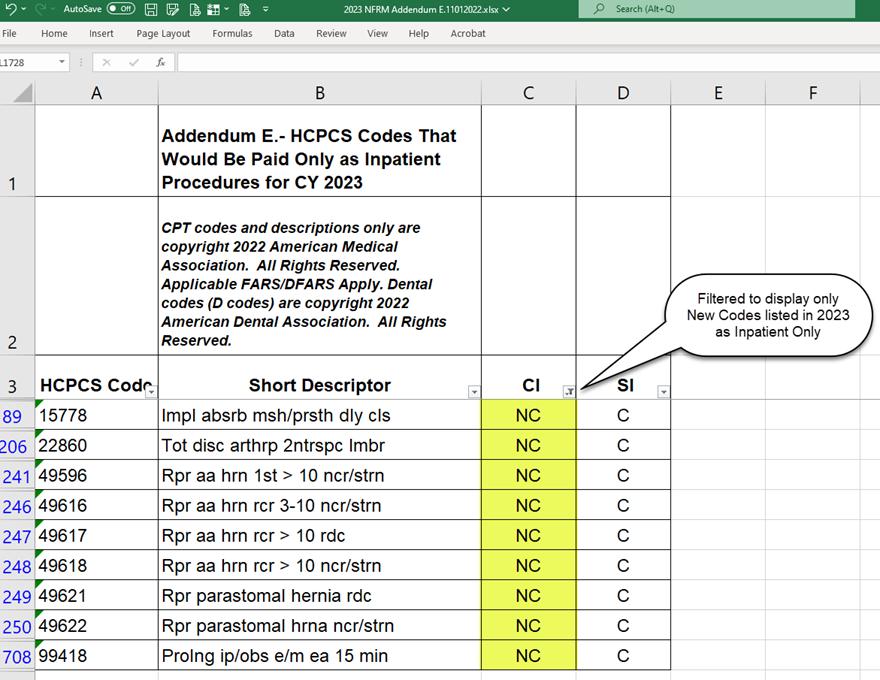
2023 OPPSUPDATE: INPATIENTONLY CHANGES
In the 2023 OPPSFinal Rule, Medicare added nine codes to OPPSAddendum E, the ?Inpatient only?list. Medicare will not cover these services when billed on an outpatient claim except if the patient expires before admission to inpatient status or when the provider transfers the patient to another facility.
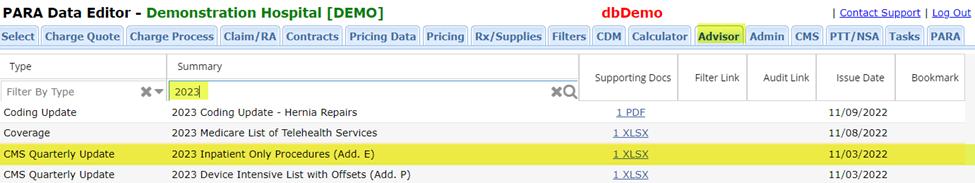
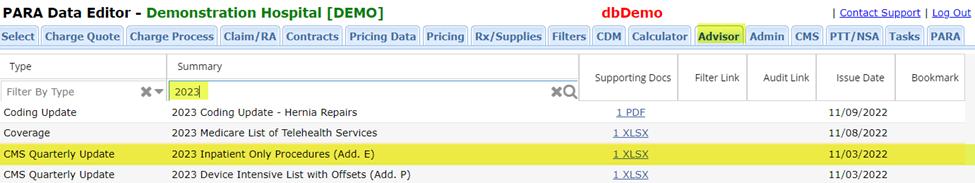
2023 Inpatient Only Procedures Addendum Emay be located by searching ?2023?in the Advisor tab of the PARA Dat a Edit or (PDE).
The nine newly added Inpatient Only HCPCSprocedures are identified with the letters ?NC?in the column labeled ?N?(Change Indicator) as shown below:
23 PARA Weekly eJournal: January 18, 2023
Medicare provides guidance on these exceptions in the Medicare Claims Processing Manual, Chapter 4 ?Part B Hospital, Paragraph 180.7 ? Inpatient-only Services: https://www cms gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c04 pdf
?There are two exceptions to the policy of not paying for outpatient services furnished on the same day with an ?inpatient-only?service that would be paid under the OPPSif the inpatient service had not been furnished:
Except ion 1:If the ?inpatient-only?service is defined in CPT to be a ?separate procedure?and the other services billed with the ?inpatient-only?service contain a procedure that can be paid under the OPPSand that has an OPPSSI=Ton the same date as the ?inpatient-only? procedure or OPPSSI = J1 on the same claim as the ?inpatient-only?procedure, then the ?inpatient-only?service is denied but CMSmakes payment for the separate procedure and any remaining payable OPPSservices. The list of ?separate procedures?is available with the Integrated Outpatient Code Editor (I/OCE) documentation. See http://www cms gov/Medicare/Coding/OutpatientCodeEdit/
Except ion 2:If an ?inpatient-only?service is furnished but the patient expires before inpatient admission or transfer to another hospital and the hospital reports the ?inpatient only?service with modifier ?CA?, then CMSmakes a single payment for all services reported on the claim, including the ?inpatient only?procedure, through one unit of APC5881, (Ancillary outpatient services when the patient dies.) Hospitals should report modifier CA on only one procedure.?
CMSsummarized the CY2023 Medicare Hospital Outpatient Prospective Payment System and Ambulatory Surgical Center Payment System Final Rule changes in its Newsroom Fact Sheet available through the following link: https://www cms gov/newsroom/ fact-sheets/cy-2023-medicare-hospitaloutpatientprospective-payment-systemand-ambulatory-surgical-center-2
24 PARA Weekly eJournal: January 18 2023
2023 OPPSUPDATE: INPATIENTONLY CHANGES
PARA YEAR-END HCPCSUPDATEPROCESS
As usual, clients will be fully supported with information and assistance on the annual CPT® HCPCScoding updates for calendar year 2023.
The PARA Dat a Edit or (PDE) contains a copy of each client chargemaster; we use the powerful features of the PDEto identify any line item in the chargemaster with a HCPCScode assigned that will be deleted as of December 31, 2022.
ParaRev will not review chargemasters loaded into the PDEolder than 12 months For this reason, it is important that clients check to ensure that a recent copy of the chargemaster has been supplied to ParaRev for use in the year-end update.
ParaRev will produce Excel spreadsheets of each CDM line item, as well as our recommendation for alternate codes, in three waves as information is released from the following sources:
- The American Medical Association?s publication of new, changed, and deleted CPT® codes; this information is released in Sept em ber of each year ParaRev will produce the first spreadsheet of CPT® updates for client review in Oct ober 2022

- Following the release of Medicare?s 2023 OPPSFinal Rule, typically in early Novem ber; ParaRev will perform analysis and produce the second spreadsheet to include both the CPT® information previously supplied, as well as alpha-numeric HCPCSupdates (J-codes, G-codes, C-codes, etc ) from the Final Rule Clients may expect this spreadsheet to be available in Novem ber 2022
- Following the publication of Medicare?s 2023 Clinical Lab Fee Schedule (CLFS) ? typically published in late Novem ber, ParaRev will prepare a final spreadsheet to be available in Decem ber 2022 This final spreadsheet ensures that ParaRev shares any late-breaking news or coding information, although we expect the December spreadsheet to be very similar to the November edition.
Clients will be notified by email as spreadsheets are produced and recorded on the PARA Dat a Edit or ?Admin?tab, under the ?Docs?subtab. When the code maps are ready, the 2023 spreadsheet will appear just as they did in 2022:
In addition, ParaRev consultants will publish concise papers on coding update topics in order to ensure that topical information is available in a manner that is organized and easy to understand ParaRev clients may rest assured that they will have full support for year-end HCPCScoding updates to the chargemaster
25 PARA Weekly eJournal: January 18, 2023

26 PARA Weekly eJournal: January 18 2023 MLN CONNECTS PARA invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF! Thursday, January 12, 2023 New s - Key Dates for First Year of Inflation Reduction Act?s Medicare Drug Price Negotiation Program - Cognitive Assessment: CY2023 Updates - Care Compare: Telehealth Indicator for Doctors & Clinicians - Clinical Laboratory Fee Schedule: CY2023 Payment File - Clinical Laboratories: PAMA Reporting & Payment Reductions Delayed - Medicare Wellness Visits: Get Your Patients Off to a Healthy Start Claim s, Pricers, & Codes - Drugs & Biologicals in Single-Use Containers: Using JW & JZ Modifiers MLN Mat t ers®Art icles - Travel Allowance Fees for Specimen Collection: 2023 Updates - ESRD & Acute Kidney Injury Dialysis: CY2023 Updates ? Revised - Home Health Prospective Payment System: CY2023 Update ? Revised - National Coverage Determination 110.24: Chimeric Antigen Receptor T-cell Therapy ? Revised

27 PARA Weekly eJournal: January 18, 2023 Therew ereTHREEnew or revised Transmittalsreleased thisw eek. To go to thefull Transmittal document simply click on thescreen shot or thelink. 3 t r ans mit
t al s
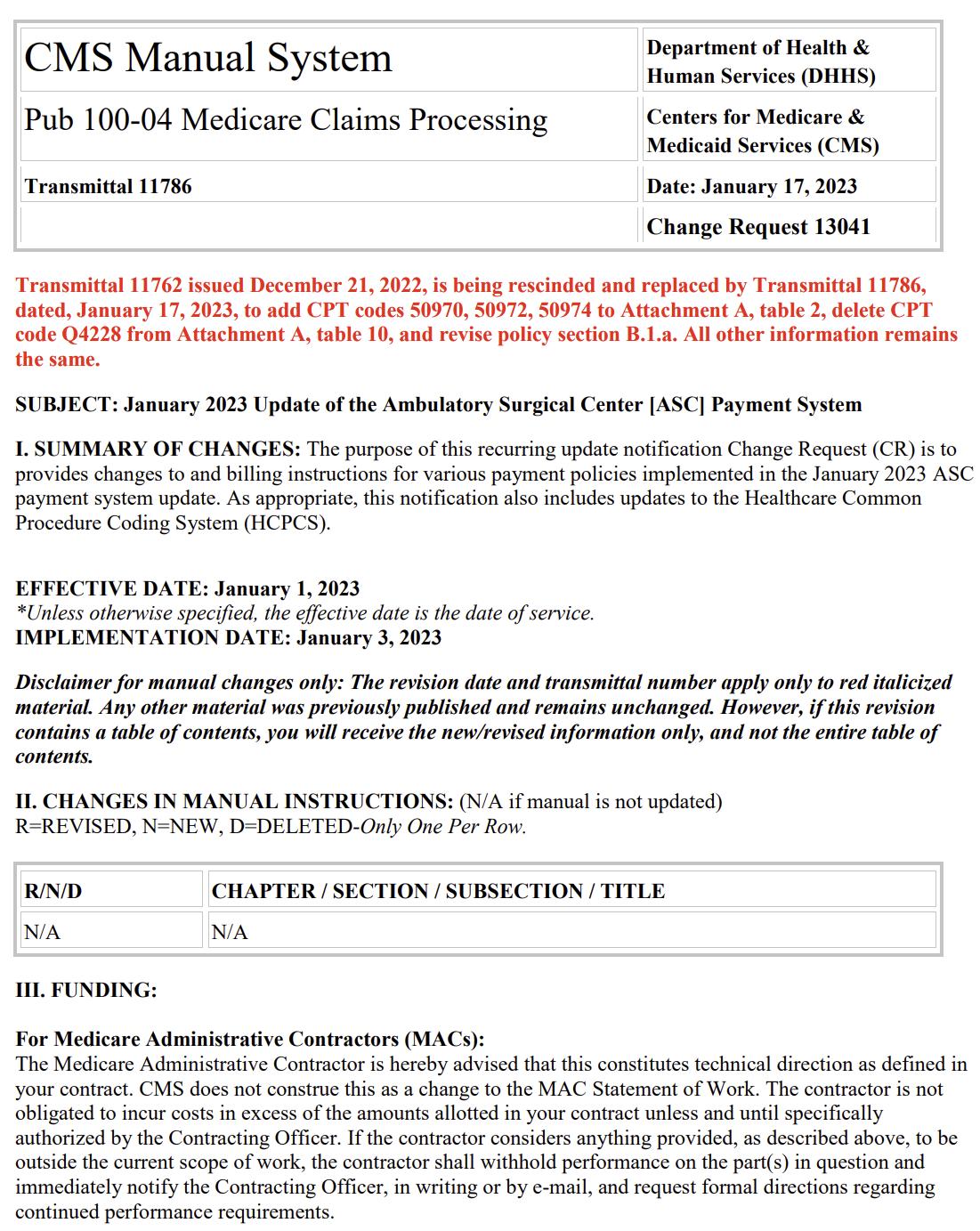
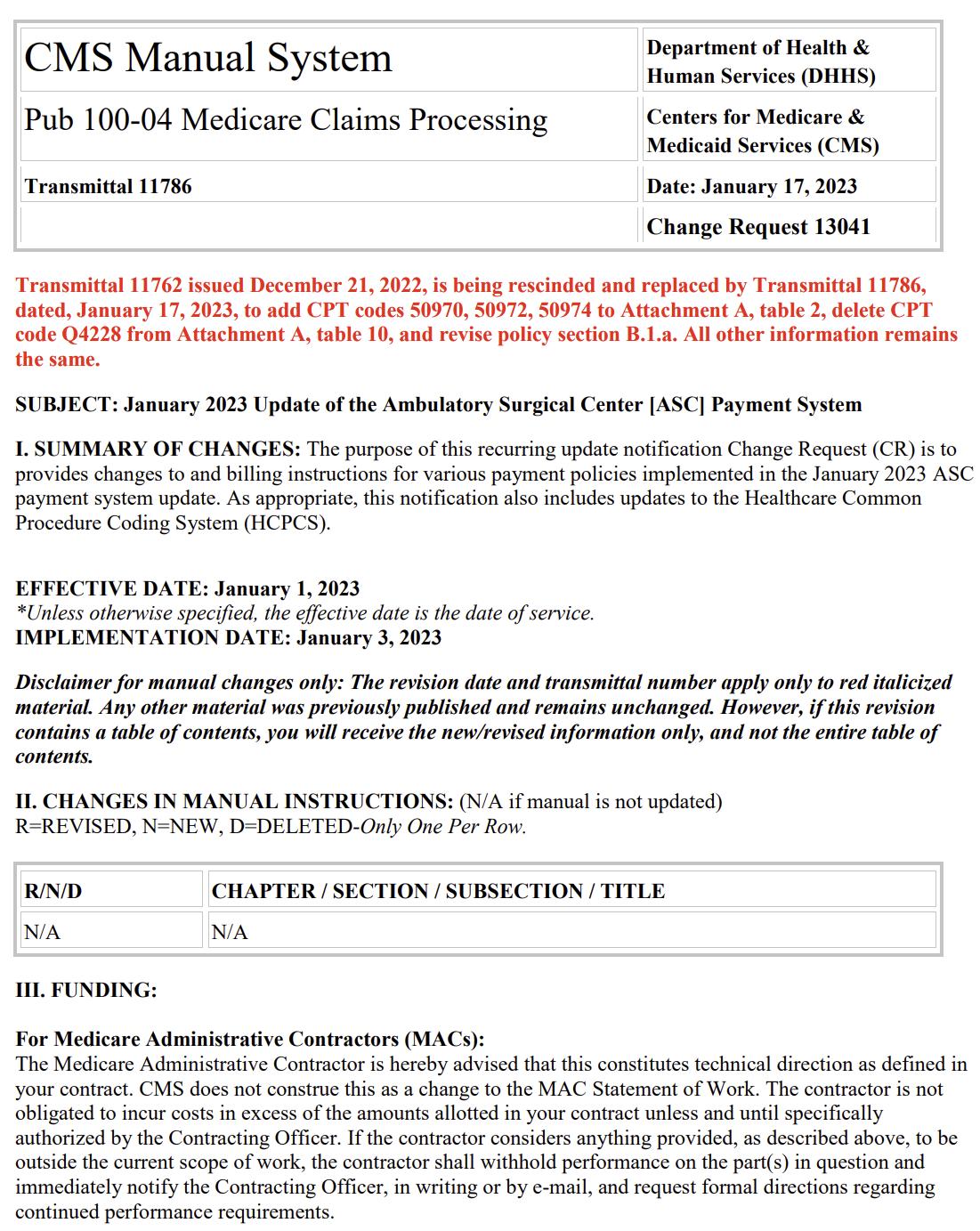
28 PARA Weekly eJournal: January 18 2023 TRANSMITTAL R11786CP

29 PARA Weekly eJournal: January 18, 2023 TRANSMITTAL R11781CP

30 PARA Weekly eJournal: January 18 2023 1 m edl ear ns Therew ereONEnew or revised MedLearnsreleased thisw eek. To go to thefull Transmittal document simply click on thescreen shot or thelink.


31 PARA Weekly eJournal: January 18, 2023 MEDLEARN MM13041