

1 SEPTEMBER28, 2022 j our nale LVAD Surgery A CorroHealth Company Handling DenialsAs "Not Medically Necessary" October Update OPPS Payable Drugs Reimbursement
A. Yes, it is still important to report the CSmodifier on outpatient claims when appropriate. The CSmodifier will ensure the payor covers in full, without patient liability, evaluation and management charges on an outpatient visit when the provider orders a COVID test This exceptional coverage is in effect for the duration of the Public Health Emergency. The CSmodifier should be reported when appropriate not just to Medicare outpatient claims, but commercial health insurer claims as well
The Public Health Emergency is still in effect; the Secretary of Health and Human Services makes a determination every 90 days as to whether to continue it. The next extension is expected in mid October, which we expect to continue the PHEinto the first quarter of 2023 CMShas assured state Medicaid agencies that it will give a 60 day advance notice of the date on which the PHEwill end, and no such notice has yet been provided.
Here?s an excerpt from Medicare?s FAQ for providers document explaining the CSmodifier: https://www

covid 19 faqs 508 pdf (page


Q. Is CSModifier relevant anymore?Does Medicare continue to waive the patient responsibility outside of the Health Emergency designation?
2 PARA Weekly eJournal: September 28, 2022
cms gov/files/document/03092020
83) CSMODIFIER
CSMODIFIER
27. Quest ion: How should the CSmodifier, which removes application of beneficiary cost sharing (deductible and co payment), be applied to telehealth services and/or E/M visits?
Answ er: The CSmodifier should be applied for certain evaluation and management services related to COVID 19 testing, whether they are furnished in person or via telehealth These services are medical visits under the HCPCSevaluation and management categories described below when outpatient providers, physicians, or other providers and suppliers who bill Medicare for Part B services orders or administers a COVID-19 lab test, regardless of the HCPCScodes they use to report the test Cost sharing does not apply for COVID 19 testing related services, which are medical visits that: are furnished between March 18, 2020, and the end of the PHE; result in an order for or administration of a COVID 19 test; are related to furnishing or administering such a test or to the evaluation of an individual for purposes of determining the need for such a test; and are in any of the following categories of HCPCSevaluation and management codes:
Office and other outpatient services
Hospital observation services
- Emergency department services
Nursing facility services
Domiciliary, rest home, or custodial care services
Home services
Online digital evaluation and management services
Cost sharing does not apply to the above medical visit services for which payment is made to:
Hospital Outpatient Departments paid under the Outpatient Prospective Payment System
Physicians and other professionals under the Physician Fee Schedule
Critical Access Hospitals (CAHs)
Rural Health Clinics (RHCs)
- Federally Qualified Health Centers (FQHCs)
For services furnished on or after March 18, 2020, and through the end of the PHE, outpatient providers, physicians, and other providers and suppliers that bill Medicare for Part B services under these payment systems should use the CSmodifier on applicable claim lines to identify the service as subject to the cost-sharing waiver for COVID-19 testing-related services and should NOT charge Medicare patients any co insurance and/or deductible amounts for those services
Additionally, the CPT® telehealth modifier, modifier 95, should be applied to claim lines that describe services furnished via telehealth. And the billing practitioner should report the POScode that reflects the place the service would have been furnished if furnished in person.
3 PARA Weekly eJournal: September 28, 2022
Q.We are trying to bill Medicare for a device dependent outpatient procedure without a device HCPCScode, which causes the claim to reject (RTP) due to edit 92 (Device intensive procedure reported without a device code)

No ?device?was necessary to successfully perform the procedure in this case The surgical procedure on the claim is CPT® 28298 (CORRECTION, HALLUXVALGUS(BUNIONECTOMY), WITH SESAMOIDECTOMY, WHEN PERFORMED; WITH PROXIMAL PHALANXOSTEOTOMY, ANY METHOD)
The surgeon performed the procedure successfully using only K Wires; no other implant was necessary Normally we do not charge separately for K Wires, however, in this instance, a device HCPCScode is required by Medicare edit 92. Can we use HCPCSC1713 for the K-Wires? (Other options that I have seen are using HCPCSC1889 or using the modifier CG )
A.K wire meets the description of a bone to bone or bone to soft tissue anchoring device. While your facility may not typically charge for K wire, many other hospitals charge for it using HCPCSC1713
We find no requirement within the Medicare Claims Processing Manual which obligates facilities to report cost savings when a device dependent procedure was accomplished by the surgeon using full-price, yet relatively inexpensive surgical implant supplies ? such as K-wire.
In the interest of providing a thorough response, here is more information on billing device dependent procedures Medicare?s Integrated Outpatient Code Editor applies Edit 92 to claims reporting a device dependent procedure on which no device code is reported on the same claim.
The edit applies to only certain HCPCSlisted in Addendum P(Device Intensive Procedures) of the OPPSFinal Rule. The list of procedures which are subject to Edit 92, and which are eligible for an edit bypass (using modifier CG) is found in the Integrated Outpatient Code Editor (IOCE) DATA HCPCSfile. (See next page).
4 PARA Weekly eJournal: September 28, 2022
HCPCSFORDEVICEDEPENDENTPROCEDURE(K WIREONLY)
Manufact urer Credit ? Sometimes an implanted device is obtained at a very low cost because it is supplied under a manufacturer?s warranty, recall, or provided as a free sample. Hospitals which report a device that was obtained at a significantly reduced cost must report Value Code FD (?Item Provided Without Cost to Provider, Supplier or Practitioner, or Credit Received for Replacement Device (Examples, but not limited to: Covered Under Warranty, Replaced Due to Defect, Free Samples)?) on the claim.
In addition, the claim must report one of the following three condition codes to characterize the nature of the savings:


 Both Addendum Pand the IOCEData HCPCSfile are available on the PARA Dat a Edit or Advisor tab:
Both Addendum Pand the IOCEData HCPCSfile are available on the PARA Dat a Edit or Advisor tab:
5 PARA Weekly eJournal: September 28, 2022
HCPCSFORDEVICEDEPENDENTPROCEDURE(K WIREONLY)
When value code FD is reported, along with one of those three condition codes, Medicare will reduce the provider?s APCpayment to correspond with the facility?s lower expense on the cost of the device. If a device HCPCSis reported, and no savings are indicated on the claim, Medicare processes the claim at full OPPSreimbursement rates.

Some Hospital claims with implant charges have been audited by the OIG to check whether free implants were reported accurately. The OIG found that providers failed to report savings on certain cardiac devices, and it reminded MACs to police this requirement Here?s a link to that OIG report:
Hospitals Did Not Comply With Medicare Requirements for Reporting Cardiac Device Credits

6 PARA Weekly eJournal: September 28, 2022
A 01 18 00502 11 16 2020 (hhs gov) HCPCSFORDEVICEDEPENDENTPROCEDURE(K WIREONLY)
The device offset for HCPCS28298 is $1,954 94, per Addendum P(Device dependent procedures list) of Medicare?s 2022 OPPSFinal Rule:
Modifier CG?Some device-dependent HCPCScan be performed with or without a device.For example, CPT® 28415 (OPEN TREATMENTOFCALCANEAL FRACTURE, INCLUDESINTERNAL FIXATION, WHEN PERFORMED) ? includes the words ?? when performed ?If no device was required because internal fixation was not performed, Medicare instructs the facility to append modifier CG (Policy criteria applied) to bypass Edit 92.
Here?s an excerpt from the Medicare Claims Processing Manual which explains this bypass: https://www.cms.gov/Regulations and Guidance/Guidance/Manuals/Downloads/clm104c04.pdf
61.2.1 ? Bypass Edit Modifier ?CG? for Claim s on Which Specified Procedures are t o be Report ed Wit h Device Codes
(Rev.4513, Issued: 02-04-2020, Effective: 01-01- 2020, Implementation: 01-06-2020)
For certain device-intensive procedures, providers may bypass the device edit requiring at least one device HCPCScode for the procedure For situations where no device was performed with certain device intensive procedures, providers may bypass the edit by reporting modifier ?CG?
Unfortunately, not all device dependent HCPCSare candidates for modifier CG Those which are eligible for modifier CG are identified in column DCof the 2022 IOCEfile HCPCS Data file:

The comment associated with column DCis as follows:

7 PARA Weekly eJournal: September 28, 2022
HCPCSFORDEVICEDEPENDENTPROCEDURE(K WIREONLY)
HCPCSFORDEVICEDEPENDENTPROCEDURE(K
Turning now to the other possible device HCPCScodes ? in general, determining the correct C-code to report on a device-intensive procedure can be a problem because HCPCScodes descriptions are sometimes vague, and not all implantable items are assigned to a specific HCPCS.


The PARA Dat a Edit or offers an ?APCClaim Analysis Report?on the Pricing Data tab. This report providers statistical analysis of coding practices on outpatient claims submitted to Medicare by hospitals nationwide The report for CPT® 28298 indicates that 94 8%of the 1,106 claims submitted between 1/1/2021 and 9/30/2021 reported implant code C1713 (Anchor/Screw for opposing bone-to-bone or soft tissue-to-bone.)The other two codes reported were C1679 (Guide Wire) and C1776 (Joint Device):
To evaluate these HCPCScodes, we consulted the most recent edition of Medicare?s ?List of Device Category Codes for Present or Previous Pass Through Payment and Related Definitions ?Within this document, Medicare offers ?Explanations of the Terms/Definitions Related to Pass Through Device Category Codes ?
https://www.hhs.gov/guidance/sites/default/files/hhs guidance documents/Complete list DeviceCats OPPS 7 1 2020 pdf

8 PARA Weekly eJournal: September 28, 2022
WIREONLY)
Here are our thoughts on each of those codes, as well as C1889: C1713 (Anchor/ screw for opposing bone-t o-bone or sort t issue t o bone (Im plant able))? is arguably the best option The difference between a pin and a wire is largely one of diameter A K wire (Kirschner wire) is a thin metallic wire or pin that can be used to stabilize bone Using that understanding as a basis for our evaluation, we allow that K-wires could be reported as C1713 ? particularly because the wires are implanted to stabilize the bones which were modified during surgery Here?s the more expansive description of C1713 provided in the Medicare document:
?Anchor for opposing bone to bone or soft tissue to bone (C1713) Implantable pins and/or screws that are used to oppose soft tissue to bone, tendon to bone, or bone to bone. Screws oppose tissues via drilling as follows: soft tissue to bone, tendon to bone, or bone to bone fixation Pins are inserted or drilled into bone, principally with the intent to facilitate stabilization or oppose bone to bone.This may include orthopedic plates with accompanying washers and nuts.?
C1769 (Guide Wire)?Among the codes reported by other hospitals for the same outpatient procedure in 2021, C1769 (Guide Wire) appears to be a viable choice, because it describes a wire and the K wires serve to ?guide?the alignment of the bones as they heal The description for C1769 is two words only ? ?Guide Wire.? There is no further explanation of C1769 within the Medicare document to support or refute the propriety of this code However, we are more accustomed to seeing C1769 reported for items used in an interventional radiology procedure, not orthopedic/podiatric surgery.

C1889 (im plant able/ insert able device, not ot herw ise classified) could be reported to represent the K wires for this case; it would resolve the billing edit, although we prefer C1713 as a more specific code to describe a K wire There is no discussion in the CMS?Device? document on C1889.
C1776 (Joint device, im plant able)is not recommended because a K wire is not a joint device, in our opinion
9 PARA Weekly eJournal: September 28, 2022
HCPCSFORDEVICEDEPENDENTPROCEDURE(K WIREONLY)
Q.Our facility inpatient claim was denied by Medicare for a ventricular assist device surgery with the remit code ?CO 50 ? Not Medically Necessary ?We don? t understand why the claim was denied, because the MAC?s Local Coverage Article lists the ICD10 procedure ICD10 5A0221D (Assistance with Cardiac Output using Impeller Pump, Continuous) as covered when billed with the diagnosis ICD10 I25.110 (Atherosclerotic heart disease of native coronary artery with unstable angina pectoris). What gives?



A.The Local Coverage Article is providing only part of the requirements to meet medical necessity.CMSNational Coverage Determination 20.9.1 (Ventricular Assist Devices) provides a more expansive explanation of the medical necessity criteria, including the requirement that the facility has been approved as an LVAD (Left Ventricular Assist Device) facility: https://www.cms.gov/medicare coverage database/view/ncd.aspx?NCDId=360

10 PARA Weekly eJournal: September 28, 2022
LVAD SURGERY NOTMEDICALLY NECESSARY
LVAD SURGERY NOTMEDICALLY NECESSARY

? Facilities must be credentialed by an organization approved by CMS The process for organizations to apply for CMSapproval to be designated as a credentialing organization for LVAD facilities is posted on our web site along with a list of approved credentialing organizations, approved standard versions, and credentialed facilities: http://www.cms.gov/Medicare/Medicare-General-Information/MedicareApprovedFacilitie/ VAD Destination Therapy Facilities.html


Unfortunately, your facility is not listed on the approved list, which includes 195 facilities (many of which are academic medical centers) in the USwhich have been approved:
Consequently, the procedure does not meet Medicare coverage requirementsThe process to obtain approval as an LVAD facility is provided at https://www cms gov/Medicare/ Medicare-General-Information/ MedicareApprovedFacilitie/ Downloads/VAD credentialing 10302013 pdf:
11 PARA Weekly eJournal: September 28, 2022
Answ er: The in network facility should expect to receive the contracted rate for an ED visit The health plan is required to pay the OON ED provider the difference between the Out Of Network rate and the cost-sharing amount. The OON ED provider cannot balance bill the patient for anything over the copayment, coinsurance, or amounts paid toward a deductible. If the OON ED provider is not satisfied with the reimbursement from the plan, they are to negotiate a higher reimbursement with the plan. If they cannot agree upon an amount, then the IDRprocess is initiated to allow a third party to determine an acceptable reimbursement eCFR :: 45 CFR Part 149 -- Surprise Billing and Transparency Requirem ent s
The plan or issuer: (B) Pays a total plan or coverage payment directly to the nonparticipating provider or nonparticipating facility that is equal to the amount by which the out-of-network rate for the services exceeds the cost sharing amount for the services (as determined in accordance with paragraphs (b)(3)(ii) and (iii) of this section), less any initial payment amount made under paragraph (b)(3)(iv)(A) of this section. The total plan or coverage payment must be made in accordance with the timing requirement described in section 2799A-1(c)(6) of the PHSAct, or in cases where the out-of-network rate is determined under a specified State law or All Payer Model Agreement, such other timeframe as specified by the State law or All Payer Model Agreement

RARCN830 = Alert: The charge[s] for this service was processed in accordance with Federal/ State, Balance Billing/ No Surprise Billing regulations As such, any amount identified with OA, CO, or PI cannot be collected from the member and may be considered provider liability or be billable to a subsequent payer Any amount the provider collected over the identified PRamount must be refunded to the patient within applicable Federal/State timeframes. Payment amounts are eligible for dispute pursuant to any Federal/State documented appeal/grievance process(es). A list of RARCs related to the NSA can be found here: Rem it t ance Advice Rem ark Codes Relat ed t o t he No Surprises Act (cm s.gov)
 Quest ion: I have an ER visit w here w e are an in net w ork hospit al, but our ER provider w as out of net w ork We received an EOB w it h t he N830 RARC code, but it seem s w e got an out of net w ork paym ent for provider. Should I expect in net w ork paym ent , or a QPA am ount ? I am asking about t he out of net w ork provider t hat should be paid at in net w ork rat es correct ?
Quest ion: I have an ER visit w here w e are an in net w ork hospit al, but our ER provider w as out of net w ork We received an EOB w it h t he N830 RARC code, but it seem s w e got an out of net w ork paym ent for provider. Should I expect in net w ork paym ent , or a QPA am ount ? I am asking about t he out of net w ork provider t hat should be paid at in net w ork rat es correct ?
12 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACTQUESTIONSAND ANSWERS More
NO SURPRISES ACTQUESTIONSAND ANSWERS
Quest ion: If a plan is out of net w ork and t hey pay us an am ount t hat seem s t oo low , are t hey required t o t ell us t heir in-net w ork rat e?
Answ er: There are no provisions in the NSA that require a plan to reveal their in network rates
Quest ion: My NSA link requires a diagnosis code?
Answ er: A diagnosis code is one of the required data elements in an estimate eCFR :: 45 CFR Part 149 Subpart G -- Prot ect ion of Uninsured or Self-Pay Individuals
Content requirementsof a good faith estimate issued to an uninsured (or self-pay) individual.
(1) A good faith estimate issued to an uninsured (or self pay) individual must include:
(i) Patient name and date of birth;
(ii) Description of the primary item or service in clear and understandable language (and if applicable, the date the primary item or service is scheduled);
(iii) Itemized list of items or services, grouped by each provider or facility, reasonably expected to be furnished for the primary item or service, and items or services reasonably expected to be furnished in conjunction with the primary item or service, for that period of care including:
(A) Items or services reasonably expected to be furnished by the convening provider or convening facility for the period of care; and
(B) Items or services reasonably expected to be furnished by co providers or co facilities (as specified in paragraphs (b)(2) and (c)(2) of this section);
(iv) Applicable diagnosis codes, expected service codes, and expected charges associated with each listed item or service;.
Quest ion: Are w e required t o supply a GFE for our clinic services?
Answ er: A GFEis required for an uninsured individual who has services scheduled at least 3 days in advance. Generally, all providers and facilities that schedule items or services for an uninsured (or self pay) individual or receive a request for a GFEfrom an uninsured (or self pay) individual must provide such individual with a GFE No specific specialties, facility types, or sites of service are exempt from this requirement.
13 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACTQUESTIONSAND ANSWERS
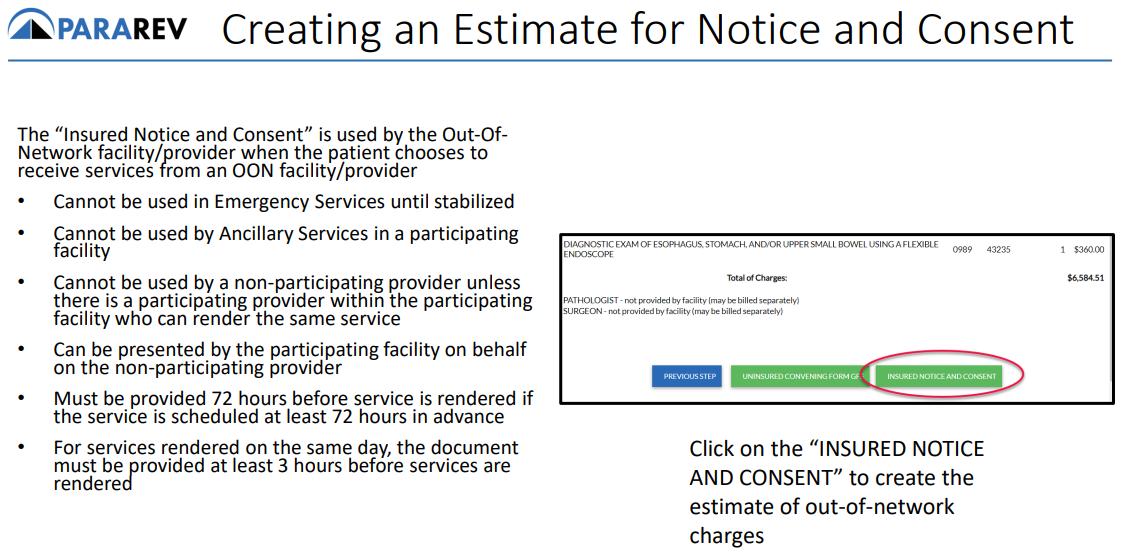
Quest ion: Do you have any inform at ion on w here w e should be using t he not ice and consent in regards t o NSA and w hen t hose w ould apply? Only during em ergency services and or an out of net w ork provider at an in net w ork facilit y?
We are seeking clarit y as you not ed t hat ?NSA is int ended t o prot ect t he pat ient from surprise balance bills w hen t hey are receiving scheduled services at an in-net w ork facilit y/ provider. They are offered no prot ect ion from balance billing w hen t hey schedule services at an out of net w ork facilit y/ provider. ?
Answ er: Patients who electively seek non emergency services at an out of network facility, have no protections under the NSA, so the patient can be balance billed without signing a Notice and Consent. The Notice and Consent is issued to a patient who presents to an in network facility when the out of network provider wishes to balance bill a patient, when balance billing is not prohibited. Emergency Services can never be balance billed.

Ancillary providers cannot balance bill patients who seek services at an in network facility
Ancillary services are defined as:
- Items and services related to emergency medicine, anesthesiology, pathology, radiology, and neonatology, provided by either a physician or non physician practitioner; Items and services provided by assistant surgeons, hospitalists, and intensivists;
- Diagnostic services, including radiology and laboratory services; and Items and services provided by an out of network provider when there is no in network provider who can provide the item or service at the in network health care facility
A provider or emergency facility can issue a Notice and Consent for post stabilization services only if all the following requirements are met:
CMSreleased a slide deck that explains the prohibitions on balance billing The link below will take you to that slide deck. The No Surprises Act ?s Prohibit ions on Balancing Billing (cm s.gov)
14 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACTQUESTIONSAND ANSWERS
Quest ion: How do w e know how t he payer det erm ined how m uch t o reim burse?
Answ er: The payer determines the Qualifying Payment Amount (QPA) and shares that information on the claim.
- The July 2021 interim final rules require that plans and issuers: Provide the QPA for each item or service involved
- Provide a statement certifying that:
(1) The QPA applies for purposes of the recognized amount, and (2) each QPA was determined in compliance with the methodology outlined in the July 2021 interim final rules
Provide a statement concerning initiating the 30 day open negotiations period and initiating the federal IDRprocess within 4 days of the end of open negotiations
- Provide contact information for the appropriate office or person to initiate open negotiations
Upon request of the provider, the payer must inform them of how the QPA was determined.
- Information about whether the QPA includes contracted rates that were not set on a fee for service basis for the specific items and services at issue and whether the QPA was determined using underlying fee schedule rates or a derived amount
- Information to identify which database was used to determine the QPA, if applicable
If a related service code was used to determine the QPA for a new service code, information to identify which related service code was used
- If applicable, a statement that the plan?s or issuer?s contracted rates include risk-sharing, bonus, penalty, or other incentive based or retrospective payments or payment adjustments for the items and services involved that were excluded to calculate the QPA
A payer can use databases to determine the QPA
Where a plan or issuer does not have sufficient information to calculate a median contracted rate, the plan or issuer must determine the QPA using an eligible database
A third party database may be an eligible database if it satisfies all of the following conditions:
- No conflicts of interest. - Sufficient information regarding in-network allowed amounts paid for relevant items/services furnished in the applicable geographic region
- Ability to distinguish amounts paid to participating providers and facilities by commercial payers from all other claims data. State all payer claims databases have been deemed eligible
15 PARA Weekly eJournal: September 28, 2022
NO
ACTQUESTIONSAND ANSWERS
Quest ion: I have one m ore quest ion regarding insurance being out of net w ork for lab services Out of net w ork insurance is not paying and denying st at ing t hat ?services rendered by out of net w ork provider not covered? and t he am ount is not m ade pat ient responsibilit y. Can t his be bill t o pat ient or w e need t o disput e?
Answ er: There are some factors to consider when discussing ancillary services and balance billing. Here are some scenarios:
- Specimen collected by an in-network (IN) provider and sent to an out-of-network (OON) Lab
The OON Lab is considered an ancillary service which is always prohibited from balance billing the patient Must dispute payment with payer
Specimen collected and processed by the OON Lab
There are no protections in the NSA for a patient who electively receives services at an OON facility/provider. Patient can be balance billed.
Specimen collected by an OON provider and sent to an OON Lab
The OON Lab is considered an ancillary service which is always prohibited from balance billing the patient. Must dispute payment with payer.
Specimen collected and processed by an IN Lab, but a non covered service by the plan
There are no protections in the NSA for non covered services The patient can be balance billed.

We have provided a link to a CMSslide deck that discusses the prohibitions on balance billing and provided two excerpts which discuss Lab services and balance billing.
The No Surprises Act ?s Prohibit ions on Balancing Billing (cm s.gov)
16 PARA Weekly eJournal: September 28, 2022
SURPRISES
NO
ACTQUESTIONSAND ANSWERS
It is never appropriate for an ancillary service to issue a Notice and Consent to the patient. I have provided an excerpt from the slide deck referenced above.

Qualitox Lab sent this letter to providers stating they will invoice the provider for lost revenue since they can? t bill the patient. That letter can be viewed here: No Surprises Act (qualit oxlab.com ) Contact your legal team if you receive a similar letter from an ancillary provider

17 PARA Weekly eJournal: September 28, 2022
SURPRISES
NO SURPRISES ACTQUESTIONSAND ANSWERS
Quest ion: Does t he post ed not ice (on w ebsit es and in facilit ies) m eet t he requirem ent of providing t he ?Right t o Receive a Good Fait h Est im at e of Expect ed Charges? in WRITING or m ust t he w rit t en not ice be present ed t o t he pat ient in t he m anner t hey choose ? em ail vs m ail? Included is an excerpt from CMS 10791 docum ent w hich leads m e t o t his quest ion. Appendix 1 St andard Not ice: ?Right t o Receive a Good Fait h Est im at e of Expect ed Charges? Under t he No Surprises Act (For use by healt h care providers no lat er t han January 1, 2022) Inst ruct ions Under Sect ion 2799B 6 of t he Public Healt h Service Act , healt h care providers and healt h care facilit ies are required t o inform individuals w ho are not enrolled in a plan or coverage or a Federal healt h care program , or not seeking t o file a claim w it h t heir plan or coverage bot h orally and in w rit ing of t heir abilit y, upon request or at t he t im e of scheduling healt h care it em s and services, t o receive a ?Good Fait h Est im at e? of expect ed charges
Answ er: To clarify Information regarding the availabilit y of a ?Good Fait h Est im at e? m ust be prom inent ly displayed on the convening provider?s and convening facility?s website and in the office and on site where scheduling or questions about the cost of health care items or services occur
Separately, the good faith estimate (GFE) must be provided in written form either on paper or electronically (for example, electronic transmission of the GFEthrough the convening provider?s patient portal or electronic mail), pursuant to the uninsured (or self pay) individual?s requested method of delivery.
GFEs provided to uninsured (or self pay) individuals that are transmitted electronically must be provided in a manner that the uninsured (or self pay) individual can both save and print, and must be provided and written using clear and understandable language and in a manner calculated to be understood by the average uninsured (or self pay) individual.
If a patient requests that the GFEinformation is provided in a format that is not paper or electronic delivery, like orally over the phone or in person, the provider/facility may provide the GFEinformation orally but must follow up with a written paper or electronic copy in order to meet the regulatory requirements
18 PARA Weekly eJournal: September 28, 2022
NO
ACTQUESTIONSAND ANSWERS
Quest ion: How does t he NSA apply t o LTACH facilit ies?
Answ er: This is the response to a similar question answered by CMS: Generally, all providers and facilities that schedule items or services for an uninsured (or self pay) individual or receive a request for a GFEfrom an uninsured (or self pay) individual must provide such individual with a GFE.
No specific specialties, facility types, or sites of service are exempt from this requirement. The terms ?health care provider (provider)?and ?health care facility (facility)?are defined in regulations for purposes of the GFErequirements for uninsured (or self pay) individuals as:
?Health care provider (provider)?means a physician or other health care provider who is acting within the scope of practice of that provider?s license or certification under applicable State law, including a provider of air ambulance services;
- ?Health care facility (facility)?means an institution (such as a hospital or hospital outpatient department, critical access hospital, ambulatory surgical center, rural health center, federally qualified health center, laboratory, or imaging center) in any State in which State or applicable local law provides for the licensing of such an institution pursuant to such law or is approved by the agency of such State or locality responsible for licensing such institution as meeting the standards established for such licensing.
There may be variations in practice patterns, such as whether a specific provider or facility furnishes services to uninsured (or self pay) individuals, along with the types of items or services provided There are some items or services that may not be included in a GFEbecause they are not typically scheduled in advance and not typically the subject of a requested GFE(such as urgent, emergent trauma, or emergency items or services); however, to the extent that such care is scheduled at least 3 days in advance, a provider or facility would be required to provide a GFE For example, individuals will likely not be able to obtain GFEs for emergency air ambulance services, as these are not generally scheduled in advance. However, making these requirements applicable to providers of air ambulance services helps to ensure that individuals can obtain a GFEupon request or at the time of scheduling non emergency air ambulance services, for which coverage is often not provided by a plan or issuer and thus even individuals with coverage must self pay.
IQuest ion: If t he disclosure form t hat is required t o be given t o each pat ient w it h a group healt h plan how do w e prove t his w as given and t he pat ient cont inued t o go t hrough w it h t he appoint m ent ?
Answ er: CMSis not giving any guidance on how to prove that a Disclosure notice was given Facilities and Providers need to contact their compliance department to draft policies/procedure and guidelines to educate, train, and monitor staff for compliance.
19 PARA Weekly eJournal: September 28, 2022
SURPRISES
HCPCSUPDATEPROCESS
As usual, clients will be fully supported with information and assistance on the annual CPT® HCPCScoding updates for calendar year 2023.
The PARA Dat a Edit or (PDE) contains a copy of each client chargemaster; we use the powerful features of the PDEto identify any line item in the chargemaster with a HCPCScode assigned that will be deleted as of December 31, 2022.
ParaRev will not review chargemasters loaded into the PDEolder than 12 months For this reason, it is important that clients check to ensure that a recent copy of the chargemaster has been supplied to ParaRev for use in the year-end update.
ParaRev will produce Excel spreadsheets of each CDM line item, as well as our recommendation for alternate codes, in three waves as information is released from the following sources:
The American Medical Association?s publication of new, changed, and deleted CPT® codes; this information is released in Sept em ber of each year ParaRev will produce the first spreadsheet of CPT® updates for client review in Oct ober 2022

Following the release of Medicare?s 2023 OPPSFinal Rule, typically in early Novem ber; ParaRev will perform analysis and produce the second spreadsheet to include both theCPT® information previously supplied, as well as alpha numeric HCPCSupdates (J-codes, G-codes, C-codes, etc ) from the Final Rule Clients may expect this spreadsheet to be available in Novem ber 2022
Following the publication of Medicare?s 2023 Clinical Lab Fee Schedule (CLFS) ? typically published in late Novem ber, ParaRev will prepare a final spreadsheet to be available in Decem ber 2022 This final spreadsheet ensures that ParaRev shares any late-breaking news or coding information, although we expect the December spreadsheet to be very similar to the November edition.
Clients will be notified by email as spreadsheets are produced and recorded on the PARA Dat a Edit or ?Admin?tab, under the ?Docs?subtab. When the code maps are ready, the 2023 spreadsheet will appear just as they did in 2022:
In addition, ParaRev consultants will publish concise papers on coding update topics in order to ensure that topical information is available in a manner that is organized and easy to understand ParaRev clients may rest assured that they will have full support for year end HCPCScoding updates to the chargemaster
20 PARA Weekly eJournal: September 28, 2022
PARA YEAR END
OCTOBER, 2022
OPPSPAYABLEDRUGS REIMBURSEMENT
In the October 2022 update to OPPS, Medicare announced changes to payment rates for separately payable drugs identified as OPPSstatus indicators G and K. A link and an excerpt are provided below:
https://www.cms.gov/files/document/mm12885 october 2022 update hospital outpatient prospective payment system opps pdf
c. Drugs and Biologicals w it h Paym ent s Based on Average Sales Price (ASP)
For CY2022, payment for most nonpass-through drugs, biologicals, and therapeutic radiopharmaceuticals that weren? t required through the 340B Program is made at a single rate of ASP+ 6%(or ASP+ 6%of the reference product for biosimilars) In CY2022, a single payment of ASP+ 6%for pass-through drugs, biologicals, and radiopharmaceuticals is made to provide payment for both the acquisition cost and pharmacy overhead costs of these passthrough items (or ASP+ 6%of the reference product for biosimilars). We?ll update payments for drugs and biologicals based on ASPs on a quarterly basis as later quarter ASP submissions are available
Effective October 1, 2022, payment rates for many drugs and biologicals have changed from the values published in the CY2022 OPPS/ASCfinal rule with comment period because of the new ASPcalculations based on sales price submissions from the fourth quarter of CY2021. In cases where adjustments to payment rates are necessary, we?ll add changes to the payment rates in the October 2022 Fiscal Intermediary Standard System (FISS) release. ?

The following table lists the changes in per unit OPPSreimbursement, sequenced by the highest rate of change. In the interest of brevity, we list only those HCPCSfor which the payment rate increased or decreased more than 10%below.
Values are rounded to the nearest penny.
21 PARA Weekly eJournal: September 28, 2022
OCTOBER,

22 PARA Weekly eJournal: September 28, 2022
2022 OPPSPAYABLEDRUGS REIMBURSEMENT
OCTOBER,

23 PARA Weekly eJournal: September 28, 2022
2022 OPPSPAYABLEDRUGS REIMBURSEMENT
got
perplexed?
You're not alone.
In this special issue of the eJournal we've assembled 20 quest ions from the hundreds of inquiries received during our No Surprises Act Webinars.
If you've never attended one of our free webinars, never fear. There's anot her one scheduled right around t he corner. Registering is easy. Just scan the QRCode and sign up. Then get ready for some great information that will prepare you for what's ahead.


24 PARA Weekly eJournal: September 28, 2022 NO SURPRISES ACTQUESTIONSAND ANSWERS HastheNoSurprises Act
youwondering, dazed,confused, befuddled,bewildered anddownright
NO
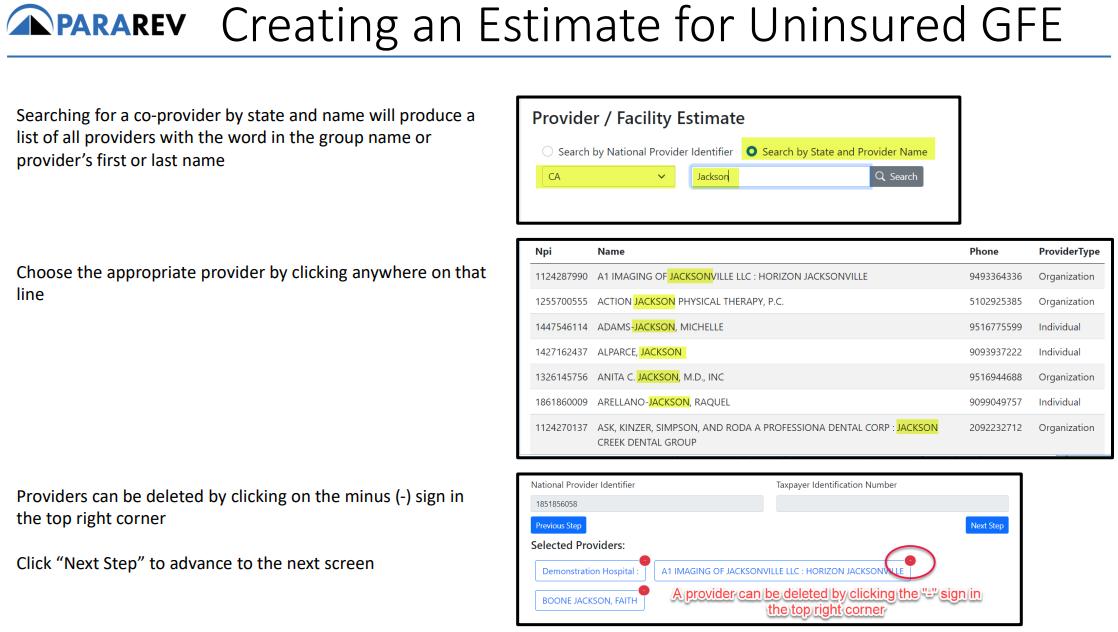
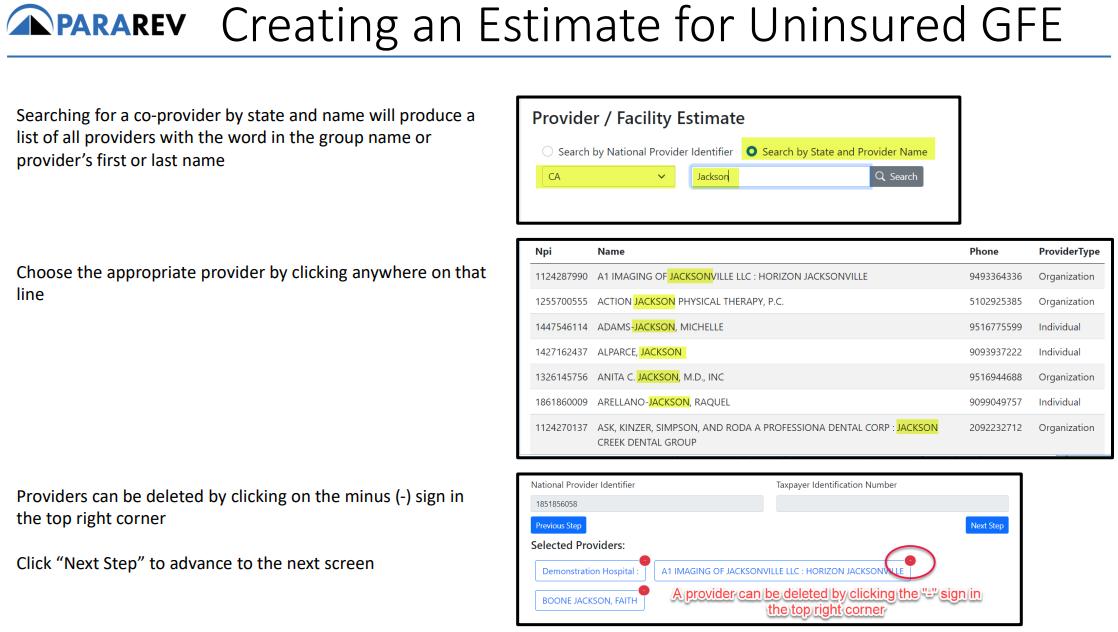
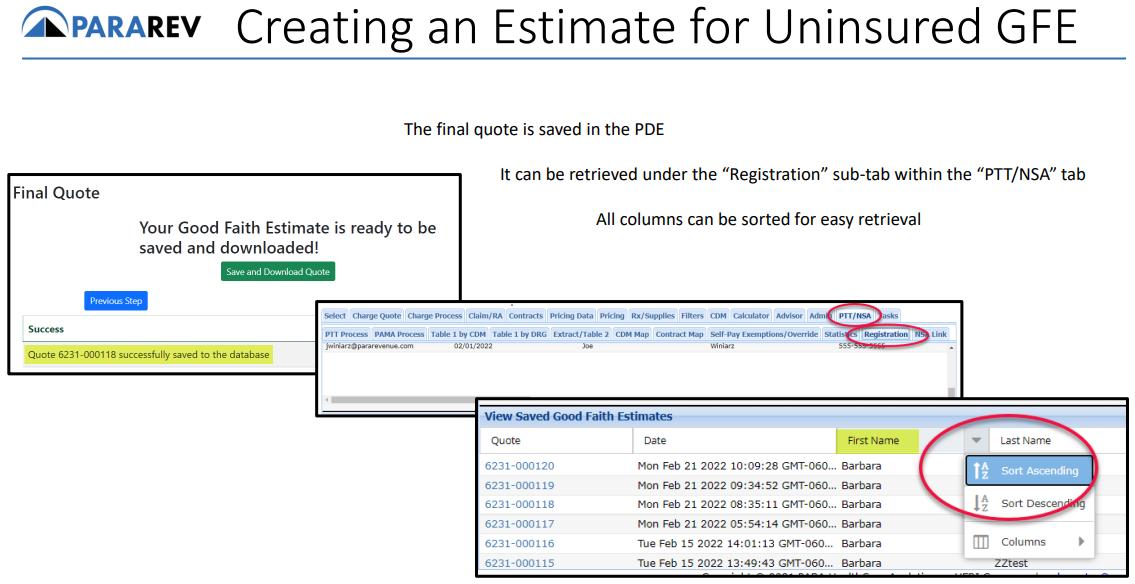
ACT: PARAREV'SNSA TOOL SLIDEDECK

Andnow,there'smore!
Here's a sneak peek of the slide deck used in our regular No Surprises Act Webinar, along with TEN MORE questions and answers that are sent in each week!
If you haven't yet signed up for our webinar, click the QRcode on the previous page and register. It's important. It's informative. And, most of all, it's free!
25 PARA Weekly eJournal: September 28, 2022
SURPRISES
NO
ACT: PARAREV'SNSA TOOL SLIDEDECK


26 PARA Weekly eJournal: September 28, 2022
SURPRISES


27 PARA Weekly eJournal: September 28, 2022 NNO SURPRISESACT: PARAREV'SNSA TOOL SLIDEDECK
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


28 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


29 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


30 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


31 PARA Weekly eJournal: September 28, 2022
NO

TOOL

32 PARA Weekly eJournal: September 28, 2022
SURPRISES ACT: PARAREV'SNSA
SLIDEDECK
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


33 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


34 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


35 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


36 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


37 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK

38 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK

39 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


40 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK

41 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


42 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


43 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


44 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK

45 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


46 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


47 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


48 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK


49 PARA Weekly eJournal: September 28, 2022
NO SURPRISES ACT: PARAREV'SNSA TOOL SLIDEDECK

50 PARA Weekly eJournal: September 28, 2022


51 PARA Weekly eJournal: September 28, 2022 This is it .Par aRev hascompl et ely updat edit s Compr ehensive COVID-19Guide.TheGuidecontains detail edinfor mat ionabout bil l ingandcoding,t est ingandot her guidancer el at edt oCOVID-19. It's online. You can download it by clicking the image to the right, or by clicking the URL here: https://apps.parahcfs.com/para/ Documents/ 2022%20Comprehensive% 20Covid-19%20Guide pdf COMPLETELY UPDATED: COMPREHENSIVECOVID 19 GUIDE
MLN CONNECTS

52 PARA Weekly eJournal: September 28, 2022
PARA invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS) It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources Click each link for t he PDF! Thursday, Sept em ber 22, 2022 New s - Flu Shot: Encourage Preferred Vaccines for Patients 65+ - Cataract Surgery: Comparative Billing Report - Do You Only Order or Certify Services?Use Revised Enrollment Form CMS-855O by January 1 - Cardiovascular Disease: Talk with Your Patients about Screening Claim s, Pricers, & Codes - October 2022 Quarterly Average Sales Price (ASP) Medicare Part B Drug Pricing Files and Revisions to Prior Quarterly Pricing Files MLN Mat t ers®Art icles - October 2022 Update of the Hospital Outpatient Prospective Payment System (OPPS) Publicat ions - Hospice Quality Reporting Program: New Resources
r ans mit t al s

53 PARA Weekly eJournal: September 28, 2022 Therew ereFOUR new or revised Transmittalsreleased thisw eek. To go to thefull Transmittal document simply click on thescreen shot or thelink. 4 t
TRANSMITTAL R11610CP

54 PARA Weekly eJournal: September 28, 2022
TRANSMITTAL R11611CP

55 PARA Weekly eJournal: September 28, 2022
TRANSMITTAL R11612CP

56 PARA Weekly eJournal: September 28, 2022
TRANSMITTAL R11613PI

57 PARA Weekly eJournal: September 28, 2022
m edl ear ns

58 PARA Weekly eJournal: September 28, 2022 1
Therew asONEnew or revised MedLearnsreleased thisw eek. To go to thefull Transmittal document simply click on thescreen shot or thelink.
MEDLEARN


59 PARA Weekly eJournal: September 28, 2022
MM12915
FORYOURINFORMATION
Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to the best of ParaRev?s knowledgeisaccurate at thetime of distribution. However, dueto theever changing legal/regulatorylandscapethisinformation issubject to modification, asstatutes/laws/regulationsor other updatesbecomeavailable.
Nothingherein constitutes, isintended to constitute, or should berelied on as, legal advice ParaRev expressly disclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anythingcontained in thematerials, which areprovided on an ?as-is?basisand should beindependentlyverified beforebeing applied.
You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability.Theinformation in this document isconfidential and proprietaryto ParaRev and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduce or transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording and broadcasting, or byanyinformation storageand retrieval system must be obtained in writingfrom ParaRev. Request for permission should be directed to sales@pararevenue.com.
ParaRev is excited to announce we have joined industry leader CorroHealt h to enhance the reach of our offerings! ParaRev services lines are additive in nature strengthening CorroHealt h?s impact to clients?revenue cycle. In addition, you now have access to a robust set of mid cycle tools and solutions from CorroHealt h that complement ParaRev offerings


In terms of the impact you?ll see, there will be no change to the management or services we provide The shared passion, philosophy and cultures of our organizations makes this exciting news for our team and you, our clients

While you can review the CorroHealt h site HERE, we can coordinate a deeper dive into any of these solutions Simply let us know and we?ll set up a meeting to connect.
As always, we are available to answer any questions you may have regarding this news We thank you for your continued partnership
60 PARA Weekly eJournal: September 28, 2022
