21 minute read
News
from Health Business 20.1
by PSI Media
Under a new law due to come into force in May, all adults in England will be automatically enrolled as organ donors unless they choose to opt-out.
It is estimated that the opt-out method, known as Max and Keira’s law, will contribute to an additional 700 organ transplants each year by 2023 and cut down the list of 5,200 people waiting for life-changing surgery. MPs are set to approve the system
as part of a bid to boost the number of transplants on the NHS. Patients who have previously declared that they do not want to donate some or all of their organs will not have to re-record their decision.
If Parliamentary approval is given, 20 May will mark the point at which all adults in England will be considered to have agreed to donate their own organs when they die – unless they explicitly state otherwise or are in an excluded group. However, relatives will still be asked for their opinion which can lead to donations being blocked if they object regardless of the wishes of the deceased.
The Department of Health and Social Care has also stated that children under 18 will be excluded from the scheme, along with people who have lived in England for less than a year or have ‘lacked capacity for a significant time’. Health Secretary Matt Hancock said: “Too many people lose their lives waiting for an organ, and I’ve been determined to do what I can to boost organ donation rates.This is an important step forward in making organ donation easier and more available to those who need it and could help save hundreds of lives every year.” The law change has been welcomed by charities including the British Heart Foundation and Kidney Care UK.
READ MORE
https://tinyurl.com/wmp7nu3
CORONAVIRUS
Pilots of home testing for coronavirus started
The NHS has started pilots of home testing for coronavirus where NHS staff, including nurses and paramedics, will visit people in their own homes rather than them having to travel.
On 23 February it was publicly confirmed that four patients transferred from the Diamond Princess cruise ship in Japan had tested positive for coronavirus. They have now been transferred to three specialist NHS infection centres.
Approximately 77,000 people in China, where the virus emerged last year, have been infected and nearly 2,600 have died. No vaccine is available so far to prevent the new coronavirus and fears are growing that the coronavirus outbreak could become a pandemic as new cases are reported globally. More than 1,200 cases have been confirmed in 26 other countries, prompting more than 20 deaths. Professor Keith Willett, NHS strategic incident director for coronavirus said: “We have started to pilot home testing for coronavirus in London, which will be carried out by NHS staff, like nurses or paramedics, allowing people to stay home rather than having to travel, which is safer for you and your family and limits the spread of infection. “Anyone who is concerned they have signs and symptoms, should continue to use NHS 111 as their first point of contact – they will tell you what you exactly what you need to do and where necessary, the right place to be tested. People should also play their part by following public health advice – wash your hands, cover your mouth and nose with a tissue or sleeve when you cough or sneeze, and put used tissues in the bin immediately. I would also like to thank the NHS staff who are back in Arrowe Park ready to provide excellent care and support to the British nationals who are returning from the Diamond Princess cruise ship in Japan.”
READ MORE
https://tinyurl.com/s3r5g2t
DIABETES
Two million people at risk of type 2 diabetes
New NHS figures show that approximately two million people in England are at risk of developing type 2 diabetes, the highest on record.
Latest statistics show there are 1,969,610 people registered with a GP who have non-diabetic hyperglycaemia, a condition which puts people at high risk of type 2, which is the highest on record. It is also likely that the problem will become even greater as the growing obesity crisis is exposing millions more to the condition.
Around nine out of 10 people with diabetes have type 2 and there were over a million obesity diagnoses in hospital admissions last year, 884,000 the year before.
NHS action to combat the problem includes the Diabetes Prevention Programme which identifies people at high risk of diabetes and supports them in living a healthier lifestyle. It has had nearly a million referrals and seen patients who have so far finished it lose the combined weight of 43 ambulances. The programme, which lasts between nine and 12 months, is designed to stop or delay the onset of illness through advice and support on healthier eating and physical exercise.
Radical low calorie diets, that have been shown to stamp out recently diagnosed type 2 diabetes, will be rolled out by the NHS to 5,000 people from April.
ZETRIX ® & ZEDOX ® Eccentric Valves for Demanding Applications
YOUR STRONG BUT TERFLY VALVE PORTFOLIO
New from ARI !

Metallic Sealing-System Solutions
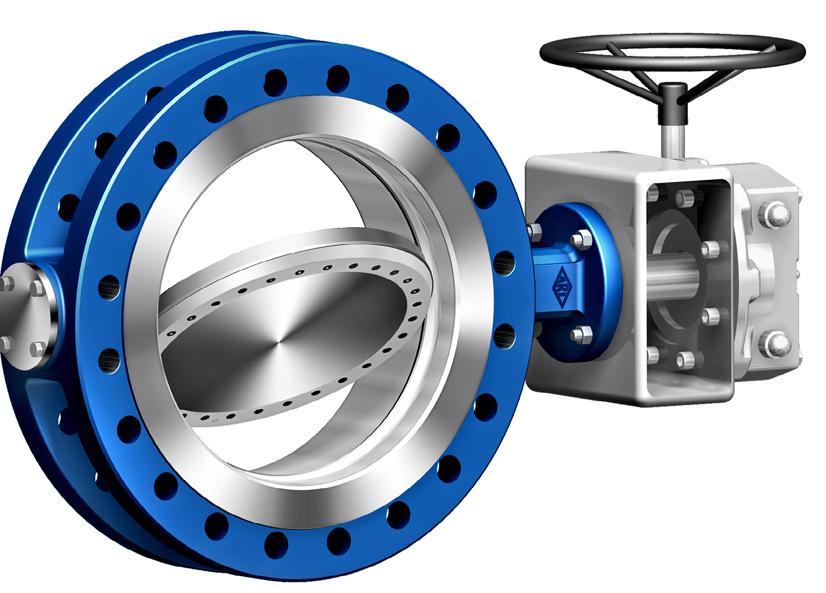
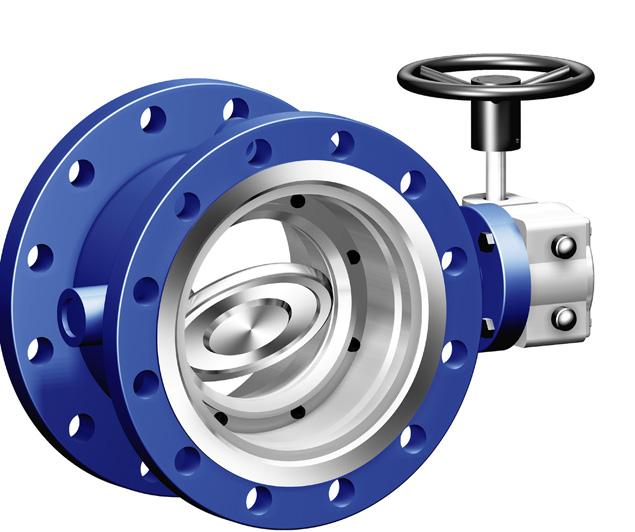
ZETRIX ® The triple-offset Process Valve - for high demanding service conditions, covering temperatures from -60°C to max. +427°C.
Optional double block and bleed arrangement and also available in butt weld ends (up to DN 600), double-flanged (up to DN 1200) or fully lugged (up to DN 600).
ZEDOX ® New from ARI: The double-offset High Performance Valve – the economical alternative.Suitable for temperatures from -40°C to +260°C (max. +400°C). Available in butt weld ends (up to DN 1600), doubleflanged (up to DN 1200) or wafer type (up to DN 800).
Request further details or more information on our full range of soft sealing butterfly valves: ZESA ® , GESA ® and ZIVA ® via our website. Alternatively contact our UK sales office!
The Institute for Government has claimed that the UK’s ‘sky-high’ visa fees could deter vital NHS staff and the ‘brightest and best’ scientists.
Nurses, lab technicians, engineers and tech experts who currently migrate to the UK from the EU may not be able to afford to do so if Prime Minister Boris Johnson’s proposed immigration overhaul becomes law. At £1,220 per person, or £900 for those on the shortage occupation list, the fees are among the highest in the world – and this is before charges for using the NHS and costs for sponsoring employers are taken into account. The think tank has published comparisons with fee structures in other countries, revealing that a family of five with a five-year work visa for one individual would have to pay £21,299 before they could enter in the country. This includes the annual £400 health surcharge that must also be paid upfront per person.
The £400 is double the fee charged by Australia and about 30 times the amount charged by Canada, where it costs just over £10,000 for a family for five years.
A single person coming to the UK is likely to be charged up to £3,220 for five years. If they want to move to the UK with a spouse, the cost would rise to £6,500 for a five-year work stint. In Canada, it is £220 for an individual visa for three years, £147 in Germany and £2,075 in France.
READ MORE
https://tinyurl.com/touzgur

New data has revealed that patient safety is at risk in ‘crumbling’ NHS mental health hospitals in desperate need of funding to improve dilapidated buildings.
Hundreds of vulnerable mentally ill patients are still being cared for in 350 old dormitory-style wards, two decades after the NHS was told to provide all patients with en-suite rooms. The research also found that funding shortfalls have meant that too many wards still have ligature points that patients can use to try to harm themselves. A briefing from NHS Providers, Mental health services: meeting the need for capital investment, sets out findings from a survey of mental health trust leaders and warns that, for 27 per cent of mental health trusts, funding allocated for capital investment would not even meet half of their current need. Furthermore, two thirds of trusts estimate that they need between £50 million and £150 million of capital investment over the next five to ten years. One trust requires just over half a billion pounds to address maintenance and transform services to meet the needs of patients.
More than one in five trusts have faced enforcement action from Care Quality Commission (CQC) over the condition of facilities and the impact on quality and safety of patient care in the last three years. However, a number of trusts are not able to access the funding required to make these improvements. Two trusts warned that they are unable to meet over 70 per cent of the costs necessary to address CQC’s safety concerns. Patients at risk in ‘crumbling’ mental health wards https://tinyurl.com/skysqrc READ MORE BUILDINGS A new report from Cancer Research UK has warned that England will fail to be smoke-free by 2030 if current smoking trends continue. The charity points to new figures which indicate that England is not expected to reach smoke-free until 2037 – seven years behind the ambitious target set last year by Health Secretary Matt Hancock in the government’s Green Paper on Health Prevention.
Currently, 14 per cent of adults in England smoke cigarettes. The government wants to see this drop to five per cent by the end of this decade, but plans on how to achieve this are yet to be set out. Cancer Research UK, alongside other health charities, stress that investing in stop smoking services and national education campaigns that encourage smokers to quit will be essential, as both have had significant cuts in recent years. The new projections show around a 20-year gap in smoking rates between the least and most deprived people in England, with the richest expected to achieve smoke-free in 2025, and the poorest not reaching it until the mid-2040s.
To reach the smoke-free 2030 target, smoking rates need to drop 40 per cent faster than projected. A fixed annual charge on the tobacco industry, which would provide funding to reduce the £11 billion burden smoking related illnesses cost society in England every year, is also seen as key to achieving this. 2030 smoke-free target likely to be missed https://tinyurl.com/upajf47 READ MORE SMOKING PHARMACY Patients who have recently been discharged from hospital will now receive greater support from local pharmacy teams to manage their medicines. The Department of Health and Social Care has revealed that, from July, hospitals will be able to refer patients who would benefit from extra guidance around new prescribed medicines to their community pharmacy.
The NHS Discharge Medicines Service will help patients get the maximum benefits from new medicines they’ve been prescribed by giving them the opportunity to ask questions to pharmacists and ensuring any concerns are identified as early as possible. Forming part of the Health Secretary’s ‘Pharmacy First’ approach to ease wider pressures on A&Es and General Practice, it means that patients will be digitally referred to their pharmacy after discharge from hospital. 79 per cent of patients were prescribed at least one new medication after being discharged from hospital. Recent research by the National Institute for Health Research shows that people over 65 are less likely to be readmitted to hospital if they’re given help with their medication after discharge.
Health Secretary Matt Hancock said: “I want all patients to get the right care close to home, and to avoid any unnecessary visits to hospital. To help do that I’ve begun the Pharmacy First programme, asking pharmacies to do more to support people in the community, as they do in other countries like France. It’s good for patients and great for the NHS because it reduces pressure on GPs and hospitals.
“These new services will help strengthen what community pharmacists can do, helping interrelation with General Practice and hospitals, and help them deliver safer, more efficient patient care right across the NHS. This new contract bolsters the enhanced role highly-skilled pharmacists are playing in preventing ill health and helping us to stay well in our communities.” Pharmacy referral service to prevent readmissions https://tinyurl.com/umpjhzb READ MORE
Fire detection and emergency lighting solutions you can trust
FREE DESIGN SERVICE
Illumino Ignis specialise in the design, planning, technical assistance, commissioning, risk assessment and on-site support for all fire alarms and emergency lighting.

Whatever combination of these services you are looking for, with Illumino Ignis you will have complete peace of mind that all our products and services conform to latest legislation requirements, all tailored to each customer’s specific requirements. Failure to comply with Fire Safety Regulations can result in serious penalties. Don’t get caught out or take risks. Speak to Illumino Ignis today for expert advice.
All fire alarm and emergency lighting design and associated products comply to British and European Industry Standards BS5266, BS5839 and EN54.
DESIGN & PLANNING TECHNICAL ASSISTANCE RISK ASSESSMENT COMMISSIONING ON-SITE SUPPORT SUPPLY
0203 00 44 855 www.illuminoignis.co.uk
Service cuts prompting worries for health visitors
The Institute for Health Visiting has warned that public health budget cuts have left health visiting services unable to offer the minimum level of support in many areas. An annual survey of health visitors in England indicates that many health visitors across England have been robbed of their ability to protect vulnerable families by devastating cuts to public health budgets, leading to calls to ringfence new funding for the profession.
Official figures indicate that around one in five health visitors were lost between 2015 and 2019 – the full-time equivalent of 18 per cent of the workforce – with 48 per cent of health visitors saying they feel so stretched that they fear a tragedy where they work. The iHV State of Health Visiting survey indicates that those professionals best placed to help children get the best possible start in life lack the resources to do so. This is due to public health budget cuts and the failure to protect health visitors’ preventative role by many cashstrapped local authorities, after health visiting commissioning moved from the NHS to local authorities in 2015.
The findings also show that only 21 per cent of health visitors rated the quality of care that they can now offer families as ‘good’ or ‘excellent’, and that 29 per cent of health visitors are now responsible for between 500 and more than 1,000 children.
While in 2015, 65 per cent of health visitors were able to offer continuity of carer to all, or most, families, by 2019 that number had fallen to just 35 per cent. Continuity of carer has been shown to be greatly valued by parents and health visitors, as it allows them to build a trusting relationship and gives parents confidence to ask for help. The Institute is calling for: new ringfenced cross-government funding for early intervention and the health visiting profession; statutory protection for the health visitor role in leading the delivery of the Healthy Child Programme and for health visiting to be returned to statutory regulation; workforce modelling and a new workforce strategy for health visiting; and a new focus on improving the quality of services which health visitors can offer families, regardless of where they live.
READ MORE
https://tinyurl.com/wdye22e
SURGERY
Nurses will attend a two-year course to become ‘surgical care practitioners’, with the ability to perform procedures such as removing hernias, benign cysts and some skin cancers. According to the Daily Mail, those who qualify will also be able to assist during major surgeries such as heart bypasses and hip and knee replacements in a bid to reduce waiting times for NHS patients in increasingly busy hospitals. Surgeons currently undergo up to 16 years of training, while a surgical care practitioner is likely to have completed a three-year degree as a nurse before the two-year course. Those qualifying will also own an average of £50,000 a year, roughly twice the average nursing salary of £25,000 a year.
Critics have been quick to label the proposals, which are due to be published in the NHS’s People Plan, unveiled next month, as only a ‘sticking plaster solution’ on the serious staffing crisis within the NHS. There are already 800 surgical care practitioners working in hospitals in the UK, but leading surgeons say there will need to be ‘thousands’ before the difference to waiting times is felt.
An NHS spokesman said: “The NHS is supporting the government to deliver its pledge to deliver 50,000 more nurses. This will require a combination of training and recruiting nurses, and helping our amazing staff who may otherwise have considered leaving our health service altogether, to retrain, upskill, develop their careers and stay in the NHS.” Nurses to become ‘surgical care practitioners’
https://tinyurl.com/uyn78qf MENTAL HEALTH
Fifth of mental health patients don’t feel safe in NHS care
A new survey has revealed that one in five people did not feel safe while in the care of the NHS mental health service that treated them. The Parliamentary and Health Service Ombudsman research shows that more than half of people with mental health problems in England also said they experienced delays to their treatment, while 42 per cent said that they waited too long to be diagnosed. Despite the concerns raised by patients about their treatment in the survey, including having to wait over six months to be referred to a specialist mental health team, 48 per cent said they would be unlikely to complain if they were unhappy with the service provided. Almost 70 per cent of people said they had not been told how to complain by NHS staff.
Furthermore, 32 per cent said they did not think their complaint would be taken seriously while a quarter were worried

complaining would affect how they were treated. The main reason given was that they would not want ‘to cause trouble’. Ombudsman Rob Behrens said: “It’s unacceptable that so many patients requiring mental health treatment are left feeling unsafe in the NHS but this survey supports what we see too frequently in our casework. Patients must be supported to speak up when mistakes happen and not left scared that their treatment will be affected if they do so. While the NHS in England must continue to implement its Five Year Forward View for Mental Health, it should also look now at what more is needed to transform mental health services so the people who need them get the care they deserve.’”


NHS saves 20,000 trees by switching copier paper SAVINGS
The NHS Supply Chain has revealed that more than 200 NHS trusts have made huge environmental savings by simply switching their copier paper.
The move from A4 virgin fibre copier paper to A4 recycled paper last year saved the equivalent of: watching 85,503 hours of a plasma TV in energy; filling 161 Olympic size swimming pools with water; felling 20,000 trees in wood; and travelling 10 times around the world in an aeroplane in Co 2 . The move has also driven financial savings to the NHS. By channelling national commitment, reducing variety from two lines of paper (70gsm and 80gsm) to one (80gsm) and changing from virgin to recycled paper, £256,000 has been saved in the first year with a cost avoidance to the NHS of £1,410,000.
Martin Toomey, head of Sustainability for the NHS Supply Chain, said: “A simple switch from recycled paper has made a big difference to the environmental footprint of NHS trusts. Procurement accounts for 58 per cent of the NHS’s total carbon footprint so there’s huge potential to effect change and help the NHS to become a low anchor institution. We want to use the purchasing power of the NHS more assertively to drive change in supply chains and embed sustainability within the procurement process.”
READ MORE
https://tinyurl.com/qpzrnj4

The Care Quality Commission has stressed that action must be taken now if the NHS is to avoid an even worse winter crisis next year.
Ted Baker, hospitals chief inspector, said that the use of corridors to treat sick patients in A&E was ‘becoming normalised’, with departments struggling with a lack of staff, poor leadership and long delays leading to crowding and safety risks.
The hospitals inspectorate has carried out more than a dozen small one-day inspections of A&E departments since December where it had specific concerns about possible safety risks. It has emphasised that capacity issues traditionally reserved for the winter months were now year-round problems. July 2019 saw the highest proportion of emergency patients spending more than four hours in A&E than any previous July for at least the last five years. The CQC also warned that poor cooperation and coordination between hospitals, social care and other local organisations had ‘led to fragmented care’ in some places, something that would not be solved with a ‘quick fix’. Furthermore, A&E departments were found not to have enough nurses with the skills and qualifications to care for children, while inspectors found long delays in ambulance staff handing over patients to the A&E team were causing crowding and patients waiting in corridors. Baker said: “Our inspections are showing that this winter is proving as difficult for emergency departments as was predicted. Managing this remains a challenge but if we do not act now, we can predict that next winter will be a greater challenge still. We cannot continue this trajectory. A scenario where each winter is worse than the one before has real consequences for both patients and staff.” The latest NHS performance data showed record numbers of patients waiting on trolleys in A&E departments, with 2019 seeing the worst cancer performance by the NHS since 2016. Action needed now to avoid worst NHS winter yet https://tinyurl.com/uhk625u READ MORE WINTER CARE The latest workforce race equality data has shown that almost a third of black and minority ethnic staff in the health service have been bullied, harassed or abused by their own colleagues in the past year.
Five years after NHS England launched a drive to improve race equality, the data reflects very poorly on the health organisation, with minority ethnic staff in the NHS reporting a worsening experience as employees across four key areas. It has even raised concerns over whether the health service was ‘institutionally racist’. The data indicates that 29 per cent of BME staff reported being bullied or abused by other NHS workers, up from 27 per cent in 2016. More BME staff also reported being discriminated against by their manager, up one per cent to 15.4 per cent since 2016.
The number of BME staff who felt they have equal career progression had also fallen, alongside a rise in staff reporting abuse and bullying from patients and the public. Across England, 49 NHS trusts have a board that was comprised completely of white directors. However, the total number of BME staff at a very senior manager level has increased by 21, from 122 in 2018 to 143 in 2019. NHS treatment of minority ethnic staff highlighted https://tinyurl.com/wdd3upq READ MORE BME WALES Figures show that the number of patients spending more than 12 hours in A&E in Wales was the highest on record again in January. As in England, there was an improvement in performance against the four-hour waiting time. However, 6,882 patients faced long waits, 226 more than in December. The target is that no patient should be waiting that long. Latest official figures for January show that 66 per cent of the most serious ‘red’ calls arriving within eight minutes, meeting the target for the first time since October. Ambulance response times also improved and hit their target for the first time since October. In other positive news, 83.5 per cent of patients were waiting less than six months to start hospital treatment - the lowest proportion since December 2015 and lower than the 95 per cent target. Furthermore, the number of patients waiting longer than the target time increased for diagnostic tests but decreased for therapy services in December. A Welsh Government spokesperson said: “We acknowledge that too many people are spending long periods in emergency departments while waiting for a hospital bed, and expect the extra £40 million we made available this winter to make improvements in this area. Waiting times for scheduled care are being severely affected by doctors reducing hours because of changes to HMRC pension tax rules by the UK government. By the end of December, this had led to about 3,200 sessions lost, affecting nearly 27,000 patients. The health minister has called on the UK government to resolve this matter urgently.” Longest waiting times in Wales hit a new record https://tinyurl.com/r3v5sxg READ MORE
Putting the Patient Front and Centre



ISS Healthcare is fully supporting the current NHS Food Review and has recently published its fully updated ‘Great Food & Beverage Services Guide’ designed specifi cally around the patient, refl ecting the current advice on allergens, the new modifi ed texture diet standards and why nutrition and hydration is so important when staying in hospital. When it comes to putting the patient fi rst, you can depend upon ISS.