TRANSFORMING HEALTH CARE

TGH IS AT THE FOREFRONT OF MEDICAL INNOVATIONS













A Hall of Famer beats cancer, with help from a serendipitous
THE EARLIER THE BETTER Dr. Jorge Marcet has changed how we think about colorectal surgery, plus insight into the importance of early colon cancer
TAKING OUT OVARIAN CANCER
Hyperthermic intraperitoneal chemotherapy is a new frontier in the treatment of abdominal cancers 50 SECOND CHANCE
An emergency transfer to TGH saved a COVID-19 patient
54 BEND THE KNEE
The VELYS Robotic-Assisted Solution for total knee replacement aids in precision, reduces post-operative pain, and improves outcomes
56 A SIMPLER SOLUTION
Women suffering from stress urinary incontinence are finding a new lease on life with Bulkamid
60 PART OF THE FAMILY
Supporting those who make a difference day in and day out at TGH is a personal mission for Patsy and Gene McNichols

ON THE COVER: Focused ultrasound is an innovative, noninvasive procedure for people suffering from essential tremor.


Phillip S. Dingle, Chairman of the Board Marylou Y. Bailey
Jeffrey W. Bak Thomas L. Bernasek, M.D.
1 Tampa General Circle Tampa, FL 33606 813.844.7000 • TGH.org
BOARD OF DIRECTORS
Kim Bruce
Raviender Bukkapatnam, M.D. Ken Burdick
Blake J. Casper Gregory J. Celestan
Drew Graham Patricia Jurinski Les Muma Corey Neil
EXECUTIVE LEADERSHIP TEAM
Scott Arnold, Executive Vice President & Chief Information Officer
Stacey Brandt, Executive Vice President & Chief Strategy and Marketing Officer
Kelly Cullen, Executive Vice President & Chief Operating Officer
Jennifer Crabtree, Chief of Staff, Office of President & CEO
Robin DeLaVergne, Senior Vice President, External Affairs
Peggy Duggan, M.D., Executive Vice President & Chief Medical Officer
Murray Shames, M.D. John T. Touchton, Jr. Bruce Zwiebel, M.D.
Rachel Feinman, Vice President of Innovation & Managing Director, TGH Innoventures
Qualenta Kivett, Executive Vice President, Chief People and Talent Officer
Jim Kennedy, General Counsel
Charles J. Lockwood, M.D., Executive Vice President, Chief Academic Officer, Tampa General Hospital; Executive Vice President, USF Health, Dean, USF Health Morsani College of Medicine
Frann M. Leppla, Senior Vice President & Chief Development Officer, TGH Foundation
Mark Runyon, Executive Vice President & Chief Financial Officer
Abe Schwarzberg, M.D., Senior Vice President, Network Development; Chief of TGH Cancer Institute
Steve Short, Senior Vice President, Tampa General Provider Network Operations
Adam Smith, Executive Vice President & Chief Ambulatory Care Officer
SHARED PURPOSE
We heal. We teach. We innovate. Care for everyone. Every day.
VISION
We will become the safest and most innovative academic health system in America.






















THE ACADEMIC DIFFERENCE
Publisher Terry Duffy
Director of Sales Deidre Wade
Associate Publisher Dina Turner
Editorial Director Daphne Nikolopoulos Editor Mary Murray Creative Director Olga M. Gustine Art Director Ashley Meyer
CONTRIBUTING EDITORS
Stacey Brandt, Lisa Greene, Jennifer McVan, Laurie Slater, Tom Zebold
CONTRIBUTING WRITERS
Paige Bowers, Chris Curtland, Judy DiEdwardo, Karen Feldman, Sandra Gurvis, Yvette C. Hammett, Kelley Marcellus, K.S. Meyer, Dave Scheiber, Liza Grant Smith
CONTRIBUTING PHOTOGRAPHERS
Alissa Dragun, Cara DeHart Lewis, Emily Panakos, Jerry Rabinowitz, Daniel Wallace
ADVERTISING
Publisher, Naples Meegan Wyatt Account Managers Kathleen Beuttel, Kathy Breen, Tanya Lorigan, Melissa Zolin Schwartz Advertising Services Coordinator Elizabeth Hackney Marketing Manager Rebecca Desir
PRODUCTION
Production Director Selene M. Ceballo Production Manager Lourdes Linares Digital Pre-Press Specialist George Davis Advertising Design Coordinators Anaely J. Perez Vargas, Jeffrey Rey Production Coordinator Ileana Caban Digital Production Coordinator Tyler Sansone
OPER ATIONS
Chief Operating Officer Todd Schmidt Accounting Specialist Mary Beth Cook Accounts Receivable Specialist Ana Coronel Distribution Manager Judy Heflin Logistics Manager Omar Morales Circulation Manager Marjorie Leiva Circulation Assistant Britney Stinson Circulation Promotions Manager David Supple IT Manager Keith Gonzalez
In Memoriam Ronald J. Woods (1935-2013)
HOUR MEDIA, LLC
CEO Stefan Wanczyk President John Balardo
Published by Palm Beach Media Group North P.O. Box 3344, Palm Beach, FL 33480 Telephone: 561.659.0210
Fax: 561.659.1736 www.palmbeachmedia.com
Copyright 2023 Palm Beach Media Group North Inc. All rights reserved.
CLINICAL BREAKTHROUGHS, BETTER RESULTS DRIVEN BY ACADEMIC MEDICINE





TAMPA GENERAL HOSPITAL AND USF HEALTH MORSANI COLLEGE OF MEDICINE ARE DRIVING INNOVATION. EVERY DAY.


Together for more than 50 years, our team of world-renowned experts, including scientists, doctors, and pioneers in the medical field perform more advanced procedures and deliver world-class results. Through our focus on research, innovative treatments and clinical trials, TGH provides patients with lifesaving medical breakthroughs. This is how we define medicine.
Florida’s Leading Academic Medical Center For Over 50 Years



ATRIPLE CROWN
Tampa General Hospital receives a trio of awards that honor CARE, PERFORMANCE, EDUCATION, and EQUALITY
BY SANDRA GURVISThis has been a banner year for Tampa General Hospital. Not only did TGH garner U.S. News & World Report’s No. 1 Best Hospital ranking in Tampa Bay and No. 3 in Florida for 2022-2023, but it was the only major teaching hospital in Florida to be named to the 2022 Fortune/Merative (formerly IBM Watson Health) 100 Top Hospitals list. As part of this recognition, TGH was among only 25 hospitals in the United States to receive the Everest Award, which honors both the highest current performance and the fastest long-term improvement. Last but not least, Forbes magazine designated TGH the No. 1 Best Employer for Women in the United States.
Advances recently sat down with TGH President and CEO John Couris to discuss what these honors mean and their impact on patients and staff.
Can you tell us more about each award and what it signifies?
This kind of recognition year after year is really a testament to the unwavering dedication and ongoing commitment by our entire team to deliver world-class care day after day. Tampa General’s rankings are a reflection of our process of aligning innovation and advanced research to improve the health and well-being of our patients. This collection of awards represents that we are operating on the level of the best institutions in the country by every measure and across the organization.
The U.S. News & World Report’s Top Hospitals recognition, which we have received for the past seven years, is one of the most widely known hospital ranking systems among patients and consumers across the country. It ranks our performance and that of 4,500 hospitals nationwide in 15 specialties and 20 procedures and conditions. This year, Tampa General is ranked as one of the nation’s top 50 hospitals in seven medical specialties, including ear, nose, and throat; diabetes and endocrinology; and obstetrics and gynecology, where TGH ranks No. 1 in Florida. TGH also ranks as “high performing,” or among the top 10 percent of U.S. hospitals, in five additional specialties.
The U.S. News & World Report ranking is one of the most comprehensive in terms of the information it gathers to determine both our overall ranking and that of our ranking in a specific specialty.
Many of the metrics considered by U.S. News & World Report contributed to our designation as a model of excellence by Fortune/Merative. As Tampa General is the primary teaching hospital of the outstanding USF Health Morsani College of Medicine at the University of South Florida, medical education and research play a critically significant role in our operation as an academic medical center, and they were key factors in receiving this recognition. As an academic medical center, our focus on research and medical education enhances our ability to develop and provide the most innovative treatments and therapies, while training the next generation of doctors, nurses, and specialists.
A key component in this designation is our focus on community health and how we provide medical services, preventative care, and education to our community. Tampa General is the safety net hospital for the region—caring for everyone regardless of their ability to pay—and is committed to enhancing the quality of health care while making it more accessible and affordable to everyone. We are incredibly proud of this recognition, as it not only reflects our commitment to patient safety, experience, and clinical outcomes, but also emphasizes Tampa General’s focus on designing the future of health care and enhancing health care quality and lowering costs.
The other Forbes award highlights our commitment to diversity and inclusion for all those who walk through our doors—regardless of gender, race, or sexual orientation—and to advancing women at all levels of our organization. Among other things, the award also reflects the atmosphere that TGH has worked hard to develop—one that supports women and families, promotes flexibility, and champions pay equity.
While this recognition showcases our commitment to the support we specifically provide to women, it also speaks to our priority to understand
TAMPA GENERAL’S RANKINGS ARE A REFLECTION OF OUR PROCESS OF ALIGNING INNOVATION AND ADVANCED RESEARCH TO IMPROVE THE HEALTH AND WELL-BEING OF OUR PATIENTS.”

what all our team members need and what is important to them in their lives so that, in return, we can provide support in ways that are most impactful to them. We know that our commitment to fairness and equity will continue to lead to a diverse workforce and drive the best possible patient outcomes.
Why should these awards matter to patients?
These awards showcase the hard work of the team and are designed to assist patients and their doctors in making informed decisions about where to receive quality health care, no matter how challenging the condition. These awards are an indication of value. As a consumer of health care, you want to go to a trusted resource and know how the care you are considering stacks up against others in the market. The recognition also signals to patients that they don’t need to leave the state of Florida when they can get the same or even better treatment at TGH.
What do they mean for team members?
In a high-performing organization, three things come into play: culture, the people themselves, and the ability to execute strategy and vision. In order to accomplish this, we need to understand what our team members require so we can provide them with meaningful and ongoing support. The Forbes recognition reinforces the efforts behind this work and helps us attract and retain the most outstanding people.
Is there a “secret sauce” behind TGH’s success as it relates to these awards?
A few years ago, we set the goal of being the safest and most innovative academic health system in America. These awards recognize and measure our efforts in terms of providing cuttingedge patient care, innovative procedures and treatments, the highest level of training, gamechanging research, and top-level academics. I like to say while other hospitals practice medicine, at Tampa General, we help define it.
Breaking
BARRIERS
THE NEW HISPANIC KIDNEY TRANSPLANT PROGRAM BRINGS VITAL CARE TO ONE OF THE COUNTRY’S LARGEST DEMOGRAPHICS
BY YVETTE C. HAMMETTA
Tampa General Hospital launched its Hispanic Kidney Transplant Program in March 2022 to ensure TGH is providing equitable access to transplants for all patients with end-stage kidney disease in our community.
“We are continuously focused on providing care to all members of our community regardless of race, gender, socioeconomic status, primary language, or disability,” stated Dr. Kiran Dhanireddy, vice president and chief of the TGH Transplant Institute. “Creation of specialized programs such as the Hispanic Kidney Transplant Program allows us to serve all our patients equitably.”

The Hispanic population grew to 62 million in 2020, according to the U.S. Census Bureau, and is the second-largest ethnic group in the nation. And while Hispanics are 1.3 times more likely to experience kidney failure compared with non-white Americans, per the National Kidney Foundation, statistics indicate that too few Hispanics receive transplants. In Florida, 26 percent of the population is Hispanic. However, only 18 percent of those on the kidney transplant waiting list in the state are Hispanic. As one of the largest kidney transplant programs in the country, performing 350 kidney transplants a year, TGH’s mission is to ensure every population has access to this lifesaving procedure.
Numerous variables could account for the disparity, said Dr. Luis Beltran, a nephrologist and expert in kidney and pancreas transplants who runs TGH’s Hispanic Kidney Transplant Program. Some of these
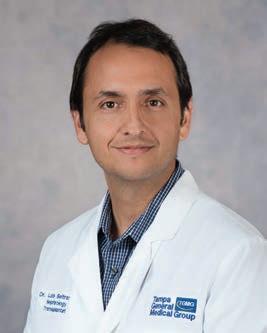

reasons include less access to health care and information on how to get on the list for a kidney transplant, how to navigate the financial and medical aspects, and the need for a good support system. As a result, the new TGH program focuses on outreach and cultural sensitivity, with the goal of bringing more awareness to the procedure.
“We understand values, principles, behaviors, and [the] structure policy that allows us to be able to work efficiently,” Beltran said. “What we want to accomplish is to have more extensive education materials, institutional support, and a path for optimum communication. We understand how the culture behaves, and that allows us to be able to deliver a competent program. When you have kidney failure, transplantation is a big burden, not just for the patient but the family, so we want to have the involvement of the families.”
These efforts go far beyond having team members who speak Spanish, Beltran noted, though that is vital. Communication with patients includes getting them the information they need to understand the process and a care coordinator who can lead them every step of the way.

TGH’s process begins with patients and their caregivers attending a Spanish-speaking roundtable, where they can learn more about the deceased donor and living donor kidney transplantation process from transplant nephrologists, coordinators, social workers, and financial
counselors. This dedicated Spanish-speaking team will guide the patient through every step of the process.
From outreach to consultation, surgery, and follow-up care, TGH’s Hispanic Kidney Transplant Program offers a clear, culturally sensitive path forward for Hispanics in the Tampa Bay area and across the state. And for Beltran, this program is close to his heart. “I feel very passionate about this, and having the backing of Tampa General Hospital finally doing this is very important.”
WE ARE CONTINUOUSLY FOCUSED ON PROVIDING CARE TO ALL MEMBERS OF OUR COMMUNITY REGARDLESS OF RACE, GENDER, SOCIOECONOMIC STATUS, PRIMARY LANGUAGE, OR DISABILITY.”
—DR. KIRAN DHANIREDDY


Follow-up CARE
A CHANCE REUNION ILLUSTRATES THE ENDURING VALUE OF HAVING A DOCTOR YOU CAN TRUST
BY KELLEY MARCELLUSWhen Rhonda Kallman appeared as the keynote speaker for the Tampa Bay Chamber’s sixteenth annual Women of Influence luncheon in April 2022, she didn’t expect to be reunited with a woman who’d had a profound influence on her.

Speaking to 560 attendees at the event, Kallman recounted her remarkable career. She is the founder and chief executive officer of Boston Harbor Distillery, that city’s premier distillery making wholegrain whiskeys. Before that, at age 24, Kallman broke into the maledominated beer industry by co-founding the Boston Beer Co., which brews Samuel Adams and other craft beers. She also touched upon her experience with breast cancer.
Kallman sat at a table of 12 high-profile attendees, including Tampa Mayor Jane Castor, Tampa Bay Chamber President and CEO Bob
Rohrlack, and executives from Tampa General Hospital, which was a sponsor of the luncheon. One of those TGH representatives was Dr. Peggy Duggan, the hospital’s executive vice president and chief medical officer. As it so happened, Duggan and Kallman had a history: Duggan had operated on Kallman 14 years ago at Brigham and Women’s Faulkner Hospital in Boston, when Kallman was being treated for Stage 3 breast cancer.
“I didn’t recognize her at first,” Kallman said of Duggan.


Duggan, however, thought the speaker seemed familiar and racked her brain for how they knew each other, aware that they were both from the same area.
At the end of the event, Duggan approached Kallman. Once they put two and two together, they embraced and cried over their shared experience.
“I’m not a crier, but every time I think of her, I tear up,” Kallman said.
Kallman was just 48 and the mother to three young children when she was diagnosed. She initially consulted another surgeon, who explained the grim reality of how a unilateral left-side mastectomy would change her body, leaving her alone in the exam room with post-surgical photographs. Traumatized, Kallman discussed the appointment with her Dana-Farber Cancer Institute oncologist, who immediately said she needed a different surgeon and referred Kallman to Duggan.
“Dr. Duggan was like a godsend to me,” Kallman said.
The treatment plan was complex, involving a mastectomy and reconstruction using Kallman’s own muscle. After the initial surgery, tests came back showing that the cancer had spread to the lymph nodes and would require another procedure.
Duggan remembered Kallman as an “incredible human being,” whom she described as bubbly, upbeat, very funny, and delightful.

“She wanted ‘care’ with a capital C,” Duggan added. “I think what most people want from their doctor is to be cared for and safe.”
When she went in for the follow-up surgery, Kallman remembered that Duggan leaned in as they discussed the details and let her know that this was the first time she’d be performing this particular surgery.
“I looked at her and said, ‘You’re going to be just fine,’” Kallman said with a chuckle, amused with the irony of a patient reassuring a doctor. “I think that really speaks to the strength of two women being in something together, something we would never forget. I had unfailing confidence in my medical team.”
And that, Kallman said, is the key to tackling medical situations: finding someone with whom you have a connection and who will provide the care that is right for you. “Some-
times your life will depend on it.”
Duggan agreed, adding that taking care of a patient is one of the greatest honors you have as a doctor, especially as a surgeon.
“Women are very intelligent consumers of medicine,” she said. “They value being met where they are, being heard, and being able to trust. They need to have access to call and ask a question when they’re struggling. They have to believe that you are going to do what you say you are going to do.”
That philosophy, Kallman said, is why Florida residents are lucky to have Duggan at the helm of TGH.
“Dr. Duggan is going to hold the members of her team responsible for being patient advocates,” Kallman said. “Dr. Duggan walks her talk, and I think that will help other doctors at Tampa General be the best that they can be.”


The duo has no intention of this chance encounter being the end of their story. Kallman plans to share a meal with Duggan when she’s in town. As for Duggan, when she heads home to Boston for a visit, she said, “I’m going to her distillery for a tour.”

























PART No Small




The TGH Parathyroid & Thyroid Institute


offers expertise found nowhere else





 BY YVETTE C. HAMMETT
BY YVETTE C. HAMMETT
Four glands the size of rice grains regulate the amount of calcium the body needs for optimal function. Parathyroid glands are sensing receptors that can sometimes become benign tumors. Patients can experience feeling tired, hair loss, lack of sleep, sweating, and excessive urination, among other symptoms.
“They are a calcium-sensing receptor,” said Dr. José Lopez, who runs the Tampa General Hospital Parathyroid & Thyroid Institute along-



side Dr. Douglas Politz. “Throughout the day, they sense where your calcium levels are. Most adults have calcium levels in the 9s.”
Lopez explained that problems within the parathyroid often start with a benign tumor. “That receptor that regulates calcium fails. Too much calcium is getting released, leading to excess calcium in the bloodstream,” which can lead to bone loss and cause kidney stones to develop, as well as renal insufficiency.
Furthermore, about 30 percent of patients experiencing parathyroid issues also have a thyroid problem.
Most people likely have not even heard of the parathyroid glands, which are part of the endocrine system and located in the neck behind the thyroid. Because of their small size, having an expert surgeon perform the necessary operation to correct the problem is of the utmost importance.
Lopez and Politz are two of the foremost parathyroid surgeons in the world. They previously had their own private practice before co-founding the TGH Parathyroid & Thyroid Institute. In addition to the 20 or so operations they perform on parathyroid glands each week, Lopez noted that they are constantly working with patients to “correct” issues left behind by less experienced surgeons.
Doing nothing to correct the problem of tumors of the parathyroid can lead to an increased risk of breast, colon, and prostate cancer and can decrease life expectancy by about five years, Lopez said. “There is no medical treatment, only surgery.”

This operation was first performed 100 years ago and required days of recovery in the hospital. Today, Lopez and Politz can complete the outpatient surgery in about half an hour, with the patient leaving within a couple of hours. “They have a small BandAid on their neck they can remove themselves,” said Lopez.
The majority of a patient’s symptoms will begin improving within two weeks to two months. “Once you have removed the tumor, these receptors start working again,” Lopez said. “If you were developing kidney stones, that usually stops. If you were having problems with [heart] arrhythmia, you may revert back to normal sinus rhythm.”
Of the four parathyroid glands, up to three and a half can be removed, meaning a patient only needs half of one parathyroid gland to regulate calcium in the body. The key is hav-
ing a surgeon who is an expert in dealing with these very tiny glands, because “once the rice grains are gone, that’s it,” Lopez said. Knowing how to remove them without injuring those that will remain is vastly important. “Right now, we perform up to 20 surgeries a week which equates to about 800 a year. That is expert care you can trust.”
Madeleine Savoie traveled from North Palm Beach to TGH to have her parathyroid surgery and said she could not be more pleased with the results.
“I rave about Dr. Lopez,” Savoie said. “He is the most wonderful human being I ever met. I [had] so many tests and was encouraged to go to Tampa General Hospital,” because of its advanced center for parathyroid surgery. “I will recommend them to everyone I know. I was getting too much calcium and getting a lot of kidney stones. I still have some, but they don’t bother me. My surgery was done in March, and I have had no ill effects.”


Back in the summer of 2021, Line Mari Kristiansen said she had “pain everywhere” and trouble walking before traveling from Norway all the way to Tampa for parathyroid surgery. Thanks to the expert care provided by TGH, Kristiansen said she felt a difference immediately after surgery and then enjoyed a few walks on Pinellas County beaches before heading back to Norway.
“Fantastic, it’s like you couldn’t believe it before you experience it,” said Kristiansen in a Spectrum Bay News 9 report. “It’s like going from a lot of pain to like no pain. It’s like incredible.”
Both Lopez and Politz were called to pursue medicine in childhood, in part inspired by supporting ill family members in times of need; Lopez helped to care for two cousins with cerebral palsy, and Politz donated a kidney to his younger brother. Together, they have a combined 25 years of professional experience, resulting in superior surgical skills that are matched only by their compassion for their patients.
RIGHT NOW, WE PERFORM UP TO 20 SURGERIES A WEEK WHICH EQUATES TO ABOUT 800 A YEAR. THAT IS EXPERT CARE YOU CAN TRUST.”
—DR. JOSÉ LOPEZFrom top: Dr. Douglas Politz and Dr. José Lopez run the Tampa General Hospital Parathyroid & Thyroid Institute, which is part of the Ear, Nose & Throat Institute.

TOP 50 IN THE NATION FOR ORTHOPAEDIC SURGERY
ONCE AGAIN, U.S. NEWS & WORLD REPORT NAMED TAMPA GENERAL HOSPITAL
ONE OF THE NATION’S BEST FOR ORTHOPAEDIC
SURGERY.
Tampa General’s Orthopaedic Institute is the most complex orthopaedic surgery program in Florida. From minimally invasive robotic treatments for joint replacement to some of the most complex cases in the state, our team of specialists performs more procedures, has more expertise and delivers superior outcomes. And as one of the nation’s best for rehabilitation, our comprehensive expertise is with you every step of the way.
























SETTING THE STANDARD
Palm Beach Media Group is a renowned publishing company with print publications representing a mix of proprietary titles and custom magazines, along with digital solutions, serving the entire state of Florida and more.
TAMING TREMORS



HOW ONE PATIENT REGAINED CONTROL OF HIS LIFE WITH THE HELP OF TGH AND NONSURGICAL FOCUSED ULTRASOUND TREATMENT



















 By Dave Scheiber
By Dave Scheiber


The stunning diamond was larger than 9 carats, featuring a pear-shaped cut and fancy cognac coloring. It rested precariously in a pair of tweezers that David Sherwood, then a veteran gemologist, held at his desk inside the Saks Fifth Avenue in Palm Beach. Preparing to examine it under a microscope, he summoned every ounce of willpower he had to steady his hands as his customer looked on, but the tremor that had become part of Sherwood’s life was unforgiving.
Suddenly, he involuntarily squeezed too hard, and the $175,000 diamond popped from the tweezers, tumbling to the floor completely out of sight.
“My thought in that moment was, ‘Well, this is the end of my career,’” he recalled. “Fortunately, I found it, but it took me a long time. So, I figured at that point it was best for me to retire gracefully, and that’s what I did. But it broke my heart.”
The scene unfolded a decade ago, leaving Sherwood’s world completely shaken. His tremor not only ended his career, but it made it impossible to pursue his passions for painting and cooking. Going out to eat with friends often became an ordeal, with the tremor causing the simplest task—like using silverware or holding a water glass—to become all but unimaginable to perform without making a mess.
“I’ll be honest, I felt kind of worthless,” he says. “Because I loved what I did, and the joy that I had—the joy that it brought to my customers—no longer existed. When I couldn’t do it anymore, I thought, ‘Wow, this is the end for me. I don’t have very much left in my life.’”
That has all changed thanks to a renowned neurosurgical team at Tampa General Hospital and an innovative procedure called


I’LL BE HONEST, I FELT KIND OF WORTHLESS. BECAUSE I LOVED WHAT I DID, AND THE JOY THAT I HAD ... NO LONGER EXISTED. WHEN I COULDN’T DO IT ANYMORE, I THOUGHT, ‘WOW, THIS IS THE END FOR ME. I DON’T HAVE VERY MUCH LEFT IN MY LIFE.’”Opposite page, from left: Dr. Yarema Bezchlibnyk and Dr. Oliver Flouty were part of the team who led David Sherwood’s focused ultrasound procedure. Dr. Theresa Zesiewicz is the TGH neurologist who initially evaluates potential patients before referring them to Bezchlibnyk, Flouty, or Dr. Donald Smith. This page: Bezchlibnyk, Flouty, and their colleagues prepare Sherwood for the procedure.
focused ultrasound, which has given him a new beginning, with plenty of living left to savor. In May, neurosurgeons with the USF Health Morsani College of Medicine at the University of South Florida employed the procedure for the first time in the Tampa Bay area at TGH. And the first person to receive the outpatient, incisionless treatment was the gem master whose life had been upended by a condition called essential tremor or ET.
A friend had urged Sherwood to visit TGH and have his tremor examined. That’s when he learned that he was among the roughly 10 million Americans who suffer from some form of ET, which causes uncontrollable shaking of the hands, head, and voice. In the early stages, the tremor is mild, but it progresses over time. In some patients, the severity can become unbearable, interfering with daily activities, such as eating, dressing, or typing on a keyboard—or, in Sherwood’s case, handling precision tools to work with jewelry.
Sherwood traveled from his home in Sebring to Tampa and was examined by Dr. Yarema Bezchlibnyk (pronounced Bezch-lib-nik), an
assistant professor in the Department of Neurosurgery and Brain Repair at USF Health Morsani College of Medicine and a neurosurgeon at TGH. The bond that developed between them would ultimately lead to a most remarkable development.

“I’ve gotten my life back,” Sherwood said. “And I can’t say enough about Tampa General. I don’t think there’s any better place.”
AThis is the story of what happened following that first doctor-patient encounter. It entwines the next generation of care and commitment to innovation provided by TGH with a new tool that can improve the quality of life for patients who struggle with disabling tremors, including those caused by Parkinson’s disease, without implanting a device.
“This definitely expands what we can do,” said Bezchlibnyk. “And it drives our efforts to help transform the lives of people living with debilitating neurological conditions. It’s the highlight of my day to see patients like David who are helped by what we do.”
Long before he ever heard the term “essential tremor” or felt a glimmer of hope over the explanation of focused ultrasound, Sherwood followed a path out of Corning, New York. Due south of Buffalo and nestled along the Chemung River, Corning is famous as the home of Corning Inc.,
THIS DEFINITELY EXPANDS WHAT WE CAN DO. AND IT DRIVES OUR EFFORTS TO HELP TRANSFORM THE LIVES OF PEOPLE LIVING WITH DEBILITATING NEUROLOGICAL CONDITIONS. IT’S THE HIGHLIGHT OF MY DAY TO SEE PATIENTS LIKE DAVID WHO ARE HELPED BY WHAT WE DO.”
Dr. Yarema BezchliBnYk
which makes glass and ceramics products for technical use.

After Sherwood attended high school and part of college there, he decided to follow his passion for gems, enrolling in the Gemological Institute of America in Santa Monica, California, and becoming certified in the field. He eventually returned to New York and worked for Corning Inc., then moved north to Rochester to become a gem and jewelry buyer for various stores. But in time, he was drawn to the Florida warmth and opulence of Palm Beach to continue his career.
His work flourished, interrupted temporarily by a bout with cancer 15 years ago. He beat it with chemotherapy and radiation, but there
was one consequential outcome. “It kick-started my tremors,” he said. “And things just progressed from there.”
Sherwood often sold jewelry in the range of $750,000 or more, and his high-end clients became his friends. But it got to the point where he couldn’t hide the tremors. “It’s very difficult when you’re shaking so badly that you can’t put a necklace or a bracelet on your customer, or put earrings in.”
At home, his love of paint morphed into a tormenting experience. “After my cancer treatments, my hands shook so much that I did one painting and destroyed it because I couldn’t stand to look at it,” he recalled.
Holding a screw to anchor it in the wall or using power tools proved too daunting. Gardening was a challenge. Meals he tried to cook in his kitchen often ended up falling onto the floor or spilling all over him. And going out to dinner, knowing people were staring, made him feel ashamed. “I did a lot of soul-searching, a lot of sleeping, and a lot of crying,” he shared.
The support of his partner made a big difference, but that wasn’t enough to keep Sherwood from worrying about his elderly parents, knowing how hard it was for them to see him suffer. To pass the time, he focused on his Corning glass collection and spent hours online researching various pieces and their prices nationwide. With a keen artistic eye, he helped neighbors with suggestions on how to rearrange furniture and modernize their homes. But privately, his anguish increased.
He might well have continued on that path if not for a friend who suffered from Parkinson’s and implored him to get evaluated at TGH

In the focused ultrasound treatment, 10,024 individual ultrasound transducers focus ultrasound beams on specific targets, like the thalamus. The procedure requires no anesthesia, incisions, or exposure to ionizing radiation.

in the hope that they could offer some relief. That led to an examination by a TGH doctor who ruled out Parkinson’s and diagnosed Sherwood with an essential tremor, referring him to Bezchlibnyk. That’s when the option of focused ultrasound was broached.
While the equipment was being put into place over the coming months, Sherwood developed a strong connection and sense of trust with the doctor he came to know simply as “Dr. B.” Finally, the call came from Bezchlibnyk’s office. The focused ultrasound equipment was ready and Sherwood was about to find out if there would be relief from his relentless misery.
When he arrived at TGH the morning of May 14, 2022, Sherwood encountered a group of some 40 medical workers prepared for the procedure—including the three-physician team of Bezchlibnyk, Dr. Donald Smith, and Dr. Oliver Flouty, associate professor and assistant professor, respectively, in the Department of Neurosurgery and Brain Repair at USF Health Morsani College of Medicine and neurosurgeons at TGH.
Sherwood recalled feeling a mix of excitement and nerves as his head was shaved for the procedure. He then lied down in an MRI machine,
with his head fitted into a helmet surrounded by a soft membrane filled with cool water. The procedure would direct high-intensity focused ultrasound beams guided by the MRI machine, requiring no anesthesia, exposure to ionizing radiation, or incisions. A computer would then calibrate 10,024 independent ultrasound transducers, arrayed around the head to precisely focus the ultrasound beams on targets such as his thalamus, an area of the brain that controls muscle activity and tremors.
As the lead neurosurgeon, Bezchlibnyk was as eager for this moment to arrive as his patient was. He had followed a path into neurosurgery after seeing how his grandfather had suffered and deteriorated from Parkinson’s disease. “It was so hard on my parents, too,” he recalled. “I would say that compelled me to enter this field.”
Smith was the senior member of the team, in terms of years of experience. He had implanted one of the first “leads” in North America in another approach to treating tremors, a surgical procedure called DBS for deep brain stimulation. Flouty joined the program in 2021, bringing extensive experience with DBS and focused ultrasound from Toronto Western Hospital, one of the busiest centers anywhere for both treatments.



THEY ARE THE GREATEST PEOPLE I COULD POSSIBLY EVER BE INVOLVED WITH. EVERYBODY FROM TAMPA GENERAL AND USF WAS JUST MAGNIFICENT.”
SherwooDDr. Donald Smith Dr. Oliver Flouty Dr. Yarema Bezchlibnyk
Results of his procedure were immediate. Sherwood, still flat on his back, was given a special pad attached to a tray on which to draw concentric circles, make lines, and then write his name—all without being allowed to rest his palm on the surface for extra balance. By the end of the tests, he was able to write his name twice with no shaking.
“When I did that, everybody in the room broke out in applause,” he said. “It was just an unforgettable moment.”
Above: Sherwood took a writing test before and after the procedure. The 9 a.m. test (left) illustrates the degree to which his tremor limited his ability to write. The 12 p.m. test (right) shows the immediate improvment in his control of his right hand. Right: Dr. Bezchlibnyk with Sherwood.

Bezchlibnyk had Sherwood use a walker for the first two weeks after the procedure, since he was leaning to one side when moving. But he quickly progressed past the walker and soon was embracing the tremor-free life he thought was gone for good.

Having recently turned 65, Sherwood has no plans to unretire from the gemology field, but he can cook, collect Corning glass pieces, tie his shoes, garden, and yes, even go out to dinner with no worries. “It’s like somebody took a magic wand and tapped me on the head,” he said.
One of his favorite daily activities is walking his Yorkie service dog, Fletcher, through the neighborhood—and once again being able to bathe him. “He’s the light of my life,” Sherwood said. “Throughout all this, he’s been a little bit of my salvation.”
Sherwood can still decide whether to have Bezchlibnyk repeat the procedure on the other side of his brain, since focused ultrasound on the right side controls the body’s left side, and vice versa. But for now,
he’s savoring a new lease on life, and thinking back on his most joyous Christmas in a long time. His tremors had prevented him from hanging ornaments in recent years. In 2021, he didn’t even bother with a tree at all. But all that changed this past December.
“I’ve collected some beautiful ornaments over the years,” he said. “I was so excited to hang them on the branches this time and not worry that they’d fall off.”
And Sherwood didn’t need any gifts, because he had already received the one he dreamt of most, delivered by Bezchlibnyk and his TGH team.
“They are the greatest people I could possibly ever be involved with,” he said. “Everybody from Tampa General and USF was just magnificent.”
Spoken by a man who knows a true gem when he sees one.
Innovations Lead to World-Class Care
AT HOME


TAMPA GENERAL HOSPITAL’S NEW HOSPITAL AT HOME PROGRAM ALLOWS LOW-RISK PATIENTS TO RECEIVE INPATIENT CARE FROM THE COMFORT OF THEIR HOMES

 BY JUDY ALEXANDER DIEDWARDO
BY JUDY ALEXANDER DIEDWARDO
The innovative new TGH at Home program enables patients with certain conditions to remain in their homes and receive continuous care from the TGH team. The Biobeat sensor allows the hospital staff to monitor vitals remotely, and patients are visited in person twice daily. They also receive food service directly to their homes.

Imagine personalized, hospital-level care in the comfort of your own home. Thanks to the newly launched TGH at Home program, that dream is a reality, explained Dr. Peter Chang, vice president of health care design at Tampa General Hospital.



“It’s a truly groundbreaking program that brings the expertise of a world-class hospital into a patient’s home, along with a full suite of services that are shifting the paradigm of how care is delivered,” said Chang, who has been at the vanguard of curating and implementing new technology and operating systems at TGH. “It allows us to evaluate whether or not a patient needs to occupy a hospital bed versus providing the same or better level of care in their home.”
The program focuses on patients with conditions such as congestive heart failure, urinary tract infections, cellulitis, chronic obstructive pulmonary disease, blood

clots, and diabetes. However, eligibility is quickly expanding across a host of other diagnoses that can be safely treated at home, including for COVID-19 patients.
To be enrolled in TGH at Home, patients are first seen after presenting to the emergency department or in the hospital if already admitted. Eligible patients must also be able to perform “activities of daily living,” such as brushing their teeth, eating, and showering without assistance.
Unlike traditional home health, TGH at Home provides an inpatient level of care, including continuous vitals monitoring versus intermittent nursing care once or twice a week. This is made possible through a


IT’S A TRULY GROUNDBREAKING PROGRAM THAT BRINGS THE EXPERTISE OF A WORLD-CLASS HOSPITAL INTO A PATIENT’S HOME, ALONG WITH A FULL SUITE OF SERVICES THAT ARE SHIFTING THE PARADIGM OF HOW CARE IS DELIVERED.”
—DR. PETER CHANGDr. Peter Chang
Biobeat sensor and a cellular-enabled tablet like an iPad that streams a continuous signal of the patient’s vitals to the hospital’s central monitoring station. The Israel-based Biobeat platform serves as an FDAapproved blood pressure cuff, pulse oximeter, and thermometer, all in one. Biobeat attaches to the patient’s chest using a small, easy-to-wear adhesive patch. For patients with allergies to adhesive materials, there is a wristwatch version with the same monitoring capabilities.
In addition to around-the-clock remote monitoring, patients are provided with at least two in-person visits per day by a dedicated member of the TGH at Home clinical team, which comprises physicians, physi-


enables physicians to
cian assistants, nurse practitioners, and registered nurses.

The TGH at Home program is available to patients living within a 30-minute drive of the hospital. Those enrolled in TGH at Home have access to every service available at TGH, including respiratory, physical, occupational, and speech therapies. In addition, a virtual health platform enables physicians to fully examine patients remotely. pitalization, including a food service that delivers meals to the patient’s
TGH at Home provides everything a patient would need during hospitalization, including a food service that delivers meals to the patient’s home, said Chang. “Every service that is available in the hospital is available in the patient’s home, including respiratory therapy, physical therapy, occupational therapy, or speech therapy.”
“TGH at Home is a true model of innovation—integrating hightech applications such as remote patient monitoring and telehealth visits with in-person care by trained health care providers,” said John Couris, president and CEO of TGH. “We can give patients what they
AT

HIGH-TECH APPLICATIONS SUCH
VISITS
CARE
TRAINED HEALTH
CARE
really want—world-class care in their own environment.”
The program is currently limited to those living within a 30-minute drive from TGH, but the hospital is in the process of exploring opportunities for TGH at Home in Palm Beach and Martin counties.

“Programs like this are gaining traction around the country, and the benefits are tangible, namely an improved patient experience, shorter hospital stays, reduced risk of hospital readmission, and more costefficient care,” said Chang. “The COVID-19 pandemic signaled a giant leap forward in the use of technology that’s been available but needed an impetus to expand. It’s definitely shifted the way we think about
how we
provide care.”
TGH has also partnered with United States–based telehealth provider TytoCare, which has created a virtual health platform that provides patients with a cellular-enabled tablet to conduct telehealth visits with providers. The equipment is available at no additional cost and is continually monitored by the TGH at Home care team.
“Not only can we remotely listen to a patient’s heartbeat and their lung sounds with digital stethoscopes, we can actually examine a patient without physically being in front of them, which is extraordinary,” said Chang.
TGH
HOME IS A TRUE MODEL OF INNOVATION—INTEGRATING
AS REMOTE PATIENT MONITORING AND TELEHEALTH
WITH IN-PERSON
BY
CARE PROVIDERS. WE CAN GIVE PATIENTS WHAT THEY REALLY WANT—WORLD-CLASS
IN THEIR OWN ENVIRONMENT ” —J OHN C OURIS
AFTER HIS MELANOMA DIAGNOSIS, HALL OF FAME SLUGGER MIKE SCHMIDT RECEIVED ALL-STAR CARE FROM AN ONCOLOGIST HE USED TO COACH
 BY PAIGE BOWERS
BY PAIGE BOWERS
Mike Schmidt played for the Philadelphia Phillies from 1972 to 1989. Following his retirement, Schmidt worked with his son’s baseball team, which included Dr. Abraham Schwarzberg. Many years later, Schmidt and Schwarzberg’s lives would intersect again, when Schwarzberg treated Schmidt for melanoma.
In his post-baseball life, former Philadelphia Phillies third baseman Mike Schmidt used to hit ground balls to The Benjamin School’s baseball team during their practices. His son, Jonathan, was playing for the Buccaneers in those days, so it was an opportunity for Schmidt to spend time with his boy while coaching others in the sport he loved.

“He’d hit us balls and say things like ‘Now [former St. Louis Cardinals shortstop] Ozzie Smith would do this,’” said Dr. Abraham Schwarzberg, the team’s former second baseman who is now senior vice president and chief of the Tampa General Hospital Cancer Institute and senior vice president of network development for TGH. “Mike really made you feel like he cared and was invested in your growth as a player and an athlete.”

For Schwarzberg, who grew up idolizing Schmidt, those days were admittedly a little hard to process. After all, Schmidt, now 73, was a 12-time MLB All-Star, 10-time Golden Glove winner, and three-time National League Most Valuable Player in his 18 seasons with the Phillies. Inducted into the Baseball Hall of Fame in 1995, he is widely considered to be the greatest third baseman in baseball history, as known for daring barehanded plays as he was for power hitting. And there he was in Palm Beach Gardens, patiently hitting ball after ball to a bunch of kids in orange and blue.
“Abe was a real tiger,” Schmidt recalled. “I’d hit him ground balls, and he worked hard and stood out. But I had no idea where life would take me and him, and then the two of us together.”
More than two decades after Schmidt coached Schwarzberg, their paths would cross again. Only this time the roles were reversed, with Schwarzberg coaching Schmidt through a Stage 3 melanoma diagnosis that threatened his life.

ABE WAS A REAL TIGER. I’D HIT HIM GROUND BALLS, AND HE WORKED HARD AND STOOD OUT. BUT I HAD NO IDEA WHERE LIFE WOULD TAKE ME AND HIM, AND THEN THE TWO OF US TOGETHER.”
—HALL OF FAMER MIKE SCHMIDTDr. Abraham Schwarzberg
For Schwarzberg, the journey into oncology was personal. When he was 13, his grandmother was diagnosed with metastatic kidney cancer, and doctors saved her life through immunotherapies that were experimental at the time.

“As a young child, I didn’t fully understand the impact of the medicine and the complexity of it, but I knew that the impact this doctor had on my family was something I wanted to emulate,” Schwarzberg said. “I wanted to do for other people what he did for us.”
Years later, Schwarzberg’s uncle, Richard David Kann, died of advanced melanoma, further convincing him of the importance of this work and inspiring his family to start a melanoma foundation in his honor. The Richard David Kann (RDK) Melanoma Foundation now aims to teach people about early detection and prevention, starting in childhood with a SunSmart America curriculum for students in kindergarten through twelfth grade.
Although melanoma is less common than other types of skin cancer, the American Cancer Society says it is more likely to grow and
spread. Exposure to ultraviolet rays is a major risk factor for most melanomas, with many of them linked to frequent sunburns. Athletes like Schmidt, who play mostly in open-air stadiums, are particularly susceptible to this type of cancer, especially if they don’t use sunscreen.
For Schmidt, all those years in the limelight—and sunshine—took their toll. In 2013, Schmidt was about to fly from Rhode Island to Florida when he was bothered by a crusty spot on his right hand that was itchy and painful. On the way to the airport, he stopped at his dermatologist to see what it was.
“The dermatologist froze it off, then said, ‘Let me look at the rest of your body while you’re here,’” Schmidt recalled. “He found this pink thing on my back and biopsied it.”
Schmidt left for Florida that day, but he was worried about what the doctor might find. Then he got a call saying he needed to return to Rhode Island for immediate scans and MRIs at Massachusetts General Hospital (MGH). The melanoma had spread into the lymph nodes on the left side of his body and required surgical removal. Then doctors found seven tiny
spots of cancer in his brain and 12 spots in his lungs. Schmidt would require brain surgery, as well as radiation and chemotherapy.
Chemotherapy didn’t work as well as doctors hoped, and Schmidt admitted that his mind was going to gloomy places. Because he split his time between Rhode Island and Florida, he needed an oncology team in the Sunshine State that could work with doctors at MGH to manage his care. He was referred to a cancer center that was 10 minutes away from his house. When Schmidt met with his doctor for the first time, he realized that “the biggest cancer doctor in the area, if not the country, was someone I used to hit ground balls to.”
It was Schwarzberg, who immediately shifted into problem-solving mode, prescribing an immunotherapy drug called Yervoy that Schmidt said, “saved my life and turned this thing around.”
At the time, Yervoy was in clinical trials. However, because Tampa General Hospital is affiliated with the USF Health Morsani College of Medicine at the University of South Florida, Schwarzberg was able to provide
emulate,” Schwarzberg said. “I wanted to do for other people what he did for us.”David Kann (RDK) Melanoma Foundation now aims to teach people about early detec- Dr. Schwarzberg was led to pursue medicine after seeing doctors save his grandmother’s life with an experimental cancer treatment. Opposite page: Mike Schmidt (at podium) honors Dr. Schwarzberg at an event.
Schmidt with “game-changing treatment in a rapid way.”
“Mike is a very tough and brave individual,” Schwarzberg said. “And he is someone who is very focused when it comes to the task at hand.”
Schmidt credited his medical team led by Schwarzberg, his faith, and the love of his wife and family for getting him through this period.
“You think about seeing your grandkids grow up, and about your wife,” Schmidt said. “But you work through those things. My wife was my nurse, my confidante, and my love. My journey was her journey as well.”
As Schmidt’s health improved, he felt compelled to use his celebrity to raise funds for melanoma awareness and research. Schwarzberg’s family foundation was right there, and for Schmidt it was a perfect fit.

“It’s easy for me to tell my story,” Schmidt said. “I tell people to wear long sleeves and a wide-brimmed hat and see your dermatologist several times a year. If you catch it early, you should be fine.”
In 2017, Schmidt worked with the RDK Melanoma Foundation to launch an effort to place
sunscreen dispensers throughout stadiums across the nation. The Phillies have become a valuable partner in spreading awareness; last year Schmidt traveled to Philadelphia to throw out the first pitch for the annual RDK Melanoma Awareness Day. The foundation is working to expand the availability of sunscreen dispensers at baseball fields, beaches, and other places where harmful UV rays might be an issue.
Though he takes a lot of medicine, gets infusions, and has frequent CT scans and MRIs for his brain, Schmidt said his health is currently good. “I’m the luckiest guy on earth. Not a lot of people can say that.”
Schwarzberg said his old coach is embracing his new role as a melanoma spokesperson with the same gusto he used in baseball—all to the community’s benefit.
“Mike is a unique individual because of his success, but also his humility and his commitment to making a difference in the community,” Schwarzberg said. “He has made that difference whether he is hitting ground balls or spreading the word about melanoma prevention.”
MIKE IS A UNIQUE INDIVIDUAL BECAUSE OF HIS SUCCESS, BUT ALSO HIS HUMILITY AND HIS COMMITMENT TO MAKING A DIFFERENCE IN THE COMMUNITY. HE HAS MADE THAT DIFFERENCE WHETHER HE IS HITTING GROUND BALLS OR SPREADING THE WORD ABOUT MELANOMA PREVENTION.”
— DR. ABRAHAM SCHWARZBERG
A

THE EARLIER THE BETTER
Advances in colorectal surgery are giving patients more options—an incredible breakthrough as colon cancer impacts younger individuals
 BY DAVE SCHEIBER
BY DAVE SCHEIBER
Throughout his distinguished career, Dr. Jorge Marcet, director of colorectal surgery services and vice chief of surgery at Tampa General Hospital, has sought to create better outcomes for patients with colorectal cancer. His goal: to spare them from radical surgery that can have a profoundly deleterious impact on their quality of life.

That desire has led the nationally renowned colorectal surgeon to help pioneer new, transformative treatments. His work has opened the door to significantly improved results through a series of landmark clinical trials—and it has played a part in lowering the recommended age to receive colonoscopy screenings from 50 to 45.

“Rectal cancer can be quite a devastating disease,” said Marcet, who is also a professor and director of the Division of Colon and Rectal Surgery at the USF Health Morsani College of Medicine at the University of South Florida. “It may involve a permanent colostomy and be a very difficult treatment to endure. From the start of my career, I thought, ‘We can improve on outcomes.’”
That first step took place some 20 years ago, when
Marcet served as lead investigator for a trial that provided a promising alternative to radical surgery. Rather than remove the rectum of cancer patients, Marcet and his team selected patients who had done well with radiation treatment and only performed a small excision of the tumor site. Ultimately, the trial demonstrated that patients could achieve positive outcomes over the long term; results were published in the Annals of Surgery.
Then, the American College of Surgeons conducted a similar study on a national level, with Marcet as a principal investigator, utilizing the same local incision approach. Results from this multi-institutional trial, published in Lancet Oncology , provided further evidence that a better option existed for early-stage cancer patients.
“But then we wondered if we could push the envelope further and help those with more late-stage cancers,” Marcet explained. “Could we increase the number of patients who might benefit from this local excision or even no surgery at all?”
The stage was set for the first of two milestone clinical trials. The TIMING trial, also published in Lancet
Dr. Jorge Marcet has helped TGH navigate a new frontier in the treatment of colorectal cancer. With the goal of lessening the frequency of surgery, Marcet has been involved in many clinical trials that have included prioritizing chemotherapy ahead of surgery as well as utilizing immunotherapy as the only form of treatment.
We wondered if we could push the envelope further and help those with more late-stage cancers. Could we increase the number of patients who might benefit from this local excision or even no surgery at all?”
—D r . J orge M arcet
Oncology , demonstrated that it was safe to delay the radical surgery, moving chemotherapy ahead of the operation. “We were able to show that the longer you waited to do the surgery for each cohort, the more chances there would be no cancer in the rectal specimen,” Marcet said.
After TIMING, Marcet, USF Health, and TGH participated in the OPRA clinical trial, short for Organ Preservation in Rectal Adenocarcinoma. The study found that not every colorectal patient requires surgery. Instead, those exhibiting no residual cancer after radiation and chemotherapy are moved to a “watch and wait” stage. “It’s a nonoperative treatment option that has been very successful,” Marcet said.
The OPRA trial, published in the Journal of Clinical Oncology in early 2022, demonstrated that over half of the patients did not go on to have immediate surgery. And the majority of those end up not having surgery at all. “It’s remarkable to see this reduction in the number of people who would otherwise be having a radical surgery. But what we’re looking
at now is, can we do even better?”
This question led Marcet to yet another study of a very small group of rectal cancer patients. Each had a particular gene mutation and received an antibody. “Immunotherapy was their only treatment—no radiation, no chemotherapy, no surgery,” he said. “This is still a small, preliminary, Phase 1 study, but it demonstrated that the cancer disappeared in these patients over a 12-month period.”
Marcet and his team are focusing on this approach, called targeted therapy, and exploring what mutations have caused this particular type of cancer. “Can we target a specific therapy to block that mutation?” he asked. “It’s so exciting how it’s developed to this point. It’s a continuum of trials that allows you to keep learning.”
That continuum has its roots in the 1990s, when TGH was the first hospital in the Tampa Bay area to adopt laparoscopic surgery and led the way in developing minimally invasive procedures for colorectal surgery including laparoscopic, robotic, and transanal minimally invasive surgeries (TAMIS).

Marcet has trained hundreds of surgeons in these advanced procedures, which provide patients an early return to a productive life.
TGH surgeons perform more TAMIS for rectal cancer than any other center in the region. In TAMIS, rather than performing abdominal surgery to remove the rectum, surgeons are able to operate through the anal opening, remove a portion of the rectum and reconstruct it. The surgery is far easier on patients, with minimal pain and an outpatient or overnight stay.
AMarcet’s findings have been instrumental in changing the age threshold for colonoscopy screenings. He and several colleagues conducted a study examining increased incidence of colorectal cancer in people younger than 50, published in Diseases of the Colon and Rectum . This resulted in the U.S. Preventive Services Task Force revising its recommendation for colonoscopy screenings to age 45 in May 2021.
Today, the American Cancer Society finds that 1 in 23 men and 1 in 25 women will be diagnosed with colorectal cancer in their

lifetimes. Could diet be a factor in the rise in cases at a younger age?
“We don’t know the exact role of diet,” Marcet said. “With this phenomenon of colon cancer skyrocketing in modern times— not just in the United States but around the world—of course we’ll suspect diet. It’s changed radically compared to 50 to 80 years ago.

“The food we eat has been mass-produced and preserved, and there’s more of it available. So, what’s the culprit? We don’t know that yet, and it may be more than one factor. The adage of ‘everything in moderation’ is good. Make sure to follow a diet low in carbohydrates and processed meat.”
Whatever the cause, Marcet urges individuals not to wait until a more advanced age to get screened.
“Most of the time, what I find when interviewing somebody who has been diagnosed with colon cancer is that they’ve been having symptoms for many months,” he said. “The most common symptom is blood in the stool. But it’s important to recognize that not all these cancers have symptoms at first. And that is why screening is so important. You want to identify a polyp before it’s a cancer. If you find it before there are symptoms, these are early-stage, highly curable cancers. But just as important, if you’re having symptoms, don’t ignore them. Awareness is so important, and you need to get checked out. This is serious business.”
KNOW
In recent years, the American Cancer Society and the National Cancer Institute have updated the recommended age to start screening for colorectal cancer. Here’s what you should know by age. To learn more visit cancer.org/colonguidelines
AGES 76 TO 85
A WHAT TO 1
AGES 45 TO 75
Adults at average risk for colorectal cancer should start regular screenings at 45. Options include stool-based tests or a visual exam such as a colonoscopy or CT colonography. Those in good health should continue regular screenings until the age of 75
Consult your doctor about whether to continue screenings. This decision is dependent upon a patient’s prior screening history, personal preferences, life expectancy, and overall health.
AGES 86+
This demographic should no longer screen for colorectal cancer.
3AM I AT HIGHER RISK? People are considered at higher risk of colorectal cancer if they have: a personal history of colorectal cancer or certain types of polyps; a family history of colorectal cancer; a personal history of an inflammatory bowel disease such as ulcerative colitis or Crohn’s disease; a confirmed or suspected hereditary colorectal cancer syndrome; or a personal history of receiving radiation to the abdomen or pelvic area to treat cancer.

T.A. Walker (left) was diagnosed with Stage 1 colon cancer in 2021 at the age of 44. He credits early detection, the team at TGH, and his partner, Charlie Lewis (right), with helping him defeat the disease. Walker and Lewis are pictured here at Lucky Shuck Oyster Bar & Taphouse in Jupiter, Florida, where they had their first date.

PATIENT SPOTLIGHT
BY DAVE SCHEIBER | PHOTOGRAPHY BY JERRY RABINOWITZT.A. Walker is best known in the West Palm Beach area for telling stories about interesting people and places on his Shining a Light segment for WPTV-Channel 5. But in 2021, Walker suddenly became the subject of a personal story with life-and-death ramifications—and now he is determined to shine a light on that, too.
Walker is a colon cancer survivor. And a colonoscopy screening at age 44 very likely saved his life. His story underscores the vital importance of getting checked for the disease earlier than the previously recommended age of 50; the National Cancer Institute’s new recommended age for colonoscopies is 45.
“If I had waited until I was 50, it would have been really bad,” said Walker, now 45. “That’s why this is something I need to talk about.”
Twenty years earlier, Walker moved to South Florida to take a morning show radio job, following a stint as an intern on The Late Show With David Letterman. It was around that time that he was alarmed to see a small amount of blood in his stool. His doctor attributed the bleeding to a hemorrhoid and Walker went on with life, continuing to notice traces of blood but chalking it up to the diagnosis.
In 2021, the amount of blood suddenly intensified, concerning him enough to get it checked out. “It was really disturbing, and I found that I was more tired than usual,” he recalled. “I remember being put under for the colonoscopy and waking up 15 minutes later unaware of anything. And that’s when the doctor blurted out, ‘You have cancer.’”
It was the start of an emotional roller coaster for Walker, who insisted on showing up for his assignment the next day covering Disney World’s fiftieth anniversary celebration. “I just needed the Mouse to keep me busy,” he said. “When you’re reporting, you can compartmentalize the emotion and what’s happening
in front of you and just tell the story.”
That story was about to take more unexpected turns. Several days later, the doctor called with apparently incredible news: Walker didn’t have cancer after all but should still see another surgeon to be sure. He barely had time to let the sense of relief sink in when the second colonoscopy suggested that he did, indeed, appear to have cancer. Even though the biopsy came back negative, the doctor was unconvinced and did a resection of a 6-inch portion of Walker’s colon, leaving no doubt this time of the cancer diagnosis.
Walker, assisted emotionally and physically by his partner, Charlie, was exhausted from the back-and-forth, the resection, and the finality of the diagnosis: Stage 1 colon cancer.
Because he didn’t put off getting a colonoscopy after noticing his increased bleeding, Walker is now cancer-free. Earlier this year, he met John Couris, the president and CEO of Tampa General Hospital, while attending the Honda Classic golf tournament in Palm Beach Gardens. The Palm Beach region boasts many excellent community hospitals, but TGH adds the presence of a large academic medical center, providing the worldclass expertise of an institution in the top 10 percent for cancer care in the nation.
Couris told Walker about Dr. Jorge Marcet’s leading-edge colorectal research. As a result, Walker traveled to Tampa to interview Marcet for a story that aired in March 2022 for National Colorectal Awareness Month.
In the piece, Marcet told Walker: “You don’t know unless you have it investigated. And an investigation is to look inside. … Colon cancer rates are going up in people younger than 50. And I suspect it’s going to lower more.”
That’s why Walker counts his blessings that he didn’t wait to get checked, and he is determined to keep shining a light on the issue.
TAKING
OUT
OVARIAN CANCER
In July 2017, Brenda Gotlen was diagnosed with Stage 4 ovarian cancer.
Hyperthermic intraperitoneal chemotherapy requires the surgical removal of all tumors before a heated chemotherapy solution is instilled and circulated in the abdomen.

 BY SANDRA GURVIS
BY SANDRA GURVIS
“I was going about my daily routine and worked very long hours outside the home,” said Gotlen, a self-professed workaholic. Seemingly out of the blue, she began to experience abdominal pain and extreme swelling. “I went to my primary care special-
ist who sent me to the ER for a CT scan. They
ist who sent me to the ER for a CT scan. They found a large mass, which they were 99 percent sure was cancer.”
Gotlen approached her devastating diagnosis with a sense of calmness. “My gynecologist recommended Dr. Thomas Rutherford at Tampa General,” she said. “He specialized in the type of cancer I had, which was Stage
4 ovarian cancer that had spread outside my ovaries.”
After extensive testing, it was determined that Gotlen would be a good candidate for hyperthermic intraperitoneal chemotherapy (HIPEC). HIPEC is an innovative treatment that, in addition to ovarian cancer, is used for other types of cancer including colon and rectal, stomach, liver, and pancreatic. Tampa General Hospital was the first center in the Tampa Bay area to make HIPEC

Several years ago, one of my patients, a 28-year-old woman with virtually no treatment options after failing a Phase 1 clinical trial, opted to try an extensive surgical debulking and HIPEC. She is still alive today and doing great.”
—Dr. Thomas J. Rutherford
part of its treatment options.
HIPEC involves a concentrated, heated chemotherapy that is delivered directly into the abdomen. It was pioneered by Dr. Paul Sugarbaker of the Washington Cancer Institute in the 1980s.
“Early on, Dr. Sugarbaker was the only one performing this type of surgery,” said


Dr. Thomas J. Rutherford, director of gynecologic oncology at the USF Health Morsani College of Medicine at the University of South Florida and medical director of the TGH Cancer Institute. “Over time, HIPEC has demonstrated improved outcomes for ovarian cancer patients.”

Initially, Rutherford referred patients to
Sugarbaker. “Several years ago, one of my patients, a 28-year-old woman with virtually no treatment options after failing a Phase 1 clinical trial, opted to try an extensive surgical debulking and HIPEC. She is still alive today and doing great.”
Now a leading expert in the surgery, Rutherford joined the team at TGH in 2017 and operates with two partners who also offer HIPEC to patients as part of the treatment options when it comes to those diagnosed with advanced stages of ovarian cancer.
“It’s gratifying to know we are ahead of the curve,” he remarked. “But it’s even better to have patients who have survived 10 or more years and counting.”
It’s gratifying to know we are ahead of the curve. But it’s even better to have patients who have survived 10 or more years and counting.”
—Dr. Thomas J. Rutherford
The complete HIPEC procedure can take anywhere from six to 10 hours, and patients typically stay in the hospital for five to seven days afterward.
STAGE ONE
“The first requires surgical removal of all visible tumors,” explained Rutherford. This is performed by a multidisciplinary clinical team that uses precise focus to ensure the area is cleared of all cancerous growth.

STAGE
The heated chemotherapy solution is instilled and circulated in the abdomen for about 90 minutes at 42 degrees centigrade. After completion of the HIPEC, the fluid and chemotherapy are drained, and the abdomi-
nal cavity is then rinsed with a saline solution before the incision is closed. Depending upon the extent of disease, the total procedure can take from six to 10 hours and often involves a hospital stay of five to seven days.
As Rutherford noted, HIPEC is safe and has demonstrated an increased overall survival in some patients with ovarian cancer. It also has the advantage of being performed once rather than multiple times over several weeks or months, as had been done with intraperitoneal chemotherapy.
“I am very thankful for Dr. Rutherford and the team at TGH who cared for me,” said Gotlen.
“Dr. Rutherford was personable, straightforward, and told me exactly what to expect. Before they put me under, he introduced me to the team who was working on me. In my case, they took out 6 inches of intestine that was damaged from the cancer. [Post-op,] I also had two catheters in my abdomen to help drain the fluid.”
Gotlen did so well that she was able to return home after only five days.
She ate and drank as instructed and did her best to remain active by walking and moving. She said that it took her almost six months to fully recover. But now, five years after her surgery, most of her symptoms are gone or manageable. Most importantly, she is cancer-free.
TWO
As part of a major surgery, HIPEC takes place in two stages.
SECOND CHANCE
A TRANSFER TO TAMPA GENERAL HOSPITAL SAVED A PALM BEACH COUNTY PATIENT’S LIFE
By Chris Curtland Photography by Jerry RabinowitzWhen K.C. Austin, a resident on Florida’s East Coast, was battling the Delta variant of COVID-19, he was rushed to a Palm Beach County hospital. Soon, he and his family were facing life-or-death decisions.

“K.C. went from playing with the kids, reading them books, going on vacation, to not being able to breathe at all. It was so fast,” said Danielle Austin, K.C.’s wife.
In the hospital’s intensive care unit, K.C. was intubated and put on a ventilator. That morning, he sent his wife a text message saying that he thought he was going to die.
“Being home alone with two children and having those be the last words you hear from your husband was really very, very scary,” Danielle said. “Our daughter was only 3, so she was just missing Daddy, but her older brother really understood that this was life and death. I tried to be as honest as possible and explain that the doctors are doing everything they can. But we don’t know.”
Dr. Ahmed El-Haddad, medical director of the Palm Beach County hospital’s ICU, realized there was nothing more he could do. His patient needed extracorporeal membrane oxygenation (ECMO) equipment that takes over the breathing process and allows a patient’s lungs to rest. But his hospital didn’t have it to offer.
“Knowing that there’s something out there that can help your patient, and you don’t have it, is torture,” he said.
El-Haddad’s team urgently searched for a hospital that offered ECMO and could also accept a patient. Danielle credits the Tampa General Hospital Health Ambassador Program for providing a fast, streamlined transfer process.
“Luckily, the doctors had started the paperwork for the transfer pretty early on,” she said. “When I got that phone call that he was being transferred to TGH, I just said, ‘Oh, my gosh, we have a chance.’ The communication at TGH, and the fact that I could speak to a physician every day, was unbelievable. I never felt like I didn’t know what was going on. I never felt that they weren’t doing everything they could.”
K.C. arrived at TGH in critical condition. As he encountered increasing complications throughout the treatment process, his condition became life-threatening. TGH had to deploy a multidisciplinary approach.
“Mr. Austin’s case is about as complex as one can get,” said Dr. Kapilkumar Patel, medical director of the Center for Advanced Lung Disease and Transplant at TGH. “The more eyes on complex cases, the better.”


The team members who worked on K.C.’s case included pulmonary specialists, critical care specialists, cardiothoracic surgeons, respiratory therapists, nutritionists, pharmacists, perfusionists, a hematologist, a trauma team, and nurses at his bedside.
“There is no textbook for how to manage a complex patient,” Patel said. “It’s years of experience, collaboration, listening, and learning from one another—egos aside—that lead to a successful outcome.”
After eight weeks in a coma, K.C. woke up.
“I walked into the room, and he said, ‘Hi,’” recalled Danielle. “I said, ‘Hi. Oh, my gosh. Is this for real?’ I’m forever grateful to all the teams for realizing, from a human perspective, that this is a young guy with a wife and young children. We have to give him a chance.”
To learn more about the TGH Health Ambassador Program or to schedule a consultation with one of the hospital’s physicians, call (561) 644-0125.


Dr. Thomas Bernasek is seen here performing a total knee replacement using the VELYS Robotic-Assisted Solution. The VELYS system is much smaller than previous designs, it contains everything a surgeon needs to complete the procedure, and it can provide real-time feedback on the implant.
Robotics has played an integral role in knee replacement surgery for more than a decade. These sophisticated devices aid in the precision of the operation, improve patient outcomes, and reduce post-operative pain.

However, they also can be cumbersome, costly, and complex, requiring company representatives to be on hand to assist in their use. In addition, the equipment can occupy a good bit of space in an operating room. But like many aspects of medical technology, robotic tools are becoming more efficient and compact as they evolve.
Such is the case for the VELYS Robotic-Assisted Solution for total knee replacement, the latest device orthopaedic surgeons at Tampa General Hospital are using to improve knee replacement procedures for their patients.

Dr. Thomas Bernasek is a board-certified orthopaedic surgeon, a founding member of the Florida Orthopaedic Institute, and TGH director of arthroplasty. He performs between 600 and 700 joint replacements a year and has nothing but praise for the VELYS Robotic-Assisted Solution.
“Some of the issues with prior designs were that they were large, bulky, and much more expensive,” Bernasek said. “Because of its much smaller footprint, [the VELYS] allows one to attach it to the side of the bed. The surgeon can walk around it on either side of the knee. It also gives us real-time information about the implant for knee replacement.”
Everything needed to perform the procedure is contained within the device, including a sterile screen the surgeon can use in place of a separate CT scan—and another person to operate it.
The VELYS RoboticAssisted Solution can place the implant on the knee and assess its stability and range of motion, allowing surgeons to make adjustments as necessary to create the best fit and balance possible for patients. This method also reduces the risk of postoperative blood loss.


BY 2026, WE EXPECT THAT OVER HALF OF TOTAL JOINT
The knee is surrounded by ligaments and soft tissue, Bernasek explained. During a total knee replacement, one of the main objectives is to make sure the knee is in as natural of a position as possible with regard to the ligaments around it. That’s what the VELYS Robotic-Assisted Solution does so well.
“Robotics allow us to assess the stability of the knee before cutting the bone,” he said. “Basically, the computer places the implant on the knee [and] checks the stability and the range of motion with the implant in place. It can tell you if it’s a little tight here, a little loose there, so you can make adjustments to get the ideal range of motion and stability of the knee. We do all the planning beforehand, log it into the robot, and it basically makes the cuts in the appropriate plane. We [then] put on the implant and assess. It’s astonishing how effective the information is.”
All that precision makes for a better, more comfortable fit for the patient—and a fascinating step forward for surgeons, Bernasek said. “It moves us much closer to achieving perfect placement and balance of the knee.”
One of the other benefits of the VELYS Robotic-Assisted Solution is that it can be used to perform surgery on almost anyone who needs a knee replacement, Bernasek explained. While there are some pa-
tients with huge, thick muscles and those with very stiff or extremely scarred knees who may not be ideal candidates, he added, the majority of those who need a replacement are likely to do well.
Surgeons at TGH began using the VELYS Robotic-Assisted Solution in July 2022, and the hospital is the first facility in the region to offer it. “In an era when we are doing everything that can be done to accelerate patient recuperation and improve outcomes, this is one additional feature,” Bernasek said.

The traditional (non-robotic) method of knee replacement requires the use of long rods inserted through the canal of the femur bone to judge alignment. This disrupts the marrow cavity, pushing blood elements into the bloodstream, creating a hole in the femur, and causing additional post-operative bleeding. With the VELYS method, alignment does not require a rod, thereby preventing blood loss.
Less bleeding and more rapid recovery also mean more procedures can be done on an outpatient basis.
“By 2026, we expect that over half of total joint replacements of the hip and knee will be done as outpatient procedures,” Bernasek said. “COVID-19 dramatically accelerated the transition to outpatient replacement. We probably got close to it in 2022.”


Stress urinary incontinence (SUI) can impact women at any stage in life, noted Dr. Raviender Bukkapatnam (left). A new urethral bulking agent known as Bulkamid is providing SUI sufferers with an easy option that is safer and less invasive than previous surgical interventions.
With so much literature and conversation focusing on cancer, heart disease, diabetes, and other life-threatening conditions, it is sometimes easy to forget that diagnoses without comparably grim prognoses can nonetheless profoundly impact patients’ quality of life. Because they might seem innocuous from a clinical standpoint, certain medical conditions run the risk of being overlooked or even dismissed as mere annoyances. Among these is stress urinary incontinence (SUI), the leakage of urine from the bladder under physical circumstances that should not cause it. SUI affects about 1 in 3 women at some point in their lives, and not always late in life.

“It’s perceived to be a disease of old age, but the fact is, it starts even in younger women as well,” explained Dr. Raviender Bukkapatnam,
chief of the Tampa General Hospital Urology Institute and president of Florida Urology Partners. “It’s typically associated with childbirth, but it can happen to anybody, in addition to happening after certain types of surgery. It’s a significant issue and affects quality of life. It often creates a change in lifestyle for someone who’s otherwise very active and wants to engage in life.”


Like many personal medical struggles, SUI is most likely something few people think much about until they experience it for themselves. However, just imagine not being able to bounce on a trampoline with your child or even pick up your child without an episode of incontinence or, at least, the threat of it. SUI sufferers experience this uncertainty when they exercise, laugh, sneeze, have sex, sit down to watch a long movie—the list of possible scenarios is endless. The anxiety associated with such limitations, as well as the

The Bulkamid procedure takes roughly 5 minutes.
It requires no incisions, nor does it come with the chance of material failing or breaking and the associated complications.
depression accompanying the drastic limitation of one’s activities to compensate, can feel crippling.
And yet, because SUI doesn’t necessarily pose mortal danger and is often viewed more as an annoying symptom than as a condition of its own, many who suffer from it may not even know that there is treatment available or bother to seek it.

“Most people brush it off because they are not aware or don’t know that there’s something that can really be done about it,” Bukkapatnam said. “The industry for protective undergarments is one of the largest, and unfortunately that’s the first stop for these patients because they’re either embarrassed to bring it up or they don’t know that there’s something that can be done about it.”
Another factor potentially inhibiting SUI sufferers from seeking treatment—even if they are aware that it exists—is the unfortunate reputation surrounding standard care options. As Bukkapatnam explained, for a long time the only available intervention was sling surgery, which utilizes mesh, a material that has gotten “a bad rap for the complications it can cause.” With recent advancements in tools
and techniques, the utilization of mesh for sling surgery is much safer than it used to be, “but it has had a stigma that is probably irreversible,” he added. “In fact, in many countries in Europe, mesh is completely banned.”

Fortunately, advances in materials and technology have also given rise to novel techniques for the treatment of SUI. One of these is poised to redefine the process and dramatically improve the lives of those with the condition.
Used as a urethral bulking agent, Bulkamid is a water-based gel that adds volume to the wall of the urethra, thereby preventing urinary leaks. Whereas sling mesh surgery relied on the invasive insertion of a relatively large foreign object (the mesh) into the abdomen to support and compress the tissues underlying the bladder, the Bulkamid process requires only very small injections of a sterile filler material directly into the urethra. The advantages are manifold, not only in that the procedure requires no incisions, but there is also no chance of the material failing or breaking apart and risking significant complications for the patient, as there would be with sling mesh procedures.

The vast majority of patients have signifi cant success. In the larger studies, about 10 to 15 percent of patients desired a second injection, so they can undergo a repeat treatment … but about 85 percent of patients were satisfi ed with only one injection.



 — DR. RAVIENDER BUKKAPATNAM
— DR. RAVIENDER BUKKAPATNAM

“The [Bulkamid] procedure itself takes maybe 5 minutes,” Bukkapatnam explained. “A small camera is placed inside the urethra, and a small needle is used to inject the material into the urethra. The surgeon injects it such that it closes the urethra. Basically, the surgeon is sculpting the urethra in such a way that would prevent leakage.”
No incisions mean a far lower risk of infection, which comes with any surgical procedure. Furthermore, the patient can go home the same day and return to her normal activities within a few days.












“If it’s done in the office, they leave in 5 or 10 minutes,” Bukkapatnam said. “If it’s done in the surgery center, maybe 30 minutes just to recover from the sedation. As far as recovery is concerned, there may be some slight soreness for a day or so, maybe some slight difficulty voiding [the discharging of waste from the body], but after that, typically by the next day, the patient is back to normal.”
This is in contrast to the six weeks until “return to normal” for sling mesh procedures—an eternity for someone wanting and needing to get back to her day-to-day activities. More importantly, the long-term efficacy seems just as promising if not better for Bulkamid injections.





“The vast majority of patients have significant success,” noted Bukkapatnam. “In the larger studies, about 10 to 15 percent of patients desired a second injection, so they can undergo a repeat treatment … but about 85 percent of patients were satisfied with only one injection.”
If it turns out that some more insidious or persistent diagnosis lurks beneath the SUI, the Bulkamid hydrogel procedure does not contraindicate any other treatments, whether in tandem or subsequently. “It doesn’t burn any bridges,” said Bukkapatnam, “so your patients remain candidates for any other therapies.”
More involved treatments are not on the horizon, however, the very notion that a long-silent and longer-suffering population may find permanent reprieve from an affliction that has made life unnecessarily more burdensome is cause for celebration. And as awareness of such a straightforward and relatively stress-free therapy becomes more widespread, there is some hope there may come a time when untreated stress urinary incontinence and all the anxieties that go along with it are relatively uncommon.

DURING THE CRISIS OF COVID-19,
HOSPITAL STAFF
—GENE MCNICHOLSIn the hardest days of the COVID-19 pandemic, patients were often separated from loved ones, relying on medical professionals to not only treat them but also provide human connection and communicate with their families outside of the hospital. Doctors, nurses, and other care staff carried an enormous burden, risking their own health to this disease, struggling to work under heavy protective gear, and enduring demanding schedules when personnel became scarce. Those days may have been among the most difficult for the medical community in modern history.
However, a bright light shone at Tampa General Hospital as members of the community recognized the stress health care professionals faced and offered a lifeline.
One couple took the extraordinary step of making generous philanthropic gifts that helped to bolster the inner workings of the hospital in big and small ways. Patsy and Gene McNichols have been supporters of TGH for more than 24 years. Gene is a former member of both the TGH Foundation and the hospital’s board. Patsy is a founding member of the Bruemmer Women’s Leadership Circle. They served as the honorary chairs of the TGH twenty-first annual gala in 2018, which raised four times the funds that previous galas earned. In the wake of the pandemic, the couple realized that the people who made their hospital a special place were suffering.
“During the crisis of COVID, the hospital staff was equally in crisis,” Gene said. “Their careers changed overnight, and you cannot imagine how that can impact a worker as a total person. We needed to try to charge them up again.”
AND GENE MCNICHOLS’ BY KELLEY MARCELLUSMr. and Mrs. McNichols focused an August 2021 gift of more than $300,000 to TGH’s Chaplain Ministry Program, which would help fund a position dedicated to serving hospital employees. Hospitals typically have a spiritual services team to counsel patients and families facing difficult diagnoses, but the TGH chaplaincy staff didn’t have the bandwidth to minister to both patients and staff.
“The McNicholses are very tied into their Christian faith,” said Jamie Powell, the TGH Foundation’s

THE
WAS EQUALLY IN CRISIS. ... WE NEEDED TO TRY TO CHARGE THEM UP AGAIN.”
executive director of events and strategic partnerships. “What they loved about this opportunity was the chance to help team members of every faith, or of no faith, turn to a dedicated team member chaplain.”
Frann Leppla, senior vice president and chief philanthropy officer for TGH and its foundation, added that the value of the expanded chaplain program is immense. “As leaders, we know that taking care of our team members means they will take better care of our patients,” she said. “Support of our team members is critical to providing the very best patient care, even more so during times of heightened stress.”
Mr. and Mrs. McNichols first learned of the hospital’s spiritual services program about 20 years ago when a minister from their own church left for TGH.
“People might know that Tampa General is a teaching hospital,” Gene said. “But they might not know that they have a teaching initiative to graduate people as chaplains. It’s important work, especially in crisis situations.”
Which is something the couple knows about. Through the years, their family has turned to TGH during difficult medical situations, but none was as impactful as watching Gene’s son recover from severe burns to his arms and legs. Gene was the vice chairman of the hospital board at the time, but he had never seen the inside of the burn unit.
“It was really a moving experience,” he recalled. “They took exceptional care of him. He has some remaining nerve problems, but he is fine [and] living a good life.”
The experience encouraged the couple to
earmark funds that are currently being used to renovate the burn intensive care unit. They’ve also supported the pediatric emergency department because “we have eight grandchildren,” Gene said. “Infants have always been close to our hearts.”
To say family is important to the McNicholses is an understatement. Three generations have worked at McNichols Co., a specialty metal fabrication business that Gene’s father, Bob McNichols, started in 1952 after serving in World War II. The company distributes metal and fiberglass products featuring perforations or holes, which are used in art, construction, decorative items, surgical trays, window coverings (like those at TGH), and more.
Bob passed away at a relatively young age from a disease that’s more easily treated today. Gene, Patsy, and their family continued the patriarch’s legacy, including incorporating their religious tenets and support for their employees and community into the business, which now has locations in 19 cities.
“In 1975, before brand marketing was really a big thing, we came up with a line to describe our narrow niche,” Gene explained. “We say we are the ‘hole’ story.”
Part of that story is that, like the couple, the third generation of the McNichols family and the company’s employees dedicate time and talent to supporting community organizations. During the pandemic, for example, McNichols Co. participated in a “clap out,” an event in which TGH leadership, foundation members, and other supporters lined the staff exits and entrances to the hospital during shift changes.
As they finished or started their shifts, exhausted employees were greeted by encouraging signs, treats, cheers, and thanks. McNichols Co. donated bags and gift cards for the staff, in the hopes of bolstering them during difficult days.
Encouraging the community to share its resources has been part of Mr. and Mrs. McNichols’ relationship with TGH for more than two decades. Their early involvement with the hospital came at the invitation of friends, who invited them to participate in the White Coat Program.

“White Coat is an exclusive opportunity for stakeholders to shadow physicians practicing in an area they have interest,” Leppla explained. “They suit up—scrubs, white coats, and all— and work side-by-side with their physician partners, giving them a firsthand look at a day in the life of our clinical teams. It’s a moving experience for all participants who witness everything from babies being born to heart transplants and everything in between.”
“It was a great way to learn about the hospital and its capabilities,” Gene said of his experience. “That is when we really became cheerleaders for the hospital.”
The couple have since encouraged other friends to give the White Coat Program a try, and they are delighted that even the children of friends are having a chance to participate.
Patsy believes that this inside look into TGH, as well as participating on the boards and committees through the years, has allowed her to watch the hospital grow. “We have a growing community, and this gets people involved when they might not otherwise have the chance to,” she said. “We’ve encouraged a lot of friends to support the hospital. And we’ve had friends and family treated at the hospital with a lot of success.”
The couple said they can feel the heartbeat of the community at TGH. And they recognize a responsibility to care for the hospital so it can continue to care for and meet the needs of the people who live here and across the state.
“Accessing medical care today is complex,” Gene said. “There’s a saying that you need a doctor in the family, but the reality is that’s not true. We are fortunate and blessed to have the leadership, doctors, nurses, and employees of this living machine of Tampa General Hospital. Tampa General has a heart, a big heart.”

Immune
SUPPORTERS
A HEALTHY, BALANCED DIET plays a vital role in overall wellbeing. Certain vitamins, minerals, and antioxidants can strengthen your body’s immune response, and getting these nutrients from foods is always favorable to supplements. Chef Stephen Asprinio, principal of SA Hospitality Ventures, shares immune-boosting foods and preparation methods that are fun, flavorful, and invigorating.
PHOTOGRAPHY BY ALISSA DRAGUNBlack Garlic and Miso-Glazed Wild Salmon
INGREDIENTS
MEET THE CHEF
Stephen Asprinio is a Top Chef All-Star, hospitality maestro, and Florida-based restaurateur. As the principal of SA Hospitality Ventures, he has successfully developed and launched projects in Manhattan, Los Angeles, Las Vegas, Washington, D.C., and throughout South Florida.

At the age of 19, Asprinio became the youngest person to ever pass the U.S. Sommelier Association certification exam, and he went on to pass the certificate-level examination from the Court of Master Sommeliers when he was just 21. With degrees from Cornell University’s School of Hotel Administration and The Culinary Institute of America, Asprinio has worked with some of the top restaurateurs and chefs in the country.

Asprinio’s vision is to create multifaceted hospitality experiences that pioneer the next evolution in dining.
2 6-oz. wild salmon filets 3 tbsp. white miso 1 tbsp. black garlic 1 tbsp. sake 1 tbsp. mirin 1 tsp. honey 1 bunch broccolini 1 tsp. grapeseed oil 1/4 tsp. kosher salt
1 tbsp. piquillo pepper (brunoised)
1 tsp. yuzu juice
1 tsp. light soy sauce
Togarashi
1 tsp. white sesame seeds
2 tbsp. micro coriander (substitute cilantro leaves)
In a small bowl, mix the white miso, black garlic, sake, mirin, and honey, and blend with an immersion blender until smooth. Pour the mixture over the salmon, rub on all sides, then marinate in the refrigerator for 4 hours. Next, toss the broccolini with the grapeseed oil and kosher salt, and grill over high heat until lightly charred and still al dente. Cut into 2-inch pieces and toss with piquillo pepper, yuzu juice, and light soy sauce. Season with togarashi to taste and set aside. On a Spanish plancha (preferred), griddle, grill, or under a broiler, cook salmon to the desired temperature (between 120 and 125 degrees is recommended). To finish, spoon the broccolini onto each plate, place the salmon on top, sprinkle with white sesame seeds, and garnish with the micro coriander.
THE IMMUNE FACTOR
All hail the “King of Carotenoids,” aka astaxanthin, which is found at its highest levels in salmon and immensely supports immune function. When combined with salmon’s selenium, zinc, complex B vitamins (3, 6, and 12), and vitamin D, you’re looking at an antioxidant powerhouse. This recipe also features immune-boosting ingredients such as broccolini, red piquillo pepper, garlic, and probiotic-laden miso.

Dandelion Salad with Citrus,
Fennel, and Avocado
INGREDIENTS
8 dandelion leaves (cut into 2-inch pieces)
1 fennel bulb (shaved thin, lengthwise)
4 mixed citrus, e.g., cara cara, blood orange, grapefruit, tangerine, clementine, etc. (supremed, reserving excess juice)
1 tsp. Dijon mustard
2 tsp. honey
1 tbsp. shallots (brunoised)
1 tbsp. sherry vinegar
1 tbsp. lemon juice
4 tbsp. extra-virgin olive oil
1/4 tsp. kosher salt
1/8 tsp. cracked black pepper
1 avocado (sliced into 1/2-inch pieces, crosswise)
6 basil leaves (cut into 1/4-inch strips)
1/4 tsp. Espelette pepper
1/4 tsp. flaked sea salt
In a small bowl, toss the dandelion leaves and fennel with reserved juice from the citrus, then set aside to marinate for 15 minutes. In the meantime, for the dressing, whisk the Dijon, honey, shallots, sherry vinegar, and lemon juice together, slowly incorporating the olive oil until emulsified. Season with kosher salt and cracked black pepper. Toss the remaining ingredients in a large bowl with the dressing. Place the salad in shallow bowls. To finish, sprinkle the Espelette pepper and flaked sea salt over top.
THE IMMUNE FACTOR
Boost your immunity with this mega antioxidant salad derived from the vitamin C–packed citrus, multinutrient avocado, and beta-carotene-rich dandelion greens. Plus, the selenium in the shaved fennel stimulates the production of killer T-cells, modulating the immune system.


Carrot and Coconut Bisque
INGREDIENTS
6 baguette slices (1/8-inch thick)
Olive oil
Smoked paprika
Kosher salt
2 tbsp. butter
1 cup leeks (white part only, thinly sliced)
2 tsp. fresh ginger (peeled, chopped)
2 tsp. fresh turmeric (peeled, chopped)
4 medium carrots (peeled and cut into 1/4-inch pieces)
1 tbsp. vadouvan curry
1/2 cup fresh carrot juice
1/4 cup Riesling
2 cups green tea
1 cup coconut milk (unsweetened)
Sea salt
Freshly ground black pepper
1 lime (halved)
1/2 tsp. sweet soy
2 tbsp. coconut chips
2 tsp. salt-roasted pepitas

2 tsp. crushed peanuts
10 chive sticks
2 tbsp. scallions (julienned, white part only)
On a sheet pan, lay out baguette slices and season with olive oil, smoked paprika, and kosher salt. In a 350-degree oven, bake the baguette slices until golden brown and set aside. In a medium sauce pot, melt butter, then add leeks, ginger, and turmeric, sautéing until leeks are translucent. Add the carrots and cook until soft. Mix in the vadouvan curry, stirring to incorporate for 2 to 3 minutes. Deglaze the sauce pot with the carrot juice and Riesling, and reduce by half. Add the green tea and coconut milk, and simmer for 15 minutes until carrots are fully cooked. Next, blend the soup until smooth and pass through a chinois. Season with sea salt, freshly ground black pepper, and lime to taste, then pour into soup bowls. To finish, garnish each with a drizzle of sweet soy, coconut chips, pepitas, crushed peanuts, chives, and scallions.
THE IMMUNE FACTOR
Can soup enhance your overall protection from evil microbes? Well, this one can. Carrots contain three minerals that are critical to the immune system: iron, zinc, and copper, plus they are full of beta-carotene, boosting the number of white blood cells in the immune system. Not to mention ginger, turmeric, and green tea are all antioxidant superstars.
Hot Rod
Resolution Revolution

















Conquer all your fitness and self-care GOALS FOR 2023 with help from these inspired tools
BY LIZA GRANT SMITHRoom to Board
UFO Sighting


VIP Lounge
Headquartered in Clearwater, Florida, HydroMassage brings an added level of luxury to an already indulgent experience. The ergonomically designed Lounge 440x (starting at $369 per month) uses wave-like streams of heated water to target 60 points on the body and provide temporary relief of minor aches, pains, and muscle stiffness. A touchscreen is programed with a catalog of relaxation videos, music, wellness articles, e-books, and more. (hydromassage.com)


Nerve Verve




Looking to get into stand-up paddling without the space commitment required to store a traditional SUP board? Watersport enthusiasts Corey and Magda Cooper designed the Bote HD Aero Native inflatable paddleboard ($1,149) to transform from backpack-size into a fully functional board engineered for stability in all water conditions. Check one out in person at Bote’s flagship location in Saint Petersburg, Florida. (boteboard.com) and

















The UFO 2 ($300) from Foreo combines thermotherapy, cryotherapy, LED light therapy, and T-Sonic massage in one device for supercharged at-home facials. Use it on its own to reduce the appearance of fine lines, puffiness, or wrinkles. Or pair it with your favorite serum or mask—such as the UFO activated mask or the Foreo sheet mask—to achieve deep hydration. (foreo.com)







Merging neuroscience and technology, the pocket-sized Xen by Neuvana ($450) sends gentle electrical micropulses through patented ear buds to stimulate the vagus nerve, which is responsible for signaling the brain to release calming neurotransmitters in times of stress. Invented by a cardiac surgeon and a team of scientists and engineers based in West Palm Beach, Florida, the Xen device connects to your smartphone through an app, where you can customize sessions with the music of your choice. (neuvanalife.com)




Strike a Pose
CrossFit veterans and Jacksonville Beach residents Haley and Shane Livensparger used PVC pipes as part of their mobility routines, but they couldn’t find any similar warm-up products for Shane to take with him during his travels as a baseball umpire. Their solution is the RomRod ($70), a portable, easy-to-assemble fitness tool that expands to over 5 feet in length and can be used to warm up for a sport, improve flexibility, or practice your barbell technique. (theromrod.com)


Become your own yogi or just look more proficient in class with Grand Basics’ instructional yoga mat ($39). The nontoxic, nonslip yoga mat offers cushioned comfort and a cheat sheet of sorts, with 75 yoga poses and 75 stretches printed directly on its colorful surface. Use the strap to toss it over your shoulder when en route to your namaste destination. (grandbasics.com)



