1 march1,2023
our nal e Telehealth Changes A CorroHealth Company Fluoroscopy In TheHospital Increased Flexibility A Detailed CodingGuide
j
DMEPRODUCTCODINGRESOURCES
Many hospitals struggle with understanding what Durable Medical Equipment (DME) can be billed to Medicare without enrollment as a Medicare DME Supplier. This paper informs clients how to use the PARA Data Editor to assist in identifying DMEitems which may be reported on a facility fee claim and reimbursed by Medicare, even though the hospital is not otherwise enrolled as a DMEsupplier In addition, it informs users how to use Medicare?s helpful product HCPCScoding lookup tools provided on the internet by Medicare Pricing, Data Analysis, and Coding contractor (PDAC), Palmetto GBA.

To identify DMEthat hospitals may bill without enrollment as a DMEsupplier, PARA Dat a Edit or users should navigate to the ?Filters?tab and run the DMEOPPSExempt Audit The PDFreport generated will identify all billable DMEitems by HCPCSand description, and will indicate whether there is an established line item within the hospital chargemaster coded with each of the billable HCPCS.
To run the audit report, go to the ?filters?tab of the PARA Data Editor and use the dropdown under ?Audit?; select the audit named ?DMEOPPSExempt?, and then click ?Create PDF?:

2 PARA Weekly eJournal: March 1, 2023
The report generated will list hundreds of billable DMEHCPCScodes, including wrist and knee braces, air splints, and cervical collars. Since the report is typically over 40 pages long, users may wish to use the ?find?function to locate the code descriptions which may contain a keyword, such as ?knee.?

Here?s an example of a report ? note that for HCPCScodes which have an established chargemaster line item, the procedure item detail, utilization statistics, and pricing is provided below the HCPCSdescription under the broken line:

Verify the Correct HCPCSAssignment: Medicare?s DMEPricing, Data, and Coding contractor, Palmetto, offers a product lookup feature to assist providers in correctly coding prefabricated DMEitems Users may search by either HCPCS, manufacturer, product model number, or by DMEclassification.

The ?Product Classification List?feature allows the user to enter a value in one or more of the data points available ? for example, we entered ?Medline?as the manufacturer and ?Wrist Splint? in the Product Name fields:
https://www4 palmettogba com/pdac dmecs/
3 PARA Weekly eJournal: March 1, 2023
DMEPRODUCTCODINGRESOURCES
DMEPRODUCTCODINGRESOURCES
The report returns a list of products with model numbers and the appropriate HCPCScode to report that item:


ParaRevenue offers a concise guideline to assist facilities in charging for DMEwithin the following paper:
https://apps.parahcfs.com/pde/documents/DMEPOS Billable by an OPPS Hospital April 2016 edited.pdf

4 PARA Weekly eJournal: March 1, 2023
FLUOROSCOPY IN THEHOSPITAL SETTING
Int roduct ion
Fluoroscopic imaging guidance is an integral component of many surgical and interventional procedures in the hospital setting. Imaging guidance provides real-time visualization of anatomical structures and can aid in the accurate placement of devices, reduce complications, and improve patient outcomes However, it is essential that the coding and reporting of fluoroscopy comply with Medicare guidelines to avoid potential errors and financial penalties
Medicare, the largest payer of healthcare services in the United States, has specific guidelines that govern coding and billing for both fluoroscopic and ultrasound imaging guidance The use of these modalities in conjunction with surgical and interventional procedures requires careful attention to ensure compliance with Medicare's rules and regulations.
It is important to note that fluoroscopic guidance (specifically CPT® 76000) is inclusive to many surgical and interventional procedures, as discussed below Some code pairs will have specific National Correct Coding Initiative (NCCI) PTPedits (as shown below) and some may not, but the National Correct CodingInitiative(NCCI) PolicyManual nonetheless prohibits fluoroscopy from being reported in conjunction with certain types of procedures

PARA Dat a Edit or users can review PTPNCCI edits on the Calculator tab:


5 PARA Weekly eJournal: March 1, 2023
FLUOROSCOPY IN THEHOSPITAL SETTING
Fluoroscopic Guidance
Fluoroscopy is a type of imaging that uses x-raysto provide real-time visualization of anatomicalstructures during a surgical or interventional procedure. Medicare has specific guidelines for coding and billing for procedures that use fluoroscopic guidance. The following are some of the nuances of correct and compliant coding for fluoroscopy in the hospital setting
Accurate and complete documentation is critical when billing for fluoroscopic guidance. The documentation should clearly indicate the type of procedure, the number of images taken (if applicable), the duration of the procedure, and the specific anatomical location of the images This information is essential to ensure that the service is accurately reported
Cent ral Venous Access
According to the NCCI Policy Manual, Chapter 1, insertion of central venous access devices frequently requires the use of fluoroscopic guidance: ?Since CPT® code 77001 describes fluoroscopic guidance for central venous access device procedures, CPT® codes for more general fluoroscopy (e g , 76000, 77002) shall not be reported separately (CPT® code 76001 was deleted January 1, 2019.)?
Endoscopic Procedures
Fluoroscopy is also considered integral to all endoscopic procedures, including (but not limited to) laparoscopy, hysteroscopy, thoracoscopy, arthroscopy, esophagoscopy, colonoscopy, other GI endoscopy, laryngoscopy, bronchoscopy, and cystourethroscopy & transurethral procedures It should not be reported separately with any endoscopic procedure. CPT® Assistant (September 2014) reiterates this advice. For example, CPT® code 76000 is not separately reportable with codes describing gastrointestinal endoscopy for foreign body removal (e g , 43194, 43215, 43247, 44390, 45332, 45379)
Laparoscopic Procedures
Fluoroscopy is considered inclusive to all laparoscopic procedures and should not be reported separately.
6 PARA Weekly eJournal: March 1, 2023
FLUOROSCOPY IN THEHOSPITAL SETTING
Art hroscopic Procedures
Likewise, CPT® 76000 is considered an integral component of arthroscopic procedures, when performed, and should not be reported separately with any arthroscopic procedure.
Spinal Procedures
Chapter 3 of the NCCI Policy Manual states, ?Fluoroscopy reported as CPT® code 76000 shall not be reported with spinal procedures, unless there is a specific CPT® Manual instruction indicating that it is separately reportable For some spinal procedures, there are specific radiologic guidance codes to report in lieu of these fluoroscopy codes.
For other spinal procedures, fluoroscopy is used in lieu of a more traditional intraoperative radiologic examination which is included in the operative procedure For other spinal procedure codes, fluoroscopy is integral to the procedure.? The May 2016 issue of CPT® Assistant reiterates this guidance.
For example, codes 62321, 62323, 62325, and 62327 represent injections of diagnostic or therapeutic substance(s) into the epidural or subarachnoid spaces at different spinal levels with either fluoroscopic or CTguidance Imaging guidance is included in these procedures and should not be reported separately
Cardiovascular Procedures
Fluoroscopic guidance is included in codes relating to cardiac catheterization and percutaneous coronary artery interventional procedures. Fluoroscopy is also not separately reportable with procedures related to pacemakers or intracardiac electrophysiology studies (represented by CPT® codes 33202-33275 and 93600- 93662, respectively) Fluoroscopy codes intended for other specific procedures may be reported separately when applicable. Additionally, ultrasound guidance is not separately reportable with these CPT® codes.
Internal cardioversion is performed using percutaneous vascular access and placement of one or more catheters into the heart under fluoroscopy. Fluoroscopic guidance is included and is not reported separately. Fluoroscopy codes (e.g., CPT® code 76000) are not separately reportable for endomyocardial biopsy
7 PARA Weekly eJournal: March 1, 2023
Codes Inclusive Of Radiologic/ Im aging Guidance
According to the NCCI Policy Manual, ?If the code descriptor for a HCPCS/CPT® code, CPT® Manual instruction for a code, or CMSinstruction for a code indicates that the procedure includes radiologic guidance, a provider/supplier shall not separately report a HCPCS/CPT® code for radiologic guidance including, but not limited to, fluoroscopy, ultrasound, computed tomography, or magnetic resonance imaging codes
If the physician performs an additional procedure on the same date of service for which a radiologic guidance or imaging code may be separately reported, the radiologic guidance or imaging code appropriate for that additional procedure may be reported separately with an NCCI PTP-associated modifier if appropriate.?
Diagnost ic and Int ervent ional Radiologic Procedures

Fluoroscopy is included in most radiological supervision and interpretation (RS&I) procedures Unless otherwise stated, NCCI policy states ?fluoroscopy necessary to complete a radiologic procedure and obtain the necessary permanent radiographic record is included in the radiologic procedure and shall not be reported separately.?Fluoroscopic guidance is considered integral to diagnostic and therapeutic intravascular procedures and is not separately reportable
Both CPT® and NCCI instruct that diagnostic angiography (arteriogram/venogram) performed on the same date of service by the same provider/supplier as a vascular interventional procedure should be reported with either modifier 59 or XU If a diagnostic angiography has already been performed before a percutaneous intravascular interventional procedure, then a second angiogram cannot be reported unless it is medically necessary to further examine the anatomy and pathology
If a repeat angiogram is required, it should be reported with a modifier 59 or XU However, if only a portion of the angiogram needs to be repeated, then a modifier 52 should also be appended to the angiogram CPT® code along with modifier 59 or XU It is important to note that if a complete diagnostic angiogram has already previously been performed, then a second angiogram should not be reported for the contrast injections necessary for the percutaneous intravascular interventional procedure, except in certain specific circumstances.
8 PARA Weekly eJournal: March 1, 2023
FLUOROSCOPY IN THEHOSPITAL SETTING
FLUOROSCOPY IN THEHOSPITAL SETTING
Chapter 9 of the NCCI Policy Manual states, ?Providers/suppliers shall not report radiologic supervision and interpretation codes, radiologic guidance codes, or other radiology codes where the radiologic procedure isintegral to another procedure being performed at the same patient encounter. PTPedits that bundle these radiologic codes into the relevant procedure codes have modifier indicators of ?1?allowing use of NCCI PTP-associated modifiers to bypass them An NCCI PTP-associated modifier may be used to bypass such an edit if and only if the radiologic procedure is performed for a purpose unrelated to the procedure to which it is integral.?
Fluoroscopic and Spot Im ages in The Hospit al Set t ing
If a procedure code does not include fluoroscopy (either in its description or by NCCI edits), either the radiology department or the operating room (but not both) may report it separately Fluoroscopy code 76000 has a status indicator of Sunder OPPS, which means it is separately payable and not subject to multiple procedure discounts.
Many radiology departments report a charge for fluoroscopy as means to track the use of radiology resources in the operating room or surgical suite. However, this may result in account errors or denials if there is a conflict between the fluoroscopy code and other procedure codes reported on the same date of service. It is therefore recommended that the radiology department utilize a different method for tracking productivity relating to operating room services
When ?spot images?are taken fluoroscopically during a surgical procedure, the hospital should report a charge for these images using the appropriate CPT® code for a plain-film x-ray of the specific anatomic site being imaged If the same spot view is taken multiple times during an operative procedure, this does not equate to a multi-view study; the code for a single-view study should be reported when applicable. For example, three lateral images of the cervical spine taken during a spinal fusion surgery should be reported as a single-view exam (72020) as opposed to a three-view exam (72040)
Conclusion
Fluoroscopic imaging guidance is a vital component of many surgical and interventional procedures in the hospital setting. However, it is critical to ensure that the coding and billing for fluoroscopy complies with Medicare guidelines to avoid potential errors and financial penalties
Understanding the nuances of correct and compliant coding for both fluoroscopic imaging guidance can help ensure that healthcare providers are properly reimbursed for their services and can continue to provide quality care to their patients.
9 PARA Weekly eJournal: March 1, 2023
OMNIBUSBILL EXTENDS PHETELEHEALTH FLEXIBILITIES

The Omnibus Appropriations Bill (H R 26 passed on December 23, 2022, extended Medicare coverage of telehealth service flexibilities that were permitted during the Public Health Emergency through December 31, 2024.

https://www.appropriations.senate.gov/imo/media/doc/JRQ121922.PDF

Before publishing the 2023 Medicare Telehealth Services file, CMSreviewed telehealth services added during the Public Health Emergency. For each service, CMS determined each would be extended through the remainder of 2023, or the providers would be required to stop providing the service through telehealth five months after the PHEends
The Omnibus bill includes health provisions that extend those telehealth services through the end of the year 2024.
10 PARA Weekly eJournal: March 1, 2023
Included in Sec. 4113 of the Omnibus ? Advancing telehealth Beyond COVID-19, the 151-day period was replaced with the period beginning on the first day after the end of the PHEand ending on December 31, 2024
Extended Flexibilities include:
- The expansion of the telehealth originating site to include any site the patient is located, including the patient?s home, is extended through 2024
- The expansion of eligible practitioners who can furnish telehealth (including occupational therapists, physical therapists, speech-language pathologists and audiologists) will continue through 2024
- Rural health clinics (RHCs) and federally qualified health centers (FQHCs) may continue to furnish telehealth services through 2024
- The six-month in-person requirement for mental health services furnished through telehealth (including the in-person requirements for RHCs and FQHCs) is delayed until January 1, 2025

- Coverage and payment for telehealth furnished via audio-only during the PHEwill continue through 2024
- Telehealth to meet the face-to-face recertification requirement for hospice care is extended through 2024
11 PARA Weekly eJournal: March 1, 2023
EXTENDS PHETELEHEALTH
OMNIBUSBILL
FLEXIBILITIES
HHScontinues to evaluate the fate of other clinician ?flexibilities?, as discussed in the following publication dated 2/1/2023:
https://www cms gov/files/document/physicians-and-other-clinicians-cms-flexibilitiesfight-covid-19 pdf


12 PARA Weekly eJournal: March 1, 2023
OMNIBUSBILL EXTENDS PHETELEHEALTH FLEXIBILITIES
Providers, billers, and coders who contend with National Correct Coding Initiative (NCCI) edits will be interested to learn that Medicare has acted to end its contract with the NCCI edit vendor, Capitol Bridge LLC, one year earlier than the performance period allowed in the original contract award.


In February, 2019, CMSawarded the contract for maintaining Correct Coding Inititiative edits, including Procedure-to-procedure (PTP) and Medically Unlikely Edits (MUE) to a small and disadvantaged business, Capitol Bridge, LLCThe contract was awarded for 60 months: https://www.fedhealthit.com/2019/02/cms-awards-15m-national-correct-coding-initiative/
In theory, the contract performance period could have continued until February of 2024; however, an automated reply to an email sent to the NCCI contractor?s contact address at NCCIPTPMUE@cms hhs gov informs the recipient that the contract ended on February 2, 2023:

13 PARA Weekly eJournal: March 1, 2023
MEDICARECCI EDITCONTRACTENDED
MEDICARECCI EDITCONTRACTENDED
The HHScontract with Capitol Bridge, worth approximately $14.7 million dollars, is described on the Federal Procurement Data website as follows:
?National Correct Coding Initiative (NCCI): Promote program integrity and compliance through guidance, edits, and other methodologies that promote the consistent administration of CMS payment policies.?
The last entry regarding the contract on the Federal Procurement Data System website indicates that on October 17, 2022, the reason the contract was modified was ?Other Administrative Action ?

https://www fpds gov/common/jsp/LaunchWebPage jsp?command=execute&requestid= 152090237&version=1 5

14 PARA Weekly eJournal: March 1, 2023
MEDICARECCI EDITCONTRACTENDED
Edits introduced by Capitol Bridge were sometimes inaccurate and disruptive.For example, in 2020, Capitol Bridge introduced several PTPedits that prevented hospitals and other providers from reporting together common and customary code pairs, such as:
-Nuclear medicine tests billed together with a radiopharmaceutical, (i e 78306 with A9503)

-Barium swallow testing (92611 with 74230);
-And PT/OT evaluations (97161-97163 and 97165-97168) billed on the same DOSas therapeutic activities (97530)
The edits were relaxed after an influx of complaints from providers and provider associations.

15 PARA Weekly eJournal: March 1, 2023
Join

Watch

16 PARA Weekly eJournal: March 1, 2023
's your opport unit y t o learn even m ore about t he No Surprises Act (NSA)!
Now
the hundreds of your colleagues who have walked away feeling more informed, more confident and ready to take action.
THEUPDATED NO SURPRISES ACTWEBINAR: MORETO KNOW!
this important webinar by clicking the " What Is NSA?" screen shot below.
REMOVAL OFNCD AND EXPANSION OFCOLORECTAL CANCERSCREENING
CMShas changed CMShas removed NCD and has expanded the coverage of colorectal cancer screening.

CMShas reduced the minimum age for coverage for the following CRCscreening tests (HCPCScodes G0104, G0106, G0120, G0327, G0328, 81528, and 82270) from 50 years to 45 years of age or older:
- Screening Flexible Sigmoidoscopy Test
- Screening Guaiac-based Fecal Occult Blood Test (gFOBT)
- Screening Immunoassay-based Fecal Occult Blood Test (iFOBT)
- Screening The Cologuard? ? Multi-target Stool DNA (sDNA) Test
- Screening Barium Enema Test - Screening Blood-based Biomarker Tests
A positive result from a non-invasive stool-based CRCscreening test no longer requires that the following colonoscopy be a diagnostic colonoscopy. CRCscreening tests now include a follow-on screening colonoscopy after a Medicare-covered, non-invasive, stool-based CRCscreening test returns a positive result
Screening colonoscopy continues to not have a minimum age limitation
Patient cost sharing won? t apply to the non-invasive, stool-based test and the follow-on screening colonoscopy in this scenario, because both are specified preventive screening services. The frequency limitations for screening colonoscopies in 42 CFR410.37(g) won? t apply to the follow-on screening colonoscopy that follows a positive result from a stool-based test
Attach the KXmodifier to a screening colonoscopy code to indicate such service was performed as a follow-on screening after a positive result from a stool-based test Our policy goal of not having frequency limitations to the follow-on screening colonoscopy after a non-invasive stool-based test returns a positive result is to remove barriers and encourage the patient to proceed to the colonoscopy procedure soon after the positive result from the stool-based test.
In Sum m ary: CMS has:
- Removed NCD 160 22 ? ambulatory electroencephalographic (EEG) monitoring
- Lowered the minimum age for colorectal cancer screening (CRC) from age 50 to 45 for certain tests
- Expanded the definition of CRCscreening tests and new billing instructions for colonoscopies under certain scenarios
- Updated three Medicare manuals
17 PARA Weekly eJournal: March 1, 2023
PARA invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

Thursday, February 23, 2023
New s
-
Hospital Price Transparency: Progress & Commitment to Achieving Its Potential
- Home Infusion Therapy Services Monitoring Report
- Immunosuppressive Drugs: Comparative Billing Report in February
- Expanded Home Health Value-Based Purchasing Model Resources: Submit Feedback through March 31
Claim s, Pricers, & Codes
- HCPCSLevel II Coding: FAQs for Single Source Drugs & Biologicals
- National Correct Coding Initiative: No April Update
Publicat ions
- DMEPOSQuality Standards ? Revised
18 PARA Weekly eJournal: March 1, 2023 MLN CONNECTS
PARA invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

Monday, February 27, 2023
New s
COVID-19 Public Health Emergency (PHE) New Overview Fact Sheet
As part of the Centers for Medicare & Medicaid Services?(CMS) ongoing efforts to provide up-to-date information to prepare for the end of the Public Health Emergency (PHE) for COVID-19, which is expected on May 11, 2023, we are providing a new overview fact sheet on CMSWaivers, Flexibilities, and the Transition Forward from the COVID-19 Public Health Emergency COVID-19 efforts have been a significant priority for the Biden-Harris Administration, and with the use of whole-of-government approach, the country is in a better place.
Over the next several months, CMSwill work to ensure a smooth transition back to normal operations.
The CMS Waivers, Flexibilit ies, and t he Transit ion Forw ard from t he COVID-19 Public Healt h Em ergency provides clarit y on several t opics including:
- COVID-19 vaccines, testing, and treatments;
- Telehealth services;
- Health Care Access
- In the coming weeks, CMSwill be hosting stakeholder calls and office hours to provide additional information. Please visit the CMSEmergencies Page for continuous updates regarding PHEsunsetting guidance as information becomes available to the public.
19 PARA Weekly eJournal: March 1, 2023 MLN CONNECTS
t r ans mit t al s
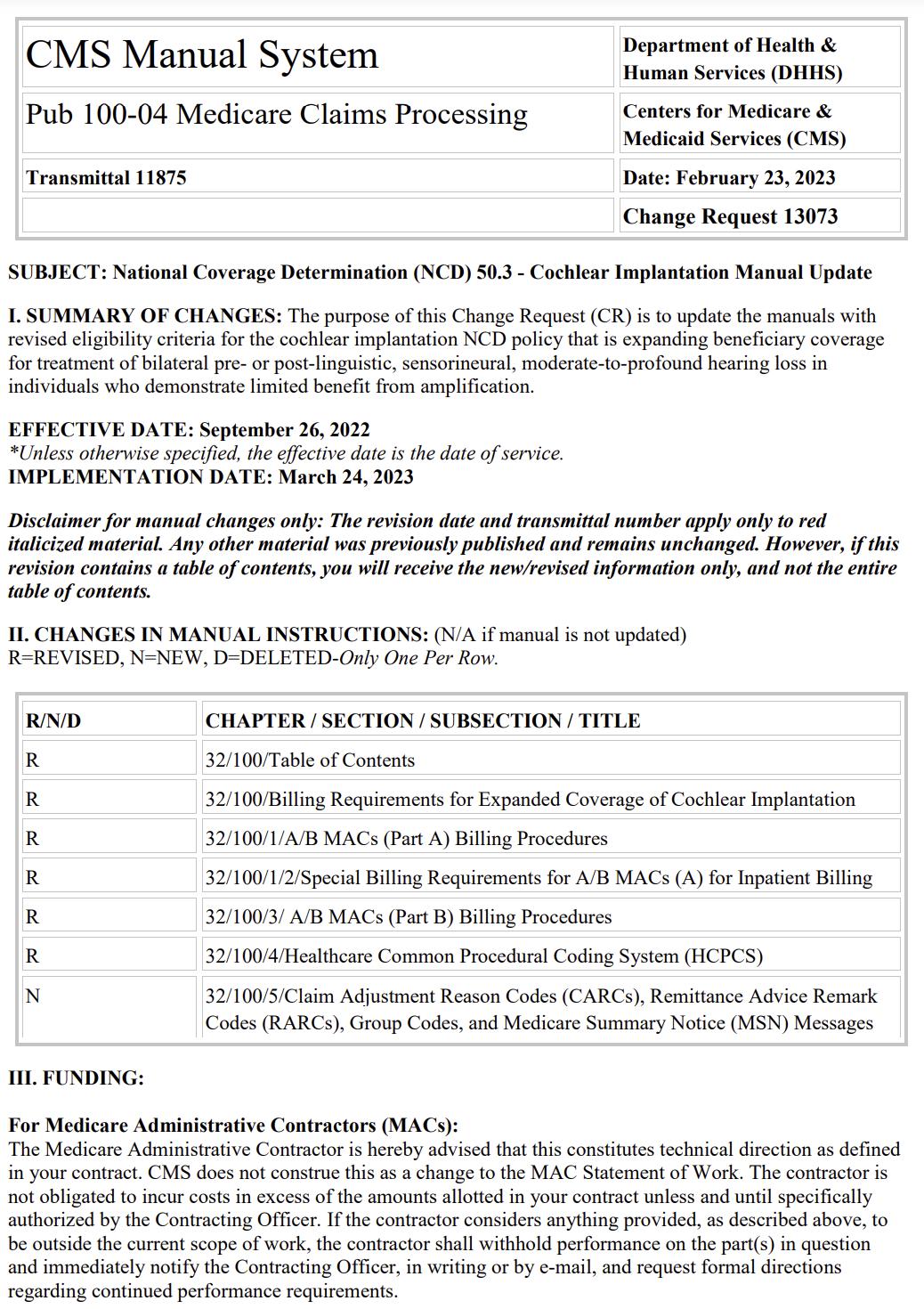
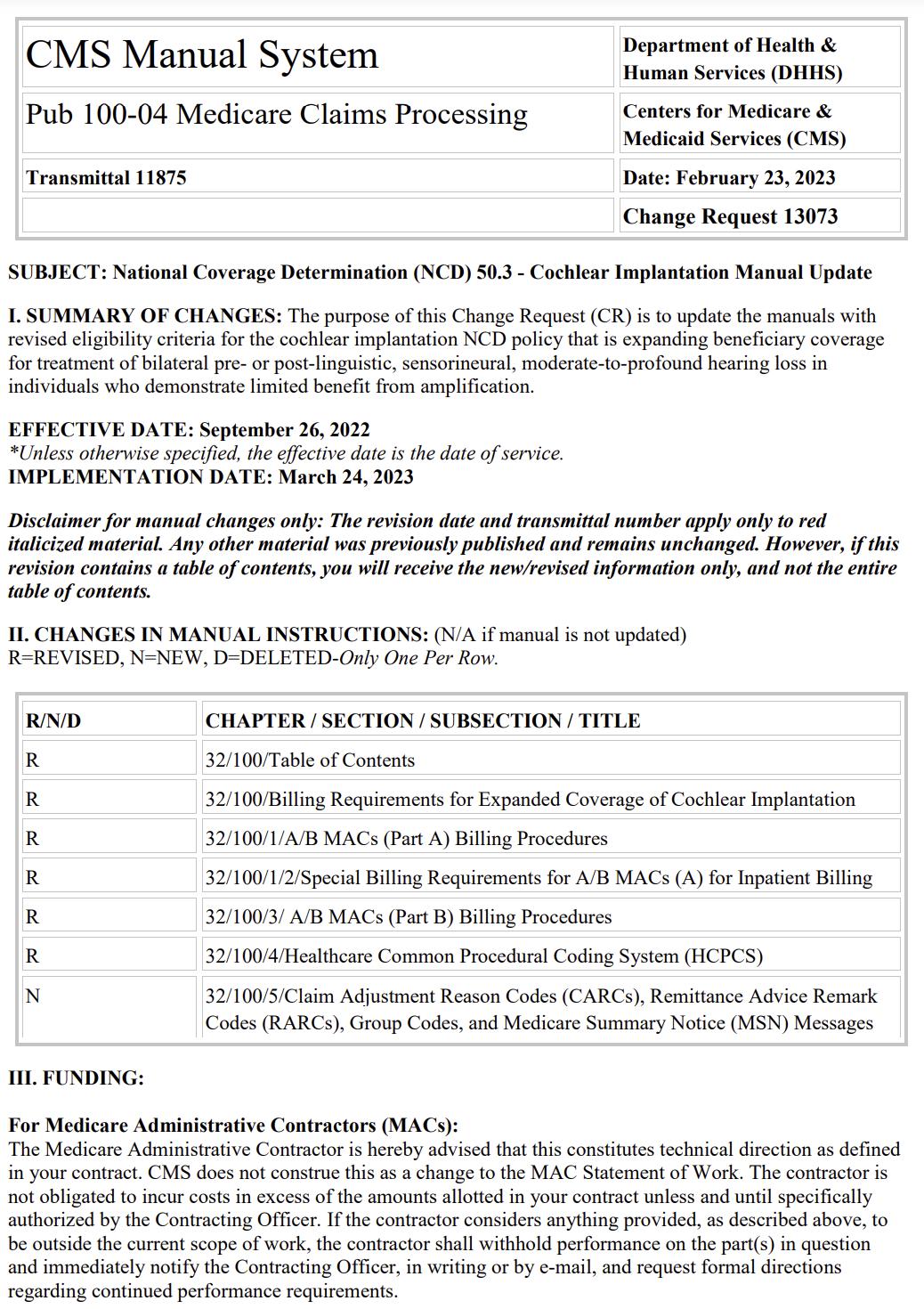
Therew ereNINEnew or revised Transmittalsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.

20 PARA Weekly eJournal: March 1, 2023
9
TRANSMITTAL R8P242I

21 PARA Weekly eJournal: March 1, 2023
TRANSMITTAL R11879OTN

22 PARA Weekly eJournal: March 1, 2023
TRANSMITTAL R11878OTN

23 PARA Weekly eJournal: March 1, 2023
TRANSMITTAL R11875CP
24 PARA Weekly eJournal: March 1, 2023
TRANSMITTAL R11875NCD

25 PARA Weekly eJournal: March 1, 2023
TRANSMITTAL R11871CP

26 PARA Weekly eJournal: March 1, 2023

27 PARA Weekly eJournal: March 1, 2023
TRANSMITTAL R11870COM
TRANSMITTAL R11869OTN

28 PARA Weekly eJournal: March 1, 2023
TRANSMITTAL R11874MSP

29 PARA Weekly eJournal: March 1, 2023
1 m edl ear ns
Therew asONEnew or revised MedLearnsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.

30 PARA Weekly eJournal: March 1, 2023


31 PARA Weekly eJournal: March 1, 2023 MEDLEARN MM13013
Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to the best of ParaRev?s knowledgeisaccurate at thetime of distribution. However, dueto theever changing legal/regulatorylandscapethisinformation issubject to modification, asstatutes/laws/regulationsor other updatesbecomeavailable.
Nothingherein constitutes, isintended to constitute, or should berelied on as, legal advice ParaRev expressly disclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anythingcontained in thematerials, which areprovided on an ?as-is?basisand should beindependentlyverified beforebeing applied.
You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability.Theinformation in this document isconfidential and proprietaryto ParaRev and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduce or transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording and broadcasting, or byanyinformation storageand retrieval system must be obtained in writingfrom ParaRev. Request for permission should be directed to sales@pararevenue.com.
ParaRev is excited to announce we have joined industry leader CorroHealt h to enhance the reach of our offerings! ParaRev services lines are additive in nature strengthening CorroHealt h?s impact to clients?revenue cycle. In addition, you now have access to a robust set of mid-cycle tools and solutions from CorroHealt h that complement ParaRev offerings


In terms of the impact you?ll see, there will be no change to the management or services we provide The shared passion, philosophy and cultures of our organizations makes this exciting news for our team and you, our clients

While you can review the CorroHealt h site HERE, we can coordinate a deeper dive into any of these solutions Simply let us know and we?ll set up a meeting to connect.
As always, we are available to answer any questions you may have regarding this news We thank you for your continued partnership
32 PARA Weekly eJournal: March 1, 2023
FORYOURINFORMATION