Expanding Health Insurance Coverage in the United States Virgin Islands






This report was prepared by Master in Public Affairs students at Princeton University’s School of Public and International Affairs. This report incorporates information gathered through students’ independent research, in-person and remote interviews conducted between October 17 and October 28, 2022, and invaluable guidance from course instructors Heather Howard and Dan Meuse. The report fulfills the Princeton School of Public and International Affairs’ degree requirements for an immersive policy workshop and associated policy proposal. We are grateful to the United States Virgin Islands Department of Human Services that enabled us to conduct research and make recommendations on this topic, particularly to Medicaid Director Gary Smith. We also wish to extend our gratitude to the many policymakers, health professionals, consumer advocates, and subject matter experts who shared their perspectives with us throughout the course of this project. We hope that this report will contribute to ongoing efforts to build on and expand the successes of the United States Virgin Islands’ Medicaid program.
Eduardo bhatia, Former President, Senate of Puerto Rico, and John L. Weinberg/Goldman Sachs & Co Visiting Professor, Princeton School of Public and International Affairs
Cheryl Charleswell , Chief Examiner, United States Virgin Islands Division of Banking, Insurance, and Financial Regulation
Tina Comissiong , Chief Executive Officer, Schneider Regional Medical Center
Justa Encarnacion, Commissioner, United States Virgin Islands Department of Health
Senator novelle E. francis Jr. , Vice President, Legislature of the Virgin Islands
Senator Donna frett- gregory, President, Legislature of the Virgin Islands
lisa Hanley, Interim Director for Healthcare Service Financials, Governor Juan F. Luis Hospital and Medical Center
Tai Hunte-Caesar, Chief Medical Officer, United States Virgin Islands Department of Health
Rosalie Javois, Interim Executive Vice President of Finance, Governor Juan F. Luis Hospital and Medical Center
natasha Joseph, Financial Advisor, St. Thomas East End Medical Center
Doug koch, Chief Executive Officer, Governor Juan F. Luis Hospital and Medical Center
Joanne luciano, Partner, Data and Technology Associates, LLC
Roida mason, Vice President of Human Resources, Schneider Regional Medical Center
g lendina m atthew, Acting Director, United States Virgin Islands Division of Banking, Insurance, and Financial Regulation
Hazel Philbert , Chief Operating Officer, Governor Juan F. Luis Hospital and Medical Center
Darice Plaskett , Chief Nursing Officer, Governor Juan F. Luis Hospital and Medical Center
Julia Sheen, Health and Human Services Policy Advisor to Governor Albert Bryan
gary Smith, Medicaid Director, United States Virgin Islands Department of Human Services
massarae Sprauve webster, Chief Executive Officer, Frederiksted Health Care, Inc.
Donna Street , Manager of Billing & Collections, St. Thomas East End Medical Center
Shawna Richards, Chief of Staff to Senator Novelle Francis
brandon Richardson, Vice President of Information Systems, Schneider Regional Medical Center
Janis Valmond, Deputy Commissioner, United States Virgin Islands Department of Health
Su- l ayne walker, Legal Counsel, Schneider Regional Medical Center
Jay w oods , Director of Revenue Services, Frederiksted Health Care, Inc.
EXPANDING HEALTH INSURANCE COVERAGE IN THE UNITED STATES VIRGIN ISLANDS
A bP Alternative Benefit Plan
ACA The Patient Protection and Affordable Care Act
APP Advanced Practice Provider
APR n Advanced Practice Registered Nurse
bEAD Broadband Equity, Access, and Deployment Program
CHIP Children’s Health Insurance Program
Cm S Centers for Medicare and Medicaid Services
CoVID-19 SARS-CoV-2, or Coronavirus 2
CSf Critical Shortage Facility
DoH Department of Health
DHS Department of Human Services
ffCRA Families First Coronavirus Response Act
fm AP Federal Medical Assistance Percentage
fQHC Federally Qualified Health Center
f Y Fiscal Year
HCoP Health Careers Opportunity Program
HIE Health Information Exchange
HPSA Health Professional Shortage Areas
HRSA Health Resources and Services Administration
ImlC Interstate Medical Licensure Compact
lCmE Liaison Committee on Medical Education
nf Nurse Faculty
nHSC National Health Service Corps
PmPm Per-Member Per-Month
R n Registered Nurse
SPA State Plan Amendment
USVI The United States Virgin Islands
USVIPl USVI Poverty Level
UVI University of the Virgin Islands

As a U.S. territory, the U.S. Virgin Islands (USVI) is situated in a unique geographical, population, and funding context. Not only is the USVI over a thousand miles away from the mainland U.S. and frequently susceptible to natural disasters such as hurricanes, but its population of approximately 87,000 people is seven times smaller than the smallest state.1 The USVI is also subject to many legal and financial challenges that impact the health of its residents. Its high cost of living paired with a high poverty rate exacerbate health disparities compared to the general U.S. population, and the USVI’s status as a territory makes it ineligible for certain federal healthcare funding opportunities that are normally available to states. This report proposes recommendations to improve access to affordable and quality healthcare given these constraints.
Our primary recommendation is to increase health insurance coverage for USVI residents by implementing a Medicaid buy-in program. We also recommend several broader health system improvements to enable the success of a Medicaid buy-in program. We selected these strategies based on their ability to improve health insurance coverage, access to care, and population health outcomes, while also considering estimated costs, political viability, and potential administrative burden on USVI government agencies. Our recommendations, which are summarized in a table on the following page, were ultimately informed by insights drawn from interviews with 27 stakeholders across government, healthcare facilities, and partner organizations in the USVI.

Establish a medicaid buy-in Program
1. Identify the eligible population and determine the income eligibility threshold
2. Establish a premium structure and use the remaining Medicaid funds allotted to the USVI to subsidize premiums
3. Adjust the Alternative Benefit Plan for the Medicaid buy-in population
4. Design a marketing strategy to promote take-up of the Medicaid buy-in program
Expand Health Education measures and Improve Health literacy
1. Promote the importance of preventive care through individual patient interactions and broader community outreach
2. Educate residents about the benefits of health insurance
1. Partner with the UVI Medical School
2. Adopt medical compacts to facilitate provider licensing
3. Increase telehealth utilization
4. Leverage health workforce development funds to increase provider supply
5. Improve care coordination
1. Create a new cross-agency Healthcare Cabinet task force
2. Develop a centralized government healthcare website for healthcare information.
1. Improve collaboration between DOH and health facilities for data sharing
2. Train interested DHS and DOH employees in data analysis
3. Establish the Health Information Exchange
Like other territories, the structure of the capped block grant Medicaid system of the USVI results in limited federal resources for the provision of care. Individuals without employer-sponsored health insurance, who earn an income that is too high to qualify for Medicaid, are left without a coverage option due to the unavailability of individual health insurance plans. The tempestuous fiscal cycles of the federal government expose additional vulnerabilities for territories by creating moments of funding uncertainty.
In this unique environment, the Department of Human Services requested our assistance in identifying options to expand coverage to more residents of the USVI. The Medicaid buy-in program serves to include more members, who would have otherwise been ineligible for coverage, and provide them with access to healthcare services.

In this report, the background section offers context on demographics, economic considerations, and the healthcare landscape of the USVI. Next, the methodology section outlines our research methods and analytical approach to developing recommendations. The subsequent set of recommendations all serve the overarching goal of covering more residents of the USVI with comprehensive health services. Recommendation
1 is our core policy recommendation, while Recommendations 2–5 are enabling recommendations which are critical to the success of core Recommendation 1.
While this is not an exhaustive list of ways to expand healthcare access, these recommendations draw on recurring themes from stakeholder interviews conducted in the USVI. We heard about individuals who would like to use Medicaid, the need to improve and expand health education and literacy, the challenge of provider shortages, a desire to improve intergovernmental coordination, and the relevance of effective health data collection and analysis.
The authors of this report are eight graduate students at Princeton University’s School of Public and International Affairs, and this report is prepared for the capstone project of the Master in Public Affairs program. This report is informed by secondary research as well as interviews with stakeholders across St. Thomas and St. Croix during autumn 2022. This project benefited from the guidance of the course’s co-instructors: Heather Howard and Daniel Meuse, two national healthcare policy experts who lead the State Health and Value Strategies program of the Robert Wood Johnson Foundation, located at Princeton University.
According to the 2020 Census, 87,146 people currently reside in the U.S. Virgin Islands (USVI). This represents an 18% decrease in population since 2010. 2 The USVI’s population decline was exacerbated by the devastation of Hurricanes Irma and Maria in 2017, after which many residents left the territory. 3 However, the population decline began in the years leading up to the hurricanes; 11,000 residents are estimated to have emigrated from the USVI prior to 2016 in response to economic issues detailed in the following section. 4
A summary of the USVI population by race, age, and income course is provided in figure 1 below. While this report uses population figures from the 2020 Census, a number of stakeholders interviewed throughout our research reported concerns with the accuracy of the 2020 Census, noting challenges around data collection during the COVID-19 pandemic. Stakeholders suspected that the number of residents without legal immigration status in the USVI were undercounted in the Census, potentially out of fear of speaking to government representatives. We provide an estimate of the undocumented population residing in the USVI in Appendix b.
The reported population decline is associated with a 27% decline in the local economy, measure d by real Gross Territorial Product, from 2008 to 2016. 5 The USVI lost an estimated 6,000 jobs during this period of economic recession.6 An additional 4,300 USVI residents filed jobless claims after the 2017 hurricanes, representing a loss of roughly 8% of all jobs in the territory.7

These economic challenges have exacerbated poverty rates in the USVI, which are significantly higher than national rates. 8 The median family income in the USVI is $52,000, compared to the national median family income of $67,521. In 2020, 22.8% of the USVI’s population lived in a household where the household income was below the federal poverty level. Child poverty rates were particularly high, with 33% of children under 18 living in a household with household income below the federal poverty level.9
High poverty rates correspond to higher health risks among the USVI’s population across multiple chronic disease areas. Obesity rates in the USVI are higher than the national average: 32.2% of adults reported a body mass index of 30.0 or higher in USVI in 2016, compared to 30.1% of U.S. adults nationally. Diabetes is also more prevalent, with 16.8% of USVI adults reporting having ever been told they had diabetes, compared to 10.5% of adults nationally in 2016. Residents who are Black, non-Hispanic, older, lower income, and with lower levels of education were all more likely to have been diagnosed with diabetes.10
One contributing factor to these health outcomes may be the limited access to preventive care in the USVI. In 2016, USVI estimates of preventive service uptake lagged behind national figures across a range of critical services, including prenatal care, routine mammograms and colonoscopies, and child vaccination.11
Healthcare remains unaffordable for many residents in the USVI. As a result of high health service costs, many forego care: 22% of people in the USVI report that they were unable to see a doctor due to high costs in the past year, compared with 13% of individuals surveyed in the 50 states and D.C.12
However, all USVI residents are guaranteed care, regardless of income or insurance status. A statutory requirement added to the USVI Code in 2019 states “no resident of the Virgin Islands shall be denied medical care because of financial inability to pay.”13 While this requirement is critical to ensuring access to care, it also creates financing challenges for the hospitals and clinics in the USVI when patients are unable to pay for services. As a result, Juan F. Luis Hospital estimates roughly $40 million per year in uncompensated care.14 While the territory allots some funding to reimburse facilities for uncompensated care, it is not sufficient to cover the full costs.
While the USVI has made notable strides toward expanding health insurance coverage over the last few years, 24.6% of the population still lacked coverage in 2020.15 This uninsured rate remains well above national uninsured rates – 6.6% in Medicaid expansion states and 12.7% in non-expansion states.16 Among the remaining three quarters of the USVI’s population, 46.6% had private health insurance in 2020 and 37.2% had public insurance coverage.17 The share of residents with public insurance has increased further over the last two years due to the continuous coverage requirement that prevents disenrollment of Medicaid enrollees during the public health
emergency (PHE). This is further discussed in the section below regarding COVID-19 policy changes.
USVI residents have limited options for health insurance coverage. Like other states and territories, the fair market rules of the Affordable Care Act (ACA) that are meant to protect consumers apply to the insurance markets of the USVI. These include guaranteed issue, restrictions on annual and lifetime caps, and protections for those with pre-existing conditions. However, unlike states, the USVI does not have access to the subsidies offered in the ACA that typically protect the stability of the insurance market while providing affordable coverage to consumers. As a result, no individual health insurance plans currently exist in the USVI. All private insurance plans are offered to large groups or through employers. Roughly a quarter of residents covered by private health insurance in 2020 were enrolled in the territorial government insurance plan offered by Cigna.18
Emigration has left a shortage of doctors and other healthcare providers in the USVI.19 In our interviews, stakeholders reported that attracting and retaining new providers is difficult given lower local salaries than those in the states. Additionally, the lack of specialist providers practicing in the territory results in the frequent need for residents to fly to Puerto Rico or the mainland for care.
Each of the USVI ’s three largest islands, St. Thomas, St. Croix, and St. John, are designated Health Professional Shortage Areas (HPSA) for primary care services, and the Health Resources and Services Administration (HRSA) estimates that 15 additional primary care providers are required to fill the access gap. 20 This would represent a 21% increase from the current 72 primary care providers. 21
In 2016, an estimated 23,177, or 22%, of Virgin Islanders received health insurance from Medicaid or the Children ’s Health Insurance Program (CHIP). As of September 2021, that number had increased to 34,158 individuals, meaning as much as 39% of USVI’s population is now enrolled in Medicaid or CHIP. 22
The USVI’s Medicaid program offers 13 of the 15 mandatory Medicaid benefits (figure 2). Additionally, the program offers two optional benefits to enrollees: prescription drugs and dental services.
The USVI has historically faced two key restrictions on federal funding for its Medicaid program.
First, the USVI has a statutory annual cap on federally matched funding, while federal funds to the 50 states and D.C. have no such cap. Second, the USVI’s Federal Medical Assistance Percentage (FMAP) is statutorily set, unlike the FMAP for the states, which is calculated annually based on each state’s per capita income. 23 While the ACA raised the FMAP for the USVI from 50% to 55%, this match rate still amounted to insufficient federal funding levels for the territory, given that the rate would have been 83% if it were calculated using the same methodology as the states. 24 However, these federal funding limitations have recently been addressed, detailed in the next subsection.
The COVID-19 pandemic dramatically altered the federal funding landscape for Medicaid in the USVI. The USVI saw an unprecedented influx of
✓ Inpatient hospital services
✓ Outpatient hospital services
✓ EPSDT: Early and Periodic Screening, Diagnostic, and Treatment Services
✓ Nursing Facility Services
✓ Home health services
✓ Physician services
✓ Federally qualified health center services
✓ Laboratory and X-ray services
✓ Family planning services
✓ Nurse Midwife services
✓ Certified Pediatric and Family Nurse Practitioner services
✓ Transportation to medical care
✓ Tobacco cessation counseling for pregnant women
x Rural health clinic services
x Freestanding Birth Center services
federal health funding beginning in Fiscal Year (FY) 2020, when the Families First Coronavirus Response Act (FFCRA) increased the USVI’s federal funding cap from $18.3 million to $128.7 million. Additionally, throughout the pandemic, Congress temporarily raised the FMAP to the maximum rate of 83% for the USVI through a series of short-term funding bills. This change was recently made permanent in the Consolidated Appropriations Act, 2023 (H.R. 2617), signed into law at the end of 2022. 25 This is a critical step toward ensuring the continuity of new services offered under Medicaid during the pandemic, including a personal care attendant program, a hospice benefit, and assistance for Medicare
premiums for some dual eligible residents. 26 Additionally, the FFCRA included a provision that required states and territories to provide continuous coverage for Medicaid enrollees throughout the PHE to receive enhanced federal funding. 27 This provision has increased Medicaid enrollment by 28% nationally since the start of the pandemic and has benefitted a significant number of USVI residents. However, the recent Consolidated Appropriations Act, 2023 set the end of the continuous coverage requirement for March 31, 2023. 28 Now, the USVI faces the challenge of implementing a redetermination process that may result in the loss of coverage for thousands of residents.

USVI, including government, health facilities, and non-governmental partners.

We collected information for this report in two stages. First, we conducted a literature review of the USVI’s health system context, key challenges, and current and past policies affecting healthcare delivery in the territory. Second, we conducted 13 interviews with USVI-based stakeholders from October to November 2022. These interviews allowed us to incorporate the perspective of 27 stakeholders in this report, representing a range of organizations across the
In the following report sections, we outline recommendations to improve health insurance coverage for U.S. Virgin Islanders developed based on our research and stakeholder interviews. Recommendation 1 first focuses on the core proposal to design and implement a Medicaid buy-in program. Then, Recommendations 2 through 5 provide broader health system strengthening strategies to enable successful implementation of the Medicaid buy-in program.
To evaluate the recommendations, we used a decision matrix and scored each recommendation based on the following criteria:
External Considerations: These factors provide estimated impacts of each recommendation on USVI residents based on how they are able to access and afford healthcare in the territory. Recommendations that have a positive, direct impact on health access and outcomes receive a higher score than recommendations with limited or no impact.
• Access to Health Insurance: How will this recommendation impact the ability for USVI residents to navigate insurance options and enroll in health insurance in the territory?
• Access to Care: How will this recommendation impact the ability of USVI residents to see providers and receive care in the territory?
• Territory Health Outcomes: How will this recommendation impact health outcomes for residents in the USVI, including disease burdens affecting the territory such as diabetes, hypertension, and obesity?
Internal Considerations: These factors provide determinations for the USVI government
and healthcare stakeholders to consider when implementing each recommendation, based on estimated cost, political feasibility, and burden on agencies and their staff. Recommendations which are more politically feasible and less costly and burdensome to the USVI government are scored higher than more expensive recommendations which may require broader agreement, legislation, and/or federal approval to implement.
• Administrative Burden: What is the capacity of the territory’s government agencies to implement this recommendation, given their current resources and staffing levels?
• Financial Impact: What is the cost of this recommendation to the USVI government, in terms of its territory budget? Will it require new local territory funds to implement?
• Political Feasibility: Does this recommendation require legislative action or approval from the federal government to implement? If so, how likely is it that the recommendation will get approved or passed into law? Will healthcare stakeholders in the territory be broadly in support of or against the proposals of this recommendation?
Recommendation 1: Establish a Medicaid Buy-In Program
Identify the eligible population and determine an income threshold.
Establish a premium structure and use the remaining Medicaid funds allotted to the USVI to subsidize premiums.
Adjust the Alternative Benefit Plan for the Medicaid buy-in population.
Design a marketing strategy to promote take-up of the Medicaid buy-in program.
Recommendation 2: Expand Health Education Measures and Improve
Promote the importance of preventive care through individual patient interactions and broader community outreach.
Educate residents about the benefits of health insurance.
Recommendation 3: Address Provider Shortages
Partner with the UVI Medical School. Adopt medical compacts to facilitate provider licensing. Increase telehealth utilization.
Leverage health workforce development funds to increase provider supply. Improve care coordination.
Recommendation 4: Improve Coordination Between Different government Agencies and Departments
Create a new Healthcare Cabinet, a cross-agency task force that meets regularly to discuss healthcare policy, programs, and insurance.
Develop a centralized government healthcare website for USVI residents to reference consolidated access points to care and information on government and community healthcare resources.
Recommendation 5: Enhance Health Data Collection, Analysis, and Coordination Practices
Improve collaboration between DOH and health facilities for data sharing.
Train interested DHS and DOH employees in data analysis.
Establish the Health Information Exchange as a centralized data repository for population health tracking by expanding patient inclusion.
Our primary recommendation for increasing health insurance coverage and improving health outcomes in the USVI is to establish a Medicaid buy-in program. This recommendation was motivated by two factors: the USVI is a high risk market for potential private insurers and the USVI receives limited federal contributions towards paying for its healthcare costs.
When we thought through how to increase health insurance coverage in the USVI, we identified three factors that make the USVI a high risk market to private insurers. First, the USVI’s relatively small population makes it challenging for insurers to operate a profitable market, since a smaller population implies a smaller risk pool (i.e., there are fewer healthy and relatively lower cost people to help offset the higher costs incurred from those with greater healthcare needs). Second, the high chronic disease burden also implies higher healthcare costs. Third, fair market rules such as guaranteed issue, protections for those with pre-existing conditions, and no annual or lifetime limits, when applied to insurance markets, make insurance premiums more expensive. Because the USVI is not statutorily eligible for ACA subsidies designed to reduce the risk and cost of providing health insurance under these market rules, there is little incentive for insurers to enter the USVI market. Given the lack of an individual insurance market, we wanted to identify an insurance coverage option that could be administered through the USVI government.
Considering both funding limitations and the need for affordable insurance coverage for those who are currently uninsured or who do not have other opportunities to purchase insurance, we chose to focus on four key populations in the
USVI: residents who either 1) earn just above the Medicaid income limit, 2) are self-employed, 3) are employed but whose provider does not provide health insurance or 4) residents who will lose their current Medicaid coverage after the continuous coverage requirement expires at the end of the PHE. Our decision matrix provides further detail on each recommendation’s feasibility and likely impact.
Medicaid buy-in programs have attracted the attention of several state and city governments throughout the country as a way to expand health insurance options for those with limited to no insurance options. Medicaid’s per enrollee costs have grown more slowly compared to other payers, 29 which makes providing Medicaid and Medicaid-like coverage an appealing option to policymakers. In recent years, fourteen states have explored Medicaid buy-in programs as an alternative insurance option, mostly through commissioning studies or proposing legislation. 30 However, states often look into Medicaid buyin programs as a way to increase competition in their state marketplaces, which would lower premiums. While such Medicaid buy-in programs in the states are typically not eligible for federal match, the USVI may be able to establish a Medicaid buy-in program that is eligible for federal match given its lack of a marketplace.
For the USVI, a Medicaid buy-in program could provide many residents who currently lack health insurance the opportunity to pay a monthly premium for Medicaid-like insurance coverage. While Medicaid currently does not require premium
contributions or other out-of-pocket payments towards the health services used, a Medicaid buy-in program would require enrollees to make income-based premium contributions (i.e., pay a premium on a sliding scale). A Medicaid buyin program would provide Virgin Islanders who earn more than the Medicaid income limit an affordable health insurance coverage option and potentially improve health outcomes.
Since the USVI does not have an individual insurance market, it would encounter a different set of challenges when implementing a Medicaid buy-in program. The following sections outline financing and implementation recommendations for establishing a Medicaid buy-in program.
we recommend four next steps to design and implement a Medicaid buy-in program:
1. Identify the eligible population and determine the income eligibility threshold
2. Establish a premium structure and use the remaining Medicaid funds allotted to the USVI to subsidize premiums
3. Adjust the Alternative Benefit Plan for the Medicaid buy-in population
4. Design a marketing strategy to promote takeup of the Medicaid buy-in program
Identify the Eligible Population
The Medicaid buy-in program for the USVI should focus on the most economically vulnerable population not currently covered by an insurance program. In the USVI, this is the population that makes just above 133% of the USVI poverty level (USVIPL), the current income limit for the territory’s Medicaid program. Extending this eligibility up to 400% of the USVIPL would allow other uninsured Virgin Islanders to access health insurance, bring in patients who could potentially afford premiums, and diversify the risk pool.
An alternative approach is to focus on population groups with certain disease burdens, such as hypertension or diabetes. However, since this population would need to utilize the healthcare system more on average than other USVI residents, the cost of insuring them through Medicaid would make insurance premiums unaffordable without subsidies by the local government. Targeting the Medicaid buy-in program to the population within a defined range above the current Medicaid income limit would provide a more stable risk pool for the program and make premiums more affordable.
groups that are currently covered under medicaid based on income, asset, residency, and citizenship criteria:
• Pregnant women
• Children under age 21
• CHIP children under age 19
• TANF children and adults
• Blind and disabled
Note: Income standard for the categorically eligible for a family of one is $15,654. For Aged, Blind, or Disabled, for a family of one the standard income level is $20,833.
Expansion option 1 (Recommended)
Population with incomes between 133% – 400% (size dependent on cost) of the USVIPL
Expansion option 2
Population groups with disease burdens (e.g., hypertension or diabetes)
The first step to determining the optimal income eligibility threshold for the new Medicaid buy-in program would be to use claims data for the current eligible population to estimate a per-member per-month (PMPM) cost for the program. Claims data from the “expansion population,” or members whose incomes are between 100% and 133% of the USVIPL, would allow calculation of a PMPM that will be closer to the potential costs of the program for the population just above the current income limit. The USVI Medicaid Office should hire an actuary to do this analysis. This analysis should include sensitivities for the premium estimates based on available data on the disease burden and healthcare usage of the new Medicaid buy-in population. If the Medicaid buyin expansion population has a higher level of chronic disease, or if they are expected to utilize the healthcare system at a rate higher than other population groups, the estimated premiums might need to be higher to account for these larger expected costs of care.
Progress on this recommendation would require broad stakeholder support across the healthcare system for a new Medicaid buy-in program in the USVI. Implementing this recommendation would likely also incur additional administrative costs for the USVI Medicaid Office. Finally, estimating an accurate PMPM for the Medicaid buy-in population would depend on the depth of data available to the USVI Medicaid Office on healthcare usage and disease burden for this population, which may be a challenge given the lack of healthcare data currently available in the territory.
Establish a Premium Structure:
Once a PMPM rate for the new population has been estimated, the next step is to think through how a pricing structure would work for the program. Since the USVI government would not be able to fund a Medicaid buy-in program on its own, the sum of the premiums paid by Medicaid buy-in enrollees should cover the territory’s share of expected Medicaid costs for this new population. During our interviews, healthcare stakeholders in the USVI generally agreed that a premium between $50-200 per month would be an affordable range for the population earning between 133% and 400% of the USVIPL.
The premium could either be a flat rate for all enrollees in the new eligibility population or work as a sliding scale, in which lower-income enrollees pay a lower premium than enrollees with incomes closer to the top of the income range. A sliding scale may lead to unaffordable premiums for higher-income enrollees and reduce takeup of the program. However, without additional funding from the USVI government, a flat rate premium would likely not garner enough funds to cover the expected costs. Based on our conversations with stakeholders in the USVI, a sliding scale premium structure should be feasible for residents who earn between 133% and 400% of the USVIPL and who 1) do not have insurance options available to them through an employer, 2) are self-employed, or 3) will lose their Medicaid coverage once the PHE ends. Focusing on these populations would fill an existing gap in insurance coverage for USVI residents.
We recommend that the USVI hire an actuary to calculate the premium range after identifying the PMPM rate and estimated disease burden.
While premiums are necessary to fund a Medicaid buy-in program, relying on premiums alone would likely make costs too expensive for USVI residents. The USVI should rely on other funds to help subsidize premiums paid by residents. Through our conversations with USVI Medicaid staff, we learned that USVI’s Medicaid agency often does not utilize its entire allotted federal match (i.e., it does not spend enough local dollars on qualifying Medicaid expenditures to maximize the federal dollars the USVI could be getting from its 83% FMAP). For example, the USVI had around $40 million remaining in potential federal dollars available for Medicaid expenditures at one point during FY 2021. Since the USVI does not always use all of its potential Medicaid funding, it could potentially categorize Medicaid buy-in premiums as Medicaid spending eligible for federal match. For example, for every $100 spent by USVI residents on premiums for coverage through a Medicaid buy-in program, the USVI could be eligible for $488 in federal funding.
The USVI should engage with the Center for Medicare and Medicaid Services (CMS) to determine how premiums paid to a Medicaid buy-in program could potentially qualify for federal match. The USVI would likely need to either file a State Plan Amendment (SPA) or apply for a Section 1115 waiver, but should confirm a path forward with CMS.
Total federal match allotment (FY 2022): $131.4M
If the USVI spends $158.3M on Medicaid, they will get the full allotment in federal match. With a 83% FMAP, the USVI would be liable for $26.9M. $40M of the federal match allotment is unused per year, meaning the federal government is only reimbursing the USVI $91.4M. This means the USVI is currently spending $110.2M on Medicaid when it could be spending $158.3M to get the full match. There is $48.2M that could potentially be used to subsidize Medicaid buy-in premiums paid by residents. With the $40M match, $8.2M would be paid by residents via premiums. This scenario is illustrated in figure 6.
Identifying a suitable premium structure will rely on actuarial calculations based on several factors, including the PMPM rate, risk pool, disease burden, and demographics. This will also rely on having adequate data on the aforementioned variables to make such calculations. Additionally, getting Medicaid buy-in premiums to qualify for a federal match will depend on CMS and their proposed path forward. Given the additional administrative burden involved with handling premiums, managing new individual intake, and filling out paperwork like an 1115 waiver application, additional administrative costs could pose a challenge given current staffing levels in the USVI’s Medicaid Office.
For Medicaid enrollees who are between 100% and 133% of the USVIPL, the USVI uses an alternative benefit plan (ABP). The Federal Employee Health Benefits Blue Cross Blue Shield Service Benefit Plan serves as the base benchmark plan. 31 When creating a Medicaid buy-in program, the USVI could either offer this same ABP to buy-in enrollees or create a new set of benefits tailored to the new population. A decision on whether to maintain the current ABP or offer a new benefit package to the buy-in population will depend on the results of the actuarial analysis. If the PMPM rate estimate is expected to be too high to support affordable monthly premiums, the USVI Medicaid Office should determine which benefits are leading to the highest costs for the program. These high-cost benefits could be removed or pared back for the new buy-in population to drive down their PMPM rate.
Additionally, the optimal benefits package would be tailored to support the buy-in population’s
unique healthcare needs. More information about these needs can be ascertained through available health data on this population or through interviews with community and other healthcare system stakeholders. This new benefits package could remove or pare back benefits that are not needed for the new buy-in population, determined based on their prior healthcare usage, or it could add or bolster benefits that are prevalent among the new population. However, without local funding to support the buyin program, it is more likely that a new benefits package would need to be less generous than the current ABP so that monthly premiums are affordable for enrollees.
If possible, maintaining the current ABP for the Medicaid buy-in population would provide the simplest approach to setting up the program and will reduce administrative barriers to enrollment. A new benefits package for the buy-in population would require USVI Medicaid office staff and providers in the USVI to understand how it differs from the ABP offered to the current adult expansion population, and it may also create confusion and frustration for enrollees when benefits change for those who move in between programs due to changes in their income. A single ABP for the population with incomes above 100% of the USVIPL would eliminate these differences and reduce friction in the Medicaid enrollment process.
Progress on this recommendation depends on available administrative capacity to design an affordable benefits package that meets the needs of the buy-in population while also resulting in affordable monthly premiums. If a new benefit package is created, there may be costs involved with providing information to consumers and providers on the differences in benefits offered to the traditional Medicaid population, the adult expansion population, and the buy-in population. A new ABP that deviates from the benchmark Federal Employee Health Benefits Blue Cross Blue Shield Service Benefit Plan may also require a waiver from CMS to ensure the
coverage is appropriate for the target population, which could require additional staff hours and resources.
Design the Marketing Strategy:
To ensure that the population eligible for the Medicaid buy-in program actually enrolls, the USVI should design a marketing strategy to increase awareness of the program and the benefits of being insured. The marketing strategy should outline the positive benefits of enrolling in the program to the skeptical uninsured population. There may be healthy USVI residents who do not see any benefit to having health insurance. USVI Department of Health (DOH) staff should design a marketing strategy that educates this population about the importance of having insurance in case of a health emergency or other sudden change in health status, as well as the importance of having access to affordable preventive care options. Sub-Recommendation 2.1 in this report further details strategies the USVI DOH and Medicaid offices can use to increase awareness of the benefits of health insurance for USVI residents.
This marketing strategy does not need to be limited to the new buy-in population; it may be advantageous to market to those who may be eligible for either the traditional Medicaid program or its adult expansion. Increased enrollment of healthier individuals will reduce the USVI risk pool and lower costs for everyone else in the program, potentially making premiums more affordable for the buy-in population.
Implement the Marketing Strategy:
The first step to implementing a successful marketing strategy is to ensure monthly premiums
are affordable for the target population. Even those who are aware of the program and its benefits will not sign up if the costs of enrolling are too high. Second, policymakers should conduct outreach and partner with community stakeholders to increase awareness of the buyin program, how it works, and how those who are eligible can sign up. USVI government officials should also work with providers to ensure they are aware of how people can buy-in to the program. When uninsured patients who may be eligible for the program access the healthcare system, providers should be prepared to explain the program and direct patients to people or resources to help with the enrollment process, if necessary.
Progress on this recommendation depends on available funding for marketing and enrollment assistance. Policymakers could consider lower-cost marketing options, such as outreach to providers and community healthcare organizations, if funds are tight. However, if funding is available to support marketing, traditional outreach methods such as radio, web, and print advertisements may also prove successful in reaching a larger population.
While a Medicaid buy-in program would fill a persistent gap in insurance coverage for thousands of Virgin Islanders, it would not come without financial and implementation challenges. Funding a Medicaid buy-in program through premiums alone would likely make premiums too expensive for Virgin Islanders. Given the budgetary constraints of the USVI government, it is also unlikely the territorial government would be able to allocate additional funds to a separate buy-in program. This makes obtaining a federal match on premiums paid to a buy-in program critical to success. This process relies on CMS approving a SPA or 1115 waiver, which comes with administrative challenges such as undergoing negotiation processes that can take months
or even years and working with contractors to evaluate (an 1115 waiver’s) outcomes.
The Medicaid buy-in program’s success is also contingent on enrollment levels and service utilization. If too few people enroll in the program or if there aren’t enough healthy people enrolled to balance out the risk from unhealthy people, then the risk may be too high. Low utilization of health services such as preventive care can also drive up overall healthcare costs. Strategies to address these challenges are discussed in Recommendation 2 .
Additionally, success of a Medicaid buy-in program could be hindered by issues related to provider participation in the program or provider capacity. However, the USVI already reimburses Medicaid costs at Medicare rates, so this should mitigate the risk that providers choose not to provide services to enrollees of the buyin program. Despite parity in reimbursement rates, provider shortages still persist in the USVI.
Strategies to address the provider shortage are detailed in Recommendation 3.
Care coordination between the government agencies and departments responsible for providing healthcare to USVI citizens will also be crucial to successful implementation of a Medicaid buy-in program. Strategies on how to improve care coordination are outlined in Recommendation 4 . Finally, collection, analysis, and coordination of territory-level updated population health data is needed to operate and maintain a Medicaid buy-in program. Strategies on how to collect and use such data are detailed in Recommendation 5.
If these administrative capacity and process challenges are addressed, a Medicaid buy-in program could provide thousands of Virgin Islanders with affordable quality health insurance that is currently non-existent due to the lack of an individual insurance market.


During our interviews, multiple stakeholders reported low health literacy as a barrier to preventive healthcare utilization in the USVI. Preventive care refers to any routine healthcare service aimed at preventing illnesses, disease, and other health problems, and includes screenings, checkups, and patient counseling. 32 Preventive care is critical to both maintaining a healthy population and avoiding medical costs associated with treating preventable disease.
Increasing USVI residents’ understanding and utilization of preventive care services would thus be critical to controlling health spending under a Medicaid buy-in program. Initial health costs could be particularly high as the risk pool expands to include residents who may previously have lacked access to preventive care services. Additionally, improving health literacy could improve the success of a Medicaid buy-in program by ensuring residents who qualify for the program have a clear understanding of how the program will improve their lives. This understanding would be key to promoting enrollment in the program.
This section outlines preventive care access in the USVI and shares key stakeholder takeaways about the barriers to accessing them. It then provides recommended strategies for increasing knowledge and uptake of healthcare services.
1. Promote the importance of preventive care through individual patient interactions and broader community outreach
2. Educate residents about the benefits of health insurance
The DOH has demonstrated its commitment to strengthening community health. We learned through our interviews about recent investments to build a new public health center that will focus on preventive care, behavioral health, and community education. The center will also include an onsite lab for testing and screening.
These investments will be critical in the USVI, where preventive service provision indicators lag behind national figures. For example:33
• Prenatal care: In 2017, 16.6% of births in the USVI had no prior prenatal care, as compared to 6% of births nationally. 34
• Routine screening: In 2016, 49.9% of USVI adults aged 50-75 reported having a colonoscopy in the last 10 years, compared with 63.3% nationwide. Additionally, 72.7% of adult women aged 50-74 in the USVI had received a mammogram in the past 2 years, compared with 77.5% of women in the same age group nationally.
• Child vaccination: Children in the USVI had the lowest rate of measles, mumps, and rubella (MMR) vaccination in the United States in
2017, at 70.5%. The national MMR vaccination rate for children in the same year was 90.8%. 35 Stakeholders reported lack of care-seeking behavior as a major challenge underlying low preventive care access. This was particularly believed to be a challenge among uninsured residents, who are perceived to seek primary care at lower rates than residents with Medicaid or employer insurance. However, preventive care-seeking is reported to be low among the insured as well. In our interviews, we heard that many people covered by the territorial government’s health insurance plan do not seek annual check-ups and mammograms despite these services being free as guaranteed by the ACA.
One underlying theme driving low preventive care-seeking behavior highlighted during our interviews is that many residents are unfamiliar with basic health insurance concepts and are unfamiliar with the benefits that health insurance provides. This is a problem of low health literacy, which is defined as the ability to navigate the healthcare system and make informed decisions regarding one’s own care. 36 Low health literacy is very common: half of Americans report that they do not understand basic health insurance terms and are not confident using health insurance to access care. 37 Low health literacy can lead to underutilization of preventive care, such as in cases where people may not understand what services are exempt from copays on their plan. 38 Accordingly, low health literacy is consistently linked to worse medical outcomes. 39
Increasing the health literacy of residents will help Virgin Islanders understand whether the Medicaid buy-in program is a good option for them, be more confident that they will be able to afford the care they need, and feel more empowered in their own care. Improving health literacy can increase both enrollment in the Medicaid buy-in program as well as utilization of services, which can help broaden the program’s risk pool and improve health outcomes.
Stakeholders also reported that cultural norms and misconceptions may also reduce care-seeking
behavior. Private doctors are viewed as the preferred health providers, and some view services from clinics as lesser quality and feel reluctant to use them. Residents may be further discouraged from using public health facilities if they are unable to pay, preferring to forego care out of pride. A desire to maintain privacy may also discourage care-seeking. People may worry about insurance providers accessing their personal health information following doctors visits.
In our interviews, we heard that these factors can delay care seeking behavior until issues become acute, and that this is especially common for patients without health insurance.
It is important to note that these barriers are not unique to the Virgin Islands. Underutilization of preventive care is widespread across the United States. Underutilization of preventive care also increases with higher unemployment, 40 and the USVI’s unemployment rate is usually higher than the 50 states. Utilization of preventive care is also closely associated with health insurance coverage, 41 and expanding access to health insurance is associated with significant increases in preventive care utilization. 42
Values and cultural ideas of health, gender, pride, and other factors can lead patients to delay preventive care or not seek it out at all. However, focusing too much on patients’ personal responsibility for neglecting their care can stigmatize patients and make them less likely to seek care.
In our conversations, we heard that Virgin Islanders will use traditional medicine and home remedies when they are sick. 43 Herbal medicine and prayer are common healing practices among Black Caribbeans. 44 We see this as evidence that Virgin Islanders do value preventive care, but that this care is currently not happening within the formal medical system.
Finally, even when people decide to seek primary care services in the formal medical system, they often face long wait times. SRMC Hospital reported that discharged patients may wait up to five weeks to have their first follow-up appointment. Both hospitals in the USVI reported that
primary care often ends up being delivered in the ER, which drives up ER wait times. Perception of long wait times can then further discourage care-seeking behavior.
In our interviews, we heard that there is currently insufficient public communication around the importance of and options for preventive healthcare. Focusing on health promotion and education efforts can help improve health literacy and increase utilization of preventive care within the territory.
Providers can serve as key educators in health literacy and use patient interactions to promote the importance of preventive care. Providers should understand that low health literacy is a risk factor for adverse outcomes, and should understand themselves as having a responsibility to explain concepts clearly, educate without judgment, and confirm understanding of important concepts, like the importance of preventive care.
To build on existing beliefs in the value of preventive care services, while moving those care-seeking behaviors into the medical system, we recommend encouraging healthcare providers to validate traditional medicine and home remedies rather than dismissing them, as long as they are not actively harmful. Providers could work with patients to understand evidence-based healthcare as being complementary to medicines they may be more comfortable and familiar with. Providers should respectfully listen and seek to understand patients’ use of alternative and complementary medicines to build trust and
facilitate information sharing within the provider-patient relationship. 45 Providers can also integrate alternative and complementary medicines into treatment, such as by identifying traditional foods and medicines that are compatible with a treatment plan for diabetes. 46
Additionally, public health leaders could consider using co-design to integrate patients into the process of creating and updating educational materials. Letting patients share their perspectives and recommendations for phrasing information in plain and accessible language produces more useful materials and increases the health literacy of participants, so they can be health literacy ambassadors in their own communities. 47 To the extent feasible, providing child care and compensation to participants could ensure a broad range of patients have the opportunity to participate in such a co-design process.
Finally, the USVI should expand outreach services to meet people where they are rather than requiring them to come to a healthcare center. Such outreach could include mobile service centers, partnerships with trusted community centers such as libraries, 48 or duplicating existing models such as the successful territorial partnership with the Diabetes Center of Excellence. 49
Implementing culturally-competent behavior-change programs will require significant resource investments, including both staffing, financing, and time. Clinical providers in the USVI already face high patient loads and may not have bandwidth for the additional work to design and implement new comprehensive community education programs. This recommendation would be more feasible if the USVI also further invested in strengthening a community health workforce. A robust cadre of community health workers would be best equipped for the type of community- and personal-level outreach required to successfully educate USVI residents on preventive care strategies.
USVI stakeholders reported a lack of general patient understanding around the benefits of and processes for enrolling in Medicaid. After qualifying for presumptive Medicaid eligibility, patients remain temporarily enrolled through the end of the following month. However, not all patients follow up to enroll in the program on a full and ongoing basis. Since patients cannot receive presumptive eligibility twice in the same year, they must be treated as uninsured if they seek care again within the same year without having converted to full eligibility. Because of the statutory requirement that no patient be denied service because of ability to pay, a patient’s insurance status will not affect their ability to receive care. This can further lead to a lack of urgency in enrolling in Medicaid for those eligible.
For many residents, a Medicaid buy-in program would be their first opportunity to have affordable health insurance in their adult lives. Health insurance is complicated, with its own language of copays, deductibles, in-network and out-ofnetwork, and other concepts that do not come intuitively to the average person. After enactment of the ACA, CMS created the Coverage to Care initiative to address this challenge by providing information to new enrollees on how to use their coverage and access primary and preventive care services.
The USVI Medicaid Office should use the CMS Toolkit for Making Written Material Clear and Effective to design fact sheets, handouts, and other written materials for potential Medicaid buy-in enrollees. 50 Because materials designed for patients familiar with basic health insurance concepts may not resonate with audiences who have never held health insurance, materials should define technical terms in plain language, break complex information down into manageable pieces, and use graphics when appropriate. 51
Concepts should be explained using analogies to more familiar terms: for example, a health insurance deductible is like an auto insurance deductible and a provider referral is like a job search referral. 52
To design education and outreach materials, the USVI Medicaid Office should work with community members and representatives to design materials that are accessible and culturally competent. This could follow the model of Insure Detroit , a partnership between researchers and community-based organizations during ACA implementation that worked with local focus groups to design a website and educational videos using storytelling techniques to promote health insurance literacy. 53
Materials and providers should also communicate how patient privacy is respected within the medical setting. We heard that in a small community, some people avoid care because they worry that their provider will share their personal information with other members of the community. This is an opportunity to invest in health literacy regarding patient privacy protections to remove a barrier to seeking care.
On the provider side, the USVI DOH should encourage healthcare providers to complete the health literate healthcare organization 10 item questionnaire. 54 This self-assessment allows providers to assess where they can better serve patients by integrating health literacy education into every aspect of their operations. The DOH should also encourage healthcare providers to establish or strengthen patient advisory boards to integrate patient perspectives and identify areas where providers can serve as key communicators. Finally, the DOH should host professional development trainings, eligible for continuing medical education (CME) credits, on educating medical providers on best practices for communicating information clearly and checking for comprehension.
The breadth of existing educational materials from other health literacy programs mean that
the USVI would not have to create new provider training curricula and community outreach materials. However, adapting these toolkits and documents would require resources for both language and cultural context translation and dissemination.

Additionally, overburdened health providers may not be able to attend professional development trainings. To mitigate this, patient communication best practices around health insurance could be incorporated into existing in-service and pre-service training modules. Offering self-guided curricula, such as the health literate healthcare organization 10 item questionnaire, can also facilitate providers’ ability to develop their communications skills at their own convenience.
Behavioral solutions to encourage people to seek preventive care can help change existing attitudes and habits related to preventive care and demonstrate the benefits of seeking more formalized preventive care. However, given the constraints and provider shortages that the USVI medical system is currently facing, behavioral change can only go so far. People cannot seek out preventive care if there are not enough healthcare professionals to supply it. While we believe
these solutions can help increase access and utilization, underutilization can also be a response to real lack of providers. These recommendations will become more feasible paired with strategies to address health workforce shortages. While effective evidence-based strategies to improve health literacy and patient outcomes are well-documented, health literacy is not useful if people cannot access healthcare. Even with a Medicaid buy-in program, many residents will still face barriers to care. The costs of care may remain high, the provider shortage may continue, and navigating the system may continue to be complicated. Accordingly, the effects of improving health literacy are limited by the ability of patients to use their new health literacy to actually access care. Further, any uninsured residents who cannot afford to buy into Medicaid will continue to face cost and access barriers even as health literacy improves.
Finally, we have provided a number of recommendations that focus on incorporating both community voices and traditional practices into health literacy efforts. Soliciting this input from a diverse array of community voices, rather than those who are frequently consulted, may require additional time and resources in order to achieve full community representation and buy-in.
During our conversations in the USVI, we heard from a variety of stakeholders that provider shortages posed a challenge to the healthcare system. As the USVI considers expanding Medicaid services to cover more people through a Medicaid buy-in program, the lack of availability of Medicaid providers could impact the success of the program. Increased demand could lengthen wait times for services, and diminish enthusiasm and desire to participate in a Medicaid buy-in program.
Implementing strategies to reduce provider shortages and maximize the efficiency of existing healthcare structures will strengthen the healthcare system as a whole, increase patient satisfaction for those who buy-in to the expanded Medicaid program, and reinforce the sustainability of the Medicaid buy-in program. As USVI healthcare stakeholders consider implementing a Medicaid buy-in program, we provide options for increasing access to providers within the program.
Strategies to address provider shortages:
1. Partner with the future UVI Medical School
2. Adopt medical compacts to facilitate provider licensing
3. Increase telehealth utilization
4. Leverage health workforce development funds to increase provider supply
5. Improve care coordination
Provider shortages are a national issue that has been exacerbated by the COVID-19 pandemic,
with rising patient demand while healthcare providers are leaving the industry in record numbers. The USVI is no exception to this challenge. The HRSA Bureau of Health Workforce designates HPSAs based on regions where the population-to-provider ratio demonstrates limited healthcare accessibility. As of September 30, 2022, the population of the designated HPSAs in the USVI was 207,477 for primary care, 207,238 for dental care, and 154,841 for mental healthcare. 55 Stakeholder interviews in the USVI confirmed the challenges of a provider shortage from a government, provider, and community perspective.
The USVI is pursuing a number of avenues to increase access and reduce health workforce barriers to the provision of care. In July 2022, the administration of Governor Albert Bryan Jr., approved $20 million to bolster USVI hospitals given staffing challenges. SRMC on St. Thomas and Juan F. Luis Hospital on St. Croix each received $10 million in American Rescue Plan Act funding to support recruitment and retention efforts. Governor Bryan, Jr. referred to this effort as, “The beginning of the giving to create an environment where we can attract medical professionals that can help treat us and give people the healthcare they deserve.” We heard from health system leaders and read accounts that this funding has helped address pressing workforce challenges. 56
Health leaders in the territory also mentioned that low Medicaid reimbursement rates and high administrative burden might have dissuaded providers from enrolling in Medicaid in the past. Recent changes by the Department of Human Services (DHS) to allow Medicaid authorization without referral have motivated providers to
enroll in Medicaid or continue seeing Medicaid patients.
Providers in the USVI are exceptional in their ability to play a wide variety of supportive service roles, in addition to their clinical duties, in order to meet the needs of their patients. However, the more responsibilities per patient assumed by a provider, the fewer patients they can see. A strong social service network – including municipal, nonprofit, religious and community-based organizations – is thus vital in every health system. Social support services help promote the overall well-being of a patient while addressing social determinants of health to achieve more equitable health outcomes.
Ensuring timely access to care is vital to the success of a Medicaid buy-in program, as increasing insurance coverage could lead to increased demand for health services. As a result, longer waiting periods to see a Medicaid provider could dissuade people from remaining enrolled in the Medicaid buy-in program. Individuals would be less inclined to pay for insurance if access fails to meet demand, or if there is a perception that making an appointment as a Medicaid member might be challenging. The following strategies aim to offset that increase in demand.
The University of the Virgin Islands (UVI) is in the process of building a new medical school, which holds great potential to increase the number of physicians in the USVI by educating a new generation of doctors. The UVI medical school intends to focus on recruiting and retaining those with roots in the USVI by reserving seats for residents. This focus will have long-term benefits for combating provider shortages and ensuring a robust primary care physician workforce in the future.
Medical professionals throughout St. Thomas and St. Croix will assist with clinical instruction
as preceptors for UVI students. The university also plans to offer away-rotations for students at other medical schools, presenting an additional opportunity for recruiting future physicians to the USVI. Creating a scholarship for those committed to practicing in the USVI after graduation, or maximizing participation in NHSC scholarship and loan repayment programs (described in more detail in section 3.4) could similarly support provider recruitment.
During medical training, UVI could send medical students for clinical rotations at Federally Qualified Health Centers (FQHCs) and community health clinics. This would expose students to the benefits and challenges of working with underserved populations and may foster future career interests in these areas. In addition, UVI could consider the creation of an “Islands Track’’ as a specialty training track within its school of medicine, modeled after special-interest tracks at other US medical schools. Such a program would serve to identify, admit, and educate students about healthcare issues specific to the USVI, with the goal of increasing the number of students who return after the completion of their training. Specialty tracks provide motivated students with additional didactic and clinical training opportunities through special lectures, tailored clinical experiences, and mentorship programs.
Apart from efforts to recruit and retain student doctors, the medical school holds promise for energizing the region economically through the establishment of an academic research hub, a state of the art simulation lab, and other new infrastructure. The Economic Development Administration of the Department of Commerce awarded a $14.1M grant to the Medical School Simulation Center, located on the Albert A. Sheen campus on St. Croix. 57 The agency also awarded an $18.6M grant to the Medical Research and Training Lab on St. Thomas. 58
The UVI School of Medicine is currently in the process of accreditation with the Liaison Committee on Medical Education (LCME) and is preparing to
move to the next step in the accreditation process in 2023. The potential benefits of the UVI School of Medicine cannot be harnessed until accreditation is complete. Additionally, the creation of a specific track program within a medical school will cost money to design, implement, and operate. Most rural track programs in U.S. medical schools are funded by grants and have great variability in funding and administration. The UVI School of Medicine will be limited by these same constraints when evaluating the addition of special-interest programming to their curriculum.
Another strategy to increase the number of medical providers in the USVI is through the use of medical compacts. Medical compacts aim to ease the barriers associated with entering into medical practice by expediting the licensing process and decreasing administrative burdens for applicants. The overarching goal of these compacts is to encourage licensure with aim of increasing access to both in-person and telehealth services.
The Bryan-Roach administration has already identified medical compacts as an avenue for increasing access to healthcare in the USVI. In December of 2021, Governor Bryan signed Bill 34-0040 into law, which enabled the USVI to participate in the Nurse Licensure Compact. 59 Through the Healthier Horizons initiative, the Governor’s Office is also exploring additional interstate licensing compacts for several in-demand medical professions, including physical therapy, psychology, and emergency medical services. With the increased use of telehealth, these compacts may be particularly useful for increasing access to care, as the provision of telehealth varies by state and inter-state practice is not always permitted.
The Interstate Medical Licensure Compact (IMLC)
is another licensing agreement that has potential to ease physician licensure burdens in the USVI by streamlining and expediting the licensure process. This compact does not change a state or territory’s existing Medical Practice Act or impede its ability to regulate the practice of medicine, but allows for faster licensing for physicians already licensed in another state. Thirty-seven states, Washington D.C., and Guam already participate in this compact.60 In order to join the IMLC and other compacts, the USVI legislature would need to introduce and enact a bill authorizing the territory to join, with language that is consistent with other states that have already joined.
The Governor’s office has already laid the groundwork for participation in several medical compacts. With minimal costs and negligible work required to draft the legislation, the main obstacle will be ensuring broad support to pass it.
Telehealth utilization increased dramatically during the COVID-19 pandemic and will likely be a permanent fixture of the healthcare landscape in the U.S. In 2021 alone, telehealth usage increased 38x compared to the pre-COVID-19 baseline.61 Increasing telehealth utilization in the USVI would not only help providers more appropriately triage care by directing patients who would normally go to urgent care or the emergency room for non-emergency cases to primary care, but would expand care access to Virgin Islanders who cannot easily travel to seek the care they need. It would also ease the care burden exacerbated by the provider shortage and lack of many types of services, including many forms of specialty care. Other benefits of telehealth include better continuity of care, decreased care costs, and improved quality of care.62
The USVI has already taken meaningful steps to increase telehealth utilization in the USVI, including identifying telehealth as one of the eleven initiatives specified in Governor Bryan’s “Healthier Horizons” healthcare reform agenda.63
The Virgin Islands Telehealth Working Group, established in January 2020, drafted the Virgin Islands Telehealth Act (“VI Telehealth Act”), which was submitted as a proposed bill to the Legislature of the Virgin Islands in June 2022.64 The VI Telehealth Act as proposed would establish insurance reimbursement parity for telehealth visits and increase both the number and types of providers available to Virgin Islanders if the telehealth provider registers with the Department of Health. The VI Telehealth Act would also work with the Nurse Licensure Compact signed into law by Governor Bryan in December 2021, which allows registered nurses and licensed practical/vocational nurses to have one multistate license and provide care both in-person and via telehealth. These provisions would directly address the provider shortage by incentivizing providers to see more patients via telehealth and expanding the types of providers available to Virgin Islanders.
Codifying the VI Telehealth Act could help the USVI lay a foundation of key policies and processes needed to effectively integrate telehealth into the USVI’s healthcare landscape. Establishing payment parity for telehealth visits for insurance reimbursement purposes and expanding the type and number of providers allowed to provide care to Virgin Islanders who currently cannot access the care they need will likely provide some much-needed relief to the USVI’s current provider shortage. Joining medical compacts like the IMLC and other profession-specific medical compacts would also increase the number of providers available to Virgin Islanders and reduce the administrative burden typically involved with allowing providers outside the USVI to provide care to Virgin Islanders via telehealth. All of these proposed flexibilities could attract more providers to the USVI.
Strong political support of telehealth from Governor Bryan and Legislators increases the likelihood of the passage of the VI Telehealth Act. However, the resources required to ensure providers have the technology needed to successfully conduct telehealth visits may be a limiting factor. The USVI’s 2021-2024 Health IT Strategic Plan clearly lays out a vision of how to empower patients and providers to use telehealth, but the implementation of such technology will require significant investment from the USVI government or other entities (e.g., ensuring providers have adequate telehealth technology and internet access).65 Current investments into improving the USVI’s broadband infrastructure include approximately $85 million 66 from the Federal Communications Commission to build out high quality fixed and mobile networks by 2027 and at least $25 million 67 from the National Telecommunications and Information Administration’s Broadband Equity, Access, and Deployment Program (BEAD), which funds planning, infrastructure development, and adoption programs. These resources could help the USVI ensure providers and other stakeholders are equipped with the proper technology they need to successfully utilize telehealth.
The USVI can facilitate the long-term stability of the healthcare workforce by leveraging several existing programs and structures. These include maximizing participation in federal programs designed to recruit providers to healthcare shortage areas, creating healthcare career pipeline programs for young Virgin Islanders, and utilizing the skills of Advanced Practice Providers (APPs) as part of the healthcare team. HRSA offers scholarship and loan repayment services that could
be utilized by providers looking to practice in the USVI.
The National Health Service Corps (NHSC) has several programs that aim to alleviate provider shortages through the use of scholarships and loan repayment in exchange for a commitment to practice in a designated HPSA for several years. Applicable programs for providers in the USVI include:
• NHSC Scholarship Program: awards scholarships to students pursuing eligible primary care health professions training in exchange for a commitment to provide primary care in a HPSA.
• NHSC Loan Repayment Program: open to licensed primary care medical, dental, and mental health providers who are employed or seeking employment at approved sites.
• Nurse Corps Scholarship Program: Scholarship program for nursing students in exchange for a two-year commitment at an eligible healthcare facility.
• Nurse Corps Loan Repayment Program: Open to RNs and APRNs, supplies 60% of total outstanding loan balance in exchange for a two year service commitment in a Critical Shortage Facility (CSF).
The Nurse Corps Loan Repayment Program pays up to 85% of unpaid debt for registered nurses (RNs), advanced practice registered nurses (APRNs), and nurse faculty (NF) in exchange for working in either an eligible nursing school, or a CSF.68
The HRSA also administers the Health Careers Opportunity Program (HCOP), which centers around eligible academic medical institutions and could be pertinent to the UVI School of Nursing, and in the future, the UVI School of Medicine. The program offers funding to high schools or professional degree programs with activities designed to support students who seek to enter into a primary care setting in a rural and/or medically underserved area. If utilized in USVI high schools whose students aim to matriculate into
medical programs, these funds could expand the reach and efficacy of health workforce pipeline efforts.69
In addition to focused programs such as those offered through the HRSA, general pipeline programs provide opportunities for mentorship, education, and exposure to a variety of healthcare careers for primary, secondary, and higher education students. These programs encourage young people from underrepresented backgrounds to pursue careers in medicine and public health. In 2019 Governor Bryan introduced a USVI Talent Pipeline Workforce Development Initiative targeting an array of industries, including health sciences. This initiative has objectives at every stage of learning, and relies on employer partners to inform, attract, acquaint, train, and hire candidates.70 ,71
Lastly, scope of practice laws are created by state or territory governments to regulate the type of services that health professionals can perform. Advance Practice Providers like Nurse Practitioners (NPs) and Physician Assistants/Associates (PAs) have the training to conduct many of the services traditionally performed by physicians, and utilizing APPs can help to increase access to care and reduce costs. In the USVI, PAs and NPs can already prescribe medications and practice with a written agreement from a collaborating physician. This team-based model can be leveraged to maximize efficiency, allowing the physician to see more complex cases. Ensuring that territory law and practice agreements in the USVI allow PAs and NPs to practice at the full extent of their training and education represents another strategy for combating the provider shortage in the USVI.
Investing time, energy, and funding into expanding a healthcare career pipeline in the USVI is a long-term strategy with minimal payoff at the outset. Likewise, administrative challenges can deter access to federal funds for workforce development. Qualifying as an eligible CSF or HPSA provider can take time and negotiation, and then
attracting talent to utilize NHSC or Nurse Corps funds within an eligible entity is the next step. For students or new providers being supported by HRSA funding, the application process can also be challenging and a bit daunting, with reimbursements prone to delay. USVI providers might consider offering support to future employees navigating this process or pooling their resources to create a local point of contact for facilitation of this process. Additionally, all of these resources should be paired with sufficient marketing to ensure the broader community is aware of these opportunities. Though it can take time to establish these opportunities, the goal of these programs is to support provider shortage areas, and health systems in the USVI would be ideal beneficiaries.
Improving care coordination among providers and public health entities can improve efficiency and health outcomes on both population and patient health levels. On a population health level, care coordination can help close system gaps, assess utilization and access, and evaluate opportunities for reducing waste. On a patient level, care coordination provides wrap-around services that address the physical, social, emotional, and cultural wellbeing of a patient, while streamlining the patient experience, improving patient satisfaction, and promoting understanding of the care plan through open communication between patient and provider. Few, if any, jurisdictions operate a fully functioning and comprehensive care coordination system. However, the USVI could lead innovation of such a system by making the following investments.
Technology in the form of interoperable electronic health records, insurance verification systems, and health information exchanges (see Recommendation 5.3), can be helpful in tracking patients and service provision and viewing larger
population health trends as they unfold. The USVI has made progress in all of these areas and showcased this progress at a 2019 Virgin Islands Health Innovation Summit.72 , 73 , 74 Continuing to pursue electronic medical record systems and medical data exchanges will improve both the effectiveness and efficiency of care coordination.
In our interviews, USVI healthcare leaders shared the challenges they faced with continuity of care as it pertained to access points for patients and tracking medical history. Patient navigators can help close these gaps by guiding patients through care and educating them about healthcare access points.I Successful patient navigator programs have included stationing navigators in facility waiting rooms to answer questions, engaging patients in post-clinical-consultation discussions before check-out, and using navigators to check in via text message or phone calls with patients between visits.II For any patient, even those with high levels of healthcare fluency, navigating access points, negotiating insurance coverage, understanding medical guidance, or recalling past services or diagnoses can be arduous. An electronic medical records system paired with trusted patient navigators can help to strengthen patient care.
Patient privacy was a recurring theme in our interviews with USVI healthcare leaders, including patient concerns about health information disclosure and potential stigmatization associated with being seen visiting health facilities. Public information campaigns could normalize accessing health services and reduce stigma. Additional privacy measures include segmented waiting rooms, noise-canceling machines to conceal conversations, and widely advertised patient privacy disclosures and consent for information
I This role goes by many names which may include: “outreach worker,” “caseworker,” “patient advocate,” or more generally, “community health worker.” “Patient navigator” can also be used in some contexts to refer to individuals who enroll patients into ACA health benefit plans .
II With the need for a private corner where conversations cannot be overheard.
sharing restrictions. Any strategy that would make patients more likely to follow-up with their doctors and remain vigilant in their preventive care routines, would assist in care coordination. Care coordination can also exist outside formal medical settings to address social and structural determinants of health. Traditional and alternative healing approaches and community support systems can also support the psychosocial wellbeing of individuals. FQHCs have a history of incorporating holistic care as organizations whose practices remain largely rooted in recognizing the marginalization of the underserved communities by whom they were founded.75 , 76 Strategy 2.1 focuses on encouraging healthcare providers to validate traditional and home remedies and would also support improved care coordination.
As demonstrated by the strong social connections of communities in the USVI, foundational elements of care coordination are already present: people have strong social networks and share information with one another. While technology can be a powerful tool, people are the greatest resource in care coordination as community health workers and patient navigators inform and guide patients through important healthcare decisions.
The USVI faces unique challenges with care coordination and patient engagement due to its
geography. Patients being transferred off-island for medical care – whether by choice or necessity – perpetuates care discontinuity, poor patient retention, negative perceptions of USVI healthcare, and high healthcare spending. By diversifying strategies to engage patient populations and increasing the supply of providers and efficiency of pre-existing resources, the USVI can improve the sustainability of the healthcare system.
An increased focus on improving care coordination via technology, staff resources, workflows, and communication and understanding will reinforce the USVI healthcare system despite the effects of provider shortages.

There are a number of challenges to addressing provider shortages, which include pipeline delays, care coordination interruptions, and technological limitations. The USVI is not alone in struggling to match patient demand with provider supply – the US as a whole faces a projected shortage of between 54,100 and 139,000 physicians by 2033.77 Provider shortages can be instigated by unpredictable elements, such as the rate of provider retirements or changes in provider participation in insurance options. This critical problem has the potential to become increasingly relevant if more people in the USVI gain insurance coverage and try to access care with greater frequency.
Responsibility for healthcare policy, as well as the provision of healthcare programs and services to residents, is spread across several government agencies and departments in the USVI. As the USVI works to implement a Medicaid buy-in program, it is necessary for the government to coordinate its programs, consolidate entry points to care in the territory, and develop a robust and coherent cross-departmental healthcare plan. Improving coordination will make it easier for Virgin Islanders to understand their insurance options and apply for the buy-in program, if eligible. A territory-wide healthcare strategy will also help to improve access to care and ensure that agency efforts do not conflict with current policy or a proposal being developed in another department.
This section outlines the current landscape of healthcare policy and programs across the USI government and addresses barriers to cross-department collaboration. It then provides recommendations for improving healthcare coordination across the USVI government.
Strategies to strengthen coordination between USVI agencies and departments:
1. Create a new Healthcare Cabinet, a cross-agency task force that meets regularly to discuss healthcare policy, programs, and insurance.
2. Develop a centralized government healthcare website for USVI residents to reference consolidated access points to care and information on government and community healthcare resources.
Healthcare policy and programs are spread across several different government agencies in the territory. The USVI DHS is responsible for managing the territory’s Medicaid and CHIP programs, while DOH operates a community health program throughout the territory and, as the territorial public health agency, conducts programs in preventive medicine, family planning, behavioral health, and drug and substance abuse prevention. The USVI Health Insurance Board of Trustees, operated under the Division of Personnel, oversees health insurance for government employees. Finally, the Division of Banking, Insurance, and Financial Regulation, under the purview of the Office of the Lieutenant Governor, is the regulatory agency for private health insurance coverage.
The work of healthcare policy development and strategic planning is also spread across departments in the USVI. The Governor’s Office has put forth its “Healthier Horizons” Initiative, a healthcare reform effort with eleven recommendations to improve and upgrade healthcare in the territory.78 Additionally, DOH is operating under a five-year strategic plan with its own set of priorities for improving healthcare.79 One of the goals of the “Healthier Horizons” initiative was to create a territorial health plan by the end of 2020. With access to healthcare services, insurance options, and policy planning spread across different agencies in the USVI, it is crucial that all government offices work together to coordinate policy development and inform each other of potential program changes that might have cross-department impact.
Stakeholders in the USVI mentioned that this lack of an integrated healthcare system in government created artificial barriers to care. Without a coordinated effort to inform residents of where and how to access care, many people in the territory are unaware of where to go for different types of services. This leads to an inefficient use of the healthcare system, such as a resident going to the emergency room for a chronic non-acute condition, instead of their primary care provider. These inefficiencies then drive up costs across the healthcare system for the government, providers, and patients.

Stakeholders also reported that while each agency successfully operates its own programs and acts as leaders in their respective healthcare areas, agencies need to do a better job communicating about changes in programs and policy
that could affect other government-provided services. For example, as DHS works to implement a Medicaid buy-in program in the territory, the Health Insurance Board of Trustees and the Division of Banking, Insurance, and Financial Regulation should be kept apprised of any changes made to the buy-in program by DHS so that both agencies are ready for any impacts it may have on the private insurance market or on government employee healthcare plans.
The USVI government should look to create a cross-agency Healthcare Cabinet, with representatives from each agency responsible for healthcare programs and services, to improve coordination and efficiency across departments. This task force would meet regularly to keep each other apprised of new healthcare plans and policies being undertaken, ensure that efforts are not duplicative, and work together to push a centralized healthcare strategy for the territory. This task force should include representatives from DHS, DOH, the Division of Banking, Insurance, and Financial Regulation, and the Health Insurance Board of Trustees. Coordination of the task force should be undertaken by the Governor’s Office, who would set meeting dates and put together meeting agendas, with input from each agency representative.
Connecticut has successfully deployed this model to inform the Governor on issues related to federal health reform implementation. The Connecticut Healthcare Cabinet also has the power to convene working groups, which include non-governmental healthcare experts and stakeholders, to make recommendations on a series of service delivery and program reform issues. 80 Additionally, many states have created multi-agency Governor’s Children’s Cabinets as a way to improve coordination of services to children across government. 81 The USVI Healthcare Cabinet should also consider regularly bringing in community stakeholders, such as private providers, representatives from FQHCs, or health experts from the University of the Virgin Islands, to provide input on the work of the task force.
Progress on this recommendation could be made with little to no funding required. However, it would require additional work from Governor’s Office staff to coordinate the meetings of the Healthcare Cabinet, create agendas, and report out the work of the task force. It will also require a time investment from each agency represented on the task force, as they should ensure they send informed decision-makers who can speak in detail about the policy and program work at their agency, to represent them at meetings.
With responsibility for health program provision spread across multiple agencies in the USVI, information on public health and healthcare programs offered by the government are likewise spread across different agency websites. This multitude of access points can make it difficult for people to find the information they need and to understand what programs are available to them. The USVI government should look to create a centralized healthcare website that includes information on government health programs, insurance options, and links to community health resources. For example, Colorado has created a centralized health information website alongside its state-based marketplace, accessible at www.colorado.gov/health. In addition to outlining insurance options for Colorado residents, the
site includes a “Health and Wellness Resources” section that consolidates links to government and community programs for behavioral health, chronic disease, pregnancy and women’s health, and immunization. 82 Colorado’s website also includes a “FAQs” section as well as a “Health Glossary,” which both work to advance the provision of healthcare information to residents and help them understand their care and insurance options.
The USVI should look to set up a similar site, run through the government’s new Office of Health Information Technology. This website should include links to DOH and DHS healthcare programs, as well as information on services provided by the territory’s hospitals, FQHCs, and DOH health clinics. The website should also include information on insurance options available in the USVI, including enrollment information for Medicaid, Medicare, government employee insurance, and private employer options. When directing residents to information on government healthcare programs, public officials would then be able to provide a single, easily accessible link to USVI health information (e.g., www.vi.gov/health), instead of several different links spread across multiple agency and department websites. This website will be an important resource for USVI residents, both in increasing health literacy across the territory, but also in helping residents navigate insurance options and enroll in the Medicaid buy-in program, if they are eligible.
Progress on this recommendation would likely require new funding to support the development and continued maintenance of the website. Administration of the site could run through the Office of Health Information Technology, which may have existing staff trained to operate the website. Federal grant opportunities may also be available to support the creation of this website, as part of a larger health technology initiative in the territory.
With responsibility for health policy, programs, and insurance provision spread across multiple agencies, cross-department coordination and the development of a robust government healthcare strategy will require collaboration and buy-in from stakeholders across the healthcare spectrum, including providers, patients, and numerous public officials. Creating a Healthcare Cabinet is a short- to medium-term step that could be established with little to no funding required, and should be the first option considered to improve government coordination. Moving forward, the Healthcare Cabinet could also be a resource to the government as it thinks through new healthcare policy ideas and ways to increase coordination across departments. Establishing a centralized healthcare website will take more time and resources and may require buy-in from the legislature if new funding is required to support the initiative. The government should see if the work of developing and maintaining the website can be supported by the new Office of Health Information Technology.
Over the course of our interviews, stakeholders expressed a lack of access to general, territory-level, up-to-date population health data. Improving health data collection, analysis, and coordination supports the establishment and maintenance of the Medicaid buy-in by identifying and quantifying population health trends, disease burdens, and medical needs. This information would support the calculation of the Medicaid buy-in premium structure and Alternative Benefit Program and would assist healthcare entities in the USVI prepare to meet the needs of the Medicaid buy-in population.
Currently, information is limited to what exists at an individual clinic, department, office, or hospital level, constraining overall knowledge of broad trends in the health needs of US Virgin Islanders. Additionally, many stakeholders voiced their need for improved data analytical capacity, as they collect information but do not have people who are trained to analyze it. Finally, data sharing between various healthcare entities is limited or nonexistent.
This section first outlines the organizations conducting health data collection and analysis in the territory and the challenges they face. We then provide recommendations for improving data collection and analysis that surfaced throughout our interviews. Progress on these points would assist health system stakeholders understand the needs of the population and enable policymakers to make data-informed health decisions.
1. Improve collaboration between DOH and health facilities for data sharing.
2. Train interested DHS and DOH employees in data analysis.
3. Establish the Health Information Exchange as a centralized data repository for population health tracking by expanding patient inclusion.
The healthcare sector in the USVI lacks a centralized data repository. To bridge this gap in critical healthcare arenas, such as diabetes tracking and immunizations, health leaders are working to establish registries as a stopgap to system-wide data collection. Individual healthcare entities collect data from patient visits, but there is no mechanism to share this data between entities and develop a territory-level view of the healthcare sector. Additionally, many individual healthcare entities lack the trained personnel to analyze existing data.
There are multiple organizations in the USVI that conduct health-related research and data analysis. The Eastern Caribbean Center (ECC) conducts the decennial census and has historically conducted the annual Virgin Islands Community Survey (VICS). 83 The VICS is an alternative to the American Community Survey. However, the disruptions of Hurricanes Irma and Maria have prevented any collection and publication of the
VICS since 2015.
The Caribbean Exploratory Research Center (CERC), established in 2007 under the Department of Nursing at the University of the Virgin Islands, focuses mainly on health research and seeks to advance health equity in the Caribbean through translational research. 84 However, in 2016 the National Institute on Minority Health and Health Disparities (NIMHD) ceased funding small research programs. As a consequence, the CERC lost operational funding. Operational funding is separate from project and contract funding, which the CERC has leveraged to continue conducting research since losing NIMHD funding. Moving forward, CERC assesses the organization requires $2.4 million in operational funding to re-establish full-time operations over next 5 years, in addition to project and contract funding. 85
The Kids Count Data Book provides data on child well-being across the United States and includes a section dedicated to health and safety. The Annie E. Casey Foundation funds the annual publication of the data book, and in the USVI the data book has relied almost entirely on VICS data from the ECC. In 2019 the Community Foundation of the Virgin Islands published their last Kids Count Data Book, and in the absence of VICS data, provided a grant to CERC to conduct stopgap research covering 2016-2019. 86 In 2021 the St. Croix Foundation for Community Development published an updated Kids Count Data Book using information collected directly from private and public agencies in the USVI. 87 Finally, the Department of Health publishes reports on the healthcare sector, including the 2020 Community Health Assessment Report and their Community Health Improvement Plan. Due to time constraints, DOH has relied on public data sources, so reports are unable to fully incorporate health data from the FQHCs, private practice medical providers, and hospitals. 88 Additionally, DOH participates in the Behavioral Risk Factor Surveillance System which surveys adult health-related risk behaviors, chronic health conditions, and use of preventive services. However,
it does not routinely participate in the Youth Risk Behavior Surveillance System (YRBS), a similar survey for high school and middle school students. The DOH secured grant funding for the CERC to conduct the YRBS in 2018.
The recommendations below offer various paths to address the data collection and analysis shortfalls in the USVI. Progress on these recommendations would supplement the work being done by the organizations discussed above, and specifically improve population health understanding at the territory level.
In conjunction with the DOH’s Strategic Priority to “Lead Public Health Collaboration in the Community,” DOH should engage with FQHCs, the hospitals, and private clinics to encourage and facilitate data sharing. DOH has meaningfully moved to assume a leadership role in the healthcare space. In its Strategic Plan for 2020-2025, the Department included a strategic priority to “Lead Public Health Collaboration in the Community,” and the cross-cutting priority to “Use Data-Driven Decision Making.” 89 DOH’s leadership is beneficial to the system, as encouraging collaboration and data sharing between healthcare entities is an important step towards reducing the well-documented data silos that exist in the USVI today.90
In line with its strategic leadership priority, DOH brought together health sector entities in 2020 and 2021 to form a steering committee to develop a Community Health Improvement Plan. DOH successfully brought together government representatives, both FQHCs, and one of the two hospitals to collaborate and collectively create a long-term health improvement plan. The DOH published the Community Health Improvement Plan in April 2022.91
Improving health data and informatics was
established as an objective under the Community Health Improvement Plan. The steering committee set initial strategies including convening a data users group, identifying gaps in existing data systems, and creating an integrated health data system, and progress in these areas would be transformative. Fully incorporating health data from FQHCs, hospitals, and private clinics with DOH data is critical to inform a holistic, accurate picture of vital health trends and indicators.
DOH is also participating in the CMS Data Modernization Initiative, a national effort to create modern, integrated, and real-time public health data and surveillance. This effort presents an excellent chance for DOH to share lessons learned and opportunities with the FQHCs and hospitals.
The territorial healthcare sector’s continued action and progress on these initial strategies is necessary to realize improvement. Previous publications, councils, and grants have laid out plans to establish electronic health records, improve data infrastructure in the USVI, and encourage data collaboration between healthcare entities.92 Because of the difficulty of creating electronic, integrated systems, focusing on collaboration and data sharing between healthcare entities is a reasonable and actionable first step. Taking this first step would alleviate the data silos that exist in the USVI today while the Health Information Exchange (HIE) is being established as the ultimate solution for data sharing.
This is the most affordable of the data-based strategies. Because of COVID-19, the CHIP steering committee met virtually. Holding in-person and virtual meetings for the data users group may maximize participation given the geographic distance between many healthcare providers. Progress on this recommendation could be
limited by the commitment level and attention from all applicable parties, including the FQHCs, hospitals, and DOH. Full participation from all involved entities is required to achieve progress. Establishing a mechanism for healthcare entities to share health data and metrics with DOH may be complicated by HIPAA requirements.
The UVI recently developed classes and a minor in data analytics. This program will assist with longterm growth in the local talent pool of trained data analysts. However, take-up of the program among current students has been limited, and it may take a few years for interest and participation to truly take off. In the meantime, DHS and DOH could solicit interest in data analysis training from current employees and fund their participation in agency-approved courses.III In addition to expanding data analysis capacity for the Departments, this would have the dual benefit of offering current staff members an opportunity for professional development.
Progress on this recommendation depends on the availability of interested current employees, training opportunities, the quality of the instruction, and the availability of funding for training. However, this is a relatively low-cost intervention that may improve, although is unlikely to solve, the data analysis shortfalls that healthcare entities like DOH and DHS currently face.
III As an example, Data and Technology Associates, LLC offers a 5-session program in Data Science .
The Office of Health Information Technology was established in October 2021 to oversee the implementation of the HIE for Governor Bryan’s Healthier Horizons Initiative. The establishment of the HIE is made possible by a grant from CMS and is limited to covering Medicaid enrollees.93 Once established, however, expanding the HIE beyond Medicaid enrollees poses the best longterm solution to the lack of a centralized repository of health data in the USVI. A high quality HIE provides the data infrastructure to pull anonymized data to generate and analyze population health indices and metrics. Colorado, Maryland, and Rhode Island operate high quality HIEs that could be used as models for the USVI.
Progress on this recommendation would be limited by securing a funding source. The grant from CMS is limited to Medicaid enrollees, and a second grant would likely be required to expand the HIE. Additionally, progress would be limited by provider compliance with data entry requirements. Expanding the HIE beyond Medicaid enrollees would also require incorporating
providers that do not see Medicaid patients and are initially unconnected to the HIE. It is also likely that legislation would be required to mandate data system adoption and data entry to facilitate the collection of territory-wide, high-quality data.
Data silos within the USVI healthcare sector are a well-documented issue, with multiple stakeholders working to fix the issue over the years. IV True progress in establishing a central data repository in the USVI will realistically take extended, coordinated efforts over multiple years. Additionally, ensuring compliance with data system adoption and data entry is likely to ultimately require legislative action. Improving collaboration among healthcare entities and training current employees in data analysis provide lower cost, shortterm solutions that may improve current conditions, but will not fully resolve the situation.
Secondly, establishing and maintaining a data repository or data systems would also require a workforce trained in IT, which some stakeholders expressed concern about in our interviews. Data systems software updates would be required routinely. Given the pace of technological change, hardware updates may also be required every few years. Finally, given the continued threat of hurricanes and natural disasters in the territory, technological systems must be future-proofed.
IV As an example, USVI received a federal grant in 2010 to improve their health information technology infrastructure. Source: Regional Health Equity Council II, Committee on Research, Evaluation, and Data. “Improving Health Data Infrastructure for the U.S. Virgin Islands.” USVI, 2016.
The USVI faces unique challenges in healthcare affordability, access, and delivery. These challenges are exacerbated by inadequate Medicaid funding from the federal government due to the USVI’s status as a territory. Inadequate and inconsistent funding has strained healthcare resources, particularly amidst increasing climate volatility and the COVID-19 pandemic. While a permanent legislative fix to the funding structure of Medicaid in the USVI (mirroring that of the states) would be the most effective solution for expanding health care access and quality, a Medicaid buy-in program represents a more politically viable and swiftly actionable option.
Our recommendation for a Medicaid buy-in program largely stems from the USVI’s extremely limited private insurance marketplace. Without a functional private marketplace, insurance plans are unaffordable and inaccessible for many Virgin Islanders. Our proposed Medicaid buy-in would provide expanded health coverage to individuals earning between 133-400% of the USVIPL, allowing USVI residents to buy into Medicaid-like coverage on a sliding scale based on individual income.
The effectiveness of such a program could be scaled by a publicly-funded effort promoting the benefits of preventive care and health insurance to increase both individual interest and participation in the buy-in program. Local health care providers can serve as effective educators by engaging individuals thoughtfully and respectfully about preventive care benefits. Educating residents on the value of health insurance, expanding health education measures, and improving health literacy all hold potential to improve health outcomes in the USVI.
Another challenge to the healthcare system in the USVI is a shortage of healthcare providers. Even a well-designed Medicaid buy-in program would be hindered by a lack of available Medicaid providers, and efforts to recruit and retain new providers would be important for the program’s overall success. Partnering with the future
UVI Medical School and adopting medical compacts to facilitate provider licensing could help to address this issue. Facilitating telehealth utilization, which has already increased significantly during the Covid-19 pandemic, has similar potential to expand access and allow providers to triage care more efficiently. Leveraging healthcare workforce development funds and increasing care coordination are two other potential strategies to reduce provider shortages.
Another strategy to support the Medicaid buyin program is to improve care coordination between government agencies and departments. This would allow for more streamlined administration of healthcare programs in the USVI. The formation of a new Healthcare Cabinet to discuss and evaluate policy, programs, and insurance holds potential for improving coordination and increasing efficiency across agencies. Likewise, developing a centralized healthcare website for USVI residents can increase access to information about insurance offerings and community health resources.
Finally, enhancing health data collection, analysis, and coordination in the USVI can support the establishment of a Medicaid buy-in program. Identifying and quantifying population health trends, burdens, and medical needs would allow for more precise delivery of healthcare and address emerging public health needs. Increasing data sharing and creating a centralized health repository would enable more accurate and extensive data analysis.
Although there are certainly costs and challenges to implementation, a Medicaid buy-in program presents an opportunity to maximize access to insurance and strengthen healthcare delivery in the USVI. The buy-in program would offer affordable access to healthcare coverage for some of the USVI’s most vulnerable populations, particularly if accompanied by supporting programs to improve health education, interagency coordination, data collection, and address provider shortages.


Adequate and stable Medicaid funding is vital for ensuring the continuous delivery of healthcare in the USVI, particularly amidst a global pandemic and increasingly volatile weather patternsI. Historically, the USVI has received inconsistent funding from the federal government for the administration of its Medicaid program, resulting in challenges to the islands’ healthcare system. On December 29th, 2022, President Biden signed H.R. 2617 into law, permanently increasing the USVI’s FMAP to 83%. This was a major step towards healthcare equity in the USVI, and brought the USVI closer to parity with the states. However, the USVI is still limited by its federal funding cap. Eliminating this funding cap would be an important step towards supporting an equitable and innovative health system in the USVI.
Longstanding disparities in Medicaid financing have contributed to broader health system challenges in the US Virgin Islands. Like the states, Medicaid costs in the USVI are shared between the federal government and the territory. The rate at which these costs are shared is called the FMAP. In states and D.C., the FMAP is adjusted annually based on a state’s per-capita income. The USVI, however, has traditionally been subject to a fixed FMAP rate as well as an annual capped allotment from the federal government.94 This FMAP level was set by statute at 55% and did not change based on the USVI’s population characteristics. When compared to states with similar income levels, USVI’s FMAP was much lower.
Congress temporarily increased the FMAP rate for the USVI and other territories several times, often in response to natural disasters or other emergency situations. Most recently, the USVI received an increased FMAP due to the COVID-19 Public Health Emergency. With the Emergency set
to expire on May 11th, 2023, the USVI was bracing for its FMAP to plummet to 55% from 89.2%.95 Fortunately, the Consolidated Appropriations Act (H.R. 2617) was signed into law on December 29th, 2022, averting this fiscal cliff and permanently increasing the USVI’s FMAP from 55% to 83%, comparable to the FMAP of states with similar income levels. The law also increases provider reimbursement rates and provides 100% funding for qualifying data system improvements.96
While the increased FMAP is undoubtedly a legislative victory for the USVI, the federal funding cap remains a limiting factor, placing the territory in a vulnerable position with limited capacity to respond to emergency situations and other unplanned expenses. In the states and D.C., Medicaid is considered an entitlement program and total dollars available from the federal government are uncapped. However, the USVI can only receive federal matching funds up to the annual allotment set in Section 1108 of the Social Security Act.97 Once the federal government has contributed enough to reach the cap, there are no additional federal funds available absent Congressional intervention. This arrangement puts patients at risk and strains resources, especially institutions and providers that serve Medicaid recipients. Without reliable funding, healthcare system expansion and innovation are difficult, and maintenance of existing healthcare infrastructure is often deferred.
Moving forward, federal legislation to remove the federal funding cap is important for the longterm stability of healthcare infrastructure and delivery in the USVI. Removing the funding cap to transition USVI Medicaid funding to mirror state Medicaid funding would support the stability and resilience of the entire USVI healthcare system.

Provision of medical care and coverage for medical expenses for the undocumented population present a unique policy challenge. The ACA explicitly excludes the undocumented immigrant population from Medicaid coverage and access to the public health insurance exchanges. In our interviews, we heard from multiple stakeholders that the USVI has a sizable population of undocumented immigrants, who usually have a limited ability to pay. However, the USVI passed a statute forbidding healthcare providers from denying care on the basis of inability to pay.98 Therefore, the undocumented population largely accesses medical care without insurance coverage which results in large uncompensated care costs for the healthcare providers.
The exact size of the undocumented immigrant population is difficult to determine, and often in the literature such populations are labeled as “the uncountable.” Several authors have utilized population and immigration data to create projections and estimates of the size of the undocumented immigrant population. However, such projections have a large margin of error and do not cover estimates at the granular level of U.S. territories like the Virgin Islands. Department of Homeland Security’s yearly immigration
statistics bucket all U.S. territories in one group and individual statistics for the USVI are not available. Hypothetically, a triangulation exercise can be done to estimate a range for the size of undocumented immigrant population if these data were available. The following paragraph provides a strategy for creating these estimates. While acknowledging that differing opinions exist around the completeness of the U.S. Census for 2020 in the USVI, we know that of the 84,891 total people in the USVI, 29,579 were born outside the United States and its territories. Assuming that the census counted everyone, this is the upperbound for the undocumented immigrant population living in the US Virgin Islands. If data on the number of naturalizations, temporary migrants (like foreign students), humanitarian migrants (such as refugees) and people with lawful permanent status were available over a certain number of past decades for the US Virgin Islands, we would be able to determine the subset of these 29,579 people living in the Virgin Islands legally. We would then subtract the number of such legal residents from the total non-native population living in the US Virgin Islands and get an estimate of the size of the undocumented population.

20,825 people in the USVI do not have health insurance coverage, which amounts to around 24% of the population. That proportion is more than twice the national uninsured average of 9%.
We used mapping data to shed light on questions related to the uninsured population in the USVI. Where do most people live in USVI? Where do the uninsured live? What are their linkages with poverty, unemployment and the income distribution?

Due to the small population of Water Island, our analysis focuses on the three largest islands.
Population Distribution: St. Thomas (top) is the most populous of the three islands, with St Croix (bottom-right) having small population concentrations, and St John having sparse quantities of people. Notable Polygons (geographic boundaries at the estate level) include:
largest: Anna’s Retreat, St. Thomas - 5,551 people
Densely Populated Areas on St. Thomas: The Whim’s East, Bovoni, Smith Bay, Thomas, Lindbergh Bay - between 1,600 and 2,500 people
Highest Population Concentration: Kronprinsens Quarter, St. Thomas - 1,804 people
most Populated Areas on St. Croix : William’s Delight, VI Corporation Land, Barren Spot West
Income Per Capita Distribution: Capturing the income distribution within the geographic boundaries is complicated by the low population levels for the USVI down to the estate level. The income distribution, as measured by income per capita within each polygon, is a complex story but offers significant insights.
High Income Areas: Of the 5 estates with per capita incomes between $85,000 and $156,500, four are on St. Croix, with a total population of only 56. Wintberg on St. Thomas has the highest density of top per capita income averages with 936 people and an average per capita income of $90,505.
middle Income Areas : 90 estates across the three islands have an average per capita income between $40,000 and $85,000. But the average masks different sub-types - some are made up of a few upper middle class individuals, while other areas are densely populated with a wide range of incomes represented. Anna’s Retreat is a top example of the latter, with 5,551 people averaging $65,402 per capita. Nazereth, with 1,010 people averaging $48,598 per capita, is another example. However, there is a density of poverty masked under that relatively high average. Areas of poverty, discussed later in the appendix, demonstrate similarly wide ranges in population densities.

Number of People Uninsured: Where do the 20,825 uninsured people live in the USVI? It seems that the highest population concentrations contain the highest number of uninsured people.
In Anna’s Retreat, the heart of St. Thomas, 1,419 out of 5,551 people are uninsured (25%) - a proportion even higher than the USVI average. This geographic concentration of an uninsured population provides an opportunity for outreach during the Medicaid Buy-in marketing campaign. Smith Bay, Bovoni, Kronprinsens Quarter (the other 3 dark blue areas), and Thomas and The Whim East (in St. Croix) are all major population hubs and are affected by a lack of health insurance coverage in proportion to their population,
with a total of 3,214 uninsured people. This pattern follows for smaller population hubs across the three islands, including William’s Delight, VI Corporation Land, and Barren Spot West in St. Croix.
Some estates, though, have medium to low levels of total population (500-1,300) yet have a high level of uninsured people (around or more than 200 people). A lot of such populations are in St. Croix, as highlighted by the splatter of medium-blue polygons in St Croix. But there are a few such estates in St Thomas as well. Estates like Altona and Welgunst, Contant 7A, and Hospital Ground have 466, 398, and 367 uninsured people, respectively.
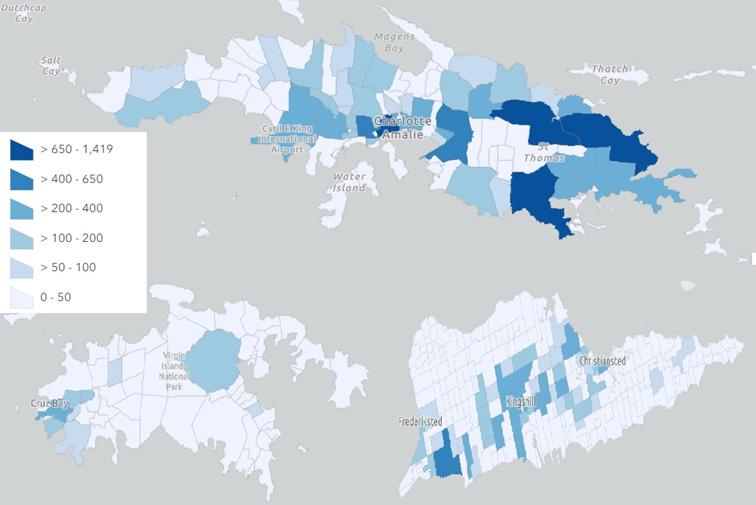
Poverty: Anna’s Retreat and Bovoni are the top two estates (dark blue) with the highest number of people experiencing poverty, with 1,066 and 813 people in poverty, respectively. The usual suspects from both St. Thomas (Smith Bay, Kronprinsens Quarter, Thomas, Lindbergh Bay, Contant 7A, Nazareth) and St. Croix (William’s Delight, VI Corporation Land, Barren Spot West) feature in the second highest scale categories for number of people in poverty (on the map in medium blue) .

Unemployment: The official unemployment rate in the USVI is below 10%, with 3,806 people unemployed out of the total labor force of 39,416. However, this masks the large number of people who are of working age but have left the labor force - in that they report neither working nor seeking to work as their employment status. 23,943 individuals in the USVI report having left the labor force, which is 37% of the working age population. The map generated below includes that population in the unemployed representations to reflect a complete picture of those without formal jobs (and hence without work related insurance). We note that these populations geographically overlap with the uninsured and poverty trends of each estate.
Conclusion: This analysis of the income distribution and concentrations of poverty, unemployment, and those lacking health insurance in the USVI reveals geographic densities of these populations. Specific outreach and marketing strategies should be targeted in these areas to optimize the enrollment of these populations in either Medicaid or the Medicaid buy-in.
Source and Methodology: The statistical data and GIS files for this analysis were obtained from data.census.gov. The statistical and GIS analysis was executed by the authors.
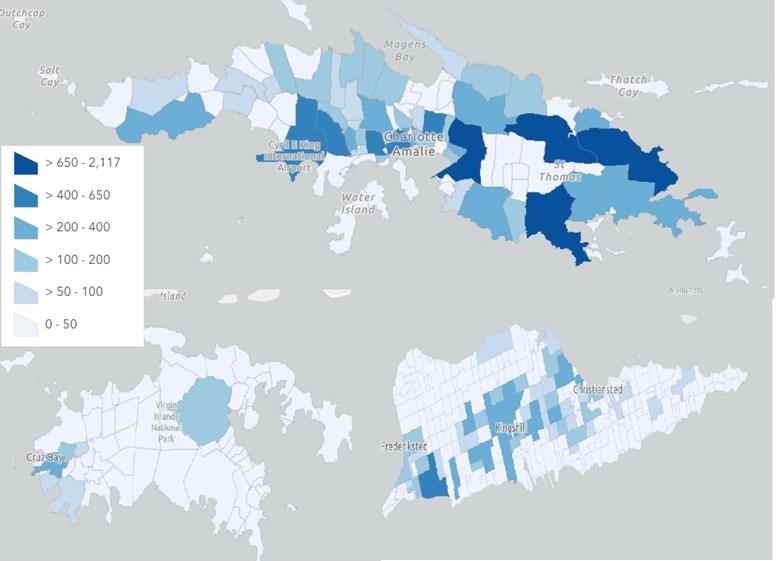

k atie Comando is originally from rural Cutchogue, New York and graduated from the State University of New York at Geneseo in 2013. She started her career as an AmeriCorps volunteer serving agricultural workers, then moved to Government Affairs for one of the largest Community Health Centers in the country. At Princeton, Katie studies domestic health policy and has interned with the Health Resources and Services Administration in the Maternal and Child Health Bureau, and as a fellow with the New Jersey Governor’s Office on the Health Team of the Wealth Disparity Taskforce.
Heather Jebb is originally from Seattle, Washington and graduated from the United States Military Academy in 2012. Heather is an active duty Army officer and has previously served as a platoon leader, company commander, and battalion intelligence and operations officer. She is studying domestic policy while at Princeton and after graduation will teach American politics at the United States Military Academy.
k irsten kuhn is originally from Carbondale, Colorado. She received a B.A. in Sociology and Social Welfare from the University of Wisconsin-Madison, and went on to earn her master’s degree at the School of Medicine at Oregon Health and Science University. After graduation she moved back to Colorado, where she worked in primary care and dermatology as a certified PA. At Princeton, she is studying domestic policy and health policy, and is interested in healthcare reform and equity, as well as improving access to affordable care in the United States.
Dillon mcnamara was born and raised in Southern New Jersey and graduated from The College of New Jersey with a B.A. in Political Science. After graduation, he worked at the New Jersey Office of the Secretary of Higher Education, where he
helped to advance college access and affordability initiatives in the state, and as a policy coordinator in the New Jersey Office of the Governor, focusing on health and human services policy. After Princeton, Dillon hopes to continue advocating for low-income and marginalized communities in the state through evidence-backed policy work.
katie Pannell is originally from Northern California and graduated from UCLA with a B.S. in Microbiology, Immunology, and Molecular Genetics. She previously worked in public health in Sierra Leone, Nigeria, and the U.S., focusing on building more resilient and equitable health systems. At Princeton, she is studying domestic policies to reduce poverty and inequality.
osama Safeer was born and raised in Pakistan and graduated from Lahore University of Management Sciences in Economics and Mathematics. After graduation, he worked on health and education in Pakistan, across the public sector, management consultancies and nonprofits. At Princeton, he is focusing on international development.
Arthur Shemitz is originally from Santa Cruz, California and graduated from Whitman College with a B.A. in Gender Studies. He previously worked in the California state government and as a graduate intern with the Senate Finance Committee. At Princeton, Arthur is studying domestic policy with a focus on taxes and retirement.
Justine Yu is originally from Bakersfield, California and graduated from UC Berkeley with a B.A. in Cognitive Science and Political Economy. She previously worked as a summer analyst at Manatt Health, policy aide at the U.S. Department of Health & Human Services, and as a behavioral science and social policy researcher at MDRC. At Princeton, Justine is studying health policy, economics, demography, and intersections therein.
Dan meuse, Deputy Director of the Advancing Coverage in States, and State Health and Value Strategies programs, is based at the Center for Health and Wellbeing. He assists the program director in managing and coordinating the technical assistance providers serving states in their implementation of the Affordable Care Act and various payment and delivery system reforms. Dan was deeply involved in Affordable Care Act implementation at the state level as Deputy Chief of Staff for Rhode Island’s Lieutenant Governor. Dan was the principle subject matter expert for the Rhode Island Healthcare Reform Commission on Health Insurance Exchange policy and delivery system and payment reform through mid-2014. He also served as the State Innovation Model project director for Rhode Island’s Model Design project and led the Exchange’s stakeholder engagement efforts. Dan received a Bachelor of Arts from Brown University and a Master’s in Business Administration from Providence College.
Heather Howard is a faculty affiliate of the Center for Health & Wellbeing and director of State Health and Value Strategies, a Robert Wood Johnson Foundation-funded program that provides technical assistance to support state efforts to enhance the value of health care by improving population health and reforming the delivery of health care services. She served as New Jersey’s Commissioner of Health and Senior Services from 2008-2010, overseeing a cabinet-level agency with a budget of $3.5 billion and staff of 1,700 responsible for public health services, regulation of health care institutions, senior services, and health care policy and research.
Previously, Howard served as Governor Jon Corzine’s Chief Policy Counsel, directing his policy agenda. She also has significant federal experience, having worked as Senator Corzine’s Chief of Staff, as Associate Director of the White House Domestic Policy Council and Senior Policy Advisor for First Lady Hillary Clinton, as an Honors Attorney in the U.S. Department of Justice’s Antitrust Division Health Care Task Force, and for the U.S. House of Representatives. She received her J.D., cum laude, from the New York University School of Law, and her B.A. cum laude, from Duke University.
1 “US States - Ranked by Population.” https://worldpopulationreview.com/states.
2 US Census Bureau, “Census Bureau Releases 2020 Census Population and Housing Unit Counts for the U.S. Virgin Islands,” Census.gov.
3 Shelly Culbertson et al., “Recovery in the U.S. Virgin Islands: Progress, Challenges, and Options for the Future” (RAND Corporation, November 11, 2020).
4 USVI Hurricane Recovery and Resilience Task Force, “USVI Report,” 2018.
5 Lina Stolyar et al., “Challenges in the U.S. Territories: COVID-19 and the Medicaid Financing Cliff,” KFF (blog), May 18, 2021.
6 USVI Hurricane Recovery and Resilience Task Force, “USVI Report.”
7 USVI Hurricane Recovery and Resilience Task Force.
8 HRSA, “Overview of the State - Virgin Islands,” 2020.
9 US Census Bureau, “2020 Island Areas Censuses.”
10 United States Virgin Islands Department of Health, “Community Health Assessment,” May 2020.
11 United States Virgin Islands Department of Health.
12 Cornelia Hall, Robin Rudowitz, Kathleen Gifford, “Medicaid in the Territories: Program Features, Challenges, and Changes” (KFF, January 2019).
13 “V.I. Code Tit. 19, § 277,” Justia Law, 2019.
14 “JFL’s Proposed $77 Million Budget Intends to ‘Do More With Less,’” St. Thomas Source, July 13, 2022.
15 US Census Bureau, “2020 Island Areas Censuses.”
16 US Census Bureau, “Decline in Share of People Without Health Insurance Driven by Increase in Public Coverage in 36 States,” Census.gov, September 15, 2022.
17 US Census Bureau, “2020 Island Areas Censuses.”
18 US Census Bureau, “2020 Island Areas Censuses.”
19 Jessica Sharac et al., “The Recovery of Community Health Centers in Puerto Rico and the U.S. Virgin Islands One Year after Hurricanes Maria and Irma” (KFF, September 2018).
20 Health Professional Shortage Areas (HPSA) - Primary Care (HRSA, November 26, 2022); KFF, “Primary Care Health Professional Shortage Areas (HPSAs),” State Health Facts (blog), September 30, 2022.
21 United States Virgin Islands Department of Health, “Community Health Assessment.”
22 “Medicaid & CHIP in United States Virgin Islands,” Medicaid.gov.
23 “Medicaid and CHIP in the Territories.” Medicaid and CHIP Payment and Access Commission, February 2021.
24 “Federal Medical Assistance Percentage (FMAP) for Medicaid and Multiplier.” Kaiser Family
Foundation.
25 Edwin Park, Anne Dwyer, Tricia Brooks, Maggie Clark, and Joan Alker. “Consolidated Appropriations Act, 2023: Medicaid and CHIP Provisions Explained.” Center For Children and Families (blog), January 6, 2023.
26 “Lack of Federal Action Puts Puerto Rico and Other Territories in Peril of Dire Medicaid Fiscal Cliff, Yet Again,” Center For Children and Families (blog), October 4, 2022.
27 Jennifer Tolbert, “10 Things to Know About the Unwinding of the Medicaid Continuous Enrollment Requirement,” KFF (blog), January 11, 2023.
28 “10 Things to Know About the Unwinding of the Medicaid Continuous Enrollment Requirement.”
29 Lisa Clemans-Cope et al., “Medicaid Spending Growth Compared to Other Payers: A Look at the Evidence - Issue Brief,” KFF (blog), April 13, 2016.
30 Kristin Wikelius, Allison O’Toole, and Medicaid Buy-in, “Medicaid Buy-In: State of Play,” n.d.
31 MACPAC, “Medicaid and CHIP in the U.S. Virgin Islands.”
32 “HealthCare.Gov Glossary,” HealthCare.gov.
33 United States Virgin Islands Department of Health, “Community Health Assessment.”
34 “Many Women Still Receive Little or No Prenatal Care Before Giving Birth | KIDS COUNT Data Center,” accessed December 9, 2022.
35 “FastStats: Immunization,” October 21, 2022.
36 “History of Health Literacy Definitions - Healthy People 2030 | Health.Gov.”
37 Jean Edward et al., “Significant Disparities Exist in Consumer Health Insurance Literacy: Implications for Health Care Reform,” HLRP: Health Literacy Research and Practice 3, no. 4 (November 2019): e250–58.
38 Renuka Tipirneni et al., “Association Between Health Insurance Literacy and Avoidance of Health Care Services Owing to Cost,” J AMA Network Open 1, no. 7 (November 16, 2018): e184796.
39 Nancy D. Berkman et al., “Health Literacy Interventions and Outcomes: An Updated Systematic Review,” Evidence Report/Technology Assessment, no. 199 (March 2011): 1–941.
40 Nathan Tefft and Andrew Kageleiry, “State-Level Unemployment and the Utilization of Preventive Medical Services,” Health Services Research 49, no. 1 (February 2014): 186–205.
41 Joseph D. Freeman et al., “The Causal Effect of Health Insurance on Utilization and Outcomes in Adults: A Systematic Review of US Studies,” Medical Care 46, no. 10 (October 2008): 1023–32.
42 Benjamin D. Sommers et al., “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” JAMA Internal Medicine 176, no. 10 (October 1, 2016): 1501–9.
43 Kim Waddell and Greg Guannel, “Health Sector Profile and Resilience Analysis for the United States Virgin Islands,” unpublished second draft.
44 Amanda T. Woodward et al., “Complementary and Alternative Medicine for Mental Disorders Among African Americans, Black Caribbeans, and Whites,” Psychiatric Services 60, no. 10 (October 2009): 1342–49.
45 Jamie C. Barner et al., “Use of Complementary and Alternative Medicine (CAM) for Treatment among African-Americans: A Multivariate Analysis,” Research in Social & Administrative Pharmacy : RSAP 6, no. 3 (September 2010): 196–208.
46 “Traditions of Health: Culturally Relevant Integration Model” (California Consortium for Urban Indian Health, August 2015).
47 Danielle M. Muscat et al., “Using Feasibility Data and Codesign to Refine a Group-Based Health Literacy Intervention for New Parents,” HLRP: Health Literacy Research and Practice 5, no. 4 (October 2021): e276–82.
48 Francisca Goldsmith, Libraries and the Affordable Care Act : Helping the Community Understand Health-Care Options (Chicago, Illinois: ALA Editions, 2015).
49 Sara Kirkpatrick, “Governor Announces Partnership with V.I. Diabetes Center of Excellence,” The Virgin Islands Daily News, November 30, 2021.
50 “Toolkit for Making Written Material Clear and Effective,” Centers for Medicare and Medicaid Services, December 1, 2021.
51 A. J. Housten et al., “Stakeholders’ Perceptions of Ways to Support Decisions about Health Insurance Marketplace Enrollment: A Qualitative Study,” BMC Health Services Research 16 (November 8, 2016): 634.
52 Mary C. Politi et al., “Knowledge of Health Insurance Terminology and Details Among the Uninsured,” Medical Care Research and Review 71, no. 1 (February 1, 2014): 85–98.
53 Minal R. Patel et al., “Use of Storytelling to Increase Navigation Capacity Around the Affordable Care Act in Communities of Color,” Progress in Community Health Partnerships: Research, Education, and Action 12, no. 3 (2018): 307–19.
54 Christoph Kowalski et al., “The Health Literate Health Care Organization 10 Item Questionnaire (HLHO-10): Development and Validation,” BMC Health Services Research 15 (February 1, 2015): 47.
55 “Designated Health Professional Shortage Areas Statistics” (Bureau of Health Workforce Health Resources and Services Administration (HRSA), September 30, 2022).
56 “Governor Bryan Approves $20 Million to Territory’s Hospitals,” The Official Site of the United States Virgin Islands Government, July 25, 2022.
57 Gilbert, “UVI Medical School”
58 Gilbert, “UVI Medical School”
59 “New Law Establishes Nurse Licensure Compact,” St. Thomas Source, December 13, 2021, sec. Community.
60 “Interstate Medical Licensure Compact,” American Medical Association, 2022.
61 “Telehealth: A Post-COVID-19 Reality? | McKinsey.”
62 Shilpa N. Gajarawala and Jessica N. Pelkowski, “Telehealth Benefits and Barriers,” The Journal for Nurse Practitioners 17, no. 2 (February 2021): 218–21.
63 “Healthier Horizons - Government of the United States Virgin Islands,” accessed November 27, 2022.
64 Governor Roach, “Virgin Islands Telehealth Act” (2020).
65 “United States Virgin Islands Health IT Strategic Plan 2021 - 2024” (Office of Health Information Technology 1, December 14, 2021).
66 “Bringing Puerto Rico Together and Connect USVI Fund Stage 2,” Federal Communications Commission, July 31, 2020.
67 “The Broadband Equity Access and Deployment (BEAD) Program,” accessed December 9, 2022.
68 “Apply to the Nurse Corps Loan Repayment Program,” Government, Health Resources & Services Administration Bureau of Health Workforce, accessed December 10, 2022.
69 Tammy Mayo-Blake, Brandon Rose, and Audrey Adade, “Health Careers Opportunity Program (HCOP): The National HCOP Academies Council on Graduate Medical Education” (Health Resources & Services Administration, March 24, 2022).
70 “Workforce Development - Official Government of the Virgin Islands,” Government, US Virgin Islands Department of Labor.
71 “Building the USVI Talent Pipeline - Supporting Governor Bryan’s Workforce Development Initiative” (US Virgin Islands Department of Labor).
72 “DOH Launches Electronic Birth & Death Records System,” Government, Government of the United States Virgin Islands Department of Health, June 11, 2017.
73 “Vital Records & Statistics,” Government, Government of the United States Virgin Islands Department of Health, accessed December 10, 2022.
74 Brandy Brookes, “Technology Seen as Key to Medical Resiliency in the Virgin Islands,” News, The Virgin Islands Daily News, November 5, 2019.
75 Aileen D. Murphy et al., “Primary Care for Underserved Populations: Navigating Policy to Incorporate Occupational Therapy Into Federally Qualified Health Centers,” The American Journal of Occupational Therapy 71, no. 2 (January 25, 2017): 7102090010p1–5.
76 “Decolonizing Medicine: Toward Equity and Inclusivity in Integrative Healthcare,” Virtual Conference Report (Integrative Medicine for the Underserved (IM4US), September 23, 2021).
77 Elaine K. Howley, “The U.S. Physician Shortage Is Only Going to Get Worse. Here Are Potential Solutions,” TIME, July 25, 2022
78 “Governor Bryan Announces ‘Healthier Horizons’ Initiative, Sweeping Healthcare Reform for U.S. Virgin Islands,” United States Virgin Islands Government (blog).
79 “Strategic Plan 2020-2025” (United States Virgin Islands Department of Health, September 2020).
80 “Overview of the Health Care Cabinet,” Connecticut State Office of Health Strategy (blog), n.d.
81 “A Governor’s Guide to Children’s Cabinets” (National Governors Associations Center for Best Practices, August 2004).
82 “Health and Wellness Resources,” Colorado Department of Health Care Policy & Financing (blog).
83 University of the Virgin Islands, “Eastern Caribbean Center.”
84 Caribbean Exploratory Research Center, “CERC Strategic Plan: Focus on Sustainability and
Social Impact” (St. Thomas: USVI, 2022).
85 Caribbean Exploratory Research Center.
86 Community Foundation of the Virgin Islands, “Building Forward for Our Children Now! U.S. Virgin Islands Kids Count Data Book 2019” (St. Thomas: USVI, 2019).
87 St. Croix Foundation for Community Development, “2021 KIDS COUNT USVI Data Book” (St. Croix: USVI, 2021).
88 United States Virgin Islands Department of Health, “Community Health Assessment.”
89 United States Virgin Islands Department of Health, “United States Virgin Islands Department of Health Strategic Plan, 2020-2025” (Christiansted: USVI, 2020).
90 Joanne S. Luciano and Janet Turnbull-Krigger, “USVI Hazard Mitigation and Recovery Plan, Health and Human Services Sector: Sector Profile and Resilience Analysis,” Draft, V2, September 1, 2021.
91 United States Virgin Islands Department of Health, “Healthy Virgin Islands 2030 Community Health Improvement Plan” (Christiansted: USVI, 2022).
92 Regional Health Equity Council II, Committee on Research, Evaluation, and Data, “Improving Health Data Infrastructure for the U.S. Virgin Islands” (USVI, 2016).
93 “Governor Bryan Announces ‘Healthier Horizons’ Initiative, Sweeping Healthcare Reform for U.S. Virgin Islands.”
94 “Medicaid and CHIP in the Territories.”
95 Mitchell, Alison. “Medicaid Financing for the Territories.” Congressional Research Service, October 12, 2022. LaFraniere, Sharon, and Noah Weiland. “U.S. Plans to End Public Health Emergency for Covid in May.” The New York Times, January 31, 2023.
96 Carolyn McCoy, and Alex Wheatley. “Bringing the U.S. Territories Closer to Medicaid Equity.” Association of State and Territorial Health Officers blog, January 13, 2023.
97 “Compilation of The Social Security Laws: Additional Grants to Puerto Rico, The Virgin Islands, Guam, And American Samoa; Limitations On Total Payments.”
98 “2019 US Virgin Islands Code :: Title 19 - Health :: Part II - Hospitals and Nursing Schools :: Chapter 17 - Government Hospital and Medical Fees :: Subchapter I - General Provisions :: § 277. Ability to Pay,” Justia Law.
