Recommendations for Maine’s Transition to a State-Based Marketplace

PREPARED FOR Commissioner Jeanne Lambrew
Megan Garratt-Reed
Katherine Fritzsche
Maine Dept. of Health and Human Services
PROJECT ADVISORS
Heather Howard
Dan Meuse
AUTHORS
Danielle Beavers
Kishan Bhatt
Molly Brune
Alice Chang
Riley Edwards
Marissa Korn
Mark Lee
Kevin McCarthy
Nabil Shaikh
Martin Sweeney
Joseph Tso
Clarke Wheeler
JANUARY 2021
TABLE OF CONTENTS | 1 Table of Contents Acknowledgments ....................................................................................... 3 Acronyms ....................................................................................................... 4 Executive Summary ..................................................................................... 5 Introduction ................................................................................................... 7 Background ................................................................................................... 8 Methodology ............................................................................................... 13 Health Equity Approach ............................................................................ 15 Broad Recommendations .........................................................................17 Enrollment Periods .................................................................................... 22 Displaying Clear Choice Plans ................................................................. 29 Auto-Renewal ............................................................................................. 36 MaineCare Integration .............................................................................. 44 Planning for the Future ............................................................................. 53 Conclusion .................................................................................................. 57 Endnotes ..................................................................................................... 58 Appendices ................................................................................................. 66 Author Biographies.................................................................................... 72
Photo

Credits: David Anderson
Cate Bligh Katie Burkhart
Benjamin
Zachary Edmunson Tyler Finck James Fitzgerald Donald Giannatti Inera Isovic Antoine Julien Keith Luke Karl Magnuson Aubrey Odom Mark Olsen Evan R
Rascoe Shadman Sakib Stephen Walker Russ Ward
Acknowledgments
This report was prepared by Master in Public Affairs students at Princeton University’s School of Public and International Affairs. This report incorporates information gathered through students’ independent research, remote interviews conducted between October 11 and November 30, 2020, and invaluable guidance from course instructors Heather Howard and Dan Meuse. The report fulfills the Princeton School of Public and International Affairs’ degree requirements for an immersive policy workshop and associated policy proposal. We are especially grateful to our partners in the Maine Department of Health and Human Services that enabled us to conduct research and make recommendations on this important topic, particularly to Commissioner Jeanne Lambrew, Meg Garratt-Reed, and Kate Fritzsche. We also wish to extend our gratitude to the many policymakers, health professionals, consumer advocates, and subject matter experts who shared their perspectives with us throughout the course of this project. We particularly appreciate their willingness to spend time with us in the midst of the coronavirus pandemic. We hope that this report will contribute to Maine’s potential transition to a state-based marketplace.
Maine Stakeholders
Jeffrey Austin, Maine Hospital Association
Mohamud Barre, Maine Access Immigrant Network
Dan Cohen, Office for Family Independence
Dan Colacino, Maine Association of Health Underwriters
Hillary Colcord, Maine Primary Care Association
Allison Conroe, Maine Mobile Health Program
Stacy Dostie, Maine Association of Health Underwriters
Kathryn Ende, Consumers for Affordable Health Care
Karynlee Harrington, Maine Health Data Organization
Katie Harris, MaineHealth
Peter Hayes, Healthcare Purchaser Alliance of Maine
Marge Kilkelly, Maine Primary Care Association
Kathy Kilrain del Rio, Maine Equal Justice
Barbara Leonard, Maine Health Access Foundation
Patty Lovell, Western Maine Community Action
Kevin Lewis, Community Health Options
Sarah Lewis, Maine Access Immigrant Network
Steven Michaud, Maine Hospital Association
Kristine Ossenfort, Anthem
Anthony Pelotte, Office for Family Independence
Tom Perrey, Maine Association of Health Underwriters
Michelle Probert, Office of MaineCare Services
Trish Riley, National Association for State Health Policy
Lisa Sockabasin, Wabanaki Public Health
Molly Slotznick, Office of MaineCare Services
Lisa Talpert, Maine Mobile Health Program
Bob Wake, Maine Bureau of Insurance
David Winslow, Maine Hospital Association
Bill Whitmore, Harvard Pilgrim
Ann Woloson, Consumers for Affordable Health Care
External Stakeholders
Emily Brice, Northwest Health Law Associates
Stan Dorn, Families USA
Tekisha Everette, Health Equity Solutions
Michael Miller, Community Catalyst
Dustin Palmer, Code for America
Kevin Patterson, Connect for Health Colorado
Eva Marie Stahl, Community Catalyst
Marissa Woltmann, Massachusetts Health Connector
ACKNOWLEDGEMENTS | 3
ACA Patient Protection and Affordable Care Act
APTC Advance Premium Tax Credit
AV Actuarial Value
BOI Bureau of Insurance
CSR Cost Sharing Reduction
DHHS Maine Department of Health and Human Services
FFM Federally-Facilitated Marketplace
FMAP Federal Medical Assistance Percentage
FPL Federal Poverty Level
OEP Open Enrollment Period
OFI Maine Office for Family Independence
OMS Office of MaineCare Services
QHP Qualified Health Plan
SBM State-Based Marketplace
SBM-FP State-Based Marketplace on the Federal Platform
SEP Special Enrollment Period
4 | ACRONYMS
Acronyms
Executive Summary
Maine’s potential transition to a state-based marketplace (SBM) presents an opportunity to expand coverage and increase affordability for health care consumers in Maine. This report explores these opportunities and provides policy recommendations to advance these goals.

Under the Affordable Care Act (ACA), states can implement their own health insurance marketplaces for the individual and small-group markets, which provide states greater flexibility and independence than using the federally-facilitated marketplace (FFM) on Healthcare.gov. Prior to November 2020, Maine’s participation in the FFM exposed the state to the Trump administration’s shortening of open enrollment periods (OEPs), funding cuts to outreach and enrollment efforts, and the refusal to create a special enrollment period (SEP) for the coronavirus pandemic.
In March 2020, Governor Janet Mills signed the Made for Maine Health Coverage Act (H.P. 1425) authorizing the development of an SBM in Maine.1 This report explores the opportunities associated with a potential marketplace transition, informed by over 30 interviews with stakeholder groups across Maine in the fall of 2020. Through this work we learned that the transition to an SBM has the potential to close cover-
age gaps, enhance outreach to groups that have been historically marginalized in the health care system, and improve population health.
This report also applies a framework of targeted universalism throughout its analysis. This goal-oriented mode of equity analysis informs many recommendations focused on making health care accessible and affordable to all Mainers, particularly those historically marginalized by the health care system.
Broad Recommendations
In addition to our below recommendations on specific topics, our interviews and research led us to make the following overarching proposals, which should guide the overall transition to an SBM and ensure that consumer engagement and support is at the core of the transition.
1. Increase consumer assistance capacity.
2. Integrate consumer engagement into the process of designing and implementing Maine’s SBM.
3. As a longer-term initiative, re-establish the Maine Office of Health Equity and empower its staff to coordinate equity efforts across the SBM, the MaineCare program, and all Department of Health and Human Services (DHHS) Offices.
EXECUTIVE SUMMARY | 5
Specific Recommendations
Using information gathered in our research and interviews, we analyze several policy options pertaining to topics that Maine’s DHHS asked our team to explore. In particular, we were tasked with identifying opportunities for reducing complexity for consumers and improving overall enrollment and affordability. We
Enrollment Periods
employ a decision matrix that assesses these policy options for their consumer impact and state feasibility. Based on this analytical framework, we propose the recommendations listed below to guide the implementation and achieve the promise of an SBM.
• Establish an OEP that runs until January 31, so the period lasts a total of 92 days.
• Implement SEPs for public health crises, for individuals who become pregnant outside of open enrollment, and for uninsured tax filers beginning the day that their state tax return is filed.
• Explore options for an SEP directly after the OEP for Mainers who had valid reasons to miss the OEP deadline.
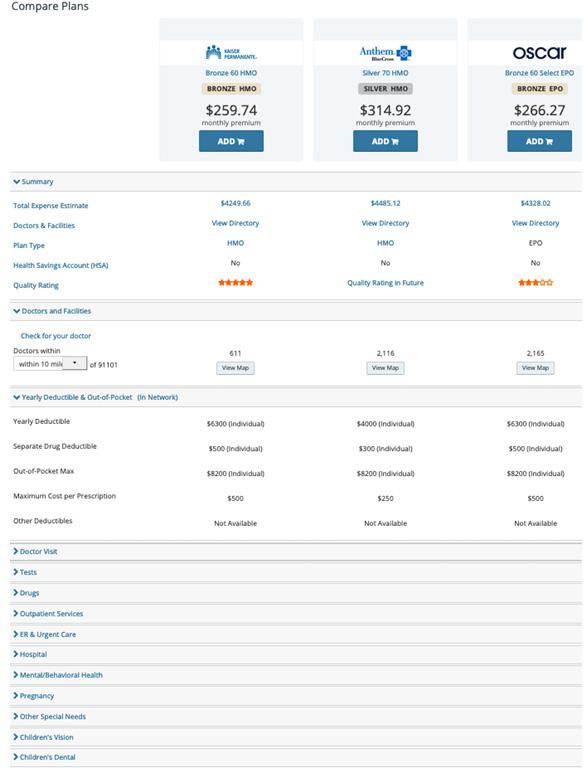
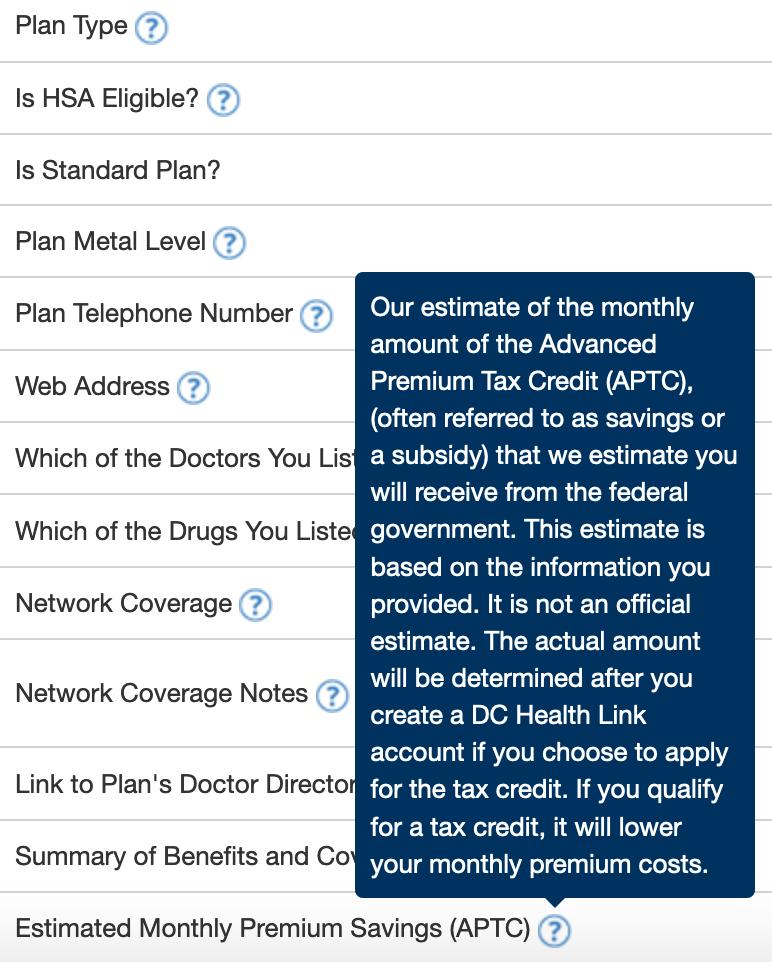
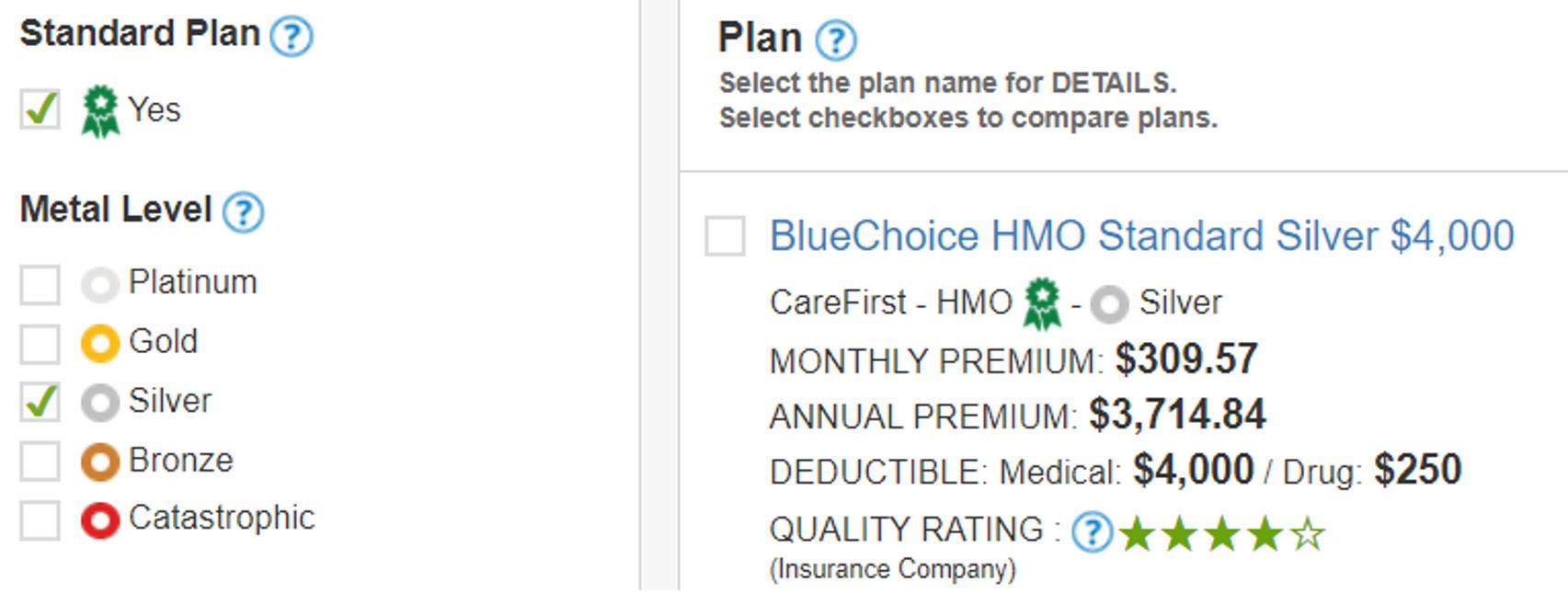
Displaying Clear Choice Plans
• Use an intake questionnaire and display plans based on responses.
• Build a comparison tool that: (1) automatically highlights differences between selected plans, and (2) includes a “Compare to Other Standard Plans” function.
• Include a pop-up glossary feature when customers hover over a technical term, and enable screen reading audio capability for accessibility.
• Distinguish Clear Choice plans with naming, visual cues, sorting, and/or filtering.
Auto-Renewal
• Design more consumer-friendly auto-renewal notices.
• Set the default for consumers eligible for cost-sharing reductions to high-value silver plans.
• Auto-renew consumers with discontinued plans into Clear Choice plans.
• Explore using auto-renewal defaults to incentivize carriers to lower costs.
• Consider allowing consumers to choose their auto-renewal priorities.
MaineCare Integration
• Use existing state data to target and personalize outreach to facilitate enrollment.
• Resolve consumer-facing bottlenecks in MaineCare and SBM enrollment.
• Embed the Office for Family Independence (OFI) in the policy planning and SBM implementation process, given their responsibility for determining MaineCare eligibility.
Planning for the Future
• In the procurement, implementation, and maintenance of the SBM eligibility and enrollment system, prioritize platform capacity to adjust the inputs for the rules engine to adapt to federal policy innovations and changes.
6 |
EXECUTIVE SUMMARY
Introduction
In recent years, the State of Maine has taken several steps to embrace the ACA and expand health care access for its residents. Since taking office in January 2019, Governor Janet Mills has implemented Medicaid expansion2 and enshrined into state law the consumer protections outlined in the ACA.3
The OEP beginning November 2020 marked Maine’s shift to a state-based marketplace on the federal platform (SBM-FP) for private health insurance. This move away from the FFM aims to improve the State’s ability to develop a marketplace more responsive to the needs of Mainers.

DHHS requested our assistance in identifying important considerations for Maine’s potential transition to a full SBM, where the State would be responsible for operationalizing both outreach to Mainers and the enrollment platform, including a website, for marketplace insurance.
In this report, the Background section outlines Maine’s health care landscape and addresses challenges and opportunities associated with an SBM transition. Next, the Methodology section outlines our approach for identifying and evaluating policy options, examining each along dimensions of consumer impact and state feasibility. This is followed by a section on our Health Equity Approach describing the equity framework central to our analysis. Our Broad Recommendations section follows, drawing on themes that arose consistently in interviews and presenting cross-cutting proposals that center and support consumers while complementing many of the topic-specific recommendations we make.
After the broad recommendations, we delve into recommendations on specific topics that DHHS identified as areas of consideration for designing a potential SBM. The policy areas that we developed and evaluated are briefly described below.
• Enrollment Periods: Would flexibility to expand the OEP and SEPS help achieve state enrollment and affordability goals?
• Displaying Clear Choice Plans: How can Clear Choice plans be best displayed to maximize their impact?
• Auto-Renewal: Would changes to automatic re-enrollment (“auto-renewal”) policies help achieve state enrollment and affordability goals?
• MaineCare Integration: How could an SBM transition improve the integration between the marketplace and MaineCare?
• Planning for the Future: How can a potential SBM transition best be designed to take advantage of future federal policy making?
The authors of this report are 12 graduate students at Princeton University’s School of Public and International Affairs, and this report is prepared for the capstone project of the Master in Public Affairs program. This report is informed by secondary research as well as interviews with stakeholders across the state conducted throughout the fall of 2020. The research also benefited from the guidance of the course’s co-instructors: Heather Howard and Daniel Meuse, two national health care policy experts who lead the State Health and Value Strategies program of the Robert Wood Johnson Foundation, located at Princeton University.
INTRODUCTION | 7
The State of Maine has had two particularly significant health care policy developments since Governor Mills took office: the implementation of Medicaid expansion in 2019, and the ongoing transition towards an SBM. Both developments stem from the flexibilities granted to states in the passage of the ACA ten years ago. By financing state expansions of Medicaid eligibility, establishing health insurance marketplaces, and providing subsidies for individuals with qualifying incomes seeking health insurance on those marketplaces, the ACA’s implementation has had a significant impact on the accessibility of health insurance for millions of Americans.
The ACA presents states with a number of decisions around marketplace structure and oversight of Qualified Health Plans (QHPs). In essence, states can decide between operating and overseeing their own SBM or relying on the federal marketplace and its rules governing QHPs. SBMs provide states with significantly greater flexibility and autonomy regarding health insurance marketplace management.
This section first presents an overview of the national context and recent developments for Maine’s marketplace and MaineCare. Next, we describe key demographic characteristics of Maine’s overall population and of marketplace and MaineCare enrollees. Finally, we outline a number of the reasons that states pursue SBMs and the challenges that an SBM transition entails.
Marketplaces
Fourteen states and Washington, DC currently operate SBMs. Thirty states remain on the FFM, and six states operate an SBM-FP—Maine being a recent addition to this latter group, as of the OEP beginning November 2020. SBM-FP states continue to utilize HealthCare. gov’s technology platform and call centers but assume responsibility for certain marketplace activities, including plan management and oversight, consumer outreach, and marketing.
Nevada’s SBM launch in 2019 marked the first migration of a state to an SBM from an SBM-FP or the FFM since 2014.4 New Jersey and Pennsylvania have since followed suit, launching SBMs in November 2020.
In March 2020, Governor Mills signed legislation that formally established the Maine Health Insurance Marketplace, enabling the State to transition to an SBM-FP and to explore the feasibility of establishing its own SBM.5 DHHS is responsible for leading this exploration phase and would oversee SBM operations.
In August 2020, Maine submitted a blueprint application to the Centers for Medicare and Medicaid Services (CMS), confirming its goals to adopt an SBM-FP for plan year 2021 (i.e., by November 2020) and an SBM for plan year 2022 (i.e., by November 2021).6
In October 2020, Maine issued a request for proposal (RFP) for technology and call center partners to set up and operate an SBM.7 At the time of this writing, Maine has identified vendors and is currently in negotiations to finalize contract terms.8
In November 2020, the State officially transitioned to the SBM-FP. Like other states, Maine is funding these operations via 0.5% user fees charged on the premiums of plans sold on the marketplace (in addition to the 2.5% user fees which the federal government charges in partnership models).9
Medicaid Expansion
Court rulings since the ACA’s implementation have further opened up state flexibilities in health care provision. In particular, the Supreme Court’s ruling in NFIB v. Sebelius made Medicaid expansion optional for states.10 As of November 2020, Medicaid expansion has been adopted by 38 states and Washington, DC.11 Oklahoma and Missouri plan to implement their adopted expansion in July 2021.
After Maine voters approved Medicaid expansion by ballot initiative in 2017, former Governor Paul LePage refused to implement the expansion, which was set to take effect in July 2018.12 In January 2019, Governor Mills instructed DHHS to implement Medicaid expansion, retroactive to July 2018.13 As of December 2020, about 67,500 Mainers14—one in four MaineCare members,i and one in twenty Mainers—were enrolled in coverage through the expansion group.ii
i Nearly 237,000 individuals were enrolled in MaineCare or CHIP as of August 2020.That same month, DHHS estimated that nearly 60,000 were enrolled through expansion. Source for total enrollment: Center for Medicare and Medicaid Services.“August 2020 Medicaid & CHIP Enrollment Data Highlights.” https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html. Source for expansion enrollment: Maine Department of Health and Human Services. MaineCare (Medicaid) Update: August 3, 2020. https://www.maine.gov/tools/whatsnew/index.php?topic=DHHS-MAINECARE-UPDATES&id=3010756&v=article ii Expansion increased the eligibility threshold for parents from 105% of the federal poverty level (FPL) to 138% FPL and made most other adults with incomes up to
8 | BACKGROUND
Background
At the same time, Medicaid expansion has accelerated changes in Maine’s individual market. For plan year 2019, about 71,000 Mainers—one in nineteen statewide—enrolled in a marketplace plan. In plan year 2020, this number dropped to roughly 62,000 Mainers, or one in twenty-two statewide, likely due to Medicaid expansion.15
The coronavirus pandemic and corresponding economic downturn has led to significant increases in Medicaid enrollment nationwide and has placed enormous fiscal pressure on state finances.16 Maine is no exception to this trend. By taking advantage of generous federal match payments available for the Medicaid expansion population, the State has succeeded in enrolling over 20,000 Mainers into expansion-group coverage since early March.17
Demographics
Governor Mills articulated a goal of making affordable health care available to more Mainers when she laid out plans for a potential SBM transition in August 2019.18 This section presents statistics on Maine’s marketplace consumers, uninsured residents, and broader population, to provide context for the challenges of increasing enrollment and affordability.
Broader Population
Many of the stakeholders we interviewed highlighted Maine’s unique demographics and geography as relevant to its health care landscape.
Geography: Maine is a large state by area—larger than all other New England states combined.19 Its population is also rural: 40% of Mainers live in rural counties.20 These factors are relevant for a number of reasons. Rural areas tend to have higher premiums than urban areas21 and often lack enough physicians. Maine ranks second nationally for the number of primary care doctors in rural counties (99.5 per 100,000), nearly double the national rate for rural counties, but rural residents still find there are too few geriatricians.22 Many Mainers living in rural areas lack internet access: in 2018, an estimated 90% of Mainers had a smartphone or computer, but only 85% had internet access at home via those devices.23 Additionally, 83,000 Mainers had no access to the internet.24 Many Mainers in rural areas therefore rely on in-person or phone interactions to enroll (or
get assistance enrolling) in health coverage, and those that utilize in-person services may face long journeys to access them.
Age: Maine’s population has the oldest median age of any state in the US, and 23% of its residents are aged 5064 (compared to the national average of 19%).25 Since older residents face higher health care costs, Mainers are more likely to struggle to pay for the health care they need.These issues are exacerbated by higher rates of disability in Maine (16%, compared to the national average of 13%).26
Race, ethnicity, and language: 93% of Maine residents are non-Hispanic white (compared to the national average of 60%). Only 6% of residents speak a language other than English at home (compared to the national average of 22%).27 This can pose challenges for Mainers that do not identify as white: language and cultural barriers may present obstacles for accessing coverage.
Income: Maine has the lowest median household income in the Northeast.28 Disparities also exist within the state, with the poverty rate in the state’s rural areas 3.4 percentage points higher than in urban areas.29
Survey data suggests Mainers with low- and middle-incomes postpone needed treatments and ration prescriptions due to high health care costs in Maine.30
Marketplace Consumers
Data from plan year 2020 published by CMS sheds light on Maine’s marketplace consumers and the types of plans they select.
• 51,400 applications for coverage were submitted, covering 77,700 individuals.iii
• 8,200 individuals were assessed as eligible for MaineCare/CHIP and referred for OFI for determination.
• About 62,000 Mainers enrolled on the FFM for 2020 coverage.
• 84% of consumers were eligible for financial assistance.iv
• 82% of consumers who were enrolled in a marketplace plan for plan year 2019 re-enrolled for 2020.
• 61% of individuals enrolled in coverage on or after December 8. 25% of consumers auto-renewed their coverage, and this figure likely includes many such consumers.
138% FPL newly eligible. According to DHHS, as of December 2020, 84% of the currently enrolled expansion group is this latter group of adults without children or caretaking responsibilities.
iii Numbers presented in this section are rounded to the nearest hundred. Percentages are rounded to the nearest whole number; the denominator is the number of enrollees (62,031). Enrollees are referred to as consumers in this section.
iv APTCs or CSRs
BACKGROUND | 9
• Average monthly individual premiums after factoring in advance premium tax credits (APTCs) were $176 (compared to a sticker price of $642).
• One-third of consumers were aged 55 to 64. Another one-third were aged 35 to 54.
• 55% of consumers were from rural ZIP codes.
• 9,200 consumers (15%) had household incomes between 100% and 150% FPL. This was down from 15,900 consumers in plan year 2019.v 13,400 consumers (22%) had incomes between 150% and 200% FPL.
Uninsured Residents
Approximately 106,000 civilian noninstitutionalized Mainers were uninsured in 2019.31 Of those uninsured, about 29,000 had household incomes less than 138% FPL and about 55,500 had household incomes between 138% and 400% FPL. A significant proportion of uninsured Mainers are thus likely eligible for either MaineCare or subsidized marketplace coverage.
Appendix Table 2 presents uninsured rates by demographic group. Adults under age 34, men, and nonwhite populations—particularly American Indian and Alaska Natives—are more likely to be uninsured than older adults (aged 35-64), women, and non-Hispanic white people, respectively.
Health Equity
In every interview, stakeholders spoke about the rurality and age of Maine’s population. These factors contribute to health disparities, which are more pronounced with limited provider access, low population density, and high health care needs. SBM policies to address these disparities affect many Mainers, but especially historically marginalized groups.
The groups most commonly discussed in our stakeholder conversations were:
• People with limited English proficiency, who represent 1.5% of Mainers.32 Languages with more than 1,000 native speakers in Maine include Spanish, French (including Patois and Cajun), Chinese (including Cantonese and Mandarin), and Cushite.33
• Immigrants, who represent 3.6% of Mainers.34 Nine out of ten report speaking English well, over a third have a college degree, and more than half are naturalized citizens.35 However, the nature of their work makes them less likely to have employer-sponsored insurance; in 2018, 2,368 immigrant business owners accounted for 2% of all self-employed Maine
residents.36 Lawfully present immigrants ineligible for MaineCare due to their immigration status may be eligible for APTCs or cost-sharing reductions (CSRs), even if their income is below the FPL.37
• Black Mainers, who represent 1.7% of residents.38 Almost half are immigrants, the highest share in the nation, from nations including Somalia and the Democratic Republic of Congo.39 The latest five-year estimates, for 2014-2018, show the rate of poverty for Maine children who are African American or Black at 46%, down from 53% for the five-year period ending in 2017. This rate is more than three times as high as the rate for non-Hispanic white children (15% in poverty) and nearly twice as high as that of Hispanic children (24% in poverty).40
• Migrant farm workers, who make up 62% of hired farmworkers in Maine. Eighty-three percent of migrant workers are foreign-born.41 A 2015 survey by the Maine Department of Labor found that 56% of migrant farmworkers were born in Mexico, 17% were born in the U.S., 10% were born in Haiti, and 8% were born in Canada.42
• Wabanaki Mainers, who represent 0.7% of the population.43 Their life expectancy is 54 years, considerably less than the 78-year life expectancy for the general population.44
Reasons to Build an SBM
Flexibility: SBMs offer greater flexibility to state governments, including more control over marketing funding, open enrollment timelines, SEPs, and health equity efforts.45 SBMs can also offer additional state-funded subsidies to improve plan affordability and increase marketplace enrollment, as Massachusetts, Vermont, California, Colorado, and New Jersey do.46 Greater autonomy additionally allows SBM states to experiment with display features that improve the consumer experience, such as default orders, search filters, and comparison tool designs. DHHS recently noted in a public announcement that “operating a State platform provides greater flexibility and opportunities to customize the Marketplace to Maine’s needs.”47
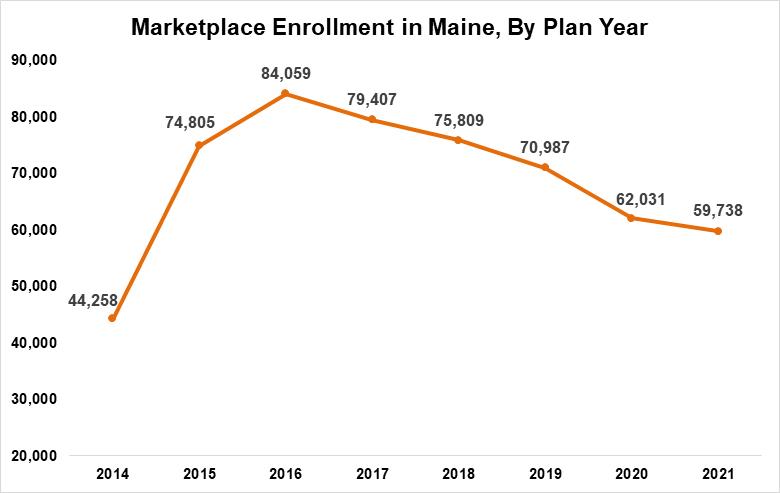
Protection: SBMs have some insulation from federal funding cuts and enrollment period restrictions, which have been common in recent years. CMS cut funding for outreach groups offering enrollment assistance, from $63 million in 2017 to $10 million in 2019, and halved the length of the OEP, from 90 days to 45 days.48,49 CMS also rejected proposals for an FFM SEP in response to the coronavirus pandemic.50 These decisions coincided with a 10% decline in individual market enrollment
v 5,300 consumers did not request financial assistance and therefore did not provide data on income.
10 | BACKGROUND
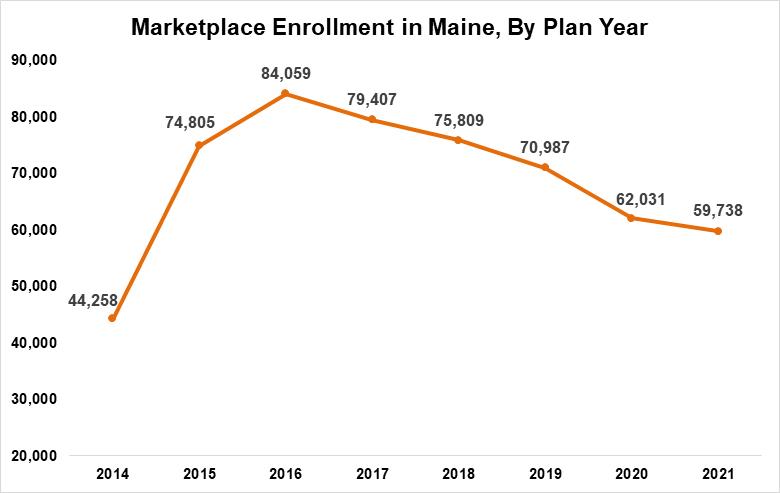
nationwide from the peak in 2016 to 2020.51 Figure 1 shows that Maine, which used the FFM during this time, experienced a steeper decline. The decrease likely reflects these and other federal actions, such as the zeroing of the individual mandate penalty, more than shifts to other coverage, as the shares of Mainers on employer-sponsored insurance and on MaineCare were stable prior to Medicaid expansion in 2019.vi
where ineligible applicants to one program are guided to another program for which they are eligible. SBM states have the opportunity to build a single streamlined application that directs enrollees to marketplace coverage or to Medicaid, depending on their eligibility.
Potential Issues in an SBM Transition
There are a number of issues that all states should consider before moving to an SBM:
Transitioning: There are significant one-time changes that carriers and others need to make, including but not limited to connecting enrollment functions with the new marketplace.
Financing: Most states rely on user fees to fund the large majority of the costs of setting up and operating their SBM. States have legislative flexibility to set user fees as they choose, but political constraints make it difficult to set fees far above 3% of premiums. Small states may have difficulty spreading the fixed costs of SBM operations over their marketplace population.ix There is a risk that some SBMs, given their limited budgets, simply replicate core functions of the FFM.55
Stability: An analysis from economists at the University of Pennsylvania reports that states with SBMs experienced much slower premium increases and fewer carrier exits than states using the FFM.53
Capturing user fees: Rather than sending premium assessment revenue (3% of total monthly premiums in FFM states, 2.5% in SBM-FP states) to the federal government, SBM states can keep this revenue in-state, creating savings to allocate towards other cost-stabilizing policies.vii
Data access: The transition to an SBM also improves state access to individual-level data, which can be used to guide outreach and improve insurance products.viii
Technology risks: Setting up a technology platform that is integrated with a call center—and integrating both with the state’s Medicaid eligibility systems—is a significant task. Some states may try to do too much at launch, resulting in core functions not operating optimally.
Accommodating stakeholders: Carriers and providers may oppose any actions which set the state on a path of increased regulation in the health care setting. Some may see the shift to an SBM as a precursor to further regulatory or administrative moves that constrain their actions or impact their business model. Internally, states may require significant resources from Medicaid eligibility offices, technology departments, or other state agencies.
Governance: Many states have flexibility in how their SBM can be established and operated under state law, including whether the SBM should be operated from
Coordination with Medicaid: SBMs are more closely connected with state Medicaid offices.54 This can (1) improve the experience of consumers experiencing churn between Marketplace and MaineCare coverage and (2) strengthen the “no wrong door” approach, vi A slight increase in the estimated share of Mainers on Medicare also contributes to this trend. See: Kaiser Family Foundation. “Health Insurance Coverage of the Total Population - Maine.” KFF (blog), October 23, 2020. https://www.kff.org/other/state-indicator/total-population/. Also, see: Centers for Medicare and Medicaid Services, 2019 Marketplace Open Enrollment Period Public Use Files https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Marketplace-Products/2019_Open_Enrollment
vii Pennsylvania, for example, intends to use funds from the user fees on its new SBM to finance its reinsurance program. See: Pennsylvania Insurance Department, “PA 1332 Waiver Frequently Asked Questions,” Pennsylvania Insurance Department, 2019, https://www.insurance.pa.gov:443/Coverage/Pages/PA1332Waiver-Frequently-Asked-Questions.aspx. Livingston, Shelby, “CMS Wants to Cut ACA Exchange Fees, End Silver-Loading,” Modern Healthcare, January 17, 2019, https://www.modernhealthcare.com/article/20190117/NEWS/190119916/cms-wants-to-cut-aca-exchange-fees-end-silver-loading viii When New Mexico moved to an entirely state-run exchange, its leaders cited this as one of the top motivations. See: Garrity, Tom “New Mexico Makes Move to a State-Based Marketplace,” beWellnm, September 21, 2018, https://www.bewellnm.com/Blog/New-Mexico-Makes-Move-to-a-State-Based-Marketplace ix Of the 15 states operating SBMs, only Vermont, Washington, DC, and Rhode Island have fewer residents (and plan year 2020 marketplace enrollees) than Maine.
BACKGROUND | 11
Figure 1. Marketplace Enrollment, Maine (Plan Years 2014-2021)52
Source: Kaiser Family Foundation Data and Center for Medicare and Medicaid Services Data.
within state government or by an outside organization with close links to state government. This decision has implications for the degree to which the SBM is subject to legislative oversight or reporting requirements or is at risk of having board members with conflicts of interest.

Plan management and oversight: The greater au-
thority that an SBM grants state officials and insurance departments over plan management and oversight comes with greater responsibilities that require a host of decisions about permissible plan features, from marketing to network breadth to consumer-facing descriptions of coverage. This work may involve more regular and difficult conversations with carriers.
12 | BACKGROUND
Methodology
This section describes the analytical approach used to develop the recommendations in this report. We first outline our approach to researching Maine’s health policy landscape and relevant policy options, followed by a discussion of the criteria we use to evaluate them. Finally, we describe how we prioritize policy options within each area using our Decision Matrix.
Research Approach
The analysis in this report is driven by interviews with 38 Maine stakeholders performed throughout October and November 2020.i These stakeholders include representatives from health care providers, advocacy groups, and carriers; state health policy experts; and senior officials from key State of Maine departments. While the majority of interviewees were Maine-based, we also consulted several experts from nationally-focused organizations and other states. In our interviews, we discussed the opportunities and challenges that Maine’s potential transition to an SBM could pose
to increasing coverage, reducing complexity, and improving affordability.

Based on analysis of these stakeholder interviews and further background research, we then developed potential recommendations. Using the following criteria aimed at evaluating consumer impact and state feasibility, we rank the priority of each recommendation within each policy area.
Consumer Impact
Affordability: What is this recommendation’s impact on premiums, deductibles, and other forms of cost-sharing for consumers?
Complexity: How does this recommendation impact the ease with which consumers can navigate accessing health coverage?
Coverage: How does this recommendation impact uninsured levels, and do impacts vary across different populations? If applicable, how does it affect wheth-
i Normally, these interviews would have been conducted in person in Maine, but due to the coronavirus pandemic they were conducted over Zoom.
METHODOLOGY | 13
er people are getting the high-quality, comprehensive coverage they want?

Equity: How does this recommendation impact marginalized populations in Maine, such as immigrants or people living in poverty?
State Feasibility
Political: How easily is this recommendation likely to move through the administrative or legislative process? Will relevant stakeholders be supportive of this proposal?
Financial: What impact would this have on the state budget? Is this recommendation realistic in the context of severe fiscal challenges and a recession triggered by the coronavirus pandemic?
Implementation Capacity: Can this recommendation realistically be implemented in terms of start-up, ongoing implementation, and long-term maintenance?
Decision Matrix
We present our decision matrix in Appendix Table 1. Each cell of the matrix is assigned a color on a scale from dark green to dark red. Dark green indicates
strong feasibility or significant positive impact on consumers, while light green indicates likely straightforward feasibility or limited impact on consumers. Similarly, dark red indicates lack of feasibility or significant negative impact on consumers, while light red indicates limited feasibility or limited negative impact on consumers. Gray indicates neutral consumer impact. Again, these determinations take into account stakeholder interviews, background research, and analysis of the political and policy landscape both in Maine and nationally.
To generate rankings, we assigned numeric scores to each color determination, weighting consumer impact more heavily. This framework was selected because the core of a promising policy is not the ease of implementation but rather its impact on consumers with respect to affordability, complexity, coverage, and equity. For instance, if a policy is feasible but has limited positive impact on consumers, we consider it to hold less value than a policy with a stronger positive consumer impact that may face higher feasibility concerns. See Appendix 1 for more details on color determination and weighting.
14 | METHODOLOGY
Health Equity Approach
This project was launched in late 2020, in the wake of a national reckoning on anti-Black racism and a pandemic that has disproportionately harmed historically marginalized communities, including those who are Black, Indigenous and people of color (BIPOC).
In June 2020, the Maine Center for Disease Control & Prevention announced that, despite only comprising 1.6% of the state’s population, Black residents represented 24% of all COVID-19 cases in Maine at the time.56 While these harrowing statistics have improved slightly since, as of January 18, 2021, Black and African American Mainers represent at least 5.4% of all documented COVID-19 cases in Maine—more than three times their share of the total population.i
The coronavirus pandemic has exposed the ways in which existing policies and structures have failed certain communities, leading to racial disparities in health, safety, and overall well-being. White Mainers are only half as likely to experience unemployment or poverty compared to BIPOC Mainers, a disparity directly linked to health access and outcomes.57 Even prior to the pandemic, Mainers of color were nearly twice as likely as white Mainers to be unable to seek medical care because they could not afford the cost.58
Maine’s potential transition to an SBM would be a significant milestone. With an SBM-FP, the State already has opportunities to invest further resources into enrolling uninsured Mainers, including through more effective outreach and consumer assistance activities—a critical investment towards health equity in the state. DHHS officials have asked us to identify best practices and policy innovations to support the success of an SBM.This transition is a chance to step back and better understand how existing systems may be contributing to inequities and how to avoid repeating missteps in a new model.
LGBTQ+, houseless, immigrants, refugees, disabled, migrant and seasonal workers, living in urban or rural areas, and/or newly eligible for MaineCare. We sought expertise and feedback from organizations who currently lead efforts to support these communities in Maine, and we applied a racial equity framework while conducting our analysis and drafting recommendations. While an SBM has the potential to expand health access for Mainers with historically marginalized identities, we heard concerns from stakeholders that its impact may be limited without improving equity coordination across OFI, the Office of MaineCare Services (OMS), and a potential SBM. In the same vein, we believe that there is an opportunity for DHHS to restructure and enhance its equity operations across the Department, which we detail in Recommendation 3 in Broad Recommendations.
Throughout this report, we suggest a number of incremental improvements that DHHS can adopt in the short-term during its potential transition to an SBM. Simultaneously, we share longer-term possibilities—including policy options that are complex and politically challenging—that we hope can help expand the State’s vision and approach to health services. As with other policy considerations, we recognize that DHHS’s choices relating to health equity will need to contend with both immediate and longer-term constraints, and hope that our report strikes a balance to assist state officials in their decision-making.
In light of this context, we use targeted universalism, a goal-oriented equity framework, to propose recommendations that would move toward all Mainers having accessible, affordable health care.ii In setting this universal goal, we pursue targeted processes for Mainers who are BIPOC, immigrants, refugees, migrant and seasonal workers, queer, trans, disabled, and/or experiencing homelessness.
We articulate our goal through a lens of care, in addition to coverage. Care is a broader term that includes all the ways Mainers might seek to address their health needs, including not only private and public health in-
While compiling this report, our team grounded equity as a foundational pillar of our work. Prior to identifying and interviewing stakeholders, we conducted background research to better understand communities in Maine, including those who are Black, Indigenous, i We say “at least” noting that over 4,250 positive cases did not report the patient’s race and/or ethnicity. Source: “COVID-19: Maine Data.” Division of Disease Surveillance, Maine Center for Disease Control & Prevention. Accessed January 19, 2021. https://www.maine.gov/dhhs/mecdc/infectious-disease/epi/airborne/coronavirus/data. shtml
ii Targeted universalism is an equity framework, created by professor and critical race scholar john a. powell, in which “universal goals are established for all groups concerned… (and) the strategies developed to achieve those goals are targeted, based upon how different groups are situated within structures, culture, and across geographies to obtain the universal goal.” powell, john a. Stephen Menendian and Wendy Ake, “Targeted universalism: Policy & Practice.” Haas Institute for a Fair and Inclusive Society, University of California, Berkeley, 2019. https://belonging.berkeley.edu/targeteduniversalism.
HEALTH EQUITY | 15
surance, but also Free Care or the Maine Mobile Health Program. These programs are critical for migrant and seasonal workers, immigrants and refugees, and those with limited English proficiency, among other groups who are systematically excluded from coverage under certain circumstances. While our recommendations would facilitate increased access to coverage for those who are eligible and interested, they would not replace the need for these sources of care.

This articulation also stems from an acknowledgement
that even with coverage, many marginalized populations continue to experience discrimination and stigma in the delivery of health care services, undermining the care they receive. Given that a full examination of the social determinants of health and systems of oppression in Maine is outside of the scope of this report, we approach universal access to affordable health care in this report as a critical economic safety net, rather than as a standalone solution to health inequities in the state.
16 | HEALTH EQUITY
Broad Recommendations

Over the course of our stakeholder interviews, it became clear that the State’s potential transition to an SBM presents the opportunity to more comprehensively center consumer voices and needs. This section focuses on broader recommendations that surfaced throughout the interviews and have implications for the topic-specific recommendations that follow. These recommendations are grounded in the perspective that, to achieve universal access to affordable, quality health care, consumer voices are critical at every step, from design to implementation to evaluation.59
We identify three key recommendations:
1. Increase consumer assistance capacity.
2. Integrate consumer engagement into the process of designing and implementing Maine’s SBM.
3. As a longer-term initiative, re-establish the Maine Office of Health Equity and empower its staff to coordinate equity efforts across the SBM, the MaineCare program, and all DHHS Offices.
Background
The possible transition to an SBM provides the opportunity to address challenges related to reduced consumer support around enrollment activities. While our stakeholder interviews highlighted existing state efforts to support consumers’ enrollment needs, policies under former Governor LePage and former President Trump—which decreased funding for marketing, outreach, and consumer assistance in the marketplace60—have limited the potential for robust and sustained support for consumers.
In this context, foundations have stepped in to provide funding for outreach and enrollment efforts, directing crucial resources to advocacy groups and community-based organizations.i As Maine looks to transition to an SBM, stakeholders stressed that they hope to pivot from functions that could be performed by the State to grassroots organizing and capacity-building among local leaders.
Consumer-facing stakeholders also expressed broad concern that a transition to an SBM may not be responsive to the needs of consumers, particularly historically marginalized Mainers. While state officials have made inroads and hold regular meetings with community organizations and advocacy groups, some stakeholders voiced the perspective that information sharing
and collaboration opportunities between community-based groups and state officials can be improved.
Another theme that emerged among our interviews was the impressive institutional knowledge, close community, and policy capacity developed among grantees of the Maine Health Access Foundation. The tight-knit nature of this community of organizations was clear throughout our interviews, with community-focused stakeholders referencing conversations we had with previous community organizations -- an indicator of frequent collaboration among such groups. A stakeholder with a national advocacy focus also noted in a conversation that Maine has a particularly robust network of community-focused health policy organizations. Additionally, one stakeholder specifically highlighted that this cohort of advocacy and community-based organizations, which has collaborated since the rollout of the ACA, would likely bring significant value through its policy and consumer-facing experiences with the marketplace. These themes highlight the opportunity to more comprehensively engage this cohort to center consumer voices in the potential SBM transition.
Recommendation 1: Increase consumer assistance capacity.
Those providing enrollment support, including navigators, assisters, and call center staff, play an important role in helping consumers with low literacy, limited English proficiency, poor internet access, or who are facing other barriers to enroll in health insurance that meets their needs. While Maine officials should work with consumer groups to make the marketplace as easy to navigate and understand as is possible, many consumers will still likely need or prefer assistance to navigate the marketplace and select a plan. For example, many rural residents rely on navigators for enrollment because they lack access to the internet or can only access it on their phones, making in-person or over-the-phone consumer assistance a lifeline for coverage. Additionally, consumers with limited English proficiency may rely on translation services provided through the call center or other consumer assistance.
CMS reduced funding for navigators during 2018 and 2019, which limited funding for enrollment assistance in Maine. In 2019, Western Maine Community Action
i These external sources of support have come to play an integral role in the consumer assistance landscape. For instance, in 2019 alone the Maine Health Access Foundation granted the DHHS Office of MaineCare Services for MaineCare Expansion $450,000 and the Wabanaki Public Health Office $50,000 for ACA MaineCare Direct Outreach and Enrollment and Health Equity Capacity Building. Maine Health Access Foundation. “2019 Annual Report: Responsive Solutions to Improve Health.” https:// mehaf.org/wp-content/uploads/2019-Annual-Report.pdf
18 | BROAD RECOMMENDATIONS
received $100,000 of CMS funding, which was the only federal funding for navigators in Maine that year.61 While Maine officials increased funding for this year, the State should continue to prioritize sustained financial support for consumer assistance programs.
Recommendations include the following:
• Increase the number of enrollment assisters and call center staff funded by the State.
• Prioritize cross-cultural communication skills in hiring and training of staff.
• Invest in targeted enrollment outreach to communities facing higher rates of uninsurance, such as LGBTQ+ individuals.62
• Increase the number of enrollment assisters able to translate material into additional languages.
• Create a centralized navigator portal to provide enrollment assisters information about changes to consumers’ health insurance enrollment.
• Identify opportunities to train people within historically disempowered communities to serve as enrollment assisters.
Consumer Impact
This policy could substantially decrease complexity for consumers by providing them with trusted advice and assistance to enroll. This would likely lead more consumers to enroll, and could advance health equity if assisters can support groups with different language backgrounds, limited internet access, or other barriers such as time scarcity to enroll in coverage. Assisters and call center workers can help consumers find the most affordable plan that offers what they need.
State Feasibility
This policy would likely receive support from stakeholders because it facilitates enrollment by those who may otherwise remain uninsured. Sustained enrollment support could impose increased costs for the State, as it could require hiring of new employees or additional granting to community-based organizations.
Recommendation 2: Integrate consumer engagement into the process of designing and implementing Maine’s SBM.
State officials can also consider how to formally embed consumer voices and needs in decision-making processes related to the possible transition to an SBM. For instance, the State could establish a consumer advisory board with representatives from key communities and
organizations. The purpose of this structure would be to assure that SBM-related policies are informed by the perspectives of Maine consumers through meaningful collaboration.
DHHS officials could consider leveraging existing infrastructure focused on narrowing disparities and elevating consumer voices, particularly those of historically marginalized health care consumers such as immigrants or the Wabanaki people. One such structure, for instance, is the Permanent Commission on the Status of Racial, Indigenous and Maine Tribal Populations. The Commission—which recently received a one-time $50,000 funding award from the Mills administration63—could receive additional support to act as a channel to embed consumer input and advance equity-focused initiatives.
The enabling statute for this Commission outlines a number of roles that this body could engage in to elevate consumer voices and health equity concerns in the potential SBM rollout. For instance, the Commission could hold public hearings and workshops to consider how an SBM could narrow health disparities. The Commission could also carry out relevant research and work with the Governor to advance policy actions promoting health equity. Such activities align with the Commission’s overarching goal to “promote, carry out and coordinate programs designed to improve opportunities for racial and ethnic populations in the State.”64 The State could also look to the existing infrastructure and community of consumer advocates and community-based organizations supported by the Maine Health Access Foundation for opportunities for more robust consumer input.
Consumer Impact
Sustained engagement with consumer-facing stakeholders would benefit consumers by centering their needs and challenges in the potential development of the SBM. Providing consumer groups a forum to voice their concerns and authentically engage in the possible SBM transition can also potentially address coverage barriers and could lead to opportunities for expanded coverage access and increased affordability.
Consumer collaboration could also help officials identify ways to decrease marketplace enrollment complexity by identifying pain points experienced by consumers in the enrollment process. Finally, centering consumer voices—particularly those of marginalized populations—advances health equity by targeting at-
BROAD RECOMMENDATIONS | 19
tention and resources towards issues impacting populations historically excluded from policymaking spaces.
State Feasibility
This policy would likely be feasible. Many advocacy groups already participate in other state health policy settings, such as Maine Equal Justice on the MaineCare Advisory Committee.65 While this recommendation requires state action to convene and consider how the body informs other processes, it is unlikely to pose significant implementation challenges.
Challenges associated with this recommendation are related to broader obstacles around stakeholder and consumer engagement. State officials will need to balance competing needs of different organizations, set expectations for how they incorporate input, and determine which organizations should represent key voices.
Recommendation
All state officials we interviewed expressed an interest in partnering more closely with community organizations to reduce inequities regarding health access for historically marginalized communities in Maine. DHHS Offices are taking proactive steps to solicit input from and collaborate with community leaders, especially given the context of the coronavirus pandemic and its disproportionate impact on specific communities.
At the same time, officials acknowledged that existing equity activities are siloed, limiting operational efficiency and overall efficacy. Internally, the burden primarily falls on leaders within each Office to foster lasting relationships on behalf of the State, all while juggling multiple priorities. As a result, equity-oriented activities are often ad hoc and/or conducted independently from other Offices within DHHS, even those with closely related responsibilities. Externally, community health groups must maintain relationships with multiple Offices. Officials expressed worries that the State may be responding to communities with greater advocacy resources, rather than targeting the communities with the greatest needs. Overall, this lack of coordination has resulted in potentially duplicative and inconsistent equity efforts, which undermine the State’s ability to
foster trust and ultimately to serve communities.
Multiple state leaders also expressed concern at the lack of uniform standards for demographic data across DHHS, a challenge that other states are also grappling with.66 This limits the State’s ability to monitor health access and outcomes across programs, including between OFI and OMS. This is a critical issue if Maine officials wish to capture and monitor community health statistics at a level more specific than the categories used by the federal government (e.g., certain ethnicities, tribes, and LGBTQ+ identities), as inconsistent usage over time could hinder longitudinal analysis.
The shift to the SBM is a chance for DHHS to think more deeply about its operational structure when it comes to equity, especially given the significant role that assisters and community organizations will play to make the new SBM a success.
Prior to the LePage administration, DHHS contained an Office of Health Equity with a mission to “[promote] health and wellness in Maine’s racial and ethnic minority communities.”67 Currently, many of these responsibilities have been carried forward by DHHS’s Manager of Diversity, Equity, and Inclusion. As a longer-term initiative, we recommend that DHHS re-establish this Office but consider expanding its authority and responsibility to (1) coordinate health equity efforts, including data, within DHHS and (2) foster longer-term relationships with community health organizations on behalf of the State.
Such a model would follow existing examples in states like California and Connecticut. California’s Office of Health Equity contains multiple business units engaged with leading the State’s health equity policy and planning, fostering community development and engagement, and providing technical guidance on health research and statistics.68 In a similar model, Connecticut’s Office of Health Equity has worked since 2016 to “ensure that health equity is a cross-cutting principle in all [Department of Health] programs, data collection, and planning efforts,” which includes coordinating efforts with community-based organizations, contractors, and local health officials.69
Many of the access barriers and community disparities relating to the marketplace overlap with those impacting OFI, OMS, and MaineCare program activities, as well as other DHHS programs. If the underlying structure of Maine’s health equity coordination is not eventually addressed, it will limit the SBM’s full poten-
20 | BROAD RECOMMENDATIONS
3: As a longer-term initiative, re-establish the Maine Office of Health Equity and empower its staff to coordinate equity efforts across the SBM, the MaineCare program, and all DHHS Offices.
tial to serve Mainers, especially those with historically marginalized identities.

Consumer Impact
A more coordinated approach to equity at DHHS will benefit consumers, especially those who have been historically marginalized or excluded from health systems. It will make it easier for DHHS to develop lasting relationships with community organizations and incorporate their needs across the department, rather than simply on a project or program basis. If DHHS standardizes data collection during this process, it will allow officials to develop, target, and evaluate policies designed to close health disparities or eliminate barriers impacting specific groups.
State Feasibility
Across the country, the national reckoning on anti-Black racism following the murder of George Floyd has led many state governments to begin developing or further enhance their equity capabilities.70,71 There are no easy fixes; racism and other dimensions of oppression are complex and deeply pervasive, and require a long-term commitment to action from all levels of an organization. It is especially important that equity staff are empowered at a level of decision-making to work with Office leaders across DHHS, which will necessitate adequate funding for staff and operations. However, given the current political and cultural moment, state leaders may be more inclined to support health equity efforts, especially in light of the disproportionate impact of COVID-19 on Mainers of color.
BROAD RECOMMENDATIONS | 21
Enrollment Periods

The flexibility of an SBM offers opportunities to expand OEPs and SEPs, which can promote greater access to health care for populations in Maine that have historically faced barriers to accessing insurance and care.
This section first outlines the current status of OEPs and SEPs for the FFM and state marketplaces. This is followed by five policy recommendations, based on our research and interviews with Maine stakeholders. These recommendations are aimed at maximizing insurance coverage while accounting for some of the potential limitations presented by adverse selection.
We recommend the following:
1. Establish an OEP that runs until January 31, so the period lasts a total of 92 days.
2. Implement SEPs for public health crises, for individuals who become pregnant outside of open enrollment, and for uninsured tax filers beginning the day that their state tax return is filed.
3. Explore options for an SEP directly after the OEP for Mainers who had valid reasons to miss the OEP deadline.
Background
Open enrollment periods are intended to give consumers a window to enroll in health coverage and prevent consumers from waiting until they are sick to enroll. The FFM currently operates an annual 45-day OEP beginning on November 1 and ending December 15. In addition, the ACA offers eligible individuals the ability to enroll in coverage outside of the standard open enrollment timeframe through various SEPs.72 These SEPs are offered by both the FFM and SBMs and are triggered by qualifying life events. The primary types of triggers are loss of qualifying health coverage, change in household size or residence, change in eligibility for marketplace coverage or subsidies for coverage, or enrollment or plan error.i
The details of eligibility and verification for an SEP depend on the event type. In 2017, the federal government added restrictions for some of these events, making it more difficult for consumers on the federal platform to enroll in health coverage outside of the OEP.73 For example, the new rules required pre-enrollment verification for all SEPs, which could act as a hurdle to consumers and reduce overall marketplace en-
rollment. These new restrictions do not apply to SBMs.
In addition to shielding consumers from restrictive enrollment policies at the federal level, SBMs provide states their own unique decision-making flexibilities. SBMs have added a number of new SEPs such as:
• Public health emergency (COVID-19);
• Pregnancy;
• Change in disability status;
• Natural disaster or act of terror;
• Loss of military insurance;
• Loss of hardship exemption; and
• Issues with insurance carriers, enrollment processes, payment, etc.
Maine may benefit from instituting any or all of the above SEP types. Implementing new SEPs could offer an opportunity to increase coverage, especially for individuals experiencing life challenges that would be exacerbated by significant health care bills. For example, during the coronavirus pandemic, most SBMs implemented an SEP to allow marketplace enrollment, while the FFM relied on its usual SEPs.74 This policy provided an opportunity for many Americans to face the pandemic better prepared for the health and economic consequences of contracting COVID-19.
Meanwhile, some believe SEPs provide a disincentive to sign up during open enrollment as individuals may wait to enroll only when they need coverage if they know they will qualify for an SEP. One analysis of an insurer’s data in 2015-2016 provides some evidence that SEP enrollees have higher inpatient and emergency department costs.75 However, the stakeholders we interviewed did not express significant concerns about SEP impacts on premiums. While we heard some concerns from carriers about risk pooling, we also heard that SEP enrollment has not been as expensive for insurers as originally feared, at least since SEPs became more strictly verified.ii Therefore, it does not appear that risk pooling concerns in general should preclude an expansion of SEPs in Maine. When implementing any new SEPs, careful consideration should be given to whether verification is truly needed, as it adds complexity to the consumer experience which may reduce the policy’s effectiveness.
The Biden administration may potentially expand en-
i There are also a number of other more complex SEPs, such as when a Medicaid application filed during OEP is denied after the deadline. Source: “Enroll in or change 2020 plans — only with a Special Enrollment Period.” Healthcare.gov. https://www.healthcare.gov/coverage-outside-open-enrollment/special-enrollment-period/ ii This statement is based on background interviews with Maine stakeholders. For a recent analysis of changes to SEP risk-adjustment since 2017, see: Dorn, Stan, Bowen Garrett, and Marni Epstein. “New risk-adjustment policies reduce but do not eliminate special enrollment period underpayment.” Health Affairs 37.2 (2018): 308-315.
ENROLLMENT PERIODS | 23
rollment opportunities in order to bolster insurance coverage in the aftermath of the coronavirus pandemic. This may be a chance for Maine to glean additional perspectives using data from any SEP or OEP expansions in the FFM.76 In addition to the recommendations we discuss below, the State should seek to leverage federal outcomes in the upcoming year to enhance analysis of enrollment trends.
Recommendation 1: Establish an OEP that runs until January 31, so the period lasts a total of 92 days.
The Trump administration has reduced the length of the FFM’s OEP from 92 days (November 1 to January 31) to 45 days (November 1 to December 15). This policy constrains the time consumers have to enroll during a season in which many Americans are already experiencing a scarcity of time, money, or other resources.77 This lack of mental bandwidth can make it harder for individuals to complete complex tasks like health insurance enrollment.78 One opportunity for states transitioning to an SBM is the ability to decide the length of their OEP, which for the most part means extending the period. Table 1 displays the OEP closing
dates used by SBMs and Table 2 displays deadlines for January 1 coverage. No OEP begins before or after November 1.
Consumer Impact
A longer OEP would have a positive effect on coverage and would allow more time for enrollment assisters to provide outreach and enrollment support to marginalized communities. Particularly for community organizations serving Mainers whose primary language is not English and/or those who cannot or will not enroll directly, an extended OEP is critical to providing sustained enrollment support to consumers. It would also allow more time for consumers to sort through any complexities they face in the process.
State Feasibility
In our interviews, stakeholders demonstrated broad interest in extending the OEP under an SBM. In fact, one stakeholder expressed that if the State was not willing to extend the OEP and add SEPs, building an SBM would not be worth the effort. Enrollment assisters see an extended OEP as an opportunity to partially make up for the barriers to enrollment in Maine,
December 15
December 22
Connecticutiii, Idahoiv, Maryland, and Vermont
Minnesota
January 15 Colorado, Nevada, Pennsylvania, and Washington
January 23
January 31
Massachusetts and Rhode Island
California, New Jersey, New York, and Washington, DC
Table 2. Deadline for January 1 Coverage by State-Based Marketplace
January 1 coverage
December 15
December 22
December 23
December 30
SBM(s)
Coloradov, Connecticut, Idaho, Maryland, New York, Vermont, Washington, and Washington, DC
Minnesota, Pennsylvania
Massachusetts
California
December 31 Nevada, New Jersey, and Rhode Island
*Coverage purchased after this date is effective February 1; however, coverage purchased between January 15 and January 31 in New York and Washington, DC is effective March 1.
iii Connecticut has extended the 2021 OEP to January 15, 2021 due to the coronavirus pandemic. If residents enroll during the extension, their coverage starts February 1, 2021.
iv Idaho has extended the 2021 OEP to December 31, 2020, the last date to apply for January 1, 2021 coverage.
v This year, Colorado temporarily extended the enrollment deadline for January 1 coverage to December 18, 2020.
24 | ENROLLMENT PERIODS
OEP Closing Date SBM(s)
Table 1. Open Enrollment Period Length by State-Based Marketplace79
for
Deadline*
including technological limitations and system outages, language barriers, low call center capacity, and delayed notices by mail. We heard from these groups that Mainers rely on enrollment assisters because they lack internet access at home, in addition to wanting one-on-one support with the enrollment process. Assisters also cited lack of trust in the health care system and confusing eligibility requirements for certain communities, like immigrants and refugees, as barriers to enrollment in a short OEP. These assisters see the current six-week period as a “mad dash” and “absolute insanity,” and would benefit from more time to adequately serve Mainers.
Although carriers highlighted that many Mainers enroll close to the deadline80 regardless of the date, they were broadly accepting of an extended OEP, as long as the length would not facilitate increased adverse selection. In response to this concern, one consumer advocacy group pointed out that shorter OEPs discourage younger consumers, for whom the costs (complexity, time, money, etc.) of enrollment outweigh the benefits, potentially cutting out a population that is traditionally valuable to carriers.81
Finally, one stakeholder expressed interest in starting the OEP earlier, rather than pushing the deadline later, due to the time constraints for processing enrollments after December 15, and one stakeholder supported extending the OEP for as long as possible.
Extending the OEP would have a limited budget impact, with the largest expenses likely to be increased marketing and employing call center staff for a longer period of time. Implementation would be relatively straightforward. If the OEP were to be extended later, the State would need to work with insurers to build adequate processes to begin coverage no later than February 1 for consumers who enroll between December 16 and January 31. The State could join most other SBMs in requiring consumers to enroll by December 15 for January 1 coverage.
Recommendation 2: Implement an SEP for public health crises.
In response to the coronavirus pandemic, 12 of 13 SBMs opened a broad SEP, while the federal marketplace did not.82 These emergency SEPs ranged from six weeks to six months. While the FFM SEP for lost coverage allowed many of the newly unemployed to
enroll, those who did not have health coverage when they lost their job do not qualify.83 We recommend using such an SEP to improve health insurance coverage in future public health crises.
Consumer Impact
The most significant consumer impact of such an SEP is that insured rates could increase during the public health crisis. There is evidence that several SBM states with a COVID-19 SEP had much greater marketplace enrollment in the first months of the pandemic response than FFM states.84 Consumers who enroll using the SEP could gain the financial security to utilize more preventive health care or access a provider when sick. This might improve their health outcomes and also could have positive spillovers to the crisis response by limiting contagion.
State Feasibility
A number of the stakeholders we interviewed expressed support for an SEP in response to COVID-19 and similar public health crises. As this was implemented in almost all SBM states, it is likely feasible from a political and implementation standpoint. While there may be some variable costs, budget impacts should be limited given that the marketplace will already be providing other SEPs.
In our stakeholder interviews, one carrier expressed concerns about possible risk pooling issues for such an SEP. However, the COVID-19 instance provides a counterexample to this concern. Carrier spending on reimbursements has dropped significantly during the pandemic.85 It appears that carriers, at least in this crisis, would have substantial cushion to absorb risk pooling costs. Meanwhile, increasing the coverage rate might be useful to provide some help to hospital budgets given they have been deeply strained during the pandemic.86
Recommendation 3: Establish an SEP for individuals who become pregnant.
Uninsured individuals who become pregnant should be eligible for an SEP following verification of pregnancy by a provider. This would lead to greater access to prenatal care, which impacts maternal and infant health. Limiting the length of this SEP may reduce the risk of pregnant individuals waiting until they have significant health care costs before enrolling.vi
vi For example, consumers who are pregnant in a state with no time restrictions on a pregnancy SEP enrollment window may wait until they experience complications before enrolling.
ENROLLMENT PERIODS | 25
Under current FFM rules, pregnancy is not a qualifying life event that triggers eligibility for an SEP. Uninsured individuals who become pregnant outside of the OEP may become eligible for MaineCare due to higher income eligibility levels for people who are pregnant than for other adults, but only qualify for enrollment in a marketplace plan through other circumstances. An SEP for uninsured individuals who become pregnant is one potential solution that some states have implemented to raise coverage levels for pregnant individuals entering a period associated with high health care costs. This policy option has received substantial support from various groups, including the American Congress of Obstetricians and Gynecologists as well as Planned Parenthood.87
Table 3 lists the states that currently allow an SEP for pregnancy. Total length of the SEP varies; in New York and Vermont, pregnant individuals are permitted to enroll at any time during their pregnancy. All states require some level of verification from a provider, which can be a barrier for uninsured individuals.vii
pregnancy SEP. Data for 2017 indicates that 36.3% of Black pregnant individuals lacked insurance prior to pregnancy, compared to 12.4% of white pregnant individuals.96 Furthermore, Black, Hispanic, and American Indian individuals who are pregnant are all more likely than white pregnant individuals to receive late or no prenatal care in Maine.97 An SEP may be able to address these gaps by encouraging and facilitating coverage for those ineligible for MaineCare.
State Feasibility
Stakeholders we interviewed recognized the importance of establishing a pregnancy SEP, but some carriers also expressed concern about extensive SEPs allowing consumers to selectively choose when they enroll in the marketplace. Enabling a pregnancy SEP may also lead to an influx of consumers with higher health care costs.Yet data suggests that the actual burden on carriers to extend coverage to pregnant individuals should be modest.98 In 2017, an estimated 13.3% of expectant Mainers were uninsured prior to pregnancy.99 Combining this figure with data from Maine’s Division of Public Health Systems provides us with an estimated 1,635 pregnant individuals who were without insurance coverage prior to pregnancy in 2017.ix However, a significant number of these individuals would likely be eligible for MaineCare, given the program’s higher income limits for pregnant individuals. Considering that 39.2% of all births in Maine were covered by MaineCare in 2017 (before the State expanded MaineCare), we would expect only a fraction of those 1,635 individuals who were uninsured prior to pregnancy to require marketplace coverage.100
Consumer Impact
Pregnancy can present health considerations that require affordable access to health care services. For pregnant individuals with no insurance, “maternity care and delivery can cost $10,000 to $20,000 without complications.”94 An SEP for pregnancy ensures that expectant individuals are able to afford prenatal care, which is linked with better health outcomes including lower rates of low birth weight and maternal mortality.95 Encouraging greater utilization of important preventive services can also forestall costlier health issues in the future.
Existing racial disparities could be mitigated with a
Placing a time limit on this SEP could lessen concerns about pregnant consumers timing their purchase of insurance to avoid paying into the shared cost pool. If Maine chooses to set a time limit for this SEP, it can follow the examples of other states with limits ranging from 30 days to 90 days.
Ensuring that individuals receive prenatal preventive care is likely to translate to lower future costs by avoiding costly complications and NICU admissions.101 Furthermore, providing insurance coverage to pregnant individuals who are ineligible for MaineCare can reduce cost pressures on the State’s Free Care program. Improvements in health outcomes for individuals
vii If necessary, expanding the scope of practice for certain health care workers would enable greater access for uninsured individuals to be able to verify their pregnancy as a requirement for triggering an SEP. This expanded pool can potentially include nurse practitioners, nurse midwives, and physician assistants. viii Starting from the day of provider verification.
ix Most recent data available at time of report. Source: “Maternal & Birth Outcomes.” Maine Division of Public Health Systems. Retrieved December 11, 2020. https:// www.maine.gov/dhhs/mecdc/public-health-systems/data-research/vital-records/births.shtml
26 | ENROLLMENT PERIODS
State SEP Lengthviii Verification Connecticut89 30 Days Provider Washington, DC90 60 Days Provider Maryland91 90 Days Provider New York92 Unlimited Provider Vermont93 Unlimited Provider
Table 3. SBMs and Availability of Pregnancy Special Enrollment Period88
and infants as well as future cost savings likely outweigh any risks of adverse selection.
Recommendation 4: Establish an SEP for uninsured tax filers, beginning the day that their state tax return is filed.
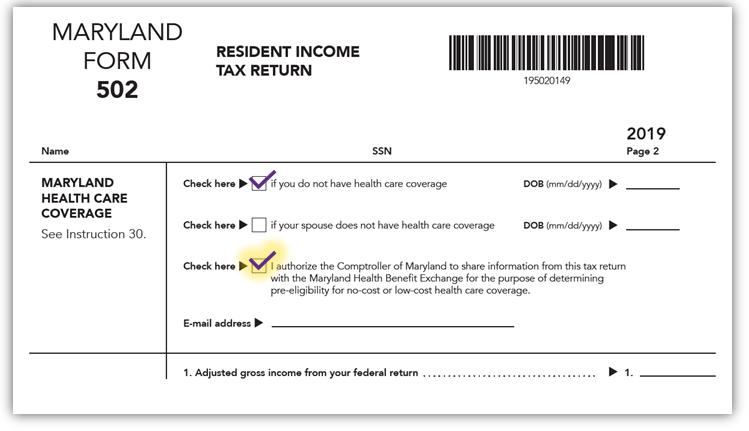
The process for this SEP could be modeled on Maryland’s Easy Enrollment system. Uninsured individuals who file taxes would first be screened for MaineCare eligibility; those ineligible for MaineCare would have a set number of days from the filing of their income taxes to enroll in a marketplace plan.
In 2015, the FFM enacted a one-time SEP during the tax season as individuals adjusted to the individual mandate and its associated penalty.102 Following the elimination of the federal individual mandate, a number of states implemented their own tax penalties for uninsurance, and similarly provided an SEP for individuals who were unaware of the penalty. This year, California and DC both provided tax filers with a tax season SEP in order to leverage the tax penalty to encourage insurance enrollment.103,104
Maryland, despite lacking an individual mandate for coverage, has established an SEP to enroll tax filers as part of the State’s Easy Enrollment system. Tax filers can check a box on their tax returns indicating that
they currently lack insurance and are interested in purchasing coverage (see Figure 2). The state marketplace subsequently coordinates with the State Comptroller to verify a tax filer’s eligibility for Medicaid or premium subsidies.105 All individuals, regardless of eligibility for subsidies, then have a 35-day SEP to enroll. A bill has been introduced in New Jersey to create a similar enrollment system.106
Consumer Impact
In our interviews, some stakeholders mentioned an Easy Enrollment program in Maine as an innovative way to increase coverage. Income taxes are a captive point of interaction between the State and its residents, allowing Maine an opportunity to communicate information on insurance that individuals might otherwise ignore or miss. The State can also obtain income information from taxpayers that can be used to initiate enrollment, including calculating eligibility for MaineCare or APTCs. Maine could leverage a tax filing SEP to drive insurance enrollment by making it convenient for taxpayers to opt-in to applying for insurance ontheir income taxes.x Enabling this SEP could also appeal to individuals who were sidelined during the OEP due to limited finances. With tax refunds in hand, some consumers may be more comfortable buying insurance after the OEP has ended.107
ENROLLMENT PERIODS | 27
x As one stakeholder group noted, Maine can also use this opportunity to register individuals to vote.
Figure 2. MD Tax Filing Checkoff108
A tax filing SEP opens up the insurance marketplace to a number of consumers who may have less health care utilization. Individuals required to file taxes are likely employed, which research suggests is associat ed with better overall health.109 Historically, income tax filers have also tended to be younger than the general population: in 2018, adults ages 18 to 35 made up 41% of income tax filers under 65, compared to 30% of the overall population of adults under 65.110 These factors all indicate that individuals who enroll as a result of a tax filing SEP may skew younger and healthier, resulting in positive impacts on the risk pool, which could translate to lower costs for consumers.
State Feasibility
This policy would require significant coordination across state government and potentially additional legislation. The SBM, Maine Revenue Services, and OFI would need to coordinate their systems and data-sharing to ensure that tax filers who elect to enroll are given accurate information on their eligibility for MaineCare or subsidies. There would be added complexity and costs for Maine Revenue Services to process and verify the date of tax filing for purposes of triggering an eligibility period.xi
Recommendation 5: Explore options for SEP directly after OEP for Mainers who had valid reasons to miss the
OEP deadline.
As discussed above, many consumers will begin marketplace enrollment near the end of the OEP regardless of its length. Ethnographic research on Rhode Island’s SBM found that bureaucratic barriers to enrollment, such as system errors, are a significant factor extending the length of the ACA enrollment process.111 These unexpected barriers may cause a consumer attempting to sign up late in the period to miss the deadline. We recommend exploring the most common reasons for missed deadlines and whether they should be addressed by an SEP extension.xii Stakeholders expressed that some delays outside of consumers’ control include technical delays in eligibility or payment processing, lack of available assister appointments until after the deadline, and long waits for necessary translation
or call center services. The technology platform vendor may also be able to proactively identify common enrollment delays in other SBM platforms.
Consumer Impact
This SEP would increase coverage by giving eligible consumers an extra chance to enroll. Given that it would function like a limited extension of the enrollment deadline, the SEP should have a similar risk pool profile to the OEP. Developing such an SEP in consultation with advocates could allow it to be responsive especially to the higher barriers faced by marginalized communities. For example, the policy could extend the deadline via SEP for consumers who did not receive needed translation services prior to the OEP deadline.
Designing a simple verification process for consumers may be difficult, given that the eligibility of the SEP is based on their user experience, not characteristics of the consumer. Still, a verification hurdle might be justified to prevent consumers from counting on the extension deadline as the “real” OEP deadline, defeating the purpose to provide a second chance to meet enrollment deadlines. These concerns will need to be carefully balanced in the design of this type of SEP.
State Feasibility
Limited SEPs for missing the enrollment deadline already exist at the federal level.112 These triggering events include technical errors on the enrollment site or inaction by professional enrollment support.xiii Furthermore, SBMs have used their platform flexibility to expand the list of reasons which qualify a consumer for SEP extension of the OEP.xiv These examples demonstrate that implementing this recommendation is feasible. Such an SEP could also be especially useful in the first year of an SBM to ease the transition and make sure that coverage rates are maximized despite any platform-related issues.
xi As Maryland enters the second year of Easy Enrollment implementation, Maine should coordinate with Maryland to share data and outcomes to better inform implementation of a similar system.
xii We envision such SEPs being triggered either by missing the deadline or being notified of an error in the enrollment process at some point after the deadline. This would qualify the enrollee for an SEP of similar length to other SEPs, at least 30 days.
xiii “Professional enrollment support” refers to insurance companies, navigators, brokers, or certified application counselors.
xiv Examples include SEPs triggered when the OEP deadline is missed due to conditional Medicaid denial after OEP, non-system error, and acts of terror. Source: Rakotoniaina, Adney. “How States Are Increasing Coverage through Special Enrollment Periods.” The National Academy for State Health Policy. September 29, 2020. https:// www.nashp.org/how-states-are-increasing-coverage-through-special-enrollment-periods/
28 | ENROLLMENT PERIODS
Displaying Clear Choice Plans

Launching an SBM offers the opportunity to adopt best practices for differential display of insurance plan options according to individual consumers’ health care and financial needs. Maine officials could use this opportunity to leverage the forthcoming standardized plan designs, called Clear Choice designs, with plan display decisions that advance the State’s broader mission of delivering SBM consumers a simpler shopping experience.This is particularly important from a health equity perspective because Clear Choice design plans can facilitate access to more comprehensive coverage for those historically marginalized by the health care system.
This section explores the plan display, comparison, and decision tool interfaces used by SBMs and how the State of Maine could adapt these for its own SBM. Some approaches are specific to standardized plans, but most are applicable to all plans.
As Maine officials consider their approach to the SBM shopping interface, we make the following four recommendations:
1. Use an intake questionnaire and show plans based on responses.
2. Build a comparison tool that: (1) automatically highlights differences between selected plans, and (2) includes a “Compare to Similar Plans” function.
3. Include a pop-up glossary feature when customers hover over a technical term, and enable screen reading audio capability for accessibility.
4. Distinguish Clear Choice plans with naming, visual cues, sorting, and/or filtering.
Background
Standardized plans empower consumers by demystifying technical vocabulary and complex cost-sharing structures that, at best, create administrative burdens for the savviest consumers and, at worst, intimidate potential consumers to the point where they abandon applications and end up uninsured. Instead, standardized plans allow consumers to focus their comparisons on the basis of premiums, provider networks, and formularies to identify plans that best meet their needs.
Seven states and Washington, DC require that some or all of the plans offered by marketplace carriers follow standardized plan designs.113 The federal marketplace also offered standard plan options for plan years 2017 and 2018.114
In Maine, Clear Choice designs will apply to plans with
effective dates of January 1, 2022 and after. Plans adhering to the same Clear Choice design will share the same “set of annual copayments, coinsurance and deductibles for all or a designated subset of the essential health benefits.”115
Current draft guidance from the Bureau of Insurance clarifies some of the requirements for Clear Choice designs on the SBM but does not address how to display the plans.116 Publicly available Clear Choice Workgroup comments show that carriers and businesses believe standard plans increase costs because the benefits are more comprehensive, but these comments do not include stakeholder views on plan display.117 Our conversations with stakeholders therefore sought to clarify opportunities for displaying Clear Choice plans in a manner that is understandable to consumers.
Recommendation 1: Use an intake questionnaire to show consumers plans that fit their needs.
Several states with SBMs use some type of questionnaire to collect basic information that can be used to tailor the selection of plans displayed or the order in which they are shown based on their fit with a consumer’s needs. These tools are anonymous and separate from the application process; data entered in them is not saved.
These tools can take different forms. Colorado’s SBM guides consumers through a questionnaire covering household members’ ages, genders, tobacco use, level of health care usage, providers, and prescription drugs before they can view plan listings, although many questions are optional.118 Washington’s SBM asks for some of this information before showing plans, with an additional, optional “Smart Planfinder” tool that asks about providers, prescription drugs, and health care usage level.119
Once this information is collected, it can be incorporated into the interface in various ways:
• Automatically sorting plans by estimated annual cost, as is done by SBMs in California, Colorado, and other states;
• Allowing filtering for plans covering the providers and prescription drugs input by the consumer, similar to Healthcare.gov or the Colorado SBM;
• Adding a visual cue to plans determined to be likely to fit the consumer’s needs, like Washington Healthplanfinder’s Smart Choice marker (see Figure 3); and/or
30 | CLEAR CHOICE PLANS
• Displaying the coverage status of the providers and prescription drugs input by the consumer with each plan listing, as is done on Healthcare.gov and Washington Healthplanfinder (see Figure 3).i
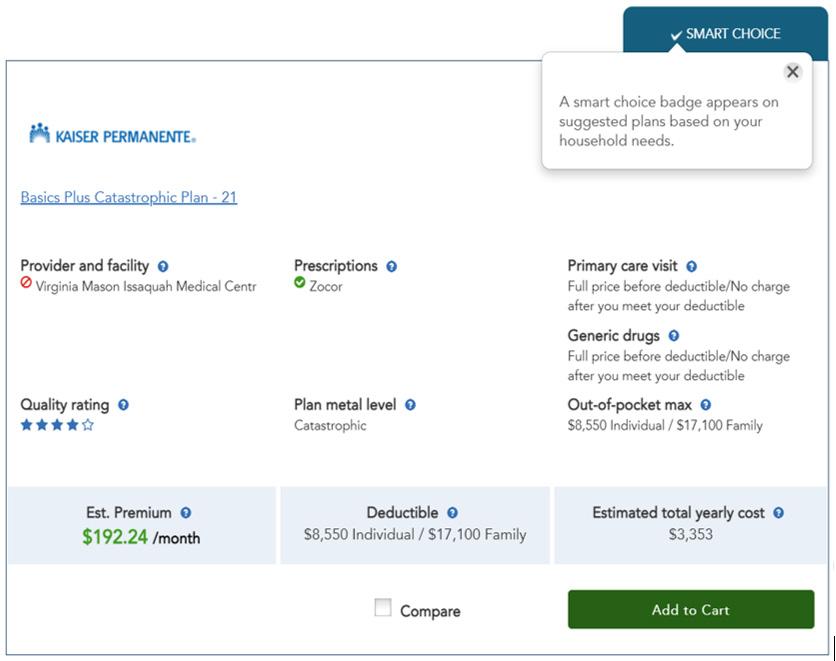
Whichever approach is chosen, the same tools should be available for anonymous “window shopping,” useful for consumers who want to compare options without submitting personal information that will be stored, and accessible for consumers who have created an account.
Consumer Impact
A questionnaire and tools to check coverage of providers and prescription drugs can limit the plans that consumers have to consider, significantly reducing the complexity of the shopping experience.This in turn reduces the “choice overload” that is endemic to health insurance shopping, increasing the likelihood that consumers will follow through with their enrollment.120 There is a chance that filtering or sorting based on broad usage levels and other limited criteria may in some cases hide or deprioritize plans that a consumer would prefer, leading them not to purchase any plan.121 However, the impact of reducing choice overload is significant enough that the impact on coverage is expected to be positive overall.
These tools can also have a positive effect on affordability by helping consumers make a cost comparison that incorporates estimated out-of-pocket expenses as well as premiums. Research on consumers’ Medicare Part D choices found that beneficiaries placed more weight on premiums than out-of-pocket costs and spent an average of $300 more than the cost of the lowest-cost plan covering their prescription drugs.122 Studies have consistently found that the order in which options are presented impacts choices.123 Sorting plans by estimated total annual cost could drive consumers toward plans with lower total cost, even if premiums are higher.
Utilizing an intake questionnaire would also have a positive health equity impact. The burden of the marketplace shopping experience is largest for marginalized populations, with limited time, higher stress and cognitive load, and on average lower levels of literacy with health insurance terminology.124 Reducing the complexity of the shopping process helps ease the burden on these consumers. However, the health equity impact of improvements to the SBM’s web interface is limited, as many populations, including immigrants, migrant workers, and rural residents work with community-based organizations and navigators or use the call center to choose and enroll in an insurance plan.
CLEAR CHOICE PLANS | 31
i Ideally, the coverage tier and copay would also be shown for each listed prescription drug and provider. Washington Healthplanfinder displays the formulary tier for each prescription drug that is selected, and each plan listing includes the copay for generic drugs, but copay information for other tiers is not shown.
Figure 3. Plan listing with Smart Choice marker and provider and prescription coverage indicators, Washington Healthplanfinder125
State Feasibility
Designing and implementing an intake questionnaire for SBM consumers is generally feasible. In our interviews, both carriers and consumer advocacy groups voiced support for these types of tools. Development of the questions themselves, particularly the health care usage levels used for estimating total annual cost, should be done in consultation with stakeholders and consumers to ensure that the options are representative of real usage patterns and that ease of use and understanding are high.
Costs for this feature are not likely to be a hindrance, as the RFP specifically requires tools for provider and formulary lookup and for estimating total annual cost.126 Accurate and up-to-date information on provider networks and formularies will be necessary for these tools to be successful.
Recommendation 2: Build a comparison tool that: (1) automatically highlights differences between selected plans, and (2) includes a “Compare to Other Standard Plans” function.
Comparison tools are an important marketplace feature and present an opportunity to leverage the simplicity and comparability of standardized plans.The FFM and SBMs that we reviewed allow comparison across three user-selected plans, with core plan features listed at the top, followed by many expandable categories to refine the side-by-side analysis (see Figure 4 below). The detailed information in these categories, while crucial, can have diminishing returns, as decision support tools are less useful when they include too many categories of comparison.127
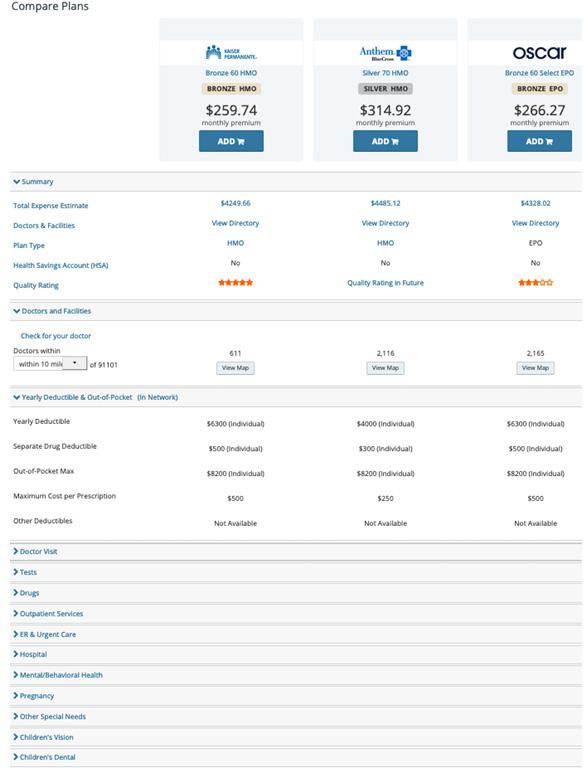
32 | CLEAR CHOICE PLANS
Figure 4. Comparison Tool in Covered California128
Highlighting plan differences within the comparison tool would address this issue, by focusing consumer attention to the most relevant points. Similarly, allowing consumers an option to navigate to a pre-filled comparison of similar Clear Choice designs after selecting one such plan for more details would mimic common practices from e-commerce sites.ii
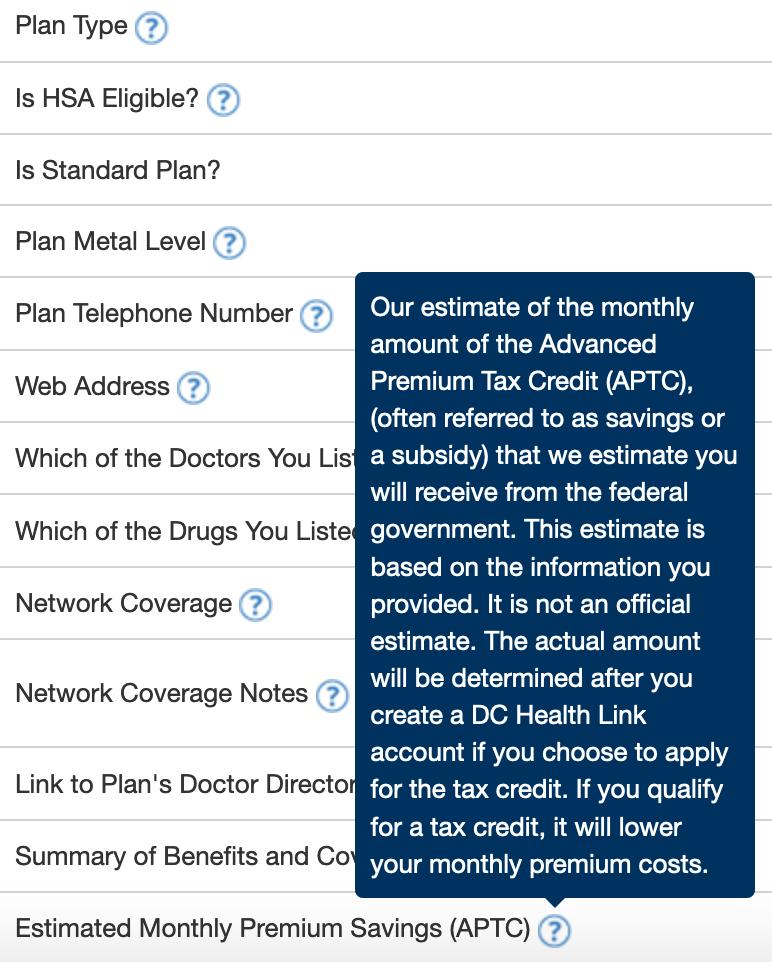
Our review of the eight SBMs with standard plans did not find another marketplace that offered either of these features. Consumer advocates and one carrier that we spoke with suggested that these features would place the Maine SBM among the best marketplaces in terms of helping consumers understand how plans differ in formulary, provider networks, and total expected cost.
Consumer Impact
Our suggestions will simplify the shopping experience. Both features would reduce the number of clicks consumers using the online SBM would need to identify plan differences. These simplifications also might make it more likely that consumers complete the enrollment process. They also facilitate finding appropriate coverage.When consumers can easily identify plan differences, they are better able to select the right plan for their health needs and financial situation. This is particularly important to improve health equity. Reducing complexity in the insurance purchasing process would help all consumers, but especially historically marginalized groups who are less likely to be insured.129
State Feasibility
Maine’s RFP for an SBM technology platform vendor already calls for “clearly displaying standard features of plans, and emphasizing points of comparison.”130 This language allows for the technical features we suggest. In addition, stakeholders did not offer any indication that they would oppose this. Most were enthusiastic about the options that clarify the insurance enrollment process, including improving plan comparison tools.
Recommendation
Several of our stakeholder conversations revealed that the accessibility of the SBM to all groups in Maine is
a critical health equity issue. One suggestion from the meetings was to improve visual cues that explain technical insurance vocabulary. Several SBMs include a popup glossary feature. The most common appearance is a question mark next to the term of interest (see Figure 5).
Including this feature on Maine’s SBM will help consumers decide among Clear Choice design plans by explaining which plan aspects are the same and which are different.
Consumer Impact
This display will improve health equity. Our conversations with patient advocates revealed that the specialized vocabulary of health insurance is a barrier to enrollment even when customers are eligible for significant subsidies. While several SBMs have collapsible pop-up glossaries for this jargon, we did not encounter any that offered an audio reader capability. Oregon and Vermont offer a potential model of a similar feature. Both states have plan comparison tools using the Consumer Checkbook platform, which offers an icon for brief explanatory videos next to technical terms. An
ison could either be between plans of the same design, with the same carrier, with different network types, or plans of the same design and network type across carriers.
CLEAR CHOICE PLANS | 33
3: Include a pop-up glossary feature when customers hover over a technical term, and enable screen reading audio capability for accessibility.
ii Since each Clear Choice design can be offered by every carrier, with up to three variations with different network types (HMO, PPO, and POS), this automatic compar-
Figure 5. Pop-up glossary on the DC HealthLink comparison tool131
audio feature would be particularly useful for customers who are visually impaired. Including multi-language capability for this tool would be an important improvement for health equity as well.iii
The feature will also reduce complexity. Including explanatory language helps make the shopping process simpler, regardless of whether a consumer opts for a Clear Choice plan.
State Feasibility
The RFP for the technology platform vendor includes “plan comparison and consumer decision support tools.”132 We believe that a pop-up glossary is a useful and important consumer decision support tool that falls under this category. Since other SBMs have similar features, the vendor may be familiar with this function. In addition, stakeholders did not offer any indication that they would oppose this. Most were enthusiastic about options that clarify the insurance enrollment process, such as clear definitions, visual elements, and high-quality translation. Advocacy groups we spoke with further recommended making it easy for consumers shopping on the SBM to contact someone by phone with questions by prominently displaying contact information and engaging with trusted community organizations to provide this assistance.
Recommendation 4: Distinguish Clear Choice plans with naming, visual cues, sorting, and/or filtering.
For consumers to make informed decisions based on the characteristics that set Clear Choice plans apart
from non-standardized plans, or to select Clear Choice plans for an apples-to-apples comparison, they must be able to identify Clear Choice plans. This can be accomplished in multiple ways, separately or in combination.
First, some states with standardized plans include the plan’s standardization status in the plan title. Naming conventions include “ST” in New York; “Standard” in Connecticut, Massachusetts, and Oregon; and “Cascade” in Washington, where standardized plans and public option plans have together been branded as Cascade Care.133 A limitation of this approach is that consumers may not pay much attention to the plan name or be aware of its meaning.134
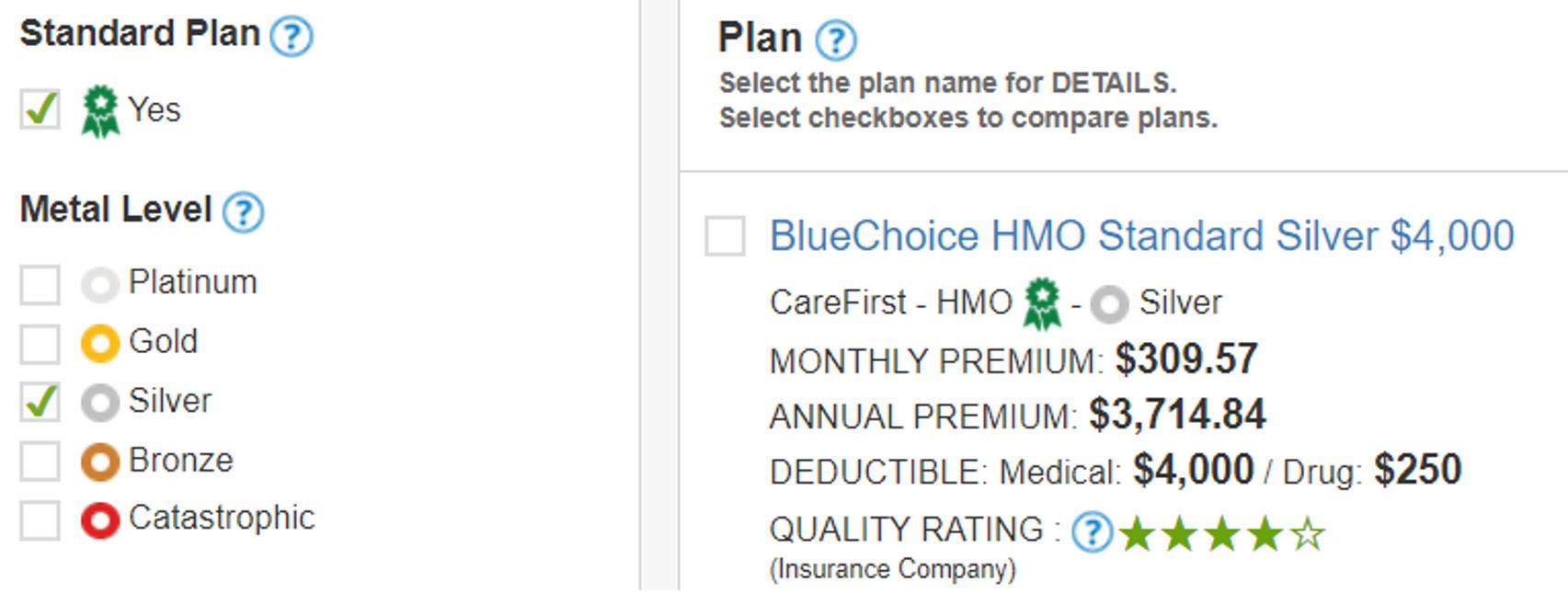
Another option is to use a visual element such as a badge or flag to mark standardized plans. DC HealthLink is the only SBM that does this (see Figure 6).135 In other SBMs, similar elements are used for other purposes: Massachusetts uses a “Network Alert” flag to mark plans with narrow networks, and Washington places a “Smart Choice” badge on plans that are suggested based on users’ reported health care usage. In both cases, hovering over the flag or badge brings up an explanation of its meaning.136 An element like this could both signify that a plan has a Clear Choice design and communicate to consumers what that designation means.
Thirdly, Clear Choice plans could be distinguished through the default sorting in the plan listings, so that they are shown first, with non-standardized plans below. This is not something other states currently do, but Massachusetts used to take a similar approach in
137
See: https://data.census.gov/cedsci/table?g=0400000US23&tid=ACSDP5Y2019.DP02
34 | CLEAR CHOICE PLANS
iii We suggest offering this tool in the most 5 common primary languages for non-native English speakers. U.S. Census data shows 6.1% of Mainers speak English as a second language, and 1.5% of Mainers report speaking English at a less than fluent level.
Figure 6. Standard Plan ribbon icon and filter on DC HealthLink’s Plan Match tool
which standardized plans were displayed first and consumers had to click to view non-standard plans. Lastly, an option to filter for Clear Choice plans could be added, like the “Standard Plan” filter in DC HealthLink’s Plan Match tool (see Figure 6).138 This would allow consumers to more directly identify plans that share the same design across network types or carriers, so that these can be compared.iv,139 Even with a relatively limited number of plans on the SBM, determining which plans are meant to be comparable may not be intuitive to consumers.
Consumer Impact
All of these options would serve to reduce the complexity of the SBM for consumers. By helping consumers identify high-value plans with low cost-sharing, they could also improve overall affordability and improve coverage. However, because the premiums for Clear Choice plans are likely to be higher than those for non-standardized plans, there is some risk that consumers who are seeking a lower-cost plan may opt out of purchasing insurance if the lower-cost options are
too difficult to find, neutralizing the potential positive impact on coverage.140
Distinguishing standardized plans to encourage consumers to consider them could have a positive impact on health equity in Maine by reducing the burden of the shopping experience, which is disproportionately high for marginalized populations because of time constraints and cognitive load.141 However, the health equity impact would again be limited as many Mainers opt to use the call center or work with an assister rather than using the SBM web interface.
State Feasibility
The feasibility of these options is generally high. Stakeholders expressed support for clearly differentiating Clear Choice plans, and while these features may add slightly to the complexity of developing the SBM technology platform, ongoing costs from updating or maintaining these features would be minimal. Ultimately, the feasibility of these features depends on whether the vendor contract is flexible enough to incorporate them without significant revision or added cost.

CLEAR CHOICE PLANS | 35
iv Carriers can offer a PPO, HMO, and POS version of each Clear Choice design.
Auto-Renewal

The potential transition to an SBM could present opportunities to rethink policies around automatic re-enrollment (“auto-renewal”). Broadly, the existing policies governing auto-renewal in the FFM have been adopted by states with SBMs. However, Maine officials could use this opportunity to leverage auto-renewal policies to advance the policy goals of accessible and affordable health insurance.
This section explores current auto-renewal policies and how the State of Maine could expand their impact under an SBM. First, we provide an overview of the purpose and current state of auto-renewal policies, as well as possibilities for change. We then detail five policies Maine could implement and the potential impact and feasibility of each.
As the State considers its approach to policies around auto-renewal, we recommend the following:
1. Design more consumer-friendly auto-renewal notices.
2. Set the default for consumers eligible for cost-sharing reductions to high-value silver plans.
3. Auto-renew consumers with discontinued plans into Clear Choice plans.
4. Explore using auto-renewal defaults to incentivize carriers to lower costs.
5. Consider allowing consumers to choose their auto-renewal priorities.
Background
Auto-renewal policies create a backstop to provide consumers continuity of insurance coverage if they do not actively re-enroll through the marketplace during open enrollment. The ACA envisioned active consumer engagement in marketplace enrollment, providing consumers an annual opportunity to find a health insurance plan that best fits their health care and affordability needs.
However, despite the benefits of active shopping, a portion of consumers do not do so. Reasons for this behavior could include limited time, indifference about their plan, insufficient information about open enrollment, or the complexity of shopping.i They could also
be satisfied with their current plan despite changes that may have been made or the availability of new attractive alternatives. Consumers historically marginalized by the health care system, such as those with lower incomes or living in highly rural areas, may face higher barriers to actively re-enrolling.
Insurance carriers, consumer advocates, and government officials alike recognize that auto-renewing people into plans provides an important backstop to help consumers maintain their health insurance coverage if they do not actively search and enroll in a plan each year.
In 2019, 30% of Maine residents who re-enrolledii in the marketplace for 2020 relied on auto-renewal.142 On average in 2018, 29% of re-enrollees on the FFM and 38% of re-enrollees on SBMs relied on auto-renewal instead of actively re-enrolling into a plan.143
Auto-renewal policies provide consumers continuity of coverage by auto-renewing consumers into the same plan or with the same carrier. At the same time, auto-renewal policies provide carriers some certainty that they will retain a percentage of consumers regardless of changes carriers make to those plans. This reduces carriers’ incentives to provide higher-quality plans and/or to offer plans at lower costs in order to compete with other carriers.
Current Auto-Renewal Policies
The enabling regulations of the ACA lay out the hierarchy by which auto-renewal takes place on the FFM. Each existing plan is mapped to a plan for the following year, a process known as “crosswalking.” FFM auto-renewal policies prioritize defaulting consumers into the same plan or, if not available, the most similar plan available with the same carrier and metal tier.iii If the same carrier stops offering any plans in the same metal tier or exits the market entirely, consumers are defaulted into the most similar plan available with another carrier. States that operate SBMs have so far adopted the same or similar auto-renewal policies.
Consumers who purchase an insurance plan on the FFM typically receive two notices by mail regarding auto-renewal before the start of the OEP.144,iv One is a
i Research has shown that consumers are prone to status quo bias, which may result in them staying with their initial insurance plan even if prices change or if new options that better fit their needs become available. Taylor, Erin Audrey, Katherine Grace Carman, Andrea Lopez, Ashley N. Muchow, Parisa Roshan, and Christine Eibner, Consumer Decisionmaking in the Health Care Marketplace. Santa Monica, CA: RAND Corporation, 2016. https://www.rand.org/pubs/research_reports/RR1567.html.
ii CMS uses the term “re-enroll” to mean people who were in the marketplace last year and still are, as opposed to new enrollees.
iii Carriers are tasked with creating the crosswalk for their plans, including which is most similar in the event an existing plan is discontinued for the subsequent year. This crosswalk is subject to review by the Bureau of Insurance.
iv While the two-notice system can create confusion for consumers and is not ideal, it is unlikely that a single notice would be possible given federal laws regarding renewal notices
AUTO-RENEWAL | 37
redetermination notice sent by the marketplace and covers what actions the consumer must take to receive their subsidy, if eligible, for the subsequent year. The other is a renewal notice sent by the carrier; it details the plan into which the carrier will auto-renew the consumer, any changes to the plan relative to the consumer’s plan from the prior year, and the premium after applying any APTC based on the income on the consumer’s tax returns from the previous year.The FFM requires carriers to use the FFM-developed templates for renewal notices to FFM consumers. However, states are able to develop state-specific notices so long as the notices include all of the essential information required by the federal notices.145
Designing New Auto-Renewal Policies
While auto-renewal policies have historically existed to provide continuity of coverage for consumers, they could be more tailored to consumers’ needs and potentially increase affordability.

A key challenge of designing auto-renewal policies is that there is significant variation in consumer preferences regarding plan choice along numerous dimensions, including affordability and coverage. Some stakeholders suggested that preferences vary substantially based on the circumstances of consumers, such
as their age, the providers available in their area, and health care utilization. The State of Maine should also ensure its auto-renewal policies are inclusive of the varying needs of a diverse population. One stakeholder indicated that current renewal policies often result in consumers paying more for the same benefits instead of paying the same amount for fewer benefits.
Maine’s Clear Choice plans will create standardization of benefits and the copays, deductibles, and coinsurance for these benefits. These could allow for more innovative auto-renewal policies because they reduce the variation between plans and make crosswalking more straightforward. Additionally, Maine officials can explore ways to use auto-renewal policies to increase enrollment in Clear Choice plans.
As we interviewed stakeholders to ask about auto-renewal policies, many offered comments about auto-renewal notices, while providing less feedback on broader auto-renewal policy changes. In particular, stakeholders had little to say about using auto-renewal to incentivize carrier behavior or allowing consumers to select their default options. As such, stakeholder perspectives may change once they more fully consider the implications of such a policy change on their business models and/or the experience of consumers.
38 | AUTO-RENEWAL
Recommendation 1: Design auto-renewal notices to be more consumer-friendly.
As described earlier, the marketplace and carriers mail consumers notices in advance of open enrollment. In addition to providing detailed information about auto-renewal, these notices present an important opportunity to encourage consumers to actively shop for plans.
Several consumer advocates interviewed raised concerns that consumers struggle to understand auto-renewal notices. Maine officials should ensure the notices provide clear and succinct information to consumers. The following section lists feasible changes that could be made to improve notices.
Policy Considerations
1. Encourage active shopping by including information about comparable Clear Choice Plans on the redetermination notice.
The redetermination notice offers an opportunity to encourage active shopping. Maine could provide basic details about the two or three Clear Choice Plans most similar to the consumer’s current plan.This could encourage consumers to actively shop, especially if another carrier clearly offers a better plan at a similar cost or a similar plan for a lower cost.
2. Leverage consumer engagement opportunities for feedback to make notices clearer.
Consumer advocates suggested changes such as using plain language, translating the notice into other languages, and shortening the length.v They also suggested more clearly communicating any changes to consumers’ plans. For example, one stakeholder recommended that carrier auto-renewal notices emphasize when a consumer’s current providers move out-of-network. Proposed changes should undergo user testing before being adopted.
3. Pair mail notices with digital notifications.
E-mail notifications could allow consumers to click on a link that takes them directly to the marketplace, facilitating active re-enrollments. In addition to the mailed notices, Maine could consider defaulting consumers into e-mail notifications and allowing consumers to opt out. This approach would help to ensure that con-
sumers do not miss critical information and deadlines. Further, this would be an additional way to reach individuals who do not have a permanent mailing address, move frequently, or check their mail less frequently due to the use of PO boxes.
4. Maintain the current timing of notices.
Currently, auto-renewal notices must be sent by the end of October so that consumers are aware of their auto-renewal status before the start of open enrollment. Some stakeholders recommended giving consumers information earlier, while others worried that sending the renewal notice too early would undermine the ultimate goal of encouraging consumers to actively shop during open enrollment. The existing timeline is likely the best path forward to ensure consumers are informed about how auto-renewal might change their plans, while also keeping the notification close enough to open enrollment to encourage active shopping. Sending digital notices as well as mail notices could mitigate the risk that auto-renewal notifications reach consumers after the start of the OEP.
Consumer Impact
Providing consumers clearer auto-renewal notices and access to translated notices will decrease complexity for consumers in understanding their auto-renewal policies and could advance health equity by targeting messaging towards communities that have historically struggled to enroll in coverage. For instance, sending both mail and digital notifications could more effectively reach those who lack stable housing and may miss mail notifications. Working with consumer advocacy groups on these changes would likely further advance health equity by centering community needs in decision-making processes. If consumers have a clearer understanding of the plans they will be auto-renewed into, and auto-renewal notifications encourage them to actively shop, consumers may be more likely to select more affordable plans that meet their coverage needs.
State Feasibility
Improving auto-renewal notices is highly feasible, as the cost to improve notices should be minimal. Almost all stakeholders interviewed, including carriers, thought that auto-renewal notices should be clearer. Developing new notification guidance in consultation
v In June 2020, HHS published a final rule on Section 1557 of the ACA regarding Non-Discrimination Regulations. These regulations eliminated requirements that non-discrimination notices must include the availability of language assistance services and taglines in the top 15 languages spoken by individuals with limited English proficiency in the state. (Musumeci, MaryBeth, Jennifer Kates, Lindsey Dawson, Alina Salganicoff, Laurie Sobel, and Samantha Artiga. “The Trump Administration’s Final Section 1557 Non-Discrimination Regulations Under the ACA and Current Status”. 18 September 2020. Kaiser Family Foundation. https://www.kff.org/racial-equity-and-health-policy/issue-brief/the-trump-administrations-final-rule-on-section-1557-non-discrimination-regulations-under-the-aca-and-current-status/)
AUTO-RENEWAL | 39
with consumer advocacy groups may take some resources initially, but would not generate ongoing costs.
Recommendation 2: Set the default for consumers eligible for cost-sharing reductions to the high-value silver plans.
Under the ACA, consumers between 138% and 250% FPL are eligible for cost-sharing reductions (CSRs), in addition to receiving subsidies.vi For most eligible consumers, plans that incorporate CSRs are only available at the silver tier and have the same premium as nonCSR silver plans.vii Known as “high-value” silver plans, these plans have an actuarial value of 94% for consumers between 138% and 150% FPL, compared to 70% for a non-CSR silver plan and 80% for a gold plan.
Because high-value silver plans and the lowest-cost silver plans have the same premiums within carriers, there is a risk that CSR-eligible consumers purchase a silver plan that does not give them the highest actuarial value at that premium. The State of Maine could create an auto-renewal policy that requires carriers to auto-renew CSR-eligible consumers under 250% FPL into the carrier’s high-value silver plans, unless they are enrolled in a gold plan that has a lower premium.viii
Consumer Impact
This policy would be highly beneficial to CSR-eligible consumers because it would ensure they are receiving higher-value plans with lower out-of-pocket costs for the same premiums. Since all carriers are required to offer high-value silver plans, consumers would keep their carriers and there would be minimal disruption to consumers’ continuity of coverage.This policy could improve health equity because it specifically targets low-income, CSR-eligible consumers to ensure they receive the financial subsidies to which they are entitled.
State Feasibility
This should be highly feasible because it will not increase costs for the State, carriers, or consumers. With regard to operational feasibility, carriers will need to map a separate crosswalk for the CSR-eligible consumers and submit it to the Bureau of Insurance
(BOI) for oversight and review, but this should present minimal additional burden.
Recommendation 3: Auto-renew consumers into Clear Choice plans when carriers discontinue non-standardized
plans.
When Maine shifts to Clear Choice plans, all carriers will have to discontinue a majority of their existing plans, as they will only be allowed to offer three non-standardized plans in addition to the Clear Choice designs.ix Maine officials could consider creating an auto-renewal policy that requires defaulting consumers enrolled in any discontinued plans into standardized plans. Over time, this practice may further advance the State’s goal of bringing more consumers into plans that offer more comprehensive coverage and lower cost-sharing than non-standardized plans are likely to have.
For the purposes of the one-time shift to Clear Choice plans, any consumers under 250% FPL could be auto-renewed into the lowest-cost high-value Clear Choice silver plan with the same carrier. Consumers above 250% FPL should be renewed into the lowest-cost Clear Choice plan with the same carrier at the same metal tier.
Consumer Impact
This policy could increase affordability and coverage for consumers because Clear Choice plans are intended to create a set of marketplace offerings across which carriers compete on the basis of price and quality.
State Feasibility
This policy should be highly feasible to implement, as it would have minimal operational and financial costs. This policy presents an opportunity to increase the use of Clear Choice plans, which are supported by many consumer advocates. Carriers, who have voiced opposition to standardized plans generally, may not support this policy.
vi While the Trump administration ended cost-sharing payments to carriers, the silver plans that automatically reflect cost-sharing reductions are still required to be offered to those eligible.
vii American Indian/Native Alaskan enrollees can receive cost-sharing reductions for any metal level plan purchased through the Marketplaces.
viii There are instances where the gold plan costs less because of silver-loading.
ix A non-standardized plan can only be offered in a service area where the carrier offers at least one clear choice design plan at the same tier. (Maine State Legislature. “Public Law, Chapter 653 = 129th Maine Legislature. “An Act to Enact the Made for Maine Health Coverage Act and Improve in Maine”. http://legislature.maine.gov/legis/ bills/bills_129th/chapters/PUBLIC653.asp)
40 | AUTO-RENEWAL
Recommendation 4: Explore using auto-renewal defaults to incentivize carriers to lower costs.
Maine officials could create policies that incentivize carriers to lower costs for consumers—whether through premiums or out-of-pocket costs like deductibles, copays, and coinsurance. Consumers may face fewer sharp increases in premiums and out-of-pocket costs if carriers compete on price to capture a higher share of auto-renewals. Conversely, a strict focus on cost may harm consumers reliant on their current plans for continuity of care and encourage carriers to offer narrower networks to create lower-cost plans. Additionally, if consumers are often shifted to other carriers, this could disincentivize carriers from investing in preventive care that would likely save costs later. Therefore, the State should identify opportunities to set auto-renewal defaults that could incentivize carriers to lower prices while maintaining consumers’ existing level of coverage.
Few other states have used auto-renewal policies to incentivize carriers to lower their costs. When consumers lose their eligibility for the Massachusetts ConnectorCare subsidy, they are mapped to the lowest-cost silver plan, instead of the most similar plan, if neither their current plan nor any other plans from the same carrier are available. Florida identified two options for implementing cost-reduction defaults for auto-enrollment into Medicaid managed care.146 However, this is only possible because people sometimes enroll in Medicaid without selecting a carrier. In the marketplace, all consumers must actively select a carrier.
Policy Considerations
We identified the following circumstances under which defaulting consumers into lower-cost plans could be appropriate.
1. When consumers age out of their catastrophic plans
Currently, consumers can buy catastrophic plans if they are under the age of 30 or have a hardship or affordability exemption. Maine officials could consider auto-renewing consumers who age out of their catastrophic plans into a plan based on cost, regardless of carrier. This policy would impact relatively few Maine residents; in 2019, 965 marketplace enrollees, or 1.3% of all Maine enrollees, chose catastrophic plans.147
When the State shifts to standardized plans, any consumers under 250% FPL and previously in catastrophic plans should be auto-renewed into the lowest-cost high-value silver Clear Choice plan, regardless of carrier. Consumers above 250% FPL and previously in a catastrophic plan should be renewed into the lowest-cost Clear Choice bronze plan, regardless of carrier.
2. When consumers lose APTC subsidies because their income exceeds 400% FPLx
Maine officials could consider changing the default auto-renewal for consumers who lose eligibility for subsidies (due to increased income) to the lowest-cost Clear Choice plan within the same metal level, regardless of carrier.
3. When no plans are available from the same carrier in the same metal level
If a carrier discontinues a consumer’s plan and does not offer other plans in the same metal level, current FFM policies allow carriers to renew these consumers into a different metal level. Maine officials could consider a policy that instead auto-renews these consumers into the lowest-cost Clear Choice plan available in the same metal level, regardless of carrier. This would be relatively easy to implement, but would likely have a limited impact because the participation by the three carriers in Maine’s individual market has been relatively steady across the state’s regions since the introduction of the reinsurance program.
Consumer Impact
Each policy consideration laid out above could increase affordability directly for a relatively small subset of consumers by defaulting them into plans with a lower total cost while incentivizing insurers to lower costs in order to increase their market share. However, these policies risk interrupting a consumer’s continuity of care if the default shifts change the consumer’s carrier. Defaulting all consumers into Clear Choice plans (Recommendation 3) would ensure a minimum standard into which consumers are defaulted.
State Feasibility
This policy should be highly feasible to implement, with minimal operational and financial costs. Implementing such a policy may require the BOI to be more involved in developing auto-renewal crosswalks, as some consumers would be crosswalked into a different carrier. In instances where consumers would be auto-renewed
x This policy should not be extended to consumers under 400% FPL who lose subsidies based on the price of plans they select. That could lead carriers to increase premiums so that more consumers receive subsidies and thus are not auto-renewed into lower-cost plans.
AUTO-RENEWAL | 41
to a different carrier, clear notices would be critical to communicate this change.
Carriers may oppose one or more of these options if they anticipate it would cause them to lose consumers. Consumer advocates could support these changes, provided that plan and carrier changes are clearly communicated.
Recommendation 5: Allow consumers to choose their auto-renewal priorities. Currently, the default on the FFM is for consumers to be automatically renewed in their existing plan, if it is available, and to keep consumers with their existing carrier even if their current plan is discontinued. Consumers are not able to change this default on the FFM; to date, no SBM has implemented policies that would allow consumers to choose how their auto-renewal default is selected. In 2019, 57% of Maine consumers who chose to actively re-enroll selected a different plan.xi It may be worth conducting a study of consumers’ motivations to actively switch into other plans to better understand what factors influence this choice.
Maine officials could consider creating a system for consumers to set their own auto-renewal preferences. For example, the SBM could have a webpage where consumers can rank, review, and change their auto-renewal preferences any time until October 1.xii Preferences consumers could rank might include the following examples:
• Staying in the same plan, with the same carrier, as they selected the previous year
• Staying with the same carrier they selected the previous year
• Maintaining continuity of in-network providers
• Maintaining the same level of coverage received under their current plan
• Prioritizing lower total costs
• Prioritizing lower premium costs
• Prioritizing lower deductible and out-of-pocket costs
All auto-renewal selections would remain within the same metal level as the previous year’s selection.xiii
Policy Considerations
Before implementing this policy, Maine officials should gauge consumer interest in changing their auto-renewal defaults by surveying a random selection of marketplace enrollees. The survey could ask consumers to rank their preferences and ask whether they would prefer to be auto-renewed into their current plan or a plan based on the criteria they selected. If there is little or no interest, the State may not wish to proceed.
If Maine officials implement this policy, they will have to consider the level of aggregation and the timing for sharing consumer preferences with carriers. We suggest that only aggregate numbers be shared to prevent cherry-picking. It would make sense to share the information on a timeline that will influence carriers’ decision-making for the next year’s plans.The State will also need to consider when and how to encourage consumers to indicate their auto-renewal preferences.
Consumer Impact
This option would allow consumers to select an auto-renewal policy based on their priorities around health care coverage. Consumers with lower health care utilization looking to choose lower-cost plans could opt to be automatically renewed into the most affordable Clear Choice plan at their metal level, instead of defaulting into their current plans.
This option could also lower costs for consumers by incentivizing carriers to compete on both price and quality. One carrier indicated that they heavily rely on passive auto-renewals, as it is more affordable to keep a customer than to enroll a new one. Providing this option may lead carriers to reconsider their plan offerings and pricing strategy, depending on consumer preferences.
Giving consumers more choices increases complexity. One concern might be that consumers may not understand the implications of their auto-renewal selections and select cost as their top priority without realizing it could jeopardize their coverage. Consumer advocacy groups we spoke to often supported the idea of centering consumer decision-making but raised concerns that this could add complexity or disincentivize shop-
xi The rate for the FFM more broadly was lower at 46%. Maine’s rate may be higher because of Anthem’s re-entry into the marketplace. Center for Medicaid and Medicare Services. Source: “2019 and 2020 Marketplace Open Enrollment Period Public Use Files” April 2, 2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/ Statistics-Trends-and-Reports/Marketplace-Products/2020-Marketplace-Open-Enrollment-Period-Public-Use-Files#:~:text=This%20includes%20the%20original%20 2020,enroll%20by%20the%20original%20deadline
xii Many states begin processing auto-renewal determination notices in October; ending the ability to change auto-renewal preference one month before open enrollment ensures that the marketplace and carriers can accurately reflect consumers’ preferences in their renewal notices.
xiii All consumers would be crosswalked into Clear Choice Plans unless they prioritized staying in the same plan they selected the previous year to further the State’s goal to increase enrollment in plans that offer more comprehensive coverage with lower cost-sharing and to reduce implementation complexity.
42 | AUTO-RENEWAL
ping. Concerns about added complexity could be mitigated by making it clear that selecting an auto-renewal preference is optional.
State Feasibility
This option could be difficult and somewhat costly to
implement, as it would require both developing a system to record preferences and conducting consumer outreach. Further, BOI would likely have to take on a larger role in crosswalking plans, as this option creates a high likelihood of cross-carrier auto-renewals.

AUTO-RENEWAL | 43
MaineCare Integration

Transitioning to an SBM could provide the State the opportunity to better integrate the marketplace with MaineCare. Our conversations with state officials uncovered a number of existing technology challenges that stand in the way of seamless FFM and MaineCare integration. Other conversations with external stakeholders identified multiple adverse impacts that applicants experience under the current system and uncovered best practices that SBMs have operationalized to improve their application and determination processes.
This section outlines our key findings and recommendations for delivering an SBM that is well-integrated with MaineCare and well-placed to help the State deliver on its goals of increased insurance enrollment. Our recommendations for Maine officials working on the SBM transition are the following:

1. Use existing state data to target and personalize outreach to facilitate enrollment.
2. Resolve consumer-facing bottlenecks in MaineCare and SBM enrollment.
3. Conduct a joint strategic planning effort across DHHS.
Background
One of the key principles of marketplace design outlined by the ACA is the principle of “no wrong door.”148 A resident should be able to log on to HealthCare. gov or their state’s marketplace and be enrolled in Medicaid if they meet their state’s Medicaid income and eligibility requirements. In addition, a resident that applies for and is denied Medicaid coverage should be referred to the marketplace for coverage.
Maine is an assessment state, meaning that the FFM makes an initial assessment of whether applicants are eligible for Medicaid, and then refers these applications to OFI for a final determination. Assessment states on the FFM can have difficulty making timely use of data associated with Medicaid referrals coming from the marketplace, which can result in a disjointed application process for consumers. Conversely, when states refer individuals denied Medicaid to the FFM, it is difficult for states to determine whether those consumers acquired coverage. States that operate SBMs typically have better integration with their Medicaid offices, and are better equipped to deliver upon the objectives of “no wrong door.”
Managing populations that experience changes in coverage, otherwise known as “churn,” is another key challenge that requires close integration between the marketplace and Medicaid. Poor integration between systems can increase the administrative burden experienced by state agencies and marketplace staff that oversee churn and lead to delays or barriers for Mainers seeking coverage. A 2016 study found that one in four individuals with household incomes below 138% FPL experienced a coverage change—this figure was consistent between participating expansion and non-expansion states.149 Adverse impacts of churn from Medicaid to the marketplace are well-documented, and these impacts can be exacerbated if the State cannot assist individuals through coverage changes in a timely manner.150
MAINECARE INTEGRATION | 45
Figure 7 describes the ideal setup for SBM and MaineCare integration from the consumer perspective. In this setup, consumers are able to easily navigate and access the insurance plan most appropriate to their eligibility status.
Ideal Setup
for SBM and MaineCare integration for consumers
Consumer seeks health insurance
If needed, obtains assistance
(e.g., from an assistor, navigator, or community-based organization that works closely with DHHS and has access to enrollment status details online)
Consumer applies for insurance somewhere
State determines eligibility:
NO WRONG DOOR
State seamlessly redirects consumers to the appropriate health plan based on their application details
Consumers (and their assisters) are notified promptly and clearly regarding status updates
Consumer is enrolled and insured under the appropriate plan
(e.g., MaineCare or the SBM with subsidies)
Later, if the consumer’s eligibility changes (e g , due to a change in income), they are notified, assisted, and enrolled in a more appropriate plan
Efficient processes for handling churn

Repeat process as needed
Existing roadblocks prevent Maine from achieving this ideal SBM/MaineCare setup:
• Enrollment assisters currently cannot easily view the application or enrollment status of an individual they are helping.
• There is an opportunity for DHHS to work more closely with enrollment assisters to identify enrollment bottlenecks and foster longer-term collaboration
• Currently, consumers have to determine whether to apply for MaineCare or enroll through the marketplace Sometimes, consumers applying through the ‘wrong’ door have to repeat the process again for the ‘correct’ door, after waiting to learn whether they have been denied by the first door This is currently the case for individuals deemed ineligible for MaineCare by OFI, who then need to initiate their own application for the marketplace
• Other states, including California and Massachusetts, have a single application portal for both Medicaid and their SBM, allowing these states to more seamlessly move consumers to the appropriate program
• In early 2018, approximately 3 in 4 MaineCare applicants waited longer than a month for their applications to be processed, after which they were notified of the result via mail
• There are concerns about whether FFM enrollees are being notified promptly that they could be eligible for MaineCare if they experience a drop in income
• The potential transition to an SBM is an opportunity to streamline churning processes and ensure Mainers are enrolled in the best coverage for their needs, including leveraging data to predict candidates likely to experience churn
46 | MAINECARE
INTEGRATION
Figure 7: Ideal setup for SBM and MaineCare integration for consumers
Box 1: MaineCare application processing times
When Medicaid and marketplace systems are not well-integrated, consumers seeking coverage can experience long delays and breaks in their enrollment journey. There is currently room for improved integration between OFI and the marketplace, and an SBM could add significant value for residents and state agencies. This box presents aggregate administrative data on Medicaid application processing times to highlight opportunities for improved integration and efficiency.
Slow processing of FFM referrals
At our request, OFI provided us with data on Medicaid application volumes and processing times broken down by source for 2018.i Table 4 presents this data and demonstrates that referrals from the marketplace face by far the slowest processing times of any application type. OFI stressed that FFM referral processing times reflect the influx of applications the office receives during the OEP. In other words, FFM applications take the longest to process on an annualized basis because, unlike other types of applications, they arrive in large volumes during a brief period of time. While OFI noted that it has been better resourced to handle application influxes in more recent OEPs, the data strongly suggest that there is significant potential for improving integration between the marketplace and OFI’s operations.
Table 4. MaineCare application processing volumes and times, by source (2018)
Delayed processing times can have significant consequences for those on the cusp of MaineCare eligibility. Four in five referrals from the FFM face wait times for applications that exceed the length of the 45-day OEP window. Applicants that are denied coverage through MaineCare and referred back to the marketplace can only enroll there under an SEP and after confirming their eligibility, adding extra steps to the process of securing health insurance.ii
Slow Medicaid application processing compared to national averages
Data on Medicaid application processing times from February through April 2018, presented in Table 5, show that Maine was the slowest of 42 states reporting data.151 As discussed above, slow processing times can adversely affect Mainers who apply for and are denied Medicaid during (or just before) the OEP: individuals must navigate the additional hurdle of proving their SEP eligibility and endure longer delays associated with enrolling.152
Table 5. Medicaid
Feb-April 2018 (“National” includes ME)
Source: “Medicaid MAGI and CHIP Application Processing Time Report.” CMS, November 28, 2018. Accessed December 17, 2020. https://www.medicaid.gov/state-overviews/ downloads/magi-and-chip-application-processing-time/magi-application-time-report.pdf.
i We requested 2018 data because 2019 and 2020 are what we consider “outlier” years: Maine expanded Medicaid in January 2019 and was overwhelmed by applications in the early part of the year, and the coronavirus pandemic has changed the eligibility and determination process for states in 2020. Although 2018 is not the most upto-date reflection of OFI’s operations, processes, and policies—which OFI stressed—we believe it is the most recent calendar year snapshot that offers a glimpse into “business as usual” operations. Other data extracts which cover shorter time horizons (perhaps from mid- or late-2019 through early 2020) may be preferable.
ii We understand that the State has extremely limited visibility into what happens to referrals it makes to the FFM. It is therefore difficult to provide a comprehensive assessment of the integration between the two systems for these referrals.
MAINECARE INTEGRATION | 47
Source Applications Received Days to Process Number Pct. of Total < 1 day 1-7 days 8-30 days 31-45 days 45+ days FFM 10,396 14% 0% 0% 5% 14% 80% In-person 26,342 36% 13% 31% 24% 13% 19% Online 17,220 24% 3% 9% 27% 23% 39% Paper 19,280 26% 0% 12% 25% 24% 39% TOTAL 73,238 100% 5% 16% 22% 18% 38%
Source: OFI
Month < 24 hrs 1-7 days 8-30 days 31-45 days 45+ days Maine Feb 5.7% 3.0% 8.9% 5.1% 77.2% National 30.8% 15.1% 27.2% 8.7% 18.2% Maine March 6.7% 3.4% 10.5% 53.6% 25.8% National 30.0% 15.8% 25.2% 9.3% 19.7% Maine April 7.4% 3.7% 9.9% 55.5% 23.6% National 32.0% 16.8% 25.6% 7.8% 17.9%
application processing times,
Findings
Interviews with stakeholders both directly and peripherally involved in the SBM transition provided the foundation for our recommendations. This section provides a high-level synopsis of key themes that surfaced across stakeholders.
There are clear opportunities for improvement in technological integration between the marketplace and OFI’s systems OFI leadership identified issues that constrain their ability to process marketplace referrals:
• Data quality: The quality of data that OFI receives from the FFM is, in their view, not very high. To compound this problem, it is not easy to get answers from the marketplace on what the data received represents. Specifically, CMS has not identified certain data fields in files it sends OFI which they need to enroll and manage MaineCare members.
• Data formats and systems: Another problem identified by OFI relates to the specific data file formats and structures that OFI receives. The files shared by the FFM do not integrate well with OFI’s Automated Client Eligibility System (ACES), which OFI uses to determine eligibility for MaineCare and other social service programs and which does not yet have the capability to automatically import and process data from an outside source.
• Manual entry: In order to process these marketplace referrals, OFI staff must in every instance perform a “side-by-side” comparison of information they receive from the marketplace and information which they already have on file in their ACES. Differences and data fields are reconciled with manual entry by OFI staff.
• Different eligibility rules: The eligibility systems and rules are not the same between the FFM and OFI, and there are certain pathways (i.e. bugs or loops) where an FFM eligibility check makes a referral to OFI, only for OFI to reject the application and refer it back to the FFM.
Appendix Table 3 highlights best practices for integrating OFI’s operations with SBM systems and assesses the extent to which Maine plans on implementing these practices and other technological improvements. By implementing the practices outlined in the table, Maine could provide its residents with a superior enrollment experience and move towards its stated goal of making more automated, “real-time” Medicaid determinations via the SBM for a significant proportion of applicants.iii This represents a clear example of how
iii SBM RFP states a goal of November 2022 for moving to real-time determinations.
Maine could maximize its SBM work to benefit OFI and MaineCare applicants and members.
One-way and/or bottlenecked communication channels are making it more difficult for the State to reach and better understand Mainers
As illustrated by Figure 7, consumers in Maine still face a number of challenges navigating and accessing the health plans most appropriate for them. Enrollment assisters, which we define to include navigators, assisters, certified application counselors, and community organizations, play a crucial role in supporting these consumers. We have identified a number of opportunities in which the State can partner more closely with these consumer-facing stakeholders to more effectively reach community members.
Competing priorities and unclear decision-making processes create inefficiencies within DHHS
OFI’s duties extend beyond MaineCare and include the screening and administration of four other means-tested programs: Temporary Assistance for Needy Families (TANF), Supplemental Nutrition Assistance Program (SNAP), and Higher Opportunity for Pathways to Employment (HOPE). Although this structure and issue is common in other states, interviewees believe this creates competing priorities for staff, especially for those tasked with ensuring compliance with SNAP’s federal deadlines. This could potentially be one factor in MaineCare’s relatively slower processing time, likely resulting in suboptimal experiences in churn and longer waits for people to receive their eligibility assessment. Compared to previous administrations, there is currently a much deeper focus on customer service and processing times are expected to decrease.
In the context of leading Maine’s potential transition to an SBM, DHHS has key opportunities to better coordinate between OFI and OMS. Both OFI and OMS have been included in planning since initial conversations about the potential transition but advocated for a greater role in future planning. This is more so the case for OMS, which is not directly connected to the FFM and relies on OFI as its liaison. The potential transition to an SBM is an opportunity for DHHS to capitalize on the insights of OFI and OMS and improve the overall health insurance system.
Lastly, when new initiatives are developed be-
48 | MAINECARE INTEGRATION
tween OMS and OFI, the process to determine where additional staff or resources to support those changes come from is unclear. Without establishing clear delineations of resources or a decision-making model for joint efforts, this matter could become even more confusing following a transition to an SBM.
Recommendation 1: Use existing state data to target and personalize outreach to facilitate enrollment.
An SBM technology platform integrated with OFI systems could enable DHHS to present personalized and accurate information about the subsidies Mainers would be eligible for or types of coverage they could receive at no or low cost. This integration could be leveraged when MaineCare members churn off the program.
Beyond churn, Maine officials can take advantage of increased access to individual-level data on marketplace health insurance coverage.iv By combining this marketplace data with existing DHHS data on MaineCare enrollees—and potentially data from other state agencies—DHHS can generate a more comprehensive picture of who is covered in the state and whether certain enrollment gaps exist for specific groups of Mainers, even in the absence of a state mandate.
DHHS could partner with other state agencies, such as the Bureau of Unemployment Compensation and Maine Revenue Services, and arrange for the sharing of individual-level data in order to identify Mainers who are likely eligible for MaineCare or subsidized marketplace coverage, given their reported AGI or change in employment status. Maine officials could then conduct targeted outreach, inviting these individuals to apply for coverage.
There is recent precedent for this work in SBM states: Maryland’s “Easy Enrollment” program, launched this year and outlined in the Enrollment Periods section, asks uninsured state tax filers for their consent to share their information with the State’s marketplace “for the purpose of determining pre-eligibility for nocost or low-cost health care coverage.”153 As of July 2020, of the approximately 41,000 tax filers that consented to data sharing, approximately 9% (3,700) enrolled in either marketplace or Medicaid coverage.154
iv The State may be able to capitalize on this data under the SBM-FP.
Consumer Impact
The vast majority of Mainers who lack coverage are low-income and likely eligible for MaineCare or APTCs. Outreach could reduce complexity that uninsured Mainers face when applying for coverage by directing Mainers to the right “door.” More intensive outreach, such as outbound phone calls, could help Mainers better understand how they stand to benefit and what they need to enroll.
Ultimately, outreach efforts could lead to many more Mainers enrolled in MaineCare or marketplace coverage with subsidies. For instance, if only half of uninsured Mainers with household incomes less than 400% FPL were identified by Maine Revenue Services for outreach, that could produce a list of about 42,000 Mainers who could be contacted. Even modest takeup rates in response to outreach within this group could lead to thousands of additional Mainers insured. Moreover, those who are most likely to change their behavior in response to outreach are typically those that stand to benefit most.
State Feasibility
Conducting this outreach presents a number of obstacles DHHS should consider. Besides getting buy-in from key State stakeholders, legislation would likely be needed to change tax forms and/or enable the sharing of individual-level income tax return data between Maine Revenue Services and the SBM.v This was the case for Maryland’s Easy Enrollment program; legislation creating and supporting the program passed with significant bipartisan support.155
Fully automating the targeting process with high accuracy would likely be difficult, but agencies could likely identify many potentially eligible individuals using personal identifiers common across data sets. Finally, there are naturally costs to outreach activities, and more personalized forms of outreach (e.g., phone calls) are more expensive—but modest forms of outreach should pose fairly limited costs per enrollee added.
Recommendation 2: Resolve consumer-facing bottlenecks in MaineCare and SBM enrollment.
There are a number of opportunities to improve upon the State’s consumer-facing processes. In the nearterm, DHHS should partner more closely with enroll-
v We are not in a position to say confidently whether legislation would be needed. Appendix D of the Report to the Legislature pursuant to Public Law 2019, Ch. 485, February 2020 suggests that only “agreement” is needed between DHHS and Maine Revenue Services for various activities leveraging income tax filings.
MAINECARE INTEGRATION | 49
ment assisters to make it easier to notify and support enrollees who are navigating their way into or across MaineCare and the SBM. In the long-run, DHHS should explore whether to join other states that have set up a “one-stop” application system for both Medicaid and marketplace subsidies.
Dedicate greater resources to solicit feedback from enrollment assisters to identify enrollment process issues.
For instance, officials at OFI noted a data gap relating to a group of consumers they are working to better understand. Specifically, they have little information on the potential enrollees who either never start an application or who open one but never finish it. In our interviews, navigators and community organizations shared insights on this phenomenon that we believe would be useful to DHHS. Several questions and issues were raised in our interviews that we believe merit further study:
• Which qualifying individuals are not completing or willing to enter the current application processes for insurance/benefits, and why? (Possible factors suggested in our interviews include technological and internet access challenges, particularly access beyond mobile devices; language barriers; and the complexity of the enrollment process.)
• What best practices have navigators/groups employed to improve completion rates and conduct effective outreach? What steps can be simplified or streamlined, including in a potential SBM?
• How much is Medicaid Estate Recovery preventing near-retirement aged individuals from participating? (Multiple stakeholders raised this issue.)
As described in the Health Equity Approach and Broader Considerations sections of this report, it is important that efforts to engage community organizations and enrollment assisters not be duplicative, which would be inefficient for state resources and community advocates. For instance, consider if OFI were to hold a meeting or conduct a survey on MaineCare enrollment issues. If SBM staff simply repeat these efforts on marketplace enrollment issues, much of the content may be the same, and an opportunity to understand key overlaps and differences would be missed. Depending on the situation, potential solutions include co-hosting meetings, sharing notes between groups, and ensuring that relevant stakeholders are present at both meetings (e.g., a Director of Health Equity or other health
equity coordination staff).
Improve the notification process for enrollment, especially among churning populations.
According to both state officials and consumer advocates, DHHS can improve how it delivers important notices regarding insurance status, especially among those transitioning between MaineCare and marketplace plans. During Medicaid expansion, OFI noticed a slow uptake rate among new enrollees even after launching a targeted campaign to notify individuals that they could now qualify for MaineCare. OFI staff expressed a keen interest in tackling these issues and have already begun exploring solutions. We further recommend that the State:
• Create a process where enrollment assisters are also notified when an individual they previously assisted needs to take action relating to their insurance status. During enrollment, make this the default selection but allow consumers to opt-out of this feature. For instance, should the State need to notify an individual that they no longer qualify for MaineCare and should enroll in a marketplace plan with subsidies, their prior assister can be alerted and follow up with the individual to support them. This system would be particularly helpful for consumers who face greater barriers to enrollment (e.g., due to language, internet access, and/or their community’s historical relationship with the government) and decrease the number who fall through the cracks as they move out of either program.
• Re-design notices to make them more accessible and easier to understand. According to OFI, the current notification system for those deemed ineligible for MaineCare involves two letters: first, a denial letter from OFI, and second, a letter with opportunities from the marketplace. Moving forward, notifications for both “no wrong door” and churning populations should be streamlined to be more accessible to consumers.vi
Employ user-friendly design principles to make it clear to consumers what is happening with their insurance, what action they need to take, and who they can contact for assistance. Prominently list the direct contact information of enrollment assisters, especially any with whom the consumer previously worked (based on feature above).
List coverage options clearly and up front. Employ
vi According to DHHS officials, OFI recently implemented newly designed notices, for the first time in the two decades since the State began using its Automated Client Eligibility System.
50 | MAINECARE INTEGRATION
social norms and positive language to eliminate stigma associated with enrolling in either plan.156 (E.g., “Like 8 in 10 Mainers, you qualify for subsidies that allow you to enroll in a more affordable health insurance plan. Take five minutes today to update your information through our state health portal.”)
• Diversify the mode of communication, particularly among “no response” individuals. Especially among individuals who do not respond to mailed notices promptly, we recommend also employing email or text message notifications and using proactive phone calls to contact them about action required. This is likely to improve response rates, especially if consumers are able to respond to any of these channels to get in contact with enrollment assistance.
Ensure that an SBM consumer portal and its OFI/MaineCare equivalent are easy for consumers and assisters to access, view, and understand their enrollment status.
According to the State’s RFP, the new SBM consumer portal is expected to have backend data integration with OFI’s systems, which would offer consumers and their enrollment assisters greater visibility into their enrollment status. As OFI designs and builds the replacement for My Maine Connection, it is critical that its own consumer portal also offer the same functionality. Navigators and community groups emphasized the importance of this feature, noting that it could help them more easily monitor and support consumers, especially those with greater access challenges to begin with (e.g., limited internet access or language barriers).
Over the medium to long term, DHHS should explore the pros and cons of Maine adopting a “one-stop shop” where Mainers can apply for MaineCare, APTCs/marketplace plans, and other benefits in a single, unified application.
Other states, including Massachusetts and California, have integrated application and eligibility systems, which allows for easier mixed eligibility enrollment and plan management (e.g., in Massachusetts the state system manages families where parents are on the SBM plan but children are on Medicaid/CHIP at the same time).157 In addition to reducing confusion, complexity, and choice proliferation for consumers, a single eligibility portal can also help to eliminate the stigma or hesitation consumers may have regarding Medicaid that might otherwise prevent them from applying.
On the backend, a single system also means that OFI, OMS, the SBM, and other agencies administering benefits could access and update data in a uniform manner, which would improve coordination between offices. It would also allow for longer-term relationship management between state agencies and Maine residents, especially those in communities that may harbor distrust or skepticism towards government due to negative historical or past experiences.
Consumer Impact
These sub-recommendations will improve “no wrong door” and support churning populations, making it easier for consumers to get enrolled and obtain information from either DHHS or enrollment assisters about which plan is more appropriate for them. Moreover,

MAINECARE INTEGRATION | 51
working more closely with enrollment assisters and community-based organizations to address enrollment issues will particularly help Mainers with higher barriers to health access, including those with historically marginalized identities.
Feasibility
All of these recommendations require buy-in from multiple departments and external organizations, but it appears that stakeholders are on board provided they are given adequate support from DHHS to prioritize these issues among other projects. The bulk of financial costs for these proposals are associated with web portal development and data integration, especially if the State eventually decides to pursue a “one-stop” platform.
Recommendation 3: Conduct a joint strategic planning effort across DHHS.
Given the transformative nature of the potential SBM transition, administrative challenges of serving the churn population, time-sensitivity of providing health insurance coverage, and the number of stakeholders involved, we recommend DHHS lead a strategic planning process. At minimum, this should include MaineCare, OFI, incoming SBM staff, and DHHS leadership. Table 6 summarizes useful topics for a strategic planning process and their anticipated benefits. Facilitating this “big picture” visioning exercise for the SBM transition will provide individual offices with an understand-
ing of how their work fits into the larger mission and goals, increase staff buy-in for new policies, and help cross-pollinate best practices across DHHS.
Along with uncovering insights, a strategic plan could include a work plan and action items that help facilitate better integration between OFI and the SBM. It is critical to dedicate staff to manage the implementation of and communication surrounding this process, and to aggregate and act on the lessons learned. This will allow the plan to remain iterative and adapt to Maine’s shifting health insurance needs.
Consumer Impact
Increased collaboration between Offices holds the potential to create a better consumer experience, especially facilitating a more optimal “no wrong door” experience and a more seamless churning process. Streamlining OMS and OFI’s role in the SBM transition will reduce coverage gaps, particularly for historically marginalized populations, by ameliorating administrative complexity.
State Feasibility
The strategic planning process would require staff time, a precious resource especially during the SBM transition. Though this may present initial challenges to various Offices’ individual priorities, in the long run we do not anticipate it would significantly affect the Department’s capacity.
Table 6. How Strategic Planning Topics Would Benefit the SBM Transition
Planning Topics
Strengths, Weaknesses, Opportunities, and Threats (SWOT) Analysis
Federal forecasting
Data inventory
Decision-making models
Accountability and Evaluation
Benefits for the SBM Transition
• Take stock of individual Offices’ assets and shortcomings
• Coordinate collectively to create a shared vision and markers of success
• Create contingency plans for upcoming Supreme Court decision and anticipate opportunities under Biden Administration
• Compare existing data across Offices, identify opportunities to standardize and exchange
• Pinpoint opportunities to create systems that capture desired data in the transition
• Establish transparent procedures for how decisions are made and how work and resources are distributed in joint DHHS efforts
• Ensure action items from strategic plan are followed through
• Create methodology to evaluate effectiveness of new systems
52 | MAINECARE INTEGRATION
Planning for the Future

This report has highlighted that with an SBM, Maine can build on its successful embrace of the ACA, which most recently includes expanding Medicaid. The State would be uniquely situated to advance effective marketplace policies, ranging from longer open enrollment timelines to more robust connections to MaineCare. Another key asset of an SBM is the opportunity to anticipate and leverage future opportunities for marketplace innovation, particularly as the federal health policy landscape shifts.
As Maine officials engage in the procurement, implementation, and maintenance of the SBM eligibility and enrollment system, we recommend the State prioritize platform capacity to adapt to future policy innovations.
This section first outlines the federal policy environment following the November 2020 election and its implications for Maine’s marketplace. This is followed by an analysis of policy opportunities to improve affordability and expand coverage in light of this new federal policy environment. We conclude our analysis by outlining our recommendation to build out a marketplace platform with nimble eligibility and enrollment structures, which would provide the State the flexibility to pursue policies discussed in the preceding section.
Background
President Joe Biden has demonstrated an eagerness to build on the ACA, centering the landmark health law in his campaign messaging158 and advancing policy proposals bolstering the ACA.159 President Biden has also signaled his pro-ACA policy intentions by nominating Xavier Becerra, who has a history of defending the ACA in court, for Secretary of Health and Human Services.160 The federal legislative landscape is murkier and indicates a narrower path for significant legislative health reforms in the near future.
Regulatory/Administrative Opportunities
Given existing electoral and institutional constraints, in the immediate term the new administration will likely make its mark on the marketplaces through administrative and regulatory policymaking. The Biden administration will likely prioritize work to unwind recent policy changes from the Trump administration, while also considering which longer-standing rules to roll back through the rulemaking process.
For instance, one rule that the Biden administration
may be interested in pulling back is the Trump administration’s latest proposed 2022 Notice of Benefit and Payment Parameters. If ultimately implemented, a number of provisions in this rule could undermine the goals of SBMs, including a new requirement for SBMs to conduct burdensome pre-enrollment verifications for SEPs.161
The Biden administration could also proactively advance their priorities without Congressional involvement by leveraging their waiver authority. In particular, the Biden administration will likely be eager to work with states to use 1332 waiver flexibilities to cover new groups, improve affordability, or provide additional health benefits. Indeed, the Biden administration is expected to work closely with states to identify opportunities that align with both state and federal priorities.
For example, the Biden administration could leverage 1332 waiver authority to advance coverage expansions such as Medicaid buy-in or state-tailored public options. The new administration could facilitate such innovations by expanding its interpretation of the 1332 waiver’s budget neutrality window,162 loosening this financial constraint by allowing states to instead point to long-run savings for the federal government given that public option plans enjoy lower reimbursement rates than commercial marketplace plans. When evaluating state-based public option proposals in the future, Maine could consider how states with similar marketplace dynamics have assessed targeted Medicaid buy-in proposals. One such state is New Mexico, which has grappled with the implications of a public option given a small marketplace population and lower-than-average benchmark premiums.163
The Biden administration could also leverage regulatory policymaking to expand access to health care for both undocumented and documented immigrants. Among the demographic groups that could benefit from actions on this front are the more than 2,000 migrant farmworkers who live and work in Maine, the majority of whom are H-2A visa holders or undocumented, as highlighted by a key stakeholder.164
The new administration could classify Deferred Action as Childhood Arrivals (DACA) recipients as lawfully present and therefore eligible for APTCs, thereby also ensuring coverage opportunities for DACA recipients. Even more impactful, the Biden
54 | PLANNING FOR THE FUTURE
administration could also repeal the public charge rule, which was expanded under the Trump administration to include Medicaid determinations for immigrants seeking permanent citizenship status and which had a chilling effect on immigrants qualifying for marketplace subsidies—despite the fact that subsidies are not within the scope of determinations.165 This could have significant implications for both MaineCare and marketplace enrollment, folding into the risk pool a new population of consumers who data suggest might be younger—and thus would likely be lower utilizers of health care—than the general population.166
Legislative Opportunities
While major legislative changes appear less likely in the immediate future, political dynamics can nonetheless shift in subsequent election cycles. Combined with the potential for sweeping change through Congressional actions, this means that legislative opportunities still deserve careful consideration.
With Democrats now in control of Congress, they can likely pursue a legislative agenda focused on building on the existing infrastructure of the ACA. President Biden’s campaign platform167 and the House-introduced Patient Protection and Affordable Care Enhancement Act168 provide a useful roadmap of likely priorities. Congress could increase the generosity of APTCs by reducing the percentage of income paid to premiums at all income levels. For instance, under the ACA Enhancement Act those with incomes between 100 and 150% FPL would be eligible for no-premium coverage, with the highest premium percentage capped at 8.5% of income for higher earners, including those earning above 400% FPL.
Congress could also improve marketplace affordability by eliminating the subsidy eligibility cliff and allowing households of all income levels to qualify for tax credits.While these legislative policy changes would be driven at the federal level, they would directly impact Maine’s marketplace platform.
President Biden could also work with Congress to lower the Medicare eligibility age to include Americans ages 60 to 64. Such an expansion would increase Medicare enrollment by 32% in 2030, 33% in 2040, and 34% in 2050, assuming all newly eligible people opt to enroll.169 This proposal would surely face opposition from hospital and provider groups in the health care community. In our interviews, for instance, the Maine hospital community expressed significant concern
over a more robust public payer role with lower reimbursement rates than those of private carriers. Maine may also want to consider this policy’s implications for the marketplace risk pool. The stakeholder interviews highlighted that many retired Mainers just under Medicare eligibility age use the marketplace to bridge coverage between employer-sponsored insurance and Medicare, meaning such a policy could siphon off marketplace enrollees.
A Biden administration with a Democratically-controlled Congress might also pursue a federal public option.This public option could be offered through the health insurance marketplaces, whether state-based or federally-facilitated, and as an option for those also considering employer-sponsored insurance. The Biden proposal could also auto-enroll those with incomes up to 138% FPL in non-expansion states, while expansion states like Maine would have the choice of keeping individuals on Medicaid or switching them to premium-free public option plans.170 While this proposal would likely face significant stakeholder and political opposition even under a Democratically-controlled Congress, Maine should nonetheless consider both the disruptive and promising implications of a federal public option offered on the marketplace.
The next section describes our recommendation for how the State can prepare for and leverage future policy opportunities, considering both impacts on consumers and state feasibility.
Recommendation: In the procurement, implementation, and maintenance of the SBM eligibility and enrollment system, prioritize platform capacity to adjust the inputs for the rules engine to adapt to future policy innovation.
Given the potential for future policy changes, it is important that the State considers how the SBM technology platform can adapt quickly to new rules surrounding eligibility and enrollment. Maine should ensure that the vendor procured for developing the SBM technology platform builds flexibility into the system. The SBM platform RFP already incorporates provisions that can make this flexibility possible, meaning that whether a nimble marketplace is developed will largely depend on the process of implementing and maintaining the SBM moving forward.
PLANNING FOR THE FUTURE | 55
The State should ensure that the vendor builds a rules engine with adjustable inputs that, on the back end, allows DHHS to adapt the state platform to future changes in eligibility criteria. This specific recommendation builds on Maine’s criteria in the RFP that the platform should allow for “modular integration of eligibility and enrollment functions with minimal changes to the solution’s codebase.”171 Instead of hard-coding the rules engine and making it difficult to adjust, a flexible approach would ensure built-in workarounds for DHHS when adjustments are needed.
Such resiliency measures should also protect the rules engine against potential glitches in the event that eligibility criteria are changed in the future. As an example, Washington’s Medicaid system experienced significant backlogs during its first OEP in 2013 and 2014. This was due, in part, to the rules engines not accurately incorporating eligibility requirements and an inability to read complex data relating to household composition.172 Resiliency measures are thus central to this recommendation. Our conversations with enrollment assisters underscored the importance of a straightforward and reliable enrollment platform for consumers. A platform that avoids such glitches would advance this objective while helping the State avoid frequent and expensive IT fixes whenever an eligibility change occurs.
Consumer Impact
By prioritizing the development of a flexible eligibility and enrollment platform, Maine is positioning itself to build an SBM able to respond to policy opportunities and responsive to the needs of Mainers. A nimble mar-

ketplace can act as a vehicle to advance future policies expanding coverage, increasing affordability, and narrowing health disparities. Moreover, the added layer of flexibility will ensure that fewer Mainers experience glitches or are not enrolled properly following changes in eligibility criteria, facilitating a smoother consumer experience.
State Feasibility
The RFP for the SBM technology platform vendor already allows for some of this flexibility in building, implementing, and maintaining the system. This recommendation encourages DHHS to play an active role in prioritizing platform flexibility with the vendor, which will require the use of time and human resources. However, since Maine will maintain at least a five-year contract with the vendor, this ongoing relationship can create touchpoints for DHHS staff to request changes in parts of the platform, such as the rules engine.
With regard to oversight, the independent verification and validation stage of the vendor contract process will enable Maine to assess its satisfaction with the level of flexibility and resiliency built into the system. The enabling statute includes the appropriation for this independent verification and validation step.173
Lastly, this recommendation would garner broad support among key carrier, provider, and advocacy stakeholders. These flexibilities could advance policies increasing the number of enrollees on carrier plans, lower uncompensated care costs for providers while expanding the volume of commercial reimbursements, and increase coverage levels for consumers.
56 | PLANNING FOR THE FUTURE
Conclusion
Through their initial steps to explore moving the State of Maine to an SBM, Maine officials have demonstrated a commitment to improving the accessibility and affordability of private health insurance.

Building and running an SBM is a technical and operational undertaking that presents Maine officials with the unique opportunity to tailor the marketplace to the needs of Mainers and advance the State’s goals around health care and coverage. Informed by interviews with a diverse set of stakeholders and secondary research, this report identifies and recommends policy options for Maine officials as they consider transitioning to an SBM.
Broadly, we highlight the need to: 1) increase consumer assistance capacity, 2) integrate consumer engagement into the process of designing and implementing Maine’s SBM, and 3) re-establish the Maine Office of Health Equity to coordinate equity efforts across DHHS.
In topic-specific recommendations, we draw on the experiences of other SBMs and on stakeholder input
to identify opportunities that could improve access to affordable and quality health insurance in Maine’s health care context. These topics include enrollment periods, plan display, auto-renewal, and integration with MaineCare. We close our recommendations by examining how the State can leverage an SBM to take advantage of future policy opportunities under a new federal administration.
We would be remiss if we did not mention the tremendous challenges ahead for state budgets generally, as the nation recovers from the staggering loss of life and accompanying economic downturn caused by the coronavirus pandemic. However, the COVID-19 crisis has also further highlighted the importance of ensuring every Mainer can access affordable health insurance and ultimately the care and resources necessary to live a healthy life. We believe our recommendations can help Maine officials make progress towards this important goal and look forward to following future developments.
CONCLUSION | 57
Endnotes

1 H.P. 1425 Made for Maine Health Coverage Act. LD 2007. Accessed from: http://www.mainelegislature.org/legis/bills/display_ps.asp?ld=2007&PID=1456&snum=129
2 Ogden, Scott and Lindsay Crete. “Governor Mills Signs Executive Order Directing DHHS to Move Forward Medicaid Expansion.” State of Maine Office of Governor Janet T. Mills. January 3, 2019. https://www.maine.gov/governor/mills/news/governor-mills-signs-executive-order-directing-dhhs-move-forward-medicaid-expansion-2019-01-03
3 “Governor Mills Signs Legislation Protecting Health Care Coverage.” State of Maine Office of Governor Janet T. Mills. March 19, 2019. https:// www.maine.gov/governor/mills/news/governor-mills-signs-legislation-protecting-health-care-coverage-2019-03-19.
4 Alberts, Corinne “Nevada’s Insurance Exchange Director Talks about Transitioning to a State-Based Marketplace and Saving Millions.” National Academy for State Health Policy. Accessed December 30, 2020. https://www.nashp.org/nevadas-insurance-exchange-director-heather-korbulic-talks-about-transitioning-to-a-state-based-marketplace/
5 H.P. 1425 Made for Maine Health Coverage Act. LD 2007. Accessed from: http://www.mainelegislature.org/legis/bills/display_ps.asp?ld=2007&PID=1456&snum=129
6 State of Maine Department of Administrative and Financial Services, Division of Procurement Services. “RFP# 202010151 Health Insurance Marketplace Technology Platform and Consumer Assistance Services,” October 23, 2020. https://www.maine.gov/tools/whatsnew/attach. php?id=3490149&an=1.
7 State of Maine, Scoresheet for RFP# 202010151: Health Insurance Marketplace Technology Platform and Consumer Assistance Services. http:// www.maine.gov/tools/whatsnew/attach.php?id=3490149&an=5
8 State of Maine, Scoresheet for RFP# 202010151: Health Insurance Marketplace Technology Platform and Consumer Assistance Services. http:// www.maine.gov/tools/whatsnew/attach.php?id=3490149&an=5
9 H.P. 1425 Made for Maine Health Coverage Act. LD 2007. Accessed from: http://www.mainelegislature.org/legis/bills/display_ps.asp?ld=2007&PID=1456&snum=129 ; Corlette, Sabrina, Kevin Lucia, Katie Keith, and Olivia Hoppe. “States Seek Greater Control, Cost-Savings by Converting to State-based Marketplaces.” (2019). Urban Institute. https://www.urban.org/sites/default/files/publication/101166/states_seek_ greater_control_cost_savings_by_converting_to_state-based_marketplaces_1.pdf
10 Supreme Court of the United States. “National Federation of Independent Business et al. v. Sebelius, Secretary of Health and Human Services, et al. No. 11–393.” (2012). https://www.supremecourt.gov/opinions/11pdf/11-393c3a2.pdf
11 Kaiser Family Foundation. State Health Facts. “Status of State Action on the Medicaid Expansion Decision.” November 2, 2020. Accessed December 16, 2020. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
12 Ollove, Michael. “After Many Twists, Maine Finally Will Expand Medicaid.” April 4, 2019. https://www.pewtrusts.org/en/research-and-analysis/ blogs/stateline/2019/04/04/after-many-twists-maine-finally-will-expand-medicai.
13 “MaineCare Eligibility Guide.” Consumers for Affordable Health Care and Maine Equal Justice. June 16, 2020. Pg 12. https://www.mainecahc. org/wp-content/uploads/2018/03/MaineCare-Eligibility-Guide.pdf
14 Maine Department of Health and Human Services. “MaineCare Expansion.” https://www.maine.gov/dhhs/data-reports/mainecare-expansion
15 Center for Medicaid and Medicare Services. “2019 and 2020 Marketplace Open Enrollment Period Public Use Files” April 2, 2020. https:// www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Marketplace-Products/2020-Marketplace-Open-Enrollment-Period-Public-Use-Files#:~:text=This%20includes%20the%20original%202020,enroll%20by%20the%20original%20deadline
16 Mabon, Sally, Marissa Korn, and Heather Howard. “State Budget Actions in Response to COVID-19 and the Impact on State Health Programs.” July 31, 2020. https://www.shvs.org/an-early-look-at-state-budget-actions-in-response-to-covid-19-and-the-impact-on-state-health-programs/
17 Source for March 2020 enrollment: Maine Department of Health and Human Services. MaineCare “MaineCare (Medicaid) Update: March 2, 2020.” https://www.maine.gov/tools/whatsnew/index.php?topic=DHHS-MAINECARE-UPDATES&id=2182997&v=article. Source for December 2020 enrollment: “MaineCare Expansion.” https://www.maine.gov/dhhs/data-reports/mainecare-expansion
18 “Governor Mills Announces Maine Will Pursue a State-Based Health Insurance Marketplace Under the Affordable Care Act.” DHHS, August 29, 2019. https://www.maine.gov/governor/mills/news/governor-mills-announces-maine-will-pursue-state-based-health-insurance-marketplaceunder
19 Maine State Legislature. “FACTS ABOUT MAINE...” Accessed December 17, 2020. https://www1.maine.gov/legis/general/facts/facts.htm.
20 Maine Department of Health and Human Services, MeCDC. “Rural Health and Primary Care - Office of Health Equity,” 2020. https://www. maine.gov/dhhs/mecdc/public-health-systems/rhpc/rural-health.shtml
21 Wengle, E. “Are Marketplace Premiums Higher in Rural Than in Urban Areas?” RWJF, November 15, 2018. https://www.rwjf.org/en/library/ research/2018/11/are-marketplace-premiums-higher-in-rural-than-in-urban-areas.html
22 Rural Health Transformation Team. “Transforming Rural Health.” Maine Department of Health and Human Services, April 2, 2020. https:// www1.maine.gov/dhhs/initiatives/transforming-rural-health. Also: Maine DHHS, MeCDC. “Rural Health and Primary Care - Office of Health Equity,” 2020. https://www.maine.gov/dhhs/mecdc/public-health-systems/rhpc/rural-health.shtml
23 “Table 702.60. Number and percentage of households with computer and internet access, by state: 2018.” National Center for Education Statistics. https://nces.ed.gov/programs/digest/d19/tables/dt19_702.60.asp
24 ConnectMaine “State of Maine Broadband Action Plan 2020”. 2020. https://www.maine.gov/connectme/sites/maine.gov.connectme/files/inline-files/State%20of%20Maine%20-%20Statewide%20Broadband%20Action%20Plan%202020_1.pdf
25 “Table S0101: Age and Sex.” American Community Survey 2019: 1-Year Estimates Subject Tables. https://data.census.gov/cedsci/ table?q=Age%20and%20Sex&g=0100000US_0400000US23&tid=ACSST1Y2019.S0101&hidePreview=true
ENDNOTES | 59
26 “Table DP02: SELECTED SOCIAL CHARACTERISTICS IN THE UNITED STATES. American Community Survey 2019: 1-Year Estimates Subject Tables. https://data.census.gov/cedsci/profile?g=0400000US23
27 Ibid.
28 U.S. Census Bureau. “2019 Median Household Income in the United States.” The United States Census Bureau, September 17, 2020. https:// www.census.gov/library/visualizations/interactive/2019-median-household-income.html.
29 F. Marie Hall Institute for Rural and Community Health. “2017 Rural Health Report Card.” Texas Tech University Health Sciences Center, 2017. https://www.maine.gov/dhhs/mecdc/public-health-systems/rhpc/documents/RHQ_Report_Card.pdf
30 Wight, Patty. “Survey: High Costs Kept Nearly 200,000 Mainers From Pursuing Medical Treatment, Filling Prescription,” October 30, 2020. https://www.mainepublic.org/post/survey-high-costs-kept-nearly-200000-mainers-pursuing-medical-treatment-filling-prescription
31 “Table S2701: SELECTED CHARACTERISTICS OF HEALTH INSURANCE COVERAGE IN THE UNITED STATES.” 2019 American Community Survey 1-Year Estimates Subject Tables. https://data.census.gov/cedsci/table?q=health%20insurance&g=0400000US23&tid=ACSST1Y2019. S2701&hidePreview=true
32 American Community Survey. “SELECTED SOCIAL CHARACTERISTICS IN THE UNITED STATES,” 2019. https://data.census.gov/cedsci/ table?g=0400000US23&tid=ACSDP5Y2019.DP02
33 U.S. Census Bureau. “Detailed Languages Spoken at Home and Ability to Speak English.” The United States Census Bureau, October 2015. https://www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html.
34 U.S. Census Bureau. “QuickFacts: Maine,” July 1, 2019. https://www.census.gov/quickfacts/ME.
35 American Immigration Council. “Immigrants in Maine,” August 6, 2020. https://www.americanimmigrationcouncil.org/research/immigrants-in-maine
36 Ibid.
37 Maine Equal Justice. “Immigrants Below Poverty Level Can Apply for Marketplace Subsidies,” n.d. https://maineequaljustice.org/site/assets/ files/1712/doc_7_2_immigrants_below_poverty_-_marketplace_subsidies.pdf
38 U.S. Census Bureau. “QuickFacts: Maine,” July 1, 2019. https://www.census.gov/quickfacts/ME.
39 Sacchetti, Maria. “Black People — Many of Them Immigrants — Make up Less than 2 Percent of Maine’s Population but Almost a Quarter of Its Coronavirus Cases.” Washington Post, July 30, 2020. https://www.washingtonpost.com/nation/2020/07/18/im-scared/
40 KIDS COUNT Data Center. “Children in Poverty by Race and Ethnicity (5 Yr ACS),” December 2019. https://datacenter.kidscount.org/data/ tables/9738-children-in-poverty-by-race-and-ethnicity-5-yr-acs?loc=21&loct=2
41 New American Economy. “The Contributions of New Americans in Maine,” August 2016. https://research.newamericaneconomy.org/wp-content/uploads/2017/02/nae-me-report.pdf
42 Maine Department of Labor. “Migrant Worker Survey,” December 2015. https://www.maine.gov/labor/labor_laws/migrantworker/results.html
43 U.S. Census Bureau. “QuickFacts: Maine,” July 1, 2019. https://www.census.gov/quickfacts/fact/table/ME/RHI325219#RHI325219
44 “Maine Native Study Resources.” Maine Department of Education. https://www.maine.gov/doe/learning/content/socialstudies/resources/ mainenativestudies/resources
45 Schwab, Rachel, and JoAnn Volk. “States Looking to Run Own Insurance Marketplace See Opportunity.” Commonwealth Fund, June 28, 2019. https://doi.org/10.26099/dq2w-7b61
46 Lueck, Sarah. “Adopting a State-Based Health Insurance Marketplace Poses Risks and Challenges.” CBPP, February 5, 2020. https://www.cbpp. org/research/health/adopting-a-state-based-health-insurance-marketplace-poses-risks-and-challenge; Murphy, Chris (D-NJ). “Governor Murphy Signs Legislation to Restore a Key Provision of the Affordable Care Act and Lower the Cost of Health Care in New Jersey,” July 31, 2020. https://nj.gov/governor/news/news/562020/approved/20200731a.shtml; Colorado General Assembly. “Health Insurance Affordability Enterprise,” June 30, 2020. https://leg.colorado.gov/bills/sb20-215
47 Maine Department of Health and Human Services. “Maine Progresses toward a State-Based Health Insurance Marketplace.” August 6, 2020. https://www.maine.gov/dhhs/blog/maine-progresses-toward-state-based-health-insurance-marketplace-2020-08-06
48 Armour, Stephanie, “Trump Administration Slashes Funds for ACA Outreach,” Wall Street Journal, July 11, 2018, sec. Politics, https://www.wsj. com/articles/trump-administration-slashes-funds-for-aca-outreach-1531272043
49 Shafer, Paul and Stacie Dusetzina, “Looking Ahead To 2018: Will A Shorter Open Enrollment Period Reduce Adverse Selection In Exchange Plans?” Health Affairs Blog, April 14, 2017, https://www.healthaffairs.org/do/10.1377/hblog20170414.059663/full/
50 Luthi, Susannah. “Trump Rejects Obamacare Special Enrollment Period amid Pandemic,” POLITICO, March 31, 2020, https://www.politico. com/news/2020/03/31/trump-obamacare-coronavirus-157788.
51 Kaiser Family Foundation, “Marketplace Enrollment, 2014-2020,” KFF (blog), April 7, 2020, https://www.kff.org/health-reform/state-indicator/ marketplace-enrollment/
52 Data Sources: Kaiser Family Foundation (2014-2020), CMS (2021) https://www.cms.gov/newsroom/fact-sheets/2021-federal-health-insurance-exchange-weekly-enrollment-snapshot-final-snapshot
53 Zhu, Jane, Daniel Polsky, and Yuehan Zhang, “State-Based Marketplaces Outperform Federally-Facilitated Marketplaces,” Leonard Davis Institute of Health Economics, March 21, 2018, https://ldi.upenn.edu/brief/state-based-marketplaces-outperform-federally-facilitated-marketplaces
60 | ENDNOTES
54 Schwab, Rachel and JoAnn Volk, “States Looking to Run Own Insurance Marketplace See Opportunity,” Commonwealth Fund, June 28, 2019, https://doi.org/10.26099/dq2w-7b61
55 Lueck, Sarah. “Adopting a State-Based Health Insurance Marketplace Poses Risks and Challenges.” (2020). Center on Budget and Policy Priorities. https://www.cbpp.org/research/health/adopting-a-state-based-health-insurance-marketplace-poses-risks-and-challenges
56 Griffin, Stockord and Sarah Blake. “Maine CDC: State population is 1.6% Black, yet 24% of Maine’s COVID-19 cases are among Black community.” NewsCenter Maine. June 19, 2020. https://www.newscentermaine.com/article/news/health/coronavirus/maine-cdc-state-population-is-16black-yet-24-of-maines-covid-19-cases-are-among-black-community/97-f39a62bb-e1db-47f3-a9e0-929bd7810465.
57 Unemployment figures from U.S. Census Bureau Current Population Survey, 2013-2018, pooled data. Poverty figures from U.S. Census Bureau American Community Survey, 15-year average, 2003-2017. Source: Myall, James. “Data on racial inequality shows need for solutions to advance racial justice”. Maine Center for Economic Policy. June 3, 2019. https://www.mecep.org/wp-content/uploads/2019/06/MECEP-racial-inequality-fact-sheet-FINAL.pdf.
58 U.S. Center for Disease Control Behavioral Risk Factor Surveillance System, 2013-2017, 5-year average. Source: Myall, James. “Data on racial inequality shows need for solutions to advance racial justice”. Maine Center for Economic Policy. June 3, 2019. https://www.mecep.org/ wp-content/uploads/2019/06/MECEP-racial-inequality-fact-sheet-FINAL.pdf.
59 Ibid.
60 Keith, Katie. “CMS to Maintain Navigator Funding at $10 Million for 2020, 2021”.Health Affairs. May 29, 2019. https://www.healthaffairs.org/ do/10.1377/hblog20190529.659554/full/
61 Center for Medicare and Medicaid Services. “2019 Navigator Funding”. 2019. https://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Marketplaces/Downloads/2019-Navigator-Grant-Recipients.pdf
62 Kates, Jennifer, Usha Ranji, Adara Beamesderfer, Alina Salganicoff, and Lindsey Dawson. “Health and Access to Care and Coverage for Lesbian, Gay, Bisexual and Transgender (LGBT) Individuals in the U.S.” Kaiser Family Foundation. May 3, 2018. https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-and-access-to-care-and-coverage-for-lesbian-gay-bisexual-and-transgender-individuals-in-the-u-s/
63 “Governor Mills Dedicates $50,000 to Permanent Commission on the Status of Racial, Indigenous, and Maine Tribal Populations.” DHHS, June 25, 2020. https://www.maine.gov/governor/mills/news/governor-mills-dedicates-50000-permanent-commission-status-racial-indigenous-and-maine-tribal
64 An Act To Establish the Permanent Commission on the Status of Racial and Ethnic Populations. H.P. 582 Sess. of 2019. http://www.mainelegislature.org/legis/bills/getPDF.asp?paper=HP0582&item=1&snum=129
65 “Advisory Groups”. Maine Department of Health and Human Services. February 2020. https://www.maine.gov/dhhs/oms/about-us/advisory-groups
66 Lukanen, Elizabeth and Zylla, Emily. “Exploring Strategies to Fill Gaps in Medicaid Race, Ethnicity, and Language Data.” State Health & Value Strategies, October 1, 2020. https://www.shvs.org/exploring-strategies-to-fill-gaps-in-medicaid-race-ethnicity-and-language-data/
67 Maine Public Health Data Reports–Health Disparities Maine Center for Disease Control and Prevention. https://www.maine.gov/dhhs/mecdc/ phdata/health-disparities/uw-statistics.htm
68 California Department of Public Health. “Office of Health Equity”. https://www.cdph.ca.gov/Programs/OHE/Pages/OfficeHealthEquity.aspx
69 Connecticut State Department of Health. “Office of Health Equity”. https://portal.ct.gov/DPH/Workforce--Professional-Development/Office-of-Health-Equity/Office-of-Health-Equity
70 Healey, Maura. “Building Toward Racial Justice and Equity in Health: A Call to Action.” Office of the Attorney General, Commonwealth of Massachusetts. November 2, 2020. https://www.mass.gov/info-details/building-toward-racial-justice-and-equity-in-health-a-call-to-action#readthe-report-
71 Chomilo, Nathan T. “Building Racial Equity Into The Walls Of Health Policy.” Health Affairs. December 1, 2020. https://www.healthaffairs.org/ do/10.1377/hblog20201119.508776/full/
72 “Special Enrollment Period (SEP) - HealthCare.Gov Glossary.” Healthcare.gov. https://www.healthcare.gov/glossary/special-enrollment-period/
73 Jost, Timothy. “Examining the Final Market Stabilization Rule: What’s There, What’s Not, and How Might It Work? (Updated).” Health Affairs Blog. April 14, 2017. https://www.healthaffairs.org/do/10.1377/hblog20170414.059646/full/
74 Lueck, Sarah, and Matt Broaddus. “Emergency Special Enrollment Period Would Boost Health Coverage Access at a Critical Time.” Center on Budget and Policy Priorities. July 30, 2020. https://www.cbpp.org/research/health/emergency-special-enrollment-period-would-boost-health-coverage-access-at-a-critical
75 Garabedian, Laura F., et al. “Costs Are Higher For Marketplace Members Who Enroll During Special Enrollment Periods Compared With Open Enrollment.” Health Affairs 39.8 (2020): 1354-1361. https://www.healthaffairs.org/doi/10.1377/hlthaff.2019.01155
76 Keith, Katie. “What Biden’s Election Would Mean for the Affordable Care Act.” Health Affairs Blog. November 5, 2020. https://www.healthaffairs.org/do/10.1377/hblog20201105.33952/full/
77 Swartz, Katherine and John A. Graves. “Shifting The Open Enrollment Period For ACA Marketplaces Could Increase Enrollment And Improve Plan Choices.” Health Affairs 33:7 (2014): 1286-1293. https://www.healthaffairs.org/doi/10.1377/hlthaff.2014.0007
78 Mullainathan, Sendhil and Eldar Shafir. Scarcity: Why Having Too Little Means So Much. New York (NY): Times Books, 2013.
79 Norris, Louise. “What Are the Deadlines for Obamacare’s Open Enrollment Period?” HealthInsurance.org. January 1, 2020. https://www. healthinsurance.org/faqs/what-are-the-deadlines-for-obamacares-open-enrollment-period/ with additional confimations from each state’s associated website.
ENDNOTES | 61
80 “2020 Marketplace Open Enrollment Period Public Use Files.” Center for Medicare and Medicaid Services. April 2020. https://www.cms.gov/ Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Marketplace-Products/2020-Marketplace-Open-Enrollment-Period-Public-Use-Files
81 Shafer, Paul and Stacie Dusetzina. “Looking Ahead To 2018: Will A Shorter Open Enrollment Period Reduce Adverse Selection In Exchange Plans?” Health Affairs Blog. April 14, 2017. https://www.healthaffairs.org/do/10.1377/hblog20170414.059663/full/
82 Rakotoniaina, Adney. “How States Are Increasing Coverage through Special Enrollment Periods.” The National Academy for State Health Policy. September 29, 2020. https://www.nashp.org/how-states-are-increasing-coverage-through-special-enrollment-periods/
83 “Enroll in or change 2020 plans — only with a Special Enrollment Period” Healthcare.gov. https://www.healthcare.gov/coverage-outside-open-enrollment/special-enrollment-period/
84 Lueck, Sarah, and Matt Broaddus. “Emergency Special Enrollment Period Would Boost Health Coverage Access at a Critical Time.” Center on Budget and Policy Priorities. July 30, 2020. https://www.cbpp.org/research/health/emergency-special-enrollment-period-would-boost-health-coverage-access-at-a-critical
85 Source 1: Plott, Caroline F., Allen B. Kachalia, and Joshua M. Sharfstein. “Unexpected Health Insurance Profits and the COVID-19 Crisis.” JAMA 324.17 (2020): 1713-1714.
Source 2: Abelson, Reed. “Major U.S. Health Insurers Report Big Profits, Benefiting From the Pandemic.” The New York Times. August 5, 2020. www.nytimes.com/2020/08/05/health/covid-insurance-profits.html.
86 Overton, Penelope. “Pandemic Takes Staggering Financial Toll on Maine Hospitals.” Press Herald. June 14, 2020. www.pressherald. com/2020/06/14/pandemic-takes-staggering-financial-toll-on-maine-hospitals/.
87 Letter to DHHS Secretary Sylvia Burwell. March 12, 2015. https://watsoncoleman.house.gov/sites/watsoncoleman.house.gov/files/documents/ yi%20pregnancy%20sep%20partner%20letter%203.12.15.pdf
88 Rakotoniaina, Adney. “How States Are Increasing Coverage through Special Enrollment Periods.” The National Academy for State Health Policy. September 29, 2020. https://www.nashp.org/how-states-are-increasing-coverage-through-special-enrollment-periods/
89 Connecticut Public Act No. 18-43: An Act Authorizing Pregnancy As a Qualifying Event for Special Enrollment Periods for Certain Individuals. June 2, 2018. https://www.cga.ct.gov/2018/act/pa/2018PA-00043-R00SB-00206-PA.htm
90 DC Law 23-135. Pregnancy as a Qualifying Event Act of 2020. October 20, 2020. https://code.dccouncil.us/dc/council/laws/23-135.html
91 Maryland HB127: Health Insurance - Health Benefit Plans - Special Enrollment Period for Pregnancy. April 30, 2019. https://trackbill.com/bill/ maryland-house-bill-127-health-insurance-health-benefit-plans-special-enrollment-period-for-pregnancy/1643701/
92 New York AB6780B. April 2, 2015.
93 Vermont Act 120. May 23, 2016.
https://www.nysenate.gov/legislation/bills/2015/a6780/amendment/b
https://legislature.vermont.gov/Documents/2016/Docs/ACTS/ACT120/ACT120%20As%20Enacted.pdf
94 Postolowski, Christina. “Without Maternity Coverage: The Need for Special Enrollment in the Health Insurance Marketplaces during Pregnancy.” Young Invincibles. December. 2014. https://khn.org/wp-content/uploads/sites/2/2015/02/without-maternity-coverage.pdf
95 Garro, Nicole, Brittany Hernandez, and Cynthia Pellegrini. “HHS Must Remove Barriers To Coverage for Pregnant Women.” Health Affairs. February 19, 2016. https://www.healthaffairs.org/do/10.1377/hblog20160219.053241/full/
96 “Peristats - Uninsured Before Pregnancy by Race/Ethnicity: Maine, 2017.” March of Dimes Foundation. Retrieved December 11, 2020. https:// www.marchofdimes.org/Peristats/ViewSubtopic.aspx?reg=23&top=11&stop=445&lev=1&slev=4&obj=35
97 “Peristats - Late/No Prenatal Care by Race/Ethnicity: Maine, 2016-2018 Average.” March of Dimes Foundation. Retrieved December 11, 2020. https://www.marchofdimes.org/peristats/ViewSubtopic.aspx?reg=23&top=5&stop=28&lev=1&slev=4&obj=1
98 Garro, Nicole, Brittany Hernandez, and Cynthia Pellegrini. “HHS Must Remove Barriers To Coverage for Pregnant Women.” Health Affairs. February 19, 2016. https://www.healthaffairs.org/do/10.1377/hblog20160219.053241/full/
99 “Peristats - Uninsured Before Pregnancy, 2012-2017.” March of Dimes Foundation. Retrieved December 11, 2020. https://www.marchofdimes. org/Peristats/ViewSubtopic.aspx?reg=23&top=11&stop=443&lev=1&slev=4&obj=35
100 “Peristats - Medicaid Coverage of Births, 2016-2018.” March of Dimes Foundation. Retrieved December 12, 2020. https://www.marchofdimes. org/Peristats/ViewSubtopic.aspx?reg=23&top=11&stop=154&lev=1&slev=4&obj=1
101 Henderson, James W. “The Cost Effectiveness of Prenatal Care.” Health Care Financing Review 15:4 (1994): 21-32. https://www.ncbi.nlm.nih. gov/pmc/articles/PMC4193436/
102 Lotven, Amy. “Advocates Upset ‘Tax Time’ Special Enrollment Period Not Offered for 2016.” Inside CMS. 18:49. December 10, 2015. https:// www.jstor.org/stable/26704744
103 “Covered California now offering a very special enrollment period.” Lake County Record-Bee. March 12, 2020. https://www.record-bee. com/2020/03/12/covered-california-now-offering-a-very-special-enrollment-period/
104 “DC Health Link to Offer Even More Opportunities for Residents to Get Covered.” DC Health Benefit Exchange Authority. February 11, 2020. https://hbx.dc.gov/release/dc-health-link-offer-even-more-opportunities-residents-get-covered
105 Maryland HB814: Maryland Easy Enrollment Health Insurance Program. May 13, 2019. https://www.billtrack50.com/BillDetail/1061464
106 New Jersey S3238. December 10, 2020. https://www.njleg.state.nj.us/2020/Bills/S3500/3238_I1.PDF
62 | ENDNOTES
107 Appleby, Julie. “Make Tax Day Also Enrollment Deadline, One Health Expert Says.” Kaiser Health News. November 7, 2013. https://khn.org/ news/make-tax-day-also-enrollment-deadline-one-health-expert-says/
108 “Maryland Easy Enrollment Health Insurance Program.” Maryland Health Connection. https://www.marylandhealthconnection.gov/easyenrollment/
109 McKee-Ryan, Frances et al. “Psychological and Physical Well-Being During Unemployment: A Meta-Analytic Study.” The Journal of Applied Psychology 90:1 (2005): 53-76. https://pubmed.ncbi.nlm.nih.gov/15641890/
110 Source 1: “SOI Tax States - Individual Statistical Tables by Size of Adjusted Gross Income.” Internal Revenue Service. Retrieved December 11, 2020. https://www.irs.gov/statistics/soi-tax-stats-individual-statistical-tables-by-size-of-adjusted-gross-income#_grp8
Source 2: “Population Distribution by Age.” Kaiser Family Foundation. Retrieved December 11, 2020. https://www.kff.org/other/state-indicator/distribution-by-age/
111 Mulligan, Jessica, Stephanie Arriaga, and Jeannette Torres. “An ethnographic study of enrollment obstacles in Rhode Island, USA: struggling to get covered on an Affordable Care Act insurance marketplace.” Critical Public Health 29.5 (2019): 547-559.
112 “Special Enrollment Periods for Complex Health Care Issues.” HealthCare.gov. www.healthcare.gov/sep-list/
113 Commonwealth Fund. States That Require Standardized Individual Market Health Plans. January 15, 2020, https://www.commonwealthfund.org/ chart/2020/states-require-standardized-individual-market-health-plans.
114 Commonwealth Fund. States Work to Make Individual Market Health Coverage More Affordable, But Long-Term Solutions Call for Federal Leadership. January 15, 2020, doi:https://doi.org/10.26099/xrhk-2n44.
115 H.P. 1425 Made for Maine Health Coverage Act. LD 2007. Accessed from: http://www.mainelegislature.org/legis/bills/display_ps.asp?ld=2007&PID=1456&snum=129
116 Maine Bureau of Insurance. 2022 Clear Choice Cost Sharing Designs. https://www.maine.gov/pfr/insurance/legal/notices/pdf/2022_clear_ choice_cost_sharing_designs_response.pdf
117 Clear Choice Workgroup. “Clear Choice Comments,” 25 August 2020, https://www.maine.gov/pfr/insurance/legal/notices/pdf/clear_ choice_comments_8-12-20.pdf, “Clear Choice Comment,” September 30, 2020, https://www.maine.gov/pfr/insurance/legal/notices/pdf/ clear_choice_comments_9-15-20.pdf, “Clear Choice Comments,” November 6. 2020, https://www.maine.gov/pfr/insurance/legal/notices/pdf/ clear_choice_comments_11-6-20.pdf, and “Clear Choice Comments,” December 4, 2020, https://www.maine.gov/pfr/insurance/legal/notices/ pdf/clear_choice_comments_12-4-20.pdf
118 Connect for Healthcare Colorado. “Quick Cost and Plan Finder.” https://planfinder.connectforhealthco.com/home
119 Washington HealthPlanFinder. https://www.wahealthplanfinder.org/HBEWeb/Annon_ShowIndividualFamilyPlans
120 Taylor, Erin Audrey, Katherine Grace Carman, Andrea Lopez, Ashley N. Muchow, Parisa Roshan, and Christine Eibner. “How Do Consumers Make Choices in ACA Marketplaces?” p. 27-29. RAND Corporation, June 28, 2016. https://www.rand.org/pubs/research_reports/RR1567.html.
121 Taylor, Erin Audrey, Katherine Grace Carman, Andrea Lopez, Ashley N. Muchow, Parisa Roshan, and Christine Eibner. “How Do Consumers Make Choices in ACA Marketplaces?” p. 15. RAND Corporation, June 28, 2016. https://www.rand.org/pubs/research_reports/RR1567.html
122 Taylor, Erin Audrey, Katherine Grace Carman, Andrea Lopez, Ashley N. Muchow, Parisa Roshan, and Christine Eibner. “How Do Consumers Make Choices in ACA Marketplaces?” p. 21. RAND Corporation, June 28, 2016. https://www.rand.org/pubs/research_reports/RR1567.html
123 Johnson, Eric J., Suzanne B. Shu, Benedict G. C. Dellaert, Craig Fox, Daniel G. Goldstein, Gerald Häubl, Richard P. Larrick, et al. “Beyond Nudges: Tools of a Choice Architecture.” Marketing Letters 23, no. 2 (May 25, 2012): 487–504. https://doi.org/10.1007/s11002-012-9186-1
124 Mani, Anandi, Sendhil Mullainathan, Eldar Shafir, and Jiaying Zhao. “Poverty Impedes Cognitive Function.” Science 341, no. 6149 (August 30, 2013): 976–80. https://doi.org/10.1126/science.1238041; Loewenstein, George, Joelle Y. Friedman, Barbara McGill, Sarah Ahmad, Suzanne Linck, Stacey Sinkula, John Beshears, et al. “Consumers’ Misunderstanding of Health Insurance.” Journal of Health Economics 32, no. 5 (September 2013): 850–62. https://doi.org/10.1016/j.jhealeco.2013.04.004
125 Washington HealthPlanFinder. https://www.wahealthplanfinder.org/HBEWeb/Annon_ShowIndividualFamilyPlans
126 State of Maine Department of Administrative and Financial Services, Division of Procurement Services. “RFP# 202010151 Health Insurance Marketplace Technology Platform and Consumer Assistance Services,” October 23, 2020. https://www.maine.gov/tools/whatsnew/attach. php?id=3490149&an=1.
127 Sanger-Katz, Margot, “It’s Not Just You: Picking a Health Insurance Plan Is Really Hard.” New York Times. Accessed on December 11, 2020. Available at: https://www.nytimes.com/2020/12/11/upshot/choosing-health-insurance-is-hard.html
128 Covered CaliforniaTM. “Shop & Compare Health Insurance Plans.” Accessed January 3, 2021. https://apply.coveredca.com/lw-shopandcompare/
129 “Fact Sheet: Data on Racial Inequality Shows Need for Solutions to Advance Racial Justice.” MECEP, June 3, 2019, https://www.mecep.org/ maines-economy/fact-sheet-data-on-racial-inequality-shows-need-for-solutions-to-advance-racial-justice/
130 State of Maine Department of Administrative and Financial Services, Division of Procurement Services. “RFP# 202010151 Health Insurance Marketplace Technology Platform and Consumer Assistance Services,” October 23, 2020. https://www.maine.gov/tools/whatsnew/attach. php?id=3490149&an=1
131 DC Health Link. “DC Plan Comparison Tool 2021 by Consumers’ Checkbook.” https://www.healthplanratings.org/hie/dc/2021/. Accessed January 3, 2021. https://dc.checkbookhealth.org/hie/dc/2021/index.cfm?page
132 State of Maine Department of Administrative and Financial Services, Division of Procurement Services. “RFP# 202010151 Health Insurance Marketplace Technology Platform and Consumer Assistance Services,” October 23, 2020. https://www.maine.gov/tools/whatsnew/attach.
ENDNOTES | 63
php?id=3490149&an=1
133 New York State of Health. “Individuals and Families: Compare Plans and Estimate Cost.” https://nystateofhealth.ny.gov/individual/searchAnonymousPlan/search
134 Source 1: Pear, Robert. “Names of Health Plans Sow Customer Confusion.” The New York Times. The New York Times, March 23, 2014. https://www.nytimes.com/2014/03/23/us/names-of-health-plans-sow-customer-confusion.html;
Source 2: Massachusetts Health Connector. “Find a Health Plan.” https://www.mahix.org/individual/prescreen/search/quotes?anonymousFlag=true&gId=1&isOEPFlow=true; Washington HealthPlanFinder. “Explore your health plan options.” https://www.wahealthplanfinder.org/ HBEWeb/Annon_ShowIndividualFamilyPlans
135 DC Health Link. “2021 Health Plan Comparison Tool for Individuals and Families.” https://dc.checkbookhealth.org/hie/dc/2021/index.cfm?page
136 Massachusetts Health Connector. “Find a Health Plan.” https://www.mahix.org/individual/prescreen/search/quotes?anonymousFlag=true&gId=1&isOEPFlow=true; Washington HealthPlanFinder. “Explore your health plan options.” https://www.wahealthplanfinder.org/ HBEWeb/Annon_ShowIndividualFamilyPlans
137 DC Health Link. “DC Plan Comparison Tool 2021 by Consumers’ Checkbook.” https://www.healthplanratings.org/hie/dc/2021/. Accessed January 3, 2021. https://dc.checkbookhealth.org/hie/dc/2021/index.cfm?page.
138 DC Health Link. “2021 Health Plan Comparison Tool for Individuals and Families.” https://dc.checkbookhealth.org/hie/dc/2021/index.cfm?page
139 Maine Bureau of Insurance. 2022 Clear Choice Cost Sharing Designs. https://www.maine.gov/pfr/insurance/legal/notices/pdf/2022_clear_ choice_cost_sharing_designs_response.pdf.
140 Taylor, Erin Audrey, Katherine Grace Carman, Andrea Lopez, Ashley N. Muchow, Parisa Roshan, and Christine Eibner. “How Do Consumers Make Choices in ACA Marketplaces?” p. 12-15, 27. RAND Corporation, June 28, 2016. https://www.rand.org/pubs/research_reports/RR1567. html
141 Mani, Anandi, Sendhil Mullainathan, Eldar Shafir, and Jiaying Zhao. “Poverty Impedes Cognitive Function.” Science 341, no. 6149 (August 30, 2013): 976–80. https://doi.org/10.1126/science.1238041
142 Center for Medicaid and Medicare Services.
2020 Marketplace Open Enrollment Period Public Use Files” April 2, 2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Marketplace-Products/2020-Marketplace-Open-Enrollment-Period-Public-Use-Files#:~:text=This%20includes%20 the%20original%202020,enroll%20by%20the%20original%20deadline
143 Center for Medicaid and Medicare Services.
2020 Marketplace Open Enrollment Period Public Use Files” April 2, 2020. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Marketplace-Products/2020-Marketplace-Open-Enrollment-Period-Public-Use-Files#:~:text=This%20includes%20 the%20original%202020,enroll%20by%20the%20original%20deadline
144 Healthcare.gov. “How to change, update, or cancel your Marketplace Plan.” December 2020. https://www.healthcare.gov/keep-or-change-plan/
145 Garner, Jackie. “Insurance Standards Bulletin Series – INFORMATION” Center for Consumer Information and Insurance Oversight. September 2, 2014. https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/Renewal-Notices-9-3-14-FINAL.pdf
146 Florida Agency for Health Care Administration. “Florida Medicaid Managed Care Auto=Assignment Methodology”. Prepared for the Florida Legislation. October 1, 2019. https://ahca.myflorida.com/Medicaid/recent_presentations/2019/Auto-Assignment_Report_100119_Final.pdf
147 Center for Medicaid and Medicare Services.“2019 and 2020 Marketplace Open Enrollment Period Public Use Files” April 2, 2020. https://www. cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Marketplace-Products/2020-Marketplace-Open-Enrollment-Period-Public-Use-Files#:~:text=This%20includes%20the%20original%202020,enroll%20by%20the%20original%20deadline
148 “Individuals will not have to apply to multiple programs nor will they be sent from one program to another if they initially apply to a program for which they are not ultimately eligible.” Federal Register. Vol 76., No. 159. Proposed Rules. https://www.federalregister.gov/d/2011-20756
149 Sommers, Benjamin D., Rebecca Gourevitch, Bethany Maylone, Robert J. Blendon, and Arnold M. Epstein. “Insurance churning rates for low-income adults under health reform: lower than expected but still harmful for many.” Health Affairs 35, no. 10 (2016): 1816-1824.
150 Ibid
151 “Medicaid MAGI and CHIP Application Processing Time Report.” CMS, November 28, 2018. Accessed December 17, 2020. https://www.medicaid.gov/state-overviews/downloads/magi-and-chip-application-processing-time/magi-application-time-report.pdf
152 “Send Documents to Confirm Why You’re Eligible for a Special Enrollment Period.” HealthCare.gov. Accessed December 17, 2020. https:// www.healthcare.gov/coverage-outside-open-enrollment/confirm-special-enrollment-period/.
153 Source 1: Linke Young, Christen, and Sobin Lee. “Making ACA Enrollment More Automatic for the Newly Unemployed.” Brookings, May 29, 2020. https://www.brookings.edu/research/making-aca-enrollment-more-automatic-for-the-newly-unemployed/.
Source 2: “Your Guide to the Maryland Easy Enrollment Health Insurance Program.” Maryland Health Connection, October 15, 2020. https:// www.marylandhealthconnection.gov/guidetoeasyenrollment/.
154 “NEARLY 58,000 MARYLANDERS GAIN HEALTH COVERAGE DURING TWO SPECIAL ENROLLMENT PERIODS.” Maryland Health Benefit Exchange. July 16, 2020. https://www.marylandhbe.com/wp-content/uploads/2020/07/End-of-SEPs-Press-Release.pdf/.
155 Maryland Senate Bill 802 / House Bill 814 (Chapter 424 / Chapter 423) – Maryland Easy Enrollment Health Insurance Program. http://mgaleg. maryland.gov/2019RS/bills/sb/sb0802e.pdf/.
156 Dagneau, Lucy, Jackson Lee and Jessicah Pierre. “Messages that Motivate: Engaging Consumers in the Second Enrollment Period”. Community
64 | ENDNOTES
Catalyst. https://www.communitycatalyst.org/resources/publications/document/Messages-that-Motivate_OEE-Memo-October-2014-FINAL.pdf; Stuber, Jennifer P., Kathleen A. Maloy, Sara Rosenbaum, and Karen C. Jones. “Beyond Stigma: What Barriers Actually Affect the Decisions of Low-Income Families to Enroll in Medicaid?.” (2000). https://hsrc.himmelfarb.gwu.edu/cgi/viewcontent.cgi?article=1052&context=sphhs_policy_briefs
157 “Apply for MassHealth, the Health Safety Net, or the Children’s Medical Security Plan” MassHealth https://www.mass.gov/how-to/apply-formasshealth-the-health-safety-net-or-the-childrens-medical-security-plan, Covered California “How Do I Apply?” “https://www.coveredca.com/ apply/,
158 Conant, Caitlin. “Biden and Democrats focus on health care messaging.” CBS News, September 16, 2020. https://www.cbsnews.com/news/ biden-and-democrats-focus-on-health-care-messaging/.
159 “Health Care.” Biden Harris Campaign Website. https://joebiden.com/healthcare/.
160 Cunningham, Paige W. “Analysis | The Health 202: Xavier Becerra Has Been Defending the ACA in Court. Now He Could Manage It.” The Washington Post. WP Company, December 7, 2020. https://www.washingtonpost.com/politics/2020/12/07/health-202-xavier-becerra-hasbeen-defending-aca-court-now-he-could-manage-it/.
161 “Proposed 2022 Notice of Benefit & Payment Parameters: Implications for States.” State Health & Value Strategies, December 4, 2020. https:// www.shvs.org/the-draft-2022-notice-of-benefit-payment-parameters-implications-for-states/.
162 “Section 1332: State Innovation Waivers.” CMS. Accessed December 15, 2020. https://www.cms.gov/CCIIO/Programs-and-Initiatives/State-Innovation-Waivers/Section_1332_State_Innovation_Waivers-.
163 Boozang, Patricia. “Evolving Public Option/Medicaid Buy-In Models and Considerations.” Maine Committee on Health Coverage, Insurance and Financial Services, December 16, 2016. https://legislature.maine.gov/doc/3628.
164 “National Agricultural Statistics Service.” U.S. Department of Agriculture, 2017. https://quickstats.nass.usda.gov/results/012661A0-39A1-3916BD84-CFEA609C8262.
165 “Inadmissibility on Public Charge Grounds.” Federal Register, October 10, 2018. https://www.federalregister.gov/documents/2018/10/10/2018-21106/inadmissibility-on-public-charge-grounds.
166 “Maine Migrant and Seasonal Farm Worker Demographic Survey.” Maine Department of Labor, December 2015. https://www.maine.gov/labor/ labor_laws/migrantworker/results.html.
167 “Plan to Protect and Build on Obamacare: Joe Biden.” Joe Biden for President: Official Campaign Website, October 11, 2020. https://joebiden. com/healthcare/.
168 “Text–H.R.1425–116th Congress (2019-2020): Patient Protection and Affordable Care Enhancement Act.” U.S. Congress, September 8, 2020. https://www.congress.gov/bill/116th-congress/house-bill/1425/text.
169 Paulson, Mariko. “Biden’s Healthcare Proposals.” Penn Wharton Budget Model, October 7, 2020. https://budgetmodel.wharton.upenn.edu/ issues/2020/10/6/biden-healthcare-proposals.
170 Riley, Trish. “The Biden Health Plan and States: Opportunities for Collaboration.” The National Academy for State Health Policy, November 10, 2020. https://www.nashp.org/the-biden-health-plan-and-states-opportunities-for-collaboration/.
171 State of Maine, Scoresheet for RFP# 202010151: Health Insurance Marketplace Technology Platform and Consumer Assistance Services. http:// www.maine.gov/tools/whatsnew/attach.php?id=3490149&an=5
172 Wishner, Jane, Ian Hill, Jeremy Marks, and Sarah Thornburgh. “Medicaid Real-Time Eligibility Determinations and Automated Renewals.” (2018). https://www.urban.org/research/publication/medicaid-real-time-eligibility-determinations-and-automated-renewals
173 H.P. 1425 Made for Maine Health Coverage Act. LD 2007. Accessed from: http://www.mainelegislature.org/legis/bills/display_ps.asp?ld=2007&PID=1456&snum=129
174 Report to the Legislature pursuant to Public Law 2019, Ch. 485, February 2020.
175 Appendix D, Report to the Legislature pursuant to Public Law 2019, Ch. 485, February 2020.
176 Ibid.
177 Maine RFP #201912213.
ENDNOTES | 65

Appendices
Appendix Table 1: Decision Matrix
The determinations below take into account stakeholder interviews, background research, and analysis of the political and policy landscape both in Maine and nationally.
TERMINOLOGY
Consumer Impact
• Potential Impact on Affordability - What is this recommendation’s impact on premiums, deductibles, and other cost-sharing for consumers?
• Potential Impact on Complexity - How does this recommendation impact the ease by which consumers can navigate accessing health coverage?
• Potential Impact on Coverage - How does this recommendation impact uninsured levels, while also considering different impacts across different populations? If applicable, how does it affect whether people are getting the coverage they want?
• Potential Impact on Health Equity - How does this recommendation impact health care access for historically marginalized populations in Maine?
Feasibility
• Political Feasibility - How likely will this recommendation move through the administrative or legislative process? How will stakeholders play into helping advance or stymie a particular proposal? How does the federal government’s involvement play into this recommendation?
• Financial Feasibility - What is this recommendation’s cost to the State in terms of budget impact?
• Implementation Capacity - What is the capacity of Maine state agencies to implement this recommendation including both the initial implementation and ongoing implementation?
To generate rankings, we assigned numeric scores to each color determination, weighting consumer impact more heavily. This framework was selected because the core of a promising policy is not the ease of implementation but rather its impact on consumers with respect to affordability, complexity, coverage, and equity. For instance, if a policy is feasible but has limited positive impact on consumers, we consider it to hold less value than a policy with a stronger positive consumer impact that may face higher feasibility concerns.
SCORING AND COLOR KEY
KEY
Dark green shade indicates significant/broad positive consumer impact or strong feasibility.
Light green shade indicates positive yet limited consumer impact or likely straightforward feasibility.
Grey shade indicates neutral consumer impact.
Light red shade indicates negative yet limited consumer impact or limited feasibility.
Dark red shade indicates significant/broad negative consumer impact or lack of feasibility.
SCORING
CONSUMER IMPACT
Dark red = -4
Light red = -2
Grey = 0
Light green = 2
Dark green = 4
FEASIBILITY
Dark red = -3
Light red = -1
Light green = 1
Dark green = 3
APPENDIX 1 | 67
68 | APPENDIX 1 Consumer Impact State Feasibility Policy Potential Impact on Affordability Potential Impact on Complexity Potential Impact on Coverage Potential Impact on Health Equity Political Feasibility* Financial Feasibility Implementation Capacity Score Broader Recommendations Invest in consumer assistance. 19 Integrate consumer engagement into the process of designing and implementing Maine’s state-based marketplace. 19 As a longer-term initiative, re-establish the Maine Office of Health Equity and empower its staff to coordinate equity efforts across the SBM, MaineCare, and all DHHS Offices. 17 Enrollment Periods OEPEarlier Start Date 15 OEPLater End Date 21 SEPPublic Health Crisis 13 SEPPregnancy 11 SEPEligibility/Technical Issues During Open Enrollment 9 SEPTax Filing 7 Displaying Clear Choice Plans Use an intake questionnaire and show plans based on responses 15 Build a comparison tool that: (1) automatically highlights differences between selected plans, and (2) includes a “Compare to Similar Plans” function 15 Include a pop-up glossary feature when customers hover over a technical term, and enable screen reading audio capability for accessibility 13 Distinguish Clear Choice plans with naming, visual cues, sorting, and/or filtering 13
Auto-Renewal Design more consumer-friendly auto-renewal notices for consumers.
Set the default for consumers eligible for cost-sharing reductions to high-value silver plans.
Auto-renew consumers with discontinued plans into Clear Choice plans.
Explore using auto-renewal defaults to incentivize carriers to lower costs.
Consider allowing consumers to choose their auto-renewal priorities
MaineCare Integration
Conduct a joint strategic planning effort across the Department of Health and Human Services
Resolve consumer-facing bottlenecks in MaineCare and SBM enrollment, specifically:
1) dedicate greater resources to solicit input from enrollment assisters,
2) improve the notification process for enrollment,
3) ensure that new portals make it easy to access and view enrollment status, and
4) explore the possibility of a “one-stop shop” for applications to both programs.
Work with other Maine agencies to implement and evaluate innovative approaches to increase MaineCare and marketplace coverage by directing outreach towards Mainers identified through income tax filing or UI claiming who lack coverage.
Planning for the Future
In the procurement, implementation, and maintenance of the SBM eligibility and enrollment system, prioritize platform capacity to adjust the inputs for the rules engine to adapt to future policy innovation.
APPENDIX 1 | 69 Consumer Impact State Feasibility
Potential
Potential Impact on Complexity Potential Impact on Coverage Potential Impact on Health Equity Political Feasibility* Financial Feasibility Implementation Capacity Score
Policy
Impact on Affordability
19
17
15
13
3
21
13
9
13
Appendix Table 2: Uninsured Rates, By Demographic Groupi
i Maine ACS 2019 Estimates; some demographics not represented
70 | APPENDIX 2
Demographic Number of Residentsii Uninsured Rateiii Male 646,177 9.1% Female 681,446 7.0% 19-25 104,980 13.4% 26-34 145,795 14.1% 35-44 152,048 11.7% 45-54 175,132 12.1% 55-64 210,347 8.5% White alone, not Hispanic or Latino 1,248,381 7.8% Hispanic or Latino (of any race) 22,416 9.3% Black or African American alone 21,465 8.4% American Indian and Alaska Native alone 9,317 18.2% Asian alone 15,203 9.7% Two or more races 27,653 12.5% Some other race alone 5,382 8.2% <100% FPL 141,734 12.9% <138% FPL 219,680 13.3% 138% to 399% FPL 568,033 9.8% ≥ 400% FPL 514,161 4.1% ii Insured and uninsured, estimated iii Estimated
Appendix Table 3: Recommendations For Technology Improvements and Integration Between SBM And OFI
Recommendations
1. Make exchanging information between the SBM and OFI as seamless as possible. Platforms should be able to seamlessly exchange applicants’ details, including documents they have uploaded and determinations made by eligibility systems.
2. Offer applicants the capability to upload documents for eligibility verification. My Maine Connection does not currently offer this functionality. This creates significant hassle for applicants and lost productivity for OFI staff, as applicants must mail, e-mail, fax, or deliver documents in person that verify their eligibility. As a DHHS working group noted, “lost documents and lengthy back and forth communications between Department staff and clients cause significant delays in the processing of benefits.”174
As a result of these frictions, MaineCare applicants that are determined ineligible may face longer delays in enrolling on the marketplace and may need to rely on an SEP to enroll. This can result in coverage gaps.
The lack of an upload service also increases demand elsewhere for OFI: because MaineCare applicants cannot accomplish everything online, many apply in-person or over the phone, which leads to long waits for assistance.
3. Automatically import high-quality data into ACES, removing the need for manual entry. The Federal Data Services Hub is available to the FFM and SBMs. It enables the systems to pull relevant data held by various federal agencies which could impact eligibility for Medicaid and APTCs.
APIs could pull information from the data hub and format it in a way that is compatible with the Automated Client Eligibility System (ACES). Afterwards, algorithms or business rules can automatically populate and update the data and information on ACES, using data held in staging tables. This would significantly reduce the administrative burden on OFI to perform side-byside comparisons.
Planned State Actions
As part of their SBM RFP, DHHS requested a technology platform that enables the transfer of images, documents, and eligibility verification information between OFI and the SBM.
The SBM RFP called for document upload tools.
OFI intends to make progress on this issue. Deloitte was contracted to redesign My Maine Connection’s front-end, and as part of this work, some back-end features like document uploading are expected to be featured.175
4. Use the same Medicaid eligibility rules for the SBM and OFI systems. Different rules engines can produce different assessments, which increases administrative burden on OFI and is confusing for applicants to navigate. Importantly, the marketplace should maintain separate business rules for the determination of APTCs.
5. When possible, make platforms and systems mobile-friendly. Multiple stakeholders, especially assisters and navigators, emphasized that the State must consider Internet access when developing its application systems. Many of Maine’s rural communities still lack reliable broadband access, and interviewees recounted multiple experiences working with consumers whose only home Internet connection was on their mobile phones.
DHHS requested that the SBM platform interface directly with the Federal Data Services Hub as part of their SBM RFP.
Moreover, a DHHS working group anticipates that Deloitte’s My Maine Connection redesign will lay important groundwork for automating data entry into ACES.176
OFI noted the importance of account transfer files created by the SBM vendor being in a standard format (for processing in the ACES rules engine). Alternatively, a translation layer created by the SBM vendor could ensure the data from account transfer files can be processed in the ACES rules engine.
The SBM is moving in this direction. In the SBM RFP, DHHS stated the goal to “[u]se API to leverage State’s Automated Client Eligibility System (ACES) business rules whenever possible while maintaining a separate SBM rules engine and business rules for SBM-only determinations (e.g., APTC)”.
The SBM RFP identified “usability and adaptability for mobile devices” as a core function. It is unclear but likely that this includes mobile document upload functionality.
The Integrated Online Services RFP, currently being delivered by Deloitte, called for the system to perform “equally” on mobile and desktop hardware, and asked for the vendor to integrate “document and photo uploads” with DHHS systems 177
APPENDIX 3 | 71

Author Biographies
Danielle Beavers
Danielle was born and raised in South Jersey. She spent 10 years in the San Francisco Bay Area, first at Stanford and then in Oakland, pursuing racial justice advocacy. As the Greenlining Institute’s director of diversity and inclusion, she worked to promote job creation for people of color through workforce and supplier diversity initiatives in the banking, environmental, health, technology, insurance, and utility industries in California and at the federal level. Danielle is excited to learn additional strategies to promote agency in marginalized communities and narrow the racial wealth gap while at Princeton. She completed her summer internship with the GreenLight Fund. Post grad, she hopes to work in philanthropy or in nonprofit consulting to ensure that anchor institutions fully reflect and benefit America’s growing majority.
Kishan Bhatt
Kishan is completing his MPA in economics and health policy after a two-year government fellowship. His most recent placement was in London at the European Bank for Reconstruction and Development, where he worked with a small team to analyze and determine U.S. votes on project investments. He also spent time at the Federal Trade Commission in Washington, D.C., where he conducted and presented economic research on price effects from antitrust-exempted health care mergers. A New Jerseyan and Buffalo Bills fan, Kishan holds an A.B. summa cum laude from Princeton. His undergraduate thesis, an examination of medical debt and bankruptcy, won the top thesis awards from the School of Public and International Affairs as well as the Global Health Program. His ongoing policy interests are health services access and economic mobility.
Molly Brune
Molly grew up right outside of Washington, D.C., and worked on various domestic social policy evaluations at Abt Associates before coming to Princeton. Previously, she also worked on international impact evaluations at Social Impact, and spent a year as a Global Health Corps fellow in Uganda doing monitoring and evaluation for
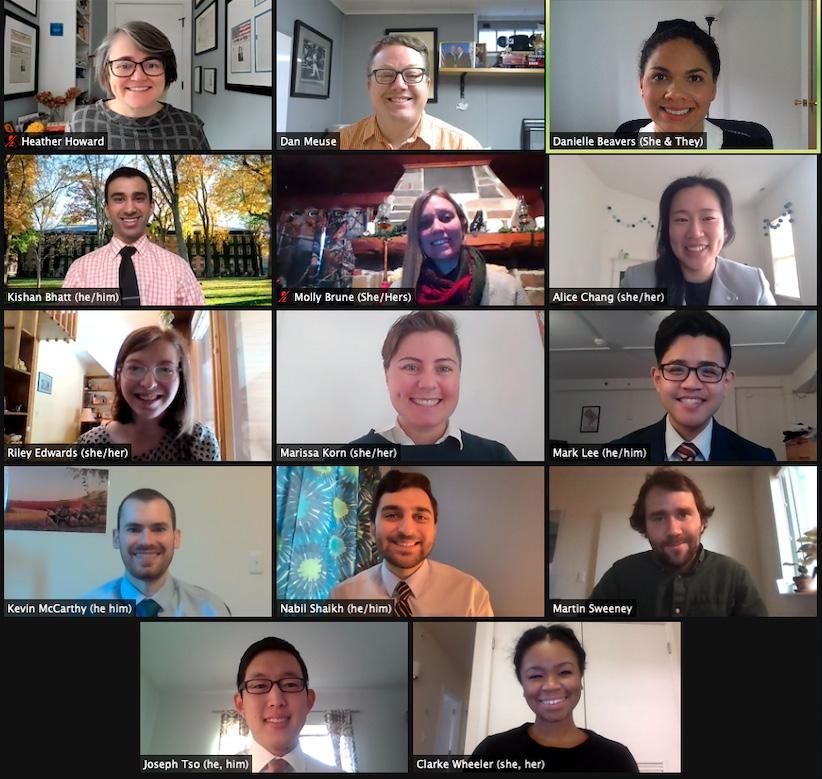
AUTHOR BIOGRAPHIES | 73
a nonprofit focused on health systems strengthening. This past summer, she completed an internship with the Office of Evaluation and Inspections at the Office of Inspector General for the U.S. Department of Health and Human Services. After completing her MPA, she hopes to work on integrated data systems and help cities better use their data to inform policy.
Alice Chang
Alice grew up in Potomac, Maryland, just outside of Washington, D.C., suburbs After studying economics and finance at the University of Maryland, Alice joined the Consumer Financial Protection Bureau (CFPB) as a director’s financial analyst. At CFPB, she worked on issues related to student loans and mortgages, including reviewing consumer complaints and assessing the effectiveness of mortgage servicing regulations. Prior to starting at Princeton, Alice was a research and policy analyst at the Student Borrower Protection Center, an organization solely dedicated towards alleviating the burden of student debt for millions of Americans. She completed her summer internship with the Citywide Analytics Team for the City of Boston. In her free time, Alice enjoys traveling, hiking, and practicing yoga.
Riley Edwards
Riley grew up in small towns in Wisconsin and Washington state before moving to New York City for college, where she majored in physics and political science. After graduating, she worked as a researcher at the Citizens Budget Commission, a nonpartisan, nonprofit research and watchdog organization focused on New York City and State government. Her focus was on increasing transparency and evaluation of economic development incentives, including the Amazon HQ2 deal. Riley’s policy interests include workforce development and economic justice for poor and working Americans. She completed her internship this past summer with the New Jersey Economic Development Authority.When not working, she can be found hanging out with her two cats, trying out new recipes, or playing bar trivia.
Marissa Korn
Marissa attended Northeastern University in Boston, earning a Bachelor of Science in political science and economics while minoring in gender studies. With a background in consumer health advocacy, Marissa has centered her career on expanding access to quality, affordable health care. Prior to arriving at Princeton, Marissa worked for Community Catalyst, providing technical assistance, campaign strategies, and capacity-building tools to state consumer health advocates promoting affordable health coverage in key states. More recently, as a Graduate Policy Fellow with State Health and Value Strategies, Marissa worked with a team of health policy experts providing technical assistance to state governments addressing COVID-19 and other policy priorities such as health equity, affordability, and coverage. Marissa is particularly passionate about reproductive rights advocacy, with experience volunteering for NARAL Pro-Choice Massachusetts and helping elect pro-choice Democratic women at the Barbara Lee Political Office in Cambridge, MA. Outside of her health care advocacy work, Marissa likes to play board games, watch the Red Sox, and visit new coffee shops.
Mark Lee
Originally from Southern California, Mark studied business administration at the University of California, Berkeley. Upon graduating in 2012, he relocated to Washington, D.C., where he spent five years working in consulting, media, and market research in the federal government sector. In 2017, he began working at the Human Rights Campaign, the nation’s largest LGBTQ rights organization. As the senior content manager of the HRC Foundation’s Public Education and Research program, he oversaw research studies and educational campaigns on a wide range of queer and trans issues, including anti-LGBTQ violence, racial justice, youth well-being, and paid family and medical leave. In the summer of 2020, he completed his MPA internship with the Office of Atlanta City Councilmember Amir Farokhi. A lifelong musician, Mark is a semi-professional pianist and vocalist who loves performing and enjoying music of all genres. He is also an avid biker, hiker, adventurous foodie, and self-professed boba tea aficionado. At Princeton, Mark will be concentrating on domestic urban policy, which he hopes to apply toward supporting marginalized communities at the local and municipal government level.
74 | AUTHOR BIOGRAPHIES
Kevin McCarthy
Kevin grew up in rural Northern California, and graduated from UC Berkeley in 2014. He most recently worked at the Center for Effective Global Action (CEGA) at UC Berkeley, where he managed a portfolio of technology-focused international development research projects. Prior to joining CEGA, he worked in the antitrust practice of an economic consulting firm, providing data analysis and research support for expert testimony. For his summer internship, Kevin worked with the Ayroles Lab at Princeton. Kevin’s academic interests are focused on technology policy, especially around the implementation of new data science tools and how it intersects with health and economic policy.
Nabil Shaikh
Through the Scholars in the Nation’s Service Initiative at SPIA, Nabil spent two years working at the U.S. Department of Justice on enforcing the civil rights of individuals with Opioid Use Disorder, prisoners on mental health watch, and nursing home residents affected by the COVID-19 pandemic. Before entering Princeton’s MPA program, Nabil worked in Congress on thwarting the attempted repeal of the Affordable Care Act, developed policies for the New Jersey state government to address health disparities, and studied global access to end-oflife care with the Princeton Center for Health and Wellbeing. He enjoys stand-up comedy, baking, and long walks with audiobooks.
Martin Sweeney
Martin entered the MPA program after working for nearly four years at the Behavioural Insights Team (BIT), a spin-off of the UK Cabinet Office that applies behavioral science and evaluation to public policy challenges. Martin joined BIT’s North America office in 2015 as one of the team’s original members and supported six US cities deliver low-cost evaluations through the “What Works Cities” initiative. Upon moving to BIT’s headquarters in London, Martin worked as a lead researcher on a wide variety of projects with partners and government departments in the UK and abroad. Prior to joining BIT, Martin worked at Innovations for Poverty Action, where he managed and analyzed data for a number of randomized controlled trials in international development. Martin graduated from Middlebury College in 2013 with a B.A. in economics and environmental studies. He completed his MPA internship this past summer working for the London Borough of Hackney. After completing the MPA, Martin hopes to continue using data and evidence to improve public policies and services.
Joseph Tso
Joseph originally hails from Los Angeles, California, but spent a decade in the Washington, D.C., area after graduating from Georgetown University in 2011. Prior to arriving in Princeton, he worked for the American Federation of State, County and Municipal Employees, a public sector labor union. As a strategic analyst, Joseph worked on both public and private sector union campaigns, and was also involved in internal data analysis for the union. He interned this past summer with the New Jersey Division of Consumer Affairs, where his portfolio included projects around the state’s COVID response efforts. Joseph’s academic passions center around the role of public policy in marginalized communities, with a specific focus on the effects of health care and social services. In his free time, he enjoys basketball, video games, and mahjong.
Clarke Wheeler
Born and raised in Washington, D.C., Clarke graduated from Barnard College with a Bachelor of Arts in political science and Africana studies in 2016. Most recently before joining the MPA program, she was a government relations associate at Planned Parenthood of New York City, where she advocated for sexual and reproductive health, rights, and justice through stakeholder engagement, coalition partnerships, and policy analysis and advising. Prior to this role, she participated in the New York City Urban Fellows Program, through which she worked at the NYC Department of Consumer Affairs Office of Financial Empowerment and coordinated the NYC Free Tax Prep Initiative. She was also a participant in the Fellowship for Emerging Leaders in Public Service, a program of NYU Wagner and the NYU Leadership Initiative. This past summer, she completed the MPA internship working with the Center for the Study of Social Policy, with a focus on child welfare, anti-racism, and abolition.
AUTHOR BIOGRAPHIES | 75
Faculty Advisors
Dan Meuse, Deputy Director of the Advancing Coverage in States, and State Health and Value Strategies programs, is based at the Center for Health and Wellbeing. He assists the program director in managing and coordinating the technical assistance providers serving states in their implementation of the Affordable Care Act and various payment and delivery system reforms. Dan was deeply involved in Affordable Care Act implementation at the state level as Deputy Chief of Staff for Rhode Island's Lieutenant Governor. Dan was the principle subject matter expert for the Rhode Island Healthcare Reform Commission on Health Insurance Exchange policy and delivery system and payment reform through mid-2014. He also served as the State Innovation Model project director for Rhode Island's Model Design project and led the Exchange's stakeholder engagement efforts. Dan received a Bachelor of Arts from Brown University and a Master's in Business Administration from Providence College.

Heather Howard is a faculty affiliate of the Center for Health & Wellbeing and director of State Health and Value Strategies, a Robert Wood Johnson Foundation-funded program that provides technical assistance to support state efforts to enhance the value of health care by improving population health and reforming the delivery of health care services. She served as New Jersey's Commissioner of Health and Senior Services from 2008-2010, overseeing a cabinet-level agency with a budget of $3.5 billion and staff of 1,700 responsible for public health services, regulation of health care institutions, senior services, and health care policy and research.
Previously, Howard served as Governor Jon Corzine's Chief Policy Counsel, directing his policy agenda. She also has significant federal experience, having worked as Senator Corzine's Chief of Staff, as Associate Director of the White House Domestic Policy Council and Senior Policy Advisor for First Lady Hillary Clinton, as an Honors Attorney in the U.S. Department of Justice's Antitrust Division Health Care Task Force, and for the U.S. House of Representatives. She received her J.D., cum laude, from the New York University School of Law, and her B.A. cum laude, from Duke University.

76 | AUTHOR BIOGRAPHIES
Dan Meuse
Heather Howard