



Sub-optimal







Sub-optimal


Fixing a fragmented care system along with new considerations around optometric Medicare items for screening and greater access to public, bulk-billed ophthalmology services would help overcome some of the biggest issues facing diabetic eyecare in Australia, the ophthalmic sector has told a government inquiry.
Optometry Australia (OA), RANZCO, ophthalmologist Dr James Muecke and other industry figures have weighed in on a major government examination of the state of diabetes in Australia, drawing attention to other issues such as “pervasive and persuasive” food marketing to children and barriers to accessing retinal imaging and intravitreal injections in diabetic retinopathy (DR).
The 270-page final report entitled: 'The State of Diabetes Mellitus in
Australia in 2024', was released in June 2024 and published 23 recommendations. It provides a sobering overview of diabetes in Australia amid a concerning trend that may see 21st century life expectancy decline due to “diseases of affluence”. DR, and other diabetic eye conditions, featured heavily in the final report. These ophthalmic conditions are thought to have an indirect annual cost of $2 billion, and growing.
RANZCO said there were mechanisms in place to manage diabetic eye disease, such as the KeepSight diabetes eye check reminder system, Medicare item numbers covering the costs of regular checks, Pharmaceutical Benefits Scheme subsidies and Medicare items for effective treatments, a highly skilled eye health workforce and capabilities
The report published 23 recommendations. Image: Department of Health.
for health data sharing via the My Heath Record.
But more is needed, including resolving “the current fragmentation of care”. Despite the availability of Medicare-funded eye checks, several studies have shown as few as half of
RANZCO’s influence on the quality of the health system is being “sidelined and bypassed” by Federal Government moves to bring more eye specialists into Australia, with fresh concerns over who will hold the power to accredit training posts in future.
In a recent letter to members, Australian Society of Ophthalmologists (ASO) president Dr Peter Sumich has repeated concerns over the recommendations of the ‘Kruk review’ and the work to “disempower our colleges”.
And he has called on ophthalmologists to use their collective influence in opposition to the proposed changes of health
practitioner regulatory settings.
The 2023 review – conducted by Ms Robyn Kruk – considered ways to make Australia a more popular destination for internationally qualified health professionals and address workforce pressures. It came up with 28 recommendations aimed at removing regulatory road blocks.
ASO has been particularly worried about RANZCO and other medical colleges potentially losing their “quality assurance” role when vetting and approving overseas-trained specialists to practise in Australia.
Kruk’s review found these medical college assessments were costly, with varying fees and processing time frames. It was noted some
colleges only reviewed applications for specialist international medical graduates (SIMG) recognition at specific times throughout the year. During the consultation process, RANZCO said it would not endorse a transition of equivalence assessments for SIMGs from the medical colleges to the Australian Medical Council (AMC).
The college said this would represent a move away from qualified assessors who are the recognised clinical experts in their field, and instead called for colleges to streamline their own assessments. Since then, Kruk’s final report has
Australians diagnosed with diabetes undergo checks as frequently as recommended.
“Other countries have successfully implemented national programs for DR screening – notably the UK and Singapore. Within seven years … in England diabetic retinopathy was no longer the leading cause of blindness in working age adults, a first in the 50 years that record had been kept,” RANZCO stated.
“At present, the diversity of Medicare item numbers that may be applicable to diabetes eye checks mean that it is impossible to disaggregate these eye checks from other optometric services. Accordingly, Australia lacks accurate nationally representative data for diabetic eye screening. This is major






16
Turning tide
Dr James Muecke on the big realisations he’s had with diabetes and how he’s spreading the message.

27 New era Vision Eye Institute exemplifies the changing face of corporate ophthalmology in Australia.


39 Setting standards
Dr Monica Jong dissects the term ‘pre-myopia’ and what do when it's suspected (0.5 CPD).

When I do my groceries today, I have a rule of thumb: try and stick to the outer perimeter of the supermarket floor. If I venture down one of the middle aisles, it’s likely I’ll pick up an ultra-processed item that’s bad for my health.
Deciphering what constitutes ‘healthy food’ has become an increasingly fraught task for Australians today, and we can’t blame them. Raw food materials are being broken down and spun up to offer the perfect blend of crunch, saltiness and/or sweetness to keep you reaching in the bag for more. It’s addictive, and even though you can’t pronounce some of the ingredients in fine print, it somehow comes with health claims: fibre, protein, multigrain etc.
I’m amazed to see some potato chips with a three-star health rating. And even a can of tuna can catch you out; marketed as if it comes with olive oil when this only makes up 7% of the oil content and is padded out with other ingredients.
Given this is allowed to happen, it’s little surprise Australia is in a dire situation with type 2 diabetes, and all its complications including the worst of all: potentially sight-stealing diabetic retinopathy. The situation is so serious that the government has held a major review to come up with some clear direction. Thankfully, we have people like ophthalmologist Dr James Muecke who was a prominent voice in the inquiry, alongside Optometry Australia and RANZCO. This edition on page 16, he lays out the moment he realised diet alone could reverse diabetes, and how he has used his eye injection clinics – and 2020 Australian of the Year platform – to relay important messages to diabetics and doctors.
It’s encouraging to see the inquiry release key recommendations, including food labelling reforms so consumers can identify products with added sugar, as well as a levy on sugar-sweetened beverages. The government has also been asked to consider regulating the marketing and advertising of unhealthy food to children.
Importantly, the committee called for an expedited review of the Australian Dietary Guidelines, ensuring they are revised to include adequate information for Australians with diabetes. It offers immense hope, and while these measures may change consumer behaviours, it’s imperative the allied health and medical professions reinforce this lifestyle messaging to Australians with diabetes. It’s something Dr Muecke is passionate about and I wish him luck.
MYLES HUME Editor












Just as Insight went to print, GLAUKOS received Therapeutic Goods Administration approval in for its iStent infinite Trabecular Micro-Bypass System, offering an improved option for Australian glaucoma surgeons and patients. The key difference between iStent infinite and previous generation iStent systems is the inclusion of three heparin-coated titanium stents – as opposed to two – preloaded into a newly designed auto-injection system offering unlimited delivery attempts. According to the company, this allows the surgeon to inject stents across a span of up to approximately
The University of Virginia School of Engineering and Applied Science has developed artificial compound eyes, inspired by a praying mantis’ binocular vision. These overcome limitations in machine vision, such as accuracy issues, data processing lag times, and high computational power requirements, enhancing real-world visual data collection and processing.
The “VisioPrinTech” process, developed by a German research group, 3D prints personalised corneas using patients’ stem cells and collagen fibres to reduce reliance on donations. The laser-based technique positions these cells, to create transparent, functional corneas with minimal rejection risk and may soon be a viable alternative to conventional transplants. The next step is scaling up with industry partners with initial production and testing in small batches.
A study has found that people appear more attractive when their pupils are constricted, making their coloured irises seem bigger and brighter. The researchers showed nearly 3,000 participants headshots with blue or brown eyes. One version had constricted pupils, and another had dilated pupils. Participants rated the faces’ attractiveness, and faces with smaller pupils – which show larger irises – were judged more attractive.
six clock hours around Schlemm’s canal, the eye’s primary drainage channel. IN OTHER NEWS, EssilorLuxottica posted a net profit of €1.746 billion (AU$2.89 b) for the first half of the year, driven by a 5.3% revenue rise to €13.3 billion (AU$21.9b), with the Asia-Pacific region seeing a 9% increase in half-year revenue to €1.589 billion (AU$2.63b). Meanwhile, Q2 figures showed a 5.2% rise in revenue to €6.955 billion (AU$11.50b) for the group. Both OPSM and Sunglass Hut improved performance in Australia in the quarter. It also recently announced an 80% stake in OCT manufacturer Heidelberg Engineering. FINALLY, Macquarie University researchers have identified a gene therapy that could help
treat glaucoma, with potential applications for other neurodegenerative conditions. The group discovered the protein Tau, implicated in Alzheimer’s disease, has also been found in retinal cells and likely plays a role in glaucoma. The researchers employed gene therapy for Tau where they both overand under-expressed the protein. Both manipulations were found to adversely affect retinal structural and functional measures, therefore suggesting there is an ideal Tau level to promote optimal retinal health. The ‘switch’ the team developed is a gene therapy carried by a viral vector, which has the unique ability to cross both the hard-to-penetrate blood-brain and blood-retinal barriers.

AUSCRS welcomed its highest ever ophthalmology and advanced trainee attendance, 188 and 26 respectively, at its recent 2024 meeting on Hamilton Island. Page 57
14 – 15 September
Specsavers has secured a high-powered speaker line up including Dr Brendan Cronin, Dr Rushmia Karim and A/Prof Chameen Samarawickrama for its Gold Coast event. specsaversclinicalconference.com.au
Complete calendar page 64
MONTH
18 – 19 October
Eyecare Plus’ conference in Sydney will celebrate independent optometry with a series of workshops, keynote speakers, cocktail party and gala dinner. eyecareplus.com.au/conference/
Published by:
379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766
www.primecreative.com.au
Chief Operating Officer
Christine Clancy
christine.clancy@primecreative.com.au
Publisher
Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Journalist
April Hawksworth april.hawksworth@primecreative.com.au
Assitant editor
Rob Mitchell
rob.mitchell@primecreative.com.au
Commissioning Editor, Healthcare Education
Jeff Megahan
Business Development Manager
Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager
Salma Kennedy salma.kennedy@primecreative.com.au
Design Production Manager
Michelle Weston
michelle.weston@primecreative.com.au
Head of Design
Blake Storey
Art Director Bea Barthelson
Subscriptions T: 03 9690 8766
subscriptions@primecreative.com.au
continued from page 3
barrier to measuring eye check coverage across the country, which is key to ensuring that eyecare service provision matches disease burden.”
The college called for “systematised and regular eye screening”, along with improved access to specialist eyecare, supported by accurate real-time data on diabetic eye disease prevalence and severity.
“Key priorities here are the expansion of public hospital ophthalmic treatment services as well as community bulk-billing ophthalmology services,” RANZCO said.
“There is an opportunity to revise Medicare item numbers for DR screening by optometrists. For instance, amending the descriptor for item 10915 to include minimum agreed requirements for an appropriate financial incentive could transform DR screening in most areas well served by optometrists.”
RANZCO also urged greater collaboration between ophthalmologists, optometrists, GPs, endocrinologists and other healthcare professionals “as eye changes can indicate other chronic complications of this condition”.
In its submission, OA echoed this sentiment, emphasising the need for optometrists to be integrated into multidisciplinary care team arrangements for people with diabetes.
“Optometrists are well-positioned to play a role in diabetes prevention. As primary
healthcare providers, optometrists can inform patients about the impact of diabetes on eye health during routine examinations,” CEO Ms Skye Cappuccio said.
“In our submission, we have recommended the government introduce a national strategy to ensure people with diabetes receive eye examinations to enable early detection and treatment of diabetic retinopathy. We are delighted to see that our recommendation has been included in the report.”
OA also explained that patients often have to pay “substantial out-of-pocket” costs for intravitreal injections, which are administered in the private system with low rates of bulk billing. As a result, the necessary numbers of injections required for effective treatment are not always administered, the organisation stated.
Meanwhile, esteemed ophthalmic industry figure Professor Hugh Taylor told the inquiry everybody with diabetes will develop diabetic eye disease if they live long enough – with 98% of that vision loss preventable if it’s detected and treated.
Importantly, it was noted that DR could be successfully managed with improved glycaemic control, eye injections and laser therapy.
Mr Stephen Bali, MP for Blacktown, noted that a key challenge for DR patients in western Sydney was finding accessible treatment locations.

“OPTOMETRISTS ARE WELLPOSITIONED TO PLAY A ROLE IN DIABETES PREVENTION ... OPTOMETRISTS CAN INFORM PATIENTS ABOUT THE IMPACT OF DIABETES ON EYE HEALTH DURING ROUTINE EXAMINATIONS.”
SKYE CAPPUCCIO, OPTOMETRY AUSTRALIA
Dr Ashim Sinha, director of diabetes and endocrinology at Cairns Hospital and Health Service District, added: “There’s lack of screening availability. Not every place has fundus cameras, which are so easy to use and can be put into each of these communities. Health workers can be easily trained to man – it is not rocket science.”
Among the recommendations stemming from the inquiry, many were focused on changes to the food industry.
Dr Muecke has used his platform in recent years to draw attention to major issues within the food industry.
“Our poor diet is responsible for more disease and death than alcohol, tobacco and inactivity combined," he said.
The committee heard that Australians do not eat enough fruit or vegetables, with the Public Health Association of Australia noting “less than 10% of adults and children eat the recommended amount” of these foods.
The committee also heard food marketing to children is “pervasive and persuasive”, and “ubiquitous in their daily lives – in their homes, schools, communities and gathering places”.
Dr Muecke also expressed concern at what he described as the food industry’s “relentless promotion of unhealthy food and drinks at checkouts and at the end of aisles within their supermarkets”.
NOTE: turn to page 16 for Dr James Muecke’s report on diabetes.
continued from page 3
emerged with some wording changes, but it is still supporting centralised “comparability assessment with the AMC, in full or in part . . . should outcomes fall short of workforce needs within ministerially agreed timeframes”.
In his letter, Dr Sumich said the Kruk recommendation for “mass importation of specialists” had been enacted, meaning “they can now come into Australia without passing through the college quality process”.
“It starts in October with expedited pathways for general practitioners and will be followed by December with anaesthesia, obstetrics and gynaecology, and psychiatry as priority specialties. Ophthalmology is rolled out some time next year,” he said.
Dr Sumich said the college had been sidelined and bypassed, which would impact on quality of service but also training.
In another major shift, he said government groups – rather than colleges – are set to now determine what training posts are accredited. This has occurred because of dis-accreditation in emergency medicine, intensive care, and radiology posts in recent times. As a result, it led to states losing registrars, which had drawn the ire of some state ministers, he said.
“Rather than improving the quality of the department, they feel it is easier to determine their own standards of training,”
Dr Sumich added.
He said the ASO would be happy to support a system bringing more ophthalmologists into Australia, if there was

appropriate workforce distribution and they were sent to places they are needed – “in rural, public hospital, and in paediatric care”.
“It would be a gross system failure if these new ophthalmologists turned up in Bondi, Chatswood, and Melbourne CBD.”
He urged younger ophthalmologists, in particular, to take an interest in “medico politics”.
“We can’t solve any of these problems ourselves, but within the framework of the medical societies, colleges and Australian Medical Association, we can make critical contributions,” Dr Sumich said.
“What we need is your membership and your influence on non-members to please join us and be heard.”
RANZCO did not wish to comment at the time of print.
EssilorLuxottica is acquiring an 80% stake in ophthalmic device manufacturer and distributor Heidelberg Engineering and is also taking over American streetwear brand Supreme for AU$2.2 billion.
Founded by Dr Gerhard Zinser and Mr Christoph Schoess in 1990, Heidelberg Engineering specialises in OCT devices, real-time image processing and analytics, large-scale data analysis and digital surgical navigation and has been supporting Australian ophthalmologists and optometrists for several years through its local subsidiary in Melbourne.
Mr Francesco Milleri, chairman and CEO, and Mr Paul du Saillant, deputy CEO at EssilorLuxottica, said Heidelberg Engineering would bolster the company’s presence in the med-tech space and foster long-term growth.
Heidelberg Engineering co-founder and managing director Schoess added that innovation and quality have been key drivers for the company since he and Dr Zinser founded it 35 years ago.
“We are delighted that EssilorLuxottica, a global leader in eyecare, embraces our vision for creating a shared care system spanning from research to home monitoring. Together, we are strongly positioned to significantly advance patient care and improve clinical outcomes.”
The deal is expected to close in the second half of 2024 pending regulatory approvals and other customary closing conditions.
Meanwhile, EssilorLuxottica has also entered into an agreement with global apparel and footwear company VF Corporation to acquire streetwear brand Supreme for US$1.5 billion (AU$2.2 billion).
Milleri and du Saillant said: “We see an incredible opportunity in bringing an iconic brand like Supreme into our company. It perfectly aligns with our innovation and development journey, offering us a direct connection to new audiences, languages and creativity.
“With its unique brand identity, fully-direct commercial approach and customer

experience – a model we will work to preserve – Supreme will have its own space within our house brand portfolio and complement our licensed portfolio as well. They will be well-positioned to leverage our group’s expertise, capabilities, and operating platform.”
VF’s president and CEO Mr Bracken Darrell said that due to the brand’s distinct business model and VF’s integrated model, the company’s strategic portfolio review concluded there are limited synergies between the two, making a sale a natural next step.
Supreme founder Mr James Jebbia added that EssilorLuxottica is a unique partner that understands the need to stay true to the brand and continue to operate and grow as it has for the past 30 years.
“This move lets us focus on the brand, our products, and our customers, while setting us up for long-term success,” he said.
The transaction is expected to close by the end of 2024, subject to customary closing conditions and regulatory approvals.







Professor Sharon Bentley, a prominent Australian optometry academic, has been appointed dean of the University of California, Berkeley’s optometry school. Currently the deputy dean at Queensland University of Technology, she brings over 25 years of experience in optometry, public health, and education. Starting in February 2025, Prof Bentley will oversee academic programs, research initiatives, and community outreach at UC Berkeley. She is recognised for her “strategic planning, commitment to diversity, and integration of Indigenous health into education”. Prof Bentley’s management experience includes enhancing eyecare services in rural Aboriginal communities and serving on Vision Australia’s board. Meanwhile, she has acquired degrees from the University of Melbourne and Johns Hopkins University.
Tokyo Medical and Dental University (TMDU) will introduce the Eyerising Myopia Management Device for its myopia patients as part of their treatment options. The Eyerising Myopia Management Device uses patented repeated low-level red-light (RLRL) technology, which its Australian-based manufacturer says offers an efficacious, safe, non-invasive, and user-friendly solution for managing myopia in patients. Eyerising said use of its treatment at TMDU marked a significant milestone in the advancement of myopia management and treatment solutions. “Both TMDU and Eyerising International are committed to ongoing research and development to further enhance the device’s capabilities and efficacy,” Eyerising stated. The Australian Therapeutic Goods Administration registered Eyerising’s RLRL therapy in July 2023 (ARTG 412752), with the device now available in more than 30 other countries.
For the second consecutive year, Professor Jamie Craig, head of ophthalmology at Flinders University, has been nominated for SA Scientist of the Year. A leading glaucoma researcher, Prof Craig developed a groundbreaking saliva test to identify individuals at high genetic risk for the disease and is trialling laser treatments to prevent vision loss. His genetic risk score is now in clinical use across Australia, allowing high-risk individuals to receive timely sight-saving treatment. Partnering with industry, he helped develop genetic tests for guiding glaucoma management, now available in eight countries. With more than 4,000 tests performed in South Australia alone, his research, supported by a $2.9 million MRFF grant, aims to enhance early-stage glaucoma patient care.
George & Matilda Eyecare (G&M) has expanded its presence on the Mid North Coast of NSW with the addition of Ms Michelle Ferguson and her practice in South West Rocks.
The announcement comes after G&M recently passed the 100-practice milestone with the acquisition of 26-practice optometry network, National Optical Care.
The network has now grown to more than 120 practices, servicing over 140 communities through its various outreach programs.

“I pride myself on giving quality care to our community,” Ferguson said. “Being the only eye health provider in town, I cherish the relationships built with patients over the years. Joining George & Matilda Eyecare allows me to extend my professional life while ensuring continuity of care for my community.”
Ferguson embarked on her optometric career in 1995 and has dedicated 25 years to her practice that has a reputation for a high level professional yet personal service.
For others considering a similar transition, she advised thorough succession planning and exploring all options, including G&M.
“Consider your work/life balance and the changes you desire,” she said. “Gather
information and seek advice from peers to make the best decision for the future of your practice.”
Throughout the transition process, she said G&M had been "very friendly, confident, and capable".
“It has been a smooth process, thanks to their guidance," she said.
Ferguson and her team will continue serving the community under the G&M banner, upholding its tradition of excellence and personalised care, along with confidence around the practice’s future after my retirement,” she added.
G&M said it had a "promising pipeline" and anticipates more announcements in the near future.

Almost 9% of people on semaglutide had NAION compared 1.8% on the other drugs. Image: myskin/stock. adobe.com.
A new study has found patients prescribed semaglutide for diabetes or weight loss had a higher risk of developing a blinding eye condition.
It was reported that patients prescribed semaglutide – more commonly known under brand names Ozempic and Wegovy – were four times more likely to be diagnosed with non-arteric anterior ischemic optic neuropathy (NAION) than similar patients who had not been prescribed these drugs.
Since its launch as Ozempic for diabetes in 2017, semaglutide – originally developed to treat type 2 diabetes by promoting weight loss – has significantly increased in popularity. It was also approved for weight management, branded as Wegovy, and released in 2021.
The study, published in JAMA Ophthalmology, analysed data from 16,827 patients at the Mass Eye and Ear Harvard teaching hospital in the US who received treatment from 2017 to 2023.
Researchers found 8.9% of these patients on semaglutide had NAION compared with 1.8% on other drugs, over a three-year period. Meanwhile, those who were overweight or had obesity and prescribed the drug were more than seven times more likely be diagnosed. Over three years, 6.7% of cohort on semaglutide had NAION compared with 0.8% who were taking other weight-loss drugs.
NAION is said to be relatively rare, occurring in approximately 10 out of 100,000 individuals per year and is the second-leading cause of optic nerve blindness.
The study does not prove causality, and why there was a difference reported in diabetic and overweight groups.
“This study’s findings suggest an association between semaglutide and NAION. As this was an observational study, future study is required to assess causality,” the study authors concluded.

Ahpra and the National Boards now have greater power when there are significant public safety concerns over health professionals that aren’t regulated by the body, with the introduction of a new mechanism called interim prohibition orders (IPOs).
The measure by the Australian Health Practitioner Regulation Agency (Ahpra) and National Boards is part of the latest suite of changes from the regulator that is ushering in its most significant reforms since the National Law came into effect in 2010.

Now, unregistered practitioners –including suspended practitioners – can be prevented from treating patients. This could have implications for non-Ahpra eyecare professionals such as orthoptists – which are self-regulated by the Australian Orthoptic Board – and optical dispensers. Also, the public will have more information about practitioners on the public register, including if they use an alternative name to practise.
The new changes complete a series of reforms to the Health Practitioner Regulation National Law agreed by all health ministers aimed at strengthening public protection and improving the
operation of the National Registration and Accreditation Scheme. The other changes in the same package of amendments to the National Law started in October 2022 and May 2023.
Ahpra CEO Mr Martin Fletcher said powers to issue IPOs about unregistered practitioners were an important safeguard for the wider health system. Some state and territory health complaints bodies already have this power.
“These powers will only be used in exceptional circumstances, when it is deemed there is a very real risk to the health and safety of individual patients or
the wider community,” he said.
Other key changes beginning on 1 July 2024 include establishing a process for renewing a practitioner’s registration after suspension and extending National Boards’ powers to exclude practitioner information from the public register if it poses a serious risk to their health, safety, or that of their family and associates. Additionally, the public will now be able to verify a practitioner’s registration more easily, with both legal and alternative names appearing on the register.
According to Ahpra, some practitioners prefer to practise under an alternative name, such as adopting a traditional name or an anglicised or shortened name. Having both names appear on public register will make it easier for the public to make informed decisions about their care.
Fletcher said completing the reforms would improve health regulation and public safety nationwide.
“Australia’s health system, as well as the reasons and ways people access it, has changed dramatically over the past 15 years,” he said.
“These reforms allow the regulation scheme to evolve, strengthening Ahpra and National Boards’ ability to protect the public and support practitioners.”
Researchers at the National Institutes of Health (NIH) have found that taking a daily supplement containing antioxidant vitamins and minerals slows progression of late-stage age-related macular degeneration (AMD).
In the study, published in Ophthalmology, they reviewed the original retinal scans of participants in the Age-Related Eye Diseases Studies (AREDS and AREDS2) and found that, for people with late-stage AMD, taking the antioxidant supplement slowed expansion of geographic atrophy (GA) regions towards the central foveal region of the retina.
“We’ve known for a long time that AREDS2 supplements help slow the progression from intermediate to late AMD. Our analysis shows that taking AREDS2 supplements can also slow disease progression in people with late dry AMD,” said Dr Tiarnan Keenan, lead author of the study.
“These findings support the continued use of AREDS2 supplements by people with late dry AMD.”
The review involved an analysis of the original retinal scans of participants in the AREDS (total 318 participants, 392 eyes) and AREDS2 (total 891 participants, 1210 eyes) trials who developed AMD, calculating the position and expansion rate of their regions of GA.
For those people who developed GA in their central vision, the supplements had little benefit. But for the majority who developed GA far from the fovea, the supplements slowed the rate of expansion towards the fovea by approximately 55% over an average of three years.
The original AREDS trial found that a supplement formula containing antioxidants (vitamin C, E, and beta-carotene), along with zinc and copper, could slow progression of

The supplements benefitted those with GA far from the fovea. Image: New Africa/ Shutterstock.com.
intermediate to late-stage AMD.
The subsequent AREDS2 trial found that substituting the antioxidants lutein and zeaxanthin for beta-carotene improved the efficacy of the supplement formula and eliminated certain risks.
At the time, neither trial detected any further benefit once participants had developed late-stage disease. However, that original analysis did not account for a phenomenon in the dry form of late AMD called “foveal sparing".
“Our high acuity central vision is essential for tasks like reading and driving. Given that there are few therapeutic options for people with late-stage dry AMD to retain or restore their vision, antioxidant supplementation is a simple step that may slow central vision loss, even for those with late disease,” Dr Keenan said.
“We plan to confirm these findings in a dedicated clinical trial in the near future.”





Compatible with contact lenses


Ahpra is advising optometrists –newly minted and experienced – to take care with both their identities and their reputations

The Australian Health Practitioner Regulation Agency (Ahpra) is warning new optometry graduates to not post their registration certificates online.
Websites are selling fake Ahpra registrations. Image: Tero Vesalainen/ Shutterstock.com.
It says identity theft is rife and it is seeing websites pop up every day selling fake Ahpra certificates of registration based on real ones that graduating practitioners have posted on their social media.
“You’ve worked hard to earn your registration; don’t let somebody steal it,” the agency said.
That might not be a concern for more experienced practitioners, but in a separate initiative, the regulator is urging them to take care with feedback and complaints.
When these are managed well they can result in improvements that increase patient, client, and community confidence in the practitioner, Ahpra stated. It can also prevent a concern escalating to an external complaint body or regulator.
Poor or inadequate responses can also undermine personal and industry reputations.
"We know that receiving negative feedback or a complaint can be confronting and stressful and as well as this resource we have published a list of general support services," Ahpra stated.
To help improve the process, Ahpra, the Australian Commission on Safety and Quality in Health Care, and the 15 National Boards have developed a checklist to help resolve feedback or complaints made to practitioners, with work also under way on resources to help consumers navigate the various complaints options available.
It may also be relevant to those who have a role in establishing and maintaining complaints systems and processes at a health service.
The checklist is available on Ahpra’s Resources page.
Specsavers has launched a new range of limited-edition frames in collaboration with Gurindji Waanyi contemporary Aboriginal artists to support The Fred Hollows Foundation.
The company said $25 from the sale of each frame within the range – now available in-store and online – would be donated towards the foundation's Indigenous Australia Program to help make eyecare more accessible for Aboriginal and Torres Strait Islander Peoples.

Now in the 13th year of its partnership with Fred Hollows, Specsavers has contributed more than $7.6 million to the foundation’s programs in Australia. The latest release marks its eighth limited-edition range.
Specsavers is aiming to raise $500,000 through the sale of these limited-edition glasses.
Ms Sarrita and Ms Tarisse King are the artists for this year's eyewear range. They are second generation artists and the daughters of Indigenous artist Mr William King Jungala.
“A collaboration between the sisters, this year’s limited- edition artwork, ‘My Country’s Story’, beautifully captures the diverse landscapes of Australia’s Top End, reflecting on the lives of families and communities who inhabit the land,” Specsavers said in a statement.
Tarisse added: “Sarrita and I got together to
Specsavers said $25 from the sale of each frame within the range would be donated to Fred Hollows. Image: Specsavers.
tell a story on a canvas and ended up creating a painting that was reflective of us and our journey.
“We have been painting this story in collaboration for years, half the canvas each, to create the work that you see on the limited-edition frames.
“To see our art, that tells our story, used to give back to our mob through the work of The Fred Hollows Foundation is so important to us. As an Aboriginal woman who practises storytelling, I want to use my skills to uplift my people, especially as we are predisposed to so many more issues than others and poor eye health is so common, especially in Indigenous communities.”

The trip to
could help bring world-class eye health services to South East Asia. Image: Quang/stock. adobe.com
The Australian Society of Ophthalmologists (ASO) is hosting its inaugural International Eye Care Mission in Hanoi, where participants will venture on to the frontlines of local health service delivery.
ASO CEO Mr Kerry Gallagher said the trip to Vietnam, at the Sofitel Legend Metropole Hanoi from 15 – 21 September, represented more than an opportunity to share clinical updates.
“It is a unique platform designed to foster collegiality, drive knowledge growth and, most importantly, cultivate a deeper understanding of medical services in [developing] countries,” he said.
“This mission will provide the opportunity to explore the realities of global disparities in eye health and the pivotal role that
ophthalmologists – and other eye health professionals – can play in addressing these disparities.”
The mission is backed by Sight For All, whose CEO Ms Judy Hatswell is keen to see increased collaboration among the ASEAN community.
“Our purpose at Sight For All is to empower communities with the skills and equipment to eliminate avoidable blindness through the ‘Teach a Man to Fish’ approach that provides a sustainable pathway to the elimination of treatable blindness,” she said.
“Sight For All visionaries have visited Vietnam in the past and we are proud to have provided support to furthering the education and training of locally based ophthalmologists.”





optomap ® is the only true, clinically validated, ultra-widefield retinal image that can capture 82% or 200° of the retina, in a single capture

Ophthalmologist and 2020 Australian of the Year DR JAMES MUECKE has been a prominent voice in a recent government inquiry into the state of diabetes in Australia. After completely changing his view on type 2 diabetes in 2019, he’s now on the crusade to convince his medical peers the solution is simpler than once thought.
I’ve been treating the blinding complications of type 2 diabetes for nearly 35 years. For most of that time the management involved painful laser burns to the peripheral retina to hopefully reverse the ingrowth of abnormal new blood vessels that could bleed in an instant and permanently blind the afflicted eye. Or it involved laser burns close to the fovea to attempt to stimulate absorption of the fluid collecting from leaky blood vessels, risking permanent damage to the vision.

Over the past decade and a half, much of this laser has been replaced with injections into the back of the eye of an antibody that can either halt the growth of the new blood vessels in the periphery or seal up the leaky blood vessels at the macula. It’s a miraculous innovation that has revolutionised the treatment of diabetes-related eye disease.
I was always the guy at the end of the line treating the end-stage complication, the most feared complication – loss of vision – of what I now realise is an avoidable man-made dietary disease. Never once did I consider my role to include discussion of lifestyle interventions that could not only prevent type 2 diabetes, but could also potentially put the condition into remission. That is, until I read a ground-breaking book in late 2019.
The Diabetes Code, by Canadian renal physician Dr Jason Fung, taught me that type 2 diabetes can be reversed naturally. It was a revelation to me. I always thought type 2 diabetes was a progressive disease, ultimately requiring oral medication, injectable insulin, a raft of unpleasant and unavoidable complications and an untimely death. Afterall, that is what I’d been taught in medical school. The message was reinforced by a variety of public health associations working in the diabetes space.
In 2020, I was selected to be on the Expert Advisory Group for Australia’s National Diabetes Strategy. I managed to get the opportunity for remission included in that document for the very first time. The strategy was published in late 2021. This was a turning point for the management of type 2 diabetes in Australia. At last, patients had hope. Hope their condition could be turned around. Hope they didn’t have to face a multitude of crippling complications and crippling expenses.
I started to talk about remission with my patients, initially the ones with vision-threatening eye disease, who I was actively treating with regular eye injections. Perhaps 100 patients. A drop in the ocean compared to the estimated 200,000 in Australia with vision-threatening retinopathy due to their diabetes. All but one of that 100, a mere 1%, were aware of this life-changing opportunity.
I wrote to the GPs for each of these patients, asking, sometimes pleading, for the concept of remission to be explored with our mutual patient. Most of my letters were seemingly ignored. Some doctors
disowned their patients. Some took it on board. More often than not, it was the patient who had to insist that their GP give it a go. I recommended a local nutritionist who specialises in dietary change to attempt remission. I encouraged active participation of the GP because of the potential need for de-prescribing diabetes medications. Eventually, all these patients returned to me for their injections. And I monitored their progress.
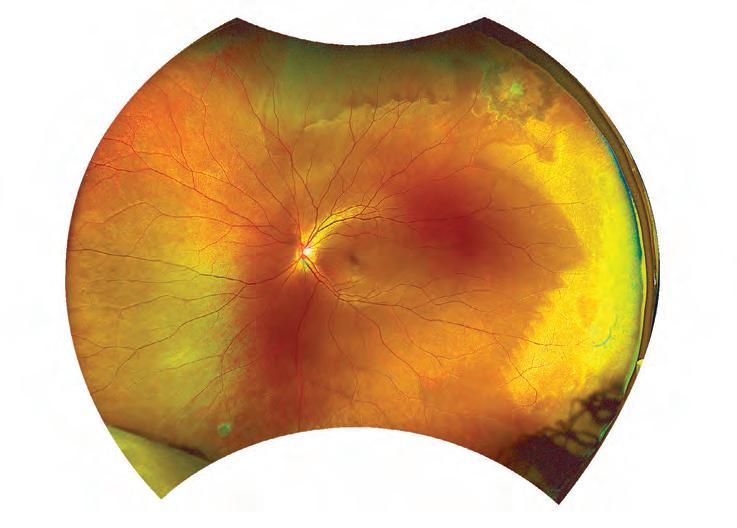
I still remember the very first patient who put his diabetes into remission. He was a man in his late 60s who had type 2 diabetes for over a decade and had been receiving eight-weekly injections into both eyes for many years. At the first visit back to me after commencing his dietary change, he had come off his insulin in less than two months. By the next appointment, he had discontinued all his oral medications. He had lost a heap of weight. He told me he was thinking more clearly, that he was seeing more clearly, and that he’d never felt better. I noticed over the next couple of years that I was able to increase the interval between eye injections, something I had not previously been able to achieve. He is now off his injections altogether and the macula in both eyes has remained free of recurrent swelling. I have noticed a similar response in all my patients with type 2 diabetes who have made the appropriate change in their diet, whether receiving eye injections or not. The macular oedema improves in all, and in most cases, resolves completely. I have recently published a case report of a young woman whose macular oedema due to her diabetes resolved in both eyes within nine months following a change in diet alone (https://journals.lww. com/retinalcases/abstract/9900/diet_induced_resolution_of_macular_ oedema.350.aspx). A larger series of case reports is to follow.
And I’ve noted a similar response in patients with macular oedema due

“I
still remember the very first patient who put his diabetes into remission. He was a man in his late 60s who had type 2 diabetes for over a decade and had been receiving eight-weekly injections into both eyes for many years.”
Dr James Muecke
Ophthalmologist

to retinal vein occlusion. This is the single most satisfying experience of my 40-year medical career. I wish all my ophthalmic and optometric colleagues can experience the joy of turning around a patient’s chronic disease, and of reversing its vision-threatening complications By using food as medicine, rather than using tablets, injections or surgery.
And what dietary change is so profoundly impactful on type 2 diabetes? It’s quite simple – real food. My dietary recommendations are to avoid the dual metabolic disruptors of highly refined sugar and seed oils. I also urge patients to eliminate the industrially-created, ultra-processed food-like substances which often contain them, and which now make up close to half of the calories in the diets of Australians. Some patients may need to be stricter with their carbohydrate consumption – if you have any type of diabetes, you are in essence intolerant of carbs. The limiting of carbs to less than 30g per day is known as a ketogenic diet and it induces a state where the body moves into a safe zone of nutritional ketosis and uses ketone bodies rather than glucose as fuel.
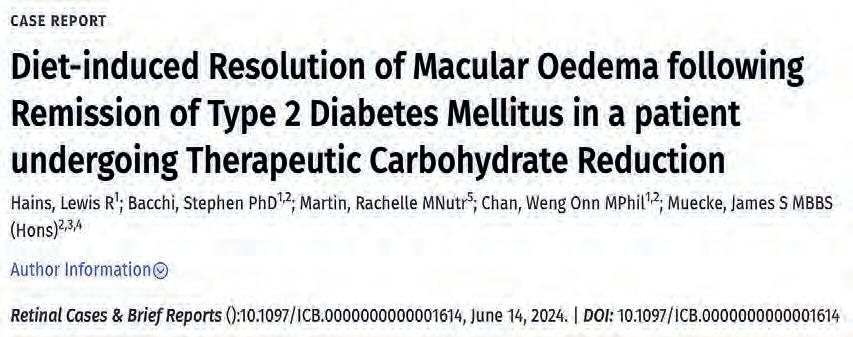
Guidelines for using carbohydrate restriction and promoting healthy natural fats, also known as ‘therapeutic carbohydrate reduction’, have now been written for Australia. They have been endorsed by Diabetes Australia and the Australian Diabetes Society. The next phase is to incorporate this critical principle into the practice of doctors and diet practitioners across the country. Plans are progressing well. I gave evidence to the Parliamentary Inquiry into Diabetes in late 2023. A number of practitioners and patients with lived experience also gave evidence. The report, ‘The State of Diabetes Mellitus in Australia in 2024’, has just been released. I was delighted to read these words in the report: “There was significant evidence revealed about the importance of low carbohydrate diets in all forms of diabetes and this needs to be further promoted and evaluated.”
Recommendation 2 states: “The committee recommends that the National Health and Medical Research Council expedites a review of the Australian Dietary Guidelines, and ensures that the revised guidelines include adequate information for Australians living with diabetes.”
There is at last hope for people living with type 2 diabetes. I just need my medical and nutrition colleagues to understand and embrace the concept.

ABOVE: In Retinal Cases and Brief Reports in June 2024, Dr James Muecke and colleagues published a case report of a young woman whose macular oedema due to diabetes resolved in both eyes within nine months following a diet change.
Other key recommendations from ‘The State of Diabetes Mellitus in Australia in 2024’, include:
• The go vernment explores the potential for effective national screening programs for all forms of diabetes, particularly type 2 diabetes
• T h e government implements a national public health campaign to increase public awareness of the early signs of all forms of diabetes mellitus
• T he government funds the development of education-based obesity screening information and resources
• T ha t equitable access to healthcare for people living with all forms of diabetes be improved through: longer appointments with a healthcare provider subsidised by the MBS; access to case conferencing models of healthcare, especially in rural and remote areas; access to telehealth services; increase in the number of item numbers for allied health consultation for those with diabetes for diabetes educators and dieticians and other allied health providers
• Acc ess to diabetes educators, including in high-risk outer metropolitan, rural and remote communities
• S u bsidised access to Continuous Glucose Monitors (CGMs) is further expanded
• Ex plore expanding subsidised access to insulin pumps for all Australians with type 1 diabetes
• T h e government undertakes a review of the price and choice of insulin pumps in Australia
• T h e government, subject to a positive recommendation from the Pharmaceutical Benefits Advisory Committee, expands the eligibility criteria for Glucagon-like Peptide-1 (GLP-1) receptor agonists, particularly for high-risk patients.
Source: Department of Health.

DWAYNE
COLLINS used YouTube to teach himself to make an ocular prosthetic for his daughter. Realising he could impact the lives of many more with damaged or removed eyes, he now runs an ocularist clinic on the Gold Coast built on compassion and technical know-how.
Aparent will do anything for their child. For Mr Dwayne Collins, when his daughter was born with microphthalmia with her affected eye 40% smaller than her other one, he didn’t flinch in the face of endless medical appointments, constant uncertainty, and the search for an ocular prosthetic. He considered them all essential steps to give his first-born child the life he envisaged during his wife’s pregnancy.
But along the way, two regrettable experiences with ocularists – who fit, paint and fabricate custom ocular prostheses – left the family reeling.
The first instance saw his daughter, Liberty, who is now 11, fitted with a prosthetic that was gazing in the wrong direction and was clearly too big for her. He questioned how someone could allow a client, let alone a child, leave in this condition.
And then the second incident occurred.
“An impression was taken of her socket that was the wrong material, in my opinion, and it got stuck to her eye – I’d already tried pulling it out myself, but it wouldn’t budge. I’m a relaxed person, and I said to the professional, ‘Look, let’s just take her to emergency’, but he wanted to be spared the embarrassment,” he says.
“My wife was hugging her and, bearing in mind it was stuck to her eye, he then pulled it out, which pretty much caused my daughter to pass out. We walked out of that appointment, my wife was bawling, and I just got angry. That was my motivator. I started buying everything that I could think of to make an eye and that’s how it all started.”
Today, Collins has turned a desire to help his daughter into a fully-fledged business, Oculus Prosthetics, working as an ocularist on the Gold Coast. He’s been doing it for almost 10 years now and – disappointed by the lack of education and standards in Australia – has trained under the world’s best overseas.
While a deep sense of dissatisfaction spurred Collins into the world of ocular prosthetics, it all began in 2013 when Liberty entered the world. The midwife told them the abnormality with her eye may be trauma from the birth. They were sent home, but in the following days when laying her on the change table and sunlight hit her face, she didn’t squint or look away.
“From there, we got thrown into a whole new world that we knew nothing about. We were passed around multiple specialists, everyone wanted to meet her because there wasn’t much documented on it at the time. She ended up in a few medical journals. It was something we had to adapt to and it became our new norm.”
As a baby, it was stressful for Liberty to endure. In addition to having bilateral microphthalmia in her right eye, she was also diagnosed with chorioretinal coloboma. This impacts her good eye, and while she’s legally blind, Collins says she is doing well with what vision she has.
In those early days, obtaining an ocular prosthetic for his Liberty started well, despite the circumstances. She was blessed to come into the care of Mr Trevor Dorahy in Brisbane, who is an expert for eye prosthetics for children during crucial growing stages.
But soon, the family needed to move and came into the care of other ocularists. It became clear to Collins that, with training, experience, and perseverance, he could do it better himself.
He initially took to YouTube and encountered a video by leading UK ocularist Mr John Pacey-Lowrie, dissecting each step and piecing together what he could to produce an artificial eye for Liberty. Creating a prosthetic that satisfied the family took over 12 months and involved much frustration, but with each iteration, he knew he was getting closer.
“I had a moment where I went out to the shed and cried, knowing she was walking around with a prosthetic I had made for her – because I had done
something for the family,” he says.
After producing several prosthetics for Liberty over the years, a family of a girl who lost her eye to cancer contacted Collins and asked if he could create an artificial eye for her. He was apprehensive at first given his inexperience, but slowly came around to the idea. The girl was autistic and didn’t like males, so he got to know the family over the course of two months.
“Then one day, she finally put her arm around me, and that’s when we knew we could get started with her eye,” he says.
Becoming an ocularist was an itch Collins could no longer resist scratching. Keen to turn his interest into a career, he was surprised and disappointed to find no official qualification or training in Australasia for the design and manufacturing of bespoke artificial eyes and cosmetic/scleral shells. Especially given what can go wrong with a poorly made prosthesis.
“You are placing a foreign object into the eye socket. So, I’ve had to put all the clinical procedures and practices in place myself because – unlike other countries – there is none for Australia,” he says.
“Post-operatively, you have to know what you’re looking at in the socket, and the scary thing is, anyone can begin making prosthetic eyes. My clients are blessed because of the background I have with my daughter, and I’ve got one of the best ocularists in the world as my mentor.”
He’s referring to Pacey-Lowrie, who has almost 50 years of experience in the field with people flying in to see him from around the world. His career also includes extensive experience at the prestigious Moorfields Eye Hospital in London.
After learning from Pacey-Lowrie’s videos, Collins completed professional development courses in 2017 through the Nottingham Trent University in the UK, tutored by the expert ocularist.
Left wanting more, he contacted Pacey-Lowrie who agreed to help Collins with one month of intense training at his UK clinic. It was a formative experience, and he remembers being blown away by his skill and the effortless way in which he painted the prosthetic.
After returning to Australia, Collins made it a full-time career alongside his window and door glazing business that he still runs today. Collins has opened a state-of-the-art clinic where he openly shares the prosthetic manufacturing process with the client – bucking a trend of secrecy common in the industry.
For his clients, the process takes place over three sessions. It usually begins eight weeks after the enucleation, evisceration, or other surgery the patient might have had, to ensure the swelling has dissipated. First, he takes an impression of the socket and then creates a wax model. It’s intentionally made too big so it can be tooled down to match the other eye symmetrically.
“A big issue we encounter is that a surgeon will tell the patient, ‘Go see Dwayne, he’ll make you look normal’, but quite often we’ve got complications in the socket, so it’s important to remain realistic,” he says. Next, he creates the iris component, which involves intricate painting. A corneal unit – that he sells to ocularists worldwide – with a pupil are then added to the painted iris disc. Once in acrylic, the veins and staining are added to the sclera, and the final part is enhanced for maximum realism. The final step is ensuring the implant sits correctly, and the gaze is in the right direction.
“We want the client to look as natural as possible and have the gaze for conversation etc,” he explains. “Being realistic, if we achieve 80% movement, that’s fantastic. If the surgeon’s done a good job and attached all the muscles correctly, that transposes onto what I make so that the prosthesis will move as much as possible. That’s why an impression is so important and the foundation for getting it right.”
While there’s a lot of technical skill involved, Collins says there’s a



significant emotional factor to his work. It can be traumatic losing an eye, so he never books appointments back-to-back.
“Eighty percent of what I do is psychological and having that understanding of what the client’s going through. So many people come to me from other states that have been treated poorly because there’s no understanding or sympathy,” he says.
“It’s something I’m passionate about. Unfortunately, it’s perceived by many as ‘aesthetics’, even though there’s a functional side to it in terms of socket health keeping the face symmetrical and preventing it from collapsing in on itself.
“The NDIS will fund as many psychology appointments as you want and spend all that money, but why not come sit with me, talk it through, go through the process and leave feeling confident you’ve got an eye in place?
"The psychological impact of not having an eye, walking around in public, is huge – so the system is a bit upside down when it comes to that.”
ProDesign is described as a trusted brand, that’s easy to dispense and a go-to for comfort.

Thoughtful design, comfort and innovation are hallmark features of eyewear that captivate and retain customer loyalty. Danish brand ProDesign embodies these principles, helping independents deliver stylish and high-quality options for their patients.
Bellarine Eyecare owner and optical dispenser Mr Matt Wilson, and practice manager Ms Johanna Scott, agree that with its clean lines, minimalism and ‘face-first’ designs, dedicating a large portion of their floor space to the ProDesign range was a no-brainer.
When Wilson took over the coastal practice in Ocean Grove, Victoria, five years ago he brought with him the philosophy of growing with his clients.
He noticed a trend, where patients would return for a replacement pair of frames after several years, and because their ProDesign spectacles held up so well, they’d request them again.
“At the end of the day it’s a very reliable frame – and at a good price point range,” Wilson says. “We can fit basically anyone that walks through the door into ProDesign if we choose to.”
ProDesign, distributed to Australian independents through Eyes Right Optical, is a Danish brand known for its designs that blend innovation, style and simplicity.
Beyond reliability and affordability – Scott says that despite there often being such a large gap between patient visits, ProDesign ensures its range is contemporary, up-to date and aligned with patient needs.
“The range continually evolves to work with our patients. This, combined with our patients coming back for ProDesign, means it aligns with what we’re looking for in a range for our patients,” she says.
“The range is all about functionality and facial fit. So, it speaks for itself with its classic shapes.”
Described as the “bread and butter” of the practice’s frame range, Wilson says that a quality over quantity business model has proven effective – and he has cut down the selection of brands on offer to focus on the staple few that he knows are high-performers – and with ProDesign as the centrepiece.
In addition to patient satisfaction, Wilson says ProDesign is a favourite among the optical dispensers.
“We can just trust it. It’s easy, and a go-to for comfort as well.”
For both the optical dispensing team and patients, a standout design element are the acetate frames with nose pads which offer superior levels of comfort. With ProDesign, Wilson says its acetate range has the optional feature of nose pads, which is not a common find in the industry.
“This means you’re always going to find the perfect fit. And we utilise that a lot. Whether it be small or large faces, we know that ProDesign will have something to cover that,” Wilson says.
“Some patients don’t understand why their glasses aren’t comfortable. But when you actually take the time to point out a good fit versus a poor fit, and what we can do to improve that, they’re really appreciative. And now, you’ve got a patient for life.”
While ProDesign has elevated Bellarine Eyecare’s patient retention and satisfaction, Wilson and Scott attribute a significant portion of the practice’s success to the support from local eyewear distributor Eyes Right Optical.
Not only does Bellarine Eyecare have a close working relationship with Eyes Right Optical – but patients often do, as well.
“Often, we’ll tell Eyes Right that we have two or three patients that have found a frame within the ProDesign range, and they want to look at other colours. Most of the time, we can get it overnight from them,” Wilson says.
“Not only that, but the sales rep comes down to see the patient themselves, which is a great opportunity for them to see the ProDesign range’s materials, frame fit, styles, and colours. It’s a very rare opportunity for the patient to view the whole range and it’s not very often that this happens. So, we’re lucky to have that relationship with Eyes Right.”
Scott adds that beyond the Eyes Right Optical sales team, and through to the eyewear distributor’s customer service and management teams, the practice is supported at all levels.
“This reliable, consistent support goes such a long way when you’re practising independently.”
The team at Design Eyewear Group – the eyewear designer and manufacturer behind ProDesign – say they are proud to create eyewear that is “designed to fit all”, offering comfortable, classical designs that are both progressive and safe, and just as diverse as their customers. The range is carefully designed with Australian consumers in mind. It is described as having a synergistic relationship with the market – consumers agree with its design principles, and the brand often


releases designs as a direct result of market feedback.
The range, created in Denmark since 1973, combines optical expertise, with a strong design focus, according to Design Eyewear Group CEO Mr Lars Flyvholm.
“Our collection is as diverse as our customers, across generations and fashion preferences. Here you will find a representation of the classics, the icons, the safe choices, the progressive details, the bold options, the essentials, along with the fun and playful details,” he says.
“We believe that high-quality eyewear should always be easily accessible, comfortable, and adjustable. Without ever compromising on either finish, materials, or durability. ProDesign gives customers the opportunity to truly express themselves, simply through their choice of eyewear.”
Eyes Right Optical has been a longstanding partner of ProDesign, serving as a gateway to the Australian market for over 21 years – one of the most important markets in the world, according to Flyvholm.
“Eyes Right Optical represents the values of our brand in the market, and they provide us with valuable feedback to products and marketing which we use globally.”
With feedback from Australian consumers, the brand has launched special products and colour variations made specifically for the
ProDesign’s new ProFlex range incorporates a flexible temple design.
market. Flyvholm also describes the Australian market as an ideal fit, as consumer preferences reflect the “unpretentious” design principles of ProDesign.

Australians seem to like very much the typical clean lines associated with Danish design, but with a twist and touch when it comes to the use of colours,” he says.
“By their very friendly and professional customer service and sales approach, Eyes Right Optical has been nominated best eyewear distributor in Australia several times, and it proves that they are the best, and we are proud to have them as our representative.
“Eyes Right Optical is our guarantee that we will be able to continue growing our presence and have even more happy ProDesign wearers in the country.”
Flyvholm says the company believes the world needs reliable high-quality eyewear that is designed from scratch. And with every element of a ProDesign frame serving a purpose, its products offer both

“When our designer makes a new flexible temple design – like the latest release ProFlex - the look at the side of the temple may appear just as decoration, but it has a purpose, as it allows the temple itself to be flexible, leaving out the need for a flex-hinge,” he says.
“We believe that consumers will value this general approach even more so in the future, and we will stay true to our heritage, while continuing to develop new technical features, colour combinations and use of different material.”
Meanwhile, Ms Cathrine Haugerud, head of global creative direction at Design Eyewear Group, says the design process is lengthy, considered, with many opportunities for technical innovation and design feedback from key partners within the supply chain.
“We take inspiration from many day-to-day situations, but the most important inspiration is the consumer – the wearer,” she says, “We say ‘face first’, so it is more important that the frame fits very well, making the wearer feel great and look good, than the fact that we are inspired by something very specific.”
She adds: “As Danish designers, we love to innovate, but not for the sake of innovation, or being different – but simply to make the product better, which almost automatically makes it timeless.”
In 2024, ProDesign launched its ProFlex design –which incorporates a flexible temple design.
“This is a product where we bring true innovation in terms of the use and design of the temple into classic eyewear shapes and colour delivering an innovative but still very timeless look and feel,”

Light adaptive lenses. Your choice is clear. Simply Sensity.
Sensity light adaptive lenses are available in 4 colours, including blue, to match your patient’s lifestyle. Whatever your shade or style, it’s simply Sensity.


The Specsavers Graduate Program is an industry success story, nurturing the transition from university to the clinic and guided by leaders like DR NATASHA FERNANDES and SARAH YEARSLEY. Now in its 15th year, Insight discovers how the initiative has evolved to remain relevant for the next generation of optometrists.
Dr Natasha Fernandes, the senior graduate optometry development manager at Specsavers, joined the company as a graduate optometrist in 2017. Today, she is helping mould new graduates into confident practitioners, using her own personal experience.
Leading a team of optometrists, Dr Fernandes is responsible for the delivery and continuous improvement of the Specsavers Graduate Program, a comprehensive initiative designed to ease the transition from student to early career optometrist.
Since the first intake of eight graduates in 2009, Specsavers’ latest cohort saw 248 optometrists onboarded – and demand is growing each year with the network often setting a new intake record year-on-year.
A structured approach to in-store mentorship, consistency in the working environment, and access to advanced clinical equipment to support the growth of graduates at every turn, make the program highly sought after.
“This structured support system is crucial for new graduates as they navigate their early career stages,” Dr Fernandes says.
For Dr Fernandes – and many other fresh optometrists – the Graduate Program presented unassuming opportunities and ignited her passion for mentorship.
“I was invited back to attend the next Graduate Induction as a peer mentor to help mentor the new incoming graduate cohort, which I absolutely loved. That was my first taste of working alongside the Graduate Optometry Team,” she says.
After working in regional practice for almost three years, she moved to a larger store in a busy metropolitan region with many graduate optometrists, and found fulfillment derived from supporting new professionals.
“I think it’s a wonderful thing to be able to support optometrists at a stage in their journey where they need support the most, and it’s fulfilling being able to relate to them through my own journey as a student to graduate optometrist and beyond that.”
The Specsavers Graduate Program is carefully designed to ease graduates
into the realities of practice over its two-year duration and features various touchpoints to support the professional development of graduates.
The first touch point is Graduate Induction which helps to set the new graduates up for success as they start their careers with Specsavers.
Professional development workshops during this induction address common graduate challenges, from clinical content to patient communication and preparing them for their first professional roles.
In the second year of the Graduate Program, graduates are encouraged to adopt a broader mindset where they explore longer-term career goals and aspirations and how they can find fulfillment and longevity in their careers. They are made aware of diverse career development opportunities, where they can explore business aspects of optometry, niche clinical areas, or roles in mentorship and training.
“We help them identify their strengths, weaknesses and passions and build the skills needed to pursue their longer-term career goals,” Dr Fernandes says.
She adds that the various Graduate Program events, CPD events, networking

“I think it’s a wonderful thing to be able to support optometrists at a stage in their journey where they need support the most, and it’s fulfilling being able to relate to them through my own journey as a student to graduate optometrist and beyond that.”
Dr Natasha Fernandes Specsavers
Dr Kalp Shah was among the 2022 Graduate Program cohort, which he completed at Specsavers Werribee. The experience shaped him into a confident practitioner in the test room, and a leader outside. Now, he is store partner at two locations in Geelong, Victoria.
“Working with the latest imaging technology and experiencing a large volume of patients helped accelerate my development as an optometrist to ensure I was able to provide the best care for my patients,” he says.
Dr Shah says the touchpoints throughout the Graduate Program were well placed to ease him into practice, and built the framework of an accomplished, holistic optometrist.
“I am now more aware of what is required for someone to be a well-rounded optometrist, so I am more mindful of the needs of new graduates when mentoring them, especially integrating the commercial and clinical aspects of optometry.”

For Dr Shah, a turning point in his graduate journey was his second-year project when he was required to drive change within the store team. He says this exposure cemented his goals of partnership.
“The guidance, support and resources provided by the Graduate Optometry Team was instrumental to my self confidence in my ability to lead a team, to drive positive change and, as a result, successfully complete the Pathway Program.”
Dr Jessica Jovanovski, from Specsavers Broadmeadows in Melbourne, says the Graduate Program and its “open-door” policy has been helpful in providing reassurance to build her clinical confidence.
“It truly felt like they cared about our transition from student to qualified optometrist and I knew I wanted to begin my career somewhere I was cared for,” she says.
“I have developed the clinical skills, knowledge and confidence to be a successful optometrist that ensures the best patient care. I’ve also had the opportunity to develop my leadership skills.”
Dr Jovanovski says the Graduate Program is focused on the growth of graduates, with a plethora of development opportunities throughout its two-year duration.
Dr Jessica Jovanovski, Specsavers Broadmeadows, Victoria.
“We recently had a development day where we were encouraged to discuss our future aspirations so that the Graduate Optometry Team could ensure that we were supported,” she says. “I have expressed my interest in outreach and Aboriginal and Torres Strait Islander eyecare and they helped me attend the National Aboriginal and Torres Strait Islander Eye Health Conference.
“We have also been given the opportunity to be a part of other outreach opportunities and to work with The Fred Hollows Foundation.”
Dr Jovanovski lists the multiple conferences, seminars and CPD events as a gateway to becoming the compassionate and skilled optometrist she has always wanted to be, with capacity for further growth.

“Our graduates are assured that they will have appropriate support, whether that be via the optometry partner or a senior optometrist. You’ll usually have a wide clinical team around you.”
opportunities, and the Specsavers Clinical Conference ensure graduates feel connected and supported throughout the program, as she once did.

“There are a few different avenues for career development as optometrists at Specsavers within our business. I wasn’t sure which specific path I wanted to go, but I discovered I was passionate about optometry development. My mentors were great in guiding me when the opportunity on the Graduate Optometry Team arose,” Dr Fernandes says.
The Graduate Recruitment Team, led by Mrs Sarah Yearsley, works closely with Dr Fernandes and the Graduate Optometry Development Team to manage recruitment campaigns and engage with university optometry students.
A recruitment consultant is assigned to each of the eight universities offering optometry in Australia and New Zealand, which Yearsley says is key to ensuring students feel heard and supported in securing their first role as graduate optometrists. A core component of the network’s relationship with students is the volume of clinical placements it offers.
“Specsavers is the largest clinical placement provider across Australia and New Zealand, with about 70% of students who complete a clinical placement in store within the network joining the Specsavers Graduate Program,” Yearsley says.
The two-year structured Graduate Program and various career paths, including the Pathway Program for business ownership, are highly attractive to graduates.

Dr Ismar Kumbara, Specsavers Midland Gate, Western Australia.
Initiatives like ‘Early Bird’ offers, and the ‘Go with a Friend’ incentive encourage graduates to consider practising regionally.
“With Early Bird offers, optometrists are offered a bonus if they sign on before the end of June,” Yearsley says. “This offer has been growing in popularity because the graduates know they’re going to benefit from the different pathology and the diverse experience associated with a regional practice.”
And the Go with a Friend program reduces the fear of graduates travelling to a new, remote location on their own.
“This way, they just feel a bit more comfortable. They’ve got someone else from their cohort going with them to the regional location. They’ve got someone to spend time with on their days off and they don’t feel so far from home. They can gel themselves into the community a little bit more,” Yearsley says.
“Our graduates are assured that they will have appropriate support, whether that be via the optometry partner or a senior optometrist. You’ll usually have a wide clinical team around you,” Yearsley says.
She adds that venture partnerships provide a stable environment, with graduates assigned to a specific store.
“The graduate will get full scope mentorship from the optometrist and from the retail team and develop well-rounded skills to run a practice,” Yearsley says.
joint-venture program to one day manage his own practice as an Optometry Director.
“I believe the Graduate Program will be instrumental not only in my development as an optometrist but also in developing my leadership skills,” he says.
“Our Graduate Program has grown significantly since we hired our first graduates in 2009. It’s wonderful to see the program grow and to hear how much it has supported our graduates.”

#Targets all layers of the tear film, suitable for evaporative, aqueous deficient & mixed dry eye TRIPLE ACTION TARGETS ALL LAYERS OF THE TEAR FILM1,2




MINIMUM PRODUCT INFORMATION
Before prescribing, please review the full product information at www.aftpharm.com/prescription/vizo-pf-dorzolatim.
Indications:
Treatment of elevated intraocular pressure (IOP) in patients with ocular hypertension or open-angle glaucoma when concomitant therapy is appropriate.
Contraindications:
Reactive airway disease, bronchial asthma or a history of bronchial asthma, or severe chronic obstructive pulmonary disease; sinus bradycardia, sinoatrial block, second or third degree atrioventricular block, overt cardiac failure, cardiogenic shock; hypersensitivity to any component of this product.
Precautions:
Adverse reactions found with systemic administration of beta-blockers may occur with topical administration.
Cardio-respiratory reactions; vascular disorders should be treated with caution; masking of hypoglycemic symptoms in patients with diabetes mellitus; masking of thyrotoxicosis; surgical anesthesia; immunology and hypersensitivity, the dorzolamide component is a sulfonamide; concomitant therapy with carbonic anhydrase inhibitors; not been studied in patients with acute angle-closure glaucoma; choroidal detachment has been reported; increased potential for developing corneal oedema in patients with low endothelial cell counts; beta-adrenergic blockade has been reported to increase muscle weakness; patients should be advised to seek their physician’s advice if they develop an intercurrent ocular condition or any ocular reactions; Dorzolamide/timolol 2%/0.5% has not been studied in people wearing contact lenses; not been studied in patients with hepatic impairment; not been studied in patients with severe renal impairment (CrCl < 30 millilitre/min); for use in the elderly and paediatric use, see full Product Information (PI).

Pregnancy Category C, (see full PI). A decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Interactions with other medicines:
See Contraindications and full PI; specific drug interaction studies have not been performed with Vizo-PF Dorzolatim.
The potential exists for additive effects and production of hypotension and/or marked bradycardia with timolol maleate; disturbances have been reported with oral carbonic anhydrase inhibitors; mydriasis resulting from concomitant use of timolol maleate and adrenaline has been reported.
Adverse effects:
Most frequently reported adverse effects were: ocular burning and stinging, taste perversion, corneal erosion, conjunctival injection, blurred vision, tearing, and ocular itching; urolithiasis was reported rarely; others (see full PI).
May affect some patients’ ability to drive and/or operate machinery.
Dosage:
One drop in the affected eye(s) two times daily; when substituting for another ophthalmic antiglaucoma agent(s), discontinue the other agent(s) after proper dosing on one day, and start Vizo-PF Dorzolatim on the next day.
If another topical ophthalmic agent is being used, the other agent should be administered at least ten minutes apart; efficacy in paediatric patients has not been established (for more information regarding safety in paediatric patients ≥ 2 and < 6 years of age, see full PI).
To avoid contamination of the solution, keep the container tightly closed, do not let the dropper tip touch any surface.
Unopened bottle: Store below 25°C. Protect from heat. Opened bottle: Store below 25°C. Discard contents 4 weeks after opening the bottle. Protect from heat.

Vision Eye Institute has revamped its operating model into something that would be unrecognisable to its founding fathers, building in new capabilities and flexibility to meet the demands of the modern-day ophthalmology workforce.

Dr Lewis Levitz (right) has been with Vision Eye Institute for 16 years.
Dr Lewis Levitz has been exposed to the advantages and pitfalls of various operating models in ophthalmology clinics – but there’s one organisation that stands out the most, and it’s the one he has been with for 16 years and counting.
In 2008, after eight years in solo practice in his native South Africa, Dr Levitz jumped at an opportunity to move to Australia to work in Hervey Bay, Queensland, for Vision Eye Institute (VEI). It was an emerging group at the time and the brainchild of a handful of established Australian ophthalmologists who figured private specialist eyecare could be better delivered and sustained at scale.
That vision was realised, with VEI now Australia’s largest private ophthalmology provider.
Based in Melbourne today, and one of VEI’s longest-standing ophthalmologists, Dr Levitz has witnessed a “seismic shift” in the way the organisation operates. This is largely due to its transition from a publicly listed entity to privately owned company in 2015 – a move that brought with it greater flexibility to accommodate the more than 100 doctors currently consulting in VEI clinics and/or operating at its associated day hospital network, Vision Hospital Group (VHG).
When he started at VEI, its rigidity meant it only catered to full time ophthalmologists. But fast forward 16 years and “its evolution has been so significant that it would be unrecognisable to those involved in the early days”.
“For example, our CEO Ms Amanda Cranage comes from an orthoptic background and has a unique patient-, service- and doctor-orientated
approach,” he says. “The realisation that all our doctors are at different stages of their careers is now what drives our company vision. Gone are the days of the one-size-fits-all partnership. It’s been replaced by an enhanced respect for the doctors’ work-life balance, academic obligations and family needs. We have the flexibility to choose our level of commitment and how our sessions are structured.
“VEI is now a niche group of ophthalmologists who have a common interest in practising ophthalmology without the additional headache of running practices or theatres. We are happy to delegate the day-to-day running of the practices to VEI, with their industry expertise and rigorous systems and processes.”
The modern-day VEI is attractive for several reasons, says Dr Levitz.
The fact VEI funds research by doctors and staff through its Future Vision Foundation (FVF) “is a terrific incentive” for some. Meanwhile, others are looking for sessional work – say two or three sessions a week – perhaps to subspecialise in lower volume clinics such as ocular oncology or oculoplastics, or to fit in with their sessions at non-VEI clinics.
But many, like Dr Levitz, simply want to free themselves from managerial and administrative overheads.
Reflecting on his solo practice in Johannesburg, Dr Levitz says it eventually dawned on him that he didn’t necessarily own the practice. In fact, he often felt like he was working for the bank. And any “freedom” to make decisions was offset by the practice consuming his leisure time.
He points to a well-documented trend amongst ophthalmologists

to consolidate practices due to rising expenses and work-life balance considerations. American Academy of Ophthalmology statistics from 2022 show 46% of ophthalmologists are now choosing to work in group practices. In Australia, a University of Melbourne study showed the number of doctors in group private practices has increased by 28.9% from 2013 to 2020.
“Firstly, VEI offered me work in already established and busy practices, but secondly it allowed me to practise clinical ophthalmology without the hassle of paperwork and the like,” he says.
“You do the work you’re trained to do, put your tools down at the end of the day and go home to spend time with your family. You’re not worrying about what will happen to the clinic if you’re struck down by a virus, or how to pay the clinic costs while you take a holiday. VEI takes away the headaches that I believe lead people to burnout.”
Today, Dr Levitz works across three of VEI’s Melbourne practices (Camberwell, Blackburn South and Coburg), with a couple of surgical lists per week. He’s remunerated based on the amount of consulting and surgical work he undertakes.
Aside from his consulting and surgical work, he is also VEI’s national medical director, reporting to the board on the company’s clinical performance and conformance to clinical standards. As part of this, he chairs the Clinical Care and National Infection Control committees.
Cranage, who has been CEO since mid-2023, says VEI explored new models that allowed more flexibility and responsiveness to changing workforce demands to attract and retain ophthalmologists. Prior to 2015, the company only offered full time contracts but now caters for a variety of scenarios including part time or sessional work.
After starting as an orthoptist in 1996 at Camberwell Eye Clinic – which later became VEI – Cranage has risen through the ranks of the organisation and had a front row seat to its transformation.
“We’ve needed to evolve with the ophthalmic workforce, and what we quickly realised is that some doctors like to work in a variety of practice types, private and public, across a number of locations. They thrive on variety and don’t necessarily want to turn up at the same place every day,” she says.
Cranage speaks proudly of how the organisation has responded to the changing needs of its medical workforce. “Doctors working in our practices have complete flexibility to set their own schedule of patient appointments and fees. We’re simply the mechanism to support them, whether they are geared towards high or low patient volumes.”
When Cranage visits VEI practices, the overwhelming feedback from previous solo operators is the new-found freedom they now enjoy. Meanwhile, they have access to the latest practice management systems
and ophthalmic technology – all with the necessary upgrades and service contracts without the worry of procurement and upkeep.
“The setting is very collegiate, yet doctors have complete professional autonomy in how they manage their patients,” she says.
“There’s also operating rights at our Vision Hospital Group day hospitals where ophthalmic procedures are performed all day, every day. Surgeons enjoy their lists because our specialist ophthalmic theatre teams live and breathe ophthalmology and are prepared for every possibility.”
Cranage says there are several remuneration models, including a fixed-payment model that might be attractive for younger ophthalmologists looking to build their practice with confidence and stability, profit-sharing models, and percentage-of-revenue models. Determining the most suitable model will depend on any number of factors.
And if it doesn’t work out as planned? Both parties can part ways amicably.
“It’s not realistic to think we will be the right fit for everyone. Fortunately, the models we now have in place have promoted strong retention," she adds.
Cranage says too much focus on the term ‘corporate’ detracts from the dedication and hard work of VEI staff.
“For us, it’s all about patient care, service and outcomes,” she says.
“But there’s no denying the value that our corporate network offers: we can be more efficient in providing that service, provide access to the latest technology, provide comprehensive training for our staff, monitor an incredible amount of patient feedback to understand how we are doing and where we can improve, pilot initiatives on a small scale before rolling them out across the organisation, and provide great opportunities to get involved in research.
“It’s been a long time coming, but people are changing their perception about us. I would encourage ophthalmologists who might be interested in working in a corporate environment at VEI to talk to their peers who work here. Ask them for their honest opinion.”
For those who might not be ready or interested, they can still choose to perform surgery through its day hospitals as a visiting medical officer (VMO). Although owned and operated by VEI, the distinct VHG brand was realised to allay any fears non-VEI ophthalmologists may have about losing patients.
“Our day hospitals aren’t always co-located with our clinics, and we do offer those services to (non-VEI) ophthalmologists who would like to build their surgical practice in the local area. We’d like to engage further with the eyecare community, so it understands the world-class service we offer,” she says.
“Many of our VMOs are complimentary of our ability to go above and beyond to ensure the process flows smoothly for themselves and their patients. They emphasise how reassuring it is to operate in a theatre where there is the expertise and equipment for any situation, so they can really focus on their patients.”
For Associate Professor Michael Lawless, who has been with VEI since its early days, Cranage embodies everything about the modern-day organisation.

“If I work harder, I earn more money. If I work less or have more weeks away, I earn less. I can choose to do as much or as little as I like.”
A/Prof Michael Lawless Ophthalmologist


“You’re not worrying about what will happen to the clinic if you’re struck down by a virus, or how to pay the clinic costs while you take a holiday. VEI takes away the headaches that I believe lead people to burnout.”
Dr Lewis Levitz Ophthalmologist
“When I look around VEI – and I’m on the Medical Advisory Board so I understand how it runs – I see a fantastic team led by a terrific CEO and very strong administrative executive staff. They’ve all been around long enough to really get ophthalmology, the day surgeries and laser suites,” he says.
From a solo practice built on his corneal subspecialty in the 1980s, to a two-man band (joining forces with Dr Chris Rogers and buying Australia’s first excimer laser) that ultimately grew into a multi-subspeciality clinic and day surgery, A/Prof Lawless experienced all modes of practise prior to joining VEI in 2005.
He balanced this alongside a public appointment at Royal North Shore Hospital for 20 years.
The hardest part of running his own ophthalmology practice was securing the funds to purchase equipment. “It’s a capital-intensive specialty,” he says. As such, VEI’s equipment procurement expertise has helped A/Prof Lawless do much of his pioneering refractive surgery work.
For example, he was the first Australian surgeon to perform laser cataract



surgery with the femtosecond laser in 2011, performed the country’s first SMILE Pro laser surgery in 2023 with one of the Southern Hemisphere’s first installed ZEISS VISUMAX 800 femtosecond lasers, and most recently completed the world’s first iris-based OcuLign for cyclotorsion adjustment.
Practising independently can also create an element of loneliness. “I always saw so much power in a group.”
When VEI came on the scene, he was curious. At the time, GPs, radiology, and pathology were all being corporatised and he liked the personalities involved with VEI. So, with a large, mature practice and co-located day surgery, he joined the group. A/Prof Lawless eventually became medical director and part of the board so he could understand and influence how the network was run.
The way he has been remunerated has evolved over the years, but as he reaches the latter part of his career, he now takes a percentage of what he earns for the group.
“If I work harder, I earn more money. If I work less or have more weeks away, I earn less. I can choose to do as much or as little as I like,” he says.
With the VEI model, he says ophthalmologists can become involved in the running of their clinic to the degree they wish. There are also various ways for ophthalmologists considering a job switch to ease their way into the group, becoming more invested over time.
“Ophthalmology is a fabulous specialty to be practising for this last generation and this coming generation. If you’re a young person in your 30s, and you’ve just graduated, have faith in yourself and your future,” he says.
“You are in a terrific bargaining position because you have great skills. Understand who you work well with, respect and trust. Above all, have the courage to make decisions that you’re happy about.”
NOTE: VEI will be an exhibitor at Adelaide’s RANZCO Congress from 1–4 November 2024, allowing ophthalmologists and support staff in attendance to learn more about the organisation, including VHG and FVF.


The Olleyes VisuALL - the virtual reality platform transforming vision testing.
• Improved patient experience and comfort with VR testing.
• Enhanced clinical results and accuracy through advanced features like eye tracking.
• Increased practice efficiency and productivity with the virtual assistant and comprehensive multi-test capabilities.

All the common visual field testing protocols you need - clinically validated for peace of mind.1
Full Threshold (Normal T)
AVA standard & AVA fast
Suprathreshold
The testing suite also covers visual acuity, colour vision, pupillometry, extraocular motility and more.
Ptosis and Esterman.
1 Griffin et al. (2024). Prospective Comparison of VisuALL Virtual Reality Perimetry and Humphrey Automated Perimetry in Glaucoma. J Curr Glaucoma Pract, 18(1), 4–9.
Increased efficiency and productivity.
With an ability to speak over 35+ languages, Annie guides patients through every step of the testing process and monitors their compliance, freeing up your time for other tasks.
Paediatric focused testing.
Animated and gamified testing that’s proven to be more child-friendly than traditional methods.2
2
An eye tracking system ahead of the rest.
The first-of-its-kind Dynamic Matrix algorithm is a game changer that accounts for the most minute eye movements, reducing fixation loss to zero during visual field testing







Australian eyecare professionals are confident in the nation’s ability to combat the global myopia epidemic. Equipped with industry-leading products, a myopia-centred practice focus, and a proactive attitude towards management, experts discuss how Australia is leading the charge.
ustralia and New Zealand are fortunate to have some of the best proactivity, enthusiasm and acceptance of myopia management anywhere in the world, and a wide availability of treatments and scope-of-practice where optometrists can prescribe atropine.
Dr Kate Gifford, clinician-scientist, peer educator and professional leader based in Brisbane, is among those at the forefront of the country’s
Alongside her husband, Dr Paul Gifford, she developed Myopia Profile, a multi-platform digital resource for education in childhood myopia

Although Australia is well placed, Dr Gifford cites barriers to implementing the optimal degree of myopia control.
“I think the biggest challenge that any practitioner would likely cite is the cost. The cost to the patient of these special spectacles or contact lenses, is a lot more upfront than just single vision spectacles, and they're not necessarily covered to any significant degree or given more benefits with private health insurance, which is minimal and has barely kept pace with the cost of glasses over many years,” she says.
“I think it’s an issue of access for patients who maybe can't afford this upfront, particularly with escalating costs of living concerns in the present day.”
A 2023 study from the Brien Holden Vision Institute explored lifetime myopia costs and found the additional early costs of early myopia management options such as low-dose atropine, antimyopia spectacles, antimyopia multifocal soft contact lenses and orthokeratology (orthoK), are substantially balanced across a lifetime by reduced refractive progression, simpler corrective lenses, fewer lens replacements, reduced risk of eye disease and vision loss, and reduced management of myopia complications.
“Modelling has shown that myopia management doesn't cost more for the patient over their lifetime when you factor in having a lower level of myopia,” Dr Gifford says. “If you have a lower level of myopia, you won't

“If we can delay or stop children becoming myopic in the first place by screening for risk factors, by talking about visual environment, such as increased outdoor time, reduced screen and near work time, then that’s going to have a huge impact on changing the trajectory of myopia.”
Dr Kate Gifford Myopia Profile
need complex corrective lenses. Not only do you get improved eye health outcomes, but the upfront costs you might pay for more complex spectacles, contact lenses or atropine eyedrops is very much balanced in the long term.”
In response, Optometry Australia (OA) has assembled a position statement on myopia management, that details its support of the World Council of Optometry Standards of Care Guidelines for Myopia Management (2021), which advise comprehensive eye exams, risk assessment, patient counseling, and appropriate treatment options.
OA endorses a shift from simply correcting vision to evidence-based strategies to mitigate myopia development and manage its progression.
And on a global scale, international bodies are just as active.
“The World Council of Optometry made a resolution to state that myopia management must be standard of care in 2021. From the ophthalmology point of view, the World Society of Paediatric Ophthalmology and Strabismus made a position statement just last year,” Dr Gifford says.
Industry momentum was accelerated in 2019 when data first showed the efficacy of soft contact lens and spectacle interventions for myopia control.
“Prior to that, we only had data for orthoK and for strong concentrations of atropine. But in 2019 we had the first publications on MiSight 1 Day contact lenses and on DIMS spectacle lens technology. We also had the landmark LAMP atropine study, which was the first to compare various low-dose concentrations of atropine.”
And in 2019, the first volume of the International Myopia Institute reports were published, which has since spurred a new era of awareness and activity in this space.
“This includes practitioner awareness, industry innovations, and the technology being matched by the scientific recognition. These consensus reports detail what myopia management is about and why it's a necessity,” Dr Gifford says.
She says that Australia and New Zealand were quick to adopt this practice mindset shift and are now leading the way for proactive myopia management and prescribing.

“Trends show us that we're much less likely to be prescribing single vision correction than colleagues elsewhere in the world,” Dr Gifford says.
This proactivity is reflected in recent research findings by Dr Gifford.
A survey conducted on Myopia Profile looked at what practitioners were identifying as their levels of confidence and barriers to myopia management from 2019-2023. The findings were presented at the ARVO 2024 conference.
“Interestingly, we found that their levels of confidence weren't much different between 2019 and 2023 which is surprising considering the increased availability of knowledge, treatments and resources in that time. They feel as though they need to know more before they can get started,” Dr Gifford says.
“Practitioners identified their level of knowledge as the biggest barrier to myopia control, and communication as their second biggest.”
Dr Gifford attributes this to wider adoption of myopia control. Eyecare professionals engaging in myopia management education and training in 2019 were considered early adopters. Since then, ECPs across the industry have adopted myopia management as standard care, and may not be as well versed in it.
“I think the barrier with clinical communication primarily, is time. There's lots to talk about. Instead of just, ‘Your child needs a new pair of glasses’, we can say, ‘We need new glasses, but we can also fit contact lenses or use atropine’,” Dr Gifford says.
According to Dr Gifford, the Myopia Profile website and platforms are attempting to address three challenges with its three pillars of activity: practitioner education, clinical resources and public awareness.
“Practitioners will learn about the research through Myopia Profile, and also have access to tools to put their knowledge into practice,” she says.
“The platform can be used to support practitioners who don’t consider myopia control the main part of their practice or professional interest to do their best in myopia management.”
In September, Myopia Profile is running the second global Myopia Action Month to deliver 30 days of tailored education for ECPs. It has also recently introduced a new set of Made Simple courses, with the first free course, Myopia Management Made Simple, launched in September 2023. Dr
Gifford says the courses are ideal for practitioners who are time poor yet understand the necessity of implementing best myopia control in practice.
“We launched the first free myopia management and practice course in 2019, but because we're now talking to a larger audience, most of whom aren’t the early adopters, we've recognised that there's a need for practitioners to learn what they need to know as efficiently as possible,” she says.
"These Made Simple Courses are all one hour in duration and intensely practical, and designed to fill that gap for the practitioner who doesn't feel like myopia management is their life's calling, but recognises that they need to learn more to be able to put it into practice.
“We have launched another five courses covering spectacles, soft contact lenses, visual environment, atropine and orthoK, and they're in process for accreditation for CPD in multiple countries.”
On a broader scale, Dr Gifford says she’d like to see proactive early intervention and preventative measures to delay the onset of myopia.
“An analysis published in 2023 said that one year of delaying the onset of myopia can give as much result as two to three years of a myopia control treatment in terms of reducing someone's final level of myopia,” she explains.
“If we can delay or stop children becoming myopic in the first place by screening for risk factors, and by talking about visual environment, such as increased outdoor time, reduced screen and near work time, then that's going to have a huge impact on changing the trajectory of myopia.”
Dr Gifford suggests nationwide screening of preschool and early primary school aged children, public awareness campaigns, powerful government-supported and widespread campaigns about increasing time spent outdoors and managing screen time.
She cites useful international research in schools, which could be implemented locally. In Taiwan, where approximately 80-90% of the population are estimated to be myopic by the time they’re 18, researchers assessed the effects of outdoor exposure during school on disease progression.
Half of the study cohort had intentionally more outdoor time during recess and, as result, showed a reduction in frequency of myopia onset.



"We're also among the early adopters of clinical outcomes and research in myopia management. We have clinicians who have such a keen eye for how their patients are responding to optical products."
Meanwhile, researchers in China have investigated the effects of classrooms with wallpaper depicting outdoor scenery compared to traditional classrooms on myopia progression.
The results showed that students in the outdoor scene classrooms showed less myopic shift compared to traditional classrooms, after one year.
Hyperopic students in the outdoor scene classrooms had significantly less myopic shift and axial elongation compared to baseline.
Dr Gifford says that myopia control solutions need to incorporate the technological culture of today’s world as close-proximity work and activities are an inevitability.
“We can't just say, ‘Get off your screens and spend time outdoors’ when we know that's not what modern life is like,” she says.
“Finding solutions that are realistic and work for parents without making them feel guilty are key, such as what can be done at school and implemented in a broad scope way.”

•6-month unconditional warranty.
•Available in all indices -
1.50, 1.59, 1.60 and 1.67.
•No child left behind - vouchers available, contact us for details. zeiss.com/myopia
Optometrist Ms SooJin Nam, the force behind Eyecare Kids in NSW, says she has always been interested in children's vision and the impact that refractive errors and binocular vision has on a child’s development.
“Vision related challenges can make learning or paying attention in the classroom more difficult. Myopia is of particular concern, because it is the one refractive error that gets progressively worse as someone gets older and associated with ocular pathology,” she says.
“At the end of the day, we're not just looking at the child as they are now; we're also looking at the potential difference we can make for them in their lifetime.”
When Nam began prescribing orthoK in 2004, she noticed the young myopes did not appear to be progressing as quickly as those wearing single vision spectacles. Since then, she has seen the landscape and industry evolve, as myopia’s acceptance grew, and management became an accepted treatment methodology.
“For a long time, the conception was still, ‘Is myopia nature or nurture?’ And for many years afterwards, there were still a lot of questions and skepticism as to whether myopia could be controlled by any means,” she says.
“We didn't really get those randomised control studies until much later, but this doesn’t meant that we were not seeing those clinical outcomes in the practice.”
Beyond a growing prevalence, Nam says this has been accompanied by growing awareness among patients. She cites much of this coming from word-of-mouth or independent online research.
“I believe there’s more conversation happening on the outside that we're not aware of,” she says.
The volume of conversations taking place outside the clinic is a step in

There is a critical need for myopia management to become a global standard of care. As eyecare professionals, we face both a challenge and an obligation to integrate myopia management into every practice. Since launching New Zealand’s first myopia management clinic in 2009, I’ve dedicated my work to advancing this field, which was once not a priority.
Today, the clinic is thriving. We’re passionate about myopia and the ability to help children better now than ever before. We banned the use of single-vision distance glasses for treating myopia and instead offer all the available options globally. Our clinic receives referrals from local optometrists, ophthalmologists, and other specialists in the Hamilton area. We then create a treatment plan, working with the referring practitioner to co-manage the patient’s myopia.
Over the past 15 years, New Zealand practitioners have advanced significantly in myopia management, surpassing many others globally in treatment options and implementation. The availability of specialised lenses, other eyecare tools, and knowledge of myopia management practices varies by region. We must continue sharing our expertise to help areas with less advanced practices enhance their myopia management capabilities.
That’s why I agreed to become an ambassador for the WCO CooperVision Myopia Management Navigator (myopianavigator. info). The World Council of Optometry (WCO), in partnership with CooperVision, launched the navigator in April 2024 to further its mission to make myopia management a standard of care globally.
It’s an interactive and educational online guide that is free for eyecare practitioners to access. Think of it as a cheat sheet for getting started with myopia. You can look through the navigator relatively quickly and be upskilled with the current evidence and myopia treatment options. It takes you through three steps: mitigation, measurement, and management, providing evidence-based resources for each.
The mitigation section walks you through how to talk to parents and children about the risk of developing myopia and how to slow its progression. It provides lifestyle-related advice, such as maximising time outdoors and limiting screen use. It also discusses risk factors for children, including spending time on near work and having myopic parents, as well as myopia’s link to other serious eye health problems.
The measurement section gives you an overview of what measurements to incorporate into a child’s eye exam to determine whether the child has myopia or is at risk of developing it. It includes four standard assessments and three additional checks for myopia. It also guides you through how often to follow up with patients and what to look for, including four key things to check and what to measure at six-month and one-year follow-up appointments.
The management section provides an overview of probing questions
ABOVE: Jagrut Lallu is a New Zealand optometrist and World Council of Optometry-appointed global myopia ambassador.

management intervention most suitable to the child’s lifestyle, the family’s budget, and the time available. It shares proven, effective clinical interventions available to manage progressing myopia, such as soft dual focus or multifocal contact lenses, orthokeratology, spectacle lenses, or atropine. Under this section, you’ll also find patient profiles to help you think about a child’s lifestyle and how it factors into which interventions best suit them.
As an ambassador, my goal is to raise awareness about the navigator and answer any questions to encourage more eyecare professionals to use it. To me, this is important because we need to ensure we lead the way in establishing the minimum standard of care. We are very fortunate in Australia and New Zealand that we have almost all available myopia management treatment options, and all practices have access to at least two or three of those options. Resources like the navigator help facilitate conversations, leading to a change in societal behavior.
There is a future health risk, with cases of myopia continuing to rise at an alarming rate. The most important thing you can do is to start doing something. Use the navigator, spread the word about it, or reach out for mentorship or guidance from people like me who are happy to share knowledge. Teamwork makes the dream work.
BIO: Jagrut Lallu is a partner of Rose Optometry in Hamilton, New Zealand. He is also the director of Innovatus Technology, which develops software to make contact lens design accessible to practitioners. In 2009, Lallu set up the first myopia control clinic in New Zealand devoted to evidence-based methods for management. In 2023, he established the New Zealand Eye Research Centre. Lallu is also a clinical senior lecturer at the Deakin School of Optometry in Geelong, and is an honorary teaching fellow at the University of Auckland. Lallu is one of four WCO-appointed global myopia ambassadors.
LEFT: The measurement section of the Myopia Management Navigator gives practitioners an overview of what measurements to incorporate into a child’s eye exam to determine whether they have myopia or are at risk.

the right direction, but Nam says the largest industry hurdle is how to communicate and subsequently manage lifestyle factors to prevent myopic progression in the first place.
“Communication to children and teenagers, regardless as to whether they're myopic or not, that they need to spend more time outdoors and less time on screens is a big challenge. I'm a mother of two teenage boys, and I know first-hand how challenging that is.
“It’s easy to say, but sometimes it's not as easy to implement. I encourage lifestyle changes, like choosing outdoor sports and activities, so that the time outdoors just happens naturally.”
Nam also says communication about management options can be a challenge due to the sheer volume of information available.
“Trying to make all that information clear and succinct is difficult. As well as explaining myopia management, I still have to go through their other visual needs.”
To condense all this knowledge in the allocated time frame, Nam relies on in-house resources such as action plans and information booklets –but keeping it relevant to her practice.
“There’s just so much information, so it’s about tailoring it, and recommending what is best for the patient with the products and services you have at your disposal,” she says.
“It's so much like going to a wall full of multivitamins: you know you need something, but you don't know which ones are the ones you should take.
Nam, along with Dr Gifford, places Australia at the forefront of understanding myopia control in the world.
“We're also among the early adopters of clinical outcomes and research in myopia management. We have clinicians who have such a keen eye for how their patients are responding to optical products,” Nam says.
THE MYOPIA EXPERT 700 MEASURES AXIAL LENGTH , ENABLING NON-INVASIVE AND ACCURATE MONITORING WITHOUT ANY NEED FOR CYCLOPLEGIA
She adds that optometrists have access to all myopia control products such as peripheral defocus spectacle lenses, myopia control contact lenses, low dose atropine, the wide range of orthoK lens designs, which well places them to provide a world-class service.
“They don’t just have access to all the myopia control products, but also access to all the technology to measure, maintain and monitor patients –which isn’t so accessible in other countries.”
In terms of the future of myopia management in tertiary care, Nam says there is promising international research in gene therapy in this space, and therapies targeting the underlying causes of myopia.
And for everyday management, she cites new wearable devices as an adjunct to spectacles that monitor and encourage healthy visual habits and make meaningful changes to behaviour.
“This includes monitoring how much time people are spending looking at something close up compared to how much time they're spending outdoors.”
For Nam, she would like to see studies evaluating the efficacy of different combinations of dual therapy.
“At the moment, we can find systemic reviews on the efficacy of combined orthoK and 0.01% low dose atropine, and some preliminary research that explores MiYOSMART and Stellest spectacle lenses with 0.01% atropine,” she says. "But I'd also like to see peripheral defocus lenses or orthoK with 0.025% or 0.05% atropine, especially as most of the current published research uses 0.01%. This is because concerns remain over the efficacy 0.01% in terms of axial length control.”
The future of myopia management will focus on customising the options available to maximise treatment efficacy.
“So, there's still a long way to go to understanding what the best options are,” Nam says.








Optometrists are adapting their myopia management strategies amid rising prevalence. With an increasing emphasis on the detection of pre-myopia, there has also been a growing consensus on the importance of integrating axial length measurement with traditional refractive error assessments. DR MONICA JONG examines the emerging standards of care in myopia management.
TABOUT THE AUTHOR:

Monica Jong PhD, BOptom, FBCLA
Visiting fellow UNSW, Sydney, Australia
Global director professional education myopia, Johnson & Johnson Medtech, Jacksonville, USA
Former executive director, International Myopia Institute Image: Monica Jong.
At the completion of this article, the reader should…
• Appreciate the importance of integrating axial length measurement into myopia management protocols for early detection and monitoring.
• Consider the implementation of the World Council of Optometry’s ‘three M’s’ approach (Mitigation, Measurement, Management) as a framework for evidence-based myopia care.
• Evaluate the clinical benefits and challenges of using axial length measurement in conjunction with traditional refractive error assessments.
he prevalence of myopia and high myopia is increasing around the world, and in some parts, it has already reached epidemic proportions.1 Thirty per cent of the global population is currently myopic, and by the year 2050, 50% will be myopic, and 10% highly myopic.
2
As a consequence of the increase in myopia and high myopia, there will be an increase in permanent sight-threatening ocular complications such as myopic macular degeneration (MMD), already a leading cause of vision impairment and blindness in parts of Europe and Asia.
3
Eyecare professionals will need to meet the challenge of an increasingly comprehensive eyecare service that detects and diagnoses, corrects and slows myopia, in order to help mitigate future visual impairment from progressive myopia. The costs from the lost productivity of uncorrected myopia, as well as permanent vision loss from MMD, alone totalled approximately $250 billion in the year 2015, 4 and it is set to rise in the future.
Currently, we have treatments to slow myopia progression, but we also need to consider prevention as that could lead to the greatest public health impact overall. Based on known risk factors for myopia and a proposed definition for pre-myopia by the International Myopia Institute, 5 a committee chaired by Professor Ian Flitcroft, we have a good basis to start evidence-based preventative myopia management.
‘Pre-myopia’ is a term understood to describe a patient with a nonmyopic refraction who has a combination of myopia risk factors and an observed pattern of eye growth that indicates a high risk of progression to myopia.
The International Myopia Institute (IMI) defines pre-myopia as “a refractive state of an eye of
≤ +0.75 D and > -0.50 D in children where a combination of baseline refraction, age, and other quantifiable risk factors provide a sufficient likelihood of the future development of myopia to merit preventative interventions”. 5
As the IMI notes, 5 most forms of myopia progress from onset for a variable period. Currently, reducing the rate of progression is a central goal of myopia research, but preventing the onset of myopia may be an even more valuable target.
As the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study has demonstrated, eyes destined to become myopic show an accelerated pattern of axial elongation several years before the onset of myopia. 6 But the best indicator of pre-myopia remains the baseline refraction – in other words, the level of refraction expected for age. For example, based on a multi ethnic study, a six-year-old should have at least +0.75 D of hyperopia otherwise they have pre-myopia. 7
Following a comprehensive eye examination where the optometrist has taken a thorough history, conducted cycloplegic refraction and ruled out any other ocular condition – and the patient is found to have less hyperopia than expected for their age with any of the risk factors below – then the patient can be considered ‘pre-myopic’.
• Ethnicity – we see a higher prevalence of myopia in certain ethnic groups. East and Southeast Asians have a higher prevalence of myopia compared with Europeans, Africans, and Indians.1
• Parental myopia – one myopic parent increases the risk three times, and two myopic parents increase the risk six times.7
• Red uced time outdoors and increased near work – clinical trials have reported that increasing additional time outdoors to at least
Myopia A condition in which the spherical equivalent refractive error (SER) is (more myopic than) ≤ -0.50 D when accommodation is fully relaxed
Low myopia A condition in which the SER of an eye is between -0.50 D and -5.75 D when accommodation is relaxed
High myopia A condition in which the SER of a myopic eye is -6.00 D or greater when ocular accommodation is relaxed ocular accommodation is relaxed
Pre-myopia A refractive state of between +0.75 D and -0.50 D in children where a combination of baseline refraction, age, and other quantifiable risk factors provide sufficient likelihood of the future myopia development to merit preventative interventions

120 minutes per day is protective against new cases of myopia 8, 9, 10 while intense near work is associated with increased risk of myopia.11,12
• U rban environment – those living in dense cities tend to have a higher risk than in rural or suburban settings,13 as urban environments are linked to less time spent outdoors and more near work activity.
Currently, there is no strong evidence to start optical and pharmacologic treatments in a pre-myope but we are seeing emerging studies in this so guidance may likely change in future. Regular yearly review as a minimum would be recommended for a child that is significantly at risk of developing myopia. (As discussed below, axial length measurement should be considered). For now, we should be advising increased time outdoors of at least 120 minutes daily (with sun protection) and reduced near-work to less than 2.5 hours per day.13 This advice should form part of the comprehensive management of a child with myopia too.
Much discussion has been directed about using axial length measurement as a critical measurement for myopia management. Measured in millimeters from the anterior cornea to the retinal pigment epithelium, axial length (AL) has emerged as the most significant contributor to refractive error and potential myopia-related visual impairment.14
Measurement of AL is objective, fast, accurate, and easily performed with many of the automated devices available on the market today. AL growth charts have been published for European15, 18 and Chinese15 children, and AL normative data is being used in various axial length biometers such as the Haag-Streit Lenstar Myopia and Oculus Myopia Master.
played a significant role in defining the myopia epidemic through its research and advocacy efforts and has been pivotal in redefining myopia as a public health issue. I have had a great opportunity to work with leaders in driving these initiatives, in particular the late Professor Brien Holden, Professors Serge Resnikoff and Earl Smith as well as partnering with the IAPB and World Health Organization and in the context of uncorrected refractive and accessibility which remains something that all industry partners can help to address collectively with their new innovations in this space.
Today, myopia can no longer be seen as a harmless refractive error with minimal long-term
“TRADITIONALLY, AL MEASUREMENT HASN’T BEEN MAINSTREAM IN OPTOMETRY. HOWEVER, AS OPTOMETRISTS WHO ROUTINELY USE OCTs KNOW, STANDARDS OF CARE AND THE ADOPTION OF NEW TECHNOLOGIES CAN, AND DO, EVOLVE RAPIDLY.”
Traditionally, AL measurement hasn’t been mainstream in optometry. However, as optometrists who routinely use OCTs know, standards of care and the adoption of new technologies can, and do, evolve rapidly. And just as OCTs revolutionised the management of ocular diseases in optometric practices, many are now considering integrating AL measurement into their myopia management protocols.
The benefits of AL measurements are significant although not mandatory to get started in myopia management:
• E stablishing baselines: baseline AL measurements allow us to track changes over time.
• Patient education: incorporating AL measurement data into discussions with parents, caregivers and patients about myopia severity, encouraging proactive involvement in their eye health.
As the clinical benefits of AL measurements expand, it is becoming helpful to integrate these data with established myopia risk factors. While it would be unwise to simply reduce ‘myopia management’ to ‘axial length management’,19 it is undeniable that the data derived from AL measurements will increasingly shape optometric decision-making in pre-myopia and myopia care.
To be clear: a comprehensive evaluation that includes refractive error assessments is still essential for accurate myopia diagnosis and personalised patient care. AL measurements augment, not replace, a comprehensive eye examination.
The Brien Holden Vision Institute (BHVI) has
impacts on eye health. Other organisations have followed suit. In 2021, The World Council of Optometry (WCO) unanimously adopted a resolution19 advising optometrists to “regularly and consistently offer scientifically proven myopia interventions within their practices”.
In the resolution, the WCO defined the ‘evidence-based standard of care for myopia’ as comprising of three main components, which they called the ‘three Ms’: 20
• M itigation
optometrists should educate and counsel pa rents and young patients, during early and regular eye exams, on lifestyle/dietary/other factors to prevent or delay onset of myopia.
• M easurement
optometrists evaluating the status of a patient during regular comprehensive vision and eye health exams, (including refractive error and AL measurements whenever possible).
• M anagement
optometrists addressing patients’ needs of today by correcting myopia, while also providing evidence-based interventions (e.g., contact lenses, spectacles, pharmaceuticals) that slow the progression of myopia, for improved quality of life and better eye health today and into the future.
The WCO’s resolution further recommended that optometrists adopt a standard of care that goes beyond vision correction to include patient education and early, frequent discussions with parents to explain:
• w hat myopia is
• lifestyle factors that may impact myopia
• the increased risks to long-term ocular health that myopia brings

• the available approaches that can be used to manage myopia and slow its progression.
In essence, this closes the debate on myopia which Brien Holden (et al.) launched as far back in 2015 when they argued that the time has come to change our understanding of myopia from merely as a benign refractive error to a condition with profound long-term implications for eye health worldwide. 21
Eyecare professionals have shifted from merely correcting vision and refractive errors to adopting evidence-based myopia management strategies. This includes educating patients on ways to prevent myopia and discussing research-backed management options to slow its progression.
Ultimately, an approach integrating clinical and lifestyle factors is essential for accurate diagnosis and optimal ongoing management of paediatric myopia. With myopia’s escalating prevalence comes a rise in severe ocular conditions like myopic macular degeneration, contributing significantly to economic costs and vision impairment. 3,4
All of us have the opportunity change a child’s life for the better today and in future. Being able to predict, manage and mitigate myopia and the risks of associated complications is something we all can do today.
REFERENCES
1. M organ IG, He M, Rose KA. EPIDEMIC OF PATHOLOGIC MYOPIA: What Can Laboratory Studies and Epidemiology Tell Us? Retina 2017;37:989-997.
2. H olden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036-1042.
3. H aarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW. The Complications of Myopia: A Review and Meta-Analysis. Invest Ophthalmol Vis Sci 2020;61:49.
4. N aidoo KS, Fricke TR, Frick KD, et al. Potential Lost Productivity Resulting from the Global Burden of Myopia: Systematic Review, Meta-analysis, and Modeling. Ophthalmology 2019; 126: 338-346.
5. F litcroft DI, He M, Jonas JB, et al. IMI – Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Invest Ophthalmol Vis Sci 2019;60:M20-M30.
6. M utti DO, Hayes JR, Mitchell GL, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007; 48: 2510–2519.
7. Z adnik K, Sinnott LT, Cotter SA, et al. Prediction of juvenile-onset myopia. JAMA Ophthalmol. 2015; 133: 683–689.
8. H e X, Sankaridurg P, Wang J, Chen J, Naduvilath T, He M, Zhu Z, Li W, Morgan IG, Xiong S, Zhu J, Zou H, Rose KA, Zhang B, Weng R, Resnikoff S, Xu X. Time Outdoors in Reducing Myopia: A School-Based Cluster Randomized Trial with Objective Monitoring of Outdoor Time and Light Intensity. Ophthalmology. 2022 Nov;129(11):1245-1254
9. Wu PC, Chen CT, Lin KK, Sun CC, Kuo CN, Huang HM, Poon YC, Yang ML, Chen CY, Huang JC, Wu PC, Yang IH, Yu HJ, Fang PC, Tsai CL, Chiou ST, Yang YH. Myopia Prevention and Outdoor Light Intensity in a School-Based Cluster Randomized Trial. Ophthalmology. 2018 Aug;125(8):1239-1250.
10. Wu PC, Chen CT, Lin KK, et al. Myopia Prevention and Outdoor Light Intensity in a School-Based Cluster Randomized Trial. Ophthalmology 2018;125:1239-1250.
11. H uang HM, Chang DS, Wu PC. The Association between Near Work Activities and Myopia in Children-A Systematic Review and Meta-Analysis. PLoS One 2015;10:e0140419.
12. M organ IG, Wu PC, Ostrin LA, Tideman JWL, Yam JC, Lan W, Baraas RC, He X, Sankaridurg P, Saw SM, French AN, Rose KA, Guggenheim JA. IMI Risk Factors for Myopia. Invest Ophthalmol Vis Sci. 2021 Apr 28;62(5):3. doi: 10.1167/ iovs.62.5.3.
13. L anca C, Saw SM. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol Opt 2020;40:216-229.
14. T ideman, J.W., et al., Association of AL with Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol, 2016. 134(12): p. 1355-1363.
15. S aw SM, Hong RZ, Zhang MZ, et al. Near-work activity and myopia in rural and urban schoolchildren in China. J Pediatr Ophthalmol Strabismus 2001;38:149-155.
16. G ifford KL, Richdale K, Kang P, et al. IMI – Clinical Management Guidelines Report. Invest Ophthalmol Vis Sci 2019;60:M184-M203.
17. T ideman JWL, Polling JR, Jaddoe VWV, Vingerling JR, Klaver CCW. Environmental Risk Factors Can Reduce AL Elongation and Myopia Incidence in 6- to 9-Year-Old Children. Ophthalmol ogy 2019;126:127-136.
18. S anz Diez P, Yang LH, Lu MX, Wahl S, Ohlendorf A. Growth curves of myopia-related parameters to clinically monitor the refractive development in Chinese schoolchildren. Graefes Arch Clin Exp Ophthalmol 2019;257:1045-1053.
19. S hould myopia management be renamed as AL management? [Internet]. The New Optometrist. [cited 2024 Jul 14]. Available from: https://www.thenewoptometrist.com/features/thecase-for-axial-length-measurement
20. R esolution: The Standard of Care for Myopia Management by Optometrists - World Council of Optometry [Internet]. 2021 [cited 2024 Jul 14]. Available from: https://worldcouncilofoptometry.info/resolution-the-standard-of-care-for-myopia-management-by-optometrists
2 1. H olden BA, Wilson DA, Jong M, Sankaridurg P, Fricke TR, Smith EL III, Resnikoff S. Myopia: a growing global problem with sight-threatening complications. Community Eye Health. 2015;28(90):35. PMID: 26692649; PMCID: PMC4675264.

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.

NORM
Rodenstock’s AI technology and data from over 500,000+ biometric eye scans, develops a detailed model of each eye. This personalized approach ensures sharper vision for your patients.

There is a critical need for early myopia intervention in young children. DR JOSEPH PAUL discusses the prevalence of child myopia in Australia and New Zealand from one of the most up-to-date datasets and the role optometrists play in recommending lifestyle-led management options, proven to slow progression and minimise the risk of more serious conditions.
In recent years, there has been a concerning prevalence of short-sightedness in Australian and New Zealand children. A Specsavers 2022 retrospective review of more than three million deidentified patient records aged 18 and under showed child myopia detection rates had increased to 28.8% in Australia and remained as high as 29.8% in New Zealand.1 This review also found that the age at which patients were being diagnosed with myopia was decreasing. In the UK, studies have found similar results and show that the typical onset of myopia occurs in children aged between six and nine, and its progression is most rapid under 10 years of age.2
When a child’s distance vision is blurry, it affects their ability to focus at school and engage in classroom lessons. This condition can prevent them from seeing the teacher or front of the room clearly and fully participating in activities requiring medium to long-range vision. Myopia can impact the child’s learning and have short- and long-term effects on quality of life. In addition to visual impacts, if not detected early and managed with proven therapeutic interventions, progressive myopia greatly increases the lifetime risk of potentially blinding eye disease. 3,4
Regular eye examinations are crucial for the early detection of myopia in children, and as accessible eye health professionals, optometrists play a central role in myopia management in the community. A range of evidence-based management options are available that have been clinically proven to provide clear vision and slow the progression of myopia into severe nearsightedness or high myopia. However, these interventions must be implemented early to have the most effect.
Research and technology into new strategies for myopia control continue to advance. Therapeutic interventions in the form of spectacle lenses,
MiSight contact lenses, and low-dose atropine eyedrops provide a range of proven methods for proactively managing myopia in children while slowing the rate of progression.
The spectacle lens uses non-invasive technology to correct vision and manage myopia simultaneously. Studies have shown that MiYOSMART lenses can effectively slow myopia progression by up to 60%, 5 making it a valuable tool in preventative eyecare for children. Contact lenses may be preferable over spectacles when a child has an overtly active lifestyle.
Suitable for kids as young as eight,6 MiSight contact lenses are fitting for those playing contact sports or energetic activities and provide a convenient and effective solution for improved sight. The daily disposable lenses are specifically designed to correct vision while slowing the progression of myopia by more than half.7 MiSight lenses encourage normal eye growth and reduce the elongation associated with myopia development, effectively mitigating the risks associated with high myopia as an adult.
Likewise, atropine eye drops are another useful management option for the control of child myopia. In an Australian clinical trial, they were shown to be a safe and effective myopia-control approach, with a 35% effect in slowing down myopia progression and 33% in slowing down eye growth after 18 months of treatment. 8
According to Specsavers national optometry data, between 20-25% of myopic kids in Australia and New Zealand are in a form of myopia management, whether that is therapeutic spectacle lenses, contact lenses or low-dose atropine eyedrops. 9 Many factors play into a patient’s decision to adopt or delay the use of a therapeutic myopia intervention. It is likely a mix of financial, lifestyle, and awareness aspects that contribute to myopic

children leaving optometry practices without a management solution. While all myopia management options require some level of investment, the costs can be managed effectively. Eye drops and contact lenses are spread across ongoing orders, while spectacle lenses often have a higher initial expense but offer an effective cost-per-wear option. Each solution boasts unique lifestyle benefits, and it is therefore essential for optometrists to discuss the pros and cons with families to help them select the right intervention, with personalised recommendations tailored to the child’s hobbies and lifestyle.
A parent’s awareness and understanding of myopia and its progression are fundamental to how receptive they are to early vision intervention. To ensure informed decisions, optometrists must take the time to thoroughly explain the condition, its impact on the child’s vision, and, if not managed appropriately, the potential eye health risks in the future. Ensuring the patient and their family are informed about the right therapy for the child’s lifestyle is crucial. In this way, optometrists play a pivotal role in tackling the growing prevalence of myopia in Australia and New Zealand. The proactive adoption of myopia management strategies will enhance the patient’s immediate visual acuity and enable other associated social and health benefits, including improved quality-of-life. Offering patient-centric, lifestyle-led management recommendations now has the power to reduce instances of more severe vision-impacting conditions in the future.

REFERENCES:
“A parent’s awareness and understanding of myopia and its progression are fundamental to how receptive they are to early vision intervention.”
ABOUT THE AUTHOR: Dr Joseph Paul is the head of professional services at Specsavers ANZ where he provides clinical and professional support to optometrists across Australia and New Zealand. He holds a PhD in glaucoma research and has extensive experience as a postdoctoral researcher at the Centre for Eye Research Australia. During the past decade, he has also practised as an optometrist at Specsavers and in private practice.
1. S pecsavers ANZ Patient Outcomes Database. [Data file]. Specsavers, Melbourne, 2024. [accessed 15 June 2024]
2. M cCullough SJ, O’Donoghue L, Saunders KJ. Six year refractive change among white children and young adults: evidence for significant increase in myopia among white UK children. PLoS One. 2016;11(1):e0146332. doi:10.1371/journal.pone.0146332
3. O ptometry Australia. The Australia and New Zealand Child Myopia Report 2022/23. Reducing the Risk to Vision. Available https://www.optometry.org.au/wp-content/uploads/National_ news_images/2022/November/Reducing-the-Risk-to-Vision_Myopia-Report-202223.pdf [Accessed 15 July]
4. T iedeman et al. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia JAMA Ophthalmol. 2016 Dec 1;134(12):1355-1363.
5. L am CSY, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363-8. DOI: 10.1136/bjophthalmol-2018-313739.
6. C hamberlain P, et al. A 3-year randomized clinical trial of MiSight® lenses for myopia control. Optom Vis Sci. 2019; 96(8):556-567.
7. B ack A, Chamberlain P, et al. Clinical Evaluation of a Dual-Focus Myopia Control 1 Day Soft Contact Lens – 2-Year Results. Paper presented at the annual meeting of The American Academy of Optometry. November 9, 2016; Anaheim, California USA.
8. S amantha Sze-Yee Lee PhD, Gareth Lingham PhD, Low-concentration atropine eye drops for myopia control in a multi-racial cohort of Australian children: A randomised clinical trial. Clinical & Experimental Ophthalmology. Volume 50, Issue 9. P 1001-1012
9. S pecsavers ANZ Patient Outcomes Database. [Data file]. Specsavers, Melbourne, 2024. [accessed 15 June 2024]
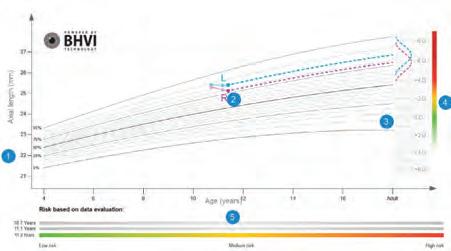

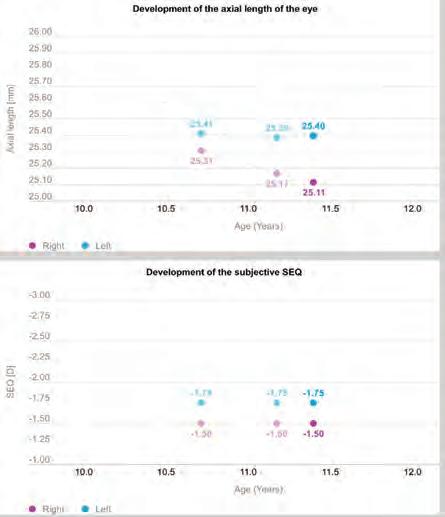

OCULUS is building on the program driving its Myopia Master device, helping Australian eyecare professionals to now understand whether a child’s progression is abnormal or not. The management software is also becoming more widely available to Pentacam AXL Wave users.
Myopia induces short-sightedness, often caused by an elongation of the eye that undermines a person’s distance vision and can create an uncertain future for their eye health. Eyecare professionals know this well, and many are now dealing with the consequences of this condition more regularly and in growing numbers.
But what they are now understanding to a greater degree is one of the most powerful ways to combat myopia – and potentially sight-threatening incidents later down the track – is to take a good look into the d istance, into the future of how a patient’s disease may progress and ways this can be curbed.
To do that, many Australian optometrists are discovering how to master it with the support of biometers with myopia management capability. It is important business because the numbers are well-known and sobering: for Australia and New Zealand currently 36% of the population is estimated to be affected which is forecast to reach 55% by 2050. Furthermore, Australia is expected to have 4.1 million high myopes by then, unless management is widely implemented.
But new technology is providing those professionals with more and better tools so they can be fully informed in their management of myopic patients.
Mr Richard White is regional director for OCULUS Asia. Many
Australian optometrists will know about the German company’s Myopia Master device that screens for myopia, helps determine why a patient might be myopic and predicts progression. It also assists in planning for treatment, monitoring its performance over time, and can now decipher if a child’s progression is normal/abnormal.
When the manufacturer first considered the myopia problem, White says OCULUS was quick to acknowledge it needed a dedicated device, rather than adapting a pre-existing technology.
“Myopia is a refractive issue, so we knew we wanted to include refractive screening to find out whether the patient is actually myopic or not myopic,” he says. “The second part is determining why are they are myopic by looking at a few different parameters: refraction, axial length, and the keratometry. By combining these important factors in myopia, we’re able to bring three into one.”
Beyond the hardware, the Myopia Master stands out for the software that helps the eyecare professional: perform objective data analysis, learn more about environmental factors impacting the individual, prepare an evaluation-based treatment recommendation and monitor treatment success.
Importantly, OCULUS is making this capability more widely available on the company’s Pentacam AXL Wave machines. This means practitioners already with this instrument – many whom offer an advanced contact lens service – don’t need to invest in an additional piece of hardware for myopia management. It fits nicely for practitioners offering orthokeratology for myopia, and will also be a welcome addition for ophthalmologists with this instrument.
The key to these advances is access to and use of data, says White.
One of the standout features, he says, is the fact OCULUS has teamed up with the Sydney-based Brien Holden Vision Institute (BHVI) to create growth curves, including ones that are region specific for Asian eyes, and for every age group.
That data is compared with raw data from the patient’s eye, allowing the practitioner to see where the subject sits in relation to axial length and subsequent myopia compared to normative values. That gives a valuable snapshot but also a glimpse into the patient’s future eye health and potential myopia, highlighting the consequences without intervention and treatment.
At the end of the exam, patient and parent receive a report to help them understand the disease itself, and the importance of treatment and follow-up appointments.
OCULUS has continued to evolve the software and earlier in 2024 rolled out a Growth Control module specifically aimed at analysis of whether a patient’s axial elongation is abnormal, borderline or normal – especially useful once treatment has been initiated to gauge its effectiveness.
The way this is displayed shows the ‘axial length growth rate’ split into red, orange or green bands. As the optometrist introduces a treatment, they can mark this up in the program, and clearly see over time whether

“One of the key things that we have always said about Myopia Master is that it’s like a myopia clinic straight out of the box – refraction, keratometry and axial length.”
Cameron Loveless Designs For Vision
it is effective (for example the patient progresses from the red band, to the orange band then to the green band).
“So from one exam to another exam, we can decide whether that’s normal or abnormal growth,” White says. “That’s when you can also see if the treatment is working or not working.”
All of this together gives patients confidence and peace of mind.
“One piece of feedback I received from an Australian eyecare professional was that when the patients come in and they see the Myopia Master machine, it gives them confidence in the practitioner and the practice; it shows them that we’ve invested in them and their eye health.”
It’s a confidence that Mr Cameron Loveless understands.
His company, Designs For Vision, is OCULUS’ sales and distribution partner in Australia and New Zealand. But that’s not the only reason why he confidently promotes the equipment.

“One of the key things that we have always said about Myopia Master is that it’s like a myopia clinic straight out of the box – refraction, keratometry and axial length,” he says.
“The other big thing is that it is backed by BHVI, and that’s pretty huge.
"There’s a lot of people pulling data from freely available sources and using that in their databases to compare eyes, but some – even the well-known studies – were done on the measurements of axial length using different devices and methods, but that’s not the case with the BHVI data.”

The new Growth Control module is free for existing users with a software update. It augments the traditional growth curves to indicate whether the child’s progression with treatment is normal/abnormal. For the growth in section one (untreated), two eyes are plotted in the pink section showing abnormal growth (red arrow). Then treated with orthoK, the growth is plotted in the yellow section (borderline abnormal growth). In section three, where orthoK was modified, the growth has dropped into the green zone (normal growth).
Loveless says optometrists are getting value out of another optional module within the Myopia Master, called GRAS (Gullstrand Refractive Analysis System). It compares the patient’s measured data to a theoretical emmetropic eye, modified to match the patient’s age using BHVI’s extensive data. It uncovers where the myopic tendency is coming from: axial length, keratometry and the crystalline lens/ accommodation.
“It gets right into the nitty gritty, so optometrists don’t need to research for themselves what a normal curvature of the cornea should be for example,” he says.
“When it reveals the axial length is too long for their age, that’s the cue for the optometrists to initiate discussions about treatment with the parent,” he says. “On the flip side, you might see someone who doesn’t seem to have axial length-related myopia, which is great news for the child, but let’s keep an eye on it.”
Loveless believes the equipment, including the regular free software upgrades, would be an ideal addition to any optometry practice, but especially independents keen to offer a high-end point-of-difference,
and less experienced practitioners wanting to professionalise their myopia service.
Among the high-profile optometrists using Myopia Master are Sydney-based Mr Oliver Woo, the first in Asia-Pacific to have one installed, and Melbourne myopia expert Mr Philip Cheng. Sydney’s Mr Jim Kokkinakis is also a user but will be trading in his Myopia Master and purchasing a Pentacam AXL Wave so that he can use it for both his contact lens work and myopia management, saving space.
Given the surge in myopia globally, White says taking it seriously through investment in technology and treatments can be a great practice builder. They are patients requiring ongoing treatment and support.
“You want to keep that patient with you and build that relationship,” he says.
“If you’re not getting active in myopia management, with the lifestyles of children today, with their iPads and so on, with the increased risk of glaucoma, retinal detachments, of cataract, how much have you really taken care of them?”
Innovative Myo-freeform technology that offers the next generation of managing childhood myopia.

Central viewing zone
Allows for clear and sharp vision for enhanced comfort, all the while sustaining a harmonious equilibrium with the treatment zone.
Peripheral treatment zone
Offers a more optimal and targeted treatment option as it takes into consideration the asymmetry of the back of the eye.*
Reading addition
Helps to relax the eyes when performing near-work tasks. The smooth transition enhances comfortability and improves compliance.
Remarkably thinner Slim and aesthetically pleasing appearance.
hub.crlabs.au/myome-ecp


With MyCon, Rodenstock developed a solution to control the progression of myopia in children, and now, with MyCon 2, the company is going a step further by including the four individual position-of-wear parameters.
According to the lens manufacturer, MyCon 2 lenses offer improved imaging properties by customising the lens to the fit of the frame and thus to the child’s unique face. This approach includes the four individual wearing parameters, the pupil distance (PD), the pantoscopic tilt (PT), the corneal vertex distance (CVD) and the face form angle (FFA), which help to adapt the lens even more precisely. By using these parameters, “improved imaging properties can be achieved in the focus area of the lens while maintaining the effect of myopia control in the periphery”.
Rodenstock MyCon 2 lenses are available in index 1.5, 1.6, 1.67, and 1.74 in clear, tinted, polarised & ColorMatic which make the lenses both thinner and sleeker than many other myopia lenses on the market and well suited to high prescriptions, Rodenstock says.
Contact: (02) 9748 0988
ZEISS MyoCare lenses, released locally in 2023, are created on the basis of simultaneous competing blur, including a clear central zone and intermittent treatment rings within the functional zone of the lens. The distinctive freeform back surface, ZEISS ClearFocus Design, is designed to prevent hyperopic defocus for all directions of gaze.

During the recent Association for Research in Vision and Ophthalmology (ARVO) 2024 conference, ZEISS presented results from two ongoing multi-centre trials in China and Europe.
“We observed that the use of ZEISS MyoCare lenses significantly slowed progression of myopia when compared to single vision lenses. After 12 months of lens wear, the difference in myopia progression in Asian children with ZEISS MyoCare compared to single vision was SE: 0.31D and AL:0.13mm. The data represents a comprehensive evaluation of ZEISS MyoCare across multiple sites involving large samples and ethnic groups,” the company says.
“We are excited to announce that in addition to our six-month unconditional warranty, we have also expanded our product range from 1.5, 1.59 and 1.6 to now include the 1.67 index.”
Contact: visioncare.au@zeiss.com

With axial length being the critical measurement in myopia management, the Myopia Expert 700 delivers a gold standard, non-invasive axial length measurement to help guide myopia management solutions and provide ongoing control.
Additionally, the instrument has a complete set of measurements for all myopia solutions. Covering the full spectrum, the Myopia Expert 700 captures key measurements necessary for the application of different myopia solutions, allowing the practitioner to recommend the optimum control solution to the patient.
These include: corneal topography, keratometry, fluorescein, pupillometry and white-to-white measurement.
Myopia Expert 700 is manufacturered by Essilor Instruments and is supplied to Australian practitioners through OptiMed.
Contact: sales@optimed.com.au
The MyoStock lens, launched by CR Labs in February 2024, is designed to combat myopia progression with Hexagon Implicated Defocus Segment (HIDS) technology.
It features a central clear viewing zone surrounded by hexagonal segments, which help slow eye elongation and reduce myopia progression.
“An in-house study shows a 45% decrease in myopia progression and a 53% reduction in axial elongation in children wearing MyoStock lenses,” CR says.

“With a thinner, aspheric design and blue light filter, MyoStock lenses offer superior aesthetics and comfort and competitive price point, making them an ideal choice for managing myopia.”
MyoStock also comes equipped with ultra-super, hydrophobic (USH) coating, making it resistant to fingerprints, oils, and scratches, and providing hydrophobic properties for easy maintenance.
Contact: info@crlabs.au
The Myopia Software available in the OCULUS Myopia Master has been expanded to work with the Pentacam AXL Wave, offering several key benefits for myopia detection and management.According to Designs For Vision, part of ParagonCare and the Australian and New Zealand distributor of this technology, it offers increased flexibility, with the software now able to process data from both devices. There’s also data exchange advantages, with the capability to share existing data between the two devices, improving efficiency in daily clinical work. Other features include:

• Comprehensive myopia package: Myopia Package combines crucial parameters to simplify myopia detection and management.
• Personalised risk assessment: the software incorporates the latest BHVI data to estimate future myopia progression based on individual factors such as age, gender, and ethnicity.
• Patient education support: software generates personalised reports detailing current myopia status and potential future outcomes, which can be used to educate patients about their condition.
• Improved reliability: by combining data from multiple sources and incorporating the latest research, the software offers more reliable myopia detection and management tools.
“This expanded functionality of the Myopia Software, along with its integration with the Pentacam AXL Wave, provides eyecare professionals with a more comprehensive and flexible toolset for managing myopia in their patients. The ability to exchange data between devices and generate personalised reports based on the latest research enhances the overall efficiency and effectiveness of myopia care," DFV says.
Contact: 1800 225 307
A five-year clinical study of the Essilor Stellest lenses has demonstrated continued long-term efficacy in controlling myopia progression and axial elongation.
The controlled, prospective, randomised clinical trial which began in 2018 was conducted at the Eye Hospital of Wenzhou Medical University in Wenzhou, China.
Optos says its Daytona device produces a 200° single-capture optomap retinal image of unrivalled clarity in less than ½ second. This fast, easy, patient friendly, ultra-widefield (UWF) imaging technology was designed for healthy eye screening and has been shown to improve practice flow and patient engagement.
Enhances Clinical
Decision-making: Evaluation of the peripheral retina is critical for optimal patient management. optomap imaging is ideal for peripheral examinations. Published studies comparing field-of-view and clinical utility of various widefield imaging systems confirm optomap captures the widest clinically usable field of view and the most retinal pathology, Optos says.

Improves Practice Efficiency and Economics: Studies show that optomap images are faster to capture and easier to review than traditional patient examination techniques. optomap enables practitioners to differentiate their practice and add an additional revenue stream.
Contact: auinfo@optos.com

The age of the children at enrolment in 2018 was eight to 13 years old. To assess the long-term efficacy, the study was extended from the original two-year clinical trial to five years.
The data showed that Essilor Stellest lenses slowed myopia progression by 1.75D*1 and axial elongation by 0.72mm**1 on average over five years for all subjects, compared to the extrapolated control group, showing conclusive evidence of their efficacy in slowing down myopia progression in children in the fifth year.
The data also showed that the efficacy in slowing myopia progression and axial elongation was sustained in older children (up to 18 years old), as the children who completed the fifth-year study were aged between 13-18 years.
It is planned to continue the study for two more years, to gauge the seven-year myopia control efficacy of the lens.
NOTE: References available upon request.
Contact: marketing@essilor.com.au
The Eyerising Myopia Management Device is described by its manufacturer as a cutting-edge solution specifically designed for myopia management using low-level red-light technology.
Developed by Australian-based Eyerising International, it “delivers safe, non-invasive light therapy to the eyes, stimulating blood flow, which in turn thickens the choroid layer in patients with myopia”.
“This innovative treatment has shown promising results in slowing the progression of myopia in children aged three to 16 years old,” the company says.

“The device is user-friendly, with a design and security features that make the treatment convenient for home use.”
The therapy requires two sessions per day, each lasting three minutes, making it simple to incorporate into daily routines without disruption, Eyerising International says.
“Backed by extensive research and clinical studies, Eyerising Myopia Management Device offers a scientifically validated approach to managing myopia, reducing the need for more invasive treatments,” it says. “This therapy provides an effective strategy for myopia management in your practice.”
Contact: info@eyerisinginternational.com



This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at https://www.tga.gov.au/reporting-problems.
MiYOSMART provides a robust and wide spectrum of evidence, empowering eyecare professionals to meet the needs of diverse patients with confidence, HOYA says.
The award winning 1-3 spectacle lenses have been shown to slow myopia progression by 60% in children aged 8 to 13, 4 the company says.
Also, the findings of the six-year, long-term follow-up study showed the MiYOSMART spectacle lens myopia control effect is sustained over time for children wearing the lens, with an average cumulative myopia progression less than 1.00D and axial elongation 0.6 mm over six years in children that wore MiYOSMART for the duration of the study, 5 according to HOYA.

The meridia advanced corneal topographer generates high-quality, reliable and precise topography maps – the key to successful orthokeratology (orthoK) design and fitting. Unlike other topographers that extrapolate data, it provides the practitioner with real topography data from limbus-to-limbus.
Proprietary composite topography capture provides users with a complete view of the cornea for utmost confidence in your orthoK lens design.
“It also confirmed that patients who stop wearing the MiYOSMART spectacle lens show no rebound effects,” 5 HOYA says.
MiYOSMART is available in clear and sun options. MiYOSMART
The recently-released MiYOSMART Chameleon, photochromic spectacle lenses, are said to be the ideal all-in-one myopia solution. Rapidly adapting to the levels of sunlight, it provides children with as much protection as they need at any time and place .6,7,8
Meanwhile, MiYOSMART Sunbird, HOYA’s polarised spectacle lenses, are the ideal addition to MiYOSMART clear spectacle lenses for extra protection from intense sunlight and glare, 7,10 the company says.
NOTE: References available upon request. Contact: ulli.hentschel@hoya.com

MiSight 1 day from CooperVision remains the only contact lens with US FDA approval for slowing the progression of childhood myopia.
The range covers -0.25D to -10.00D (0.50D steps after -6.00D) – which means it covers 99.97% of prescriptions for Asian children, and 99.97% for Caucasian children who have myopia and less than 1D of astigmatism,1 the company says.
MiSight 1 day contact lenses are also said to be backed by the longest-running soft contact lens study among children.
“This extraordinary study, also confirmed the overwhelming preference children have for contact lenses, giving optometrists the evidence to support their decision-making and parental conversations,” CooperVision says.
Reference:
CVI Data on file, 2022. SERE coverage of childhood myopia prescriptions with MiSight 1 day for 104,810 eyes in Asia (China, Korea) and 116,336 eyes in Europe and USA aged 8-18 years. Contact: cs@au.coopervision.com

“Achieve the perfect fit in the way that suits you best with the meridia’s convenient lens design options. Use the effortless contact lens simulator, integrate with custom lens design software such as EyeSpace and WAVE, or send your data to your contact lens lab so they can design the lens for you,” manufacturer Medmont states.
“Assess and document fit at a glance with the meridia’s easy-to-interpret subtractive map function and powerful fluorescein imaging and video.”
The meridia is considered an indispensable tool for determining orthoK candidacy, designing lenses, evaluating fit and achieving quick orthoK lens success for myopia patients.
Contact: info@medmont.com
B-OCT is an innovative method of using the Optopol REVO OCT device to measure ocular structure along eye axis. OCT biometry provides a complete set of biometry parameters: axial length, central cornea thickness, anterior chamber depth and lens thickness.
B-OCT is a software licence feature for the ‘REVO’ OCT available through OptiMed. It is considered an ideal tool for myopia control, with many Australian myopia management key opinion leaders successfully using this technology. All measurement callipers are shown on all boundaries of OCT images provided by REVO. Now, practitioners can visually verify, identify and, if required, make corrections as to which structure of the eye has been measured. With a simple cursor shift, it is possible to precisely set boundaries for every patient.

From now, ECPs can eliminate the common uncertainty as to how most optical biometers classify the boundaries in non-typical patients.
• 3 mm scan allows precise evaluation of retinal conditions
• 5 μm resolution gives the highest level of detail.
The REVO Biometry licence was recently updated to include progression analysis (retrospective data enabled) to provide a powerful management software package that includes normative database. Choroidal thickness evaluation will be available in the next software release, to help better evaluate treatment effectiveness. Contact: sales@optimed.com.au

Eikance 0.01%, the first pharmacotherapy registered on the Australian Register of Therapeutic Goods to slow the progression of myopia in children aged 4 – 14 years1#, may be initiated in children when myopia progresses ≥-1.0 D per year.1
EIKANCE 0.01% single-use ampoules are sealed in foil pouches and are available in packs of 30 x 0.3 mL ampoules. The ophthalmic solution is sterile and preservative-free. EIKANCE 0.01% is a prescription only medicine available at community pharmacies across Australia.
PBS information: This product is not listed on the PBS.
Before prescribing, review full Product Information accessed via www.tga. gov.au/resources/artg/331960
NOTE: This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at www.tga.gov.au/reporting-problems
Reference:
1.Eikance Approved Product Information
# Australian Register of Therapeutic Goods. Accessed: 11 March 2024. Aspen Australia, St Leonards NSW 2065. AU-ATR-032024-08305
Contact: customerservice@aspenpharmacare.com.au

MyoME, available through CR Labs, is a lens designed using ‘Myo Freeform’ technology and offers an exciting approach to managing the silent pandemic of childhood myopia, the company says.
According to CR, MyoMe is a peripheral defocus lens with a near addition. The lens is composed of a clear central zone. The nasal and temporal side of the lens incorporates areas of asymmetrical positive defocus to ensure light is focused in front of the retinal plane, effectively preventing axial elongation, and slowing down myopia progression.

A 2024 clinical trial investigated the efficacy of the MyoME lens in European children with myopia. The study found that at the 12-month review, MyoME had reduced axial elongation by 39%, in comparison to children wearing single vision lens,1 the company states.
“MyoME is the myopia management lens that has been developed and tested. Its freeform technology incorporates the research behind peripheral myopic defocus and asymmetric defocus to reduce axial elongation and slow down myopia progression,” CR says.
Reference:
1. Sánchez-Tena, Miguel Ángel, et al. “Effectiveness of a Spectacle Lens with a Specific Asymmetric Myopic Peripheral Defocus: 12-Month Results in a Spanish Population.” Children 11.2 (2024): 177.
Contact: info@crlabs.au
Large cone corneal topographers often rely on extrapolated (estimated) data at the peripheral cornea. But that’s where large contact lenses land.
Fast-track first-fit success with a more accurate baseline map built from real corneal data.
The Medmont Meridia™ uses a high-precision small cone design to give you extreme corneal coverage. Get up to 11mm+ in a single automatic capture and 13mm+ with ‘Composite Topography’.
Scan to see how the Meridia™ supports first-fit success >

Call Jason to learn how Medmont can support your practice success: 0419 889 086.





At every stage of lens design evolution, HOYA has made its presence felt, leaving an indelible mark. As the company celebrates its 50th year in Australia, managing director CRAIG CHICK hints at what’s still to come.
Since HOYA Lens Australia opened its doors in Surry Hills, Sydney, in 1974, it has played a pivotal role in shaping the industry. Now, five decades later, it has no intentions of changing course.
A modern-day lens product is composed of three key aspects: the design, the coating, and the material. HOYA Lens Australia managing director Mr Craig Chick says the company has driven innovation on all these fronts. “Historically, we have been at the forefront at each of these technologies.”
With the industry standing on the brink of a new era in lens technology, he says the company has been riding the ebbs and flows of a market in constant flux, while foreseeing industry needs to catalyse a technological evolution.
Throughout its half-a-century history, the strength of the company, according to Chick, is defined by its relationship with optometrists, and its responsiveness to industry demands.
For example, HOYA was among the first to put power on to the front and the back surface of the lens with its freeform technology. And a significant breakthrough occurring in the late 1980s was the introduction of high-index glass lenses such as the Hoya THI -2, 1.80. This provided thinner and lighter options for high prescriptions – at this time, with a high prescription, there was a trade-off between thickness and weight.
With coating technologies, Chick says the company’s contributions have
been “revolutionary”. This includes high quartz coating – the first multicoat on plastic lenses – and double-sided hard coating which was said to have significantly improved lens durability.
And in the new millennium, Chick says HOYA’s Diamond Meiryo coating “set a new standard with its extreme durability, and longer lasting clarity”.
The company has consistently stayed ahead in lens technology through incremental advances, vigilance, and proactive innovation.
“We’re always looking at how we can improve lens designs,” Chick says.
Reflective of the company’s ability to stay ahead of the curve, and one of the most significant advancements HOYA has introduced in recent years, is the MiYOSMART lens launched in Australia and New Zealand in 2020. Many of the major lens companies have since launched their own myopia spectacle lenses.
“This revolutionary product was the first of its kind outside the Asia-Pacific region and has made a substantial impact on myopia management globally,” Chick says.
Chick highlights the importance of the MiYOSMART lens in the ongoing battle against myopia as the product is at the forefront of the fight. The lens has been shown to slow myopia progression by 60% in children aged eight to 13. It’s now backed by a six-year, long-term follow-up study showing that its myopia control effect is sustained over time for children wearing the lens, with an average


“Looking ahead, HOYA remains committed to innovation and excellence, poised for another 50 years of success in the optical industry.”

Uniquely, Australia was one of the first locations outside of Japan to open a HOYA lab.
“When HOYA made that decision to start to expand, the Australian market was well received. And even in 1974, it was quite a mature, and good value market,” he says. “As the first non-Asian country with a HOYA lab, this was a step forward.”
Today, the Australian market remains an important part of HOYA’s global business, with highly trained and well-regarded optometrists.
Craig Chick HOYA Lens Australia
cumulative myopia progression less than 1.00D and axial elongation of 0.6 mm over six years in children that wore MiYOSMART for the duration of the study.
HOYA has also confirmed that patients who stop wearing the MiYOSMART
“We’re very proud of this product, and with the clinical trials and the clinical results it has delivered,” Chick says. “In fact, I would argue with that design and the technology that’s gone into it has created a completely new segment.”
For HOYA, the key to staying ahead of the curve is adhering to its core values of collaboration, appreciation, respect, excellence, and social responsibility. Chick says these have been maintained through a clear commitment from the
“It starts from me and our corporate CEO and travels all throughout our employee structure. It’s something we discuss regularly. We have certain people within our organisation who are champions for certain aspects of those collaborations,” he says.
“The values are something that we live by. You have to be really careful with this, because they’re easy to say, but they’re not always easy to do.”
Beyond setting new market trends, Chick says HOYA’s robust presence in the country was pivotal in advancing lens design and strengthening its relationship with optometrists.
He says infrastructure in each corner of the country gives the company a ‘local presence’.
“Apart from opening our doors in 1974, the next biggest thing was the evolution in 1994 of constructing our own laboratory. The setup of our infrastructure, with an office in every state and a customer service team in every state, was a significant thing,” Chick says.
“Our service levels are well regarded, and the fact that we have fitting and mounting in each state creates that local point.”
“The fact that they can prescribe ophthalmic lenses, contact lenses, and therapeutic drugs is unique. And products are sold on the benefits, not as a commodity,” Chick says.
Regarding the future of lens design, HOYA expects to make as big an impact as it has historically such as setting an environmental precedence through its One Vision program.
The program is defined by three essential pillars: environmental sustainability, community outreach, and ensuring a happy, healthy, and thriving workplace.
One of the program’s key environmental goals is to achieve carbon neutrality in operations within the next 10 years and to be powered by 100% renewable energy by 2040.
The company has made strides toward this goal, as evidenced by the recent installation of a 2.7 MWh solar system at its major factory in Bangkok and exploration of ways to upcycle manufacturing waste into other products and implement more sustainable packaging.
For example, HOYA’s Sydney lab switched to dry-cutting machines, which eliminates water usage in lens manufacturing.
“Lenses are an interesting product because they are predominantly plastic, even though the resins may vary,” Chick says.
On the technological front, HOYA says there is potential to integrate data collected from its measurement devices with lens manufacture, for product optimisation and precision.
“Our measurement device – visuReal MasterAI – uses AI technology for precise frame fitting. The next stage is then the incorporation of that data into the manufacturing of the lens, and taking into account certain measurements that currently really aren’t being used,” Chick says. “We expect 2025 to be an exciting year, as we introduce things we haven’t done before.”
Above all, Chick says HOYA’s enduring success can be attributed to its team.
“The company boasts a wealth of experience and a strong organisational culture. This stability has been instrumental in maintaining HOYA’s high standards and continuous innovation,” he says.
“Looking ahead, HOYA remains committed to innovation and excellence, poised for another 50 years of success in the optical industry.”
































Functional vision continues to decline as lesions grow, even when visual acuity remains unchanged.1-5
At Apellis, our goal is to bring to market a treatment for geographic atrophy (GA).
To learn more about GA and its impact, scan here

Vision impairment due to geographic atrophy may vary.
References:
1. Boyer DS, et al. Retina. 2017;37(5):819-835.
2. Sunness JS, et al. Ophthalmology. 1997;104(10):1677-1691.
3. Sunness JS, et al. Ophthalmology. 1996;103(9):1458-1466.
4. Sunness JS, et al. Am J Ophthalmol. 2005;140(6):1085-1093.
5. Sunness JS, et al. Ophthalmology. 2007;114(2):271-277.
Apellis Australia Pty Ltd, L3, 141 Camberwell Rd. Hawthorn East, VIC, 3123, ABN 87 600 316 612 April 2024 | AU-GA-2400033


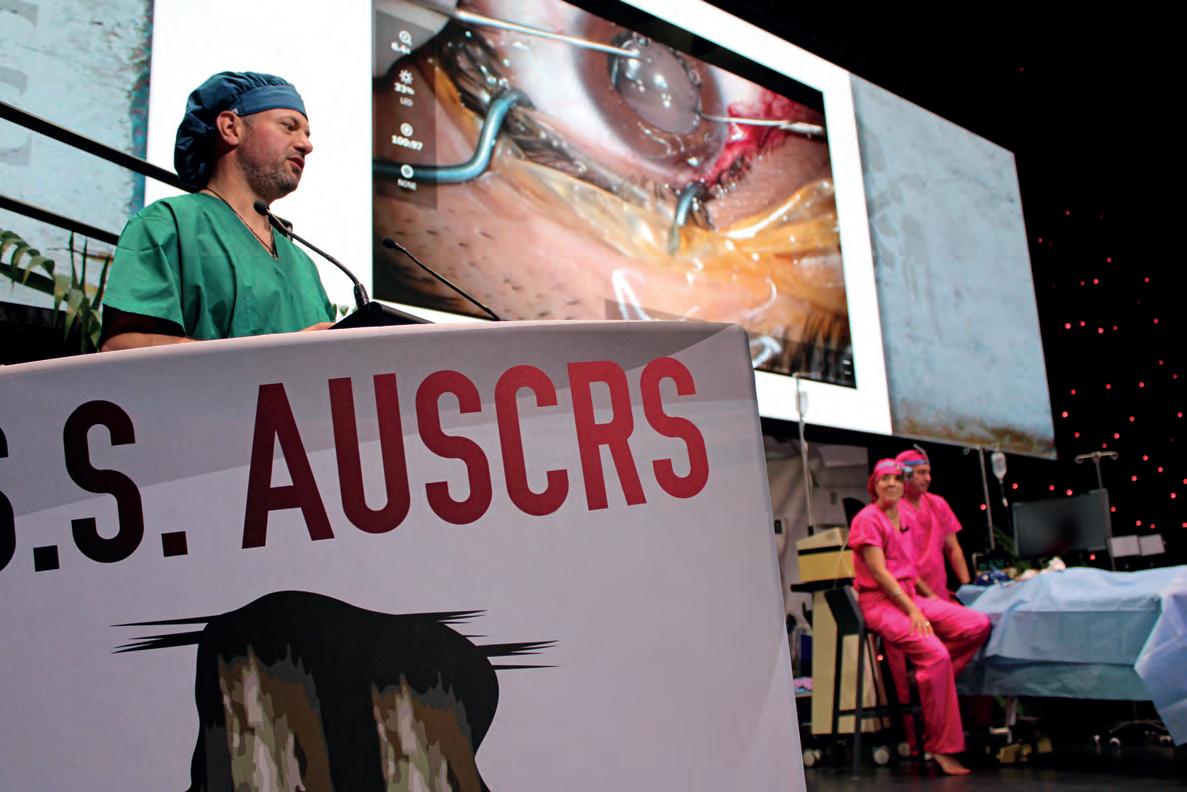
AUSCRS is a feature on the ophthalmology calendar, taking attendees to the leading edge of cataract and refractive surgery globally. Insight was there on Hamilton Island to cover the highlights.
Arecord-setting AUSCRS 2024 has concluded on Hamilton Island and there were many talking points for Australian cataract and refractive surgeons from this year’s program, but nothing came close to the interest around the rapidly evolving field of extended depth of focus (EDOF) intraocular lenses (IOLs).
This year’s event from 24-27 July 2024 provided an ideal mid-winter getaway for non-Queensland ophthalmologists, and an idyllic holiday spot for the international guests who flew in from nearly every corner of the globe.
Since its inception in the mid-1990s, AUSCRS welcomed its highest ever ophthalmology and advanced trainee attendance (188 and 26 respectively), second highest number of support staff (99), and a record-setting gala dinner (280) at the 2024 meeting.
During the event, it was mentioned multiple times that AUSCRS is the gold standard in cataract and refractive surgery conferences, blending a fun, laid back atmosphere with scientific rigour. A key feature is getting the presenters, often leaders in their field, to dress in themed costumes. Each is also addressed in their first name, rather than ‘doctor or professor’. But there’s a key reason, helping to break down traditional hierarchical barriers in the industry. Even the most highly respected
figures – such as Professor Graham Barrett – aren’t exempt.
One of the most thought-provoking sessions was the EDOF showdown where proponents of the latest EDOF designs stated their case for why their favourite IOL was the best.
Visiting international guest Dr Lena Beckers (Denmark) started with a strong argument for the Teleon Acunex Vario and Lentis Comfort IOLs, Dr Luke Anderson (UK) discussed how the Bausch + Lomb LuxSmart helped him as a glaucoma subspecialist compete with refractive surgeons, Dr Josefina Botta (Argentina) backed the RayOne EMV that Rayner has developed with Prof Barrett, and Dr Armand Borovik (Australia) was emphatic about his go-to lens, Alcon Vivity, which is now implanted in more than one million eyes.
But it was Dr Dan Black (Australia) advocating for the new Johnson & Johnson PureSee who came out the winner. Much of the discussion throughout the session, and indeed the whole AUSCRS 2024 conference, focused on what this new IOL offered over other more established EDOFs.
“The EDOF sessions were incredibly popular due to the influx of new and exciting technologies, and the diverse experiences shared by our international speakers,” AUSCRS co-president Dr Jacqueline Beltz said.


“Additionally, the refractive laser session sparked extensive discussions during breaks, as it featured unparalleled insights from experts across all platforms, making it a world-class session that many attendees had never seen before.”
Dr Beltz said the type of ophthalmologist attending AUSCRS has evolved over time. Initially, it was primarily refractive cataract surgeons highly tuned to their outcomes.
“Now, with advanced technologies and techniques being the norm, any ophthalmologist dedicated to improving and providing the best for their patients attends, sharing a common drive to excel and enhance their practice annually,” she said. “We were so happy to break so many records this year. Especially the advanced trainee numbers as they are really important to us at AUSCRS.”
The event kicked off with a welcome evening on Wednesday 24 July where Dr Beltz, her AUSCRS co-president Professor Gerard Sutton, and the rest of the AUSCRS board emerged dressed as members of Gilligan’s Island, with a humourous video playing on screen.
But the real program began on Thursday 25 July with Dr Florian Kretz
LEFT: Dr Lena Beckers fielding a question from Dr Andrea Ang as part of a discussion on ICLs, with Prof Graham Barrett listening intently.
OPPOSITE TOP, L TO R: Dr Elizabeth Yeu, from the US, also delivered a session on a complex case; AUSCRS co-presidents Dr Jacqueline Beltz and Prof Gerard Sutton performing mock surgery in the complicated cases session.
presbyopia-correcting landscape. This included an exploration of the pros and cons of using diffractive EDOF IOLs, EDOF’s using spherical aberrations and a case of a six-year-old boy with unilateral congenital cataract who he implanted with an IC-8 pinhole lens.
Next it was complicated cases co-chaired by Dr Beltz and Prof Sutton who were humorously performing incompetent surgery on a dummy, punctuated with the quips like “bugger”, “double bugger”, “is that tool for ophthalmology?”, and squirting of syringes in the hope to make it better. As things would descend into chaos, a guest speaker would come to the rescue in a “thank God you’re here”-themed session.
It featured Dr Kretz again who played footage of some impressive surgical saves, while India’s Dr Sheetal Brar discussed her experience with the ZEISS Quatera 700 phaco machine for enhanced chamber stability in challenging cases. American ophthalmologist Dr Elizabeth Yeu explored why a dislocated IOL that was visible in the sulcus at pre-op visit with supine exam might have disappeared, and Dr Ron Yeoh delved into the uncomfortable topic of a dropped nucleus in cataract surgery.
Immediately after this, there were presentations on implantable collamer lenses (ICLs) by Dr Beckers and Dr Dean Corbett. While these present a nice option for patients ineligible for refractive laser surgery due to their corneal irregularities, there was much debate over whether they should be marketed to patients as “reversible”, along with discussion over the ideal dioptre threshold to implant them in myopic patients.
The future of IOL formulae was also up for discussion, and no one is better placed to discuss this than Prof Barrett – who developed the Barrett formulae used by many cataract surgeons globally. He discussed whether artificial intelligence could surpass human

intelligence when developing next generation formulae, ultimately stating that he didn’t believe it would, and predicted that each manufacturer will soon have its own formulae for their own lenses.

Post-event, he said feedback had been “extraordinary”, with attendees enjoying the balance between good clinical information and fun.
Prof Sutton said while EDOF lenses and the new lenticular laser eye procedures were a focal point throughout, another session stood out.
“I think the session that Jacqui Beltz and Jo Mitchell ran about the ophthalmologist’s journey and dealing with hurdles was exceptional,” he said, with the session focusing on dealing with failure and setbacks, and key tips on how to thrive in one’s career.
Dr Beltz agreed: “The overwhelming feedback was that people learnt a lot, and had a brilliant time.
“I hope attendees leave AUSCRS 2024 with new knowledge, skills, and, most importantly, renewed energy and enthusiasm for our work. Additionally, I hope they have built or refreshed a network of like-minded friends and colleagues to look forward to seeing at the next meeting.”
AUSCRS is returning in 2025 in the Top End from 16-19 July 2025.
Our flexible partnerships give you immediate access to:
Leading technology and specialist ophthalmic day hospitals
Professional autonomy within a collegiate setting
All-around support from highly trained staff, backed by a management team with industry expertise
Practice-building services, such as our Clinical Relationships Team and referrer engagement programs
Research opportunities, including grants through our research charity, Future Vision Foundation
With the rise of optical retailers online, DOMINIQUE JORGENSEN weighs up the importance of optical dispensing skills and patient outcomes versus the consumer’s freedom of choice and accessibility.

“DISPENSING IS AN IN-DEPTH PROCESS OF FRAME AND LENS SELECTION WITH PRECISE MEASUREMENTS, REQUIRING SPECIALISED KNOWLEDGE, AND MUST BE SPECIFIC TO THE PRESCRIPTION AND LENS TYPE ORDERED.”
When I began this article, it was easier to think of the cons, rather than the pros, for ordering spectacles online. As an optical dispenser, my mind went to all the interpersonal skills we use, tailored advice, and the specific measurements and variables we juggle when dispensing for patients. However, with the growth of online spectacle retailers, there’s clearly a demand for this service.
It makes sense some optical retailers would jump at the opportunity for a new, cost-effective income stream in the online marketplace. Using existing lab and supply chain resources but expanding their market reach from the local area to interstate or even international consumers seems like a no-brainer.
misinterpretation, shape selection, and an adorable quip about the glasses looking “very expensive” on the screen, but then actually arriving looking “…very cheap, so it’s not worth the money”.
These are issues most online shoppers face, though when provided with enough information from retailers, accurate dimensions (such as Dresden Vision’s ingenious printable size guide), AR-technology, and customer reviews, a lot of these risks can be mitigated.
possible, however it doesn’t seem widely available yet.
Other prescription considerations that may slip through are conditions like anisometropia – where the strength of the prescription may fit under their ‘suggested index for this prescription’ but the difference in spectacle magnification can cause significant adaption issues.
BELOW: Ordering spectacles online can be a risk, especially for patients with more complicated prescriptions.
Then for some patients, there’s always been an issue about the cost of spectacles. I’ve experienced the distrust of patients ‘burnt’ previously by retailers promising the world, charging exorbitant prices, then providing a subpar product. So, the opportunity to purchase suitable spectacles at a cheaper price is understandably enticing. Add to that the astounding range of styles, colours, and materials available online, with new frame technology and the use of social media to market them, it makes purchasing online even more appealing. However, when I first mentioned buying glasses online to my seven-year-old daughter, her response was “but how do you know if they fit properly?”. Then came a slew of comments about colour
The risk for consumers when purchasing prescription glasses online, however, lies in the lack of understanding that every pair of glasses are customised for them. It’s not just a matter of choosing a shape and colour you like, and that the ‘size’ or numbers on the temples match your current pair. Dispensing is an in-depth process of frame and lens selection with precise measurements, requiring specialised knowledge, and must be specific to the prescription and lens type ordered.
These mostly need to be conducted in-person, with the frame sitting on the customer’s face. Ordering a +1.00 DS pair of readers online will have a relatively high success rate, due to the low, uncomplicated prescription, however how will a pair of -6.00 DS spectacles, or even a pair of progressives, for a first-time wearer transpire?

This is where the accuracy – or sometimes complete absence – of measurements during an online order come into play. Most online retailers provide instructions on how to measure pupillary distance. Doable, and in some cases passably accurate. Many retailers, though, lack the ability to consider height measurements. Whether that’s centre of rotation rule heights for single vision, or fitting heights for progressives, it’s difficult to take that frame-dependent measurement without the frame present. Other measurements for high-prescriptions such as back vertex distance (BVD), pantoscopic tilt, and wrap are impossible to take without the frame present. An adaption to the digital frame fitting technology available in stores by using AR technology may be
When thinking of online purchasing, this raises a few questions for me: are the patient’s expectations lower or higher because of the online purchasing process? Are the consumers more lenient on issues with fit or vision/ clarity because they purchased online? And where does the responsibility lie for online spectacle distributors to abide by Australian and New Zealand Standards for mounted spectacles? Especially when some retailers send their spectacles directly from overseas labs, how can we ensure patients are receiving the ideal correction, within AUS/NZ Standards, if we have no hand in supplying the spectacles?
Dispensing concerns aside, the ability to purchase spectacles online does improve access. Previously, people with disabilities, elderly patients, and rural residents would either go without, or undertake long and expensive trips to purchase glasses. And immunocompromised people would need to risk their he alth for in-person visits.
With the ever-expanding digital retail environment, I’m interested to see the development of online spectacle retailers and how they can overcome the practical requirements for dispensing. While I believe no technology or online retailer can replace a qualified optical dispenser, there are some areas where online retailers can offer a solution when traditional methods can’t – as long as they’re within AUS/NZ Standards.
ABOUT THE AUTHOR: Dominique Jorgensen is a qualified optical dispenser, assessor for the Australasian College of Optical Dispensing, and a technical officer and optical dispensing instructor at The University of Western Australia. She is also the marketing assistant for Optical Dispensers Australia.

Chief orthoptist at The Royal Children's Hospital CATHY LEWIS discusses the projects in place to ensure robust collaborative care models in paediatric eyecare.

Paediatric ophthalmic conditions are often complex and can require lengthy investigations over many years. As the demand for paediatric eyecare increases, orthoptists are taking a lead role in adapting service delivery to ensure children have access to appropriate care in a clinically appropriate timeframe.
“AS THE DEMAND FOR PAEDIATRIC EYECARE INCREASES, SERVICE DELIVERY MUST ADAPT TO ENSURE CHILDREN HAVE ACCESS TO APPROPRIATE CARE IN A CLINICALLY APPROPRIATE TIMEFRAME.”
Traditional approaches to paediatric eye care are provided by orthoptists and ophthalmologists through public hospital outpatient eye clinics. However, due to tight budgets and fixed clinic space, staff recruitment and clinic expansion are rarely an option to improve access to care in public hospital outpatient eye clinics.
As such orthoptists are identifying opportunities for collaboration which can result in improved, affordable, patient focused and clinically appropriate care.
In 2020, with the support the director of ophthalmology at The Royal Children’s Hospital (RCH) in Melbourne, a collaboration between the RCH orthoptic team and orthoptists in the La Trobe University Orthoptics Department resulted in the establishment of the orthoptic student led Latrobe University Eye Clinic (LTEC). RCH patients with strabismus and/or amblyopia who met the referral criteria were referred into the orthoptist managed pathway of shared care.
Following the success of shared care with LTEC, director of ophthalmology, Dr Anu Mathew and I explored additional opportunities for collaboration to provide and maintain a sustainable model of
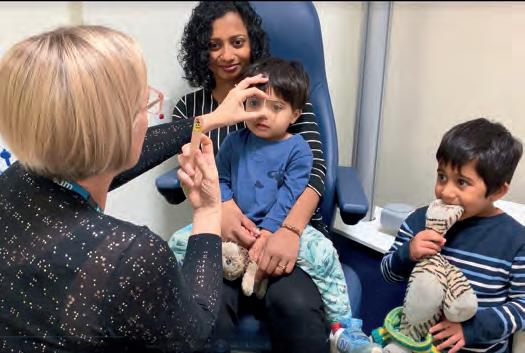
paediatric eyecare provision. A second collaboration was established with the optometry student led Melbourne Eyecare Clinic (MEC), which is linked to the Melbourne University School of Optometry. In this pathway of shared care, RCH patients with craniosynostosis, juvenile infantile arthritis, NLDO and chalazion who met the referral criteria were referred into the MEC.
Although different patient groups were involved with each collaboration, the process of establishing and implementing the pathways of care were the same. Patients were managed according to the evidence-based RCH guidelines, and additional protocols relating to patient care and administrative workflow were developed collaboratively for each pathway of shared care. Patient surveys and quality control audits have shown both models of collaborative care are patient focused and provide timely and appropriate care.
Collaboratively managing over 1,000 children in the community has had the added benefit of improving access to care within the RCH eye clinic for children with complicated conditions unable to be managed externally.
These models of shared care benefit all stakeholders, the patients, the RCH, our collaborative partners, and student learning, which in turn benefits future community care. Yet at RCH, we continue to struggle to reduce outpatient waitlist numbers and patient access. Additional education, collaboration and community-based paediatric eyecare is essential to meet demand.
The RCH Ophthalmology Department is developing online paediatric ophthalmic education resources to build and support relationships with optometrists in the community who are interested in providing evidence based, paediatric ophthalmic care both independently and in collaboration.
Projects of this scale are not possible without financial support, and therefore Dr Anu Mathew, and I were honoured to be the 2024 recipients of the RCH Foundation, Frank Billson Research Scholarship. This scholarship was
awarded to support the development and implementation of online education and collaboration modules.
An online module containing paediatric ophthalmic collaborative-care resources is being developed for optometrists in the local community interested in collaborative care with RCH.
A separate online education module is simultaneously being developed to support optometrists locally and nationally, who are interested in further developing their knowledge and skillset in the field of paediatric ophthalmology. This module will include information on paediatric ophthalmic assessment, and diagnosis and management of paediatric ophthalmic conditions.
To ensure content meets end user requirements, all optometrists in the community are invited to provide feedback by completing a short anonymous survey. To participate in the survey, please scan the QR code at the end of this article. Participation is strongly encouraged to enable development of appropriate educational resources aimed to support regional, metropolitan, and remote based optometrists in both clinical and non-clinical roles, with a wide range of experience and knowledge in the field of paediatric ophthalmology.
Thank you in advance for your participation, and we look forward to providing an update on the project in the near future.
ABOUT THE AUTHOR: Cathy Lewis is the chief orthoptist at The Royal Children’s Hospital in Melbourne and a casual lecturer in orthoptics at Latrobe University. She has over 30 years’ experience working and volunteering as an orthoptist both locally and abroad and has co-developed and implemented several initiatives at the RCH to improve access to patient centred care.
ORTHOPTICS AUSTRALIA is the national peak body representing orthoptists in Australia. OA’s Vision is to support orthoptists to provide excellence and equity in eye health care. Visit: orthoptics.org.au
Finding and managing staff can be one of the most challenging parts of running an eye clinic. KAREN CROUCH walks through the key aspects, starting with recruitment.

I“COMPLYING WITH REGULATIONS IS NOT JUST AVOIDING PENALTIES. IT’S ALSO ABOUT SERIOUSLY PROTECTING THE HEALTH OF STAFF.”
n 2023, we published a three-part article on starting up a practice, essential reading for a new practice creation. In the next two articles, we will identify actions to develop a strong, responsive and effective staffing structure to support staff in delivery of quality healthcare services.
At this point, there is an assumption that the following has been completed: the owner has formulated a vision and defined their target market, a suitable premises has been selected with fit-out work commenced, and staff have been selected.
We will focus on appointing appropriately experienced employees and essential preliminary actions to complement the overall group effort aimed at maximising high quality customer service.
This foundational document, viewed as the ‘practice bible’, is for reference, training and other purposes such as practice protection against litigation or complaints from internal or external parties – such as tradesmen. The practice’s documented operating processes should be favourably viewed by courts, insurers, or Workers’ Compensation authorities.
Policy & Procedures (P&P) comprises two distinct parts: Procedures – a comprehensively documented, regularly updated, P&P Manual serves the following purposes:
• Reference: new or existing staff may clarify procedures
BELOW: Short listed candidates should attend final interviews at which point the owner may be involved in final decisions.
• Risk management: instructions and staff training, defence against claims that employers may be liable for
• Induction: training tool for new staff to absorb practice policies and procedures

• Service standards: by which performance may be measured during staff appraisals or salary reviews
• Professional standards: regular reviews will ensure highest professional standards and compliance with current regulations
• Practice accreditation: will impress an accreditation assessor and provide grounds for a favourable practice performance report.
Policies – defines extent and who can develop policies – a sort of “policy on policies”. The following matters deserve inclusion:
• Authority: employees empowered to dictate ‘policy’, including a delegation schedule listing relevant authorised staff
• Nature and extent within which delegated employees may frame a policy and whether it requires review by a senior employee. Implementation may be entrusted to a different individual/team to confirm the overall process achieved the desired outcome.
Responsibility for compiling and updating the P&P usually rests with experienced practice managers. Additionally, clinical staff should be involved for a meaningful clinical governance structure.
Complying with regulations is not just avoiding penalties. It’s also about protecting the health of staff. Practices should comply with latest WHS legislation/regulations, training and reporting requirements and best practice management techniques. Employers’ legal obligations include:
• Ensuring premises are free of health and safety risks
• Providing and/or maintaining equipment and safe systems without risks to health
• Providing information, instruction, training and supervision necessary to ensure employees’ health and safety
• Consultation process by committee, representative or other arrangement
• Return-to-work obligations.
Job Analysis – analyse each role and determine nature/expertise of individuals necessary to perform each role – attendance
requirements, educational qualifications, work experience and personal values. Next steps:
• Document detailed position descriptions, key performance indicators (KPIs), roles and responsibilities
• Develop a comprehensive questionnaire in preparation for applicant interviews.
Decide who will undertake the important recruitment task – owner/s, staff member or recruitment agent, preferably one with experience in the health industry.
Advertising – an advertisement must be carefully constructed to attract suitable applicants that match job functions. Appropriate advertising streams should be selected for maximum exposure to the industry, within reasonable geographical boundaries.
Screening and culling – resumes should be sorted into ‘yes, maybe and unsuitable’ categories. All resumes, including ‘unsuitable’, should be acknowledged by e-mail or telephone.
Interviews & selection – contact ‘yes’ applicants, and some ‘maybes’ if ‘yes’ numbers are low for interview times and dates. Also, allow time gaps between interviews to avoid candidates ‘bumping’ into one another for confidentiality. Record detailed interview notes, responses to aforementioned questionnaire, recommendations and prepare a short list of candidates for final interviews.
References – reference checking must be conducted by personal discussion with nominated referees. A pre-prepared list of probing questions should ensure responses are genuine and meaningful.
Implementation – successful applicants should be issued a letter of appointment, citing all relevant employment conditions (salary rates, awards, superannuation, leave etc.).
Periodical meetings with new staff should ensure they are progressing or whether further guidance is necessary. We are now ready for the second performance management phase.
ABOUT THE AUTHOR: Karen Crouch is managing director of Health Practice Creations, a company that assists with practice set ups, administrative, legal and financial management. Contact her via email kcrouch@hpcnsw.com.au or visit, www.hpcgroup.com.au.

Patients were questioned about aspects of vision processing that would be more helpful to them. They spoke about the social isolation of profound visual loss and identified several features they felt would
A particular request was the ability to detect a face, so people can be differentiated from objects at the same height. This would be useful when walking in the street, and when speaking to someone so they can direct their conversation towards a forward-facing person.
Additionally, the ability to identify an empty chair in a café or other social situations was also felt to be useful for social engagement. The ability to gauge proximity of objects was also identified as useful for navigation.
Following the Generation Two trial we immediately obtained ethics approval to enrol the same participants in further work, firstly to continue monitoring the devices within the eye and secondly to use new vision-processing algorithms to try and achieve these aims. Ensuring the safety of a retinal prosthesis within the eye for the lifetime of the user is crucial. When we design the suprachoroidal retinal prosthesis we use materials and methods with this aim in mind.
the social isolation issues identified by our participants.
We have been testing these new algorithms in comparison with our original comprehensive vision processing algorithm developed by Professor Barnes. The results of this testing have been submitted for publication.
More than 35 groups from around the world have been working on visual prostheses. Most are intraocular, but a few groups are working on cortical prostheses which connect directly to the visual cortex at the back of the brain.
The three groups who have achieved European or US regulatory approval for retinal prostheses for use in patients with profound visual loss due to retinal dystrophies have unfortunately ceased production of their devices due to a combination of either technical failure, limited market penetration and/or poor patient outcomes.
Bionic Vision Technologies continues to work towards commercialisation of the suprachoroidal retinal prosthesis – improving functionality of the devices to provide better experiences for participants is vital to achieving this.
people with late-stage inherited retinal disease (NCT03406416) was exciting because we could publish results demonstrating the devices’ stability, both in position and performance, as well as positive outcomes for participants both in the lab and at home.
This followed on from our 2012-2014 (NCT01603576) proof-of-concept prototype trial which showed electrical stimulation within the suprachoroidal space would result in reliable phosphenes (artificial visual impulses). However, the device does not provide complete independence. We are keen to improve its performance to better support current and potential future users.
We were fortunate to be able to use biocompatible platinum and silicone - materials that had been used in many prosthetic devices in the past – and conducted extensive testing of the intraocular components and lead wires prior to any participant implantation surgery.
However, regular ocular health checks conducted by clinical examination, fundus photography and OCT are also vital to demonstrate the long-term viability of the suprachoroidal approach. Hence, we are collecting a further five years of ocular health data.
New vision processing algorithms developed by our long-term collaborator Professor Nick Barnes from Australian National University and our commercial partner Bionic Vision Technologies have addressed some of
Our past work has demonstrated the ease of the surgical approach, the devices are stable within the eye, and their performance is reliable. We continue to actively collect data on ocular health to confirm the feasibility of long-term implantation of our devices and ongoing performance. We also continue to seek input from our current participants to identify further improvements in vision processing, aiming to enhance their daily living.
Name: A/Prof Penelope Allen
Qualifications: MBBS, FRANZCO
Affiliations: Centre for Eye Research Australia (CERA), Melbourne Retina Associates
Location: Melbourne
Years in industry: 30
ENSURING THE SAFETY OF A RETINAL PROSTHESIS WITHIN THE EYE FOR THE LIFETIME OF THE USER IS CRUCIAL. WHEN WE DESIGN THE SUPRACHOROIDAL RETINAL PROSTHESIS WE USE MATERIALS AND METHODS WITH THIS AIM IN MIND.
To list an event in our calendar email: myles.hume@primecreative.com.au

ESCRS 2024
Barcelona, Spain
6 – 10 September escrs.org
BLUE SKY
Adelaide, Australia
13 – 14 September bluesky.optometry.org.au

ORTHOPTICS AUSTRALIA CONFERENCE
Adelaide, Australia 2 – 4 November orthoptics.org.au
EYECARE PLUS NATIONAL CONFERENCE & AGM
Sydney, Australia 18 – 19 October eyecareplus.com.au/conference/
RANZCO CONGRESS 2024
SPECSAVERS CLINICAL CONFERENCE (SCC) 2024
Gold Coast, Australia 14 – 15 September specsaversclinicalconference.com.au
ASO INTERNATIONAL EYE CARE EXPO Hanoi, Vietnam
15 – 21 September asoeye.org
SILMO PARIS
Paris, France
20 – 23 September silmoparis.com
APAC STRABISMUS AND PAEDIATRIC OPHTHALMOLOGY SOCIETY MEETING Colombo, Sri Lanka. 27 – 28 September apspos2024@gmail.com
Adelaide, Australia 1 – 4 November ranzco2024.com
ODA INTERNATIONAL CONFERENCE
Sydney, Australia 7 – 8 March odamembers.com.au
ODMA FAIR
Sydney, Australia 27 – 29 June odma.com.au


WHY DID YOU PURSUE A DISPENSING CAREER?
I saw it as a role that blends healthcare, customer service and fashion, which have always been my interests. It would enable me to directly contribute to improving people’s vision and quality-of-life. Also, I enjoy working with people so a role that allows me to interact with customers and create positive experiences is something I was looking for.
HOW DID YOU COME TO WORK AT SPECSAVERS?
I saw Specsavers as an organisation that offered great professional growth and training opportunities and also focuses on a collaborative work environment. I value being a member of a team that is always looking to help other team members. Specsavers also stays abreast of technological advancements in eyecare which is important to me.
I’ve been fortunate to have some incredible growth opportunities. I started as an optical assistant in 2017 and gradually moved up the ladder, first as a supervisor and then as an in-store trainer. Each step allowed me to expand my skills and take on more responsibilities, which was really rewarding. One of the biggest milestones was completing my Cert IV in Optical Dispensing. Not only did it give me a deeper understanding of the industry, but graduating at the top of my class was a huge confidence boost. Now, I’m focusing on two exciting paths: the Manager Ascent Program and achieving Level Gold certification in In-Store Trainer. These opportunities not only push me to grow professionally but also allow me to contribute more to the team and company. Overall, I’m grateful for the chances to develop and progress in my career at Specsavers. It’s been a journey of learning and improvement, and I’m excited to see where it takes me next.
One of the most memorable cases involved a patient who had recently experienced a brain injury. Communicating with them was challenging because they found it difficult to maintain a conversation. Our goal was to find the right type of lenses to address their needs, but it wasn’t straightforward. We knew that traditional progressive lenses wouldn’t be suitable due to the patient’s limited mobility and communication abilities. So, I took the time to talk slowly and patiently with them, trying to understand their needs as best I could. Working closely with the optometrists, we brainstormed ideas and eventually came up with a unique solution: to go with a lens that provided a balance between distance and intermediate vision in the top half, while the bottom half was optimised for reading. This way, they could access the different prescriptions within the lens without needing full mobility. When the patient finally received their new glasses, their gratitude was overwhelming. It was incredibly rewarding to see how much of a difference our solution made in their day-to-day life. Moments like these remind me why I love what I do.
What truly excites me is the chance to make a difference, not only for our patients but also for my team and helping them with their growth in the business. Helping patients is my passion. Whether it’s guiding them to find the ideal frames or sorting out their vision issues, every interaction presents an opportunity to brighten someone’s day. Knowing that I contribute to enhancing someone’s vision and overall wellbeing makes it all worth it.
Optometrist Joint Venture Partnership Opportunity – Jesmond, NSW
Specsavers has an exciting opportunity for a passionate and experienced Optometrist to join our established store in Jesmond, New South Wales, as a Joint Venture Partner. Specsavers Jesmond offers 2 test rooms, a varied patient demographic, and an extremely welcoming, supportive team. If you’re looking for a perfect blend of natural beauty and urban convenience, just a short drive from Newcastle CBD, look no further than Jesmond!
Optometrist Joint Venture Partnership Opportunity – Hobart, TAS
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Carly Parkinson on +61 (0) 478 201 057 or carly.parkinson@specsavers.com
Optometrist employment enquiries: Specsavers Recruitment Services anz.srsdepartment@specsavers.com
Locum employment enquiries: ANZ.locumteam@specsavers.com
Graduate employment enquiries: apac.graduateteam@specsavers.com
Specsavers have an amazing opportunity for an Optometrist looking to accelerate their career by becoming a Joint Venture Partner within our well-established Hobart store. Specsavers Hobart is located within The Cat and Fiddle Arcade, which houses over 70 specialty stores including H&M, Target and Myer. The store itself is 164 sqm in size, boasts 4 optical test rooms, 6 dispense desks, over 1100 frames on display, and state of the art equipment including OCT.
Up to $40k sign-on bonus for an experienced Optometrist in Darwin! Darwin is the capital of Australia’s Northern Territory and the gateway to the massive Kakadu National Park. From incredible sunset cruises and crocodile encounters to Asian food markets and outdoor cinemas, Darwin has it all. Specsavers is located in Hibiscus Shoppingtown and offers 2 test rooms, an experienced and supportive retail team and well-established relationships with local Ophthalmologists and GPs. Flexible options are available, including full-time, part-time or short-term contract of 6, 12 or 24 months, so you can get a feel for the area before committing to a permanent role. Excellent career development opportunities are available, including Pathway to Partnership.
Optometrist opportunity – Specsavers Invercargill, NZ
Seeking a talented optometrist to join our extraordinary team at Specsavers Invercargill. We offer cutting-edge technology, a friendly environment, and a commitment to professional growth. Embrace the relaxed pace of life and enjoy a perfect work-life balance. Explore stunning coastal views and enjoy a fantastic outdoor lifestyle. Don’t miss this incredible opportunity to be part of Specsavers Invercargill.
Graduate Opportunities
Are you a final year student still looking to secure your first role as a Graduate Optometrist? Specsavers have provided rock-solid career development paths for optometrists, offering great graduate packages and a diverse range of patients in locations all across Australia and New Zealand. By joining us as an optometrist, you can be certain you will have everything at your disposal to help improve health outcomes for your patients.

Sydney vitreoretinal surgeon and ophthalmologist Professor Andrew Chang is the only Australian on Opthea’s newly formed Medical Advisory Board. Prof Chang is among 10 retina thought leaders from countries around the world who were appointed. He holds academic appointments of Conjoint Professor of the Department of Surgery UNSW and Clinical Associate Professor at the University of Sydney. He is a consultant ophthalmologist and the Head of Ophthalmology at the Sydney Eye Hospital, and the Medical Director of Sydney Retina Clinic, Australia.

Manager for Opticare in Queensland. He started his career in the UK and has a wealth of experience in lab, wholesale, and retail optics. He also worked in the Rx section of Maui Jim and had been an Account Manager in NSW and Queensland for OSA and Essilor. Outside work, Vickers is passionate about sports and fitness and has participated in triathlons and done city-to-surf every year for the past eight years. He will be based in Opticare’s Brisbane office.



cial intelligence (AI) digital health company, has appointed Bryan Haardt as CEO. He has more than 25 years of experience founding and leading healthcare technology enterprises. Prior to joining Eyenuk, Haardt led digital therapeutics at Boehringer Ingelheim and was GM of Pawru. He co-founded Decisio Health Inc, served as COO for Prognosis Health, founded Cgate Health, and started



