
























The recent arrival of non-surgical equipment targeted at primary eyecare professionals and a willingness to diversify optometry businesses through more privately billed services are driving greater interest in cosmetic procedures among Australian optometrists, Optometry Australia says.
However, practitioners seeking to broaden their scope by o ering non-surgical, eye-related cosmetic services are being urged to consider any implications around their professional indemnity insurance (PII) cover, and remain on top of proposed regulations set to determine how such services can be marketed to the public.
The notion of optometrists performing cosmetic services is nothing new, but the advent of
intense pulsed light (IPL) therapy and – during the past 12 months – new bipolar radiofrequency and micro needling to rejuvenate the periorbital region from aesthetics company InMode have prompted renewed interest in the area.
The trend has already taken o in the US where the industry has coined the term “ocular aesthetics”. Historically, these services were limited to surgeries such as blepharoplasty and other eyelid procedures such as ptosis, entropion and ectropion, but new non-surgical methods have allowed optometry to enter the picture.
OA chief clinical o cer Mr Luke Arundel concurred, telling Insight the recent release of new non-invasive and non-surgical equipment for cosmetic procedures

privately billed services, which is an area Optometry Australia has been active in supporting members to introduce, with many resources available in this area on our website,” he said.
Arundel said Australian optometrists had been performing cosmetic procedures for many decades, including cosmetic shells or lenses for damaged or disfigured eyes, and coloured contact lenses.
was likely the primary driver for some OA member optometrists to consider broadening the range of services they o er to patients.
“Many practices are also looking to decrease reliance on dispensing income through o ering a range of
“Or, as far as Medicare is concerned, fitting prescription contact lenses to any patient under +/- 5.00D,” he said.
“Optometrists have for many years also been assisting dry eye patients through application of IPL. Treatment of vascular lesions like rosacea may
continued page 8
The average number of hours a RANZCO trainee works has climbed to 53.3 a week – the highest for ophthalmology trainees in the five years of the Medical Training Survey (MTS) – and almost eight hours more than the average Australian doctor in training.
While long work hours remain an issue, the next generation of eye doctors are more likely to feel positive about their prospects of passing their course, securing employment, and are less likely to be considering a career outside of medicine.
The insights from 68 RANZCO trainees were contained in the 2023 MTS that received 23,298 responses at a rate of 55%. It’s the fifth nationwide survey of all doctors in training and is a
confidential way to obtain national, comparative, profession-wide data to strengthen training.
The latest snapshot revealed ophthalmology still ranks well in terms of trainees recommending their position to other doctors – 82% of RANZCO trainees versus the 80% national average, however this is significantly down on other years (89% in 2022 and 94% in 2021).
When it comes to their workload, RANZCO trainees reported much higher strain compared to other trainee doctors, with 43% rating their workload ‘heavy’ (vs 38% national average) and 16% heavy (9% nationally).
“On average, RANZCO trainees worked 53.3 hours a week, compared
to 45.6 hours a week for the national average,” the report noted. “For RANZCO trainees, 88% were working 40 hours a week or more, compared to the national response of 64%.”
The survey also delved into the impact of unrostered time. When this occurred, 70% of ophthalmology trainees received payment for this (vs 68% nationally). Thirty-two percent said it had a negative impact on their training, against the 22% national average.
The national report revealed what the Australian Medication Association (AMA) has described as an “extremely concerning” number of trainee doctors considering a career outside of medicine (19%).
continued page 8
"'Interventional glaucoma' is all about diagnosing and treating earlier, being more proactive and perhaps using more aggressive treatments at an earlier stage in the disease,” says Sydney specialist Dr Colin Clement.
40




ZEISS
AU: 1300 365 470
NZ: 0800 334 353







• Experience chamber stability independent of IOP and flow
• Virtually eliminates post occlusion surge: IOP recovery in about 200ms
• Digitally integrated surgical workflow
zeiss.com/quatera700







One of the joys of putting this issue together was our interview with Ms Nandita Chowdhury, who opened her Picton Eyecare greenfield practice a little over a year ago with already incredible results.
As corporatisation of the optometry market continues, Chowdhury's story (page 20) is a breath of fresh air for the independent scene, and an example of the opportunity that awaits in private practice if executed well.
While some independents at the end of their career are selling to groups – as is their prerogative – it’s interesting to note a wave of early- to-mid career optometrists seeking a new challenge through independent ownership. In fact, there’s at least 117 of them going o ProVision’s Associate Program that educates prospective owners about the commercial aspects of practice ownership. The program also acts as a match-maker to facilitate the succession between retiring independents and aspiring owners – thereby keeping the independent market intact.
In Chowdhury’s case, ProVision walked her through the exhaustive checklist of going greenfield. It’s an avenue that – despite its inherent challenges – is of growing interest among next-gen owners. Oftentimes, with the influence of consolidators, solo operators are increasingly being outbid – and if they win, there’s a chance they’ve paid too much.
Therefore, greenfield become a more realistic option. To thrive, they need to nail the fundamentals. Location, capital, good sta , and a willingness to roll up the sleeves are the qualities that stand out in Chowdhury’s case, making Picton Eyecare one of the most successful greenfields of late. But also, independents have an edge by delivering a personalised experience that’s hard to replicate over many years with the same practitioner. There’s also an opportunity to commercialise more time-intensive special interests, and access to a great network of pro-independent suppliers o ering di erentiated frames and lenses.
Corporate or independent, each plays a vital role in our industry, but the strength of independents is vital for competition and consumer choice. To maintain its foothold, greenfields are one solution, but the other is carefully mapped out succession plans that continue not only the legacy of the practice, but the independent market as a whole.
MYLES HUME Editor









Just as Insight went to print, EYERISING INTERNATIONAL says its device has been “misrepresented” in a recent Ophthalmic & Physiological Optics study over the safety of low-level red-light (LLRL) in myopia management. The company has provided four counter points to the paper that said "clinicians should be cautious with the use of LLRL therapy for myopia in children until safety standards can be confirmed". Eyerising took issue with several
references to its device “in a negative and inaccurate manner; despite having not tested the device or contacted Eyerising International for information or comment”. IN OTHER NEWS, Australia Day Honours were announced for three members of the ophthalmic community. Emeritus Professor Christian Joseph Lueck was awarded Member of the Order of Australia (AM) in the General Division for “significant service to neurology and neuro-ophthalmology through medical research and clinical practice”. Retired Melbourne optometrist Mr
Michael John Aitken received a Medal of the Order of Australia (OAM) for his service to optometry while Ms Sandra Elizabeth Knight was awarded an OAM for her service to people who are blind or have low vision. FINALLY, global eyewear company Safilo – a major supplier to Australia’s independent optometry market – renewed licensing agreements with several brands. These include the HUGO BOSS collections until December 2023, Levi’s branded eyewear until the end of 2029, and Moschino and Love Moschino eyewear collections until December 2033.
New research from Dartmouth College and the University of St Andrews has outlined how the capacity of reindeer to see light in the ultraviolet spectrum helps them to distinguish lichen – their o -white food source – from snow.
“Reindeer don’t want to waste energy wandering around searching for food in a cold, barren environment. If they can see lichens from a distance, that gives them a big advantage, letting them conserve precious calories at a time when food is scarce,” the researchers said.
University of Sydney engineering honours student Ms Phoebe Peng is developing technology to allow people with low vision and blindness to play ping pong. The process uses event cameras that track changes in an image over time, making them ideal for the observation of small objects. The images are then processed into sound using a specialised algorithm. This is then communicated back to the player via an array of loudspeakers, ultimately with the aim of allowing players to track the ball and movements acoustically.
WACKY
A Veterinary Sciences study has shown endangered fish can live longer after cataract surgery. The researchers performed lensectomies on 11 fish belonging to three at-risk populations. “Our results show that 73% of the operated fish resumed feeding, regained normal body condition and appeared clinically normal. The median survival time was around one year, which is a positive outcome for fish of this age,” the researchers said.

Australian volunteers with Cambodia Vision recently screened 3,589 Cambodians, provided 551 prescription glasses, thousands of sunglasses and 564 surgeries, mostly for cataract. Page 57.
THIS MONTH WAVE 2024
16 17 MARCH
The event returns in Fremantle, WA, presented with Optical Dispensers Australia featuring a one-day dispensing program alongside a two-day optometry conference.
admin@optometrywa.org.au
Complete calendar page 68.
NEXT MONTH AVC 2024
6 7 APRIL
Australian Vision Convention will be held at the Gold Coast Convention and Exhibition Centre for optometrist delegates from across Australia and New Zealand.
events@optometryqldnt.org.au
insightnews.com.au
Published by: 379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766 www.primecreative.com.au
Chief Operating O cer
Christine Clancy christine.clancy@primecreative.com.au
Group Managing Editor Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Journalist April Hawksworth april.hawksworth@primecreative.com.au
Commissioning Editor, Healthcare Education Je Megahan
Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Salma Kennedy salma.kennedy@primecreative.com.au
Design Production Manager Michelle Weston michelle.weston@primecreative.com.au
Head of Design Blake Storey
Art Director Bea Barthelson
Subscriptions T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright – No part of this publication can be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.
continued from page 3
be an obvious complimentary adjunct with dry eye therapy. While in the early days, we will be monitoring with interest use of new devices in Australia which may be able to assist with non-surgical blepharoplasty through RF microneedling.”
Arundel said OA had fielded inquiries through its Optometry Advisor Help Desk, with optometrists curious about regulation, scope-of-practice, advertising rules and restrictions and coverage for techniques through PII.
Regarding the implications for PII, he added: “It would be sensible for optometrists to seek advice from their professional indemnity insurance provider, or financial advisor to ensure their PII covers all the techniques they wish to use if considering expanding into cosmetic work.”
Meanwhile, the Australian Health Practitioner Regulation Agency (Ahpra) is putting non-surgical cosmetic procedures under the microscope that will likely lead to clearer rules around who can perform them and guidelines on advertising.
Amid the crackdown, there is expected to be tighter regulations around the use of testimonials and how before and after images are used to demonstrate results.
Ahpra is concerned about the non-surgical cosmetic sector due to what it described as a lack of clear information
about the qualifications and experience of practitioners, and advertising that minimises the risk and complexity of procedures or implies unrealistic results.
It’s also worried about the number of young and potentially vulnerable people seeking out non-surgical cosmetic services, financial gains that can sometimes outweigh patient wellbeing and safety, and ongoing cost and frequency of procedures to maintain outcomes.
Arundel said with this review under way, optometrists looking to move into non-surgical cosmetic services should be aware that current guidelines may change in the near future.
“As part of the association’s strategic plan to lead the sector, Optometry Australia does input into all consultations a ecting optometrists and this consultation has been recently been extended to accommodate for the holiday season, with submissions closing on 1 March 2024,” he said.
“In addition, new National Safety and Quality Cosmetic Surgery Standards were launched late last year, following broad consultation with consumers, clinicians, services, professional and peak bodies, regulators, and other representatives of the sector. These standards aim to protect the public from harm and improve the quality of cosmetic surgery in Australia.”
• In September 2022, an independent review is released regarding regulation

“WE WILL BE MONITORING WITH INTEREST USE OF NEW DEVICES IN AUSTRALIA WHICH MAY BE ABLE TO ASSIST WITH NONSURGICAL BLEPHAROPLASTY THROUGH RF MICRONEEDLING.”
LUKE ARUNDEL, OPTOMETRY AUSTRALIAof medical practitioners performing cosmetic surgery and made 16 recommendations – that were all accepted Ahpra and the Medical Board.
• In July 2023, the Medical Board’s new guidelines for doctors performing cosmetic surgery came into e ect.
• Ahpra noted: “The comments by the independent review that the cosmetic surgery sector ‘is unique and somewhat of a health market disrupter, largely sitting outside of the existing health system frameworks’ are equally relevant to non-surgical cosmetic procedures.”
• For example, Medicare item numbers are not available for non-surgical cosmetic procedures, these procedures are not o ered by the public health system and they are generally not covered by private health insurance.
• The draft guidelines emphasise practitioners’ responsibilities around informed consent, including financial consent, and consideration of patient suitability, including assessment for underlying psychological conditions such as body dysmorphic disorder (BDD).
• Ahpra said inappropriate advertising of non-surgical cosmetic procedures has the potential to pathologise normal changes in appearance, exploit vulnerabilities or insecurities of individuals, contribute to poor body image and create unrealistic expectations.
• Consultation ended 1 March 2024.
continued from page 3
Fortunately for ophthalmology trainees this was just 7%. And, overall, 98% of RANZCO trainees versus 94% nationally intended to continue with their specialty.
When asked if they were concerned about not successfully completing their training program to attain fellowship, meet pathway requirements or securing place in their preferred college training program, 7% of RANZCO trainees harboured concerns against 35% nationally.
Unsurprisingly due to a strained ophthalmology workforce, a lower proportion (15%) of ophthalmology trainees said they were concerned about securing employment on completion of training against 40% nationally.
A concerning finding from the 2021 MTS found that one in five ophthalmology trainees have experienced bullying, harassment and discrimination, with 92% opting not to report it. These figures have since improved, with the 2023 survey finding that although a similar proportion had experienced these issues, 40% of alleged victims reported this behaviour, while 21% who witnessed it reported it.

dissatisfaction with examination feedback.
“We know for a fact there is a link between the wellbeing of healthcare sta and patient care. Our patients deserve to know they are in the hands of healthcare workers who are supported and enabled to provide the best care possible,” he said.
Robson said many of the issues in the survey were a result of the overall logjam in the hospital system.
Another interesting workplace culture finding in 2023 saw 69% of RANZCO trainees believe their workplace had a positive culture versus 80% nationally.
Commenting on the 2023 MTS, AMA president Professor Steve Robson said trainee doctors were su ering from the burden of heavy workloads, problems in workplace culture and a higher level of
“It’s not exactly rocket science — the ability to support medical workforce wellbeing, training and education are significantly impacted by overall health system capacity,” he said.
“Governments across the country need to better fund healthcare and show our workforce that Australia values them and wants to provide the necessary resources to ensure they can perform at their best.”
The Australian Medical Association (AMA) has released its '2023 Private Health Insurance Report Card' showing the rebates for identical procedures still vary wildly between insurers, with a 6% variation identified for cataract surgery.
The peak body’s president Professor Steve Robson encouraged consumers to carefully consider which private health insurance option is best for them, with a focus on products that deliver treatment they are most likely to need in the future.
“Our report card highlights the importance for consumers to look closely at their options, as the benefits can vary dramatically between insurers for the exact same product,” he said.
“For the uncomplicated delivery of a baby, we uncovered a dramatic 30% variation of rebates between the highest and lowest paying insurers. That is a staggering $520 di erence, which would understandably cause much frustration and confusion for patients when looking for insurance.”
An analysis of the most common
procedures showed the benefits paid for cataract surgery as of 1 November 2023 varied from $1,341 to $1,266. Although this represented a sample of health insurers, this was a 6% di erence and among the lowest variation rates in the report.
“When there is a di erence between the doctor’s fee and the insurance benefit, out-of-pocket costs can occur. It is a common misunderstanding that the doctor’s fee is the reason for an out-of-pocket cost, but the reality is that there can be a large di erence in the amount an insurer will pay towards a medical service, and it varies from fund to fund and procedure to procedure,” the report stated.
“These di erences contribute to di ering out-of-pocket costs paid by patients and point to the importance of looking beyond the premium charged for di erent policy products to ensure you get value for money.”
Robson said the report card also showed the need for a Federal Government mandate that would require every insurer to return a minimum amount to patient care

Benefits for cataract surgery varied from $1,341 to $1,266. Image: Warren Scherer/ Shutterstock.com
each year. In 2022-23, the AMA said gross insurer surplus from hospital insurance was about 18% of hospital premiums paid – an increase of $1.36 billion from the 2020-21 financial year.
But, the proportion of hospital insurance policy premiums returned to patients fell to 81% in 2022-23 –down from 88% in 2018–19.
“The reality is the value many consumers receive from their private health insurance is declining, relative to the big profits insurers are making,” Robson said.
Acknowledging rising premiums in 2024, CEO of Private Healthcare Australia Dr Rachel David said health funds had made this request to the government to due to inflation, record claims over the past year, and additional costs such as IT upgrades to combat cyber-attacks.
“The cost of medical and hospital services increased 5.9% this year and there’s been a 9.6% surge in hospital admissions funded by insurers. This is putting pressure on premiums,” she said.




Five patients have been left with permanent vision loss and five remain critically ill after complications arising from cataract surgeries at a hospital in the Indian state of Gujarat. Out of the 20 patients, 10 have shown improvement, with two regaining their vision completely and eight exhibiting gradual recovery, according to media reports. However, five have su ered extensive infections rendering them with permanent vision loss. “Despite our best e orts, including intensive treatment with antibiotics, injections, and medication, the damage caused by the infections is irreversible,” said a senior doctor at the institute. The infections are now the focus of multiple investigations.
A new Israeli-based cross-sectional study has revealed a link between males with keratoconus and attention-deficit /hyperactivity disorder (ADHD). As eye-rubbing has been shown to trigger onset and progression of keratoconus, the researchers sought to identify a potential link between various psychiatric disorders associated with heightened sensitivity and the disease. Published in JAMA Ophthalmology, the study included 940,763 adolescents and adults who underwent systematic medical and ophthalmologic evaluation. The researchers examined the prevalence of keratoconus among patients with anxiety, obsessivecompulsive disorder (OCD), autism and ADHD. A total of 1,533 participants were diagnosed with keratoconus, equivalent to a 0.16% prevalence. Patients with keratoconus were found to be 1.58 times more likely to be diagnosed with ADHD than the general population.
The World Council of Optometry (WCO) will celebrate World Optometry Week 2024 with the theme: 'Advancing optometry’s commitment to global eyecare'. The awareness week will be held from 17 to 23 March, including World Optometry Day on 23 March, which serves to highlight the profession’s role in promoting the adoption of Integrated People-centered Eye Care (IPEC) in countries’ health systems, as recommended by the World Health Organization (WHO)’s 2019 World Report on Vision. “I am encouraged to see how optometry is embracing the need to address the large burden of preventable vision impairment,” WCO president Dr Sandra Block said. “We continue to educate our patients as well as stakeholders who understand the importance of access to quality eyecare. Optometry has taken a leadership role in addressing the many challenges.”

Optometry Australia (OA) has made several requests ahead of the 2024-25 Federal Budget, outlining a pathway to accessible and a ordable eyecare with investments in collaborative care models, tele-optometry Medicare items and public campaigns to raise awareness of the myopia epidemic.
With vision loss said to cost the Australian economy $27.6 billion annually, the submission focuses on “practical, low-cost initiatives” that address structural and systemic issues impacting the ability of optometrists to deliver eyecare services to disadvantaged Australians, OA stated.
“In many geographic locations and disadvantaged communities, patients wait inordinate lengths of time or go without treatment altogether. Without substantive action, this problem will only worsen,” the submission said.
OA cites overstretched public hospitals, long wait times for elective surgery and outpatient appointments, significant out-of-pocket costs, specialist workforce shortages – particularly in regional and rural areas – and ine ective patient pathways as contributing factors to many Australians not being diagnosed or treated in a timely manner.
In 2023, RANZCO, Optometry Australia and Orthoptics Australia jointly announced a cross-discipline collaborative eyecare working group to enhance patient access, reduce wait lists and wait times, and lower health system costs.
“The crucial next step is to resource the next phase of collaborative eyecare in a way that builds on these successful projects," the submission said.
OA CEO Ms Skye Cappuccio said that with an ageing population and the increased prevalence of chronic eye conditions, there is a need to maximise opportunities to increase the contribution of optometry in the health system.
“Optometry Australia’s 2024-25 Pre-Budget Submission focuses on three overarching areas of strategic importance to patients and the future of the profession,” she said, including:
1. Adjustments to optometrists’ remuneration under Medicare, through a review of optometric scheduled fees that have not kept up with inflation, along with the fasttracked establishment of telehealth items for brief and comprehensive tele-optometry consultations, and
asynchronous tele-ophthalmology consultations. Analysis of practice costs indicate the actual cost of providing a comprehensive consultation is over $30 more than the Medicare scheduled fee.
2. Investment to embed innovative, collaborative models of eyecare in the health system, enabling optometrists to practise in a multidisciplinary treatment environment, underpinned by shared data and enhanced use of digital technologies.
3. Funding for targeted initiatives to deliver benefits in areas of need. These include:
• Increasing the optometric domiciliary loading to $85.00 per visit (paid proportionally for multiple patients) to ensure access for elderly Australians in aged care
• Increasing investment in the Visiting Optometrists Scheme (VOS) to support 29,000 additional eye examinations to First Nations people annually
• Supporting the First Nations Eye Health Alliance (FNEHA) by investing in initiatives to build the capability of the First Nations eye health workforce, and developing the next national Aboriginal and Torres Strait Islander eye health sector plans
• Partnering with the eyecare sector in a multi-channel campaign to raise community awareness of the global myopia epidemic reducing its impact on younger Australians.
The eye health peak body also lodged a submission, calling for investment to ensure that Australians can access the eyecare services in a timely manner by:
• Supporting a self-determined future for First Nations eye health
• Ensuring eyecare, early intervention and education are accessible for all Australian children including those with irreversible vision loss and blindness
• Investing in eye health and vision research.
“We wish to thank the valuable contributions and insight from members which ensured the submission is a strong representation of the current eye health and vision care environment,” Vision 2020 Australia said.
“We will continue our advocacy strategies to raise the voice of the sector over the coming months in the lead-up to the Federal Budget in May.”














OPSM has “reimagined the patient experience” with the introduction of remote consultations that will benefit communities currently under-serviced by optometry.
The move comes after a successful pilot program in 2023 and leverages the latest remote-optometry technology and practitioner patient communication tools developed by EssilorLuxottica.
In some locations, OPSM now has the capability to provide comprehensive eye exams where the patient visits a conveniently located practice, accompanied step-by-step by a trained technician, while the optometrist works remotely.
“A comprehensive remote consultation with in-depth scans and analysis using the latest equipment can bring access to primary eyecare in communities which have been under-serviced by optometry, while helping qualified optometrists engage with patients remotely,” Ms Sephora Miao, senior manager of eyecare operations at EssilorLuxottica ANZ, said.
“It also provides the opportunity for optical dispensers in remote locations to further their skills, while allowing more flexible work arrangements for optometrists.”
After a pilot in OPSM South Hedland, Albany, and Kalgoorlie in 2023, the company is widening its remote optometry availability across additional locations in 2024.

“We are very satisfied with the initial results, where we saw strong favourable reception and adoption by optometrists and technicians and collected exceedingly positive feedback from patients. The technology has performed seamlessly, thanks to the revolutionary software that managed the consultation and through which all the clinical data was collected, transmitted, and stored,” Mr Carl James, senior vice president of store operations at EssilorLuxottica ANZ, said.
“The software also facilitated the video interaction between the patient and the optometrist, while providing interactive
visualisations of eye conditions.”
Following the collection of informed consent to remote consultation, the technician performs pre-test procedures and provides the data to the optometrist for review prior to the consultation. This includes a comprehensive measurement using the Wave Analyser Medica 800 (WAM800), encompassing autorefraction, low and high order aberration assessment, topography, pupillometry, retro-illumination of the crystalline lens, pachymetry, and tonometry.
The technician proceeds to conduct an ultra-wide digital retinal scan capturing a 200-degree view of the retina, as well as OCT with biometry capability. The technician plays a pivotal role in the patient journey, and accompanies the patient to the consultation, where a connection allows the optometrist to remotely control and perform the eye examination. The optometrist can remotely operate the phoropter and chart, with the option to choose from the patients’ existing prescription or autorefraction as a starting point.
A slit lamp examination is also performed utilising the Essilor SL650. During the diagnosis and management discussion, the optometrist can present scans and results on screen, demonstrate any changes to prescription at the touch of a button and present visualisations of common eye disorders.
Tokai Optical Australia general manager
Mr Justin Chiang and Opticare director Mr Michael Nasser are among four new appointments to the Optical Dispensers Australia (ODA) Advisory Board.
They have joined Ms Jessica Kingsley – a trained optometrist who is now a technical sales and product application specialist at ZEISS Vision Care ANZ – and Will Street Eyecare (Bendigo, Victoria) optical dispenser-practice manager Ms Sarah Thompson.
ODA CEO Ms April Petrusma said the new appointments came after the terms of founding advisory board members ended.
“We are beyond grateful for the time and efforts invested by our retired board members. Each of them played an integral role in cementing our place in the industry and contributed to the nation-wide growth we have seen since launching two
years ago,” she said.
“Our new additions bring a variety of perspectives and expertise to the board, o ering a diverse range of ideas and specialised knowledge. We are excited about how this will contribute to ODA’s mission in supporting optical dispensers and providing continuing professional development opportunities.”
The newly-appointed quartet round out a 10-strong ODA Advisory Board that also comprises:
• Australasian College of Optical Dispensers (ACOD) directors and senior trainers Mr James Gibbins and Mr Chedy Kalach
• Experienced optical dispenser and business owner Mr Wayne Puxty
• Specsavers Baldivis dispensing partner Ms Linden Sawyers

• Former International Opticians Association president and Vision West owner Mr Paul Clarke
• Ms Gladys Mak who has local and international industry experience and is one of the optical dispensing workshop instructors for Doctor of Optometry at University of Western Australia.










9 modalities provide additional retinal visualisation*
2500 studies demonstrate clinical value and practice efficiency*
Patients choose to pay for Optos imaging ≥ 80% of the time*




Almost $10 million in research grants have been awarded to Australia’s most promising eye health projects, as part of the National Health and Medical Research Council (NHMRC)’s Investigator Grants program.

Two Flinders University projects received substantial funding, recognising the potential of their projects to improve millions of lives, the university said.
Professor Justine Smith’s project –‘Addressing the greatest unmet needs in uveitis' – received a $2,953,040 funding boost. Meanwhile, Professor Jamie Craig secured $2,476,520 for his work to expand the indications for polygenic risk testing in glaucoma.
The Investigator Grant scheme is NHMRC’s largest funding program and is a major investment in Australia’s health and medical research workforce. The grants support projects by high-performing researchers for five-year periods.
Other ophthalmic grant recipients at other institutions included:
• ‘The role of RNA-mediated spatio-temporal transcriptome changes in age-related macular degeneration’ ($1,457,887), A/Prof Jiayu Wen, Australian National University
• ‘A vision to prevent vision loss: RNA base editing as a strategy to treat inherited retinal disease’ ($1,289,706), A/Prof Guei-Sheung Liu, Centre for Eye Research Australia
• ‘Next-generation gene editing strategies to treat autosomal dominant retinitis pigmentosa’ ($922,058), Prof Paul Thomas, The University of Adelaide
• ‘Markers and mediators of retinopathy and response to fenofibrate in people with Type 1 diabetes’ ($866,385), Prof Alicia Jenkins, Baker Heart and Diabetes Institute
• ‘Prevalence, risk factors and impact of visual impairment in Australia’ ($117, 302), Dr Richard Kha, University of Sydney
• ‘Understanding the contribution of adaptive and innate immunity to RPE/ choroidal dysfunction in diabetic retinopathy’ ($97,835), Dr Jason Ha, University of Melbourne.

Melbourne-linked biopharmaceutical company Azura Ophthalmics has announced positive results from a Phase 2 clinical trial of its investigational dry eye therapy AZR-MD-001 in patients with contact lens discomfort (CLD).
The multicentre, vehicle-controlled study achieved topline e cacy and safety results at three months.
Sixty-seven participants were recruited who could not comfortably wear their lenses as desired and who demonstrated signs of meibomian gland dysfunction (MGD), a leading cause of dry eye disease and CLD.
The trial met its primary endpoint of showing a statistically significant improvement in number of open meibomian glands. Patients in the AZR-MD-001 arm gained at least three hours of comfortable contact lens wear time daily.
The study also met additional secondary and clinically meaningful endpoints, including significant improvements in meibum quality, tear stability, ocular surface staining and contact lens wear time. AZR-MD-001 was also reported to be safe and well tolerated with all observed adverse events considered mild to
moderate and none resulting in treatment discontinuation.
“In addition to meeting its primary MGYLS endpoint, we are especially encouraged that AZD-MD-001 allowed patients who had given up using contacts to wear their contacts again – safely and comfortably – for an additional three hours every day over their normal wear time,” Mr Marc Gleeson, CEO of Azura, said.
“We now have two studies showing AZR-MD-001 can improve the signs and symptoms of MGD and we look forward to discussing these results with the FDA as we advance our Phase 3 development program.”
Mr Lyndon Jones, director and professor at the Centre for Ocular Research & Education in Ontario, Canada, said many patients had given up on wearing contact lenses due to discomfort. With “innovation in this space stalling”, AZR-MD-001 addresses this by treating the underlying causes.
“I’m encouraged to see a potential treatment that may address the underlying cause of contact lens discomfort, and I believe my patients would find an extra three hours of comfortable contact lens wear time to be very meaningful.”
Boroondara Day Surgery – Vision Hospital Group (VHG)’s new ophthalmic day hospital in the Melbourne suburb of Hawthorn –has opened its doors to both patients and healthcare professionals.
The hospital was acquired by VHG in mid-2023 and has undergone refurbishment. VHG now operates 11 day hospitals across Australia.
Dr Jack Kane, a Vision Eye Institute ophthalmologist who recently completed his first cataract surgery list at Boroondara, remarked on the smoothness of the operation.

“Boroondara’s specialist ophthalmic nursing team and state-of-the-art facilities provide an exceptional experience for my cataract patients,” Kane said.
Boroondara Day Surgery is led by recently appointed director of nursing (DoN) Ms Margarette Cortez. She has almost 10 years of clinical experience within the nursing
industry, including the perioperative setting, where she specialised in ophthalmology.
“My journey to Vision Hospital Group has been a wreath of faith, luck and perfect timing,” Cortez said.
“I’ve also been fortunate to have strong support from Vision Hospital Group’s national team of DoNs as I take the reins at Boroondara.”


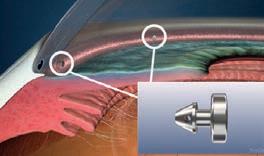
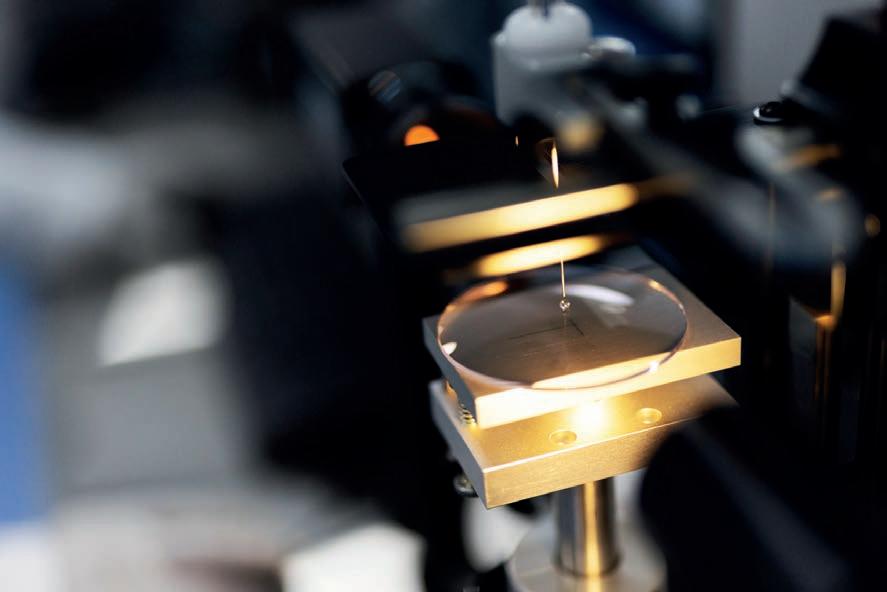
Intraocular lens (IOL) manufacturer Rayner has acquired Swiss-based This AG, which developed and manufactured Sophi phaco emulsification machines.
In a statement, UK-based Rayner – with operations in Australia – said the acquisition marked a new chapter for the company as it branched out to include phaco technology as part of its product portfolio.

The system will complement Rayner’s cataract surgery portfolio.
Image: Rayner.
Sophi (Swiss ophthalmology innovation) is phaco technology that is said to provide mobility, simplicity, and safety within the operating theatre. Rayner said that Sophi presented an advanced surgical system with features including triple pump fluidics, active IOP control, clean venturi and day cassette, cable free power supply and wireless communication.
“The phaco machine plays a central role in cataract surgery. At Rayner we aspire to launch the highest quality products, inspired by surgeons and driven by science,” Mr Tim Clover, Rayner CEO, said.
“Sophi shares this vision, and their machines are truly di erentiated with breakthrough technology combined with stunning design which makes them such a good fit for Rayner. I’m excited about their product range today, as well as what we will be planning together for tomorrow.”
Mr Thomas Koeppel, founder and CEO of Sophi, said the agreement would advance the distribution of the phaco system.
“Sophi was created by viewing things from a completely new perspective; to redefine the requirements of a perfect phaco system by focusing on the point of view of the surgeon and their team,” he said.

Nuance Audio may eliminate the psychological barrier with traditional hearing aids.
Image: Havas Red.
EssilorLuxottica has made a splash at its first Consumer Electronics Show (CES) appearance in Las Vegas, unveiling first-of-kind glasses with an advanced hearing solution alongside its Ray-Ban Meta smartglasses and a new platform o ering tele-optometry and big data services for eyecare practices.
The company’s latest moves in consumer technology were on display 9-12 January, with a prototype of its Nuance Audio system attracting headlines. It is described as “a pair of beautiful glasses with advanced hearing technology built in seamlessly”.
EssilorLuxottica believes hearing solutions is an underpenetrated market where – similar to vision care decades ago – consumers are averse to wearing traditional corrective devices for several reasons including their visibility, discomfort and price.
“Almost 50 years ago, EssilorLuxottica removed the stigma of wearing prescription glasses by turning a necessary medical device into an iconic fashion accessory. Since then, the company has reimagined
what a pair of glasses can do for the person who wears them,” a company statement said.
“Designed for consumers with mild to moderate hearing loss, Nuance Audio will eliminate the psychological barrier that has stood in the way of adoption of traditional hearing aids integrating proprietary state of-the-art open-ear hearing technology into fashionable eyeglasses. Nuance Audio is expected to launch in the market starting with North America in the second half of the year.”
Meanwhile, the EssilorLuxottica booth also featured Ray-Ban Meta, its iconic Ray-Ban glasses with built-in cameras, open-ear audio, AI-powered solutions and the ability to livestream and take calls hands-free.
The group also provided more details on its new HELIX division and the Vision(X) platform, an intelligent and interconnected system to help modernise eyecare practices o ering a full range of innovative digital solutions, including tele-optometry and big data services for the optical market.

“We saw the same philosophy in Rayner and are excited to combine in order to o er Sophi through an expanded commercial team and to accelerate our innovation projects.”
According to Rayner, the acquisition will enhance the company’s breadth of products for cataract surgery, also encompassing IOLs, ophthalmic viscosurgical devices (OVDs), eye drops, pharmaceuticals, digital tools and single-use recyclable instruments.
Aflibercept 8 mg may deliver annual sales over AU$1.5 b in five years. Image: Dragonstock/stock. adobe.com.
Bayer’s higher dose aflibercept 8 mg –now approved in the European Union and US – has been labelled one of 13 potential blockbuster drugs for 2024 in the annual ‘Drugs to Watch’ report by global analytics firm Clarivate.
The anti-VEGF therapy for neovascular (wet) age-related macular degeneration (nAMD) and diabetic macular edema (DME) was the only ophthalmic therapy to make the 2024 list comprising late-stage treatments forecast to deliver annual sales of more than US$1 billion (AU$1.5 b) within five years.
Aflibercept 8 mg represents a higher dose to the standard of care aflibercept 2 mg (marketed as Eylea 2 mg), which is currently o ered to patients in Australia.
The report also identified hurdles that may need to be overcome to reach blockbuster status.
“Clarivate experts expect that, by 2032, approximately 45% of US patients with drug-treated wet AMD receiving aflibercept will receive Eylea [high dose] while 34% will receive an aflibercept biosimilar,” the report said.
“Moreover, they expect that 43% of US patients with wet AMD will receive a competing, newly launched therapy (including biosimilars) by 2032. Novel therapies in development include treatments promising even longer dosing intervals than Eylea HD and gene therapies that could require a single IVT injection, which would greatly reduce the burden of treatment.”












Preservative-free
Can
Compatible



At











Delivered through

US government agency the Advanced Research Projects Agency for Health (ARPA-H) has announced the Transplantation of Human Eye Allografts (THEA) program, which intends to transplant whole human eyes to restore vision for the blind and visually impaired.
The goal of the program is to restore vision in people blinded by conditions a ecting the retina and optic nerve by transplanting the whole donor eye and reconnecting the nerves, muscles, and blood vessels to the brain.
THEA will leverage emerging microsurgical techniques, coupled with genetic and cell-based therapies, to preserve or regrow nerves from the eye to the brain, the agency said in a statement.
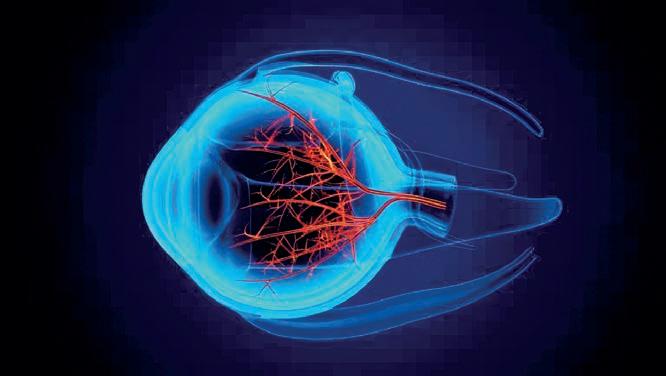
THEA intends to test and evaluate the best therapies to repair damaged nerves, to maintain critical structures in the eye, such as the retina and optic nerve viable after damage, and to prevent postoperative inflammation or rejection.
Through a forthcoming Innovative Solutions Opening, THEA will request proposals focused on three technical areas:
1. retrieval of donor eyes and maintenance of the health of donor eyes until transplantation;
2. optic nerve repair and regeneration; and
3. surgical procedures, post-operative care, and functional assessment.
ARPA-H said these regenerative solutions could prevent degenerative blindness and are a critical step towards successful whole eye transplantation to restore vision. The agency is collaborating with academia and industry to accelerate these discoveries with unique tools not yet applied to ocular surgery.
“For centuries, doctors have theorised eye transplantation to repair vision without
success. However, very recent discoveries in vision science and neuroscience may now help solve the hurdles of reattaching the donor eye’s optic nerve to the recipient,” ARPA-H THEA program manager Dr Calvin Roberts said.
“With THEA, we aim to revolutionise the reconnection of nerves to the brain and make these advancements accessible in the United States and around the globe, with the ambition to o er an alternative to lifelong blindness.”
“While it has been nearly 60 years since the first successful human heart transplant, we have not been able to use similar approaches to restore a person’s sight, and that’s what makes this an ARPA-hard problem to solve,” ARPA-H director Ms Renee Wegrzyn, said.
“Through THEA, we’re seeking to develop the next breakthroughs in transplantation, preservation, and neuroscience to address the challenge: ‘What if we could restore vision to those who are blind?’”
Healthcare private equity firm TVM Capital Healthcare has announced its investment in Alina Vision, an Australian-linked eyecare business that currently operates two hospitals in Vietnam.
The social enterprise was established by The Fred Hollows Foundation in 2018 to address the growing demand for cataract surgeries in Vietnam. With a network of eye surgery centres across the country, Alina is said to bring an a ordable model of eyecare that is sustainable and equitable.
In 2023, Alina completed more than 2,800 cataract surgeries and wants to grow its network to a chain of hospitals across Vietnam with significantly increased capacity.
Until recently, Vision Eye Institute CEO Ms Amanda Cranage was a director and board chair of Alina Vision. In this role, she expanded services in the north of Vietnam, including setting up the ophthalmology department in one of Hanoi’s main hospitals.
Over the past five years, Fred Hollows and Rohto Pharmaceutical, an eyecare company
in Japan, have provided financial backing, eye surgery training and clinical support to Alina Vision to grow the organisation from inception to more than 80 employees across two eye hospitals.
The investment of industry specialist growth capital investor TVM Capital Healthcare is expected to provide Alina access to operational, clinical, training, and management resources, in addition to the equity investment, and accelerate the growth plans while elevating quality of care.
“This deal marks the most substantial investment by TVM Capital Healthcare in the region to date. We look forward to working closely with the management team of Alina Vision to execute our mutually agreed expansion plans,” Ms Hoda Abou-Jamra, managing director of TVM Capital Healthcare in Southeast Asia, said.
“This investment is testament to our impact investment strategy, which is to design, build, and scale promising healthcare solutions that address patients’ needs and fill market gaps, ultimately contributing to equal access

Fred Hollows CEO Mr Ian Wishart added:
“We are pleased to have TVM Capital Healthcare on board to support us and the Alina management team in scaling the business to help reduce avoidable blindness in Vietnam and the region. Alina Vision already invests significant resources in recruiting and training ophthalmologists, optometrists and nurses with our and Rohto’s help. We can now enhance our e orts and execute on our growth plans.”





















ProVision has benchmark KPIs for how greenfield independent practices should be performing in the initial phases – and one of its newest businesses, Picton Eyecare, is exceeding these on almost every measure thanks to the drive of principal optometrist NANDITA CHOWDHURY.
From the moment optometrist Ms Nandita Chowdhury decided that greenfield, independent ownership was the way to feel truly fulfilled in her career, it had taken the best part of a year before she found a location she was happy with. And once she did, she instantly fell in love.
“The first day I came to Picton, I sat in a cafe and thought this town is buzzing. There was this vibe I observed just looking through the window –so I went and told my husband and parents, ‘this is the place’,” she recalls.
“I then went to a few di erent towns, came back to Picton on a very di erent day in the middle of the week, sat down in a di erent cafe and I was still convinced. It’s been just over a year now since we opened, and it’s been a wonderful journey.”
Picton is a small town in the Macarthur Region of New South Wales. Despite its regional feel, it is technically part of south-western Sydney –approximately 90km from the Sydney CBD. For Chowdhury and her family who live 30 minutes away (including school drop o ), this was one of the first major attractions to establishing Picton Eyecare in December 2022.
But there were many other attributes, the strongest being Picton’s sense of community. With only one other independent in town, she was also encouraged by one simple observation: that a lot of people in town seemed to wear glasses.
Her instincts told her it was a sound business decision – and she has been proven right.
“When I was building my business plan, I was told to keep my expectations low, that I wouldn’t make any money for the first couple of years, watch my outgoings etc. But I have been blessed to be busy from day one. In this economic climate, with 13 interest rate rises, it’s a big deal,” she says.
It made sense career-wise too. Chowdhury had spent 11 years as an OPSM franchisee split evenly across stores in Parramatta and Bowral. She sought a new challenge and although locuming meant she could spend more time with her family, it never left her fully satisfied. Independent optometry called – and she yearned for the community connection this a orded.
“The sense of community isn’t like anything I’ve experienced, and I’ve worked in many di erent settings with OPSM, ranging from regional practice through to flagship stores. It amazes me how much locals want to support local businesses,” says Chowdhury, who has already begun sponsoring
local sporting and other local organisations.
“Even when I didn’t have a physical location to work from, café owners would be happy for me to sit at a table all day while I met with suppliers.”
But it would be misleading to say she has achieved it alone. Early on, Chowdhury knew she’d have blind spots, and saw the value in joining the ProVision network which provides business support, services and buying power to more than 440 Australian independents.
In the early stages, she joined the organisation’s Associate Program that provides information, tools and resources about the commercial aspects of practice ownership. While the program can facilitate the succession of an existing practice between a retiring independent and aspiring owner, in Chowdhury’s case ProVision took her through the checklist of setting up a greenfield site.
She was also introduced to ProVision’s NSW business coach Mr Kelvin Bartholomeusz who has been in the role for around 11 years, not long after he sold Sydney’s famous Jones The Grocer chain.
Like any greenfield practice owner, Chowdhury came up against unexpected issues. In her case these were delays with a development application with the council and delays with shop fitters, seeing the practice open three months later than planned. It was di cult given that rent and


“[NANDITA CHOWDHURY’S] CAPACITY TO WORK THROUGH EVERY ASPECT AND BE PREPARED TO DO THINGS HERSELF HAS BEEN ADMIRABLE.”KELVIN BARTHOLOMEUSZ PROVISION BUSINESS COACH
wages for two sta needed to be paid, but things could have been much worse without the guidance of Bartholomeusz and ProVision.
“Because this was an entirely new experience for me, in the early stages I spoke to several independent optometry bodies and ProVision stood out with their approach. Especially Kelvin, the first time I talked to him, he took the time to understand my goals. Initially, he showed me other options, but when I said, ‘no this is what I want to achieve’, he was so supportive,” she says.
“We both knew that it might not happen right away, and it took almost a year, in fact, to find the shop. Kelvin held my hand throughout the whole journey, sometimes taking five calls a day.”
With a focus on elevated customer service, Chowdhury has built her practice on the philosophy that every patient should be treated as she would like to be. This includes getting to know patients, their families and interests. A major factor is employing like-minded sta .
From her time as a franchisee, she knew Ms Melinda Tritico (store manager) who told Chowdhury if she ever opened a practice, she’d work for her – and kept that promise. The other, Ms Libby Tully, recently left a previous role and was keen for a new challenge. She is a local resident and qualified optical dispenser and came in for an eye test after hearing positive feedback about Picton Eyecare in the community. She was so pleased with the service and the environment she decided to join the practice.
“Nothing beats people who are experienced, and I’m happy to pay more for someone who knows what they’re talking about and recommends the right product to suit each patient’s individual need. I can’t be here all the time; they’re the face of the practice, so you need to be confident you can leave the business in their hands,” she says.

Bartholomeusz says Chowdhury is among a growing number of earlyto mid-career optometrists seeking independent ownership through a greenfield practice. Location is important for independent owners, and often after exhausting various avenues to purchase an existing practice, if nothing is available, a greenfield practice can be the next best option.
“In Nandita’s case, as well as other Associate Members, there were very few alternatives. One is a succession plan, which we encourage, gradually buying into a private practice. And the other is setting up from scratch,” Bartholomeusz says.
“With people new to the independent world and setting up a greenfield practice, the first six months are the hardest, particularly pre-setting up, for instance lease negotiations and choosing the right site are fundamental.”
In Chowdhury’s case, ProVision’s business services manager Mr Mark Cordu – an expert in lease negotiations – helped secure a great deal for Picton Eyecare.
Bartholomeusz says Chowdhury and Picton Eyecare shone for many reasons. In fact, he refers to her as his “star performer”.
Firstly, in Picton there was only one other independent in town. When Chowdhury found the store location, it ticked several boxes, including the number of people walking past the shopfront, and its adjacency to services that attract people. The proximity to other shops appealing to women in their 50s is also crucial, given this demographic is important to independent optometry.
“We even look at whether there is too much afternoon sun on the windows, which would ruin your frames and sunglasses,” Bartholomeusz says.
“When Nandita showed me the site, I said, 'take it. I love it'. It had very good adjacencies and a high profile.”
While the location is important, Bartholomeusz says it’s the people that matter most. Plus, starting a greenfield practice can be a $300,000$400,000 upfront investment, in addition to a multi-year lease.
“Our role is stopping people from making mistakes: Do they have the ability to fund the fit out and equipment? Secondly, we insist every person wanting to set up a greenfield completes a comprehensive cash flow

document. We need to know every detail regarding what the anticipated turnover will be and the estimated costs and profit for the next two years. There is an element of guesswork, but it’s an important starting point that removes the rose-coloured glasses perception that everyone will come running in and spend money. That does not happen in optometry,” he says.
“We also provide a template for a comprehensive business plan – both these documents need to be submitted to the ProVision Board before going any further.”
In Chowdhury’s case, Bartholomeusz says she ticked all these boxes, plus more.
“I think experience in optometry does help but her ability to implement has been the secret to her success,” he says.
“Her capacity to work through every aspect and be prepared to do things herself has been admirable. And then her ability to engage her team, and meet the requirements quickly and do it well was the second thing.
“As an example, we tell every new owner to visit the businesses around them, introduce themselves and possibly give them something to remember them by. Nandita had chocolates with her own branding on it and she walked the streets with her now store manager, Melinda.”
For Chowdhury, it’s been the dream start, but she acknowledges she’s in for the long haul. Ultimately, she wants Picton Eyecare to be the place she retires from.
“You’re never completely done,” she adds. “I come to work every day with a list of things that I have to get done either today, this week or within the month. You’ve got to always be improving.”








Eye Trend has become a force in east Melbourne’s independent optometry scene after opening its sixth site. This time, the innovative business has added a twist after obtaining ZEISS Vision Expert status for its latest location.
Walking through Eye Trend’s newest site in Eastland shopping centre in Melbourne’s east, it’s clear Ms Helen Lee – owner of the multi-site independent optometry business – has left no stone unturned. A kid’s corner, paediatric consultation room, on-site lens edging service, and what she describes as a “mini hospital” of diagnostic equipment indicate this new venture is her most audacious yet.
On closer inspection, there also isn’t a PC anywhere in-store. Instead, the entire patient journey is managed seamlessly on iPads (even the subjective refraction), with the patient readings from each device immediately available at the touch of a button. But one of the most notable features of this Eye Trend practice is the omnipresence of advanced equipment and lenses from ZEISS.
Eye Trend has been a major proponent of ZEISS lenses since it switched to the brand in 2018. However, when the prospect of entering Eastland arose, it wasn’t only an opportunity to expand the Eye Trend business, but a chance to deepen its ties with the lens supplier by becoming a ZEISS Vision Expert practice.
So, what does this mean? ZEISS Vision Care Australia and New Zealand recently launched its partner program comprising of multiple levels for independent practice customers: the pinnacle of this is ZEISS VISION CENTRE (more on this later), with the next tier being ZEISS Vision Expert.
For Eye Trend Eastland, instead of carrying ZEISS lenses, it has been purpose built to incorporate the full gamut of ZEISS refractive, diagnostic and dispensing equipment. This is all seamlessly linked via ZEISS Forum data management software. The practice also received comprehensive in-person support during the fit-out stage, and practice sta have been trained on all aspects of the company’s equipment and lenses. ZEISS also supports the practice with customised marketing.
Importantly, Eye Trend maintains its independence, without ZEISS determining the way the practice is designed, run or the product it stocks –although the ZEISS brand remains prominent.
“Being a ZEISS Vision Expert store helps us to elevate the customer experience from the moment a patient enters our store to the moment they leave,” says Ms Charlotte Ng, Lee’s daughter and Eye Trend’s marketing manager who has been influential in setting up the new site.
“There are ZEISS touchpoints that help us deliver a modern, digitalised
and high standard of service, whether that’s in eyecare or dispensing eyewear. When you walk past our store, you’ll see the attention-grabbing ZEISS Visufit 1000 digital centration device in the front window. The ZEISS lens experience bar allows us to explore all the lens options with the patient and find the one that best suits their vision needs and lifestyle. Then, in the consultation room, mostly everything is ZEISS diagnostic and vision testing equipment.”
The practice is fitted out with the ZEISS Visuscreen 500 & ZEISS Visuphor 500 that Ng says “provides an innovative contactless digital vision testing experience”, ZEISS Visuref 150 autorefractor, and the ZEISS SL220 Slit Lamp. But Eye Trend has invested in ophthalmology-grade diagnostics too.
Instruments such as the ZEISS Cirrus 5000 OCT featuring angiography, ZEISS Clarus 500 ultra widefield fundus camera, and the ZEISS Humphrey Field Analyzer 3 perimeter can be found in a dedicated room where more advanced testing is done on selected patients.
When you combine this with the on-site lens lab – and thereby quick turnaround times – paediatric vision testing, vision therapy and management – it’s easy to see how this practice is the realisation of Lee’s vision for the business she took over in 2007. That is, placing equal importance on full-scope optometry and excellent optical dispensing, believing “one cannot survive without the other”.
“We want to show to our customers that you can attain this level of eyecare, no matter your background,” Ng says. “It’s not just for people who have a lot of money or with significant problems, we actually need patients to go through the eye exam journey at an earlier stage so that we can get a baseline and catch or identify those problems early on.”
Coming from a poor family in Hong Kong, Lee says she struggled to focus at school. Teachers didn’t invest in her education, but she believes she would have benefitted from vision therapy. That’s why she has invested so much in her practice, with altruistic motivations.
“The number one reason I like working with ZEISS is because of the quality of their products. Number two is the quality of their support team,” she says.
Ng adds: “Ever since we started o ering ZEISS, people have really appreciated the quality of the lenses we o er. We actually have people





says the ZEISS Vision Expert program centres around the practice’s business ambitions to drive growth and success in its local market.

purchasing a cheaper frame so they can invest in the right lenses for their specific eyecare needs. This shows consumers are more focussed on looking after their health.
“I’ve always said if my mum wasn’t doing this, she would be doing charity work. At the end of the day, we want to make sure we’re leaving a positive impact on the people that we serve.”
For Eye Trend Eastland, becoming a ZEISS Vision Expert practice has been a positive experience, given the stress that comes with establishing a practice from scratch.
“The support has always been first rate, but since becoming a ZEISS Vision Expert practice, it’s gone to a new level. Even after we opened, we had members from the ZEISS team visit us every day to ensure we were supported. They understood we’ve just opened and need their support in delivering the ZEISS experience to our customers," Ng says.
Mr Jason Bowen, national sales manager at ZEISS Vision Care ANZ,

“A requirement of a ZEISS Vision Expert practice is an investment into the consumer journey including utilisation of ZEISS equipment, visibility of the ZEISS brand within the practice and online, prescribing ZEISS branded lenses, and electronic ordering. ZEISS interactive point-of-sale supports an exceptional consumer journey – including a ZEISS lens experience bar, creating a dispensing destination within the practice," he says.
“ZEISS also o ers significant digital marketing support with complete audits of the practices’ social footprint and digital tools such as ZEISS Visuconsult, Visustore and apps including ZEISS Vision Screening.”
For Eye Trend, the advantage of being a ZEISS Vision Expert practice means it can benefit from the lens company's brand and technology, while maintaining its operational freedom.
“We have been very lucky to find ZEISS,” Ng says. “It’s been very good to leverage a premium brand based on innovation and aligns perfectly with our business. A large portion of our customer base are now also familiar with the ZEISS brand, and are seeking it out when they come back in store.”
Ms Gail Giordani, head of ZEISS Vision Care ANZ, says Eye Trend has been a partner for many years, so this is a natural evolution for the practice.
“They continue to prioritise premium lenses and utilising the latest ZEISS equipment to deliver exceptional eyecare via the consumer experience,” she says.
By launching the ZEISS partner program, Giordani says the company is excited to introduce new business concepts for independent customers seeking to elevate and di erentiate their practices.
The pinnacle of the partner program is the ZEISS Vision Centre concept that creates a new optical shopping experience for patients using digital technology networked end-to-end together with innovative technology, premium products and “a clear, modern yet timeless shop design”.
The first of these – ZEISS Vision Centre by Sigo Eyecare – opened in December 2023 at Westfield Booragoon in Perth, Western Australia.
“The ZEISS Vision Centre ecosystem provides precise vision analysis, in-depth lens consultation, and a selection of perfectly fitting lenses and frames,” Giordani says.
“To date, more than 200 ZEISS Vision Centres have opened in around 35 countries, including the US, China (Hong Kong), South Africa, Brazil, Germany, and now Australia. These specialist retail stores are owned and operated by independent eyecare providers who enter an exclusive, long-term partnership with ZEISS.”







Victorian lens manufacturer CR Labs has been at the forefront of independent Australian optometry for more than 45 years. Today, it describes itself as Australia’s largest manufacturing lens laboratory producing premium ophthalmic lenses with industry-leading turnaround times.
Growing up, CR Labs’ (CR) CEO Mr Adam Fletcher’s free time was spent in the Melbourne-based lens manufacturing lab that his father built from the ground up. It was here that he developed and nurtured his passion for optics and helped his father cement values that still resonate throughout the company today.
“Dad was a stickler for quality and service,” he says.
Although his career path was decided for him, Fletcher wouldn’t have it any other way. He’s now in charge of the lab that his father established almost five decades ago, working to maintain and evolve the hallmarks that have made it a go-to lens supplier for independent optometry practices.
Today, CR is well-known for its innovative, high-quality lens production, original designs and customer service. The company completes approximately 1,200 jobs per day and provides customers with what it describes as market-leading turnover rate of four to six days for a complete job.


CR employs a tight-knit team of 53 people, with some of them having been with the business since the very beginning. Mr Dunston Shepherd –Fletcher’s high-school friend – would work alongside him at the lab after school and during the holidays. He now is the COO. Current production manager, Mr Brett Butler, taught Fletcher much of the craft during his early days. And the family legacy will endure with Fletcher's son, Cooper, now part of the team.
“Dad always said, you’ve got to make sure that you’re surrounded by good people, and we have the best people here at CR,” Fletcher says.
CR considers itself a pioneer in the Australian lens market, providing independents with the opportunity to shine with the highest quality of lenses suited to all frame types, and an e cient service.
“The knowledge that we have here is nearly 1,000 years old,” Fletcher explains.

“You can’t buy optical knowledge, and from a laboratory perspective, we’re extremely proactive in training people to work with the latest processes. CR continues to make significant investments in new technologies and capacities. Our o ering is truly world-class.”

This wealth of knowledge was born out of a small lab in South Yarra in 1976, the year that the business started. CR quickly outgrew this location, and the next one at Surrey Hills, then the one after that in Nunawading. The current location in Dandenong South has been home to the company’s operations for seven years. Although it boasts half an acre of lab space, there is still much scope for future growth.
Fletcher himself began working full-time as an apprentice in Optical Surfacing and Fitting at RMIT University in 1989. Despite being the boss’ son, there was no favouritism. He has completed, in his own words, “the longest apprenticeship”, gaining extensive experience working in every department.
Back in the early days, a lot of the work was performed by hand, and Fletcher was able to refine the craft and gain expertise in manual production, before moving into quality control – arguably the most important aspect of the operations. He became managing director in 2002, and in 2022 he became CEO. Nowadays, the team are still likely to find him working alongside them at various stations.
“I say you can have any title on your business card, as long as you live up to the expectation that comes with that. Our laboratory is extremely busy, so whenever there’s a need, I can fill any spot. I will never truly be ‘o the tools’ as I want to keep learning and understand what my people do on a day-to-day basis, and support them through the challenges they face,” Fletcher says.
“If you remove yourself from the day-to-day operations, I believe that you remove yourself from the company.”
He says the growth of CR can be attributed to its reliable service and quality, and the team’s “can-do attitude”. But above all, it’s an unwavering commitment to Australian independent optometry and local manufacturing.
Not only does the company provide locally manufactured products and thus quick turnaround times, but it continues to develop innovative customer solutions through its extensive product portfolio.
It’s all made possible through substantial investments in machinery sourced from the best manufacturers across the world. No expense is spared, with approximately $3 million invested last year in the latest technologies and machinery.
“In traditional labs, you would run the equipment until it stops working. Whereas with the technology we’re dealing with today, we ensure that we replace it at least every five years to stay at the forefront of lens manufacturing,” Fletcher says.
Being a local, privately owned company means CR can be agile and
“I WILL NEVER TRULY BE ‘OFF THE TOOLS’ AS I WANT TO KEEP LEARNING AND UNDERSTAND WHAT MY PEOPLE DO ON A DAYTODAY BASIS, AND SUPPORT THEM THROUGH THE CHALLENGES THEY FACE.”ADAM FLETCHER CR LABS
have to be able to roll out that change globally, whereas we only have to change it for Australia, so we can respond much more rapidly to local customer demand,” he says.
Like the rest of the industry, transitioning from cast to freeform technology has also revolutionised CR’s foothold in the market.
“Freeform technology and automation for laboratories was the equivalent of the Benjamin Franklin bifocal,” Fletcher says.
“It has provided massive opportunities to tailor solutions, but it also gives businesses like ours the opportunity to create our flavour on things. When we look at the automation and processes we have in place, I am extremely proud. Our lab is the most advanced of its kind in the world as far as technology is concerned, and it means the products we o er are up with the key global innovators in the industry.”
Fletcher says the goal of CR's product range is to provide independents with a point of di erence. At the pinnacle of CR’s portfolio is the Australis family of lenses, which are tailored to suit patients’ lifestyles and preferences.
One key di erentiator is its Australis VR technology, adopting virtual reality that Fletcher says can produce truly a personalised lens.
“Progressive multifocal lenses are biased to lifestyle, whether it’s occupational, reading, or distance,” he says. “Whereas the VR starts with a blank canvas, so it is truly a tailored product.”
CR’s lens design for children within the Australis range is described as the first progressive lens designed specifically for children. This lens provides a unique solution for children with accommodative convergence excess and
The company completes around 1,200 daily orders, with a turnover rate of four to six days for a complete job.

is designed to support their movements and behavioural norms.
Other developments in the paediatric space include the recently launched MyoME lens that utilises new Myo-Freeform Technology, clinically proven to slow down the rate of myopia progression in children.
Elsewhere, the company’s Shaw Lens incorporates the knowledge and physics of optics to create a lens that minimises distortions caused by conventional eyeglasses, providing clear and binocular vision.
In 2022, CR was also chosen as the Australian lab partner for the US-developed Avulux Lens which has been clinically proven to manage patients with light sensitivity and migraines.
Fletcher says Avulux has garnered positive feedback among optometry prescribers and patients.
“We’ve helped people to see, but never been able to change lives in this way,” he says.
For CR, international collaborations like this require an assessment of its suitability to the Australian market. As a local manufacturer, the company understands what Australians require, and can redefine internationally designed lenses for Australian patients.
“It’s only through our experience and what we’ve gained in optics that we can actually achieve that for patients,” Fletcher says.
While CR remains committed to its core business, the company also recognises the need to evolve.
That’s why – for the first time – the company has recruited optometrist Ms Fiona Om in a professional services capacity, with a second optometrist to join soon. In addition to delivering educational content to customers, Om also gathers market feedback so that CR can look at manufacturing through an optometry lens and determine future trends.
Additionally, the company has established a partnership with frame supplier Safilo to provide ‘a complete pair’ for practices in a single order, helping them remain commercially competitive. The new ‘Full Circle Program’ eliminates the need for practices to send a patient’s desired frame to the lab. Instead, the frame is selected through online ordering with the prescription.
CR currently o ers Carrera, Privé Revaux and Kate Spade brands, with four more ranges coming soon. The company holds all the necessary stock of the frames to complete the order, e ectively reducing freight costs and significantly improving delivery times.
“From a practice perspective, the frame and the lens also come under the one bill, so it’s convenient for accounting purposes too,” Fletcher says.
“When we look at what’s happening around the world, this is the way forward for lens labs and frames suppliers that is not only environmentally responsible but contributes by lowering the overall costs, providing significant savings and better margins.”
Further assessing the future of CR, Fletcher says the biggest challenge is supporting a market that has gone from 80% to 27% ‘true independent’ during his career.
“We want to be more involved and have a voice in that independent space. We want to support and grow independents,” he says.
“With that in mind, we are working very hard with our customers to make sure they’re not only viable but that we have the same long-term objectives for independent optometry.”
He adds: “With the young optometrists, we can especially make a di erence by showing them the massive opportunity for greenfield sites. When you get the look right, along with the right support in sales, service, quality and turnaround times – all those things make a di erence in the market.”




















‘How long will it be down for?’. It’s the first question any ophthalmic service engineer will be familiar with during an equipment fault, and one that may be answered with more accuracy and confidence for ZEISS customers thanks to several recent improvements to its service offering.
When an OCT, ophthalmic surgical microscope or refractive laser system breaks down, the financial impact is often the first consideration for an eye clinic. This is because it is the most measurable metric, but cancelled appointments can also be counted in less concrete terms like reputational damage to the business and patient impact.
Following the installation of ophthalmic equipment, the supplier or manufacturer will ultimately be judged on the device’s performance. This is closely followed by their responsiveness when things go awry, the clarity of their communication and the time it takes for their equipment to become operational again.
“And if suppliers like us can nail these key aspects, then customers are going to be happy and see the value of their investment, but that’s the challenge,” says Mr Dane Moloney, head of Medical Technology for ZEISS in Australia and New Zealand.
Moloney’s remit is wide, overseeing all functions within ZEISS’ medical division in the region: sales, marketing, clinical applications and service. It encompasses around 90 people, but what’s interesting is that more than half of these employees are in the technical service team.
This speaks to the emphasis manufacturers are placing in the aftersales service space – an area where ZEISS is reinforcing its commitment with a recent restructure of its service team, and the rollout of two new platforms, ZEISS Smart Service and MyZEISS, that promise to enhance the service experience


“THE TECHNOLOGY IS A HUGE PART OF WHAT THAT SURGEON IS OFFERING, AND IF IT’S NOT MAINTAINED AND PERFORMING AS EXPECTED, THE REPUTATION IMPACT, NOT TO MENTION THE PATIENT IMPACT, FOR THE SURGEON IS SIGNIFICANT.”
DANE MOLONEY
ZEISS ANZ
for practices and operating theatres. More sophisticated remote diagnostic and repair capability are what’s being promised, alongside less equipment downtime and greater oversight for practices of their inventory and repair history.
“Our technical service team is a huge investment from a sta perspective, and that comes down to the fact that we’ve got a large installation base with surgical microscopes, diagnostics and refractive lasers. The ability to be able to maintain that equipment and get the clinics up and running quickly is key,” Moloney says.
“We recognise that if an optometrist doesn’t have their OCT working, that’s real

service and real revenue impact. Equally, if a cataract surgeon has to cancel a case because the microscope is down, you can imagine the e ect on the patient. And then there’s a more commercial space like refractive lasers where people are paying a premium for laser vision correction, which is largely elective and completely out-of-pocket. The technology is a huge part of what that surgeon is o ering, and if it’s not maintained and performing as expected, the reputation impact, not to mention the patient impact, for the surgeon is significant.”
Traditionally, Moloney says ZEISS has had a small customer service team based in Sydney that would take calls, and triage and troubleshoot before scheduling engineers to visit the practice or theatre. Sometimes these engineers would drive hours with multiple part options before arriving to diagnose and attempt to fix the issue. But when the problem can’t be rectified on the first visit, this is where delays creep in.
This was the ZEISS service model for many years but four years ago the company assessed how it conducted this part of its business and whether it was delivering what customers demanded. This led to an overhaul of the service department, starting with the customer service team by creating roles solely devoted to either scheduling engineers for maintenance and repairs, to schedule preventative maintenance, or to manage 12-month service agreements.
“On the engineering side, we’ve now expanded to 30 engineers, with three of those roles – and I anticipate more in the future – being purely remote. Two are in Sydney and one is in Melbourne, and they don’t ever go on site. Instead, they’re surrounded by an IT setup and can dial into diagnostic equipment mostly, but sometimes microscopes and lasers, and expedite the diagnostic process and sometimes conduct the repair,” Moloney says.
“The great example of that is with our large installation base of Forum software; practices can’t wait for us to drive two hours across town because that can disable the whole clinic if it goes down. So, our ability to remotely fix any software related issues is crucial.
“On top of that, we’ve now started to place engineers not just in the capital cities. For example, most recently we hired an engineer in Christchurch, New Zealand. We’ve also expanded how many spare parts we keep here in Australia, with the value of these components now totalling in excess of $3 million – when you service equipment like refractive lasers and neurosurgical microscopes, the parts are high value and we recognise that if customers are investing large amounts, then they shouldn’t have to wait weeks for it to arrive from Germany to get it fixed.”
While ZEISS’ service team is ultimately judged on how long it takes to rectify the issue, Moloney says customers
are also sensitive to how the process it handled. They want responsiveness and communication. It’s something the company takes seriously, with 100% of cases sent a Net Promotor Score (NPS) survey – a gold standard customer service metric.
“We analyse that closely. We get feedback and occasionally we get detractors. We review them as a management team and try to figure out what we should be changing to try and reduce that experience from happening,” he adds.
Mr Aaron Semler, digital projects coordinator and part of the ZEISS team for more than 10 years, can envisage a future where big data can predict breakdowns before they even happen.
It’s the direction the industry is heading, and it has seen ZEISS focus on the rollout of two digital platforms that will elevate the service experience for its customers.
The first of these is the ZEISS Smart Services secure remote access platform. The big innovation for customers on board with this service is that ZEISS service engineers can obtain remote access to the clinic’s instrumentation – through the ZEISS central server – with a touch of a button at the practice end.
Semler says ZEISS’ Refractive Service Team has seen particular success with this platform. It all comes down to accessing logfiles that provide important clues as to why the equipment isn’t functioning. By accurately diagnosing remotely, it sets the scene for quicker repairs – hopefully on the first visit.
“With implementing ZEISS Smart Services on all our new VISUMAX 800 installations and some existing MEL90 lasers as upgraded, it allows the Refractive Service Team to remotely retrieve the logfiles and diagnose faults. This saves precious time by arriving prepared for a repair with the required parts or to check for potential faults prior to arriving for a scheduled maintenance service. This is a remote functionality that previously hasn’t existed for the refractive team,” he says.
“The next phase is to focus on making this available to microsurgery customers, including cataract surgery, another segment where we aim to see the same benefits to customers.”
The second digital tool ZEISS is introducing is a Service Portal special feature within its existing MyZEISS platform. Becoming widely available in 2024, this allows customers to log and track service calls for their ZEISS equipment, as well as upload images and videos of faults to provide extra clarity around issues to better inform the service team prior to attending or connecting instruments. Customers can then review service history for all jobs logged via the MyZEISS Service Portal.
MyZEISS also gives customers a detailed overview of their inventory, the location of their devices, and the status of service contracts and warranties. It’s all designed to take the hassle out of tedious phone calls to report the details of a fault, as well as locating documentation before a service engineer is dispatched.

“And, based on the information provided through the Service Portal, maybe ZEISS Smart Services can be used to pull the logfile and check before we call the customer back,” Semler adds.
Moloney says ZEISS is prioritising the migration of more practices, clinics and hospitals across to ZEISS Smart Service, which comes at no charge. Most can see the value conceptually and private clinics have been quick with uptake, but more work is needed to motivate other customers.
“We have to help them achieve that. We see real value to the customer and real value to us – and in that sense, we need engagement from customers to come on that journey because invariably they need to tap into some of their resources, such as IT, to set it up. But once it’s operational, it’s very e ective,” Moloney says.
Regarding the MyZEISS Service Portal feature, he believes having the capability to report an issue via an online portal without a phone call – as well as a place for practice’s to view

repair history of their equipment – is overdue for the ophthalmic market. It’ll also remove the need for customers to manually enquire about the model, age and location of their equipment.
“It’s no di erent to if you own a fleet of cars, you want to know the history of your devices, the age, the performance, and the issues, so that customers, particularly hospitals, can make decisions around when they should budget the capital expenditure to then upgrade,” he says.
As the medical service manager for ZEISS ANZ, Mr Simon Kacimaiwai oversees the 30-strong service engineer team, as well as the customer service team. He has been with ZEISS for almost 18 months, but worked in a similar role for Device Technologies for 12 years.
During his ZEISS tenure, he’s already seen exceptional examples of service, including an engineer who serviced multiple customers on a multi-day, 1,800km road trip covering Kununurra, Broome, Fitzroy Crossing and other outback towns across WA. He also recalls craning a refractive laser into the eighth floor of a Laser Vision Centre in Sydney, requiring the closure of a busy street.
“The team started around 5pm and finished around 5am. That was an exceptional piece of work, and the machine was ready to go for the customer who didn’t experience any disruption to their business,” he says.
Running the service department is an unenviable balancing act. Engineers can only be dispatched to jobs if they have the appropriate training, and it’s made all the more di cult by Australia’s vast geography. Sometimes engineers can have up to three days out of their schedule in remote cases.
“And for some of our high-end machines like the refractive lasers, an engineer will have to go to Germany for four weeks training on no less than three occasions. That’s a big commitment on personal time and expense,” he adds.
Kacimaiwai says there is a major focus on the “first time fix rate”; when

ZEISS wants to reduce the need to call in faults in future.

engineers repair the device on the initial visit. With triage being key to this, he expects programs like ZEISS Smart Service and the Service Portal on MyZEISS to o er easier access to logfile information without much input on the user end. But where he thinks the ZEISS service shines most is the access to “a global knowledge compendium”. That means if local service engineers can’t resolve an issue, it can be escalated to a technical product specialist. Following this, it’s raised to a second level of support to experts in Europe and India with immediate response.
“Everything is done very quickly, and you essentially have the manufacturers and creators of the equipment almost talking directly to our engineers to resolve an issue – the global support is fantastic,” he says.




PBS Information: Xalatan (latanoprost 0.005% eye drops, 2.5 mL) is listed on the PBS as antiglaucoma preparations and miotics.













Before prescribing please review Product Information available via www.aspenpharma.com.au/products or call 1300 659 646.
Minimum Product Information: XALATAN® (Latanoprost 50 µg/mL) Eye Drops. Indication: Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Contraindications: Hypersensitivity to ingredients. Precautions: Change in eye colour due to increased iris pigmentation; heterochromia; eyelid skin darkening; reversible eyelash and vellus hair changes; macular oedema often associated with aphakia / pseudoaphakia; other types of glaucoma; contact lenses; severe or brittle asthma; herpetic keratitis; driving or using machines – transient blurry vision; elderly: no data; children: do not use, no data; lactation- metabolites present in breast milk, risk / benefit. Pregnancy:
Category (B3) Interactions: other prostaglandins, thiomersal. See PI for details. Adverse Effects: Eye Disorders: blurred vision, burning, conjunctivitis, excessive tearing, eye pain, foreign body sensation, hyperaemia, iris hyperpigmentation, itching, punctate epithelial erosions, grittiness, stinging, eyelash and vellus hair changes, punctate keratitis, blepharitis, eyelid oedema, localised skin reaction on eyelids; Systemic: bronchitis, upper respiratory tract infection, eczema, rash, urinary tract disorder, abnormal liver function, myalgia, arthralgia, dizziness, headache, rash, chest pain, asthma, dyspnoea . See PI for details and other AEs. Dosage and Administration: One eye drop in the affected eye(s) once daily. Other eye drops should be administered at least 5 minutes apart.
References: 1. Clinical Practice Guide for the Diagnosis and Management of Open Angle Glaucoma. Optometry Australia 2020 2. Australian Commission on Safety and Quality in Healthcare Active Ingredient Prescribing Guide - list of medicines for brand consideration December 2022
Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma.com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2023 Aspen group of companies or its licensor. All rights reserved. Prepared: July 2023 AU-LAT-072023-07653

Innovation is at the core of everything we do. At Glaukos, we push the limits of science and technology to solve unmet needs in chronic eye diseases.


PM-GL-0077
All rights reserved. ©2021
Experience a world of firsts in vision care. Learn more at Glaukos.com.


As the sector marks World Glaucoma Week (10-16 March), recent developments have provided eyecare professionals with even more confidence the disease can be managed and optimism for patients.
With an ageing population and more than 300,000 people estimated to be living with glaucoma in Australia – half of those completely unaware they even have the condition –new surgical interventions, translational research projects and innovative care models are emerging to soften its impact.
One such development is the transition from traditional therapeutic avenues as first line treatment to medication free alternatives. As issues with compliance and a reduction of life-quality are commonly associated with eye drops, the industry is exploring new avenues that are revolutionising the treatment landscape.
A current snapshot of glaucoma management shows that newly diagnosed glaucoma patients are increasingly being treated with selective laser trabeculoplasty (SLT) as a first line treatment. This is based on evidence from the LiGHT trial; a landmark study demonstrating that starting with SLT as first line therapy compared to medical therapy exhibited greater intraocular pressure (IOP) control and thus patients were more likely to be medication free.
Currently, nearly three-quarters of these patients are still medication free, six years after SLT. More importantly, people treated with laser first have a lower rate of losing peripheral vision and a much lower rate of needing to go on to have further invasive surgery.
One surgeon who has been following the data closely is Dr Nathan Kerr, of Eye Surgery Associates in Melbourne, a researcher at the Centre for Eye Research Australia (CERA) and one of Australia’s most wellcredentialled glaucoma specialists.
“In recent years, SLT has emerged as the preferred first line approach for open-angle glaucoma and ocular hypertension, o ering a more patient-centric solution. This method significantly reduces
the challenges associated with adherence - a notable obstacle, as numerous patients find daily eye drop application challenging. Moreover, SLT avoids the potential side e ects commonly associated with eye drops and reduces the risk of field progression and need for incisional glaucoma surgery. By integrating SLT as our initial treatment strategy, we e ectively address these concerns, enhancing overall patient care and outcomes,” Kerr says.
He says that the industry is witnessing a profound paradigm shift in the approach to treating glaucoma.
"A decade ago, the standard protocol involved initiating treatment with medical therapy. Typically, if a single agent proved insu cient, we escalated the treatment, often incorporating up to three di erent medications before even considering laser therapy. However, now we have a deeper understanding of the benefits of SLT.”


“IT IS REALLY EXCITING THAT WE NOW HAVE MANY MORE OPTIONS FOR TREATING GLAUCOMA PATIENTS. OUR FOCUS INITIALLY WAS ON PREVENTING VISION LOSS AND BLINDNESS WHICH IS STILL ONE OF OUR MAJOR FOCUSES BUT IT’S REALLY MOVED BEYOND THAT.”
“The integration of MIGS during routine cataract surgery not only maintains an excellent safety profile but also enhances the overall surgical outcomes. By reducing or eliminating the need for glaucoma drops, MIGS plays a crucial role in improving the ocular surface which is vital for optimal IOL performance. Patients benefit from a dual therapeutic approach that addresses both cataract and glaucoma in a single, streamlined procedure,” Kerr says.
Although relatively new to the Australian market, large ophthalmic studies have mitigated uncertainty surrounding the MIGS procedure.
“As we approach a decade of utilising MIGS in Australia, our understanding and expertise in this field have grown significantly. Globally, the body of data on MIGS devices has surpassed the 10-year mark. Notably, the HORIZON study on the Hydrus Microstent stands out as not only the largest trial specifically focused on MIGS but also one of the most extensive in the field of surgical ophthalmology,” Kerr says.



Kerr completed the first surgery in Australia using the iStar MINIject minimally invasive glaucoma surgery (MIGS) device late last year since it became commercially available. He says the device represents a significant advancement in MIGS, which is a surgical option for patients where medical therapy is ine ective or poorly tolerated.
“MIGS is playing a pivotal role in reducing the need for trabeculectomy. While trabeculectomy is a highly e ective procedure, it’s also considerably invasive and demands an extended recovery period. The current market o ers a range of MIGS devices, supported by a robust and continually growing body of evidence underscoring their safety and e cacy. This advancement has revolutionised the management of glaucoma,” Kerr says.
Ultimately, the goal of these procedures is to extend beyond preventing vision loss; with the aim to enhance overall quality of life. This involves minimising reliance on medications, lowering the risk of side e ects, and ensuring a swift recovery so that patients can return to their normal activities.
“These innovative technologies are not just about treating a condition; they’re about o ering a superior patient experience and significantly improving their quality of life. It’s an incredibly exciting time in the field of ophthalmology,” Kerr says.
There are two natural drainage routes inside the eye: The conventional pathway (Schlemm's canal) – which the iStent, Hydrus, and iTrack utilise – has been shown to be safe and e ective; and the uveoscleral pathway which is the focus of the MINIject. This procedure creates a pathway for aqueous to flow into the suprachoroidal space, which e ectively lowers IOP. Additionally, the suprachoroidal space is less prone to scarring compared to traditional filtration surgeries, possibly leading to more sustained IOP control.
“Unlike MIGS devices which primarily facilitate aqueous outflow through Schlemm’s canal and into the episcleral venous system, the MINIject o ers an alternate approach. It bypasses the episcleral venous pressure floor, which inherently limits the extent to which IOP can be reduced. This bypass mechanism allows the MINIject to potentially achieve lower IOP levels, granting it a unique advantage in certain clinical scenarios,” Kerr says.
When performed with routine cataract surgery, Kerr says that Schlemm’s canal and MINIject procedures boast good safety profiles that are very similar to that of standalone cataract surgery.
MIGS preserves the ocular surface by avoiding glaucoma drops so the patient’s ocular surface remains intact which is important for intraocular lens (IOL) performance. Therefore, the outcomes of cataract surgery are improved.
“Initially, there was a degree of uncertainty surrounding the safety and e cacy of MIGS. However, with nearly 10 years of clinical experience and robust data, we’ve e ectively addressed these concerns. The current focus is now on ensuring that this advanced care is accessible to all patients who could benefit from it."
Kerr says the trajectory of the glaucoma landscape not only o ers a wide range of treatment options that can be tailored to patients’ needs, but provides quality-of-life that traditional methods have not been able to achieve.
“The advancements in glaucoma treatment over the past few years have been truly remarkable. While our primary objective continues to be the preservation of vision, the scope of our care has broadened significantly,” he says.
In the past, postoperative periods following conventional surgical methods often meant a prolonged recovery for patients, characterised by frequent follow-up visits, blurred vision, and eye discomfort. Kerr welcomes the shift towards newer techniques that facilitate a quicker and more comfortable recovery process.
“Being able to provide these advanced treatment options and witnessing the positive impact on our patients’ lives is exceptionally rewarding. It’s an indication of meaningful progress in our field, enhancing both the e ectiveness of our treatments and the quality of life for our patients,” he says.
With the rising numbers of patients diagnosed with glaucoma – and oversubscription of public ophthalmology departments – the Glaucoma Community Collaborative Care Program (G3CP) at the Royal Victorian


Eye and Ear Hospital (Eye and Ear) in Melbourne is designed to alleviate some of this pressure.
The Glaucoma Unit at the Royal Victorian Eye and Ear Hospital provides more than 12,000 outpatient appointments a year, but there are still challenges with demand for services exceeding capacity. Established in 2018, the G3CP aims to ease this demand at the same time as ensuring patients receive appropriate and timely care. It is the largest program of its kind in Australia and has proven successful with a high degree of patient and practitioner satisfaction.
The program focuses on low-risk or suspect patients with stable glaucoma who need to remain under the care of an ophthalmologist and require close monitoring, but do not need to come to hospital clinic for every appointment.
The hospital has partnered with community optometrists who are recruited to provide care in geographical areas with high demand. Instead of having to attend the hospital for glaucoma monitoring, the clinical assessment is performed by the participating optometrists with the results of testing forwarded to the hospital and reviewed by a glaucoma specialist.
After the initial pilot program, which demonstrated safety, e ectiveness and high patient and clinician satisfaction,the program is continuing to expand, with an additional 20 optometrists recently recruited.
Dr Catherine Green, AO, head of the Glaucoma Unit and ophthalmology lead of G3CP says the program has been shown to be very safe and e ective. It allows patients easier access to appointments because the public system is oversubscribed by a substantial amount with low-risk patients often having their appointments delayed.
A defining characteristic of G3CP is its a ordable delivery of eyecare




“THERE’S A VERY HIGH ACCEPTANCE FROM PATIENTS THAT THEY ACTUALLY PREFERRED SEEING A LOCAL OPTOMETRIST FOR SOME OF THE VISITS KNOWING THEY ARE STILL UNDER THE SUPERVISION OF THE GLAUCOMA CLINIC.”

services which allows it to make a di erence in patients’ lives, particularly in a cost-of-living crisis.
“I think a key strength of our program is the informed consent, because some patients do have a small out-of-pocket expense that needs to be discussed with them while participating optometrists provide as low cost care as they can,” Green says.
In adherence to RANZCO glaucoma collaborative care guidelines, G3CP recruits optometrists through an expression of interest. They are required, at minimum, to have a means of applanation tonometry, optic disc imaging, and access to visual field testing.
Patients are assessed in clinic by a glaucoma specialist, and those that are stable are deemed suitable for G3CP. From then on, community-based optometrists can monitor IOP and prescribe medication, working within specific guidelines. If a change in treatment is required, they will defer to the Eye and Ear for a decision.
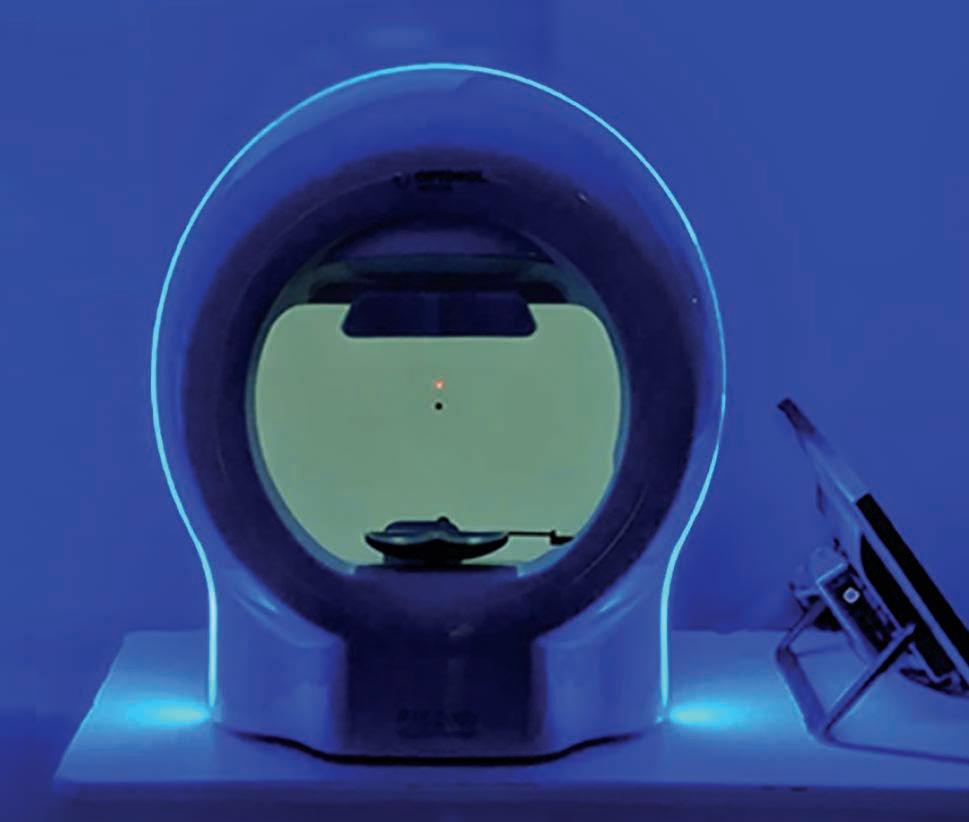





be used for patients who may have a genetic likelihood of developing the disease, based on familial disease patterns. He wants to see broad implementation of the tests in the health system.
A $2.9 million funding injection from the Australian Government Medical Research Future Fund (MRFF) Genomics Health Futures in November last year will support the rollout of the test in Australia.
“Now we have the ability to simply send a patient saliva-based testing which is not much di erent to COVID tests. The test is sent back to a lab and within four weeks, you can be given a probability of developing glaucoma at some stage in your life,” he says.
“As an organisation we’re now currently working with Professor Craig and commercial partners to see how we might be able to use that test in the Australian health system to identify people who might be at risk even though they may not know it.”
Ideally, this system would encourage immediate relatives of glaucoma patients to participate in early testing.

“WE HAD AROUND 3,000 PEOPLE ENROLLED IN [SIGHTWISE] OVER THE PAST FOUR MONTHS AND 25,000 ACTIVE ON THE PROGRAM RIGHT NOW. BUT REALLY, WE’RE ONLY SCRATCHING THE SURFACE OF THE TOTAL POPULATION.”
“The system would make sure these patients schedule in regular appointments and determine whether the optometrist is going to be a part of their lives going forward. It would determine whether they need to undergo proactive treatment so the disease doesn’t progress in the first place. That’s a massive opportunity,” Wylie says.
“We’re very, very interested to see how this availability of the new saliva test impacts ongoing identification and also, treatment of patients going forward.”
Wylie cites not only glaucoma, but its comorbidities, as a major economic burden for Australia. It’s been predicted by health economists that the strain to the overall health system is going to reach $4.3 billion by 2025, largely due to Australia’s ageing population.
“In terms of some of the consequences for the health system, people with low vision and glaucoma are four to eight times more likely to have falls. And obviously, hip fracture is a significant risk of falls so there’s also a greater risk of hospitalisations and premature death,” he says.
“Additionally, people with low vision are admitted to aged care earlier than those with full vision. And they’re also twice as likely to su er from depression. So, not surprisingly, the consequences of having mid- and late-stage sight loss are quite substantial.”
To mitigate this growing burden, Glaucoma Australia’s SiGHTWiSE program is a valuable asset featuring a free support line that people can access to speak with qualified healthcare counsellors. The program also features a comprehensive website, series of live monthly Q&A webinars with expert speakers, social media support groups, bi-monthly newsletters and various brochures and fact sheets to support patients.
practice all doing the same thing.”
Despite a sophisticated eyecare system in Australia, Glaucoma Australia’s biggest challenge is ensuring the disease is diagnosed before it results in vision loss. It does this through encouraging the community to get their eyes tested regularly, so that glaucoma can be identified early.
Glaucoma Australia CEO Mr Richard Wylie says that he is pleased with the strides being made in this space, with Specsavers o ering OCT scans as part of general checkups, at no cost to the patient.
But more importantly, he heralds a new saliva DNA test to assess individual risk of developing glaucoma, known as SightScore by Seonix Bio and developed by Professor Jamie Craig and his team at Flinders University.
If widely adopted, Wylie says this represents a game changer and can
“It’s been shown that SiGHTWiSE patients are more compliant with their prescribed therapies. They attend their appointments with their eye health professionals more regularly, and they’re also generally more knowledgeable about their glaucoma. They also have reduced anxiety about the future,” Wylie says.
To reflect growing glaucoma incidence and detection rates, demand for the program is growing annually. However, these enrolments only constitute a small percentage of current glaucoma patients.
As part of Glaucoma Australia’s long-term vision, and to alleviate strain on public ophthalmology services and raise awareness of the program, its integration with the health system is among Wylie’s top priorities. This would entail enrolling those on the waiting lists on to SiGHTWiSE at no cost and educating them on their treatment or referral options.
“We had around 2,800 people enrol in the program over the past 12 months and almost 23,000 active on the program right now. But really, we’re only scratching the surface of the total population,” Wylie says.























The revolutionary Corvis® ST records the reaction of the cornea to a defined air pulse with a newly developed high-speed Scheimpflug camera. It allows for a detailed assessment of corneal biomechanics.
The information obtained is used to calculate a biomechanically corrected IOP (bIOP) and corneal stiffness parameters which play an important role in glaucoma management.




1800 225









Biomechanical
bIOP/CCT measurements
Biomechanical Glaucoma Factor (BGF)
The BGF is a very early risk indicator of NTG which will guide you to the best clinical decisions for your patient. The software allows for an easy screening for glaucoma based on the biomechanical response.

- More accurate IOP readings even in cases of altered biomechanical properties.1,2,3,4
- Data is easy to read and to interpret and IOP follow-up is neatly arranged.

IOP follow-up bIOP/CCT Measurements
Distribution of BGF in healthy eyes (green) and NTG patients (red). The black line shows the BGF-output for this patient.
Output of the Biomechanical Glaucoma Factor (BGF)

1.Joda AA, Shervin MM, Kook D, Elsheikh A. Development and validation of a correction equation for Corvis tonometry. Comput Methods Biomech Biomed Engin. 2016;19(9):943-53.
2.Chen S, Lopes BT, Huang W, Zheng X, Wang J, Zhu R, Vinciguerra R, Li Y, Wang Q, Li H, Bao F, Elsheikh A. Effectiveness of 4 tonometers in measuring IOP after femtosecond laser-assisted LASIK, SMILE, and transepithelial photorefractive keratectomy. J Cataract Refract Surg. 2020 Jul;46(7):967-974.
3.Eliasy A, Chen KJ, Vinciguerra R, Maklad O, Vinciguerra P, Ambrósio R Jr, Roberts CJ, Elsheikh A. Ex-vivo experimental validation of biomechanically corrected intraocular pressure measurements on human eyes using the Corvis ST. Exp Eye Res. 2018 Oct;175:98-102.
4.Chen KJ, Joda A, Vinciguerra R, Eliasy A, Sefat SMM, Kook D, Geraghty B, Roberts CJ, Elsheikh A. Clinical evaluation of a new correction algorithm for dynamic Scheimpflug analyzer tonometry before and after laser in situ keratomileusis and small-incision lenticule extraction. J Cataract Refract Surg. 2018 May;44(5):581-588.



To accommodate an ageing population, glaucoma management is transitioning from reactive treatment regimens to proactive ones. Three key experts detail what this mindset shift entails and how they employ it in practise.
“It’s 2024; glaucoma should not be a blinding condition.”
This sentiment by Dr Aparna Raniga, a subspecialist glaucoma and cataract surgeon at Macquarie University Hospital in Sydney, reflects a new mindset in glaucoma care. That is, casting aside the conventional reactive approach in favour of a method that proactivity manages and treats the disease before it becomes severe enough to impact on day-to-day life.
The concept – “interventional glaucoma (IG)” – is a relatively new term coined by the ophthalmic industry, and thanks to recent technological developments and landmark studies, it reflects a paradigm shift and could be the future of glaucoma management.
IG has emerged from the idea that although glaucoma cannot be prevented, blindness or significant vision loss can be slowed with early enough – and aggressive enough – intervention.
Traditional glaucoma care models involve administering eye drops –which can be associated with adverse side e ects, and ocular surface and compliance issues. When ine ective, patients may then make the significant leap to conventional surgeries such as a trabeculectomy or tube shunt, which are e ective but invasive, carry significant risks and require intensive follow-up.
Glaucoma and cataract expert Dr Colin Clement, of Sydney Eye Associates in Sydney, says the goal of IG is to minimise morbidity that not only results from the disease, but also its treatments.
“[IG] is all about diagnosing and treating earlier, being more proactive and perhaps using more aggressive treatments at an earlier stage in the disease,” he says. “The rationale behind this – and the primary objective of glaucoma management – is to maximise quality-of-life which we achieve through preserving vision. It’s easier to preserve vision if you can treat the disease earlier on.”
IG is an unconventional concept and glaucoma management still largely follows traditional treatment algorithms. However, momentum is building behind IG thanks to an expanding suite of diagnostic methods and the emergence of robust evidence supporting the use of more middle-ground treatments such as micro-invasive glaucoma surgery (MIGS).
Another example contributing to this mindset shift is the Laser in Glaucoma and Ocular Hypertension (LiGHT) study published in 2019. In this landmark trial, a comparison between selective laser trabeculoplasty (SLT) and eye drops identified SLT as having a similar e cacy profile to eye drops when used as first-line treatment, but with improved quality of life, and a greater reduction


“[IG] IS ALL ABOUT DIAGNOSING AND TREATING EARLIER, BEING MORE PROACTIVE AND PERHAPS USING MORE AGGRESSIVE TREATMENTS AT AN EARLIER STAGE IN THE DISEASE.”
DR

of adverse side e ects and additional surgical requirement.
Raniga acknowledges the benefits of early intervention with SLT and says there needs to be a shift away from administering eye drops, as they have the potential to complicate other treatment interventions.
“SLT bypasses the side e ects of drops, and issues with adherence and compliance. It’s e ective, and it’s also safe. So, I’m certainly o ering and performing laser treatment earlier,” she says.
“Patients who’ve been on drops for decades tend to have much more scarring potential, no matter which surgery they have. Long term studies have demonstrated that the e ectiveness of a trabeculectomy for a patient who has been on drops for decades is not as good as a trabeculectomy that’s done early.”
Early and aggressive intervention for Raniga often entails a discussion of eye drops and SLT with early disease, or eye drops and SLT with surgical intervention if the disease is advanced.
Contributing to IG’s growing support is the proliferation of MIGS on to the treatment landscape. First introduced in 2010, it works to treat mildto-moderate disease and bridges an important gap.
“MIGS has emerged to fill a treatment gap that exists between medication, laser and surgery, because in terms of risk for the patient, there’s a large step up when undertaking surgery,” Clement says. “The reason it fills that gap is because it’s very safe, so the risk to the patient is fairly low.”
Clement says, in his experience, patients who do not adequately respond to medication or laser can achieve the pressure reduction they need with MIGS, as opposed to the traditional invasive glaucoma surgery.
“There is the possibility that MIGS can be used earlier in the treatment paradigm and there’s even the possibility that it could be used as primary treatment,” he says.

Image: Glaukos.


iStent inject and Hydrus propensity matched cohort at 24 months (Holmes et al., 2022)
One barrier to early uptake, Clement says, is patient selection. Information regarding which patients respond well to MIGS and which do not is still being collected. As patient selection improves, surgeons will be able to o er MIGS with greater confidence of achieving a positive outcome.
“Currently, MIGS is performed in a day surgery setting or hospital and there’s time and cost associated with that. One thing that would be a real game changer is if these procedures could be o ered as a treatment in clinic so there’s no inconvenience to the patient. It’s quick and makes it considerably more cost e ective.”
The data shows the current crop of MIGS devices appear to boast ideal safety and e cacy profiles. Ongoing evidence is available, with safety and e cacy constantly monitored so surgeons and patients can be confident they’ll deliver the desired results.
Glaucoma and cataract surgeon Associate Professor Mitchell Lawlor of Sydney Eye Surgeons, has been influential in capturing some of this data through the Fight Glaucoma Blindness! (FGB) registry at the Save Sight Institute.
The registry serves to compare ‘real-world’ safety and e cacy outcomes of devices released to the market. Specifically, it tracks iStent inject surgeries, Xen implants and conventional glaucoma surgeries such as trabeculectomy and tube shunts.
In the case of the CyPass Micro-Stent, where concerns of corneal endothelial cell damage emerged after five years of follow up, the significance of registries such as FGB cannot be understated. Although the CyPass has since been voluntary withdrawn, Lawlor says the other devices are still showing a favourable safety and a good e cacy profile over time.
Glaukos’ iStent inject and the Hydrus Microstent (now owned by Alcon), are the two most-used MIGS devices and have Medicare reimbursement as both a standalone procedure, or combined with cataract surgery. The newly available MINIject, alongside Allergan’s Xen device also come under this category.
“Some of the new devices that have been o ered have had a pretty quick uptake given how they’re only recently come to market in the last decade, but they’re already playing quite a big role in our treatment,” Lawlor says.
Glaukos’ iStent inject is one example. Commercially, it has been around the longest in Australia and thus has the most evidence to support its use.


*Data from complete cohort; iStent inject n=224, Hydrus n=120
A 2022 study by Clement, Lawlor and their colleagues explored the 24-month safety and e cacy profiles of iStent inject and Hydrus in combination with cataract surgery. The devices demonstrated sustained IOP reductions and good safety profiles.
“I think that also allows surgeons to have comfort the procedures should be part of their repertoire,” Lawlor says.
Raniga says there is still work to do in catching the disease early, including identifying high-risk patients through family history of glaucoma.
“Understanding the individual patient’s risk profile really helps with proactively treating those fast progressors. In patients with greater risk factors, such as those who have a strong family history of glaucoma, it is vital to check their rate of progression more closely,” she says.
“For those patients, I think we should definitely intervene much earlier because we’re hopefully going to prevent that end-stage glaucoma that we want to eliminate and to maintain a good quality of life.”
Lawlor says that for wide adoption of MIGS and earlier intervention, data captured through the FGB registry will help to understand which subgroups of patients most benefit from which type of device. This information will allow more targeted invention in the group of patients most likely to benefit.
While there are upsides to IG, increased testing, OCT access, genetic testing, potentially more surgeries and the manpower to oversee all of this could place more pressure on an already-stretched glaucoma care system.
“[IG] is a concept that’s very much suitable for a health system that’s highly resourced. So, if you tried to apply this to a system that’s not, it would be very challenging,” Clement says.
With an ageing population, and with more earlier diagnoses, the capacity of ophthalmologists to sustainably service this population also comes into question.
“If you’re seeing more patients and intervening earlier, and with an ageing population, the overall number of patients we’re treating is going to increase, which raises issues about capacity to serve patients. Collaborative care could potentially help with that,” Clement says.
“This care model may entail optometrists taking on a greater role in managing stable patients, with a shift toward ophthalmologists providing more of a ‘surgical’ service.”
With early diagnosis holding the key to greater IG uptake, primary eyecare providers, who see a wide scope of patients, hold the key to timely referrals.
Additionally, Lawlor believes collaborative care models are also useful when monitoring disease progression.
“We work together as professionals to make sure that patients are monitored over time, with a cohort who may well have a lower risk of progression given they’ve had a glaucoma intervention,” Lawlor says.
Ultimately, he says that transitioning to an IG model requires consideration of risk and patient suitability.
“While early intervention is beneficial in those patients who are likely to develop significant vision loss, there is a risk that it could lead to over treatment of some patients. We therefore need to continue refining methods of stratifying those who are at higher risk of progression to determine which patients need early intervention.”


Before prescribing, please review the full product information at www.aftpharm.com/prescription/vizo-pf-dorzolatim.
Indications:
Treatment of elevated intraocular pressure (IOP) in patients with ocular hypertension or open-angle glaucoma when concomitant therapy is appropriate.
Contraindications:
Reactive airway disease, bronchial asthma or a history of bronchial asthma, or severe chronic obstructive pulmonary disease; sinus bradycardia, sinoatrial block, second or third degree atrioventricular block, overt cardiac failure, cardiogenic shock; hypersensitivity to any component of this product.
Precautions:
Adverse reactions found with systemic administration of beta-blockers may occur with topical administration.
Cardio-respiratory reactions; vascular disorders should be treated with caution; masking of hypoglycemic symptoms in patients with diabetes mellitus; masking of thyrotoxicosis; surgical anesthesia; immunology and hypersensitivity, the dorzolamide component is a sulfonamide; concomitant therapy with carbonic anhydrase inhibitors; not been studied in patients with acute angle-closure glaucoma; choroidal detachment has been reported; increased potential for developing corneal oedema in patients with low endothelial cell counts; beta-adrenergic blockade has been reported to increase muscle weakness; patients should be advised to seek their physician’s advice if they develop an intercurrent ocular condition or any ocular reactions; Dorzolamide/timolol 2%/0.5% has not been studied in people wearing contact lenses; not been studied in patients with hepatic impairment; not been studied in patients with severe renal impairment (CrCl < 30 millilitre/min); for use in the elderly and paediatric use,




































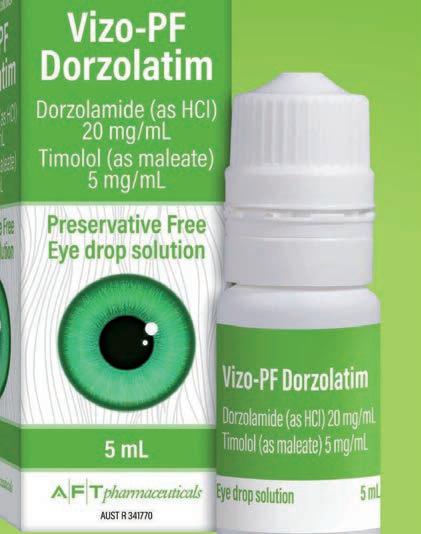
see full Product Information (PI).


Interactions with other medicines:


Pregnancy Category C, (see full PI). A decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
See Contraindications and full PI; specific drug interaction studies have not been performed with Vizo-PF Dorzolatim.
The potential exists for additive effects and production of hypotension and/or marked bradycardia with timolol maleate; disturbances have been reported with oral carbonic anhydrase inhibitors; mydriasis resulting from concomitant use of timolol maleate and adrenaline has been reported.
Adverse effects:
Most frequently reported adverse effects were: ocular burning and stinging, taste perversion, corneal erosion, conjunctival injection, blurred vision, tearing, and ocular itching; urolithiasis was reported rarely; others (see full PI). May affect some patients’ ability to drive and/or operate machinery.
Dosage:
One drop in the affected eye(s) two times daily; when substituting for another ophthalmic antiglaucoma agent(s), discontinue the other agent(s) after proper dosing on one day, and start Vizo-PF Dorzolatim on the next day.
If another topical ophthalmic agent is being used, the other agent should be administered at least ten minutes apart; efficacy in paediatric patients has not been established (for more information regarding safety in paediatric patients ≥ 2 and < 6 years of age, see full PI).
To avoid contamination of the solution, keep the container tightly closed, do not let the dropper tip touch any surface.
Unopened bottle: Store below 25°C. Protect from heat. Opened bottle: Store below 25°C. Discard contents 4 weeks after opening the bottle. Protect from heat.


A peer reviewed Journal of Glaucoma article featuring Specsavers’ data has reinforced what the company has known all along: that routine use of OCT – combined with innovative processes – is the pathway to more timely glaucoma detection and prevention of avoidable vision loss. Here, Specsavers ANZ director of clinical services DR BEN ASHBY and his team detail each component underpinning this transformative strategy that’s capturing global attention.
THE STRATEGY
SPECSAVERS ANZ DIRECTOR OF CLINICAL SERVICES
Specsavers has placed significant emphasis on the early detection of glaucoma for close to a decade. In 1996, the Blue Mountains Eye Study revealed 50% of people with glaucoma had the condition undetected, even after appropriate eye testing, and in 2017 the National Eye Health Survey repeated this finding. As optometrists who are passionate about providing patients with the opportunity to protect vision through early detection and access to diagnosis and treatment, we wanted to change the unfortunate statistic and enhance eye health outcomes for our patients.

While standard optometry obviously includes appropriate testing
techniques for the condition resulting in detection and referral, Specsavers has constantly trialled and engaged in new processes and procedures, measuring their impact in the name of increased and earlier
This has led to our optometrists increasing our detection rates to approximately 90% of all patients with glaucoma among our patient base, including those previously undiagnosed. Since 2016 across Australia and New Zealand, we have detected glaucoma for more than 200,000 patients and sent more than 300,000 referrals to specialists for diagnosis and treatment. We’ve also been able to discover a lot of new insights into the condition, and how it is diagnosed in Australia and New Zealand. For instance, high intraocular pressure is the classic risk factor for glaucoma, but three quarters of patients we have referred for treatment have an IOP in the normal range.
We know the findings we’ve discovered on our journey are groundbreaking, so much so that Specsavers' glaucoma detection data was globally celebrated in a recent peer-reviewed article in the Journal of Glaucoma and now we are receiving requests from around the world for
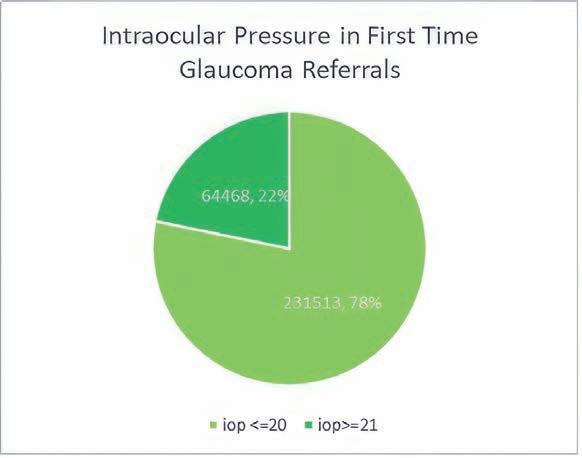
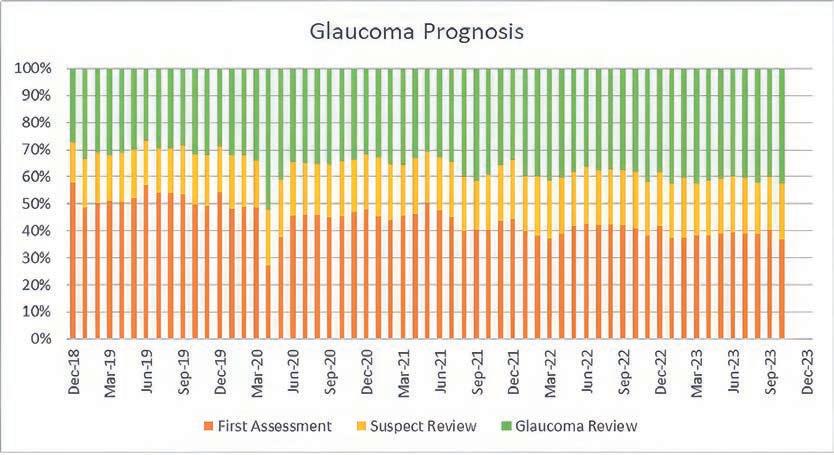
"OUR GLAUCOMA STRATEGY IS MULTIFACETED AND HAS COME ABOUT OVER MANY YEARS WITH A LOT OF DETERMINATION FROM A DEDICATED TEAM. THIS ARTICLE SEES JUST SOME OF THE PEOPLE BEHIND THIS STRATEGY EXPLAINING ITS VARIOUS ASPECTS THAT THEY HAVE CONTRIBUTED TO AND ANY DATA AND LEARNINGS ASSOCIATED WITH EACH."
more information as optometrists worldwide work to replicate what we are learning in Australia and New Zealand.
Our glaucoma strategy is multi-faceted and has come about over many years with a lot of determination from a dedicated team. This article sees just some of the people behind this strategy explaining its various aspects that they have contributed to and any data and learnings associated with each.
If you have any further questions or are a non-Specsavers optometrist and want to employ some of these strategies in your testing environment, please don’t hesitate to contact us. The more we can do as an industry to detect initial stages of glaucoma, the more likely we are to have a future without preventable vision loss from the condition.
TECHNOLOGY JEENA TAN, SPECSAVERS ANZ HEAD OF CLINICAL SYSTEMSDuring the past decade, Specsavers’ clinical systems and technology have been redeveloped and refined to ensure that all patients are receiving gold standard clinical diagnostics, and that this information is seamlessly accessible for optometrists. The most tangible element of the strategy was in 2018 when we installed OCT machines in every practice in Australia and New Zealand. We found that when we systematically used OCT on every patient as a part of their standard eye test in addition to consistent structural and functional assessment as per the RANZCO Referral Pathway for Glaucoma Management, detection of glaucoma increased substantially. On top of this, there were minimal changes to corresponding false positive referral rates. This data has most recently been published in detail in the Journal of Glaucoma study.
data, imaging and reports captured by each of these machines in their consulting room, they can be used in everyday testing and results can easily be compared over time, all at the click of a button. A feature to write therapeutic prescriptions electronically has also made it easier to prescribe treatments for glaucoma patients as required.
This has enabled our optometrists to confidently and appropriately co-manage more patients with glaucoma, ensuring our ophthalmology colleagues aren’t being inundated with appointments for routine checks that could have been carried out by optometrists thus enabling them to focus on the patients who truly need their support. This has become valuable in regional and rural locations where access to ophthalmology is not as readily available.
This is supported by our data which shows that over time, reviews for patients with confirmed glaucoma are increasing, indicating that patients are being actively reviewed and co-managed in Specsavers practices.


Since the rollout of OCT, we have integrated OCTs with our practice management system, networked our visual field analysers and integrated with our electronic referral platform. We continue to focus on leveraging technology to make it easier for optometrists to care for their patients. We know that if optometrists have straight-forward access to
Constant monitoring of patient outcomes has been critical to ensuring Specsavers’ glaucoma strategy has had the necessary impact on detecting previously undiagnosed glaucoma. Interrogating this data and making changes to our approach as needed has kept us on the right course. The high volume of patients seen across the Specsavers network means data is captured that can be analysed in a meaningful way to establish individual, practice-level, regional and national patterns in glaucoma detection rates. We empower our optometrists by feeding this information back to them through weekly reports, providing them with an understanding of how they are providing the right outcomes for their patients. This includes information on how each optometrist’s glaucoma (and other eye conditions) detection rates compare to expected population prevalence, as well as giving information on their referral patterns, inter-professional communications, and their use of diagnostic tests. These benchmarked
reports allow optometrists to understand their own practice patterns and identify any opportunities where the optometrist could further enhance patient outcomes or work on their professional development.
One example of this is when we discovered through data insights that if it was clinically indicated that a patient required a visual fields test, patients who underwent the visual field test on the same day were more likely to have glaucoma detected and a referral made. Whereas patients who did not have the test on the same day were more likely to not receive the test at all, making them less likely to have glaucoma detected, to be referred or to receive a diagnosis or treatment. To improve eye health outcomes for our patients, we worked closely with optometrists and practices to identify and eliminate the reasons why visual fields tests weren’t occurring on the same day. This was achieved through improved e ciency of clinic processes, communication and agility of roles and responsibility across store teams. Now, same-day visual fields tests occur for most patients, helping ensure that all patients receive the care they need.
Equipping optometrists with the latest knowledge, skills and processes to detect glaucoma in early stages is crucial to enabling best health outcomes for our patients.
As a part of my role, I am responsible for a team of clinical performance consultants who work across each Australian state
and in New Zealand, supporting optometrists and store partners to deliver best health and sight correcting outcomes through ongoing coaching and training. This includes working closely with store teams to enhance processes and communication techniques specific to their store, patients or technology. It also involves identifying opportunities for improvement as found in weekly benchmark reports.
Our team has been able to improve glaucoma detection rates and health outcomes for patients with glaucoma by focusing on processes such as increasing the occurrence of same-day visual fields, training clinical support sta in capturing high quality retinal imaging and even increasing patient support group referrals.
Specsavers is committed to ensuring that our optometrists are supported in their clinical practice with local and national opportunities for formal and informal education, whether it be our flagship Specsavers Clinical Conference, local CPD events or online education. In addition to cutting edge clinical training, our optometrists have access to education on communication, leadership and development to help them become the best optometrists they can be. By marrying gold-standard diagnostic equipment with focussed education to help optometrists get the most out of that equipment, we are able to help all our optometrists confidently diagnose and manage glaucoma.















V irtual Reality Visual Field device - incorporates complete Visual Field analysis.
Detailed progression analysis and the most versatile & efficient vision screening technology.














Latest technology provides the same reliability and reports as the “gold standard”.
Supplied complete with a Tablet PC –BlueTooth interface with the VF2000 NEO.



Compact/Space-saving/Portable - can be used anywhere, no need for a darkened room.

Ph: 1800804331 Email: sales@bocinstruments.com.au




















Features include:
FDT Testing





Active eye tracking –enhances reliability.
Full and Fast Thresholds VF Testing plus Neuro, Kinetic, Ptosis and Estermann tests














Stereopsis











Sensitivity
Visual Acuity and Contrast
Colour Testing (Ishihara, D15 and Advanced Colour Tests)
Eye Mobility and Strabismus






When Sunshine Coast ophthalmologist Dr James Walker opened his own private practice in 2022, space constraints and after-sales service influenced his choice of diagnostic equipment – but not as much as quality and ease-of-use.

Once he had committed to establishing his own rooms, Dr James Walker decided against ‘sticking with what he knew’ in diagnostic equipment, instead casting a wide net, exploring all the options before finding the right models to purchase – including a visual field analyser.
“When I was setting up my own purpose-built clinic about 18 months ago, as part of the process, I reviewed all the di erent equipment options,” Walker says, who previously worked in a group practice on the Sunshine Coast.
“I was accustomed to using a particular visual field analyser and was familiar with its printouts and presentation. However, the machine could be di cult to fit into certain spaces and the software had to be purchased as part of a package.”

Although he was familiar and proficient with the technology, Walker decided to look at alternative options for his new practice, Central Ophthalmology, located in the Maroochydore Central Precinct. Built from the ground up, the state-of-the-art practice is 200m2 and has four consultation rooms.
A colleague recommended the PTS 2000 Automated Projection Perimeter, manufactured by Polish company Optopol Technology and distributed in Australia by OptiMed.
“I liked the PTS 2000 because it o ered a cost-e ective solution that provided equivalent quality data in the same presentation format I was accustomed to, so I didn’t have to learn to interpret a di erent report,” he says.
“It also o ered the ability to have the machine controls separate from the examination bowl, which meant better use of floor space, and ergonomically, it’s better for my sta and patients.
"This means one sta member can easily monitor two machines at once because the control screens are separated. You can monitor a patient from a computer that’s remote from the machine, which was a big advantage for me as both a space saver and being a more e cient use of sta .”
Walker says OptiMed invited him to look at the PTS 2000 in its Brisbane workshop, and provided accurate measurements so he could assess where it would be best placed in his private practice.
OptiMed then loaned it to him for a month on a trial-basis.
Walker, who is also director of ophthalmology at the Sunshine Coast University Hospital and Health Service and provides remote public ophthalmology services in Mount Isa Hospital one week in four, liked how it performed from the get-go.
“Another advantage of the PTS 2000 is that the software and the remote review stations for doctors are all included in the purchase. OptiMed set it all up, and it worked well from the outset,” Walker says.
He has since linked his suite of equipment together using Pliny,

a Melbourne-based start-up that solves the fragmented and manual access of diagnostic imaging and data and retrieves it in real time to a single interface.
“Pliny enabled all my equipment software to talk together – my fundus camera, OCT machine, Anterion, the PTS 2000, slit lamp cameras, ultrasound – so numerous reports can be brought together in one cloud-based system, which I can review anywhere – any place with internet access.”
• Threshold testing can be completed in three minutes depending on a patient’s condition, delivering ZETA, ZETA Fast and ZETA Faster strategies for high reliability and precise threshold estimation
• New 24-2C pattern captures 10 additional central field locations with the new 24-2C pattern.
• Eye Tracking – monitors patient pupil movement during examination
• Blink detection – the software detects when the eye is closed, and will not present stimuli to the patient.
• H ead Tracking – monitors and adjusts the patient’s head position throughout the test
• DPA Defect Progression Analysis – creates a baseline and allows the following of disease progression over time.
• Eye See module – records an image of a patients eye during stimulus presentation.
• Journal of Ophthalmology study (Feb 2022) comparing ZETA Fast (Optopol Technology) and Humphrey SITA Fast (ZEISS) threshold strategies, concluded: “Both strategies enable effective identification of glaucomatous defects within six minutes; they also offer high sensitivity with a high correlation in global indices between the two strategies. The Optopol strategy is an alternative to the ZEISS counterpart with the limitation of a marginally longer testing protocol but a higher sensitivity of detecting glaucomatous defects.”
• When combined with the Optopol REVO S-OCT, the PTS 2000’s intuitive software enables practitioners to combine both OCT and visual field results for a quick and comprehensive structure and function single page report.
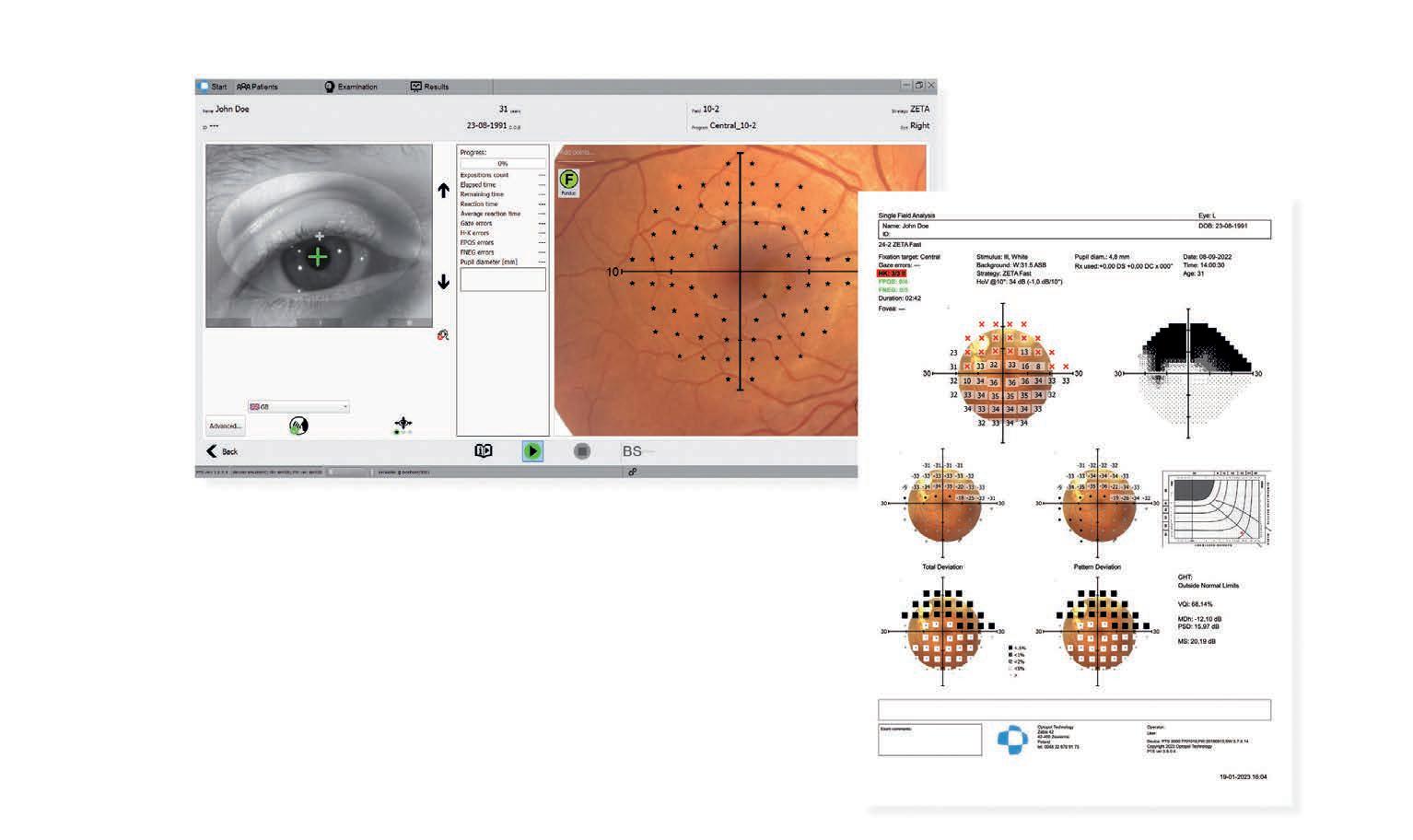
Structure & function analysis:
• PTS perimeter data can be exported to Optopol SOCT software, allowing the user to overlay the perimetry examination with fundus image or the SOCT layer thickness map.
• Thi s fundus-orientated perimetry approach helps to understand the relationship between structural glaucoma damage and the functional impact on patients’ field of vision
• U nderlay historical results with the newly acquired fundus maps
• Provides a comprehensive single-page report for glaucoma management
Quick field extension:
• Peripheral points – points from 30-2 added
• M acula points – points from 10-2 added
• Defect neighbour points – points 30-2/10-2 added
According to Optopol, its PTS 2000 has one of the world’s largest field testing ranges and options, including all of the Goldman stimuli sizes and colours used in perimetry, and its intuitive interface makes it easy for Walker’s clinical support sta to use.
It monitors patient pupil movement during the examination and its software detects when the eye is closed, and will not present stimuli to the patient. It also performs automated or semi-automated Kinetic perimetry.
While he primarily uses it to diagnose and manage disease progression in his glaucoma patients, Walker says the PTS 2000 has a wide range of functions, including familiar statistical and progression analysis and, of course, visual field testing for a driver’s licence.
“It can also capture 10 additional central field locations with a new 24-2C pattern, but generally speaking, although equivalent to competitors in terms of its diagnostic capability, the PTS 2000 has ergonomic advantages and is more cost-e ective and requires less maintenance with regard to software,” he says.
“The field analyser had to be comparable in quality and useability for patients before secondary aspects, such as how much space it requires or how fast it was, were considered. Once I’d established comparable quality and useability, it was these secondary aspects that pushed the PTS 2000 over the line in my final decision.”
Initially, Walker made provisions for two machines to support patient flow, but found one was su cient, as a typical glaucoma patient could have both eyes tested in under 15 minutes.
“Ophthalmology equipment’s footprint is growing, and space is at a premium. I had to think through how to utilise the floor space as optimally as I possibly could, and not compromise on quality,” Walker says.
“OptiMed were brilliant in that regard; they sent the key measurements to our draftswoman and the information they gave was correct and accurate, so when it came to installing it, it easily slotted into place.”
He says OptiMed quickly resolved minor teething issues without compromising the clinic or patient flow, which was important to Walker, as the only surgeon in his then-new private practice.
OptiMed’s excellence in product knowledge and after-sales service has led Walker to purchase additional equipment through the local supplier, including the Duo standalone swing table with Takagi UN-21 reclining chair system plus two Medinstrus compact motorised wall mount table systems.
“I also trialled – and then purchased – two of OptiMed’s Takagi premium slit lamps with camera, USee visual acuity charts, their LightLas YAG/SLT combo laser and the Iridex table mounted retinal laser,” he says.
“Their service has been first class. After-sales service was one of the main factors I was concerned about because once you have the machine, the last thing you want is it holding up your clinic, stressing out sta and leaving patients waiting unnecessarily.
“Whereas if you have good after sales service – they answer the phone, they’re attentive, and they’ll come and fix problems promptly – I think that’s money well spent.”


“I LIKED THE PTS 2000 BECAUSE IT OFFERED A COSTEFFECTIVE SOLUTION THAT PROVIDED EQUIVALENT QUALITY DATA IN THE SAME PRESENTATION FORMAT I WAS ACCUSTOMED TO.”
DR JAMES WALKER CENTRAL OPHTHALMOLOGY


Completely automated alignment, focus and measurement acquisition.
Flexible colour touch screen for versatile positioning.
Integration with Practice Management Software.
All four measurements, in both eyes, fully automatic.
Auto-Refraction
Auto-Keratometry
Non-contact Tonometry
Non-contact Pachymetry

Topcon’s fully automatic lensmeter.
Fully automated functionality
Large colour touch screen, great for lens mapping and light transmittance
Integration with Topcon CV-5000 or practice management software
For more information contact your Device Technologies

1300


Computerised Vision Tester - optional integration with PC-50s LCD Visual Acuity Chart.
Automated Refractor Head controlled by KB-50 colour touch screen and dial controller
Advanced integration – pull through previous script and/or auto-refraction, and export final subjective data to practice management software

Computerised lensmeter.
Colour touch screen control
Auto-progressive lens detection and UV transmittance
Integration with Topcon CV-5000 or practice management software
0508
At the completion of this article, the reader should be able to improve their detection of glaucoma using gonioscopy ...
Including:
• Review the types of gonio lenses
• Understand the Preferred Practice Pattern (PPP) Classification for Primary Angle Closure Spectrum
• Understand the limitations of anterior segment imaging and how gonioscopy can complement its use
• Develop evidence-based management plans based on gonioscopy and other clinical findings.
As primary eyecare providers, optometrists require every tool at their disposal to meet the rising incidence of glaucoma. Yet gonioscopy, one of the oldest – and arguably one of the most illuminating – techniques isn’t performed as often as it should be. In this two-part series, the authors share learnings from interactions with optometrists attending their gonioscopy workshops at the University of Western Australia optometry facility in 2023.
In 2023, we had the opportunity to conduct a series of gonioscopy workshops at the University of Western Australia. The workshops included a gonioscopy and primary angle closure theory refresher followed by a 30-minute guided gonioscopy practice session.
The optometrists who attended our gonioscopy workshops were WA-based and ranged in experience from new graduates to some with more than 30 years of experience. Most attendees acquired their degree in Australia with good representation across all states, others did their training overseas in countries such as New Zealand and the UK.
The attendees brought with them a shared curiosity about gonioscopy and a determination to master its use in their clinics. Because of that, they were also eager for us to discuss – and debunk – a number of gonioscopy myths.
MYTH: ANTERIOR SEGMENT IMAGING CAN REPLACE GONIOSCOPY
Anterior segment imaging has improved in recent years with faster anterior-segment OCT (AS-OCT) devices. However, one of the challenges with traditional AS-OCT is the limited number of radial B-scans used to acquire the image. This may give the clinician a false impression of the angle configuration given that virtually only a thin slice of each angle is examined.
This means isolated regions of peripheral anterior synechiae (PAS) or patchy pigment dispersion appearing between the image planes will be missed. The resolution may be improved by increasing the radial sampling such as through the use of radial rotating Schiempflug cameras (e.g. Pentacam) or swept-source OCTs, which can acquire in excess of 128 radial B-scans. Even so, gaps between scans are still not visible, resulting in only moderate agreement with gonioscopy.1 Another barrier to high-density AS
scanning is artefacts caused by eye movements or blinking. Furthermore, critical features such as trabecular meshwork pigments, blood and neovascularisation might not be appreciated well via an AS-OCT scan due to its absence of colour.
The iridocorneal angle plays an important role in the drainage of aqueous humour, accounting for up to 90% of aqueous outflow via the trabecular meshwork. The remaining outflow occurs through the ‘non-traditional’ or uveoscleral route. 2 It is the balance between aqueous production and drainage that gives rise to the intraocular pressure. Consequently, an obstruction or narrowing of the iridocorneal angle may give rise to increased intraocular pressure – though this is not always the case clinically.
Due to the unique properties of the cornea, direct visualisation of the iridocorneal angle is not straightforward. Light entering the limbus travels to the other limbus through the transparent


cornea in a phenomenon known as ‘total internal reflection’. This is partly due to the di erence in refractive indices between the cornea/tear-air interface. To break free of total internal reflection, light striking the corneal limbus has to return to the viewer at an angle > 46°. This may be achieved using direct or indirect forms of gonioscopy.
DIRECT GONIOSCOPY
In direct gonioscopy, a high powered ‘contact’ lens such as the Koeppe gonio lens is introduced to neutralise the air-cornea interface and to bend light away from the cornea and into the clinician’s view (Figure 1A). This often requires the patient to lie on their back while the practitioner views through the lens using a free space light source such as a Barkan illuminator. Direct gonioscopy is used mainly in operating theatres.
INDIRECT GONIOSCOPY
In indirect gonioscopy, a ‘contact’ lens containing mirrors, also known as a ‘gonio prism’, is placed on to the cornea to neutralise the air-cornea interface and to allow reflected light from the iridocorneal angle to be viewed (Figure 1B). With indirect gonioscopy, the patient sits upright and a slit lamp is used, allowing for comfortable viewing of the angles and better magnification.
Examples of indirect gonioscopy lenses include the large-diameter Goldmann lens and the smaller-diameter Volk G4 (Figure 1C). Indirect gonioscopy is the most commonly used type of gonioscopy in optometry.
Many clinicians would have encountered a ‘three-mirror’ lens, typically a Goldmann lens. The central lens is a contact fundus lens allowing the clinician to view the posterior pole. There are three mirrors; the rectangular mirror is used for the mid-periphery, the trapezoid mirror for the
equator, and the apical ‘thumbnail’ mirror for the far periphery/ora serrata under dilation and for viewing the iridocorneal angle.
Because only one mirror is used for gonioscopy, three-mirror lens-users have to rotate the lens on the eye to view each quadrant separately. Due to the large diameter of the Goldmann lens, even without a flange, dynamic gonioscopy is not possible.
Another common lens is the ‘four-mirror’ gonioprism known as the Sussman lens, which comes with a flange (large contact diameter) or without (small contact diameter). In some cases, they come with a handle (Posner style). Popular examples of Sussman lenses include the Volk G4, Ocular 4 mirror Sussman or the Katena Diamond 4 mirror lens.
Sussman style lenses without a flange are most convenient as they do not require a coupling fluid and do not require rotation as all four quadrants are in view simultaneously. They are generally also more comfortable for the patient.
Gonioprisms with flanges are typically more stable on the eye as they vault the cornea, creating a mild ‘suction’ force. The use of a viscous coupling fluid is essential to neutralise the air-corneal interface to ensure an unobstructed view of the angle as well as for comfort. However, as these lenses have a larger diameter than the horizontal visible iris diameter (HVID), this comes at the cost of not being able to perform corneal indentation.
To ensure consistency and unambiguity, it’s important that clinicians use consistent definitions for angle closure. One common misconception is to think that primary angle closure glaucoma (PACG) is synonymous with acute angle-closure crisis (AAAC). AAAC is more dramatic, but thankfully rarely encountered in primary practice.
The American Academy of Ophthalmology
Primary Angle Closure Disease Preferred Practice Pattern panel of 2019-2020 provided the following definitions of primary angle closure disease (Table 1).
Iridotrabecular contact (ITC), also known as an ‘occludable angle’, is generally defined as an angle ≤20° (Sha er system) or the non-visibility of the posterior trabecular meshwork (PTM). 3.4 Though it is worth noting that the AAO PPP5 defines ITC as the iris “appearing to touch the PTM”.
Given that the PTM is the site of the opening to Schlemm’s canal in which drainage occurs, it makes sense that a visible PTM would allow for aqueous outflow to occur. However, there may be situations where the more conservative definition of the AAO PPP may be better applied. This may include situations where only a small sliver of the PTM is visible, which may mean that drainage is still partially obstructed.


1 2 3
INFLAMMATION
Rosacea and blepharitis
DEMODEX

● Improved tear film quality
● Better meibum quality and expression




● Reduction in patient symptoms and neuropathic pain relief
● Reduced inflammatory markers in tears
● Maximising patient comfort through a flash-lamp water-cooling system to guarantee homogenous energy throughout the treatment process, which maximises patient comfort

● Regulated Pulse Train for safety and e ectiveness, resulting in less inflammatory reaction and no thermal damage

● Unique Stim-ULITM (Uniform Light Intensity) technology that o ers the best combination of clinical e cacy and patient comfort with a perfectly homogenous spatial distribution of energy







Images: Priscilla Ganesan.
One of the main changes to the definition of primary angle closure disease is the reclassification of angle closure suspects from the original International Society of Geographic and Epidemiologic Ophthalmology (ISGEO) classification of 270° ITC (three quadrants) to the more widely-accepted 180° (two quadrants or six clock hours). One of the reasons for this shift is that population studies 6 have found that >50% of primary angle closure disease is missed if the 270° definition was used. Even at 180°, it is believed that primary angle closure disease is missed. [For more information, see the review paper by Sun et al., 2017 7].

One promising development in anterior segment imaging is the hyperparallel OCT (HP-OCT) developed by Cylite. The HP-OCT acquires the entire anterior image instantaneously, thereby reducing the chances of motion artefacts encountered in traditional OCT. This allows for the acquisition of a dense volumetric scan of the AC providing the examiner a qualitative assessment of the full 360° view of the AC angle. With time, it is believed that Cylite will develop more software tools to assist in the automatic analysis of the AC for the measurement and quantification of the AC angle. Future studies are needed to validate its agreement with gonioscopy.
Another approach to AC angle imaging is the use of a purpose-built anterior angle imaging device in the market known as the Nidek GS-1000, which utilises a contact 16-mirror gonioprism attached to a camera, allowing for 360° imaging of the angle. Although the closest substitute to actual gonioscopy, this use of a Goldmann mirror precludes corneal
indentation, limiting the detection of PAS. Alternatively, practitioners fortunate enough to own a slit lamp camera, may choose to perform goniophotography manually.
At present, the only AAO PPP-endorsed imaging modality is ultrasound biomicroscopy, which is operator-dependent and time-consuming, but allows for better characterisation of plateau iris configuration4 than AS-OCT due to its ability to image the peripheral crystalline lens through the iris root.
Having said that, it is acknowledged that the advantages of AS-OCT, namely the repeatability and quantification of the AC biometry may lead to a better understanding of the natural history of angle closure and its prognosis over time. At this stage, we can only recommend the use of anterior segment imaging after gonioscopy for the documentation of regions of PAS, neovascularisation or anatomical features of clinical interest. In our experience, goniophotos are good for documenting the extent of PAS, the presence of neovascularisation, angle recession, pigment showers or other anatomical features as they cover a large region (typically a quadrant as opposed to a single slice) and you can appreciate colour. AS-OCT, on the other hand serves as a complementary teaching tool for both the clinician (e.g. the gonioscopy novice) and for patient education especially in cases where a referral for treatment is warranted.

for use with a slit lamp.
In Part 2 of our ‘Gonioscopy Primer’, we challenge the myths surrounding routine IOP measurement and reliance on Van Herrick (VH) angle measurements. Until then, keep practising your gonioscopy skills. The practice and the community you serve will no doubt benefit from it.
1. Porporato N, Baskaran M, Tun TA, Sultana R, Tan M, Quah JH, et al. Understanding diagnostic disagreement in angle closure assessment between anterior segment optical coherence tomography and gonioscopy. British Journal of Ophthalmology. 2019.
2. Fautsch MP, Johnson DH. Aqueous humor outflow: what do we know? Where will it lead us?. Invest Ophthalmol Vis Sci. 2006; 47 (10): 4181-4187. doi:10.1167/iovs.06-0830
3. B askaran M, Kumar RS, Friedman DS, Lu QS, Wong HT, Chew PTK, et al. The Singapore Asymptomatic Narrow Angles Laser Iridotomy Study: Five-Year Results of a Randomized Controlled Trial. Ophthalmology. 2022; 129 (2): 147-58.
4. H e M, Jiang Y, Huang S, Chang DS, Munoz B, Aung T, et al. Laser peripheral iridotomy for the prevention of angle closure: a single-centre, randomised controlled trial. Lancet. 2019; 393 (10181): 1609-18.
5. G edde SJ, Chen PP, Muir KW, Vinod K, Lind JT, Wright MM, et al. Primary Angle-Closure Disease Preferred Practice Pattern. Ophthalmology. 2021; 128 (1): P30-P70.
6. Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86(2):238-42.
7. S un X, Dai Y, Chen Y, Yu D-Y, Cringle SJ, Chen J, et al. Primary angle closure glaucoma: What we know and what we don’t know. Progress in Retinal and Eye Research. 2017; 57: 26-45.
Although both old and new devices can complement learning and management, particularly in challenging cases, a skilfully performed gonioscopy examination still remains the gold standard for AC assessments due to its 360° view and dynamic assessment of the AC angle.

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.




If you’re looking for a company where you can build a career –from graduate programs to full and part-time roles and store partnership, you’ll shine at Specsavers. spectrum-anz.com/ careers-at-specsavers











At the completion of this article, the reader should be able to improve their management of people with low vision ...
Including:
• Understand the fundamental importance of empathy in the diagnosis of low vision
• Review the latest developments in magnification devices, screen readers and other tools
• Understand the value of early referral, and how it impacts the patient journey
• Review a list of National and state low-vision support services.
Senior orthoptists from the Centre for Eye Research Australia NIKITA
THOMAS and FLEUR O’HARE share their perspectives on holistic low vision care, and how timely referrals for support can have a positive impact on quality-of-life for affected patients.
In a world that often takes clear vision for granted, individuals with low vision face unique challenges. Navigating daily activities can be a complex task, but with the right support and timely referrals, the journey becomes more manageable. Eyecare and allied health practitioners are in an excellent position to provide services that can improve the quality-of-life for people with low vision.
According to Vision 2020 Australia, it is estimated that over 575,000 Australians are vision impaired or blind.1 The prevalence of low vision in our community is higher in older age adults, commensurate with higher rates of sight-threatening eye conditions such as glaucoma and age-related macular degeneration.
The term ‘low vision’ refers to permanent vision impairment that significantly interferes with visual function, and cannot be adequately
corrected with spectacles, contact lenses, medication, or surgery. 2 Vision impairment may be caused by various eye conditions, such as macular degeneration, diabetic retinopathy, glaucoma, and inherited retinal disease, as well as neurological or traumatic injuries.
When considering referrals for low vision support and care, it’s essential to have a comprehensive understanding of the cause of the vision loss and its impact on the person’s daily function. It is also important to consider the individual’s personal and social circumstances when considering management options and to discuss this with them to encourage agency in managing their needs.
A truly person-centred and collaborative approach to low vision management is



achievable. It is vital that optometrists, orthoptists, ophthalmologists and the individual patients work together to map out the low vision management options available and identify the best plan. This also promotes a holistic partnership to low vision care and allows for a more comprehensive evaluation of a person’s needs. A strong multidisciplinary collaboration allows the individual to feel cared for and supported.
In our experience, we often hear stories of how the diagnosis of eye disease, and the reality of expected progressive vision loss, was delivered in a non-empathetic way. Our experience corroborates with the experiences shared in the UK where patients can feel like the diagnosis was ‘like being hit with a brick’. 3 The manner in which such news is delivered can have long lasting impact. Providing empathy, support and facilitating the provision of appropriate support services is key to alleviating some of this impact.
Certainly, early detection and early referral also supports this journey as well. In fact, they are cornerstones of e ective low vision management. Regular comprehensive assessments, that go beyond standard visual acuity tests, are vital. These should encompass visual field evaluations, reading ability and contrast sensitivity measurements,
All eye care providers should be aware of the pivotal role low vision rehabilitation services play in empowering individuals with low vision. In Figure 1 below, Vision 2020 Australia has produced the following list of organisations and services they provide:
Blind Citizens Australia
BCA is the national representative organisation of people who are blind or vision impaired.
Glaucoma Australia
Peak body providing free ‘sight saving’ education and support to people with glaucoma.
Keratoconus Australia
Helpline to answer questions about keratoconus, outreach services to connect people with keratoconus, advocacy on issues a ecting the keratoconus community, public information campaigns and seminars, and involvement in eye-carer training.
Macular Disease Foundation Australia
National helpline and resources, providing information on: macular disease, including age-related macular degeneration and Medicare rebates and safety nets, transport, accessing low vision services, latest research and carer support.
Retina Australia
Facilitate support to individuals, families and friends a ected by inherited retinal disease, provide information related to inherited retinal disease.
National Service and Support Organisations
Guide Dogs Vision Services
Provides tailored services throughout Australia including: Orientation and Mobility (O&M) services for children, teens, adults, including those over 65 years.
Vision Australia
Age-appropriate emotional support groups, occupational therapy, orientation and mobility training, orthoptists and functional vision assessments, education and employment support, aids and equipment sales, technology training, early intervention specialised services.
National Program
KeepSight
A national program led by Diabetes Australia and Vision 2020 Australia to reduce the current level of late presentations of diabetic retinopathy.
South Australia
Blind Welfare Association of SA Inc. Social and peer support groups, social activities, day trips and overnight travel groups.
Royal Society for the Blind Independent living training, assessment services
Tasmania
Guide Dogs Tasmania
Guide Dogs, Autism Assistance Dogs, Therapy Dogs and Companion Dogs.
VisAbility Tasmania
Occupational therapy, speech pathology, physiotherapy, exercise physiology, counselling, orientation and
Victoria
1800 033 660 bca@bca.org.au www.bca.org.au
1800 500 880 glaucoma@glaucoma.org.au www.glaucoma.org.au
0409 644 811 info@keratoconus.org.au www.keratoconus.org.au
1800 111 709 info@mdfoundation.com.au www.mdfoundation.com.au
1800 999 870 info@retinaaustralia.com.au www.retinaaustralia.com.au
Visit www.guidedogsaustralia.com
1300 84 74 66 info@visionaustralia.org www.visionaustralia.org
1800 533 774 support@keepsight.org.au www.keepsight.org.au
08 8367 6088 info@blindwelfare.org.au www.blindwelfare.org.au
1300 944 306 ndis@rsb.org.au or agedcare@rsb.org.au www.rsb.org.au
1800 484 333 info@guidedogstas.com.au www.guidedogstas.com.au
1800 484 333
03 9349 7400
Western Australia
Guide
VisAbility Western Australia
1800 847 466
1800 847 466
which all contribute to understanding how best to optimise residual vision. 4
Implementing standardised assessment protocols enhances the accuracy of low vision diagnoses, facilitating appropriate referrals based on the individual’s unique visual function profile. A focus on what is achievable (‘abilities’) rather than what has been lost (‘disability’) is the ultimate goal.
Don’t wait until your patient’s vision has reduced to legal blindness, or near-complete blindness. There is a window of opportunity to allow training and education before vision is severely limited.
Encourage referrals to certified low vision rehabilitation specialists who can provide personalised training, adaptive technology recommendations and orientation and mobility instruction. These services, as listed in Figure 1, aim to enhance independence and quality-of-life for those with low vision. These services often also provide individuals with training, job placement assistance and community integration programs, giving a sense of independence within the community.
Advancements in assistive technology allow for individuals to lead a more independent life. It Is crucial for optometrists and orthoptists to keep informed about the latest developments in magnification devices, screen readers and other tools. Knowledge in the area also allows for informed referrals to the correct specialists who can provide further expert guidance on how to incorporate the devices into daily living.
Functional aids and alterations in an individual’s home or work environment facilitates a sense of freedom. Tactile markings, voice-activated appliances, large print calendars, and better lighting make a huge di erence in ability to complete day to day tasks independently and inclusively.
If your patient is new to vision loss, it’s important they are introduced to the equipment and assistive technologies that truly support their needs.
1. Magnifiers, from basic hand-held glass magnifiers to electronic versions and iPhone apps
2. Mobility canes
3. Dots – basic stickers and tactile markers to help those with diminished vision use home appliances
4. Large print phones/keyboard
5. Electronic personal assistants, such as Google Home or Alexa
6. Seeing A.I. – A free app that provides a talking camera specifically designed for users with low vision
7. Liquid level indicator – small cup attachment that allows those with low vision to pour liquids without over filling their cup
8. Screen readers – software that uses an automated voice to read out loud words from text and alt-text based files on a computer screen
9. Plastic writing guides
10. Vision Australia library – Australia’s largest audio library.
Beyond the clinical aspects, optometrists and orthoptists contribute significantly to enhancing the overall quality-of-life for individuals with low vision. As mentioned, we recognise that emotional and well-being support across the entirety of the sight loss pathway may be needed.
Referrals to appropriate mental health professionals who specialise in vision-related challenges can provide tailored support. These support people may be found through enquiry to organisations that support those living with low vision.
As eye healthcare professionals, we play a crucial role in educating individuals and their family members about low vision and the unique challenges associated with it.
“A FOCUS ON WHAT IS ACHIEVABLE (‘ABILITIES’) RATHER THAN WHAT HAS BEEN LOST (‘DISABILITY’) IS THE ULTIMATE GOAL.”
Participating in community engagement events promotes health awareness and shared understanding. Community engagement is also useful in fostering social connection, where people can learn from each other. Actively learning from, and listening to, people with lived experience of low vision has helped us become better clinicians.
Education around low vision support to individuals and their families is an extremely important part of low vision care. Providing timely information on adaptive aids, assistive technologies, and community resources helps to strengthen agency and patient driven decision making. Together, we can enhance and optimise low vision care. Note: Although this article does not provide a comprehensive list of the organisations that provide low vision care in Australia, it does provides a few points of reference to help find the right people to help support those with low vision.


REFERENCES:
1. B. Ah Tong, G. Du , G. Mullen and M. O’Neill, August 2015, A Snapshot of Blindness and Low Vision Services in Australia, Vision 2020 Australia, National Disability Services, Australian Blindness Forum, Sydney. URL: https://www.vision2020australia.org.au/resources/a-snapshotof-blindness-and-low-vision-services-in-australia/
2. Australian Institute of Health and Welfare. A guide to eye health data. Vision problems in older Australians URL: https://www.aihw.gov.au/reports/eye-health/vision-problems-in-older-australians/summary
3. Ferrey A, Moore L, Jolly JK. ‘It was like being hit with a brick’: a qualitative study on the e ect of clinicians’ delivery of a diagnosis of eye disease for patients in primary and secondary care. BMJ Open. 2022 Jul 21; 12 (7): e059970. doi: 10.1136/bmjopen-2021-059970. PMID: 35863827; PMCID: PMC9315907.
4. Vision Matters – Orthoptic Vision Services. 1 Whitehorse Road, Deepdene VIC 3103 Australia. URL - https://www.visionmatters.com.au/
5. Vision Australia. Top 10 pieces of assistive technology for newly diagnosed patients. URLhttps://visionaustralia.org/news/top-10-assistive-tech-for-patients
6. Adult referral pathway for blindness and low vision services [Internet]. 2023 [cited 2024 Jan 15]. Available from: https://www.vision2020australia.org.au/resources/adult-referral-pathway/

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.


Each year, not-for-profit organisation Cambodia Vision recruits hundreds of volunteers to 'give the gift of sight' to disadvantaged and remote Cambodian communities. With research showing the country has one of the highest rates of preventable blindness, the organisation is doing what it can to address this statistic.


Family is at the crux of Cambodian culture and considered the foundation of life. Vision loss can sever this dynamic, with individuals in the family unit losing a sense of purpose. They feel burdensome to their relatives; childhoods are lost as kids become caregivers to their parents, and parents no longer able to provide for their family.
So, when their sight is restored by the Australian volunteers at Cambodia Vision, they approach them with their hands together in a bow of gratitude because they have recaptured the essence of a meaningful life.
Cambodia Vision is a not-for-profit that services the eyecare needs of a selected disadvantaged region in Cambodia each year. Since the first aid trip in 2007, it has provided critical eyecare and hearing services to thousands of Cambodians. In 2023, on 29 October to 4 November, the team setup in Mekong and Kampong Cham hospitals in south-eastern Cambodia, comprising 140 volunteers including nine ophthalmologists, 10 optometrists, four orthoptists, three anaesthetists, 17 nursing sta , a GP, two audiologists, a pharmacist and other support sta and interpreters.
Ms Thida Yang is among the founding members of the charity organisation. A Cambodian refugee now living in Australia, she takes this as an opportunity to resonate with her roots and give back to her community.
She continues to be a key organiser and has participated in every aid trip since its conception. “It gives me an opportunity to learn more about where I came from and contribute in a small way to help people in need,” she says.
Few would have envisaged the influential body that Cambodia Vision would become. What first began as a team of 13 servicing 150 people, now constitutes a team of 140 volunteers servicing an average 4,000 people each year. Although the growth was not anticipated, it has been welcomed and provides a beacon of hope for disadvantaged Cambodians dealing with refractive error and vision loss – some for many years.
Mr William Robertson, of Designs for Vision (DFV), first got involved in 2012 when he joined a friend for an aid trip to Cambodia. He says the rest is history and has been involved annually ever since, leveraging his ophthalmic equipment expertise.
“I became almost addicted since then. It feels like a real calling for me,” he says.
“Cambodia Vision addresses eyecare health disparities and conditions that would be treated immediately in Australia and not result in blindness, which are often overlooked here. The eye health in this country is exacerbated by inadequate education and diet.”




Robertson says the mission of the foundation is “to give them Australian standard eyecare”.
His role at DFV has equipped him with access to connections within the optical industry to provide Cambodia Vision with much needed equipment for the philanthropic e orts in Cambodia. This a liation with the optometry and ophthalmology diagnostics company has proven instrumental where he has been able to organise nine Keeler LED slit lamps, optical biometer and B-scan ocular ultrasound in addition to glasses and frames for the aid trips.
This, in addition to donations made by companies such as Bupa Optical, HOYA and Alcon, play an essential part in mobilising this cause.
“HOYA essentially gave us 600 IOLs and Bupa Optical, during World Sight Day, were donating $5 a frame for each pair of glasses,” Robertson says.
Yang adds: “Bupa Optical have sold more than 9,000 pairs of glasses and contact lenses, which means they’ve raised over $45,000.”
The foundation is generously supported by several corporations, one of them is the ABC Tissues company, which also provides funds and locations to store the equipment until a container can be sent to Cambodia stocked with medicines, drops, drapes and scalpels for surgeries, as well as glasses and hearing aids, among a host of other supplies.
Everyone at Cambodia Vision is celebrating the recent mission, which was a success emerging from the pandemic. In fact, it was the first full-fledged trip since 2019.
To prepare, the foundation established a pilot mission in December 2022


"CAMBODIA VISION ADDRESSES EYECARE HEALTH DISPARITIES AND CONDITIONS THAT WOULD BE TREATED IMMEDIATELY IN AUSTRALIA AND NOT RESULT IN BLINDNESS.”WILLIAM ROBERTSON

to identify and quash any obstacles or hindrances. They realised that the aftermath of the pandemic still lingered: medical sta and supplies were in high demand, so volunteers struggled to take time o and there were di culties sourcing stock.
Yang says the ‘great resignation’ within the medical industry a ected the relationships with the companies through which they organised many supplies.
“We’re finding that we now have to build new relationships with most of the drug companies that we have dealt with before,” she says. “That’s another big challenge for us because we’re still relatively quite small and 100% run by volunteers. So, we rely on fundraising for community donations and on corporate sponsorship.”
Despite these impediments, the volunteers forged ahead as thousands of people awaited their care at Cambodia Vision marquees from the outset. Some had travelled for days along the roadside in hope to be seen. Often, there’s no time for settling in, as the locals stood waiting in their droves.
“There’s just a sea of people sitting out in the marquees waiting to be seen,” Robertson says.
“There would have been 6,000 to 7,000 people who turned up to see us. A lot of volunteers would have been daunted by the amount of people already waiting, because we only got to screen more than 3,500 people,” Robertson says.
Despite the volume, Robertson says there’s a fluidity and rhythm that defines the team dynamic. Although chaotic, everything seems to flow.
After registration, the locals wait for a visual acuity test.
To help manage the queues, Robertson explains to them: “We’re lucky. By the fluke of birth we were born in Australia which has an advanced health care system to look after us. But we are all brothers and sisters and, in turn, we need you to look after one another. So, look at who is on the left and right of you and stay with them until your eye testing is complete.”
Moving six people at a time, they then undergo autorefraction, tonometry and eye drop dilation.
This prepares them to see one of 10 optometrists, who are equipped with their own slit lamps and translator. At this station, the optometrist will inspect the structures of the eye and identify whether they require surgery for pterygium or cataract – or whether they cannot be treated.
“We get lots of people who’ve got chemical burns and penetrating eye injuries possibly needing corneal transplants,” Robertson says.
By the conclusion of the week, Yang says that 3,589 people were screened, 551 pairs of prescription glasses dispensed, thousands of sunglasses distributed and 564 – mostly cataract – life-altering surgeries performed. One-thousand and twelve people were assessed for hearing, and hearing aids were provided where appropriate.
The turnout for Cambodia Vision clinics is attributable to the reputation
the organisation has built over the last 15 years. It has earned the trust of the Cambodian people by ensuring the service is of upmost quality. That is, medical volunteers are registered ophthalmologists, nurses, anaesthetists, GPs, orthoptists, pharmacists and optometrists who are experienced and trained in Australia, and technology, equipment and medicine are up to date.
“We do what we can to maintain our reputation. The work we’ve done beforehand, we need to hold on to that,” Robertson says.
The organisation’s services are promoted on national TV in addition to radio broadcast and social media. But a lot of the awareness comes through word of mouth.
Cambodia Vision is entirely self-funded, relying on donations from sponsors and community support. Fundraising e orts occur throughout the year and provide the necessary support for its annual missions.
These include Buddhist ceremonies at Cambodian temples in Melbourne and Sydney, and a major fundraising night in Sydney, Brisbane and Melbourne.
Commercial support includes the East Chinese Restaurant on Sydney’s harbour at $40,000 annually, ABC Tissues, Mur Thai Food Company, Lim's Pharmacy and National Auto Glass Supplies at $10,000 annually. The 2CR China Radio Network – A Loving World also conducts fundraising every second year for the cause. Additionally, Granata Eyecare in Northmead, Sydney donate frames to the foundation every couple of months.
“There’s many things happening almost organically in the background,” Robertson says.
He explains that the work of Cambodia Vision is important for breaking the cycle of disadvantage and the ripple e ect of helping a single person.
For example, an elder who is dependent on a child for basic tasks is potentially withholding that child from an education and social life. Therefore, by delivering eyecare services to this elder, Cambodia Vision is alleviating the healthcare burden of preventable blindness within the entire family unit.
It also provides children with refractive errors access to glasses, and suddenly schooling becomes much easier.
The impact that the services provide on these one or two individuals starts to positively impact the broader community as they become functioning members of their village.
“For those people who’ve helped, and especially those who came this year; you’re to be congratulated. They should feel proud of themselves because we made a huge change and we’ll be back to do it again this time next year,” Robertson says.
“It’s an amazing thing to do. I really am honoured to be able to do it.”
Yang adds: “We’re changing things in a small way, but it makes a big impact. It makes quite a big dent in the community, and the country as a whole. We’ve been really pleased; it’s what keeps us going.”
For next year’s mission, Cambodia Vision is seeking registered ophthalmologists, optometrists, ophthalmic nurses, general practitioners, optical dispensers and orthoptists. To donate, enquire, or get involved, visit: cambodiavision.org.au/

















Optical Distributors and Manufacturers Association’s upcoming trade fair, OSHOW24, is poised to champion the Australian independent optical market. The event is known for its boutique feel and lively atmosphere, and is returning with some notable improvements in May.
With an extensive product showcase, professional development opportunities for the entire practice team and all-new industry awards program, Optical Distributors and Manufacturers Association (ODMA)’s OSHOW24 is building on its predecessor to be the largest, and most invigorated yet.
A biennial event that alternates years with the O=MEGA conference, the boutique trade fair is unique to the industry, boasting features that cannot be found in other events within the same bracket.
This year it will feature a well-balanced blend of professional development for the broader practice team, fashion-focused presentations, topped o with the presentation of awards to champion the release of exemplary products since O=MEGA23. A few other additions have also been made to enhance the attendee experience.
The optical trade show is returning to Sydney’s Hordern Pavilion in Moore Park, running from 17-18 May 2024. In a strategic collaboration, this coincides with the Optometry NSW/ACT Super Sunday clinical conference event set for 19 May (o ering 10 CPD hours at Doltone House, Darling Island), meaning optometrists can shop around for the latest products and equipment before getting their fix of CPD content across the same weekend. The event is also strategically being held near the end of the financial year to promote greater trade.
ODMA CEO Ms Amanda Trotman says the association’s flagship trade event, OSHOW, fills a gap in the optical event market that already has an abundance of clinically focused programs. The 2022 show featured 130 booths, with almost 1,000 unique buyers visiting the event. Held shortly after lockdowns lifted from the pandemic, ODMA expects 2024 to be larger.
“[OSHOW] was born out of two things; one to have a free event that people can come in and see all the products under one roof, and two, it’s not necessarily linked to a clinical conference that’s happening alongside it,” Trotman says.
ODMA’s ethos is strengthening the independent optical market, bolstering Australian distributors, and ensuring consumers have choice.
With this in mind, Trotman says OSHOW bridges the gap between excellence in clinical service delivery – a hallmark of independent optometry – and the commercial aspect that supports it.
“We bring suppliers together to encourage practices to come out and get excited about the product and about the opportunity of selling it,” she says.
A defining characteristic of the event is that it provides one of the only opportunities to see such a comprehensive range of products in person and with demonstrations. As sales representatives cannot take their entire suite of products to practices, this may be the only instance where attendees can see such a wide range in one place.
As such, OSHOW works to empower practitioners with choice and Trotman ensures they will find something suitable to their clientele demographic.
“There is something there regardless of whether your practice is located regionally or in the city, and to meet the specific needs of your particular practice demographic; it’s really a chance to walk around and see everything,” Trotman says.
“You can get a demo of five di erent machines in a couple of hours; that’s quite a good investment of your time.”
Aside from frames, lenses, diagnostic equipment and other technology, the event has been curated with the whole practice team in mind.
ODMA has made it a priority to ensure optometrists, practice managers and optical dispensers can be engaged in its events and Trotman says there will be valuable management tips covering commercial aspects such as succession planning, stock management and social media strategy.
“We’re providing an opportunity for practices to invest in their team. We appreciate that time is money so even a free event is an investment. However, this really does help involve the whole team in the future of the business,” she says.


“It is so important to keep sta aware of all the new products and technologies on o er, to have them contributing to ways the practice can better service patients' needs whilst having them all contributing to an improved bottom line.”
Geographically, OSHOW24 will cater mainly to the Sydney/NSW demographic. Last time, in 2022, 69% of attendees were from NSW. But when OSHOW was held in Melbourne around 80% were from the home state. This perhaps indicates Sydney is a more accessible location for the show for interstate attendees. In 2022, Victorians and Queenslanders made up around 11% of attendees each, while 3% came from South Australia, 2% from Western Australia and 1% from New Zealand.
Trotman says what di erentiates OSHOW is the opportunity it gives relatively smaller market players to display their products.
She says there is a cap on the maximum number of booths per exhibitor and few custom-built stands to ensure a diverse, equitable display so "everyone’s on a level playing field and it’s all about the product".
Another key feature of the 2024 program is Frames Central, where the frame displays are smaller to hero a single range or brand, so they do not get lost in a sea of products.
Trotman says these displays are a more economical option, as smaller distributors are not required to purchase a more expensive booth.
However, while there is an emphasis on frames, there is equal emphasis on lenses – with notable market players involved including ZEISS, HOYA, Rodenstock, CR Surfacing Laboratories and EssilorLuxottica.
Carefully designed, OSHOW24 will ensure attendees can network even if they have clinical obligations during event hours. ODMA has extended the trade fair opening hours until 7pm and, with the Super Sunday conference held on the Sunday, OSHOW24 will hold a networking event on the Saturday evening, ensuring a seamless transition from commercial to clinical activities.
As a first, ODMA will also hold an industry award program for OSHOW24. Previously, the association’s industry awards were only run biennially at O=MEGA.
An almost four-year hiatus due to the pandemic meant that a lot of high-quality candidates missed out on awards. Thus, to properly celebrate industry players, Trotman says the awards are a key feature of OSHOW24 this year.
Additionally, as previous awards at O=MEGA have mainly focused


“WE BRING SUPPLIERS TOGETHER TO ENCOURAGE PRACTICES TO COME OUT AND GET EXCITED ABOUT THE PRODUCT, AND ABOUT THE OPPORTUNITY OF SELLING IT.”
on technical achievements, award categories for OSHOW24 have broadened to capture commercial winners and celebrate creativity, fashion and flair.
And coming o the back of recent SILMO Paris (29 September to 2 October 2023) and MIDO (Milan 3-5 February 2024) eyewear releases, there is expected to be a multitude of candidates.
All entries will be displayed in a dedicated area within the venue. Trotman says every candidate will receive publicity, with the winners announced at the networking event on Saturday evening to “add to the buzz of the OSHOW event”.
“Whilst ODMA ran an extensive awards program in 2023 at O=MEGA, OSHOW provides a great excuse to focus on a few specific awards that relate more to new product releases, fashion and trending items,” she says.
“Award categories will be focused on eyewear released since O=MEGA23, with a focus on the materials used, colour and fashion trends. Plus, there will be awards for innovative products released in the last 12 months.”
Although categories and judging processes are still in development, ODMA’s current plans are to include some practice focused awards, in addition to practice voting for products to emulate a “people’s choice” type award program.
POLARISED LENSES DON’T HAVE THE MARKET PENETRATION THEY PERHAPS DESERVE. APRIL PETRUSMA BREAKS DOWN THE OPTICS SO MORE PEOPLE CAN BENEFIT FROM THIS LENS OPTION.

"THE ROWS OF IODINE CRYSTALS CONTAINED WITHIN THE POLARISED LENS BLOCKS THE DISABLING HORIZONTALLY VIBRATING POLARISED LIGHT WAVES AND ALLOWS ONLY
THE VERTICAL VIBRATING LIGHT WAVES TO REACH THE EYE."
n today’s world, most would assume it to be common practise amongst eyecare professionals to recommend polarised filters for patients’ sunglasses with the aim of reducing disabling and blinding reflected glare. Unfortunately however, data shows that few optical dispensers fully understand the nature of polarisation and how polarised lenses can truly benefit the patient.
According to Younger Optics – a global leader in prescription polarised eyewear – polarised Rx sunglasses make up just 7% of global prescription eyewear sales. This isn’t because only 7% of patients benefit from them, rather there is a lack of awareness from both eyecare professionals and consumers.
For eyecare professionals to fully understand how polarised lenses work, it helps to understand the basics of how light behaves.
Light itself is the interaction of both electric and magnetic fields travelling through space. The electric and magnetic vibrations of a light wave occur perpendicularly to each other. This means the electric field moves in one direction and the magnetic field in another. These electric and magnetic vibrations can occur in numerous planes but will always be at right angles to each other or 90 degrees apart.
To keep it simple when describing light behaviour in optics, we generally consider the directions to be horizontal or vertical as shown in Figure 1.
A light wave that is vibrating in more than one plane like this is known as “unpolarised light”. The light emitted by the sun, the stars, by a lamp or a torch are all unpolarised light sources.
The process of transforming unpolarised light into polarised light is known as polarisation.
Contrary to unpolarised light, polarised light waves are light waves in which the vibrations occur in a single plane only. This means plane polarised light consists of waves in which the direction of vibration is the same for all waves. We no longer have a horizontal and vertical direction of travel, only one or the other.
In Figure 2 you can see that when unpolarised light hits a flat horizontal surface, some of the light is refracted and absorbed beyond the surface and some bounces straight back o the surface and is reflected. The light that is reflected is on the same angle as the surface and is a single light wave only, which means it is now vibrating in only the horizontal plane and has become ‘polarised light’.
Unfortunately for us and our eyes, when light is reflected off shiny horizontal surfaces and the light is transformed into polarised light, that light produces blinding glare. This blinding glare can obscure or completely block our vision which is why we care about it so much.
If you’re wondering how this phenomenon occurs, it’s all to do with the exact angle the light hits the surface in the first place. When light strikes a surface so that there is a 90 degree angle between the reflected and refracted rays, this is when the reflected light becomes plane polarised.
The direction of polarisation will then always be parallel to the surface, so if we are talking about a horizontal body of water, the plane polarised light will also be vibrating horizontally. The angle of incidence that produces the 90 degree angle is a phenomenon called Brewster’s angle.
It was Sir David Brewster, a Scottish
physicist, who first discovered this in 1811. Brewster’s law states that maximum polarisation happens when the reflected ray and the refracted ray are perpendicular to each other.
Polarising filters work just like an invisible picket fence or jail bars. To fully understand the process, if you picture yourself holding a broom handle horizontally and trying to pass it through the fence or the jail bars – it’s not going to happen, it’s impossible! But if you held it vertically, it would travel through the gaps nicely.
It’s the same analogy for polarised light waves. The vertical light we need, passes through the gaps no problem. But the horizontal polarised light is blocked and can’t penetrate through to the eye (Figure 3).
This is because polarised lenses have millions of parallel rows of tiny iodine crystals (so small they can’t be seen with the naked eye) and they act just like the fence. The rows of iodine crystals contained within the polarised lens blocks the disabling horizontally vibrating polarised light waves and allows only the vertical vibrating light waves to reach the eye.
Non-polarised sunglasses only filter ultraviolet (UV) rays and reduce the amount of general light transmission.



They do not prevent glare as they do not stop unwanted horizontal polarised light from reaching the eye.
While polarised lenses offer numerous benefits in reducing glare and enhancing visual clarity, there are certain occupations or activities where they may not be suitable


or recommended like in aviation and some medical or sporting professions. For the most part, however, as stated by Rodenstock’s Nicola Peaper “the most efficient solution for disabling and blinding glare is a polarising lens with a back surface anti-reflection coating that also reduces UV reflection”.
APRIL PETRUSMA is the CEO of Optical Dispensers
Australia and a Senior Lecturer at the Australasian College of Optical Dispensing. She is a qualified Optical Dispenser, RTO Trainer and Business Manager with a degree in Visual Communication.




































ORTHOPTICS AUSTRALIA PRESIDENT DR AMANDA FRENCH DISCUSSES A CURRENT FOCUS ON THE ORTHOPTICS SCOPE OFPRACTICE, AND THE BENEFITS TO EYECARE DELIVERY IF EXPANDED.

GAIN FROM ORTHOPTISTS WORKING IN EXTENDED AND ADVANCED SCOPE OFPRACTICE, WE NEED TO ADDRESS WHY CURRENT SCOPEOF PRACTICE IS NOT BEING MET."
Orthoptics Australia is celebrating 80 years since its establishment in 1944 as the peak body for orthoptists in the country. This reflects the long history of the healthcare professionals working together nationally to advance the profession and improve quality of eyecare. It also marks the 80th Orthoptics Australia Conference, a testament to the peak body’s commitment to building the evidence-base for the discipline and disseminating research to improve eyecare services. We are looking forward to celebrating our significant progress in the past 80 years, both as a national peak body and as a profession that is well established, highly skilled, and essential to eye healthcare delivery.
In 2024, Orthoptics Australia is putting a focus on orthoptists working to the top of their scope-of-practice –‘making a di erence’ to eyecare service delivery and, most importantly, to the lives of their patients. We are continuing to implement our 2023-2026 Strategic Plan, with several key initiatives focused on promoting the value of orthoptics, increasing awareness, and growing the profession. Our strategic vision places an emphasis on not just supporting orthoptists to provide excellence, but
improve access and equity of eyecare services.
This message is timely, given the government’s ‘Unleashing the Potential of our Health Workforce’ Scope of Practice Review is well under way. Orthoptics Australia’s submission in the project’s first round of consultation highlighted the significant advantages to be gained by orthoptists working to the top of their scope within primary care settings. This included expanding access to management in primary care and community health settings, particularly for paediatric patients with strabismus and amblyopia and those with post-stroke visual impairment, strengthening referrals into tertiary eyecare, and reducing burden on public eyecare services. However, several barriers were identified, including a lack of awareness of orthoptic scope-ofpractice and competencies, as well as legislative and regulatory barriers.
We have several examples of innovative practice where orthoptists are working to the top of their scope and in advanced and extended practice through orthoptic-led services and clinics both in Australia and abroad. The positive impact of these models of
valuable and impactful to the health system, employers, and patients. Unfortunately, this is not the norm and more must be done to support orthoptists to take on these roles that will benefit patient care and the broader healthcare system.
As part of this work, Orthoptics Australia vice president Ms Catherine Mancuso and I facilitated a workshop on orthoptic scope-of-practice as part of the 2023 Orthoptics Australia Conference held in Perth. Orthoptists in attendance provided feedback on aspects of this, with over 50% indicating that they did not feel they were working to the top of their scope within their current workplace. This so clearly demonstrates that orthoptists are not being enabled to work to their scope-of-practice and are severely underutilised. Given the potential gain from orthoptists working in extended and advanced scope-of-practice, we need to also address why this is currently not being met.
Orthoptics Australia welcomes the Scope of Practice Review, with this work having the potential to make significant advances in Australia’s approach to health service delivery. As an organisation, we will continue to actively consult throughout the project, as well as work to clearly define extended and advanced scope-of-practice for orthoptists and advocate for structures limiting this to be addressed. We hope these initiatives will result in positive changes for orthoptists and for the benefit of our patients and the healthcare system.

ABOUT THE AUTHOR: Associate Professor Amanda French is the President of Orthoptics Australia. She graduated as an orthoptist from the University of Sydney in 2007 and completed her PhD in 2013.
 KAREN CROUCH
KAREN CROUCH
"CONSIDER EMERGING COMMUNITY OR PATIENT DEMANDS TO BE ACCOMMODATED OR OPPORTUNITIES TO DIFFERENTIATE THE PRACTICE BY INTRODUCTION OF NEW SERVICES."
When the New Year rolls around, it’s an ideal time for practices to look inward. Reflections and resolutions to improve performance should be a priority, alongside analysis of lesser achievements for implementation during the upcoming year.
Practices are comprised of certain essential factors that operate in direct relationship to each other, such as:
• plans and goals (financial, non-financial, clinical, strategic)
• administrative (client service, service e ciency)
• personnel (employees, owners – human resource management).
The most obvious consideration at this mid-point of the financial year is a half yearly review of progress to date, as well as achievements to targets and budgets.
Accountants and practice managers should construct a snapshot forecast of likely progress to financial year end, reflecting performance and trends indicated by past six month actuals. For example, does performance to date suggest targets will be met or exceeded? Are changes required (New Year resolution) to ensure year-end targets are met? Not all targets are financial.
• Client surveys: if regularly conducted, do they reflect targeted levels of satisfaction, clinical and administrative? Do responses reflect satisfactory client opinions including pre and post consultation?
• Regulations: consider changes to government policy that require rewriting of ‘policy and procedure manuals’. Do technological advances deserve investigation to maintain competitive positioning?
• Marketing: have there been notable changes in community health conditions that require new treatment methods or employment of modern equipment?

• New business: is the practice maintaining close ties with all referral sources by ongoing relationship management?
• HR: is an e ective ‘sta appraisal’ system in place, well documented, and well planned to occur during upcoming months?
As a starting point, let’s look at the business-as-usual structure of the annual ‘business plan’ that typically comprises two main sections: tactical (micro level) and strategic (macro vision). One is short term operational, the other targets are longer term practice owners’ objectives.
TACTICAL:
This is the ‘business-as-usual’ framework by which practices function (healthcare, services, revenue generation, expense management) to ensure financial viability and support for initiatives to achieve strategic goals, including:
• Expenses: line-by-line budgets, based on historical experience or educated guesstimates for start-ups, remembering cyclical peaks and CPI increases;
• Income: revenues based on practitioner numbers, working hours, charging rates and consultation/treatment numbers. Any shortfall or excess should be carefully analysed as both are vital to maintaining a viable practice;
• Measuring: tracking mechanisms that measure performance to targets, including ‘variance explanations’, are vital to ensure performance is on track, or requires adjustment. Monitoring is achieved through measurement of:
- KPIs: performance rates e.g. 90% patient satisfaction, patient numbers, individual sta performance targets;
- Ratios: (e.g. salaries-to-expense, overheads-to-expense) benchmarked to industry norms;
- Analysis: better-than-budget performance highlights repeatable practice strengths; poorer outcomes present opportunities to analyse problems and remedy them;
• Non-financial: it may be necessary to adjust, or introduce new clinical and administrative procedures to ensure compliance with changing business imperatives or external factors;
• Human Resources: this vital element covers plans to develop sta and practitioners, targeting ‘employer of choice’ status;
• Capital: if expansion or upgrades are planned, related costs such as borrowing, and repayments should be factored;
• Profit & loss: expenses vs. income reflects the likely year-end result. Current ‘year-to-date run rates’ across the upcoming month are a useful indicator.
• Landscape Changes:
- Competition: Have new practices opened in the area? Do they o er services your practice may not? Apart from product or service di erentiation, perhaps consider something more client focused; for example longer opening hours, including weekends. Consider emerging community or patient demands to be accommodated or opportunities to di erentiate the practice by introduction of new services.
- Technology: has new technology improved patient care, productivity or reduced costs? Has cost benefit of new technology justified investment from a financial or competitive perspective?
- Previous year’s results: if objectives have been exceeded, higher goals, including stretch targets, should motivate success and the practice mantra that ‘satisfactory results are not enough, we aim to exceed expectations’;
- Continuous improvement: have employee meetings and forums been adequately focused on operational productivity and the general theme of ‘working smarter, not just harder’?
STRATEGIC:
Vital to growth prospects is the optimisation of new opportunities. This could include business expansion by acquiring another practice, or reputation enhancement by becoming recognised field leaders.
As the current ‘business plan’ is reviewed, concurrent attention should be given to the longer term ‘strategic plan’. Does it also deserve tweaking and is it still achievable?
If strategic plans cover three year periods, annual business plans should target progressive completion of stated goals so aspirations are successfully achieved by three years.
ABOUT THE AUTHOR: KAREN CROUCH is Managing Director of Health Practice Creations Group, a company that assists with practice set ups, administrative, legal and financial management of practices. Contact Karen on email kcrouch@ hpcnsw.com.au or www.hpcgroup.com.au.

one of the more macabre. However, it’s a very apt description of how we do surgery. There are so many nuances to how clinicians perform an operation, all a totally acceptable standard of care and all giving excellent outcomes. Clinicians work out what works best for themselves and for their patients.
Although these di erent approaches all provide good quality care to our patients, they are not all equal when it comes to sustainability. Waste is an enormous issue in healthcare. Not only do wasteful practices lead to unnecessary physical waste, often depositing more plastic into the natural world already su ering under a sea of plastic, but also lead to increased greenhouse gas emissions. Wasteful practices also come at a significant financial cost, adding expense to an already financially stretched system for little or no benefit. This drives up the cost of running hospitals, public and private, and can undermine the private healthcare system leading to increased insurance premiums putting pressure on insurance rates.
The RANZCO Sustainability Committee is developing Sustainable Practice Guidelines (SPGs) for various types of procedures. The aim is to assess the di erent approaches taken by di erent surgeons when

together in one place, the SPGs. This can then be used by surgeons to ensure that they are not only providing good care, but also using an evidence-based approach to provide care in the most sustainable manner. Less waste, lower emissions and less cost to the healthcare sector.
The SPGs are only recommendations, but they are evidence based where evidence is available and can provide for a more sustainable practice benefiting patients, hospitals, surgeons and the wider community. They are meant to enable surgeons to make changes, knowing that these practices have been assessed and supported by their peak body, RANZCO. Where relevant, RANZCO will also involve other key stakeholders in the development of these guidelines. Groups include those representing nurses, infection control, together with other medical colleges such as the Australian and New Zealand College of Anaesthetists (ANZCA) and the Royal Australian College of Surgeons (RACS) and international, multinational groups such as EyeSustain.
SPGs are currently near completion for both cataract surgery and intravitreal injections, with new areas hopefully to be added in the future. Once completed, they will be uploaded to the RANZCO website.
The SPGs contain a number of common themed recommendations. A simple one is to review the surgical
drape type that is utilised: is it larger than it needs to be? The use of postoperative topical antibiotics in both intravitreal injection procedures and cataract surgery; the latter in the setting of the common practice of intraoperative intracameral antibiotics has enough evidence base that many clinicians and institutions have stopped using topical antibiotics following both procedures. This not only saves on waste and money but may reduce the development of resistant strains of bacteria in the community and reduce post-operative corneal epitheliopathy associated with multi-drop usage. A common practice for identifying waste when performing surgical procedures involves looking for items opened but not used, especially those present in a standard, pre-packed set. These packs invariably come with single use items such as a speculum, caliper and forceps. As highlighted in recent studies, whether used or not, they all end up in the waste. Individuals can give this feedback to hospitals, day surgeries and suppliers, indicating that waste will be a factor in evaluating the usage and purchase of future consumables. Apathy, a lack of awareness of the waste that we produce, and the fear of deviating from standard practice are perceived deterrents of change. Developed using an evidence-based approach and endorsed by RANZCO, the SPGs should encourage and enable change, helping to save the environment and to contain the cost of delivering the highest possible standard of medical care to the Australian community.
Names: Dr Michael Loughnan PhD FRANZCO; Dr Sukhpal Sandhu MD FRANZCO
Affiliations: Eye Surgery Consultants; Clinical Trials Research Unit, Centre for Eye Research Australia, University of Melbourne, The Royal Victorian Eye and Ear Hospital
Location: Melbourne (both) Years in industry: 35; 25
APATHY, A LACK OF AWARENESS OF THE WASTE THAT WE PRODUCE, AND THE FEAR OF DEVIATING FROM STANDARD PRACTICE ARE PERCEIVED DETERRENTS OF CHANGE.
email: myles.hume@primecreative.com.au

MARCH 2024
OPTICAL DISPENSERS AUSTRALIA GALA
Melbourne, Australia 1 March odamembers.com.au
SKI CONFERENCES FOR EYECARE PRACTITIONERS
Furano, Japan 3 – 10 March skiconf.com

ARVO 2024
ANZ CORNEA SOCIETY AND EYE BANK MEETING
Melbourne, Australia 7 – 8 March ranzco.edu/events
WAVE 2024
Fremantle, Australia 16 – 17 March admin@optometrywa.org.au
APRIL 2024
AUSTRALIAN VISION CONVENTION (AVC)
Gold Coast, Australia 6 – 7 April optometryqldnt.org.au
SILMO SINGAPORE
Singapore 24 – 26 April silmosingapore.com/
MAY 2024
SQUINT CLUB MEETING 2024
Melbourne, Australia 3 – 4 May ranzco.edu/events
Washington, US 5 – 9 May arvo.org
OSHOW24
Sydney, Australia 17 – 18 May o-show.com.au
SUPER SUNDAY 2024
Sydney, Australia 19 May (immediately after OSHOW24) vision@oaansw.com.au
JUNE 2024
AUSTRALIAN SOCIETY OF OPHTHALMOLOGISTS EXPO 2024
Sydney, Australia 1 – 2 June asoeye.org
THE ART OF OCULAR IMAGING (AOI) CONFERENCE 2024
Sydney, Australia 8 – 9 June artofocularimaging.com.au
GENEYE 2024
Melbourne, Australia 19 – 21 June geneye.org.au
JULY 2024
AUSCRS 2024
Hamilton Island, Australia 27 – 27 July auscrs.org.au
AUGUST 2024
OPHTHALMOLOGY UPDATES! Sydney, Australia 24 – 24 August ophthalmologyupdates.com


Every year at the University of Melbourne – where I completed the Doctor of Optometry course – there’s an optometry student conference. During my second year, there was a Specsavers booth. They were inquiring if any students wanted the opportunity to work as optical assistants. Wanting to get my foot in the door in the industry, I was soon interviewed at Specsavers Craigieburn. Both Keon and Rahul (the directors) showed me around. It felt like a great fit and soon after they wanted to hire me. During my final year, I interviewed for an optometrist role and there was coincidentally an opening there.
Word of mouth from my peers that already worked in optical businesses generally said that Specsavers was well structured and had a lot of support. The range of equipment and the accessibility of eyecare (fully bulk-billed tests) also resonated with my ideals.
As part of the Specsavers Graduate Program I successfully ran an in-store project. It provided insights into what it takes to initiate change in a store while gaining leadership and management experience. I cemented this by completing the Pathway Program in 2023 that set me up with further skills and leadership qualities to eventually become a director and own my own Specsavers. I was also invited to come back as a Pathway Mentor for a later intake of candidates.
If I had to give a top three, I would start with successfully starting and completing the Pathway
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Carly Parkinson on 0478 201 057 or carly.parkinson@specsavers.com
Australia employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Matthew Cooney matthew.cooney@specsavers.com or 0447 276 483
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
Program in 2023. Secondly, it would be my contributions towards the Early Career Optometrist (ECO) program – as the Victorian representative on the program’s advisory committee – and successfully helping and shaping it through its pilot year. Helping create a recurring two year program that will be used by future Specsavers early career optometrists – and knowing it will help future generations coming out of their Graduate Program – fills me with joy and fulfillment. The final career highlight is being an ‘on demand’ speaker for the Specsavers Clinical Conference for 2023. It’s surreal that I could go from attending one year to presenting the next. Despite feeling like a fish out of water, my video was the most watched on demand video of the conference. It shows that anything is possible.
A female patient in her 40s who presented for a general routine exam. History was normal and refraction was unremarkable. However, looking at her OCT scans, there was a very fine symmetrical hairline tear through her macula on both eyes. It looked a lot like solar retinopathy and I chanced by asking her if she had ever stared at the sun or a solar eclipse before. Shocked, she admitted when she was six years old and overseas with her family that she witnessed a solar eclipse. She had been given X-ray film to look through to protect her eyes, but being a curious child she peeked out to look directly at the eclipse. No one had ever asked her about it until that day. I thought it was cool that with the technology we have available, we could determine something like that.
$50k sign-on bonus – Designate Partnership in Emerald, QLD
Specsavers Emerald has an exciting opportunity for an experienced optometrist to join the store on a 2-year Designate Partner program - No upfront cost and opportunity to try partnership before committing long term. Specsavers Emerald is 3 test room store with a varied patient demographic and an extremely welcoming, supportive and social team. You will be supported with a relocation package tailored to your needs, be partnered with an experienced Specsavers Retail Partner and have access to our Pathway and Partnership development program for duration of time in role.
Optometrist opportunity – Specsavers Dunedin, NZ
Seeking a two optometrists to join our extraordinary team at Specsavers Dunedin, they are in fact our store of the year. We o er cutting-edge technology, a friendly environment, and a commitment to professional growth. Embrace the breathtaking beauty of the region and enjoy a perfect work-life balance. Don’t miss this incredible opportunity to be go with a friend and be part of Specsavers. Apply now and unlock a rewarding journey.
Optometrist opportunities o ering up to $170k packages in QLD!
Looking for great weather all year round? Specsavers are expanding our Optometry team in QLD’s far north. Home to rainforests, beaches, markets and a vast array of great cafes, bars and restaurants along with access to the Great Barrier Reef there is something to suit everyone. You’ll work with market-leading equipment – including OCT free for all patients, be supported by experienced retail teams and have access to excellent opportunities for career development. Part or full-time considered. Great salary including relocation support, birthday/volunteer leave, Specsavers Perks sta discount program, free glasses and family and friends discount voucher each year.
Newcastle Locum Opportunities
Specsavers are seeking experienced optometrists to locum in Newcastle, allowing you to choose your own days and locations. This is an opportunity to combine work and travel. We have a variety of locum openings across 9 of our stores in Newcastle starting now and going throughout 2024. Whether you’re locally-based and looking to fill up your diary with that regular one day a week or to escape the cold and work in the sun for a few weeks, Specsavers has you covered with all travel and accommodation provided and booked for you.
Graduate Opportunities
Are you moving into your final year of optometry study and starting to consider what company would be right for you as a graduate optometrist? Specsavers provides the support and mentorship to set you up for success, o ering great graduate packages and extraordinary patient-focused environments. By joining Specsavers, you can be certain you will have everything at your disposal to cater to your diverse patient base.






















Unleash your full potential with OPSM. With our unwavering support and experience, you have the freedom to pursue an area of expertise and practice full-scope optometry. Choose the field you love and thrive with OPSM.
Accelerate your career aspirations with OPSM. Visit opsm.com.au/careers today.
