BEHAVIORAL INSIGHTS TO
PROMOTE DEMAND FOR COVID-19 VACCINES IN SUB-SAHARAN AFRICA


PROMOTE DEMAND FOR COVID-19 VACCINES IN SUB-SAHARAN AFRICA

Zainab Amjad specializes in international development with a focus on urban policy. Prior to Princeton, she worked as a development consultant with Delivery Associates, supporting sanitation reform with the government of Pakistan, implementation of reforms for Vision 2030 with the government of Saudi Arabia, and education reforms at the Prime Minister’s office in Saint Lucia. At Princeton, Zainab has taken courses in urban policy and public health, while deepening her skills in spatial analysis and econometrics.
Chloe Cho specializes in economics and public policy, with a focus on public finance and international development. Prior to Princeton, she worked as a research analyst at the International Budget Partnership, conducting cross-country analyses of budget deviations. Previously, she worked at the Center on Budget and Policy Priorities and Verité Research, analyzing budget, tax, trade, and other government policies in the United States and Sri Lanka.
Jack Diao is a CPA who has held progressive positions at the federal level, where he oversaw $400M+ in spending for large-scale publicprivate partnership infrastructure projects. He has also held numerous policy dialogues, engaging stakeholders at all levels. He has also worked for the World Bank in researching policies enabling resilient growth and green private sector development, as well as led fiscal and public finance reforms to improve the efficiency and collection of tax systems. Speaking Spanish, French, and Mandarin, Jack hopes to continue working in international economic development.
Eunji Kim is a journalist by training and worked as a radio producer at Korean Broadcasting System (KBS) in Seoul prior to Princeton. She has produced documentaries, talk shows, and news programs, covering South Korea’s politics, history, culture, and society, that reached audiences worldwide. At Princeton, she is focusing on international relations and international development with a concentration on environmental policy.
McKenzie Leier is a fourth-generation North Dakotan who grew up with the extraordinarily flat land of the Red River Valley in her backyard. McKenzie completed a Fulbright fellowship in Malaysia and has worked for the Iowa Department of Public Health and Boston Children’s Hospital. Most recently, she worked as a project manager for Partners in Health’s U.S. COVID-19 response. At Princeton, she is focusing on global health and development.
Nash Mepukori is a global health advocacy, communications, and policy specialist, passionate about strengthening health systems in emerging economies to improve wellbeing. Working at the intersection of global health practice and policy, her expertise lies in driving outcomes on key health issues, including maternal and newborn survival, reproductive health, immunization, universal health coverage, and health financing. She has worked closely with Ministries of Health, private sector, civil society, and development partners in East and Southern Africa, India, and the United States.
Caitlin Quinn previously worked for the federal government on the House Foreign Affairs Committee and the State Department's Office of Central American Affairs as a Scholars in the Nation's Service Initiative (SINSI) graduate fellow. Most recently, she worked on systemic police reform efforts at the Civil Rights Division of the Department of Justice. At Princeton, she is focusing on both foreign and domestic policy.
Nausheen Rajan worked as a Senior Associate in the Asia Regional Business Unit at Chemonics International, where she provided project management and business development support for USAID-funded projects, before Princeton. Previously, she has engaged with issues at the intersection of foreign affairs and economic development through work with the United States Department of State, think tanks, and initiatives that have built the capacity of women to create, sustain and scale their businesses in Pakistan. At Princeton, she is focusing on international development and urban policy.
This report was prepared by second-year Master in Public Affairs students at the Princeton School of Public and International Affairs. The authors would like to thank the many experts who lent their time and knowledge to our group. We are especially grateful to our professor, Varun Gauri, for sharing his behavioral science expertise and guiding us in creating this report. Finally, we would like to thank the Mind, Behavior, and Development (eMBeD) Unit at the World Bank for their partnership and guidance. Any errors in the report should be attributed to the authors, not the experts listed below. We hope that this report will be useful to the eMBeD team and make a small contribution to the understanding of vaccine hesitancy.
Specifically, we would like to thank:
Zeina Afif Senior Behavioral Scientist, eMBeD Unit, World Bank
Thomas Black Senior Program Officer, Global Delivery Programs, Bill & Melinda Gates Foundation
Katherine E. Bliss, Ph.D. Senior Fellow and Director, Immunizations and Health Systems Resilience, Global Health Policy Center, Center for Strategic and International Studies (CSIS)
Corey Morales Cameron Consultant, eMBeD Unit, World Bank
Sergio Cecchini Infodemic Management Officer, Africa Infodemic Response Alliance Coordinator, World Health Organization Regional Office for Africa (WHO AFRO)
Alin Coman, Ph.D. Associate Professor, Princeton University
Christopher Giles Researcher, Stanford Internet Observatory
Shelby Grossman, Ph.D. Research Scholar, Stanford Internet Observatory
Ellen Elizabeth Moscoe, Ph.D. Behavioral Scientist, eMBeD Unit, World Bank
Ifeanyi Nsofor, M.D. Public Health Physician; Senior Atlantic Fellow for Health Equity, George Washington University; Director of Policy and Advocacy, Nigeria Health Watch
Victor Hugo Orozco-Olvera, Ph.D. Senior Economist, Development Impact Evaluation (DIME) group, World Bank
Joachim Osur, Ph.D. Vice Chancellor, Amref International University
Jeff Pituch Senior Consultant, DevGlobal
Justin Sandefur, Ph.D. Research Fellow, Center for Global Development
Sema Sgaier, Ph.D. Co-Founder and Chief Executive Officer, Surgo Ventures
Jana Smith Managing Director, ideas42
Morgan Wack Doctoral Candidate, University of Washington Department of Political Science
This report, prepared for the Mind, Behavior, and Development (eMBeD) Unit at the World Bank, applies a behavioral science lens to analyze the impact of misinformation on COVID-19 vaccine demand, with a focus on sub-Saharan Africa.

Based on our review of the relevant literature, we find five major thematic enablers of COVID-19 vaccine hesitancy: 1) health concerns and risk perceptions, 2) low trust in institutions, 3) automatic thinking and heuristics, 4) social processes, and 5) cultural and religious beliefs. Given time and resource constraints, we were unable to conduct primary research for this report. As a result, we relied on other scholars’ work on diagnosing vaccine hesitancy in sub-Saharan Africa to draft our original diagnostic questions.
For each of the five enablers of vaccine hesitancy, we propose interventions tailored to the eMBeD team’s needs, meaning that most of these interventions take place online. We suggest social media advertisements, most of which are customized to persona type, WhatsApp chatbots, and interactive games based on inoculation theory. In addition to these online interventions, we propose several in-person interventions based on our findings about social norms, cultural and religious beliefs, and automatic thinking.
Just days before the Omicron variant was first detected in sub-Saharan Africa in November 2021, South Africa made global headlines by asking Johnson & Johnson and Pfizer to delay scheduled COVID-19 vaccine shipments. Demand for the vaccines had slowed, and officials were worried that additional doses might expire before they could be used. The situation in South Africa demonstrated that while supply-side issues have been the preeminent roadblock to widespread vaccination thus far for sub-Saharan Africa, vaccine hesitancy is emerging as another significant barrier to vaccinating the region.
As of December 2021, over 290 million cases of COVID-19 have been confirmed worldwide, and over 5 million people have died of COVID-19.1 Despite having fewer public health resources compared to the rest of the world, Africa has been perhaps the least affected region in the world (with the notable exception of South Africa). According to the World Health Organization (WHO), Africa accounts for just 4% of the world’s COVID-19 infections and just 3% of the world’s total deaths from COVID-19.2 By contrast, roughly 18% of the world’s population lives in Africa.3 These low case rates suggest that much of Africa’s population remains susceptible to the virus.
As of December 2021, 56% of the world’s population has received at least one dose of a COVID-19 vaccine, but differences in regional vaccination rates
are stark. Whereas 72% of those in the United States and Canada have received at least one dose of a COVID-19 vaccine, only 11% of their African counterparts have done the same.4
While developed countries initially monopolized the supply of COVID-19 vaccines, availability has increased in developing countries in recent months. However, misinformation threatens to impede vaccination efforts by fueling hesitancy and outright hostility toward the vaccines. As internet and social media use have become more widespread across the globe, people increasingly turn to online sources to stay informed and communicate with one another. Information is circulated throughout society more rapidly and in greater quantities than ever before. As a result, COVID-19 misinformation has proliferated on social media platforms such as Facebook and WhatsApp across the world.5 Moreover, multiple studies have shown that exposure to misinformation through nontraditional media sources—especially social media—has been linked to reduced vaccine acceptance.6 From these results, it is clear that misinformation may have deleterious effects on vaccination rates and public health.
In sub-Saharan Africa, multiple studies have shown that COVID-19-related misinformation has proliferated in the region and fueled concerns about COVID-19 vaccines. For example, in a 2021 study by the African Union and
the Africa Centers for Disease Control and Prevention (Africa CDC), data was collected from over 15,000 individuals in 15 African countries, including 13 in sub-Saharan Africa. Two-thirds (66%) of respondents reported being exposed to “some” or “a lot” of misinformation.7 The researchers found that respondents “who self-report exposure to rumors also show a higher propensity to believe them.”8 The study also found that nearly half of respondents believed that COVID-19 is a planned event by foreign actors, and that online sources, particularly social media, tend to be the most trusted source of information among vaccine-hesitant individuals.9
Another 2021 study by Afrobarometer surveyed a representative sample of 6,000 individuals in five West African countries and found that only four in 10 people said they would be likely to accept a COVID-19 vaccine.10 Similarly concerning results were reported in a study of South Africa and Zimbabwe, two of the first sub-Saharan African countries to receive COVID-19 vaccines.11
While a substantial portion of COVID19-related misinformation is not based in truth, it is important to note that
vaccine hesitancy in sub-Saharan Africa is often grounded in actual events. Historically, people in colonial Africa were victims of unrestricted medical experimentation, with little to no oversight or accountability. For example, as late as 1955, a prominent British physician at Oxford University stated enthusiastically: “[I]t is the almost unlimited field that Africa offers for clinical research that I find so enthralling.”12 In a more recent example, a 1996 Pfizer meningitis drug trial in northern Nigeria killed 11 children and generated lasting distrust of vaccines within and beyond the region.13
In light of the proliferation of online COVID-19 misinformation and the evidence that misinformation reduces vaccine acceptance, this report seeks to offer behavioral insights to promote demand for COVID-19 vaccines in subSaharan Africa. We analyze the issue of online misinformation as a potential driver of vaccine hesitancy, summarizing the literature, proposing diagnostics, and suggesting interventions.
In this report, we focus on the impacts of COVID-19-related misinformation on vaccine hesitancy in sub-Saharan Africa. However, the broader issue of vaccine uptake in sub-Saharan Africa is significantly more complex. Much of the literature we review focuses on individuals’ thoughts and feelings about vaccines, but as Brewer et al. note in their 2017 review paper, “few randomized trials have successfully changed what people think and feel about vaccines, and those few that succeeded were minimally effective in increasing uptake.” They elaborate: “Interventions appear to be able to increase vaccine confidence, but the impact of increased confidence
on uptake is unknown.”i This insight was echoed by public opinion researchers from the Gates Foundation, who noted that although the causal link between exposure to COVID-19-related misinformation and reduced vaccine uptake may seem intuitively obvious, it has yet to be empirically proven in the existing literature.ii Research from Goldstein et al. in Nigeria found no relationship between overall belief in misinformation and willingness to be vaccinated among a group of urban, middle-class Nigerians.iii The figure below shows how people’s thoughts and feelings about vaccines may contribute to their choice to get vaccinated.
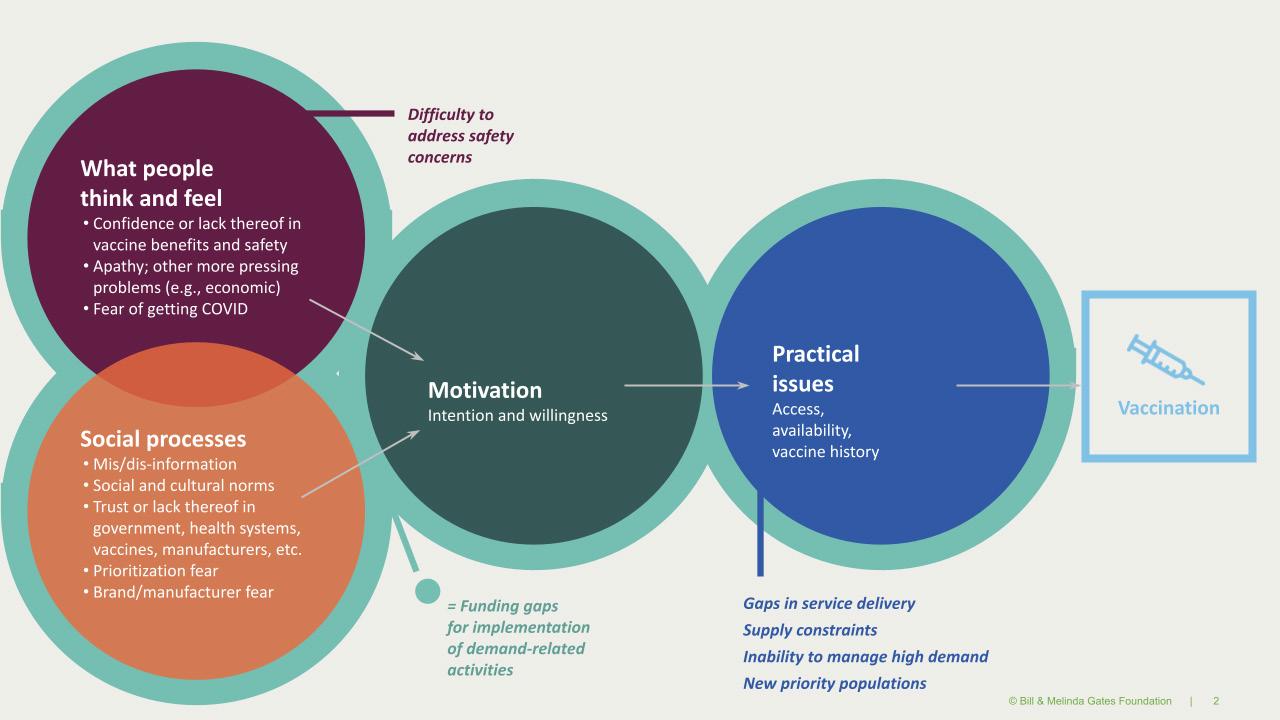
According to Brewer et al., the available evidence (as of 2017) on using behavioral science interventions to increase vaccination suggests that the most effective interventions focus not on individuals’ thoughts and feelings, but rather on reducing barriers and directly facilitating action. In terms of reducing barriers, Brewer et al. list a number of obstacles individuals may face when seeking to get vaccinated: lack of reliable transportation or childcare, inconvenient clinic opening times, language barriers, and cost (even if a vaccine is “free,” the opportunity cost of missing wages can be steep). Interventions meant to reduce these barriers might include setting up mobile vaccination clinics or using defaults. An example of default-setting is presumptively scheduling people for vaccine appointments and giving them the option to reschedule or cancel their appointment by phone, which had a significant effect on vaccine uptake in one randomized trial.iv
In terms of directly facilitating action, Brewer et al. emphasize that even people who are favorably inclined toward vaccination often fail to follow through on their intentions to get vaccinated,
which implies that interventions meant to close the intention-action gap can help increase uptake. The authors cite studies finding that telephone reminder/recall systems worked well in this respect, and that such reminders were most effective when managed by a centralized health institution and endorsed by patients’ providers. Healthcare provider recommendations and presumptive announcements have also been shown to be effective at increasing vaccination, especially among hesitant individuals: “By framing vaccines as routine care, presumptive announcements speed the decision process for people with positive vaccination intentions. For people who are hesitant or opposed to vaccination, the process will slow down, allowing them to ask questions and the provider to ease their concerns.”v Finally, using incentives, such as rewards for getting vaccinated or penalties for remaining unvaccinated, and vaccine requirements can be effective interventions, but the authors caution: “[D]epending on the prevailing reasons for undervaccination in a population, it may be sufficient or more advisable to apply other less coercive measures.”vi
i Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing Vaccination: Putting Psychological Science Into Action. Psychological science in the public interest: a journal of the American Psychological Society, 18(3), 149. https://doi.org/10.1177/1529100618760521
ii Black, T. & Pituch, J. (2021, October 22). Personal communication [Zoom interview].
iii Goldstein, J.A., Grossman, S., & Startz, M. (2021, October). Belief in COVID-19 Misinformation in Nigeria. Manuscript under review. Abstract available at: https://www.sites.google.com/site/shelbygrossman//papers/
iv Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017).
v Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017).
vi Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017).
To effectively mitigate the potential consequences of COVID-19 vaccine hesitancy caused by misinformation, we must first clearly define the problem. Put simply, misinformation is any content that is false or misleading.i Key features include unverified or false content, information shared with no background context, conspiracy theories, and poor quality content, regardless of source.ii Misinformation can also take subtler forms, such as content that is only partially accurate, or that contains plausible-sounding half-truths. In the context of COVID-19 vaccines, misinformation often comes from hearsay or news stories from unverified or unreliable sources, as well as from social media through one’s social circles.iii
The WHO has stated that rumors and conspiracy theories online continue to undermine pandemic response efforts, and that social media is often a vector
of misinformation.iv In addition, it has become increasingly clear that some parties are deliberately proliferating false narratives to cause discord and to discredit public officials for political gain.v,vi Here, it is important to note a distinction: whereas misinformation simply contains falsehoods regardless of source or intention, disinformation is a subset of misinformation that involves deliberately spreading fake news for purposes such as attempting to sway public opinion or diminish public trust. Disinformation is spread online by both foreign and domestic actors, often for political reasons. Empirical studies have shown a significant link between foreign disinformation campaigns and vaccine hesitancy.vii Regardless of the type of misinformation, our goal is to gauge the impact of misinformation-related vaccine hesitancy and devise strategies to combat it.
i Vraga, E., & Bode, L. (2020). Defining Misinformation and Understanding its Bounded Nature: Using Expertise and Evidence for Describing Misinformation. Political Communication. 37(1), 136-144. https://doi.org/10. 1080/10584609.2020.1716500
ii WHO & Pan-American Health Organization. (2020). Understanding the infodemic and misinformation in the fight against COVID-19: Digital Transformation Kit, Knowledge Tools.
iii Alaoui, S. (2020). Immunizing the public against misinformation. United Nations Foundation.
iv WHO & Pan-American Health Organization. (2020).
v Bliss, K.E. & Morrison, S.J. (2020). The Risks of Misinformation and Vaccine Hesitancy within the Covid-19 Crisis. Center for Strategic and International Studies (CSIS).
vi Tagliabue, F., Galassi, L. & Mariani, P. (2020). The “Pandemic” of Disinformation in COVID-19. SN Comprehensive Clinical Medicine, 2, 1287–1289. https://doi.org/10.1007/s42399-020-00439-1
vii Wilson, S.L., & Wiysonge, C. (2020). Social media and vaccine hesitancy. BMJ Global Health, 5(10). http://dx.doi.org/10.1136/bmjgh-2020-004206
What are the best methods for measuring online misinformation? In this box, we briefly review some techniques used in the literature and offer some of our own.
We can measure COVID-19-related misinformation and vaccine hesitancy in terms of people’s exposure to misinformation (whether they have heard of different misinformation narratives or conspiracy theories); their stated beliefs in misinformation or conspiracy theories (whether they believe misinformation); and their behavior when it comes to sharing that misinformation (whether they forward, repost, or otherwise spread misinformation narratives online).
The 2021 Africa CDC study surveyed people about whether they had heard of popular but false narratives
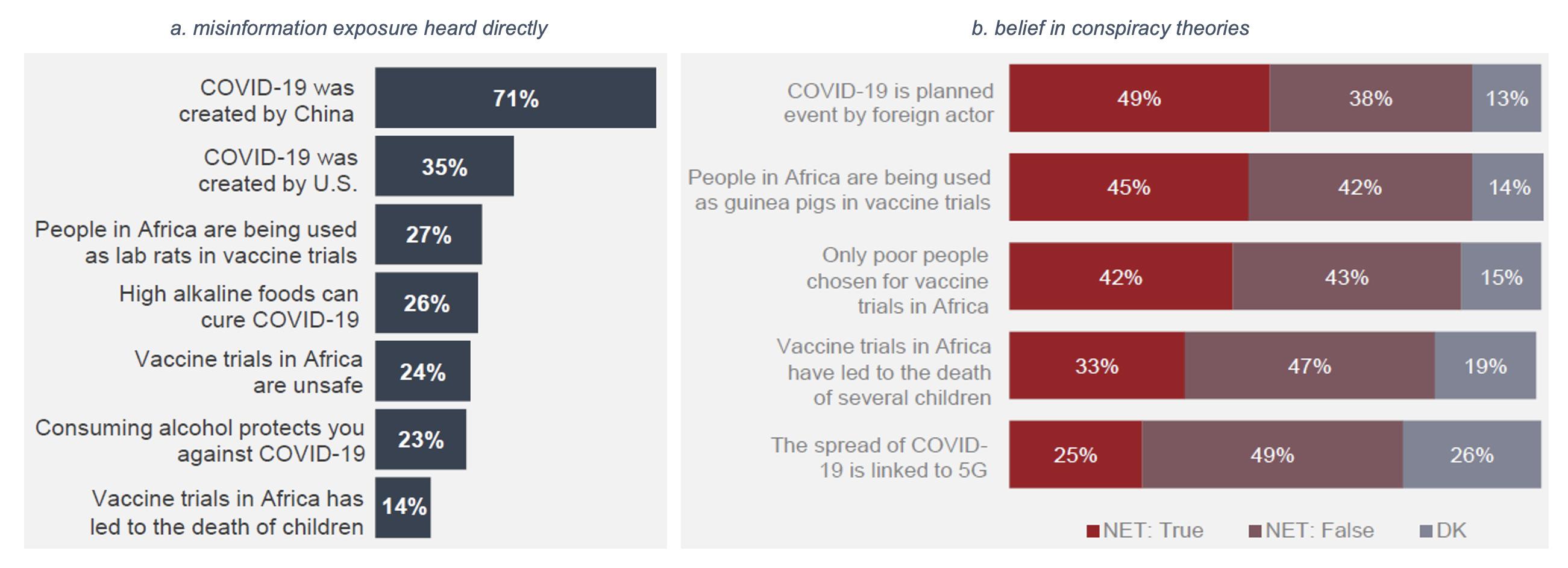
surrounding COVID-19 and vaccines, as well as the extent to which people believed this misinformation. In all parts of the continent studied except West Africa, online sources were the most popular sources of information, with social media comprising a significant proportion. Demographically, men (44%) and young people between the ages of 18 and 24 (51%) were on average more likely to report getting their information from online sources, including social media platforms like WhatsApp. Furthermore, those more susceptible to misinformation were also more likely to rely on online sources and to trust social media as their main source.i
The survey found that there has been widespread exposure to conspiracy theories, as well as a sizable minority who believe in them (Figure 1.2).
Source: Africa CDC. (2021).
Thus, by surveying people about their exposure to different conspiracies, researchers can gauge the relative popularity of different misinformation narratives. Furthermore, asking whether people believe those narratives can help researchers estimate the potential impact that misinformation has on people’s opinions of the vaccine. Similar to the method followed by Schmelz and Bowles, survey questions could ask about respondents’ beliefs, their willingness to accept a COVID-19 vaccine, and whether or not they are aware of popular misinformation in circulation.ii Surveys should also measure demographic characteristics such as age, education level, vaccination status, and attitudes toward COVID-19
vaccines, thereby allowing researchers to study trends across demographic and other characteristics. The table below outlines some questions researchers can use to measure misinformation.
Using the questions and metrics in the table below could help researchers evaluate how many or what percentage of people believe misinformation, social norms around belief in misinformation, and individuals’ attitudes toward vaccination. If a particular population segment exhibits both high hesitancy and high rates of belief in misinformation relative to other groups, then they could be targeted for further study and, if feasible, intervention.
Exposure Average agreement/exposure rate (%) to misinformation
Beliefs Average agreement rate (%), supporting misinformation
How strongly beliefs are held about certain pieces of misinformation
Social norms around belief in misinformation
Average agreement rate (%), misinformation-associated hesitancy
Vaccine uptake rates or vaccination status (%)
Have you heard of [Conspiracy X]?
Do you believe [Conspiracy X] is true?
How confident are you in your belief that [Conspiracy X] is true?
Do you feel that this belief is accepted in your community?
Given what you heard, are you hesitant to get a COVID-19 shot?
Have you had the vaccine? If not, do you support it?
Source: Princeton team.
i Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a-15-country-study/ ii Schmelz, K. & Bowles, S. (2021, June). Overcoming COVID-19 vaccination resistance when alternative policies affect the dynamics of conformism, social norms, and crowding out. PNAS, 118(25). https://doi. org/10.1073/pnas.2104912118
We conducted our literature review using a snowball approach. Our team reviewed over 60 scientific publications on misinformation and public health related to COVID-19 and other infectious diseases. The most relevant of these publications are discussed below, and detailed information on 36 of our source articles can be found in a separate attachment. In addition, we have consulted researchers and practitioners in the fields of medicine, health policy, misinformation, behavioral science, and international development. Our interviewees hail from institutions including the Center for Strategic and International Studies, Stanford University, and the Bill and Melinda Gates Foundation and are listed in our Acknowledgments.
In this section, we review literature on the processes, mechanisms, and beliefs that enable two related behaviors that we seek to disrupt. The first behavior is believing misinformation about COVID-19 encountered online. The second is sharing that misinformation with others. By examining the factors that enable these behaviors, we hope to assist the eMBeD team in diagnosing the sources of vaccine hesitancy in various contexts and, in turn, identifying
opportunities and methods for intervention. We have identified five enablers of misinformation belief and sharing behaviors:
• Health concerns and risk perceptions
• Low trust in institutions
• Automatic thinking and heuristics
• Social processes
• Cultural and religious beliefs
In addition, understanding the particular underlying drivers of COVID-19 vaccine hesitancy among various populations in sub-Saharan Africa is critical to intervention design. High-quality diagnostics can provide insights into locally and demographically specific COVID-19 vaccine attitudes, beliefs, and behaviors. Practically, conducting diagnostics involves use of diverse tools, including surveys, face-to-face interviews, observational data, and data on demographics, service use, problem or issue tracking, and epidemiology.14 Data should ideally be collected frequently and on an ongoing basis, given the rapid evolution of the pandemic and hesitancy patterns. For example, the Johns Hopkins COVID Behaviors Dashboard, which presents data from global surveys of COVID-19 knowledge, attitudes, and practices, is updated on a bimonthly basis.15 Additionally, data from 343 (and counting) quantitative studies conducted globally is aggregated on the Risk Communication and Community
Engagement platform and updated monthly.16 While diagnostics can shed light on which interventions are likely to be most effective in preventing certain groups from believing and sharing misinformation, it is crucial to take note of the regional diversity in sub-Saharan Africa and differences among countries that may not be fully captured by the studies and surveys presented in this section.
Among the most prevalent enablers of vaccine hesitancy in sub-Saharan Africa are concerns about health and safety. These concerns can distort individuals’ perceptions of the potential risks and benefits of getting vaccinated against COVID-19. As Brewer et al. explain, multiple factors influence an individual’s vaccination decision. Examples include the perceived likelihood of getting infected; the perceived severity of the disease if one does get infected; and affective risks such as worry, anxiety, and fear.17
With regard to the perceived likelihood of getting infected, research suggests that a combination of true information and misinformation has led many Africans to underestimate the risk that COVID-19 infection poses to people in sub-Saharan Africa. It is true that, while countries like the United States, Brazil, and much of Western Europe were devastated in the early months of the pandemic, Africa was largely spared. As Dzinamarira et al. explain, “The low effect at a personal level of COVID-19 in its first wave in Africa contributed to a widespread belief that COVID-19 is overwhelmingly not an African
problem.”18 South Africa, of course, has been a notable exception to this trend. Unfortunately, the disease’s lack of early penetration in most of sub-Saharan Africa has fueled myths that threaten the success of vaccination efforts in the region. These myths include that COVID-19 only kills non-Africans; that it does not affect young people; and that traditional African remedies work as well as or better than vaccines to prevent COVID-19.19 Researchers from the Africa Center for Strategic Studies have emphasized the need to tackle these myths directly: “Restoring trust in the COVID vaccine campaign will require pushing back against vaccine myths and creating an environment of people-centered, transparent, and inclusive vaccine outreach.”20
Besides misinformation, a lack of information also appears to be contributing to COVID-19 vaccine hesitancy. In a 15,000-person, 15-country survey conducted between August and December 2020 by the African Union and the Africa CDC, over half of respondents considered themselves either “not very well” or “not at all” informed about the development of COVID-19 vaccines.21 Individuals who are not well informed about the vaccines’ development may be more susceptible to misinformation narratives that contradict the overwhelming scientific evidence that COVID-19 vaccines are safe and effective. Consequently, a lack of accurate information about the vaccines can lead people to make vaccination decisions based on misleading narratives that portray the vaccines as unnecessary or even harmful. Unsurprisingly, beliefs about the vaccines’ safety are closely correlated with vaccination intentions: in the Africa CDC survey, among respondents who indicated they would
reject the vaccine, 60% said they believed it was not safe, compared to 16% of those who intended to accept a vaccine.22
Concerns about the safety of COVID-19 vaccines tend to be rooted in a combination of true and false information. In addition to the aforementioned 1996 Pfizer drug trial in northern Nigeria that killed 11 children, the temporary pause of the AstraZeneca COVID-19 vaccine in several European countries following reports of a rare but serious blood-clotting side effect caused lingering doubts about the vaccine’s safety among many Africans.23 Unfortunately, misinformation about the purported health risks of COVID-19 vaccines have exploited the reasonable misgivings that incidents like the Pfizer trial and the AstraZeneca pause have created for many Africans.
Researchers from the Africa Center for Strategic Studies provide several examples of such misinformation:
One myth holds that live viruses are injected into the body and that individuals can die after vaccination. Another says that the vaccines cause infertility or serious side effects that are worse than contracting the virus. Other conspiracy theories hype that the vaccines are in fact poisons that alter the DNA to reduce Africa’s population. They also claim that vaccines are a cover to implant traceable microchips, and that Microsoft founder Bill Gates and the U.S. government are behind it.24
The cumulative effect of this misinformation and lack of information appears to be causing many people to overweight the costs and underweight the benefits of accepting a vaccine against COVID-19. This is evident in the fact that, in the 15-country survey by
the African Union and the Africa CDC, about half of the more than 15,000 respondents felt that the threat of COVID-19 had been exaggerated. This view was particularly prevalent among men, young people, and people who cited social media as a trusted source of information.25
Notably, health-related concerns about COVID-19 vaccines do not necessarily translate to hesitancy about vaccines more generally. Many people in subSaharan Africa—a region with a history of remarkable vaccination success stories—view COVID-19 vaccines as less safe than other types of vaccines. Although women in the region have higher levels of vaccine confidence in general compared to men, they appear to be more skeptical when it comes to COVID-19 vaccines.26 Additionally, in one study in Zambia, just 66% of parents and other caregivers who brought their children to a measles-rubella vaccination site indicated that they planned to receive a COVID-19 vaccine, which seems indicative of fears about the novelty of the COVID-19 vaccines. Yet a much larger share—92%—of the caregivers said that they intended to have their children vaccinated against COVID-19.27 This suggests that vaccine hesitancy may be due in part to a perception that vaccines are helpful for children, but unnecessary or even harmful for adults. As the study’s authors explain, “Agreeing to vaccinate a child likely reflects confidence in the vaccine, while refusal to self may reflect a lower perceived risk to personal health. Targeted messaging will be required to capture a population less familiar, and possibly less comfortable, with receiving vaccines.”28
Concerns about infertility are also dominant across the continent.
Popular misinformation narratives have suggested that the COVID-19 vaccine contains abortion drugs.29 Concerns about fertility can be shaped by mental models that women in particular may have. One expert, pointing out that many African women’s only adult encounter with injections is as a contraceptive method, suggested that a mental model in which shots are either for children or for birth control may contribute to fertility-related fears surrounding COVID-19 vaccines and their possible side effects.30 In addition, the thought of a new medicine affecting one’s ability to have children can evoke a particular fear for women living in communities where their identity as a mother is regarded as a central aspect of womanhood.31
For individuals who are hesitant about COVID-19 vaccines due to health concerns, research suggests that trusted messengers can help dispel misinformation and provide accurate information about the vaccines. This in turn can help individuals recalibrate their vaccine risk assessments to better account for the true benefits and risks of accepting a vaccine. Research by Brewer et al. suggests that recommendations from healthcare providers in particular are strongly associated with vaccination behavior, in part because these recommendations “may affirm or augment people’s perceptions of the value and safety of the vaccine.”32
In addition to enlisting healthcare providers as vaccine proponents, Nsoesie and Oladeji suggest several actions that social media companies could take to promote credible information and remove misinformation about COVID-19 vaccines from their sites. The researchers argue that algorithms could better identify and remove misleading content if the
algorithms were designed to recognize the similarities and differences in the framing of misinformation about COVID-19 transmission, prevention, treatment, and vaccination. Beyond these measures, the researchers encourage interventions aimed at increasing public understanding of the possible adverse health effects of misinformation. They write: “Health misinformation should be incorporated into digital education curriculum to educate the public on how to find, assess, validate, and corroborate information from trusted sources before adopting recommendations seen on social media platforms.”33
This recommendation appears repeatedly in the relevant literature. For instance, Brewer et al. urge policymakers to try to instill accurate knowledge and understanding of vaccines as much as possible before misinformation has a chance to spread in a community.34 This proactive approach is related to the “prebunking” or “inoculation” style of intervention that seeks to get out in front of misinformation. It reflects the reality that changing someone’s mind once they have already formed an opinion about a controversial topic is typically more difficult than nudging an individual toward a position on an emerging topic. As van der Linden et al. succinctly put it, “Prevention is better than cure. This is true as much for diseases as it is for the spread of misinformation.”35 As evidence, the researchers report that in one study of “prebunking” versus “debunking” interventions, “vaccination intentions only improved when participants were presented with anticonspiracy arguments prior to exposure to the vaccination conspiracy theories but not when presented with counter arguments afterward.”36
misinformation about COVID-19 vaccines, policymakers should take care to avoid interventions that might inadvertently backfire. Brewer et al. caution against two such approaches. The first is using pharmaceutical companies to reassure people about the safety and efficacy of vaccines. Evidence suggests that people do not perceive vaccine manufacturers as credible sources in this context, and the reassurances can actually increase suspicions that the vaccines are risky and/or ineffective. The second approach is relying on fear to motivate vaccine behavior. Brewer et al. cite evidence that suggests that fear communication can elicit anger, which undermines the effectiveness of the intervention.37
Concerns about the safety of COVID-19 vaccines remains the most cited reason for hesitancy both globally and in subSaharan Africa. Recent data show that on average, approximately 57% of vaccinehesitant individuals globally and 54% in Africa are worried about side effects, with the proportion ranging from 73% in Côte d’Ivoire to 40% in Tanzania.38 In the previously described 15-country study by the Africa CDC, researchers asked respondents if they agreed with the following statements to measure perceptions of vaccine safety:
• “COVID-19 vaccines are safe.”
» Responses among people who report willingness to accept a COVID-19 vaccine: 84% “yes”; 14% “no”; 2% “don’t know”
» Responses among people who report unwillingness to accept a COVID-19 vaccine: 59% “yes”; 37% “no”; 4% “don’t know”
This mixed-method study utilized faceto-face and telephone interviews to gather responses from at least 1,000 respondents per country. The top five most common reasons respondents gave for not wanting to take a new COVID-19 vaccine were:
• “I do not trust the COVID-19 vaccine”;
• “I do not believe that the virus exists”;
• “I am concerned about the safety of the vaccine”;
• “I do not feel that I am at risk of catching the virus”; and
• “I do not have sufficient information to make a decision”.39
COVID Behaviors Dashboard suggests similar concerns. The most common reason given for vaccine hesitancy in the WHO African Region is “concern about side effects”, reported by 54% of respondents, followed by “plan to wait to see if it’s safe” (Table 2.1).
Source: COVID Behaviors Dashboard.
Note: Individuals who reported they would probably, probably not, or definitely not get vaccinated were asked about the reasons for their decision.
Source: The Collective Service for Risk Communication and Community Engagement.
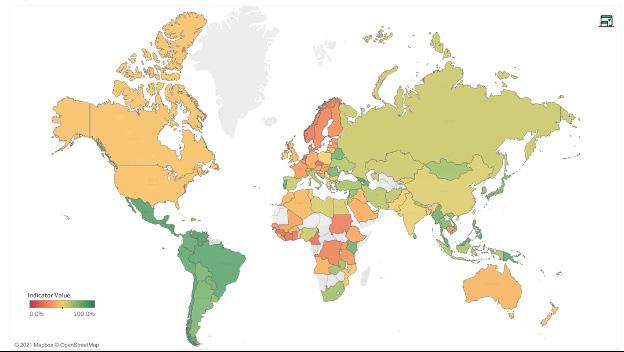
At the same time, risk perception varies widely by region within Africa. Data from Risk Communication and Community Engagement (RCCE) shows that close to half of all respondents in East and Southern Africa believe they are at risk of contracting COVID-19, compared to 39% in West and Central Africa—where vaccine hesitancy prior to the pandemic had been higher.40, 41 In the map above from the RCCE database, East and Southern African countries are mostly shaded green and orange, indicating a higher fraction of individuals who believe they are at risk of contracting
COVID-19. By contrast, many countries in Central and West Africa are shaded red, indicating lower risk perception among surveyed individuals.
Table 2.2 breaks down the percentage of survey respondents in each country who believe they are at risk of contracting COVID-19. Countries such as Mauritius and Kenya have relatively high risk perception, at 89% and 75%, respectively, while Guinea and Côte d’Ivoire have the lowest risk perception in the region, at approximately 20%.
Percentage of individuals who believe they are at risk of contracting COVID-19 (October 2021)
Source: The Collective Service for Risk Communication and Community Engagement.
Concerns about side effects and risk perception can also be driven by exposure to and belief in misinformation. Mental models shape the way people process misinformation. For example, polled respondents in Africa cite recurring disinformation narratives:
• “COVID-19 is a planned event by a foreign actor.” (49% “true”; 38% “false”; 13% “don’t know”)
• “People in Africa are being used as guinea pigs in vaccine trials.” (45% “true”; 42% “false”; 14% “don’t know”)
• “[COVID-19] Vaccine trials in Africa have led to the death of several children.” (33% “true”; 47% “false”, 19% “don’t know”).42
• “People in Africa are being used as guinea pigs in vaccine trials.” (45% “true”; 42% “false”; 14% “don’t know”)
• “[COVID-19] Vaccine trials in Africa have led to the death of several children.” (33% “true”; 47% “false”, 19% “don’t know”).43
Broadly, data suggests that concerns about the health and safety of COVID-19 vaccines and underestimates of the threat the disease poses lead many Africans to feel hesitant about accepting a COVID-19 vaccine. Additionally, populations in West and Central Africa have lower risk perception of COVID-19 compared to their counterparts in East and Southern Africa. These disparities may be due to lower access to factual information about COVID-19 in West and Central Africa; higher rates of disinformation circulating on social media platforms; and/or deeperseated factors such as a lack of trust in government, foreign actors, and the medical establishment.44 The issue of trust is discussed in greater detail in the next subsection.
Earlier, we described a 15-country survey by the African Union and the Africa CDC that surveyed over 15,000 individuals and examined sources of vaccine hesitancy in Africa. In large part, the study attributes vaccine hesitancy among respondents to doubts about the safety and efficacy of COVID-19 vaccines and misinformation about the disease.45 Similarly, Afrobarometer conducted a survey from October 2020 to January 2021 in which researchers collected responses from 6,000 individuals—1,200 per country—in five West African countries: Benin, Liberia, Niger, Senegal, and Togo. As was mentioned earlier, that study found that just four in 10 respondents indicated they were likely to accept a COVID-19 vaccine, and that lack of trust in government institutions drives much of the concern about vaccine safety. According to Seydou of Afrobarometer, “Vaccine hesitancy/ resistance skyrockets alongside doubts about the government’s ability to ensure that vaccines are safe…Large majorities in Niger (89%), Liberia (86%), and Senegal (71%) believe that prayer is more effective than a vaccine in preventing coronavirus infection.”46
Lack of trust has developed for many reasons. First, memories of colonization and other abusive political and economic practices committed in Africa by foreign powers are deep-rooted. Research has shown that countries in Central Africa that were targets of invasive colonial medicine projects involving painful and damaging forced procedures have lower acceptance of vaccination and blood tests today.47 Additionally, as was mentioned earlier, West Africans are
particularly distrustful of new vaccines after an experimental meningitis vaccine tested by Pfizer in 1996 killed 11 children and paralyzed dozens more in northern Nigeria.48 That tragedy resulted in drastic reductions in routine vaccinations for tuberculosis, tetanus, measles, and polio, and set back the global goal to eradicate polio by a decade.49 Since this historical episode is a part of recent memory for the region, it potentially has reinforced mental models that shape the way people receive and process misinformation. For example, some misinformation narratives circulating today suggest that Africans are being used as guinea pigs (45% of polled respondents believe this to be true) or that COVID-19 vaccine trials in Africa have led to the death of several children (33% believe this to be true).50
Where people get their information also plays a significant role in shaping individuals’ attitudes toward vaccines and their exposure to misinformation. In the Africa CDC study, 64% of respondents listed television as one of their most trusted sources of information about COVID-19; 51% listed radio (61% in West Africa); 41% listed online sources; 23% listed health bodies; and just 18% listed government sources. The survey also found that “[o]nline channels, particularly social media, tend to be the most trusted source among hesitant groups,” and that misinformation about COVID-19 “appears to be widespread, with those who self-report exposure to rumors also showing a higher propensity to believe them.”51 Additionally, trusted information sources vary across countries and across demographic groups; for example, older respondents were more likely to trust healthcare bodies and government sources, while online sources tend to be trusted more by men and by young people.52
The reasons for lack of trust vary across countries, communities, and individuals. For example, distrust in powerful foreign institutions and conspiracy theories about efforts to “depopulate” Africa have led to pervasive concerns about COVID-19 vaccines causing infertility across the continent. Similarly, recurrent misinformation narratives have suggested that the COVID-19 vaccines contain abortion drugs.53 Misinformation about COVID-19 vaccines being dangerous and harmful for Africans is particularly pernicious because such content is spread using highly sophisticated techniques on social media, such as content modification, coordinated copy-pasting across dozens of groups with thousands of users, coordinated link sharing, and crossplatform posting within a few hours or days, resulting in tens of thousands of shares.54 This mass amplification of misinformation erodes trust in the very institutions tasked with delivering COVID-19 vaccines in Africa. Data shows that mistrust in institutions and external actors is strongly linked to vaccine refusal, especially among individuals who are more educated, younger, urban, and social media users.55
In-group and out-group attitudes also play a significant role in trust in COVID-19 vaccines. The groups that individuals identify with may have an effect on their behavior during the COVID-19 pandemic, including the decisions to wear masks, socially distance, and accept a COVID-19 vaccine. In-group bias is the tendency for individuals to give preferential treatment to members of their own group, as well as disregarding or actively harming outgroups. Perhaps most significantly for our work, that preferential treatment includes increased trust inof fellow in-group members. In-group bias is
based on social identity theory, which postulates that individuals construct a large part of their identities through their membership in groups.56 Research on vaccine-rejecting parents in Australia (conducted before the COVID-19 pandemic) showed that these parents constructed themselves and their vaccine-rejecting peers as an in-group important to their sense of identity, and considered vaccinators as an outgroup, thinking of them as the “Unhealthy Other.”57 Research on social identity and in-groups also tells us that people are more likely to trust individuals within their in-group and to distrust, and less likely to trust individuals in the outgroup. As a result, traditionally vaccinerejecting individuals are unlikely to trust messages coming from out-group members. Depending on the country context, as COVID-19 vaccination rates increase and certain demographics in sub-Saharan Africa begin to be more likely to be vaccinated compared to others, it is possible that in-group/outgroup dynamics will also emerge along the lines of vaccination status.
While it is difficult to debunk misinformation once it is widespread, an important step articulated by Kumar and Geethakumari is “identifying the most influential nodes whose decontamination with good information would prevent the spread of information.”58 Early detection campaigns, proactive countermessaging, and communications that address deep-seated issues of trust with actors and institutions connected to vaccines are all vital in weakening belief in the misinformation presented and ultimately reducing vaccine hesitancy. Therefore, bolstering the legitimacy of these institutions among populations exposed to certain disinformation narratives will be necessary to stem hesitancy in the long-term. Bolstering
legitimacy entails having a recognized justice and dispute resolution system that is seen as fair, a consistent provision of basic services for citizens, the assurance of physical security for civilians, and governing institutions that are deemed accountable to citizens.59 Achieving this essentially means systemic change throughout the continent. For the time being, in order to curb vaccine hesitancy in the short-term, it is important to rely on institutions and individuals that are trusted by individuals who are prone to vaccine hesitancy. These trusted individuals may include religious leaders, local healthcare providers, and some intergovernmental officials from organizations like the WHO.
Additional research from Australia conducted by Cruwys et al. found that people indicated a greater willingness to take a vaccine and perceived it to be less risky when it was developed by an ingroup rather than an out-group source.60
The research included two prospective surveys and one experiment. In the experiment, which took place before any COVID-19 vaccines were available, the researchers tested respondents’ willingness to get a vaccine when the vaccine was developed by Australians (in-group, treatment 1) as compared to the French (out-group, treatment 2). The authors note that not all outgroups are the same. For example, most Australians perceive the United States to be a higher-status country, and France to be a similar-status country. The authors intentionally chose France, and they found that respondents were indeed more willing to accept a vaccine developed by in-group members—fellow Australians—compared to French outgroup members. When considering this research in the context of sub-Saharan Africa, one needs to carefully consider how different out-groups are perceived,
including the various countries that have produced COVID-19 vaccines. Cruwys et al. limited their study to Australian participants, meaning that we should be cautious about external validity for sub-Saharan Africa. However, despite being conducted in a different context, the study’s implications are important to consider in sub-Saharan Africa. The authors interpret their results to mean that the tendency to trust in-group members can be harnessed to improve COVID-19 public messaging.
As noted in the literature review, trust—or lack of trust—can shape how misinformation “sticks” in people’s minds. Therefore, identifying the trustworthy entities conveying vaccine-related information is important to reduce misinformation that would otherwise hinder vaccine acceptance. Trust in institutions varies depending on each individual’s socioeconomic, religious, and racial background, and their level of trust also varies across institutions. Among different institutions, governments and how they are perceived by their citizens provide a notable insight into expected vaccine uptake.
Afrobarometer’s survey on five West African countries asked respondents about their trust in government in relation to their vaccine acceptance.
• “How much do you trust the government to ensure that any vaccine for COVID-19 that is developed or offered to citizens is safe before it is used in this country?” (68% Not at all/Just a little; 31% Somewhat/A lot)
• “If a vaccine for COVID-19 becomes available and the government says it is safe, how likely are you to try to
get vaccinated?” (44% Very unlikely; 16% Somewhat unlikely; 19% Somewhat likely; 20% Very likely)
Using these questions, Afrobarometer was able to compare vaccine hesitancy and resistance in relation to people’s trust in government. They found that vaccine hesitancy or reluctance runs high where people highly doubt “the government’s ability to ensure that vaccines are safe.”61 The high (negative) correlation between people’s trust in government and vaccine acceptance rate is consistent with studies focused on other regions, such as North America and Asia.62
Identifying the most trusted sources of information about COVID-19 is a key step in dispelling or correcting misinformation. The Johns Hopkins COVID Behaviors Dashboard provided eight trusted sources as answer choices in its related question.
• “How much do you trust the following sources to provide accurate news and information about COVID-19?” (Trusted sources: local health workers and clinics; scientists and other health experts; WHO; government health authorities or officials; politicians; journalists; friends and family; and/ or religious leaders)63
The Dashboard uses a two-by-two grid, using exposure level (“the percentage of people who get information from that source”) and trust level as the axes.64 WHO data from the African region shows that local health workers, scientists, and other health experts, on average, are trusted information sources (Figure 2.2). The country-specific graphic provides insight into how messaging can have varying effects on the national and
local levels, as well as into which sources would likely be effective carriers of messages and interventions correcting misinformation.
Data indicates that the WHO is generally regarded as a more trusted information source than government health authorities or officials in Africa. The country-level differences in trust
levels in government and international health organizations are important to note, however. This is consistent with the findings from the Africa CDC’s 15-country survey (Figure 2.3), which notes “regional differences are evident, suggesting that a country-specific approach would be necessary" when advocating for vaccine safety and effectiveness.65
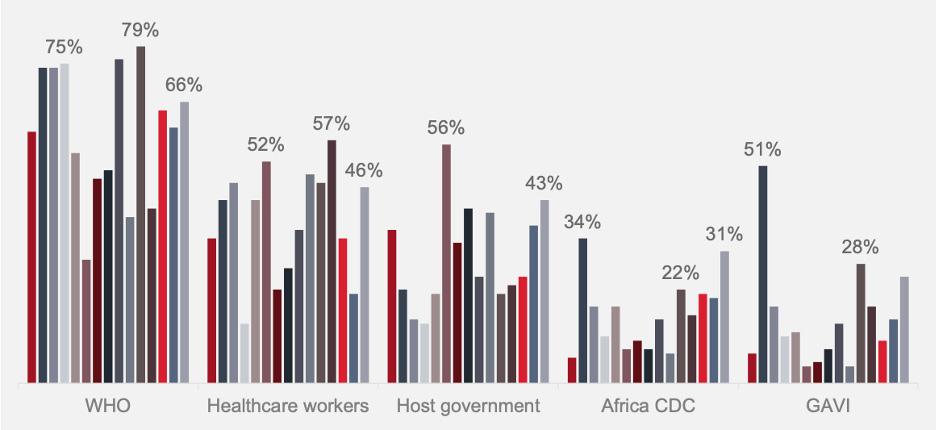
Note:
Source: COVID Behaviors Dashboard.

Note: Results for the period from Nov 1 to Nov 15, 2021
Source: Africa CDC. (2021).
Depending on the country-specific or regional context, survey questions can be worded to attempt to gauge how people’s socioeconomic, racial, religious, and/or geographical background has contributed to their trust in institutions. In the United States, where many people of color have had negative experiences within the healthcare system due individual and systemic racism, people’s perception of fairness in the medical system can be asked in relation to race, as in Surgo Ventures’s survey question: “How strongly do you agree/disagree that people of your race are treated fairly in a healthcare setting?”66 A variation of this question could be utilized to test people’s trust in the healthcare system that is context-variant. Given this paper’s geographical focus on subSaharan Africa as a whole, it is important to note the varying degrees of impact different identity markers will have in various countries and regions. While a question tailored for the specific country or community of focus is recommended, a two-part question could account for some heterogeneity of the survey region when conducted across many countries:
• A. How strongly do you agree/ disagree that people with the same identity as you are treated fairly in a healthcare setting?
• B. What identity are you referring to in Part A?
Answer choices for Part B of this sample question can include: country, race, gender, tribe, ethnic group, religion, and economic status. These answer choices are inspired by questions included in the Afrobarometer Round 8 survey in South Africa, specifically in its “Identity and society” section.67 The order of Parts A and B will anchor the survey respondents in different ways.
Literature review
When individuals encounter information online, especially on social media, how carefully do they consider its veracity? Do they engage their deliberative system of thinking, expending mental effort to consider indicators of credibility? Or do they engage in “automatic thinking,” absorbing the information without concentrating on whether or not it is likely to be true?68 Might individuals choose to share misinformation without going through the cognitively effortful process of attempting to ascertain whether or not it is true?
Depending on the answers to these questions, we may conclude that automatic thinking drives individuals to believe online misinformation, to share it on social media, or both. The implication is that if individuals paused and engaged in deliberative thinking, they would be less likely to believe and/ or share misinformation online.
This was the conclusion of a review article by Pennycook and Rand in which the researchers synthesized existing literature on online misinformation and found that “poor truth discernment is associated with lack of careful reasoning and relevant knowledge, and the use of heuristics such as familiarity”—trademarks of automatic thinking.69 The authors concluded that a large proportion of misinformationsharing online happens as a result of this automatic thinking process. They also reported findings that a simple intervention designed to address inattention—asking participants to rate the accuracy of each headline before deciding whether or not to share it—
reduced the sharing of misinformation by 51% relative to a control group.70 To state these results in a different way, according to Pennycook and Rand, automatic thinking is largely responsible for the sharing of misinformation; therefore, interventions that combat automatic thinking by forcing people to pay attention to the veracity of the content they encounter should reduce misinformation sharing.
An additional study that appears to support the hypothesis that automatic thinking drives misinformation sharing behavior comes from Rosenzweig et al. The researchers found that feeling any emotion, and particularly happiness and surprise, was positively correlated with belief in and sharing of false, relative to true, headlines.71 Emotional responses are a key component of automatic thinking; they drive impulsive, nondeliberative thought processes and decision-making.
Both Pennycook and Rand and Rosenzweig et al. focused on misinformation sharing behavior, rather than belief. It is not clear from their research that interventions designed to combat automatic thinking might work uniformly to interrupt both individuals’ belief in and their sharing of misinformation. Indeed, Pennycook and Rand note the “substantial disconnect between what people believe and what they share on social media.”72
This disconnect has also been observed in the specific context of COVID-19 misinformation behaviors in two subSaharan African countries. Wasserman and Madrid-Morales surveyed approximately 1,967 individuals in Kenya and South Africa in April 2020 and found that a significant percentage of respondents showed an interest in
sharing misinformation about COVID-19 online, even if they did not believe the content. The researchers report: “The most common motivation to share these social media posts was a perceived moral or civic duty to share information (whether true or not) and raise awareness about an issue. There was also a desire to spark debate and solicit other people’s views. Many respondents also said they would share misinformation for fun or entertainment.”73 Given these findings, it seems likely that at least for some people, the threshold for sharing social media content is lower than the threshold for actually believing it.
If automatic thinking is a major contributor to sharing misinformation, can educative interventions decrease misinformation sharing? The approach proposed by Pennycook and Rand— prompting social media users to pay attention to content veracity before they share—is a top-down intervention that hinges on the use of sites such as Facebook and Twitter, where the platform can flag misleading content and deliver prompts directly to users. In developing countries such as India, however, encrypted messaging services like WhatsApp are much more popular. Consequently, top-down interventions are less feasible on these services. Considering the challenge of encryption, educative interventions that encourage user-driven learning and fact-checking offer another possible path to curbing automatic thinking and misinformation sharing.
Evidence on such an approach comes from an experiment by Badrinathan in India, in which participants received a media literacy training program intended to improve their ability to identify misinformation. The intervention was designed to mitigate
some of the effects of automatic thinking by teaching individuals how to use deliberative thinking processes to identify misinformation. However, Badrinathan found that the intervention did not, in fact, significantly increase recipients’ ability to correctly identify misinformation. Further, among one important subgroup—supporters of the Bharatiya Janata Party (BJP), to which the current Indian prime minister belongs—the intervention actually reduced recipients’ ability to identify pro-attitudinal stories as false.74 This “backfire effect” suggests that, at least for BJP partisans, encouraging deliberative thinking may not be enough to dislodge belief in misinformation. In some contexts, motivated reasoning and identity-based cognition heavily influence belief in misinformation.75
Badrinathan’s findings demonstrate the importance of both identitybased cognition and consideration of local context when designing misinformation interventions. Slowing down automatic thinking and shifting to deliberative thinking may not be enough. Interventions that work in developed countries may not transfer to developing countries, particularly given differences in the demographics of social media users. Educative interventions about misinformation also may differ in their effectiveness based on the political nature of the content featured in the experiments. This would suggest that the degree to which COVID-19 is perceived as a political or ideological issue within any given context may impact the efficacy of interventions designed to counter automatic thinking.
In one of the studies reviewed in the Pennycook and Rand article described above, 1,005 participants who regularly
shared political news on social media were randomized to see 36 true and false news headlines on Facebook and Twitter.76 Before participants were selected and randomized, to ascertain whether or not potential participants shared political news on social media, every potential study participant was asked:
• “Would you ever consider sharing something political on Facebook?” (“yes”; “no”; “I don’t use social media”). Those who responded yes were included in the main analysis.
• Individuals in one arm of the study— the accuracy condition—were asked:
“To the best of your knowledge, is this claim in the above headline accurate?” (“not at all accurate”; “not very accurate”; “somewhat accurate”; “very accurate”)
• In the sharing condition, participants were asked: “Would you consider sharing this story online (for example, through Facebook or Twitter)?” (“yes”/“no”)
In a follow-up study, researchers recruited 401 participants to investigate the extent to which individuals value accuracy when deciding to share information online. Participants were asked:
• “When deciding whether to share a piece of content on social media, how important is it to you that the content is...?” (column labels—“not at all”, “slightly”, “moderately”, “very”, “extremely”; row labels—“accurate”, “surprising”, “interesting”, “aligned with your politics”, “funny”)
Subsequent studies aimed to identify whether calling attention to accuracy increases sharing of accurate news online. As a pretest, participants in this
study were asked to judge the accuracy of a politically neutral news headline to see if this “accuracy cue” had an effect on participants’ capacity to pay closer attention to news accuracy in subsequent tasks. They were also asked:
• “Do you agree or disagree that it is important to only share news content on social media that is accurate and unbiased?” (Likert scale ranging from “strongly agree” to “strongly disagree”)
• “If you were to see the above article on Facebook, how likely would you be to share it?” (“extremely unlikely”, “moderately unlikely”, “slightly unlikely”, “moderately likely”, “extremely likely”)
The authors found that when asked to rate the accuracy of a headline before sharing, participants reduced sharing of false headlines by 51%.
People may also rely on heuristics or mental shortcuts when evaluating whether to read and share content online. Pennycook and Rand note that a salient feature of misinformation is its emotional evocativeness, and especially its ability to provoke moral outrage.77 Indeed, misinformation is “sticky” because it often features deeply emotive human stories that elicit reactions such as anger, surprise, happiness, and fear. For example, in a study of 409 adults in the United States, Martel et al. found that people who report positive or negative emotions before encountering a headline were more likely to believe false news headlines. Participants completed a 20-item Positive and Negative Affect Schedule scale and for each item were asked:
• “To what extent do you feel [itemspecific emotion] at this moment?”
(Likert scale: 1=very slightly or not at all; 2=a little; 3=moderately; 4=quite a bit; 5=extremely)
Following this assessment, participants were randomized and shown a series of 20 actual headlines, half of which were accurate and the rest fake news. Some headlines were favorable to the Republican Party and some to the Democratic Party. Headlines were presented in the form of Facebook posts with a picture, headline, byline, and source. All participants were asked a follow-up question:
“
To the best of your knowledge, how accurate is the claim in the above headline?” (Likert scale: 1=not at all accurate; 2=not very accurate; 3=somewhat accurate; 4=very accurate)
The researchers found that belief in fake news is nearly twice as high for participants with the highest aggregate positive and negative emotion scores compared to participants with the lowest emotion scores. However, the study does not find significant threeway interactions among political concordance, emotion, and news type (accurate versus fake).78
The Rosenzweig et al. study discussed above found that COVID-19 headlines that generate emotions among social media users were more likely to be believed and shared.79 The online study recruited 1,341 Facebook users in Nigeria and showed them a mix of 10 true and false COVID-19 headlines. After reading the headline, participants were asked to rate their emotions using emojis:
• “Please select the emoji(s) that best represent your emotional state when you read the headline.” (surprised; scared; angry; disgusted; happy; sad)
• “On a scale from 1 (not very strongly) to 7 (very strongly), how strongly did you feel [emotion]?”
The authors measured belief using the question:
• “Do you think this headline accurately describes an event that actually happened?”
• “Are you interested in clicking to read the headline and sharing the headline online?”
The researchers found that happiness and surprise were associated with greater belief in and sharing of false COVID-19 headlines relative to true headlines.
Literature review
Social norms are defined as the “tacit rules that members of a group implicitly recognize and that affect their decisions and behavior.”80 There are two types of social norms: descriptive and injunctive norms. Descriptive norms indicate the behavior of relevant others and inform behavior by example, while injunctive norms represent how important others would like one to behave and they influence behavior through informal reinforcements or punishments. One source expands on the notion of social norms further: “We look to other people when in doubt…Taking cues from other people’s behavior is a valuable resource when we seek to improve our own decision-making.”81
As an example, healthcare providers can create and communicate injunctive social norms by indicating to their patients, either through explicit recommendations or implicit cues, that they expect patients to get vaccinated.
Their recommendations can also communicate descriptive social norms by implying that most other patients get vaccinated or that vaccination is what most previous patients have chosen before misinformation proliferated.82
A study by Gauri et al. illustrates how shifting social norms reduced the problem of open defecation in rural India. Although it was not directly related to vaccines, this experiment explored how mental models and social norms influenced individuals’ attitudes and behaviors toward an important public health resource, and aspects of the intervention may therefore be applicable to the context of COVID-19 vaccines. The researchers found that there were two pathways through which social norms inhibited the use of toilets in rural India: (1) beliefs about ritual notions of purity that dissociate latrines from cleanliness; and (2) beliefs and expectations that others do not use toilets or latrines, nor find open defecation unacceptable. Thus, the researchers piloted an information campaign to test the effectiveness of two strategies. The first was rebranding latrine use to associate it with cleanliness. The second was promoting positive social norms by providing information about the increasing prevalence of latrine use among individuals’ neighbors.
As the study explains, “If practices are motivated by social beliefs, changing empirical and/or normative expectations can shift people away from engaging in the practice. If information about the positive practices and behaviors of others in one’s reference group can be highlighted, it can induce positive behavior change by updating people’s perceptions of what others do and what the social norms are within their reference group.”83 A version of this intervention adapted to the COVID-19
context might inform individuals about how other people in their reference group—perhaps their local community, or their country, or their religious group— regard COVID-19 vaccines. If individuals learn that the majority of their referents intend to accept a COVID-19 vaccine, for example, it might nudge them toward acceptance as well.
Relatedly, findings about demographic trends in vaccine attitudes suggest that social norms may reinforce vaccine acceptance or hesitancy for different groups of people. For example, the Africa CDC has observed higher-thanaverage vaccine hesitancy among young people, city residents, the unemployed, and women. In the Africa CDC’s 15-country survey, the researchers found that vaccine acceptance was highest in Ethiopia and Niger and lowest in Senegal and the Democratic Republic of the Congo. Factors associated with vaccine skepticism included not knowing anyone who had tested positive for COVID-19; believing that the threat of the disease had been exaggerated; and believing in conspiracy theories.84
Social norms are also impacted by the influence of social networks. Lack of social norms about fact checking before sharing information online can lead individuals to fail to identify misinformation. Online misinformation spreads quickly in part because it elicits an emotional response. In one article, Lewandowksy et al. summarize studies that show how repetition in the echo chambers of social media can create a “perceived social consensus,” even if such a consensus does not exist, and how this can result in pluralistic ignorance and solidify one’s belief in misinformation. This effect is stronger when information comes from within people’s reference groups. Once an individual’s social
network has shared misinformation, anything that is inconsistent with it is deemed as inconsistent or incompatible. The researchers elaborate: “Messages that are inconsistent with one’s beliefs are also processed less fluently than messages that are consistent with one’s beliefs… In general, fluently processed information feels more familiar and is more likely to be accepted as true; conversely, disfluency elicits the impression that something doesn’t quite ‘feel right’ and prompts closer scrutiny of the message.”85
Social networks can also serve as a positive source of information and set communal behavior. For example, the Social Mobilisation Action Consortium was Sierra Leone’s coordinated community engagement initiative during the Ebola outbreak. The Consortium worked across 14 districts and approximately 12,000 communities, comprising organizations such as mosques, churches, and radio stations. The Consortium facilitated over 2,000 Community Mobilizers to implement behavioral change interventions. These interventions were effective when communication channels and platforms were appropriately used, combining community-based interpersonal communication with mass media. Specifically, consistent information and messaging that supported communityled responses and were repeated and reinforced via multiple channels demonstrably increased information credibility. Additionally, radio provided a platform to disseminate accurate information using trusted messengers, including religious leaders, community champions, traditional healers, survivors, and others. Religious leaders, in particular, were able to use social networks to persuade communities to adopt behavioral changes related
to modifications in traditional burial practices.86
Other effective mobilization strategies that have utilized social networks include campaigns like the Oseto-Ose Tok (House-to-House Talk) campaign, which brought together social mobilizers, youth, and volunteers who went door-to-door to share information on ways families could protect themselves against the Ebola virus and prevent its spread. Groups that went door-to-door consisted of a health worker, a community volunteer, a youth leader, and a teacher. In addition to spreading helpful information and providing communication materials on Ebola prevention, these groups also dispelled rumors and misconceptions about Ebola. Another low-technology tool, megaphones, became an important communication device across West African countries in rural and urban areas. Megaphones were used to gather crowds and make announcements containing Ebola prevention messages, sometimes on moving vehicles, through town criers or traditional communicators.
In conclusion, social learning and normsetting strategies can shift social norms to promote greater COVID-19 vaccine acceptance. If individuals witness their friends, relatives, and other reference group members getting the vaccine, they may be more likely to follow suit, as they can rely on immediate information from close contacts who are reliable sources rather than on the questionable information they may encounter online.
To restate a few key insights from our literature review, the scope of social norms largely depends on what is considered normal within an individual’s
reference group. Researchers often distinguish descriptive norms, which “offer information people can use to orient their actions,” from injunctive norms, which “put pressure on people to meet other people’s expectations.”87 While the workings of social processes are complex, the literature establishes a strong correlation between social norms and individuals’ behaviors. Specifically regarding COVID-19 vaccines in Africa, a data synthesis paper from Tulloch et al. noted that “local social norms may be more influential on people’s actions than rumours or misinformation.”88 A systematic literature review on H1N1 vaccine uptake from Bish et al. similarly concluded that there is “evidence of an influence of social pressure in that people who thought that others wanted them to be vaccinated were more likely to do so.”89
This is consistent with what Graupensperger et al. found in their November 2020 study of vaccination attitudes among U.S. undergraduate students: “[S]ocial norms...are robust predictors of health behaviors.” To assess both descriptive and injunctive norms, Graupensperger et al. asked:
• To assess descriptive norms:
“Considering typical young adults in America, what percentage do you think will get a[COVID]/[flu] vaccination/shot?” (On a scale of 0% to 100%)
• To assess injunctive norms: “In your estimation, how important do typical young adults think it is to get a [COVID]/[flu] vaccination/shot?” (A 7-point Likert scale, 1 = Not at all important and 7 = Extremely important)
The authors found that “estimated social norms were positively associated
with participants’ own intentions and perceived importance of getting a COVID vaccine.”90
Others have analyzed social norms through the lens of Theory of Reasoned Action and Theory of Planned Behavior to predict the behavioral outcome in other parts of the world. For such studies, the questions were more direct in connecting the respondents’ behavior and their perception of social norms:
• “The opinion of family and friends is important in my decision to take COVID-19 vaccine” (A 10-point scale, 1 = Absolute negative and 10 = Absolute positive)91
• “My relatives expect from me to do X” (A 5-point Likert scale: 1 = Completely disagree; 5 = Completely agree) where X referred to health behaviors such as handwashing and limitation of social contact.92
In addition to influencing vaccination behavior, social norms can be a strong driver of misinformation belief and sharing. Lewandowsky et al. note that “perceived social consensus can serve to solidify and maintain belief in misinformation.”93 As the impact of social norms is well established across cultures, a crucial aspect to utilizing social norms to curb misinformation is identifying demographic factors that construct social norms. In addition to unearthing these broad trends, it is important to identify the motivations for individuals’ attitudes toward COVID-19 vaccines. Such motivations appear to vary widely across individuals and groups, ranging from protecting oneself and others to asserting freedom of choice to acting upon a sense of civic responsibility. Understanding these motivations is key to designing context-specific and effective interventions.
Religious and cultural beliefs are powerful determinants of an individual’s identity, worldview, and decisionmaking process. How should these beliefs be considered in the context of misinformation and vaccine hesitancy?
Behavioral scientists have long known that cultural cognition affects how individuals process information. When this psychological phenomenon is applied to misinformation, cultural cognition leads to a clear cognitive problem: the worldview/identity effect, in which the way that individuals process evidence, information, and misinformation is dependent on their identity, worldview, and/or culture.94 Oftentimes, when individuals encounter new information that is contradictory to their worldview, culture, or identity, they are skeptical of this information. It is also possible that when individuals encounter information contradictory to their worldview, they will engage in motivated reasoning and may experience a “backfire effect,” causing them to double down more fervently on their deeply held, identitydriven beliefs. As was described in our discussion of automatic thinking, Badrinathan’s 2021 work showed the strength of motivated reasoning and cultural cognition. After an hour-long media literacy intervention designed to train Indians to identify misinformation, supporters of the BJP political party were actually less likely to be able to discern fake news.95 Although the concept of the backfire effect has been given significant theoretical consideration in the literature, Badrinathan’s work is one of the few papers that finds evidence for the phenomenon. While
Badrinathan does not explicitly call the results of her experiment a “backfire effect,” she attributes the decreased ability to identify misinformation to identity-based motivated reasoning. Badrinathan’s experiment suggests that in environments where beliefs about COVID-19 are closely linked to ideology, identity, and politics, messages must be carefully tailored in order to achieve the intended goal while simultaneously affirming the identity of the target audience. .
In addition to cultural and political identity, religious identity also likely plays an important role in how individuals process misinformation. Rutjens et al. found that self-identifying as religious was a more potent predictor of vaccine skepticism than political affiliation.96 Their study surveyed 5,973 respondents across 24 countries. While the study included survey data from Egypt, Morocco, and Tunisia, notably, no countries in sub-Saharan Africa were included. Nevertheless, given the consistency of the results, we suspect that the trend is likely to apply to that region as well.
How can the negative effects of cultural cognition be countered? The evidence suggests that two strategies are most likely to succeed: rebranding and choosing culturally congenial messengers.97 Rebranding refers to altering the messaging around a topic in order to cater to a different target audience. Rebranding can bypass cognitive resistance by presenting information not in its usual form, but rather in a way that is congruent with a person’s identity. For example, religious leaders could discuss the COVID-19 vaccine in relation to their religious principles, such as protecting and loving your neighbor (to give a Christian
example). In other words, evidence must be framed in a worldview- or identity-affirming manner to conform to the values of the intended audience. Second, the identity of the messenger is crucial. Culturally congenial messengers share the culture and background of the audience they are trying to reach. As was discussed in our subsection on social processes, an individual is more likely to be receptive to a message, particularly an identity-contradicting message, if it comes from someone who shares their worldview. Culturally congenial messengers may be able to identify the values, worldviews, and priorities that are most salient for their communities. As we develop strategies for countering misinformation later in this report, we will return to the strategy of using trusted messengers who come from the same cultural or religious background, as well as presenting information in an identity-affirming way.
The impact of “the unconscious influence of cultural context” is well understood in behavioral science, and cultural beliefs and values are a critical factor when it comes to dispelling misinformation.98
A study published in the Journal of Information Warfare found that “cultural values are critical in creating and disseminating misinformation” and that cultural understanding could be used to create more effective responses against misinformation and disinformation.99
In addition to cultural beliefs, religious beliefs can be strong drivers of misinformation in sub-Saharan Africa, which has been characterized as “one of the most religious regions” in the world.100
The African Youth Survey, conducted by the South Africa-based Ichikowitz
Family Foundation, collected data from 4,200 youth across 14 African countries. The survey noted the heterogeneity of personal characteristics that influence people’s cultural identity by asking:
• “Thinking about your own identity, which of the following do you identify with most?” (51% “my country”; 17% Africa; 17% “my tribe”; and 13% “my race”)101
These markers of identity can drive misinformation that is targeted at specific groups, such as the myth that “COVID does not pose a serious threat to Africans”; “China, Russia, and the United States are competing against one another while trying to kill Africans and shrink our population for their own interests”; or “Traditional tonics will cure me. I have no need for vaccines.”102
Misinformation can spread through influential individuals such as religious leaders, and people’s faith sometimes leads them to dismiss scientificallygrounded truth. Religious leaders are regarded as “low exposure and low trust” information sources, according to the Johns Hopkins COVID Behaviors Dashboard, but they can be powerful influencers in local contexts and among co-religionists.103 In fact, one study found that religious leaders are “more trusted and less widely seen as corrupt than any other group of public leaders” among believers.104 In other words, religious leaders could be strong allies to enhance vaccine uptake in subSaharan Africa, but they could also be effective vectors of misinformation. A study by the Africa Center for Strategic
Studies found that myths about the origins and risks of COVID-19 are highly prevalent in the region partly due to influential religious leaders spreading misinformation from the pulpit.105 On the positive side, Ifeanyi Nsofor, a public health physician in Nigeria, noted that in religious countries like Nigeria, working with influential religious leaders can be part of the solution to mitigating misinformation.106
In order to identify misinformation based on religious beliefs, Afrobarometer asked the following question to 6,000 West African survey respondents:
• “Some people think that prayer is an effective way to alter events in the world. Others put more faith in science to solve problems. Some people believe in both. What about you? Do you think that prayer is more effective or less effective than a vaccine would be in preventing COVID-19 infection?” (“Prayer is somewhat more/much more effective than vaccine”; “About equally effective”;“Prayer is somewhat less/much less effective than vaccine”)107
The survey found that 65% of respondents believed prayer to be more effective than vaccines—a striking number, compared to 11% who believed the two were about equally effective and 22% who considered prayer less effective.
After having reviewed the literature and built some hypotheses about how misinformation can contribute to vaccine hesitancy in sub-Saharan Africa, we now turn to proposing potential interventions—both online and offline— that can help address several of the enabling factors presented in the previous section. In accordance with the focus of our report, all interventions proposed in this section attempt to influence the belief in and sharing of misinformation, under the assumption that this would increase vaccine confidence and in turn vaccine uptake. Yet, as previously suggested, the assumption may not always hold, and structural barriers remain as perhaps the most significant driver of vaccine hesitancy in sub-Saharan Africa. While we believe misinformation is important, evidence is sparse on just how important it is in impacting vaccine uptake. Given the narrow objective of our proposed interventions and the complex nature of vaccine uptake, we urge policymakers and practitioners to consider a holistic approach that incorporates other interventions that more directly address vaccination behavior. Additionally, we suggest that they consider available resources and capacity constraints in each country to ensure that our proposed interventions do not undermine other useful interventions.
Because diverse populations rarely respond uniformly to interventions,
we allow for segmentation and tailor our interventions for each segment where appropriate. This section relies on the five personas developed using data collected by the World Bank: 1) champions, 2) those with specific health concerns, 3) those who have low trust in institutions, 4) those uninformed or unaware, and 5) the classically antivaccine.108 A short description of each persona is provided below.
• In most countries, champions are the dominant group. This persona believes COVID-19 vaccines are good, has minimal concerns about getting vaccinated, and trusts the government and other institutions. Interventions for this persona should aim to provide information on where, when, and how to access vaccines when they become available.
• Those with specific health concerns are also a major group. These individuals are not anti-vaccine; they typically take greater preventative measures than other groups, are riskaverse, and rely on social proof—in other words, they wait to see that their peers have safe and positive experiences before they seek out the vaccine. This persona would benefit from targeted information that addresses specific concerns—for example, about vaccine safety and efficacy, manufacturing processes and clinical trials, and side effects.
• The low-trust persona distrusts institutions, including government, pharmaceutical companies, and/ or multilateral organizations. This persona may be more persuaded by misinformation purporting malfeasance by government officials or other powerful individuals and responds best to social norms messages showing their peers are getting vaccinated, rather than to messages endorsed by institutions.109
• Those uninformed or unaware generally hold beliefs such as that COVID-19 is not a threat and that vaccines are unnecessary for people who have previously contracted and recovered from COVID-19. Better information and correction are thus most useful for reducing hesitancy for this persona.
• The classically anti-vaccine persona tends to be the smallest group. These individuals are strongly opposed to vaccines due to factors they are passionate about—such as political views—or have trouble articulating— such as religious or cultural beliefs. They are the most difficult group to sway, as behavioral interventions have limited effect on them.110
Data collected by Surgo Ventures from December 20, 2020 to January 4, 2021 in the United States showed similar persona segmentation. Enthusiasts were the dominant persona, comprising about 40% of the population in the United States. Like champions, this persona was eager to get vaccinated as soon as a vaccine became available. The watchful was the second largest group, comprising about 20% of the population and relying on social proof. The third largest group was the cost-anxious (14%), for whom time and cost were the
main barriers to getting vaccinated. The fourth group consisted of conspiracy believers (17%), who had deep-seated beliefs around COVID-19, took fewer preventative measures, and had a lower risk perception of the disease. Finally, system distrusters (9%) had low trust in the healthcare industry and were overwhelmingly people of color. Like the World Bank low-trust persona, this group may have been historically harmed by institutions.111
The interventions proposed in this section primarily target people who are open to changing their attitudes toward COVID-19 vaccines, or those who may be open to updating their beliefs. In other words, these interventions do not focus on converting those who are classically anti-vaccine. Still, some interventions have the potential of reaching even that persona—there is growing evidence they may be persuaded by former anti-vaccine individuals who have changed their minds, for example.112 Understanding what may or may not motivate or enable vaccine acceptance of each persona through diagnostic surveys is thus imperative to the success of any intervention, as previously suggested. Additionally, because these factors can vary by country, the specific local context must be considered before implementing behavioral interventions.
Our online and social media strategies generally attempt to address social norms, automatic thinking, and health concerns and risk perception. For select personas or threads of misinformation, they also attempt to address—or circumvent—the challenges of low trust and cultural and religious beliefs. In one’s information
journey, online interventions target the following steps: believing in a given piece of information, filling in any gap that is unexplained by the information, developing or updating one’s worldview based on the information, and choosing to share the information (Figure 3.1).
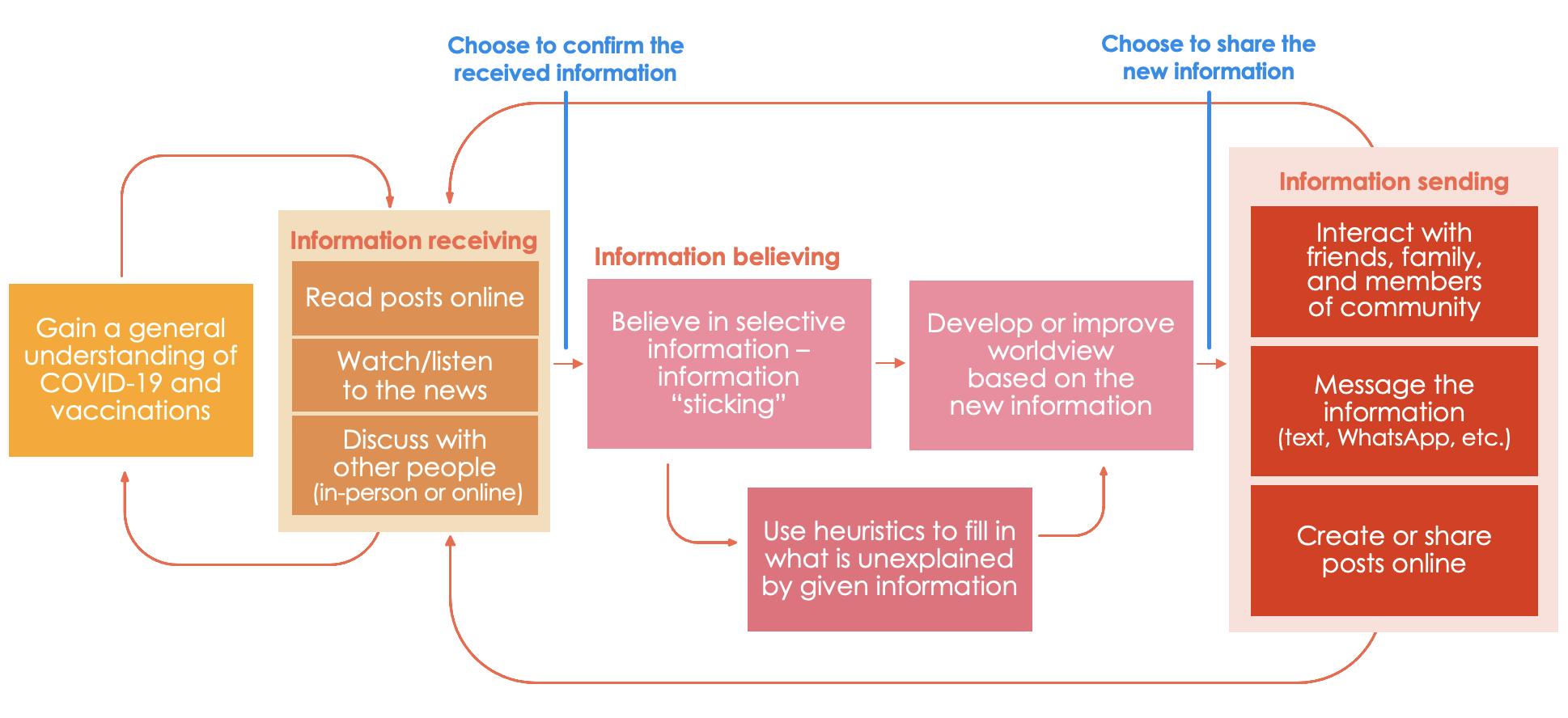
The proposed interventions utilize three strategies for prebunking and debunking: advertisements, chatbots, and inoculation games. Prebunking can help people detect false information and encourage them to use deliberative thinking throughout the steps depicted in the journey map. In turn, prebunking strategies can help change people’s worldview, increase their perceived risks of vaccination, and/or prevent misinformation from sticking in the first place. Debunking can help in similar ways, especially for those who decide to double-check the information they encounter. To increase the effectiveness of debunking, we also consider an intervention that targets social norms around double-checking before sharing potentially false information. Two major
social media platforms are considered for implementation: Facebook and WhatsApp. The eMBeD team could also consider low-cost expansion to other platforms such as Instagram and YouTube.
The first set of interventions will build on the eMBeD team’s partnership with Facebook and surveys currently administered on that platform. We propose post-survey advertisements that can provide accurate information and refute common threads of misinformation among hesitant groups. We also propose two additional sets of messages: 1) “stick it to the man” framing, which will target a select population with strongly held values and present misinformation as incompatible with those values (or vaccination as compatible); and 2) graphics that will focus on slowing or stopping the spread of misinformation. More details about these two interventions, including the rationales, will be provided later.
All advertisements should consider local contexts and reflect latest diagnostic results as more surveys are conducted. Advertisements should also employ the “Easy, Attractive, Social, and Timely (EAST)” framework and tips provided in the Vaccine Misinformation Field Guide. To summarize, the EAST framework suggests 1) using simple and clear messages, 2) grabbing the reader’s attention using images or personalization, 3) encouraging the reader to make a commitment to others or describing how most people engage in the desired behavior, and 4) prompting the reader when they are most likely to be receptive, speaking to immediate costs and benefits, or helping people develop specific plans to act.113 The Vaccine Misinformation Field Guide makes similar suggestions but in a more specific context. For example, it recommends communicating vaccination as an aspiration rather than an act, showing “happy, healthy, productive people” in graphics rather than needles and tears, and using emotionally resonant, salient visuals or narratives that are “stickier” than antivaccine messages.114
Advertisements to encourage vaccination, fill information gaps, and debunk myths
Facebook advertisements to encourage vaccination, fill information gaps, and debunk myths will be customized for the four types of persuadable personas (excluding the anti-vaccine) identified by the eMBeD team. As previously discussed, these personas include: those with low trust in institutions, those with specific health concerns, those unaware or uninformed, and the “champions” who only need to close the intention-action gap. Individuals will be classified into personas via Facebook
surveys. Then, using Facebook’s ability to use cookies to track users, these users will later be targeted with advertisements customized to their persona. For those already vaccinated, we propose replacing the post-survey advertisement(s) with an invitation to apply a “I got my COVID-19 vaccine” profile frame or sticker. The general format and ideas for advertisements are discussed below, and sample original messages are provided in Table 3.1.
Least likely to be or have been influenced by misinformation, this group will receive a simple call to action in advertisements that share specific information on how to get vaccinated in their region (e.g. through a link to a webpage where they can set up an appointment, sign up for vaccine notifications, or check vaccine availability in local clinics). Since the champions are more likely to espouse social norms supportive of vaccination and show altruism, the eMBeD team should also consider messages that can encourage them to help other members of their family or community get vaccinated.
Advertisements for this group should focus on providing simple, accurate information about vaccine safety and efficacy. They may also address specific myths that can affect people’s risk perception. For example, since surveys indicate infertility concerns are dominant in sub-Saharan Africa, a refuted version of this message may be provided for women in this group; alternatively, we may link vaccination as something that bolsters rather than threatens their identity as a mother. Because this persona also tends to
rely on social proof, information about vaccination rates may be useful, although the specific data presented should depend on the local context (e.g. in the initial stages of vaccine rollout, it may be more useful to show the percent increase in the number of people vaccinated as opposed to the overall vaccination rate). Some advertisements for the low-trust persona—ones that address concerns around vaccine safety and utilize storytelling from trusted messengers who have been vaccinated, as discussed later—may also be useful for this persona.

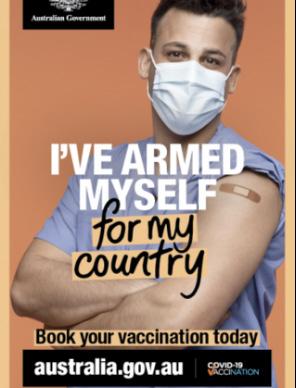
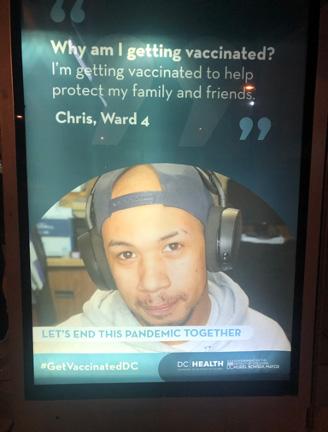
Preliminary diagnostic results show that this group responds best to community norms messages rather than to messages endorsed by institutions. Advertisements for this group can thus focus on personal stories of their trusted messengers, as determined by the eMBeD survey (e.g. healthcare workers; see Figure 3.2 for sample advertisements). The low-trust persona may also have concerns about vaccine safety, either because they believe COVID-19 vaccines are a tool used by
foreign institutions to harm Africans, reduce population, and/or plant microchips, or because they do not trust the process of vaccine development and distribution. As such, we should consider incorporating messages that can debunk such conspiracy theories or more generally improve trust around vaccine safety. Finally, as the low-trust persona is less likely to believe that people should vaccinate to protect others, advertisements will focus on individual benefits.
For the unaware or uninformed Advertisements for this group will attempt to fill in common and relevant information gaps, for instance about how people who have had COVID-19 would still benefit from the vaccine. This group may be prone to believing identitybased myths discussed in the literature review and diagnostics section, such as “COVID-19 does not pose a serious threat to Africans” and “Traditional tonics will cure me. I have no need for vaccines.”115 Accordingly, they will be
targeted with messages that provide accurate information about the threat of COVID-19 in sub-Saharan Africa and the benefits of vaccines. Advertisements for this persona may also discuss the new variants (e.g. Omicron) to highlight the need for vaccination.
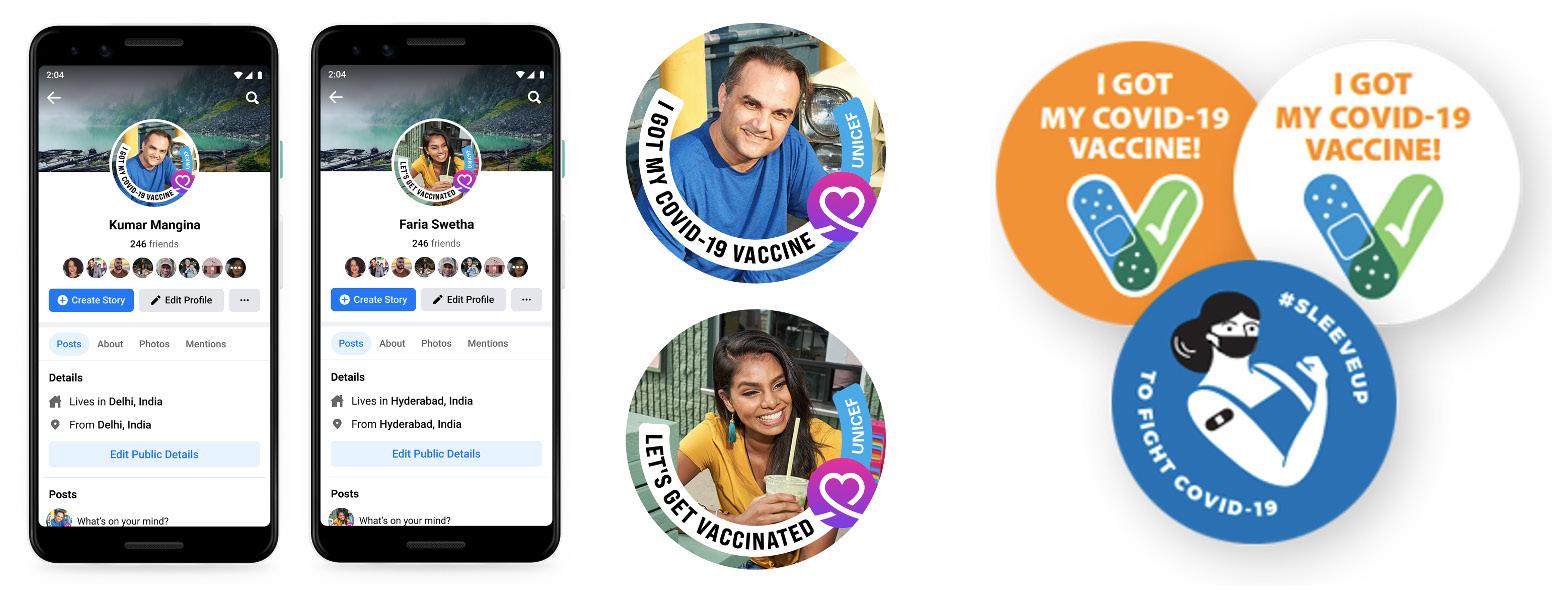
For those already vaccinated (not specific to a persona)
Survey participants who answer that they have been vaccinated will be subject to an intervention that will promote descriptive social norms. At the end of the survey, these participants will be taken to a page where they can change their Facebook profile frame to an available COVID-19 vaccine profile frame. In countries where a profile frame is not available, a virtual sticker that can be shared on Facebook or other social media platforms may be provided instead (see Figure 3.3 for a sample profile frame and sample stickers; profile frames can be created on Facebook Frame Studio, as well).
Champions
- COVID-19 vaccines are available throughout town X. Learn how to get yours today.
- Be a leader and get your COVID-19 vaccine today. Available at local clinics.
- Protect yourself and your loved ones against COVID-19. Get vaccinated today.
- Let’s get vaccinated and stop the pandemic together. No more lockdowns! Set up an appointment for yourself and your loved ones today.
(Insert a link to availability calendar, appointment scheduler, etc. for all advertisements.)
Concerned
- X people in country A have been vaccinated against COVID-19, with most reporting minor or no side effects. Join them and get yours today.
- Why am I getting vaccinated? Because as a mom, I want to protect my children against COVID-19. (Show a mother with her children.)
- Everyone at our center got vaccinated against COVID-19, and we are stronger than ever. Join us and protect yourself. (Show a worker from a local health care center.)
- COVID-19 vaccines are as safe as measles vaccines you give your kids.
Low-trust - Why vaccinate? Because COVID-19 vaccines are safe and help me get back to doing things I enjoy / helping people in my community / meeting with the members of my church. (Show a person from town X / nurse from hospital Y / pastor from church Z.)
- COVID-19 vaccines were developed quickly without compromising safety. After multiple clinical trials, it is now available for everyone over age X in our country. I got mine already, and I feel confident that it can protect you, too! (Show a doctor.)
Uninformed - Did you know a new COVID-19 variant was detected in Africa? Protect yourself against Omicron. Get vaccinated today.
- Did you know you can get COVID-19 again, even if you had it before? Vaccines can help minimize the risk. Get yours today.
- X people in country A have suffered from COVID-19; X more unreported cases are estimated. Protect yourself and get vaccinated now.
Source: Princeton team.
Note: Messages should be revised as necessary based on the local context and up-to-date diagnostic results.
“Stick it to the man”
advertisement to target those with strongly held values
Evidence suggests that younger, educated, urban adults in sub-Saharan Africa may be more vaccine-hesitant than other demographics, thus making them an important target for vaccine confidence interventions.135 As noted in the literature review and diagnostics, a 15-country study by the Africa CDC found that social media is cited as the most trusted source of information among COVID-19 vaccine hesitant groups, and more than 50% of young Africans cite social media as their primary source of news.116, 117 Further,
mistrust in institutions and external actors is strongly linked to vaccine refusal, especially among people who are more educated, younger, urban, and social media users.135
In a longitudinal, randomized controlled field experiment, Bryan et al. found that reframing unhealthy dietary choices as incompatible with important adolescent values helped counter the impact of manipulative food marketing on middle schoolers in Texas. The authors argue that such “values-alignment” interventions can be effective because reframing appeals to people’s existing source of motivation, tapping into their deeply held values or immediate
goals. One of the identified values for participants of this study was the desire to assert autonomy from adult control.118
Following Bryan et al., we propose an advertisement that can target younger adults who may feel strongly about external actors trying to influence their decisions. Rather than messaging around remaining autonomous from the “controlling, hypocritical adult,” as Bryan et al. did in the American context, we propose messaging that encourages young adults in sub-Saharan Africa to reject the influence of foreign disinformants. The advertisement will present disinformants as manipulative and include one of the following messages:
• “Don’t let creators of fake news control your opinion about COVID-19 vaccines. Find out yourself: [Link to the WHO’s vaccine safety page or a similar resource].”
• “Tons of misinformation about COVID-19 vaccines comes from the West. Don’t let foreigners decide your fate. [Link to the WHO’s vaccine safety page or a similar resource].”
• “The majority of anti-vaccine rumors originate from political actors in other countries. Don’t let them derail our vaccination campaign!”
The final message emphasizes that many major misinformation narratives come from foreign sources, including Russian disinformation networks and American or French anti-vaccine groups.119
While we have made some informed guesses about the value systems of educated young adults in sub-Saharan Africa, careful diagnostics, like the ones conducted by Bryan et al., are necessary for this intervention to identify the targeted population and ensure that it fits
the context. Diagnostics may reveal that the intervention would be most effective on the low-trust persona or those with strong cultural or national identity, for example. Effective messaging may also differ across countries and should be designed according to the diagnostic results.
The eMBeD team may also want to consider promoting advertisements that specifically target the spread of misinformation by creating social norms about fact-checking before sharing. The objective is to create friction in the process of information sharing or sending (see Figure 3.1). We anticipate that the advertisements may also help reduce automatic thinking and increase the detection of fake news, therefore reducing people’s belief in misinformation and eventually influencing their vaccination intentions. These advertisements could target all personas, including the anti-vaccine persona. In partnership with the WHO and independent fact-checkers, Facebook launched campaigns and produced a series of graphics that offer tips on how to spot misinformation (see Figure 3.4). The eMBeD team could easily incorporate these graphics into their intervention by randomly showing one of the two main graphics (i.e. “Don’t share if you’re not sure” and “Together against COVID-19 misinformation”) to survey respondents upon completion of the survey.
We propose evaluating the Facebook advertisements by implementing an A/B testing strategy and surveying users after exposure to the advertisements. After completing the initial survey, users will be randomized to receive either “A” advertisements or “B” advertisements. The “A” messages present a generic advertisement in favor of COVID-19 vaccines, while the “B” messages present a tailored COVID-19 vaccine advertisement for individuals’ specific personas (as outlined above). The same survey taken before the advertisements were delivered will then be repeated after the user sees the advertisements.
Because we will have baseline survey data and post-intervention data, we can do a simple pre-post analysis and difference-in-differences analysis to see if the Facebook advertisements changed survey responses for each of the two groups and the differences between their changes in survey responses. If resources and technology allow, followup surveys could be administered longitudinally at three different points in time to measure the temporal effect of the targeted advertisements. A single, tailored advertisement may have a small effect on an individual, but if they are later inundated with misinformation, they may go back to their baseline beliefs about COVID-19 vaccines. Administering surveys would allow us to see how long the effects of the advertisements last, if an effect is detected. Possible time points could be: three days after seeing

the advertisements, one week after, and two weeks after. If sample sizes are sufficiently large for multiple layers of randomization, users could also be randomized to receive different numbers of advertisements, making it possible to measure possible differential impacts of the advertisements. The eMBeD survey is included in Appendix A.
We propose evaluating the “stick it to the man” advertisements in a manner similar to the A/B strategy outlined above. The eMBeD survey already includes questions about individuals’ age and education level, which we can use to target this demographic. Users who meet the criteria as young (ages 1830) and educated (completed secondary school or more) will be included in this evaluation. By nature of the survey being administered via social media, all possible participants in this experiment will be social media users. Following the A/B strategy, these users will be randomized to either “A” advertisements or “B” advertisements. The “A” messaging will be generic messages in favor of COVID-19 vaccines, and the “B” messaging will be the “stick it to the man” messaging. The same survey will be administered after the advertisement(s) to detect any changes in responses. Again, follow-up surveys could be administered longitudinally at three different points in time to measure the temporal effect of the targeted advertisements.
Similar to the advertisements that explicitly encourage COVID-19
vaccination, we could randomize the advertisements to combat the sharing of misinformation online. Surveys would need to be administered to test subjects before and after seeing the advertisements. Like the suggested interventions for the other Facebook advertisements, post-intervention surveys could be administered at different time points to gauge the longevity of the advertisements’ effects. Furthermore, the experimental design could randomize the number of advertisements shown to different users in order to test the effectiveness of multiple advertisements as compared to a single advertisement. Following the randomization, surveys, and advertisements, we could conduct pre-post analyses and difference-indifferences analyses.
Given that the goal of this intervention is to prevent belief in and sharing of misinformation, the following survey questions could be used in addition to the standard eMBeD survey:
• In the past week, have you seen any misleading articles about the COVID-19 pandemic or COVID-19 vaccines?
a. Yes
b. No
• In the past week, have you shared any articles about the COVID-19 pandemic or COVID-19 vaccines on social media, WhatsApp, or in other ways?
a. Yes
b. No
• When you consider sharing an article about the COVID-19 pandemic or vaccines, how much time do you spend deciding if it is a credible source or not?
a. Less than 1 minute
b. 1-5 minutes
c. 5-10 minutes
d. More than 10 minutes
• Which of the following, if any, techniques do you use when reading news articles about COVID-19? Select all that apply.
e. Check the context; read other articles about the same topic
f. Check how the article makes you feel
g. Check the source
h. None of the above
• On a scale of 1-10, how confident do you feel in your ability to spot misinformation online or on WhatsApp?
We could also evaluate this intervention by showing a series of news article headlines, then asking users, “How manipulative do you find this news story, on a scale of 1-10?”. This type of evaluation would be modeled after the survey given at the beginning and the end of the Go Viral game, which we will discuss shortly.
The advertising interventions outlined above focus on Facebook, largely because the diagnostic surveys will be conducted there. Facebook tends to be more widely used in sub-Saharan Africa than other similar platforms such as Instagram, Twitter, or YouTube, but expansion to additional social media platforms could provide an easy, lowcost addition to the intervention.120 Customization suggested for postsurvey advertisements and required for the “stick it to the man” advertisement
may not be feasible elsewhere, so any expansion will focus on misinformation advertisement. The same graphics could be adapted to a different platform to simply extend the intervention’s reach, or they could be recorded in a short video format. Depending on the availability of resources and diagnostic survey results, recruiting trusted messengers to promote strategies to spot misinformation may also prove effective.
According to the Economist, WhatsApp is the most popular social media platform in many sub-Saharan African countries, including South Africa, Kenya, Ghana, and Nigeria. While in the global North it is more common to use multiple types of social media, WhatsApp often serves as “an efficient one-stopshop” for users in sub-Saharan Africa. WhatsApp groups in the region tend to be much larger than in the global North, and these groups often include trusted sources such as respected community leaders. As a result, misinformation can spread quickly on the platform.121 With this background, disseminating accurate information about COVID-19 vaccines and providing fact-checking for those seeking to verify information they encountered on WhatsApp in real time could be an efficient way to combat misinformation in sub-Saharan Africa.
Interventions on WhatsApp are naturally challenging given the platform’s endto-end encryption, but the WHO and several governments, including those in India and the United Kingdom, have managed to work around this issue. In partnership with fact-checkers and artificial intelligence companies, these institutions have established chatbots and tiplines that people can use to ask
questions, find the most up-to-date news and information, and request verification of what they suspect to be fake news. Fact-checkers associated with WhatsApp can recognize multiple languages and respond back with correct information in the preferred local language, which the requester can then share with their network. Public evaluations and information on the challenges of these chatbots are sparse, but one article has been published highlighting the successes of the WHO chatbot, suggesting that the WHO’s multilingual chatbot provides content that is informal, conversational, culturally sensitive, and visually appealing (e.g. by utilizing video animation and emojis). Such content is “received more readily by users” and helps “circumvent ambiguity,” thereby helping promote trust.122
The eMBeD team is already in conversation with partner organizations to develop a similar chatbot. Such service can be “ideal for countering people’s exposure to misinformation, as it gives people direct access to information they need from credible sources.”123 The process through which people report potentially false news they encounter can also help identify and track misinformation that is prevalent in different countries and regions.
Currently, however, all proposed and technologically feasible WhatsApp interventions require users to opt into the intervention at some point. This feature means that the intervention would have significant selection bias, likely only reaching those who are already less susceptible to misinformation. Another limitation with automated chatbots is that they may not be able to answer complex or nuanced questions. To improve engagement, a live chat function could be considered as an
additional feature; but any increase in the costs of operation, especially personnel, should be compared against its estimated value added.
Evidence on the effectiveness of chatbots is still developing, but certain types or features of chatbots may help encourage their use and maximize their impact. Some studies have found that anthropomorphic design features, for example, can have a significant and positive effect on users’ perceptions of their usefulness. Empathic virtual counselors also had a positive effect on user acceptance and helped reduce alcohol consumption, although Ling et al. (2021) note that it may be more relevant to certain contexts than others.124 In the context of the human papillomavirus (HPV) vaccine, Tsai et al. (2021) found that when anger was elicited, participants who were randomly assigned to a chatbot were less likely to report satisfaction than those who were assigned to a human representative. However, when embarrassment was elicited, they were more likely to disclose concerns about HPV risks or elaborate on their answers.125 Thus, while it may be useful to develop a chatbot that can show emotion and react the same way humans would, the context of COVID-19 vaccine communication should be carefully considered.
Höhn and Bongard-Blanchy have evaluated 24 chatbots on different channels using a framework with 12 principles, which they call heuristics. Among the three chatbots on WhatsApp (one each from the WHO, the German Red Cross, and the Russian Ministry of Health), the German Red Cross chatbot received the highest score, as it can not only understand number codes but also extract keywords from natural phrases. Including such
conversational capabilities seem most critical for chatbots, especially those on Whatsapp, which has design and privacy limitations.126 Comparing other available
chatbots (examples in Figure 3.5), and how successful they have been may help us gauge which additional features should be included.
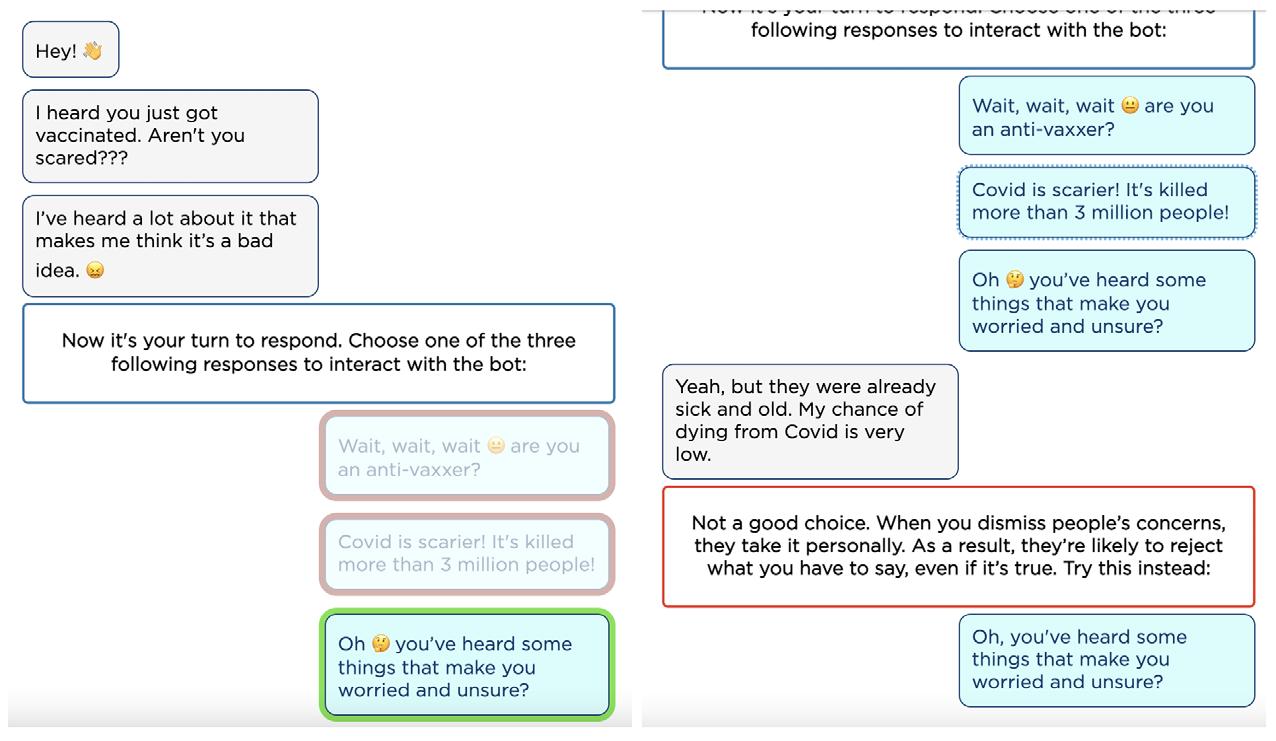
Source: Business Insider on WHO WhatsApp chatbot for coronavirus information, Princeton team screenshots of WHO WhatsApp chatbot, online chatbot “Vira” (Vaccine Information Resource Assistant), WhatsApp chatbot “Sahabat Peduli Corona” (Your COVID Protection Buddy) from Save the Children, and online vaccine chatbot developed by Gagneur and Tamerius from Kaiser Permanente.
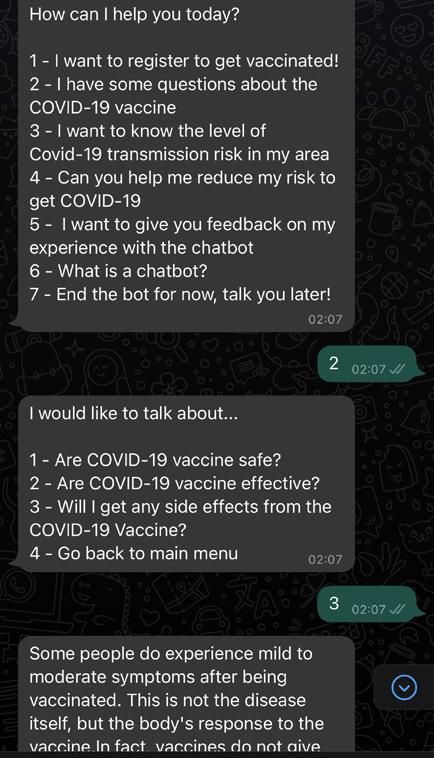
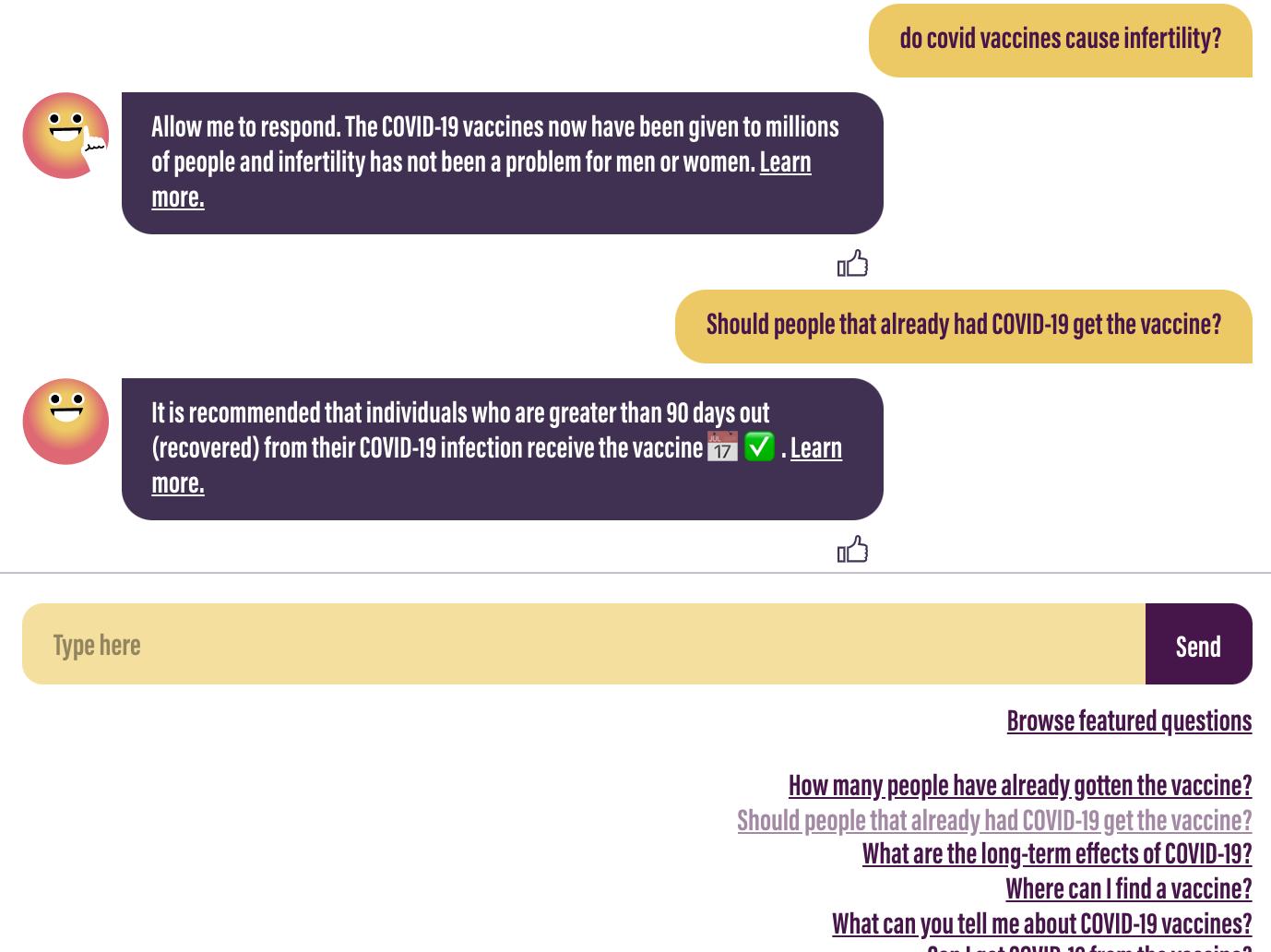

If the eMBeD team is able to set up a WhatsApp chatbot, they could hypothetically develop an evaluation model parallel to the one described above for the Facebook advertisements. Users would answer baseline survey questions, then receive a “treatment” of interacting with a COVID-19 chatbot. Ideally, the chatbot could answer some of their questions about the COVID-19 vaccine. Users could be randomized to have access to the chatbot or to not have access to the chatbot. These same users (both treatment-group members and controls) would then be surveyed about their beliefs and attitudes regarding the COVID-19 vaccine, using the same questions as above and from the eMBeD survey.
There is growing evidence that games that cast players in the role of a disinformant can improve their ability to detect misinformation and decrease their perceived credibility of fake news. This intervention will use Go Viral, a 5-minute game that focuses on COVID-19 misinformation and techniques used by disinformants. Developed by the WHO and the British government, the game is an iteration of another game called Bad News, which has been played over a million times and was linked to significant inoculation effects that lasted for months. A recent in-game survey experiment on Go Viral also suggested that players were more likely to regard misinformation as manipulative and less willing to share it after the game.127
To incorporate the Go Viral game into the portfolio of misinformation interventions, we suggest inviting participants to play the game at the end
of the current eMBeD vaccine hesitancy survey. The link could be added to an advertisement—which will be shown randomly to the four personas as previously discussed—or added as another question to the survey. The invitation message on an advertisement may say: “Protect yourself against COVID-19 misinformation. Play Go Viral!” or “Can you spot fake news about COVID-19? Play Go Viral!” The message could be included as a hyperlinked textbox, or, alternatively, accessed using a QR code. If added as a question, after all other questions are completed, the survey would ask:
• Are you interested in playing a 5-minute game to protect yourself against misinformation about COVID-19?
a. Yes, let me play!
b. No, I will pass
c. Tell me more about the game
The Go Viral homepage would open in a new tab for participants who answer “yes.” For those who answer “tell me more about the game,” a more detailed invitation would appear, along with two follow-up options: “Okay, I will play” and “I will pass.”
Difficulties with recruitment and retention, which are likely to be a challenge for all online interventions, may be even greater for the game. Some people may click on the link but decide not to play; some may not come back to report any effect the game has had on their ability to identify misinformation. To encourage participation and reduce attrition, we may want to enter participants into a lottery to win a gift card as a relatively low-cost incentive. The eMBeD team may also be able to receive in-game data for the players who come through their Facebook surveys
from the game developers. Because ingame surveys provide information on changes in a player’s ability to detect misinformation, such cooperation may eliminate the need for a follow-up survey.
The Go Viral game is currently available in multiple languages, including English, French, and Portuguese. The eMBeD team may wish to collaborate with the game developers to add more languages in which their diagnostic surveys are conducted. As a final note, while we propose this intervention given the growing evidence in support of inoculation games and their increasing popularity, there is a valid and significant concern that we may end up producing more disinformants by teaching people effective manipulation techniques. To prevent such unintended consequences, the intervention should be targeted to groups or personas that are likely to benefit from inoculation games and can then “pay it forward.”128 These may include: gamers and young people, perhaps with specific health concerns, who may learn how to tell conspiracy narratives apart from real side effects and invite their friends to also play the game; and champions, who may be motivated to dissuade their family and friends from misinformation based on what they learn from the game.
Previous research on the effects of inoculation games has shown promising results. Bad News, an iteration of the Go Viral game that was developed before the COVID-19 pandemic, reduced the perceived reliability of fake news by 21%, relative to a control group.129 Given that there is already evidence that these prebunking games can reduce the perceived reliability of
misinformation, it may be more useful to investigate different research questions. Considering that the Go Viral game already collects data on participants before and after playing the game, a collaboration to combine the eMBeD survey data with the Go Viral data could reveal interesting correlations between persona types and the effectiveness of the game. Possible research questions include:
• Does the Go Viral inoculation game have differential effects on the different personas?
• Does the Go Viral inoculation game lead to increases in intentions to get the COVID-19 vaccine?
For each research question, users can be directed to the Go Viral game from a link following the eMBeD survey. Users can then be evaluated in a manner similar to the evaluation strategies for the persona-targeted Facebook advertisements. The link to the Go Viral game can be randomized, meaning that some users will be encouraged to follow the link and play the game, while others will not be shown this option.
In order to evaluate the first research question (Does the Go Viral inoculation game have differential effects on the different personas?), data from both the eMBeD survey and the Go Viral game would be needed. Sample in-game questions are provided in Figure 3.6.
If users are directed to the Go Viral game from the eMBeD Facebook survey, their eMBeD survey results could then be linked to their results from the Go Viral game, allowing us to determine if the Go Viral game has differential impacts on different personas. Additional exploratory analyses could also be performed with the other survey
questions to see if other factors may influence the effect of the Go Viral game.
To evaluate research question 2 (Does the Go Viral inoculation game lead to increases in intentions to get the COVID-19 vaccine?), the existing questions in the eMBeD survey may be used. Survey questions 3 “Have you been vaccinated for COVID-19 (at least one dose)?” and 6 “Do you plan to get the COVID-19 vaccine?” will help us answer this research question of interest.

In many parts of sub-Saharan Africa, however, social media usage tends to be limited to a small subset of the population that is predominantly young and male. Also, the Africa CDC has found that television and radio tend to be more trusted sources of information than online sources.130 For these reasons, we also explore television, radio, and inperson strategies, designed specifically for countries and communities with low rates of internet or smartphone penetration.
Many offline interventions require government resources and partnerships, as well as better access to local communities. Rather than implementing these interventions directly, the eMBeD team may wish to suggest them to governments or civil society organizations. This section presents interventions at three different levels:
1) a national-level intervention which will use a catchy phrase and tune to “put brakes” on people before sharing, 2) a university-level intervention where participants will attend information sessions and play Go Viral, and 3) a community-level intervention that will combine a set of multiple strategies.
In this report, we focus on online interventions for two primary reasons.
First, the eMBeD team has existing partnerships and projects with social media platforms. Second, the internet facilitates “quick and wide dissemination of misinformation.”129 Online campaigns may thus be implemented faster and be relatively cost-effective given the prevalence of misinformation.
The first intervention will attempt to establish a new social norm not to engage in automatic thinking or to think twice before sharing social media posts or forwarding text messages on group chats, which targets several steps on the journey map in Figure 3.1. The key message will be something simple, short, and catchy, such as the phrase “Don’t share if you’re not sure,” used by Facebook, or a new, shorter message “STOP before sharing.” In order to leave a
lasting imprint on people’s minds, a simple yet catchy tune should be attached to the message; and in order to maximize any impact on vaccination intentions or uptake, pro-vaccine messages—which could contain accurate information that speaks to prescriptive and descriptive norms—from public health officials or other trusted messengers should follow.
Musical association with the message makes the campaign an intervention that is suitable for various media. First, it can play on the radio. Second, it can be adapted for a video format to be disseminated via television or even social media platforms. Again, depending on diagnostic results, the campaign could recruit local religious leaders, public health officials, and/or celebrities to participate in the video. These well-known individuals could also help expand the campaign to online platforms, posting the videos on their own social media accounts, perhaps using popular filters. The intervention could be expensive to implement, but the costs could be reduced if the messengers could be recruited on a volunteer basis. Finding “champions” that are well-known and well-trusted in each country might be a challenge.
Given that the focus of our report is on online misinformation and our suggested offline interventions above remain hypothetical, we will not go into great detail on an evaluation strategy for a national media campaign. Regardless of the on-the-ground details of potential national media campaigns, we would recommend mixed-methods analyses in order to learn from both quantitative and qualitative data. If conditions are appropriate for randomization or A/B testing, an evaluation could be modeled
after Paluck’s experiment with mass media in Rwanda, in which a reconciliation radio soap opera was randomly assigned to some communities, while others received a health radio soap opera. The study found that the reconciliation radio program did not change listeners’ beliefs, but it did change perceived social norms and some behaviors.131 Similar to Paluck’s experiment, outcomes could be measured with standardized questionnaires, focus groups, and interviews.
This intervention is intended to act as a “misinformation vaccine” for university students in sub-Saharan Africa, who tend to be more prone to engaging with misinformation, due to their relatively heavy use of social media.132 The intervention will (1) provide access to fact-checked, relevant, and persuasive information on COVID-19; and (2) attempt to prebunk common threads of misinformation and train young social media users to spot disinformation tactics using inoculation theory. Once again, this intervention mainly focuses on hindering automatic thinking at different points of the journey map and perhaps addressing other drivers, depending on which type of misinformation is most relevant to the specific group of students. These drivers might include low trust in institutions, health concerns and risk perception, or cultural and religious beliefs.
This intervention would utilize the online game Go Viral, which was discussed in the previous section. Participants will attend two one-hour sessions: an interactive session that will provide information on COVID-19 and vaccines, and one that
will be dedicated to playing the game, reflecting on the game, and learning about more misinformation techniques. Both sessions will be in person, to maximize the benefits of the reflection and learning components and to ensure that participants have stable access to the internet. Costs of implementation could be lowered through partnerships with universities. Partner universities can provide a space for information sessions and devices on which participants will play the game; promote the event and encourage participation; and help identify interested faculty members who can gather students or even facilitate the sessions. Partnerships may also be built with individual departments, such as social sciences or the medical center.
Once again, it is difficult to design a suitable evaluation strategy without knowing the details on the ground. Below, we outline an ideal evaluation strategy if country and university partnerships, resources, and pandemic circumstances align.
To test the intervention, we could run a clustered randomized controlled trial (RCT) across 20 African universities located in major cities.133 The experiment could be concentrated in a few countries or more broadly dispersed across countries. The study will comprise four arms, with five universities in each arm. Universities will be randomly assigned to each arm, as follows:
1. Control: Control participants will play a simple logic game that is unrelated to COVID-19. (5 universities)
2. Four interactive information sessions / dialogues, one hour each, on the COVID-19 disease, variants, and vaccines. (5 universities)
3. Four one-hour online game (e.g., Go Viral!) sessions on COVID-19 misinformation / prebunking. (5 universities)
4. Combined dialogue and online game sessions on misinformation. (5 universities)
After identifying the 20 African universities and randomly assigning each school to one of the four arms of the study, we can then randomly select 400 students from each school, bringing the total number of study participants to 2,000 per arm and 8,000 total. To ensure a representative sample from each school, sampling will be stratified by year, gender, course of study, and other key characteristics. We will run balance tests to ensure similarities in school and student characteristics before the start of the intervention.
The primary outcomes of interest are willingness to receive a COVID-19 vaccine, attitudes toward COVID-19 vaccines, and truth discernment of COVID-19-related misinformation. The study will use survey data to assess the main outcomes of interest. Students will be surveyed at the beginning of the study and at the end of each of the four training sessions. Participants could also be classified into personas with the pre-intervention survey, enabling the study to assess possible heterogeneous impacts.
We hypothesize that the combined intervention (filling information gaps and prebunking) would likely have the largest impact, given that many young, educated urbanites in Africa have cited social media as their most trusted source of information and are thus vulnerable to misinformation spreading online. Additionally, we anticipate this result because many governments in
sub-Saharan Africa have not adequately disseminated relevant information on COVID-19 vaccines (e.g. regarding their options, efficacy, and potential side effects), and this intervention would directly provide such information and encourage dialogue.
This intervention will be comprehensive in its objectives and strategies and will target specific communities (e.g. towns). We suggest some combination of the following features:
1. Pamphlets featuring tips to detect misinformation and personal stories that highlight the impact of misinformation (e.g. about a young man or woman who believed the myth that young, healthy individuals do not need the vaccine but contracted COVID-19 and spread it to their grandparents, who then passed away). They may be printed as posters and displayed at key community meeting points as well.
2. Biweekly text messages from trusted members of the community. They would alternate between factchecking a common misinformation narrative about COVID-19 and reminding the recipient about the importance of vaccination using four types of messages: helping loved ones, approval from healthcare workers, notion of the individual’s role for the community’s return to normalcy, and social proof.134
3. A radio campaign that will use storytelling to highlight misinformation as a public health crisis and provide accurate information about COVID-19. It
would feature similar information and personal narratives to the pamphlets described above in (1).
4. Interfaith dialogues moderated or provided by local religious leaders
To illustrate the impact such an intervention could have, we provide the example of an imam in the United Kingdom, who “hammered away” at misinformation in his sermons, encouraged congregants to “rely on the experts, not someone [who] throws something on Facebook,” turned his mosque into a vaccination site, and got vaccinated himself. Thanks to the imam’s efforts, he was able to change people’s minds about COVID-19 vaccines and increase uptake.135
5. Live radio or television broadcasts of people getting vaccinated. Showing other community members getting vaccinated can be a way to clearly present social proof. In addition to the live stream, the program could feature short interviews with people at the vaccination site. If collecting appropriate consent from everyone at site proves difficult, a special program with prominent members may be considered.
Given that this communications strategy includes multiple avenues of behavioral change, it would be difficult to separate the impact of any one component of the intervention or do any true impact evaluation. Rather than using experimental techniques to evaluate this comprehensive strategy, we would recommend iterative, agile implementation studies that can quickly inform small changes to the overall communication strategy.
Misinformation acts like a virus and can spread rapidly once it appears on a platform. However, the spread of misinformation is not automatic, and we recognize the diverse drivers behind it. We know that the way people think, feel, and act influences the volume of misinformation and the speed with which it circulates online. On the spectrum of vaccine hesitancy, there are anti-vaxxers, the unaware/uninformed, those with health concerns, those with low trust in institutions, and “champions.” Each persona may behave differently when it comes to believing misinformation and spreading it. In this report, we have summarized five psychological enablers of misinformation belief and sharing: health concerns and risk assessment, lack of trust in institutions, automatic thinking, social norms, and cultural and religious beliefs.
The diagnostic tools we have proposed aim to reveal the relative importance of each enabler in different contexts. Given the time constraints of this project, we have not been able to put these diagnostic tools into action, but we hope that these tools will help the eMBeD strengthen their understanding of the vaccine-hesitant population of sub-Saharan Africa.
Based on our understanding of what might be happening, which is informed by extensive research and interviews with practitioners, researchers, and experts of sub-Saharan Africa, we have designed
interventions for those whom we think are moveable (all personas except antivaxxers). We have described a number of online and offline interventions that our research suggests might work in the sub-Saharan Africa context. However, one size does not fit all, and these interventions would need to be adapted to each country’s political and cultural context. Implementation of these largescale behavioral interventions would also require coordination between multiple stakeholders and buy-in at the country level. Keeping this in mind, we suggest the following actions the eMBeD team may want to consider:
Expanding Facebook survey capacity across countries of sub-Saharan Africa to roll out the Facebook advertisements intervention. Literature on pre-bunking described in earlier sections suggests that it is harder to change beliefs after significant exposure to misinformation has occurred. Thus, the longer it takes to roll out pre-bunking interventions since the start of an “infodemic,” the less effective these interventions become. A strategy to roll out targeted Facebook advertisements at the same time across all countries of interest would be most effective if done fast.
Increasing the Facebook advertisement bank to target each persona with relevant messaging. The previous section highlights the types of messaging that would be most effective for each persona. Consultations with
World Bank country officers and local staff would be a next step to identify how to adapt messaging to a country’s local language and culture. If cultural, persona-tailored messaging is absent in existing advertisements, conversations with Facebook advertisement designers would be useful to develop the necessary content for roll-out.
Building a team for the WhatsApp chatbot, including human representatives to respond to queries. Our research suggests that user satisfaction is higher when chatbots have human representation. Factchecking services supporting these human representatives may be reliant on AI or human fact-checkers. In either case, building capacity at the country level to staff and train teams would be a next step. As with other interventions, ensuring teams are aware of and can respond to cultural nuances when engaging with users would be key.
Securing a budget to increase participation in inoculation games by engaging with governments, country officers, and potential donors. Earlier, we suggested that respondents could be incentivized to participate in inoculation games through gift cards or other benefits. The eMBeD team may want to hold consultations with relevant stakeholders to determine incentives and the amount of gift money awarded, along with confirming how the prizes would be distributed to recipients.
Partnering with teams at the country level responsible for COVID-19 communications to discuss offline
interventions. These teams may have knowledge about how to leverage partnerships with television, radio channels, and local behavior change organizations; which community meeting points to prioritize for behavior change messaging; and how to coordinate behavioral change goals with religious leaders. Considering eMBeD’s focus on online interventions to combat misinformation, identifying the right teams who could take responsibility for the offline interventions would be useful to counter misinformation circulating outside the internet. These teams may benefit from eMBeD’s expertise on how to design and distribute content to achieve behavioral change. Their input could also help refine online interventions.
Beyond the implementation of these interventions, it is also key to consider how to monitor their effectiveness. The evaluation strategies we have designed might provide eMBeD with additional approaches to monitor results. There is much to learn from these evaluation strategies to determine the degree to which the proposed interventions would work in sub-Saharan Africa. Considering the iterative nature of intervention design, it may take several rounds of testing and redesign to land upon effective approaches. The eMBeD team is already moving the needle on reducing vaccine hesitancy driven by misinformation through existing interventions; this report has attempted to further the research to support current and future iterations.
1 WHO Coronavirus (COVID-19) Dashboard. (2022, January 5). WHO. https://covid19.who.int/
2 Weekly Bulletin on Outbreaks and Other Emergencies, Week 48. (2021, November). WHO Africa. https://apps.who.int/iris/bitstream/ handle/10665/349801/OEW48-2228112021.pdf
3 Distribution of the global population 2021, by continent. (2021, December 5). Statista. https://www. statista.com/statistics/237584/distribution-of-theworld-population-by-continent/
4 Holder, J. (2021, December 8). Tracking Coronavirus Vaccinations Around the World. World Vaccination Tracker, The New York Times. https:// www.nytimes.com/interactive/2021/world/covidvaccinations-tracker.html
5 The World Bank. (2021, June 21). Reaching Herd Immunity Behaviorally: Using Social Media Insights to Inform COVID-19 Vaccination Efforts. [Video]. https:// www.worldbank.org/en/events/2021/06/22/
6 Wilson, S.L., & Wiysonge, C. (2020). Social media and vaccine hesitancy. BMJ Global Health, https://gh.bmj.com/content/5/10/e004206.abstract
7,8,9 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
10 Seydou, A. (2021, March). Who wants COVID-19 vaccination? In 5 West African countries, hesitancy is high, trust low. Afrobarometer Dispatch No. 432. https:// afrobarometer.org/publications/ad432
11 Dzinamarira, T., Nachipo, B., Phiri, B., & Musuka, G. (2021, March). COVID-19 Vaccine Roll-Out in South Africa and Zimbabwe: Urgent Need to Address Community Preparedness, Fears and Hesitancy. Vaccines 9(3), 250. https://doi.org/10.3390/vaccines9030250
12 Tilley, H. (2016). Medicine, Empires, and Ethics in Colonial Africa. AMA Journal of Ethics, 18(7), 743753. https://doi:10.1001/journalofethics.2016.18.7.mh st1-1607
13 Archibong, B., & Annan, F. (2021). “We Are Not Guinea Pigs”: The Effects of Negative News on Vaccine Compliance. SSRN. https://doi.org/10.2139/ ssrn.3765793
14 French, Jeff, Sameer Deshpande, William Evans, and Rafael Obregon. (2020). Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. International journal of environmental research and public health 17, no. 16 p.5893.
15 Babalola, S., Krenn, S., Rosen, J. G., Serlemitsos, E., Shaivitz, M., Storey, D., Tsang, S., Tseng, T. Y., & Shattuck, D. (2021, September). COVID Behaviors Dashboard. Johns Hopkins Center for Communication Programs in collaboration with Facebook Data for Good, Delphi Group
at Carnegie Mellon University, University of Maryland Social Data Science Center, Global Outbreak Alert and Response Network. https://covidbehaviors.org/
16 Collective Service for Risk Communication and Community Engagement (RCCE). (2021, October 19). COVID-19 Behavioural Indicators. https://www.rccecollective.net/data/behavioural-indicators/#overview
17 Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing Vaccination: Putting Psychological Science Into Action. Psychological science in the public interest : a journal of the American Psychological Society, 18(3), 149–207. https://doi. org/10.1177/1529100618760521
18 Tafadzwa Dzinamarira et al., “COVID-19 Vaccine Roll-Out in South Africa and Zimbabwe: Urgent Need to Address Community Preparedness, Fears and Hesitancy,” Vaccines 9, no. 3 (March 2021): 5. https://doi. org/10.3390/vaccines9030250
19,20 The Africa Center for Strategic Studies. (2021, May). Dispelling COVID Vaccine Myths in Africa. https:// africacenter.org/spotlight/dispelling-covid-vaccinemyths-in-africa/
21,22 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
23,24 “Dispelling COVID Vaccine Myths in Africa.”
25,26 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. 6. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
27,28 Carcelen, A.C., Prosperi, C., Mutembo, S., Chongwe, G., Mwansa, F.D., Ndubani, P., Simulundu, E., Chilumba, I., Musukwa, G., Thuma, P., Kapungu, K., Hamahuwa, M., Mutale, I., Winter, A., Moss, W.J., & Truelove, S.A. (2021, July). COVID-19 Vaccine Hesitancy in Zambia: A Glimpse at the Possible Challenges Ahead for COVID-19 Vaccination Rollout in Sub-Saharan Africa. Human Vaccines & Immunotherapeutics. https://doi.org/1 0.1080/21645515.2021.1948784
29 Dotto, C. D., & Cubbon, S. C. (2021, June). Disinformation exports: How foreign anti-vaccine narratives reached West African communities online. First Draft. https://firstdraftnews.org/long-form-article/ 30,31 Smith, J. (2021, October 22). Ideas42. Personal communication [Zoom interview].
32 Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing Vaccination: Putting Psychological Science Into Action. Psychological science in the public interest : a journal of the American Psychological Society, 18(3), 186. https://doi. org/10.1177/1529100618760521
33 Nsoesie, E.O., & Oladeji, O. (2020, April). Identifying Patterns to Prevent the Spread of Misinformation during Epidemics. Harvard Kennedy School Misinformation Review. https://doi.org/10.37016/ mr-2020-014
34 Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing Vaccination: Putting Psychological Science Into Action. Psychological science in the public interest : a journal of the American Psychological Society, 18(3), 149–207. https://doi. org/10.1177/1529100618760521
35,36 van der Linden, S., Roozenbeek, J.S., & Compton, J. (2020). Inoculating Against Fake News About COVID-19. Frontiers in Psychology, 11, 4. https://doi.org/10.3389/ fpsyg.2020.566790
37 Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing Vaccination: Putting Psychological Science Into Action. Psychological science in the public interest : a journal of the American Psychological Society, 18(3), 149–207. https://doi. org/10.1177/1529100618760521
38 Babalola, S., Krenn, S., Rosen, J. G., Serlemitsos, E., Shaivitz, M., Storey, D., Tsang, S., Tseng, T. Y., & Shattuck, D. (2021, September). COVID Behaviors Dashboard. Johns Hopkins Center for Communication Programs in collaboration with Facebook Data for Good, Delphi Group at Carnegie Mellon University, University of Maryland Social Data Science Center, Global Outbreak Alert and Response Network. https://covidbehaviors.org/
39 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
40 Collective Service for Risk Communication and Community Engagement (RCCE). (2021, October 19). COVID-19 Behavioural Indicators. https://www.rccecollective.net/data/behavioural-indicators/#overview
41 West and Central Africa lag in DTP3 vaccine coverage (at 66%) while Eastern and Southern Africa boast 81% coverage. A high DTP3 coverage rate implies high vaccination rates for other important vaccines, such as those administered to protect against tuberculosis, polio, pneumonia, and rotavirus.
42,43 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
44 Dotto, C. D., & Cubbon, S. C. (2021, June). Disinformation exports: How foreign anti-vaccine narratives reached West African communities online. First Draft. https://firstdraftnews.org/long-form-article/
45 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
46 Seydou, Aminatou. “Who wants COVID-19
vaccination? In 5 West African countries, hesitancy is high, trust is low.” (2021). https://afrobarometer.org/ publications/ad432
47 Lowes, S., & Montero, E. (2021). The Legacy of Colonial Medicine in Central Africa. American Economic Review, 111(4), 1284–1314. https://doi.org/10.1257/ aer.20180284
48,49 Archibong, B., & Annan, F. (2021). “We Are Not Guinea Pigs”: The Effects of Negative News on Vaccine Compliance. SSRN. https://doi.org/10.2139/ ssrn.3765793
50,51,52 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
53,54 Dotto, C. D., & Cubbon, S. C. (2021, June). Disinformation exports: How foreign anti-vaccine narratives reached West African communities online. First Draft. https://firstdraftnews.org/long-form-article/
55 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
56 Billig, M. & Tajfel, H.. (1973). Social categorization and similarity in intergroup behaviour. European journal of social psychology, 3(1), 27-52. https://doi.org/10.1002/ ejsp.2420030103
57 Attwell, K., Smith, D.T., & Ward, P.R. (2018, March). The Unhealthy Other’: How vaccine rejecting parents construct the vaccinating mainstream. Vaccine, 16211626. https://doi.org/10.1016/j.vaccine.2018.01.076
58 Krishna Kumar, K.P., & Geethakumari, G. (2014). Detecting misinformation in online social networks using cognitive psychology. Human-centric Computing and Information Sciences, 4(1), 1-22. https://doi.org/10.1186/ s13673-014-0014-x
59 Center for American Progress National Security and International Policy Team. (2016, September). State Legitimacy, Fragile States, and U.S. National Security. Center for American Progress. https://cdn.americanprogress. org/wp-content/uploads/2016/09/08062435/ StateLegitimacy-report.pdf
60 Cruwys, T., Stevens, M., Donaldson, J. L., Cárdenas D., Platow, M. J., Reynolds, K. J., & Fong, P. (2021). Perceived COVID-19 risk is attenuated by ingroup trust: Evidence from three empirical studies. BMC Public Health, 21, 869. https://doi.org/10.1186/s12889-02110925-3
61 Seydou, A. (2021, March). Who wants COVID-19 vaccination? In 5 West African countries, hesitancy is high, trust low. Afrobarometer Dispatch No. 432. https:// afrobarometer.org/publications/ad432
62 Lin, C., Tu, P., Beitsch, L. M. (2020). Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 9:16. doi: 10.3390/vaccines9010016
63,64 Babalola, S., Krenn, S., Rosen, J. G., Serlemitsos,
E., Shaivitz, M., Storey, D., Tsang, S., Tseng, T. Y., & Shattuck, D. (2021, September). COVID Behaviors Dashboard. Johns Hopkins Center for Communication Programs in collaboration with Facebook Data for Good, Delphi Group at Carnegie Mellon University, University of Maryland
Social Data Science Center, Global Outbreak Alert and Response Network. https://covidbehaviors.org/
65 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
66 Surgo Ventures (2021). The Challenge of our Time: Achieving High Vaccination Coverage during the COVID-19 Pandemic. https://surgoventures.org/resourcelibrary/the-challenge-of-our-time-achieving-highvaccination-coverage-during-the-covid-19-pandemic
67 Afrobarometer (2021). Summary of results: Afrobarometer Round 8 survey in South Africa in 2021. https://afrobarometer.org/publications/summary-resultsafrobarometer-round-8-survey-south-africa-2021-0
68 Also known as System II thinking. See, e.g., World Bank. (2015). World Development Report 2015: Mind, Society, and Behavior. 26, https://www.worldbank.org/ en/publication/wdr2015
69,70 Pennycook, G., & Rand, D. G. (2021). The Psychology of Fake News. Trends in Cognitive Sciences, 25(5), 388–402. https://doi.org/10.1016/j. tics.2021.02.007
71,72 Rosenzweig, L.R., Bago, B., Berinsky, A.J., & Rand, D.G. (2021, August). Happiness and Surprise Are Associated with Worse Truth Discernment of COVID-19 Headlines among Social Media Users in Nigeria. Harvard Kennedy School Misinformation Review. https://doi. org/10.37016/mr-2020-75
73 Wasserman, H. & Madrid-Morales, D. (2021, April). Social media users in Kenya and South Africa trust science, but still share COVID-19 hoaxes. The Conversation. https://theconversation.com/social-mediausers-in-kenya-and-south-africa
74 Badrinathan, S. (2021, June). Educative Interventions to Combat Misinformation: Evidence from a Field Experiment in India. American Political Science Review.115(4), 1325-1341. https://doi.org/10.1017/
S0003055421000459
75 Nyhan and Reifler describe the backfire effect as follows: “[I]ndividuals who receive unwelcome information may not simply resist challenges to their views. Instead, they may come to support their original opinion even more strongly.” Nyhan, B., & Reifler, J. (2010). When Corrections Fail: The Persistence of Political Misperceptions. Political Behavior. 32, 307. https://doi.org/10.1007/s11109-0109112-2
76 Pennycook, G., Epstein, Z., Mosleh, M., Arechar, A.A., Eckles, D., & Rand, D.G. (2021). Shifting attention to accuracy can reduce misinformation online. Nature, 592, 590–595. doi: 10.1038/s41586-021-03344-2
77 Pennycook, G., & Rand, D. G. (2021). The Psychology of Fake News. Trends in Cognitive Sciences, 25(5), 388–402. https://doi.org/10.1016/j. tics.2021.02.007
78 Martel, C., Pennycook, G. & Rand, D.G. (2020). Reliance on emotion promotes belief in fake news. Cogn. Research, 5, 47. https://doi.org/10.1186/s41235-02000252-3
79 Rosenzweig, L. R., Bago, B., Belinsky, A. J., & Rand, D. G. (2021, August). Happiness and surprise are associated with worse truth discernment of COVID-19 headlines among social media users in Nigeria. Harvard Kennedy School Misinformation Review. https://doi. org/10.37016/mr-2020-75
80 Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing Vaccination: Putting Psychological Science Into Action. Psychological science in the public interest : a journal of the American Psychological Society, 18(3), 149–207. https://doi. org/10.1177/1529100618760521
81 iNudgeyou. (2012, June). Nudging by Descriptive Norms. https://inudgeyou.com/en/nudging-bydescriptive-norms/
82 Brewer, N. T., Chapman, G. B., Rothman, A. J., Leask, J., & Kempe, A. (2017). Increasing Vaccination: Putting Psychological Science Into Action. Psychological science in the public interest : a journal of the American Psychological Society, 18(3), 149–207. https://doi. org/10.1177/1529100618760521
83 Gauri, V., Rahman, T., & Sen, I.K. (2020). Shifting social norms to reduce open defecation in rural India. Behavioural Public Policy, 1-25. doi:10.1017/bpp.2020.46
84 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
85 Lewandowsky, S., Ecker, U. K. H., Seifert, C. M., Schwarz, N. & Cook, J. (2012). Misinformation and Its Correction: Continued Influence and Successful Debiasing. Psychological Science in the Public Interest, 13(3):106-131. doi:10.1177/1529100612451018
86 Bedson, J., Jalloh, M. F., Pedi, D., Bah, S. M., Owen, K., Oniba, A., Sangarie, M., Fofanah, J., Jalloh, M. B., Sengeh, P., Skrip, L. A., Althouse, B. M., & HébertDufresne, L. (2020). Community Engagement during outbreak response: standards, approaches, and lessons from the 2014–2016 Ebola outbreak in Sierra Leone. BMJ Global Health, 5(8). doi:10.1136/bmjgh-2019-002145
87 Legros, S. & Cislaghi, B. (2020, January 1). Mapping the Social-Norms Literature: An Overview of Reviews. Perspectives on Psychological Science 15, no. 1. pp. 62–80. https://doi.org/10.1177/1745691619866455
88 Tulloch, O., Roldan de Jong, T., & Bardosh, K. (2021). Data Synthesis: COVID-19 Vaccine Perceptions in Africa: Social and Behavioural Science Data, March 2020 – March 2021. Social Science in Humanitarian
Action Platform. https://www.socialscienceinaction.org/ resources/data-synthesis-covid-19-vaccine-perceptionsin-africa
89 Bish, A., Yardley, L., Nicoll, A., & Michie, S. (2011). Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine, 29(38), 6472–6484. https://doi.org/10.1016/j. vaccine.2011.06.107
90 Graupensperger, S., Abdallah, D. A., & Lee, C. M. (2021). Social norms and vaccine uptake: College students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine, 39(15), 2060–2067. https://doi.org/10.1016/j. vaccine.2021.03.018
91 Cordina, M., Lauri, M. A., & Lauri, J. (2021). Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharmacy Pract (Granada), 19(1). https://dx.doi.org/10.18549/ pharmpract.2021.1.2317
92 Wollast, R., Schmitz, M., Bigot, A., & Luminet, O. (2021). The Theory of Planned Behavior during the COVID-19 pandemic: A comparison of health behaviors between Belgian and French residents. Plos One. https:// doi.org/10.1371/journal.pone.0258320
93,94 Lewandowsky, S., Ecker, U. K. H., Seifert, C. M., Schwarz, N. & Cook, J. (2012). Misinformation and Its Correction: Continued Influence and Successful Debiasing. Psychological Science in the Public Interest, 13(3):106131. https://doi.org/10.1177/1529100612451018
95 Badrinathan, S. (2021, June 15). Educative Interventions to Combat Misinformation: Evidence from a Field Experiment in India. American Political Science Review.115(4), 1325-1341. https://doi.org/10.1017/ S0003055421000459
96 Rutjens, B.T., Sengupta, N., van der Lee, R., van Koningsbruggen, G.M., Martens, J.P., Rabelo, A., & Sutton, R.M. (2021, April). Science Skepticism Across 24 Countries. Social Psychological and Personality Science. https://doi.org/10.1177/19485506211001329
97 Rachlinski, J.J. (2021, October). What Is Cultural Cognition, and Why Does It Matter? Annual Review of Law and Social Science. 17, 277–91, https://doi.org/10.1146/ annurev-lawsocsci-011921-060754
98 Armstrong, K. (2018, March 30). The WEIRD Science of Culture, Values, and Behavior. Association for Psychological Science. https://www.psychologicalscience. org/observer/
99 ICF. (2019, June 12). Understand cultural values to develop effective responses to fake news. https://www. icf.com/insights/cybersecurity/developing-effectiveresponses-to-fake-news
100 Aina, T. A. (2018). Region Report 2018: SubSaharan Africa. Partnership for African Social & Governance Research. https://hdl.handle.net/1805/15906
101 Ichikowitz Family Foundation. (2020). The Rise of Afro-Optimism: African Youth Survey 2020. https://
ichikowitzfoundation.com/ays2020-book/
102 The Africa Center for Strategic Studies. (2021, May). Dispelling COVID Vaccine Myths in Africa. https:// africacenter.org/spotlight/dispelling-covid-vaccinemyths-in-africa/
103 Babalola, S., Krenn, S., Rosen, J. G., Serlemitsos, E., Shaivitz, M., Storey, D., Tsang, S., Tseng, T. Y., & Shattuck, D. (2021, September). COVID Behaviors Dashboard. Johns Hopkins Center for Communication Programs in collaboration with Facebook Data for Good, Delphi Group at Carnegie Mellon University, University of Maryland Social Data Science Center, Global Outbreak Alert and Response Network. https://covidbehaviors.org/
104 Howard, B. (2020). Religion in Africa: Tolerance and trust in leaders are high, but many would allow regulation of religious speech. Afrobarometer Dispatch No. 339. AD339: Religion in Africa
105 The Africa Center for Strategic Studies. (2021, May). Dispelling COVID Vaccine Myths in Africa. https:// africacenter.org/spotlight/dispelling-covid-vaccinemyths-in-africa/
106 Nsofor, I. (2021, October 22). Personal communication [Zoom interview].
107 Seydou, A. (2021). Who wants COVID-19 vaccination? In 5 West African countries, hesitancy is high, trust low. Afrobarometer Dispatch No. 432. https:// afrobarometer.org/publications/ad432
108 Personas are psychobehavioral archetypes that represent different types of barriers to accepting vaccines. For more information, see: The World Bank. (2021). Vaccination Confidence, Access and Roll-out: COVID-19 Global lessons from the field using behavioral science. UN Innovation Network.
109 Moscoe, E. (2021, October). Personal communication [Group interview].
110,111 Surgo Ventures (2021). The Challenge of our Time: Achieving High Vaccination Coverage during the COVID-19 Pandemic. https://surgoventures.org/resourcelibrary/the-challenge-of-our-time-achieving-highvaccination-coverage-during-the-covid-19-pandemic
112 Coman, A. (2021, November). Personal communication [Group interview].
113 Service, O., Hallsworth, M., Halpern, D., Algate F., Gallagher, R., Nguyen, S., Ruda, S., & Sanders, M. (2014). EAST: Four simple ways to apply behavioural insights. The Behavioural Insights Team. https://www.bi.team/wpcontent/uploads/2015/07/BIT-Publication-EAST_FA_ WEB.pdf
114 United Nations Children’s Fund. (2020). Vaccine Misinformation Field Guide. https://vaccinemisinformation. guide/
115 Africa Center for Strategic Studies. (2021, May). Dispelling COVID Vaccine Myths in Africa. https:// africacenter.org/spotlight/dispelling-covid-vaccinemyths-in-africa/
116 Africa CDC. (2021, March). COVID 19 vaccine
perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
117 Dotto, C. D., & Cubbon, S. C. (2021, June).
Disinformation exports: How foreign anti-vaccine narratives reached West African communities online. First Draft. https://firstdraftnews.org/long-form-article/ foreign-anti-vaccine-disinformation-reaches-west-africa/
118 Bryan, C.J., Yeager, D.S. & Hinojosa, C.P. (2019). A values-alignment intervention protects adolescents from the effects of food marketing. Nature Human Behaviour 3, 596–603. https://doi.org/10.1038/s41562-019-0586-6
119 Dotto, S., & Cubbon, S. (2021, June 23).
Disinformation exports: How foreign anti-vaccine narratives reached West African communities online. First Draft News. https://firstdraftnews.org/long-form-article/ foreign-anti-vaccine-disinformation-reaches-west-africa/
120 Data from Social Media Stats Africa. https:// gs.statcounter.com/social-media-stats/all/africa
121 The Economist. (2019). How WhatsApp is used and misused in Africa. https://economist.com/middleeast-and-africa/2019/07/18/how-whatsapp-is-usedand-misused-in-africa
122 Walwema, J. (2020, September 16.).
The WHO Health Alert: Communicating a Global Pandemic with WhatsApp. Journal of Business and Technical Communication. https://doi. org/10.1177/1050651920958507
123 Vital Strategies: Resolve to Save Lives. (2020, May). WhatsApp Campaign Guidance During COVID-19: Approach to developing WhatsApp campaigns. https:// cities4health.org/assets/library-assets/ccc_084_ whatsapp-campaign-guidance_050820.pdf
124 Ling, E. C., Tussyadiah, I., Tuomi, A., Stienmetz, J., & Ioannou, A. (2021). Factors influencing users’ adoption and use of conversational agents: A systematic review. Psychology & Marketing, 38, 1031-1051. https://doi. org/10.1002/mar.21491. See Rietz et al. (2019) and Amini et al. (2013) in particular.
125 Tsai, W. S., Lun, D., Carcioppolo, N., & Chuan, C. H. (2021). Human versus chatbot: Understanding the role of emotion in health marketing communication for vaccines. Psychology & marketing, 10.1002/mar.21556.
Advance online publication. https://doi.org/10.1002/ mar.21556
126 Höhn, S. & K. Bongard-Blanchy. (2020). Heuristic Evaluation of COVID-19 Chatbots. In: Følstad A. et al. (eds) Chatbot Research and Design. Conversations 2020. Lecture Notes in Computer Science, vol 12604. Springer, Cham. https://doi.org/10.1007/978-3-030-68288-0_9
127 Basol, M., Roozenbeek, J., Berriche, M., Uenal, F., McClanahan, W. P., & Linden, S. van der. (2021). Towards psychological herd immunity: Cross-cultural evidence for two prebunking interventions against COVID-19 misinformation. Big Data & Society. https:// doi.org/10.1177/20539517211013868
128 Go Viral! Game. About page. https://www. goviralgame.com/en. Accessed 2021.
129 Roozenbeek, J., & van der Linden, S. Fake news game confers psychological resistance against online misinformation. Palgrave Commun 5, 65 (2019). https:// doi.org/10.1057/s41599-019-0279-9
130 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
131 Paluck, E.L. (2009, March). Reducing intergroup prejudice and conflict using the media: a field experiment in Rwanda. Journal of Personality and Social Psychology. 96(3), 574-87. https://doi.org/10.1037/a0011989
132 Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https:// africacdc.org/download/covid-19-vaccine-perceptions-a15-country-study/
133 Consistent access to the internet would be crucial for the online game aspect of the intervention.
134 These four types of messages are based on the evidence from Hallsworth, M., Snijders, V., Burd, H., Prestt, J., Judah, G., Huf, S., & Halpern, D. (2016). Applying behavioral insights: simple ways to improve health outcomes. World Innovation Summit for Health.
135 Langfitt, F. (2021, April 26). How a U.K. imam countered vaccine hesitancy and helped thousands get the ‘jab’. NPR. https://www.npr. org/2021/04/26/988165812/
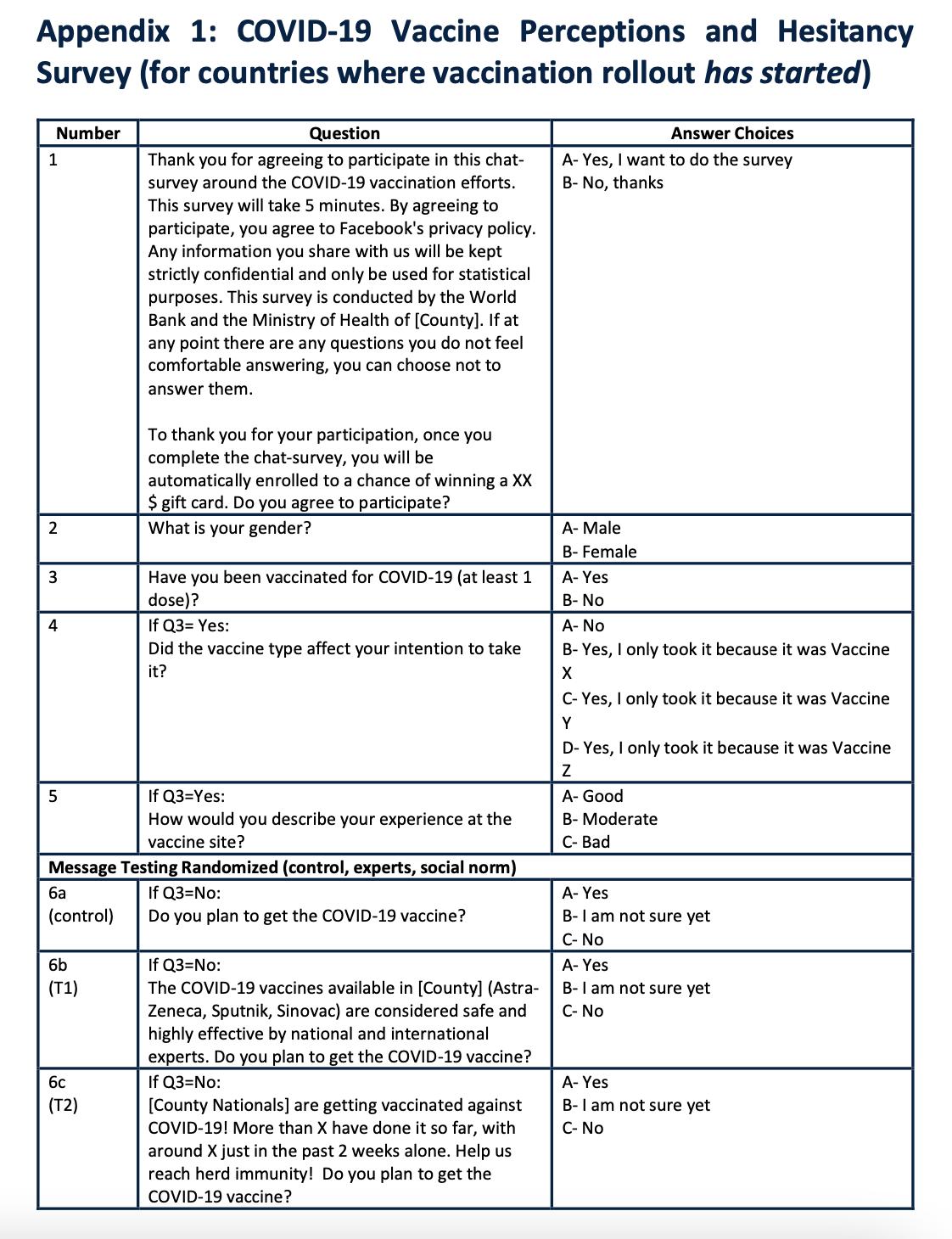
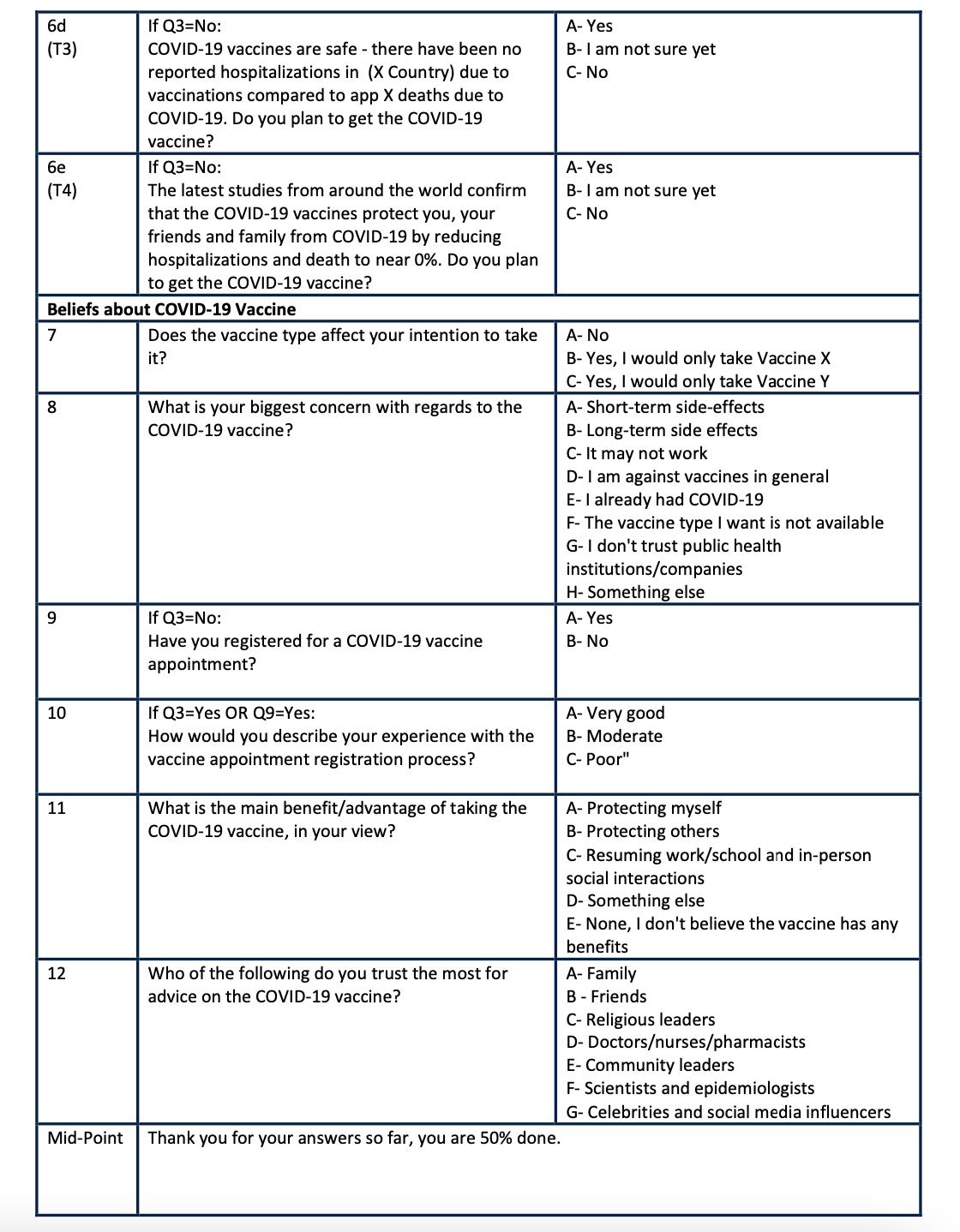
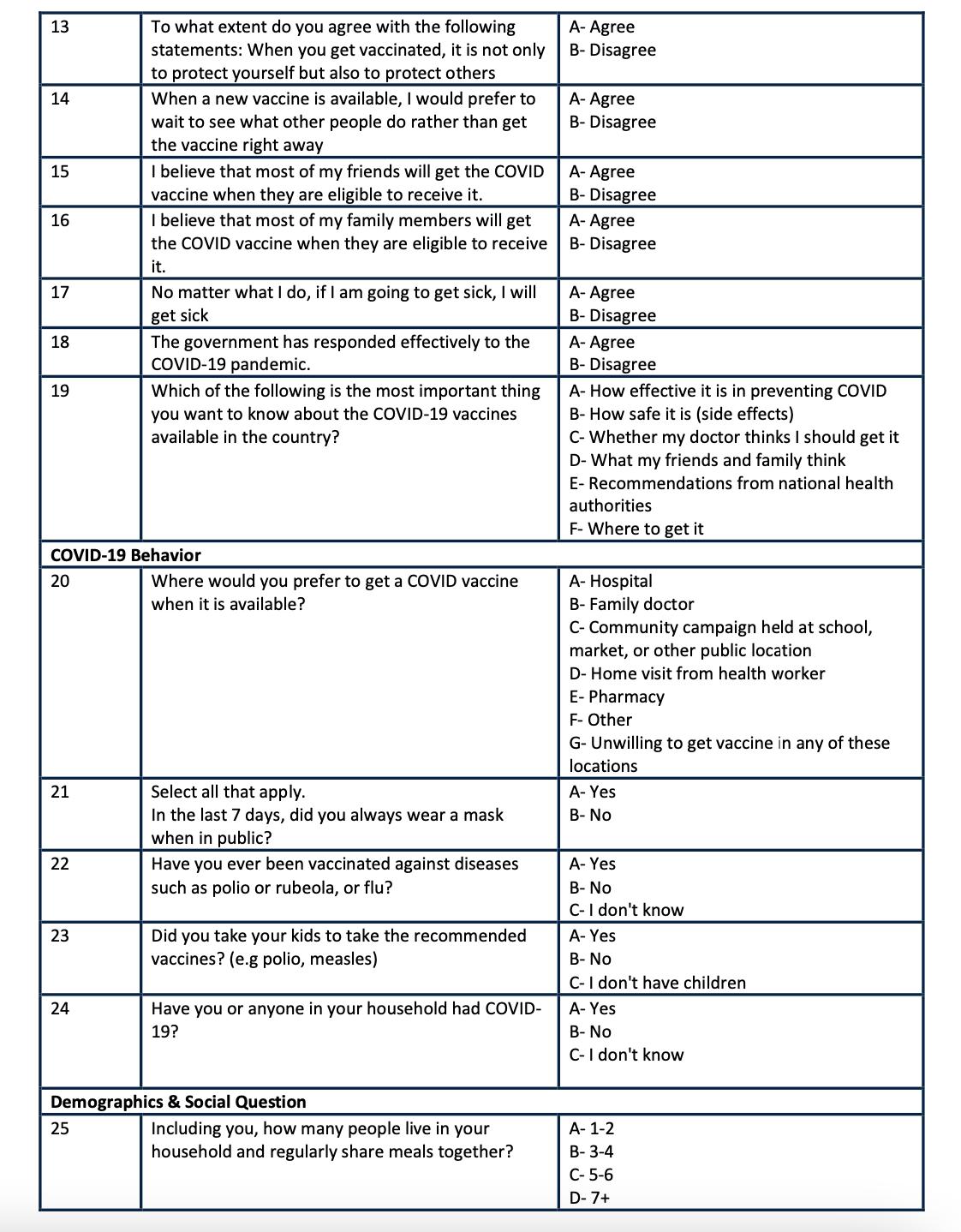
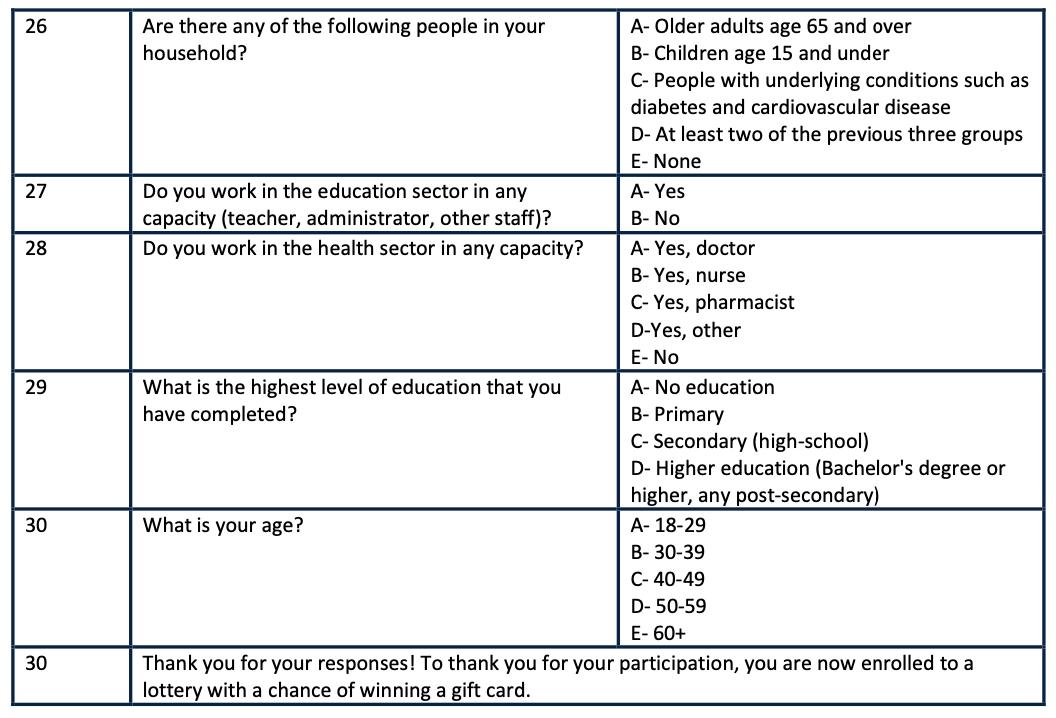
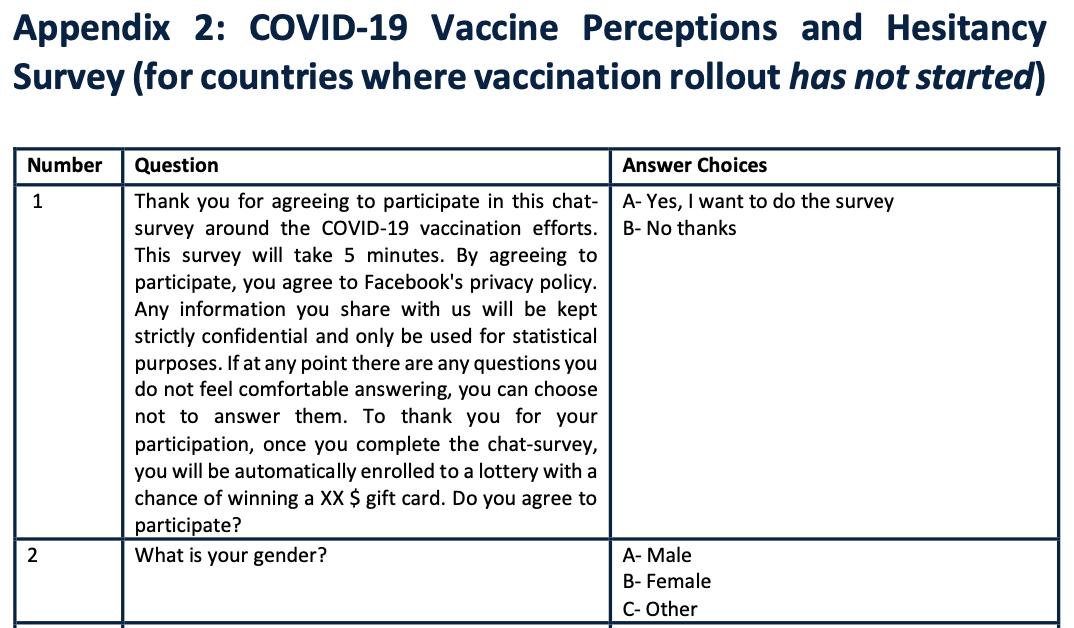
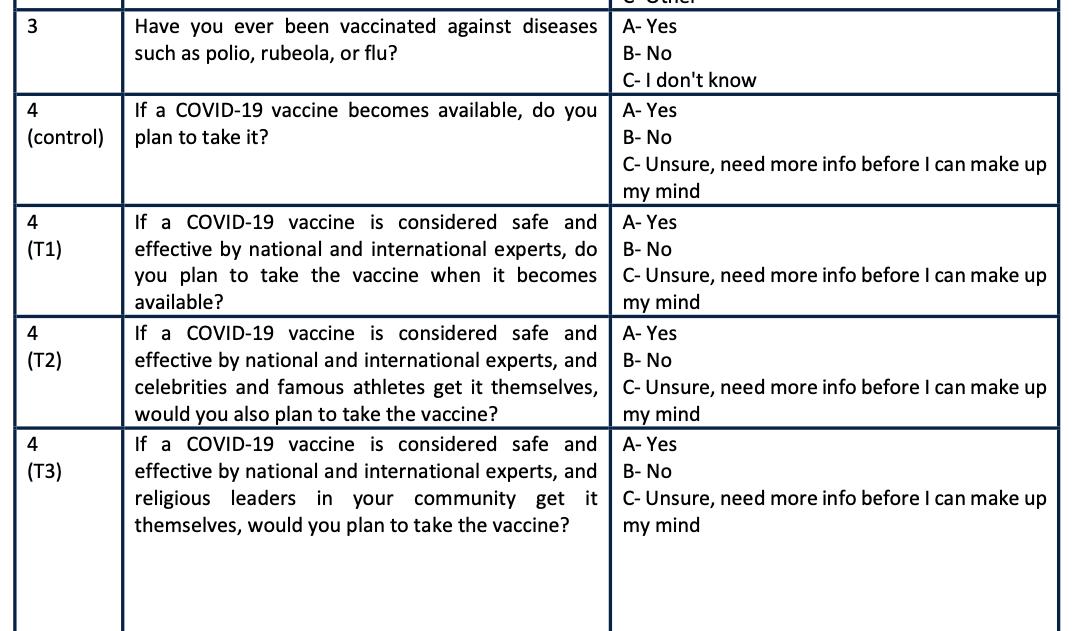
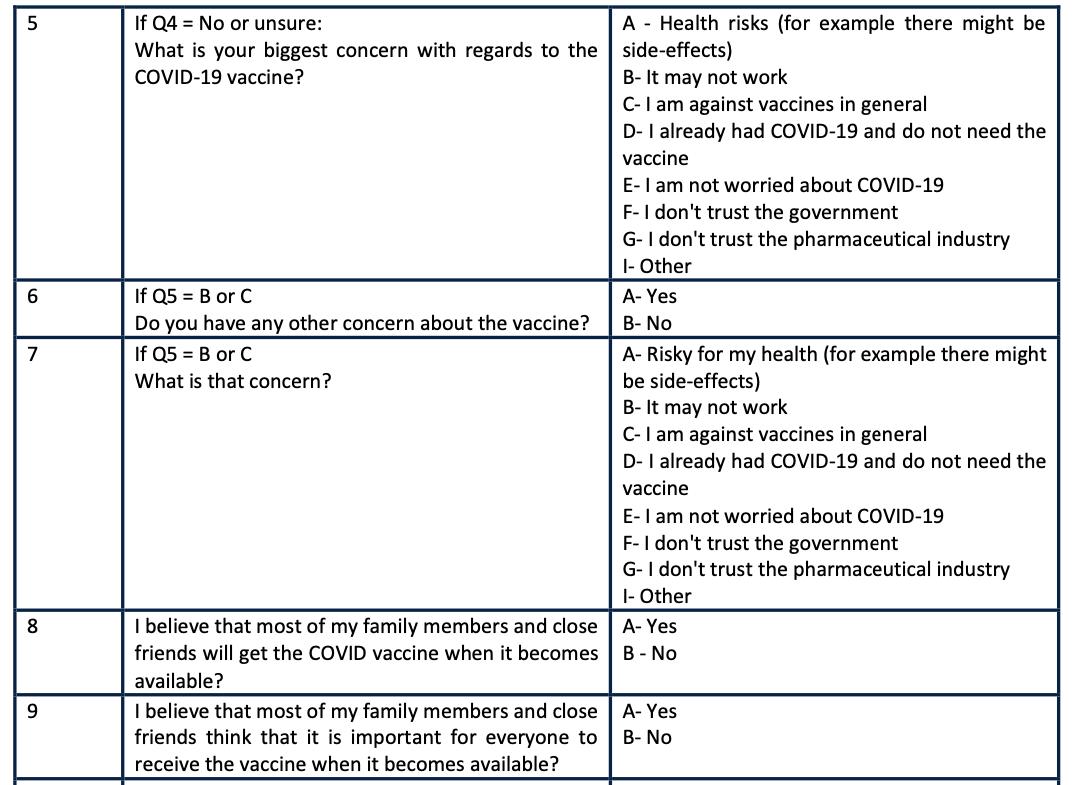
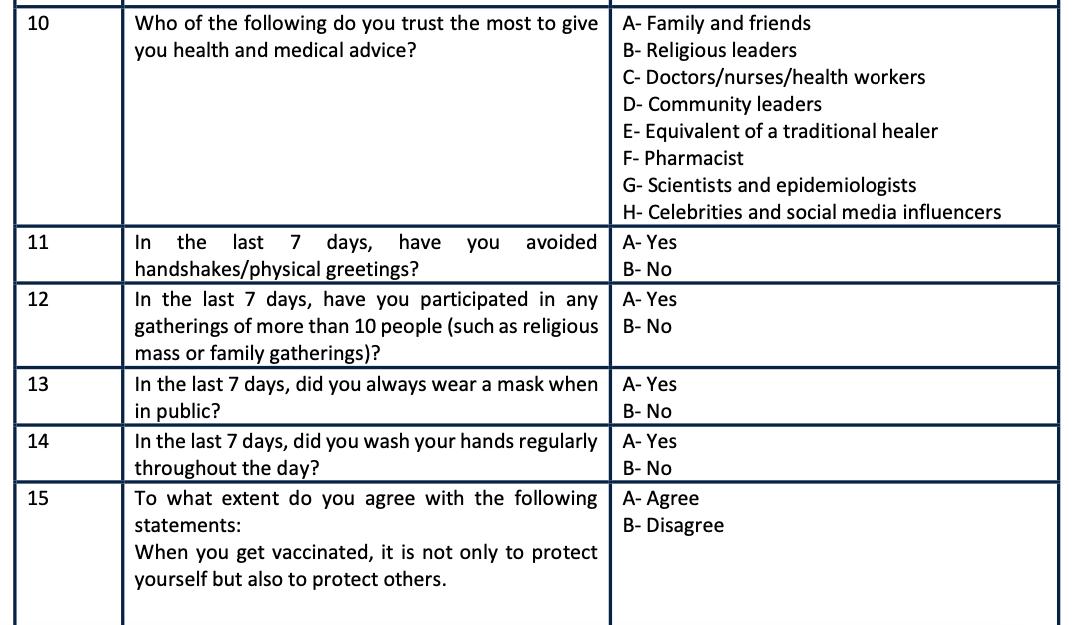
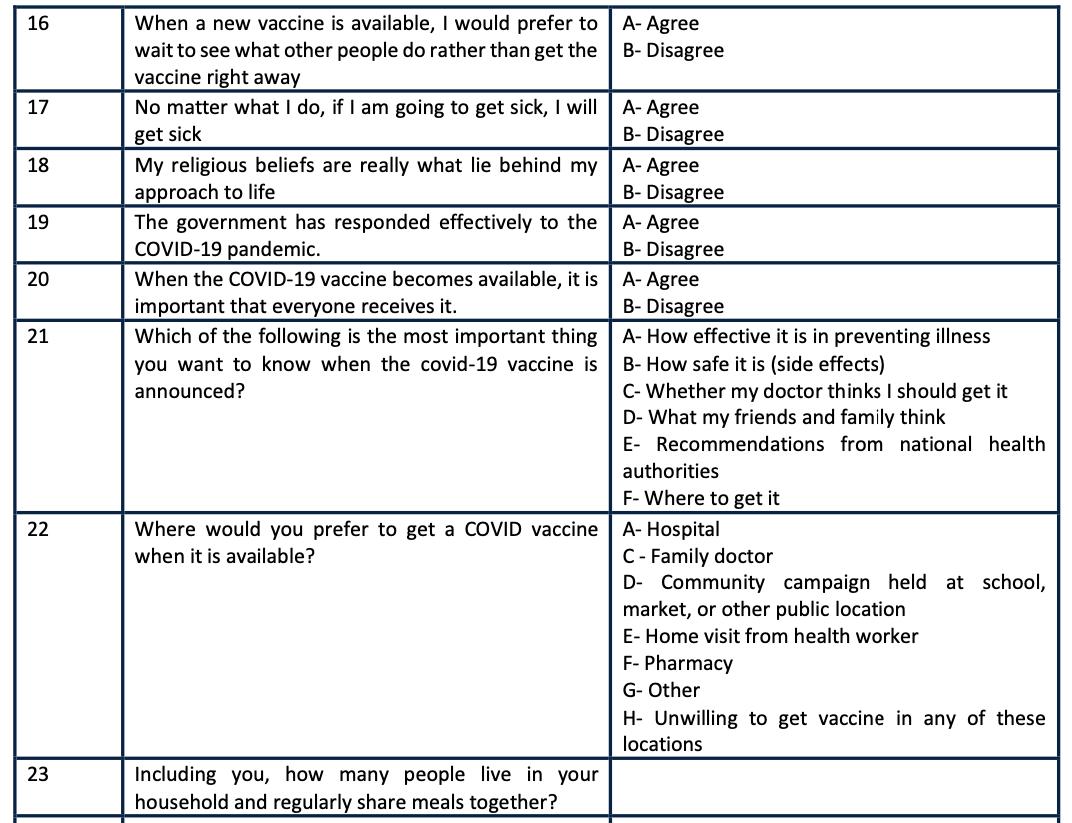
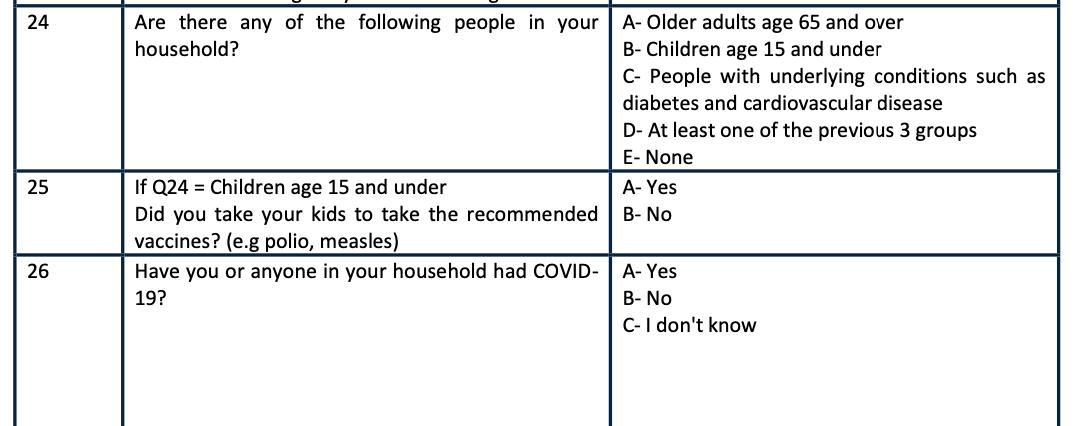
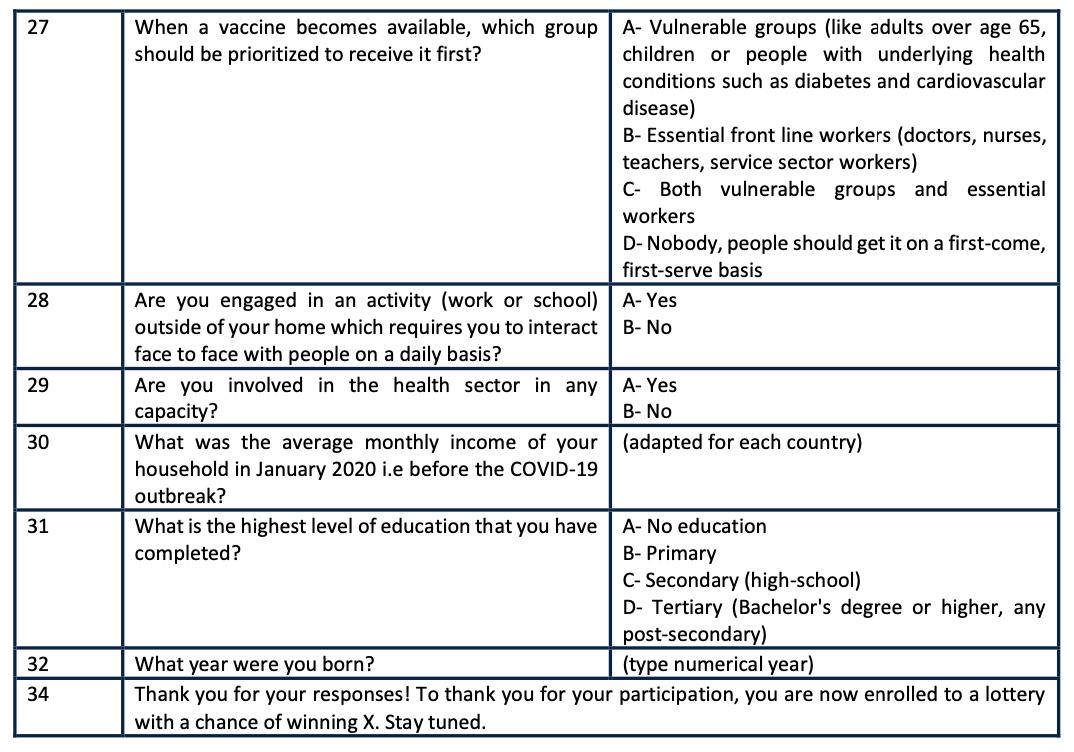
The following diagnostic questions were proposed to the eMBeD team as additions to the survey in October of 2021. They are included here for ease of access with the rest of the report.
Since the literature has shown the mode of transmission of misinformation matters for designing an intervention,i we believe it is important to diagnose where individuals are getting their (mis) information from. The Africa CDC has reported some related statistics from their 15-country survey on misinformation. They found that 64% of respondents mention television as one of their most trusted sources for information about COVID-19, followed by radio (51%), online sources (41%), health institutions (23%), and government sources (18%). Africa CDC reported that these sources showed significant variation across countries, so it will be important to collect countryspecific data. In addition, the Africa CDC study surveyed respondents via both face-to-face and telephone interviews.ii Based on our conversation with the Gates Foundation, it seems that the results from face-to-face surveys and telephone interviews as compared to Facebook surveys are quite different; Facebook surveys consistently produce higher levels of self-reported hesitancy than other modes of surveys.iii
1. Where do you frequently get information about COVID-19 vaccines?
a. Social media
b. WhatsApp
c. Other messaging service (ex. Facebook Messenger, Email)
d. Radio
e. Television
f. Newspaper
g. Family or friends
The next question is intended to test whether the mental model of vaccines as an international tool of manipulation/control is prevalent.
2. “Powerful people in foreign countries are using COVID-19 to take advantage of people like me.” Do you agree or disagree?
a. Agree
b. Somewhat agree
c. Neutral
d. Somewhat disagree
e. Disagree
This question is intended to test whether the mental model of vaccines as a domestic tool of manipulation/control is prevalent.
3. “Powerful people in my own country are using COVID-19 to take advantage of people like me.” Do you agree or disagree?
a. Agree
b. Somewhat agree
c. Neutral
d. Somewhat disagree
e. Disagree
Question 4 aims to identify people’s perception of the social norm of vaccine uptake, preparing a possible nudge with descriptive norms.
4. What is your estimate of the percent of people in your country that plan to get the COVID-19 vaccine?
a. 90-100%
b. 80-90%
c. 70-80%
d. 60-70%
e. 50-60%
f. 40-50%
g. 30-40%
h. 20-30%
i. 10-20%
j. 0-10%
Question 5 tests whether it is possible to increase risk perception and trigger loss aversion, thus influencing respondents’ intention to get vaccinated.
5. The Omicron variant, now circulating in Africa, is more than two times as contagious as the original COVID-19 strain, and has infected millions of Africans. It is infecting young people, and driving the threat in Africa to a whole new level. Do you plan to get the COVID-19 vaccine?
a. Yes
b. Most likely
c. Perhaps
d. Probably not
e. No
f. I can't say
Question 6 is intended to gauge perceptions of behavior around sharing COVID-19 information, given that literature has suggested much of the sharing of misinformation is due to inattention.iv
6. “I verify information about COVID-19 before I share it with others.” Do you agree or disagree?
a. Agree
b. Somewhat agree
c. Neutral
d. Somewhat disagree
e. Disagree
i Badrinathan, S. (2021, June 15). Educative Interventions to Combat Misinformation: Evidence from a Field Experiment in India. American Political Science Review.115(4), 1325-1341. https://doi.org/10.1017/ S0003055421000459
ii Africa CDC. (2021, March). COVID 19 vaccine perceptions: A 15 country study. African Union. https://africacdc.org/download/ covid-19-vaccine-perceptions-a-15-country-study/
iii Black, T. & Pituch, J. (2021, October 22). Gates Foundation. Personal communication [Zoom interview].
iv Pennycook, G., & Rand, D. G. (2021). The Psychology of Fake News. Trends in Cognitive Sciences, 25(5), 388–402. https://doi. org/10.1016/j.tics.2021.02.007