
15 minute read
Using a New, Modern UI Framework for Inpatient App Keeps Caregivers Rounding Efficiently
Carelign is a responsive web application used during inpatient rounding by a variety of caregivers at HUP, PPMC, and PAH hospitals to help maintain a patient’s care plan and manage handoffs between care teams. Carelign has been used weekly by over 4,000 residents, attendings, nurses, and other clinicians to help facilitate their rounding activity. Carelign was initially developed in 2014 using the JavaScript framework Angular.js.
Over the last few years, Angular.js was no longer supported and has been replaced by other, more modern frameworks. As a result, the Carelign user interface (UI) needed to be re-architected using a newer framework. Because Carelign can be launched from within our EHR, the new Carelign UI also needed to continue to support IE11, the browser that our EHR vendor uses when an application is launched in the sidebar; however, modern UI frameworks no longer supported IE 11 natively.
Advertisement
As a team, Application Development selected Vue.js as our preferred JavaScript framework. With the aid of a consultant, 6 application developers undertook learning Vue.js, redesigning key structures in the Carelign UI to better accommodate Vue.js, and then re-wrote the entire Carelign UI in Vue.js. The team also had to add in backwards compatibility with IE11, and perform an end-to-end test, covering all pathways within the UI. Re-writing Carelign on a new framework extended the life of the Carelign application for at least another 5 years.
TOTAL LOGINS TO CARELIGN DURING THE REPORT PERIOD
2,416,892 59% FROM PENNCHART
872,289 21% FROM DESKTOP
805,624 20% FROM MOBILE
4,094,805 TOTAL
Penn Medicine Welcomes Cedar Avenue Campus to the Health System

For many decades, Mercy Hospital’s West Philadelphia Campus had been an anchor health care institution providing essential services to its surrounding communities. When financial difficulties put the facility at risk of closure in fall 2020, Penn Medicine formed a partnership with Public Health Management Corporation, Children’s Hospital of Philadelphia, and Independence Blue Cross Blue Shield that allowed the healthcare system to maintain clinical operations at that location. Operating under the license of The Hospital of the University of Pennsylvania (HUP), Penn Medicine now provides emergency medicine and behavioral health services at this location. To make this move possible, the IT team partnered with HUP’s executive leadership and the departing health system and successfully replaced all technology associated with the needs of patient clinical care.
Over six months, the IT team worked diligently on a comprehensive plan to install Penn Medicine’s standard information technologies and systems. This effort included the deployment of over 100 health system applications, the training of over 650 new staff members and clinicians, the installation of new lab and pharmacy equipment, and the installation of a telemedicine support system. This project was unique because the team could not complete this work prior to the night of go-live. All information systems were replaced overnight, as the ownership of the building and services transitioned. The hospital remained open throughout the transition and continued to provide care to the community.
Because the transition to standard processes and computer systems was completed overnight, Penn Medicine was able to forgo a costly transitions services agreement, which resulted in notable cost savings for the health system. Extending our electronic health record, clinical imagining systems, human capital management systems, the use of Penn Medicine’s existing network infrastructure and telephony services allowed for reduced costs for licensing and professional services as well as considerable time and cost savings.
Penn Medicine Acquires Tower Health Transplant Institute, Expanding Access to World-Class Care
In December of 2021, Tower Health Transplant Institute and related transplant nephrology and hepatology practices transitioned to Penn Medicine. As part of the careful integration of both programs into the healthcare system, Tower Health transplant surgeries transitioned to the Penn Transplant Institute at the Hospital of the University of Pennsylvania in Philadelphia. The kidney and liver transplant programs were fully integrated with the Penn Transplant Institute, resulting in the Penn Medicine Regional Transplant program at Reading Hospital. The new regional transplant program has continued to provide high-quality patient screening and pre- and posttransplant kidney and liver care within central Pennsylvania.
Due to the acquisition, Penn Transplant Institute expanded to 4 locations, with a new location in Philadelphia on the Broad Street corridor. This transition required the replacement of all technologies with Penn Medicine supported devices. The IT team provided a robust infrastructure and hardware platform to support three clinical operations which allowed for the seamless transition to the Penn Medicine’s EHR application within a 4-month window.
Gastroenterology & Endoscopy Expands at Penn Presbyterian Medical Center











Penn Presbyterian Medical Center’s Gastrointestinal/Endoscopy department outgrew its existing space and expanded its operation. The department relocated to a new space across the street from the Penn Medicine
University City building, moving both the clinic and outpatient endoscopy procedure unit. The new space included four procedure rooms and nine prep/recovery bays, allowing for some of the clinical space at PPMC to be redeployed for additional use. Numerous IT teams were involved in this successful expansion which resulted in increased patient procedure volumes.
Mobile 3D Mammography Screenings for At-Risk Residents in North and West Philadelphia

Penn Medicine partnered with Siemens to offer free breast cancer screenings to women in need, over the age of 40. This program provided a valuable service to underserved communities, addressing health disparities. A 54-foot-long mobile mammography unit featured the company’s MAMMOMAT Revelation digital mammography system, accredited by the American College of Radiology, and provided state-of-the-art mammography’s.
“Cancer disproportionately impacts lower socioeconomic groups and the medically underserved because they are unable to access cancer screening tests, and thus more likely to be diagnosed with late-stage cancer. This mobile mammography initiative is one of many efforts we have committed for engaging underserved communities with access to important healthcare resources and education.”
Carmen Guerra MD, Vice Chair of Diversity and Inclusion, Department of Medicine at University of Pennsylvania
The first engagement took place in mid-October 2021 during Breast Cancer Awareness Month at 21st Street and West Allegheny Avenue. The second event was held in June 2022, in partnership with the Church of Christian Compassion and its annual health street fair at 61st Street and Cedar Avenue. By bringing the mobile mammography unit to locations in Philadelphia, the program provided mammography services for women who may not have otherwise access to this type of care.
HUP Pavilion Elevates the Inpatient Patient Experience with Iris Careboard and Outside Door Displays













The vision behind designing the new patient Pavilion at HUP has been to create a state of the art ‘hospital of the future’. Included in this vision, from a technology approach, were two key components:
» Designing an electronic patient whiteboard, called Careboard, which replaced the physical whiteboard typically present in a patient room. The Careboard was developed to automatically update from our PennChart EHR with key information of interest to the patient and the patient’s family, including pictures and names of key members of the patient’s care team. The Careboard design was encompassed in part of a larger footwall monitor that also includes a television and countless other features.
» A touchscreen outside door display device was mounted outside each patient room to display key safety and precaution information for staff and visitors before entering.
Integrating the digital display of clinical systems to the staff was designed to improve patient care and provide a connection between the patient, the family, and the care providers of every specialty who entered the patient room. From the doctors and nurses to the therapist and social workers, to dietary and environmental service workers - all healthcare workers were integral to helping our patients feel part of the care team to manage their care and get well again. By integrating both the Careboard and outside door display with the EHR, patients and staff automatically received the latest information. Staff were also relieved of the onus of updating the whiteboard and of hanging/removing various safety signs outside the door of the patient’s room.
Working with the HUP technology and clinical committees, we identified the key pieces of patient data to be included on both the Careboard and outside door display. Then, working with our low-voltage integration partners, UPHS Application Development designed the mechanism for displaying the Careboard and outside door display—both web pages—on their respective devices. Application Development analysts further worked with the EHR team to acquire patient data needed for the Careboard or outside door display that they did not already have.
Unlike most web pages, the Careboard was designed with no input device. This meant that the ability to refresh it, to detect if it had become unresponsive, and to refresh it, each had to be built into the architecture of the web page and the device that controlled the footwall.
The outside door display would, however, have an input device—it is a touchscreen—so we were able to build into it two additional features: first, the ability to get more information about a selected icon by tapping on it, and second, the ability to put the device into “diagnostic mode” to assist with troubleshooting.

Clinicians began receiving real time information about the patient from the outside door display, which is also fed from the EHR. It replaced manual workflows indicating when a patient is in isolation, at risk of falling, or risk of seizures, among other vital information. It was also designed to inform a team member prior to entering the room if the patient has any communication challenges or needs assistance with activities like feeding. The outside door display was constructed to keep both the patients and clinicians safe from exposure to infectious diseases and harmful environmental conditions unique to each patient, like not bringing flowers into a room where a patient is neutropenic or latex balloons to a patient with a latex allergy.

Using technology to transform the delivery of care and develop a patient centered approach resulted in the ability to foster cutting edge medicine toward new medical innovations and advances. Automating the precautions and warnings using the outside door display has saved clinicians from manually hanging thousands of caution signs outside the rooms of patients since the HUP Pavilion opened.
Anecdotally, displaying the Careboard on the monitor facilitated discussion among the patient, patient’s family, and care team, providing valuable opportunities for education and feedback. Patients also reported increased satisfaction at knowing exactly who has just entered their room along with a certain “wow” factor that is apparent the first time anyone sees the system. The innovative technology engages the patient, which has been noted to improve patient experience and health outcomes.
Penn Genomics Results Portal Enables Genetic Counseling Sensitivity for Patients
The Application Development team implemented a web portal solution for the processing of genetic test results so that genetic counselors would receive exam results before being released to patients. Designing this technology workflow allowed genetic counselors to interpret the results first and plan their counseling approach appropriately for the patient expecting the results.
Genetic counselors signified the importance of creating the proper channel for delivery of information and counseling for patients learning their genetic test results. In some cases, these results which could confirm a lifelimiting diagnosis, were previously being released to patients without benefitting from this important expertise and opportunity for patients to be better advised as to the significance of the results.
At Home Colon Cancer Patient Screening Increases Patient Monitoring
Colon cancer screening is essential for early detection and treatment. Penn Medicine primary care and select specialty providers offer adult patients, who are over 45 years old and at average risk for colon cancer, the option to screen for the disease using at-home testing. The at-home test option uses DNA markers and blood in the stool to screen for colon cancer.
To expedite the submission and attainment of test results into a patient’s electronic health record, and to eliminate the need for in/out bound faxes, an IT team was formulated to develop an outbound orders interface and solicit result interfaces to support at home testing integration into the EHR. The project resulted in:
• The creation of a new interface/orders results anywhere (ORA), the first ever at Penn Medicine
• Re-purposing an existing EHR ambulatory order and configuring the order transmittal rule Partnering with Community Connect sites for integrated testing
• Partnering with Primary Care service line, GI and OB/GYN service lines
• Partnering with myPennMedicine to validate patient can receive the integrated results
• Integrating results to populate Health Maintenance topics. The results indicate a positive, negative, or inconclusive test result in the EHR
Transitioning from a manual process to an integrated workflow yielded the following benefits:
• Positive impact on patient care – faster processing, delivery and turnaround of results and integration with myPennMedicine
• Improved workflow for technicians and providers
• Reduced inefficiency and associate satisfaction
• Trackability of test kit workflow and completion metrics
• Elimination of 200+ weekly faxes
• Reduced time spent by staff sending and processing orders
The at home testing interface went live on December 7, 2021. Approximately 200 orders were placed electronically during the first week, with 9497 additional orders placed through the end of fiscal year 22. This development highlights the importance of colon screening and the critical role of technologies in enhancing the screening process.
LGH Launches Colorectal Cancer Detection Proactive Screening Program












At LGH, a new colorectal cancer screening outreach campaign was made available to relevant patients. Technologists developed an automated, text-based, patient identification and cancer screening workflow which aligned with a patient’s birthday, for those 50 years old and above. The workflow was coordinated with colonoscopy referrals to various GI practices with automated FIT (fecal immunohistochemical testing) for those who declined colonoscopy. Document workflow for program support staff was also included. For patients enrolled in the FIT testing, automated reminder texts were sent out at specific intervals to encourage completion.
Program goals were set to improve the overall colorectal cancer screening rate and targeted improving health outcomes by detecting cancer earlier and increasing patient engagement toward their health. This project also sought to streamline current outreach methods and ease the burden from the individual practices by measuring screening completions in total and across key demographics to ensure that the program strategy was equitable.
There were more colonoscopy and FIT completions and clinical time for the staff was recouped due to this project. Employment of the campaign resulted in a 2% increase in patient engagement from 73% at go-live in August 2021 to 75% in May 2022 (1,500 additional patients screened in 9 months); exceeding the goal by a full percentage point.
New Addiction Medicine Services Help Patient Population Struggling with Substance Use
The LGH Behavioral Health Service Line created an Addiction Medicine program to improve access to evidenced based care for patients with opioid use disorder and other substance use disorders. Originally, this project was piloted to determine the need and assess the proof of concept, which led to additional rollout of regional sites that now support the broader community.
This addiction medicine division established the required processes for management and billing for the new practice sites. The addiction medicine providers and care management team have operated from a defined hub and spoke model of delivery in the areas and offices in which patient populations have been most comfortable.
The LGH eHealth team built out and deployed the substance use specific documentation tools, scheduling, and billing workflows to 35 departments spread across the primary care network to allow for improved access to care and to support regional care management delivery.
Establishing this addiction medicine program increased revenue through the creation of multiple regional practice locations which increased appointment availability. The additional departments also optimized billing for care management services delivered to patients served by both addition medicine providers and primary care providers. The referral process was optimized in support of more timely access to care for patients during the continuing opioid epidemic.
Managing the Opioid Crisis Toward Better Healthcare Outcomes



Nationally, practice varies widely and opportunities to treat patients for Opioid Use Disorder (OUD) are missed due to difficulty identifying OUD patients, and not having a consistent workflow for initiating MOUD (Medications for Opioid Use Disorder) treatment among care providers. Substantial best practice evidence-to-practice gaps in treatment with medication for OUD existed.
Penn Medicine implemented an ED nurse driven triage screening protocol for OUD, wherein a positive screen triggers targeted electronic health record prompts to assess for withdrawal and initiate buprenorphine treatment.





An increase in positive OUD screen rate identified additional patients for ED triage screening and treatment protocol which led to increases in assessment and treatment with MOUDs. Protocols were designed to identify patients and prompt treatment, making treatment the default. These protocols show promise in increasing implementation of standard and consistent evidence-based treatment for Emergency Department OUD care.
An Opioid Use Disorder dashboard was also developed to measure key quality metrics for OUD care; including use of evidence-based medication treatment, prescription of Naloxone for overdose prevention, and patientdirected discharges.


The OUD dashboard allowed measurement of outcome across Penn Medicine Emergency Department and hospitals to target opportunities for improvement and to measure progress in treating OUD patients. We could also identify equity issues, including racial and other disparities in outcomes. This tool became invaluable for targeting and tracking progress of new initiatives, including an addiction medicine consult service (piloting in 2023).
There is wide variability in a patient’s opioid needs after surgery, leading to a tendency to prescribe enough pills to cover the most severe anticipated needs. However, many patients end up with more opioid pills than needed which results in excess opioids in the community. An automated text messaging system was used to collect patients’ self-reported number of opioid pills taken after surgery. Eligible patients received automated text messages at specific days after the procedure asking a series of questions including pain intensity, number of opioid tablets used, and the number remaining. A recommendation to reduce the default number of pills was made and implemented. This keeps less unused prescribed pills in the community.
Patients who had lower pain scores at discharge and who were opioid naïve had lower post-op opioid consumption and were more likely to have pills left over. This information enabled the team to create nudges to prescribers and automated clinician feedback to encourage prescribing changes when appropriate.


Provider specific feedback was developed showing an individual’s prescribing metrics. The graphical view format provided straight forward comparison with target levels, their practice, and health system peers. Next generation guidelines will help clinicians make better prescribing decisions.

A Naloxone best practice alert was created and implemented to trigger when an opioid order overreaches a particular threshold. Co-prescribing Naloxone decreases risks of adverse events.
Patients that were prescribed opioids and met evidence-based criteria for increased risk of OIRD were listed for pharmacist triages to perform individual provider outreach for patients on the list – suggesting alternative analgesics, naloxone co-prescribing, sleep medicine consult/follow-up.
In addition to identifying patients at risk for OIRD and working with their attending providers, the technical development team added those patients to a co-prescribing best practice advisory that flag prior to discharge, created a workflow to ensure co-prescribing to the identified patients at risk for acetaminophen toxicity and updated order sets to provide the appropriate alternative.
Improving Hepatitis C Screening, Linking to Care During Hospitalization
The Center for Disease Control and Prevention and United States Preventative Services Task Force recommend one-time universal screening for hepatitis C for all adults over the age of eighteen. In addition, Pennsylvania law mandated hepatitis C screening for people born between 1945 and 1965. To improve hepatitis C screening, Penn Medicine implemented the automatic hepatitis C screening among previously unscreened patients who were born between 1945 and 1965, from the default order embedded into admission order set at HUP and PPMC. The Hepatitis Linkage Team was notified of all positive tests through a PennChart EHR mobile push notification. The team then followed up for test result disclosure, education, and among patients with hepatitis C viremia, linkage to curative treatment at timely manner.
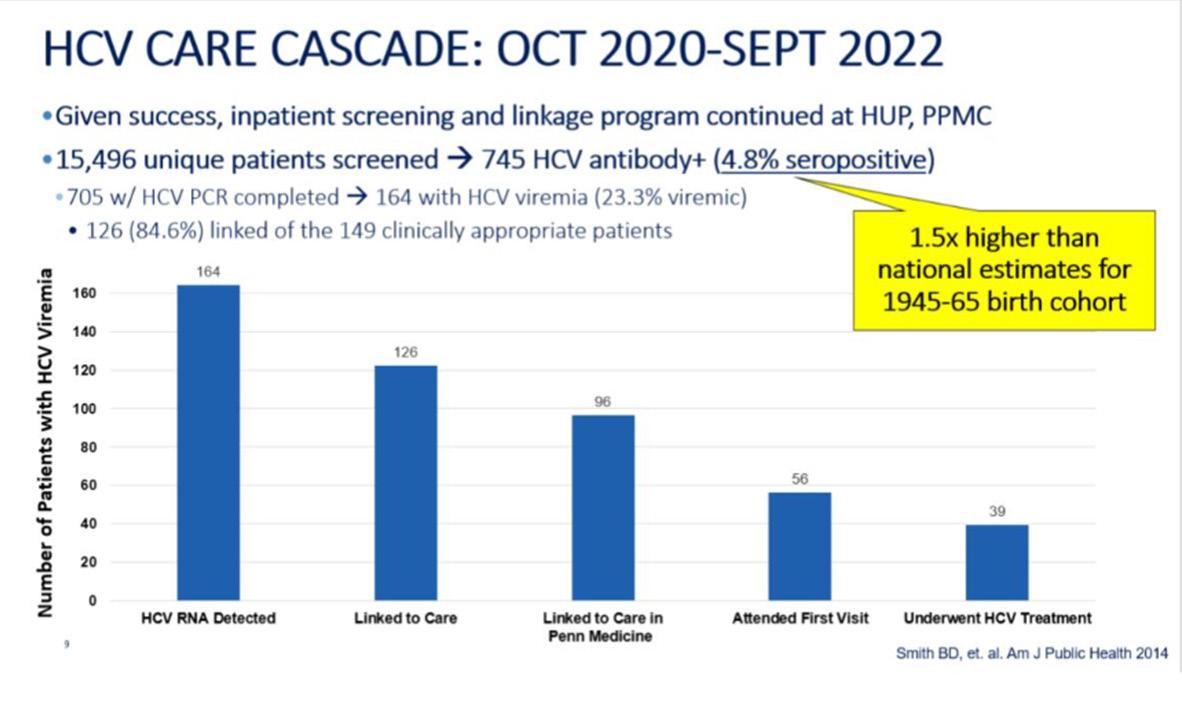
With this universal screening approach, 15,496 unique patients were screened between 9/2020-9/2022 and identified 164 patients with HCV (Hepatitis C virus) viremia status. The linkage group followed up with 126 patients and 39 patients underwent HCV treatment. Due to the multidisciplinary collaborative approach, we satisfied the Pennsylvania HCV screening and linkage mandate (2016 Act87), provided sustained increased HCV screening, and improved patient care quality.
A universal ordering process was developed using an admission order set typically used for all patients upon hospitalization. The HCV order was auto populated for all patients born between 1945-1965 with no prior HCV testing in Penn Medicine and no report of HCV on their problem list. Clinicians could opt out of the testing if it were not clinically indicated from the order set. Additionally, the technical team embedded the EHR result, and documentation follow up process in PennChart, so the hepatitis C linkage group facilitated a treatment and follow-up care plan in a timely and effective way.
The new order approach contributed to an increase in HCV test completion by 31.8%. A total of 15,496 unique patients were screened from October 2020 to September 2022. There were 745 HCV antibody positive patient cases identified. 4.8% were seropositive cases which is 1.5 times higher than national estimates for the 1945-1965 cohort. Of 745 patients, 705 HCV PCR tests were completed and 164 were identified as HCV viremia (23.3%). The linkage team followed up with 126 (84.6%) patients for the next step of the plan. 39 patients underwent the HCV treatment. This universal ordering model and the linkage follow-up demonstrates support for continuity of patient care and engagement while being done efficiently.










