DSCSA DEADLINE LOOMING
Will you be ready by November 27?
AI CHATBOTS
The pros and cons

DSCSA DEADLINE LOOMING
Will you be ready by November 27?
The pros and cons
Improve outcomes for patients and your pharmacy

Wherever your pharmacy is with clinical services, Workflow Services can help you commercialize new services, optimize existing workflows, and maximize revenue potential.
We will guide you to:
• Launch services allowed in your state
• Secure contracts with medical insurance companies
• Develop and deploy clinical protocols
• Get paid for services with cash or insurance

• User-Decision Support Software & Digital Protocols

• Patient Communication & Education Tools
• Payor Credentialing & Contracting for Pharmacists
• Patient Self-Pay & Co-Pay
• Universal Patient Health Record Access
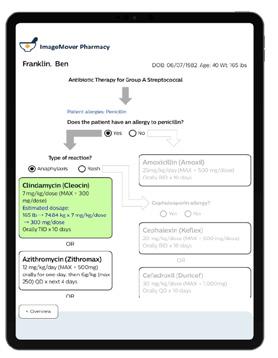
• Building & Submitting Medical Claims
• Pharmacy Management System Integration



Payor Credentialing & Contracting
Pharmacy Locator and Patient Engagement



Pharmacy Workflow
Cash Pay and Medical Claims Reimbursement


VOLUME 12, ISSUE 3
SEPTEMBER 2023
PUBLISHER & EDITORIAL DIRECTOR
Matthew Shamet EDITOR
Gina Klein
GRAPHIC DESIGNER
Logan Whetzal
CONTRIBUTING WRITER
Cecilia Vigliaturo
INTERESTED IN ADVERTISING?
elements@pbahealth.com
Mental health illnesses are among the most common health conditions in the United States. In fact, statistics show that mental health conditions are on the rise while access to care is becoming even more difficult.
Proper medications and counseling support are two major factors playing into a patient’s smoking cessation success. As a community pharmacist, you’re in a perfect position to deliver both while getting reimbursed.
Diabetes is a chronic health condition that affects more people today than ever before. About one in 10 Americans have the disease, and one in five people don’t know they have it. This is an area where your independent pharmacy can help.
As a partner, you’ll have access to: Group purchasing organization (GPO) pricing
An extensive, expanding vaccine portfolio, including flu vaccines
Access to numerous manufacturers
Streamlined ordering platforms
Shipping visibility
Marketing support and vaccine expertise

Anew variant landed this summer and has been making its way to being at the top of all COVID-19 cases in the U.S.
EG.5.1, unofficially nicknamed “Eris,” is an offshoot of the omicron variant EG.5 and has been circulating throughout the country since spring. And as of August 5, the Centers for Disease Control and Prevention (CDC) said it accounts for 17.3% of COVID infections. CDC data shows this is an increase from the 1.1% of cases it was estimated to make up at the end of May.
The good news is that while it’s been deemed by experts to be the fastest growing strain thus far, public health officials say there is no evidence that EG.5 causes more severe illness. Furthermore, it’s completely normal for the virus to mutate and new variants to emerge.
EG.5 is an offspring of omicron, and while contagious, it’s not more serious. In fact, it’s less invasive and lethal in the body. The response to it is generally the same as for other variants. The CDC also indicates that the EG.5 variant appears to be susceptible to coronavirus vaccines.
Symptoms to look for with this subvariant are very similar to the coronavirus in general:
• Dry cough
• Runny nose
• Sneezing
• Fever
• Chills
• Fatigue
• Muscle or body aches
• Shortness of breath
• Loss of taste or smell
• Headache
The symptoms can range from mild effects to more serious illness. But with fluctuations in weather and a lack of testing, it can be difficult to differentiate between an EG.5 infection and the flu or a common cold.
Elderly people are at higher risk and may be the most vulnerable to these new strains. Plus, their immunity from vaccination can dwindle more rapidly. While EG.5 doesn’t seem to be increasing the number of cases in intensive care or deaths, it could be responsible for more hospitalizations.
Health experts say vaccines and boosters should still be encouraged, along with safe social practices, such as wearing face masks, and keeping rooms well ventilated.
U.S. health officials are preparing to administer booster doses of coronavirus vaccines in the fall. The vaccines are made with a new formula that targets the XBB subvariants that accounted for most infections in 2023.
According to the World Health Organization (WHO), the coronavirus remains a major threat. Though the international public health emergency was declared officially over May 5, the WHO urges member states to maintain their established COVID-19 infrastructure rather than dismantle it.
Public health officials say there is no evidence that EG.5 causes more severe illness.
Lure them in with first-rate products
Your customers are on a mission. Whether they’re in your pharmacy to pick up a prescription, grab a box of bandages, a magazine, or a bottle of multivitamins, they know you’ll have what they need. What they don’t know, however, is what fun, exceptional items they may find in the front of your store that will make its way into their cart.
Displaying the right products in your front end will help boost foot traffic and improve your bottom line. In fact, average margins on front-end merchandise are 15 percent higher than the margins on prescription sales. So, what are you waiting for?
Do you remember the last time you studied the front end of your store? If not, it’s time. You need to know what products are displayed and how long they’ve been there. Your front end should draw attention and bring in sales. If your customers don’t linger for long, it’s time to revamp the shelves with something new.
Make a great impression on your patients by keeping up with the cleanliness and layout of your store. Here are some ideas to consider:

Motivate your patients to shop and increase retail sales by changing up your front-end layout. Look at your shelves and fixtures. Consider moving them around to make areas look larger or less cluttered. Increase end-cap space. Highlight a particular display to draw more attention. If you feel you need help with this project, hire a design expert.
If your lighting is too dim and dismal, it’s time for improvement. The right lighting can make your front end look completely different and much more exciting. Remove any fluorescent lighting. It’s been proven to induce stress. Instead, boost the natural light coming into your pharmacy. If that doesn’t work, incandescent lights are the next best option.
Increase sales with attractive pharmacy shelving. Find custom shelving that fits with the overall design of your front end to dramatically improve the look and usability.
“We have a very non-traditional front end,” said Erin Merritt, PharmD and owner of Modern Apothecary Pharmacy in Kenosha, Wisconsin. “I have maybe two gondola racks in my entire store. Most of our shelving came from a legal library, so it’s older-looking wood shelving. I have a lot of antiques sprinkled throughout the store in displays on shelves, next to the homemade soap made by a local artisan, jewelry, and so on. I also found a vintage bathtub that we converted into a table so that all of our soap is in the bathtub.”
Excite patients with your endcap displays. Use them to feature, promote, and sell products. But be sure to change the displays at least once a month and with every season.
Once you’ve got the right lighting, shelves, and layout, get creative with the front of your store. As you begin stocking, include hot-selling items people want and need, such as cellphone needs, first aid, pain relief, and sunglasses. But don’t forget to add a sprinkle or three of unique products here and there to draw in even more sales. Here are some ideas to get you started:
• Custom jewelry: Present some one-of-a-kind, fun styles that aren’t found at most stores. Find a local jewelry artist and offer to display his or her chic designs along with some fashionable retail jewelry.
• Popular toys: Once upon a time, fidget spinners were the hot trend filling front ends. While that fad has passed, others have taken its place. Stock the front of your store with dolls, toy cars, coloring books, baseball cards, candy, and today's latest trend.
• Local honey: Find someone in your community who makes and sells honey. Customers love homemade products made by someone in their vicinity.
• Greeting cards made by local artists or design studios: Shoppers are always looking for something out of the ordinary to give to a loved one. Be sure to restock as the display starts to dwindle, otherwise your sales will plummet as well.
• Soaps and lotions made by local artisans: If there is someone in or near your community who makes natural soaps or lotions, this is a great front-end product because it’s natural and locally made.
Also, Merritt says she’s found a lot of different options for products on the website faire.com. “It allows you to buy from smaller, local vendors and you can filter by location if you want something local to your state. We’ve found a lot of our products that way.
Some of the specific brands we carry have been requests from patients, and some products are things that I like and what I thought people would like.”
Merritt also carries a lot of locally sourced products, regional products, and natural products, such as candles, greeting cards, professional supplements, men’s grooming items, and even supplies recommended by a local lactation consultant along with a depot and dispensary for breast milk.
To make sure her inventory is turning, Merritt keeps an eye on sales numbers. “We have pharmacy software and have everything in there individually. That way we can pull up day-by-day sales if we want to. We usually just check them every couple of weeks.”
Wanting to change things up in your pharmacy front end? Merritt suggests buying unique front-end products in small quantities to see how they’ll sell. Look for local talent, or check out sites like faire.com, and a marketplace where you can search for locally sourced products.
When it comes to your front end, show your patients you mean business. Invite them into your pharmacy with your clean, clutter-free shelves, bright and inviting lighting, and a variety of truly special products they’ll love.
Educating patients on what’s right for them

ctober 2022 was a big turning point for the hearing industry. Pharmacies and other retailers were allowed to sell over-the-counter (OTC) hearing aids after having been restricted for decades. What’s more, different types of hearing aids are now categorized with very clear lines of demarcation to differentiate them. Patients can choose from prescription hearing aids, OTC hearing aids, and personal sound amplification products (PSAPs), also known as amplifiers.
With over-the-counter hearing aids now stocked on store shelves along with PSAPs, it’s important to talk with patients about the differences between the two. While they both utilize technology to help with hearing, they have completely different outcomes.
It wasn’t until recently that PSAPs began gaining popularity. With improved technology and much lower prices, they’ve caught the attention of many consumers with hearing loss. However, they are intended for those who do not have hearing loss, but instead wish to enhance their listening experience in certain situations.
Here are the main differences between hearing aids, OTC hearing aids, and PSAPs:
Prescription Hearing Aids: These FDA-approved, sound-amplifying medical devices are made to compensate for impaired hearing. They are medical devices manufactured and programmed for a person’s specific hearing loss and are worn behind or in the ear. A prescription is needed for purchase. They’re distributed by licensed audiologists; ear, nose, and throat doctors; or sellers who are licensed to dispense hearing aids. Cost: $4000—$6,000
Over-the-Counter (OTC) Hearing Aids: OTC hearing aids make up a new category of hearing aids for those with perceived mild-to-moderate hearing loss. These are self-care devices, which means patients can buy them in the store or online without seeing a physician for an exam or an audiologist for help with fitting. Cost: $300—$2,000
Personal Sound Amplification Product (PSAP): PSAPs are consumer electronic products that amplify sounds or provide clarity in noisy environments. They make all sounds louder, including the ones that wearers already hear well. They are not made for people with hearing loss. The National Institute on Deafness and Other Communication Disorders (NIDCD) states that amplifiers are best for those with little-to-no hearing loss to boost their ability to hear in certain situations. Cost: $250—$500
“The PSAPs aren’t indicated for someone with hearing impairments, and they’re not an FDA-registered medical device,” said Anthony Florek, President of Soundwave Hearing, LLC. “They were originally designed for hobbyists who walk through the woods and want to hear the birds from a distance. They’re also great if you’re in a very quiet room while talking to one person across a table. But as soon as you get out into a noisy environment of any kind, it can be very frustrating because amplifiers amplify everything.”
Knowing which type of hearing help is best can be frustrating for your patients. That’s where you come into the picture to help them understand the differences between hearing aids and PSAPs. You can also help them compare the features of each and let them know if a visit with an audiologist is needed.
Your patients may want to consider a PSAP if they:
• Sometimes have trouble focusing on people’s voices during conversations
• Need a higher volume setting on the TV than other people
• Take part in hobbies that may require amplified sound (i.e. bird watching, movies, etc.)
• Often have difficulty hearing a speaker’s voice during a lecture or presentation
Your patients may want to consider a hearing aid if they:
• Were diagnosed with a form of mild to severe hearing loss by a professional, licensed hearing specialist
• Are affected by their hearing loss negatively in day-to-day situations
• Want to protect themselves from further hearing loss
OTC hearing aids aren’t for everyone. Here’s why:

OTC hearing aids are intended for people with mild-tomoderate hearing loss. Those with severe or profound hearing loss need specialized, high-powered hearing aids or surgically implanted devices.
People who have a history of chronic ear infections or fluctuating hearing loss should seek the help of a hearing care professional.
OTC hearing aids are not designed for children with hearing loss. Hearing aids for kids need to be programmed and optimized to help them do their best in school. Plus, children’s ears change shape as they grow. This requires custom earpieces and specialized, pediatric hearing aids.
Anyone with a sudden change in hearing should seek immediate medical advice from an ENT or emergency department. A sudden hearing loss can be a sign of another medical problem and should be evaluated, especially if accompanied by dizziness or tinnitus. Prompt treatment might restore hearing, but if not, a prescription hearing aid will likely be needed.
If there is hearing loss in both ears, but one ear hears better than the other, OTC hearing aids are not the right treatment option. The same is true if only one ear has hearing loss. The first step should be to see an audiologist or ENT to rule out other medical conditions that can cause this type of hearing loss.
People with very narrow ear canals, curvy ear canals, or surgical ears, should consult with a professional before considering an OTC hearing aid.
(Source: https://www.healthyhearing.com)





As a busy community pharmacist, it can sometimes be a struggle to keep up with all your patients’ needs. Answering questions, scheduling appointments, and sending reminders are only a few areas that take up a lot of your time. There’s also the tracking of routine data and symptoms, creating medical records, and much more. That’s where artificial intelligence (AI) chatbots can help.
There are numerous advantages to having an AI chatbot. Not only does it provide an around-the-clock, constant source of interaction for your patients with the healthcare system, but patients feel confident with the chats due to the anonymity associated with them. The chatbot can provide personalized health advice and recommendations based on the patient’s symptoms and medical history. Plus, AI-powered platforms can provide easy access to information about healthcare products, such as OTC medications and food supplements. This can help your patients understand the potential benefits, any risks, and the correct way to use the products.
Here's a full rundown on how medical chatbots can help your pharmacy and your patients:
Chatbots (aka virtual assistants) handle the initial contact with patients. They do the asking and answering of routine questions that come up, and can recommend care options after users enter their symptoms. This saves money and manpower, yet accomplishes efficient screening.
Chatbots can also enable patients to schedule appointments and refill prescriptions. Additionally, they can help them get a second opinion on their diagnosis or treatment plan, if needed.
Patients may need urgent medical attention at times when healthcare advisors may not be available. Healthcare chatbots provide real-time assistance and are extremely helpful in situations like this. There are no wait times because AI answers all the questions patients and caregivers may have that don’t require a medical professional.
A medical chatbot can also interact with patients who suffer from anxiety, depression, or even feelings of loneliness. The chatbot allows them to share their emotions without the fear of judgment. It also offers good advice.
Believe it or not, chatbots can help patients get their healthcare insurance claims approved quickly and without hassle. After all, they’ve been with your patient throughout their illness. They can help patients choose the most useful insurance policies for their medical conditions. They also save them time and money by shortening the process of claiming insurance and simplifying the payment process.
With an AI chatbot, you can collect data on target customers (i.e. demographics, preferences, and purchasing habits) using surveys, sales data, and social media.
While healthcare chatbots are a wonderful way to help patients and customers connect with their healthcare providers, there are also some disadvantages to keep in mind. For instance, while chatbots are great for providing information, there is no real human interaction.
Human interaction is better than using a chatbot for several reasons. First, it can connect patients with a real person who can help them make decisions about their care. It also lets your patients take an active role in their own treatment, and doctors are given more opportunities to assess patients’ behaviors and symptoms.
A chatbot will work just fine if your patient’s trying to get help with something minor, such as an upset stomach or a flu bug. But if it’s something serious, they should talk to a real person. Many chatbots can help them connect with a healthcare professional through a live chat.

Another drawback with chatbots is the amount of limited information available. They’re designed to be simple and easy to use, so they only offer a small amount of data at any given time. So, if your patients are looking for an in-depth answer to a complex medical problem, they might get a bit flustered.
Over time, patients will start to trust chatbots more and more. But placing too much trust in them can be damaging because users can potentially be exposed to data hacking. Security concerns are one of the biggest disadvantages of healthcare chatbots. And while they’re still in the early stage of development, many security concerns need to be addressed before they can be used more widely.
Let your customers know you care about their needs. Here are some great ways customers can use your pharmacy chatbot:
With a pharmacy chatbot, your customers will be able to transfer prescriptions or request refills. The chatbot will forward the prescription request to an agent to fulfill.
Using the patient’s reference number, the chatbot can quickly share the status of their prescription. It uses an application programming interface (API) integration to track the order status.
Some chatbots can forward the patient to an agent or pharmacist for emergencies or when they need to speak to someone face to face.
A chatbot can help answer general questions patients may have regarding side effects or ingredients for a specific medication. Pharmacists can even send helpful studies and research documents that patients can download directly from the chat.
Your chatbot can be programmed to remind patients of upcoming appointments. This alone is one of the reasons why many healthcare organizations are considering adopting them.
Woebot
This mental-health chatbot provides its users with cognitive-behavioral therapy (CBT) via a conversational interface. It provides personalized support and guidance for managing symptoms of anxiety, depression, and other mental-health conditions.
Babylon Health chatbot offers a range of services, including symptom checking, triage, and virtual consultations with healthcare professionals. It uses AI and natural language processing (NLP) to provide personalized recommendations and treatment plans based on users’ symptoms and medical history. It also offers a range of health-monitoring tools, including fitness tracking and sleep monitoring.
Sensley offers a virtual medical assistant to help patients manage their health and navigate the healthcare system. It uses AI and NLP to provide personalized support for medication management, appointment scheduling, and accessing health resources.
Florence
This chatbot monitors a user’s health, such as their body weight, mood, or menstruation. It assists them in achieving their objectives. Florence can also be programmed to locate the closest pharmacy or medical facility.
The Cancer Chatbot is dedicated to charitable causes. On Facebook Messenger, it’s useful for cancer patients, carers, friends, and family. It provides patients with a wealth of options, including free services and advice on chemotherapy. It also offers resources for carers and supports friends and relatives.
This health chatbot prompts users to describe their symptoms before sending the information to physicians, who diagnose and issue prescriptions in real time. The service is available on Facebook Messenger and Alexa, but they hope to make it available on other messaging platforms, too.
With Buoy Health, patients can look up their symptoms online or search the extensive database to determine what might be wrong with their health. The chatbot probes them about specifics of their medical condition and presents them with a range of options and doable next steps.
Suki offers voice-activated, AI-backed medical documentation solutions. It has a digital assistant that can record doctor-patient discussions, help clinicians take notes orally using natural language, and listen to them. It uses cloud and NLP technology.
This chatbot offers a symptom assessment tool to help patients determine the underlying cause of their symptoms. It uses AI and NLP to understand users’ symptoms and medical history, and provides personalized treatment and further evaluation recommendations.
This healthcare chatbot offers a virtual billing assistant that helps patients manage their medical bills and insurance claims. It uses AI and NLP to understand patients’ billing questions and concerns, and provides personalized support for payment scheduling, insurance verification, and claim status updates.
(Source: www.botpenguin.com)
Quality Choice focuses on providing your business with over-the-counter health, beauty, and wellness products in multiple categories. A leader in the industry with over 25 years of experience, we provide products with everyday savings for our customers.

PBA Hea lth’s Program with QC offers:

• Gross margins as high as 89%
• An extensive selection of categories with over 700 SKUs
• Free merchandising and marketing services

• Everyday savings for consumers with a 100% satisfaction guarantee
• Assistance with filling orders when your wholesalers are out of product stock
• Expedited order processing & shipping

F or as long as people have been prescribed medications, medication adherence has been a struggle.
The National Community Pharmacists Association (NCPA) pointed out in its “Medical Adherence Report Card” that patients most likely to be non-compliant with their medication regimen are those who lack a strong relationship with their pharmacist. In fact, the survey detected one out of three patients over 40 with a chronic condition rated a D or an F when it came to taking their medications correctly.
The World Health Organization (WHO) suggests that patients are considered adherent if they take 80% of their prescribed medicines. Research shows that one-fourth of new prescriptions are never filled at all. And when they are filled, nearly half of patients with chronic conditions fail to take the medications as prescribed. This often leads to detrimental health outcomes such as more hospitalizations, higher healthcare costs, and even death.
Non-adherence also costs your pharmacy business. Remember: Every time your patient refuses to take medication, you lose revenue. And it’s not just a financial problem; it’s also physical.
“Our number one expense can be controlled by simply working on an adherence program. Patients who aren’t on
an adherence program are typically those patients who take a lot of expensive medications,” said Tim Mitchell, RPh, Mitchell’s Drug Store. “So, there’s no sense in us ordering and keeping $50,000 to $60,000 of extra medicine on hand. We’re going to call them and say, ‘This is when your insulin is due,’ or ‘This is when your $1,500 medication is due,’ and then make a determination from there.”
The mortality rates among patients who don’t adhere to their medication are nearly double the rates of those who take their medications as prescribed. At least 125,000 preventable deaths every year can be attributed to non-adherence. On the other hand, good adherence is associated with a 21 percent reduction in long-term mortality risk.
“As we all know, staffing has been a challenge over the past couple of years with turnovers occurring in community pharmacy. But now that we’re able to staff accordingly, we can get our tasks done,” Mitchell said. “When we know we’re working on medication synchronization, which is about every day, I’d say probably 60 to 70 percent of our prescriptions are filled by 2 or 3 o’clock in the afternoon. After those are done, we start working on being more efficient with other things, such as calling patients for the following day or the next week.”
There isn’t a perfect solution to get patients to take their medicine. They fail to stay adherent for a variety of reasons, such as:
• Failing to refill
• Forgetting to take their medication (perhaps due to age or dementia)
• Multiple medications with confusing instructions
• Fears or confusion about the medication
• Medication costs they can’t afford
• Intolerable side effects
• Medications that make them feel worse
• Lack of transportation to a pharmacy to pick up refills
• Poorly educated on their medication or not at all
A medication adherence program is centered around patient education, proactive counseling, and overall synchronization. The goal is to improve patient medication use and reduce medication overuse or underuse.
DID YOU KNOW?
• More than 1 in 5 new prescriptions go unfulfilled.
• At least 125,000 Americans die annually due to poor medication adherence.
• 50 percent of people taking a chronic medication stop taking it in the first year.
• Half of patients do not take their medications as prescribed.
Loyalty to a medication routine can have extensive impacts on the quality and length of your patients’ lives, their health outcomes, and overall healthcare costs.
“We use adherence programs as a foundation for clinical services,” said Lacy Epperson, PharmD, at Mitchell’s Drug Store. “Pharmacists are one of the most successful healthcare providers, and with that, it's a way to best control our workflow. Whether it’s inventory management, employee staffing, clinical management, or overseeing a patient’s profile, I feel like that’s the most organized approach to taking the best care of the patient and the best care of the business.”
The Medicare Modernization Act requires Medicare Part D prescription drug plans to include MTM services delivered by a qualified healthcare professional— especially pharmacists.
Although MTM can include many different services, just having a conversation about all of a patient’s medications and providing suggestions on how to manage them can go a long way to improving adherence. The hands-on help you provide is the most crucial benefit.
This is the most powerful of adherence strategies. Research has shown dramatic improvement in adherence when pharmacists employ a med sync program.
A study by the NCPA shows that patients who use these programs are:
• Five times more likely to be adherent to their medications
• 21 percent less likely to discontinue drug therapy
• Averaging more than 100 additional days on therapy per year
• Poor medication adherence costs the U.S. $100 billion per year in hospital admissions.
(Source: unchealthcare.org)
• 30 percent more likely to take their medication as prescribed
Med sync allows patients to pick up all of their ongoing prescription refills at the pharmacy on the same day each month. This makes it easier for patients to manage their medications and remember when to take them.
Save Time and Money with a Single Supply and Equipment Vendor
Save Time and Money with a Single Supply and Equipment Vendor
InSource is your go-to source for clinical supplies, equipment, pharmaceuticals, and more.
InSource is your go-to source for clinical supplies, equipment, pharmaceuticals, and more.
Between stocking your store or warehouse, maintaining your equipment, and sanitizing your space, it takes time and labor to keep your business running smoothly. Simplify the process by partnering with one vendor for all of your purchasing needs.
Between stocking your store or warehouse, maintaining your equipment, and sanitizing your space, it takes time and labor to keep your business running smoothly. Simplify the process by partnering with one vendor for all of your purchasing needs.


Streamline logistics and fulfillment with a single medical supply partner
Streamline logistics and fulfillment with a single medical supply partner



Benefit from cooperative purchasing and long-term supplier relationships
Benefit from cooperative purchasing and long-term supplier relationships
Carrying the majority of the load for medication adherence are MTM and med sync services. The use of scheduled monthly appointments makes them stand out even more. In an appointment-based model (ABM) adherence program, patients meet with you monthly. The appointment includes consultation and synchronization, but can also involve a lot more, such as the use of motivational interviewing to encourage patients to make healthy choices. For example, enrolling in further services at your pharmacy, such as immunizations or a diabetes prevention program.
Forgetfulness is a large reason for non-adherence. That’s why it’s so important to set reminders. Set them up via phone calls, mobile-app alerts, or automated text messages to remind your patients when it’s time to take or refill their medications. Plus, the reminders can be customized to the patient’s preferences.
Wearable devices also monitor medication adherence and provide feedback to patients and healthcare providers.
Here are some of the digital medication adherence systems available for both you and your patients:

1. Pillpack: A medication delivery service that provides presorted doses of medications in individual packets and delivers to customers.
2. Mango Health: A mobile app that allows users to manage their medication regimen and track their health.
3. Digital Pharmacist: Provides digital solutions for independent pharmacies including a branded app, digital refills, communications, and engagement tools.
4. Surescripts: An app that supports standard electronic prescription transactions to pharmacists to securely e-prescribe within their existing workflow.
5. Medisafe: This app sets medication reminders, tracks your progress, and alerts the user for potential drug interactions.
6. AdhereTech: A smart pill bottle that helps patients manage their medication regimen.
7. MedMinder: A smart pill dispenser that tracks medication adherence and provides alerts.
8. CareZone: This mobile app is for medication regimen tracking, setting reminders, important health information, symptom checker, and a directory of healthcare providers.
9. Reminder Rosie: This medication management system consists of a voice-enabled alarm clock and mobile app.
10. Pillboxie: This mobile app allows patients to track their medication regimen, set reminders for taking medications, and receive alerts about their medication adherence. It also provides drug information.
“We’ve got patients in different demographics who love our rapid packs,” said Epperson. "Our rapid-pack machine is very efficient and that’s a big part of our adherence program.
I like to think of our adherence program in three layers. In step one, you have your regular med-sync patients. At the Community Pharmacy Enhanced Services Network (CPESN) level, we’re using the term ‘care sync’ because we’re not just looking at their medicines. There’s a lot that we’re doing for the patient during that monthly touch point. Once we have caresync patients all taken care of and we’ve got them regimented, step two is our adherence packaging. So, for us that’s going to be our rapid pack. Step three is our Medical at Home program.”
Having the ability to automate manual processes to work as efficiently as possible is probably one of the greatest benefits of using advanced technology in your pharmacy. By automating dispensing workflows with a medication synchronization program, you can free up more time to spend with your patients. And with built-in care alerts, it’s easy for you to target patients who need intervention counseling to improve their medication adherence.
When patients take their medication as prescribed, they’re much more likely to notice positive treatment results. Adherent patients are also more likely to engage proactively in their own health.
When you have the right technology, you can implement a med sync program that will improve both adherence and your profits. Your pharmacy and patients will be healthier as a result.
Make it as easy as possible for your patients to take their medication. If you decide not to go with a med sync program, offer adherence packaging.
Partner with a company that creates blister packs for patients with chronic conditions or patients who manage multiple medications. Want to go the extra mile? Invest in smart blister packs. That way, your patients can keep track of the medications they’ve already taken and those they still need to take. Blister packs are beneficial for those who find it difficult to read small print or have vision problems. Many packs have large, easy-to-read labels and are color coded.
Pharmacy Revenue Boost:
With fewer missed refills and a consistent prescription volume, med sync programs help increase your pharmacy revenue and spark profitability. With higher medication adherence rates, it’s easier for you to predict your weekly and monthly flow of cash since refills are filled consistently each month.
Better Clinical Care Services:
Often included with medication adherence solutions are features that allow you to offer enhanced clinical care services. A lot of the medication adherence solutions available today give much-needed support for many clinical care services, including:
• Immunizations/flu shots
• Point-of-care testing
• Durable medical equipment
• Medication therapy management
• Chronic disease management
Higher Quality Scores:
Because quality scores are now directly tied to reimbursement, there’s a significant financial motivation to improve medication adherence rates.
This helps your patients identify their medication. Plus, blister packs have symbols near each cavity that indicate the time of day it should be taken.
All your patients have to do is puncture the backing on the compartments to access their medications. For those with dexterity issues or arthritis, many backings are perforated.
Blister packs reduce the risk of medication errors and reinforce prescribed medication regimens. They also reduce the likelihood of patients double dosing, missing a dose, or taking the wrong dose.
If you want to go further, you can invest in smart blister packaging like the Med-ic ® Electronic Compliance Monitor (ECM). It monitors patients’ adherence by tracking when they open each dose. That way, they stay on track with their medications.
Along with blister packs, you can improve convenience by offering delivery service. Studies show that home delivery increases patients’ adherence, especially for those with chronic conditions.
Your patients who have a hard time swallowing pills aren’t alone. Nearly 40 percent of people struggle to get their medications down, which causes adherence issues. Patients may delay taking their medication. They might skip the dose or even quit taking the medication all together.
Help your patients swallow their pills and continue taking their meds as directed with these tactics:
• Teach them proper head posture
• Stock products to aid swallowing
• Explain the pill-taking process
• Teach breathing exercises
• Suggest placing pills in tasty treats
Patients stop taking medications for numerous reasons. Whether they’re tired of taking them, don’t like side effects, or just can’t remember to take them, educating them will help solve any issues they may have.
First, make sure your patients understand how to take their pills as directed. ABM and MTM are effective for this type of counseling. Then, make sure patients understand the health consequences of missing doses.
If you haven’t already, make information on diabetes, high cholesterol, and hypertension readily available. You might even consider offering wellness classes for further education or sending patient education videos through text message. Your patients will then have access to information about their prescriptions available on demand.
The health benefits of the drug outweigh the side effects, so remind your patients why they’re taking the medication. If they still have concerns about the risks, encourage them to speak with their physician.
More and more online and mail-order pharmacies keep popping up. Because of that, delivery options have become more of an expectation for patients. But without that convenience, patients are more likely to become non-adherent because getting their medications is more of a hassle.
“It’s time to make some changes,” Mitchell said. “If you’re not sure what to do, reach out to a colleague or a consulting company. Reach out to whomever can help you move forward. Don’t sit around and wait for things to change. Make those changes now. It’s important that we take pharmacy back into our hands.”
With
Multiple presentations from top manufacturers.
Aligned with manufacturers' estimated shipping commitments.
SAFETY CONFIDENCE
Dependable deliveries to meet your patients' needs.
Guaranteed Channel Integrity® ensures safe, reliable products for your patients.

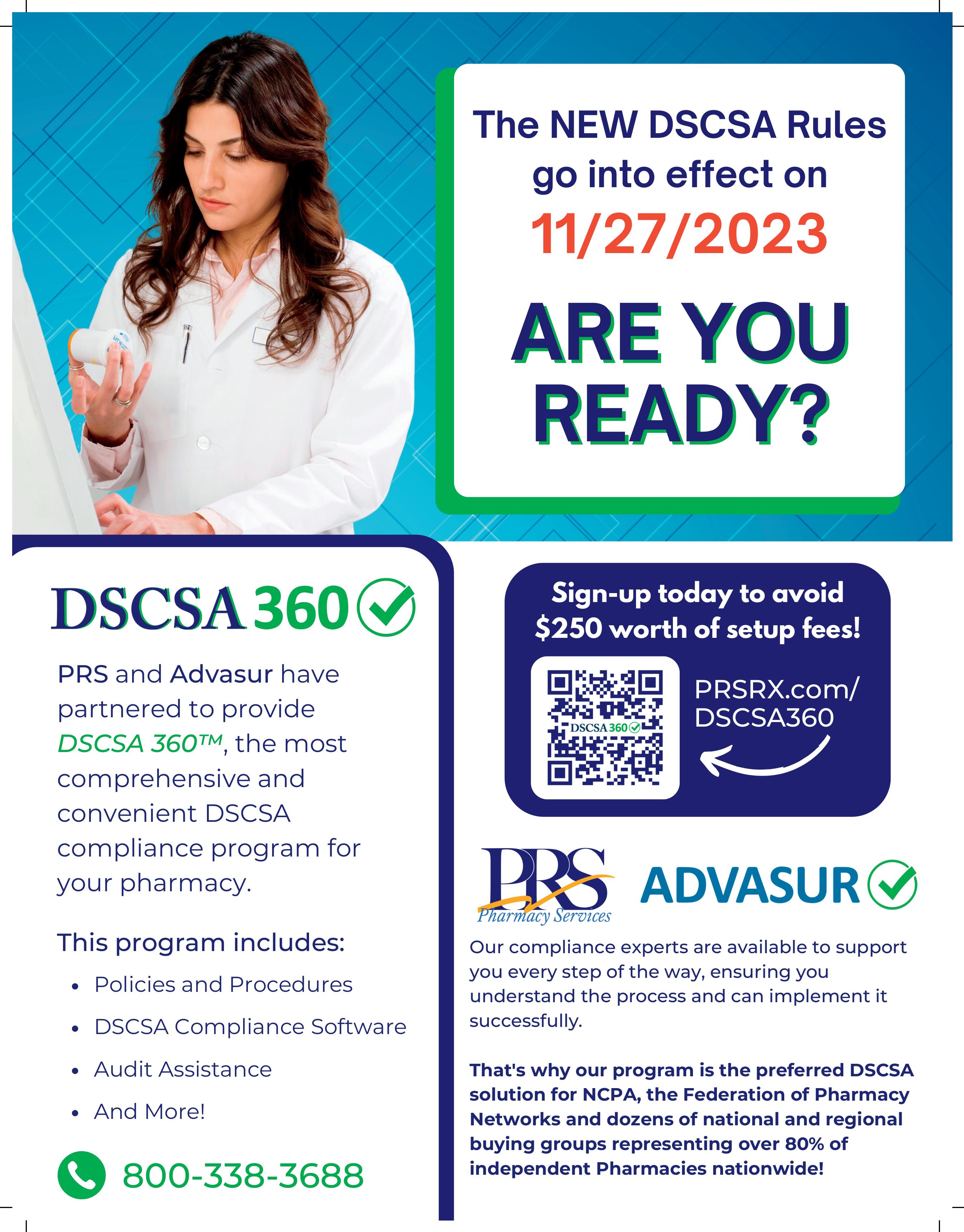
Will you be ready by November 27?
The final deadline for the Drug Supply Chain Security Act (DSCSA) is fast approaching, and for those who are wondering, the DSCSA plan is in place. Any changes from this point on will be minuscule.
The purpose of the DSCSA is to protect patients from illegitimate prescription drugs by enabling a safe, secure flow of data along the pharmaceutical supply chain. And according to the FDA, the deadline of November 27, 2023 is firm.

Still scrambling to get everything checked off the list? The time to get it done is now. The threat of counterfeit drugs making their way into the U.S. supply chain is heightening. This happens when companies operate outside of legitimate drug distribution channels, such as the gray market. Add to that the ease of purchasing drugs illegally from fake, online pharmacies. And with the immediate availability of these drugs, consumers think they’re safe. But they’re not. These drugs are unauthorized and can be fatal.
With more and more counterfeit drugs sneaking into the market, the first phase of the DSCSA was introduced by the FDA in 2013. Two years later, Congress signed the act requiring products to be traceable at the lot level with the intent of increasing visibility in the pharma supply chain. While it accelerated the move toward digitizing the drug supply chain, it wasn’t enough.
Between 2014 and 2019, cases of drug counterfeiting doubled in size. That same year, there was a record high of drug-induced seizures in North America derived from illegal pharmaceuticals. This is why more action is needed to allay these counterfeit drugs from reaching patients.
The deadline will be here before you know it, so it’s important to make sure you’re fully prepared. To ease your nerves, here is a checklist listing every DSCSA requirement to ensure you’ll be ready and confident on November 27.
1. Verify that all trading partners are licensed and registered:
• Check that they have a valid license and are registered per federal and state law. Have protocols in place or routine verification for all new trading partners and regularly audit current trading partners.
2. Identify and report suspect products that may be illegitimate. Have procedures in place to:
• Identify suspect product currently in inventory and among new products
• Inform trading partners about suspect products
• Quarantine suspect products
• Remove illegitimate products from supply chain
• Notify your upstream supplier promptly
3. Accept and maintain transaction data:
• Only accept products if the previous owner provides the transaction information, transaction history, and transaction statement (“3Ts”)
• Maintain the “3Ts” for six years from the date of the transaction
• Provide the “3Ts” to the subsequent owner (unless the subsequent owner is a patient) when selling or loaning products
4. Only accept products with the proper identifier. A product identifier is a standardized graphic that includes:
• The product’s standardized numerical identifier (the NDC and a unique alphanumeric serial number)
• Lot number
• Expiration date
Exempt products include:
• Blood or blood components intended for transfusion
• Certain radioactive drugs or radioactive biological products
• Imaging drugs
• Certain intravenous products
• Any medical gas
• Homeopathic drugs
• Drugs compounded in compliance with sections 503a or 503b of the FD&C Act
If you want to be ready by November, continuously evaluate and update your standard operating procedures (SOPs) to ensure compliance with changing DSCSA requirements. Stay proactive by identifying any gaps or areas for improvement in your processes, and implement necessary changes accordingly. It’s work, but it will safeguard your patients from counterfeit and possibly deadly drugs.
• Looks different than the product on the shelf
• Altered product information
• No “Rx only” symbol
• Missing information on the label
• Bubbling on the label
• Lot numbers or expiration dates do not match the outer/inner container
• Foreign language
• Open package
• Damaged or broken seal
• Missing or wrong package inserts
• Different product name than FDA-approved version
Owning a community pharmacy is much more than just filling medications. It involves numerous tasks throughout each day that keep you and your technicians on your toes, such as inventory management.
Inventory doesn’t always match up with the demand of your customers. This leads to stranded products on the shelves, and most are beyond your control. Some patients may need to switch the strength or dose of their maintenance medications over time. Or there may be managed-care issues causing a PBM to switch from one covered drug to another. A simpler cause may be that a manufacturer’s packaging leaves you with unused products.
Whatever the reason, you’ll need to decrease the quantity of unsalable products that are in your inventory with a third party in order to return the expired products to your manufacturer or wholesaler for credit. The least costly approach is to return the unsold products, near or after their expiration date, every quarter. And if the product is in its original container, it may be eligible for credit as long as it’s properly returned in a timely manner.
Products that may be eligible for credit:
• Unopened products that are sealed in original manufacture packaging
• Some manufacturer policies (mostly branded products) allow opened containers or “partials” as eligible products
Products that are not eligible for credit:
• Injectables, ampules, and cartridges
• Damaged products
• Partial products whose packaging has been opened with some of the pills or packaged contents dispensed
• Products not in original packaging or have been repackaged
• Products not in their original manufacturer container (e.g. re-packs or medication that’s been placed in a prescription vial)
• Products too far past their expiration date (eligibility periods for returns range from 3 to 12 months after product expiration)
• Products too far within their expiration date as deemed by manufacturer policy (i.e. expiration is too far in the future)
• Products sold by manufacturer as nonreturnable
• Products with a non-returnable lot number
• Products that are a sample or complimentary item
• Products purchased from unauthorized distributers
When handling returns, identify your unsalable pharmaceutical products by looking at the products on the shelves, in the vault, and in the refrigerator. Inspect them carefully and check expiration dates. This should be done quarterly.
Partially dispensed products or those with the most recent expiration dates should be arranged at the front of the shelf. You can also use color-coded tags. They work well and make it easy to recognize a product’s expiration date.
Separate the products to send to the returns company into groups (short-dated, expired, or recalled products) for return processing. Then, check out each company’s web portal for a workflow on how to create an inventory of products and the steps to prep and ship products back to their warehouse. If you’re really lucky, they’ll provide onsite resources to process the returns on your behalf.
The whole process sounds like a lot of work for pharmacies, and to be honest, it is. That’s why pharmacy returns companies exist. They can help navigate the challenges of returning drugs for credit and help you get the most out of your pharmacy’s expired products.

“I would say that most pharmacies don’t have the manpower to do their returns themselves,” said Adrienne Vandergriff, Vice President, Sales & Marketing at Return Solutions.
Here are some things to ask before you decide:
1. Is the company reputable?
2. Do they have recommendations or partnerships with industry leaders you trust?
3. Do they require you to sign a contract, or can you end the service at any time?
4. Does the company understand environmental, legal, and economic ramifications of drug returns?
5. Is the company trustworthy?
6. Does the company have the industry relationships necessary to get you the most for your returns?
7. Will the company give you the value you deserve for the price you want to pay?
“It’s a lot of work on a pharmacy’s part. They would have to find out where to send each product for each manufacturer, though a lot of them have processors that you submit to. So, pharmacies would have to ship product to each manufacturer individually.”
It can also be difficult to determine if a manufacturer will issue a credit for a product if you don’t have the manufacturer policy.
“A lot of times, they won’t even accept returns from an individual pharmacy,” said Vandergriff. “It has to go through a third party.”
If you can, avoid unsalable returns at all costs. When you have an open container of generic medication, fill as many scripts as you can before unsealing a new one. Partial generics may not be eligible for credit. Also, stay on top of prescriptions that are not picked up by customers. Return an unclaimed drug to its original container if your state’s pharmacy regulations allow it.
You can regain losses by minimizing returns wherever you can by keeping up with your pharmacy inventory management. If the process is too time consuming, consider partnering with a pharmaceutical returns company. That way, you’ll sleep well at night knowing that the right products are returned, properly disposed of, and credited in a timely manner.
Pharmacies typically have two options for returning expired drugs when they’re working with a returns company: mail-in or on-site service.

Expired drugs are removed from the shelves by your staff. Then, they inventory them online and ship them to the returns company.
This option is usually less costly, but you have to pull the expired drugs from your stock yourself. It’s not an easy job, and it’s easy to miss some of the expired products. This means there will be some expired bottles left on your shelves. By the time you find them, they’re too old to return for credit.
“Our mail-in service is located on our website, drugreturns.com,” Vandergriff said. “Customers can create returns, inventory items, and print the necessary forms and prepaid UPS shipping labels on their own schedule.”
A representative from a returns company visits your pharmacy and scans your prescription shelves. They look at the expiration date on each product and remove those that are expired. Then, they inventory them and arrange for them to be picked up by a common carrier the following business day.
This option is a bit more expensive, but it saves your staff time so they can keep helping customers or take care of other tasks in your pharmacy.

The over-the-counter hearing aid Clinical Service is designed specifically to benefit pharmacies. This is an exclusive program by Soundwave Hearing.
Earn additional profit while furthering Point of Care Testing in your pharmacy, as a trusted health provider with a 45-day, riskfree money back guarantee for both you and your customers.
Soundwave's otoTune® Assistant is the only patented 2-button hearing test that tests both ears simultaneously, delivering quick, accurate results. The test has been clinically validated at Northwestern University Audiology Clinic and is comparable to an audiogram.
Purchase the otoTune Assistant.


Receive Free: A Poster For Your Store Window
An Acrylic Box With Visual Sontro Hearing Aids
50 Bag Stuffers/ 50 Patient Brochures
2 Counter Cards

For many years, independent pharmacists like you have been duped by PBMs. The good news is things are turning around.
Changes to how your direct and indirect remuneration (DIR) fees are collected will take place next year on January 1, 2024. The Centers for Medicare and Medicaid Services (CMS) announced that significant reforms will be implemented to the DIR program.
These changes are intended to reduce the financial burden on independent pharmacies as well as to increase transparency in the pharmacy benefit management (PBM) industry. However, the process of getting there may have some ups and downs in terms of cash flow.


DIR fees are retroactive, and they aren’t applied at the time of sale because they’re backdated. Because DIR fees are calculated on various factors, you don’t always learn how much you owe in fees until months later, after you’ve dispensed a drug. This is a concern since it can have a consequential impact on cash flow. For instance, some pharmacies may owe more in DIR fees than they earned from dispensing the drug in question. This makes it a struggle to plan and manage your finances. They’re dealt with weeks or months after the prescriptions are filled. This means you may take a loss and not even recoup the dispensing cost.
The good news is the new rule does come with benefits for independent pharmacies, such as:
Fewer Financial Worries: The new DIR changes will reduce your financial stress. Right now, PBMs can charge DIR fees for various reasons (e.g. drug utilization reviews, medication therapy management, and performance metrics), and the fees can be tough for you to budget for. With the new changes, the types of fees that can be charged will be limited and PBMs will be required to provide more clarity around those fees.
Increased Clarity: Providing more detailed information about the fees they charge will be a requirement for PBMs. This includes the amounts they charged and why they charged them.
Decent Reimbursements: Right now, DIR fees can be charged after the fact. This means you may not know the final reimbursement amount for a prescription until months after it’s been filled. With the new changes, however, that will change. PBMs will be required to provide timely and accurate reimbursement rates. This will make it easier for you to manage your cash flow.
Not only will you benefit from the new rule, but so will your patients. Patients will have reduced out-of-pocket costs, thanks to the final rule moving all pharmacy price adjustments to the point of sale so patients will have lower cost sharing.
Now for the not-so-good news with the new rule:
PBMs are not eliminated from the use of DIR fees. PBMs will still be able to use DIR fees to extract arbitrary fees. This, along with extracting other unreasonable compensations from pharmacies.
The impact on pharmacy cash flow is not addressed. The final rule states that changes in cash flow could possibly cause some struggling pharmacies to decrease services or medication availability as well as have to close their doors for good, thus impacting pharmacy networks. What CMS fails to address is the transition period for pharmacies from calendar year 2023 to 2024. It also states that pharmacies will receive the “lowest possible reimbursement” in 2024 while PBMs continue collecting pharmacy DIR fees from 2023. This could create major cash flow issues for pharmacies during the transition.
Other PBM loopholes haven’t been closed. This means PBMs can still continue other harmful business practices, such as negative reimbursements, and refund the pharmacy less than it costs to acquire the drug.
As the new changes are implemented, there may be some uncertainty. Don’t be surprised if there are delays and confusion as the changes are implemented, as PBMs may also struggle to adapt to the new rules and requirements.
Be aware that with changes comes risks. Unfortunately, it can’t be avoided. With the DIR changes, competition may decrease in the PBM industry. This could result in higher prices for consumers and a decrease in access to care.
There may also be a bit of chaos when it comes to cash flow. You’ll double the amount of DIR fees you normally would during the first part of 2024. This is because you’ll have the retroactive DIRs from 2023 and the new DIRs that’ll occur at the point of sale.
If you’d like to further prepare for the new changes, keep up with the latest news and developments on DIR changes and have a solid financial plan ready. Put aside cash as a contingency; increase your profit margins; figure out how to offset fees; and initiate additional revenue streams, such as nutraceutical packs or CBD products. These are among the best cash-based revenue streams.
Understanding and preparing for these changes now will ensure that you’re well-positioned for any and all challenges that come your way.




