
This independent optometry practice doesn't sell glasses, so how does it stay afloat?
VERDICT IN ON 'WORLD-FIRST' IOL Australasia's early users discuss where Rayner's new spiral IOL has an edge


This independent optometry practice doesn't sell glasses, so how does it stay afloat?
VERDICT IN ON 'WORLD-FIRST' IOL Australasia's early users discuss where Rayner's new spiral IOL has an edge


Approval of Australia’s first-ever therapy for geographic atrophy (GA), Syfovre (pegcetacoplan), is being hailed a “landmark moment” for the nation’s medical retinal community, as attention now turns to how the drug may be funded, patient eligibility and how eyecare professionals can ensure their patients gain access.
Some of Australia’s foremost retinal subspecialists have also told Insight there are some distinctions between how Syfovre works compared with therapies for neovascular age-related macular degeneration (nAMD), meaning patient expectations need to be carefully managed.
On 27 January 2025, the Therapeutic Goods Administration (TGA) approved Syfovre for the every-other-month treatment of adult patients with GA secondary to AMD with an intact fovea and when central
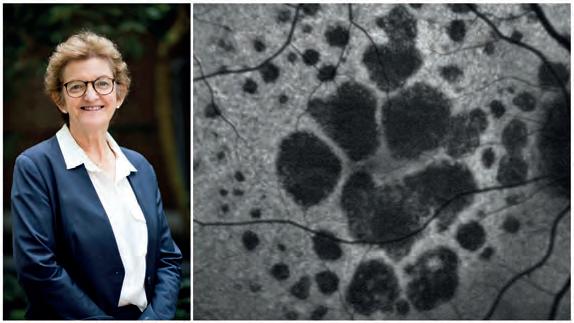
vision is threatened by GA lesion growth. By targeting C3, the drug is designed to provide comprehensive control of the complement cascade, part of the body’s immune system.
Australia became just the second market globally to approve the Apellis Pharmaceuticals-owned drug after the US cleared it in February 2023.
A second GA therapy, IZERVAY by Astellas Pharma, has also been approved in the US and this drug is currently being evaluated by the TGA.
Apellis has faced hurdles in Europe to obtain market clearance and an application for the Astellas drug was withdrawn there.
Professor Robyn Guymer, head
Optometry Australia says it is working with all private health funds towards standardisation, as practices continue to navigate a “minefield” around inconsistent claiming rules with frames, lenses and contact lenses. It comes after the organisation released the latest update to its ‘Private health insurance rules & rebate conditions’ guide, which it began producing eight years ago.
“Health fund entities set their own requirements around claiming for ancillary services, and due to the varied and confusing rules currently in place Optometry Australia developed a private health insurance claiming guide back in 2017 to help members navigate this ‘minefield’,” OA said.
2024 guide is currently on its fifth update.”
A common question practices grapple with is whether a product can be purchased over two years (frames and lenses) to maximise rebate. While most don’t permit this, some do, with some conditions.
Another example is whether a benefit can be provided on a frame-only purchase, if the patient chooses to get lenses elsewhere.
One independent Insight spoke to said a major problem was incontinences around whether patients could use the benefit as a deposit, or claiming before the spectacles were fully paid for.
purchases as the patient is meant to claim only after ordering frames and lenses.
It can be a total quagmire of problems, they said, when health funds become dogmatic about their rules.
OA said communication of rules and changes with eyecare providers was often “lacking”.
of macular research at the Centre for Eye Research Australia, said Syfovre was a historic moment for the Australian GA community who have been waiting for a treatment.
Often, a GA diagnosis led to a slow demise in patients’ vision. They eventually lose their fine, central vision and often rely on low vision support and services to get by in life. Eventually, difficult discussions come about driving and their independence.
Professor Adrian Fung, head of the Westmead Hospital Vitreoretinal Unit in Sydney, said as a medical retina specialist, he also saw patients slowly going blind with GA every day.
“Patients who are highly educated, physically and socially active can become incapacitated and depressed as they lose their

“As an example Optometry Australia is currently negotiating with one provider for audit repayments to be refunded to members – penalised for not following rules which they were never informed about,” the organisation said.
“Work is ongoing in 2025 with all private health funds to help simplify
“Claiming rules have often changed across this period and our November continued page 8
There have also been cases where practices have been asked to refund the health fund for frame-only
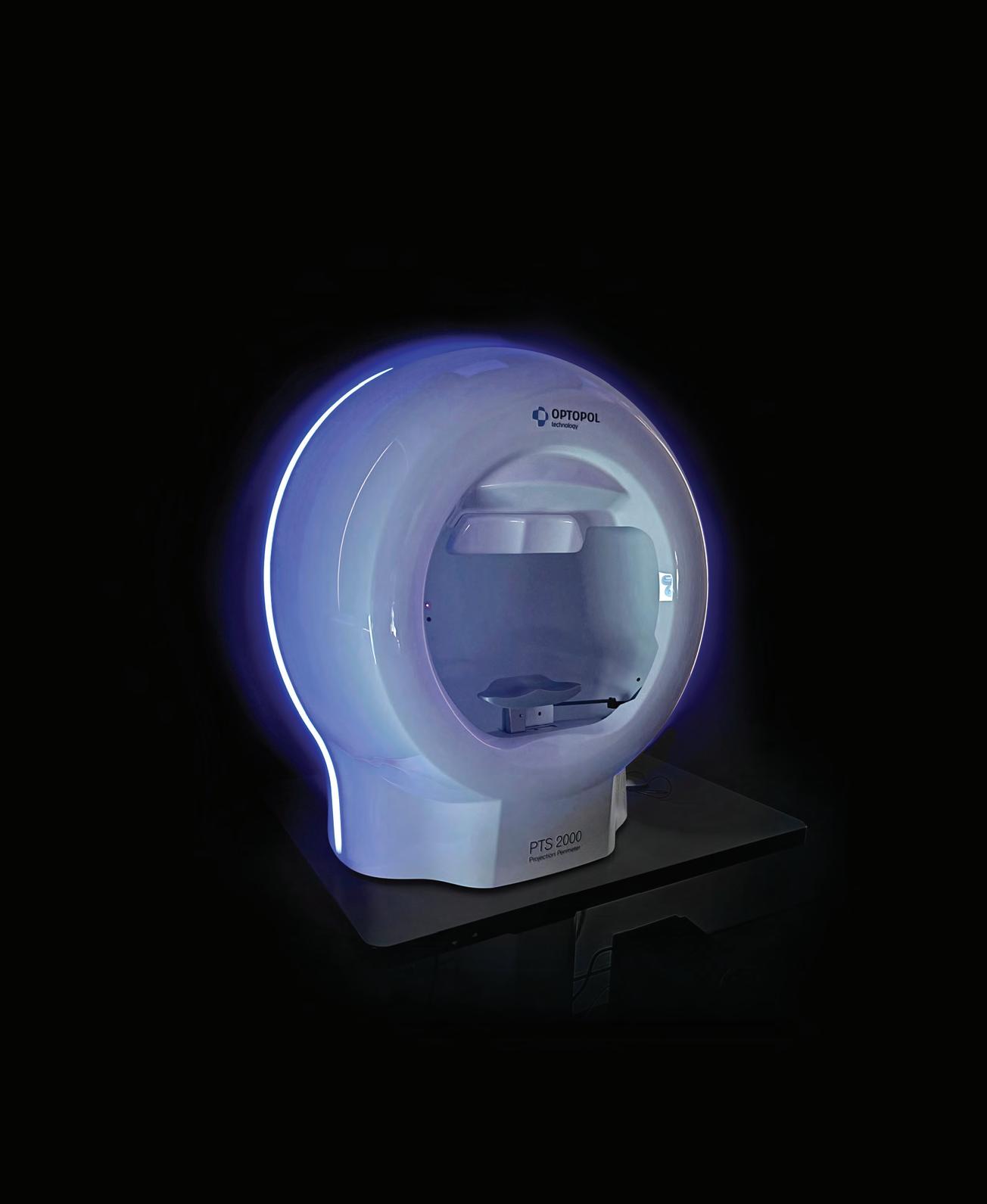
A/Prof Simon Skalicky has had a front row seat to the frustrations patients with glaucoma face. But instead of lamenting the standard of care, he did something about it. How far can the Melbourne ophthalmologist take his new, simplified perimetry test?







ZEISS ANZ invite submissions of unique diagnostic chronic eye disease fundus imaging, captured with the CLARUS 500 or 700, to appear on our online CLARUS image gallery. To view the image gallery just scan the QR code.
Submissions are open to all ANZ CLARUS photographers until 31st March 2025 after which 12 images will be selected by our expert panel to feature in our 2026 CLARUS Calendar (ANZ). Selected images will be announced in April 2025.
How to submit *: Post the CLARUS image to your social media with the hashtag:

Amanda Duffy and James Paton have complementary skills ideal for running an independent practice.

Mark Wymond has taken Aussie eyewear company Modstyle to global markets and quickly gained a foothold.

Toxic relationship
Poor mental health and glaucoma can feed one another, but eyecare professionals can help.

The nation's most experienced ophthalmologists on how they continue to extract the most from their careers.
Have you thought about building a personal brand to prop up your business?
It might sound icky in the age of social media “influencers”, but hear me out, especially if you’re an independent optometrist or run a private ophthalmology clinic.

These ideas aren’t my own, in fact, they are from Australian-born entrepreneur Mr Daniel Priestly who’s an author and has been interviewed on some of the world’s biggest podcasts as of late.
The businesspeople doing the best right now, he says, have two pillars in place: they have built a strong personal brand and placed that alongside an elegant, user-friendly business model.
Priestly, who has worked with some 4,500 founders on this topic, says many want to know if they can build a business brand while running things in the shadows. The answer’s no, and here’s why.
The human brain is not programmed to remember logos and company slogans. Instead, it more readily recognises names, faces and voices. Personal brand gets the most cut through: Richard Branson > Virgin, Elon Musk > Tesla and more historically Steve Jobs > Apple. A key distinction is becoming a ‘key person of influence’, rather than an ‘influencer’.
Instead of being in the spotlight, he urges business owners to "become the spotlight" on their areas of expertise, positioning themselves as an educator and thought-leader that their community can trust and look to.
For the independent optometrist, building a personal brand might sound daunting and unnatural, but using Priestly’s advice, you can start small. For instance, visual or written social media content explaining myopia, dry eye or progressive lens design in simple terms could be a great starting point. Make it consistent, even weekly.
One interesting post I saw from an independent showed five different ways people can fix broken frames themselves while on holiday.
For the ophthalmologist, it might be creating an Instagram Reel showing how you prepare for cataract surgery, explaining new IOL designs in layman’s terms, or having a personal website with links to the locations you practice at.
Also, it doesn’t hurt to form opinions and share them. In a society looking for clear direction, people resonate with this. Maybe you’re ahead of the curve of emerging topics like the influence of diet in dry eye?
Building a personal brand to support your business also makes sense for other reasons. You’ll attract talent, drive purchases of your product and service ecosystem, and make the practice an attractive proposition when it’s time to sell.
Above all, it’s another way to differentiate, creating a business fingerprint that can't be replicated.
MYLES HUME Editor

Just as Insight went to print, RANZCO received a compliance advice letter from New Zealand’s Commerce Commission following an investigation into concerns the college sought to restrict optometrists from receiving training to perform laser procedures. It stemmed from an April 2023 letter RANZCO wrote to fellows, which "counselled ophthalmologists against facilitating optometrists to perform two types of laser eye surgery", despite a legal change in optometrists’ scope in 2022. The investigation was closed after
Researchers in Ireland have discovered that a mutation in a gene called EMC1 causes major vision problems in zebrafish. The fish with this mutation had poorly developed eye cells, weaker responses to light, and changes in the normal structure of their retinas, in findings that could help researchers study eye diseases in humans and create new treatments.
A University of Houston study has shown the benefits of wearing multifocal contact lenses to slow myopia continue even after the lenses are no longer used. The BLINK2 Study also concluded children fitted with multifocal contact lenses for myopia control at a younger age – and continuing treatment until the late teenage years – is a reasonable strategy.
Data from continuous glucose monitors can predict nerve, eye and kidney damage caused by type 1 diabetes, University of Virginia Center for Diabetes Technology researchers have found. The amount of time patients were in a safe blood-sugar range of between 70 and 180 mg/DL over a 14-day period was as good a predictor of neuropathy, retinopathy and nephropathy as the standard approach using hemoglobin A1c levels, the researchers reported.
RANZCO "sent a clarifying letter" on its position. IN OTHER NEWS, Sydney's Circular Eyewear is reinventing the lifecycle of eyewear, transforming discarded glasses into high-quality, traceable new frames. The firm has two components: Spexcycle, Australia’s first closed-loop eyewear recycling initiative; and Objekt Eyewear, a premium sustainable frames range. “Spexcycle and Objekt Eyewear represent a critical step towards building a circular economy within our field, setting new benchmarks for innovation and responsible manufacturing," said founder Mr Chris Savage.
FINALLY, ' Eyes to the future: Optometry improving global wellness' will be the theme for World Optometry Week 2025, kicking off Monday 17 March. According to the World Council of Optometry, this year’s annual celebration will highlight "optometry is far more than just vision correction; it is a key pillar in global healthcare, contributing to overall wellness, disease prevention, and the diagnosis of health conditions that affect more than just the eyes". "When incorporated into health systems, optometry can act as an entry point for detecting a range of health issues," the WCO said.

A global consortium involving Australians has now published 312 gene loci associated with glaucoma, paving the way for new testing techniques. Page 32
7 – 8 March
The 2025 Optical Dispensers Australia International Conference is a biennial two-day event in collaboration with the International Opticians Association. odamembers.com.au
3 – 6 April
Published by:
Complete calendar page 64 insightnews.com.au
The Asia-Pacific Academy of Ophthalmology Congress is taking place in New Delhi, India, with 18 invited speakers from Australia. 2025.apaophth.org
379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766
www.primecreative.com.au
Chief Operating Officer
Christine Clancy christine.clancy@primecreative.com.au
Publisher
Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Assitant Editor
Rob Mitchell
rob.mitchell@primecreative.com.au
Commissioning Editor, Healthcare Education
Jeff Megahan
Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Isabella Fulford isabella.fulford@primecreative.com.au
Head of Design
Blake Storey
Art Director
Bea Barthelson
Subscriptions T: 03 9690 8766
subscriptions@primecreative.com.au
The
continued from page 3
independence, ability to read or see faces of friends or family.
“What this decision does is give ophthalmologists a new therapeutic option and patients hope that their disease can be slowed.”
It remained to be seen whether Syfovre becomes available via the Pharmaceutical Benefits Scheme (PBS), meaning the drug would be government-subsidised and financially viable for most patients. An outcome for this can take “many months”, Prof Guymer said.
She said treatment with Syfovre is administered via intravitreal injections at fixed intervals between four to eight weeks, but unlike nAMD it would not likely be able to be individualised to alter the treatment interval.
In nAMD, most cases end up having anti-VEGF intravitreal injections, but Prof Guymer, who is on the international and local advisory board for Apellis, warned it would not be so straight-forward with GA.
“The decision to treat or not will be based on many factors relating to the actual GA lesion, the vision and AMD status in the eye, as well as individual circumstances.
“So the best advice for now, whilst we await understanding of how and when we can access the new drug, is for clinicians to image the retina, ideally with autofluorescence, so that the rate of growth of the GA lesions can be determined, as this will be one factor to consider when advising on treatment.”
Clinicians, including optometrists, should also take this time to upskill in diagnosis GA secondary to AMD and to be familiar with lesion characteristics associated with fast growth, Prof Guymer said.
“They should also read the trials results of OAKS and DERBY studies (the two pivotal Phase 3 clinical trials which the TGA approval was based on) to be familiar with what was found to be able to inform patients of the trial and its conclusions.”
stands to benefit?
Citing the OAKS and DERBY trials, Prof Fung said the rate of GA expansion can be reduced by about 20% over two years, following monthly or every other month Syfovre treatment. This benefit appears to increase the longer a patient stays on treatment. But two aspects needed to be considered when selecting patients, he said.
“Firstly, the patient needs to understand that this treatment can slow progression of their disease, but not stop or reverse it. They will not experience an improvement in their vision. Spending time educating patients on this aspect is critical to setting realistic expectations and maintaining treatment compliance,” he said.
“Treatment of GA with Syfovre is analogous to treatment of glaucoma with an intravitreal injection if there were no other available therapies. Patients should understand that the benefit of treatment needs to be weighed up against potential complications such as infection, inflammation or macular neovascularisation.”
Secondly, he said the ophthalmologist

“EYES WITH EXTRAFOVEAL, MULTIFOCAL LESIONS, A ‘DIFFUSE TRICKLING’ PATTERN AND ASSOCIATED RETICULAR PSEUDODRUSEN GROW THE FASTEST AND ARE MOST LIKELY TO BENEFIT.”
PROF ADRIAN FUNG
needed to select eyes most likely to benefit. This should include eyes with AMD and not a masquerader of macular atrophy, such as an inherited retinal dystrophy.
“The GA should have been documented to progress on macular imaging. Eyes with extrafoveal, multifocal lesions, a ‘diffuse trickling’ pattern and associated reticular pseudodrusen grow the fastest and are most likely to benefit from this treatment.”
For now, he encouraged optometrists to identify suitable patients and refer them to an ophthalmologist if they are motivated for treatment. Ophthalmologists should also keep a database of their AMD patients, and use imaging modalities such as fundus autofluorescence and en-face OCT to measure growth of geographic lesion size.
“They should be prepared to spend sufficient chair time, so that their patients are properly informed to decide for themselves if they wish to commence this new therapy,” he added.
Prof Andrew Chang, head of ophthalmology at the Sydney Eye Hospital and a vitreoretinal surgeon, said the challenge for eyecare professionals is how to screen, investigate and determine which GA patients would benefit most from long-term intravitreal injections of Syfovre.
“Patients and carers will need to be educated and supported to optimise compliance with therapy and manage their expectations of this new treatment,” he said.
“Clinicians are still learning about the disease and how to investigate the structure and function of the disease and how these correlate.”
continued from page 3
and standardise claiming rules in the optometry sector.”
Dr Rachel David, CEO of Private Healthcare Australia – the private health insurance industry’s peak body with 22 registered health funds representing more than 98% of policyholders – said the organisation was “keen to engage with Optometry Australia regarding any proposals to improve our private health system”.
“We welcome any suggestions for our member funds to consider,” she said.
More than half of Australians (54.6%) have extras cover that includes optical and other

Communication of rules and changes is often ‘lacking’. Image: Andrzej Rostek/Shutterstock.com.
services like dentistry and physiotherapy. The average benefit paid per optical service is $82, in the latest data, with $212.3 million in benefits paid in the September 2024 quarter.
• Can a rebate be used as partial payment at time of ordering if the product is paid in full?
• Can a product be purchased over two years (frames and lenses) to maximise rebate?
• Can a rebate be provided on a frame only if they choose to get lenses elsewhere?
• Do plano lenses need to be retained if a patient purchases a complete pair of prescription sunglasses?
• If a locum/part-time optometrist has undertaken the clinical examination, but is not physically present on the day the health fund rebate claim is made electronically, which provider number is most appropriate to use?
• Optical HICAPS items 225, 228 and 515 are for complete pairs. Can any and all registered providers use these items with your health fund? Or are these only for preferred providers?
• Is it permitted, where contact lenses are purchased in different claiming years, to provide the right lens in one year and left lens in the following year to maximise the patient rebate?
• Is it permitted to claim optical appliances for myself (provider) or on behalf of my spouse, dependents and practice partners?
New analysis says allowing optometrists to prescribe oral medicines for ocular conditions could save the Australian health budget $50 million a year.
The report is to be shared with federal and state health ministers as part of Optometry Australia’s (OA) push for change on the profession’s scope-of-practice.
The organisation is also calling on the Optometry Board of Australia (OBA) to “take action to review and contemporise the Guidelines for the Use of Scheduled Medicines”.
With optometrists able to prescribe oral drugs in other countries with similar health systems, OA has long advocated for this change. However, the move is not supported by the entire industry, with both RANZCO and the Australian Society of Ophthalmologists previously telling Insight they oppose this scope change, stating optometrists don’t have the appropriate medical training and experience, which could compromise patient safety.
The report, The Value of Expanding Optometrists’ Prescribing Rights in Australia, prepared by HTANALYSTS and
commissioned by OA, is an economic analysis of common cases of ocular conditions such as severe dry eye, herpes zoster ophthalmicus, and preseptal cellulitis.
It outlines health budget savings of around $50 million per year, patient savings of approximating $27 million per year, and significant improvements to productivity and access to care through optometrist oral prescribing.
The report also said that allowing optometrists to prescribe oral medicines would mean time savings for ophthalmologists by reducing “unnecessary onward referrals”.
It compares the patient journey, system and patient costs, professional time saved, and productivity implications of treating various ocular conditions now and into the future, enabled by optometrist oral prescribing.
Key highlights of the analysis include:
• Treatment of severe dry eye by optometrists with oral medicines has the potential to save over 700,000 GP visits per year, equating to over $30 million of federal funding, and $8 million of patient

The move could save 700,000 GP visits per year for severe dry eye. Image: doucefleur/stock. adobe.com.
incurred expenses, in addition to almost 200,000 ophthalmology appointments being saved for more critical conditions. Treatment of acute angle closure glaucoma by optometrists, when a patient does not have appropriate access to emergency ophthalmologist care, would not only improve visual outcomes, but would also save around $8500 per patient in treatment costs.
An OA media release said the Federal Government’s Scope of Practice Review – Unleashing the Potential of our Health Workforce – had acknowledged that there is “strong evidence of improved consumer access to care, consumer experience of care and health outcomes when health professionals are enabled to work to full scope-of-practice”.

OA has also released a Position Statement on Medicines, outlining its position on the prescribing of medicines by optometrists.
“Australia’s approximately 7,000 optometrists currently face significantly more limitations to their scope-of-practice than their counterparts with similar training in other countries,” OA said.



ZEISS is inviting Australian and New Zealand eyecare professionals to submit images captured on its CLARUS 500 or 700 retinal imaging system to be featured in a gallery exhibition and photo calendar. From 1 February to 31 March 2025, ZEISS ANZ is seeking CLARUS users' “unique diagnostic chronic eye disease fundus images” to feature in the CLARUS Gallery and 2026 CLARUS Photo Calendar. They will be reviewed by an expert panel, with 12 images to be selected for display at the CLARUS Gallery exhibition on 14 May 2025 at Stanley Street Gallery in Darlinghurst, NSW. Selected images will also feature as a monthly page within the 2026 ZEISS ANZ Capture with CLARUS calendar, which will be released in November 2025. Entries can be submitted through LinkedIn or Facebook by accompanying a unique chronic disease photo with the hashtag: #ZEISSCLARUSWOWANZ
Organisers of the third Asia-Pacific Strabismus and Paediatric Ophthalmology Society (APSPOS) Congress, taking place in Brisbane 29 June to 1 July 2025, have unveiled the theme for the event: ‘Inspiring Collaboration’. The congress will highlight the importance of multidisciplinary approaches when delivering world-class care for children and adults with visual impairments. Some key highlights include a focus on collaborative care, myopia prevention and amblyopia management. The congress will also highlight the importance of strengthening partnerships between ophthalmologists, orthoptists, optometrists, and other allied health professionals to improve patient outcomes. Sessions will cover topics such as team-based care models, integrated patient pathways, and collaborative strategies for tackling complex cases and new approaches to amblyopia treatment.
Volk Optical is celebrating a major milestone in ophthalmic visualisation with the launch of its 50th Anniversary Lens Collection. Available through Designs For Vision, part of ParagonCare, the limited-edition series features lenses “adorned in a striking champagne-gold colour, symbolising five decades of innovation and excellence in eyecare technology”. The 50th Anniversary Lens Collection includes a range of specialised lenses designed for various ophthalmic applications, such as the Classic Series, Super Series, and Digital Series. Each lens is crafted to provide superior visualisation, ensuring that eyecare providers can deliver optimal patient outcomes.
EssilorLuxottica’s Nuance Audio Glasses – spectacles incorporating hearing aids –have received approval for use and sale in the US and European markets, with plans to make them available in its own retail network, traditional audiology practices and for optical wholesale customers.
The company is marketing its Nuance Audio Glasses as a “breakthrough in hearing technology” and an “over-the-counter (OTC) hearing aid integrated into smart glasses for perceived mild to moderate hearing loss in adults aged 18 and over”.
The audio component is invisible as it is embedded within the spectacle frames. Optional lens upgrades, which are not required for use, include customising the glasses with the client’s preferred optical lenses, whether they need a prescription, Transitions lenses or blue light filtering. The product includes a wireless charging pad.
A companion app personalises the listening experience, the company said, while the glasses’ “open-ear design and directional microphones ensure comfort and clarity in challenging auditory environments, such as noisy trains, busy offices, or lively restaurants”.
EssilorLuxottica announced on 3 February 2025 that it had received clearance from the US Food and Drug Administration (FDA) for its OTC Nuance Audio Glasses.
The group simultaneously achieved the CE marking under the Medical Devices Regulation in the EU, alongside the development of an ISO Quality Management System certification dedicated to Hearing Aids, which will allow Nuance Audio to launch in Europe.
Open-ear design and directional microphones help wearers in challenging auditory environments. Image:
“Paving the way for a disruptive new category in the med-tech space, Nuance Audio Hearing Aid Software is the first FDA-cleared, preset Software as Medical Device (SaMD) in the US,” the group said.
“It delivers a groundbreaking open-ear
hearing solution seamlessly integrated into a pair of stylish smart glasses. After decades of adoption barriers ranging from comfort to visibility, consumers will finally be able to see clearly and hear clearly with a single product that is both beautiful and highly functional.”
The glasses will be available for purchase in the US in Q1, and in the first half of 2025, they will be available in European countries including France, Germany and UK, starting progressively from Italy in Q1.
“As part of EssilorLuxottica ’s open business model, the group will leverage its extensive retail network, while also engaging both traditional audiology practices and optical wholesale customers to make this technology accessible to consumers wherever possible,” the company said.
Mr Francesco Milleri, chairman and CEO of EssilorLuxottica, said that two years ago, the business set out to “create a first-of-itskind product that would change the way people see and hear”.
“We didn’t just aim to combine two medical devices – we created an entirely new smart glasses form factor to support the two human senses we depend on the most.
"It is not only groundbreaking, but also incredibly accessible.
“We’re pleased now to turn our focus to getting this life-changing technology into the hands of people around the world who truly need it.”
The product was recognised as an honoree in the digital health category of the 2025 Consumer Electronics Show (CES) Innovation Awards in Las Vegas from 9 to 12 January 2025, attended by 141,000 people.
Meanwhile, EssilorLuxottica announced on 2 January 2025 that it had acquired Pulse Audition, a French start-up delivering AI-based noise reduction and voice enhancement through algorithms, allowing people with hearing impairment to better understand speech, even in noisy environments.

By integrating its proprietary technologies, expertise in AI software development, embedded AI, and audio signal processing, EssilorLuxottica said it would complement proprietary hardware and software to improve the quality of its products and solutions.
The buy aligns with the group’s strategy in the hearing solutions space, marking an evolution in the journey started in 2023 with the acquisition of Nuance Hearing, it said.
See the bigger picture with more images, information, efficiencies.

optomap is multimodality imaging technology, able to generate high-resolution 200° ultra-widefield (UWF™) images to visualise vitreoretinal, retinal and choroidal layers from pole to periphery.1
9 * modalities including OCT make a practice…


HOYA Vision Care has launched a new power range of MiYOSMART spectacle lenses, specifically designed for children suffering from high myopia.

The company said the extended power range was designed to unlock MiYOSMART spectacle lenses for patients with a broader range of negative and cylindrical powers, has a slimmer edge thickness compa red to previous MiYOSMART spectacle lenses, and can be housed in a wider selection of frames to suit individual requirements and preferences due to their larger diameter.
Image: HOYA.
Nominations are now open for the revamped industry awards at ODMAFair 2025.
From 3 February to the end of March 2025, businesses can be nominated for the awards, before final voting begins in April. The winners will be announced on Friday, 27 June at the ODMA Fair in Darling Harbour, Sydney. ODMA CEO Ms Amanda Trotman said: "This year, we've designed the awards to ensure the entire industry can participate –from storefronts to product innovation."

This year’s awards featured an “impressive line-up of categories to celebrate excellence and innovation across the industry”. They included:
• Independent Practice of the Year –Self-nominated or nominated by providers. Nominators are asked to provide wording and images if applicable. Examples could include renovations, team, customer service, local industry involvement, good news stories, staff retention, and practice financial or patient results.
Nominated by independent optical businesses as to who gives the best service.
• Instrument of the Year - Nominated by independent practices as to what piece of equipment they are using and why.
• Versatile Frame of the Year - Nominated by independent practices. What frame has stood out over the last 12 months for its appeal to people, its versatility for different shape faces, colour range, adaptability, etc.
“There is an urgent need to provide comprehensive solutions for children with high myopia as early as possible in order to reduce the risk of myopia-related complications in later life,” said Dr Natalia Vlasak, global head of Medical and Scientific Affairs at HOYA Vision Care.
“Slowing down the progression of myopia by just one diopter can reduce the risk of myopic maculopathy by 40%.
“With the extension of MiYOSMART’s power range to treat high myopia, it is not too late for these children to preserve their vision health for the future.”
The company said the power range extension accommodated both high myopia and astigmatism, with a wider span of prescriptions up to a highest combined power of -13.00 D. This action will increase access to effective and innovative solutions for more myopic children, so they can achieve better vision outcomes.
Within the new power range extension, MiYOSMART spectacle lenses are now available in larger lens diameters and with optimised lens edge thickness.
The increased lens diameters mean that the lenses can be housed in larger frames, accommodating older children and teenagers with larger pupillary distances, in addition to those who choose these frames for aesthetic reasons.
The practice is located in Paradise Point, north of the Gold Coast. Image: Eyecare Plus.
• Supplier of the Year – Nominated by independent practices as to what instrument is used in the practice and is highly valued and why.
• Top Supplier Customer Service Team - Nominated by independent optical businesses.
• Sales Representative of the Year -
• Window Dressing - Best independent practice window dressing. Window displays that have stood out, gained great results and helped attract new clients. Nominate up to two different window displays and send up to two images of each display.
For more information, visit: odmafair.com.au/awards.
Independent optometry business partners
Mr Michael Hare and Mr Jonathan McCorriston have opened a greenfield practice, Eyecare Plus Paradise Point, in Queensland.
“With a legacy spanning over four decades, their fourth practice is a big plus for patients living at the northern end of the Gold Coast,” Eyecare Plus National Office said.

neighbouring areas Southport, Benowa and Burleigh.
McCorriston recently became a co-owner of the practices, partnering with Hare – a longtime mentor – having worked alongside him for 20 years.
Their four locations are all busy and the duo say they have surrounded themselves with a wonderful, highly skilled team.
“It's very gratifying to know the combined knowledge, experience and enthusiasm shown by partners and staff is infectious –and the key ingredient for continued growth,” they said.
“Independent optometry is about playing to our strengths – our expertise and the personalised care we provide,” Hare said.
“Our goal is to not only protect but also enhance the vision and quality of life for every patient who walks through our doors."
Clinician-scientist Professor Lauren Ayton AM has been named a Member of the Order of Australia as part of the 2025 Australia Day Honours List.
The award recognises her “significant service to optometry, ophthalmology, and public health as a clinician and researcher”.
Prof Ayton, a researcher at the Centre for Eye Research Australia (CERA), was honoured and humbled, according to a statement.
“Research is a huge team effort, and this award is a credit to the efforts of the many teams I work with to raise the profile of eye health and find new ways to stop vision loss,” she said.
On Linkedin, she added: “And a huge thank you to everyone who has taken the time to text, message, call and/or give me a big hug on this news.
"My favourite moment has been watching my kids and their friends excitedly read about it in the paper.”
Prof Ayton currently holds dual
appointments at CERA and the University of Melbourne, and her current research focuses on inherited retinal diseases – the leading cause of blindness in working-aged adults.
At CERA she co-leads the Retinal Gene Therapy Unit and VENTURE inherited retinal diseases registry, alongside Dr Tom Edwards.
As well as pioneering clinical trials for gene therapy, her work connects families who have a history of genetic vision loss with clinical trials for new treatments as they emerge.

to me,” Prof Ayton said.
She noted the advances in gene therapy and new treatments beginning to enter clinical trials, offering hope to people who otherwise faced irreversible
“It is such an exciting time to be researching eye diseases, especially inherited retinal diseases.
“There is a wave of treatments on the horizon that will soon be entering clinical trials – I’m excited to be a small part of the clever and passionate teams helping lead this work.”
She is an advocate for the low vision community and holds a number of leadership positions, including on the board of UsherKids Australia, the scientific and medical advisory committee of Retina Australia, and the board of the Australian College of Optometry.
“I had a brother who was blind due to a brain injury, so efforts to restore vision are both deeply important and personal
CERA deputy director Professor Robyn Guymer AM congratulated Prof Ayton on the award.
“We’re thrilled to see Professor Ayton recognised in this year’s Australia Day honours.
“She has worked tirelessly to help those with poor vision in the community, especially those with inherited retinal disease. We all offer our hearty congratulations.”

Alcon has acquired Australian company
Cylite and its Hyperparallel Optical Coherence Tomography (HP-OCT) technology.

deal took place in January 2025. Images: Konektus Photo/ Shutterstock.com & Cylite.
Alcon confirmed it would "not continue to commercialise the standalone HP-OCT device".
"However, we look forward to providing updates in the future on how we are integrating this innovation into our growing eyecare diagnostics portfolio."
Cylite was founded in 2013 in Melbourne with the backing of four prominent Australian scientists – Dr Steve Frisken, Mr Grant Frisken, Mr Trevor Anderson, and Dr Simon Poole – drawn from the fields of photonics, optics, instrumentation, and software development.
It was thought to be the only Australian company working in the ophthalmic diagnostic OCT space, a segment traditionally dominated by the US, Germany, and Japan.
Cylite has been an Australian manufacturing success story, with the company able to develop, scale and commercialise its highly specialised medical technology in-house at its Melbourne factory, under Ms Kylee Hall, who took over from Dr Steve Frisken as CEO in April 2022.
While OCT is mostly perceived as a retinal imaging system, the HP-OCT’s greatest initial strength has been in the front of the eye where it creates true volumetric, or 3D, images of intricate anterior segment structures in a single snapshot. It has retinal capability too.
Scans are acquired at industry-leading rates of more than 300,000 A-scans per second. This means it can capture a full biometry scan in seconds, enabling accurate, motion- and artefact-free measurements of all ocular surfaces.
The technology is already in real world clinical use.
Cylite said: “We are thrilled that the global leader in eyecare sees the immense potential of our cutting-edge technology for whole-eye OCT imaging and measurement diagnostics.”
Australian firms and global companies in the ophthalmic sector have featured prominently in a list of the world’s most trusted healthcare businesses.
In fact, right at the top of Newsweek’s list of the world’s most trusted Healthcare and Life Science businesses is Australia’s Cochlear, which took the top spot for its work in manufacturing implantable hearing devices, which are distributed around the globe.
Australian Clinical Labs, a private provider of pathology services, secured the ninth spot, while CSL Limited, Australia, which produces Ikervis and Cationorm eye drops for dry eye disease, among its many medical offerings, was placed 37th.
Other ophthalmic businesses that made the list were German manufacturer of optical systems and optoelectronics Carl Zeiss Meditec at number six, and Canadian eyecare giant Bausch + Lomb in 24th spot.
A Newsweek media release said trust was “an essential part of any relationship –from personal relationships to ties between businesses and consumers”.
It said trust was “on the decline across various industries, with concerns about data privacy, the use of AI and lack of marketing transparency emerging in the

fast-paced global economy”. Newsweek said the list recognised companies that had earned the confidence of consumers, investors and employees by producing quality products, paying employees fair wages and appointing effective leaders. The ranking was based on an independent survey of more than 70,000 participants and 230,000 evaluations from customers, investors and employees who responded to prompts like "I trust this company's advertising and communications claims" and "I believe this company treats its employees fairly." It also incorporated "social listening”, an analysis of company mentions across social platforms.

He leaves a legacy of “enthusiasm, innovation, dedication, and unwavering commitment”.
Image: Corneal Lens Corporation.
Mr Graeme Curtis, the well respected owner of New Zealand’s Corneal Lens Corporation, has passed away.
He died on 9 January 2025 after a battle with cancer.
“It is with profound sadness that we announce the passing of Graeme Curtis,” Corneal Lens & Contact Lens Corporation Australia (CLCA) said in a statement.
“Graeme leaves behind a legacy of enthusiasm, innovation, dedication, and unwavering commitment to the eyecare industry.
“For many years, Graeme was the driving force behind our organisation. His vision and leadership shaped Corneal Lens Corporation into the trusted and innovative company it is today.
“He built not only a successful business but also long-lasting relationships with all those he worked with – valued customers, suppliers, and colleagues alike.”
The company wanted to assure its customers that the operations of Corneal Lens Corporation would continue as usual.
“Our team remains committed to upholding the high standards and values that Graeme instilled in us.
“We understand that many of you had personal and professional connections with Graeme. [His] legacy will live on in the work we do and the relationships we cherish.”
A funeral service was held on 16 January.

An analysis of pain and anxiety experienced by patients has concluded that those having immediate sequential bilateral cataract surgery (ISBCS) reported significantly decreased anxiety scores before the second surgery.
And it suggested that ISBCS may be a good strategy for more anxious patients who expect to experience increased pain during the second operation.
The research at Korea University Guro Hospital’s Department of Ophthalmology compared pre-operative anxiety and intraoperative pain between the first and second cataract surgeries in patients who underwent ISBCS.
This retrospective study was conducted between 20 June and 20 September, 2023, and involved a total of 170 cataract surgeries, with 130 eyes undergoing ISBCS, and 40 eyes unilateral cataract surgery.
Among the unilateral cataract surgery patients, 13 (7.65%) had previously experienced cataract surgery on the other eye, while 27 (15.89%) had not undergone
previous cataract surgery.

In the study, each patient’s anxiety score and pain score were measured at the operation room immediately preceding and immediately following each surgery.
Before starting the surgical draping, patients were asked their anxiety level using the visual analog scale for anxiety of between 0 (no anxiety) and 10 points (overwhelming terror).
After the surgical procedure, the pain score was investigated using the VAS for pain, from 0 points for no pain to 10 points for unbearable pain.
The results showed a significant drop in

anxiety between the first and second ISBCS surgeries, but not pain.
The researchers said “it is possible that ISBCS patients might have overestimated the pain score of the first surgery”.
“When we compared anxiety and pain scores from the first ISBCS surgery and the first unilateral surgery, they did not statistically differ. Also, there was no statistical difference in either score between the second ISBCS surgery and the second unilateral surgery.”
They concluded that ISBCS patients reported significantly lower anxiety scores before the second cataract surgery.
One reason could be the shorter time between the surgeries, they said.
After a positive experience during the first cataract surgery, patients feared the second surgery less, they said.
“We suggest that, as the interval between the ISBCS first and second surgeries is short, ISBCS patients have a relatively vivid memory of the previous surgery as the time gap between the two surgeries is not sufficient to induce recollection error.”


Australian researchers have established that a vascular ‘fingerprint’ at the back of the eye can accurately predict stroke risk.
The study, which involved researchers from the University of Melbourne, Monash University and Hong Kong Polytechnic University, and which was published by the Centre for Eye Research Australia (CERA), showed that the ‘fingerprint’ was as accurate as traditional risk factors and could be used without the need for invasive tests.
Stroke affects around 100 million people around the globe and kills 6.7 million every year.
A media release supporting the research said the 'fingerprint', comprising 29 indicators of vascular health, was a practical and readily implementable approach “that is particularly well suited for primary healthcare and low-resource settings”.
“The retina’s intricate vascular network is known to share common anatomical and physiological features with the vasculature of the brain, making it an ideal candidate for assessing damage from systemic ill health, such as diabetes,” said the researchers.
“Its potential for stroke-risk prediction
Researchers have found a new way to potentially predict stroke risk, using eye scans. Image: Sudok1/stock.adobe.com.

hasn’t been fully explored, due to variable study findings and inconsistent use of the specialised imaging technique for the back of the eye— fundus photography.”
They said machine learning (AI), such as the Retina-based Microvascular Health Assessment System, had opened up the possibilities for the identification of biological markers that could predict stroke risk.
To explore this further, they measured 30 indicators across five categories of retinal vascular architecture in fundus images from 68,753 UK Biobank study participants. The five categories included calibre
(length, diameter, ratio) density, twistedness, branching angle and complexity of the veins and arteries. And they accounted for potentially influential risk factors: background demographic and socioeconomic factors; lifestyle; and health parameters, including blood pressure, cholesterol, HbA1c (blood glucose indicator), and weight (BMI).
In all, 118 retinal vascular measurable indicators were included, of which 29 were significantly associated with first-time stroke risk after adjusting for traditional risk factors. Over half (17) were density indicators; eight fell into the complexity category; three were calibre indicators; and one came under the twistedness category.
Each change in density indicators was associated with an increased stroke risk of 10-19%, while similar changes in calibre indicators were associated with an increased risk of 10-14%.
Each decrease in the complexity and twistedness indicators was associated with an increased risk of 10.5-19.5%. This retinal ‘vascular fingerprint’ was as good as the use of traditional risk factors alone for predicting future stroke risk, the findings showed.








When the Kiwi optometrist decided on a very different business model, many in the industry thought he was a little crazy. Now they are thinking he might be more than a little right.
You would have heard the one about the pub with no beer. But have you heard the story about the optometrist with no glasses?
While Slim Dusty famously sang that there was “nothing so lonesome, morbid or drear than to stand in the bar of the pub with no beer”, the optometrist with no glasses can report happy clients, happy colleagues and a very happy bank manager.
And Mr Alex Petty, owner of Bay Eye Care in Tauranga, New Zealand, doesn’t see his venture as simply a bizarre experiment or quirky outlier; he’s convinced it’s the future of the industry.
Before we can get to that future, we need to understand a little more about his past, and the motivation – some of it existential – that has brought him to this present-day, alternate ophthalmic universe.
Petty’s own focus on optometry as a career began with the lack of focus in his own vision.
Severe myopia as a young child meant plenty of trips to the optometrist.
“I’ve always had eye problems myself, which meant that I’ve always been exposed to someone peering in my eyes as a kid and a teenager,” he says.
And the New Zealand-born youngster was also exposed to plenty of different methods as the family travelled extensively in the wake of his civil engineer father, who worked on wastewater projects around the globe.
Petty might have been given a wider view of the world but, sadly, the optometry of the day had a narrow field of view when it came to combating myopia – it was
single vision glasses, glasses and more glasses, with contact lenses added to help with sport.
“Anyone who’s practised through the 90s and early 2000s will know that, unfortunately, there wasn’t that knowledge about myopia, that there was actually a way of controlling that excessive eye growth.
“I was gutted a little bit that I missed the boat in terms of myopia control being an option and I kept getting stronger glasses, stronger contacts and ended up being very short-sighted by the time I was in my mid-teens and, probably not surprisingly, having three retinal detachments.”
That didn’t dim his enthusiasm for optometry, however.
A strong interest in maths and science, and a “really healthy respect for being able to change someone’s life in terms of giving them vision” led to optometry studies at the University of Auckland, from which he graduated in 2010.
University drove a passion for some of the more interesting aspects of optometry; a passion that took flight as his passport bulged and education broadened in trips and clinics around the world, including to South America and the United States.
Petty and Rachel, the woman he would later marry, ended up in Adelaide, where he worked with well-known Australian optometrist and contact lens authority Mr Lachlan Hoy, who opened the Kiwi’s eyes even more to the possibilities of the profession.
As a young myope, Petty had gravitated towards contact lenses.

“Having that freedom of sight without having a frame on your face is something I think, for a child especially, was huge.”
Later, as a professional, his work with Hoy strengthened that passion and fuelled greater interest in orthokeratology and other special interests.
Hoy became something of a mentor as the pair introduced the little-known intense pulsed light (IPL) device at the time, and established the first myopia control clinic in South Australia.
The boy who had previously only known single vision correction for his eye condition was now the man with new tools to help treat it in future generations.
“Lachlan was a trailblazer, and still is in his own right, so working in that environment certainly highlighted to me how those areas could become a big part of a practice.”
Petty was starting to get a sense that things could be done differently.
“The specialisation side of things was really probably the engine room of Lachie’s practice,” he says.
“And we were talking, on a Friday night after a busy week, and he said, ‘look, if I could do things again, differently’ – because he had bought into a big, established practice – ‘I’d buy a few pieces of really important equipment, and I’d just see patients, just do contact lenses, just manage ocular disease, low overheads, and that’s how I’d do it.’”
It was a throwaway comment – two professionals ruminating on their paths in the industry.
But it stuck.
And after Petty and Rachel moved back to New Zealand, and he struggled to find the right role in Auckland, that idea began to nag once more.
It grew louder when his bank manager suggested that, rather than buying into an Auckland practice, he could maybe target opportunities further south and go out on his own.
That chorus for change grew even more when they moved to Tauranga and he considered his options there.
“There were really nice, established optometry practices, with great clinicians and a collegial group,” he says. “But no one was really fitting or doing ortho-k in a big way, no one was fitting scleral lenses, no one was doing dry eye in a really comprehensive way with things like IPL treatment. And these were all things that had been my bread and butter over the last few years.”
That conversation with Hoy jumped into his head once more.
The chorus had become a crescendo.
Even the bank manager was in tune.
So in 2017, Petty set up the Bay Eye Care consulting practice in a single room at a GP’s clinic, specialising in the use of contact lenses, orthokeratology, myopia control, ocular disease management, dry eye and glaucoma.
It was just Petty, plenty of high-end diagnostic equipment, an IPL device and not a single pair of specs.
His reputation grew, as did word of mouth and referrals from GPs, ophthalmologists, even other optometrists lacking his specialist skills. And a few years later he was moving into his own, bigger three-room clinic,

“Optometry now, especially our areas of medical knowledge, really doesn’t align very well with retail. I think those are two completely different things.”

with two consulting rooms, and one equipment and testing room.
Since then, he’s also taken on another optometrist, Mr Aidan Quinlan, and office manager Ms Georgia Crawford.
But interestingly, and crucially, no dispensing staff. The only things dispensed are contact lenses, drops and solutions, good advice and treatment support.
Petty has no regrets. Only positives. And plenty of people keen to pay for his services.
“It’s about charging what you’re worth, making sure that you have the technology, equipment and the treatments that drive patients to your practice, and then making sure patients see the value in what you can offer them.”
All of which are laid out in a comprehensive list of consultation fees, most of which must come from a patient’s own pocket because New Zealand does not subsidise much of what Petty offers.
Another thing he does not have are high overheads.
“We don’t have dispensary opticians or front-of-house staff choosing the frames,” he says. “We don’t have money kept in stock; we’ve got a much smaller footprint with consulting rooms rather than a big floor for glasses, so our costs are much smaller as well.”
Revenue can be a tricky topic to discuss, but Petty is happy to offer two thumbs up when asked about the profitability of his business. And he reports his bank manager is also happy.
So successful is this “different way of thinking” that Petty believes it’s the future of the industry.
“Optometry now, especially our areas of medical knowledge, really doesn’t align very well with retail,” he says.
“I think those are two completely different things.
“If we look at optometry in 30 years’ time, I think it’d be very much optometry managing eye disease and offering management of eye conditions, and opticians managing the glasses and frames.
“The dispensers would be worth more, the optometrist would be worth more to a patient, and I can see that being very successful.”
Nothing has been able to shake Petty’s resolve. Not even an existential crisis.
When he was diagnosed with rectal cancer four years ago, the then 33-year-old father of one, with another child on the way, had plenty to think about as he endured surgery and three months off work.
The “heartwarming” support of his patients made him realise he was on the right track, and a desire to spend more time with family encouraged him to double-down on the business model and hire the extra optometrist, allowing reduced hours at the clinic.
Alex Petty Bay Eye Care
When he started down this alternative path, many colleagues thought he was crazy. Now they look on with envious eyes.
The optometrist with no glasses – maybe that could become a catchy tune.
He fled to Australia at the age of five, part of a family keen to flee an Iraq savaged by war. Now this award-winning optometrist is giving back to the community that gave him a second chance.
Not many Victorians can talk about COVID in a positive light.

But as the conversation turns to the pandemic that held much of the world in a vice-like grip, optometrist Dr Mohammed Al Ebrahimi leans back and flashes a huge smile.
That’s because while Victoria was busy racking up days in lockdown, Dr Al Ebrahimi was just as busy making the most of his own enforced isolation.
“COVID turned out to be a positive experience for me,” he says. “It was my fourth year at Melbourne University, but there was no requirement for me to go to uni or do a placement.”
While Dr Al Ebrahimi was busy finishing his optometry degree, the idea of a health empire came to fruition.
This involved establishing an aged-care business supported by a range of critical allied health services, of which optometry was just one.
“I was busy because COVID hit aged care hard, and we were full gear, helping people,” he says.
The irony is that the tables had turned for Dr Al Ebrahimi and his family.
They were the ones who had endured long periods of hardship, not only in their perilous journey 24 years ago, but also the struggles of adapting to a strange new culture in their adopted home.
They might have made it to the Lucky Country but they were the ones who needed help and for them, the only way out was hard work and education.
While other primary school children were doing homework, their parents reading to them, Dr Al Ebrahimi was struggling with a new language, foreign education system and a tiger mum.
“My mum's way of education is, ‘there's a massive textbook you’ve got to study’.”
And study he did. Not just the textbooks but also the Aussie way of life.
“They gave me an education, free health care, support; I think the great thing about Australians is that they are very giving people.
“So I tried to understand the Australian culture and fit into Australian society.”
“Mate” is spread liberally through the conversation; he even played a bit of footy.
But AFL wasn’t his future. Driven by a family that prioritised education and hard work, and keen to give something back to his new home, he studied optometry at the University of Melbourne.
“I am very passionate about healthcare, and I fell in love with optometry because it's a critical part of life,” he says. “Almost everybody's got some form of vision problem, everyone's going to need an eye test, no matter where they are in their life journey.”
As passionate as he is about optometry, he is equally passionate about business.
His vision stretched beyond optometry to a wider, more holistic view of health, the large number of people struggling for access, and the opportunities that represented.
“I've always been business-minded,” says Dr Al Ebrahimi. “I started when I
was 17, 18 years old, providing vocational education to the migrant community.
“But I realised they were applying for jobs and were not getting an opportunity because of the language barrier.”
In one hand he had plenty of qualified people struggling to find work; on the other, the aged care industry was struggling to find workers and support.
Those pockets of unmet need would become the bricks with which his growing healthcare empire would be built.
So while Dr Al Ebrahimi studied for his optometry degree, he was also working hard to bring those two together, establish an aged care business and lay that next brick.
What he now jokingly refers to as “side hustles” became serious business ventures encompassing allied health services and support for the elderly, the disabled and many others in the migrant community.
“In 2021 I wanted to build the Costco of healthcare,” he says.
COVID provided another opportunity.
Failing businesses left faltering leases and empty buildings, so “I came in and signed a 15-year lease” and People First Healthcare was born.
The business was built on a vision of delivering exceptional quality care within the age care and disability sectors while helping to alleviate the suffering and isolation that many people, especially older migrants and refugees, found themselves.
Three years later, Dr Al Ebrahimi is CEO of the People First Healthcare group, a business employing over 400 staff in Victoria, New South Wales and Queensland.
Most of these staff were the ones who had been held back by language and cultural barriers.
But thanks to the vocational training business that Dr Al Ebrahimi had started in his teens, they have found meaningful employment and a whole new pathway in life.
Today, the People First Healthcare group offers a range of services that are much greater than the original vision of optometry and aged care, including

"Australia
has given me an opportunity to get an education, make a living and obviously support the community. So I've always had the motivation to give back to the community." through my business ventures.”
Dr
Mohammed Al Ebrahimi People First Healthcare


Australians, including migrants and refugees.
“So I set up this not-for-profit organisation and the sole purpose is to break people from isolation, who are vulnerable, who might go to the pokies for
example, who need to be part of something.
“We bring these older people in, take them out on buses to the zoo or the park.”
This and the healthcare business are an important part of Dr Al Ebrahimi’s work to give back.
“I came to Australia as a refugee from Iraq,” he says. “Australia has given me an opportunity to get an education, make a living and obviously support the community.
“So I've always had the motivation to give back to the community through my business ventures.”
He loves Australia, and the feeling is mutual.
Victoria nominated him as its 2025 Young Australian of the Year, for which he was named as a finalist, and recently he was one of 20 “outstanding health professionals” in the Stronger Medicare Awards.
At 29 he has accomplished so much.
All of this means he is now ‘semi-retired’ as an optometrist – “I leave my fantastic optometrist to do what they love, seeing patients in the room”.
But the profession is never far from his mind.
On the “vision board” behind him is a large Specsavers logo.
He admires the company’s business model and its national coverage.
“I think they do a fantastic job, I want to be in a place where I can run my business all around Australia.
“My vision is to provide different communities with care and love and compassion, provide health care. And I guess the vision is to be an Australian brand that's national, bringing the service to their home or they can come to the clinic.”
He’s young, smart, ambitious.
He doesn’t sleep much.
Australia’s first plant-based optical lenses. ECO6 is the first lens material crafted entirely from plant-derived resources, revolutionizing traditional optical lens manufacturing.
By replacing petrochemicals with biomass plant-based materials, ECO6 is designed to significantly lower greenhouse gas emissions compared to conventional petroleum-based products. crlabs.au/range/eco6

You wouldn’t bet against him. Join the green revolution.

An optometry qualification isn’t necessarily the only ticket towards independent practice ownership, which can be configured in many ways regardless of job title.
Independent optometry practice isn’t for everyone, but it also isn’t limited to a certain ‘type’ either. The Type A optometrist, perhaps, is the first stereotype that springs to mind.
Young mums, orthoptists, optical dispensers and even more mature practitioners have all taken the plunge into independent ownership within the Eyecare Plus network in recent times – bringing their own flavour of primary eyecare through various ownership structures.
Diversity across the network of 120 businesses is one of the hallmarks of Eyecare Plus. It’s something high performance manager Ms Yvette Safier says the organisation is proud of and brings value to members.
“At our recent meetings it has been great to hear the views of both young and more mature members – they can learn a lot from each other,” she says.
“Younger members are often better at social media and digital advertising, are happy to give things a try and have a lot of energy. Our more mature members have experience under their belt, they have done the hard yards and recognise where to divert their energy.”
The Eyecare Plus group has some clear distinctions. For example, members can opt to align their practice brand under the Eyecare Plus banner to leverage national and sophisticated marketing campaigns, or they can co-brand to also benefit from this. Others choose to maintain their own brand identity. It operates under a protected territories model so practices aren’t competing in the same communities, promoting collegiality. Members have complete independence and can opt into any initiatives by head office, and have autonomy over their product mix.
But another key feature is that membership, and therefore ownership, is open to non-optometrists.
“And we have some members who are optical dispensers, as well

“Owning a practice will mean that you have to put in the hard yards to get it established – it won’t be a 9 to 5 job – but the effort you put in during the early years will pay off later.”
Yvette Safier Eyecare Plus
as some partnerships between optometrists and optical dispensers,” Safier adds.
Beyond job titles, Safier notes there are some common mental barriers that hold people back from diving into independent ownership.
The big one is that it’s easier to work for someone else with a guaranteed salary each week than it is to buy a practice.
“However, it is not as rewarding,” she says.
“If you don’t have a lot of money and you purchase an established but small practice as your first practice, it may not be shiny and new but over time you can build it up, renovate or move down the road.”
Mr Nathan Tsalkos, who has changed the fortunes of Eyecare Plus Heidelberg (next page), is a case in point.
“Owning a practice will mean that you have to put in the hard yards to get it established – it won’t be a 9 to 5 job – but the effort you put in during the early years will pay off later when you can take a day off or hire a second optometrist,” Safier says.
She has some thought-provoking advice on proven methods to enter independent ownership.
Buying a business first and a house later is one pearl.
“If you build your business then you will be able to buy a house. Be prepared to move out of the metro areas where there is more opportunity. There are small practices for sale that you can build if you put the effort in.
“While in the growing phase, you could do some locum work for extra money. Eyecare Plus can assist you to market your practice to grow.”
Being able to offer tailored solutions for each patient is a major advantage – and is where the highest performing independents succeed.
“If you have a passion for dry eye, myopia control, orthokeratology, children’s vision, contact lenses, or any other specialty, then you can make this a focus of your practice to differentiate yourself. If you are passionate about what you do and you do it well, you will find that referrals will grow without even trying,” Safier adds.
For those with the commitment and savviness for independent optometry, Eyecare Plus can help locate a practice to purchase.
There are several options on the table other than straight-out ownership. Aspiring owners can work in a practice with the option of buying-in if the owner is looking for a succession plan.
“As well as assistance that national office staff can provide, our members are happy to give advice from experience. Due to our territory protection, our members always share ideas freely at meetings and conferences, which is a huge advantage of Eyecare Plus membership,” Safier says.


Mr Jonathan McCorriston recently became a co-owner of Eyecare Plus Optometrists Southport, Benowa, and Burleigh, partnering with long-time mentor Mr Michael Hare. Having worked alongside Hare for 20 years, McCorriston admires his leadership and expertise in practice ownership. Together, they’ve expanded their reach, opening a fourth location in Paradise Point, at the northern end of the Gold Coast.
Their now-four locations are all busy and the duo have surrounded themselves with a wonderful, highly skilled team. They say it’s gratifying to know the combined knowledge, experience and enthusiasm shown by partners and staff is infectious – and the key ingredient for continued growth.
“It’s sad to hear of new graduates, especially, who become disillusioned with their mode of optometry practice, where their patients often feel rushed and treated like a number. They sadly leave the profession or are unhappy in their role. This is one reason why there will always be a need for independent optometry practices,” Hare says.
Ms Flora Luk’s acquisition of Eyecare Plus Optometrists Cheltenham marked the beginning of an extraordinary life chapter. Shortly after acquiring the practice, she got married and welcomed her first child, a whirlwind of life-changing events within less than 12 months.
Balancing professional and personal milestones, Luk exemplifies resilience and determination. Owning a business requires strategic planning and leadership, while embracing marriage and motherhood brings emotional and logistical challenges. Together, the journey highlights how partnerships and support systems are crucial during transformative life stages.
This story may resonate with many, a reminder that significant life events often converge. Navigating such transitions requires adaptability, communication, and self-care. Luk’s experience can inspire others to “approach these challenges with confidence and grace”.



Ms Amanda Duffy and Mr James Paton joined Eyecare Plus in July 2023 when they purchased an established but somewhat neglected practice in Belmont, NSW, and have quickly become “the dynamic power couple of the Eyecare Plus family”. Duffy, an optometrist, and Paton, with his engineering and project management background, have a synergy that is propelling Eyecare Plus Belmont forward.
Fast forward to today, and they are on the verge of acquiring their second practice, further demonstrating their drive for exceptional eyecare and serving the local community.
Mr Pierre Elmurr is the owner of Primary Eye Care in Burwood & Mona Vale, NSW. In 2023 he purchased Eyecare Plus Burwood and incorporated it into his existing Burwood practice. He qualified as an orthoptist in 1992 and also completed a Masters in Exercise and Sports Science by research in 1995, both from the University of Sydney.
Elmurr became self-employed in 2012 with Primary Eye Care and continued to develop his clinical interests in paediatric vision and management of ocular motility disorders, rehabilitation, vision and sport and occupational vision. The Burwood clinic is an accredited University teaching facility for orthoptic students from UTS.
He encourages anyone with a passion for their profession to consider self-employment: “The rewards are greater than the challenges.”
Ms Li Chen and Mr Paul Cha approached Eyecare Plus in late 2010, looking to establish their own practice. Chen is an optometrist, while Cha has a business background, and is today the director of their two practices.
Initially, they ventured out of Sydney and established their first practice in 2011, Eyecare Plus Lake Munmorah on the Central Coast, building it from the ground up. It was a success and after a decade of learning, the next challenge awaited – a well-established practice in Avalon Beach, Sydney, in 2022.

Cha says taking the first step towards self-employment is the hardest decision.
“But as long as you assess your risks and set your goals, then the whole process becomes more predictable. The satisfaction you get from seeing your efforts come to fruition is the greatest reward, both financially and intrinsically.”
As a young optometrist, Mr Nathan Tsalkos took the bold step of purchasing Eyecare Plus Heidelberg, and was driven to expand and modernise the practice. It would be a challenge, as the practice trends showed declining patient numbers and the last renovation was done in 1985.
“What drove me to take the chance was the excitement of knowing that if I take the obvious potential of the practice and grow it, that I would be extremely satisfied and proud of what I would have achieved.”
Initially managing the practice solo, Tsalkos handled all optical dispensing while delivering eyecare. Now, with the addition of an optical dispenser to his team, he continues to focus on growth, innovation, and providing exceptional service.

Australian eyewear company Modstyle has been quietly gaining a foothold in UK and US, taking frames designed in a small Melbourne studio to independents around the world.
Mr Mark Wymond is ready to talk about some of the big boulders he’s been shifting with Modstyle.
As of late, the company – one of four eyewear wholesale businesses he operates out of Melbourne – has been demanding much of his attention. And for good reason.
“I can almost feel the switch in my head sometimes, from the right to left brain, as I go from the studio where we design Avanti, Eclipse and Kaleyedoscope frames before walking into a meeting with the bank manager.”
After acquiring an “in distress” Modstyle in 2016, Wymond and his co-owner and sister Ms Lisa Wymond have reinvigorated the company into how 1981 founder Mr Royce Jackson intended: quality, affordable, Australian-designed eyewear that sells through independent practices.
In recent times, Wymond and fellow designer Mr Peter Bienvenu, Modstyle procurement officer, have been flexing their creative muscles to come up with more edgy designs that not only follow market trends, but aim to create new ones. Frames like Avanti Pride, the Optical Distributors and Manufacturers Association (ODMA)’s 2024 Outstanding Frame under AU$300 at O-Show 2024, are a sign of this educated experimentation. But despite a natural flare for eyewear creativity and business, Wymond still has his work cut out for him with Modstyle.
The big reason is that Modstyle has gone global.
Given it has been in the US for the past three years and the UK for two, it’s perhaps not a huge secret, but one that Wymond is now happy to discuss after reaching a critical mass in both markets and exhibiting at

major events like Silmo Paris in 2024.
With 300 independent accounts expected in the UK by the end of 2025, and 250 in the US, the strategy is galvanising the Modstyle business while taking Melbourne-designed eyewear to the world.
After fending off naysayers about these “tough markets” with price-conscious consumers, Wymond is happy with the way Modstyle is tapping into the 4,000-strong, densely-populated independent UK market, and 16,000-20,000 independent shopfronts in the US.
“There’s a number of accounts in the UK that are already very loyal who love what we do and are selling the product really well.
“The independent market in Australia is somewhere around 1,500 practices, so to find an extra 200 customers, which we currently have in the UK, is almost impossible. We’re opening a couple of new accounts each week.
“Sometimes you’ve got to trust your gut and go for it and be careful who you listen to. I’m sure there’s a lot of businesspeople that if they knew how hard it was, they wouldn’t do it again – and this can feel in that category sometimes. It is tough, but it was always going to be a marathon; we’re a few kilometers in now and starting to see progress.”
Naturally, it puts more strain on Wymond’s shoulders. But building a team he can trust has been key to the global expansion. In the UK his country manager is Mr Will Cooksey, a former national sales manager for Eyes Right Optical in Australia, who is running the business out of Camberley, an hour southwest of London.
In the US, Mr John Justice, who worked for a firm called Kenmark Eyewear for 30 years, is the vice president of sales for North America market for Modstyle International. They’ve started out and are finding great success in Kentucky, Ohio, Indiana and Tennessee.
“The difference with the American market is that our sales rep can go in any five directions from a city, and every hour there’s a town with a population closing in on the size of Adelaide,” Wymond says.
“You don’t need to have too many states to be quite successful there, so we’re well on our way.”
Aside from the prosperity of the Modstyle business, for Wymond it’s pleasing to see his concepts on the faces of patients in new markets. Around 70% of the overseas sales are Avanti, and 30% Eclipse.
“Over the years we’ve seen colour become a big part of Avanti collections, and in the Australian market we love colour in general, but interestingly worldwide it isn’t the same story. Certainly, in the States, it seems like there’s a lot more interest in black and tortious shell, and to go bright pink or orange is quite foreign to them.”
Many of these designs wouldn’t be possible if it wasn’t for an important project completed at the Modstyle headquarters in Scoresby, suburban Melbourne, a couple of years ago. A new purpose-built space became the creative engine room for Wymond and Bienvenu to formulate their Avanti, Eclipse and Kaleyedoscope designs.
It’s something that comes naturally to Wymond and he’s careful to carve out time, uninterrupted. No electronics are welcome, and business decisions can wait.
His other companies – Eyes Right Optical, Sunglass Collective and Morel Australasia – are fulfilling ventures in their own right, but they all focus on supplying eyewear from other manufacturers. That’s where Modstyle differs.
“Eyewear design is a great creative outlet for me and I get so much satisfaction from creating something from the initial drawings and final production, all the way to it being sold in the practice.”
Rewarding moments can be found in his daily life, like a recent trip to Bunnings where an attendant was wearing an Avanti frame he designed.
“Peter and I are commercial designers, we typically design for the market and trends, eyewear that’s an easy sell, but we have had some special projects along the way where we’ve been intentional about creating a whole new concept from start to finish, turning Modstyle into a creation company as well.”
Avanti Pride is a case in point. The heart-shaped frame has a striking rainbow-coloured acetate to embody inclusivity and diversity, offering a unique, bold look that resonates with contemporary trends. It also supports a noble cause, with $5 from every sale donated to the Elton John AIDS Foundation.

Avanti – "Modstyle’s flagship brand with a huge focus on quality acetates and hinges in exciting wearable colour ways. This award-winning collection consists of more than 300 skus."
Eclipse – "Materials like titanium, multiflex, stainless steel and TR90 are features of this collection that embodies more of a conservative, corporate look. We’re making robust, well-made frames through some exceptional factories in South Korea that puts the quality aspect into a frame but is still at the entry level price point."
Kaleyedoscope – "This is a small kids collection that’s very colourful. We have about 15 active models, so about 45 skus at one time, and that’s the sort of size I like to keep it at. A quick-moving collection like that is probably where our market’s at right now."
Nifties – "It’s a collection for those smaller eye shapes, but not with love hearts and other bits and pieces. They’re for adults with smaller faces, but also kids that want to look like what mum and dad are wearing too."
Inface – "A Danish-designed collection that embodies the Scandinavian spirit of design, balance."
My Style – "For the budget conscious – high quality, wearable styles starting at $9.90."
Modstyle was proud to have the piece recognised through ODMA’s awards at O-Show as voted by independent optometrists, dispensers, etc. Now, Wymond is adapting the design with a more modern frame shape to be entered for the awards at 100% Optical in London, where Modstyle is exhibiting in March 2025.
“It’s a big challenge to create collections that are going to resonate with the market in different ways. The only limitation is our creativity, but even as we push boundaries, we still have a strong focus on saleability.
“We don’t want to create frames just because they look good on the shelf.”
Keeping the Modstyle brand collections fresh and relevant is a big ask, but it’s a taller order ensuring the P&L is on track across several markets.
All while juggling a young family with three children, and 42 staff. The increased workload was one of the things his parents, Mrs Gaye and Mr David Wymond, were most concerned about. They understand the pressure of running a business after founding Eyes Right Optical.
He needs to be deliberate about work-life balance. There’s always work to do. “I could work 24/7 if I allowed myself to.
“I’m still young. I want to work hard but it’s not all about just working harder and more hours. The one thing we’ve been able to develop is an exceptional team that’s helping Modstyle go to a new level, especially overseas.”
For Jackson, who founded Modstyle 44 years ago, he couldn’t imagine a better custodian than the Wymonds.
“The growth into the US and UK markets is very exciting, it is so good to see the company Modstyle in safe hands. It is great to see Peter Bienvenu still invovled too; he has been with the company for more than 30 years.”

There are a number of reasons why Australians are facing issues accessing quality eyecare in many parts of the country, which is why Specsavers is taking a number of approaches to ensure it can deliver for those needing help.
Accessing quality, regular eyecare services remains a challenge for many Australians.
Geographical barriers mean regional towns and remote areas either lack permanent eyecare facilities or face a shortage of optometry professionals to meet community needs, leading to disparities in eye health outcomes for residents. Fortunately, innovative telehealth solutions, mobile optometry career opportunities, and a focus on regional placements for Specsavers graduates are some of the things helping to bridge this gap and make primary optometry services more accessible to more people, no matter where they live.
A 2023 Deloitte Access Economics report, commissioned by Specsavers, highlighted the critical role optometrists play in delivering frontline eyecare to Australians and the need for investment in a pipeline of eye health services to prevent avoidable vision loss.
The report predicted a shortfall of more than 1,000 optometrists by 2042, with the country’s regional areas expected to be the hardest hit.
Without adequate optometry professionals in these areas, there is concern people will not be able to access the timely, routine eyecare that could detect and treat ocular conditions early and save their sight.
One way Specsavers is trying to address the inequity in accessible care in Australia is by offering graduate optometrists incentives to relocate to regional practices.
Specsavers graduate recruitment manager Ms Sarah Yearsley says many recent graduates are choosing to work outside metro areas. This is in part due to additional perks, but many are inspired by the prospect of being able to make a significant health impact within smaller communities.
“We’ve had 260 of our graduates over the past three years successfully placed in regional practices,” she says.
“These types of placements are an attractive option for early-career optometrists as they offer diverse clinical experiences and the opportunity to develop a broad skill set.
“Additionally, the cost of living is generally lower in regional areas, and the lifestyle is often more relaxed and community-oriented compared to metropolitan areas.”
Specsavers recruitment services manager Ms Madeleine Curran explains that it’s not just graduates who are eligible for relocation; as Australia’s largest optometry provider, Specsavers offers attractive packages to experienced optometry professionals willing to move to communities experiencing a skills shortage.
“We highlight the benefits of each unique regional community to ensure the optometrist knows what life could be like,” she says.
“We also support them with regular trips home or extra leave time to make sure
they have a chance to reconnect often with family and friends.”
Specsavers says it is committed to ensuring its optometrists enjoy living and working within their local communities. While this is often the case, Curran acknowledges that long-term settlement can sometimes be a challenge.
“We do everything we can to support optometrists in relocating and integrating into their new communities. Ultimately, though, people thrive where they feel most at home and, as a result, we still have some permanent opportunities available in Australia’s more remote regions.”
One Specsavers optometrist who is thriving after moving to a regional practice is Mr Shuwen Yu.
He chose to relocate to a regional practice in Grafton, northern New South Wales, because of the unique sense of community, professional fulfilment and the chance to make a real difference in people’s lives.
“My goal before graduating optometry school was to start in a regional area.
“Throwing myself into the deep end allows me to quickly put what I learnt during my training into practice, which makes me a better clinician to care for my patients.”
Yu explains it’s common for people in regional areas to skip regular allied health appointments because of a lack of accessibility or perceived out-of-pocket cost. This can result in many patients in their 30s coming in with eye problems who have never had an eye test before.
“These patients think they are just bad at school because it is difficult to focus on the words on the paper or can’t see the whiteboard without squinting,” says Yu.
“Adult patients may develop binocular amblyopia and have never experienced clear vision.
“The most memorable experiences for me are the moments like when a 45-year-old -10.00 D myopic patient picked up his glasses for the first time and could suddenly see the world, or when a 12-year-old child who only read

“Throwing myself into the deep end allows me to quickly put what I learnt during my training into practice, which makes me a better clinician to care for my patients.”

word-by-word could read whole sentences by wearing the trial frames. “These are the real impacts that I can see from my work in regional areas.”
Yu believes people will be able to see better and ultimately live a better life when there are ample eye health services available in regional communities.
Of course, for optometrists who do decide to relocate, it can be a challenge to find practitioner cover so they can take annual leave.
Yu manages this within his own practice by co-ordinating with colleagues wherever possible.
Specsavers also employs trained mobile optometrists who travel to provide optometry cover and continuity of care for patients in regional areas.
Specsavers’ team of mobile optometrists is a movable workforce that travels to underserved communities lacking eye health services. Thanks to this support system, regional optometrists can take much-needed leave, helping to prevent burnout and maintaining a healthy work-life balance.
Mr An Cao, a Specsavers mobile optometrist, finds the diversity in his role fulfilling.
He services areas in all Australian states and territories, including Port Pirie, Whyalla, and Kadina in South Australia; Cairns, Sunshine Coast, Townsville, and Toowoomba in Queensland; Darwin and the Northern Territory; Wagga Wagga and Orange in New South Wales; and Northam in Western Australia.
Adaptability in this type of work is essential. As Cao explains, each location has a different practice environment and patient demographic. Without easy access to healthcare, routine appointments may not be a top priority for regionally based patients, and they often have a higher frequency of pathology.
“I’ve had patients who have gone years without an eye exam, and seeing the impact of providing them with clear vision with glasses or identifying serious eye conditions gives me a deep sense of satisfaction,” he says. “Knowing that I am helping prevent vision loss or improving quality of life is very rewarding.”
Cao believes there will always be a need for mobile optometry, which he predicts will continue to grow as more emphasis is placed on reaching more remote communities, driven by technological innovation, expanded services, and a focus on better integration with local healthcare systems.
In addition to mobile services and regional graduate placements, the evolution of telehealth represents an innovative answer to overcoming geographic barriers to eyecare.
Remote Eye Care, currently piloted by Specsavers, uses technology to bring optometry expertise to underserviced locations.
Optometrists provide comprehensive eye tests, including diagnostic and clinical tests via video conferencing.
The model reverses telehealth definitions, with the patient attending their local optometry practice and the practitioner delivering the clinical services from another location, eliminating the need for patients to travel long distances.
Ms Jeena Tan, Specsavers ANZ head of clinical systems, says Remote Eye Care is a viable, comprehensive sight test service that can be part of the solution to addressing the current and future shortage of healthcare professionals in remote and regional areas.
“While in-person consultations will always be a part of optometric care, Remote Eye Care has an opportunity to be transformative for people living in regional and rural areas, allowing them to access high-quality, routine eyecare appointments more often,” says Tan.
It is clear that a variety of solutions are required to meet the future eyecare needs of Australians.
More optometrists considering relocating to regional towns, a flexible workforce of mobile optometrists, and optometry technology will all be essential elements in ensuring Australians have access to the equitable eyecare they deserve.




PBS Information: Xalatan (latanoprost 0.005% eye drops, 2.5 mL) is listed on the PBS as antiglaucoma preparations and miotics.














Before prescribing please review Product Information available via www.aspenpharma.com.au/products or call 1300 659 646.
Minimum Product Information: XALATAN® (Latanoprost 50 µg/mL) Eye Drops. Indication: Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Contraindications: Hypersensitivity to ingredients. Precautions: Change in eye colour due to increased iris pigmentation; heterochromia; eyelid skin darkening; reversible eyelash and vellus hair changes; macular oedema often associated with aphakia / pseudoaphakia; other types of glaucoma; contact lenses; severe or brittle asthma; herpetic keratitis; driving or using machines – transient blurry vision; elderly: no data; children: do not use, no data; lactation- metabolites present in breast milk, risk / benefit. Pregnancy: Category (B3) Interactions: other prostaglandins, thiomersal. See PI for details. Adverse Effects: Eye Disorders: blurred vision, burning, conjunctivitis, excessive tearing, eye pain, foreign body sensation, hyperaemia, iris hyperpigmentation, itching, punctate epithelial erosions, grittiness, stinging, eyelash and vellus hair changes, punctate keratitis, blepharitis, eyelid oedema, localised skin reaction on eyelids; Systemic: bronchitis, upper respiratory tract infection, eczema, rash, urinary tract disorder, abnormal liver function, myalgia, arthralgia, dizziness, headache, rash, chest pain, asthma, dyspnoea . See PI for details and other AEs. Dosage and Administration: One eye drop in the affected eye(s) once daily. Other eye drops should be administered at least 5 minutes apart.
References: 1. Clinical Practice Guide for the Diagnosis and Management of Open Angle Glaucoma. Optometry Australia 2020 2. Australian Commission on Safety and Quality in Healthcare Active Ingredient Prescribing Guide - list of medicines for brand consideration December 2022


If clinically necessary for the treatment of your patient, prescribe by brand and disallow brand substitution2

Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma.com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2023 Aspen group of companies or its licensor. All rights reserved. Prepared: July 2023 AU-LAT-072023-07653



Research has long established the link between mental health and glaucoma, but a new study suggests each can make the other worse in a vicious cycle of deterioration. Australian disease experts discuss what professionals can do to support their patients’ vision and well-being.

The connection between mental health and glaucoma is now well proven and accepted by the scientific and ophthalmic communities. It’s backed up as well in the daily calls patients make to support organisation Glaucoma Australia, which says that about half of those callers report being occasionally or frequently anxious about the eye disease and its impact on their vision.
But recent US research has looked a little harder at this toxic relationship and now suggests that each might be driving the other, with a person’s deteriorating mental well-being also potentially impacting on their eyesight, and vice versa.
“Factors like anxiety, depression, and allostatic load – the cumulative burden of stress on one’s mind and body – are intertwined with the effects of glaucoma,” says Dr Sarah Van Tassel, director of the Glaucoma Service and Glaucoma Fellowship at Weill Cornell Medicine Ophthalmology in New York City.
She and her colleagues reviewed a number of studies, including several linking visual field (VF) defects with both the incidence of falls and the fear of falling. Among these, a three-year study of 342 patients with primary open-angle glaucoma found that inferior peripheral VF defects were significantly associated with fear of falling.
They concluded that anxiety could affect glaucoma progression through “stimulation of the autonomic nervous system, however the mechanism is not known”.
“It’s a complex web of interactions and it’s not as well understood in eye disease [as in some systemic diseases],” says Dr Van Tassel.
The study might not have been able to reach a conclusion about the mechanism driving this vicious cycle, but the researchers did conclude that “taking steps to help patients manage their mental health may help improve their quality of life”.
That is likely to be a challenge in many busy ophthalmic practices and businesses where chair time is at a premium and the focus is more on the eye rather than what goes on in the dark recesses behind it.
But as prominent Australian glaucoma sub-specialists Dr Brian Ang and Associate Professor Simon Skalicky point out, a more holistic view of what ails the patient is vital if glaucoma is to be treated and managed effectively.
And there are ways to do that which can preserve everyone’s well-being, including seeking support from organisations with a strong focus on the debilitating eye disease.
The results of the US study are no surprise to Dr Ang.
“I couldn’t agree with this more,” says the Melbourne glaucoma specialist and Nutravision co-founder. “There has been recent research showing that
people who are stressed, who are anxious all the time, their eye pressure actually increases.
“And for people with glaucoma, this elevation in eye pressure, up to an additional 4-5 mmHg, could make a big difference in terms of their overall glaucoma outcomes.”
That deteriorating mental health can also impact treatment.
“If you are feeling down and depressed about your vision, your motivation to continue with lifelong treatments, to be compliant with the instructions given by your eye specialist, would undoubtedly be affected,” he says.
“Sometimes you might feel, ‘what’s the point of me using the eye drops or having surgery if it’s still going to get worse, and I’m not going to bother’.”
Anxiety, stress and depression, and their impact on glaucoma patients, were part of Dr Ang’s presentation at the 2024 Specsavers Clinical Conference on the Gold Coast.
He told the hundreds of optometrists at the event and online that stress reduction was one of “five pillars” key to managing the debilitating eye condition, with the others being physical activity, restorative sleep, diet and nutrition, and what he termed neuroprotection.
“Mental stress can be overlooked for its impact on glaucoma,” he said at the time.
Between 45 and 60 minutes of daily meditation was shown to reduce intraocular pressure (IOP) by up to 25%. Also, deep breathing exercises: “Three times daily, 6 breaths a minute, 5 seconds in and 5 seconds out.”
Glaucoma was a devastating eye condition, but “optometrists can be the


coach along their patients’ eye health journey”, he told the group.
Dr Ang tells Insight that just the idea of visiting an ophthalmologist can make many of his patients stressed and increase IOP.
“I try to get them to relax,” he says. “They can do deep breathing techniques to slow down their heart rate, which often helps to reduce the eye pressure to more normal levels.”
He talks about meditation with them, too.
As part of what he terms “proactive glaucoma care, a focus beyond just our conventional treatments”, he will talk to his patients about their stress management, sleep patterns, nutrition, and neuroprotection.
“They’re interconnected, and you can’t really talk about one thing without influencing the others.”
Nutrition is an important part of that conversation.
“If you eat well then you have the essential nutrients needed to function optimally, including for your eyes. But certain vitamins play a particularly important role in helping the brain and eyes adapt to stress.
“Take vitamin D and folate, for example. Both are critical for regulating neurotransmitters like serotonin and dopamine, which influence mood, cognitive function and stress response. Deficiencies in either of these can impact mental well-being and affect eye health at a cellular level.
“But beyond vitamins, certain botanicals also help the body build resilience to stress. For instance, saffron has been shown to improve mood, reduce cortisol levels, and even help lower eye pressure. Ginkgo biloba promotes circulation to both the brain and eyes, further supporting cognitive function, neuroprotection and visual health.
“So the role of nutrition in supporting the eye-brain connection – whether through diet or supplementation – should not be underplayed.”
Social support for the patient is also an important topic.
“If you’ve got family members or friends who are incredibly supportive, then you’re also more motivated to comply with your treatments, to go and do your daily exercises, do the meditation, improve your diet, etc.
“Mental health affects not just eye health but the rest of the body, and in ophthalmology we are very much into this sort of concept where, ‘oh, we don’t deal with the rest of the body, and much less mental health’,” he says.
“But the reality is that mental health will affect your eyes and if we truly want the best outcome for our patients, then this is something that we have to be cognisant of, and we have to appreciate that mental health plays an important role.”
Dr Ang acknowledges that taking a more holistic approach and discussing a patient’s mental health and general well-being also takes more time, which is not always plentiful at busy practices.
“When you’ve only got 15-20 minutes, the last thing you want is a lengthy chat about mental health, so just start with one or two questions – how’s your mental health been? Have you been stressed at work?
“At the next consultation you can go with how are you doing? How do you feel and do you need help? That way they can open up.”
He believes his patients respond well to that extra level of care and interest in their well-being, which builds all-important trust.
But like their patients, eyecare professionals don’t have to do this alone.
Dr Ang says there are numerous excellent groups to support the mental health of both practice and patient.
“If you want support with regards to glaucoma, then Glaucoma Australia is an excellent resource,” he says.
“In terms of specific mental health organisations, there are a few – Beyond Blue is an excellent organisation, and sometimes even talking to the counsellor, the GP or the family doctor will be quite a good option.”
Looking elsewhere for support is good advice, says A/Prof Skalicky. It is important that optometrists, ophthalmologists and others recognise their limitations.
“I’m an ophthalmologist, not a psychiatrist,” he says. “And in the odd case where I really feel like mental health here is a big issue, and it’s not under control, I would call the GP.
"It’s not necessarily my place to refer directly to a psychiatrist.”
Like Dr Ang, the conclusions of the recent US research are not surprising to the glaucoma and cataract sub-specialist, who is also an Associate Professor at Melbourne University.
“I published work with Professor Ivan Goldberg almost 20 years ago, and we looked at the link between glaucoma and depression, and we found very similar results – that depression seems to magnify the quality-of-life impact of glaucoma, and that glaucoma was linked with worse depression.
“But I note that having any chronic illness that is potentially degenerative, like glaucoma, is linked with depression, so much of the relationship between glaucoma and depression is not necessarily specific to glaucoma.”
That impact on mental health can start even before the deterioration of vision.
“Patients might see fine but they’re worried that they’re going to lose their vision over time, or they’re worried that they might pass this on to their children or they’re worried about the medical interventions and many visits to the doctor that might impact on their life and job,” says A/Prof Skalicky.
“There is a certain degree of psychological overlay in there, and I think that’s important for us as clinicians to recognise.
“It often startles me when I see a patient for whom I think there’s no problem here – they’ve got healthy optic nerves, the pressure is just a little bit high but not a concern for me as a clinician,” he says.
“But from where the patient is sitting, they’re incredibly anxious, incredibly upset; they’ve been waiting for this appointment and have really focused their energy on it.
“If I am not aware of that dimension and I just send them on their way, I’ve missed an opportunity to do some good, to open that dialogue.”
He believes nothing is more important for patients than keeping up with visits to their eyecare professionals and sticking to the treatment regime.
But there is also plenty of evidence to show that lifestyle plays an important role and lifestyle habits like meditation can reduce stress and IOP.
“My patients commonly ask me, what can they do in their lifestyle to help with glaucoma? As well as having this laser treatment or taking these drops and regularly seeing me, what can they do in their life to help?”
Again, that could be about promoting certain foods rich in various

vitamins, such as vitamin B3, which is known to play a role in halting the progression of glaucoma, but also fresh fruit and green leafy vegetables as part of a healthy, balanced diet.
But busy professionals don’t have to have all the answers.
They can share the load with others, says A/Prof Skalicky.
“You should remember you are just one piece of the puzzle,” he says.
“There are plenty of other people involved here – the optometrist, the pharmacist, the GP, the support person, even the administrative staff at our practices, and the family to talk to.”
He believes handing out flyers linked to his website, or from organisations like Glaucoma Australia, can help them with further support.
Patients with good information about their ailment and their options feel empowered, and that supports good mental health.
“Patients want to feel empowered to look after their own illnesses, and that ultimately comes back to these concepts of a quality therapeutic relationship and putting your patients first.”
But professionals also need to be mindful of their own mental health, especially when anxious, vulnerable patients are sitting in front of them contemplating deteriorating vision.
Self-awareness is important.
“It’s about, as a clinician, just being aware of your own mindset,” he says. “If something’s annoying you and you’re not addressing it, that will come out, and in a negative way in your patient interaction.”
Clinicians should practise what they preach: “Look after yourself mentally, physically exercising, getting good sleep, eating well, having support around you, taking breaks, taking holidays, and also talking, feeling free to talk to colleagues about when cases don’t go so well.”
A problem shared can be a problem halved.
“We don’t need to solve everything on our own.”

“My patients commonly ask me, what can they do in their lifestyle to help with glaucoma? As well as having this laser treatment or taking these drops and regularly seeing me, what can they do in their life to help?”
Simon Skalicky Eye Surgery Associates Image: Simon Skalicky.
That’s where Glaucoma Australia comes in. It provides free support to not only the patients but also their family and carers.
“Many patients have questions that are not able to be addressed ‘on the spot’ due to being overwhelmed or not completely understanding the information that has been relayed,” it says.
“Initial contact can be made via our national free-call number, web chat, or Oculo referral.
“Also, our website provides detailed information on glaucoma through online resources, such as articles, videos, live webinars and downloadable guides covering topics from diagnosis and treatment options to lifestyle tips.”
People can access one-on-one tailored support through the organisation’s SiGHTWiSE patient support program, which provides access to Orthoptist Patient Educators.
“Our team is also aware of external third-party resources, such as agencies for low vision aids and financial assistance.”



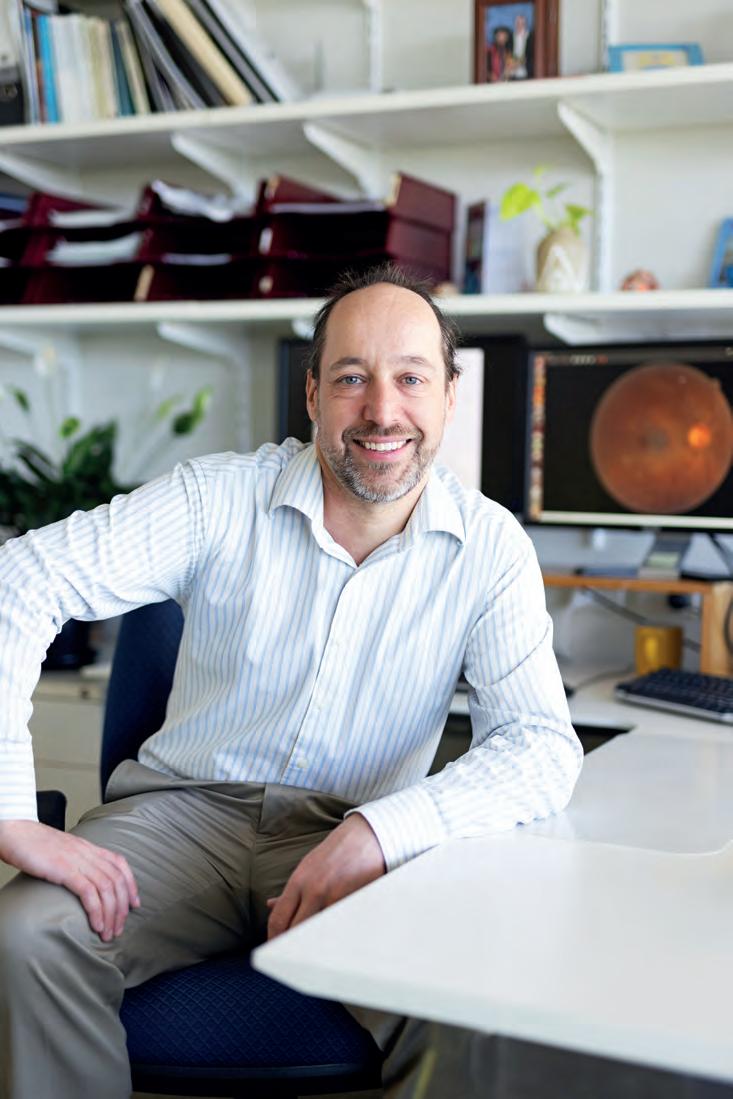








“That was very encouraging.”



relative infancy.




70-90th percentile higher risk and 90-100th percentile the highest risk group.


















For Myopia management – predict and monitor the progression of myopia.
Simple operation with 3D Auto tracking and Auto shot.
Myopia risk evaluation can be monitored and assessed against typical AL growth rates.
The MV-1 software presents trend reports influenced by treatment and patient behaviour.




Virtual Reality Visual Field device -




incorporates complete Visual Field analysis.
Detailed progression analysis and the most versatile & efficient vision screening technology.


and reports as the “gold standard”.

Latest technology provides the same reliability

Supplied complete with a Tablet PC -
BlueTooth interface with the VF2000 NEO.

Compact/Space-saving/Portable - can be used anywhere, no need for a darkened room.







Leader in hand-held Fundus Imaging
Expanded 50 degree field of view
Sleek modern design
Versatile and compact

Clear Fundus & Anterior Eye imaging
Autofocus and AutoExposure

Integrated image quality analysis





High resolution quality display screen
WLAN or USB connectivity




9 Internal fixation points for Peripheral imaging








Active eye tracking – enhances reliability.
Full and Fast Thresholds VF Testing plus Neuro,
Kinetic, Ptosis and Esterman tests
FDT Testing
Stereopsis

Visual Acuity and Contrast Sensitivity
Colour Testing
(Ishihara, D15 and Advanced Colour Tests)
Eye Mobility and Strabismus








Experience the power to do more for your patients
* Glaukos Data on File
(POAG)


proper maintenance of IOP. Three out of 61 participants (4.9%) in the pivotal clinical trial were phakic. Therefore, there is insufficient evidence to determine whether the clinical performance of the device may be different in those who are phakic versus in those who are pseudophakic. ADVERSE EVENTS. The most common postoperative adverse events reported in the iStent infinite pivotal trial included IOP increase ≥ 10 mmHg vs. baseline IOP (8.2%), loss of BSCVA ≥ 2 lines (11.5%), ocular surface disease (11.5%), perioperative inflammation (6.6%) and visual field loss ≥ 2.5 dB (6.6%). CAUTION. Please see DFU for a complete list of contraindications, warnings, precautions, and adverse events.

What began as a local project on A/Prof SIMON SKALICKY’S computer is now being rolled out globally. Could this change the game for glaucoma management?
Associate Professor Simon Skalicky has had a front row seat to the frustrations patients with glaucoma face.
But instead of lamenting the standard of care, the Melbourne-based ophthalmologist, sub-specialising in glaucoma and cataract, sought to change it, culminating in an Australian MedTech success story that’s making ripples in almost two dozen countries.
In 2019, he founded Eyeonic, a quantified perimetry test using any computer or tablet, through a web-based application.
By improving the patient experience, ease of sharing data and democratising access to this vital technology, he believes online visual field testing is the future of glaucoma diagnosis and management.
Eyeonic’s test has been approved by the Australian Therapeutic Goods Administration (TGA) as a perimeter for in-clinic and at-home use, with more than 13,000 tests already performed in more than 20 countries.
A/Prof Skalicky says it has been scientifically validated in Australia and overseas, with similar diagnostic performance and progression analysis to standard visual field machines. It has 24-2, 10-2, 30-2 protocols, as well as a

binocular driving licence screening test and a monocular pilot licence test.
Early in his career, he recognised the challenges of traditional visual field testing on machines – patients found these stressful and uncomfortable, a potential impediment to regular glaucoma monitoring.
He wondered if visual field testing could be performed in an easier, more intuitive way.
“My journey led me to the world of programming, deployment and cybersecurity, all ably supported by experts from Microsoft. As the project grew and supportive colleagues became involved, we quickly realised the many other benefits; namely streamlining perimetry in contemporary clinics, expanding glaucoma services to remote and regional communities, and glaucoma home monitoring with telehealth,” says A/Prof Skalicky, whose academic work is conducted at the University of Melbourne.
“Online perimetry helps our eyecare services cope with increasing demand and a tightening health budget, to achieve worthwhile aims of democratising healthcare access and creating sustainable care models, while at the same time reducing costs for clinicians and patients alike.”
Eyeonic has raised capital and today involves a team of business and tech experts, as well as collaborations with major institutes in Australia and globally.
“The journey has been rewarding, fun, with many challenges – clinical research and supervision, programming and deployment, team building and project management, developing quality systems, achieving regulatory approval, commercial development, marketing, financing and sales,” A/Prof Skalicky says.
“Entrepreneurship is not always easy but is required to drive meaningful reform.”
Eyeonic’s online visual field test works by integrating the fundamentals of traditional perimetry into a web-based browser experience. It uses large flickering contrast targets designed for consistency across different screen displays to assess sensitivity thresholds at 52 loci across the visual field.
To achieve standardisation, the software resizes and repositions the targets based on the size of the screen and informs the user the correct viewing distance. The correct viewing distance is ensured by locating the blind spot and maintained by utilising AI to measure the head position relative to the screen. Verbal instructions guide the user through a user-friendly and intuitive test that lasts two to five minutes, with multilingual options.
With eight publications in the international literature and numerous scientific presentations globally, A/Prof Skalicky says the software has been well validated with similar performance to traditional machineperimetry.
What began as a local project from his computer and in his rooms, is now deployed and used internationally.
He says the uptake is “humbling” – in India, for example, the software is being piloted by three major health institutes: All India Institute of Medical Sciences (AIIMS), LVPrasad Eye Institute and Shroff Eye Hospital.
The project has also been recognised by AusTrade and the Australian High Commission (Delhi) as an important Indian/Australian healthcare partnership. Eyeonic has been awarded the AIIMS medal for its collaborative work to help manage patient backlogs and reduce need for remote communities to travel many hours for testing.

“I believe that online visual field testing, over time, will become the clinical standard for perimetry globally,” A/Prof Skalicky says. “The improved user experience, reduced cost and maintenance, easy networking with electronic medical record systems, provision for out-of-clinic testing and data sharing between centres will bring advantages in line with the needs of modern eyecare delivery.”
NOTE: In Australia and New Zealand the Eyeonic Online Visual Field Test is distributed by OphthalmoPro. For further information, visit: www.eyeonic.com.au
Develop your skills through continuous learning. Unlock leadership potential for career advancement and business ownership. Can you see yourself in Specsavers? spectrum-anz.com/ careers-at-specsavers



The growing number of aging glaucoma patients presents both challenges and opportunities for eyecare professionals. DR KENNETH OOI explores how advancements in minimally invasive glaucoma surgeries and a deeper understanding of ocular surface disease are shaping personalised treatment strategies.

Over the past decade, myopia treatment has gradually evolved towards a more tailored approach. At the same time, there has been a growing consensus among eyecare professionals suggesting that it is now time for glaucoma care to follow a similar path. The reason for this is the increasing availability of minimally invasive glaucoma surgery (MIGS) devices, making interventional glaucoma management a more realistic option.
This progress enables eyecare providers to individualise diagnosis and monitoring based on each patient’s unique risk factors, while also creating treatment plans that align with the patient’s unique lifestyle and the severity of their condition.
One of the key considerations driving this evolution in glaucoma care is ocular surface disease (OSD) which as we know is a leading cause for referrals. Ocular surface disease prevalence in glaucoma can be up to 59%,1 and symptom manifestation has been documented in up to 74% of glaucoma sufferers.2 Glaucoma drops can contribute to OSD, but more importantly, it is the preservatives used with them that are causative.3
The presence of OSD not only reduces adherence to glaucoma drops and quality of life, but also increases glaucoma surgical failure, such as reduced trabeculectomy bleb survival from excessive inflammation.4-6
Another key consideration in this paradigm shift is cataracts, which often occur alongside glaucoma. Although the range of intraocular lens (IOL) options
At the completion of this article, the reader should…
• Understand the evolving landscape of glaucoma care and the shift towards interventional management.
• Learn to identify when shared care is necessary, particularly in patients with more advanced glaucoma and co-morbidities.
• Develop strategies to educate glaucoma patients on treatment options, emphasising early intervention and tailored approaches for long-term management.
continues to grow as we work towards achieving aberration-free multifocality, the currently available multifocal IOLs are linked to increased dysphotopsia and reduced contrast sensitivity compared to monofocal IOLs. Since OSD is already associated with decreased contrast sensitivity, post-operative patients with OSD may experience an additional, compounded loss of contrast sensitivity. 7
The most identifiable causes of multifocal IOL dissatisfaction are residual refractive error and OSD, with both as the most frequent concurrent complaints as highlighted in our review on cataract surgery and dry eye.7
Selective laser trabeculoplasty (SLT) is an established intraocular pressure (IOP)-lowering procedure performed with a doubled pulsed-frequency meodymium (Nd):YAG laser accessible to cataract/refractive surgeons. The laser selectively targets pigmented tissue of the trabecular meshwork (TM) to augment aqueous flow. iStent devices bypass the TM as a major aqueous outflow barrier, create a new drainage path, and allow fluid to flow more easily, reducing eye pressure. During surgery, three heparin-coated, non-ferromagnetic titanium microstents can now be implanted in the form of iStent infinite (Figure 1). As with any form of surgery, MIGS devices and SLT have associated risks, but these have been found to be mostly transient and non-serious as highlighted in a systematic review by Cantor et al. (The most commonly reported complications were hyphema, peripheral anterior synechiae
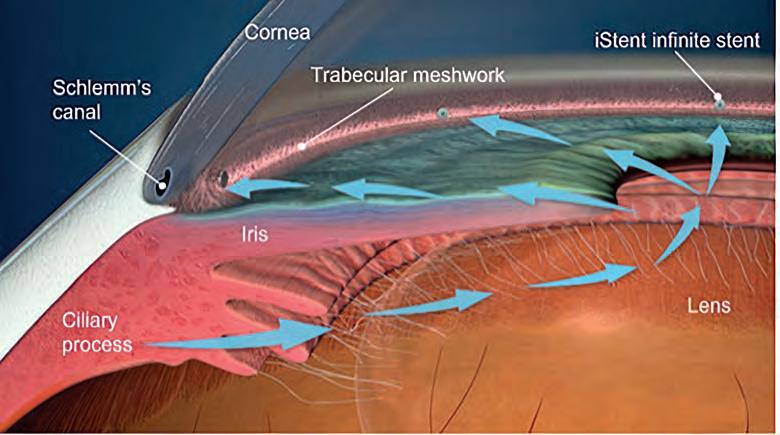
FIGURES 2A AND 2B. A: Estimated mean IOP and number of glaucoma medications in eyes implanted with iStent inject W combined with cataract surgery over six months; B: Estimated mean IOP and number of glaucoma medications in eyes implanted with iStent inject W as a standalone procedure over six months.
formation, mild inflammation and IOP elevation).8
More iStent-specific events include malposition and stent obstruction. Complications after SLT were reviewed as being generally rare with only use of rescue IOP-lowering medications and diurnal IOP fluctuations being noted.8
In the literature thus far, no significant difference in IOP-lowering at three years has been found between implantation of two iStents in the form of iStent inject W and SLT.9 The IOP-lowering effect of SLT has been shown to diminish over five years.10 There is a trend for iStent inject W lowering of IOP and glaucoma medications at least until the seven-year mark, whether combined with cataract surgery or as a standalone procedure.11
This trend for lowering of glaucoma medications has been replicated in a six-month local retrospective study of consecutive mild-to-moderate open-angle glaucoma private practice patients implanted with iStent inject W combined with cataract surgery and as a standalone procedure (Figures 2A-B). The percentages of eyes that were medication-free, ≥ one glaucoma medication reduction, and ≥ one mmHg IOP reduction in combined cataract surgery and iStent inject W patients (n=12) and standalone iStent inject W patients (n=11) were 50% and 36%, 75% and 73%, and 83% and 64%, respectively. Interestingly, the two exfoliative glaucoma eyes in the combination group also became medication-free despite the high pre-operative burden of four glaucoma drops. Only two cases of self-resolving small hyphema were observed in the standalone cohort.12
In terms of health economics, despite the higher initial cost of iStent implantation, it has been found that the annual costs after implantation were lower than those of both the medication-only group and the SLT group.13 A systematic review published in 2023 also showed greater reductions in medication use with iStents compared to SLT. The review concluded that, although further evidence is needed, existing economic studies suggest that MIGS devices, when combined with cataract surgery, are a cost-effective option for lowering IOP compared to cataract surgery alone.8 Additionally, studies have demonstrated significant
improvements in OSD and quality of life following iStent implantation combined with cataract surgery, including reduced OSDI scores and medication use.14, 15 One prospective single-arm study by Schweitzer et al of patients with mild-to-moderate open-angle glaucoma on one to four glaucoma medications studied the effect of pressure-lowering on OSD of 47 eyes which underwent cataract surgery and iStent or iStent inject implantation. They showed that 73% of patients had moderate or severe OSDI scores pre-operatively but only 29% had such scores at three months post-operatively.
Furthermore, OSDI scores were recorded as normal in 57% at three months versus 9% pre-operatively. Significant improvements in TBUT, Oxford conjunctival/corneal staining and reductions in glaucoma medications were evidenced at three months.14
Similar significant improvements in OSDI, TBUT, surface staining and reductions in medications were also reported in a retrospective study of 57 patients who underwent iStent combined with cataract
“IN
led to better patient-reported quality of life and a greater likelihood of being medication-free for a longer period.
Averages were 58.0% vs 45.8%; P < .05 for visual function questionnaire (VFQ)-25 composite scores and 56.7% vs 48.9%; P < .05 for OSDI composite scores. It found 75.8% of cataract surgery and iStent group versus 61.9% of the cataract surgery alone group experienced 20% or greater reduction from baseline in unmedicated IOP. In this 20% or greater group, 84% of treatment eyes versus 67% of control eyes were not receiving glaucoma medication at 23 months. Those who were VFQ-25 responders were also more likely to be medication-free at 24 months.15
As the range of treatment options for cataract and glaucoma care continues to expand, eye health care providers are presented with more opportunities to adopt a more tailored approach for cataract patients with mild to moderate glaucoma. As the concept of an ‘interventional approach to glaucoma’ gains more traction, glaucoma surgeons are, increasingly, advocating for early diagnosis and intervention treatments, including MIGs and SLT to preserve vision and quality of life. This approach enables more effective long-term management and highlights the need to explore alternatives to glaucoma drops that contribute to OSD.
Individualised diagnosis and monitoring, with an eye on the patient’s unique risk factors early on, for example, a tendency towards allergies or indeed pre-existing dry eye in those with rosacea blepharitis, can lead to better ocular surface preservation later when cataract surgery is required.
TERMS OF HEALTH ECONOMICS, DESPITE THE HIGHER INITIAL COST OF ISTENT IMPLANTATION, IT HAS BEEN FOUND THAT THE ANNUAL COSTS AFTER IMPLANTATION WERE LOWER THAN THOSE OF BOTH THE MEDICATION-ONLY GROUP AND THE SLT GROUP.12”
surgery at four months. This study, by Jones et al, also returned significantly improved glaucomaspecific (GQL-15 and GSS) and general health (EQ-5D) patient-reported outcome measures of quality of life.15
iSTENT AND CATARACT SURGERY
Samuelson et al. compared iStent inject implantation combined with cataract surgery to cataract surgery alone and found that the combination treatment resulted in greater improvements in patient-reported outcome measures at all follow-up visits over a 24-month period.16 The study, titled ‘Quality of Life in Primary Open-Angle Glaucoma and Cataract: An Analysis of VFQ-25 and OSDI From the iStent inject Pivotal Trial,’ shows that adding iStent to cataract surgery not only reduced eye pressure but also
For pressure lowering of around 20-30%, in those who are appropriate candidates, SLT is a safe modality which can be successful 80% of the time. There are a variety of scenarios that I have encountered where patients have been unsuccessful with SLT or indeed unwilling to have SLT, thus making MIGS devices an appropriate alternative. These scenarios include patients who do not have enough brow clearance for the SLT gonio laser lens or who have too much in the way of iris processes insertion into the TM preventing laser access. Other settings include those with submaximal drops reduction and persisting OSD with debilitating dryness irritation, vision blur and unacceptable redness despite successful withdrawal of a glaucoma medication after SLT. There are also those also who are afraid of or reluctant to have laser treatment despite

counselling and those who are unwilling to have multiple procedures in terms of cost and/or time when cataract surgery is more within sight and there is the realisation that a combined procedure can be conducted.
Developing treatment plans early that suit the patient’s severity of disease as well as lifestyle and age will also enable more appropriate IOL selection as well as better aftercare for glaucoma patients post cataract surgery. It is therefore important that we are able to best educate our patients by informing them of all alternatives available for mild to moderate glaucoma in order to prevent disease progression and morbidity.
There is an increased range of extended depth of focus (EDOF) lenses being used by surgeons in well-controlled mild-to-moderate glaucoma cases with non-centre involving visual field defects. With refractive segmental as well as now non-diffractive extended wavefront EDOF IOLs having less loss of contrast sensitivity being available, surgeons are now more confident in their utilisation in glaucoma patients where OSD may be minimised with interventional glaucoma.
As multifocal IOLs are less likely to be implanted in patients with more glaucoma co-morbidities, the need for shared-care is paramount with tailored
reading glasses as well as glaucoma monitoring still required.
Ultimately, our glaucoma patients deserve the best of the premium lens technologies available to us and with spectacle assistance still required by many postoperatively, care of OSD along with long-term vision and IOP stability can be had with timely interventional glaucoma management.
ACKNOWLEDGEMENTS: Dr. Kenneth Ooi would like to acknowledge the assistance of Jeff Megahan, commissioning editor, healthcare education in the writing of the article.
DISCLOSURES: Dr Kenneth Ooi is a paid consultant of Glaukos Corporation.
REFERENCES
1. L eung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma. 2008;17(5):350–5.59%
2. M ylla Boso AL, Gasperi E, Fernandes L, et al. Impact of ocular surface disease treatment in patients with glaucoma. Clin Ophthalmol. 2020; 14:103–11.
3. T irpack AR, Vanner E, Parrish J, et al. Dry eye symptoms and ocular pain in veterans with glaucoma. J Clin Med. 2019; 8:1076.
4. R obin AL, Covert D. Does adjunctive glaucoma therapy affect adherence to the initial primary therapy? Ophthalmology. 2005; 112:863–8.
5. S kalicky SE, Goldberg I, McCluskey P. Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol. 2012;153(1–9): e2.
6. B roadway D, Hitchings R, Grierson I. Topical antiglaucomatous therapy: Adverse effects on the conjunctiva and implications for filtration surgery. J Glaucoma. 1995; 4:136.
7. O oi KGJ, Leung KFC, Xiong J, Khoo P, Watson SL. Cataract Surgery and Dry Eye [Internet]. Cataract - An Update on Clinical and Surgical Management. IntechOpen; 2023. Available from: http://dx.doi.org/10.5772/ intechopen.1002481
8. C antor L, Lindfield D, Ghinelli F, et al. Systematic Literature Review of Clinical, Economic, and Humanistic Outcomes
Following Minimally Invasive Glaucoma Surgery or Selective Laser Trabeculoplasty for the Treatment of Open-Angle Glaucoma with or Without Cataract Extraction. Clin Ophthalmol. 2023 Jan 6; 17:85-101.
9. P ahlitzsch M, Davids AM, Winterhalter S, et al. Selective Laser Trabeculoplasty Versus MIGS: Forgotten Art or First-Step Procedure in Selected Patients with Open-Angle Glaucoma. Graefes Arch Clin Exp Ophthalmol. 2023 Apr;261(4):1063-1072.
10. L eahy KE, White AJ. Selective laser trabeculoplasty: current perspectives. Clin Ophthalmol. 2015; 9:833–41.
11. H engerer FH, Auffarth GU, Conrad-Hengerer I. 7-Year Efficacy and Safety of iStent inject Trabecular Micro-Bypass in Combined and Standalone Usage. Adv Ther. 2024 Apr;41(4):1481-1495.
12. O oi KG. A cataract and refractive surgeon’s early experience with iStent inject® W in Australian patients with open-angle glaucoma. Poster at APAO Bali, APACRS Chengdu, AUSCRS Hamilton Island and RANZCO Adelaide.
13. B erdahl JP, Khatana AK, Katz LJ, et al. Cost-comparison of two trabecular micro-bypass stents versus selective laser trabeculoplasty or medications only for intraocular pressure control for patients with open-angle glaucoma. J Med Econ. 2017;20(7):760–6.
14. S chweitzer JA, Hauser WH, Ibach M, et al. Prospective Interventional Cohort Study of Ocular Surface Disease Changes in Eyes After Trabecular Micro-Bypass Stent(s) Implantation (iStent or iStent inject) with Phacoemulsification. Ophthalmol Ther. 2020 Dec;9(4):941-953.
15. J ones L, Maes N, Qidwai U, et al. Impact of minimally invasive glaucoma surgery on the ocular surface and quality of life in patients with glaucoma. Ther Adv Ophthalmol. 2023 Feb 13
16. S amuelson TW, Singh IP, Williamson BK, et al. Quality of Life in Primary Open-Angle Glaucoma and Cataract: An Analysis of VFQ-25 and OSDI From the iStent inject® Pivotal Trial. Am J Ophthalmol. 2021 Sep; 229:220-229

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.

the MAX difference.






Compatible with contact lenses



Optometrists can play a crucial role in addressing corneal conditions prior to cataract surgery. DR COLBY HART says proper management of these conditions is essential to reduce complications and ensure more accurate surgical results.
MABOUT THE AUTHOR:

corneal disease and surgery
Eye Specialists, Brighton, Victoria
odern advancements in intraocular lens (IOL) technology, selection formulae and surgical equipment have enabled most cataract surgery patients to achieve excellent outcomes. However, corneal disease in these patients is increasingly common and is a source of patient dissatisfaction when not addressed adequately prior to surgery. When corneal conditions are not identified and managed appropriately before surgery, they can lead to postoperative dissatisfaction and diminished visual quality, even with technically successful surgeries.
The intersection of cataract surgery and corneal health is a critical area for collaboration. By working together to diagnose, manage and treat corneal conditions in the pre-operative phase, optometrists and ophthalmologists can enhance surgical outcomes and improve overall patient satisfaction.
Dry eye disease (DED) in patients undergoing cataract surgery is very common. In a recently published meta-analysis on this topic, it was estimated that 21.2% of the population suffer from meibomian gland dysfunction (MGD) and 8.1% of the population have clinical DED.1 In some studies, up to 50% of routine cataract surgery patients had central corneal staining despite being asymptomatic prior to surgery.2
Given the high prevalence of DED in patients undergoing cataract surgery, addressing and optimising this condition prior to surgery offers a valuable opportunity for optometrists and ophthalmologists to enhance clinical outcomes.

DED is a complex disease process that can be influenced by many factors including: reduced tear production, ineffective tear production, chronic inflammation, allergy and lid disease.4
One component common to all forms of dry eye disease is that patients have increased inflammatory cytokines in the tear film.5 Those patients with more severe dry eye disease have higher levels of inflammatory cytokines than those with less severe disease, and these cytokines reduce after ocular surface optimisation.6,7
CPD
At the completion of this article, the reader should…
• Have an ability to effectively assess the corneal endothelium's health
• Understand, and communicate to patients, the importance of delaying surgery to improve surgical outcomes
• Collaborate effectively on preand post-operative care for cataract patients with corneal conditions.
• Identify corneal guttata and its implications for cataract surgery outcomes.
One important point to consider is that DED can mimic the symptoms of cataract. Both conditions cause patients to experience a reduction in visual acuity, increasing glare and light sensitivity, difficulty driving at night and reduced contrast sensitivity.3 In fact, many of the questions asked on the ocular surface disease index (OSDI) questionnaire to grade dry eye symptoms relate to these very symptoms. This means that there are a cohort of patients who, once their ocular surface disease has been optimised, may not actually require cataract surgery. At the very least, minimising the impacts of dry eye disease on these symptoms will allow the optometrist or ophthalmologist to better understand and discuss the risks and benefits of surgery when all other reversible contributing factors have been eliminated.
Basic DED optimisation techniques such as the use of preservative free lubricants, warm compresses and lid hygiene provide a good foundation for optimisation but are often not sufficient to rapidly improve the ocular surface which is required to minimise delay in patients needing cataract surgery.8
In this setting, topical steroids or ciclosporin eye drops are often required. Recent studies have shown that a four-week course of fluorometholone9 or 0.09% ciclosporin drops10 significantly improve the signs and symptoms of DED, reduces tear inflammatory cytokine levels, and don’t cause any significant steroid related complications. This optimisation improved the accuracy of refractive outcomes within 0.75D of target after cataract surgery from 88%cto 95%.10 These treatments are easily accessible by optometrists, and initiation of them at the time of referral for cataract surgery in

patients with signs of DED and no contraindications to therapy can lead to improved patient satisfaction8 and refractive outcomes.10
In my experience, almost all patients are willing to postpone their cataract surgery by a month to optimise their ocular surface once they understand the significant benefits. Explaining how a short delay can enhance the precision of refractive outcomes and reduce postoperative complications helps patients appreciate the value of this approach. By prioritising the health of the ocular surface, both optometrists and ophthalmologists can achieve better long-term visual outcomes and overall patient satisfaction.
Corneal guttata is another frequently encountered condition in patients scheduled for cataract surgery. Mild, asymptomatic forms of guttae have been reported in up to 60% of the elderly population.11 Pre-operative assessment is vital for identifying patients at risk of corneal decompensation following surgery, enabling timely referral and appropriate management.
Central corneal guttata can diminish visual acuity and contrast sensitivity. Recognising this condition during the pre-operative evaluation allows clinicians to manage patient expectations regarding potential vision improvements after cataract surgery, fostering informed decision-making and improved clinical outcomes.
The most accurate way to measure endothelial cell density is using specular microscopy, a device very rarely purchased by optometrists or ophthalmologists outside of major public hospitals. In the absence of this device, it is important to have a repeatable method of examining the endothelial surface in patients requiring cataract surgery. Endothelial guttae have a ‘beaten metal’ appearance (Figure 1) and can be visualised using the slit lamp with high magnification and a 45-degree slit beam. Transillumination (Figure 2) and specular

reflection (Figure 3) techniques are also fantastic for visualising guttae and identifying those patients at risk of decompensation after surgery.
CORNEAL DECOMPENSATION
Most people are born with around 3,000 endothelial cells per mm.2 As we age, there is a natural loss of endothelial cells which reduces this count on average to around 1,800 endothelial cells per mm2 by the age of 60. After this, we lose around 1-2% of the remaining endothelial cells per year.
Patients who have less than 1,000 endothelial cells per mm2 at the time of cataract surgery are at high risk of decompensating after surgery, and those with less than 500 endothelial cells per mm2 are likely to be experiencing symptoms of corneal decompensation which starts with morning misting that clears through the day.
be evaluated quite accurately by asking the following questions:
• Does your vision appear misty when you first wake up in the morning?
• Is your vision mistier first thing in the morning compared to later in the day?
• How many hours after you wake up does your vision usually clear?
• Is the time that it takes for your vision to clear longer now than it was three months ago?
Water is constantly flowing from the anterior chamber, into the cornea, and back into the anterior chamber through the endothelial cells. These cells have salt pumps that pump the salt out of the cornea to create an osmotic gradient which the water follows.
The other mechanism by which water leaves the cornea is by movement across the epithelium into
“THE INTERSECTION OF CATARACT SURGERY AND CORNEAL HEALTH IS A CRITICAL AREA FOR COLLABORATION.”
Cataract surgery is often the precipitating factor in corneal decompensation, because it leads to the loss of up to 16% of remaining endothelial cells. If this tips the patient over the ‘corneal decompensation threshold’, then they will start to experience symptoms which continue to worsen as they continue to lose 1-2% of their remaining cells per year.11
The majority of optometry and ophthalmology practices don’t have specular microscopy facilities to evaluate the endothelial cell count of every patient considering cataract surgery. Furthermore, the symptoms experienced by patients who are at high risk of corneal decompensation after cataract surgery may have completely resolved if they are being reviewed by their eyecare practitioner in the afternoon.
The health of the patient’s endothelium can
the tear film. In a simplified way, the tear film has a combination of water and salt. When we are awake with our eyes open, the water component of the tears can evaporate, which increases the concentration of salt compared to water in the tear film. This increased concentration of salt pulls water from the cornea into the tear film to reduce oedema of the cornea. During sleep, with our eyes closed, the water component of the tear film is unable to evaporate, which reduces the concentration of salt in the tear film. Overnight, this reduces the pull of water from the cornea into the tear film and we rely predominantly on the endothelial cell mechanism to clear the cornea. In patients with compromised endothelial cells, this leads to corneal oedema.
Patients who have symptoms of morning misting are likely to decompensate further following cataract surgery. Ideally, patients with confluent guttae should have their cataract surgery before they develop these symptoms, to reduce the risk of requiring an
endothelial transplant after the surgery.
As the cataracts become denser, they require more energy during the operation for removal. The surgery can also take longer, which can increase the number of endothelial cells lost. Generally, if patients with guttae are unable to achieve 6/6 vision after excluding other causes, have early symptoms of cataract such as increasing glare at night, or early lens changes on slit lamp examination, it is worthwhile referring them to an ophthalmologist for consideration of cataract surgery.
Clear communication from the ophthalmologist to the optometrist regarding the duration of surgery, amount of energy required and expected clinical course of improvement in corneal oedema in these cases are particularly important, particularly if patients are being co-managed with optometrists. Most cases of corneal oedema after cataract surgery should have cleared by four-to-six weeks in the absence of persistent inflammation. If there is persisting oedema after this time in the settings of guttae pre-operatively, it is less likely to clear. Asking a patient to keep a diary once per week of subjectively how misty the vision is when they first wake up, and then again at one-hour, two-hours and three-hours after waking can give an insight into the trajectory of their improvement.
I ask patients to attach a printed Snellen chart to their fridge, cover the unoperated eye and stand at
the same distance once per week to record this. If there are no trends of improvement after four-to-six weeks, they are likely to continue to lose the normal 1-2% of endothelial cells per year, so discussing the potential for an endothelial transplant in this setting is usually appropriate.
Managing corneal conditions like DED and being aware of corneal guttata before cataract surgery is essential for improving patient satisfaction and surgical outcomes. Addressing these issues proactively helps reduce complications and enhance refractive accuracy. Collaboration between optometrists and ophthalmologists ensures better long-term visual results and sets realistic patient expectations, ultimately leading to improved cataract surgery outcomes.
REFERENCES
1. M cCann P, Abraham AG, Mukhopadhyay A, Panagiotopoulou K, Chen H, Rittiphairoj T, Gregory DG, Hauswirth SG, Ifantides C, Qureshi R, Liu SH. Prevalence and incidence of dry eye and meibomian gland dysfunction in the United States: a systematic review and meta-analysis. JAMA ophthalmology. 2022 Dec 1;140(12):1181-92.
2. Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The prospective health assessment of cataract patients’ ocular surface (PHACO) study: the effect of dry eye. Clinical Ophthalmology. 2017 Aug 7:1423-30.
3. Szczotka-Flynn LB, Maguire MG, Ying GS, Lin MC, Bunya VY, Dana R, Asbell PA. Impact of dry eye on visual acuity and

contrast sensitivity: dry eye assessment and management study. Optometry and Vision Science. 2019 Jun 1;96(6):387-96.
4. L emp MA, Foulks GN. The definition and classification of dry eye disease. Ocul Surf. 2007 Apr;5(2):75-92.
5. R oda M, Corazza I, Bacchi Reggiani ML, Pellegrini M, Taroni L, Giannaccare G, Versura P. Dry eye disease and tear cytokine levels—a meta-analysis. International journal of molecular sciences. 2020 Apr 28;21(9):3111.
6. C hen Y, Mallem K, Asbell PA, Ying GS. A latent profile analysis of tear cytokines and their association with severity of dry eye disease in the Dry Eye Assessment and Management (DREAM) study. Scientific Reports. 2024 Jan 4;14(1):526.
7. N a KS, Mok JW, Kim JY, Rho CR, Joo CK. Correlations between tear cytokines, chemokines, and soluble receptors and clinical severity of dry eye disease. Investigative ophthalmology & visual science. 2012 Aug 1;53(9):5443-50.
8. S tarr CE, Gupta PK, Farid M, Beckman KA, Chan CC, Yeu E, Gomes JA, Ayers BD, Berdahl JP, Holland EJ, Kim T. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. Journal of Cataract & Refractive Surgery. 2019 May 1;45(5):669-84.
9. Avunduk AM, Avunduk MC, Varnell ED, Kaufman HE. The comparison of efficacies of topical corticosteroids and nonsteroidal anti-inflammatory drops on dry eye patients: a clinical and immunocytochemical study. American journal of ophthalmology. 2003 Oct 1;136(4):593-602.
10. H ovanesian JA, Berdy GJ, Epitropoulos A, Holladay JT. Effect of cyclosporine 0.09% treatment on accuracy of preoperative biometry and higher order aberrations in dry eye patients undergoing cataract surgery. Clinical Ophthalmology. 2021 Sep 1:3679-86.
11. V ital MC, Jong KY, Trinh CE, Starck T, Sretavan D. Endothelial cell loss following cataract surgery using continuous curvilinear capsulorhexis or precision pulse capsulotomy. Clinical Ophthalmology. 2023 Dec 31:1701-8.

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.



Medical professionals working past the age of 70 are a small portion of the sector but apparently attract more than their fair share of complaints. Two older ophthalmologists sit down with Insight to discuss what keeps them going and the value they bring to the nation’s eye health system.
Dr Joe Reich won’t be back ice skating any time soon. He used to be rather handy as a teen, but he could barely stand on the things during a recent visit to a Canadian ice rink with his grandchildren.
His golf isn’t what it once was either – “these are things that happen with ageing”.
But the Melbourne ophthalmologist, who is well into his 70s, had no qualms about heading into the surgical suite, until an accident on Christmas Eve resulted in a broken finger.
“This will allow me to transition earlier than I expected but at a time when my surgery was still at a high level,” he says.
He may be looking to hang up the surgical greens and focus a little more on the golfing variety, but he still plans to continue consulting and his refractive practice.
Sydney’s Dr Frank Martin, aged 83, is another ophthalmologist who has continued past the traditional age of retirement and who bolsters the country’s vulnerable health workforce.
He no longer operates but continues to consult and support colleagues. They are just two among a small number of medical professionals still practising in Australia beyond the age of 70, and sometimes up towards 90.
The health and fitness of Australia’s older medical professionals and the sector in general has been brought into sharper focus after the Medical Board of Australia (MBA) announced in August 2024 it was considering health checks for those aged over 70.
The checks, which would include ophthalmologists, were one of three options put forward as part of a public consultation campaign in response to a rise of complaints and notifications involving the nation’s older health professionals.
Figures from the Australian Health Practitioner Regulation Agency (Ahpra) show those over 70 years old are 81% more likely to be the subject of a notification for any reason (not just impairment) than those under that age.
Notifications for doctors in the 70- 74-year age bracket have risen more than 130%, from 32 for every 1,000 doctors in 2015, to more than 74 per 1,000 in 2023. For medical practitioners aged 80 and over, notifications climbed by more than 180% between 2015 and 2023.
In comparison, notifications about doctors aged under 70 years increased 63% from 23.4 to 38.3 per 1,000 over the same period.
Those figures and the reaction of MBA suggest a big problem, but the reality is that the number of medical professionals still on the tools beyond 70 years in Australia is small, especially compared with other Aussies working beyond retirement age.
Ahpra’s statistics show that in 2023, there were 849,259 “practising registrants” across all medical disciplines in the health sector, with just 18,686 of them – 2.2% – aged 70 and over. In optometry, of the 6,503 practising registrants, just 90 (1.4%) were over 70.
And in ophthalmology, RANZCO figures show 114 professionals still practising over the age of 70, with 88 of those working fulltime. Just nine were aged over

Image: Frank Martin.
“We have a shortage, especially in paediatric ophthalmology and strabismus management, including surgery. We need every person who is capable of delivering service to be available to continue to work.”
Dr Frank Martin Children's Hospital Westmead

Dr Joe Reich was still operating, well into his 70s. He remains confident of his abilities.
80. With 1,092 practising ophthalmologists, according to MBA data, that’s 10% of the workforce over 70 and 0.8% over 80.
That compares with Australian Institute of Health and Welfare figures showing that in 2021, 15% of all Aussies were working beyond the age of 65.
Small those numbers might be, but both Dr Reich and Dr Martin believe the impact of more ophthalmologists far outweighs its few numerical parts.

And Dr Peter Sumich, president of the Australian Society of Ophthalmologists (ASO), believes that a health sector struggling with workforce issues simply “can’t afford to lose people”.
He says older professionals are involved in mentoring and training younger colleagues, they are taking leading roles in their profession and their experience is actually saving lives, not just eyesight.
Dr Reich works three days a week. He continued past retirement age because he was still confident of his abilities and issues with his surgical patients had been rare.
“I was getting plenty of referrals, and my colleagues were still asking me for advice and sending me difficult cases. I didn’t feel any need to stop.”
He acknowledges continuing past the age of 70 will not be possible for everyone, and not just ice skaters and golfers.
“Human physiology is such that we all vary, and some people are quite happy to retire early, particularly if they feel that they’re not quite as skilled as they were.
“And there’s the old 10,000-hour rule, which says the more you have practised something, the better you’re likely to be at it.”
Those 10,000 hours can help an experienced ophthalmologist pick up something that might be missed by a younger colleague. Even something potentially life-threatening.
“Recently I saw a patient with a bulgy eye that could have had any number of diagnoses, and when I referred it on to somebody who knows that area, I said, ‘I think this patient has a lymphoma’, and he came back with a biopsy and said, ‘you’re right’. Now that’s from having seen a few of these over a career.”
He believes that those who step away from surgery can still diagnose and treat eye disease.
“If you’re doing general ophthalmology there are many other fields that do not require surgery, and probably the largest of those is glaucoma,” says Dr Reich. “And then there’s macular degeneration issues, and many of the sort of incidents that can creep up on people that do not require an operation.”
Dr Martin stopped surgery four years ago, at 79, but that barely dented his workload. His “part-time”, four-days-a-week schedule includes private work in a Macqaurie St practice and a role as a visiting medical officer at Children’s Hospital Westmead.
On top of that, he, like Dr Reich, has other medical management roles,


urged him to change his mind, but “I said, no, I’d much rather have this discussion than a discussion saying, ‘hey, when are you going to stop?’”
That collective scrutiny and discussion, within a team of professional colleagues, is key to supporting older practitioners but also ensuring they remain fit to practise.
“Working in a group, you’re being constantly peer-reviewed, because we see each other’s patients, and we work together,” says Dr Martin. “It is the same as when I work in a clinic at the Children’s Hospital; I have registrars, fellows of other ophthalmologists working with me, and so I feel that at the moment, the quality of my work is still fine to keep doing it.”
Dr Reich agrees: “I get people from my own practice who spend time with me, I’ve always felt very open to that.”
ASO president Dr Sumich believes that’s a feature of work within the ophthalmic discipline that helps to ensure practitioners are up to speed, fit to practise and the public is safe, no matter what age the specialist is.
“What we have with RANZCO is a practice visit component of our CPD where a colleague comes and visits for a day and spends time with the professional, and both write a report for the CPD,” he says.
“I would suggest that should become more of a feature for people over 70, which takes care of their abilities and their cognitive abilities, and also how up to date they are. That’s far more valuable than a health check.”
Self-audits are also important, and keeping up to date on complication rates, as ophthalmologists continue to assess their own skills, their ages and the potential impacts on patients.
“As a professional, it’s on you to present yourself as healthy enough to do your job,” says Dr Sumich. “So health-wise, I don’t think there’s any difference between a 70-year-old and a 50-year-old.”
Dr Reich agrees: “I’m not so full of myself to think that I’m the only surgeon in town.
“I think that’s one of the problems that you can have as a doctor. And you’ve got to be aware that there are times when you have to look at slowing down or stopping.”
That’s why both work hard to keep up to date with advances in technology and
treatment, through conferences and CPD, but also by rubbing shoulders and sharing knowledge with younger colleagues.
It’s also what keeps them mindful about how they communicate with a variety of patients and colleagues.
Dr Sumich believes it’s that failure to communicate and a clash of generational cultures – rather than a failure in ability or standards – that may be to blame for the rise in complaints against older medical professionals.
“As younger doctors, I suspect we’re a little bit more patient in dealing with patients who are difficult and patients who need to be smoothed over and maybe get an explanation,” he says.
“I strongly suspect that as you get older, you just become a little bit grumpier, and what could have been smoothed over ends up as a complaint.”
Dr Martin disagrees.
“My personal experience has been that there are just as many younger grumpy practitioners,” he says. “I know for fact that in my many years of practice I have never been grumpy or rude to a patient.”
He says his ability to communicate "comes naturally; just as I communicate with my grandchildren, my children, others in the community, I can communicate with patients young and old".
Both he and Dr Reich are surprised that older professionals are pulling in more complaints, and both report to having received none personally.
“I think one of the issues we have is a lot of doctors tend to work alone,” says Dr Reich, “and without that scrutiny are sometimes reliant upon their receptionist or their practice nurse to tell them they’re not at the standard that you once were, or what the patients expect.
“The advantage in working in a group is that you get the immediate feedback.”
Communication was not part of training for older medical professionals, he says.
“And that’s one of the real risks, is that you can still be practising 50 years after you’re trained, and still practising in a manner that you were originally taught. And that might mean not communicating well with patients, and not actually practising as you should,” Dr Reich says.
“There’s no doubt that the younger generation, even in their medical school, have been taught communication skills.”
Attitudes towards doctors had changed over time, as well.
“I think there have been doctors in the past who had a great degree of selfimportance,” he says. “And arrogance, where the doctor knew what was best for you.”
He felt that there could be more training, especially for older medical professionals, to help them communicate better with patients.
Dr Sumich said the ASO had touched on communication in previous events and conferences, including video sessions on how to deal with difficult patients, but there could always be more training and support.
While he was less enamoured with the idea of health checks for older professionals, and felt organisations like ASO and RANZCO had the tools in place to ensure the fitness of older professionals and the safety of the public, Dr Reich and Dr Martin offered a collective shrug of the shoulders.
People their age were used to health checks in order to keep driving their vehicles. It was “not unreasonable” to expect similar testing for ageing medical professionals.
“I’ve got no problem with it,” says Dr Martin. “I’d be very happy to go to my general practitioner, just like when I renew my driver’s licence.
“People over a certain age are taking certain medications,” says Dr Reich. “There’s probably very few people over the age of 70 who aren’t on antihypertensive or cholesterol-lowering drugs. And there are more serious conditions, which probably the patient needs to know about.”
But like Dr Sumich, he wonders if a health check would be focused on the right things. He mentions Portuguese football star Cristiano Ronaldo; at 40 he remains one of the world’s best and is still scoring goals at the highest level.
“If you take your 40-year-old footballer and you gave him a health check, he’s probably going to be in fabulous health, right?
“But ask him whether he passes the football as quickly or his reactions are as quick as they were when he was 10 years younger and you can understand that a health check may not pick up the things, in surgery, for example, which is where it’s most critical, and also in consulting.
“You need to have a check on what a person’s skills are like in terms of handling the procedure that they’re doing, and are they still doing it as well as they did, or are they doing it better and whether they are competent in maintaining up-to-date diagnosis and care of patients with complex disease,” he says.
Both are happy to offer that reassurance of their remaining prowess; if not for the patients then at least for a health sector with a vulnerable and stretched workforce. One that, as Dr Sumich points out, can’t afford to lose ophthalmologists.
He believes there are fewer issues in ophthalmology, where the challenge is more about distribution of that workforce and resources in the regions and remote parts of the country.
But Dr Martin believes a problem does exist.
“We have a shortage, especially in paediatric, ophthalmology and strabismus management surgery, and we need every person who’s capable of delivering service to be available and continue to work.”
That vulnerability was highlighted in the RANZCO publication Vision for Australian Eye Healthcare to 2030 and Beyond, which said the ophthalmology workforce was “struggling to meet the nation’s needs”.
“Adult and paediatric public ophthalmology services across Australia are under-resourced to meet the needs of the population they serve, with increasingly long waitlists to access outpatient and inpatient (elective surgery) services,” the report said.
“A national shortage of specialist ophthalmologists in Australia is inevitable. To avert this crisis, Australia needs an immediate and steady increase in the overall

And until there are enough trainees coming through to meet the sector’s workforce challenges, it will continue to rely on this ageing population of medical professionals.
Older medical professionals are still making a meaningful contribution to the health of their patients and communities.
Even if they are not what they once were on the ice rink and putting green.



The launch of Rayner’s world-first spiral IOLs in Barcelona last year set tongues wagging in the global ophthalmic community. Early adopters in Australasia discuss how the all-new design measures up.
Dr Lourens van Zyl’s mother can rest easy. So can many of his patients who have waited for this moment – even delayed their own cataract surgery in anticipation of an intraocular lens (IOL) that ticks more boxes than any other he has previously used.
The world’s first spiral IOL has arrived. The RayOne Galaxy and RayOne Galaxy Toric lenses are now available in Australia, and it appears surgeons and their patients can’t wait to get their hands on what has been described as the “next evolutionary step” in IOL technology.
Dr van Zyl goes a little further.
The eye surgeon at Perth’s Crystal Eye & Laser Centre, who was one of the first practitioners in Australia to use the new lenses, says the latest offering from UK-based manufacturer Rayner is “absolutely the closest we’ll get to the holy grail of lenses”.
“What we’re looking for is good near, good distance, good intermediate vision, with almost no night-time symptoms,” he says.
“This is it.”

So impressed is he that he would happily offer the IOL to his mother.
Other surgeons Insight spoke to, including Dr David Gunn and Dr Ben LaHood, are also excited about the promise Rayner’s newest offering holds, which they described as a “refractive full range of vision lens.".
RayOne Galaxy caused a big stir at the European Society of Cataract and Refractive Surgeons Congress in Barcelona last year, where over 600 surgeons packed a lunchtime symposium moderated by Dr Başak Bostancı (Turkey) to hear from a number of early implanters, including Mr Allon Barsam (UK), Professor Claudette Abela-Formanek (Austria), Dr Alain Saad (France) and Dr Dean Corbett (New Zealand).
They reported that the lens, designed using a proprietary AI engine trained on patient outcomes and the expertise of Brazilian ophthalmologist Dr João Lyra, was indeed worthy of that excitement.
The company says that RayOne Galaxy’s unique spiral delivers a continuous full range of vision with minimised dysphotopsia, achieved through a non-diffractive optic with 0% diffractive light loss.
The surgeons reported excellent early outcomes and discussed how the spiral optic works to elongate focus and minimise dysphotopsia.
Dr Corbett presented video testimonials from his first two patients, who reported excellent visual acuity with no halos or bothersome night-time visual disturbance.
He has now implanted the IOLs in at least 30 patients, and he says they are happy with the IOL’s performance, their “great near vision and the lack of halos”.
One of his patients, an 80-year-old male said that “I can read that very small
print which I certainly couldn’t do before’ and ‘I can see the birds in the trees”.
He also compared his night vision while driving with that of his wife, who has bilateral diffractive bifocals, and was ecstatic that he does not experience the halo and glare that she does.
For Dr van Zyl, about 90% of his work is refractive cataract surgery and he uses a number of Rayner products because he likes the range and the ease of use during surgery.
“I use the RayOne EMV lens quite extensively, and I also use the aspheric lens a lot in patients who want Presbyond [laser surgery] or who have cataracts.”
But he has steered away from multifocal lenses in the past because of the diffractive pattern, the glare and night halos they usually bring.
“My preference is an extended depth-of-focus lens.”
Often, he has needed to explain to patients that such lenses can come with compromises.
“I tell patients that there’s no free lunch,” he says. “I’m not God or Jesus. You will have to compromise somewhere.”
That has often meant putting up with compromised near-vision, and halos at night, making driving late difficult, even dangerous in some cases.
But he has been very impressed, and a little surprised, at the ability of the RayOne Galaxy lenses to deliver excellent vision across the board, and particularly the big challenge of near vision, all while minimising halos and glare.
At time of writing, Dr van Zyl had implanted the Galaxy IOLs into 12 patients.
“The fact that they have excellent near vision with distance vision and a

good range, obviously, I think Rayner has [launched] something as close to the holy grail as we can probably get at the moment.”
Social media chatter meant that many of his patients had also picked up on that buzz and had delayed their surgery so they could get access to the RayOne Galaxy IOLs.
They won’t need to wait long now, after Rayner released them into the Australian market in January 2025. However, the company is yet to gain Prostheses List (PL) approval allowing healthcare reimbursement.
That is unlikely to be a deterrent for many people, says Dr van Zyl, and particularly those patients wanting to be free of their spectacles.
It’s a great lens for the surgeon to use as well.
That meant the product would be ideal for those looking to venture into offering more advanced lens designs to patients.
“I think the RayOne Galaxy lens is the gateway product for a general ophthalmologist to go into vision correction surgery. It’s a very easy lens for young surgeons who are a bit wary of premium lenses.”
At this early stage, Dr Gunn, from the Queensland Eye Institute, is a little more cautious than his WA counterpart, but says the lens shows a lot of promise. About 80% of his IOL implants are presbyopia-correcting IOLs and toric, and he uses products from all of the major manufacturers.
At time of writing, he had implanted the RayOne Galaxy IOL in 10 patients.
They had reported excellent results.
“My first case, the patient had a complete range of focus, zero halo, zero glare,” he says.

“She’s like, ‘I’ve never seen like this in my life, my vision is perfect; I’ve got no issues at night’.”
But one swallow doesn’t make a summer, and Dr Gunn is looking forward to seeing the longer follow-up of the multicentre data evaluation.
Like Dr van Zyl, he has patients who have done their research, picked up on the excitement and are now queueing up to use the RayOne Galaxy IOLs, even if that means paying out of their own pocket for now.
They are eager. So is Dr Gunn, in part because he’s been following the development of the technology for some time.
“I’d heard a bit about spiral optics before, and I just love that idea, to be able to give a patient a full range of vision, giving them distance into being near, but not needing diffractive rings and all the issues that come with that design.”
He believes there will be many patients, particularly younger ones keen to be spectacle-independent, who will be ideal candidates for the RayOne Galaxy IOLs. And he believes that group will grow larger when the RayOne Galaxy IOLs are approved on the PL.
“Maybe those patients who couldn’t have had a diffractive multifocal suddenly can have a spiral optics lens.”
It was Dr LaHood, a consultant ophthalmologist at Adelaide Eye and Laser Centre, The Queen Elizabeth Hospital in Adelaide, and senior lecturer at

“Despite their relatively smaller size, I am sure that these types of innovations, combined with their friendly team, will see Rayner become one of the big players in the eye world for years to come.”
Ben
LaHood Adelaide Eye and Laser Centre
the University of Adelaide, who said the RayOne Galaxy IOL was the “next evolutionary step” in the technology.
He stands by that claim, although, like Dr Gunn, he is eager to see the long-term outcomes.
Dr LaHood implanted his first Galaxy IOL in October last year, and now has 10 bilateral patients he continues to follow closely. He’s treating it as “another multifocal option alongside a traditional trifocal diffractive IOL”.
“So far, near-vision has been the first thing patients have noticed to be improved,” he says.
“Distance visual acuity has taken a little longer to reach a steady state.”
Now he is routinely getting 6/6 distance vision in those patients.
“Unlike standard trifocal implants, my patients are not as aware of ‘sweet spots’ of focus but rather a good continuous range of vision from distance to reading. This is consistent with defocus curve data from the early user group.”
His patients have not complained about halos.
Asked about advice for his colleagues, Dr LaHood says he hasn’t had any adverse events or refractive surprises but he would still consent patients they may have a higher risk of needing refractive laser enhancement, IOL exchange or even glasses – “simply because we do not yet have as much experience with this lens”.
“Personally, my experience has been that I have had to do fewer enhancement procedures compared to my standard trifocal cohort of patients, and this is reflected in the excellent prediction error data from the early user group.
"I recommend using the Barrett Universal II formula or Rayner’s Raytrace premium IOL calculator website which has been updated to include the PEARL-DGS formula from Damien Gatinel and colleagues. Aim for mild hyperopia with the current A-constant. Somewhere between plano and +0.25D should be sufficient.”
He’s consenting patients by asking them if they would prefer a trifocal with a longer history of usage, or the new Galaxy technology knowing that there’s still more to learn about the lens that doesn’t have reimbursement yet.
Overall, he felt that would help increase his candidates for full range of vision lenses and, long term, “I see it replacing the diffractive trifocal and eating into the EDOF mini-monovision space”.
“One of the key features that impresses me [about Rayner], has been that from CEO to local staff, the Rayner team have a great attitude towards surgeons, with great communication and making things happen,” Dr LaHood says.
“Despite their relatively smaller size, I am sure that these types of innovations, combined with their friendly team, will see Rayner become one of the big players in the eye world for years to come.”

Hoyalux iD WorkStyle 3 are premium lenses designed for the clearest, most comfortable & natural vision for your specific needs
Hoyalux iD WorkStyle 3 are recommended for wearers of premium progressive designs (e.g. Hoyalux iD designs) and individuals who constantly switch from one device to another at the near to far intermediate distances.
• Our most premium lens design
• Up to 2m, 4m or 6m distance
• Three individual designs (Close, Screen, Space) that can be utilised based on visual preferences
• Excellent for far-intermediate to near fields of view To learn more about



Melbourne ophthalmologist Dr ELVIS OJAIMI outlines his pre- and post-operative treatment regime for surgical patients, and why he reaches for preservative-free products whenever he can.

Throughout an ophthalmologist’s career, there are many moments when one might look back at the way things were done with a mixture of curiosity, admiration, and sometimes disbelief.
For Dr Elvis Ojaimi, a Melbourne surgeon with expertise in complex cataract surgery and vitreoretinal surgical procedures, one thing that perplexes him –knowing what he knows today – was the lack of emphasis placed on the tear film in ophthalmic surgical patients.
But beyond that, there is the impact of preservatives, despite the good intentions of eyecare professionals prescribing eye drops to relieve discomfort.
“Compared to 10 years ago, there’s a much higher priority put on the tear film, especially before surgery, so we can obtain accurate biometry measurements, such as A scans and keratometry.
“Today, I go as far as prescribing patients eye drops before they see me for their first visit (two to four weeks). Many I see are older with meibomian gland dysfunction (MGD), some have aqueous insufficiency or rosacea. I’m more attuned to picking up these ocular surface issues early because in the past we didn’t, and it came back to bite you. Patients would get fantastic refractive outcomes but would be unhappy with pain and intermittent blurriness.”
Thankfully for Dr Ojaimi today, such occurrences are a rarity, after making lubricating eye drops a key part of his pre- and post-operative regime in the face of overwhelming evidence, especially in cataract cases.
But he has gone a step further, ensuring his patients only use preservative-free products, after multiple studies highlighted the benefits in terms of dry eye symptoms, inflammation and, in Dr Ojaimi’s own experience, recovery time.
“If you’ve got preservatives in your drops, I think it disrupts and slows down the healing of the incisions and the ocular surface.”
It all began a few years ago at a conference when Dr Ojaimi was talking to corneal surgeons lauding Hylo Forte (sodium hyaluronate 2 mg/mL), a preservative- and phosphate-free product available in Australia through AFT Pharmaceuticals.
The company is one of the country’s best known sellers of preservative-free ophthalmic products, including lubricants, eye wipes and heat masks.
Upon further investigation, he discovered the company also supplied NovaTears (perfluorohexyloctane) and NovaTears+ Omega-3, a unique preservative-free eye lubricant and tear film stabiliser specifically designed for the relief of evaporative dry eye disease.
With many of his patients suffering from MGD, which comes under the evaporative dry eye umbrella, NovaTears has now become a pre-operative go-to in his clinic. He’s also talking to them about warm compresses and eye lid hygiene – to ensure the tear film is optimal ahead of the crucial work-up phase. With increasing demand for premium multifocal and extended depth of focus
intraocular lenses, he argues highly accurate biometry readings have never been more important.
He prescribes Hylo-Forte standalone often in slightly younger patients with aqueous deficiency.
And about 20% of patients are recommended a combination of the two therapies – those who may be struggling with issues like Sjögren’s syndrome and poor aqueous volume along with MGD and/or blepharitis.
Post-operatively, Dr Ojaimi encourages patients to continue with their preservative-free drops for two months until they stabilise. This even includes his surgical and medical macular patients too.
“When we perform vitrectomy, we put three trocars into the conjunctiva, there’s Betadine, and so much disruption to the ocular surface,” he says.
“And even with intravitreal injections, and patients with sensitivity and bad dry eye beforehand, they’re the ones that can really suffer after treatment, and it takes them a few days to recover.”
While these products tick many important boxes for Dr Ojaimi, they also have some added benefits.
This includes availability in specially designed multidose containers, making them easier to handle for patients with arthritis and dexterity issues.
Hylo-Fresh, Hylo-Forte and Novatears are available over the counter, can last up to six months after opening, and for some, they’re also available via the Pharmaceutical Benefits Scheme.
That makes them an affordable and accessible option for many.
What’s more, the company recently released a preservative-free glaucoma medication, Vizo-PF (dorzolamide hydrochloride; timolol maleate). It’s encouraging news with a 2024 study showing that prolonged pre-operative use of topical glaucoma medications with preservatives may negatively affect long-term trabeculectomy outcomes.
Three years since switching his regime to preservative-free eye drops from AFT Pharmaceuticals, Dr Ojaimi says the difference in patient outcomes has been palpable.
“Acuity recovery is pretty fast with cataract surgery, but it’s the irritation and intermittent blurring, having to blink to get their vision right, that causes the most concern.
“It used to take months longer for patients to recover after surgery, but we now know, with pre-operative moderate or severe dry eye, preservative free drops such as NovaTears in the perioperative period allows for a smoother recovery.”
And 10 years from now, it’s a decision he can look back on, knowing he did right by his patients.
ABOVE, L to R: Hylo-Forte, Hylo-Fresh and NovaTears are commonly prescribed by eyecare professionals because they don’t contain preservatives; Dr Elvis Ojaimi says preservative-free eye drops are key to desired post-operative outcomes.






ZEISS’s ultra-widefield retinal camera is finding a home in optometry practices and ophthalmology clinics across the country. Insight explores how it’s being used in both settings, underpinned by advanced software.
n 2003, after moving from Ireland to Australia with his young family, optometrist Dr David Shanahan opened a boutique practice in Fremantle, Western Australia, a location he continues to occupy today under the name David Shanahan Optometrists.
He kitted out his rooms with the best equipment, with a retinal camera being a top wish list item when they became available around 2006. A couple of models have served him well over the years, but nothing has come close to the resolution and widefield view he can obtain with the ZEISS Clarus 500.
Since becoming available in 2018, the instrument has developed into a must-have device in independent optometry practices across the country. It’s a staple in ophthalmology clinics too, where specialists are making highly informed clinical decisions thanks to its availability on the ZEISS Retina Workplace, powered by Forum.
At David Shanahan Optometrists, the Clarus 500 was installed in 2019 as part of a broader investment in a suite of ZEISS devices and software.
Dr Shanahan says ultra widefield imaging is becoming increasingly commonplace in optometry, knowing that indications of disease are often located in the far periphery of the retina.
One of the big advantages with the Clarus 500 instrument, according to its manufacturer, is that it allows clinicians to use colour to their diagnostic advantage.
The device generates images that closely resemble the colouration of the fundus as seen during clinical examination, aiding the diagnosis and documentation of ocular disease, and instilling confidence when evaluating the optic disc, nevi and lesions where colour is important.
Dr Shanahan agrees, but for him one of the most useful functions is the
use of IR Preview that allows the user to optimise alignment, intervene with lid and lash, and remove artifacts before capturing an image.
He says it’s akin to a live infrared image that allows the optometrist to assess the retina and identify the target area in “excellent quality” before acquiring the image.
Routinely, each patient’s retina is examined with the slit lamp before jumping on to the Clarus 500 for review in IR Preview and an image is taken, undilated. For patients with suspicious retinal pathology, a more thorough examination takes place on the slit lamp with a retinal lens, and they are dilated before having their eye scanned in multiple positions.
The technology can produce a 133-degree widefield image, which can then be automatically merged to achieve a 200-degree ultra-widefield of view.
“One thing that concerned me with some other retinal cameras was they would provide an oval-shaped image, which is horizontally wide and vertically narrower. When you’re looking for retinal detachments, you’re especially interested in those in the superior retina, they’re the ones you don’t want to miss, and the Clarus is great for that.
“The big reason everyone’s interested in ultra-widefield imaging is that it allows us to photograph a suspect area that you see with your retinal lens or slit lamp, allowing us to document those the lesions in the peripheral retina.
“And sometimes the Clarus has detected retinal detachments in the peripheral retina that weren’t visible on the slit lamp.”
That’s happened a few times, with a notable case involving a patient who is a medical specialist. It couldn’t be seen on the slit lamp but was clearly defined with the IR Preview function before being scanned. A sectional OCT scan over the lesion confirmed the retina was elevated and he was
referred and subsequently received laser treatment.
A big part of that diagnosis was the use of the Blue Channel function. Although this is designed to increase visibility of the anterior retinal layers, allowing easier visualisation of the retinal nerve fibre layer and epiretinal membranes, Dr Shanahan has found it serves another purpose in his practice.
“Something that’s not really spoken about is that it’s great for detecting retinal detachments and retinal holes, helping diagnose if a retinal hole is old or new, or if there’s an area of elevated detached retina around the hole,” he says.
“It’s proved useful for detecting and diagnosing how serious a retinal lesion is. Is it just a hole that’s not leaking, or is it a hole with a whole area of retina surrounding it that’s elevated and detaching?”
To ensure he got the most out of his ZEISS equipment, Dr Shanahan went the extra mile and invested in the company’s Forum data management software. It works to provide seamless data integration of various diagnostic devices.
“It puts all the patient data in one place, and it’s easier to share with specialists we refer to; it’s a software that many ophthalmologists have.”
One of those ophthalmologists is Dr Michael Karpa.
The owner and sole ophthalmologist of Best Practice Eyecare, in Caloundra, Queensland, says Forum has been a game-changer for his high-volume clinic that sees a lot of glaucoma, medical retina, and dry eye cases.

“The colour is as close as you can get to the real thing, but it’s the definition that impresses me the most.”
After all, one of the biggest challenges for busy ophthalmologists today is not only capturing images and data, but finding ways to compile these into meaningful analyses that balance efficient workflow with an exceptional patient experience.
Dr Karpa has a suite of ZEISS equipment that feeds into the Forum software, one of them being the Clarus 700 that he installed as soon as it became available in Australia.
“Every single piece of patient data I capture, whether it’s from the Clarus 700 or my other ZEISS equipment like the OCTs, visual field machines or slit lamp, it all comes into Forum in a single location. It’s seamless, efficient and patients love it when you’re able to show them what’s going on.
“I’m avoiding the need to run around and check results on different machines, and can make much better and informed clinical decisions.”
Forum is the software powering the ZEISS Retina Workplace. It allows ophthalmologists like Dr Karpa to elevate their practice with software that can align ultra-widefield fundus images with OCT angiography

Dr Michael Karpa Best Practice Eyecare
images — all on one screen within seconds.
For example, on the platform users can navigate multiple analyses at the same time; they can review synchronised data such as OCT macular cubes registered with OCT raster scans and fundus images. Pathological changes can also be tracked over time with one click, by comparing three exams on a single screen.
History charts can record treatment decisions over time to help assess effectiveness.
That allows Dr Karpa to track subtle changes in pathology as well as view, compare and annotate images. It’s comprehensive, yet efficient.
After conducting a trial on two leading ultra-widefield systems, access to ZEISS software was a major factor in Dr Karpa’s decision, but not the only one.
The Clarus 700 hardware stood out for two big reasons. Even though his staff were more familiar with another piece of technology, he says they found the Clarus 700 simpler to use from the get-go.
“It gives off a bright flash that patients don’t always like, but other than that we have no difficulty getting them positioned perfectly to acquire an image.
“You can get out to 200 degrees, it does take a few shots, however the image quality is superior – there’s really no comparison. The colour is as close as you can get to the real thing, but it’s the definition that impresses me the most.”
That high-resolution, ultra-widefield image can be captured down to seven microns.
While each patient has a retinal scan to establish a baseline regardless of their case, imaging of the optic nerve head in glaucoma, monitoring of macular degeneration, including geographic atrophy (GA), choroidal nevi, peripheral lesions, lattice retinal tears, and checking the stability of retinoschisis are all common pathologies where the Clarus 700 becomes indispensable.

“It’s also an excellent record for diabetic maculopathy retinopathy; it’s much better than any description I can write.
“Fundus autofluorescence is something we use all time, which is helpful to monitor disease in the retina without any visible changes, and is also useful for monitoring of GA.
“We also perform a lot of fluorescent angiograms (fundus fluorescein angiography) here, and we find the blue channel very easy to use for this.”


































Glasses and contact lenses are not the only things that can help people with poor vision. Insight discovers there is more that can be done when a patient is living with permanent vision loss, if the professionals allow theirs to be opened to the help available.
Pop quiz – you’re an optometrist in a busy practice. You have a patient whose sight has deteriorated so much that they are defined as low vision or blind. You have performed all of the tests, prescribed glasses but now realise you have done all you can to save what sight they have left.
What’s your next step? Does your responsibility to that person end when they leave the store?
Optometrist Mr Michael Peter says the answer is no.
Peter, optometry director of two Specsavers stores in rural western Victoria – Horsham and Stawell – says that not only does an optometrist’s responsibility extend beyond the test room, there are simple, effective ways to extend that support in ways that can improve the patient’s quality of life, and make the most of their remaining sight.
That’s about coming to terms with the limitations of what can be done and then working with support and rehabilitation organisations like Vision Australia as an extension of care.
Peter understands the frustration and emotion that can come with realising there is little more you can do to help a patient with deteriorating eyesight.
“I think there’s a sense of failure,” he says, “and I can feel quite frustrated with not being able to improve people’s vision and dealing with the emotions as well.”
He believes up to 10-15% of his patients could be classified as low vision or blind, living with a degenerative condition that is not correctible by glasses or contact lenses.
That’s on top of the many other ocular ailments they deal with in their busy rural practices.
“We see a lot of pathology, so we are sort of the first port of call where we have to deal with a lot of diabetic retinopathy, a lot of macular degeneration, dry eye, cataract.
"We also see your infective cases, do a lot of foreign body removals, even retinal detachments.”
His optometrists do have the support of ophthalmologists in Ballarat and
Bendigo, but when a patient’s eyesight has become so bad that there is little more he or his staff can do, Peter looks elsewhere for support.
As part of his consultation, he’ll talk with the patient about the help and information available from Vision Australia and other support agencies.
“I have a discussion with them about how they are coping at home: Do they have help? Are they living alone? And based on that, you can make that decision about whether they need further assistance – all in the interests of ensuring their safety.
“Once you get their consent you can make a referral, and that’s pretty easy these days.”
Using the Oculo patient reporting system, he can refer the patient to Vision Australia; those without Oculo can do this directly on the organisation’s easy-to-navigate website.
“I just fill in the patient’s details, I give a description of why I’m referring them and what their condition is, and then I add the actual report that I wrote up on Oculo. And then Vision Australia contacts the patient, and they take it from there.”
As part of that ongoing support, he will normally get an email back to say that Vision Australia has contacted the patient and also about the progress made.
He says that support becomes an extension of the follow-up consultations he has with the patients, most of whom are happy to get help navigating their homes and their communities with failing eyesight.
“I’ve got one older patient, she lives rurally, and she lives on her own, and the biggest help they could give her was actually within the home – how to navigate safely around the house, in the kitchen or laundry, with magnifiers and other daily living aids. This extends to learning how to navigate outside the home and travelling around the community safely and things like that. She was happy about it.”
The irony is that it’s not just the patients who live with the limitations of low vision.
Peter admits that many optometrists, even his own team members, don’t fully understand the support that organisations like Vision Australia can provide.
“That elderly woman, she didn’t know she could be eligible for certain disability support funding or access services and products that organisations like Vision Australia offer that could be helpful for her.
“I think there’s awareness of Vision Australia,” he says, “but the attitude [among optometrists] is that they can only help with visual aids.
“It’s about more than just visual support. Vision Australia gives people access to mobility training, emotional and wellbeing support, an array of daily living aids (not just magnifiers), connection to social and recreational groups, information services like library and radio, all those sort of things – it’s a wider spectrum than just vision.”
That’s where Mr Nabill Jacob comes in.
The senior orthoptist is the clinical relationship manager at Vision Australia and a key part of that role is helping the ophthalmic sector better understand the support available to them and their low vision and blind patients.
He too has witnessed some of the misconceptions in the community about what Vision Australia does, the support it provides, even who it represents.
“I realised as a clinician that ongoing low vision care of patients tends to be a little bit back of mind for eye healthcare practitioners,” he says.
“Often, I’m at a conference and I’ll have a prominent health practitioner come up to me and ask me, ‘you only work with children, right?’ Or ‘you only do mobility training’.
“So, there’s a lot of misunderstanding as to what we do,” says Jacob. What Vision Australia does offer is a comprehensive range of programs and products for all ages and stages in life, be it someone born blind or someone with low vision as they age.
In addition to its core allied health services such as occupational therapy and orthoptic low vision assessments, it can assist young children to develop life skills, help someone find or keep a job, provide a comprehensive range of accessible technology products, peer support programs, mobility training, including Seeing Eye Dogs, as well as information services such as a dedicated library and radio network.
Jacob says Vision Australia is this country’s leading blindness and low vision agency, with over a century of service and advocacy to the blindness community - seeing close to 40,000 people per annum.
And it’s keen and ready to take on more.
That’s why it has been working with Specsavers since September 2023 to deliver a more holistic approach for its many low vision and blind patients.
Specsavers says it realised its optometrists could be further supporting patients with low vision.
“Specsavers responded with open arms,” says Jacob.
It has become an education and awareness-led partnership, with Vision Australia and its services being highlighted in a growing number of Specsavers stores through their “morning team huddles” that have become commonplace across their store network before doors open.
“We go out for about 20 minutes to talk to them about the low vision referral process, the services we offer, and how it can help their patients. The in-practice team also have an opportunity to ask questions.
“We’re involved with the annual Specsavers Clinical Conference. We exhibit there. We’ve also seen a number of their team members coming into a Vision Australia office and spending half a day with us to better understand what it is we do.”
That ongoing engagement has helped grow awareness within one company, but Jacob sees an opportunity to help others understand, while also helping more low vision and blind people.
“We estimate over half of the estimated 450,000 people in Australia with low vision or blindness are going without support, either unaware or reluctant to seek help,” he says.
Which is why he’s keen to work with other optometry and ophthalmology


practices and businesses. Independent or corporate, it does not matter.
To help make that happen and the process as easy as possible, Vision Australia has cut down barriers and simplified the referral process, including signing up to Oculo, which is used by a large number of ophthalmic practices around the country.
Vision Australia is keen on more meaningful relationships with patients and practices – not just a last, passing thought as the person leaves the store.
“We want the practitioner to actually make the referral, not to give them a phone number or suggest to the patient or their loved one that they self-refer,” says Jacob.
“We want it done in the clinic, before they leave, when risk factors or injuries are identified, or they’ve just been diagnosed with a progressive condition, or they’ve just lost their driver’s licence.”
As optometrist Peter points out, that’s easy enough to do as part of the normal consultation.
But, more importantly, it’s part of the ongoing responsibility of eye health professionals to the patients under their care.
“When their vision goes and they have deteriorating sight, we as optometrists need to know that they’re OK out in the community and at home as well,” he says.

ALLYSON CAFFELL discusses the harsh realities of independent practice ownership, why it’s ultimately worthwhile and how an optical dispensing qualification gave her the confidence to take the plunge.
fter starting an optical career in 1998, I spent the first 15 years working for an independent and then a chain store in reception, but decided to further my skill set with a Cert IV in optical dispensing. Upon completion, I had new knowledge, lots of ideas and heaps of motivation, which I tried implementing right away.
I was quickly shut down and thought to myself: why did I waste all of that time and effort? Disheartened for a while, I eventually emerged from my slump and wondered if I could go into business
So that’s what I did, opening Northam Optical in Western Australia and I’ve never
I have now been open for 11 years and trust me there have been challenges, COVID-19 just to name one. As many dispensers and front-of-house staff will know, the biggest hurdle was stock control, and so was tax payable, but with great advice from my accountant, I overcame my taxation problem.
I recently entrusted the help of Ms Joanne Scott-Dostine, a commercial manager for Optipro, with my stock control. Having been in the practice for more than 10 years, with no stock management plan, it is fair to say, my stock levels were not only out of control, but I also had no consistent price strategy. She helped me rein in my buying and create a pricing structure that myself and all staff now can follow.
I have just recently moved location, from renting to now owning. This was a decision not made lightly but am glad the opportunity arose. The premises I was renting came up for sale, having rented there for nearly 11 years and knowing not a lot of maintenance had been done, my husband and I decided against purchasing it. Instead, we found a store in much better condition and location. Talk about a challenge, relocating is just as hard as starting up a new store. Changing provider numbers, HICAPS information, internet, phone numbers, not to mention changing trade account details. We were closed for three weeks and spent every single day setting up. For ambitious optical dispensers wanting

to open their own store, here are some things to consider:
• Have a clear plan and budget, and stick to it. Changes will not only blow your budget but your timeline as well. You will need trusted tradespeople who know your time frame and are on board to have their part done in time for the next tradesperson to arrive.
• Talk to someone like Joanne from Optipro about a stock management plan; it will make the restocking process more seamless.
• I prefer dealing with other independent companies as stockists for frames and lenses. We share similar struggles and our relationships are a lot more personable.
• Have a trusted accountant, you will need their ongoing advice. Whether it be tax instalments or setting up companies or family trusts.
• Keep on learning, this will keep you ahead of the game and give you a point of difference against your competitors. I can’t stress how important it is to stay up to date with advances in technology and product enhancements. You can do this in so many fun ways like attending trade fairs run by the Optical Distributors and Manufacturers Association (ODMA) and WAVE in Western Australia. This will also give you the opportunity to mingle with like-minded people. Become an Optical
Dispensers Australia (ODA) member, allowing access to ongoing professional development, skill improvement and support.
Having been in small business for 11 years, Northam Optical is still reaching new heights.
Achieving a Cert IV in optical dispensing, which is no mean feat, has given me the confidence and knowledge to run my own business. I had years of practical experience before studying, but knowing the theory behind what we do is empowering. I encourage my staff to undertake the certificate, because I want my business to be the best it can be. I have never worked so hard in my life, but it has been the most rewarding thing I have ever done in my career. If you’re an optical dispenser, assistant or practice manager thinking about going into business for yourself, there will be highs and lows, you will put in a lot of hours – more than anyone you will ever employ – but it will be all worth it, because it’s all yours.
ABOUT THE AUTHOR: Allyson Caffell is a 45-year-old mum of three teenage girls and owner of Northam Optical, WA, dedicated to providing exceptional customer service to her patients.

The Government’s Aged Care Act 2024 is a welcome commitment to the country’s older citizens, but a lack of clarity about how the funding within it works remains a concern, writes Orthoptics Australia’s JANE COWAN.

“DELIVERING A CARE FUNDING FRAMEWORK THAT ENSURES ACCESS TO SPECIALISED VISION CARE FROM ORTHOPTISTS REDUCES THE RISK OF VISIONRELATED DISABILITY AND PROMOTES INDEPENDENCE AND SAFETY.”
As Australia’s population ages, the demand for healthcare services tailored to older Australians is rapidly increasing. Many older Australians, whether living independently or in residential aged care, rely on allied health services to maintain their health, independence, and quality of life.
Orthoptists, as highly trained allied health professionals, are critical in managing eye health, supporting those with age-related vision impairment and addressing neurological eye conditions resulting from stroke, brain injury, and neurodegenerative diseases.
Currently, government programs such as the Commonwealth Home Support Programme (CHSP) and Home Care Packages (HCP) provide funding for orthoptists to deliver essential eye health services, assistive technology, and home modifications to older Australians.
Orthoptics Australia (OA) supports the commitment made by the Australian Government with the adoption of the Aged Care Act 2024 to put the rights and needs of older people at the centre of the aged care system. However, in consultation regarding aged care funding reform, it remains unclear how older Australians will continue accessing vital vision services under reformed funding models.
Despite two-thirds of the 13 million Australians with low vision being over the age of 65, vision care has not been
explicitly included in the draft Aged Care Rules 2024 (service list).
This exclusion raises serious concerns about older Australians’ ability to access necessary vision services, like orthoptics.
Worryingly, the draft Aged Care Rules 2024 (service list) defines the Allied Health Professional as those registered under the National Law and does not acknowledge the many self-regulated allied health care professions.
The recently released Unleashing the Potential of our Health Workforce Scope of Practice Review, Final Report, identified that references to the National Law in legislation indirectly limits the scope of practice of highly trained allied health professionals, like orthoptists, to deliver health services in Australia, despite their adherence to high professional standards.
This oversight significantly limits the delivery of critical eye health services to older Australians.
Additionally, proposed legislation, such as the draft Residential Care Service List Consultation Discussion Paper (December 2024) only commits funding for facilitating access to allied health services, rather than covering the costs of service delivery.
This approach risks distancing government responsibility from funding essential allied health care. Without supported access to allied health, older Australians face diminished health outcomes and increased health care system costs.

The impact of vision loss on older Australians extends beyond individual health, affecting family, social connections, and overall well-being. Orthoptic services such as vision rehabilitation training empower individuals facing blindness, low vision, or significant vision impairment to regain independence and improve their quality
Case studies illustrate the transformative impact of orthoptic care.
A 74-year-old male with bilateral wet AMD regained the ability to read, communicate online, and engage in hobbies like woodworking
through orthoptic treatment and assistive technology.
His renewed independence allowed him to rejoin community groups, volunteer with family, and travel independently, reducing his reliance on depression medication and improving his emotional well-being.
Similarly, a 68-year-old stroke survivor experienced significant relief from dizziness and visual fatigue after orthoptic therapy.
He now moves freely around his home, enjoys meals with his family, and has reconnected with hobbies like gardening and reading.
The proposed aged care funding framework’s failure to demonstrate how older Australians will be supported to access orthoptic services leaves them at increased risk of further vision loss and associated disabilities, particularly in cases of progressive or newly diagnosed eye conditions.
Orthoptists are uniquely qualified to assess and prescribe assistive technologies, products, and home modifications that support older Australians with vision impairments. Delivering a care funding framework that ensures access to specialised vision care from orthoptists reduces the risk of vision-related disability and promotes independence and safety.
Orthoptics Australia looks forward to further consultation with government to clarify how aged care funding models can ensure older Australians receive vision care adequate for safeguarding their well-being, autonomy, and social engagement, ultimately enriching lives and strengthening communities.
THE
is
Australia’s executive officer. She has extensive experience in public policy with a passion for contributing to initiatives that deliver positive social impact.
Deliberately impersonating a patient is less common than other forms of identity theft but there have been reports of it in Australia. Why does it occur and how can practices mitigate this type of fraud?

“WHILE
FRAUDS MAY BE ELABORATE AND HARD TO DETECT, THEY CAN SIMPLY INVOLVE INDIVIDUALS TAKING ADVANTAGE OF BUSY PRACTICES AND INSUFFICIENT IDENTITY CHECKS.”
ack of access to affordable healthcare has been known to contribute to cases of impersonation in the US. In such cases, individuals may adopt a false identity to access healthcare or devices they cannot afford or prefer not to pay for.
In Australia, identity theft in healthcare often involves individuals stealing patient information to submit fraudulent insurance claims, obtain medical treatment, prescription medications or government benefits.
Motivations for impersonations or identity theft in healthcare may include:
• access treatments an individual has been refused, or fear they would be ineligible for
• avoid stigma if they fear a condition could affect their insurance, reputation, or professional opportunities
• a ccess personal information about the real patient to cause them further harm.
Whatever the impersonator’s reasoning, these frauds can harm both the person whose identity they stole and the practice involved. Consequences can include:
BELOW: Fraud victims in the US have faced major medical bills and endure years disputing debt collection and restoring credit ratings.
Financial harm – fraud victims in the US have faced medical bills totalling hundreds of thousands of dollars and endure years disputing debt collection and restoring credit ratings. Practices
may also face financial losses if required to reimburse insurers or patients and could become subject to audits and penalties.
Privacy breaches – if health providers are misled into sharing personal information, patients can be put at risk. For example, angry former partners have used fraud to locate a patient’s address. Practices involved in such breaches may face penalties under privacy laws, reputational damage and legal liabilities. Health risks - fraud could mean someone’s medical history is inaccurate and now includes information about the imposter. Victims of medical identity theft report experiencing misdiagnosis, treatment delays and even discrimination. Details including allergies or blood type could be incorrect and could lead to the patient themselves receiving inappropriate treatment or medication.
While frauds may be elaborate and hard to detect, they can simply involve individuals taking advantage of busy practices and insufficient identity checks. Reviewing your privacy and security processes may help avert a fraud.
Check you have clear processes for identifying patients and ideally use three approved patient identifiers (e.g. full name, date of birth and address). Remind staff why they need to confirm a patient’s identity at each visit.

Where family members share a Medicare or private health insurance card, check you are using the correct patient ID number on the card. This will help prevent honest mistakes as well as deception.
Check your processes for communicating with patients electronically to ensure you do not accidentally disclose information that could be used by an impostor. For more information Avant’s has developed a factsheet on email communication with patients.
Make sure staff consider patient privacy at the front desk and do not inadvertently disclose identifying information where it could be read or overheard.
Victims of identity theft can face years of work and anxiety to have their medical records cleared of their impostor’s information. If you become aware a patient’s records have been compromised, you will usually need to:
• C opy any of the impostor’s information into a new ‘unknown patient’ record. In this case it would be appropriate to delete inaccurate information in the real patient’s record after transferring it to the ‘unknown patient’ record or other location. Add a note explaining what happened. For more information see Avant’s resources on correcting records.
• N otify the real patient as appropriate if they are unaware of the issue, and keep them informed.
• C ontact any other providers if you have provided reports or referrals. Also cancel any prescriptions and follow the procedures for reporting prescription fraud in your state.
• C ontact Medicare. You may also have to reverse the billing for the consultation.
Private health insurers may also need to be notified, as the practice may need to reverse any claims submitted for the impersonator’s treatment. Failure to do so could result in penalties or further audits.
• C onsider whether you also notify the Office of the Australian Information Commissioner (OAIC) and/or contact police. For further information see Avant’s resources on Responding to a data breach.
Addressing identity fraud not only supports your patients but also demonstrates your commitment as an individual practitioner and as a practice to safeguarding personal and health information and ensuring compliance with legal requirements.
Always prioritise your team’s personal safety. Evaluate the situation and consider carefully before directly confronting the imposter.

coffee shop most mornings, where MAMILs (middle-aged men in Lycra) review the details of their latest bike ride using apps like Strava, receiving immediate and detailed feedback. Similarly, school and university students undergo regular testing, and many of us rely on smartwatches that provide intricate data on our health and even our sleep patterns. These are all forms of audit – seamlessly collecting real-time data on our daily activities to enhance well-being.
However, audit is less embedded in our professional lives. Unlike cyclists, students, or smartwatch users, clinicians and surgeons do not receive immediate and seamless feedback on their work. Why, for instance, don’t we have real-time feedback for cataract surgery outcomes? Surely, these are at least as important as cycling performance, academic progress, or sleep quality.
Clinical audit is defined as a focused review aimed at assessing and improving a clinician’s practice by comparing performance against established standards or guidelines, identifying areas for improvement, and implementing changes to enhance patient care and outcomes. It should be a routine part of our practice, seamlessly integrated into daily operations.

security. Outcomes in our field are generally excellent, with complications being rare. As one senior academic ophthalmologist once told me, “I don’t need to know my cataract surgery results; I already know they’re good!” However, low complication rates do not mean there’s no room for improvement. Clinical audit challenges us to make excellent results even better.
Our professional body’s continuing professional development (CPD) requirements include a clinical audit component. Yet, barriers to widespread adoption of high-quality audits persist. Audit can be onerous and time-consuming, and the process may feel confronting.
A colleague once expressed concerns, asking, “What if my results are bad? Will knowing them increase my stress and negatively impact my performance? What if I’m not as good as I think I am?”
To overcome these challenges, audit in our professional lives should be engaging and approachable, not burdensome. It should go beyond the minimum required for CPD compliance. We must also avoid the pitfalls seen in the US where individual surgeons’ results are publicly available online, effectively creating a league table. In such systems, surgeons may avoid difficult cases to protect their statistics. In some Australian specialties, surgeons are obligated to report their results and face actions against outliers. While these measures aim to improve accountability, they may compromise reporting accuracy
surgeons – that is the role of the Australian Health Practitioner Regulation Agency (Ahpra). Instead, it should be driven by motivation, not fear. To ensure clinical audit is seamless, it must integrate naturally with routine patient care. Data, such as visual acuity measurements, should be entered into an intuitive electronic medical record (EMR) system with fields designed to maintain data integrity. An automated query can then aggregate the clinician’s data, allowing performance comparisons against established standards or guidelines. Crucially, clinicians must have confidence in the privacy and security of their data. Audit should never devolve into a competition among peers. We all take great pride in our work. Clinical audit should reflect this, be an embraced part of patient care and facilitated by modern EMRs. Are we up to the challenge?
Conflict of interest: I'm a Strava-using MAMIL, frequently spotted at a cafe in Melbourne’s inner north on Sunday mornings.
Name: Dr Ben Connell
Qualifications: FRANZCO MPH
Affiliations: Cataract, refractive, and corneal surgery at Eye Surgery Associates, Melbourne; consultant on the Corneal Unit at the Royal Victorian Eye and Ear Hospital.
Location: M elbourne
Years in industry: 25
WE MUST ALSO AVOID THE PITFALLS SEEN IN THE US WHERE INDIVIDUAL SURGEONS’ RESULTS ARE PUBLICLY AVAILABLE ONLINE ... IN SUCH SYSTEMS, SURGEONS MAY AVOID DIFFICULT CASES.

100% OPTICAL
London, UK
1 – 3 March 100percentoptical.com
ODA INTERNATIONAL CONFERENCE
Sydney, Australia
7 – 8 March odamembers.com.au
2025
ASIA-PACIFIC ACADEMY OF OPHTHALMOLOGY CONGRESS
New Delhi, India
3 – 6 April 2025.apaophth.org
2025
ARVO 2025
Utah, US
4 – 8 May arvo.org/annual-meeting
INTERNATIONAL ORTHOPTIC CONGRESS
Brisbane, Australia
27 – 29 June ioc2025.com.au
ODMAFAIR25
Sydney, Australia
27 – 29 June odma.com.au
ASIA-PACIFIC STRABISMUS AND PAEDIATRIC OPHTHALMOLOGY SOCIETY CONGRESS
Brisbane, Australia 29 June – 1 July apspos.org/apspos-congress-2025

AUSCRS 2025
Darwin, Australia 16 – 19 July auscrs.org.au/2025-conference
SILMO PARIS
Paris, France 26 – 29 September silmoparis.com/en
RANZCO CONGRESS
Melbourne, Australia 14 – 17 November ranzco2025.com

I came to Specsavers originally for more career opportunity. At the time I was working for another company mainly edging and fitting lenses but it was hard to see myself doing much more than these everyday tasks. At Specsavers I saw there would be more opportunities for progression within stores and also the option to become a partner in my own store which was really what attracted me to the business.
WHAT WAS YOUR FIRST ROLE WITHIN THE BUSINESS?
My first role with Specsavers was at the Cranbourne store as a dispenser. There was a wealth of knowledge across the team when I began, as most staff at the store had worked in optics for years so it was a great environment to fill any knowledge gaps I had. My original tasks were mainly dispensing glasses to patients, fitting glasses to patients on collection, as well as other everyday tasks including unpacking deliveries, calling customers and other general customer service activities.

WHAT GROWTH OPPORTUNITIES HAVE PRESENTED THEMSELVES?
I have been given amazing opportunities to learn and grow throughout my journey with Specsavers. At my first store, I had an amazing mentor who allowed me to take on responsibilities and trained me up to eventually move into a management role. He also allowed me to take part in the Pathway Program which gave me the skills and tools to be a successful partner in my own business. Since taking on my own store, I have completed my Cert IV in optical dispensing and have also taken part in numerous leadership development programs which are all made available through Specsavers.
WHY DID YOU PURSUE A DISPENSING CAREER?
I pursued a career as a dispenser mainly due to my own eye condition. I was diagnosed with keratoconus at age 11 and that sparked my initial interest in the optical field. This interest grew as I got older.
WHAT IS YOUR MOST INTERESTING DISPENSING CASE?
There’s been so many interesting cases over the years but one that stands out is a patient who required +21.00 lenticular lenses. The prescription made frame selection a challenge, but we were able to find something that the patient was really happy with.
WHAT ADVICE WOULD YOU OFFER TO SOMEONE CONSIDERING A CAREER AS AN OPTICAL DISPENSER?
Do it. It is such a rewarding, dynamic job where you can genuinely change peoples’ lives for the better. One of the best feelings is seeing the excitement patients get when we fit them with their new spectacles. It can sometimes feel like it’s not significant, but the truth is we make a huge difference to all of our patients’ day to day lives. At Specsavers, we have the expertise, systems, and brand presence that allows us to care for a high volume of patients which means the impact you can have is huge.
WHAT EXCITES YOU MOST ABOUT TURNING UP FOR WORK EACH DAY?
The team environment we have with our team, the people I work with and knowing the difference we make to people’s lives. I really love developing my team to hopefully create our next set of leaders within the industry.
Joint Venture Partnership Opportunities – New Stores in Australia and New Zealand! Specsavers is offering an exciting opportunity for Optometrists ready to advance their careers by becoming Joint Venture Partners at multiple new stores across Australia and New Zealand. These stores will be a new site, offering the latest advancements including optical test rooms, pre-test rooms, dispensing desks, state-of-the-art equipment including OCT, and showcasing the latest Specsavers fit out with digital displays and illuminated shelving. Successful applicants will receive Specsavers’ award-winning support in building up their business, including team recruitment support and end-to-end financing on new stores.
Full-Time Experienced Optometrist Opportunity – Specsavers Dubbo, NSW
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Carly Parkinson on +61 (0) 478 201 057 or E carly.parkinson@specsavers.com
Optometrist employment enquiries: Specsavers Recruitment Services anz.srsdepartment@specsavers.com
Locum employment enquiries: ANZ.locumteam@specsavers.com
Graduate employment enquiries: apac.graduateteam@specsavers.com
In the heart of the beautiful Macquarie Valley, Dubbo is a vibrant regional city on the banks the majestic Macquarie River. We have a great opportunity for an experienced optometrist to join our four-test room store, offering market-leading equipment, including OCT free of charge for every patient. Collaborate with a team of 5 optometrists, focusing on pathology, chronic disease management, and therapeutics. Benefit from regular, in person CPD events, providing opportunities for ongoing learning and skill enhancement to collaborate with local ophthalmologists to co-manage patients, ensuring comprehensive and holistic care along with excellent career development opportunities, including Pathway to Partnership.
Optometrist opportunity – Specsavers Hastings, NZ
We’re seeking a dedicated, full-time Optometrist to join our team in Hastings, New Zealand. Enjoy a supportive, dynamic environment with competitive pay and professional development opportunities. If you’re passionate about eye care and providing exceptional patient service, we’d love to hear from you. Apply now to start your next career chapter!
Locum Opportunities
Looking for extra weekend work? Specsavers stores across our Newcastle and Central Coast regions have fantastic locum opportunities available. If you’re interested and would like more details, please don’t hesitate to get in touch with our Specsavers locum team. We’d love to hear from you!
Graduate Opportunities
Looking at starting your career with a dedicated mentor to support your development as you step into the Optometry world? Specsavers have a few final positions available across Australia and New Zealand with some exciting incentives in place to help kick start your career. To discuss these opportunities and find out more, please contact your Graduate Recruitment Consultant or email anz.graduateoptometry@specsavers.com.
INSIGHT'S MONTHLY BULLETIN TO KEEP THE AUSTRALIAN OPHTHALMIC SECTOR UPDATED ON NEW APPOINTMENTS AND PERSONNEL CHANGES, NATIONALLY AND GLOBALLY.

Dr Shivanand Sheth has formally commenced in the role as head of the Ocular Motility Unit at the Royal Victorian Eye and Ear Hospital. It’s the only strabismus clinic in Australia providing medical and surgical management for patients of all ages with simple to complex ocular motility problems such as strabismus, nystagmus and diplopia.
“I aim to ensure that the Ocular Motility Clinic continues to be a centre of excellence for patient care and also remains a destination of choice for the brightest ophthalmologists around the world to undertake a fellowship in this amazing ophthalmic sub-specialty,” he said.

Ms Jaselle Muscat has recently taken on an expanded role as head of human resources – retail and optics at Specsavers. With nearly a decade of experience at Sthe company, she will be working closely with the people director, with her expanded responsibilities allowing her to continue to lead and shape the people plans across Australia and New Zealand "to ensure Specsavers remains an employer of choice in the competitive retail and optics landscape".

J&J PROMOTES FROM WITHIN FOR REGIONAL SALES MANAGER ROLE
Johnson & Johnson Vision Care has announced Mr Hirdesh Nair's transition to regional sales manager for VIC/TAS, SA, NZ, WA, effective January 2025. His six-year tenure as professional development manager has seen him drive key initiatives like JNJVISIONPRO and significant contributions to product launches and industry engagement. "His experience and leadership will continue to elevate ACUVUE's market impact," the company said.

A/Prof Amanda French is an academic and researcher in orthoptics and has been appointed as head of UTS Orthoptics. In the role since May 2024, she has a clinical background in orthoptics, a Graduate Certificate in Educational Studies and a PhD on the Epidemiology of Childhood Refractive Errors from the University of Sydney. She has been course director and responsible academic officer teaching and learning for the Master of Orthoptics course in the Graduate School of Health at UTS since 2014, and previously an academic in orthoptics at the University of Sydney.

Vision Eye Institute has welcomed Dr Nishan Ramachandran to its Brisbane clinic. He is an internationally trained ophthalmologist and vitreoretinal surgeon. He specialises in cataracts, medical retina, vitreoretinal surgery and general ophthalmology and has extensive experience in retinal laser, all types of intravitreal injections and complex retinal detachment care. Dr Ramachandran is fluent in Tamil as well as English.

Prof Kathryn Rose was head of discipline (orthoptics) at the University of Sydney and her current appointment at the University of Technology Sydney (UTS) commenced in 2014, where she established a new school for orthoptics education in NSW. After retiring in March 2024, she is now Adjunct Professor at the UTS Graduate School of Health, working with several national and international research groups as a leading international researcher on the development of vision and refractive errors in children and adolescents.









Acetylcholine
Acetylcholine
Latex