Advancing Health Equity in North Carolina
Recommendations for Improving Sickle Cell Disease and Maternal Health Care Among Medicaid Enrollees


Recommendations for Improving Sickle Cell Disease and Maternal Health Care Among Medicaid Enrollees

Princeton School of Public and International Affairs Policy Workshop Report
February 2022
Workshop Instructors
Heather Howard
Daniel Meuse
Authors
Nitya Agrawal
Emily Audet
Rachel Fehr
Sophie Graham
Philippa Haven
Conor Hussey
Jenna Overton
Jeff Simon
Annie Yu
Christine Zizzi
This report was prepared by Master in Public Affairs students at the Princeton University School of Public and International Affairs. This report incorporates information gathered through students’ independent research, interviews conducted from October to December 2021, and guidance from course instructors Heather Howard and Dan Meuse. The report fulfills the Princeton School of Public and International Affairs’ degree requirements for an immersive policy workshop and associated policy proposal.
The authors acknowledge the generous support and insights offered by the individuals listed below. Their perspectives and insight into the health care landscape of North Carolina guided the research and analysis used to develop the recommendations included in this report. The authors would like to especially acknowledge the guidance, wisdom, and support of professors Heather Howard and Dan Meuse. Finally, the authors would like to thank the staff of the North Carolina Department of Health and Human Services and the Princeton University School of Public and International Affairs, without whom this report would not have been possible. Specifically, Dr. Emma Sandoe for the opportunity to do this report and Ryan Linhart for his support with policy workshop logistics.
This report includes insights from a range of individuals, but the analysis and recommendations contained herein are solely the views and responsibilities of its authors.
North Carolina Department of Health and Human Services
Dr. Mandy Cohen, Former Secretary
Emma Sandoe, Associate Director of Strategy and Planning, NC Medicaid
Dave Richard, Deputy Secretary, NC Medicaid
Jay Ludlam, Assistant Secretary, NC Medicaid
Dr. Shannon Dowler, Chief Medical Officer, NC Medicaid
Julia Lerche, Chief Strategy Officer and Chief Actuary, NC Medicaid
Kimberley Kilpatrick, Contract and Compliance Specialist, NC Medicaid
Johns Hopkins University School of Medicine
Dr. Sophie Lanzkron, Director, Sickle Cell Center for Adults and Professor of Medicine
Justin Calhoun, Sickle Cell Program Supervisor
Susan Johnson, Sickle Cell Educator Counselor
Naomi Moore, Sickle Cell Educator Counselor
Community Care of North Carolina

Dr. Tom Wroth, President & CEO
Kimberly DeBerry, Maternal Child Health Director
Dr. Marian Earls, Deputy Chief Medical Officer
Carlos Jackson, Executive VP & Chief Data and Analytics Officer
Dr. Kate Menard, OB Physician Champion
North Carolina Community Health Workers Association
Honey Yang Estrada, President
Duke University Sickle Cell Center and SCD Community Advisory Committee
Dr. John Strouse, Hematologist, Pediatric Hematology-Oncology Specialist
Members of the SCD Community Advisory Committee
East Carolina University Sickle Cell Comprehensive Clinic
Dr. Darla Liles, Chief, Division of Hematology/ Oncology
Dr. Beng Fuh, Director
Dr. Charles Knupp
NC Child
Kaylan Szafranski, Health Program Director
La-Mine Perkins, Assistant Director of Community Engagement
North Carolina General Assembly
Representative Ricky Hurtado (D – District 63)
North Carolina Justice Center
Hyun Namkoong, Deputy Project Director, Health Advocacy Project
North Carolina Medical Society
Chip Baggett, Executive Vice President & Chief Executive Officer
Alan Skipper, Vice President, External Affairs
Ashley Rodriguez, Chief Legal Officer
NCCARE360
LaQuana Palmer, Program Director
Princeton University
Dr. Keith Wailoo, Henry Putnam University Professor of History and Public Affairs
Triangle Doulas of Color
Ste’Keira Shepperson, Owner, Birth Doula, Postpartum Doula, and Childbirth Educator
UnitedHealthcare
Karla Theobold, Director of Maternal and Child Health
Dr. Michelle Bucknor, Chief Medical Officer, Community & State
Dr. Robert Eick, VP of Clinical Strategy
Dr. Derrick Hoover, Medical Director, Community & State
Kern Eason, Clinical Practice Performance Consultant, Maternal and Child Health
University of Minnesota School of Public Health
Katy Kozhimannil, Distinguished McKnight University Professor, Division of Health Policy and Management
University of North Carolina Collaborative for Maternal and Infant Health

Erin McClain, Assistant Director and Research Associate
Kimberly Harper, Perinatal Neonatal Outreach Coordinator
University of North Carolina Gillings School of Global Public Health
Dorothy Clienti, Associate Professor, Department of Maternal and Child Health
University of North Carolina OneSCD
Dr. Jane Little, Director of the Adult Sickle Cell Program
Dr. Jacki Baskin, Pediatric HematologyOncology Specialist
Tara Alin, Nurse Practitioner
Diana Wells, Clinical Social Worker
WellCare
Sue Lynn Ledford, North Carolina Director of Field Services
Affordable Care Act
American Society of Hematology
Cesarean Section
Community-Based Organization
Community Care of North Carolina
Centers for Disease Control and Prevention
Children’s Health Insurance Program
Community Health Worker
Certified Midwife
Centers for Medicare & Medicaid Services
Certified Nurse Midwife
Certified Professional Midwife
Delayed Hemolytic Transfusion Reactions
Day Hospital
Department of Health and Human Services
Division of Public Health
East Carolina University
Emergency Department
European Medicines Agency
Early and Periodic Screening, Diagnostic, and Treatment
External Quality Review Organization
Food and Drug Administration
Federal Poverty Level
Health Effectiveness Data and Information Set
Health Resources and Services Administration
Hydroxyurea
Institute for Clinical and Economic Review
Local Health Departments
Mountain Area Health Education Center
Managed Care Organization
Maternal, Infant, and Early Childhood Home Visiting Program
Michigan’s Maternal Infant Health Program
North Carolina Department of Health and Human Services
Non-Emergency Medical Transportation
Nurse-Family Partnership
National Institutes of Health
National Quality Forum
Primary Care Physician/Provider
Prepaid Health Plans
Pregnancy Medical Home
Quality-Adjusted Life Year
Red Blood Cell
Subscription-Based Payment Model
Sickle Cell Disease
Sickle Cell Data Collection
Social Determinants of Health
State Plan Amendment
Transcranial Doppler
Ultrasonography
Transportation Network Companies
University of North Carolina
Vaso-Occlusive Crisis
The following report outlines strategies for the North Carolina Department of Health and Human Services (NC DHHS) to consider implementing in order to improve Medicaid enrollees’ access to and quality of care. These strategies specifically focus on the health outcomes and racial and ethnic disparities that exist among two populations, enrollees living with sickle cell disease (SCD) and enrollees who are pregnant or postpartum.
This report is based on stakeholder interviews conducted in North Carolina in Fall 2021 and a literature review focused on Medicaid’s role in advancing health equity for these two populations. The interviews and literature review revealed that Medicaid enrollees, including enrollees with SCD and who are pregnant or postpartum, face similar barriers to quality care, such as transportation, provider bias, care management, and data gaps. Several SCD-specific challenges were identified, including continuity of care during the pediatric to adult transition, access to care, and lack of universal screenings. Challenges specifically related to pregnant and postpartum enrollees were also identified, including the lack of clinical and non-clinical support during pregnancy and postpartum and the lack of continuity of care across the peripartum period.
This report provides recommendations for NC DHHS to address each of these challenges. The goal of these recommendations is to ensure that the promise of Medicaid Managed Care is fulfilled, and that the needs of enrollees who are at a higher risk of experiencing barriers to quality care are sufficiently addressed.
Below is a high-level summary of recommendations for NC DHHS, Medicaid, and/or DPH to implement in order to improve Medicaid enrollees’ access to and quality of care.

Rural Health
• NC DHHS should convene a working group with two subcommittees—one for SCD and one for maternal health—to develop best practice standards for establishing hub and spoke models of care.
Transportation
• NC Medicaid should offer ridesharing as a form of Non-Emergency Medical Transportation (NEMT).
• NC Medicaid should provide NEMT tailored to the needs of pregnant and postpartum women.
Provider Bias Training
• NC DHHS should expand and improve its implicit bias training requirements to include perinatal and SCD providers.
Non-Medical Drivers of Health
• NC DHSS should increase resources in NCCARE360 and CBOs to ensure their ability to address non-medical drivers of health.
Data Gaps
• NC DHHS should ensure the public has access to timely and useful data.
Care Management
• Pediatric to Adult Transition Care Models. NC Medicaid should encourage support during the transition of pediatric patients with SCD into adult care.
• Primary and Specialty Care Coordination. NC Medicaid should invest in the development of a network of primary care providers (PCPs) knowledgeable about the treatment of SCD and should implement additional financial incentives for care coordination between PCPs and SCD experts.
• DPH Existing Programs. NC DHHS should support legislation to increase funding for the NC Sickle Cell Syndrome Program to ensure continuous care and treatment for people with SCD.
Access to Care and Services
• Telehealth. NC Medicaid should cover physician and hospital outpatient telehealth services at parity for people with complex care needs, including the Medicaid population that experiences SCD.
• Sickle Cell Day Hospitals. NC DHHS should bolster established SCD day hospitals in North Carolina.
• Hydroxyurea. NC Department of Health Benefits (DHB) should aim to improve hydroxyurea (HU) access and uptake among people with SCD.
• Pain Management. NC Medicaid should require PHPs to take steps to improve pain management approaches within the SCD population.
• Red Blood Cell Molecular Testing. NC Medicaid should expand required newborn traditional blood testing.
• Transcranial Doppler Ultrasonography. NC Medicaid should facilitate annual transcranial doppler ultrasonography (TCD) screening for children with SCD aged 2 to 16.
Leveraging Prepaid Health Plan Contracts
• Priority Population. NC Medicaid should include “people with sickle cell disease” as a priority population in PHP contracts.
• Quality Measures. NC Medicaid should assess PHP performance on outcomes for people with SCD.
Payment Models
• Incentive Programs. NC Medicaid should explore innovative payment models, such as incentive programs, to increase utilization of recommended SCD treatments and improve SCD health outcomes.
• Subscription-Based Payment Models. NC Medicaid should explore innovative payment models, including SubscriptionBased Payment Models (SBPMs), to increase utilization of new therapeutics and improve SCD health outcomes.
Care Management
• Home Visits. NC Medicaid should expand the coverage and quality of services provided through home visiting programs.
• Postpartum Continuity of Care. NC Medicaid should improve access to and continuity of care during the postpartum period.
Care Services
• Doula Services. NC Medicaid should cover and support doula services.
• Group Prenatal Care. NC Medicaid should require PHPs to cover group prenatal care.
Access to Care and Services
• Midwife Workforce. NC DHHS should support changes to the state midwifery certification and reimbursement processes..
• Screening of Perinatal Mental Health Conditions. NC Medicaid should incentivize PHPs to conduct perinatal mental health screenings.
Quality Measures
• NC Medicaid should encourage PHPs to decrease disparities in maternal health outcomes.
Administrative Burden
• NC Medicaid should reduce administrative burdens that keep pregnant and postpartum enrollees from enrolling in Medicaid.
• NC Medicaid should improve enrollees access to translation services during perinatal appointments.
North Carolina has long been a leader in designing and implementing innovative and bipartisan programs that address health care delivery and non-medical drivers of health. Almost 50 years ago, the state created the Sickle Cell Syndrome Program. This program is focused on delivering services to meet the changing needs of sickle cell disease (SCD) patients.1 Ten years ago, the NC Department of Health & Human Services (DHHS) established a pregnancy medical home (PMH) model for Medicaid patients. PMHs deliver care to pregnant and postpartum enrollees in a holistic way that includes non-clinical support such as health management and community services.2 In 2018, NC DHHS’ five-year Healthy Opportunities program was approved through a Centers for Medicare & Medicaid Services (CMS) 1115 Medicaid Waiver. Healthy Opportunities funds projects focused on non-medical drivers of health, such as the nation’s first electronic, statewide directory of organizations connecting health care and human services, called NCCARE360.3
2022 represents a pivotal year for DHHS. DHHS is operating amidst the COVID-19 pandemic, which is disproportionately impacting those with Medicaid and, as we have seen, Black communities.4 On top of the pandemic, NC Medicaid began transitioning the majority of Medicaid enrollees from fee-for-service to Prepaid Health Plans (PHP)—typically called Managed Care Organizations (MCOs) in states with similar models—in July of 2021. PHPs encompass both Standard Plans and Tailored Plans—designed for people with significant behavioral health needs and intellectual/ developmental disabilities—that will launch in December 2022.5 In this report, we will use PHPs when discussing North Carolina Standard Plans and MCOs when discussing other state models.
NC DHHS officials requested assistance on two health equity-focused policy areas. Specifically, the state Medicaid agency welcomed recommendations on how to design care and payment models for enrollees living with SCD and how to decrease racial and ethnic disparities in maternal health outcomes. While these are two different health experiences, both are marked by glaring racial inequities.
One limitation of this report is that NC Medicaid alone cannot adequately address the systematic racism that leads to inequities in SCD and maternal health outcomes. A second limitation is that this report’s scope does not include the Eastern Band of Cherokee Indians Tribal care management plan. As a result, the barriers to care that the North Carolina Indigenous population faces are not addressed. Nevertheless, NC DHHS has the ability to greatly improve the health outcomes and reduce disparities within SCD and maternal health, as this report recommends.
This report envisions a North Carolina where Medicaid enrollees face no shortage of providers and can access care without barriers, Medicaid providers are trained to overcome biases in care, and non-medical drivers of health are fully integrated into the health system. Medicaid enrollees with SCD would receive care from medical professionals who understand their community and holistic care needs, have the option of receiving medical care from the comfort of their home, and have access to fundamental SCD services like hydroxyurea, red blood cell molecular testing, and transcranial doppler screenings. Medicaid enrollees who are pregnant would have access to navigators, multiple home visits, and doulas and certified midwives, and those who are postpartum would receive pre-discharge postpartum care plans and depression screenings and treatment.
The authors of this report are ten Master of Public Affairs candidates at Princeton University’s School of Public and International Affairs. The graduate students had assistance and guidance from co-instructors Heather Howard and Daniel Meuse, who lead the State Health and Value Strategies program of the Robert Wood Johnson Foundation.
Between October and December 2021, 22 stakeholder meetings were conducted with representatives from 17 organizations in North Carolina, along with several maternal health and SCD experts from across the nation. Stakeholders included health care providers, PHPs, medical research and academic institutions, government agencies, and patient advocacy groups. The following report incorporates feedback from these meetings, as well as a review of data, academic literature, and evaluations of other state Medicaid policies.
One limitation to our methodology is that our investigation lacks interviews with Medicaid enrollees. Obtaining institutional review board approval was not feasible given our report timeline. We recommend that NC DHHS invites Medicaid enrollees who are SCD patients or pregnant or postpartum mothers to speak about their experience accessing care. Given Medicaid enrollees face resource constraints, NC DHHS should compensate enrollees for taking the time to speak with them.
Stakeholders were overwhelmingly receptive to the recommendations outlined in this report and believed that the recommendations would take North Carolina one step closer to ideal care. We addressed any concerns about operational feasibility that came up in our interviewees, either by adjusting our recommendation or detailing the implementation challenges. North Carolinian stakeholders agreed that while the political will to pass the following recommendations is strong, the prospects of legislative approval are unlikely. Given the political landscape, we recommend prioritizing the recommendations that can be implemented unilaterally.
In this report, we use “women” and “mothers” to describe pregnant or postpartum people. Of note, we recognize that not all people who become pregnant or give birth identify as women. We use these terms to align with the language in the Social Security Act, which establishes pregnancy Medicaid.
Part I of our report details overlapping themes and recommendations for the SCD and maternal population. Part II provides recommendations for designing care and payment models specifically for the SCD population. Part III provides recommendations on Medicaid interventions to improve maternal health outcomes through innovative care and payment models.
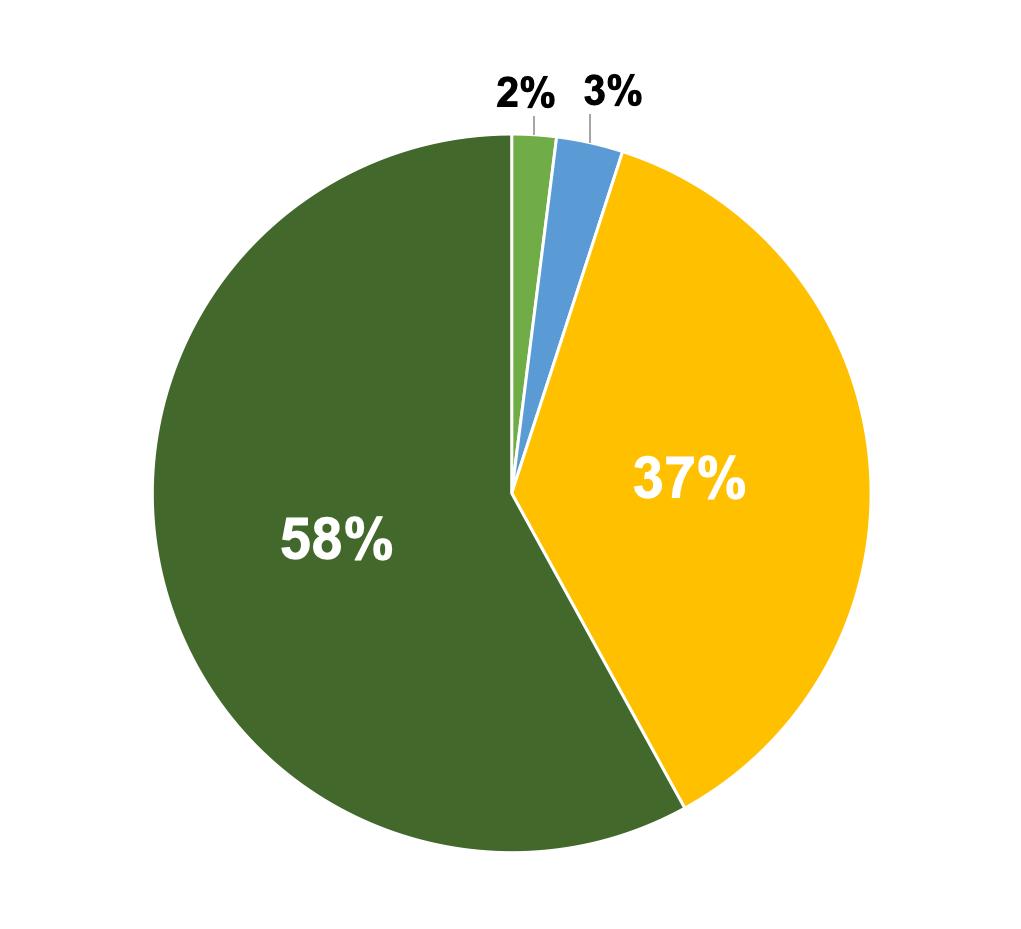
North Carolina’s population is 70.6 percent white alone, 22.2 percent Black or African American alone, 3.2 percent Asian alone, and 1.6 percent American Indian or Alaska Native alone.6 The state’s population is 9.8 percent Hispanic or Latino. Twelve percent of North Carolinians speak a language other than English at home.7 Figures 1 and 2 display the Black population by county and the overall racial demographics of Medicaid enrollees in North Carolina.
The median household income is $54,602 (in 2019 dollars) and 13.6 percent of people are below the poverty line.8 Figure 3 shows the poverty rate by county and Figure 4 shows urban/rural designations by county.
Sickle cell disease (SCD) is the most common inherited blood disorder in the United States, with approximately 100,000 Americans having SCD.9 Medicaid is the predominant source of health insurance for people with SCD, covering about 67 percent of children and 45.7 percent of adults with the disease nationally.10 Within North Carolina, approximately 5,000 North Carolinians have SCD.11
Percent of Population that Identifies as Black/African-American (2020)
Figure 1. Percent of North Carolina Population that Identifies as Black/African-American (2020)
0% 60%
© OpenStreetMap
Source:2020 US Census
Data source: 2020 UC Census
Data source: NC DHHS
Indigenous Asian Black White
8% 28%

© OpenStreetMap
Data source: 2019 American Community Survey 5-Year Estimates
Source: 2019 American Community Survey 5-Year Estimates
© OpenStreetMap
Data source: USDA Economic Research Service
Source:USDA Economic Research Service
Additionally, 80 infants in North Carolina are diagnosed with SCD each year.12 In 2017, 2,082 North Carolina enrollees, or five percent of Medicaid and Children’s Health Insurance Program (CHIP), had SCD.13
SCD is rare among white Americans, with Black newborns being 24 times more likely than white newborns to carry the sickle cell trait.14 It is important to note that SCD affects people of other ethnic minorities, although at a lower rate. One in 12 Black Americans carry the SCD trait, while one in 100 Hispanic Americans carry the SCD trait.15
SCD is caused by a mutation affecting red blood cells (RBCs). While healthy RBCs are round and glide easily through blood vessels, RBCs in people with SCD are sickle-shaped and stiff. This results in RBCs sticking together and blood vessel blockages damaging vital organs and tissue.16
The sickle-shape can cause extensive and severe morbidity.17 Blood vessel blockages can result in the following: i) acute pain episodes, known as “vaso-occlusive crises” (VOCs) or “pain crises;” ii) chronic pain, whose origins are not well-understood; iii) heightened risk of strokes, which in turn may result in cognitive deficits; and, iv) acute chest syndrome if there are blockages in the lung tissue, which is the most common cause of death among people with SCD.18 Median life expectancy for people with SCD is only 42 to 47 years.19
Care utilization for people with SCD is very expensive and often involves hospitalization. In 2012, SCD was ranked the fifth most common principal diagnosis for hospital stays among Medicaid “super-utilizers”—those with four or more hospital stays during the year.20 Pain is the most common SCD morbidity and the primary driver of SCD-related hospitalizations.21 About 81 percent of the costs for SCD-related complications are attributable to inpatient hospital care. Improvements in comprehensive care have the potential to reduce hospitalizations and related costs.22
North Carolina has a strong infrastructure for caring for individuals with sickle cell disease because of its Sickle Cell Syndrome Program, located within the Division of Public Health (DPH). The NC Sickle Cell Syndrome Program provides genetic counseling, education, medical services, reimbursement for treatment, screening, and care coordination. It includes nine regional Educator Counselors, one community-based organization, the Piedmont Health Services and Sickle Cell Agency, six comprehensive sickle cell medical centers, and state program staff.23 However, the NC General Assembly has not increased the program’s budget since the 1980s (except for modest salary increases). The program’s funding levels have not kept pace with the availability of new, more expensive treatments for SCD. The Governor’s appointed Council on Sickle Cell Disease and Other Blood Disorders is currently developing a ten-year plan to address this funding constraint.
The U.S. has one of the highest rates of maternal death and maternal morbidity of any high-income country, and North Carolina’s rates are below the national average. Nationally, an estimated 13 percent of women become pregnant experience life-threatening or potentially life-threatening conditions during the peripartum period.24 An additional 15 percent of women have other maternal complications that are not lifethreatening but serious nonetheless.25 Between 2014 and 2015, 35 North Carolinians died of pregnancy-related causes during pregnancy or within one year postpartum, and many more suffered from maternal complications that did not end in death.26
Examining aggregated data, however, does not show the whole picture. There are significant disparities in health outcomes experiencedby Black pregnant women compared to white pregnant women. In North Carolina, Black women have almost twice the risk of dying from pregnancy-related complications than white women.27 Racial inequities are particularly stark
among the Medicaid population—nationally, Black women with Medicaid are about four times more likely to suffer a severe maternal morbidity than white women with Medicaid.28 Sadly, racial disparities in maternal outcomes are not narrowing, and actually have increased in North Carolina over the past 20 years. 29
Because Medicaid covers more than half of births in North Carolina (see Figure 5), NC Medicaid plays an important role in reducing maternal mortality and morbidity and eliminating racial disparities. Recent steps toward expanding pregnancy-related Medicaid coverage to one year postpartum, along with the transition to Medicaid Managed Care, make this an ideal moment for NC Medicaid to address maternal health disparities.
Women can die from pregnancy-related causes or experience other pregnancy-related issues throughout the peripartum period. Nationwide, 31 percent of maternal deaths occur while women are pregnant, 17 percent during childbirth or in the period shortly after childbirth, and the remaining 52 percent occur after the day of delivery during the first year postpartum.30 The leading causes of pregnancy-related deaths among Black women are a weakened heart muscle (cardiomyopathy) and cardiovascular conditions.31 Of note, these mortality statistics only focus on pregnancy-related issues. Overall, homicide is the leading cause of death while a woman is pregnant or within one year postpartum, with Black women at the highest risk.32 Policies to reduce the risk of homicide during the peripartum period are beyond the scope of this report. However, domestic violence referrals are a component of NC Medicaid’s Healthy Opportunities pilots.33
© OpenStreetMap
Note:"Prenatal Medicaid" means that Medicaid paid for prenatal care and delivery.
Data source: State Center for Health Statistics, NC DHHS
Source:State Center for Health Statistics NC Department of Health and Human Services
Researchers point to a multitude of factors contributing to the high rates of maternal mortality and morbidity across the U.S. First, increased rates of underlying—often undiagnosed—conditions, such as hypertension or diabetes, result in increased health risk for the person while pregnant and postpartum and can increase the likelihood of preterm labor.34 Second, the lack of access to adequate prenatal care throughout pregnancy can result in under-management of pregnancy conditions and risks.35 Third, hospitals overutilize labor interventions, such as cesarean sections (C-sections) and epidurals, that can worsen health outcomes when used unnecessarily.36 Fourth, the lack of continuous care after sixweeks postpartum results in clinicians missing early detections of postpartum complications.37 Finally, structural racism in the health system affects patients’ access to care and results in bias in care received while in clinical settings.38
We must examine these racial disparities through a lens that considers systemic factors and non-medical drivers of health. Women with preexisting chronic conditions (e.g., diabetes, hypertension), mental health disorders (e.g., depression, substance abuse) and prepregnancy obesity have an increased likelihood of experiencing a poor maternal outcome.39 Black women suffer from these medical conditions at a higher rate due in part to systemic racism and non-medical drivers of health such as access to housing, food, and social support systems. Black pregnant women are also more likely to be treated at underfunded, low-quality hospitals, which contributes to worse outcomes.40 Even when receiving care at the same hospital, Black women are at higher risk for maternal mortality and morbidity than white women.41 In rural areas, these racial disparities can be compounded by access issues and provider shortages, as many rural North Carolina hospitals have shut down their maternity units in recent years.
The North Carolina Maternal Mortality Committee determined that 63 percent of maternal deaths were preventable. Forty-one percent of these
preventable deaths were classified as “having a good chance to avert the outcome ‘by one or more changes to patient, family, provider, facility, system and/or community factors.’”42 Although the Committee did not break down the data by race, nationally Black pregnant women are more likely to die from a preventable death.43
Not only are these poor maternal health outcomes disastrous for the women and babies in North Carolina, they also cost the state’s health care system money. Medicaid births with complications cost almost twice as much as births with no complications.44 Additionally, postpartum women with poor maternal health outcomes have a higher chance of being readmitted to the hospital and may have longterm health issues that cost the state.
Infant mortality, and racial disparities present in the infant mortality rates, are also major issues in North Carolina. In 2019, the Black infant mortality rate was 2.7 times that of the white infant mortality rate. Many of the same factors that contribute to maternal mortality and morbidity within the Black population in North Carolina also affect poor infant outcomes. While reducing the infant mortality rates is an extremely important component of improving the health of North Carolinians, this report will focus on efforts to improve maternal health.
In the U.S., systemic racism has led to unequal resource allocation and Black, Indigenous, and people of color having less wealth, lower socioeconomic status, poorer access to health care, and worse health outcomes compared to their white counterparts—all of which impact health outcomes. Racism also negatively impacts mental and physical health and is a fundamental driver of racial and ethnic health disparities.45
The health care system itself is not immune to the racist and discriminatory practices of broader society. Hospitals were rigidly segregated in the 19th and 20th century until the threat of losing federal funding from Medicare in 1965 forced them to desegregate. Medical professionals participated in state-sanctioned sterilizations of Black, Indigenous, and other people of color in the 20th century, and also led the Tuskegee Syphilis Study that withheld treatment from hundreds of Black men to track the course of disease. Medical education perpetuated false beliefs of biological differences like greater pain tolerance among Black people.46 These legacies of mistreatment that generated medical mistrust among communities of color are exacerbated by the firsthand negative experiences people of color have with providers who discriminate against them.
In recent years, racial health disparities have gained attention as the country reckons with racial injustice. This report provides policy recommendations that are focused on addressing coverage, access, and clinical health needs. These recommendations also incorporate the understanding that racism is embedded in the health care system and improving health outcomes requires more than addressing health care. Improving health outcomes requires confronting the systems that have led to generational injustices that result in racial and ethnic health disparities, as well as a peoplecentered approach and a critical assessment of policies.
Sickle cell disease sits at the intersection of racism and the health care system. SCD primarily affects people with African ancestry. The perception of SCD as a “Black disease” and proxy for Black health has shaped attitudes towards people affected by the disease. In the early 20th century, sickled cells were viewed as an “inherent feature of Negro blood” and
used to confirm fundamental biological race differences and prejudice about racial mixing and integration.47 As medicine’s interest in the disease grew, people with SCD became valued as medical subjects—however, there was a reductionist focus on blood cells and the molecular level of the disease, not the patient experience or pain associated with SCD.
Pain is a major symptom of the disease, but the difficulty of objectively measuring pain led to a decline in sympathy for people with SCD and a crisis of patient credibility; the frequent pain episodes and fatigue that people with SCD experience can cause absenteeism, contributing to a stereotype of unreliability and fragility. Society also began to associate inferiority, addiction, and low mental capacity as the “real” problems with SCD, and this stigma has led to discrimination, devaluation, lower quality of care, strained patient-provider relationships, and greater pain from being labeled as drug seeking and providers not taking their pain seriously. Many problems intersect with anti-Black prejudice: studies show racial disparities in pain assessment and treatment, and providers are more likely to dismiss Black people’s pain.48,49
In 1972, the National Sickle Cell Anemia Control Act of 1972 was passed, which provided funding for research, patient care, and reproductive counseling for parents. Although the legislation provided much needed attention to SCD, reproductive counseling also raised very real concerns of discrimination, eugenics, and reproductive control of Black bodies. Linus Pauling, one of the people who discovered that hemoglobin played a major role in the formation of sickle red blood cells, once suggested “[t] here should be tattooed on the forehead of every young person a symbol showing possession of the sickle-cell gene…”50 Thus, promises of innovations like gene therapy are tempered by mistrust and negative experiences with the health care system.
Despite being the most common genetic disease, SCD suffers from a lack of attention and resources. In the U.S., the projected life expectancy for people with SCD is 54 years compared to 76 years for people without SCD in the U.S.; quality-adjusted life expectancy is 33 years for people with SCD compared to 67 years for people without SCD.51 Despite gains in life expectancy, there is still no formal protocol for the transition from pediatric to adult care, leaving gaps in treatment and care.
Cystic fibrosis (CF), which is a comparable inherited, life-threatening disease that primarily affects white people, affects one-third fewer Americans than SCD, but receives four times the amount of federal funding and seven times the foundation funding.52 Few adult hematologists focus on SCD and most providers lack knowledge on SCD, which prevents people with SCD from receiving recommended therapies and appropriate pain management.53
Furthermore, stigma still surrounds SCD and the pain experienced by people with SCD continues to be undertreated. The story of SCD presents what Dr. Keith Wailoo, a historian of medicine, describes as a “disturbing portrait of America, one in which basic health and social services are often hard to obtain, in which skepticism about the motives of patients in pain is rampant, and in which high-stakes gambles [of expensive and risky treatments such as bone marrow transplantation and gene therapy] are too often championed as remedies instead of attending to basic health care needs.”54 Most SCD research has focused on dreams of breakthrough medicine without considering how the marketplace prevents people with SCD from accessing these expensive breakthroughs and overlooking the development of basic care protocols that could benefit many people with SCD.
There is a long history of racism within obstetrics and maternal care. During the era of slavery, J. Marion Sims—often referred to as the “father of modern gynecology”—developed his surgical techniques by experimenting on enslaved Black women.55 Additionally, François Marie Prevost developed the C-section by repeatedly performing the technique on enslaved Black women without consent and without any type of pain medication.56 Once these techniques were developed, however, doctors often failed to perform these interventions on Black women who needed them, choosing to use resources to provide these interventions to white women instead.57
During the 19th century, most U.S. women delivered their babies out of the hospital under the care of midwives, and labor and delivery was a woman-centered, autonomous process. Black midwifery had a strong presence within communities of color, as generations passed down an abundance of knowledge of labor and delivery techniques. However, with the professionalization of medical degrees among white men and a growing concern for the country’s high maternal and infant death rate, Black midwives were pushed out of the workforce. One North Carolina physician rejected Black midwives as having “fingers full of dirt” and “brains full of arrogance and superstition.”58 As deliveries became medicalized, the institutional knowledge of birth possessed by Black midwives was lost and the woman-centered, autonomous process was rejected. By 1950, most deliveries in the U.S. occurred in the hospital setting, placing the doctor in the forefront of the process and often ignoring women’s, and specifically Black women’s, wants and needs. Although the maternal and infant death rate drastically decreased since the 1950s, it is important to note that much of the credit is due to improved public health measures and that racial disparities actually grew during this time.59
The history of obstetric trauma experienced by Black women and the rejection of Black women being actively involved in the birthing process are still felt now. Although the rates of maternal death in the U.S. have drastically decreased compared to rates 100+ years ago, the number of deaths has increased over the past 20 years and the racial disparity in maternal outcomes has increased with it. In the 1990s, Dr. Arline Geronimus coined the term “weathering” to describe the physical and emotional toll being a Black woman in the U.S. takes on the body.60 A recent article described the concept—which has become widely accepted among maternal and child health researchers—as a “kind of toxic stress trigger[ing] the premature deterioration of the bodies of African-American women as a consequence of repeated exposure to a climate of discrimination and insults.”61 This concept, as theorized by Dr. Geronimus, can lead to greater adverse pregnancy outcomes among Black women.62 Today, Black women in the U.S. are five times more likely to die to due to pregnancyrelated causes than white women.
The intersection of SCD and maternal health culminates in poor health outcomes. Pregnant women with SCD have a high risk of morbidity and mortality. Women with SCD are 16 times more likely to die in childbirth than other women and 28.5 percent of women with SCD experience crisis during delivery.63 There is also an increased risk of stillbirth for pregnant women with SCD.64 These issues underscore the importance of quality care and coordinated care for this population that has been marginalized.
Health equity means that everyone has a fair and just opportunity to attain the highest level of health possible.65 Achieving health equity requires more than a focus on disease and treatment because the absence of disease does not equate to good health. 80-90 percent of a person’s health is determined by non-medical factors such as socioeconomic, physical environment, and health behaviors.66 Achieving health equity requires focused efforts to address systemic inequalities—including poverty, racism, and discrimination—that result in differences in health outcomes. As health policymakers in a position to elevate the needs of communities that are marginalized, we must intentionally apply a health equity lens and ensure that policies will uplift, and not harm, these communities. In this report, the authors provide targeted recommendations to improve the health outcomes of two Medicaid populations experiencing health disparities in North Carolina: people with SCD and pregnant or postpartum women.
NC DHHS has taken approaches to advance health equity. In 2021, NC Medicaid launched a temporary health equity payment initiative, which enhanced payments to Carolina Access primary care practices serving enrollees from areas in the state with high poverty levels.67 The goal of the program was to improve access to primary care and preventive services where historically marginalized populations faced challenges highlighted by the pandemic. NC Medicaid will evaluate this initiative and gather information to target future investments in programs that improve access to care and address health disparities.
NC DHHS’ Healthy Opportunities pilot emphasizes the importance of non-medical interventions in improving health outcomes. This investment in connecting residents to needed resources are likely to improve maternal health, especially for mothers of color, and aid individuals living with SCD. As the state implements its Healthy Opportunities strategy, it should look for ways to use pilots and lessons learned to advance the goals of this report.
In 2015, the NC General Assembly directed NC DHHS to transition Medicaid from a fee-forservice model to a Prepaid Health Plan (PHP) model. Under the fee-for-service model, NC Medicaid reimbursed providers based on the services they provided and procedures they ordered. In contrast, under the PHP model, the state contracts with insurance agencies, which receive a capitated per-member rate for health care services that is pre-determined and therefore allows for improved budget predictability. Under the PHP model, patient health outcomes are used to assess the performance of providers.
This shift reflects a national trend—approximately 70 percent of Medicaid enrollees in the U.S. are covered by PHPs, and before the transition, North Carolina had been the largest state in the country without substantial PHP involvement in Medicaid provision.68 The state estimated that 1.7 million of its 2.6 million Medicaid enrollees would transition to NC Medicaid Managed Care, which consists of a system of five PHPs.69 The North Carolina PHPs are AmeriHealth Caritas North Carolina, Healthy Blue, Carolina Complete Health, UnitedHealthcare Community Plan of North Carolina, and WellCare of North Carolina.
Beginning July 1, 2021, most Medicaid enrollees in North Carolina began receiving health care coverage through NC Medicaid Managed Care. Some enrollees with more intense health care needs and specific populations like people eligible for both Medicaid and Medicare and children in foster care continued to participate in traditional Medicaid, administered in a fee-for-service model through NC Medicaid
Direct.70 The transition to NC Medicaid Managed Care is still in early stages, but some smaller providers reported challenges in adapting their administrative processes and navigating the new PHP system.71
As Governor Cooper recently reiterated, North Carolina Medicaid expansion remains the ideal policy. Per North Carolina’s 202122 budget, a joint legislative committee was created in January 2022 in order to study the potential effects of Medicaid expansion in North Carolina.72 Build Back Better, federal legislation currently pending in Congress, offers the potential of providing greater coverage to North Carolinians through expanded Marketplace subsidies in non-expansion states. As the legislation has been written and passed in the U.S. House of Representatives as of November 19, 2021, people currently in the coverage gap in North Carolina would not pay premiums and would have access to low-deductible Marketplace plans.73
The recent postpartum coverage extension the NC General Assembly passed has the potential to significantly reduce maternal morbidity and mortality in North Carolina. More than half the maternal deaths in the U.S. happen after giving birth, making the postpartum period an especially vulnerable period for new mothers.74 For the most recent years with available data, Black non-Hispanic women in North Carolina had on average three times greater risk of dying during childbirth than white non-Hispanic women.75 The continuous coverage through oneyear postpartum holds significant promise to improve these disparities.
Expanding Medicaid is the single most meaningful step North Carolina could take to reduce racial health disparities in sickle cell disease and maternal health outcomes.
Over 2.6 million people, or one in four North Carolinians, are enrolled in Medicaid.76 However, over 1.1 million people, or 11 percent of the state’s population, remain uninsured.77 Medicaid expansion, which was not included in the FY 2022-23 state budget, would have cut the uninsured rate in half by providing Medicaid coverage to more than 600,000 North Carolinians.78
In states like North Carolina that have not closed the coverage gap—the population that is not eligible for Medicaid nor premium subsidies for a Marketplace insurance plan—people are at risk of churning into the coverage gap from Medicaid or the Affordable Care Act (ACA) Marketplace. In North Carolina, one in five income-eligible adults are at high risk of losing their Medicaid coverage because of the low eligibility threshold (41 percent of the federal poverty level (FPL)).79 The postpartum period is a particularly high-risk time for churn, and 20 percent of pregnant women who lose Medicaid coverage become eligible within a year.80 Similarly, people with SCD have high levels of churn: 31 percent of people with SCD enrolled in California’s Medicaid program and 40 percent of people with SCD enrolled in Georgia’s Medicaid program experienced gaps in coverage.81
Research on the impact of Medicaid expansion has found improvements in uninsured rates, access to care, care affordability and financial stability for enrollees, enrollee health outcomes, and economic benefits to states.82 Many of these changes are particularly impactful for people of color, those with very low incomes, and those living in rural areas.83 Medicaid expansion has benefited states through increased tax revenue, reductions in overall spending, and accelerated economic growth. Medicaid expansion has been shown to lead to roughly seven fewer maternal deaths per 100,000 births.84 This impact was driven by substantial drops in mortality among non-Hispanic Black mothers, leading to overall narrowing of racial disparities.
The following recommendations are based off of a critical analysis of the barriers SCD, pregnant, and postpartum Medicaid patients face in accessing quality care in North Carolina. Several overlapping barriers were identified after interviewing a diverse range of North Carolina stakeholders and perusing empirical studies focused on people with Medicaid. Developing standards for establishing hub and spoke models of care, expanding non-emergency medical transportation, improving implicit bias training, and publicizing key public health data will benefit the health outcomes of SCD, pregnant, and postpartum Medicaid enrollees.
NC DHHS should convene a working group with two subcommittees—one for SCD and one for maternal health—to develop best practice standards for establishing hub and spoke models of care.
Implementation:
• NC DHHS should convene a working group with two subcommittees—one for SCD and one for maternal health—to develop and publish best practice standards for providers that would like to establish or join a hub and spoke system.

• NC DHHS should incentivize providers to operate through hub and spoke models.
• NC DHHS should provide financial support for providers to establish and operate hub and spoke models.
• NC DHHS should support a telementoring program to facilitate instruction between hub and spoke sites.
Background
A “hub and spoke” model of health care delivery consists of a “hub” care provider, which offers a wide range of services and specialist care, and a network of “spokes”, or smaller outlying care centers that offer fewer services.85 The hub and spoke sites coordinate with each other to direct patients to the site most appropriate for their needs and assess the services they require, their risk level (e.g., their SCD care history, whether they have had pregnancy-related complications in the past), and the distance they can travel for care.
For SCD care, the spokes may be internists, primary care physicians (PCPs), emergency nurses, and hospitalists located in rural regions where SCD specialists are inaccessible. Shortages of SCD specialists drive the need for these spokes.
For maternal care, the spokes may be local community hospitals, family practices, midwifery services, or other clinics that focus on routine prenatal and postpartum care but may not have the resources to deliver babies or handle highrisk pregnancies.
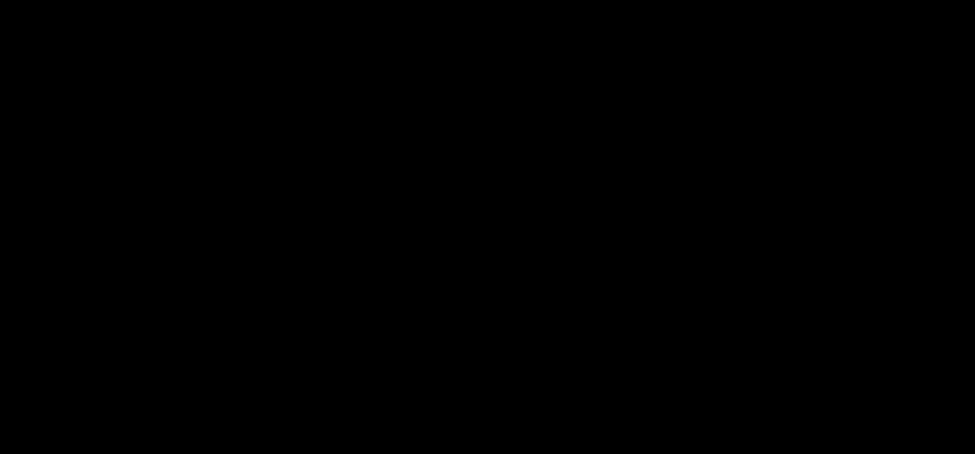
There is a range of potential SCD care models for high-need and/or high-risk patient populations, as displayed in Figure 6. Each model operates best in a specific setting— urban, suburban, or rural regions. For example, a classic comprehensive care center is ideal and feasible in an urban setting. However, this is not feasible in rural regions, including the rural regions of North Carolina.
Currently, North Carolina has six SCD comprehensive care centers: Atrium Health, Duke University, East Carolina University (ECU) School of Medicine, University of North Carolina (UNC)-Chapel Hill, Wake Forest University School of Medicine, and Mission Hospital (pediatric only).86 As a result, there are geographic disparities in access to physicians specializing in SCD care, such as hematologists/ oncologists. In North Carolina in 2019, about one hematologist/oncologist existed per 20,000 residents. Over 40 counties had no hematologist/ oncologist, including many counties in eastern North Carolina, which has a sizable population of newborns with SCD.87 There is a mismatch between the geographic distributions of hematologists/oncologists and newborns with SCD in the state. See Figures 7 and 8 for details, and note that these maps may underestimate the full extent of the problem.
Individuals with SCD who reside in rural areas are more likely to lack comprehensive coordinated care, have higher rates of acute care utilization and readmission, and greater dissatisfaction with care received, compared to their urban counterparts.88 In interviews with several key provider-facing and patient-facing NC stakeholders, difficulty with access to SCDspecific care for rural community members
was repeatedly raised. Stakeholders frequently mentioned difficulty surrounding the time required to travel long distances, money to pay for gas, timing of appointments, and low energy levels to make necessary drives.
Lack of access to specialized care hinders provision of standard SCD care, including standard treatments (e.g., hydroxyurea, iron chelation, transcranial doppler ultrasound screening). Additionally, as new medications for SCD offer hope for patients (e.g., crizanlizumab, voxelotor, L-glutamine), these treatments and, subsequently, potentially improved outcomes will not be available without access to specialized care. New therapeutics cannot stand alone— regular comprehensive care is needed.
In a 2020 Institute for Clinical and Economic Review (ICER) report, patients with SCD expressed concerns about doctors not knowing enough about new therapies to be willing to write prescriptions.89 In a 2021 study of providers in the U.S., significant barriers to providing care were influenced by providers’ specialty, training, and practice setting.90 Providers that were not SCD specialists were not comfortable providing essential SCD care.
Access to adult comprehensive SCD programs is associated with numerous improved health outcomes, including fewer acute care visits, fewer emergency department (ED) visits, fewer hospitalizations, and decreased health care costs overall.91 Additionally, access to SCD care leads to increased likelihood of being prescribed hydroxyurea (HU), which has been shown to lead to improved psychosocial outcomes.92 All of these improvements contribute to anticipated improved qualityof-life and improved cost-effectiveness when compared to ED-based care. With many SCD patients living in rural communities and without immediate access to one of North Carolina’s six comprehensive care centers, improved care coordination between rural providers and comprehensive SCD centers is essential and can be achieved through hub and spoke models.93
Source: Julie Kanter et al., “Building Access to Care in Adult Sickle Cell Disease: Defining Models of Care, Essential Components, and Economic Aspects,” Blood Advances 4, no. 16 (2020): 3804–13.
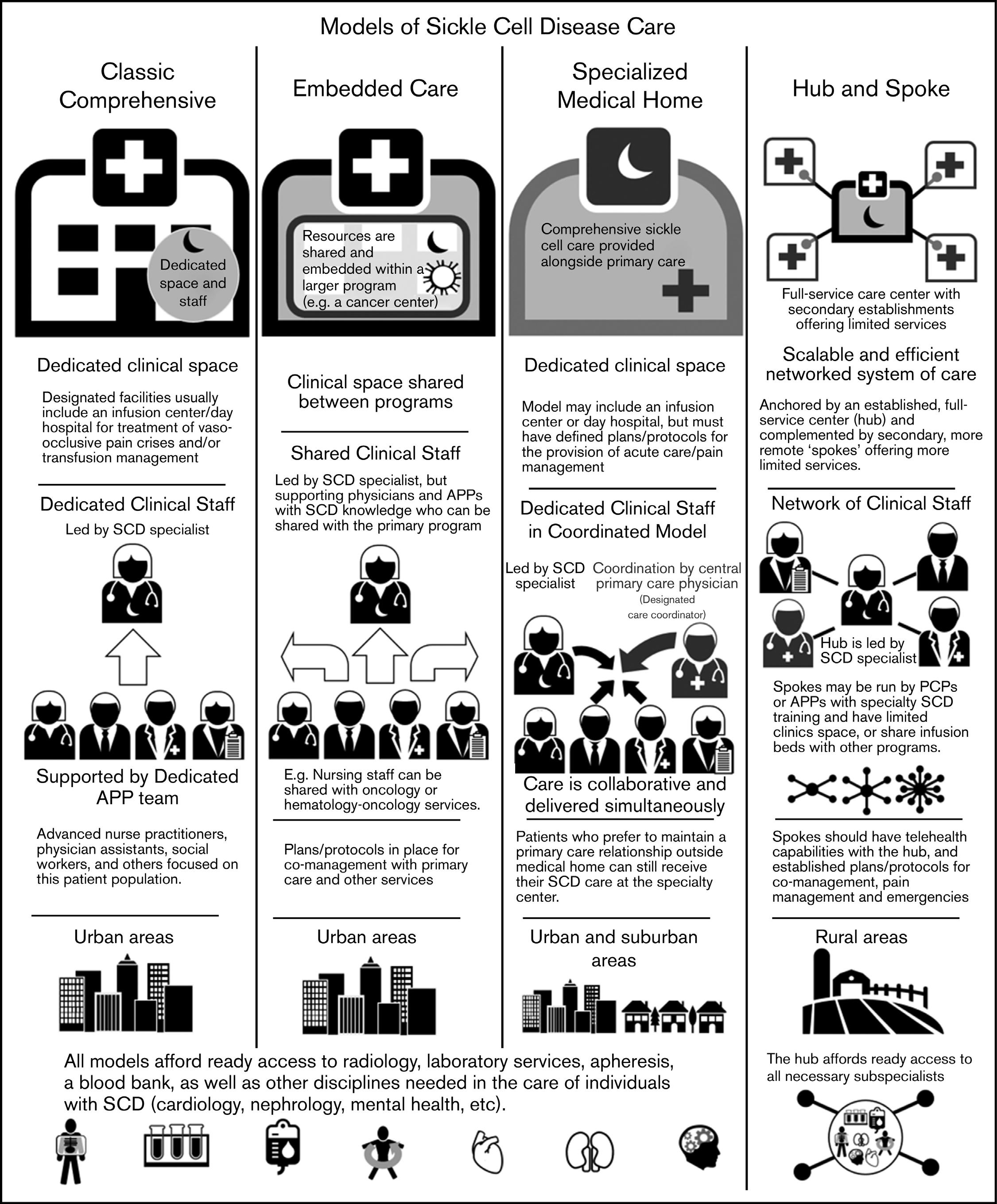
Source: North Carolina Health Professions Data System, Program on Health Workforce Research and Policy, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill. Created February 08, 2022 at https://nchealthworkforce.unc.edu/interactive/
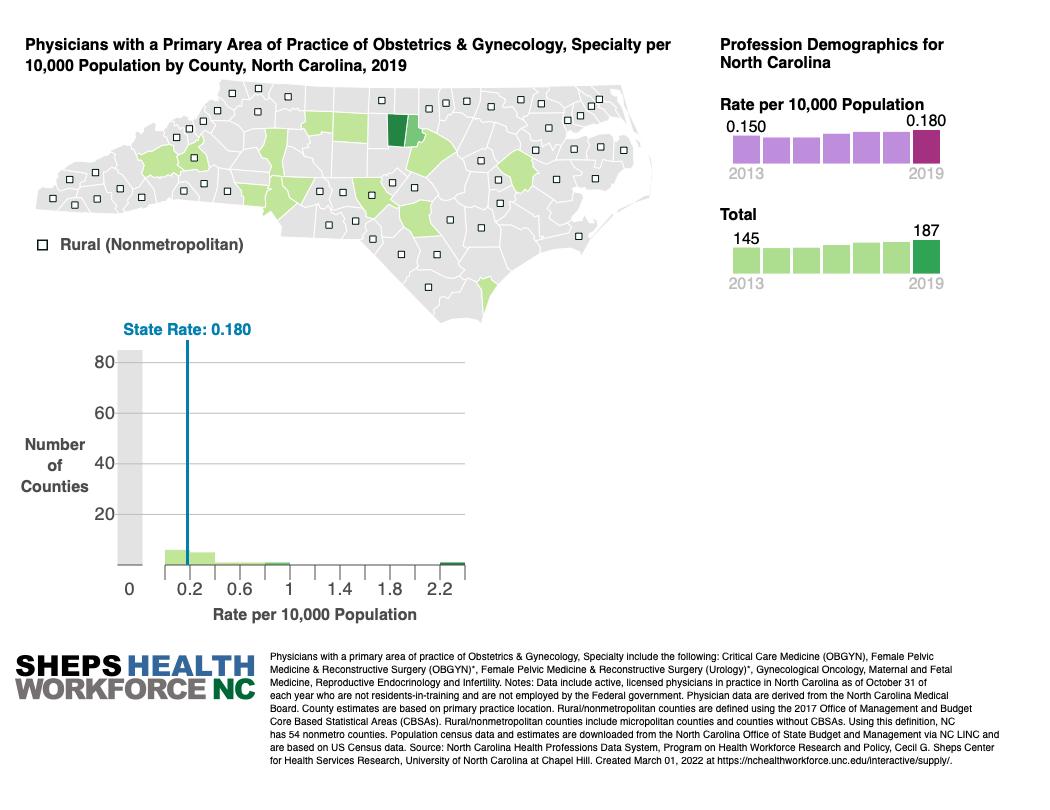
Similarly to SCD patients, pregnant and postpartum North Carolinians have difficulty in accessing care in rural areas. North Carolina, like the U.S. overall, has a concerning shortage of maternal health care providers, particularly providers of color and in rural areas. The national OB-GYN workforce is roughly 6,0008,800 providers short of the necessary levels, according to CMS.94 The shortage of providers of color and providers in rural areas is even more severe. As of 2019, 25 counties in North Carolina, including 16 rural counties, have no OB-GYN providers, and another 12 counties have a single OB-GYN (Figure 9).95 Midwife care is also severely lacking in North Carolina (see Midwife Workforce Section in Part III for more detail).
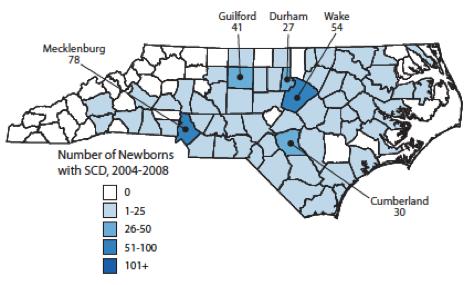
Source: National Center on Birth Defects and Developmental Disabilities, Division of Blood Disorders, “Sickle Cell Disease in North Carolina” (Centers for Disease Control and Prevention).
Source: North Carolina Health Professions Data System, Program on Health Workforce Research and Policy, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill. Created February 08, 2022 at https://nchealthworkforce.unc.edu/interactive/ supply/.
Medicaid enrollees living in rural parts of North Carolina generally have to travel much further for pregnancy-related care than those in urban areas. Maternity care units are often the first department that struggling rural hospitals cut, as they can be a drain on hospital finances. At least ten rural hospitals in North Carolina closed their maternity care units between 2013 and 2020.96 Pregnancy-related care in rural areas is relatively more expensive than in other areas since family physicians and hospitals that deliver babies in low-volume areas typically pay higher malpractice insurance costs and may be charged low-volume penalties.97
In North Carolina, some centers like Mission Hospital in Asheville are already serving as de facto hubs for the surrounding area, since it is a large hospital with the capacity to provide specialist care. However, “hubs” like Mission Hospital would benefit from financial support to cover the costs of coordinating care and ensuring effective communication and records sharing across different hospitals.98
Establishing a North Carolina hub and spoke model of care for SCD will improve access to care and outcomes for people living with SCD. Individuals, especially young adults, with SCD experience optimal care when their care plan is co-managed by a sickle cell specialist and primary care provider.99
Similar to SCD specialists in North Carolina, SCD specialists in South Carolina are often located in urban centers, while many patients and their primary care providers reside in rural regions.100 As a result, South Carolina has implemented a hub and spoke state network called (SC)2 The (SC)2 network utilizes the Lifespan Comprehensive Sickle Cell Clinic at the Medical University of South Carolina (MUSC) as its hub, with spokes throughout the state in Beaufort, Columbia, and Georgetown.101 Lifespan is modeled off of New Mexico’s Project ECHO— originally a hepatitis C hub and spoke care model utilizing telementoring to train more frontline providers in specialty care—and applying it to the state’s SCD care network. Below is
Hub and spoke care models already exist in North Carolina, specifically to improve care for people with substance use disorders. In 2020, experts at Mountain Area Health Education Center (MAHEC) and UNC at Chapel Hill established a partnership to create a regional referral network.105 This hub and spoke model of care is funded by a $1 million, two-year grant, where the “hub” is the clinic with addiction specialists and the “spokes” are primary care providers and community health centers. The goal of this partnership is to address the challenges of sparse and fragmented addiction care across the state and “to create stronger connections between clinics that care for low-income people and experts at MAHEC and [UNC] so patients receive seamless care.”106
Similarly to caring for those with SCD or high-risk pregnancies, caring for patients experiencing addiction typically requires specialty care, yet there is a shortage of doctors who have the training and licensing requirements to prescribe addiction treatment medications. The medical director of Project CARA, a MAHEC program used to help pregnant women with opioid addiction, stated that “what makes the hub and spokes model work is the idea that it is alive and it is a network where the providers that deliver care have to understand and have relationships with each other.”107 Other states have also implemented the hub and spoke model to improve access to opioid treatment, including Vermont, New Hampshire, Washington and California.108
a description of how one “spoke,” Beaufort Memorial Hospital in (SC)2 operates. The SCD clinic at Beaufort Memorial Hospital:
• Is run by a full-time advanced practice provider, for example a nurse practitioner, trained by the hub;
• Provides care Monday through Friday;
• Serves 40 individuals with SCD in the Beaufort region;
• Offers transfusion therapy, hydroxyurea management, and acute pain management with individual care plans;
• Has local, emergency backup through the ED and hospitalist service;
• Provides care under the hub’s supervision, with check-ins as needed for patient-care issues;
• Has a supervising SCD provider from the hub utilize telemedicine to see patients remotely (on a scheduled and as-needed basis); and
• Has a supervising SCD provider travel from the hub to the spokes to provide patient care and assess new patients (on a quarterly basis).102
A hub and spoke model will improve access to care and health outcomes for enrollees living in rural areas of the state, where there are few (if any) maternal health providers. Hub and spoke models can achieve “Perinatal Regionalization of Care,” as recommended by CMS, which ensures that women have access to whichever providers can deliver risk-appropriate care. This approach has worked well in other states. For example, Avera Health in South Dakota has developed a system of connected rural hospitals that collaborate via “labor analysis software that supports providers in identifying risks and potential need for transfer during labor and delivery.”103
MUSC also operates a hub and spoke model by matching local pregnancy care providers with specialists to collaboratively manage care for women with high-risk pregnancies. In this program, women can meet simultaneously with their local provider and the specialist, who is
often located in a different part of the state, using telehealth. Telehealth-based hub and spoke models can work particularly well for providing mental health care, as in programs like “Lifeline4Moms” and Georgia’s “Live Health Online” programs.104
NC DHHS should convene a working group with two subcommittees—one for SCD and one for maternal health—including providers, enrollees, advocates, and PHP representatives to develop and publish best practice standards for rural providers that are interested in establishing or joining a hub and spokes system. NC DHHS should also provide some form of incentive and financial support for providers to cover the costs of creating a hub and spoke system in their region. This includes costs such as establishing sufficient telehealth capacity and managing data from different spoke providers’ medical records systems. This financial support could take several forms, including direct reimbursement from PHPs or a competitive grant program (run either by NC DHHS directly or by PHPs). To facilitate a hub and spoke model operation, NC DHHS should support telementoring directly or provide guidance to PHPs between specialists at hubs and providers at spokes throughout the state for utilizing telementoring. These reforms are relatively long-term solutions.
Implementation:
• NC Medicaid should apply for CMS approval to require or incentivize PHPs to offer ridesharing as a form of NEMT by partnering with companies like Uber or Lyft.
• NC Medicaid should offer competitive grants for PHPs to innovate in the NEMT market to provide expanded transportation options, specifically for rural enrollees where ridesharing-based NEMT is not a viable option.
Implementation:
• NC Medicaid should require PHPs and NEMT brokers to allow enrollees to bring their children, and possibly an adult attendant if needed, to their appointments in all cases.
Effective NEMT is critical for enrollees to access either SCD treatment or pregnancy-related care. In North Carolina, Medicaid covers transportation to appointments using personal vehicles, taxis, vans, mini-buses, mountain area transports, and public transportation. Since the transition to managed care, PHPs have each operated their own NEMT systems by contracting with brokers (including Modivcare and OneCall). PHPs may choose to offer additional transportation services, but they are not required or incentivized to do so. Healthy Blue offers all enrollees a $20 Uber gift
card each year.109 Complete Care provides $75 in annual “healthy rewards gift cards,” which can be used for transportation among other uses.110
Currently, all PHPs guarantee that enrollees who use NEMT will not have to arrive at their appointment more than one hour early and will not have to wait more than one hour after their appointment is done to leave.111 However, there are no limits on the amount of time transportation itself will take, as vehicle may pick up and drop off many other enrollees along the way. All PHPs guarantee enrollees that they will be informed about who is allowed to accompany them on NEMT without cost. PHPs allow caretakers and guardians to accompany enrolled children to their appointments. However, PHPs do not include any guarantee or guidance in their contracts, member handbooks, or other enrollee resources explaining their policy on children accompanying their parent to appointments for their parent’s care.112
In interviews, stakeholders reported that many enrollees do not view the current NEMT system as meeting their needs. In particular, enrollees struggle with the long wait times as their NEMT vehicle makes several stops to pick up other enrollees. Further, they often assume or are informed by the NEMT broker or driver that they cannot bring their children on NEMT if the medical appointment is for the parent’s care. This is particularly a problem for women who are breastfeeding, people with unpredictable and inflexible work schedules, and people who do not have stable child care.
A MACPAC focus group of Medicaid enrollees across the U.S. also found that “late pickups and driver no-shows are the primary reasons for complaints from [enrollees], providers, and care managers.”113 All of these issues can result in enrollees missing scheduled appointments. One of our interviewees noted that if the “no-show” rate becomes a major problem, some providers become reluctant to see Medicaid patients. This can further reduce access to necessary care.
Over 20 percent of state residents live in rural areas and coordinating care for this population can be especially challenging, particularly for individuals with complex health needs like pregnant and postpartum enrollees and enrollees living with SCD.114 Enrollees in rural areas have less access to public transportation, taxis, rideshare services, and other means of transportation than their urban and suburban counterparts. In interviews, stakeholders confirmed that challenges in accessing NEMT are exacerbated in rural areas.
Insufficient NEMT may lead to racial disparities, both in maternal health outcomes and outcomes for people with SCD compared to other enrollees. Black non-Hispanic Medicaid enrollees delay care due to transportation issues much more often than white non-Hispanic enrollees.115
Reimbursing ridesharing services as a form of NEMT is a promising approach that 18 states have incorporated into their Medicaid NEMT systems.116 This includes several large states with substantial rural populations, including Florida, Georgia, Tennessee, and Texas. Transportation Network Companies (TNCs) like Lyft and Uber have experience in the NEMT market since 2016 and 2018, respectively.117 Research on the success of rideshare-based NEMT is somewhat mixed, but several studies have found a positive impact on decreasing driver no-shows and late pickups, increasing customer satisfaction, and decreasing health care costs.118 A Lyft-sponsored study found that a Washington, D.C. program allowing Medicaid enrollees to use ridesharing to travel to prenatal appointments, urgent care, and appointment follow-up care led to a 12 percent drop in ambulance use and a 40 percent drop in emergency department use.119
Rideshare-based NEMT does not need to be scheduled as far in advance as traditional NEMT services, which may improve convenience of use for enrollees. Additionally, Medicaid enrollees do not need a smartphone or the Uber/Lyft apps to use rideshare-based NEMT, as they can access service through a simple text message-based system. This may increase access for people who are low-income and may not be able to afford to maintain a phone data plan.
Ridesharing-based NEMT may improve access to care for urban and suburban enrollees, but it is likely not a viable option for rural residents. NC DHHS could offer competitive grants for PHPs to innovate in the NEMT market to provide expanded transportation options, specifically for rural enrollees.
Several states have experimented with tailoring NEMT to better serve pregnant and postpartum Medicaid enrollees. In 2019, Texas started a pilot program to provide NEMT dedicated only to transporting pregnant and postpartum women and their children to appointments, without sharing the vehicle with other enrollees.120 Georgia allows pregnant and postpartum women to bring their children on NEMT for their mother’s appointments, whereas other enrollees are only allowed to bring an escort that provides medically-necessary assistance to the patient.121
Rideshare-Based NEMT
NC Medicaid should require or incentivize PHPs to offer ridesharing as a form of NEMT by partnering with companies like Uber or Lyft. Alternatively, NC Medicaid could require all PHPs to incorporate some form of ridesharing as a value-added service. Additionally, NC Medicaid should offer competitive grants for PHPs to innovate in the NEMT market and offer expanded transportation options for enrollees. This is a relatively short-term solution which can be implemented by updating PHP contracts.
NC Medicaid should require PHPs to provide NEMT tailored specifically to pregnant and postpartum women. Specifically, NC DHHS should require PHPs and NEMT brokers to allow enrollees to bring their children, and possibly an adult attendant if needed, to their appointments in all cases. This policy should be clearly communicated to enrollees. For an approach even more tailored to pregnant and postpartum women, NC Medicaid could require or incentivize PHPs and their NEMT brokers to provide a dedicated vehicle to transport groups of pregnant and postpartum women directly to their appointments without waiting for other enrollees to complete their appointments. This is a relatively short-term solution which can be implemented by updating PHP contracts.
Implementation:
• NC DHHS should convene a working group to recommend an approach for expanding and improving implicit bias training.
Implicit bias in the health care system is a serious barrier for patients of color receiving the care they need. Although the state already requires PHP staff to undergo equity and implicit bias training, stakeholder interviews revealed that implicit bias training is a critical need for North Carolina.122
The North Carolina Institute of Medicine’s 2020 “Healthy Moms, Healthy Babies” report, which proposed recommendations to reduce infant and maternal mortality and morbidity in the state and address racial disparities, discussed implicit bias as a key factor that contributes to health disparities. Similarly, a needs assessment survey of ED providers in North Carolina on barriers to care for people with SCD revealed that nearly 40 percent of ED providers identified implicit bias as a barrier.123
Research has shown that Black patients have lower levels of trust in the health care system due to experiences with biased providers and historical racist practices.124 Distrust in health care is associated with lower rates of recommended disease prevention and treatment of acute and chronic illness, as well as worse health status.125 It is crucial that providers
NC DHHS should expand and improve its implicit bias training requirements to include perinatal and SCD providers.
understand this context and develop strategies for building trust and communicating across lines of difference.
In SCD care, implicit racial bias leads to negative interactions with providers, longer ED wait times during pain crises, and restricted access to adequate pain management.126 Racial bias also prevents patients with SCD from accessing opioids essential for pain management.127
Providers are more likely to suspect that Black patients and patients with SCD are addicted to opioids and engage in drug-seeking behavior than white patients and patients with non-SCD chronic conditions, even though rates of opioid use among patients with SCD did not rise while opioid use was accelerating in the general population.128 Patients with SCD report that opioid stigma has made providers more likely to underestimate and undertreat their pain.129
Implicit racial bias can lead to negative maternal and child health outcomes for Black women, as they are less likely to receive prenatal education resources.130 Bias can contribute to Black mothers’ risk of serious pregnancyrelated conditions like postpartum hemorrhage and preeclampsia, as their concerns are often overlooked and ignored by health care providers.131
Several states including California, Illinois, Maryland, Michigan, and New Jersey require some form of bias training for health care providers by law.132 California specifically requires hospitals that provide pregnancyrelated care, alternative birth centers, and certain primary care clinics to establish an
“evidence-based implicit bias program” that covers unconscious biases, strategies to communicate across different identities, and maternal health inequities, among other topics.133
It is difficult to estimate the impact of bias training programs because outcomes are hard to quantify.134 However, researchers have developed a series of best practices based on provider feedback. Providers reported that shorter trainings would be most effective, and that modules should be easy to divide into multiple sessions to fit into physicians’ busy schedules. Training courses should be available for free or at a low cost to low-resource hospitals.135 Ideally, Medicaid enrollee advisory boards or patient focus groups should inform the creation of training materials.
NC DHHS should establish a working group to investigate best practices to improve implicit bias training. The working group could consider recommending or requiring provider participation in the Carolina Global Breastfeeding Institute’s ENRICH program, which offers maternal healthfocused provider bias training, or the perinatal provider-focused, evidence-based training model developed by Diversity Science.136
Although SCD-focused bias training has yet to be implemented, NC DHHS can look to states like Michigan, which requires bias training for health care providers writ large for initial licensure or registration and renewal under the Michigan Public Health Code, for examples of bias training content and implementation strategy.137
These are relatively medium-term reforms. because NC DHHS already requires PHP staff to engage in some degree of bias training. The best practices the working group formulates for providers can be implemented quickly.
NC DHSS should increase resources in NCCARE360 and CBOs to ensure their ability to address non-medical drivers of health.
Implementation:
• NC DHHS should increase advertising and communication to community-based organizations on NCCARE360.
• NC DHHS should invest in technical assistance and resources to communitybased organizations to incorporate NCCARE360 into their practice.
• NC DHHS should set a community reinvestment requirement for PHPs.
Many North Carolinians face conditions including food insecurity, housing instability, unmet transportation needs, and interpersonal violence, all of which impact their health and well-being. More specifically, over 1.2 million North Carolinians cannot find affordable housing; the state has the eighth highest rate of food insecurity; 47 percent of North Carolina women experience intimate partner violence; and nearly a quarter of North Carolina children have experienced adverse childhood experiences.138 Screening and identifying these unmet needs provide opportunities for intervention, to improve health outcomes and to generate cost savings.
NC Medicaid is a leader in the country in its effort to integrate non-medical drivers of health into models of care. The state has taken several initiatives to address non-medical drivers, including creating a set of nine standard screening questions for providers to determine if Medicaid enrollees face barriers related to transportation, food, housing, or interpersonal safety and developing Healthy Opportunities
to improve screening for social needs, care coordination, and the provision of non-medical services to its Medicaid population.139
Furthermore, the state has created a statewide platform called NCCARE360, where providers can refer and connect patients to community-based organizations (CBOs). The coordinated care network was launched in 2019 and now boasts over 1,000 CBOs that connect people to resources they need in all 100 counties.140 However, one challenge has been a lack of widespread use of NCCARE360 by health care providers and community-based organizations.141 Stakeholder interviews indicated a need for greater awareness of NCCARE360 across provider networks as well as greater organizational capacity to implement it. CBOs cited a lack sufficient staff and technical training to implement NCCARE360 at a larger scale.
The effectiveness of these programs to connect people to local services depends heavily on CBOs’ resources and ability address people’s needs. The COVID-19 pandemic has impacted nonprofits in the state; 87 percent of nonprofits report lower than usual revenue and 77 percent report higher demand than usual for services.142
Non-medical drivers of health are particularly important for people with SCD, who are more likely to experience structural barriers and racial disparities that exacerbate the physical and behavioral health challenges associated with SCD and result in worse health outcomes.143 A study examining universal screening for social determinants in patients with SCD in a pediatric hematology clinic at the Boston Medical Center found that 66 percent of patients screened positive for at least one unmet socioeconomic need with an average of 2.1 unmet needs per patient (among patients with unmet needs). The most common unmet need was food insecurity, followed by difficulty paying utilities, a desire for more education, unemployment, transportation, housing, and childcare.144 The same study found that patients were proactive after being referred
to community organizations, with 45 percent reaching out to resources within two weeks, demonstrating the benefits of a screening and referral program for people with SCD.
Similarly, for pregnant and postpartum women with Medicaid, non-medical drivers of health can affect health outcomes. A study found that attending fewer than 10 prenatal appointments and having preexisting conditions, such as obesity or diabetes, were significantly associated with maternal mortality.145 Non-medical factors, such as lack of transportation or lack of healthy foods, inhibit access to prenatal care and contribute to adverse risk factors such as obesity and diabetes. Screenings and referrals have shown promise in improving health outcomes for pregnant and postpartum women. For example, women referred to and participating in the Supplemental Nutrition Assistance Program (SNAP) benefits have a reduced likelihood of pregnancy-related ED and lower rates of preterm births.146 Additionally, screening for domestic violence among pregnant women increased identification of and interventions for domestic violence.147
In the short-term, NC DHHS should increase funding to increase resources and technical assistance to CBOs to adequately implement NCCARE360. Additionally, there is still a lack of wide-spread awareness of NCCARE360, which inhibits its uptake. Potential avenues to increase engagement include web conferences, print material in newspapers and flyers, and social media posts.
In the medium-term, NC DHHS can increase the capacity of CBOs to address non-medical needs through community reinvestment requirements, which require PHPs to spend a portion of profits or reserves on local communities. Currently, NC DHHS requires PHPs to engage with community organizations and incentivizes (but not mandates) PHPs to invest in communities; PHPs can include voluntary contributions to “health-related resources and initiatives that advance public health and Health Equity” towards their medical loss ratio, including
“support for community-based organizations that provide meals, transportation or other essential services.”148 NC DHHS should set a community reinvestment requirement for PHPs, which can be modeled after Arizona’s MCO contracts. Arizona mandates its MCOs to re-invest six percent of their profits towards community reinvestment.149 PHPs have leeway to determine where to invest, which can include investing in CBOs or generally tackling non-medical drivers of health.150
Implementation:
• NC DHHS should create an online data dashboard that includes maternal and SCD morbidity and mortality, disaggregated by specific demographics.
CMS requires state Medicaid agencies to submit enrollment, service utilization, payment, provider, and other information from claims data every month, through a standardized data format. The required data include the number of pregnant enrollees and average cost of pregnancy benefits. However, there is no federal requirement for state Medicaid agencies to collect data regarding the number of enrollees with SCD, or mortality and morbidity statistics specific to SCD and maternal populations.
Data collection is more rigorous at the state level, especially in North Carolina where DHHS has made their commitment to reducing data gaps as a key goal. We applaud NC DHHS’ plan to collect data on maternal and SCD morbidity and mortality, disaggregated by specific demographics. NC Medicaid last publicly reported data from the Health Effectiveness Data and Information Set (HEDIS) in 2016. This data includes frequency of prenatal care and timeliness of prenatal and postpartum care.151 The NC DHHS website has no publicly available data on the prevalence, mortality, or comorbidities rates of SCD or maternal populations. However, NC DHHS received a surveillance data grant from the Centers for Disease Control and Prevention in FY2021 to support these data collection efforts.152
While there is some uncertainty in implementation as NC Medicaid transitions from fee-for-service to managed care, NC DHHS released a detailed plan for data collection (although there is no detailed plan for publicizing data post-managed care transition) and PHPs will be expected to use data to promote health equity. NC DHHS also plans on requiring each PHP to submit stratified enrollment data, such as age, race, ethnicity, gender, primary language, long-term services and supports needs status, disability status, and geography (rural/urban and service region). Per a NC Medicaid employee, NC DHHS has data on SCD prevalence for all children with Medicaid disaggregated by gender, age group, race, ethnicity, rural/urban indicatory, primary language, foster care status, and disability, but the dataset is not public.
Data gathering is the first step in making informed policy decisions for remedying health inequities. Without Medicaid-specific data stratified by demographic groups, NC DHHS cannot be confident that PHPs are providing equitable care nor can NC DHHS adequately address barriers to quality health care.153
All data collected should be made publicly available, except in cases of privacy issues due to small sample sizes. Timely, accurate, and accessible data allow Medicaid enrollees, providers, advocates, and researchers to adequately understand where NC DHHS should focus. This recommendation has challenges internal to NC DHHS, such as limited staffing capability to create consumer-friendly material that people--who might have English as a second language or access to the internet only on mobile devices--can easily intuit.
We recommend that NC DHHS take the next step beyond collecting data and commit to publicizing and updating these statistics every month on a multilingual and userfriendly dashboard. Publicizing data will hold PHPs accountable to the public, including Medicaid enrollees, providers, advocates, and policymakers. The public dataset should be able to be disaggregated by more than one
demographic (e.g., by race and geography). Sharing disaggregated data in an accessible format will help fulfill the promise of managed care by building trust with communities across the state and informing stakeholders as to the progress of PHPs to date. NC DHHS should also keep historical data available online to allow the public and agencies to track health outcomes over time. This dataset would be in addition to the health equity report the North Carolina External Quality Review Organization (EQRO) will develop.154 We recommend EQRO publish this health equity report in a timely manner, disaggregated by relevant demographic groups—age, race, ethnicity, gender, primary language, long-term services and supports needs status, disability status, and geography— listed earlier, and by plan to serve as scorecard for each plan.

NC DHHS should consult Georgetown University Health Policy Institute’s tracker of state Medicaid dashboards focused on children’s health.155 Two states in particular—Texas and Washington—stand out as being user-friendly and comprehensive.156 This is a medium-term investment. PHPs are already collecting this data via provider claims reports; thus, NC DHHS will not need to amend the PHP contracts. NC DHHS will need to change their internal processes. The biggest lift for NC DHHS will be dedicating personnel to creating a new, public database and infographics.
Drawing upon the SCD empirical literature and the expertise present within North Carolina’s academic, clinical, and advocacy settings, we present recommendations to NC DHHS for Medicaid care and payment models for SCD. We expect that improvements in care management, access to comprehensive care, the pediatric to adult transition, clinical care models, strategic contracts with Prepaid Health Plans (PHPs), innovative payment models, and coordination with other NC DHHS programs will improve health outcomes and reduce health care costs for people with SCD, a patient population which has long been stigmatized and marginalized by the health care system and greater society due to its classification as a “Black disease.”157
NC Medicaid should encourage support during the transition of pediatric patients with SCD into adult care.
Implementation:
• NC Medicaid should require PHPs to provide support services to transition pediatric patients with SCD into adult care.
• NC Medicaid should reimburse providers for transition activities.
Mortality, morbidity, acute care utilization and hospitalization all increase at alarming rates for young adults with SCD just after transitioning out of pediatric care and more than 95 percent of individuals with SCD survive into adulthood and the mortality rate for children with SCD has dropped about three percent per year from 1979-2005.158 Despite this progress in pediatric care, the adult mortality rate rose about one percent per year from 1979-2005.159 Adults aged 25 to 34 have the highest mortality rates among all patients with SCD, in part because of relatively higher ED utilization and rehospitalization rates and less preventive health care.160
The decrease in health outcomes immediately after transitioning to adult SCD care—usually around ages 18 to 25—are attributed to inadequate adult care and poor preparation for the transition. Many providers are not prepared for the increased complexity of adult SCD complications.161 Further, pediatric and adult providers often do not communicate about transitioning patients. Recently-transitioned patients also report receiving little preparation for transition.162 Poor relationships with adult providers can isolate young adults, leading to
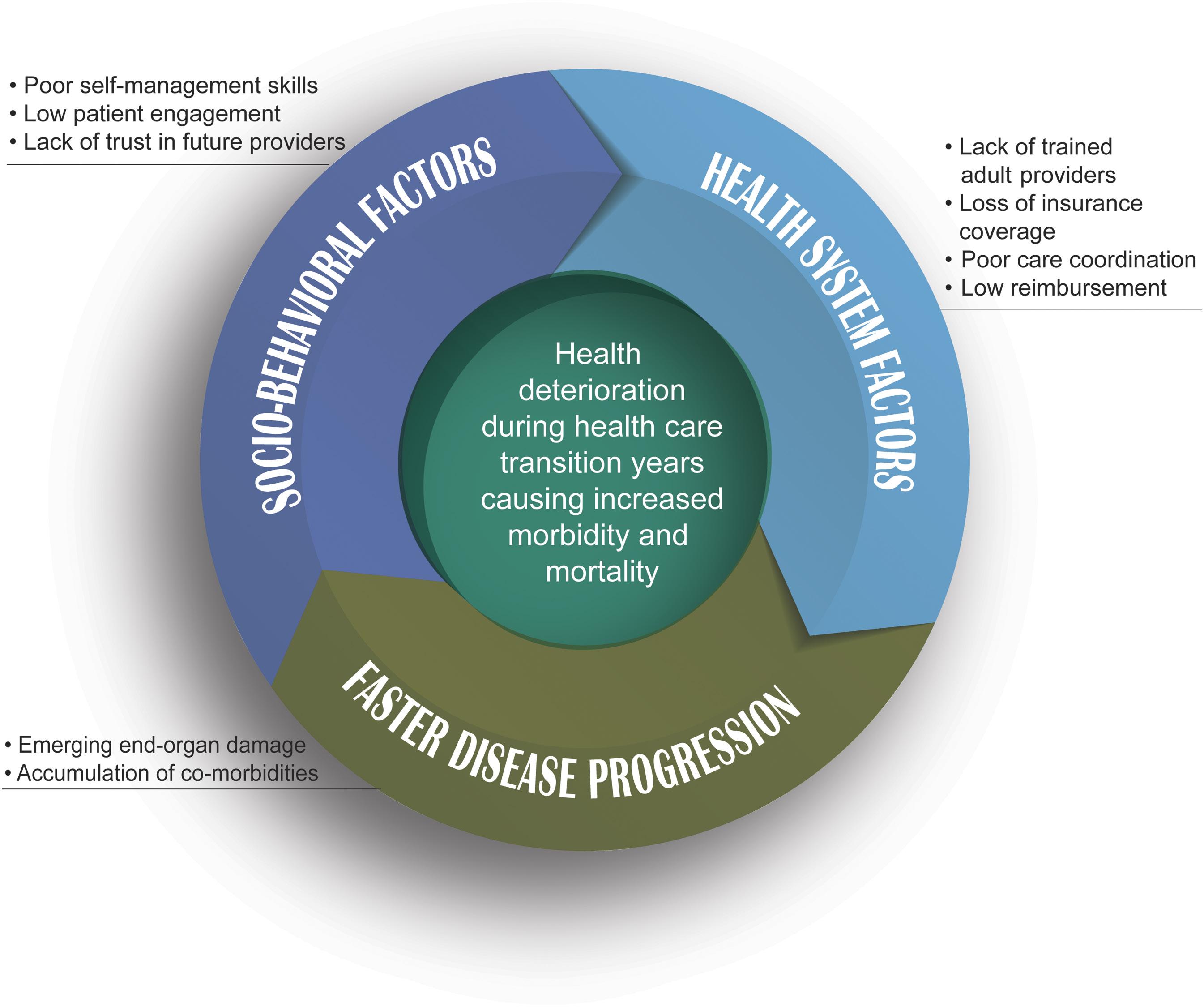
costly ED care and poor health outcomes.163 Recently-transitioned adults report poor experiences in adult care, including long ED wait times as well as provider mistrust about their disease and pain severity.164 Finally, insurance coverage is a barrier as well, as young adults are often transitioning into adult care at the same time they become ineligible for Medicaid.165 Figure 10 depicts the health deterioration detailed in this paragraph.
The transition from pediatric to adult care for patients with SCD is not standardized in North Carolina. According to North Carolina stakeholders, SCD providers across the state employ a variety of practices. NC Medicaid should consider implementing evidence-based approaches to care transition. The transition to adult care often requires support from age 18 to 25, whereas Medicaid eligibility ends at age 21 in North Carolina.166
St. Jude Children’s Research Hospital developed a transition program consistent with the APHON/ ASPHO policy for patients aged 12 to 25. The following summarizes the program’s key transition activities:
• Provider activities. Providers track patient knowledge, transition readiness, adult provider information, and transition outcomes. A transition nurse case manager coordinates care between pediatric and adult providers from ages 17 to 25. Documentation of care plans and medical summaries can either be in writing or via a mobile application and shared with the new adult provider.174
• Patient education initiatives. Interactive learning is incorporated into visits using lessons with the nurse case manager and supplemental tools like the Sickle Cell Transition E-Learning Platform, which consists of modules 10-15 minutes in length.175 Patients learn about disease management, communicating care needs to new providers, insurance, self-advocacy, academic planning, and finding support.176 Just before transitioning, patients receive a written medical summary, information about SCD community-based organizations, and information about their first adult appointment.
• Age of program eligibility. The pediatric transition team continues to see the patient until age 26. Current evidence strongly suggests that continued support will improve outcomes for adults with SCD.177
The St. Jude program and a similar program developed at Virginia Commonwealth University, the Transition Intervention Program (VCU-TIP), both saw significant declines in care abandonment.178
At St. Jude, the median latency period between pediatric and adult care dropped from 64 months to one month, and acute care utilization did not rise during the transition years.179 VCU-TIP had 100 percent of patients complete an initial adult visit and 78 percent continue to receive regular adult care, whereas just 50 percent completed an initial visit prior to program implementation.180
Outcome measures for transition programs include acute care utilization, adherence to longitudinal care, and quality of life.181
The Association of Pediatric Hematology/ Oncology Nurses (APHON) and the American Society of Pediatric Hematology Oncology (ASPHO) issued a SCD transition policy recommendation in 2015. They recommend the following: early discussion of transition (by age 12); collaboration among patients, families, and providers to create the transition plan; annual transition readiness assessment; and communication between pediatric and adult providers during transfer of care.167 The American Society of Hematology (ASH) has also developed a transition toolkit to support providers with the transition process.168
Peer mentoring, pairing pediatric patients with recently transitioned young adults, and engaging with community health workers (CHWs) also show promise as components of transition programs.169 Indeed, as discussed above, North Carolina already has a network of CHWs with local relationships it can leverage, and CHWs have been recommended at the national level to coordinate SCD care.170
NC Medicaid should consider requiring PHPs to develop transition care that address one of the four APHON/ASPHO best practices at a time. This would allow for improved care in the shorter term, rather than requiring PHPs to develop a comprehensive transition plan that addresses all best practices at once. Transition services should cover Medicaid enrollees with SCD up to age 21 and, to the extent possible, include work to ensure that patients can seamlessly transition into new insurance plans that cover the desired adult provider. Coordination with the North Carolina Division of Public Health (DPH) Sickle Cell Syndrome Program would help ensure that individuals aging out of Medicaid can continue receiving appropriate care.171
This is a medium-term investment, because PHPs need time to develop transition programs for both urban and rural care. For urban areas, PHPs can emulate the St. Jude and VCU-TIP models. For rural areas, comprehensive sickle cell centers and pediatric providers can provide telementoring services for local adult providers. Telementoring allows pediatric providers to inform adult providers about new patients, address preconceptions, and build mutual trust to facilitate communication about how to best serve patients.172 Hub and spoke models, as detailed in Part I, benefit young adults in particular and therefore would be ideal to facilitate well-coordinated transitions into adult care in rural North Carolina.
NC Medicaid should also consider reimbursement for transition coordination activities and require coordination specifically for SCD care.173 Adjustment of PHP contracts to cover coordination is a short-term investment because it can be done unilaterally by NC Medicaid.
NC Medicaid should invest in the development of a network of primary care providers (PCPs) knowledgeable about the treatment of SCD and should implement additional financial incentives for care coordination between PCPs and SCD experts.
Implementation:
• NC Medicaid should identify PCPs already providing care to several patients with SCD.
• NC Medicaid, the PHPs, and the state’s sickle cell centers should invest in these PCPs’ knowledge of SCD through means such as telementoring.
• NC Medicaid should encourage PHPs should make their members with SCD aware of these PCPs.
• NC Medicaid should convene a working group to explore additional financial incentives NC Medicaid can implement to encourage primary and specialty care coordination for individuals with SCD.
Every individual living with sickle cell disease should see both an SCD specialist and a primary care provider. However, the need to see multiple providers can burden individuals with SCD, and this burden can be made heavier if the PCP is uncomfortable providing basic care to someone with SCD or if there is poor coordination among the PCP and SCD specialist. According to one provider interviewed, because of PCPs’ lack of knowledge and the burden of visiting multiple providers, individuals living with SCD often rely on their SCD specialist to fill the role of a PCP. Hematologists, however, are not equipped to fill this role.
Several North Carolina SCD specialists expressed that most PCPs are uncomfortable with caring for patients with SCD. Independently, these providers gave the example of their patient’s PCP calling them for assistance when the patient visited the PCP with a fever. While NC Medicaid reimburses care management, stakeholder interviews suggest that current efforts are insufficient. A provider at UNC’s Sickle Cell Program stated that Medicaid does not reimburse PCPs for coordinating with their patients’ SCD specialists. Additionally, a 2016 and 2017study of individuals with SCD enrolled in Medicaid in North Carolina during a 1-year period found that only 34 percent of patients were co-managed by their PCP and hematologist.182 A survey of PCPs seeing at least five Medicaid patients with SCD in North Carolina found that only one-third of respondents had even occasional contact with a SCD specialist, and 37 percent of respondents said that they never communicated with an SCD specialist.183
The Sickle Cell Disease Treatment Demonstration Program, administered by the Health Resources and Services Administration (HRSA), provides funding to four regional teams, which include sickle cell centers, federally qualified health centers, and community-based organizations. One of the three goals of this program is to improve provider knowledge of SCD and to connect patients with knowledgeable providers.184
NC Medicaid can use the recently awarded Sickle Cell Data Collection (SCDC) program funding from the Centers for Disease Control and Prevention to support this recommendation.185 Sickle Cell Disease Foundation of California, a community-based foundation is using data from the SCDC program to provide disease-specific education to PCPs already seeing patients with SCD and to direct new patients with SCD to these providers.186 NC Medicaid should leverage this program to identify PCPs already caring for patients with SCD. This recommendation can likely be implemented in the medium-term because the funding is already secured however planning and implementation will take a few years.
Implementation:
• NC DHHS should support legislation to increase funding for “Sickle Cell Adult Treatment” (fund code 1421) and “Sickle Cell Support – Children” (fund code 14A0), which fund the NC Sickle Cell Syndrome Program, in the state budget.
The NC Sickle Cell Syndrome Program provides genetic counseling, education, medical services, reimbursement for treatment, screening, and care coordination.187 It includes nine regional Educator Counselors, one Community-based organization, the Piedmont Health Services and Sickle Cell Agency, six comprehensive sickle cell medical centers, and state program staff.188
The NC Sickle Cell Syndrome Program offers a DPH-Sickle Cell Benefit Plan for individuals aged 19 and over with SCD at or below 100 percent of the Federal Poverty Level. This program employs a fee-for-service payment model and reimburses services at the same rate as Medicaid. Individuals who do not qualify for Medicaid or Medicare, have reached these programs’ payment limits, or do not have insurance can rely on DPH’s plan as a safety net. This plan covers outpatient visits, ED visits, hospitalization, medications, dental visits, and vision visits, with limits for many of these services. Prior authorization is required for any reimbursement under this plan. In a stakeholder interview, a representative from the DPH Sickle Cell Program stated that the plan currently has around 150 enrollees. This representative also explained that individuals transitioning from Medicaid to DPH’s Benefit Plan usually continue seeing their same
PCP and hematologist. Thus, the Benefit Plan helps to mitigate the care disruptions that usually result from Medicaid churn.
DPH’s Sickle Cell Educator Counselors are each responsible for a different region of the state.189 They provide counseling care management support to individuals with SCD throughout their life, as well education and advocacy on SCD to providers and the general public. The Educator Counselors work with all individuals with SCD in North Carolina, regardless of their income status or insurance coverage.
The DPH-Sickle Cell Benefit Plan can provide coverage for individuals living with SCD who churn in and out of Medicaid, especially for adults. Thus, the plan can be leveraged to mitigate some of the problems associated with Medicaid churn. One study found that compared to individuals with consistent Medicaid coverage, individuals with multiple transitions into and out of Medicaid had 10 percent to 36 percent more ED visits, outpatient visits, and hospitalizations, and 19 percent lower usage of prescription medications on average.190
By covering medications, the DPH-Sickle Cell Benefit Plan may allow its patients greater access to prescription medications than the average individual who transitions into and out of Medicaid can obtain. Regular use of medication may, in turn, lower the outsized rates of ED visits and hospitalizations for the churn population. Thus, DPH’s plan likely protects the health of individuals living with SCD during periods when they are ineligible for Medicaid coverage.
In addition to protecting the health of individuals transitioning in and out of Medicaid, the DPHSickle Cell Benefit Plan likely also provides cost-savings to Medicaid itself. One study of Medicaid churn in the population with diabetes found program expenditures increased $239 (in 2008 U.S. dollars) per member per month, on average, for the first three months after a lapse in coverage. These increased program costs were likely driven by heightened ED use and inpatient
stays.191 By providing coverage when Medicaid is unavailable, DPH’s plan likely prevents some of the need for ED and inpatient care when a member is re-enrolled in Medicaid, thereby lowering program costs.
While the Families First Coronavirus Response Act has largely put a pause on Medicaid churning during the national public health emergency, the issues presented by churn will reappear with the end of the emergency. North Carolina should be forward-thinking in how to improve patient health and reduce costs from lapses in Medicaid coverage. Expansion of the DPH-Sickle Cell Benefit Plan, and the NC Sickle Cell Syndrome Program more broadly, is a viable option.
The NC General Assembly provided a net appropriations amount of $1.6 million to the NC Sickle Cell Syndrome Program in FY2022, with $553,000 in net appropriations to “Sickle Cell Adult Treatment” (fund code 1421) and $1 million in net appropriations to “Sickle Cell Support – Children” (fund code 14A0).192 The NC General Assembly has not increased the program’s budget since the 1980s (except for modest salary increases), limiting its ability to cover treatments and services, especially new and more expensive SCD therapies. With additional funding, the program can cover more medications and increase staffing so Educator Counselors have more capacity to follow-up on individual cases. Educator counselors’ expertise on SCD care makes them unique from CHWs and care managers who do not focus on the disease, and equips them to handle issues specific to the disease (including pain management barriers in EDs and skipped school or work days due to pain episodes).
NC Medicaid should cover physician and hospital outpatient telehealth services at parity for people with complex care needs, including the Medicaid population that experiences SCD.
Implementation:
• NC Medicaid should cover physician telehealth services at parity for the population that experiences SCD.
• NC Medicaid should consider covering hospital outpatient services facilitated by telehealth for the population that experiences SCD, potentially through a hub and spoke model.
Getting to medical appointments is a consistent challenge for people living with SCD and their caregivers. This can result in a high incidence of “no-show” appointments for SCD care as well as administrative and financial challenges for providers. While not all SCD appointments are well-suited for telehealth treatment, routine check-ups and behavioral and psychological appointments can be delivered effectively via telehealth. Additionally, patients living with SCD generally experience greater challenges in experiencing continuity of care between primary care providers, specialists, and emergency health facilities than those who do not have SCD. Increased use of telehealth could fill in treatment gaps and thereby significantly improve continuity of care for people living with SCD.
As a result of the COVID-19 pandemic, all 50 states and Washington, D.C. were given broad flexibility to determine whether and how to cover expanded telehealth services in their Medicaid programs. The Coronavirus Aid, Relief, and Economic Security (CARES) Act appropriated $29 million annually for five years to the Telehealth Network Grant Program to fund telehealth services specifically in rural and medically underserved areas.193 At the outset of the health emergency, NC Medicaid modified its Telemedicine and Telepsychiatry Clinical Coverage Policy to expand telehealth services and notably include payment parity to providers for telehealth services, which can be particularly important for serving rural populations.194 NC Medicaid has continued to expand telehealth to cover many services, including pediatric services and some reproductive and maternal health services and has even made some expansions permanent.195 NC DHHS published a North Carolina Telehealth Playbook, which includes comprehensive information about telehealth provider and consumer resources, how NC Medicaid interacts with telehealth services, and more.196
In interviews, North Carolina stakeholders noted that their utilization of telehealth in treating enrollees with SCD increased substantially as a result of the pandemic and NC Medicaid policy changes. Stakeholders reported that individuals living with and/or caring for loved ones with SCD had positive experiences using telehealth during the pandemic, expressing that telehealth services were convenient and saved travel time to get to appointments. This is especially important since many enrollees in North Carolina live in rural areas.
North Carolina stakeholders also reported that telehealth can be an effective system for delivering some health services for people living with SCD, such as having consultations to adjust pain medications or check in on the effectiveness of treatments. However, they reported that for many critical functions of SCD care, which often involve monitoring vital health metrics and running lab studies, telehealth
cannot replace in-person care. They suggested that a model in which patients access lab services at a location more convenient for them and then review the results using telehealth could be an effective solution. Consequently, this recommendation can be appropriately deployed with the recommendation for hub and spoke models of care outlined in Part 1.
The Community Preventative Services Task Force (CPSTF) recommends several telehealth interventions for patients who suffer from chronic diseases such as cardiovascular disease, diabetes, end-stage renal disease, and obesity.197 The CPSTF found that such interventions can improve medication adherence, clinical outcomes, and dietary outcomes for affected patients. Since SCD is a chronic disease like those aforementioned, patients with SCD could likely benefit from telehealth interventions.
North Carolina stakeholders noted that telehealth is particularly promising in the area of behavioral and psychological services for people living with SCD. People living with SCD face an array of mental and behavioral health challenges associated with their SCD that could be treated effectively using telehealth.
While telehealth can be an effective health care delivery system, those without reliable broadband cannot access telehealth services equitably. It is estimated that over 1.1 million households in North Carolina lack high-speed internet access, and these households tend to be concentrated in rural areas, where accessing health care services is already a challenge.198 The Build Back Better infrastructure bill includes approximately $1 billion to improve broadband affordability and accessibility.199 NC Medicaid should ensure that it has a seat at the table in decisions as to how broadband funding will be distributed throughout the state, recognizing that unequal access to broadband will limit its ability to provide telehealth services to enrollees.
Other states have found success in expanding telehealth services specifically for their SCD patients. During the COVID-19 pandemic, Boston Medical Center used video and phone communications to assess the needs of people with SCD and prevent lapses in care.217 Patients’ responses to the use of these remote communications were overwhelmingly positive and no-show rates dropped significantly.
The Medical College of Georgia (MCG) Sickle Cell Center established three telemedicine clinic sites in rural areas throughout the state of Georgia to meet the clinical needs of patients with SCD and reduce no-show appointments.218 This resulted in an increase from 1,143 to 1,889 encounters per year, including an increase from 271 to 745 rural encounters, with the addition of just one physician assistant.
The University of Alabama at Birmingham School of Medicine conducted a retroactive review of hydroxyurea laboratory and clinical outcomes and found that establishing satellite sites and implementing telehealth was just as effective in treating SCD patients with hydroxyurea as traditional in-person treatment.219
In the short term, requiring PHPs to cover telehealth services would set a floor for behavioral and psychological health services covered by Medicaid throughout the state. In the medium- to long-term, NC Medicaid should consider supporting telehealth clinic sites in rural areas, potentially through a hub and spoke model—as outlined in Part I—and reimbursing hospital outpatient and physician services at parity.
NC DHHS should bolster established SCD day hospitals in North Carolina.
Implementation:
• NC DHHS should support legislation approving increased funding through state grants for established SCD day hospitals in North Carolina.
Vaso-occlusive crises (VOCs)—the most common cause of acute morbidity in SCD— lead to episodes of intense pain and are the defining feature of SCD.200 These pain crises are unpredictable, start suddenly, and are poorly treated, leading to much of the current care for VOCs to occur through emergency department (ED) visits and hospitalizations.201
Entering the ED is often a last resort for patients.202 Patients report, “feeling intense anxiety and stress about going to the hospital, sometimes delaying or avoiding seeking necessary care.”203 When experiencing VOCs, individuals with SCD are left with limited options. They often end up an ED—the last place they want to be—where they are “too often…treated with stereotypical idealism and inherent bias that ultimately leads to them avoiding going for help or simply not receiving it in their greatest time of need.”204
Individuals with SCD repeatedly report suboptimal care in EDs.205 Non-SCD specialist providers often hold the misperception that SCD is simply a pain condition, an oversimplification that can lead to inappropriate care (e.g., lacking treatment with fluids, oxygen, and other medicines). Too often ED providers have negative attitudes and perceptions of SCD patients. ED providers frequently label individuals with SCD as “drug seeking” or “Sickler,” a derogatory term steeped in the historic and racist disregard for the SCD
patient.206 In one study, the use of the term “Sickler” amongst ED providers was significantly associated with negative attitudes toward people with SCD.207 Patients with SCD are forced to experience “inadequate disrespectful and even humiliating treatment” which, unfortunately, also leads to longer wait times than people with other pain issues and delays in analgesic administration.208
As an alternative to EDs—when funding is available—SCD providers operate and run SCD day hospitals (DHs). DHs offer several benefits beyond the capacity of EDs for treatment of uncomplicated VOCs, including improved patient-centered care, improved pain relief, and reduced hospital admissions.209 DHs are staffed with providers familiar with SCD and its treatment, such as Advanced Practice Providers under the supervision of a SCD physician. Patients experiencing uncomplicated VOCs can enter this facility, a stable setting for their comprehensive management, instead of going to an ED. Often, DHs are operated in conjunction with comprehensive SCD care facilities.
Currently, three SCD DHs operate within North Carolina at ECU, Duke University Medical Center, and Wake Forest School of Medicine.210 Duke’s DH operates Monday through Friday, 8 AM to 9 PM and Saturday, 8 AM to 4 PM. ECU’s DH operates Monday through Friday, 9 AM to 5 PM. At ECU’s DH, a major challenge is limited funding for necessary staff and appropriate hours of operation. Currently, the ECU DH has two nurses at only 80 percent full-time equivalent plus vacations. Part of the DH program is funded through the state, which initiated funding in 1998 by including it in the state budget. However, state funds dedicated to this DH has not increased, resulting in the need to search for additional funding elsewhere.
SCD specialists from the ECU DH explained that the use of SCD DHs can dramatically reduce hospital admissions for adult patients. Further, the literature finds that treating uncomplicated VOCs in DHs consistently reduces rates of hospital admissions compared to the ED.211 DHs are able to assess uncomplicated VOCs and begin analgesics to treat pain more rapidly than EDs.212 Patient satisfaction is higher in day hospitals than in EDs, with patients sometimes opting to manage pain at home while waiting for DHs to open in an effort to avoid the ED.213
SCD specialists at NC sickle cell centers at Duke, UNC and ECU all emphasized that individuals with SCD only choose to go to the ED when they are absolutely out of all other options, which is consistent with the literature.214 DHs are able to provide a supportive environment with improved patient care. The improvements in outcomes and care show a potential for overall savings for both payers and providers.215 For example, providers from the ECU DH explained that often when patients go to the ED because their DH is closed, they receive unnecessary and costly scans such as computerized tomography (CT). Institutional cost savings are attributable to use of DHs and reduced hospitalizations.216
Sickle cell DHs reduce ED use, subsequent admissions, and overall costs. North Carolina has several operational DHs already, which makes the implementation of this recommendation a feasible short-term task. NC DHHS should encourage the NC General Assembly to take advantage of the infrastructure already in place within the state’s current DHs and dedicate additional funds and resources to expand the hours of operation during the week and weekend at these sites.
The Montefiore Medical Center established a DH in the Bronx Comprehensive Sickle Cell Center as a demonstration project between 1989 and 1993. Following its establishment, a five-year study showed a 40 percent reduction in the hospital admission rate for patients with VOCs. Admission rates were five times less frequent from the DH (8.3 percent) compared to the ED (42.7 percent) for uncomplicated VOCs. Further, the length of stay for patients seen in the DH decreased by 1.5 days compared to patients seen elsewhere.220 Similarly, a DH in Texas reduced hospital admission rates by 43 percent.221
The University of Illinois at Chicago Comprehensive Sickle Cell Center’s DH expanded its operations and saw positive benefits for patients and the health system. In 2014, the DH expanded hours of operation from 8 AM to 5 PM Monday through Friday to 8 AM to 11 PM Monday through Friday. This increased utilization by SCD by almost five-fold while decreasing hospital admission rates and decreasing lengths of stay for inpatient admissions.222 Expanding hours of operation provided SCD patients experiencing VOCs an alternative care option that allowed them to avoid the ED. This expansion improved outcomes and may represent significant cost savings to the health system.
Expansion of DH hours provides people with SCD the opportunity to experience improved care and outcomes. The ECU team explained that, with limited hours, patients who call in for treatment later in the day do not have the opportunity to receive full treatment before the DH closes for the day. Instead, they may need to be directed to the ED to initiate or continue treatment.
Patients with SCD consistently lack access to even the minimum standard of SCD clinical care, leading to exacerbated morbidities and mortality risk. Without such basic clinical treatment, patients frequently rely on costly emergency room care. We have formulated four recommendations—improving hydroxyurea compliance, pain management care access, and RBC and Transcranial Doppler Ultrasonography screenings—that we expect will improve SCD care, reduce pain episodes, minimize risk of strokes, and lower care costs.
Implementation:
• NC DHB should reimburse PHPs when they work with co-management of primary and hematology care, telehealth services, pediatric-to-adult transition strategies, and community health workers and educations in order to improve HU access and use among Medicaid patients with SCD.
The National Institutes of Health (NIH) recommends HU for all people living with SCD ages nine months and older.223 The American Society of Hematology (ASH) recommends HU for those who have more than three moderate to severe pain episodes in a twelve-month period.224 HU reduces incidence of pain episodes and acute chest syndrome by 50 percent, prevents or reverses organ dysfunction, and reduces hospitalization rates.225
NC Medicaid expects patients with SCD to try HU prior to other treatments.226 HU benefits are realized over a long period of time, but has immediate side effects, so many patients abandon HU before they experience health improvements.227 Providers in North Carolina have observed such behavior among their patients with SCD.
Despite the benefits and low cost of HU compared to other SCD treatments, access and uptake remain low.228 In 2017, just over one third of Medicaid and CHIP enrollees with SCD (37.1 percent of children and 34.5 percent of adults) had any days of HU use. Very few enrollees with SCD—15.6 percent of children and 9.6 percent of adults—had more than 180 days of HU use.229
Both provider-related barriers (e.g., expectations of patient non-compliance, concerns about side effects) and patient-related barriers (e.g., lack of follow-up with providers, side effects, not wanting to undergo monitoring, difficulties with transportation to clinics or pharmacies for refills) are likely depressing HU access.230 Poor transitions from pediatric to adult care are also associated with low HU uptake.231
Improved HU access relates to other recommendations in this report, including:
1. Co-Management of Care Between Primary Care Physicians and Hematologists. Frequent monitoring and visiting a hematologist are all associated with improved HU uptake and adherence.232
2. Telehealth. Telehealth can be helpful for monitoring HU use among rural populations.233
3. The Transition from Pediatric to Adult Care. Strategies that improve transition from pediatric to adult care are expected to improve HU adherence.234
4. NC Sickle Cell Syndrome Program Educators. In North Carolina, SCD clinicians suggested having state educators contact patients to explain the benefits of HU and encourage them to continue using the medication.
PHPs can cover telehealth and other remote services—whether performed by providers or CHWs—to remind patients with SCD to adhere to an HU regimen. PHPs should ensure that patients with SCD are being prescribed and adhering to HU as recommended, and that both providers and patients are aware of HU’s efficacy and safety. For both children and adults, PHPs can do this by facilitating coordination between primary care physicians and hematologists, and NC DHB can reimburse such coordination activity. For pediatric patients transitioning to adulthood, the recommendations outlined in Part II section 1a should increase HU adherence by increasing patient interactions with adult providers. Adjustment of PHP contracts to reimburse pain management would be a shortterm investment because contracts can be changed unilaterally.
Implementation:
• NC Medicaid should require PHPs to offer a variety of opioid and non-opioid pain management techniques.
• NC Medicaid should encourage destigmatization of opioid use amongst this patient population.
• NC Medicaid should reimburse individualized pain management planning.
Pain is the most common SCD morbidity and the leading cause of SCD-related hospitalization.235 Opioids are a mainstay of SCD pain management, but in light of dependency concerns, people living with SCD have difficulty accessing opioids for pain management.236 A significant reason for this difficulty is opioid stigma among providers and suspicions that patients are abusing opioids. Integrative, non-opioid therapies such as cognitive behavioral therapy, yoga, acupuncture and dietary supplements have also demonstrated effectiveness in reducing pain severity in patients with SCD. These therapies can help reduce patient dependence on opioids, which can have harmful long-term effects.237
In addition to opioid stigma, a North Carolina SCD clinician noted that provider oversight may also be undermining SCD pain management. Clinicians prescribing opioids for patients with chronic pain fear scrutiny from state medical boards and federal regulators.238 NC Medicaid does not require prior authorization for some short-acting opioids used for SCD pain management for up to five days, but it does require prior authorization for longer use.239 Patients with SCD often remain hospitalized for
six to ten days. As a result, they are often likely to need prior authorization to address their VOCs, or pain crises.240 By contrast, no prior authorization is required for opioids used to manage pain associated with cancer.241
NC Medicaid already covers behavioral health interventions, chiropractic services, and acupuncture, all of which could be useful for SCD pain management.242 However, NC Medicaid does not cover many non-opioid therapies.243 Moreover, providers in North Carolina indicate that NC Medicaid does not sufficiently reimburse work with patients on pain management.
ASH recommends that pain management be individualized to maximize benefits to the patient and to minimize risk of hospitalization.244 Individualization of pain management plans also mitigates bias- and stigma-associated withholding of appropriate pain care.
Without Medicaid coverage for more nonopioid therapies and reimbursement for pain management, providers are unable to optimally manage pain for their patients, increasing their risk of pain crises and hospitalization.
Other states have provided coverage for an array of non-opioid pain management techniques that have resulted in significant health improvements and cost reductions. Florida’s Medicaid program, offering acupuncture, chiropractic services, and massage therapy for eligible individuals with chronic pain, resulted in improvements in cognitive and physical function a nine percent reduction in per member per month costs.245 Likewise, Vermont Medicaid enrollees saw decreases in opioid use as a result of acupuncture therapy.246
Access to both opioid and non-opioid therapies is essential to successfully managing pain and reducing costly utilization.247 Federal guidelines recommend excluding patients with SCD from restrictions on opioid access.248 Providers in eastern North Carolina report giving their patients pain management plans which they can present when they see other providers (e.g.,
in an ED or primary care setting). They believe that this helps non-SCD providers deliver more effective care consistent with the patient’s needs.
Reimbursement for pain management, exemptions from opioid oversight regulation, and provider education to identify the role of bias and stigma in limiting access to pain treatment would enable providers to individualize treatment for patients, better address pain and reduce SCDrelated hospitalization costs.249
Adjustment of PHP contracts to reimburse pain management would be a short-term investment because contracts can be changed unilaterally by including them in PHP value added services/ in lieu of services. Determination of non-opioid therapies to cover would be a medium-term investment because it would take time to develop. For example, some non-opioid pain management techniques, including yoga, virtual reality, and guided relaxation, are not wellstudied.250 NC Medicaid should seek additional information to ensure that the pain-reducing benefits of covering any particular technique justify the costs.
In the long term, NC Medicaid should work with state regulators to exempt SCD clinicians from opioid audits while still ensuring that they do not over-prescribe opioids. NC Medicaid should also work with PHPs to engage providers in bias training, opioid education, and opioid destigmatization efforts.
Implementation:
• NC Medicaid should cover red blood cell (RBC) molecular testing (“genotyping”) for patients with SCD.
Background
RBC transfusion is a mainstay of SCD treatment. It is recommended preoperatively and to treat acute SCD complications like acute chest syndrome, stroke and organ failure.251 However, for patients with SCD, RBC transfusion carries a high risk of alloimmunization, a serious complication in which the patient’s own immune system destroys newly-transfused RBCs that do not match the patient’s blood type.252 Alloimmunization can also cause delayed hemolytic transfusion reactions (DHTRs), an extreme, life-threatening reaction to mismatched blood.253 Patients with SCD have the highest alloimmunization rate of any transfused patient population.254 One study estimated that about 50 percent of patients with SCD suffer alloimmunization.255
RBC molecular antigen testing beyond traditional serological testing can ensure that transfused blood is a proper match for a recipient, thereby avoiding these dangerous and costly complications in the future. The traditional serological tests used to match donor and recipient red blood are insufficient. They do not test for RBC antigens that are most frequently implicated in alloimmunization (i.e., C/c, E/e and K antigens), and they carry significant risk of error for patients transfused in the past three months.256
NC Medicaid covers traditional blood testing as part of newborn screens for SCD, but a 2018 NC Medicaid bulletin suggests that NC Medicaid does not cover RBC molecular antigen testing.257 However, Blue Cross Blue Shield of North Carolina (Blue Cross NC) covers such testing under its private plans and considers it medically necessary for SCD treatment.258 Patients with SCD receiving blood transfusions are at significant risk of complications like alloimmunization and DHTRs without properly matched donor blood.
RBC molecular testing is a once-in-a-lifetime test.259 ASH strongly recommends RBC genotyping for patients with SCD at the earliest opportunity, optimally before the first transfusion, to ensure that donor blood is safe to transfuse.260 It has near-perfect concordance with traditional serological testing, but it is insensitive to prior transfusions and provides additional, clinically significant antigen information to improve blood matching.261 In one survey of hospitals, 37 percent of respondent hospitals indicated that they obtain RBC molecular tests for all new patients with SCD.262
Alloimmunization and DHTRs are potentially deadly and very costly transfusion complications, requiring extended hospitalizations and risky treatments. Genotyping to prevent these complications would save lives and reduce morbidity. At the same time, genotyping is likely cost-justified.263 Physicians from the UNC Comprehensive Sickle Cell Disease Program estimate that preventing even one DHTR would likely pay for genotyping for 1000 patients with SCD. Further, molecular antigen testing can save time in transfusion management during acute situations.264
Adjustment of PHP contracts to cover RBC molecular antigen testing is a short-term investment. NC Medicaid can look to Blue Cross NC’s medical policy for language regarding the scope of coverage. Blue Cross NC recommends two FDA-approved panel test systems—
BLOODchip® ID CORE XT™ by Grifols
Diagnostic Solutions Inc. and PreciseType® HEA Test by Immuncor, Inc.—that are appropriate for patients with SCD who require frequent transfusions.265
NC Medicaid should facilitate annual transcranial doppler
ultrasonography (TCD) screening for children with SCD aged 2 to 16.
Implementation:
• NC Medicaid should remove prior authorization requirements for TCD.
• NC Medicaid should reimburse PHPs to coordinate care between radiologists and SCD clinics and training of SCD clinical staff to perform TCD screening.
Annual TCD screening is standard for children with SCD aged 2 to 16. TCD identifies those individuals who need transfusions, which in turn reduces their risk of stroke.266 If left untreated, approximately 11 percent of children with SCD will experience a stroke by age 20, a rate 250 times higher than the child population at large.267
Nationally, TCD screening rates among Medicaid patients are under 40 percent.268 Patient-related barriers to annual TCD screenings include inadequate transportation, duration of clinic visits, missed appointments, lack of awareness of the need for annual screenings, and mistrust of the procedure.269 Provider-related barriers include lack of awareness that TCD should begin at age 2, expectations that children will be uncooperative, lack of motivation, and poor coordination.270
As of February 2021, NC Medicaid covers TCD screening, however, the screening requires prior authorization, even for children.271 This prior authorization requirement results in an unnecessary barrier and burden to care.
In many clinics, TCD screenings are managed
by radiology departments rather than SCD centers. Many radiology departments refuse to perform TCDs when patients are already at the clinic with their SCD provider, necessitating follow-up visits which make successful TCD completion less likely.272 This additional complexity means that patients may have to manage scheduling across multiple clinical departments, which often do not coordinate their appointments. NC Medicaid does not have a policy regarding TCD screening coordination and provider reimbursement.
In a seminal study, TCD-based identification of children at risk of stroke, followed by appropriate transfusions, led to a reduction in stroke risk by 92 percent.273 In a United Kingdom systematic review and economic evaluation, the clinical- and cost-effectiveness of TCD scans combined with appropriate blood transfusions was demonstrated, with an incremental costeffectiveness ratio of £24,075 (about $38,422) per quality-adjusted life-year gain and avoidance of 68 strokes over the lifetime of a population of 1000 patients.274 The lives saved and stroke care avoided justified the treatment cost.
Patient education and coordination of TCD and SCD care can cost-effectively improve TCD adherence and reduce stroke incidence. Education and coordination of TCD within SCD care consists of a variety of activities. For example, coordinating radiology and SCD clinic appointments so that parents can obtain TCD screening in conjunction with a SCD clinic visit, improves TCD screening rates.275 Phone outreach by providers to parents explaining the purpose of TCD, sharing videos illustrating a typical procedure, and reminding them to bring children for annual screenings improves both TCD and SCD clinic appointment adherence.276
At St. Jude Children’s Research Hospital in Tennessee, a SCD clinic nurse was trained to perform TCDs, obviating the need for separate appointments with an unfamiliar radiology department.277 The St. Jude program, which also involved patient education and communication of abnormal TCD results and recommendations for transfusion, reduced initial stroke incidence among patients by 80 to 85 percent.
NC Medicaid should remove prior authorization requirements to facilitate access to this lifesaving procedure. Adjustment of PHP contracts as such would be a short-term investment. NC Medicaid should also reimburse providers for coordination between radiology and SCD departments and training nurses or other SCD clinical staff to perform TCDs. Developing TCD screening programs which PHPs would be required to implement is a medium-term investment. NC Medicaid can look to St. Jude and the Cincinnati Comprehensive Sickle Cell Clinic’s TCD program, which had 100 percent of eligible patients—most of whom were Medicaid enrollees—complete an initial TCD screen, with the average patient receiving an initial screen at 25 months old.278
NC Medicaid should include “people with sickle cell disease” as a priority population in PHP contracts.
Implementation:
• NC Medicaid should add “people with sickle cell disease” to its list of priority populations in the PHP contracts.
NC Medicaid’s PHP contract tasks PHPs with identifying high-need enrollees, or priority populations, needing care management; performing a Comprehensive Assessment for enrollees identified as being within a priority population; and creating individualized care plans for high-needs enrollees. Priority populations are defined as “populations likely to have care management needs and benefit from care management, including…individuals with Long Term Services and Supports needs; adults and children with Special Health Care Needs;…at-risk children (age 0-5); high-risk pregnant women; and other priority populations as determined by the PHP (i.e., [enrollees] with complex conditions like HIV, Hepatitis C, or Sickle Cell).”282 Notably, it is up to each PHP whether it considers enrollees with SCD a priority population that will receive comprehensive assessments and individualized care plans. If plans choose not to designate people with SCD as a priority population, people with SCD will continue to experience fragmented care and their health outcomes may worsen, exacerbating existing health disparities.
Care management and individualized care plans improve health outcomes for people with SCD.
Individualized care and pain plans drafted by the patients’ hematologists or primary care providers facilitate optimal pain management and decision making in the ED by mitigating biases in opioid prescribing and instructing the management of complications.283 Implementing individualized care plans can reduce hospital length of stay, readmission, and health care costs for high-utilizing adults with SCD.284 In interviews with hematologists in several comprehensive sickle cell centers in North Carolina, providers recommended individualized pain plans as an effective intervention because they address provider concerns about administering high doses of opiates for SCD pain and allow people with SCD to get individualized treatment
States have begun to pay increasing attention to SCD in recent years. The Michigan Department of Health and Human Services has made SCD a public health priority and has developed a sickle cell strategic plan to improve the care of Michigan residents with SCD.279 The South Carolina legislature appropriated funds to the Department of Health and Environmental Control to create a Sickle Cell Disease Study Committee to establish comprehensive treatment programs and establish standardized treatment protocols.280 Subsequently, the department formed the South Carolina Sickle Cell Disease Advocacy Team with local providers, health plans, SCD CBOs, and other stakeholders to produce the South Carolina Sickle Cell Disease State Plan 2019-2022; one recommendation was to provide case management to people with SCD in recognition that a comprehensive “whole person” approach to care can improve physical health and quality of life.281
anywhere, including in EDs. In a separate interview, the state’s Sickle Cell Educator Counselors confirmed that many of the state’s SCD centers produce provider-signed pain management plans for their patients to present in the ED.
The addition of “people with sickle cell disease” to the list of priority populations will task PHPs to collaborate with providers to bring resources to SCD and reverse the neglect the disease has historically received. This will ensure that people with SCD who have complex care needs will consistently receive care management and individualized care plans that improve their health outcomes, regardless of the PHP they are enrolled in. The state’s PHP contract already requires care management and individualized care plans for other complex populations and acknowledges that “people with sickle cell disease” could be a priority population as determined by PHPs, so creating a standalone designation of “people with sickle cell disease” as a priority population is a change that can be achieved in the short-term. It is unclear which PHPs already designate people with SCD as a priority population. Member handbooks for the plans do not mention comprehensive assessments and individualized care plans for enrollees with SCD, but interviews with some plans demonstrate that they recognize enrollees with SCD have complex health care needs that require comprehensive support.
NC Medicaid should assess PHP performance on outcomes for people with SCD.
Implementation:
• NC Medicaid should convene a workgroup of stakeholders, including people with SCD, to determine appropriate quality measures for SCD.
• NC Medicaid should add quality measures for SCD to “Required PHP Quality Metrics” that measure PHP performance.
NC Medicaid’s PHP contract requires PHPs to report a set of quality and administrative measures to assess the PHP’s processes and performance and, “beginning in Contract Year 3, the Department may implement withhold measures based on quality measures used to administer a PHP quality withhold/incentive program”.285 The list of required PHP quality metrics totals 66 quality measures and includes measures like “Medication Management for People with Asthma”, “Comprehensive Diabetes Care”, “Statin Therapy for Patients with Cardiovascular Disease”, among others. NC DHHS has the right to add additional quality metrics, providing opportunities to leverage quality metrics to identify weaknesses and prioritize populations.
NC Medicaid’s PHP contract does not include any quality measures that assess the PHP’s performance with SCD. Without quality measures and the quantification of outcomes and disparities for patients with SCD, it is difficult to determine where existing gaps are and develop effective interventions.
Quality measures improve processes of care and adherence to guideline-based process measures.286 Furthermore, quality measures provide an opportunity to increase transparency into existing disparities of care and ultimately reduce disparities.
Many sickle cell-specific quality measures have been developed in recent years that examine sickle cell care delivery, care use, patient experience, and outcomes. The National Quality Forum (NQF) has endorsed three quality measures for SCD care, including: i) NQF #2797, “Transcranial Doppler Ultrasonography Screening among Children with Sickle Cell Anemia”;287 ii) NQF #3166, “Antibiotic Prophylaxis Among Children with Sickle Cell Anemia”;288 and iii) NQF #3595, “Hydroxyurea Use Among Children with Sickle Cell Anemia.”289 In an interview with providers at a comprehensive sickle cell center in North Carolina, one provider identified adherence to medical visits and medication as simple quality metrics that improve health outcomes for people with SCD. NQF has several medication adherence measures for specific classes of medication therapy (but not SCD specifically) that can serve as examples.290
In FY2020, Michigan implemented a Medicaid quality improvement project focused on pediatric SCD that impacts its Children’s Special Health Care Services population; the project assessed three pediatric SCD quality measures: i) Proportion of Pediatric Members (ages 2 -15 years) with Sickle Cell Anemia with a Completed Transcranial Doppler (TCD) screening;
ii) Proportion of Pediatric Members with Sickle Cell Anemia <5 years old with at least 300 days of Dispensed antibiotics; and
iii) Proportion of Pediatric Members (ages 1 through 17) with Sickle Cell Anemia with at least 300 days of Dispensed Hydroxyurea.291
In an interview with a PHP representative in North Carolina, the interviewee explained that Medicaid has minimal quality measures and many PHPs are already collecting their own quality measures independent of Medicaid requirements to ensure their enrollee population is healthy. They noted it is not an issue for plans to incorporate additional quality measures, which NC Medicaid already has plans to do.
Existing SCD quality measures are a starting point for NC DHHS to create a stakeholder group (that includes people with SCD) with the goal of determining appropriate SCD quality measures that should be incorporated into the PHP contract to foster high-quality SCD care and identify opportunities for improvement. Thus, the addition of SCD quality measures is achievable in the medium-term.
The population of people with SCD is small, so there may be methodological challenges when trying to measure PHP performance. Programs that assess providers’ performance relative to an expected target or comparison group can be biased by random variation.292 Thus, NC Medicaid should pursue guardrails and appropriate statistical approaches in its design of quality measures. Some strategies include assessing prior variations and risk adjusting for case-mix.293
NC Medicaid should explore innovative payment models, such as incentive programs, to increase utilization of recommended SCD treatments and improve SCD health outcomes.
Implementation:
• NC Medicaid should implement an incentive program for SCD to drive use of evidence-based care.
• NC Medicaid should incorporate the use of SCD quality measures into its incentive programs.
NC Medicaid’s PHP contract requires PHPs to have incentive programs for Advanced Medical Homes and allows PHPs to develop their own physician incentive plans to award other providers for positive health outcomes.294 There are several problems outlined within this report that a SCD incentive program can address, including the lack of hydroxyurea uptake, transcranial doppler ultrasound screenings, primary care provider familiarity with SCD, and individualized pain plans.
A needs assessment of ED providers throughout the state found that only 32.4 percent of providers were aware of the National Heart, Lung and Blood Institute SCD recommendations.295 Thus, lack of provider knowledge can be a barrier that prevents people with SCD from getting the most effective treatment for their condition.
Incentive programs provide an opportunity to drive health plans and providers to use evidence-based care, improve their performance, and target investments in two ways: paying for services and meeting quality metrics.
Incentives for Health Plans:
• New York’s Medicaid Managed Care Quality Incentive program provides bonuses and performance-based autoassignments to health plans based on composite scores from quality measures, satisfaction measures, prevention quality, and compliance.296 The state has seen improvements in quality of care.297
Incentives for Providers:
• Pennsylvania Medicaid’s ACCESS Plus program, an enhanced primary care case management fee-for-service program, contracts with a vendor to provide primary care case management and disease management. A portion of the contractor’s capitation fee is allocated to providing financial incentives for providers to participate in disease management services.298 The program pays physicians a one-time payment of $200 just for participating in Access Plus, an annual $17 per-patient bonus for patients who take necessary medications, and a $60 bonus per completed Chronic Care Feedback Form every six months, among others. The program was associated with a statistically significant reduction in ambulatory visits per enrollee.299
• The Office of Minority Health at the U.S. Department of Health and Human Services issued a $1.25 million grant to New York City Health + Hospitals/ Queens to “determine the feasibility and effectiveness of providing financial incentives to providers to improve the quality of life for children with SCD through increased prescription rates of hydroxyurea.”300 The goal of the demonstration is to test whether physician incentives can drive increased hydroxyurea use in people with SCD; the program is currently underway.
In an interview with a hematologist at a comprehensive sickle cell center in North Carolina, the provider identified rewards for providers as a way to guide provider behavior and improve health outcomes for people with SCD. The concept of “what gets paid gets done” was echoed in an interview with a PHP representative in North Carolina, who explained that payment incentives can be a “carrot” to guide desired behaviors and reach necessary quality measures.
An incentive program for SCD at the health plan-level and/or provider-level can work in tandem with SCD quality measures to improve health outcomes for people with SCD. NC DHHS should leverage its ability to convene a stakeholder group to determine appropriate quality measures and appropriate methods of reaching those quality measures, including the use of incentive programs. These actions will direct resources and high-quality care towards people with SCD and improve health outcomes for this population. The creation of a Medicaid incentive program for SCD is a long-term goal given that NC Medicaid’s priority in the shortterm is implementing managed care and further exploration into feasible incentive structures is needed.
Similarly to the quality measurers recommendation, because people with SCD are a relatively small population, methodological challenges could arise when trying to measure performance and rewards. Thus, NC DHHS should pursue guardrails and appropriate statistical approaches in its incentive program design. Some strategies include assessing prior variations and risk adjusting for case-mix.301
NC Medicaid should explore innovative payment models, including Subscription-Based Payment Models (SBPMs), to increase utilization of new therapeutics and improve SCD health outcomes.
Implementation:
• NC Medicaid should apply for a Medicaid State Plan Amendment (SPA) that will allow NC DHHS to leverage SBPMs as expensive SCD therapeutics come to market that improve SCD outcomes.
By 2030, an estimated 40 to 50 gene therapies will provide novel curative options for a variety of conditions.302 Gene therapies for treatment of SCD that aid in the production of normal red blood cells (RBCs) are currently in the drug pipeline and appear promising. In an ongoing phase 1/2 clinical trial, lentiviral-based therapy demonstrated efficacy, suggesting that it may improve the lives of patients with SCD.303 In the European Medicines Agency (EMA), a gene therapy using the lentiviral vector received conditional approval in 2019, which indicates that this gene therapy may soon be entering U.S. markets.304 The cost of this therapy in Europe was set at 1.58 million euros ($1.78 million) over five years. The pharmaceutical company, bluebird bio, Inc., expects that pricing will be similar in the United States.305 This therapy is anticipated to be a one-time, potentially curative therapy.
Subscription-Based Payment Models (SBPMs) are a novel approach to paying for drugs that allows state Medicaid programs to contract exclusively with a single manufacturer to supply treatments at a reduced price while improving budget predictability. States pay a reduced price per prescription or treatment up to a set threshold. Once that threshold is met, the cost of
additional prescriptions is nearly zero.306 SBPMs achieve goals for both the Medicaid program and the pharmaceutical company: SBPMs cap payments and increase access to expensive, life-saving treatments that would otherwise be inaccessible to Medicaid enrollees, while ensuring pharmaceutical manufacturers receive guaranteed, negotiated revenue.307 Typically, Medicaid programs have to cover all drugs of participating manufacturers that have been approved by the Food and Drug Administration (FDA), but subscription models approved by CMS allow Medicaid programs to contract with only one manufacturer for one treatment.308 Thus, the manufacturer with which the state contracts gains the state’s entire market share of patients that need the treatment—an appealing proposition when there are other competing treatments in the pipeline (Table 1).
Currently, NC Medicaid covers all medications and treatments for SCD, without requiring prior authorization. As the majority of SCD patients nationally—an estimated 70 percent of children and 50 percent of adults—are covered under Medicaid or Medicaid administered programs, it is extremely important that innovative treatments continue to remain covered under Medicaid.309 And with five percent of Medicaid and CHIP enrollees in NC having SCD, it is crucial for the state to employ innovative methods to keep expenses down while providing access to these treatments.
Gene therapies have the potential to be costeffective in the long run. As of 2020, lifetime SCD-related health care expenditures exceed approximately $550,000 per person.310 One study estimated that a hypothetical treatment for SCD provided at birth would provide a costeffectiveness of $150,000 per quality-adjusted life year (QALY).311
Table 1. Gene Therapies in the U.S. Drug Pipeline through US Clinical Trials Intervention Clinicaltrials.
Genetic: GPH101 Drug Product Gene Correction in Autologous CD34+ Hematopoietic Stem Cells (HbS to HbA) to Treat Severe Sickle Cell Disease
Phase
Phase 2 12 to 50 years old May 2023 bluebird bio, Inc.
Phase 3 2 to 50 years old July 2024 bluebird bio, Inc.
Phase 1 Phase 2 12 to 40 years old May 2026 Graphite Bio, Inc.
Phase 1 Phase 2 18 to 50 years old August 2025 Editas Medicine, Inc. Gene transfer.
Biological: single infusion of autologous bone marrow derived CD34+ HSC cells transduced with the lentiviral vector containing a short-hairpin RNA targeting BCL11a
Gene Transfer for Sickle Cell Disease
Phase 1 3 to 40 years old
June 2022 *Trial is funded by National Institutes of Health (NIH)
Source: Clinicaltrials.gov
However, balancing the budget may be difficult in the short-term if and when gene therapies enter the U.S. market. SBPMs offer an alternative payment model that, if implemented, will allow NC DHHS to ensure their SCD patients receive these essential therapies at a reduced-price level. SBPMs remove the incentive to ration access due to no additional cost occurring after a certain threshold.
To date, NC Medicaid covers all treatments for SCD. This pattern of coverage should continue. A typical, pure subscription model requires waiver approval from CMS. To avoid this requirement, Louisiana and Washington had pharmaceutical companies bid on a price and used specific language in their agreement.312 This supplemental rebate agreement using a SBPM allowed the two states to avoid the waiver approval process. CMS approved both Louisiana’s and Washington’s programs through Medicaid SPAs.313
SBPMs allow NC Medicaid to anticipate highcost interventions and treatments as therapeutics are developed for SCD, particularly within the domain of gene therapy. Another benefit of SBPM is that states experience fixed, upfront costs regardless of the number of people treated. This allows states to avoid the risk of spending overbudget and facilitates state budget planning and predictability. Finally, SBPMs encourage the treatment of as many individuals who would benefit from the drug as possible.
Models in Louisiana and Washington
Medicaid programs in Louisiana and Washington have implemented SBPMs for hepatitis C drugs. Hepatitis C, which typically impacts low-income and disproportionately marginalized communities, has seen a recent surge in available and effective treatments. While these treatments are essentially curative, they remain costly at a list price between $25,000 to $95,000 per prescription.314 The expensive price-tags were leading Medicaid programs to impose strict eligibility requirements. In an effort to increase access to and utilization of these treatments and to improve budget predictability, Louisiana and Washington implemented SBPMs with pharmaceutical companies.
A recent cross-sectional study of Louisiana and Washington evaluated trends in prescription fills before and after the changes in SBPM Medicaid-covered prescriptions. Louisiana saw a sharp increase of 534 percent in prescriptions filled (from 43.1 to 206.0 average rate of prescription fills per 100,000 Medicaid enrollees).315 Washington did not see a significant change in prescription fills. Possibilities for these differences in outcomes may include state-level differences in implementations, historical restrictions on access to the medications, and responses to the COVID-19 pandemic, as the study included data from January 1, 2017 to June 30, 2020.316
Relying upon evidence-based research and the stakeholder interviews conducted in North Carolina, we present recommendations to NC DHHS to use innovative care and payment models to reduce maternal health disparities. We expect that improvements in care management and administrative feasibility, increased access to non-medical caregivers, innovative models of care, and PHP contracts that prioritize equitable outcomes will improve health outcomes and reduce the enduring racial and ethnic disparities among pregnant and postpartum women in North Carolina.
Care management is defined as a “teambased, person-centered approach to effectively managing patients’ medical, social and behavioral conditions.”317 This includes managing high-risk patients who may have chronic conditions or psychosocial needs, creating care plans, and coordinating care such as appointments and referrals.318 For pregnant and postpartum women that are high-risk and low-income, home visit programs are a key pathway for identifying needs and providing care management. Additionally, as women transition from perinatal period to birth and then postpartum, care coordination is key so that women can access continuous care without facing barriers. Given that Black women are more likely to suffer from chronic conditions or live in vulnerable environments as compared to white women in North Carolina, improving care management can improve the racial disparities in maternal health outcomes.319
Implementation:
• NC Medicaid should implement teambased home visits that include CHWs and leverage the Community Health Workers Initiative to deploy CHWs.
• NC Medicaid should expand eligibility for home visit case management to all pregnant and postpartum women on Medicaid.
• NC DHHS should support funding increases into home visit programs.
North Carolina has implemented several home visit programs through a combination of federal and state funding, including the Pregnancy Management Program (PMP) and Maternal, Infant, and Early Childhood Home Visiting Program (MIECHV).
NC Medicaid runs the PMP (formerly the Pregnancy Medical Home), which requires providers to coordinate high-risk pregnancy case management and home visits with case managers at the local health department, who are typically licensed social health workers or nurses.320 The program is available in every county, and has made North Carolina a national leader for pregnancy care management.
North Carolina also receives federal funding through the U.S. Health Resources and Services Administration (HRSA)’s Maternal, Infant, and Early Childhood Home Visiting (MIECHV) program. HRSA’s MIECHV program “supports home visiting for pregnant women and families with children up to kindergarten entry who live in communities at risk for poor maternal and child health outcomes.”321 Currently, the NC MIECHV program funds two models: i) Nurse-Family Partnership (NFP) which connects specially
educated nurses with young, first-time momsto-be; and ii) Healthy Families America (HFA) which works with families who may have histories of trauma, intimate partner violence, mental health issues, and/or substance use issues.322 84 percent of NFP clients in North Carolina are enrolled in Medicaid at intake.323
These home visiting programs are promising. However, access issues remain. First, home visits are not available for all the mothers that need them in the state. NFP is only available in 26 counties and HFA is only available in five counties.324 Second, PMP case management and home visits is offered statewide but is limited to pregnancies are identified as highrisk. Although high-risk screening is an effective tool, it may be limited in identifying all high-risk mothers who need case management; women may not be willing to share all their needs due to stigma related to mental health or substance use.325 Third, it can be challenging to offer home visiting services in locations that lack access to providers, especially in rural areas.
The existing home visiting programs in the state have resulted in improved outcomes and reduced costs. Participation in PMP was associated with a three percent increase in timeliness to prenatal care and a ten percent increase in attending postpartum visits.326 North Carolinians served by NFP had higher rates of full-term pregnancies and increased initiation of breastfeeding; NFP also estimates that for every $1 invested in its North Carolina program, $5.50 is saved in future costs for families that are classified as highest-risk.327
To ensure that home visit programs can meet a range of social needs experienced by pregnant and postpartum women with Medicaid coverage, the state can provide a wider set of services.328
In Michigan, the Maternal Infant Health Program (MIHP) relies on teams of providers to conduct home visits to all Medicaid-eligible pregnant and postpartum women, including a registered nurse, licensed social worker, infant mental health specialist, registered dietician, and a lactation consultant.329 By incorporating staff with a variety of trainings into home visits and using a teambased approach, pregnant and postpartum women can better have their needs met.
CHWs should be included in this team-based approach and incorporated into maternalfocused home visits. CHWs offer a unique lens because they tend to be local to the neighborhood and can be more effective at creating trust due to common languages or cultural background.330 As a result, CHWs have positive effects on the health of people of color and people with lower socioeconomic status, which can narrow health disparities.331 Additionally, the incorporation of CHWs has resulted in reduced unnecessary health service utilization and cost savings.332 Several studies demonstrate the impact of CHWs on maternal health specifically. Arizona’s Health Start program integrated CHWs into its maternal health home visit programs and the change was associated with improved birth weight outcomes.333 A randomized trial testing the impact of a nurse-CHW team home visiting intervention on Medicaid-eligible pregnant women found that the nurse-CHW team reached far more women, especially those with mental health-related problems, and were able to deliver more services to these women.334
Given the positive outcomes associated with home visits and the fact that high-risk screenings can miss women that would benefit from additional care, we recommend expanding home visit services to all pregnant and postpartum women with Medicaid coverage. Various states have implemented strategies to expand home visits to all Medicaid-eligible pregnant and postpartum mothers, including MIHP in
Michigan. MIHP covers all Medicaid-eligible pregnant women and infants until the age of 18 months for home visits.335 This program is part of partnerships with managed care organizations, and health plans are obligated to refer every pregnant woman covered under their plans to MIHP.336 MIHP has demonstrated positive effect on prenatal and postnatal care, including increased adequate prenatal care and increased timely postnatal care. It has also been shown to reduce infant deaths, both amongst Black populations and other populations of color.337
In the short-term, NC Medicaid should increase the role for CHWs in maternal health by integrating them into PMP. NC DHHS operates the Community Health Worker Initiative with the goal of “establish[ing] a sustainable infrastructure that acknowledges the value of CHWs, supports their professional identity, and integrates their role in the healthcare team”.338 NC DHHS should consider how it can leverage the Community Health Worker Initiative to deploy CHWs to maternal home visiting programs like PMP, similarly to how NC DHHS deployed over 400 CHWs to 55 counties.339
In the medium-term, NC DHHS should support funding increases to home visiting programs to expand their capacity to provide services through additional locations or staffing. Programs like NFP and HFA operate on a combination of federal, state, and/or private funding.
In the longer-term, NC Medicaid should expand eligibility for home visit case management to all pregnant and postpartum women on Medicaid.
Implementation:
• NC Medicaid should integrate postpartum care into well-child visits where the birthing mother is present.
• NC Medicaid should utilize care coordinators for all Medicaid-eligible postpartum women to integrate them into medical homes.
• NC Medicaid should specifically offer postpartum home visits to all Medicaideligible women.
Continuity of care throughout pregnancy and postpartum is key to improving maternal and infant health outcomes.340 Acknowledging the importance of the postpartum period, North Carolina’s new budget includes a permanent expansion of pregnancy Medicaid to one year postpartum. Despite this progress, ensuring women, and specifically women of color, actually receive quality postpartum care should remain a top priority.
In North Carolina, postpartum visit attendance among Medicaid enrollees is troublingly low. A study of six Atrium Health hospitals in Mecklenburg County in 2014-15 found that 90 percent of mothers with commercial insurance, but only 50 percent of mothers with Medicaid, received a six-week postpartum checkup.341 Notably, a majority of the mothers insured by Medicaid were women of color—49 percent identified as Hispanic and 32 percent identified as non-Hispanic Black.342
Multiple factors inhibit attendance at postpartum visits. These include challenges in caring for a new baby, lack of transportation, and limited access to childcare (see Transportation Section in Part I).343 Another major challenge is scheduling around well-child visits. Mothers already have to find time to bring their children in for well-child visits, making it difficult to schedule additional visits for their own postpartum care.344 When mothers do attempt to schedule postpartum appointments, they may lack information on their type of coverage and who to call to schedule an appointment.345 Furthermore, mothers often see different providers during prenatal, birth, and postpartum periods, which can inhibit the creation of trust between women and their providers.346
One method to improve postpartum care attendance is to integrate care within well-child visits. Research shows women with Medicaid are more likely to attend well-child visits than to attend their own postpartum visit. A study of women in a Chicago hospital found that 86 to 94 percent support this kind of care integration.347 The IMPLICIT (Interventions to Minimize Preterm and Low Birth Weight Infants through Continuous Improvement Techniques) network—which has more than 20 sites across several states, including North Carolina— provides interconception care at well-child visits. This care includes screening and counseling focused on smoking, depression, contraception, and multivitamin consumption.348 The IMPLICIT interconception care program offers various billing options through Medicaid, depending on the service provided. For example, counseling on smoking and depression can potentially be billed under the child’s benefits—since these issues impact the child—or the mother’s benefits. Counseling on family planning or multivitamin consumption can be billed under specific codes in the mother’s coverage if she is enrolled in Medicaid.349 Additionally, under Virginia’s BabyCare program, providers are reimbursed for conducting behavioral health screenings for
mothers at well-child appointments under the infant’s insurance, which help uncover issues such as mental health, domestic violence, or substance use.350
Care coordination that supports mothers in creating postpartum care plans and scheduling appointments may improve postpartum care. A study at a Medicaid-based clinic in Chicago evaluated the impact of a patient navigator who provided appointment scheduling assistance, referrals to other services, and information on contraception and breastfeeding. The study found positive associations with postpartum checkups by 12 weeks postpartum, as well as receipt of contraceptive methods and postpartum depression screening.351
Mothers should receive a postpartum care plan from an interdisciplinary provider team before hospital discharge or within 24 hours after discharge.352 The postpartum care plan should include information on the following:
• Assignment to a medical home and a point of contact.
• Plans for a postpartum follow-up visit as well as any other follow-up appointments for other medical conditions.
• Information regarding social services, breastfeeding, contraception, chronic conditions and mental health.353
Continuity of care can be improved by facilitating contact between postpartum and prenatal providers or ensuring the same care coordinator through pregnancy and postpartum.354
As discussed in the above section (see Home Visits), home visits are a key pathway to provide care management, especially for low-income mothers of color. The Maternal Infant Health Program (MIHP) in Michigan covers all Medicaideligible pregnant women and infants until the age of 18 months for home visits.355 New Jersey and Oregon have implemented universal
mother and infant home visiting programs in the postpartum period.356 A study conducted in Durham, North Carolina found that a universal postpartum home visiting program conducted by nurses had a positive impact on maternal mental health and infant health care in the first year after birth, as well as a decrease in ED utilization by the mother.357
In the shorter term, as NC Medicaid expands its eligibility to postpartum women up to one year, all Medicaid-eligible mothers can benefit from care coordination to facilitate appointment scheduling and continuity of care. Case management and medical home integration for all postpartum women can be arranged through PHP contracts. Furthermore, the inclusion of postpartum care into well-child visits when the birth mother is present, including screening for risk factors, can improve access to postpartum care. In the longer term, for marginalized mothers struggling to attend postpartum visits, home visits can be a pathway to increasing access to postpartum care. NC Medicaid should consider expanding home visits beyond high-risk pregnancies to all Medicaid-eligible postpartum women through PHP contracts within a medical home model.
NC Medicaid should cover and support doula services.
Implementation:
• NC Medicaid should submit a SPA to cover doula services as a preventive service and allow doulas to support pregnant women without working under a doctor’s permission.
• NC Medicaid should learn from the other state Medicaid programs and set reimbursement rates for doula services at a livable wage.
• NC Medicaid should encourage the NC General Assembly to appropriate funds to create grant programs to build up the doula workforce in low-income communities of color in the state.
A doula—as defined by North Carolina-based doula program, Sistas Caring 4 Sistas—is “a trained professional who provides continuous physical, emotional, and informational support to a mother before, during, and after childbirth to support her in achieving the healthiest, most satisfying birth and postpartum experience possible.”358 Often, a doula is a member of the same community as the pregnant woman (i.e., a community-based doula). Doulas are not medically trained and do not perform any medical tasks. Instead, doulas work alongside medical staff—acting as an advocate for the woman, combatting discriminatory practices, and ensuring the woman’s preferences and concerns are listened to by medical staff.359
Community-based doulas can employ culturallyappropriate interventions and recenter the pregnant woman’s experience in care practices, resulting in improved maternal and infant health outcomes, increased breastfeeding initiation, fewer complications, and more positive patientreported medical experience. Extensive evidence has shown the impact of doulas on C-section rates, preterm birth rates, and breastfeeding initiation, as summarized below.
• Improved C-Section and Preterm Birth Rates. In a study of Medicaid enrollees in Minnesota, the C-section rate was 40 percent lower among women who received doula support compared to women who did not, after controlling for clinical and sociodemographic factors.360 A follow-up study also found the preterm birth rate was 25 percent lower among doula-supported births.361 These lower C-section and preterm rates were maintained among Black Medicaid enrollees with doula support compared to Black enrollees without a doula.362
• Improved Breastfeeding Initiation. Women receiving doula-supported pregnancy care have greater attendance at prenatal and postpartum visits and near-universal breastfeeding initiation.363 Notably, when receiving culturally-appropriate doula care, 93 percent of Black women with Medicaid initiated breastfeeding compared to 70 percent when not receiving doula care.364 While not directly related to mortality or morbidity, all of these are strong indicators of healthy outcomes for women.365
Currently, Medicaid does not reimburse for doula services and North Carolina does not have a state doula certification. Despite this, doulas still practice within the state—below is a map of where doulas currently practice in North Carolina (see Figure 11).
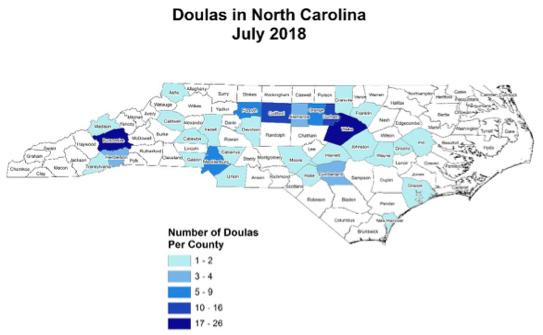
Multiple PHPs currently include doula services as a value-added benefit for a subset of their Medicaid enrollees or as a partially reimbursable service. Healthy Blue includes doula services as a value-added benefit for enrollees in limited locations.366 WellCare of North Carolina offers a similar value-added benefit specifically for teenage enrollees that are experiencing unstable housing.367 UnitedHealthcare reimburses Medicaid enrollees up to $100 for doula services.368 Additionally, Blue Cross NC and University of North Carolina have provided grants to doula programs that train community-based doulas of color and provide doula services to low-income Black pregnant women.369
Various stakeholders expressed strong support for expanding access to doula services for pregnant North Carolinians during interviews; without Medicaid coverage of doulas, these services become inaccessible to most pregnant women in the state. The interviews are consistent with findings from research that suggests the major barrier to receiving doula care is the outof-pocket cost, since doulas are not typically covered by insurance.370 Additional barriers include the lack of access for rural communities and the lack of racial or ethnic concordance between the pregnant woman and the doula.371
A universal doula benefit would specifically improve access to usage of doula services for Black women and women with Medicaid coverage. Notably, in a national survey of women who recently gave birth, these populations were most likely to want doula support but not have access to it during their pregnancy.372
On the supply side, the cost of training to become a certified doula can be prohibitive.373 Many people are discouraged by the low and often unlivable wages earned by doulas. Although private and non-profit entities have provided grants to fund training of communitybased doulas and support women in accessing doula care, grants are unsustainable in the longrun and at-scale.
Community-based doulas in North Carolina, much like results shown in other states, have been associated with improved maternal and infant care and outcomes. A 2008-2010 study of doula care among low-income, primarily Black women in Greensboro, North Carolina concluded that “doula-assisted mothers were four times less likely to have a low birth weight (LBW) baby, two times less likely to experience a birth complication involving themselves or their baby, and significantly more likely to initiate breastfeeding.”374 These results are consistent with more recent data from Sistas Caring 4 Sistas, a doula program run by and for Black women in the Asheville-area. Their clients were 12.4 percent more likely to begin prenatal care in the first trimester of pregnancy and about 50 percent less likely to have their baby born with low birthweight than the average Black woman within the county.375
Four states currently cover doula services— Minnesota, New Jersey, Oregon, and Virginia. An additional six states are set to begin Medicaid coverage of doula service in 2022, including California, Illinois, Maryland, Nevada, Rhode Island, and Washington, D.C..376 These states learned from the early-adopters and shaped their policies accordingly.
Most of the states are following Oregon’s approach, which consists of covering doulas as a preventive service that does not require supervision, rather than covering doulas as a pregnancy-related service. This removes the barrier of needing to work under a supervising provider (see the Midwife Workforce section for more detail on this). Minnesota doulas, who are required to practice under a doctor within pregnancy-related services, note that many providers are unwilling to supervise them.
Evidence suggests Medicaid reimbursements rates for doula services must be enough to i) incentivize doulas to take on Medicaid patients, and ii) allow doulas to maintain a livable income. Doulas in Oregon point to Medicaid billing rates as the most significant barrier to taking on Medicaid clients and operating a sustainable doula practice. In contrast, New Jersey and Virginia set their reimbursement rates much higher to ensure doulas make a livable wage.
Additionally, North Carolina stakeholders expressed concern regarding whether the certification and accreditation process would create an additional barrier for people, especially low-income women, to become doulas. New Jersey has taken steps to address these concerns by making the accreditation process short. The state is also partnering with local community-based doula programs to help with certification and accreditation. Finally, New Jersey is offering grants to community-based organizations, specifically in communities of color, to set-up doula training programs and to subsidize people going through the training.
Covering doula services as a preventive service is a medium-term investment. It requires NC Medicaid to submit a State Plan Amendment (SPA) to CMS and receive federal approval. New Jersey, Oregon, and Virginia were approved for their doula-related SPAs, while other states are currently in the SPA submission process.
Medicaid reimbursement of doula services may require additional funds from the NC General Assembly to initiate this new benefit; however, doula services can be cost-saving in the long run. Relying upon Medicaid data from multiple states, a team of researchers modeled the cost effectiveness of doula care and estimated an average saving of $986 per birth due to reductions in preterm births and C-sections.377
Encouraging the NC General Assembly to appropriate funds for doula training grant programs may be more difficult given state budget restraints. Yet, given these grant programs would be a minor appropriation amount it may be more feasible. A bill introduced in the NC General Assembly would establish awarding up to five doula training grants ranging from $10,000 to $50,000 annually.378 Alternatively, NC Medicaid could encourage PHPs to privately fund community-based doula programs, similarly to BlueCross NC’s current grant program.
Implementation:
• NC Medicaid should add group prenatal care in PHP contracts.
• NC Medicaid should work with stakeholders to develop an adequate incentive payment rate for group prenatal care.
Group prenatal care differs from traditional childbirth education classes in several ways. In traditional classes, the program is not clinicallybased and provides information on subjects such as newborn care, breastfeeding, and the labor and delivery process. In contrast, in group prenatal care, women with similar due dates meet with a health care provider in a group setting, where group discussions are facilitated by the clinical staff. Women participate in collecting health metrics, such as taking blood pressure and charting, and have the opportunity to meet one-on-one with the medical specialists.379 CenteringPregnancy is a specific evidence-based group prenatal care that has been implemented across the country.
As discussed in the background section, Black women experience much higher rates of poor maternal outcomes. Specifically—as it relates to group prenatal care—Black women experience higher rates of depression during the pregnancy and postpartum period.380 Black women also are at higher risk for giving birth to a preterm and/or low-weight baby, which, in addition to causing worse outcomes for the infant, can be associated with increased rate of maternal depression and other maternal health conditions.381 Black women generally experience higher levels of stress in their daily life, which in turn can negatively impact their pregnancy health and outcomes.382
Black women with Medicaid expressed higher levels of dissatisfaction and lower levels of medical support during pregnancy care than white women with Medicaid.383 Low levels of medical support are also associated with pregnant women underutilizing low-cost pregnancy care options (e.g., office visits) and overutilizing high-cost care. In a study in North Carolina, pregnant women with Medicaid were three times more likely to visit the emergency department for nonurgent reasons than pregnant women with private insurance. The researchers point to “uncertainty regarding symptoms, a lack of consistent medical care, or psychosocial issues” as the primary reasons for the overutilization of emergency services.384
In North Carolina, group prenatal care models are not covered by Medicaid. However, NC Medicaid has previously considered covering group prenatal care, specifically through CenteringPregnancy. A 2019 report commissioned for the NC Office of State Budget and Management concluded CenteringPregnancy’s benefits would outweigh its costs for the pregnant person and baby, as well as for taxpayers and other indirect entities.385 Additionally, UnitedHealthcare is currently providing grants for North Carolina OB-GYN practices to create and run CenteringPregnancy programs.386
Group prenatal care can help reduce incidences of maternal and infant morbidity for Medicaid enrollees, specifically for Black pregnant women. A systematic literature review of group prenatal care studies found high-quality evidence, across multiple studies, that group prenatal care is especially beneficial to Black pregnant women.387 Specifically, low-income Black women that receive group prenatal care have a reduced risk of delivering before term or at term to a low birthweight baby, a reduced risk of receiving a C-section, and an increased rate of breastfeeding initiation.388 Additionally, Black women report being more satisfied with their pregnancy-related care.389 Researchers posit
that “one potential explanation for improved outcomes in African American women is the provision of social support, coping strategies and stress reduction through group prenatal care.”390 Group prenatal care may also reduce overutilization of high-cost care (e.g., visiting the emergency department for a nonurgent reason).391
CenteringPregnancy, a specific group prenatal care method, has showed positive results among Medicaid populations. In Georgia, multiple studies throughout the state confirm the positive effects of the program specifically on Black Medicaid enrollees.392 Of note, one of the Georgia studies was run through telehealth and still found positive effects.393 In South Carolina, Medicaid enrollees were more likely to attend their postpartum visit and less likely to have a preterm birth if they went through the group prenatal care program.394
Nine states, including Louisiana, Michigan, South Carolina, and Texas, currently reimburse providers for group prenatal care at a higher rate than traditional prenatal care.395 These enhanced reimbursement rates vary from $40 per patient per visit for group prenatal care to a rate that only is enhanced if the provider serves large groups. This would be difficult to implement in North Carolina, where PHPs are reimbursed via bundled package payment models instead of a fee-for-service schedule.396 However, NC Medicaid could use incentive payments, which is a similar tool to higher reimbursement rates but fits within NC Medicaid’s pregnancy medical home bundle. NC Medicaid already provides two incentive payments: $52.50 for every pregnant patient receiving care in a PMH who received standardized risk screening and $157.50 for every patient receiving a comprehensive postpartum visit 14-60 days after giving birth.397
After speaking with several North Carolina stakeholders, we believe if NC Medicaid provides an incentive payment for a patient who received group prenatal care, more providers would offer this model of care. Implementing a new incentive payment for group prenatal care would be a medium-term investment because it will take several months for NC Medicaid to convene relevant stakeholders and determine an average incentive payment based on the cost service and private insurance reimbursement rates. According to North Carolina stakeholders, it also takes several months for NC Medicaid to engage with PHPs and other stakeholders to develop the payment rate. NC Medicaid should also encourage the NC General Assembly to appropriate a small amount of additional funds for grants to local health providers that want to initiate a group prenatal care program.
An additional challenge to expanding group prenatal care, such as CenteringPregnancy, is the cost for PHPs or clinics to initiate the program and train clinical staff in the group prenatal care model.
Implementation:
• NC DHHS should support legislation to remove the requirement that Certified Nurse Midwives must have a supervising physician and allow them to work autonomously.
• NC DHHS should work with other state agencies to create certification requirements for Certified Professional Midwives and Certified Midwives and to support the NC General Assembly to approve this new certification.
• NC Medicaid should set their midwife reimbursement rate at parity with the OBGYN rate for providing the same care.
A midwife is a trained health care professional who specializes in pregnancy, delivery, and postpartum care. There are three professional designations in the field:
1. Certified Nurse-Midwife (CNM). CNMs are trained nurses with additional training in midwifery.
2. Certified Midwife (CM). CMs receive similar midwifery training to CNMs but are not certified as a nurse.398
3. Certified Professional Midwife (CPM). CPMs spend multiple years learning about midwifery care and acting as an apprentice before becoming certified.399
All types of midwives apply the midwifery model of care to maternity care, which takes a patient-centered approach and limits birthing interventions to those deemed necessary.400
In North Carolina, the vast majority of pregnancy care is done by OB-GYNs and most births occur in hospitals, with reliance upon midwifery care being much lower than in other states. In a national study examining the integration of midwives in the health care system, North Carolina ranked as the worst integrated state, earning a score of 17 out of 100.401
As of 2020, there are only 318 CNMs practicing in the state. In 48 counties, including 34 rural counties, there are no CNMs. Most counties do not report race data for CNMs, but in the 21 reporting counties only 12.9 percent of CNMs are underrepresented minorities.402 North Carolina is one of three states that require CNMs to practice under a physician’s written permission, making certification difficult for CNMs. Finding a physician to work under can be especially difficult in rural areas. As one midwife stated, “I have stories of many midwives who have ended up working in Raleigh, or working in Chapel Hill when really they wanted to be working in Henderson, when really they wanted to be working out in the western part of the state.” 403
Additionally, North Carolina does not license CPMs or CMs.404 One CPM lives in North Carolina but drives to South Carolina to practice because of this restriction.405
Furthermore, NC Medicaid reimburses CNMs at a lower rate than OB-GYNs for providing the same services. The current reimbursement rates for select services performed by CNMs and OB-
GYNs are shown in Table 2. This discourages hospitals from employing CNMs.406 It also is an indicator that the state values midwives less than OB-GYNs.
Increasing the scope of practice can improve maternal health outcomes in the state. Compared to OB-GYN care, midwifery-led care is associated with a reduction in unnecessary interventions during labor (e.g., epidural, C-section) and improvements in maternal and infant outcomes.407 Evidence also suggests midwives are associated with an increased likelihood of breastfeeding initiation.408 Midwives may also be an important first step to combat mistreatment felt by women of color in health care spaces. In a seminal study, women of color were less likely to experience mistreatment during maternity care (e.g., verbal abuse, loss of autonomy) when a midwife was the primary prenatal provider as compared to care by OBGYN providers.409
Removing the requirement for CNMs to practice under physicians and certifying CPMs to practice in the state may increase the supply of midwives. In a recent study, states that allowed CNMs to practice autonomously averaged 4.85 CNMs per 1,000 births compared with 2.17 CNMs in states that did allow independent CNM practices.410 North Carolina OB-GYN Society supports removing this requirement, releasing a statement in support in 2017.411 Allowing midwives to practice more autonomously may also help increase the supply of perinatal providers within rural areas of North Carolina.412
NC Medicaid setting the reimbursement rate at parity with the OB-GYN rate is feasible in the short term. NC Medicaid adjusts these rates throughout the year.
Expanding CNMs scope of practice and licensing CPMs is a medium-term solution as both require legislation. CNM legislation has been introduced in previous sessions and is expected to be introduced in future sessions. Highlighting the support of the North Carolina OB-GYN Society will be helpful in pushing through legislation.
NC Medicaid should incentivize PHPs to conduct perinatal mental health screenings.
Implementation:
• NC Medicaid should explicitly include mental health screenings in all three obstetrics bundles.
• NC Medicaid should require well-child care providers to conduct postpartum mental health screenings during the infant’s medical visits for the first year postpartum when the birth mother is present.
More than one in ten women suffer from postpartum depression, and seven in 100 experience depression and/or anxiety during their pregnancy.413 Women with severe forms of depression may commit suicide—a leading cause of maternal mortality.414 Maternal depression is also associated with other risk factors for maternal mortality and morbidity.415 Women of color have a much higher rate of perinatal depression than white women (38 percent v. 13-19 percent).416 Conversely, Black women receive lower levels of treatment for their perinatal mental health condition.
Currently, mental health screenings are not included in the obstetrics service packages. The antepartum service package bundle includes antepartum visits, services, counseling, fetal surveillance testing, and genetic testing case management. The postpartum service package bundle includes exams, contraceptive counseling and contraceptives, and vaccinations.417 The global obstetrics package includes the services in the antepartum and postpartum packages, as well as labor and delivery. Starting in 2018, NC Medicaid allowed obstetrics providers to be reimbursed for three emotional/behavioral assessments in the postpartum period, but these assessments
are not required.418 Additionally, NC Medicaid does not currently allow providers to conduct postpartum mental health screenings for mothers at their infant’s well-child visits.419
NC Medicaid requires PHPs to report both the percentage of deliveries in which members were screened for clinical depression while pregnant and, if positive, received follow-up care.420 While data collection is an important first step, there is more NC Medicaid can do to ensure all Medicaid enrollees, particularly Black mothers, are screened for peripartum mental health conditions and referred to timely and adequate mental health care.
NC Medicaid should include in all three obstetrics bundles a requirement for providers to conduct depression screenings. Screening is the first step in detecting and treating perinatal mental health conditions. After speaking with North Carolina stakeholders, we recommend not tying performance measures to incentive payments because there is a risk providers might select against taking on patients who are more likely to bring their quality metrics down. Therefore, this policy might have the opposite of its intended effect of delivering equitable perinatal care. Performance measures directed at PHPs, however, should be considered. PHPs cannot discriminate against seeing patients in the same way providers can, so tying quality metrics to PHP payments would not result in serious adverse selection issues.
Additionally, NC Medicaid should allow providers to conduct postpartum mental health screenings at the infant’s well-child visits. Based on interviews with stakeholders and a review of research, women with Medicaid are more likely to attend well-child visits than to attend their own postpartum visit. CMS allows states to include maternal depression screenings during a well-child visit as part of the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit.421 EPSDT benefits are not subject to cost-sharing and, if the member requests it, come with scheduling and transportation assistance.422 Many states require providers to
conduct maternal depression screenings as part of the EPSDT well-child visit and reimburse accordingly. North Carolina should adjust their PHP contracts to require—rather than just recommend—coverage of four maternal depression screenings per child under the age of one.423 One drawback of this approach is that children and parents with NC Health Choice are excluded because NC Health Choice does not require EPSDT.
These two recommendations—including mental health screenings in all three obstetrics bundles and requiring maternal mental health screenings during well-child visits—would require a medium-term investment from NC Medicaid. The Medicaid agency would need to update PHP contracts, which according to DHHS employees will happen twice a year starting in 2022.
Implementation:
• NC Medicaid should tie quality metrics in PHP contracts to tobacco cessation, perinatal depression, substance use disorder, and hypertension among pregnant and postpartum women.
NC Medicaid requires PHPs to report two Health Effectiveness Data and Information Set (HEDIS) measures, timeliness of prenatal care and postpartum care, as well as contraceptive care. It requires PHPs to report non-HEDIS measure indicating the percentage of women who had a live birth and were provided a most effective/ moderately effective contraceptive method or long-acting reversible method of contraception within 60 days of delivery.424
During the first two contract years, NC Medicaid will not tie these maternal health quality metrics to provider payment rates. Starting in the third contract year (2023-2024), NC DHHS will withhold payments for certain services that do not meet quality metrics. NC Medicaid will consider overall performance improvement for each plan’s enrolled population relative to other PHPs, as well as the relative improvement in the performance for a group with disparate outcomes when it determines rewards for quality metrics.425
Several North Carolina stakeholders reported that tying quality metrics to payments might exacerbate health inequities. If providers are concerned that their Medicaid payments might decrease, they could be selective in the patients they see; specifically, they might not see patients who are historically associated with poor maternal outcomes.
However, because these payments are tied to PHPs instead of providers, there is a lower risk of adverse selection. According to stakeholder interviews, these incentives may encourage PHPs to ensure enrollees receive adequate treatment for their conditions and specifically support women of color in receiving treatment to reduce racial disparities in care. For example, even when a provider conducts a perinatal depression screening (see Screening of Perinatal Mental Health Conditions recommendation above) and a woman tests positive, there is no accountability to ensure the pregnant or postpartum woman receives adequate treatment. Thus, a large portion of people do not end up receiving treatment. Black women, specifically, are much less likely to be properly screened for depression and receive mental health treatment.426
Quality measures present opportunities to improve maternal health among Medicaid enrollees. The Centers of Medicaid and CHIP Services published a set of recommendations on three focus areas to improve maternal and infant health: i) cesarean section births among women at low-risk for complications, ii) improved postpartum care, and iii) improved well-child visits.427 All the recommended strategies are accompanied by quality measures that can be incorporated into quality improvement systems.
NC Medicaid should consider other perinatal data as additional quality metrics to withhold payments. Other perinatal data could include perinatal depression screening and followups, which PHPs are already required to report. Additionally, PHPs are required to report hypertension, tobacco cessation, and substance use screening and intervention. These outcomes—all of which contribute to maternal mortality and morbidity—should be broken down by pregnancy and postpartum status and considered as quality measures.428
When determining the withhold percent, NC Medicaid has several payment specificities to consider. Some states have robust methods to these calculations with respect to quality measures. For example:
• Louisiana withholds one percent of each MCO monthly capitated payment, which can be earned back if the MCO meets the state-established measure or improves two percentage points from the prior year.429
• Missouri and Ohio withhold three percent of each MCO annual capitated payment, which can be earned back if the MCO meets certain standards on HEDIS measures. High-performing MCOs in Ohio are eligible for an annual bonus, which is funded by an unreturned withheld dollars.430
NC Medicaid’s plan to consider overall and relative performance improvements in disparate outcomes when it determines rewards for quality metrics is promising. Disaggregating the quality measures (hypertension, tobacco cessation, perinatal depression screening and follow-up, and substance use screening and intervention) specifically for pregnant and postpartum women as separate measures to withhold PHP capitation payments would incentivize PHPs to improve maternal health outcomes but requires a medium-term investment from NC Medicaid. NC Medicaid cannot withhold payments until 2023. Additionally, NC Medicaid would need to analyze the disaggregated data submitted by PHPs in order to confirm that there have been recent and consistent racial and ethnic disparities among these quality metrics.
NC Medicaid should reduce administrative burdens that keep pregnant and postpartum enrollees from enrolling in Medicaid.
Implementation:
• NC Medicaid should create a shortened Medicaid enrollment form specifically for pregnancy Medicaid.
• NC Medicaid should pursue a State Plan Amendment to exempt under 21 pregnant people from income determination for pregnancy Medicaid.
Implementation:
• NC Medicaid should incentivize PHPs to reduce wait times for translation services during perinatal appointments and increase access to translation services through telehealth.
Much of the administrative side of NC Medicaid happens at county health departments, making for unique management challenges in easing administrative burdens for Medicaid enrollees. North Carolinians may apply to Medicaid by phone, paper application, in-person, or online. A simplified web application is available across the state in English and Spanish through ePass offered by NC Medicaid.
Administrative burdens present a barrier for potential enrollees to access benefits and care. Data from NC DHHS suggests that some pregnancy Medicaid enrollees do not enroll until relatively late in their pregnancy. In 2019,
56 percent of pregnancy Medicaid enrollees received care during their first trimester, with significant disparities between racial and ethnic groups: when disaggregated by race, 65 percent of non-Hispanic white enrollees received first trimester care, while the rate of first trimester care was 58 percent and 52 percent for nonHispanic Black enrollees and Hispanic enrollees, respectively.431
Looking at the state overall, there is a disconnect between Medicaid enrollees and poverty rates (see Figures 12 and 13). Despite the higher poverty rates in the eastern region of the state, pregnancy Medicaid enrollment is lower than in the west. These data suggest there may be Medicaid-eligible pregnant women in the eastern part of the state that never enroll in coverage.
NC Medicaid has made progress on easing administrative burden by starting to reimburse for translation services used by enrollees during appointments. However, language inaccessibility was identified in our stakeholder interviews as a barrier to maternal care. A 2021 study of Spanish-speaking pregnant women in North Carolina found that patients who do not speak English have longer appointment wait times due to the time needed to find a translator.432 In a focus group conducted as part of this study, women reported that care centers did not provide sufficient interpreters and sometimes relied on the enrollee’s family members to interpret during appointments.433

Easing administrative burden offers a chance to reduce disparities and increase Medicaid enrollment for eligible pregnant people. The White House identified administrative burden as a key priority in increasing equitable outcomes through social safety net programs. Their 2021 report offers an application design framework, which NC Medicaid should consider in streamlining pregnancy Medicaid applications (see Table 3).
By using plain language and clear step-bystep instructions, NC Medicaid can increase pregnancy Medicaid enrollment and reduce geographic, racial, and ethnic disparities. The most recent available data on pregnancy Medicaid enrollment processes shows 25 states use shortened Medicaid enrollment forms.434
Exempting people under 21 from pregnancy Medicaid income determination will further reduce hurdles for accessing coverage. California and New York have enacted this policy in their Medicaid programs through State Plan Amendments.435 Given there are racial age disparities for when pregnant Medicaid enrollees give birth in North Carolina, pursuing this recommendation could reduce racial and ethnic disparities by making it easier for younger enrollees to access pregnancy Medicaid coverage. In 2019, Medicaid enrollees under 18 had 1,484 births, about 2.3 percent of all births covered by Medicaid. For all Black non-Hispanic Medicaid enrollee births, 2.5 percent were to those under 18 and for all Hispanic enrollee births, 3.3 percent were to those under 18.436

Reducing form complexity and improving comprehensibility
• Lengthy forms and instructions driven by legal design requirements.
• Questions that cannot be answered based purely on an applicant’s own memory or knowledge about themselves.
• Multiple or supplemental forms during a single application experience.
• Eligibility requirements that are overly complex and not well known.
• Ensure that all instructions and notices are written in plain language and translated into multiple languages.
• Adopt principles of human-centered design (e.g., early and routine user interviews and A/B testing to continually refine design and language).
• Provide step-by-step examples of process involved in claiming benefits, accessing protections, or navigating a service.
Pursuing a State Plan Amendment requires legislative action, and therefore it is a mediumterm solution to reduce administrative burden for under 21 enrollees. In comparison, creating a shortened application form and improving translation services act are short-term solutions because both can be implemented without legislative action.
To ensure that enrollees have access to timely translation services, NC Medicaid should provide financial rewards to PHPs that achieve shorter wait times for enrollees, though all translation services to continue to be reimbursed at a base level regardless of wait times. NC Medicaid should also work with PHPs to expand access to translation services provided through telehealth during enrollee appointments, particularly in areas with translator shortages or for enrollees who speak less commonly spoken languages. These are relatively short-term solutions, as these changes can be made by altering PHP contracts.
North Carolina Medicaid is a leader in innovative approaches to health care delivery and addressing non-medical drivers of health. The ongoing transition to Medicaid Managed Care represents an opportunity for the state to bring comprehensive, quality health care to enrollees who face barriers to care because of social determinants of health such as race, ethnicity, primary language, and rural residence.
This report specifically addresses the challenges of enrollees with SCD and who are pregnant or postpartum. These ubiquitous challenges relate to churn, provider supply, care management, transportation, and data gaps. For SCD enrollees, challenges relate to continuity of care during the pediatric to adult transition and lack of universal screenings. Pregnant and postpartum enrollees face challenges related to continuity of care across the peripartum period and lack of clinical and non-clinical support.
The recommendations in this report were determined after four months of research, including 22 interviews with North Carolina stakeholders and a review of academic literature and evaluations of other states’ policies. We hope this report helps NC Medicaid succeed in fulfilling the promise of managed care, especially with respect to addressing the inequities in SCD and maternal health outcomes.

The following visualization depicts how our recommendations vary based on their estimated costs (time, information technology, and personnel), equity implications, and stakeholder support (see the legend below for specifics). These determinations were made based on background research and stakeholder interviews. The purpose of this matrix is to summarize the high-level implications of our recommendations, and ultimately help NC DHHS prioritize the recommendations.
Matrix Legend
Short/Medium/Long Term:
ST
NC DHHS can implement quickly/without additional funds
MT NC DHHS can implement over a few years/with additional funds
LT NC DHHS can implement over a few years/with new legal authority
Requires Legal Authority:
No Does not require legislation
Yes Does require legislation
Stakeholder Support:
Almost universal agreement among stakeholders that this was a priority
Some agreement among stakeholders that this was a priority
No agreement among stakeholders that this was a priority
Equity Implications:
Addresses equity
Is neutral on equity
Works against equity
Initial Costs to the State:
Has small cost (less than $100,000)
Has a moderate cost (approximately $100,000 - $500,000)
Has a significant cost
Administrative Capacity:
Requires only a few people
Requires a moderate number of people and/or IT resources
Requires a significant number of people and/or IT resources
1 “NC DPH: N.C. Sickle Cell Syndrome Program,” accessed December 7, 2021, https://www.ncsicklecellprogram.org/.
2 “Value-Based Payment for Maternity Care in Medicaid: Findings from Five States” (MACPAC, September 2021), https:// www.macpac.gov/wp-content/uploads/2021/09/Value-Based-Payment-for-Maternity-Care-in-Medicaid-Findingsfrom-Five-States.pdf.
3 “Proposed Program Design,” NCDHHS, n.d., https://www.ncdhhs.gov/proposed-program-design.
4 “Introduction to COVID-19 Racial and Ethnic Health Disparities,” CDC, n.d., https://www.cdc.gov/coronavirus/2019ncov/community/health-equity/racial-ethnic-disparities/index.html.
5 “North Carolina’s Transformation to Medicaid Managed Care,” NC Medicaid, n.d., https://medicaid.ncdhhs.gov/ transformation.
6 “QuickFacts: North Carolina,” United States Census Bureau, n.d., https://www.census.gov/quickfacts/NC.
7 “QuickFacts: North Carolina.”
8 “QuickFacts: North Carolina.”
9 “About Sickle Cell Disease,” Genome.gov, accessed December 5, 2021, https://www.genome.gov/Genetic-Disorders/ Sickle-Cell-Disease.
10 Sophie Lanzkron, C. Patrick Carroll, and Carlton Haywood, “The Burden of Emergency Department Use for Sickle Cell Disease: An Analysis of the National Emergency Department Sample Database,” American Journal of Hematology 85, no. 10 (2010): 797–99.
11 “About Sickle Cell Disease.”
12 Community Care of North Carolina, “Sickle Cell Program,” Community Care of North Carolina, 2021, https://www. communitycarenc.org/what-we-do/care-management/population-health-outreach-and-care-coordination/sickle-cellprogram.
13 S. Wilson-Frederick et al., “Medicaid and CHIP Sickle Cell Disease Report, T-MSIS Analytic Files (TAF) 2017,” Center for Medicaid and CHIP Services, Dvivision of Quality and Health Outcomes, Centers for Medicare & Medicaid Services, January 2021, https://www.medicaid.gov/medicaid/quality-of-care/downloads/scd-rpt-jan-2021.pdf.
14 CDC, “Incidence of Sickle Cell Trait in the US | CDC,” Centers for Disease Control and Prevention, May 4, 2018, https://www.cdc.gov/ncbddd/sicklecell/features/keyfinding-trait.html.
15 “About Sickle Cell Disease,” National Human Genome Research Institute, n.d., https://www.genome.gov/GeneticDisorders/Sickle-Cell-Disease.
16 “About Sickle Cell Disease.”
17 Courtney Fitzhugh et al., “Morbidity and Associated Sudden Death in Sickle Cell Disease,” Blood 106, no. 11 (2005): 2348.
18 Bianca Nogrady, “Why Severe Sickle-Cell Pain Has Been Neglected,” Nature 596, no. 7873 (2021): S10–12; “About Sickle Cell Disease”; Amanda Friend and Daniel Girzadas, “Acute Chest Syndrome,” in StatPearls (Treasure Island (FL): StatPearls Publishing, 2021).
19 “Longevity for Those with Sickle Cell Disease Linked to Care Maintenance, Family Involvement,” American Society of Hematology, accessed December 5, 2021, https://www.hematology.org:443/newsroom/press-releases/2016/rarepatients-with-sickle-cell-disease-live-nearly-twice-as-long-as-average.
20 H. Joanna Jiang, Marguerite L. Barrett, and Minya Sheng, “Characteristics of Hospital Stays for Nonelderly Medicaid Super-Utilizers, 2012: Statistical Brief #184,” in Healthcare Cost and Utilization Project (HCUP) Statistical Briefs (Rockville (MD): Agency for Healthcare Research and Quality (US), 2006), http://www.ncbi.nlm.nih.gov/books/ NBK269028/.
21 Deepika S. Darbari and Amanda M. Brandow, “Pain-Measurement Tools in Sickle Cell Disease: Where Are We Now?,” Hematology 2017, no. 1 (2017): 534–41.
22 Santosh L. Saraf et al., “Improved Health Care Utilization and Costs in Transplanted versus Non-Transplanted Adults with Sickle Cell Disease,” PLOS ONE 15, no. 2 (2020): e0229710.
23 NCDHHS, “North Carolina Sickle Cell Syndrome Program,” NCDHHS, September 18, 2020, https://www. ncsicklecellprogram.org/.
24 Eugene Declercq and Laurie Zephyrin, “Severe Maternal Morbidity in the United States: A Primer,” The Commonwealth Fund, Data Brief, October 28, 2021.
25 Declercq and Zephyrin.
26 Maria J. Small et al., “Addressing Maternal Deaths in North Carolina: Striving to Reach Zero,” North Carolina Medical Journal 81, no. 1 (2020): 55–62.
27 Small et al.
28 Declercq and Zephyrin, “Severe Maternal Morbidity in the United States.”
29 Small et al., “Addressing Maternal Deaths in North Carolina.”
30 Eugene Declercq and Laurie Zephyrin, “Maternal Mortality in the United States: A Primer,” The Commonwealth Fund, Data Brief, December 2020.
31 “Report from Nine Maternal Mortality Review Committees” (Centers for Disease Control and Prevention, 2019).
32 Cecilia Nowell, “Homicide Is a Leading Cause of Death in Pregnant People, a New Study Finds. Black Women Are at Greatest Risk.,” The Lily, December 6, 2021, https://www.thelily.com/homicide-is-a-leading-cause-of-death-inpregnant-people-a-new-study-finds-black-women-are-at-greatest-risk/.
33 “Temporary Clinical Policy Modifications: Payment for Healthy Opportunities Screening and Referral,” NC Medicaid, February 1, 2021, https://medicaid.ncdhhs.gov/blog/2021/02/01/temporary-clinical-policy-modifications-paymenthealthy-opportunities-screening-and.
34 Rhitu Chatterjee, “Premature Birth Rates Rise Again, But A Few States Are Turning Things Around,” NPR, November 1, 2018, https://www.npr.org/sections/health-shots/2018/11/01/662683176/premature-birth-rates-rise-again-but-afew-states-are-turning-things-around.
35 Elizabeth A. Howell, “Reducing Disparities in Severe Maternal Morbidity and Mortality,” Clinical Obstetrics & Gynecology 61, no. 2 (June 2018): 387–99.
36 Lauren Jansen et al., “First Do No Harm: Interventions During Childbirth,” The Journal of Perinatal Education 22, no. 2 (2013): 83–92.
37 Gray Babbs, Lois McCloskey, and Sarah H. Gordon, “Expanding Postpartum Medicaid Benefits to Combat Maternal Mortality and Morbidity,” Health Affairs Blog, January 14, 2021.
38 Declercq and Zephyrin, “Maternal Mortality in the United States.”
39 Roy Ahn et al., “Initiatives to Reduce Maternal Mortality and Severe Maternal Morbidity in the United States,” Annals of Internal Medicine 173, no. 11_Supplement (2020): S3–10.
40 Annie Waldman, “How Hospitals Are Failing Black Mothers,” ProPublica, December 27, 2017, https://www.propublica. org/article/how-hospitals-are-failing-black-mothers.
41 Elizabeth A. Howell et al., “Race and Ethnicity, Medical Insurance, and Within-Hospital Severe Maternal Morbidity Disparities,” Obstetrics and Gynecology 135, no. 2 (2020): 285–93.
42 Small et al., “Addressing Maternal Deaths in North Carolina.”
43 “Black Women’s Maternal Health: A Multifaceted Approach to Addressing Persistent and Dire Health Disparities,” Issue Brief, Black Maternal Health (National Partnership for Women & Families, n.d.), http://www.nationalpartnership org/our-work/health/reports/black-womens-maternal-health.html.
44 Declercq and Zephyrin, “Severe Maternal Morbidity in the United States.”
45 David R. Williams, Jourdyn A. Lawrence, and Brigette A. Davis, “Racism and Health: Evidence and Needed Research,” Annual Review of Public Health 40, no. 1 (2019): 105–25; Yin Paradies et al., “Racism as a Determinant of Health: A Systematic Review and Meta-Analysis,” PLoS ONE 10, no. 9 (2015): e0138511, https://doi.org/10.1371/ journal.pone.0138511.
46 Kelly M. Hoffman et al., “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs About Biological Differences Between Blacks and Whites,” Proceedings of the National Academy of Sciences 113, no. 16 (2016): 4296–4301.
47 Keith Wailoo, Dying in the City of the Blues: Sickle Cell Anemia and the Politics of Race and Health (University of North Carolina Press, 2001).
48 Hoffman et al., “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs About Biological Differences Between Blacks and Whites.”
49 Sophie Trawalter and Kelly M. Hoffman, “Got Pain? Racial Bias in Perceptions of Pain,” Social and Personality Psychology Compass 9, no. 3 (2015): 146–57.
50 Keith Wailoo and Stephen Pemberton, The Troubled Dreams of Genetic Medicine (Johns Hopkins University Press, 2006).
51 Deborah Lubeck et al., “Estimated Life Expectancy and Income of Patients With Sickle Cell Disease Compared With Those Without Sickle Cell Disease,” JAMA Network Open 2, no. 11 (2019): e1915374.
52 Faheem Farooq et al., “Comparison of US Federal and Foundation Funding of Research for Sickle Cell Disease and Cystic Fibrosis and Factors Associated With Research Productivity,” JAMA Network Open 3, no. 3 (2020): e201737
53 Carlton Haywood et al., “A Systematic Review of Barriers and Interventions to Improve Appropriate Use of Therapies for Sickle Cell Disease,” Journal of the National Medical Association 101, no. 10 (October 2009): 1022–33.
54 Wailoo and Pemberton, The Troubled Dreams of Genetic Medicine.
55 Deirdre Cooper Owens and Sharla M. Fett, “Black Maternal and Infant Health: Historical Legacies of Slavery,” American Journal of Public Health 109, no. 10 (2019): 1342–45, https://doi.org/10.2105/AJPH.2019.305243.
56 Owens and Fett.
57 Harriet A. Washington, Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present (Doubleday Books, 2006).
58 Waldman, “How Hospitals Are Failing Black Mothers.”
59 Declercq and Zephyrin, “Maternal Mortality in the United States.”
60 A. T. Geronimus, “The Weathering Hypothesis and the Health of African-American Women and Infants: Evidence and Speculations,” Ethnicity & Disease 2, no. 3 (1992): 207–21.
61 Linda Villarosa, “Why America’s Black Mothers and Babies Are in a Life-or-Death Crisis,” The New York Times, April 11, 2018, https://www.nytimes.com/2018/04/11/magazine/black-mothers-babies-death-maternal-mortality.html.
62 Villarosa.
63 Nada Alayed et al., “Sickle Cell Disease and Pregnancy Outcomes: Population-Based Study on 8.8 Million Births,” Journal of Perinatal Medicine 42, no. 4 (July 2014): 487–92, https://doi.org/10.1515/jpm-2013-0275.
64 Silvia P. Canelón, Samantha Butts, and Mary Regina Boland, “Evaluation of Stillbirth Among Pregnant People With Sickle Cell Trait,” JAMA Network Open 4, no. 11 (November 24, 2021): e2134274, https://doi.org/10.1001/ jamanetworkopen.2021.34274.
65 P. Braveman et al., “What Is Health Equity? A Definition and Discussion Guide,” Robert Wood Johnson Foundation, May 1, 2017, https://www.rwjf.org/en/library/research/2017/05/what-is-health-equity-.html.
66 Sanne Magnan, “Social Determinants of Health 101 for Health Care: Five Plus Five,” National Academy of Medicine Perspectives, 2017, https://doi.org/10.31478/201710c.
67 “Health Equity Payment Initiative | NC Medicaid,” March 19, 2021, https://medicaid.ncdhhs.gov/blog/2021/03/19/ health-equity-payment-initiative.
68 Clarissa Donnelly-DeRoven, “Three Months into Medicaid Transformation, Providers Say the New Administrative Burdens Are Crushing,” North Carolina Health News, October 19, 2021, http://www.northcarolinahealthnews. org/2021/10/19/three-months-into-medicaid-transformation-providers-say-the-new-administrative-burdens-arecrushing/.
69 “Fact Sheet Introduction to Medicaid Transformation: Part 1 - Overview,” NC Medicaid 2021 Provider Playbook (NC Department of Health and Human Services, June 2021).
70 “Beneficiaries,” NC Medicaid, Division of Health Benefits, n.d., https://medicaid.ncdhhs.gov/beneficiaries.
71 Donnelly-DeRoven, “Three Months into Medicaid Transformation, Providers Say the New Administrative Burdens Are Crushing.”
72 “Joint Legislative Oversight Committee on Medicaid and NC Health Choice,” North Carolina General Assembly, n.d., https://www.ncleg.gov/Committees/CommitteeInfo/NonStanding/6660; Anne Blythe et al., “COVID Funds Beef up Health Care Spending in Proposed State Budget, Which Still Lacks Medicaid Expansion,” NC Health News, November 17, 2021, https://www.northcarolinahealthnews.org/2021/11/17/covid-funds-beef-up-health-carespending-in-proposed-state-budget-still-lacks-medicaid-expansion/.
73 Solomon, Judith, and Tara Straw. 2021. “Build Back Better Increases Health Coverage and Makes It More Affordable.” Center on Budget and Policy Priorities. https://www.cbpp.org/research/health/build-back-betterincreases-health-coverage-and-makes-it-more-affordable.
74 Declercq, Eugene, and Laurie Zephyrin. 2020. “Maternal Mortality in the United States: A Primer.” The Commonwealth
Fund. https://www.commonwealthfund.org/publications/issue-brief-report/2020/dec/maternal-mortality-united-statesprimer.
75 Trends in Maternal Mortality Statistics.” 2019. North Carolina Department of Health and Human Services. https://schs. dph.ncdhhs.gov/data/maternal/.
76 “Enrollment Dashboard | NC Medicaid,” NC Department of Health and Human Services Division of Health Benefits, accessed December 7, 2021, https://medicaid.ncdhhs.gov/reports/dashboards#enroll.
77 Logan Rockefeller Harris, Mel Umbarger, and Suzy Khachaturyan, “U.S. Census Bureau Releases Data on Health Insurance Coverage in N.C.,” North Carolina Justice Center (blog), September 15, 2020, https://www.ncjustice.org/us-census-bureau-releases-data-on-health-insurance-coverage-in-n-c/.
78 Mandy Cohen, “Governor’s Recommended Budget, 2021-23 - NC Department of Health and Human Services,” 2021, 24.
79 Laura Benzing and Cynthia Doug, “Churn Patterns in Adult Medicaid Beneficiaries from North Carolina: 2016-2020” (Duke University Margolis Center for Health Policy, 2021), https://healthpolicy.duke.edu/sites/default/files/2021-05/ Churn%20Adults%20Fact%20Sheet.pdf.
80 Benzing and Doug.
81 CDC, “Medicaid Coverage Patterns for People with SCD,” Centers for Disease Control and Prevention, March 24, 2021, https://www.cdc.gov/ncbddd/hemoglobinopathies/scdc-fact-sheet-medicaid-data.html.
82 Madeline Guth, Rachel Garfield, and Robin Rudowitz, “The Effects of Medicaid Expansion under the ACA: Studies from January 2014 to January 2020,” Kaiser Family Foundation (blog), March 17, 2020, https://www.kff.org/medicaid/ report/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review/.
83 Madeline Guth, Rachel Garfield, and Robin Rudowitz.
84 Erica L. Eliason, “Adoption of Medicaid Expansion Is Associated with Lower Maternal Mortality,” Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health 30, no. 3 (2020): 147–52, https://doi. org/10.1016/j.whi.2020.01.005.
85 Julie Kanter et al., “Building Access to Care in Adult Sickle Cell Disease: Defining Models of Care, Essential Components, and Economic Aspects,” Blood Advances 4, no. 16 (2020): 3804–13.
86 Kanter et al.
87 “North Carolina Health Professional Supply Data,” Sheps Health Workforce NC, accessed December 7, 2021, https:// nchealthworkforce.unc.edu/interactive/supply/; National Center on Birth Defects and Developmental Disabilities, Division of Blood Disorders, “Sickle Cell Disease in North Carolina” (CDC), accessed December 7, 2021, https:// www.cdc.gov/ncbddd/sicklecell/documents/scd_in_nc_providers.pdf.
88 Kanter et al., “Building Access to Care in Adult Sickle Cell Disease: Defining Models of Care, Essential Components, and Economic Aspects”; Alyssa M. Schlenz et al., “Needs Assessment for Patients with Sickle Cell Disease in South Carolina, 2012,” Public Health Reports (Washington, D.C.: 1974) 131, no. 1 (2016): 108–16; Kristen J. Alston et al., “Experiences of Pediatric Patients with Sickle Cell Disease in Rural Emergency Departments,” Journal of Pediatric Hematology/Oncology 37, no. 3 (2015): 195–99.
89 P Bradt et al., “Crizanlizumab, Voxelotor, and L-Glutamine for Sickle Cell Disease: Effectiveness and Value,” Evidence Report (Institute for Clinical and Economic Review, February 9, 2021), https://icer-review.org/material/sickle-celldisease-draft-evidence-report/.
90 Matthew P. Smeltzer et al., “Identifying Barriers to Evidence-Based Care for Sickle Cell Disease: Results from the Sickle Cell Disease Implementation Consortium Cross-Sectional Survey of Healthcare Providers in the USA,” BMJ Open 11, no. 11 (2021): e050880.
91 Sophie Lanzkron et al., “Impact of a Dedicated Infusion Clinic for Acute Management of Adults with Sickle Cell Pain Crisis,” American Journal of Hematology 90, no. 5 (2015): 376–80; Givi Basishvili et al., “Comprehensive Management Reduces Incidence and Mortality of Acute Chest Syndrome in Patients with Sickle Cell Disease,” American Journal of Hematology 93, no. 3 (2018): E64–67; Michael R. DeBaun, “The Challenge of Creating an
Evidence-Based Guideline for Sickle Cell Disease,” JAMA 312, no. 10 (2014): 1004–5; Kathryn L. Koch et al., “Intensive Management of High-Utilizing Adults with Sickle Cell Disease Lowers Admissions,” American Journal of Hematology 90, no. 3 (2015): 215–19; Y M Yang et al., “Comparison of Costs to the Health Sector of Comprehensive and Episodic Health Care for Sickle Cell Disease Patients.,” Public Health Reports 110, no. 1 (1995): 80–86.
92 Monica Ter-Minassian et al., “Quality Metrics and Health Care Utilization for Adult Patients with Sickle Cell Disease,” Journal of the National Medical Association 111, no. 1 (2019): 54–61; Barbara P. Yawn et al., “Management of Sickle Cell Disease: Summary of the 2014 Evidence-Based Report by Expert Panel Members,” JAMA 312, no. 10 (September 10, 2014): 1033, https://doi.org/10.1001/jama.2014.10517.
93 Kanter et al., “Building Access to Care in Adult Sickle Cell Disease: Defining Models of Care, Essential Components, and Economic Aspects.”
94 “Improving Access to Maternal Health Care in Rural Communities | CMS” (Centers for Medicare & Medicaid Services, September 3, 2019). (p16)
95 Cecil G. Sheps Center for Health Services Research, “North Carolina Health Professional Supply Data,” Cecil G. Sheps Center for Health Services Research, December 7, 2021.
96 Liora Engel-Smith, “When a Rural Maternity Unit Closes, Alternatives Are Hard to Come By,” North Carolina Health News, February 24, 2020, http://www.northcarolinahealthnews.org/2020/02/24/when-rural-maternity-units-closealternatives-are-hard-to-come-by/.
97 Carolina Public Press, North Carolina Health News September 29, and 2017, “Mountain Maternity Wards Closing, WNC Women’s Lives on the Line,” North Carolina Health News, September 29, 2017, http://www. northcarolinahealthnews.org/2017/09/29/mountain-maternity-wards-closing-wnc-womens-lives-on-the-line/.
98 Engel-Smith, “When a Rural Maternity Unit Closes, Alternatives Are Hard to Come By.”
99 “Turning Point: Improving the Care of Young Adults With Sickle Cell Disease,” accessed December 7, 2021, https:// muschealth.org/health-professionals/progressnotes/2017/spring/features/sickle-cell-disease.
100 “Turning Point.”
101 Kanter et al., “Building Access to Care in Adult Sickle Cell Disease: Defining Models of Care, Essential Components, and Economic Aspects.”
102 Kanter et al.
103 “Improving Access to Maternal Health Care in Rural Communities | CMS.”
104 “Improving Access to Maternal Health Care in Rural Communities | CMS.”
105 Liora Engel-Smith, North Carolina Health News April 9, and 2020, “Initiative Aims to Connect Patients to Addiction Treatment by Building Better Networks,” North Carolina Health News, April 9, 2020, http://www. northcarolinahealthnews.org/2020/04/09/opioid-addiction-hub-and-spoke/.
106 Engel-Smith, April 9, and 2020.
107 Engel-Smith, April 9, and 2020.
108 Engel-Smith, April 9, and 2020.
109 “Healthy Blue Member Handbook: NC Medicaid Managed Care,” June 2021, https://www.healthybluenc.com/northcarolina/ncnc_caid_memberhandbook_eng.pdf. (p39)
110 “NC Medicaid Managed Care Member Handbook” (Carolina Complete Health, July 2021). (p39)
111 “AmeriHealth NC Medicaid Managed Care Member Handbook” (AmeriHealth Caritas, August 2021); “NC Medicaid Managed Care Member Handbook”; “Healthy Blue Member Handbook: NC Medicaid Managed Care”; “UnitedHealthcare NC Medicaid Managed Care Member Handbook” (UnitedHealthcare Community Plan of North Carolina, March 2021); “WellCare of North Carolina - NC Medicaid Managed Care Member Handbook” (WellCare of North Carolina, July 2021); “Revised and Restated Request for Proposal #: 30-190029-DHB Prepaid Health Plan Services” (State of North Carolina, Department of Health and Human Services Division of Health Benefits, January 25, 2019).
112 “AmeriHealth NC Medicaid Managed Care Member Handbook”; “NC Medicaid Managed Care Member Handbook”; “Healthy Blue Member Handbook: NC Medicaid Managed Care”; “UnitedHealthcare NC Medicaid Managed Care Member Handbook”; “WellCare of North Carolina - NC Medicaid Managed Care Member Handbook”; “Revised and
Restated Request for Proposal #: 30-190029-DHB Prepaid Health Plan Services.”
113 MACPAC, “Chapter 5 Mandated Report on Non-Emergency Medical Transportation,” June 2021, 45. (p20)
114 “Rural Health for North Carolina Overview - Rural Health Information Hub,” accessed December 8, 2021, https:// www.ruralhealthinfo.org/states/north-carolina.
115 MACPAC, “Chapter 5 Mandated Report on Non-Emergency Medical Transportation.” (p9)
116 Laura Fraade-Blanar, Tina Koo, and Christopher M Whaley, “Going to the Doctor: Rideshare as Nonemergency Medical Transportation,” n.d., 52. (p27)
117 Fraade-Blanar, Koo, and Whaley. (p15)
118 Fraade-Blanar, Koo, and Whaley. (p15)
119 FierceHealthcare, “Modernizing Medical Transportation with Rideshare” (FierceHealthcare, 2020).
120 Sharon Silow-Carroll et al., “Medicaid’s Non-Emergency Medical Transportation Benefit: Stakeholder Perspectives on Trends, Challenges, and Innovations” (MACPAC, August 2021). (p13)
121 Silow-Carroll et al. (p13)
122 Rita Vanessa Masese et al., “Barriers and Facilitators to Care for Individuals with Sickle Cell Disease in Central North Carolina: The Emergency Department Providers’ Perspective,” PloS One 14, no. 5 (2019): e0216414, https://doi. org/10.1371/journal.pone.0216414; “Healthy Moms, Healthy Babies: Building a Risk-Appropriate Perinatal System of Care for North Carolina” (North Carolina Institute of Medicine, April 2020), 15, https://nciom.org/wp-content/ uploads/2020/04/Perinatal-Report-FINAL.pdf.
123 Rita Vanessa Masese et al., “Barriers and Facilitators to Care for Individuals with Sickle Cell Disease in Central North Carolina: The Emergency Department Providers’ Perspective,” PloS One 14, no. 5 (2019): e0216414, https://doi. org/10.1371/journal.pone.0216414.
124 Michelle van Ryn and Jane Burke, “The Effect of Patient Race and Socio-Economic Status on Physicians’ Perceptions of Patients,” Social Science & Medicine 50, no. 6 (2000): 813–28; V N Gamble, “Under the Shadow of Tuskegee: African Americans and Health Care.,” American Journal of Public Health 87, no. 11 (1997): 1773–78.
125 Katrina Armstrong et al., “Prior Experiences of Racial Discrimination and Racial Differences in Health Care System Distrust,” Medical Care 51, no. 2 (February 2013): 144–50, https://doi.org/10.1097/MLR.0b013e31827310a1.
126 Carlton Haywood et al., “Perceived Discrimination in Health Care Is Associated with a Greater Burden of Pain in Sickle Cell Disease,” Journal of Pain and Symptom Management 48, no. 5 (November 2014): 934–43, https://doi. org/10.1016/j.jpainsymman.2014.02.002; Carlton Haywood et al., “The Impact of Race and Disease on Sickle Cell Patient Wait Times in the Emergency Department,” The American Journal of Emergency Medicine 31, no. 4 (2013): 651–56, https://doi.org/10.1016/j.ajem.2012.11.005; Jeffrey Glassberg et al., “Among Emergency Physicians, Use of the Term ‘Sickler’ Is Associated with Negative Attitudes toward People with Sickle Cell Disease,” American Journal of Hematology 88, no. 6 (2013): 532–33; Cynthia B. Sinha et al., “Management of Chronic Pain in Adults Living With Sickle Cell Disease in the Era of the Opioid Epidemic: A Qualitative Study,” JAMA Network Open 2, no. 5 (2019): e194410; Daniel Sop et al., “Survey of Physician Perspective towards Management of Pain for Chronic Conditions in the Emergency Department,” Modern Clinical Medicine Research 1 (2017).
127 Sinha et al., “Management of Chronic Pain in Adults Living With Sickle Cell Disease in the Era of the Opioid Epidemic.”
128 Sinha et al.; Darbari and Brandow, “Pain-Measurement Tools in Sickle Cell Disease”; Amanda M. Brandow et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease: Management of Acute and Chronic Ppain,” Blood Advances 4, no. 12 (2020): 2656–2701; Sop et al., “Survey of Physician Perspective towards Management of Pain for Chronic Conditions in the Emergency Department”; Samir K. Ballas et al., “Opioid Utilization Patterns in United States Individuals with Sickle Cell Disease,” American Journal of Hematology 93, no. 10 (2018): E345–47.
129 Sinha et al., “Management of Chronic Pain in Adults Living With Sickle Cell Disease in the Era of the Opioid Epidemic.”
130 Michael C. Lu et al., “Closing the Black-White Gap in Birth Outcomes: A Life-Course Approach,” Ethnicity & Disease 20, no. 1 0 2 (2010): S2-62–76.
131 Cynthia Gyamfi-Bannerman et al., “Postpartum Hemorrhage Outcomes and Race,” American Journal of Obstetrics and Gynecology 219, no. 2 (2018): 185.e1-185.e10, https://doi.org/10.1016/j.ajog.2018.04.052; “Healthy Moms, Healthy Babies: Building a Risk-Appropriate Perinatal System of Care for North Carolina.”
132 “State Policies to Improve Maternal Health Outcomes,” Commonwealth Fund, November 19, 2021, https://www. commonwealthfund.org/publications/maps-and-interactives/2020/nov/state-policies-improve-maternal-healthoutcomes.
133 “Bill Text - SB-464 California Dignity in Pregnancy and Childbirth Act.,” October 8, 2019, https://leginfo.legislature. ca.gov/faces/billTextClient.xhtml?bill_id=201920200SB464.
134 Jonathan Y. Siden et al., “Reducing Implicit Bias in Maternity Care: A Framework for Action,” Women’s Health Issues, 2021.
135 Stephanie Teleki, “Challenging Providers To Look Within Themselves: A New Tool To Reduce Bias In Maternity Care | Health Affairs Blog,” Health Affairs, July 6, 2021, https://www.healthaffairs.org/do/10.1377/hblog20210630.980773/ full/.
136 “Healthy Moms, Healthy Babies: Building a Risk-Appropriate Perinatal System of Care for North Carolina”; Stephanie Teleki, “Challenging Providers To Look Within Themselves.”
137 “FAQs for Implicit Bias Training” (Michigan Department of Licensing and Regulatory Affairs, September 24, 2021), https://www.michigan.gov/documents/lara/Implicit_Bias_FAQs_FINAL_7.22.2021_731300_7.pdf.
138 “About Healthy Opportunities,” NC DHHS, n.d., https://www.ncdhhs.gov/about/department-initiatives/healthyopportunities/about-healthy-opportunities.
139 “Healthy Opportunities,” NC DHHS, n.d., https://www.ncdhhs.gov/about/department-initiatives/healthy-opportunities.
140 “North Carolina Creates Nation’s First Statewide Infrastructure Connecting Healthcare and Human Services | NC Gov. Cooper,” accessed February 6, 2022, https://governor.nc.gov/news/north-carolina-createsnation%E2%80%99s-first-statewide-infrastructure-connecting-healthcare-and-human.
141 Zachary Wortman, Elizabeth Cuervo Tilson, and Mandy Krauthamer Cohen, “Buying Health For North Carolinians: Addressing Nonmedical Drivers Of Health At Scale,” Health Affairs 39, no. 4 (April 1, 2020): 649–54, https://doi. org/10.1377/hlthaff.2019.01583.
142 “North Carolina Nonprofit Organizations and the Impacts of COVID-19” (North Carolina Office of Strategic Partnerships and The Policy Lab at Brown University, September 2020), https://files.nc.gov/ncosbm/documents/files/ NC-Nonprofits-COVID-Survey-Results-2020.pdf.
143 Alexandra Power-Hays et al., “Universal Screening for Social Determinants of Health in Pediatric Sickle Cell Disease: A Quality-Improvement Initiative,” Pediatric Blood & Cancer 67, no. 1 (January 2020): e28006, https://doi. org/10.1002/pbc.28006.
144 Power-Hays et al.
145 Daniel B. Nelson, Michelle H. Moniz, and Matthew M. Davis, “Population-Level Factors Associated with Maternal Mortality in the United States, 1997–2012,” BMC Public Health 18, no. 1007 (December 2018), https://doi. org/10.1186/s12889-018-5935-2.
146 Cavaliere, B. N., Martin, K. S., Smith, M., & Hake, M., “Key Drivers to Improve Food Security and Health Outcomes: An Evidence Review of Food Bank - Health Care Partnerships and Related Interventions.” (Feeding America, 2021).
147 Rebecca O’Reilly, Barbara Beale, and Donna Gillies, “Screening and Intervention for Domestic Violence During Pregnancy Care: A Systematic Review,” Trauma, Violence, & Abuse 11, no. 4 (October 1, 2010): 190–201, https:// doi.org/10.1177/1524838010378298.
148 “Amendment Number 3/4 Prepaid Health Plan Services #30-190029-DHB – PHP Name” (NC Department of Health and Human Services, n.d.), https://medicaid.ncdhhs.gov/media/9087/download.
149 “Promote Accountability Mechanisms for Managed Care Organizations: Advancing Primary Care Innovation in Medicaid Managed Care” (Center for Health Care Strategies, Inc., November 2020), https://www.chcs.org/media/ PCI-Toolkit-MCO-Accountability-Tool_111720.pdf.
150 Manatt Health, “Addressing Social Factors That Affect Health: Emerging Trends and Leading Edge Practices in Medicaid” (State Health & Value Strategies, April 2019), https://www.manatt.com/Manatt/media/Documents/Articles/ Social-Factors-That-Affect-Health_Final.pdf.
151 NC Medicaid, “HEDIS Dashboards,” n.d., https://medicaid.ncdhhs.gov/reports/dashboards.
152 Centers for Disease Control and Prevention, “Select State-Based Activities and Funding in North Carolina,” January 12, 2022, https://www.cdc.gov/ncbddd/aboutus/state-funding/north-carolina.html.
153 Marcelo D’Agostino et al., “Open Data and Public Health,” Revista Panamericana de Salud Pública 42 (June 5, 2018): e66, https://doi.org/10.26633/RPSP.2018.66; Kimá Joy Taylor and Sarah Benatar, “The Pandemic Has Increased Demand for Data and Accountability to Decrease Maternal Health Inequity,” n.d., 9; Julie Kanter et
al., “Improving Outcomes for Patients With Sickle Cell Disease in the United States: Making the Case for More Resources, Surveillance, and Longitudinal Data,” JAMA Health Forum 2, no. 10 (2021): e213467, https://doi. org/10.1001/jamahealthforum.2021.3467.
154 North Carolina Department of Health and Human Services, “North Carolina’s Medicaid Quality Measurement Technical Specifications Manual for Standard Plans and Behavioral Health Intellectual/Developmental Disability Tailored Plans,” March 5, 2021, https://files.nc.gov/ncdma/Technical-Specifications-Manual-20210401.pdf.
155 Georgetown Center for Children & Families, “A Round-Up of Current Child Health Dashboards,” September 29, 2021, https://ccf.georgetown.edu/2021/09/29/a-round-up-of-current-child-health-dashboards/.
156 Texas Health and Human Services, “HHSC Performance Indicator Dashboard,” n.d., https://thlcportal.com/ dashboards/hhscperformance; Washington State Health Care Authority, “Medicaid Maternal and Child Health Measures Dashboard,” October 26, 2021, https://hca-tableau.watech.wa.gov/t/51/views/MaternalandChildHealth/ Dashboard.
157 Wailoo, Dying in the City of the Blues: Sickle Cell Anemia and the Politics of Race and Health.
158 Anjelica C. Saulsberry, Jerlym S. Porter, and Jane S. Hankins, “A Program of Transition to Adult Care for Sickle Cell Disease,” Hematology 2019, no. 1 (2019): 496–504; Arlene Smaldone et al., “HABIT, A Randomized Feasibility Trial to Increase Hydroxyurea Adherence, Suggests Improved Health Related Quality of Life in Youth with Sickle Cell Disease,” The Journal of Pediatrics 197 (2018): 177-185.e2.
159 Sophie Lanzkron, C. Patrick Carroll, and Carlton Haywood, “Mortality Rates and Age at Death from Sickle Cell Disease: U.S., 1979–2005,” Public Health Reports 128, no. 2 (2013): 110–16.
160 Jerlym S. Porter et al., “Pediatric to Adult Care Transition: Perspectives of Young Adults With Sickle Cell Disease,” Journal of Pediatric Psychology 42, no. 9 (2017): 1016–27, https://doi.org/10.1093/jpepsy/jsx088.
161 Marsha Treadwell et al., “Transition from Pediatric to Adult Care in Sickle Cell Disease: Establishing Evidence-Based Practice and Directions for Research,” American Journal of Hematology 86, no. 1 (2011): 116–20.
162 Treadwell et al.
163 Saulsberry, Porter, and Hankins, “A Program of Transition to Adult Care for Sickle Cell Disease.”
164 Porter et al., “Pediatric to Adult Care Transition.”
165 Treadwell et al., “Transition from Pediatric to Adult Care in Sickle Cell Disease.”
166 “Beneficiaries.”
167 Rosalind Bryant et al., “APHON/ASPHO Policy Statement for the Transition of Patients With Sickle Cell Disease From Pediatric to Adult Health Care,” Journal of Pediatric Oncology Nursing 32, no. 6 (2015): 355–59.
168 “Pediatric to Adult Hematologic Care Transition,” American Society of Hematology, n.d., https://www.hematology. org/education/clinicians/clinical-priorities/pediatric-to-adult-care-transition.
169 Treadwell et al., “Transition from Pediatric to Adult Care in Sickle Cell Disease”; Lewis L. Hsu et al., “Community Health Workers as Support for Sickle Cell Care,” American Journal of Preventive Medicine 51, no. 1 Suppl 1 (2016): S87–98.
170 Marie McCormick, Henrietta Awo Osei-Anto, and Rose Marie Martinez, eds., Addressing Sickle Cell Disease: A Strategic Plan and Blueprint for Action (Washington, DC: The National Academies Press, 2020), 16, https://doi. org/10.17226/25632.
171 “NC DPH: N.C. Sickle Cell Syndrome Program.”
172 Treadwell et al., “Transition from Pediatric to Adult Care in Sickle Cell Disease.”
173 Nowogrodzki, “No Adult Left Behind.”
174 Porter et al., “Pediatric to Adult Care Transition.”
175 Jennifer R. Frost et al., “Improving Sickle Cell Transitions of Care Through Health Information Technology,” American Journal of Preventive Medicine 51, no. 1 (2106): S17–23; “Sickle Cell Transition E-Learning Program (STEP) for Teens with Sickle Cell Disease - St. Jude Children’s Research Hospital,” St. Jude Children’s Research Hospital, n.d., https://www.stjude.org/treatment/disease/sickle-cell-disease/step-program.html.
176 Saulsberry, Porter, and Hankins, “A Program of Transition to Adult Care for Sickle Cell Disease.”
177 Anna Nowogrodzki, “No Adult Left behind: Bridge the Health-Care Gap for Sickle-Cell Disease,” Nature 596, no. 7873 (2021): S13–15, https://doi.org/10.1038/d41586-021-02143-z; Hsu et al., “Community Health Workers as Support for Sickle Cell Care.”
178 Wally R. Smith et al., “Lessons Learned from Building a Pediatric-to-Adult Sickle Cell Transition Program,” Southern Medical Journal 112, no. 3 (2019): 190–97; Saulsberry, Porter, and Hankins, “A Program of Transition to Adult Care for Sickle Cell Disease.”
179 Saulsberry, Porter, and Hankins, “A Program of Transition to Adult Care for Sickle Cell Disease.”
180 Smith et al., “Lessons Learned from Building a Pediatric-to-Adult Sickle Cell Transition Program.”
181 Hsu et al., “Community Health Workers as Support for Sickle Cell Care.”
182 Nirmish Shah et al., “Outpatient Healthcare Utilization and Rates of Co-Management Among Medicaid Patients with Sickle Cell Disease in North Carolina,” Blood 132, no. Supplement 1 (November 29, 2018): 4725, https://doi. org/10.1182/blood-2018-99-110737.
183 Joseph Lunyera et al., “Attitudes of Primary Care Physicians Toward Sickle Cell Disease Care, Guidelines, and Comanaging Hydroxyurea With a Specialist,” Journal of Primary Care & Community Health 8, no. 1 (January 1, 2017): 38, https://doi.org/10.1177/2150131916662969.
184 NICHQ, “Congressional Report: Sickle Cell Disease Treatment Demonstration Program” (NICHQ, September 2017); “Sickle Cell Disease Treatment Demonstration Program,” NICHQ - National Institute for Children’s Health Quality, accessed February 1, 2022, https://www.nichq.org/project/sickle-cell-disease-treatment-demonstration-program.
185 CDC, “NCBDDD Select State-Based Activities and Funding in North Carolina,” Centers for Disease Control and Prevention, January 12, 2022, https://www.cdc.gov/ncbddd/aboutus/state-funding/north-carolina.html.
186 Mandip Kaur et al., “Understanding Sickle Cell Disease: Impact of Surveillance and Gaps in Knowledge,” Blood Advances 4, no. 3 (February 6, 2020): 496–98, https://doi.org/10.1182/bloodadvances.2019001000.
187 NCDHHS, “N.C. Sickle Cell Syndrome Program: Services,” NCDHHS, October 14, 2019, https://www. ncsicklecellprogram.org/services.asp.
188 NCDHHS, “North Carolina Sickle Cell Syndrome Program.”
189 “North Carolina Sickle Cell Syndrome Program Service Regions,” September 25, 2019, https://www. ncsicklecellprogram.org/Documents/SC-CatchmentMap-092519.pdf.
190 Ritesh Banerjee, Jeanette Y. Ziegenfuss, and Nilay D. Shah, “Impact of Discontinuity in Health Insurance on Resource Utilization,” BMC Health Services Research 10, no. 1 (July 6, 2010): 8, https://doi.org/10.1186/1472-696310-195.
191 Allyson G. Hall, Jeffrey S. Harman, and Jianyi Zhang, “Lapses in Medicaid Coverage: Impact on Cost and Utilization Among Individuals With Diabetes Enrolled in Medicaid,” Medical Care 46, no. 12 (2008): 1223–24.
192 “NC Budget and Spending - SAS® Visual Analytics,” accessed February 1, 2022, https://ncreports.ondemand.sas. com/SASVisualAnalytics/?reportUri=/reports/reports/b00debfc-51e7-45a6-92d4-3efaf33a3daa§ionIndex=0&sso_ guest=true&reportViewOnly=true&sas-welcome=false.
193 Elizabeth Hinton Published: Jun 22 and 2020, “State Efforts to Expand Medicaid Coverage & Access to Telehealth in Response to COVID-19,” KFF (blog), June 22, 2020, https://www.kff.org/coronavirus-covid-19/issue-brief/stateefforts-to-expand-medicaid-coverage-access-to-telehealth-in-response-to-covid-19/.
194 “SPECIAL BULLETIN COVID-19 #9: Telehealth Provisions - Clinical Policy Modification | NC Medicaid,” accessed December 7, 2021, https://medicaid.ncdhhs.gov/blog/2020/03/20/special-bulletin-covid-19-9-telehealth-provisionsclinical-policy-modification.
195 “SPECIAL BULLETIN COVID-19 #66: Telehealth and Virtual Patient Communications Clinical Policy Modifications - Well Child Visits | NC Medicaid,” accessed December 7, 2021, https://medicaid.ncdhhs.gov/blog/2020/04/24/ special-bulletin-covid-19-66-telehealth-and-virtual-patient-communications-clinical.
196 “North Carolina Telehealth Playbook” (NC Department of Health and Human Services, February 19, 2021), https:// www.ncdhhs.gov/media/10611/download.
197 CDC, “Telehealth Interventions to Improve Chronic Disease | Cdc.Gov,” Centers for Disease Control and Prevention, May 11, 2020, https://www.cdc.gov/dhdsp/pubs/telehealth.htm.
198 “North Carolina Broadband Infrastructure Office,” accessed December 7, 2021, https://www.ncbroadband.gov/
199 “Build Back Better Includes $1 Billion-Plus for Broadband,” Benton Foundation, November 1, 2021, https://www benton.org/headlines/build-back-better-includes-1-billion-plus-broadband.
200 “Sickle Cell Disease: Access-to-Care Summit 2018” (Sickle Cell Disease (SCD) Therapeutics Conference, Global Blood Therapeutics, Inc, 2018), 4.
201 Orah S. Platt et al., “Pain in Sickle Cell Disease,” New England Journal of Medicine 325, no. 1 (July 4, 1991):
11–16, https://doi.org/10.1056/NEJM199107043250103; Patricia Houston-Yu et al., “Frequent and Prolonged Hospitalizations: A Risk Factor for Early Mortality in Sickle Cell Disease Patients,” American Journal of Hematology 72, no. 3 (2003): 201–3.
202 “Sickle Cell Disease: Access-to-Care Summit 2018”; Christian T. Evensen et al., “Quality of Care in Sickle Cell Disease,” Medicine 95, no. 35 (September 2, 2016): e4528.
203 Bradt et al., “Crizanlizumab, Voxelotor, and L-Glutamine for Sickle Cell Disease: Effectiveness and Value.”
204 Bradt et al.
205 “Sickle Cell Disease: Access-to-Care Summit 2018.”
206 Glassberg et al., “Among Emergency Physicians, Use of the Term ‘Sickler’ Is Associated with Negative Attitudes toward People with Sickle Cell Disease.”
207 Glassberg et al.
208 “Sickle Cell Disease: Access-to-Care Summit 2018”; Caroline E Freiermuth et al., “Attitudes Towards Patients with Sickle Cell Disease in a Multi-Center Sample of Emergency Department Providers,” Advanced Emergency Nursing Journal 36, no. 4 (2014): 335–47, https://doi.org/10.1097/TME.0000000000000036; Haywood et al., “The Impact of Race and Disease on Sickle Cell Patient Wait Times in the Emergency Department”; Susan M. Lin et al., “Improving Quality of Care for Sickle Cell Patients in the Pediatric Emergency Department,” Pediatric Emergency Care 32, no. 1 (2016): 14–16, https://doi.org/10.1097/PEC.0000000000000369.
209 Lennette J. Benjamin, Gwendolyn I. Swinson, and Ronald L. Nagel, “Sickle Cell Anemia Day Hospital: An Approach for the Management of Uncomplicated Painful Crises,” Blood 95, no. 4 (February 15, 2000): 1130–37, https://doi. org/10.1182/blood.V95.4.1130.003k03a_1130_1136; Jean L. Raphael et al., “Treatment of Uncomplicated VasoOcclusive Crises in Children with Sickle Cell Disease in a Day Hospital,” Pediatric Blood & Cancer 51, no. 1 (2008): 82–85, https://doi.org/10.1002/pbc.21483.
210 “Division of Hematology/Oncology,” East Carolina University, n.d., https://internal-medicine.ecu.edu/hematology/; “Duke Sickle Cell Center | Medical Services,” Duke University School of Medicine, n.d., https://medicine.duke.edu/ divisions/hematology/patient-care/duke-sickle-cell-center/medical-services.
211 Jean L. Raphael et al., “Day Hospital versus Inpatient Management of Uncomplicated Vaso-Occlusive Crises in Children with Sickle Cell Disease,” Pediatric Blood & Cancer 51, no. 3 (2008): 398–401, https://doi.org/10.1002/ pbc.21537; Benjamin, Swinson, and Nagel, “Sickle Cell Anemia Day Hospital.”
212 Andrew Binding et al., “An Innovative Short-Stay Health Care Model for Treatment of Uncomplicated Vaso-Occlusive Crisis in Adult Sickle Cell Disease Patients in Canada to Reduce Emergency Department Utilization,” CJEM 21, no. 1 (2019): 55–62.
213 “Sickle Cell Disease: Access-to-Care Summit 2018”; Biree Andemariam and Sasia Jones, “Development of a New Adult Sickle Cell Disease Center Within an Academic Cancer Center: Impact on Hospital Utilization Patterns and Care Quality,” Journal of Racial and Ethnic Health Disparities 3, no. 1 (2016): 176–82.
214 Evensen et al., “Quality of Care in Sickle Cell Disease.”
215 Kanter et al., “Building Access to Care in Adult Sickle Cell Disease: Defining Models of Care, Essential Components, and Economic Aspects.”
216 Adeboye H. Adewoye et al., “Effectiveness of a Dedicated Day Hospital for Management of Acute Sickle Cell Pain,” Haematologica 92, no. 6 (2007): 854–854.
217 “Using the Virtual New Normal to Care for Sickle Cell Disease Patients,” Boston Medical Center, accessed December 7, 2021, https://development.bmc.org/our-impact/stories/using-the-virtual-new-normal-to-care-for-sicklecell-disease-patients/.
218 K. F. Woods et al., “Sickle Cell Disease Telemedicine Network for Rural Outreach,” Journal of Telemedicine and Telecare 6, no. 5 (2000): 285–90, https://doi.org/10.1258/1357633001935923.
219 Giuliana Grossi, “Evaluating the Impact of Telehealth on Hydroxyurea Response,” HCPLive, accessed December 13, 2021, https://www.hcplive.com/view/impact-telehealth-hydroxyurea-response.
220 Benjamin, Swinson, and Nagel, “Sickle Cell Anemia Day Hospital.”
221 Raphael et al., “Treatment of Uncomplicated Vaso-Occlusive Crises in Children with Sickle Cell Disease in a Day Hospital.”
222 Jin Han et al., “Program Expansion of a Day Hospital Dedicated to Manage Sickle Cell Pain,” Blood 130, no. Supplement 1 (2017): 4664.
223 Wilson-Frederick et al., “Medicaid and CHIP Sickle Cell Disease Report, T-MSIS Analytic Files (TAF) 2017.”
224 Trisha E. Wong et al., “Update on the Use of Hydroxyurea Therapy in Sickle Cell Disease,” Blood 124, no. 26 (2014): 3850–57, https://doi.org/10.1182/blood-2014-08-435768.
225 Rohit Kumar Agrawal et al., “Hydroxyurea in Sickle Cell Disease: Drug Review,” Indian Journal of Hematology & Blood Transfusion 30, no. 2 (2014): 91–96.
226 Amy Williams, “Outpatient Pharmacy Prior Approval Criteria Sickle Cell Anemia Agents,” North Carolina Department of Health and Human Services, 2019.
227 “Hydroxyurea Treatment for Sickle Cell Disease” (St. Jude Children’s Research Hospital, Departments of Hematology, Patient Education, and Biomedical Communications, 2008), https://www.stjude.org/content/dam/ en_US/shared/www/patient-support/hematology-literature/hydroxyurea-treatment-for-sickle-cell-disease.pdf; Otis W. Brawley et al., “National Institutes of Health Consensus Development Conference Statement: Hydroxyurea Treatment for Sickle Cell Disease,” Annals of Internal Medicine 148, no. 12 (2008): 932–38.
228 Agrawal et al., “Hydroxyurea in Sickle Cell Disease: Drug Review”; Gina Kolata, “Two New Drugs Help Relieve Sickle-Cell Disease. But Who Will Pay?,” The New York Times, December 7, 2019, https://www.nytimes. com/2019/12/07/health/sickle-cell-adakveo-oxbryta.html; Wilson-Frederick et al., “Medicaid and CHIP Sickle Cell Disease Report, T-MSIS Analytic Files (TAF) 2017.”
229 Wilson-Frederick et al., “Medicaid and CHIP Sickle Cell Disease Report, T-MSIS Analytic Files (TAF) 2017.”
230 Amanda M. Brandow and Julie A. Panepinto, “Hydroxyurea Use in Sickle Cell Disease: The Battle with Low Rates of Prescription, Poor Patient Compliance, and Fears of Toxicities and Side Effects,” Expert Review of Hematology 3, no. 3 (2010): 255–60.
231 Brawley et al., “National Institutes of Health Consensus Development Conference Statement: Hydroxyurea Treatment for Sickle Cell Disease.”
232 Nancy Crego et al., “Sickle Cell Disease Co-Management, Healthcare Utilization and Hydroxyurea Use in North Carolina,” Journal of the American Board of Family Medicine : JABFM 33, no. 1 (2020): 91–105; Joacy G. Mathias et al., “Hydroxyurea Use After Transitions of Care Among Young Adults With Sickle Cell Disease and Tennessee Medicaid Insurance,” JAMA Network Open 4, no. 10 (2021): e2128971, https://doi.org/10.1001/ jamanetworkopen.2021.28971.
233 Sarah Shaner et al., “Impact of Telehealth Visits on Hydroxyurea Response in Sickle Cell Anemia,” Pediatric Blood & Cancer 68, no. 12 (2021): e29354.
234 Brandow and Panepinto, “Hydroxyurea Use in Sickle Cell Disease: The Battle with Low Rates of Prescription, Poor Patient Compliance, and Fears of Toxicities and Side Effects.”
235 Darbari and Brandow, “Pain-Measurement Tools in Sickle Cell Disease.”
236 Brandow et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease: Management of Acute and Chronic Ppain”; Sinha et al., “Management of Chronic Pain in Adults Living With Sickle Cell Disease in the Era of the Opioid Epidemic.”
237 Varun Sagi et al., “Integrative Approaches to Treating Pain in Sickle Cell Disease: Pre-Clinical and Clinical Evidence,” Complementary Therapies in Medicine 51 (2020): 102394.
238 “Pain Management Best Practices Inter-Agency Task Force Report: Updates, Gaps, Inconsistencies, and Recommendations” (U.S. Department of Health and Human Services, May 2019), https://www.hhs.gov/ash/advisorycommittees/pain/reports/index.html.
239 “NC Medicaid: Outpatient Pharmacy Prior Approval Criteria, Opioid Analgesics” (North Carolina Department of Health and Human Services, March 1, 2021), https://medicaid.ncdhhs.gov/media/9006/open.
240 Samir K. Ballas et al., “Hydroxyurea and Acute Painful Crises in Sickle Cell Anemia: Effects on Hospital Length of Stay and Opioid Utilization During Hospitalization, Outpatient Acute Care Contacts, and at Home,” Journal of Pain and Symptom Management 40, no. 6 (December 2010): 870–82, https://doi.org/10.1016/j.jpainsymman.2010.03.020.
241 “NC Medicaid: Outpatient Pharmacy Prior Approval Criteria, Opioid Analgesics.”
242 “Outpatient Behavioral Health Services,” NC Medicaid, accessed December 5, 2021, https://medicaid.ncdhhs.gov/ providers/programs-and-services/behavioral-health-idd/outpatient-behavioral-health-services; “Plans | NC Medicaid Managed Care,” 2022, https://ncmedicaidplans.gov/plans?program=102&plans%5B0%5D=166.
243 “Healthy Blue Member Handbook: NC Medicaid Managed Care.”
244 Brandow et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease: Management of Acute and Chronic Ppain.”
245 “Integrative Therapies Pilot Project: A Holistic Approach to Chronic Pain Management in Medicaid” (Health
Management Associates, Inc., February 25, 2008), http://www.aomsm.org/Resources/Documents/Florida%20StudyCAM%20and%20Chronic%20Pain.pdf.
246 Robert T Davis et al., “Acupuncture for Chronic Pain in the Vermont Medicaid Population: A Prospective, Pragmatic Intervention Trial,” Global Advances in Health and Medicine 7 (April 10, 2018): 2164956118769557, https://doi. org/10.1177/2164956118769557.
247 Paul Telfer and Banu Kaya, “Optimizing the Care Model for an Uncomplicated Acute Pain Episode in Sickle Cell Disease” 2017, no. 1 (2017): 525–33.
248 Cara V. James and Shondelle Wilson-Frederick, “The Invisible Crisis: Understanding Pain Management in Medicare Beneficiaries with Sickle Cell Disease” (CMS Office of Minority Health, September 2018).
249 Brandow et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease: Management of Acute and Chronic Ppain.”
250 Brandow et al.
251 Jo Howard, “Sickle Cell Disease: When and How to Transfuse,” Hematology 2016, no. 1 (2016): 625–31.
252 Stella T. Chou et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease: Transfusion Support,” Blood Advances 4, no. 2 (2020): 327–55, https://doi.org/10.1182/bloodadvances.2019001143.
253 K Yazdanbaksh, RE Ware, and F Noizat-Pirenne, “Red Blood Cell Alloimmunization in Sickle Cell Disease: Pathophysiology, Risk Factors, and Transfusion Management,” Blood 120, no. 3 (2012): 528–37, https://doi. org/10.1182/blood-2011-11-327361; Russell E. Ware et al., “Sickle Cell Disease,” The Lancet 390, no. 10091 (2017): 311–23.
254 Chou et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease.”
255 Elliott P Vichinsky, “Current Issues with Blood Transfusions in Sickle Cell Disease,” Seminars in Hematology, Transfusion-Related Iron Overload in Sickle Cell Anemia, 38 (2001): 14–22.
256 Chou et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease.”
257 “Health Check Program Guide” (NC Medicaid, May 2020), https://files.nc.gov/ncdma/documents/Providers/ Programs_Services/EPSDT/Program-Guide-2020.pdf; S Terrell and P Guthery, “N.C. Medicaid Bulletin, January 2018” (North Carolina Department of Health and Human Services, January 2018).
258 “Corporate Medical Policy: Red Blood Cell Molecular Testing” (BlueCross BlueShield of North Carolina, 2021), https://www.bluecrossnc.com/sites/default/files/document/attachment/services/public/pdfs/medicalpolicy/red_blood_ cell_molecular_testing.pdf.
259 Lilian Castilho, “Molecular Typing of Blood Group Genes in Diagnostics,” Annals of Blood 6 (2021), https://doi. org/10.21037/aob-20-73.
260 Chou et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease.”
261 Jessica Casas et al., “Changing Practice: Red Blood Cell Typing by Molecular Methods for Patients With Sickle Cell Disease,” Transfusion 55, no. 6 Pt 2 (2015): 1388–93.
262 I. A. Shulman, “Prophylactic Phenotype Matching of Donors for the Transfusion of Nonalloimmunized Patients with Sickle Cell Disease,” Immunohematology 22, no. 3 (2006): 101–2.
263 Grace E. Linder and Stella T. Chou, “Red Cell Transfusion and Alloimmunization in Sickle Cell Disease,” Haematologica 106, no. 7 (2021): 1805–15, https://doi.org/10.3324/haematol.2020.270546.
264 Yazdanbaksh, Ware, and Noizat-Pirenne, “Red Blood Cell Alloimmunization in Sickle Cell Disease: Pathophysiology, Risk Factors, and Transfusion Management.”
265 “Corporate Medical Policy: Red Blood Cell Molecular Testing.”
266 Samiya Hussain et al., “Implementation of Transcranial Doppler Ultrasonography Screening and Primary Stroke Prevention in Urban and Rural Sickle Cell Disease Populations,” Pediatric Blood & Cancer 62, no. 2 (2015): 219–23.
267 Lena N Naffaa, Yasmeen K Tandon, and Neville Irani, “Transcranial Doppler Screening in Sickle Cell Disease: The Implications of Using Peak Systolic Criteria,” World Journal of Radiology 7, no. 2 (2015): 52–56, https://doi. org/10.4329/wjr.v7.i2.52; M. G. Cherry et al., “The Clinical Effectiveness and Cost-Effectiveness of Primary Stroke Prevention in Children with Sickle Cell Disease: A Systematic Review and Economic Evaluation,” Health Technology Assessment 16, no. 43 (2012): 1–129, https://doi.org/10.3310/hta16430.
268 Wilson-Frederick et al., “Medicaid and CHIP Sickle Cell Disease Report, T-MSIS Analytic Files (TAF) 2017.”
269 Shannon M. Phillips et al., “Identified Barriers and Facilitators to Stroke Risk Screening in Children with Sickle Cell Anemia: Results from the DISPLACE Consortium,” Implementation Science Communications 2, no. 1
(2021): 87, https://doi.org/10.1186/s43058-021-00192-z; Hussain et al., “Implementation of Transcranial Doppler Ultrasonography Screening and Primary Stroke Prevention in Urban and Rural Sickle Cell Disease Populations”; M. Beth McCarville et al., “Evaluation of a Comprehensive Transcranial Doppler Screening Program for Children with Sickle Cell Anemia,” Pediatric Blood & Cancer 50, no. 4 (2008): 818–21, https://doi.org/10.1002/pbc.21430; Lindsay M. Bollinger et al., “Caregivers’ Perspectives on Barriers to Transcranial Doppler Screening in Children with SickleCell Disease,” Pediatric Blood & Cancer 56, no. 1 (2011): 99–102.
270 Lori E. Crosby et al., “Implementation of a Process for Initial Transcranial Doppler Ultrasonography in Children With Sickle Cell Anemia,” American Journal of Preventive Medicine 51, no. 1 (2016): S10–16, https://doi.org/10.1016/j. amepre.2016.01.021.
271 “N.C. Medicaid: Medicaid and Health Choices Transcranial Doppler Studies Clinical Coverage Policy No: 1A-19 Amended,” February 1, 2021, https://medicaid.ncdhhs.gov/media/8332/open.
272 Phillips et al., “Identified Barriers and Facilitators to Stroke Risk Screening in Children with Sickle Cell Anemia.”
273 Robert J. Adams et al., “Prevention of a First Stroke by Transfusions in Children with Sickle Cell Anemia and Abnormal Results on Transcranial Doppler Ultrasonography,” New England Journal of Medicine 339, no. 1 (1998): 5–11.
274 Cherry et al., “The Clinical Effectiveness and Cost-Effectiveness of Primary Stroke Prevention in Children with Sickle Cell Disease.”
275 McCarville et al., “Evaluation of a Comprehensive Transcranial Doppler Screening Program for Children with Sickle Cell Anemia.”
276 Crosby et al., “Implementation of a Process for Initial Transcranial Doppler Ultrasonography in Children With Sickle Cell Anemia.”
277 McCarville et al., “Evaluation of a Comprehensive Transcranial Doppler Screening Program for Children with Sickle Cell Anemia.”
278 McCarville et al.
279 “A Public Health Strategic Plan to Address Sickle Cell Disease Across the Lifespan 2015-2018” (Michigan Department of Health and Human Services Lifecourse Epidemiology & Genomics Division - Hemoglobinopathy Quality Improvement Program, October 2015), https://www.michigan.gov/documents/mdhhs/MDHHS_Final_SCD_ Strategic_Plan_504325_7.pdf.
280 “Sickle Cell Disease Study Committee: Report to the General Assembly,” June 30, 2016, https://www.scstatehouse. gov/CommitteeInfo/SickleCellDiseaseStudyCommittee/SickleCellDiseaseReportToTheGeneralAssembly.pdf.
281 “A Call to Action: South Carolina Sickle Cell Disease State Plan 2019-2022” (The South Carolina Sickle Cell Disease Advocacy Team, October 2018), https://scdhec.gov/sites/default/files/Library/CR-012241.pdf.
282 “State of North Carolina Department of Health and Human Services Division of Health Benefits: Revised and Restated Request for Proposal #: 30-190029-DHB Prepaid Health Plan Services” (State of North Carolina Department of Health and Human Services Division of Health Benefits, January 25, 2019), https://files.nc.gov/ncdma/Contract-30-190029-DHB-Prepaid-Health-Plan-Services.pdf.
283 Brandow et al., “American Society of Hematology 2020 Guidelines for Sickle Cell Disease: Management of Acute and Chronic Ppain.”
284 Jena L Welch-Coltrane et al., “Implementation of Individualized Pain Care Plans Decreases Length of Stay and Hospital Admission Rates for High Utilizing Adults with Sickle Cell Disease,” Pain Medicine 22, no. 8 (August 1, 2021): 1743–52, https://doi.org/10.1093/pm/pnab092.
285 “State of North Carolina Department of Health and Human Services Division of Health Benefits: Revised and Restated Request for Proposal #: 30-190029-DHB Prepaid Health Plan Services,” January 25, 2019.
286 Paula Chatterjee and Karen E. Joynt, “Do Cardiology Quality Measures Actually Improve Patient Outcomes?,” Journal of the American Heart Association 3, no. 1 (n.d.): e000404, https://doi.org/10.1161/JAHA.113.000404.
287 “National Quality Forum 2797: Transcranial Doppler Ultrasonography Screening Among Children with Sickle Cell Anemia,” May 4, 2016, https://www.qualityforum.org/QPS/2797.
288 “National Quality Forum 3166: Antibiotic Prophylaxis Among Children with Sickle Cell Anemia,” July 2, 2021, https:// www.qualityforum.org/QPS/3166.
289 “National Quality Forum 3595: Hydroxyurea Use Among Children with Sickle Cell Anemia,” accessed December 7, 2021, https://www.qualityforum.org/QPS/3595.
290 “NQF: Quality Positioning SystemTM,” National Quality Forum, n.d., https://www.qualityforum.org/QPS/QPSTool.aspx.
291 “Michigan Department of Health and Human Services Comprehensive Quality Strategy 2020-2023” (Michigan Department of Health and Human Services, December 17, 2020), https://www.michigan.gov/documents/mdhhs/ Quality_Strategy_2015_FINAL_for_CMS_112515_657260_7.pdf.
292 Nancy McCall and Deborah Peikes, “Tricky Problems with Small Numbers: Methodological Challenges and Possible Solutions for Measuring PCMH and ACO Performance” (Robert Wood Johnson Foundation, April 2016), https://www shvs.org/wp-content/uploads/2016/04/SHVS-Mathematica-Tricky-Problems-with-Small-Numbers-April-2016.pdf.
293 McCall and Peikes.
294 “State of North Carolina Department of Health and Human Services Division of Health Benefits: Revised and Restated Request for Proposal #: 30-190029-DHB Prepaid Health Plan Services,” January 25, 2019.
295 Masese et al., “Barriers and Facilitators to Care for Individuals with Sickle Cell Disease in Central North Carolina,” 2019.
296 “2019 Quality Incentive Report: A Report on the Quality Incentive Program in New York State” (New York State Department of Health, 2020), https://www.health.ny.gov/health_care/managed_care/reports/docs/quality_incentive/ quality_incentive_2019.pdf.
297 “Medicaid Pay-for-Performance: Ongoing Challenges, New Opportunities,” The Commonwealth Fund, accessed December 7, 2021, https://www.commonwealthfund.org/publications/newsletter-article/medicaid-pay-performanceongoing-challenges-new-opportunities.
298 Thomas Hartman and Kathryn Kuhmerker, “Pay-for-Performance in State Medicaid Programs: A Survey of State Medicaid Directors and Programs - Appendix B. State Pay for Performance Program Summaries” (The Commonwealth Fund, n.d.); “Medicaid Pay-for-Performance: Ongoing Challenges, New Opportunities,” The Commonwealth Fund, accessed December 7, 2021, https://www.commonwealthfund.org/publications/newsletterarticle/medicaid-pay-performance-ongoing-challenges-new-opportunities.
299 Meredith B. Rosenthal et al., “Pay for Performance in Medicaid: Evidence from Three Natural Experiments,” Health Services Research 51, no. 4 (August 2016): 1444–66, https://doi.org/10.1111/1475-6773.12426.
300 “HHS Office of Minority Health Awards $1.25 Million to Improve Treatment for Children with Sickle Cell Disease,” U.S. Department of Health and Human Services Office of Minority Health, October 1, 2020, https://www.minorityhealth. hhs.gov/omh/Content.aspx?ID=17509&lvl=2&lvlid=8.
301 McCall and Peikes, “Tricky Problems with Small Numbers: Methodological Challenges and Possible Solutions for Measuring PCMH and ACO Performance.”
302 Casey Quinn et al., “Estimating the Clinical Pipeline of Cell and Gene Therapies and Their Potential Economic Impact on the US Healthcare System,” Value in Health 22, no. 6 (2019): 621–26, https://doi.org/10.1016/j. jval.2019.03.014.
303 Julie Kanter et al., “Resolution of Sickle Cell Disease Manifestations in Patients Treated with Lentiglobin Gene Therapy: Updated Results from the Phase 1/2 Hgb-206 Group C Study,” Blood 134, no. Supplement_1 (2019): 990.
304 Patrick DeMartino et al., “A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease: The Medicaid Perspective,” JAMA Pediatrics 175, no. 6 (2021): 617–23.
305 “Bluebird Prices Gene Therapy at 1.58 Million Euros over 5 Years,” Reuters, June 14, 2019, sec. Healthcare & Pharma, https://www.reuters.com/article/us-bluebird-bio-gene-therapy-price-idUSKCN1TF1HP.
306 Jillian Mckoy, “Subscription-Based Payment Models May Improve Access to Hepatitis C Medications,” Healthcare Costs, August 27, 2021, https://www.bu.edu/sph/news/articles/2021/subscription-based-payment-models-mayimprove-access-to-hepatitis-c-medications/.
307 Samantha G. Auty, Paul R. Shafer, and Kevin N. Griffith, “Medicaid Subscription-Based Payment Models and Implications for Access to Hepatitis C Medications,” JAMA Health Forum 2, no. 8 (2021): e212291, https://doi. org/10.1001/jamahealthforum.2021.2291.
308 Harry Liu and Abdrew Mulcahy, “Why States’ ‘Netflix Model’ Prescription Drug Arrangements Are No Silver Bullet,” Health Affairs, July 1, 2020, https://www.healthaffairs.org/do/10.1377/hblog20200629.430545/full/.
309 Lanzkron, Carroll, and Haywood, “The Burden of Emergency Department Use for Sickle Cell Disease.”
310 DeMartino et al., “A Budget Impact Analysis of Gene Therapy for Sickle Cell Disease.”
311 Jonathan Salcedo, Jenniffer Bulovic, and Colin M. Young, “Cost-Effectiveness of a Hypothetical Cell or Gene Therapy Cure for Sickle Cell Disease,” Scientific Reports 11, no. 1 (2021): 10838.
312 Rebecca Pifer, “CMS Clears Louisiana Medicaid ‘Netflix Model’ for Hep C Drugs,” Healthcare Dive, June 26, 2019,
https://www.healthcaredive.com/news/cms-clears-louisiana-medicaid-netflix-model-for-hep-c-drugs/557696/.
313 “CMS Approves Louisiana State Plan Amendment for Supplemental Rebate Agreements Using a Modified Subscription Model for Hepatitis C Therapies in Medicaid,” CMS.gov, June 26, 2019, https://www.cms.gov/ newsroom/press-releases/cms-approves-louisiana-state-plan-amendment-supplemental-rebate-agreements-usingmodified.
314 Mckoy, “Subscription-Based Payment Models May Improve Access to Hepatitis C Medications.”
315 Auty, Shafer, and Griffith, “Medicaid Subscription-Based Payment Models and Implications for Access to Hepatitis C Medications.”
316 Auty, Shafer, and Griffith.
317 North Carolina Department of Health and Human Services, “North Carolina’s Care Management Strategy under Managed Care” (North Carolina Department of Health and Human Services, March 9, 2018), https://files.nc.gov/ ncdhhs/documents/CareMgmt-AMH_ConceptPaper_FINAL_20180309.pdf. 7
318 North Carolina Department of Health and Human Services. 7
319 NC Department of Health and Human Services, “Racial and Ethnic Health Disparities in North Carolina: North Carolina Health Equity Report 2018,” 2018, https://schs.dph.ncdhhs.gov/SCHS/pdf/MinorityHealthReport_Web_2018. pdf.
320Division of Health | NC Medicaid, “Program Guide: Management of High-Risk Pregnancies and At-Risk Children in Managed Care” (NC Department of Health and Human Services, May 12, 2021), https://files.nc.gov/ncdma/ProgramGuide-for-Care-Management-of-High--Risk-Pregnancies-and-At-Risk-Children-in-Managed-Care-5.12.pdf. 8
321 “The Maternal, Infant, and Early Childhood Home Visiting Program” (U.S. Human Resources and Services Administration, July 2021), https://mchb.hrsa.gov/sites/default/files/mchb/about-us/program-brief.pdf.
322 “WCH: Maternal, Infant, and Early Childhood Home Visiting Program,” NC DHHS, accessed December 7, 2021, https://publichealth.nc.gov/wch/aboutus/ebhv.htm.
323 “Nurse-Family Partnership: North Carolina 2021 State Profile” (Nurse-Family Partnership, June 2021), https://www. nursefamilypartnership.org/wp-content/uploads/2021/06/NC_2021-State-Profile.pdf.
324 Rachel Herzfeldt-Kamprath, Maura Calysn, and Thomas Huelskoetter, “Medicaid and Home Visiting: Best Practices from States,” January 25, 2017, https://www.americanprogress.org/article/medicaid-and-home-visiting/.
325 Alex F. Peahl et al., “Right-Sizing Prenatal Care to Meet Patients’ Needs and Improve Maternity Care Value,” Obstetrics & Gynecology 135, no. 5 (2020): 1027–37, https://doi.org/10.1097/AOG.0000000000003820.
326 “North Carolina Pregnancy Medical Homes,” Zero to Three, September 20, 2016, https://www.zerotothree.org/ resources/866-north-carolina-pregnancy-medical-homes.
327 “Nurse-Family Partnership: North Carolina 2021 State Profile.”
328 Lenette Azzi-Lessing, “Home Visitation Programs: Critical Issues and Future Directions,” Early Childhood Research Quarterly 26, no. 4 (2011): 387–98.
329 “Maternal Infant Health Program (MIHP),” U.S. DHHS, Home Visiting Evidence of Effectiveness, 2019, https:// homvee.acf.hhs.gov/effectiveness/Maternal%20Infant%20Health%20Program%20%28MIHP%29/In%20Brief.
330 Nadia Islam et al., “Integrating Community Health Workers Within Patient Protection and Affordable Care Act Implementation,” Journal of Public Health Management and Practice: JPHMP 21, no. 1 (2015): 42–50, https://doi. org/10.1097/PHH.0000000000000084.
331 Nadia Islam et al., “Integrating Community Health Workers Within Patient Protection and Affordable Care Act Implementation,” Journal of Public Health Management and Practice: JPHMP 21, no. 1 (2015): 42–50, https://doi. org/10.1097/PHH.0000000000000084.
332 Nadia Islam et al., “Integrating Community Health Workers Within Patient Protection and Affordable Care Act Implementation,” Journal of Public Health Management and Practice: JPHMP 21, no. 1 (2015): 42–50, https://doi. org/10.1097/PHH.0000000000000084.
333 Syed K. Hussaini, Paul Holley, and Douglas Ritenour, “Reducing Low Birth Weight Infancy: Assessing the Effectiveness of the Health Start Program in Arizona,” Maternal and Child Health Journal 15, no. 2 (2011): 225–33.
334 Lee Anne Roman et al., “Addressing Mental Health and Stress in Medicaid-Insured Pregnant Women Using a Nurse-Community Health Worker Home Visiting Team,” Public Health Nursing 24, no. 3 (2007): 239–48, https://doi. org/10.1111/j.1525-1446.2007.00630.x.
335 “Maternal Infant Health Program (MIHP).”
336 Johnson K., “Medicaid and Home Visiting: The State of States’ Approaches” (Johnson Group Consulting, Inc, January 2019). 18
337 Cristian I. Meghea et al., “Statewide Medicaid Enhanced Prenatal Care Programs and Infant Mortality,” Pediatrics 136, no. 2 (2015): 334–42, https://doi.org/10.1542/peds.2015-0479.
338 “NC Department of Health and Human Services: Implementing Recommendations: NC Community Health Worker Initiative,” July 15, 2021, https://nciom.org/wp-content/uploads/2021/03/NCCHW-Initiative-Update-7-15-21.pdf.
339 “The North Carolina Community Health Worker and Support Services Programs: Promoting Safe Quarantine and Isolation for COVID-19 in Marginalized Populations” (NC Department of Health and Human Services, March 2021), https://www.pih.org/sites/default/files/lc/LT-CRC_case_study_NC_march_2021_Final.pdf.
340 Maggie Clark and Allexa Gardner, “More States Moving to Extend Medicaid Postpartum Coverage Option Under ARP, Why Are Georgia and Missouri Limiting Its Reach?,” Georgetown University Health Policy Institute Center for Children and Families, May 20, 2021, https://ccf.georgetown.edu/2021/05/20/medicaid-postpartum-coverage-optiongeorgia-missouri/.
341 Yhenneko J. Taylor, Tsai-Ling Liu, and Elizabeth A. Howell, “Insurance Differences in Preventive Care Use and Adverse Birth Outcomes Among Pregnant Women in a Medicaid Nonexpansion State: A Retrospective Cohort Study,” Journal of Women’s Health 29, no. 1 (2020): 29–37. Taylor, Liu, and Howell. 30 and 32
342 Taylor, Liu, and Howell, “Insurance Differences in Preventive Care Use and Adverse Birth Outcomes Among Pregnant Women in a Medicaid Nonexpansion State: A Retrospective Cohort Study.” 34
343 Arden Handler et al., “A Two-Generation Approach to Postpartum Care: Building on the Well-Baby Visit,” Birth 48, no. 3 (2021): 347–56.
344 Handler et al.
345 Kristin Allen, “Strategies to Support Postpartum Visits for Women in Medicaid,” Health Management Associates, August 22, 2019, https://www.healthmanagement.com/blog/strategies-to-support-postpartum-visits-for-women-inmedicaid/; Rachel S. Ruderman et al., “Provider Perspectives on Barriers and Facilitators to Postpartum Care for Low-Income Individuals,” Women’s Health Reports 2, no. 1 (November 1, 2021): 254–62, https://doi.org/10.1089/ whr.2021.0009.
346 Allen, “Strategies to Support Postpartum Visits for Women in Medicaid”; Ruderman et al., “Provider Perspectives on Barriers and Facilitators to Postpartum Care for Low-Income Individuals.”
347 Handler et al., “A Two-Generation Approach to Postpartum Care.”
348 Sukanya Srinivasan et al., “Delivering Interconception Care During Well-Child Visits: An IMPLICIT Network Study,” The Journal of the American Board of Family Medicine 31, no. 2 (March 1, 2018): 201–10; John Lines, “One Appointment, Multiple Healthier Outcomes: Screening Moms at Well-Baby Visits,” Penn Medicine News, February 9, 2018, https://www.pennmedicine.org/news/news-blog/2018/february/one-appointment-multiple-healthier-outcomesscreening-moms-at-well-baby-visits.
349 IMPLICIT NETWORK and March of Dimes, “IMPLICIT Interconception Care Toolkit” (Family Medicine Consortium, 2016), https://ohioaap.org/wp-content/uploads/2021/09/Implicit-Toolkit.pdf. 18
350 Megan Lent, “Virginia’s BabyCare Program: Working to Improve Birth Outcomes through Medicaid” (National Academy for State Health Policy, November 2018), https://www.nashp.org/wp-content/uploads/2018/12/BabycareVA-Fact-Sheet.pdf. 2-3
351 Lynn M. Yee et al., “Using a Patient Navigator to Improve Postpartum Care in an Urban Women’s Health Clinic,” Obstetrics and Gynecology 129, no. 5 (2017): 925–33.
352 Alliance for Innovation on Maternal Health, “Postpartum Discharge Bundle” (American College of Obstetricians and Gynecologists, 2021), https://safehealthcareforeverywoman.org/wp-content/uploads/FINAL-Update_AIM_Bundle_ PPDT-1.pdf.
353 Alison M. Stuebe et al., “Consensus Bundle on Postpartum Care Basics: From Birth to the Comprehensive Postpartum Visit,” Obstetrics & Gynecology 137, no. 1 (2021): 33–40.
354 Diana Rodin et al., “Strategies to Promote Postpartum Visit Attendance Among Medicaid Participants,” Journal of Women’s Health 28, no. 9 (2019): 1246–53; Centers for Medicare & Medicaid Services Maternal & Infant Health Initiative, “Resources on Strategies to Improve Postpartum Care Among Medicaid and CHIP Populations,” February
2015.
355 “Maternal Infant Health Program (MIHP).”
356 Lilo Stainton, “Home Visits Boost Health of Newborns, Mothers,” NJ Spotlight News, July 30, 2021, https://www. njspotlightnews.org/2021/07/new-nj-law-provides-home-based-wellness-checks-for-mothers-and-newborns/.
357 Kenneth A. Dodge et al., “Effect of a Community Agency–Administered Nurse Home Visitation Program on Program Use and Maternal and Infant Health Outcomes: A Randomized Clinical Trial,” JAMA Network Open 2, no. 11 (November 1, 2019): e1914522.
358 “SistasCaring4Sistas Doula Services: What Doulas Do,” MAHEC - Mountain Area Health Education Center, accessed December 6, 2021, https://mahec.net/patient-information/ob-gyn-care/doula-services/what-doulas-do.
359 Cara B. Safon et al., “Doula Care Saves Lives, Improves Equity, And Empowers Mothers. State Medicaid Programs Should Pay For It,” Health Affairs Blog, May 26, 2021, https://www.healthaffairs.org/do/10.1377/ hblog20210525.295915/full/.
360 Katy Backes Kozhimannil et al., “Doula Care, Birth Outcomes, and Costs Among Medicaid Beneficiaries,” American Journal of Public Health 103, no. 4 (2013): e113–21.
361 Katy B Kozhimannil et al., “Modeling the Cost Effectiveness of Doula Care Associated with Reductions in Preterm Birth and Cesarean Delivery,” Birth (Berkeley, Calif.) 43, no. 1 (2016): 20–27.
362 Kozhimannil et al., “Doula Care, Birth Outcomes, and Costs Among Medicaid Beneficiaries.”
363 Katy Backes Kozhimannil et al., “Doula Care Supports Near-Universal Breastfeeding Initiation among Diverse, Low-Income Women,” Journal of Midwifery & Women’s Health 58, no. 4 (2013): 378–82; Laurie Zephyrin et al., “Community-Based Models to Improve Maternal Health Outcomes and Promote Health Equity,” The Commonwealth Fund, Data Brief, March 4, 2021, https://www.commonwealthfund.org/publications/issue-briefs/2021/mar/communitymodels-improve-maternal-outcomes-equity.
364 Kozhimannil et al., “Doula Care Supports Near-Universal Breastfeeding Initiation among Diverse, Low-Income Women.”
365 Kozhimannil et al.
366 “Healthy Blue Member Handbook: NC Medicaid Managed Care.”
367 “WellCare of North Carolina - NC Medicaid Managed Care Member Handbook.”
368 “UnitedHealthcare NC Medicaid Managed Care Member Handbook.”
369 Hannah Critchfield, “Program Seeks to Increase Number of Black Doulas in NC,” North Carolina Health News, March 29, 2021, http://www.northcarolinahealthnews.org/2021/03/29/program-seeks-to-increase-number-of-blackdoulas-in-nc/; Akira Kyles, “‘We Are an Asset’: Fayetteville Doula Aims to Have Doula Recognized in the Healthcare System,” The Fayetteville Observer, September 4, 2021, https://www.fayobserver.com/story/news/2021/09/04/ fayetteville-doula-addresses-maternal-care-and-racial-disparities-momnibus-healthcare/5601621001/.
370 Katy B. Kozhimannil et al., “Potential Benefits of Increased Access to Doula Support during Childbirth,” The American Journal of Managed Care 20, no. 8 (2014): e340–52; Kozhimannil et al., “Doula Care, Birth Outcomes, and Costs Among Medicaid Beneficiaries.”
371 Kozhimannil et al., “Doula Care, Birth Outcomes, and Costs Among Medicaid Beneficiaries”; Kozhimannil et al., “Potential Benefits of Increased Access to Doula Support during Childbirth.”
372 Kozhimannil et al., “Potential Benefits of Increased Access to Doula Support during Childbirth.”
373 Critchfield, “Program Seeks to Increase Number of Black Doulas in NC.”
374 Kenneth J. Gruber, Susan H. Cupito, and Christina F. Dobson, “Impact of Doulas on Healthy Birth Outcomes,” The Journal of Perinatal Education 22, no. 1 (2013): 49–58, https://doi.org/10.1891/1058-1243.22.1.49.
375 Lisa Rab, “The Secret to Saving the Lives of Black Mothers and Babies,” Politico, December 15, 2019, https://www. politico.com/news/magazine/2019/12/15/black-mothers-matter-079532.
376 “Doula Medicaid Project: Current State Doula Medicaid Efforts,” National Health Law Program, Fall 2021, https:// healthlaw.org/doulamedicaidproject/.
377 Kozhimannil et al., “Modeling the Cost Effectiveness of Doula Care Associated with Reductions in Preterm Birth and Cesarean Delivery.”
378 Hannah Critchfield, “Sweeping Legislation Aims to Combat Black Maternal Mortality,” North Carolina Health News, April 15, 2021, http://www.northcarolinahealthnews.org/2021/04/15/sweeping-legislation-aims-to-combat-blackmaternal-mortality/.
379 Jeannette R. Ickovics et al., “Cluster Randomized Controlled Trial of Group Prenatal Care: Perinatal Outcomes Among Adolescents in New York City Health Centers,” American Journal of Public Health 106, no. 2 (2016): 359–65; Jeannette R. Ickovics et al., “Effects of Group Prenatal Care on Psychosocial Risk in Pregnancy: Results from a Randomised Controlled Trial,” Psychology & Health 26, no. 2 (2011): 235–50.
380 Jamila Taylor and Christy M. Gamble, “Suffering in Silence: Mood Disorders Among Pregnant and Postpartum Women of Color,” Center for American Progress, November 17, 2017.
381 “Preterm Birth | CDC,” Centers for Disease Control and Prevention | Reproductive Health| Maternal and Infant Health| Maternal and Infant Health, November 1, 2021, https://www.cdc.gov/reproductivehealth/maternalinfanthealth/ pretermbirth.htm; R. Su et al., “Relationship of Maternal Birth Weight on Maternal and Neonatal Outcomes: A Multicenter Study in Beijing,” Journal of Perinatology 36, no. 12 (2016): 1061–66.
382 Villarosa, “Why America’s Black Mothers and Babies Are in a Life-or-Death Crisis.”
383 Saraswathi Vedam et al., “The Giving Voice to Mothers Study: Inequity and Mistreatment during Pregnancy and Childbirth in the United States,” Reproductive Health 16 (2019): 77.
384 Taylor, Liu, and Howell, “Insurance Differences in Preventive Care Use and Adverse Birth Outcomes Among Pregnant Women in a Medicaid Nonexpansion State: A Retrospective Cohort Study.”
385 “Child and Family Health: Pew-MacArthur Results First Initiative” (North Carolina Office of State Budget and Management, May 2019), https://www.osbm.nc.gov/media/956/download.
386 “UnitedHealthcare and UWH of North Carolina to Address Maternal Health Needs With Group Prenatal Care Initiative,” Business Wire, October 20, 2021, https://www.businesswire.com/news/home/20211020005147/en/ UnitedHealthcare-and-UWH-of-North-Carolina-to-Address-Maternal-Health-Needs-With-Group-Prenatal-CareInitiative.
387 Brittany M. Byerley and David M. Haas, “A Systematic Overview of the Literature Regarding Group Prenatal Care for High-Risk Pregnant Women,” BMC Pregnancy and Childbirth 17 (2017): 329, https://doi.org/10.1186/s12884-0171522-2.
388 E. B. Carter et al., “Group Versus Traditional Prenatal Care in Low-Risk Women Delivering At Term: A Retrospective Cohort Study,” Journal of Perinatology 37, no. 7 (2017): 769–71, https://doi.org/10.1038/jp.2017.33.
389 Byerley and Haas, “A Systematic Overview of the Literature Regarding Group Prenatal Care for High-Risk Pregnant Women.”
390 Carter et al., “Group versus Traditional Prenatal Care in Low-Risk Women Delivering at Term.”
391 Taylor, Liu, and Howell, “Insurance Differences in Preventive Care Use and Adverse Birth Outcomes Among Pregnant Women in a Medicaid Nonexpansion State: A Retrospective Cohort Study.”
392 Adrianne M Smith, Mehak Zainab, and Brad Lian, “Effects of CenteringPregnancy on Pregnancy Outcomes and Health Disparities in Racial Groups versus Traditional Prenatal Care,” Journal of the Georgia Public Health Association 8, no. 1 (2020); Elizabeth Patberg et al., “Postpartum Contraceptive Use and Other Reproductive Health Outcomes Among CenteringPregnancy Group Prenatal Care Participants,” Journal of Women’s Health 30, no. 7 (2021): 990–96, https://doi.org/10.1089/jwh.2019.8241; Jacqueline H. Grant et al., “Implementing Group Prenatal Care in Southwest Georgia Through Public–Private Partnerships,” Maternal and Child Health Journal 22, no. 11 (2018): 1535–42, https://doi.org/10.1007/s10995-018-2576-0.
393 Ahn et al., “Initiatives to Reduce Maternal Mortality and Severe Maternal Morbidity in the United States.”
394 “North Carolina Pregnancy Medical Home,” Fact Sheet (MACPAC, September 2021); Chelsea Abshire et al., “The Impact of CenteringPregnancy Group Prenatal Care on Birth Outcomes in Medicaid Eligible Women,” Journal of Women’s Health 28, no. 7 (2019): 919–28, https://doi.org/10.1089/jwh.2018.7469.
395 “Prenatal-to-3 State Policy Roadmap 2021: Group Prenatal Care,” Prenatal-to-3 Policy, 2021, https://pn3policy.org/ pn-3-state-policy-roadmap-2021/us/group-prenatal-care/.
396 “North Carolina Pregnancy Medical Home.”
397 “North Carolina Pregnancy Medical Home.”
398 “Certified Midwife Credential,” American College of Nurse-Midwives, accessed December 6, 2021, https://www midwife.org/certified-midwife-credential.
399 Saraswathi Vedam et al., “Mapping Integration of Midwives across the United States: Impact on Access, Equity, and Outcomes,” ed. Dongmei Li, PLOS ONE 13, no. 2 (2018): e0192523.
400 Vedam et al.
401 Vedam et al.
402 “North Carolina Health Professional Supply Data: Certified Nurse Midwives per 10,000 Population by County, North Carolina, 2020,” Sheps Health Workforce NC, accessed December 6, 2021, https://nchealthworkforce.unc.edu/ interactive/supply/.
403 Russ Bowen, “How Midwives Are Helping to Fill OB/GYN Gap in North Carolina,” CBS17, August 25, 2021, https:// www.cbs17.com/news/north-carolina-news/how-midwives-are-helping-to-fill-ob-gyn-gap-in-north-carolina/.
404 Vedam et al., “Mapping Integration of Midwives across the United States.”
405 Sarah Delia, “Midwife Care Is Dramatically Different In NC, SC,” WFAE 90.7 - Charlotte’s NPR News Source, June 1, 2017, https://www.wfae.org/health/2017-06-01/midwife-care-is-dramatically-different-in-nc-sc.
406 Waldman, “How Hospitals Are Failing Black Mothers.”
407 Roosa Tikkanen et al., “Maternal Mortality and Maternity Care in the United States Compared to 10 Other Developed Countries,” Issue Briefs, Commonwealth Fund, 2020.
408 Christopher J. Conover and Robert Richards, “Economic Benefits of Less Restrictive Regulation of Advanced Practice Registered Nurses in North Carolina: An Analysis of Local and Statewide Effects on Business Activity” (Duke University, Center for Health Policy and Inequalities Research, February 2015).
409 Vedam et al., “The Giving Voice to Mothers Study.”
410 Y. Tony Yang, Laura B. Attanasio, and Katy B. Kozhimannil, “State Scope of Practice Laws, Nurse-Midwifery Workforce, and Childbirth Procedures and Outcomes,” Women’s Health Issues 26, no. 3 (2016): 262–67, https://doi org/10.1016/j.whi.2016.02.003.
411 “FAQs on NCOGS Certified Nurse Midwife Policy,” North Carolina Obstetrical & Gynecological Society, March 3, 2017, https://www.ncmedsoc.org/wp-content/uploads/2013/06/FAQs-NCOGS-Policy-on-CNMs-March-2017.pdf.
412 Vedam et al., “The Giving Voice to Mothers Study.”
413 Declercq and Zephyrin, “Severe Maternal Morbidity in the United States.”
414 Taylor and Gamble, “Suffering in Silence.”
415 Jamila Taylor et al., “Eliminating Racial Disparities in Maternal and Infant Mortality: A Comprehensive Policy Blueprint,” Center for American Progress, May 2019.
416 Taylor and Gamble, “Suffering in Silence.”
417 “North Carolina Pregnancy Medical Home.”
418 Clinical Policy and Programs, “Postpartum Depression Screening | NC Medicaid,” NC DHHS, January 5, 2018, https://medicaid.ncdhhs.gov/blog/2018/01/05/postpartum-depression-screening.
419 MACPAC, “Inventory of State-Level Medicaid Policies, Programs, and Initiatives to Improve Maternity Care and Outcomes” (MACPAC, March 2020), https://www.macpac.gov/publication/inventory-of-state-level-medicaid-policiesprograms-and-initiatives-to-improve-maternity-care-and-outcomes/.
420 North Carolina Department of Health and Human Services, “North Carolina’s Medicaid Quality Measurement
Technical Specifications Manual for Standard Plans and Behavioral Health Intellectual/Developmental Disability Tailored Plans.”
421 Vikki Wachino, “Maternal Depression Screening and Treatment: A Critical Role for Medicaid in the Care of Mothers and Children” (Center for Medicaid and CHIP Services, n.d.), https://www.medicaid.gov/federal-policy-guidance/ downloads/cib051116.pdf.
422 “State of North Carolina Department of Health and Human Services Division of Health Benefits: Revised and Restated Request for Proposal #: 30-190029-DHB Prepaid Health Plan Services” (State of North Carolina Department of Health and Human Services Division of Health Benefits, January 25, 2019), https://files.nc.gov/ncdma/Contract-30-190029-DHB-Prepaid-Health-Plan-Services.pdf.
423 Wachino, “Maternal Depression Screening and Treatment: A Critical Role for Medicaid in the Care of Mothers and Children.”
424 MACPAC, “Inventory of State-Level Medicaid Policies, Programs, and Initiatives to Improve Maternity Care and Outcomes.”
425 North Carolina Department of Health and Human Services, “North Carolina’s Medicaid Quality Measurement
Technical Specifications Manual for Standard Plans and Behavioral Health Intellectual/Developmental Disability Tailored Plans.”
426 Taylor and Gamble, “Suffering in Silence.”
427 JudyAnn Bigby et al., “Recommendations for Maternal Health and Infant Health Quality Improvement in Medicaid and the Children’s Health Insurance Program” (Centers for Medicare & Medicaid Services - Medicaid & CHIP Maternal & Infant Health Quality Improvement, December 18, 2020).
428 North Carolina Department of Health and Human Services, “North Carolina’s Medicaid Quality Measurement Technical Specifications Manual for Standard Plans and Behavioral Health Intellectual/Developmental Disability Tailored Plans.”
429 The Bureau of Health Services Financing, “Louisiana’s Medicaid Managed Care Quality Strategy,” May 2021, https:// ldh.la.gov/assets/docs/MQI/MQIStrategy.pdf.
430 Missouri Department of Social Services, “Managed Care Performance Withhold Technical Specifications,” 2019, https://dss.mo.gov/business-processes/managed-care-2017/bidder-vendor-documents/managed-care-pwt-spec19. pdf; Ohio Department of Medicaid, “The Ohio Department of Medicaid Managed Care Quality Strategy,” 2018, https://medicaid.ohio.gov/Portals/0/Medicaid%20101/QualityStrategy/Measures/MCQ-Strategy2018.pdf.
431 “Trends in Maternal Mortality Statistics” (North Carolina Department of Health and Human Services, November 14, 2019), https://schs.dph.ncdhhs.gov/data/maternal/.
432 Kimberly Fryer et al., “Identifying Barriers and Facilitators to Prenatal Care for Spanish-Speaking Women,” North Carolina Medical Journal 82, no. 1 (2021): 7–13.
433 Fryer et al.
434 Ian Hill et al., “Medicaid Outreach and Enrollment for Pregnant Women: What Is the State of the Art?” (Urban Institute, March 2009), https://www.urban.org/sites/default/files/publication/30386/411898-Medicaid-Outreach-andEnrollment-for-Pregnant-Women-What-Is-the-State-of-the-Art-.PDF.
435 “State Plan Amendment (SPA) #: 13-029” (Centers for Medicare & Medicaid Services, January 14, 2015), https:// www.medicaid.gov/sites/default/files/State-resource-center/Medicaid-State-Plan-Amendments/Downloads/CA/ CA-13-029.pdf; “State Plan Amendment (SPA)#: NY-13-64” (Centers for Medicare & Medicaid Services, February 5, 2014), https://www.medicaid.gov/sites/default/files/State-resource-center/Medicaid-State-Plan-Amendments/ Downloads/NY/NY-13-64.pdf.
436 “Trends in Maternal Mortality Statistics.”