FALL 2011
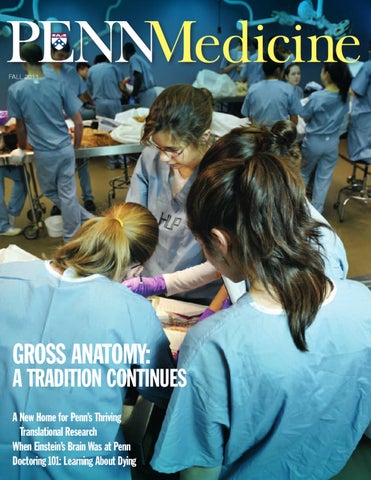
GROSS ANATOMY:
A TRADITION CONTINUES A New Home for Penn’s Thriving Translational Research When Einstein’s Brain Was at Penn Doctoring 101: Learning About Dying
FALL 2011
GROSS ANATOMY:
A TRADITION CONTINUES A New Home for Penn’s Thriving Translational Research When Einstein’s Brain Was at Penn Doctoring 101: Learning About Dying