
FEEL PROUD of making a difference to customers through the help and care you provide. Can you see yourself in Specsavers? spectrum-anz.com/ careers-at-specsavers




FEEL PROUD of making a difference to customers through the help and care you provide. Can you see yourself in Specsavers? spectrum-anz.com/ careers-at-specsavers


Workloads on RANZCO trainees continue to weigh heavily, according to the latest 2024 Medical Training Survey (MTS), with the average working week continuing to be almost eight hours longer than other doctors in training.
And it appears to be impacting life beyond the practice, with less than half of the next generation of eye doctors able to achieve good work/life balance and a third saying unpaid overtime has impacted their wellbeing.
While long work hours remain problematic, RANZCO trainees are more likely to pass their exams, feel confident of securing employment, and are much less likely than other trainees to be considering a career outside of medicine.
Plus, 98% of RANZCO trainees

Shutterstock.com.
intended to continue with their specialty.
The work lives of ophthalmology trainees were revealed in the 2024 MTS that received 46,440 responses at a rate of 53%. It’s the
sixth nationwide survey of all doctors in training and is a confidential way to improve training across specialities and the health system.
The ophthalmology report had 52 respondents, of whom 92% were registrars, and 5% Aboriginal and/ or Torres Strait Islanders. Male and female respondents were evenly split.
On average, RANZCO trainees worked 52.2 hours a week, which was slightly down from the high of 53.3 hours reported in 2023. But it is still much higher than the 44.8 hours a week for the average doctor in training.
“For RANZCO trainees, 91% were working 40 hours a week or more, compared to the national response of 62%,” the report also added.
When asked to rate their workload, 31% of ophthalmology trainees said
Healthscope, Australia’s second-largest hospital operator, will be hoping the new year brings greater fortune as it struggles with substantial debt and questions over moves to address its financial problems.
Concerns about the future of the organisation and the private health sector in general were so great that, as 2024 ended, the Australian Society of Ophthalmologists (ASO) launched a petition for the Federal Government to establish a private health commission.
The move followed months of ongoing and unresolved disputes between health insurers and the private hospital sector, including the closure of more than 70 private facilities.
The future of Healthscope, which owns 38 private hospitals, including Sydney’s Northern Beaches Hospital and Gold Coast Private Hospital, remains the greatest focus of those growing fears.
An article in Australia’s Financial Review said the company had received “tens of millions” in emergency funding from its Canadian private equity owner Brookfield, and a warning that it was on borrowed time unless it secured government help urgently or more money from insurers.
The article said the funding was to give Healthscope more time to renegotiate its $1.6 billion in debt “with a consortium of increasingly nervous lenders”.
The closure and/or sale of some
of those private hospitals remains a possibility.
The Australian health sector, including ophthalmologists who use many of Healthscope’s facilities, will be watching on with interest and some concern.
Facing rising costs and significant debt, in November 2024 Healthscope announced plans to charge members of several health funds a “hospital facility fee” of $50 for same-day services and $100 for overnight services "due to these insurers’ failure to sustainably cover the cost of patient care”.
It then announced it would terminate its contracts with some health insurers.
continued page 8
it was moderate (vs. 49% nationally), but 58% said it was heavy (38% nationally), and 11% (9% nationally) very heavy.
As such, the amount of work ophthalmology trainees are expected to do adversely impacted 35% of respondents (vs 25% nationally). So did unpaid overtime (30% vs 18%), and having to relocate for work (40% vs 24%).
Further drilling into workplace and culture, 56% of ophthalmology trainees said their workplace supports them to achieve a good work/life balance against a national average of 71%. And 46% (vs. 65% nationally) said they had a good work/life balance.
RANZCO censor-in-chief Dr Andrew Thompson said the college
continued page 8

A recent CPD event for Specsavers optometrists has demonstrated how the industry can better serve LGBTQIA+ patients. It showed how frontline community health care providers, including optometrists, have a unique opportunity to show ‘allyship’ by practising sensitivity, embracing nuances of gender identity, and making small adjustments, like offering options for pronouns in patient forms.
page 52






The Australian College of Optometry hopes a new name and strategy will bring better health outcomes for all.

A lens that adapts to the patient’s visual profile rather than having the patient doing the heavy lifting.
It’s difficult to predict what the next 12 months might hold for the ophthalmic sector. For 2024 I predicted a TGA-approved therapy for geographic atrophy (wrong), and that remote optometry consultation would be carried out at scale (not yet).

But if we were to stare into a crystal ball what would emerge for 2025?
I think it’ll be an intriguing year for the optometry market. Despite a tighter trading period due to price-conscious consumers, in 2024 EssilorLuxottica added 25 more locations (EyeQ acquisition) and invested in 80 new ultra-widefield retinal devices and 55 OCTs. Specsavers announced 17.7% revenue growth, and George & Matilda added 34 independents to its network. Significant momentum seems to be gathering behind the big players, and I can’t see much stopping them.
Let’s also not forget the Chemist Warehouse-based network is waiting in the wings (currently with two locations).
As these networks strengthen, new ways to evolve the customer experience will emerge, blending virtual and in-store interactions. They’re also poised to add streams once considered the domain of independents, such as IPL for dry eye.

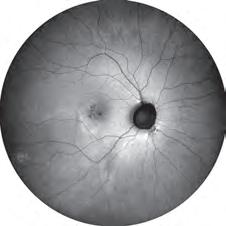
Summer is a critical time to raise awareness about recognising malignancies, says Dr Helen Garrott.
But I expect the independent market to respond. If anything, it serves as an opportunity to double down on the things that make them unique, whether it be an advanced contact lenses, behavioural optometry, or an eyecare and dispensing experience that's hard to find elsewhere.
Many people are thinking about ways to keep the independent market intact. That is, an exit strategy with a deliberate path to another independent owner. This, and many other practical tips, will be a major focus at ODMAFair25 that I’m excited to see returning as the industry’s flagship optical trade show in 2025.
Meanwhile, some big forces are at play in ophthalmology. As I write this, the rhetoric is amping up over the fast-tracking of overseas-trained doctors into Australia, RANZCO’s monopoly on training future ophthalmologists is in question, and the lengths Healthscope was prepared to go by terminating health fund contracts surprised many. Let’s hope there’s some resolution on these matters early on, so doctors can get about their business.
Rayner’s new spiral Galaxy IOL was all the rage towards the end of 2024, and looking overseas there’s likely to be some big cataract innovations hitting our shores in the coming months.
As for more predictions, they can be found on pages 14-19 where industry figures share their hopes and concerns for the year ahead. There’s never a dull moment.
MYLES HUME Editor

Just as Insight went to print, the WAKE FOREST INSTITUTE FOR REGENERATIVE MEDICINE in the United States was announced as the latest organisation to join the AU$195 million challenge to make whole eye transplants a reality. The institute joins more than 40 scientists, doctors, and industry experts from around the US working to meet the challenge and restore vision to millions. The studies spearheaded by Dr Vijay Gorantla, a renowned expert in vascularised composite allotransplantation and
Aussie golf prodigy Jeff Guan has opened up on a freak eye injury threatening his playing career. As Insight reported in December, he was struck during a recent tournament. The injury was so bad that he spent weeks in intensive care at Sydney Eye Hospital. “During my nights in hospital, I almost drowned in thoughts about the injury and my future in the sport. Not only was I utterly distraught … but the whole situation made me very depressed and somewhat angry,” the Sydney Morning Herald reported.
In a first, Monash University inclusive technology researchers have developed new guidelines to create 3D-printed educational and other accessible tools to support people who are blind or have low vision. Freely available, they provide information attuned to the needs of blind and low vision users, including inclusive design considerations, directions to create braille or audio labels, and accessible resources for blind makers.
WACKY
Magpie season in Australia has struck again, with several eye injuries reported. This time, a 40-year-old mother was left with a bloody and bruised eye after being attacked during a morning walk on Coogee beach, Sydney. After seeking help, a pharmacist said she was the third person they’d seen after being swooped by what was thought to be the same magpie, news.com.au reported.
professor at the institute, will play a pivotal role in addressing the technical, biological, and immunological hurdles in whole eye transplant. IN OTHER NEWS, EssilorLuxottica has opened a state-of-the-art fulfilment centre in Sydney that can handle tens of thousands of shipments per month to service the company’s own retail network and wholesale customers.
The 4600 sqm facility, which began operating earlier in 2024, is described as a “powerhouse in our logistics network across Australia and New Zealand” located strategically at Kemps Creek. For the first time,
EssilorLuxottica has consolidated all of its brands and entities under one roof, including product and optical services.
FINALLY, Vision 2020 Australia has advocated for a $12 million Federal Government investment into assistive technology (AT) in the Indo-Pacific. “Assistive technology plays a critical role in ensuring people with vision loss remain independent. Simple devices like glasses and white canes can transform lives, helping people to see and navigate effectively, benefiting the health, economic and social well-being of individuals and communities,” CEO Ms Carly Iles said.

Aussie patch covered
Figures from 2021 show there were 1,055 orthoptists, equating to 3.1 full-time equivalents per 100,000 people, and closely parallelling the number of ophthalmologists in Australia. Page 57
14 – 16 February
insightnews.com.au
Published by:
379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766
www.primecreative.com.au
Chief Operating Officer
Christine Clancy christine.clancy@primecreative.com.au
Publisher
Sarah Baker sarah.baker@primecreative.com.au
Editor
Myles Hume myles.hume@primecreative.com.au
Assitant editor
Rob Mitchell
rob.mitchell@primecreative.com.au
Commissioning Editor, Healthcare Education
Jeff Megahan
Business Development Manager
Luke Ronca luke.ronca@primecreative.com.au
Head of Design Blake Storey
Art Director
Bea Barthelson
Subscriptions T: 03 9690 8766
subscriptions@primecreative.com.au
Complete calendar page 60
NEXT MONTH ODA CONFERENCE
7 – 8 March
The 2025 Optical Dispensers Australia International Conference is a biennial two-day event in collaboration with the International Opticians Association. odamembers.com.au THIS MONTH
The Australian and New Zealand Glaucoma Society’s annual event will include the highly popular and somewhat unpredictable interactive panel and case presentations. anzgsconference.com
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright –No part of this publication can be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.
continued from page 3
closely reviewed the MTS and conducted its own surveys and reports, as well as training post inspections.
“RANZCO sets the training program for ophthalmology trainees and works closely with the training jurisdictions and trainers to ensure the trainees are supported to complete their training,” Dt Thompson said.
“There is an obvious tension between this and the need to provide service delivery to patients. The college will continue to advocate for protected training time and work-life balance for our trainees, as well as for trainers, tutors and supervisors.”
In other more positive findings, just 12% of trainee ophthalmologists were concerned about securing employment versus a 41% national response rate.
Plus, 56% of RANZCO trainees were interested in rural practice – seven percentage points above the national average – despite just 6% training regionally and 2% rurally.
Other results showed 94% felt the RANZCO training program was relevant to their development, 84% would recommend their current training position to other doctors, and of those who received exam results, 91% passed.
“I think a combination of factors gives trainees confidence about their future employment prospects,” Dr Thompson said.
“Certainly, the close-knit nature of
the [ophthalmology] profession makes networking easy and there is a culture of mentoring and supporting one another.
The flexibility to find work across public and private and through mixed models – solo practice, joining a group practice, working as a locum, doing outreach, etc. – gives trainees confidence that there is always something available to them.
“The existing workforce maldistribution highlights the many opportunities to work in regional, as well as rural and remote, settings. Finally, the diversity of ophthalmology itself means trainees have a wide choice of remaining as generalists or subspecialising or doing a combination of these.”
'We can’t risk losing talent'
One of the big headlines to come out of the 2024 survey was that 33% of all trainees had experienced and/or witnessed bullying, discrimination, harassment, sexual harassment and/or racism. This figure spiked to 54% of Aboriginal and Torres Strait Islander trainees.
For ophthalmology trainees, the number was 26% and, somewhat encouraging, they were more likely to report these instances if witnessed (40% vs 26%).
There has also been alarm at the one in five doctors in training considering a career outside of medicine. This was much lower for RANZCO trainees at 12%.
Australian Medical Association president Dr Danielle McMullen said these results

“DOCTORS IN TRAINING ARE THE FUTURE OF OUR PROFESSION AND WE MUST ENSURE THEIR TRAINING EXPERIENCES ARE VALUABLE AND ENJOYABLE SO WE DO NOT LOSE THEIR TALENT TO OTHER PROFESSIONS.”
DANIELLE MCMULLEN
were disappointing and unacceptable.
“This survey should be a major wake-up call to tackle the systemic issues that impact the training experience and wellbeing of doctors in training,” she said.
“We are disappointed doctors in training are still experiencing racism and sexual harassment, and we are particularly alarmed that 19% of all doctors in training are considering a career outside of medicine.
“Doctors in training are the future of our profession and we must ensure their training experiences are valuable and enjoyable so we do not lose their talent to other professions.”
Medical Board of Australia chair Dr Anne Tonkin was ”appalled” that 38% of Aboriginal and Torres Strait Islander trainees reported experiencing or witnessing racism, compared to 17% of other trainees.
“Clearly, our efforts to strengthen cultural safety in medicine and the health system more widely are urgent and well targeted,” she said.
But there were some bright spots, with the national quality of trainee supervision, orientation, teaching, education and training on patient safety again high. Broadly, 2024 results are stable compared to previous years.
“The value of the MTS is rock solid. What remains is a challenge to our collective ability – and will – to apply MTS data to shape strategies for positive change,” Dr Tonkin said.
continued from page 3
The initial decision to raise the fee concerned a number of bodies, including the Australian Medical Association and Private Healthcare Australia, whose CEO, Dr Rachel David, called it an “unethical new low”.
The ASO e-petition was launched through the Parliament of Australia website (EN6877) and it ended on 25 December 2024.
It stated a commission was required to regulate the private health insurance and private hospital landscape to ensure the survival of Australia’s “world-class egalitarian health system”.
In announcing the petition, ASO CEO Mr Kerry Gallagher said the Healthscope stoush was the latest in a long line of examples that reinforced the need for

the private health sector.
“Minister [Mark] Butler has clearly decided to ignore his responsibilities and is distancing himself, declaring private hospitals should resolve their own disputes with private health insurers,” Gallagher said.
“There are ongoing issues in the private health sector that are not being resolved
and are forcing the closure of services and redirecting unexpected costs on to patients, and it is everyday Australians who are losing out and questioning the value of private health insurance.
“In lieu of the intervention of government, and the elusive presence of the Commonwealth Ombudsman to provide oversight and resolve issues, it is clear the only way forward is the establishment of a private health commission,” he said.
ASO president Dr Peter Sumich said a strong private health system was essential for the sustainability of Australia’s overall healthcare landscape.
“Without appropriate funding, private hospitals may face significant challenges that threaten the safety and quality of care they provide," he said.
Mr Theo Charalambous has been appointed president and Mr Shuva Bose as vice-president of Optometry Australia (OA).
Charalambous succeeds Ms Margaret Lam, who has served in the position since 2022.
Co-opted director Mr Ramy Aziz has stepped into the role of treasurer, bringing a depth of finance, management and governance experience. And South Australian optometrist Ms Elise Pocknee-Clem joins the national board as a new director.
The appointments were announced during an OA annual general meeting on 29 November 2024.
In a statement supporting the changes, Charalambous praised Lam’s leadership of OA and acknowledged the contributions she had made to the association over the past few years.
“Margaret has been an exceptional leader, guiding the profession through significant milestones, and I’m excited to continue building on her work,” he said in the release.
“I look forward to working with my fellow colleagues to support optometrists and
advocate for better eyecare across Australia.
“I’m particularly looking forward to helping drive Optometry Australia’s new advocacy campaign to reinstate two-yearly eye exams, and the upcoming 2025 myopia awareness campaign, both of which will have lasting impacts on eye health and the optometry profession in Australia."
Charalambous joined the national board in 2021. A 2001 Bachelor of Optometry graduate from The University of Melbourne, he also holds a Senior Executive MBA from the Melbourne Business School and the Australian Institute of Company Directors course in 2022.
He entered the optometry profession in 2002, working in practices in the Berwick and Pakenham areas before opening his own independent practice, ModernEyes, in 2008. Charalambous now owns and works across a number of OPSM practices across Melbourne and an independent practice in Hastings, Victoria.
Bose has practised optometry in retail and medical settings within metropolitan and rural settings, and is currently working in an independent practice. He is also

a clinical supervisor at Queensland University of Technology, where he assists students in developing clinical diagnostics and management.
The OA statement said Aziz was the former CEO of ASX Ltd and holds a wealth of experience in the finance, strategy, risk and governance sector.
Pocknee-Clem is the managing director of three independent practices in Port Lincoln, Whyalla and Ceduna in SA and is a partner in a fourth practice in Victor Harbor. She has previously served as president of both Optometry South Australia and Optometry Victoria South Australia (OV/SA) and oversaw the integration process of OV/ SA with Optometry Australia in 2023.

Experience clearer vision with new concept designs powered by



The fovea centralis, a part of the retina with maximum visual acuity, is located slightly closer to the ear than the center of the eyeball. When a person looks at an object, their eyes unconsciously attempt to focus the image on the fovea centralis.
Tokai HR lenses utilise the fovea-centralis-transmitted-light design to focus the image on the fovea centralis, thereby improving visual clarity and increasing the eld of view.


The University of Western Australia has appointed Associate Professor Khyber Alam as the new head of the Department of Optometry and Vision Science. A/ Prof Alam is an experienced higher education leader, researcher and clinician with skills in accreditation, lecturing, curriculum mapping and organisational development. A media release announcing the appointment said he would bring a broad range of expertise to the role, where he would continue to shape the future of higher education, academic governance, health and medical education, research and community engagement. “I see the world as a small home where we all need to learn with each other, collaborate, and support one another,” he said in the release.
Indian eyewear giant Lenskart is set to spend AU$277 million building what is claimed to be the world’s largest eyewear manufacturing facility in Telangana’s Fab City. The Gurugram-based company has signed a memorandum of understanding with the Telangana government for the project, says state IT and Industries Minister Mr Duddilla Sridhar Babu. “This state-of-the-art facility will produce eyewear, lenses, sunglasses, accessories, and other products to cater to both domestic and international markets, including Southeast Asia and the Middle East,” Babu said. Led by CEO Mr Peyush Bansal, Lenskart has disrupted the eyewear industry with its click-and-mortar model. The company operates over 2,500 stores globally, including 2,000 in India, while competing with brands like Titan Eyeplus and Luxottica.
A US agency supporting medical research has announced the teams who will share up to US$125 million (AU$195m) in funds to bring about the first-ever transplant of the human eye. The Advanced Research Projects Agency for Health (ARPA-H), an agency within the US Department of Health and Human Services (HHS), has named the teams to receive awards from its Transplantation of Human Eye Allografts (THEA) program. A media release said the agency’s commitment was a groundbreaking investment to develop the first-ever complete eye transplantation procedure and restore vision for the blind and visually impaired.
An Australian study has shown that cataract surgery using multifocal intraocular lenses (mfIOLs) can achieve good outcomes for patients and be cost-effective in a public hospital setting.
Cataract surgery is a safe and effective procedure that is performed in both the private and public sectors, and advances in lens technology now offer the possibility of multifocality.
However, mfIOLs are not readily available in the public sector, due to the complexity of patient selection and of trainee experience with them.
A study at Sydney’s Westmead Hospital showed it was possible to develop a trainee-led selection pathway that ensures the cost-effectiveness of mfIOL implantation within the government funded health system.
As part of the single-surgeon prospective cohort study, 54 eyes from 27 patients underwent cataract surgery with mfIOL implantation.
The study evaluated outcomes including the resultant visual acuity, the experience of visual disturbances, dependence on glasses and patient satisfaction.
They also performed a cost analysis.
Multifocal IOLs are not available in the public system for various reasons.Image: arren Schere/ Shutterstock.com.

most patients achieved excellent visual outcomes with mfIOLs, with high satisfaction rates reported".
“Around 85% were able to see well without glasses at a distance, 81% at intermediate distances, and 59% at near distances.”
It said the conclusion was that the additional cost of mfIOLs was comparable to the cost of glasses over time, making them a cost-effective option.
“In conclusion, the study demonstrated that the selection pathway effectively addressed challenges in choosing patients for mfIOLs in public hospitals, which can facilitate access to mfIOLs for public patients.”

Federal Health Minister Mr Mark Butler has vowed to stop insurance companies using “loopholes” and unfair practices to charge people millions more for their health cover.
He said insurers were using “sleight of hand” tactics to “force some customers to take out more expensive policies”.
Those tactics, which affect many ophthalmic services, were highlighted in a recently released Commonwealth Ombudsman’s report into the way insurance companies charge their customers, including those using ophthalmic services.
The Ombudsman found that insurers were charging new customers more, with secret premium increases above what is allowed under the annual premium review process.
According to a media release from the minister’s office, the secret premium increase occurs when an insurer closes a policy to new customers and then launches a new, almost identical policy at a higher cost – a practice known as ‘product phoenixing’. This means new customers taking out
gold-tier policies are paying hundreds of dollars more than existing customers each year, and hundreds more in excess fees if they ever need to go to hospital.
Some of these gold-tier services are performed by ophthalmologists, including cataract surgery.
Butler said he shared the Commonwealth Ombudsman’s concerns that this practice “may be circumventing the premium approval processes and restricting consumer choice”.
“This ‘loophole’ tactic is a sleight of hand that makes the best value policies disappear and forces customers to take out more expensive policies,” he said.
“Insurers are putting a new name on the same policy, with a higher price tag. It’s a cheap trick that makes your health insurance more expensive, and it’s got to stop.
“Let me be clear: we will be monitoring this closely. If insurers don’t stop this practice immediately, then I will force them to stop,” said the minister.
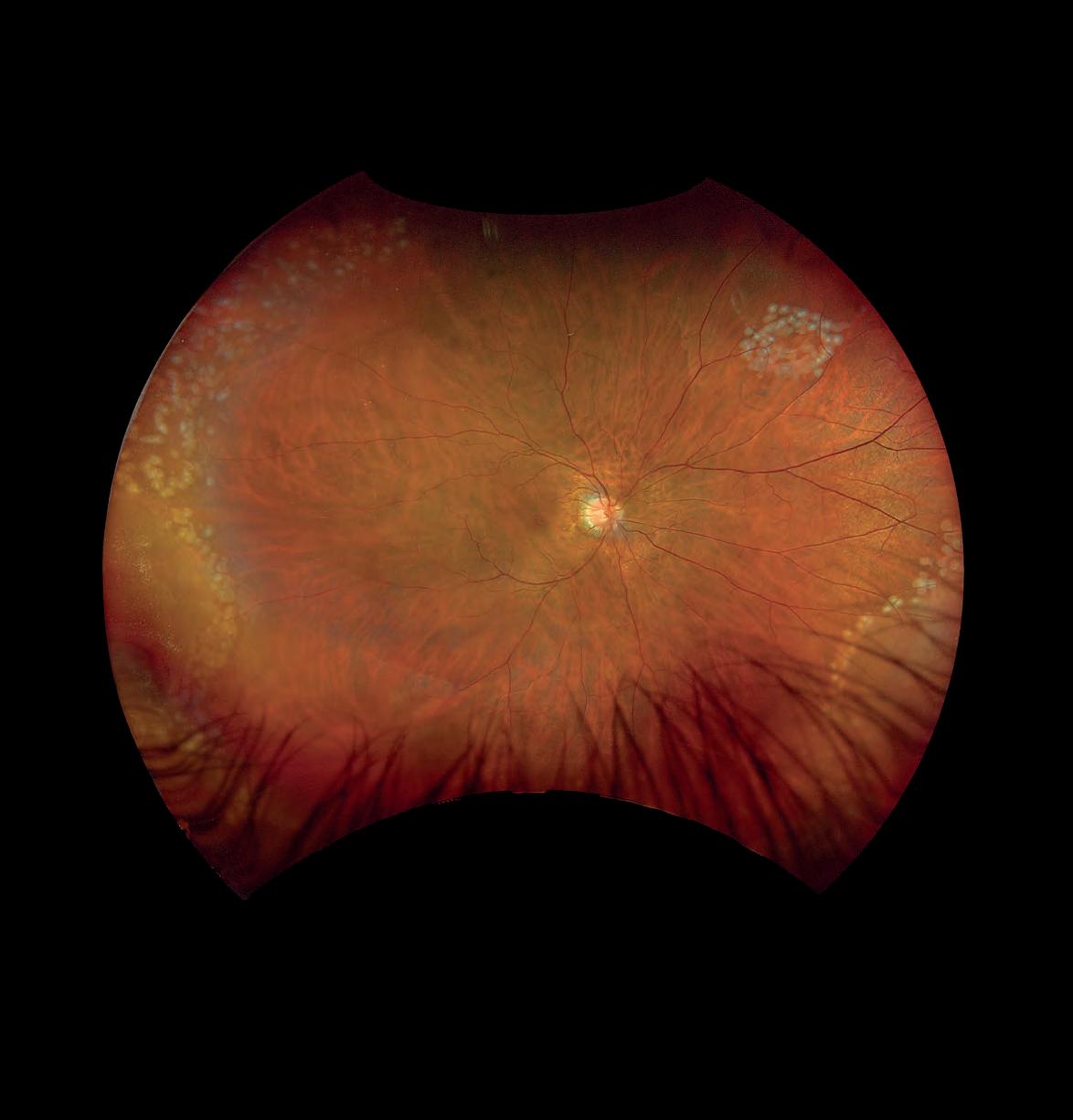
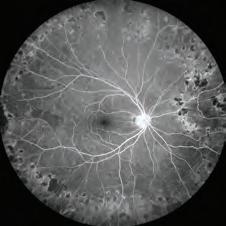
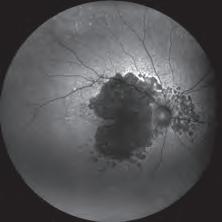
optomap®, the ONLY single-capture, 200° ultra-widefield retina image


The wait time for eye surgery is improving with at least 50% of patients now waiting almost 100 days in the public system, but the numbers are the second worst only behind ENT surgeons, according to the latest Australian Institute of Health and Welfare (AIHW) elective surgery data.
The new statistics also show public hospital admissions for elective surgery were the highest on record in 2023-24, indicating a return to pre-COVID levels of elective surgical activity.
Cataract extraction remains the most common procedure, accounting for 11% of all intended procedures. There were 83,089 cataract surgeries during this period, which is 8.4% more than the 2019-20 period.
Across all surgeries, 50% of all patients were admitted within 46 days in 2023-24, an improvement from 49 days in 2022-23.
This is a key metric in the AIHW statistics. For ophthalmology, 50% of all patients were admitted within 98 days which is double the national average.
Across all surgeries, 90% of patients were admitted within 329 days, down from 361 days in 2022-23. Around 6.4% of patients

waited more than a year – down from 9.6% in the previous reporting period (2022–23).
Ophthalmology didn’t fare as well with this metric either.
Ninety percent of patients received their surgery within 350 days, while 6.5% waited more than 365 days.
Otolaryngology, head and neck surgeons, otherwise known as ENTs, had some of the worst wait times, with 50% admitted within 111 days, 90% within 429 days and 16.5%
waiting more than a year.
But wait times have improved for eye surgery in recent years. Pre-COVID the average wait times were 82 days, but this increased to 118 days in 2020-21, 107 in 2021-22, and 105 in 2022-23. Now it’s 98 days.
The number of patients waiting more than a year for eye surgery has also come down after peaking during COVID at 12.7% in 2020-21, with this number now halved in the latest 2023-24 data.
AIHW spokesperson Ms Clara Jellie said while most elective surgeries performed in Australia were undertaken in private hospitals, the data provided an overview of elective surgeries from public hospital waitlists.
“The increase in the number of admissions from public hospital elective surgery waitlists follows a period of considerable disruption to the health system as a result of the pandemic, where we saw fluctuations in the numbers of elective surgeries being performed as outbreaks of COVID-19 impacted patients, and the availability of hospital staff and resources,” she said.


Unleash your full potential with OPSM. With our unwavering support and experience, you have the freedom to pursue an area of expertise and practice full-scope optometry. Choose the field you love and thrive with OPSM.
ACCELERATE YOUR CAREER ASPIRATIONS WITH OPSM. Visit opsm.com.au/careers today.


Optometry’s resilience during a cost-of-living crisis, big changes to medical workforce regulation and tension in the private health sector are big issues expected to spill over into 2025. Prominent industry figures offer their predictions for the year ahead, with Insight asking for the key events that will shape their area of expertise, and the matters that will keep them up at night.


Organisation:
Optometry Australia, CEO
Area of interest:
Optometry advocacy
The national cost-of-living crisis combined with an emerging workforce oversupply are placing pressures on optometry that won’t quickly abate. Whilst the profession faces challenges, there are also promising trends that bode well for a robust future for the profession, including more optometrists working more consistently to their full scope-of-practice in response to community needs and growing recognition of the benefits of integrating optometry across the health system.
Our key focus for 2025 is on supporting our members today, whilst working to grow demand for optometry services in ways that deliver for the profession and the community.
Key focal points as we move into 2025 are ensuring all Australians under 65 years can get a Medicare rebate for a comprehensive initial examination at least every two years, increasing community awareness of the need for children to have regular eye exams, introducing our advanced practice recognition program and enhancing our capacity to provide members one-to-one professional support.

Organisation:
Optical Dispensers
Australia, CEO
Area of interest:
Optical dispensing
The forthcoming release of the updated HLT47815 - Certificate IV in Optical Dispensing training package in mid-2025 promises to significantly enhance the education and training landscape. Last reviewed a decade ago, this is long overdue, and while we await the final product, employers, employees, and registered training organisations are excited about its potential implications.
Encouraging individuals to pursue an optical dispensing career has proven difficult in recent years but retaining experienced dispensers in their positions has posed a bigger challenge. While an increase in renumeration packages was evident in 2024, this must continue to keep skilled dispensers in the industry.
In response to staff shortages, ODA launched a pre-employment program in late 2024. These ‘Introduction to Optics’ courses in Melbourne during November and December surpassed capacity. It’s a promising indication of our potential growth trajectory.
The 2025 ODA International Conference (Sydney, 7-8 March) will be the largest and most engaging event Australia has seen for optical dispensers. It’s been curated with the profession in mind, featuring international speakers and a trade show with over 25 exhibitors.


Organisation:
Specsavers ANZ, managing director
Area of interest: Corporate optometry
Specsavers remains focused on changing lives through better sight and hearing and is committed to providing the best quality, accessible, and affordable services and products. We now care for five million Australians and New Zealanders annually, and our optometrists have set a new standard of 92% success rate in detecting causes of preventable blindness, resulting in sight-saving interventions for over 130,000
Following KeepSight’s success, which Specsavers has supported since its 2018 inception, I look forward to more private-public collaboration, driving detection and early vision loss intervention.
Access to eyecare continues to be a significant challenge for Australians, especially outside metro areas. We will continue pushing for Medicare funding for remote eyecare to help alleviate barriers to regular optometry care in regional and rural areas.
In 2025 and beyond, we will evolve our customer experience, blending digital, online, and in-store interaction so customers can effortlessly engage with us. Through technology investments, such as IPL for dry eye that’s being piloted in some locations, we’ll continue to provide the very best care when patients visit any one of our 450 practices across ANZ.

Organisation:
Optical Distributors and Manufacturers Association, CEO
Area of interest:
Trade suppliers and manufacturers
It will be interesting to see how the market is influenced by trends such as greater consumer control of their care, an increasingly integrated health system, the rise in direct-to-consumer marketing (i.e. lenses), and the wave of myopia control products. The increasing appetite for sustainable products will also be intriguing.
Supplier-wise, I expect greater investment in streamlined, integrated ordering systems for both eyecare- and eyewear-related sales.
I will worry about corporatisation of the optical practice market and what ODMA can do to help independents flourish, compete and foster succession plans that keep the independent market intact.
I see opportunities for suppliers to support more practices choosing to specialise or establish points of difference. ODMA could also explore consumer initiatives that drive spend through independent practices. The big priority for 2025 is increasing networking opportunities, and delivering the year’s biggest optical event, ODMAFair25, at Sydney’s ICC. Trade fair success and a practical education program are the big aims here. I’d also like to see how we can improve our research and data offering, leveraging this to help independent practices grow.

Tony Jones
Organisation:
ProVision, CEO
Area of interest: Independent optometry
As we step into 2025, ProVision is focused on supporting our members through technological adoption and continuous learning.
Artificial intelligence is ready to make a major impact in streamlining practice operations, allowing optometrists to work more efficiently. This year, we’ll be helping practices gain the confidence to adopt new technologies through digital training platforms, increasingly flexible learning methods, and additions to our own suite of innovative systems.
While there are signs that the retail environment may be slow to rebound, independent optometrists can strengthen their businesses by investing in skills to enhance customer experience and service differentiation in areas of clinical interest.
Collaboration, and the sharing of both knowledge and learnings, will ensure that independents have a sustainable future in the year ahead.

Organisation:
George & Matilda Eyecare, professional services manager
Area of Interest: Optometry & eyecare education
With cost-of-living pressures persisting, patient expectations evolving, and an uncertain economic climate ahead, 2025 will be an opportunity for optometry businesses to remain competitive and improve their clinical outcomes through practice differentiation – either via clinical specialty, eyecare technology, and/or customer service.
This will see optometrists upskill and increase their scope in areas such as myopia, dry eye, and chronic disease management. They will also integrate more deeply into the broader healthcare system, with a focus on collaborative care, hospital alignment programs, and multidisciplinary teams, to provide patients with greater value and higher-quality clinical care.
As a network of independent optometrists – each of whom run their businesses in a slightly different way based on the needs of their local community – George & Matilda Eyecare supports practices with tailored training, education, and significant investments in new eyecare technology, to ensure personalised and accessible eyecare for our patients in 2025 and beyond.


in myopia prevention and management.
With latest statistics predicting that five billion people could be myopic by 2050, this will continue to be one of the biggest threats facing healthcare for current and future generations.


Organisation:
Eyecare Plus, general manager
Area of interest
Independent optometry
Our industry is full of opportunities in 2025. If you are a young optometrist with an entrepreneurial drive, opening your own practice could be a most fulfilling decision. The generational change occurring in our industry will allow young business owners to find the perfect fit for themselves.
The next generation of optometrists are generally more digital savvy, so this will be reflected in their approach to marketing, making the clinical care aspects of optometry more visible to the broader population.
Interest rates are unfortunately remaining stubbornly high and economic forecasters keep pushing back their expected timing of a cut.
This may delay consumer purchasing decisions and keep people cautious of over-spending.
Our independent practices have a great opportunity to differentiate themselves by highlighting the ‘Locals caring for locals’ and ‘Proudly independent’ aspects of their practices.
Using social media well requires some practice, so we are providing practical assistance with that.




Organisation:
Royal Australian and New Zealand College of Ophthalmologists, president
Area of interest:
Ophthalmology
This year will be one of change and opportunity. With the launch of a new CPD ecosystem, our members will be able to focus more on robust learning activities and less on frustrating administration.
Externally, ophthalmology is in the firing line for regulatory intervention across various areas. Notably, for the assessment of international medical graduates to address a perceived shortage of ophthalmologists, which is misguided as the reality is there is a maldistribution rather than a
RANZCO will also maintain its focus on education and standard setting for current and future ophthalmologists. The college’s commitment to education underpins its other endeavours, especially in the advocacy space. In 2025, the college will be working with government and regulators in Australia and New Zealand on solutions that address equity of access to the very best in patient care. We will collaborate with all stakeholders across the vision sector to ensure the best outcomes for our patients and our communities.

Organisation:
Vision Eye Institute, ophthalmologist
Area of interest: Private ophthalmology
I was amazed at the new technology at last year’s RANZCO meeting that will make ophthalmology safer and provide better outcomes. But these advancements come with a price, which cannot always be borne by a single or even a two-person practice. Costs to purchase or lease equipment will continue to rise, as will staff costs. Small ophthalmic practices will become unsustainable, so I anticipate more clinics to be
Rules preventing patients from intravitreal injections in theatre – and therefore covered by health insurance – concern me greatly. These patients are not accustomed to paying for this service and I anticipate reluctance and disappointment. Although the advice was well intentioned, as visual outcomes are equal and the health funds would save money, shifting costs on to patients won’t be regarded as a sterling example of patient advocacy. Some people may inevitably lose vision during the transition.
We have over 100 surgeons using our operating facilities. This will likely grow as larger hospital groups may not be as tightly aligned to the needs of clinicians as we are.


Dr Peter Sumich
Organisation:
Australian Society of Ophthalmologists, president
Area of interest:
Ophthalmology
The year 2025 will have some major themes running through all aspects of business and life.
The Australian dollar is sagging under the weight of reducing commodity prices and the strengthening American dollar. Therefore, everything that comes from overseas will be more expensive. So expect medical inflation and the increasing cost of imported goods to show no signs of slowing down.
A weak Australian dollar also means no immediate relief in sight for interest rates.
We then tie the above into an election year which is likely to be in May. Expect to see private insurers apply for large 7% increases in member premiums and the health minister resist these. On the background of the Healthscope vs. Bupa battle, this will make for interesting viewing as the health minister tries to stay out of the fracas. On the sidelines of this issue, ASO launched an e-petition late last year to get a government inquiry into the feasibility of a private health authority to tidy up the sector.
We have been supported by the Australian Medical Association and other medical provider groups in this aim.

Organisation: Orthoptics Australia, president
Area of interest: Orthoptics
Allied health has been a focus in 2024 through the ‘Unleashing the Potential of our Health Workforce: Scope of Practice Review’. The proposed reforms offer significant opportunities for orthoptists and other allied health professions to work to top of scope-of-practice.
Harmonisation of legislation and removal of short-hand references to health professionals regulated by the National Registration and Accreditation Scheme (NRAS) could have a significant positive impact. We’re optimistic recommendations will be funded for implementation in the 2025 Federal Budget.
The need for better recognition of self-regulated health professions, including orthoptists, was an overarching theme of the review, prompting discussion of expanded national regulatory models through the NRAS Complexity Review. This has completed initial consultation in 2024 and will continue through 2025, with regulatory changes expected.
A key issue for self-regulated professions is the lack of national workforce data. Orthoptics Australia is undertaking a comprehensive workforce survey in 2025, allowing for greater workforce planning and to inform future directions. The National Allied Health Workforce Strategy will continue into 2025 and should prompt further reform across the health sector.


Dr Kathy Chapman
Organisation: Macular Disease Foundation
Australia, CEO
Area of interest: Macular disease
The forthcoming federal election makes this a very important advocacy year for Macular Disease Foundation Australia (MDFA).
By 2030, we project 2.1 million Australians will have a macular disease. This is a particularly concerning statistic given our health care system is already stretched to provide the necessary support to everyone living with a macular condition.
Systemic change is critical. It’s time for the Australian Government to step-up and act. MDFA is tabling recommendations that would result in greater affordability and access to sight-saving treatments, while bringing cost savings to the economy.
We know people living with macular disease need support beyond the clinic. Participant feedback from our new Eye Connect service has been extremely positive. Our focus in 2025 is to grow the number of people we support, so I encourage eyecare professionals to refer their AMD patients.
Finally, our annual Macula Month campaign commences in May. It will be underpinned by the results of our latest social impact study, including deeper insight into the impacts of vision loss on driving, and the costs associated with living with macular disease.

Organisation:
Glaucoma Australia, orthoptist patient educator
Area of interest: Glaucoma patient support
Glaucoma Australia (GA) is committed to preventing glaucoma blindness through early detection and improving patient outcomes. Our SiGHTWiSE program, supported by GA orthoptist patient educators, offers non-clinic support for patients caught-up on public hospital waiting lists or between private clinic visits. In 2025, we plan to expand this service to meet the growing demand from an ageing population and rising costs of living, which delay many patients seeing their ophthalmologists privately and further complicating disease management.
GA is also strengthening public/private partnerships, advocating for government funding and collaborating with other eyecare organisations to boost community awareness. During World Glaucoma Week, GA will host activities to encourage Australians to “get checked”.
This year will see advancements in glaucoma research, including a potential therapeutic agent by Quinlivan recipient, Professor Andrew White; patient education videos developed with UNSW to support those undergoing glaucoma surgery; and ongoing research in genetic testing.

Organisation:
Vision 2020 Australia, CEO
Area of interest: Eye health advocacy
The upcoming federal election gives the sector an opportunity to put eye health and vision care further on the political agenda with the continued rollout of our ‘Clear Vision’ election platform. We’re thrilled that a key election ask has already been accepted by the government, with $12 million committed to assistive technology in the Indo-Pacific.
Other key priorities include strengthening primary and community-based eyecare to prevent and improve early detection of eye conditions, as well as investment in early intervention services for older adults with vision loss.
First Nations eye health is an ongoing priority and we’re eager to assist our members, the First Nations Eye Health Alliance and key Aboriginal and Torres Strait Islander health organisations to progress what will be the next iteration of ‘Strong Eyes, Strong Communities’.
Finally, 2025 will also be a big year for Vision 2020 Australia, as we celebrate our 25th anniversary and reflect upon the history and success of the sector during this period.

Organisation: Keratoconus Australia, president
Area of Interest: Keratoconus
With prevalence at much higher rates (up to one in 84) than previously thought, keratoconus is becoming a major eye health issue. Its potentially severe impact on vision, quality of life and the mental health of young patients requires a meaningful policy response in 2025 from both eyecare professionals and government – something that has been sorely lacking.
We urgently need adolescent eye screening programs, including early diagnosis and referral for corneal crosslinking of young patients who are most at risk of severe vision loss from keratoconus. We also need to ensure all patients receive optimal fits of affordable speciality contact lenses, recognition of these speciality lenses as a medical device, and funding for more research, including the Save Sight Keratoconus Registry.
Peer support groups like Keratoconus Australia – marking its 25th anniversary this year – are now recognised globally as integral to best-practice health policy and patient outcomes. Keratoconus is a lifelong disease and our community needs an independent patient group advocating for systemic change while assisting individuals via peer support.
There is a desperate need to broadcast that eye rubbing can trigger and worsen keratoconus too.

In 2025 we’re expecting new therapies to make their way to Australia. The first treatments for geographic atrophy are starting to be used in the US,
And after 20 years of research, the MacTel Consortium has provided the evidence, much of it from clinical sites in Australia including CERA, that will see the first treatment for macular telangiectasia be considered
At CERA, in 2025 we aim to increase referrals into Cerulea Clinical Trials for clinical trials and establish registries, particularly of people with early disease so that we can be ready for when new trials come. Funding of research and researchers in general is always a challenge – particularly funding for a treatment trial for intermediate age-related macular degeneration.

A/Prof Mitchell D Anjou AM
Organisation:
Minum Barreng: Indigenous Eye Health Unit, The University of Melbourne, director Area of interest: First Nations eye health
Make space, step back and support self-determination. In 2025 I hope we see a new national plan for Aboriginal and Torres Strait Islander eye health – led entirely by First Nations people. Allies and whitefella organisations must better align with blakfella leadership and it would be great if peak bodies like NACCHO and FNEHA could clarify roles, and through their expertise and strong sector engagement drive improved eye health and vision care outcomes.
At Minum Barreng: Indigenous Eye Health Unit, we’re transitioning our work to First Nations organisations and leaders, whilst maintaining our focus on trachoma elimination, eye health promotion, supporting systems improvement and reform through jurisdictional and regional stakeholder groups, and research capacity development.
The sector is looking forward to a great FNEHA national conference in Boorloo (Perth) in May. Meanwhile, optometry must take some meaningful steps to improve recruitment, retention and graduation of First Nations optometrists.
Let 2025 be a year of bold leadership and transformative action in Aboriginal and Torres Strait Islander eye health.


Organisation: Australian Vision Research, chair
Area of interest:
Ophthalmic research
Australia ranks as one of the top three most productive countries for ophthalmology research when measured by publications adjusted for population. Australian Vision Research has supported these research efforts by investing over $15 million over the past 70 years. Our funding has helped to support the development of a highly skilled ophthalmic research workforce. The challenge for our organisation is to keep our funding at levels that can support researcher’s careers and keep pace with rising research costs; for this we are reliant on donors and sponsors such as the Perth Eye Foundation, NSW RANZCO and ANZSRS.
With our new fund-raising committee we are looking for new donors and sponsors. In 2025, our annual research grant program will be seeking applicants, including those wanting to start a research career via our priming grants and for the second year we will be honouring Australian ophthalmic researchers via our Excellence Awards.

Organisation:
First Nations Eye Health Alliance, CEO Area of interest: First Nations eye health
In 2025, we anticipate a growth in the capability of the Aboriginal and Torres Strait Islander eyecare sector through the amplification of First Nations leadership and voices.
We look forward to, with other First Nations agencies, leading the development of the next Aboriginal and Torres Strait Islander eye health plan, along with building pathways that prioritise prevention and early intervention to offset future poor eye health risks for our communities. An immediate and future priority is to ensure the requisite improvements to systems and workforce infrastructure are made to meet the projected First Nations eyecare service and workforce gaps into 2030.
First Nations children and people living with diabetes are a funding priority, along with Aboriginal and Torres Strait Islander agencies, which are best placed to integrate cultural principles and knowledge needed to strengthen models of care for First Nations people and close the gap in vision.

Alcon’s new Unity surgical systems are setting the scene for the way vitreoretinal and cataract surgery will be performed for the next decade, says an Australian ophthalmologist who performed the world’s first human case with the platform.
Early in 2024, Australian vitreoretinal surgeon Professor Andrew Chang performed surgery to peel an epiretinal membrane at Sydney Retinal & Day Surgery. It was a momentous occasion, not just because of the impact on the patient, but because of the implications for patients globally.
It was the world’s first human surgery using Alcon’s new vitreoretinal cataract system that Prof Chang anticipates will set new standards in ophthalmic operating rooms.
At the time, the system was not yet approved in any country, so he was sworn to confidentiality alongside seven other Australian ophthalmologists who also had early access, including fellow Sydney vitreoretinal surgeon Professor Adrian Fung.
That all changed in October 2024, just before the 2024 RANZCO Congress, when the new Unity Vitreoretinal Cataract System (VCS) and Unity Cataract System (CS) were included on the Australian Register of Therapeutic Goods (ARTG) and notified to the WAND database in New Zealand – the first markets outside the US to have the technology available.
Alcon has tested Unity VCS and Unity CS during investigational advisory wet lab sessions with more than 200 experienced surgeons from 30-plus countries. The technology will supersede its Constellation Vision System for vitreoretinal and combined procedures, and the Centurion Vision System with Active Sentry for cataract surgery.
ANZ will become one of the first jurisdictions with commercial access to the all-new Unity product line, which Alcon plans to expand, and Prof Chang is excited about the possibilities.
“It will be the machine for the next decade,” he says.
Prof Fung concurs it will revolutionise vitreoretinal surgery.
From the get-go it was clear the Alcon engineers had gone back to the drawing board to re-engineer the vitreoretinal system from the ground up.
“Unity VCS isn’t just a minor evolution of the current Constellation and Centurion systems, it’s a complete overhaul of those platforms.”
Unity VCS integrates vitreoretinal and cataract surgical capabilities in one device. It also has optional laser capabilities in photocoagulation.
Meanwhile, on the same system, surgeons can opt for Unity CS as a standalone system for phacoemulsification cataract surgery.
Either way, surgeons using Unity VCS or CS will have access to Alcon’s best-in-class cataract and phacoemulsification technology.
Unity VCS provides surgeons and technicians the benefits of maximised operating room space with a single device, something Prof Chang predicts will be particularly attractive to public hospitals.
As part of the multi-site trial beginning in February 2024, Prof Chang, Prof Fung and the other principal investigators performed surgeries using Unity VCS for a range of pathologies, including retinal detachments, diabetes-related tractional retinal detachments, simple macular surgery and combined vitrectomy and cataract cases.
Alcon engineers flew in for the first cases to explain how the machine was responding in real time. All up, the Australian contingent of surgeons performed over 120 cases to pave the way towards regulatory approvals.
“It has been an amazing opportunity for Australian vitreoretinal surgeons to have participated in this,” Prof Chang says.
“The technology recognises a real trend in ophthalmology, that surgical sub-specialists are merging surgeries on the front and back of the eye. Vitreoretinal surgeons are doing more anterior segment work, and anterior segment surgeons are using some vitreous capability to perform middle segment surgery.”
At the November 2024 RANZCO Congress, Unity was a hot topic, and Alcon had the system in a closed-off room where selected surgeons could provide feedback.
The company flew Mr Daniel Velasco, international product director, next generation surgical platform, in from Barcelona to support the launch. Alongside Ms Penny Stewart, cluster franchise head surgical and country manager ANZ, they discussed the major step change with Unity.
“For cataract, we now have a phacoemulsification modality that will deliver up to two times faster nucleus removal^ with 40% less energy* into the eye1,” Stewart says.
“And in vitreoretinal, the new technology will offer cutting speeds of up to 30,000 cuts per minute#2, so the platform offers surgical stability and efficiency, along with a unique proprietary fluidics system3 that we will share more about with the commercial launch in 2025.”
According to Prof Chang, the reason Alcon Unity marks a significant shift over traditional systems largely comes down to the new generation dual peristaltic and vacuum pump system.
By applying this to both the Unity VCS and Unity CS, it meets the growing demand for surgical systems that allow surgeons to perform accurate and predictable surgery, switching between the anterior and posterior segments with relative ease and confidence.
“Traditionally, anterior segment machines used peristaltic pumps that squeeze fluid through tubes to achieve suction. Posterior segment retinal work conventionally used vacuum pumps to produce suction,” he says.
“The major innovation is adopting a peristaltic pump system for both cataract and vitreoretinal work. Fluid flow is more controlled and accurate and very high vacuum can be achieved. "That’s an advantage, especially for the posterior segment.”
Prof Fung adds the system can intelligently detect flow resistance – for

instance whether the vitrectomy tip is in vitreous, fluid or air – and adjust the fluidics accordingly. “One can operate at a lower IOP with high vacuum. This flow control-based system will alter the way we perform vitrectomy surgeries and make it safer.”
Prof Chang says enhanced predictability with Unity VCS is key for vitreoretinal surgeons performing highly intricate procedures, sometimes near mobile retina.
Alcon has also made improvements to 27-gauge probe, something Prof Fung says has been dynamically stiffened to act like a 25-gauge probe. This will make it more appealing for vitreoretinal surgeons to use 27-gauge as their standard set-up.

Prof Chang says with smaller gauge probes surgeons can access micro surgical tissue planes more effectively, while smaller access wounds are advantageous for recovery. Silicone oil can even be injected through the 27-gauge cannula, Prof Fung notes.
There’s been other advances, like redesigned ports that allow instrumentation to more readily pass through into the eye, a customised adhesive for the infusion line and an all-new wireless foot pedal.
“These innovations make the surgeon’s experience so much better,” says Prof Fung. “The LED illumination has improved colour control, allowing for improved tissue visualisation. The use of yellow light can reduce reflections during fluid air exchange, and green light may be beneficial when performing internal limiting membrane peeling.”
Another key feature in Unity VCS is a Tetraspot Multi-Port laser probe, producing a four spot pattern laser burn.
“In the Unity system, every time you put your foot down, the four burn pattern laser allows the procedure to be performed quicker and evenly,” Prof Chang says.
And Prof Chang says Alcon has aligned the user interfaces, so it is the same for both cataract and vitreoretinal surgery.
It means scrub nurses can more effortlessly switch between posterior and

Image: Adrian Fung.
anterior segment when setting up for surgery.
It’s something that struck Prof Fung too.
“Compared to the Constellation, the Unity VCS is smaller and more streamlined in design. It has a much faster set-up and tear down for the nurses, with notably less tubing. Even the wheels have been re-designed with cable pushers on casters to make the unit more mobile and user-friendly.”
After performing combined procedures, Prof Chang expects cataract surgeons to experience improvements, pointing to new technology dubbed 4D phaco.
“Here, the phaco tip changes shape and direction to quickly pulverize the lens. It rapidly removes the cataract, evenly and smoothly – that was immediately obvious.”
For Prof Fung, he’s never performed phacoemulsification as quickly as with the Unity platform. “The increased speed is immediately noticeable”.
This is also assisted by Intelligent Sentry, which mitigates phacoemulsification surge and a Thermal Sentry to avoid wound burn, he notes. The fragmatome has been reduced down to 22-gauge too.
“This allows for much more efficient fragmentation of dropped nuclei through a smaller wound.”
With Unity VCS and CS, Prof Chang notes “everything’s changed”.
“It’s not just the machine itself. It’s the instrumentation, the forceps, the cutter speed, the foot pedal and laser probes.”
He likened the experience with Unity to driving a new race car. During the first lap, the all-new engine, steering, gearbox and brakes produced noticeable differences in performance. “I’ve been using Alcon equipment for a while, and you could really feel fluid moving differently.”
Prof Fung also uses a car analogy to describe the difference.
“Today’s modern cars are increasingly computerised with automated features like lane assist, active emergency braking, adaptive cruise control; there’s a lot of systems in the Unity platform that help the surgeon avoid problems with either collapse of the globe or issues with IOP.”
Australia and New Zealand will be among the first to have Unity available commercially in 2025.
With Unity VCS expected first, it will be a phased launch followed by Unity CS and a new range of consumables. Current handpieces, like the Active Sentry, are still compatible, but Unity itself has its own next generation handpiece.
Velasco says Alcon painted a clear picture of surgeons’ needs and has delivered on this with Unity VCS and CS.
“The two main objectives we had when we started developing this project were stability and efficiency,” Velasco says.
“It might sound obvious but the two don’t always go together. Maybe you can increase the stability, but then you lose efficiency. And if you’re seeking to increase speed, creating more efficiency, then you sacrifice stability. To increase both at the same time hasn’t been easy.”
And after speaking to ophthalmologists at the RANZCO Congress, Stewart says local surgeons noticed this difference.
“Unity
VCS isn’t just a minor evolution of the current Constellation and Centurion systems, it’s a complete overhaul of those platforms.”
Prof Adrian Fung Principal investigator
“We hear a lot from surgeons thinking technology like this is going to be an upgrade to an existing system, but it’s really not – it’s a whole new innovation,” she says.
“We can make claims around the efficiency, but is that actually going to be felt and experienced in the theatre and in the surgeon’s hands? And do they feel that extra level of stability? From surgeons who have experienced it so far, we’re hearing that it is.”
^ 2x faster nucleus removal than OZIL Torsional phaco
* Based on N=10 HPs, Artificial cataract lens IOP 55mmhg vacuum of 450 mmHg
#Compared to Constellation HYPERVIT 20k vitrectomy probe
REFERENCES:
1. Alcon Data on File, 2024 - REF-24379.
2. Alcon Data on File, REF- 24644.
3. Unity VCS and CS User Manual 2024 – REF -24980.


Advocates for contact lenses in Australia are a committed bunch, but as Insight finds out, they make a good argument that others in their industry may be missing out on a chance to improve not only their patients’ vision but their practices’ bottom line.
It’s one of the great ophthalmic mysteries.
Australia is a country known for its love of the outdoors and the many sports enjoyed in the long, hot sun that bakes the Lucky Country.

But despite this clear leaning towards an active, outdoor lifestyle, the people enjoying it have not warmed to the full spectrum of vision-correction tools that would help them make the most of it.
Contact lenses don’t always get the love they perhaps deserve in the shadow of those flashy, fashionable frames, and appear to be largely consigned to those patients whose optometrists actively suggest them, or to those experiencing very specific eye conditions.
And the experts interviewed by Insight are among many to scratch their heads and wonder why that is, despite Australia’s world-leading research, innovation and education in the area. And, of course, the satisfaction patients can achieve in contact lenses or as a ‘dual wearer’.
Part of the problem lies in traditional barriers to contact lens adoption, including well-documented fears about putting something in your eye, hygiene and the risk of infection, and cost.
These are common issues around the world.

“Look at dentists – they don’t make money
on toothpaste
and toothbrushes, so why should we make money on contact lenses, right?”
But those experts also highlight the industry’s role in this particular Australian mystery, including some business models that don’t always build in adequate time, resources and capacity to sit down with patients for a contact lens consult.
Let’s get to that later.
Firstly, let’s consider the opportunities in promoting contact lenses. Depending on what you read, there is reportedly plenty of growth tipped for the global contact lens market.
Reports from international market analysts, including Coherent Market Insights and Fortune Business Insights, value the industry at between US$10.45 billion and US$19.52 b. In Aussie money that’s between AU$16.25b and AU$30.35b.
And they expect that to grow by between 6.5% and 8.7% in compound annual growth (CAGR) in the next seven to eight years.
Despite that global market being worth many billions of dollars, Australia generated just AU$190m in contact lens sales in 2024, according to Germany-based online data-gathering platform Statista.
That suggests there is plenty of room to move if Australia is to realise the full potential of the contact lens market.
Beyond the macro trends, there are many benefits at the practice level too, as pointed out by a number of experts and practitioners.
They believe that investing more time in a patient and discussing options that include contact lenses builds greater trust, increases loyalty and encourages more referrals from friends and family.
They are also less likely to source their contacts online, preferring to deal
with the practice. And these practices are finding plenty of ways to get round what others see as barriers with contact lenses.
As Optometry Australia’s 2020 Vision Index confirms, for a number of reasons, contact lenses continue to strike the glass ceiling with patients.
Two-thirds of the 1000 Australians surveyed wore prescription glasses, with just 13% in prescription contact lenses.
But the same survey revealed that 41% of Australians would prefer to wear contact lenses over glasses while playing sport, even if many didn’t end up doing so.
Intriguingly, other figures suggest that might be because they were either discouraged from wearing contact lenses by their optometrist or possibly not offered them as an option at all.
A US study of consumer perceptions by the Contact Lens Institute (CLI), which would be of interest to Australian practitioners, shows among glasses-only wearers, contact lens trials are largely underutilised.
Thirty-two per cent of that patient population said that a free trial would increase their consideration. Yet among the subset who reported that contact lenses were discussed at their most recent exam, only 10% were subsequently offered trials.
CLI says “our profession has inadvertently made glasses and contacts an ‘either-or’ selection, when the real choice lies in having the ability to pick between the two on any given day and time to suit ever-changing environments”.
Another figure hints at an opportunity lost – at least for now.
The Contact Lens Spectrum has been monitoring the market for close to 30 years.
It started in 1996 as a United Kingdom-only initiative but now collects data from 71 countries.
Its figures show that, similar to other nations, Australia’s uptake of contacts surged around 2007, with the evolution and growing popularity of disposable

soft contact lenses. That continued over the next decade but once again hit the glass ceiling and plateaued around 2017, leaving Australia possibly lagging behind other countries, and certainly its counterparts in the Asia-Pacific region.
So the opportunity exists, but how can Australia fully realise it?
Associate Professor Tony Phillips knows plenty about the value of contact lenses for patients and practices, and the loss of opportunity in not promoting them to a wider group.
Few have done more in Australia to advocate for the use of contacts, drive innovation of the product and train others in their use than the now-retired A/Prof Phillips.
So significant has his contribution been over almost six decades that he was recently awarded the 2024 Ken Ball Medal by the Cornea and Contact Lens Society of Australia (CCLSA).
A/Prof Phillips moved to Australia from the UK in the early 80s to join SOLA Optical, an Adelaide-based company looking to develop the world’s first disposable contact lens.
“I had to fit rabbits with lenses; all that was done and we went on to the human trials,” he says.
“The case design was all finalised, and we had a really good product that seemed to work extremely well.”
But like earlier, unsuccessful versions of their world-first design, the project began to unravel due to personnel changes and politics and was then shelved.
“The sad thing was that, at that point, we were several years ahead of the rest of the world.”
To this day, A/Prof Phillips struggles with the short-sightedness of that decision.
And he’s equally perplexed about why contact lens penetration is behind where he might expect it to be in Australia.
“I’ve no idea why,” he says. “We’ve got very good practitioners. The training is very good.”
After a little more prodding, A/Prof Phillips suggests that Australia’s largely hot, dry climate might not be ideal for contact lenses, possibly exacerbating any irritation.
But like others, he thinks more could be done to create a framework that supports contact lens prescribing.
“It’s so much easier and less time involved to simply prescribe spectacles,” he says, “and the Medicare fees when involved are very low if they are intended to cover an initial fitting appointment, an instruction session and an average of, say, two after-care follow-ups.
“With many optometrists being pressured to cut the examination time down, this does not leave sufficient time to discuss alternative corrective options such as contact lenses, the types of lens available, and the various pros and cons.”
He believes the points noted above have taken the “fun and clinical challenge” out of fitting lenses and that some of this could be addressed by practices charging above the Medicare rebate, to make contact lens visits a more viable financial option.
That would also give professionals more time to discuss lenses and at least give patients an option.
Mr Gavin Swatz acknowledges that contacts can be a challenge for some businesses and their commercial models.
Swatz is director and chairman of the Abernethy Owens group of optometry practices in Western Australia. He is also the vice-president of CCLSA, a lecturer in contact lens use at the University of Western Australia and is completing a PhD on different ways to improve outcomes in complex keratoconus cases.
He got into optometry because he felt it was the perfect mix of health and physical sciences, but he realises that many businesses sometimes struggle to offer a perfect mix of options for patients with vision issues.
“I think that sometimes there is a lack of time to spend with patients, fitting multifocal lenses and the number of visits required,” he says.
“I think a lot of optometrists might shy away from them, and some environments aren’t necessarily as conducive to spending time on the more complicated cases.”
Frames also appeared to make more cents and sense on the bottom line too.
“There’s certainly bigger margins in glasses than there are in disposable contact lenses, and the internet sellers have really commoditised the disposable lens, where it’s really become a volume game.”
But there remains a major advantage in the contact lens space, especially for independent practices.
“I think that’s when independents need to be looking for their points of difference,” says Swatz.
“If you’re trying to compete with corporates on the same playing field, you’re not going to win, so you need to be looking at service-based offerings that really enhance that care for your patients.”
Beyond those patients for whom contact lenses were the best option, there were potentially many others who may not have thought that they could wear contacts occasionally.
As the Vision Index 2020 figures showed, 41% of Australians would prefer to wear contact lenses while playing sport but some were discouraged from doing so by their optometrists and other perceived barriers.
“There’s certainly a lot of patients who wear spectacles and think that they can’t wear contact lenses, and would like the opportunity to be able to wear contact lenses when they’re going out, going to the gym, etc,” Swatz says.
“So you’re not losing the spectacle business; you’re actually enhancing that
"With many optometrists being pressured to cut the examination time down, this does not leave sufficient time to discuss alternative corrective options such as contact lenses, the types of lens available, and the various pros and cons.”
A/ Prof Tony Phillips Retired
and increasing that engagement of that patient in your practice.”
More time spent with these patients on fitting, instruction and follow-up helped to establish a relationship of trust and increase the likelihood they would return for help with other vision issues and spread the word among family and friends.
But that time was valuable in a busy practice with a premium on chair time.
To help with that, Swatz empowers a team member to be the “champion” for contact lenses within the practice.
“They can have insertion and removal instruction sessions booked into a spare room to free up your clinic chair time,” he says.
“It’s always great to ‘pop in’ on these sessions to see how they’re going and offer encouragement, as this gives the patient confidence that this session is under your oversight.”
The practice and the patient have gained even more confidence from the advancements in contact lens technology, which have lowered many of the traditional, troublesome barriers for uptake.
“The advances in corneal topography and the associated software have enhanced our ability to understand our patient’s corneal shape,” says Swatz.
“This allows us to better understand potential outcomes and make better lens choices. The improvements in access to corneal tomographic devices like the Cylite HP-OCT means we can have more accurate data on highly complex corneas for specialty lens fitting.”
That technology has also helped in the ongoing competition from online providers.
“These lenses are tailored specifically to meet the needs of our patients and are unable to be offered by online retailers that otherwise treat contact lenses as a commodity, rather than the medical device that they are.”
Also, to help with the financing, Swatz charges a fitting fee that may or may not be covered by Medicare, depending on the circumstances, and he issues 12-month prescriptions for contact lenses, encouraging the patient to return for further check-ups.
Ms Jessica Chi understands the opportunities and advantages that contact lenses can bring – professionally but also on a personal level.
Before she became an optometrist, the owner of Eyetech Optometrists in Carlton, Melbourne; the Victorian president of the CCLSA; and a contact lens specialist, Chi was a young myope who lacked confidence.
“I remember putting glasses on for the first time and thinking, ‘Oh, my God, everything is so clear’,” she says.
That helped her vision, but not her confidence; she was desperate to fit in but couldn’t help standing out because she was overly tall and not many others were wearing glasses back then.
“I hated wearing them,” says Chi. “I thought they made me look like such a nerd.
“So I became quite shy and introverted, and often I would not wear my glasses, which further reduced my confidence because I couldn’t see.
“At 13 I started wearing contact lenses, and I know it sounds really cliche, but they really changed my life, especially with sport and also just selfconfidence.”
It’s part of the reason why she has always been so passionate about contact lenses. That passion drove her to specialty contact lenses, with her clinic prescribing a large number of orthokeratology, for keratoconus and irregular cornea and ocular injuries.
Those can be tricky and time-consuming, so much so that a third of the practice’s referrals come from other optometrists.
She understands that time is money in the competitive optometry business, which is why, like Swatz, she will do the main consult and then pass the patients on to other staff.
“I don’t do the tuitions at my practice,” she says. “If you delegate that to one of the other staff, then they can spend two hours with the patients and they’re not

eating into the more valuable optometry chair time.”
Neither is she too hung up about selling contact lenses.
“If you charge appropriately for your services, then with the contact lenses, if they buy from you, great; if they don’t, then you haven’t lost anything.
“Look at dentists – they don’t make money on toothpaste and toothbrushes, so why should we make money on contact lenses, right?”
She admitted there was not a lot of money to be made in soft contacts, but the margin on specialty contact lenses was high because they were custom-designed – “and that’s not something that they can buy on the internet”.
Chi thought many optometrists were missing out by not offering contact lenses to complement their patients’ glasses.
“It’s very rarely glasses or contacts, because most people that wear contact lenses will need glasses as well.
“And it might be too difficult to wear contacts and be comfortable all day, but it doesn’t mean that they can’t have something to wear for social occasions or on the weekend or when they’re playing sports.”
That was simply about giving people the option.
Chi’s practice will start doing that from the first interaction with a patient.
“We ask them, when they book in, whether it’s for glasses and or contact lenses. We ask them if they want contacts, if they wear contacts, or if they’re interested in contacts. And our optometrists will always talk about contact lenses during the consult.”
They are also happy to promote themselves as confident wearers of contact lenses. And they have some novel ways to address concerns and fears.
Chi will offer patients contacts lenses to help them choose their frames.
“They think that it’s going to be uncomfortable, that they’ve got something plastic in the eyes, but then if you can get it into the eyes and they can feel it, they can feel actually really comfortable.”
Fear about putting something in the eye can be conquered with practice and support. Even plenty of return visits.
That creates plenty of touchpoints, says Chi, “because you’ll see them for the fitting, you’ll see them for the aftercare, you’ll see them pick up the contacts and all the glasses, and so then they have the familiarity with you, and so it builds patient loyalty, which often can drive referrals.”
A third of the referrals to Chi’s practice are from other patients.
That can also build revenue.
“It’s just plus, plus, plus – you have the glasses, but then you have the contacts as well.
"Then you’ve also got the consult fees. The patient has also had an experience, which they may or may not have thought they could do, but they’re much more likely to refer someone on to you.”
And that’s bound to boost the confidence of even the shyest optometrist.




A South Australian independent describes how the locally produced HP-OCT is paving the way for empirically fit contact lenses, offering hope for patients otherwise resigned to a lifetime of sub-optimal vision.
Few clinicians in Australia would have a better vantage point than Mr Lachlan Hoy to appreciate just how revolutionary the Cylite Hyperparallel OCT (HP-OCT) will be in the advanced contact lens arena.

And he’s quick to point out that it’s still early days with more to come for the Australian designed and manufactured instrument.
As one of Australia’s pre-eminent contact lens practitioners, Hoy has made this interest a cornerstone of his independent practice, Innovative Eye Care, often seeing patients with irregular corneas who have had little luck obtaining good vision correction.
A little over a year ago, the Adelaide practice added the HP-OCT to its arsenal and the device is quickly filling the role of multiple other instruments to capture essential corneal data for advanced contact lens designs.
As if he isn’t busy enough, across the hallway he runs a contact lens manufacturing business, EyeSpace, that produces topography-guided scleral, orthokeratology and rigid gas permeable (RGP) contact lenses. The goal is to make custom-fit lenses using a simulation of the patient’s eye, moving away from the guesswork involved in traditional trial fitting.
EyeSpace also recently integrated with the HP-OCT’s software, streamlining the lens ordering process for practitioners using the device.
Stradling the clinical and manufacturing fields, you’d be hard-pressed to find someone more qualified in real-world optometry to discuss the HP-OCT.
The Melbourne-made system, commercially available since September 2023, is finding a home among independent optometrists here and abroad, offering a new edge to contact lens prescribing, as well as myopia and corneal disease management.
From the get-go, Hoy is already envisaging how the HP-OCT – and its “phenomenal” anterior segment imaging capabilities – will lift an already-good 85% first-time fit rate for corneal contact lenses to around 95%.
“But where it's really going to change lives is for patients with major astigmatism from corneal grafts and keratoconic eyes with irregular cornea that are extraordinarily difficult to fit and manage.”
There’s also the potential to reduce corneal re-graft surgeries, reluctantly offered to people struggling with vision correction after an initial surgery.
“By providing these patients with good vision with RGP lenses – because we can now measure their eye with a 3D volumetric scan to produce a custom-made lens – that's life-changing. These people end up with 6/6 or 6/5 vision, starting from a place of 6/30 or 6/40.”
Hoy has a saying with empirically designed contact lenses: “Rubbish in equals rubbish out”.
He’s referring to how sub-optimal data will deliver poor contact lens designs and results.
But the opposite is true too, and the HP-OCT has entered a new realm by
delivering insights previously unattainable for patient and practice.
“With the Cylite OCT, suddenly you've got amazingly accurate central corneal data, you've got data past the limbus to the sclera, posterior corneal elevation, epithelial thickness, full anterior chamber, lens thickness, axial length,” he says.
“It's everything, and it's fast.”
That’s because the HP-OCT offers industry-leading 302,400 A-scans per second. It can simultaneously image across a wide area of the eye with minimal motion artefacts.
In one scan, the system captures a full 3D image of the anterior segment. It means optometrists like Hoy can slice and cut in any direction, X, Y or Z axis – all without any gaps, holes or B-scan stitching artefacts to manage. For contact lens practitioners, they can deliver personalised fitting with highly accurate and repeatable elevation and curvature maps.
Other biometric measurements, including axial length, support myopia management, plus the same volumetric imaging technique can be applied to the posterior segment to produce volumetric retinal images.
“What Cylite has achieved with their beam splitting technology is unreal,” Hoy says. “The ability to instantaneously be capturing a 9.4 x 16.6 mm grid at more than 300,000 scans per second is phenomenal.
“The depth of the scan is enormous and they’ve built beautiful hardware. In the contact lens space, it's providing so much data to create essentially freeform contact lenses. That's where the manufacturing technology is changing; a CNC lathe can manufacture nearly anything you can throw in it.”
Optometrist Mr Wes Butler has been with Innovative Eye Care since 2023 and, under the mentorship of Hoy, sees a lot of “weird and wonderful eyes”, often referred from other optometrists.
He has access to several high-end instruments for advanced contact lens prescribing.
These include Scheimpflug imaging, offering combined corneal
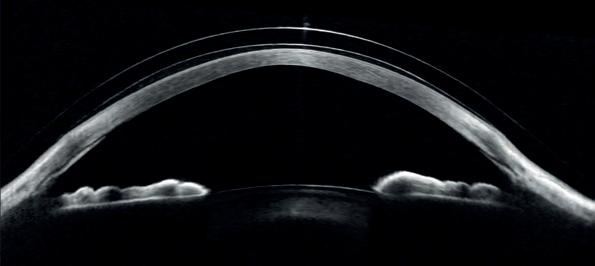
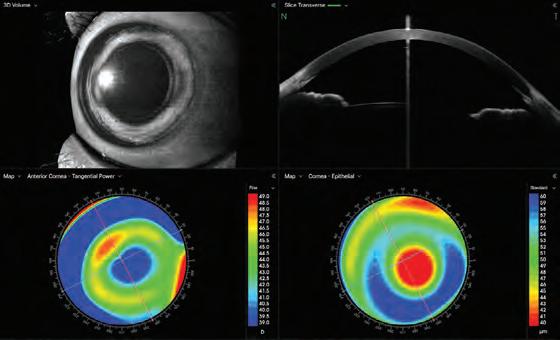
tomography, scleral shape, axial length and wavefront aberrometry; an anterior segment OCT machine; placido-ring corneal topographer, plus others.
While they perform well in their own right, limitations exist, meaning Butler and colleagues tend to jump across devices, depending on the case.
For example, he notes the quality of data taken from placido-based instruments is tear-film dependent and might only be able to cover 9 mm horizontally and 6-7 mm vertically. Other devices can measure limbus-to-limbus horizontally, though are impeded by eyelids vertically, making it difficult for Asian eyes.
Elevation-based instruments perform incredibly well and capture data across a wide area, though often take longer to capture, making them subject to eye movement.
While acknowledging the HP-OCT isn’t entirely free from “kinks”, it’s already at an extremely high standard.
“By performing a quick and enormously wide field scan that also measures axial length, coupled with very intuitive web-based software that’s regularly updated, it feels as though Cylite ticks a lot of boxes in terms of convenience,” Butler says.
“It's great to have access to a wide range of instruments, and they are brilliant in their own right, but my preference would be to reduce overall chair time. We’re big advocates for software-based, empirical contact lens fitting. The ethos is: as quickly and as reliably as you can get that data, the better, and the HP-OCT delivers on that.”
As such, Innovative Eye Care has altered its workflow so that all new orthok patients are put through Cylite’s system, with Hoy anticipating it will become more of a workhorse in future.
“And that comes with the confidence that the data is good, the clinical workflow is good, the speed is good, and the software is now where we want it to be,” Hoy says.
“If all these boxes are ticked, then why wouldn't we fully adopt it? The software is such now that our clinic is set up with six consulting rooms, and our optometrists can review the results at their own stations – that's a key requirement for us and the team at Cylite have managed to do that.”
Butler is already seeing how the HP-OCT can improve orthok fitting. A common pain point when troubleshooting a poorly performing lens is the month-long wait to see improvements, without knowing whether the baseline data or the lens design is at fault.
“With Cylite’s HP-OCT, the scan is completely volumetric. You can take height measurements from anywhere on the cornea, so if a lens doesn't behave as expected on the eye, you can make the necessary adjustments and completely trust what you’ve done will come out as intended,” he says.
“There have been instances where we have been struggling to
troubleshoot poorly performing orthok lenses that seemed perfect on paper, and the HP-OCT was able to shed a light on the problem, as it provided so much more data that we didn't have at initial fitting.”
Cylite’s HP-OCT is also able to capture an expanded 16.6x16.6mm area, and within several seconds Butler says it collects the elevation and landing angles of large-diameter scleral contact lenses, while simultaneously imaging the cornea underneath the lens.
Beyond the image acquisition, Butler notes how easy HP-OCT’s user interface is to use.
It’s one of the advantages of having a web-based platform, with updates easily rolled out.
“The software is intuitive, and if you want to know the axial length, front surface curvature and corneal thickness, you can set your own reports, so that it presents the data how you want for every patient,” he says.
“That was only added in recent months, but what’s cool is they are constantly responding to feedback, and making updates quickly.”
For Hoy, technology like the HP-OCT brings him closer to the ultimate aim of EyeSpace, a business he devised on Friday nights over pizza and beer with a friend studying high computation physics.
Realising the untapped potential of devices capturing 3D images of the anterior segment, he saw an opportunity with computer-simulated contact lens fitting.
“You don’t need to put a lens in the eye to see how it fits. You can do that with a computer program that works quickly, and it means you don't have to be a practitioner who's fitted thousands of rigid lenses.”
Actively supplying the industry since 2013, the first instrument EyeSpace integrated its manufacturing software with was the Medmont E300, with many others following.
Wind forward to 2024, the integration with Cylite’s HP-OCT represents a significant leap that will enable EyeSapce to obtain better data for more individualised lens designs.
One of the big challenges has been working out how to handle delivering the “enormous” amount of data that comes with a HP-OCT scan.
“We want to create something that's simplified and easy-to-use, that provides clinical workflows that optometrists and ophthalmologists can follow for these highly complex lenses. Then it’s dealing with the manufacturing capabilities because technologies like HP-OCT are unlocking a whole new understanding of the ocular surface.
“But it's more about what's to come. It’s similar to the challenges Cylite has ahead of them. They’ve built this amazing hardware, but then developing the software to analyse it and make it increasingly more clinically useful, they’ve got a lot of exciting work ahead of them.
“And it’s the same for EyeSpace. We've got five software developers and five optometrists also working on this, trying to find innovative solutions to complex problems, and it’s a challenge we’re excited about.”

“We can now measure their eye with a 3D volumetric scan to produce a custom-made lens – that's life-changing. These people end up with 6/6 or 6/5 vision, starting from 6/30 or 6/40.”
Hoy EyeSpace
The results are clear. NovaTears® demonstrates statistically significant and clinically meaningful improvements in the signs and symptoms of Dry Eye Disease associated with Meibomian Gland Dysfunction.
NovaTears® is a unique preservative-free non-emulsion eye lubricant utilising patented EyeSol® Technology:
NovaTears® acts as a lipid layer stabiliser & evaporative barrier for improved tear film stability & quality:
Stabilises & thickens outer tear film
Lubricates the surface of the eye, spreading quickly without blurring vision
Preservative, phosphate, water and surfactant free.
Allows replenishment of underlying water layer with natural tears.
months shelf life after opening
free

STREAMLINED AUTHORITY CODE 6172
PBS Information: Authority Required (STREAMLINED): Severe dry eye syndrome in patients who are sensitive to preservatives in multi-dose eye drops.
Reference 1. Tauber J, Berdy GJ, Wirta DL, Krösser S, Vittitow JL, on behalf of the GOBI Study Group, NOVO3 for Dry Eye Disease Associated with Meibomian Gland Dysfunction: Results of the Randomized Phase 3 GOBI Study, Ophthalmology (2023), dol: https://doi.org/10.1016/j.ophtha.2022.12.021.
NovaTears ® Eye Drops (Perfluorohexyloctane 100% v/v, 3mL) are for the lubrication and relief of dry and irritated eyes. Do not use NovaTears ® with contact lenses. If using any other eye medication, allow at least 15 minutes between using the other product and applying NovaTears ®. NovaTears ® should not be used in children under 18 years. NovaTears ® should not be used while pregnant or breastfeeding. AFT Pharmaceuticals Pty Ltd, Sydney. ABN 29105636413.

Fullanteriorandposteriorcorneal topography,plusscleralprofilometryina singleOCTscan
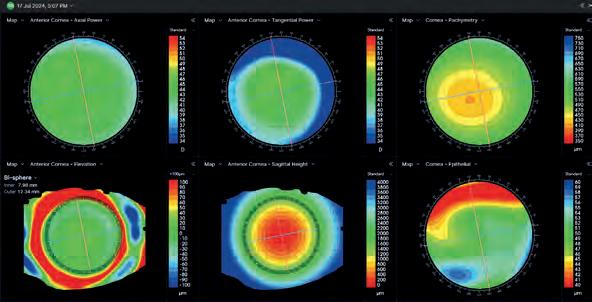
AxialLengthandbiometrydata,with comprehensivemyopiacontrolsoftware
Completeanteriorimagingallowsfortear filmindependentdata,capturingthemost difficultcorneas
RetinalOCTcompletesthesystem
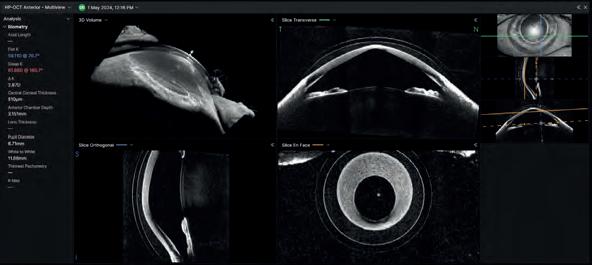
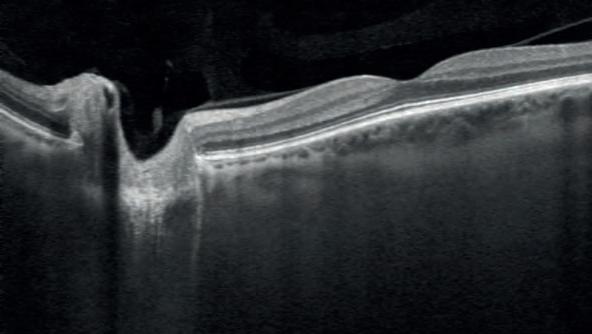



The Australian College of Optometry hopes a new name, website and strategy will end confusion for practitioners and patients, and help build better pathways and health outcomes for all.
What’s in a name? Well, plenty if you ask the Australian College of Optometry (ACO).
The Victoria institution has been around for 85 years but, incredibly, there is still a fair bit of misunderstanding about what the ACO does and its public health role in the state’s eye care sector.
And not just among many of the 50,000 patients it helps every year in its main Carlton facility, seven other metropolitan sites, and outreach clinics in close to 300 locations around Victoria.
Politicians and other key stakeholders – even people in health care –assume its main purpose is teaching optometry students or representing the profession as a peak body. Although the ACO’s early years centred on training, today 90% of the not-for-profit’s work is dedicated to delivering publicly funded care to the state’s most vulnerable people and its First Nations communities.
Making that clearer and creating a stronger identity is vital to helping those people understand what the organisation does, encouraging them to engage with its eye care services and creating better pathways for patients, says ACO director of operations Ms Kylie Harris, and Dr Josephine Li, general manager of Rural Victoria Eye Service (VES) and Outreach Programs.
A clearer, stronger identity would also help politicians and other key partners better understand what they are funding and why it is so important.
Which is why the organisation has announced an historic rebrand.
The ACO’s clinical and patient services, which make up the great majority of its work around the state, have been renamed as ACO Eye Health.
The plan was put forward as part of the ACO’s 2023-26 Strategic Plan and has involved all of its staff.
“The whole website redevelopment has been a critical part of it,” says Harris, “and we’ve involved our patients and teams across the organisation in terms of the final name.
“We ran a selection process and a voting process around that, the colours and the branding. We’ve tried to ensure that our staff have visibility and ownership of that.”
A media release announcing the January 2025 rebrand said the move was

part of “a number of changes to strengthen our public health mission and improve understanding of our role as a community eye care provider”.
As part of the move, the ‘Australian College of Optometry’ will remain the legal business name, representing the entire organisation comprising professional development, research, membership and clinical services. ACO’s trusted certificate courses and CPD programs will remain under the familiar brand.
But when it comes to delivering optometry services, ACO Eye Health is the new name it’s going by.

“It’s so important that those working in eye care and broader health services understand that ACO Eye Health’s purpose is to provide equitable, accessible, high-quality optometry care to the community.”
Dr Josephine Li has been at ACO for close to 20 years, but confusion over ACO’s role meant some patients thought she was a student.

PUBLIC HEALTH PRIORITY
Harris and Li say it can be difficult to make the connection with other health care professionals and even patients.
“It’s so important that those working in eye care and broader health services understand that ACO Eye Health’s purpose is to provide equitable, accessible, high-quality optometry care to the community,” says Harris. “We are a public health eyecare provider first and foremost.
“We work very closely with many community health organisations, but there will be ones that don’t know we exist.”
In addition to care delivered through ACO Eye Health’s network of Melbourne clinics, its Outreach team partners with a variety of other like-minded organisations across Melbourne and Victoria to reach the most vulnerable communities.
Through this outreach eye care program, thousands of individuals receive comprehensive eye tests and heavily subsidised or free glasses.
Those needing more detailed testing are referred to their local ACO Eye Health clinic.
“For example, if the patient was seen in the South-East region, they could be referred to Dandenong or Knox, and in rural Victoria, we will refer them to our rural VES practitioners,” says Dr Li.
Dr Li, who manages the team of 19 staff travelling about 50,000 kilometres each year to deliver this care, has experienced confusion around ACO’s name herself.
“Sometimes patients will say, ‘Oh, you’re from the college, are you? Are you a final-year student?’,” she says. “I say no, I’ve been around for about 20 years!
“There are situations where, because our name is so long, that all people can remember is that we’re the 'college people'.”
Apart from confusion among health professionals, the not-for-profit is conscious that many of their patients struggle with health care literacy.
“Often they have limited English language skills, don’t know anything about eye care, may never have had an eye test, maybe fled their country as a refugee without their glasses, all sorts of scenarios,” says Harris.
“And the state government also has a very strong emphasis on building up First Nation eye care and facilitating equity.”
That often means delivering “more complex care to patients with more complex, challenging conditions”.
Adding to that challenge has been a lack of understanding about the ACO, what it is and what it does.
That meant some patients with vision issues had been missing out on ACO’s services and clinics.
“This affects patients who would not even understand our services, or where they are if they visited our website,” says Harris.
“The existing site doesn’t clearly outline the appointment booking process; for somebody who might have limited English, how do they know they’ve landed in the right place? Nor does the website really speak to eyecare. Our new site aims to makes the experience much easier for patients, and also our optometry, ophthalmology and other health care colleagues who refer to us."
The new identity, which will include a new logo and updated car fleet, will give ACO Eye Health a strong and clearer presence around the state and within the communities it serves.
It will also strengthen that presence with the politicians and other key partners so important to ongoing funding, says Harris.
She believes misconceptions about ACO and its role may have played a part in limiting funding to the organisation.
“We look after over 50,000 patients a year for a very good price for the Victorian Government,” she says. “And there’d be very few people in government who could name the ACO as the organisation that actually delivers that. When we’re talking to politicians and we say, you know, we’re from the Australian College of Optometry, sometimes they don’t appear very interested, because they don’t want to talk to a member college that they perceive as being very wealthy.
“We had a funding cut this year, and it was interesting as we ramped up our communications with politicians during that period to find that very few had any idea of what we do.”
The rebrand plans to address and conquer those misconceptions.
“It helps moving forward, because we need to clearly articulate the work we do in order to improve our service delivery models and establish additional revenue streams,” says Harris.
“Being able to speak to what we do very directly in our branding is an extremely useful tool when we’re talking to any partner that might become part of our story.”
But if the rebrand is indeed a very useful tool, it’s just one in ACO Eye Health’s growing toolkit.
Its strategy to make eye care more accessible in Victoria goes beyond a new website, a new logo, and a few new colours.
It is also about building more collaborative networks with better health outcomes beyond just eye care.
“A really big part of what we have planned for 2025 is how we leverage off the rebrand to engage better with the community,” says Harris.
“We’ve undertaken a full review of our VES services during 2024 that feeds into what our clinic network and services should look like going forward into 2030-2040.”
She says that will involve a huge amount of work with stakeholders on the ground to understand “exactly where those health hubs and vulnerable people are going to sit”.
It is about improving service delivery and making it more efficient by collaborating with other health professionals to best serve vulnerable patients.
“For example, we look after patients who have diabetes because they need to be managed for potential diabetic eye disease, but you also have podiatrists, dietitians and many other allied health and medical practitioners involved in the care of those with diabetes.
“So how do we position ourselves to be part of these evolving hubs caring for vulnerable communities.”
She says that is the most “exciting” part of the work ahead.
“We want to make sure that we’re in the right place at the right time and have the right networks to get there.”
Now they believe they also have the right name to help do that.


FRI 27SUN 29 JUNE




Helps resist deposits and bacteria for a clean lens‡4–12 Approaches 100% water at the surface†2,3 Introducing TOTAL30TM: Combines Water Gradient and Celligent® technology for a reusable lens that feels like nothing, even at day 30.*1

*>70% of wearers agreed with ‘These lenses were so comfortable I didn’t feel anything’ and ‘I did not have to think about my contact lenses today’ (n=66).1 †Based on in vitro measurements of unworn lenses.2,3 ‡OPTI-FREE Puremoist used for cleaning, disinfecting, and storing, following package insert directions. Tested against 5 strains of P. aeruginosa (MCC 3478, 3480, 3481, 7142, ATCC 10145) (p<0.0001 for all) and E. coli (p<0.01).4–12
References: 1. Alcon data on file, 2021 [CLY935-C013, p.4]. 2. Alcon data on file, 2021 [A02491-REP-197506, p.4]. 3. Alcon data on file, 2021 [A02491-REP-198231-1, p.4,7,8]. 4. Alcon data on file, 2020 [TDOC-0057567, p.4,8,11]. 5. Alcon data on file, 2020 [TDOC-0057569, p.4,8,11]. 6. Alcon data on file, 2020 [TDOC-0057570, p.4,8,11]. 7. Alcon data on file, 2020 [TDOC-0057571, p.8]. 8. Alcon data on file, 2020 [TDOC-0057712, p.4,8,11]. 9. Alcon data on file, 2020 [ V-RIM-0027277, p.1,5]. 10. Ishihara K, et al. ACS Omega. 2021;6:7058–7067. 11. Alcon data on file, 2021 [V-RIM-0034922, p.1,4,6]. 12. Alcon data on file, 2021. [V-RIM-0035878, p.1]. © 2024 Alcon Laboratories Pty Ltd. AUS: 1800 224 153; Auckland NZ: 0800 101 106. ANZ-T30-2400019. ALC8487. Date of preparation: March 2024.






A lens that adapts to the patient’s visual profile rather than having the patient doing the heavy lifting. A global lens manufacturer believes it has cracked the numbers and the science to produce just that.
The numbers Rodenstock crunches to produce premium lenses are mind-boggling.
Millions of eyes scanned and analysed as part of its on-going research, in what is believed to be the industry’s biggest optical database, and countless multiple-year studies around the globe.
And it is harnessing all of that and the power of data science and artificial intelligence (AI) to produce something very singular – a unique optical lens custom designed to work for just one person – the wearer.
But the company has taken that a step further with a new lens available to Australian practices and patients in April 2025, called the B.I.G. EXACT Sensitive.
It’s the next extension of a portfolio currently spearheaded by B.I.G. EXACT lenses available to practices with its DNEye Scanner instrument. These lenses alone incorporate more than 7,000 data points of 80 parameters, allowing a biometric model of the eye to be ‘built’ and used to calculate the final lens.
Rodenstock says the new B.I.G. EXACT Sensitive design is based on more than five years of research, the analysis of millions of eyes, two complex wearer trials and a scientific eye-tracking study.
That has all been done to evolve the company’s knowledge and application of individual “visual sensitivity”, a key advance in the new lenses that will provide an even better wearing experience for patients.
And for independent practices it means they can now offer the first spectacle lenses optimised for both individual visual sensitivity and biometry.
Rodenstock has established that visual sensitivity is highly individual and linked to the individual eyes’ biometry.
It developed a Visual Sensitivity Index, which has demonstrated that people with lower visual sensitivity don’t or hardly perceive small changes in vision quality while in those with high visual sensitivity, even slight changes in vision quality can cause disturbances and disrupt vision flow.
As Dr Dietmar Uttenweiler, Rodenstock’s executive vice president innovation, points out: “Biometric lenses are one of the few real paradigm changes in the ophthalmic lens industry of the past two decades.”
But the company’s analysis of biometric data has revealed that 83% of those lenses do not fit the spectacle wearers’ individual visual sensitivity, presenting an area of untapped opportunity.
Visual sensitivity can disrupt a person’s visual flow, says Rodenstock
Australia’s professional services manager Mr Alex Rigby.
“Throughout our daily activities, our eyes are constantly receiving input from our environment, and they do so by rapidly shifting focus across different fields of vision,” he says.
“They move rapidly through various viewing fields and directions. In certain areas on the lenses there are distortion and blurred fields, which lead to a decrease in visual acuity and an interruption in the visual flow.”
That can lead to visual issues when transitioning between near and far tasks, causing discomfort; making tasks like navigating through crowds more challenging; and disruption while reading.
“The common thread among these issues is a sense of visual disruption, where the patient feels that something is interfering with their vision,” says Rigby.
He says Rodenstock’s research found these aberrations vary from person to person, depending on the overall characteristics of the individual’s visual system.
“For instance, a person with a higher sensitivity may experience more pronounced blur in certain fields, while someone with lower sensitivity may not notice the same degree of distortion.”
To help fix this, Rodenstock plunged into its industry-leading dataset to develop an advanced AI algorithm that uncovered the correlations and connections, allowing the lens manufacturer to get additional insights into the brain mechanisms of vision and determine the individual visual sensitivity.
Those insights can be gathered from an important piece of Rodenstock technology – its DNEye Scanner, a technology that has become the centrepiece in the retail area of many independent practices in Australia. The device is an aberrometer, topographer, pachymeter, and additionally a tonometer.
While competitors also use measurement devices, no one actually transmits this full set of data directly into the production of the lens. Rodenstock does.
“Once we measure these parameters using the DNEye Scanner along with subjective assessments, we can leverage the AI model to analyse the data,” says Rigby.
That combination of a patient’s unique DNEye scan and Rodenstock’s new research and AI data creates a “more precise and personalised lens design”.



“This approach represents a significant advancement in personalised lens design . . . rather than having the patient adjust to the limitations of a standard lens, the lens adapts to the patient’s visual profile.”
Alex Rigby Rodenstock
To develop its B.I.G. EXACT Sensitive lenses, Rodenstock has fine-tuned its state-of-the-art biometric lens calculations and collaborated with the University of Applied Science in Munich to study and test the results.
The findings confirmed that the new B.I.G. EXACT Sensitive lenses were more precisely optimised for each individual. Wearers experienced an improved visual performance.
The company states that, for people with high visual sensitivity, the new lens can provide up to 42% larger aberration-free zones, reducing the potential for vision disruptions.
Lenses for these wearers feature smaller, more concentrated aberration fields.
And lenses optimised for people with low visual sensitivity have more evenly distributed aberration fields, offering up to 30% reduced peripheral aberrations and softer transition zones, meaning the wearer will have a more seamless vision flow.
In its trials, Rodenstock found that spectacle wearers strongly preferred the new lenses. On average, they experienced notable improvements, such as 28% better reading flow, meaning the process of reading undisturbed was improved. The participants also reported a 35% improved visual orientation from far to near and from central to peripheral vision.
Rigby says that what sets the new lens technology apart is its ability to “consider not only the biometric data – like the size and shape of the eye – but also the individual visual sensitivity of the user”.
“This results in a truly personalised lens design that adapts to the unique needs of the entire visual system, ensuring improved visual comfort, and more natural transitions between different viewing fields.
“In essence, the lens works with the patient’s eye-brain connection to provide an enhanced, customised visual experience.”
That experience will be available to any practice that uses the DNEye Scanner and Rodenstock lenses.
“Practices already equipped with the current DNEye technology can offer B.I.G Exact Sensitive advanced lens technology without needing to alter their existing procedures,” says Rigby.
That would be a win not only for the practice but also the patient.
“This technology allows practices to further differentiate themselves by offering innovation, while ensuring their patients receive the most personalised level of visual comfort.
“This approach represents a significant advancement in personalised lens design, where lenses are tailored not just to the anatomical measurements of the eye but also to the patient’s unique visual sensitivity.
“Rather than having the patient adjust to the limitations of a standard lens, the lens adapts to the patient’s visual profile.”




PBS Information: Xalatan (latanoprost 0.005% eye drops, 2.5 mL) is listed on the PBS as antiglaucoma preparations and miotics.

















Before prescribing please review Product Information available via www.aspenpharma.com.au/products or call 1300 659 646.
Minimum Product Information: XALATAN® (Latanoprost 50 µg/mL) Eye Drops. Indication: Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Contraindications: Hypersensitivity to ingredients. Precautions: Change in eye colour due to increased iris pigmentation; heterochromia; eyelid skin darkening; reversible eyelash and vellus hair changes; macular oedema often associated with aphakia / pseudoaphakia; other types of glaucoma; contact lenses; severe or brittle asthma; herpetic keratitis; driving or using machines – transient blurry vision; elderly: no data; children: do not use, no data; lactation- metabolites present in breast milk, risk / benefit. Pregnancy: Category (B3) Interactions: other prostaglandins, thiomersal. See PI for details. Adverse Effects: Eye Disorders: blurred vision, burning, conjunctivitis, excessive tearing, eye pain, foreign body sensation, hyperaemia, iris hyperpigmentation, itching, punctate epithelial erosions, grittiness, stinging, eyelash and vellus hair changes, punctate keratitis, blepharitis, eyelid oedema, localised skin reaction on eyelids; Systemic: bronchitis, upper respiratory tract infection, eczema, rash, urinary tract disorder, abnormal liver function, myalgia, arthralgia, dizziness, headache, rash, chest pain, asthma, dyspnoea . See PI for details and other AEs. Dosage and Administration: One eye drop in the affected eye(s) once daily. Other eye drops should be administered at least 5 minutes apart.
References: 1. Clinical Practice Guide for the Diagnosis and Management of Open Angle Glaucoma. Optometry Australia 2020 2. Australian Commission on Safety and Quality in Healthcare Active Ingredient Prescribing Guide - list of medicines for brand consideration December 2022
Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma.com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2023 Aspen group of companies or its licensor. All rights reserved. Prepared: July 2023 AU-LAT-072023-07653

Two practices explain how their customers are happy to pay more for premium lens and coating products renowned for their clarity, UV protection and scratch-resistance.
Before she was an optometrist and business owner, Ms Minh Le was a qualified engineer.
While she studied for that degree, she worked for her uncle, an optometrist.
And after she qualified and then realised there wasn’t enough engineering work, her focus once more turned to his business and optometry as an option.
“I found that optometry is very well blended between technology, clinical and business,” she says.
So she went back to university, qualified as an optometrist and the rest is history for the woman who now owns the Optimax Eyecare practice in Burwood, NSW.
Now, you can take the person out of engineering, but you can’t necessarily take engineering out of the person.
And when she was considering her options for lens suppliers for her practice and patients, Le wasn’t to be swayed by slick advertising or marketing. She had to test the options herself.
“I only sell a product that I have personally experienced and trust,” she says.
“I love technology,” says Le. “So that›s why I went online and started searching about innovation in lenses.”
Plenty of companies promised all kinds of things, but one in particular caught Le’s eye. One offered a 1.76 high-index lens, which it claimed was the thinnest refractive plastic lens in the world.
“That made me curious.”
She investigated further, liked what she saw and then, rather than wait for the company to come to her, Le sent an email to Japanese lens manufacturer Tokai Optical, offering to sell and test the product herself.

The company has been a good fit for a professional with an engineering background and a love of technology.
The Tokai Optical Product Division, initially established as the Thin Film Division, has developed significant resources and technological expertise to create advanced ophthalmic lens coatings.
This division has extended its capabilities beyond ophthalmics, offering various industries specialised coatings such as dichroic filters for medical instruments, semiconductor manufacturing equipment and inspection systems, and laser-processing applications.
These products and coatings often surpass the complexity of ophthalmic lens coatings, with some featuring up to 300 layers and demanding exceptionally precise and stringent measurement standards, particularly within the semiconductor industry.
Furthermore, the Tokai Optical Product Division has actively explored
astronomical applications, contributing to the development of optical collectors for sensors installed in the Cherenkov Telescope Array situated in La Palma, Canary Islands, Spain.
Leveraging the resources and technological advancements cultivated by the Product Division, Tokai Optical has consistently driven the production of premium coatings for ophthalmic lenses.
Notably, Tokai Optical holds the distinction of being the first company globally to introduce hydrophobic coatings for ophthalmic lenses.
A decade on from that initial research, Le regards the ongoing relationship with the company as a success story for both her practice and patients.
Optimax Eyecare has a largely middle-aged clientele in an area with a significant Asian community. Le and her staff deal with a fair bit of glaucoma and macular degeneration.
She has a number of lens options, from Tokai and other companies, but finds it’s often the former that is her ‘go-to’ product for a mix of patients that range from tradies to retired people. From wealthy to those unable to afford health insurance.
Le says the Tokai lenses and coatings, especially the new Ultra Shield Performance (USP) product, offer outstanding UV protection and scratch-resistant technology, with that UV protection being standard over the past 25 years.
The USP coating became available to Australian independents in September 2024, with major selling points being its durability and ultra-low reflection, balanced with aesthetic appeal.
“I also found that their UV protection is really good,” Le says. “And you


“Japanese manufacturing is widely recognised for its precision and commitment to quality, producing finished products that exemplify their craftsmanship. This is actually a very strong selling point.”
Ethan Ong Eyemax Optical
know, in Australia, our UV rate is much higher than other countries.”
The price of the Tokai lens is a little higher than other products but many of her customers are happy to pay that for a premium product from a company known as a world-leader in optical and laser technology.
The firm’s coatings are not only used on optical lenses but also sensitive and sophisticated medical devices such as surgical equipment.
Again, rather than take Tokai’s word for it, the engineer in Le wanted further proof, so she visited the company’s factory during a trip to Japan.
“In 2017 I went to Japan to see the cherry blossoms and the Tokai agent
They put their Tokai lenses and two from other manufacturers through the company’s UV spectrometer and it was the host’s product that came out on top.
That’s why she’s confident in offering the Tokai lenses to her patients, and particularly tradies working under Australia’s harsh sun.
Even patients without access to health insurance, who must pay for the high-end premium USP-coated lenses from their own back pocket.
“So they want one pair of glasses, right, that will last them for years. You can pay a little bit extra but they will last longer.”
Le is particularly impressed with Tokai’s latest coating.
The company says it is made with high molecular density and hybridised molecules and particles, meaning it is two times more scratch-resistant than its Max Shield Coating and with no reflection.
While she visited Tokai, Le was offered a metal kitchen scrub to test the strength of the coating and the company’s claims.
“They gave me the normal lens and the USP one, and I scrubbed it by myself, and it was so amazing, the scratch-resistance.
“They do scratch. I used a key but you can see that the scratch is much shallower and slender than in other lenses,” she says.
Like Le, Mr Ethan Ong has visited the Tokai site in Japan. And like his NSW counterpart, the co-owner of Eyemax Optical in Footscray, Melbourne, was very impressed.
“Being able to visit Tokai’s factory and being able to observe its operations was a truly enlightening experience,” he says.
“It was fascinating to see the seamless co-ordination of machinery to the meticulous attention to detail in each stage of production; it highlights the impressive engineering and planning that went into creating such quality lenses.”
He was also given an insight into the technology behind the company’s many products, “which instills confidence that the lenses we sell represent the latest advancements in technology and provides our patients with the highest-quality lens available on the market”.
His practice sells a number of lenses from different providers, but the Tokai lenses and coatings are now his first port of call.
And his patients understand and appreciate their quality and durability.
Like Ong, they are impressed by the origin of their manufacturing.
“Japanese manufacturing is widely recognised for its precision and commitment to quality, producing finished products that exemplify their craftsmanship. This is actually a very strong selling point.”
Eyemax Optical has been selling Tokai lenses and coatings for a number of years.
Ong has become a big fan. Not just of their well-established UV protection, scratch-resistance and durability, but also the range of colours and tints in their multi- and single-focus lenses.
“They offer a wide range of colors and can also match specific tints when required,” he says.
“We offer as standard RMC (Rear Multi Coats) on all our tinted lenses, as it significantly reduces reflections on the back surface of the lens, where light entering from behind can bounce off the inner surface of the lens and create distracting glare.
“The RMC also enhances visual clarity and comfort. Additionally, it improves the overall efficiency of light transmission through the lens, ensuring better optical performance.”
Like other optometry practices, frames are an important part of Ong’s business, but he believes the lens is the more vital part of the transaction.
“It’s essential to pair premium lenses with our frames, as the lens is the most critical component of eyewear.
"Ultimately, the lens determines the wearer’s visual experience, as it is what they rely on to see clearly,” he says.
“Offering my patients premium lenses that deliver superior quality and performance is our top priority.”
That often means offering patients the Tokai product.
And over the past few months, that has included offering Tokai’s new premium USP coating.
“We have been offering that coating to patients who spend more time indoors, such as office workers,” says Ong.
“The new USP coating offers several advantages above and beyond traditional multi-coats – the lenses are clearer and more scratch-resistant.”
The patients like the exceptional clarity and are very impressed with the anti-reflective properties.
Customers were quite comfortable paying extra because they were getting a better lens.
And Ong is comfortable recommending the Tokai products to others in the eyecare industry.
“For those seeking to provide their patients with optimal eye protection, exceptional vision, and superior clarity, I would highly recommend Tokai lenses and coatings.”


As the local, ‘clever kid’, contemplating which university degree to do, Michelle’s grandfather asked: “what sort of life do you want at 35’? Michelle knew she wanted to have a positive impact on people while also being able to have a family life one day where her children would grow up, within walking distance of their grandparents. “As an optometrist, I love that I have a genuine impact on people. I also have the flexibility to manage my appointments. When the kids were growing up, I was able to go to school assemblies and piano eisteddfods.”
“It’s a privilege to support my regional community. Joining George & Matilda Eyecare has allowed my team and I to continue to give a high level of service to our patients for now and into the future.”
Michelle credits Steve Mason as being a great mentor in her clinical work as a new graduate, and Tony Hanks for supporting her to open her own practice. South West Rocks Optometry joined George & Matilda Eyecare in June 2024; serendipitously timed as predicted 15 years ago, when Michelle said she would sell her business when she was 52.
Her advice to anyone considering a business partnership is to “leave yourself open to the opportunity to say ‘yes’. Explore before you say ‘no’. You don’t know, what you don’t know”.



Optometrists play a vital role in detecting eyelid malignancies during routine exams and are often the first to identify suspicious lesions. With Australia experiencing peak summer UV exposure, this is a critical time to raise awareness about recognising malignancies, writes DR HELEN GARROTT.
ABOUT THE AUTHOR:


As front-line providers of eyecare, optometrists play a crucial role in early detection of ocular and periocular abnormalities, including eyelid malignancies. Recognising potential malignancies can help reduce morbidity and in some cases save lives by facilitating early diagnosis and referral to an ophthalmologist. This article will guide optometrists in identifying the main types of eyelid malignancies, recognising warning or ‘red flag’ signs, and understanding when a referral is necessary.
CLINICAL CPD HOURS
This activity meets the OBA registration standards for CPD
At the completion of this article, the reader should be able to improve their identification and referral of eyelid lesions, including:
• Distinguish between benign and malignant eyelid lesions.
• Apply the ‘ABCDE’ rule for melanoma assessment.
• Identify the most common eyelid malignancies, including basal cell carcinoma (BCC), squamous cell carcinoma (SCC), sebaceous gland carcinoma and malignant melanoma.
• Know when to refer a patient to an ophthalmologist for further evaluation.
Most eyelid malignancies are skin cancers deriving from the skin of the eyelids or in some cases the eyelid margin. The most common malignancies, in order of frequency, are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), sebaceous gland carcinoma and malignant melanoma. Each type presents unique characteristics, risks and levels of aggressiveness.
tendency to metastasise over time, SCCs require more aggressive and more urgent management than BCCs.
This is a rare and highly aggressive cancer originating from oil glands in the eyelids. It may originate either from the meibomian glands or Glands of Zeiss. It has a high mortality rate and can mimic benign conditions such as styes. The diagnosis must therefore be considered in a non-resolving chalazion in an elderly patient. It is often mistaken for chronic blepharitis and sebaceous gland carcinoma, so it must be considered in cases of so-called ‘unilateral blepharitis’.
Although rare, eyelid melanoma is extremely aggressive and can metastasise quickly. These usually present as new or changing pigmented lesions of the eyelid, with or without bleeding. Malignant melanoma requires urgent referral and management to minimise morbidity and

The most common form of eyelid cancer, BCC accounts for 85-95% of malignancies. It is slow-growing with minimal risk of metastatic disease but can cause significant local tissue destruction. It often occurs on the lower eyelid, the medial canthus, and less commonly, the upper eyelid. Owing to its slow growth and low metastatic potential, BCC is rarely life-threatening.
Although less common, SCC is more aggressive than BCC as evidenced by its more rapid growth and metastatic potential. It occurs more frequently on the lower lid than the upper lid and typically presents as a crusting and bleeding lesion. As a result of its



5. A typical Cyst of Moll is shown affecting the medial upper eyelid. Note the very thin skin overlying the cyst and the impression that this is ‘fluid-filled.’ The fact that it is filled with clear fluid would be confirmed with a process called transillumination, in which a small torch light which is shone on one side of the lesion results in the entire fluid-filled cavity ‘lighting up.’
Sebaceous Gland Carcinoma is a cancer that develops from the meibomian glands of the upper or lower eyelids. It often appears as a firm, round red or yellowish enlarging nodule. It more commonly occurs in the upper eyelid than the lower eyelid. These nodules are commonly mistaken for a benign chalazion. The diagnosis must be considered in an elderly patient with no history of chalazia, especially If the lesion is persistent, recurrent, or associated with eyelash loss. It should also be considered in cases of unilateral resistant blepharoconjunctivitis.
Local spread is frequent particularly to the conjunctiva, and orbit. In these cases, removal of the entire orbital contents (exenteration) is required for cure. It is important to diagnose Sebaceous Gland Carcinoma early as late diagnoses can result in metastatic disease and a high mortality rate.
RECOGNISING WARNING SIGNS
Knowing what to look for can make a significant difference in identifying potential malignancies and guiding urgency of referral. Here are some key warning signs for each type:
Basal Cell Carcinoma
• A persistent ‘sore’ that does not heal
• A raised pearly nodule with telangiectatic vessels
• Focal loss of eyelashes
• Raised, ulcerated lesions, sometimes with crusting
• Bleeding or oozing spontaneously or with minimal trauma
• An unexplained eyelid margin notch Squamous Cell Carcinoma
• Rough, scaly, thickened patches
• Wart-like growths or lumps that bleed easily
• A ‘sore’ that does not heal Sebaceous Gland Carcinoma

6. A
to overlying skin.
It is a well-defined, solid,
to the eyelid
distinction to a Cyst of Moll, it does not transilluminate as it is filled with opaque sebaceous material.
• Persistent eyelid swelling or thickening, often misinterpreted as a stye
• Yellowish nodules, particularly on the upper eyelid
• A non-resolving or recurrent chalazion, particularly in an elderly person
• Diffuse thickening of the eyelid margin, often mistaken for ‘unilateral blepharitis’ Malignant Melanoma
• Dark, irregularly pigmented lesions
• Asymmetry in shape, irregular borders or colour variation
• Pigmented lesions that change shape, size or colour over time
• Presence of new ‘moles’ around the eyelid
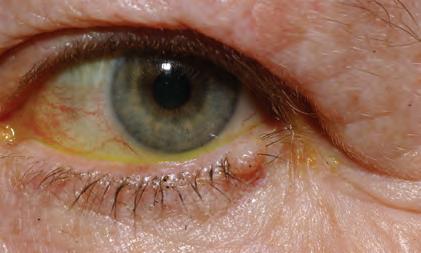
Figure 7. A benign compound naevus or ‘mole’. It is typically located on the eyelid margin or within the lash line. They are often minimally or pale tan or pink in colour. In this case, the naevus demonstrates some subtle speckled pigmentation. There are typically lashes growing through the lesion, as in this case, and this is extremely reassuring that the lesion is benign
For optometrists assessing pigmented eyelid lesions, the ‘ABCDE’ rule can be helpful in assessing the risk of melanoma:
Asymmetry: Melanomas tend to be asymmetrical, unlike benign lesions. This means that one half of the lesion does not match the other half.
Border: Irregular blurred or notched borders may suggest malignancy. This means that the edge of the lesion is not well defined.
• Colour: Multiple colours within the same lesion, such as brown, black, red or blue, are warning signs.
• Diameter: Larger lesions >6mm are more likely to be malignant.
• Evolving: Any change in size, shape, or colour should be viewed with caution. Essentially if the patient thinks that a pigmented lesion is changing in any way, or there is evidence of any change in the characteristics of the lesion on serial follow up, this should prompt urgent referral for assessment. Patients may notice that the edges of the lump are changing, that it is becoming thicker, progressively enlarging, or that there is new bleeding, oozing or itching.
Differential diagnosis: benign vs malignant lesions
It is important for optometrists to distinguish between benign and potentially malignant lesions, as many benign conditions can resemble malignancies. Here are some common benign eyelid lesions: Chalazion
A common, benign swelling of the meibomian glands, typically self-limiting and treatable with warm compresses, but occasionally requiring surgical drainage with incision and curettage.
Stye
An acute infection of the meibomian glands, usually tender red and located at the eyelid margin. Usually rapidly self-limiting but can evolve into a more chronic chalazion.
Xanthelasma
Yellowish plaques within the skin, most commonly in the superior medial canthus, due to cholesterol deposits. Usually bilateral but may be asymmetrical. In some cases, associated with raised serum lipid levels.
Naevi
Benign pigmented moles that remain stable in appearance over time, without change in size, shape of pigmentation.
Cyst of Moll
Benign sweat gland cyst usually close to the eyelid margin. Typically transilluminates.
Cyst of Zeiss
Benign oil gland cyst usually at the base of an eyelash. Typically presents as a discrete opaque whitish yellow spot or lump.
Seborrhoeic keratosis
A waxy, often pigmented lesion with a ‘stuck-on’ appearance, but alternatively can be lobulated or pedunculated.
Below are some reassuring features that a lesion is benign:
• Longstanding
• Not growing or changing
• Not bleeding
• Lashes are growing through it
When a lesion does not fit the typical characteristics of these benign conditions or fails to improve with treatment, it is essential to consider the possibility of malignancy.
Optometrists should refer any suspicious eyelid lesion to an ophthalmologist, ideally with expertise in oculoplastic surgery. Prompt referral is warranted for the following:
• Persistent or growing nodules or sores that do not heal, or that bleed or ooze.
• Eyelash loss
• Telangiectatic vessels
• Central ulceration
• Lesions that recur in the same location after prior resolution (e.g. recurrent chalazion)
• Any new lesion in a patient with a history of skin cancer
• History of immunosuppression
• Pigmented lesions that are irregular in colour, size or shape, particularly if they meet any ‘ABCDE’ criteria
Optometrists should routinely examine for lesions around the eye in their patients and enquire as to whether the lesions are new or longstanding. In particular, patients should be asked about whether there is any growth, bleeding or crusting of the lesion, all of which should prompt referral to an ophthalmologist, preferably with subspecialist oculoplastic training. Even in cases in which an optometrist has a low suspicion for malignancy, they should advise the patient to monitor for any warning signs which should trigger repeat examination and/or referral, namely: growth, bleeding, crusting or any significant change in the lesion.
• Worldwide exclusive one key operation
expert for any new or changing skin lesions and that the same principle applies to eyelid lesions.
Understanding the warning signs for eyelid malignancies allows optometrists to play a key role in early diagnosis, prompt referral and subsequent treatment, which in turn significantly improves patient outcomes. A timely referral can make the difference between preventing local invasion, metastasis, and potential vision and eye loss.
REFERENCES
1. S lutsky JB, Jones EC. Periocular cutaneous malignancies: a review of the literature. Dermatol Surg. 2012; 38 (4): 552-569.
2. S un MT, Rajak S, Selva D, Smith H. Periocular basal cell carcinoma: a comprehensive review. Expert Rev Ophthalmol. 2017; 12 (3): 221-232.
3. M oran JM, Phelps PO. Periocular skin cancer: Diagnosis and management. Dis Mon. 2020 Oct; 66 (10): 101046.
4. R ana H, Stokkermans TJ, Purt B, et al. Malignant eyelid lesions. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Available from: https://www.statpearls.comw
Optometrists should advise general sun protection including sunglasses, hats and sunscreen, particularly in those with a history of skin cancers. In cases where an optometrist feels a referral to an ophthalmologist is warranted for a suspicious lesion, they should explain to the patient that it is always sensible to get an opinion from an

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this
• Automatic alignment, Automatic focus, Automatic capture & Automatic exposure
• Intelligent system - precise positioning with impressive focusing speed & accuracy
• True colour restoration with crystal clarity for accurate diagnosis
• 4K high-definition resolution display with 27”
• Soft exposure technology – reduced pupil shrinkage and enhanced patient comfort
• Powerful multifunctional software analysis system
• Compact with built-in PC – even ideal where available space is restricted

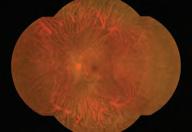
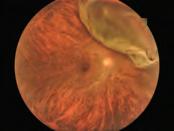


The growth of Optical Dispensers Australia during the past three years is evident for all to see ahead of its 2025 conference that will have a strong international influence.
Since its launch in 2022, Optical Dispensers Australia (ODA) has introduced a fresh standard of expertise and structure to a profession that was calling for clearer direction since deregulation many years ago.
Now, optical dispensers have somewhere to turn to for advice, continuing professional development and employment opportunities. Someone in their corner. And, importantly, dedicated events to network and dissect the issues impacting the everyday optical dispenser.
So often, optical dispensing education has been limited to a ‘stream’ as part of a larger industry event. But, as ODA CEO Ms April Petrusma says, optical dispensing is a “unique, multifaceted profession”, demanding a diverse skill set and evolving in response to technological advancements and ongoing research. To remain competent, it’s essential for optical dispensers to keep on top of the latest product innovations, new dispensing techniques, and emerging research findings.
In other words, they face an unusual set of challenges, prompting her organisation to run its inaugural national conference in 2023 in Sydney. It was a resounding success, marking the largest and first event of its kind in Australia “created by dispensers, for dispensers”.
But ODA will be eclipsing that on 7-8 March when it hosts the 2025 ODA International Conference. Everything about it will be bigger and better. If the venue – InterContinental Sydney – isn’t enough to go by, or the fact ODA is collaborating with the International Opticians Association (IOA) this time around, then one only needs to look at the speaker line-up.
It’s a high-powered contingent, with several flying in from overseas to deliver talks on various subjects now in the dispenser’s sphere, such as myopia management, and other topics like dispensing for children,
frame selection communication techniques, and dispensing atypical lens orders, plus more.
“The program has been curated through extensive research into current industry trends and challenges, allowing us to focus on the most relevant topics for our delegates,” says Petrusma.
“We have partnered with prominent experts and industry innovators to assemble an impressive line-up of speakers, each offering unique perspectives and invaluable insights. Our collaboration with the ODA community has also played a big part in helping us identify key themes that resonate with today’s optical dispensers.”
Regardless of job title role or level of experience, she is confident the program will inspire attendees and equip them with knowledge to elevate their skills.
“We also haven’t forgotten about the importance of growth through networking. During the breaks within the exhibitor areas, delegates will have ample opportunity to optimise their interactions with suppliers over complimentary refreshments,” she adds.
Another highlight of this event is the ODA Gala – taking place on the evening of Friday, 7 March – where the presentation of the coveted ODA National Excellence Awards will recognise some of the industry’s top performers.
The evening includes the Australasian College of Optical Dispensing (ACOD) Cert IV graduation ceremony too. The last gala in Sydney in 2023 saw a record 246 guests attend, with ODA anticipating similar numbers for 2025. But beyond the networking opportunities and celebrations, it’s the speaker line-up that’ll provide the biggest magnet.
Those keen to know more can go to odamembers.com.au/ odaconference.
ABOVE, L to R: ODA CEO April Petrusma at the 2024 conference gala; The speaker line-up has been curated to engage optical dispensers of all varieties.

MEETING THE DISPENSING
B.I.G. VISION: SEE MORE OF THE WORLD –THE VISUAL SYSTEM IN ALL ITS INTEGRITY FOR THE CREATION OF LENS DESIGNS
Dr Alexandra Sipatchin, Ph.D. neuroscientist, international product & project manager at Rodenstock
Fiona Anderson, dispensing optician, Upper Warden Worshipful Company of Spectacle Makers UK Anderson will deliver two lectures. The first will explore the nuances of paediatric dispensing, including how to foster trust and compliance. Considering facial anatomy and development, frame fit, and comfort will also be discussed. Her second talk will focus on children and vulnerable adults with additional needs – whether they’re physical, such as facial or cranial abnormalities, or physiological. She will highlight common syndromes in paediatric care and offer strategies for ethical dispensing.

Claire Ferreira, frame designer at Face á Face, co-artistic director at Design Eyewear Group
Ferreira, behind many of the eyewear designs available through supplier Eyes Right Optical, will offer a glimpse into her design philosophy and the inspiration behind her iconic frames. Attendees can learn how colour choices evoke emotions and enhance personal style, hear about emerging trends and how innovation will shape the industry.
CURRENT TRENDS IN MYOPIA MANAGEMENT
Prof Padmaja Sankaridurg, Professor at UNSW, head of global myopia management at ZEISS



EFFECTIVE COMMUNICATION TECHNIQUES FOR FRAME SELECTION
Samantha Day, dispensing optician, national dispensing manager at Matthews Eyecare NZ
Communication skills, particularly during frame selection, are essential to building lasting patient relationships. Day’s lecture will prompt dispensers to consider body language, choice of language, and tone to create a more engaging and supportive environment. The importance of empathy, honesty, and collaboration will be emphasised, as well as insightful lifestyle questions to understand the patient’s needs.
Shiva Taghvaei, optical dispenser, senior commercial manager at Safilo Australia
Taghvaei will explore the transformative power of data analytics and consumer psychology. By leveraging insights on local trends, purchasing patterns, and social media influence, practices can choose frame collections that better align with customer preferences and boost sales. Touching on sustainability, she will outline the importance of catering to environmentally-conscious customers and contributing to a more sustainable future.

IMPROVING DISPENSING OUTCOMES THROUGH BEHAVIOUR PROFILING
Virgilia Readett, assessor at the Australasian College of Optical Dispensing
Exploring the far-reaching consequences of myopia, Prof Sankaridurg will also discuss the latest in myopia control, such as orthokeratology, soft contact lenses, and pharmacologic options. Plus, she will delve into factors influencing effective management, including age, compliance, and individual patient needs. Optical dispensers will obtain actionable advice, including patient selection, treatment plans, and monitoring.


EMMETROPISATION IN THE HUMAN VISUAL SYSTEM, BIOMETRY, POSITION OF WEAR
Grant Hannaford, ophthalmic physicist, director of AAOO & 2022 IOA International Optician of the Year
This lecture will describe the process of ocular growth and outline strategies for providing optimal ophthalmic lens fittings. Core concepts will include: emmetropisation processes and the aetiology of refractive errors, optically imposed blur and the impact on growth and refractive outcomes, impact of optical and biometric interaction, and a case study in lens interactions in the developing eye, plus more.
UNLOCKING THE EARLY PRESBYOPE MARKET & NAVIGATING THE MYOPIA MAZE
optical dispenser, national training & development manager at Hoya Lens Australia
Hentschel will divide his time across two lectures. The first will delve into the emerging – and potentially lucrative – early presbyopia market, encompassing digitally focused patients in their late 30s to mid-40s and their heavy near and intermediate demands. His second talk, on myopia, will cover the latest progression research and various management options, including combination therapy and HOYA’s

Craig Johnston, optical mechanic, national sales & marketing manager at Younger Optics
Unravelling the complexities of eyewear, Johnston will tackle extreme prescriptions and how to leverage specialised labs for exceptional results. The intricacies of variable and nominated inset progressives will be discussed, along with the science behind DriveWear photochromic lenses.
THE OPTICAL DISPENSER:
Nabill Jacob, senior orthoptist, clinical relationship manager at Vision Australia
Jacob will outline how optical dispensers can identify patients with low vision and refer them for appropriate assessment and rehabilitation.
The presentation will also canvas low vision aids and devices, including magnifiers, telescopes, and specialised eyewear. Plus, attendees can learn communication techniques and counselling strategies so patients can make informed decisions about their management.

Are you a dove, owl, peacock, or an eagle? By understanding these distinct personality types within the D.O.P.E. evaluation framework, Readett will show how optical professionals can enhance their communication and dispensing techniques. Through case studies and practical tips, attendees can learn to identify behavioural types and tailor their approach.



Justin Chiang, optical dispenser, general manager at Tokai Optical Australia
To help optical dispensers thrive in today’s competitive market, Chiang will talk to the importance of understanding one’s strengths, setting goals, and exploring diverse career opportunities. Continuous learning and staying updated on industry trends are crucial, he will say, along with developing a strategic mindset to capitalise on emerging trends, enhance patient experiences, and drive business growth.
CASE STUDIES: ATYPICAL LENS ORDERS
Fiona Om, optometrist, professional services manager at CR Labs
Navigating the challenges of high-powered prescriptions and significant interocular differences can be daunting, but Om hopes to equip the audience with the tools to tackle these complex cases. High-power prescriptions, significant power differences between the eyes and frame considerations will be covered. So will optimising lens design, strategies to balance prism, minimising thickness and weight, frame fit, and patient comfort for optimal performance.



This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at https://www.tga.gov.au/reporting-problems.

The Optical Distributors and Manufacturers Association hopes that rewinding the clock to bring back the ODMAFair will galvanise the future of independent optics in Australia.

By going back to the future with ODMAFair in 2025, the Optical Distributors and Manufacturers Association (ODMA) has a clear mandate to run an event that breathes new life into the very reason for its existence.
Beyond the opportunity to bring its flagship biennial event back to Sydney (Friday 27 – Sunday 29 June 2025), it’s secured a premier location that satisfies exhibitors while offering an educational program striking at the very heart of the challenges optometrists, practice managers, optical dispensers and owners face in their professional lives.
Take, for example, major issues like HR that business owners too often learn on the fly. That’s why ProVision’s people & culture manager Ms Leanne Jackson has been allocated several slots for her session: ‘Engaging your team: From probation to peak performance’.
There’s also topics many would rather not think about, such as protecting one’s reputation and career. But Optometry Australia’s chief clinical officer Mr Luke Arundel will put this under the microscope in a session on handling medicolegal exposure, Medicare audits, Ahpra complaints and lawyer letters.
A frames repair workshop run by Optical Dispensers Australia, one on managing inventory and product displays, and ever-popular ProVision-Eyecare Plus sessions like how to become an independent p ractice owner round out a content schedule that should satiate anyone within the practice regardless of their job title.
Getting granular is the key, according to ODMA CEO Ms Amanda Trotman, who has been instrumental formulating the ODMAFair25 program taking place inside Sydney’s International Convention Centre (ICC) in the Darling Harbour precinct.
These topics, plus more, have been selected after going to all corners of the industry to understand the pain points in independent optics.
For ODMAFair25, sessions will be allocated time on their merit, and carefully scheduled to allow ample time for trade on the exhibit floor. It’s a departure from filling a standard 45-minute slot with speakers who put themselves forward.
“In some cases we’re allocating a couple of hours and making it more of a workshop where someone leads the discussion, and then the group breaks off into small roundtable discussions about real world solutions,” Trotman says.
“People can then report back to everyone. That way, attendees can get hands on and leverage the collective wisdom of the room.
“There’s a lot of clinical CPD available today, but we realised there’s a lot of other content the industry seeks, and ODMA is perfectly positioned to provide that.”
For those who have attended ODMA events in recent years, ODMAFair25 will have quite a different flavour.
That’s because its previous major show O=MEGA had a strong clinical CPD focus. This was intentional due to it being a joint venture event run with Optometry Victoria South Australia in Melbourne. It was O=MEGA that superseded ODMAFair (last run in 2017), with two shows run in 2019 and 2023, but currently there are no further O=MEGA events scheduled and they could only occur in Victoria or South Australia.
Meanwhile, O-SHOW, a solely ODMA-owned show held at Sydney’s Hordern Pavilion in recent times, is more of a boutique trade event, with a small breakout room for educational sessions. (As an aside, this will now alternate with ODMAFair going forward, with future dates and locations to be announced).
But returning as the flagship show, ODMAFair25 is a key opportunity for ODMA to get back to its roots, supporting the commercial success of independent optical practices.
By rewinding the clock, ODMA is re-leveraging an event brand well-known in the industry, and can curate a program with plenty of breadth and depth to attract a spectrum of optical industry professionals.
“Our charter is very commercial in nature, our 56 members are all suppliers, and if our program can help practices grow and generate a profit, then the suppliers by default are going to do better,” she says.
But as Trotman points out, ‘profit’ isn’t a word that should be banished from the practice owner’s vocabulary. Nor should there be any shame about emphasising the retail element of optometry businesses that can account for as much as 80% of revenue. Success in this regard allows owners to invest in more staff, branch out into other areas of special interest and acquire new technology to better serve their patients.
With this in mind, ODMAFair25 organisers have established a content program with three distinct streams: optical dispensing, practice management, and a new one, business.
“After O-SHOW this year, a survey showed us about a third of attendees were optical dispensers, a third optometrists and another third had ticked the box of owner. It was clear we were getting a lot of people who owned a business, whether they were health-trained or not,” Trotman says.
The program currently has nine sessions in the business stream, ranging from optical market research insights, a panel discussion involving industry experts and practice owners who have recently bought or sold, and tips to deal with the digital transformation and its influence on the patient journey and optical dispensing.
“At the end of the day, these are small businesses. They’re not necessarily people who are trained in business management, and yet, they’ve got to handle everything,” Trotman says.
“It may not strictly be CPD but I feel it’s an important educational piece
that’s missing in the industry right now, and ODMA’s in a position to help the whole practice team gain those important skills.”
But the program caters for optometrists looking to scratch their clinical itch too.
For the first time, ODMA is collaborating with Optometry NSW/ACT and the Australasian College of Behavioural Optometry (ACBO), who will run their own annual events alongside ODMAFair25 at the same location and across the same weekend.
As soon as Trotman secured the ICC venue, Optometry NSW/ACT was the first call she made, asking them to consider running the Super Sunday clinical conference. Optometrists flock to this event to obtain a significant number of CPD hours in a single day.
Next, she called ACBO, which agreed to running its ACBO Connect 2025 conference on the Friday and Saturday.
“A lot of work has gone into the program format to ensure streams and sessions did not conflict with each other, that there were sessions for all team members within a practice and that there was ample time for all visitors to explore what will be a large and valuable product and service showcase in the nearby trade fair halls,” Trotman says.

the trade fair, so we’re hoping people then go down into the trade fair as soon as it opens.”
“At the same time, we’re creating efficiencies and saving money for all three organisations and feeding each other’s event. We’re completely respecting they have their own successful event with their own branding. It’s a true collaboration in my eyes.”
One thing Trotman has learned from running live events for 35 years and attending SILMO Paris 2024 is the small touches really matter.
Complimentary tea and coffee, breakout areas where practice decision-makers can talk business with suppliers, and placing catering in the trade hall are all intended to maximise the opportunity for attendees and exhibitors.
But another big change coming in 2025 is the early morning keynote address on the first morning with Mr Adam Spencer. He’s an iconic radio and TV star and now prominent figure on the speaker circuit on artificial intelligence (AI), cyber security, the future of work, and the ChatGPT revolution.
While his talk won’t be optics-specific, Trotman says there will be advice all attendees can transfer into their own careers. The session will kick off the event at 8.30am on the first day, with breakfast provided for a nominal fee.
“It’s a lovely way to open the event, and we’re hoping people can make connections at their breakfast table. It’s taking place before we open

It’s also hoped ODMAFair25 will be the birthplace of a new Women in Optics meeting, and this inaugural one at ODMAFair25 will be sponsored by ProVision.
Trotman acknowledged there were similar groups organised across the country, but nothing existed nationally. While optometry is becoming increasingly feminised (around 60%), women still faced unique challenges.
“Now we’re at ICC in Darling Harbour, this is going to hopefully be one of the bigger events that we run. It’s a prime opportunity to try and bring women together from across the industry, and consider questions like how you go about handling menopause, or juggling work with a family.”
With ODMA events evolving in recent years and the coming and going of O=MEGA, Trotman is keen to stress her organisation’s current intentions.
ODMAFair is now the flagship, to be held in Sydney in 2025 and, if the industry wants more, running every second year thereafter.
In the alternative years, O-SHOW will run, with the location yet to be confirmed for 2026. Collaborating with other optical educational events would be the aim.
It’s basically getting back to the way ODMA events were structured prior to 2019 when the first O=MEGA was introduced.
“The reason for this is twofold. Firstly, we feel there’s enough CPD and other training out there, so we need to come up with a program that takes this into account.
“The second reason is, O-SHOW gives suppliers a more affordable exhibition option. There’s limits on the numbers of booths that can be booked and exhibitors don’t need a custom booth. It really helps the small suppliers and helps to level the playing field.”
As for the value of live industry events, Trotman says her message is clear. They work.
“I have seen it time and time again in my years of involvement with live events across multiple industries.
“There is no reason not to attend an event of this nature whether you’re in Australia or New Zealand; there’s so much under one roof to benefit from across the three days with multiple team members encouraged to attend. There are encounters that wouldn’t happen waiting for sales reps to visit, there are learnings beyond written industry content, and conversations that will lead to business growth that wouldn’t have been imaginable.”




















TINA NGAN recounts the key takeouts from a CPD event for Specsavers optometrists on how the industry can better serve LGBTQIA+ patients, starting with some small adjustments.
As frontline community health care providers, optometrists have a unique opportunity to show ‘allyship’ by practising sensitivity, embracing the nuances of gender identity, and making small adjustments in clinic processes – like offering options for pronouns in patient forms.
These inclusive practices not only enhance comfort but can also positively impact health outcomes for LGBTQIA+ patients.
Specsavers optometrists and team members recently attended an ‘Introduction to Trans Allyship’ CPD event.
This article outlines some of the key learnings and takeaways that other optometry practices can adopt.
As one of Australia’s largest optometry providers and employers of optometrists, Specsavers is dedicated to fostering an environment that respects gender diversity, enhancing care for all patients and team members.
Prism, Specsavers’ employee-led LGBTQIA+ network, partnered with the LGBTQIA+ youth charity Minus18 to host the ‘Introduction to Trans Allyship’ CPD event. This interactive session equipped Specsavers employees with insights to deliver informed care to transgender and nonbinary patients, promoting a safe space where everyone feels respected and valued.
Mr Neil Webster (he/him), Specsavers human resources business partner and diversity and inclusion lead, believes that such initiatives go beyond supporting individuals; they demonstrate a commitment to fostering a culture of compassion and inclusivity in the workplace.
“By promoting inclusivity, we create a more welcoming environment for both our people and customers. This awareness can lead to better support, interactions, and health outcomes for transgender customers and enhance overall customer satisfaction with the experience they have when they come in for an eye test,” he says.
“Furthermore, for transgender team members, knowing their workplace champions allyship significantly improves their sense of belonging and mental well-being.”
The CPD webinar was facilitated by Minus18’s Charlie (she/they), an advocate with lived experience, who shared their personal journey to build empathy and compassion for the challenges faced by the queer community.
Charlie discussed essential topics, including the differences between sex, gender, and sexuality, and highlighted the concept of gender diversity
across cultures. This personal approach resonated with attendees and set the stage for meaningful learning.
Charlie also shared practical recommendations for active allyship, including the importance of asking a patient or colleague their pronouns and how to use inclusive language. These discussions were complemented by insights into the experiences of LGBTQIA+ individuals in health care settings, which gave attendees a more profound understanding of the significance of allyship in both professional and personal contexts.
For optometrists like Mr Cafa Huynh (he/him), optometry director from Hurstville, New South Wales, the session was a reminder of the importance of respect and empathy.
“Allyship is an ongoing practice that begins with actively listening, showing genuine concern, and putting oneself in other’s shoes to encourage supportive work environments for everyone. Ignorance is not an excuse anymore,” he says.
After attending the CPD webinar, Huynh noted that with greater awareness of gender diversity, optometrists can create a safe space for transgender patients who may otherwise feel hesitant to have an eye test and uncomfortable disclosing their needs.
“We all want our patients to feel safe when they attend a practice. That starts by respecting and understanding all members of our community, whether they’re a customer or a team member,” he says.
“Passing judgments or making assumptions can cause patients to hold
The Prism network plays a pivotal role in championing the rights and representation of the LGBTQIA+ community at Specsavers. Comprised of LGBTQIA+ colleagues and allies from practices and support offices, Prism is committed to empowering team members to bring their full selves to work by creating a positive, supportive atmosphere that extends to both employees and customers.
The network educates on LGBTQIA+ issues, offers a platform for networking and socialising, and acts as a point of contact when colleagues need support. Additionally, it provides encouragement, mentoring, and coaching, helping team members feel empowered and supported.
By continuing to support LGBTQIA+ rights and advocating for diversity, Prism aligns Specsavers Australia and New Zealand with the organisation’s broader corporate social responsibility goals.

Tina Ngan – clinical services development consultant at Specsavers ANZ.

Specsavers.
Image:
back on explaining symptoms. Only when we communicate with sensitivity and openness do patients feel more comfortable expressing their concerns, which leads to better health outcomes.”
Huynh also says that Specsavers has more recently made a simple yet impactful change to incorporate the use of inclusive language and pronouns in patient records and communication. “We offer the option of ‘Mx’ as a title alongside the traditional Mr, Ms, Miss, and Mrs. This simple change plays a crucial role in making all patients feel seen and respected.”
Reflecting on the webinar, Huynh’s top takeaway is the importance of understanding and recognising that “no two people are identical”. The ability to appreciate individual differences fosters compassion and
empathy, qualities that are at the heart of effective allyship.
His advice to other optometrists looking to improve in this space is simple yet powerful: “When it comes to gender diversity and pronouns, it’s OK to not know, but only by asking, with genuine care and empathy, can we truly seek to understand.”
There are several small adjustments all optometry practices can adopt for a more inclusive culture, improved health outcomes, and stronger patient relationships.
1. Adopt inclusive language and set up internal policies to ensure a safe space for all.
2. Ask about a patient or colleague’s pronouns respectfully and with sensitivity.
3. Ad d additional pronoun options to your patient intake form and management system.
4. Apply training that educates team members on evolving concepts related to gender identity and sexual orientation.
5. Achieve a deeper understanding of the issues the LGBTQIA+ community faces in health care and a culture of continued learning.
6. Avoid making assumptions. Instead, communicate with empathy to create a non-judgmental space that builds patient trust.
As the field of optometry continues to embrace inclusivity, initiatives like allyship CPD events can help to promote affirmative action that supports employee well-being and creates the space for positive patient experiences.

Insight’s new website keeps you updated on the latest industry news and information. With a world-class responsive design, Insight is now accessible seamlessly on any device, 24/7.
Sign-up FREE to our eNewsletters and industry reports delivered weekly straight to your inbox.


































Name: David Sofatzis
Position: Practice manager & optical dispenser
Location: Lumiere Eyecare, Wentworth Point, NSW
Years in industry: 4
1. What inspired you to pursue an optical dispensing career, and how has your perspective changed over time?
I was drawn to optical dispensing because it uniquely combines clinical health care, sales, and hands-on tasks like frame repairs and adjustments. It allows me to make a tangible difference in people’s lives by providing tailored optical solutions that improve their vision and confidence. Earning my Certificate IV in Optical Dispensing from ACOD in 2023 gave me the theoretical knowledge and practical skills to recommend eyewear and dispense advanced optical lenses based on each individual's unique anatomy, needs, lifestyle and habits. Over the past four years, I’ve also come to appreciate the flexibility within the optics field. From managing a practice to exploring opportunities with lens labs, frame sales, or equipment companies, the career paths are diverse. Training new staff has boosted my confidence and solidified my expertise, enabling me to pass on my knowledge to others.
2. What are the most influential moments and people that led you to this point?
The dedicated Lumiere Eyecare team who mentored me early in my career and the support I received from ACOD during my studies were instrumental in developing my skills and confidence. I’m especially grateful to my family and friends, who have consistently motivated and encouraged me throughout this journey.
3. What’s something you know now that you wish you understood at the start of your career?
One important lesson I’ve learned is the value of taking your time during a dispense. Rushing can lead to mistakes, but careful attention to detail ensures the best outcomes for both patients and the practice. Patients appreciate attention to

detail, and many are happy to wait if they see you are providing expert care.
4. Can you share a moment where you made a significant impact on a patient’s life?
There have been many instances where patients have shared that the glasses I dispensed were the “best” they’ve ever had. This feedback is incredibly rewarding and reaffirms the importance of accurate dispensing measurements and tailoring solutions to individual needs. For example, I’ve helped patients struggling with progressive lenses by ensuring accurate fitting and providing detailed explanations. Seeing them regain confidence and comfort in their vision is one of the most fulfilling aspects of my work.
5. What innovations in eyewear or technology are you most excited about, and why?

I’m particularly excited about advancements in myopia control, as these solutions help slow its progression while providing clear vision. Ortho-k lenses are a standout innovation; they not only manage myopia but also offer patients the freedom to go without glasses during the day, which is especially beneficial for sports or personal preferences. I’m also inspired by the evolution of progressive lens designs. Utilising biometric technology, we can now customise lenses to an individual’s eye model, offering improved adaptation, wider fields of view, enhanced night vision, and reduction in higher-order aberrations. These innovations significantly improve patient outcomes and satisfaction.
6. What skills or qualities do you believe are most important for an optical dispenser to thrive in today’s market?
An optical dispenser must excel at troubleshooting, as this ensures patient concerns are resolved effectively. Communication is another vital skill – explaining product options clearly builds trust and confidence in the optical product being offered. Qualities like cultural sensitivity, active listening, and adaptability are equally important. My background in social work has helped me tailor my communication style to establish rapport with a wide range of patients, from affluent customers to those facing disadvantage. This ability to connect and
provide professional advice ensures patients feel supported and valued.
7. How do you ensure your skills and knowledge stay up-to-date in such a fast-moving industry?
I stay informed by attending webinars and trade shows, which offer valuable insights into emerging trends and technologies. I also study educational materials from lens labs and engage with lens representatives to keep up with advancements. Collaborating with colleagues is another key strategy. By discussing challenging cases with the team, I not only share knowledge but also learn from their experiences. This ongoing exchange helps me continuously refine my skills and deliver better outcomes for patients.
8. Why did you become a member of ODA, and what value do you see in the organisation?
Joining ODA has been a great asset in growing my confidence and expertise. Their webinars provide practical knowledge that directly benefits my work, while their networking opportunities allow me to connect with others in the profession. ODA also plays a vital role in representing optical dispensers and supporting our continuing professional development, which is crucial for advancing the industry and enhancing patient care.

From their emergence in a rock crystal material to the accessory worn by billions today, DANUTA SAMPSON traverses the history of spectacle lenses and their journey to a giant global industry.

Spectacles have evolved from reading stones to advanced vision aids and fashion accessories, with a rich history spanning centuries.1 Initially used for simple magnification in ancient times, spectacles have been transformed due to advancements in materials, optics, craftsmanship, and our understanding of vision. Some experts claim they are history’s fifth most important invention, allowing millions to enjoy good vision despite their native imperfect vision.1 Here, I will briefly describe the optics behind, and the history of, spectacle lenses. The evolution of spectacle lens materials is a fascinating topic in its own right but that’s for another day.
BELOW: Brass spectacles (1850) at the Megane Museum, Sabae City in Fukui, Japan. Image courtesy of Gladys Mak, optical dispenser, currently technical officer at the University of Western Australia and advisory board member of Optical Dispensers Australia.
A lens is an optical element that, through the process of refraction (bending of light rays), can converge (positive lens – used to correct hyperopia) or diverge (negative lens –used to correct myopia) a bundle of rays. The term lens originates from the Latin lēns, meaning lentil, the double-convex seed we eat. 2 The lens is defined by two refractive surfaces formed from a transparent optical medium (e.g., glass or plastic). The lens surface may have any shape, including a double-convex shape – like a lentil. The lens properties, such as being positive or negative, and its power, depend on its shape and the ratio of the material’s refractive index to the index of the surrounding medium.
Evidence suggests the first lens (known as the Nimrud lens, made of rock crystal) was created in 750-710 BCE in Mesopotamia (now Iraq); however, its purpose remains unknown. 3 The idea behind using lenses as a visual aid was

initially described in Ptolemy’s Optics (1st century CE) and further advanced by Ibn al-Heitam (Alhazen) in his Book of Optics (10th century CE).1,4 Around the 10th century, Italian monks developed the reading stone, a semi-spherical lens made of rock crystal and quartz, which we know today as a magnifying glass. The first evidence of wearable spectacles was documented in the 13th century in Northern Italy.1,4 It coincides with advancements in glassmaking on the Italian island Murano near Venice and translations of Alhazen’s book into Latin. These early spectacles featured lenses set in frames that rested on the nose, marking a pivotal moment in the history of vision correction.
It wasn’t until the 18th century that the spectacles we recognise today took shape.1 Also then, American Benjamin Franklin proposed the concept of split bifocal lenses, often referred to as a Franklin bifocal. 5 These marked a significant advancement in vision correction, offering a practical but sub-optimal solution to seeing distant and near objects using a single pair of eyeglasses.
The 19th century brought further refinements, including toric lenses for astigmatism correction (invented by English astronomer George Airy) 6 and improvements in bifocal designs to enhance comfort and functionality. Trifocal lenses followed, aiming to provide correction for intermediate distances, though these early designs suffered from visible segment lines and limited depth of focus.
The 20th century witnessed the development of progressive addition lenses (PALs), offering a seamless transition between different optical powers for clear vision at all distances. Englishman Owen Aves was granted the first patent for PALs in 1907, but he could never produce such lenses due to the manufacturing limitations.7 In the 1960s, the first commercially successful progressive lenses became available thanks to the inventions of France’s Bernard Maitenaz.
The original progressive lenses were made from pre-produced, semi-finished
moulds. From about 1980 onwards, multifocal lenses were transformed thanks to the integration of freeform technology. This innovation allowed for custom-designed lenses tailored to the unique needs of each wearer. Freeform technology utilises computer algorithms to create personalised multifocal lens designs based on a patient’s prescription, frame measurements and specific visual habits. However, they have some limitations, including lower effectiveness of the refractive zone and higher peripheral distortion in low-light conditions. In the case of specialised vision needs, the design options afforded by progressive lenses can be limited. Lens design continues to advance. A recent innovation is the spiral shaped diopter lenses by researchers from Bordeaux in France. 8 These lenses are designed to maintain clear focus at various distances and lighting conditions, overcoming some limitations of traditional multifocal lenses. They use a spiral-shaped design to achieve multiple points of focus, potentially revolutionising multifocal lens technology if it successfully becomes a consumer product.
In conclusion, spectacles have evolved remarkably to become a global accessory worn by billions. Looking forward, research continues to focus on improving lens materials, manufacturing techniques, and optical algorithms to enhance the quality and versatility of spectacles. The “perfect lens” remains an exciting goal, promising further advancements in vision correction and optical technology.
NOTE: References will feature in the online version of this article.
ABOUT THE AUTHOR: Dr Danuta Sampson is a translational researcher and senior lecturer jointly appointed between the Lions Eye Institute and the School of Optometry at the University of Western Australia. She is involved in the global optics and photonics community through engagement with Optica and SPIE – the largest optics and photonics societies globally. She serves as a light science ambassador and supports various committees for Optica and, with SPIE, designs STEM children’s books and educational games/materials.

Australia appears to have a shortage of orthoptists, but as Orthoptics Australia president A/Prof AMANDA FRENCH and executive officer Ms JANE COWAN point out, there’s also a shortage of good data to better understand the issue.

There is high demand for orthoptists in Australia and abroad, with professionals highly sought after for their specialised skillset across clinical eyecare, public and private health, ophthalmic and pharmaceutical industries, and rehabilitation and disability.

IN AUSTRALIA IS PROJECTED TO CONTINUE GROWING, IN PART DUE TO THE NATION’S AGEING POPULATION AND THE RISING PREVALENCE OF CHRONIC HEALTH CONDITIONS.
Anecdotally, there is a worldwide shortage of orthoptists, from which Australia is not exempt.
Orthoptics Australia regularly hears from employers in both public and private sectors that they are challenged to find orthoptists to fill critical roles.
The demand for orthoptists in Australia is projected to continue growing, in part due to the nation’s ageing population and the rising prevalence of chronic health conditions.
NSW Health estimates an annual increase in the NSW Health orthoptic workforce of 2.4% (in a low-demand scenario) to 3.4% (in a high-demand scenario) per year would be required to meet demand by 2040.
This is not unique to orthoptics, with workforce shortages and retention challenges prevalent across most allied health professions in Australia.
This has sparked work to develop a National Allied Health Workforce Strategy led by the newly appointed Australian government chief alied health officer, Ms Anita Hobson-Powell.
Orthoptics Australia has been engaging in consultation related to the strategy and is hopeful it will support training and retention of allied health professionals within the workforce.
However, despite the Jobs and Skills Australia (JSA) 2024 Occupational Shortage List identifying workforce shortages in NSW, WA, and regional Victoria, there were no shortages reported in metropolitan VIC, QLD, SA, TAS, NT or the ACT.
This is perplexing, given the higher concentration of orthoptists in NSW and VIC, where the two training programs are delivered, at the University of Technology Sydney (UTS) and LaTrobe University. This highlights issues around accurately quantifying the orthoptic workforce through available national data and determining job demand in the context of chronic shortages.
In 2021, the Australian Institute of Health and Welfare (AIHW) reported there were 1,055 orthoptists across the country, closely

830 orthoptists working in Australia in 2016.
The increase of 225 professionals over five years demonstrates an average increase of 45 orthoptists per year.
While this indicates substantial workforce growth, it is less than expected based on estimated graduate numbers of approximately 100 per year across the two programs.
The UTS Master of Orthoptics course alone has graduated over 400 orthoptists between 2016 and 2023.
The gap in workforce data of approximately 55 orthoptists per year may be accounted for by orthoptists moving into management and other healthcare roles or general workforce attrition.
One challenge in data availability is that orthoptists are not included in the National Registration and Accreditation Scheme (NRAS) administered by the Australian Health Practitioner Regulation Agency (AHPRA).
Systematic data collection for NRAS-registered professions provides key workforce trend information that is unavailable for self-regulated allied health professions.
The orthoptic profession is self-regulated by the Australian Orthoptic Board (AOB), an independent body which oversees professional standards and maintains a public register, mirroring AHPRA boards.
Orthoptics Australia, as the peak body for the profession, advocates for orthoptists, advances education, and supports the profession in adapting to the increasing demand.
Orthoptists are very sought after, in Australia and abroad.
allied health professionals and likely improve workforce data availability.
In the interim, Orthoptics Australia is working to create a better understanding of workforce challenges and enable workforce planning by undertaking a comprehensive workforce survey.
This is crucial to inform professional advocacy and ensure the profession continues delivering essential eye health services.
In November 2024, JSA opened its 2025 Occupation Shortage List Stakeholder survey. The information collected through the survey captures occupations that may be in shortage and informs Australia’s Skilled Occupation List, with any implications for skilled migrant visas.
Orthoptics Australia is encouraging participation from all sectors employing orthoptists and is committed to working with stakeholders to improve data collection and ensure future workforce capacity.
ABOUT THE AUTHORS: Associate Professor
Amanda French is the president of Orthoptics Australia and head of orthoptics at the University of Technology Sydney. Jane Cowan is Orthoptics Australia’s executive officer. She has extensive experience in public policy with a passion for contributing to initiatives that deliver positive social impact.
ORTHOPTICS AUSTRALIA is the national peak body representing orthoptists in Australia. OA’s Vision is to support orthoptists to provide excellence and equity in eye health care. Visit: orthoptics.org.au
COLLEEN SULLIVAN has been involved in health practice management for decades and has consolidated her ideas in a book. She shares some key takeouts to ensure nothing slips through the net.

EVERY RESOURCE AND ALMOST EVERY ACTIVITY WITHIN A PRACTICE CAN BE MEASURED IN FINANCIAL TERMS.
My colleague Mr Gary Smith AM and I have been involved in health practice management for many years. We decided to join forces and publish a book: Principles of Healthcare Practice Management – Your Handbook
Each health care practice comprises unique clinical expertise supported by a range of business and technology systems. Our book is for the entire practice, including practitioners, nursing staff, clinical staff, administrative assistants, receptionists and business and practice managers. The principles highlighted show the inner workings of a high-performing health clinic. They also aim to ensure satisfaction among patients, practitioners and clinical staff, and how to sustain and enhance this. Plus, they address emerging trends in practice services, risk-resistance and financial viability.
Health care services are evolving with emerging technology, new services, staff shortages, practice costs and patient expectations. Quality needs to be the cornerstone in everything they do.
THE PRINCIPLES
• Business operations and systems
• Financial management
• Human resource management
• Leadership in the 21st century
• Information management
• Risk and compliance
• Practice development
• Professional development
BELOW: A high-quality patient experience should be the priority
Business operations and systems: This covers business continuity planning; strategic planning; systems design and implementation; monitoring systems for
licences, accreditation and re-certification; facilitating staff development and team building.
Financial management: This includes detailed coverage of financial systems, accounting, budgeting, managing the revenue cycle, fee schedules, accounts payable, inventory control systems, financial reporting and financial analysis. Every resource and almost every activity within a practice can be measured in financial terms.
Human resource management: It is the people who are crucial to the practice’s success – patients, customers, clinicians, administrative staff and support staff. Human resource management is vital for optimal performance and shouldn’t be underestimated.
This principle includes recruitment, selection and induction of new employees, and staff retention. Other elements include practice culture, induction programs, managing staff performance, team development and leadership, emotional intelligence, risk and compliance with employment law and cybersecurity, creating a learning culture and mentoring and succession planning. Quality of staff and leadership are two essential ingredients.
Leadership: In the 21st century health care practice, leadership is important to achieve the best outcomes for individuals and the practice team, while remaining focused on quality patient care. Here, we identify the qualities and characteristics of leaders, different styles and the challenges of leadership, the importance of practice teams, understanding teams, team development and team leadership.

Leadership is relevant to all areas of the practice, as is the diversity of leadership. Information management: Data analytics is one of the most important ways to understand the business. Protection of data through cybersecurity is an essential component as well, in terms of the duty to prevent cyber-attacks, protect patient and practice information and reduce data breaches, and identity theft. It allows practices to collect data across all practice areas and track performance and trends and, in some areas, across a broad section of their specialty. This principle includes the importance of AI safety, quality and security, and involves the workforce, consumers,
health care industry and research. Risk and compliance: This addresses identification of risk in business, financial and clinical areas; professional liability insurance; conflict resolution procedures; understanding and managing compliance with legislation, regulations, standards and ethical practice; self-assessment of your practice – clinical and business areas in terms of risk and compliance.
Practice development: Professional networking, marketing plans, establishing partnerships and strategic alliances are covered here. As is networking, reputation and public relations, and customer-relation programs for patients, referrers and the wider health care community. Professional development: By identifying areas of growth, individual goals and interests, training and education, mentoring and coaching, practices can lift their performance. Performance feedback and education are also vital, along with a mechanism to review and refine. To get the most from these principles:
• Quality is the essential element to underpin the practice.
• Practice principles require attention, resources and education.
• Incorporate the principles into daily operation and strategy.
• Develop and maintain a culture of leadership.
• Adopt risk management across all areas of the practice.
• Induction for every person who joins the practice to understand the principles.
• Provide education, information and communication.
• Create and conduct strategic planning. Think about how you can get the most from this handbook and make it specific to your practice.
Our goal was to develop a user-friendly handbook in a practical format with checklists relevant for the whole practice. Good practice management helps reach excellence and adhere to the highest standards. Those keen to know more about the handbook can visit www.amazon.com. au/dp/B0D46BBD3T.

BY SKYE CAPPUCCIO
Medicare has played a vital role in supporting relatively good community access to optometric care for decades. The structure of Medicare Benefits Schedule (MBS) items shape what eyecare Australians access.
To ensure we maintain and enhance community access to much-needed primary eyecare, Australia cannot afford to wait – we must ensure that Medicare continues to evolve to best support eye health and vision care needs.
In recent years, optometrists have been telling us that they have been seeing a decline in initial comprehensive eye examinations for asymptomatic younger and middle-aged patients. This is of great concern – we know that these patients may have, or be at risk of, ocular conditions that do not currently affect their sight, but can result in vision impairment or vision loss if not identified early enough to be managed effectively.
Optometry Australia undertakes comprehensive analysis of MBS billing data every six months. While we have seen increased year-on-year
inconsistency in billing data as a result of the COVID-19 pandemic, over recent years there has been a significant fall in the numbers of Australians aged under 65 receiving initial comprehensive eye examinations.
Per capita initial comprehensive eye examinations reduced 18.1% nationally for people under 65 between 2017-18 and 2023-24. All age cohorts from 0-5 years to 55-64 years have reduced. The raw number of Australians aged under 65 getting Medicare-subsidised initial comprehensive eye xaminations fell 12.4% from 2017-18 to 2023-24. Critically, if the 2017-18 per capita rate for under 65s was maintained in 2023-24, there would have been an additional 424,000 initial comprehensive eye examinations. In terms of enhancing access to primary eyecare, Medicare data shows that Australia is going backwards. There are likely multiple reasons for this disturbing drop-off. The 6.2% reduction in per capita initial comprehensive eye examinations between 2022-23 and 2023-24 indicates that cost-of-living issues may be having an impact. Also understandably, numbers fell during COVID. We recognise that optometrists may be making greater use of other MBS items for progressing eye conditions (particularly in older patient cohorts), however, analysis shows a reduction in per capita usage of all comprehensive eye exams.

The most significant contributor is likely the change introduced by the Federal Government in 2015, to reduce the frequency with which people under 65 years can access a rebate for an initial comprehensive examination from two to three years.
This change was strongly opposed by Optometry Australia when first announced; we argued that it was inconsistent with good practice. The Optometry Clinical Committee of the MBS Review Taskforce subsequently recommended altering it to support more frequent access for middle-aged Australians.
Australians should be as concerned as we are that asymptomatic Australians
aren’t accessing the regular eyecare they need. Projections show that the greatest increase in the absolute number of Australians with vision loss is expected between 2020 and 2030. We must address the root cause – not enough Australians accessing comprehensive eye examinations to enable early identification of – and effective intervention in – eye disease and vision problems. As we head toward a Federal Election, Optometry Australia is calling on all major parties to commit to supporting Medicare rebates that enable all Australians under 65 to access a rebate for a comprehensive eye examination at least every two years. This is in the interests of patients, population health and the profession. Our advocacy efforts are well under way, and in the coming months, we will be calling on optometrists and stakeholders to support our efforts. Collectively, we have a responsibility to ensure Medicare items evolve to support the best outcomes for our communities.
Name: Skye Cappuccio
Qualifications: BA, PgradDPH, GAICD, MBA
Affiliations: Optometry Australia
Position: CEO
Location: Canberra
Years in industry: 10+ years
OPTOMETRISTS HAVE BEEN TELLING US THAT THEY HAVE BEEN SEEING A DECLINE IN INITIAL COMPREHENSIVE EYE EXAMS FOR ASYMPTOMATIC YOUNGER AND MIDDLE-AGED PATIENTS. THIS IS OF GREAT CONCERN.

FEBRUARY 2025
MIDO EYEWEAR SHOW
Milan, Italy
8 – 10 February mido.com
ANZGS CONGRESS
Perth, Australia
14 – 16 February anzgsconference.com
VISION EXPO EAST
Florida, US 19 – 22 February east.visionexpo.com
MARCH 2025
100% OPTICAL
London, UK
1 – 3 March 100percentoptical.com
ODA INTERNATIONAL CONFERENCE
Sydney, Australia
7 – 8 March odamembers.com.au
APRIL 2025
ASIA-PACIFIC ACADEMY OF OPHTHALMOLOGY CONGRESS
New Delhi, India
3 – 6 April 2025.apaophth.org
MAY 2025
ARVO 2025
Utah, US 4 – 8 May arvo.org/annual-meeting
2025
ODMAFAIR25
Sydney, Australia 27 – 29 June odma.com.au

2025
AUSCRS 2025
Darwin, Australia 16 – 19 July auscrs.org.au/2025-conference
NOVEMBER 2025
RANZCO CONGRESS Melbourne, Australia 14 – 17 November ranzco2025.com


WHY DID YOU PURSUE AN OPTOMETRY CAREER, AND HOW DID YOU ENTER THE PROFESSION?
For as long as I can remember I’ve been interested in science and biology. At some point during my early teenage years I realised I wanted to pursue a career in the health sciences. I remember being fascinated with the eye and how vision works, so I decided to do my work experience in high school for an optometrist. After that I was sold and my fascination ended up eventually turning into a career.
HOW DID YOU COME TO WORK AT SPECSAVERS, AND WHAT ATTRACTED YOU TO THE BUSINESS?

I have worked for Specsavers before in different capacities, so I knew prior to rejoining how well the business model works. It’s such a great system for both staff and customers alike; being able to provide a service like OCT on every patient, without charge, is a game-changer clinically.
WHAT WAS YOUR FIRST ROLE WITHIN THE BUSINESS, AND WHAT DID IT ENTAIL?
My first role was working as an optical assistant in Indooroopilly when I was an optometry student in Brisbane. It entailed optical dispensing, pre-testing and front-of-house duties. During this time I got to experience first-hand how well structured the customer journey is, and this is one of the big reasons that ultimately drew me back to working at Specsavers.
SINCE THEN, WHAT GROWTH OPPORTUNITIES HAVE PRESENTED THEMSELVES?
I have worked in different capacities for Specsavers over the years, as an optical dispenser, locum optometrist, full time optometrist, but the most exciting growth opportunity
afforded to me so far is the Pathway Program. During this time I learnt a lot, but the key gems I took away were around how to be the best leader that I can, both through self-development and specific tools to mentor and guide teams successfully.
CAN YOU RECALL A CASE WHERE YOU MADE A SIGNIFICANT DIFFERENCE?
One case I will never forget is when a patient presented with a recent onset, very localised headache at the top of her head. She also had a very subtle ptosis and smaller pupil on one side. My disease lecturer at university would often talk about how life threatening a sudden onset Horner’s Syndrome can be, and as she had never noticed her eyelid or pupil being smaller, I referred her immediately to the hospital emergency rooms. When I followed up with her, she confirmed that she had a carotid dissection. It was a real wake-up call that what we do can actually save lives.
CAN YOU OUTLINE YOUR TOP CAREER HIGHLIGHTS SINCE JOINING SPECSAVERS?
The highlight that comes fresh to mind is being able to implement my learnings from doing Pathway in store. It’s been really rewarding to be able to use what I’ve learned to create meaningful change in store and to develop my leadership skills.
WHAT EXCITES YOU MOST ABOUT TURNING UP FOR WORK EACH DAY?
It might sound cliche, but it’s the ability to make a difference to the eyesight and quality of life of people every day. The gift of sight can’t be understated, and I think that’s why we’re all here doing what we do, at the end of the day.
Optometrist Joint Venture Partnership Opportunity – New Store, Hamilton, VIC
Specsavers has a rare opportunity for an Optometrist looking to take the next step in their career and join the brand as a Joint Venture Partner at our brand-new store in Hamilton, Victoria. Hamilton is a vibrant regional city known for its natural beauty, rich culture and familyorientated community; it also boasts convenient transport links to both Melbourne & Adelaide. Successful applicants will receive Specsavers’ award-winning support in building up their business, including team recruitment support and end-to-end financing on new stores.
Full-Time Experienced Optometrist Opportunity, Specsavers Shellharbour – NSW
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Carly Parkinson on +61 (0) 478 201 057 or E carly.parkinson@specsavers.com
Optometrist employment enquiries: Specsavers Recruitment Services anz.srsdepartment@specsavers.com
Locum employment enquiries: ANZ.locumteam@specsavers.com
Graduate employment enquiries: apac.graduateteam@specsavers.com
Join the friendly team at Specsavers Shellharbour as a full-time Optometrist. Located just 90 minutes from Sydney, Shellharbour offers a convenient lifestyle. Enjoy a fantastic package of up to $140,000 + CPD allowance + super, plus the option of a flexible 9-day fortnight. Work in a high-tech, six-room store offering Orthokeratology and free OCT for every patient! Be part of a passionate, experienced team that ensures seamless patient care. This role is perfect for those eager to make a real impact in their careers!
Optometrist opportunity – Specsavers Napier, NZ
Join our team in Napier - New Zealand, famous for its stunning Art Deco architecture, beautiful beaches, and vibrant outdoor lifestyle. We’re seeking a full-time optometrist to deliver exceptional care in a supportive and growing community. If this sounds like your ideal next role, we’d love to hear from you!
Graduate Opportunities
Are you a final year Optometry student looking for your first optometry role in early 2025? Specsavers has a limited number of vacancies remaining across Australia and New Zealand, with competitive sign-on bonuses and fixed-term contracts available in select locations. To explore these exciting opportunities or learn more about the Specsavers industry-leading 2-Year Graduate Program, please reach out to your Graduate Recruitment Consultant or email anz.graduateoptometry@specsavers.com
Regional Locum Opportunities
Looking for extra locum work over the coming months? Specsavers has seen work dry up in Sydney, but we still have great weekend opportunities available at our Newcastle stores! Whether you’re filling gaps in your schedule or looking to boost your income, reach out to us today to secure your spot!

Dr Nicole Lim has joined the team at Eyehaus, Randwick. Dr Lim is a comprehensive general ophthalmologist with a sub-specialty interest in glaucoma. She is a consultant ophthalmologist at Prince of Wales Public Hospital. Dr Lim is also a part of the Outback Eye Service, delivering eyecare to regional NSW.

Trained optometrist Ms Tegan Matheson has been appointed into the role of senior professional services manager NSW/ACT at EssilorLuxottica ANZ. She was previously country eyecare manager New Zealand, based in Auckland.

Ms Melanie Free has been appointed as the new Queensland sales consultant for HOYA. She has a wealth of professional experience in sales and key account management within the optical industry and joins the team with the aim of enhancing its sales department and contributing to the continued growth and success of HOYA Lens Australia.

Mr Theo Charalambous has been appointed president of Optometry Australia, succeeding Ms Margaret Lam, who has served in the position since 2022. He joined the national board in 2021. He entered optometry in 2002 working in practices in the Berwick and Pakenham areas before opening an independent practice, ModernEyes, in 2008. Charalambous now owns and works across a number of OPSM practices across Melbourne and an independent practice in Hastings, Victoria. He holds a Senior Executive MBA from the Melbourne Business School and undertook the Australian Institute of Company Directors course in 2022.
Mr Shuva Bose has been named the new vice-president of Optometry Australia. He has practised optometry in retail and medical settings within metropolitan and rural settings, and is currently working in an independent practice. He is also a clinical supervisor at Queensland University of Technology, where he assists students in developing clinical diagnostics and management. Bose’s prior research experience involves working in a research clinic investigating contact lenses and sports vision.


South Australian optometrist Ms Elise Pocknee-Clem joins the national board as a new director. She is the managing director of three independent practices in Port Lincoln, Whyalla and Ceduna in SA and is a partner in a fourth practice in Victor Harbor. The practice group provide extensive outreach services across six other towns on the Eyre Peninsula. She has previously served as president of both Optometry South Australia and Optometry Victoria South Australia and oversaw its integration process with Optometry Australia in 2023.
Discover NGENUITY® the true Digital 3D Visualisation System1
with 1.5
Next-Gen Digital Optimisation
Visualise like never before*
with 1.5
Easy integration with the Alcon Vision Suite
Simplify your workflow by connecting clinic and OR2-4
Freedom from binoculars
Revolutionise teaching and improve Ergonomics5

to
microscopes

Assist


Digital Filters
