



INSIDE NEW LOOK DESIGN PLUS: ENERGY | FIRE SAFETY | IT | NHS STAFF SURVEY ISSUE 23.3 www.healthbusinessuk.net CAREERS TECHNOLOGY SCAN TO ENTER * *Read T&Cs for more details What has the NHS achieved and what does it mean to those who work there? CELEBRATING 75 YEARS OF THE NHS NHS 75







Brilliance 7000 27” (68.6 cm) | Mini LED | Thunderbolt 4 | 4K UHD 27B1U7903/00 MINI LED Local Dimming MiniLED with Thunderbolt docking Simply brilliant Monitors

Comment Welcome to Editor’s Comment Health Business 23.3 PUBLISHED BY PUBLIC SECTOR INFORMATION LIMITED 226 High Rd, Loughton, Essex IG10 1ET. Tel: 020 8532 0055 Web: www.psi-media.co.uk To register for your FREE Digital Subscription of Health Business magazine, go to www.healthbusinessuk.net/digital-subscription or contact Public Sector Information, 226 High Road, Loughton, Essex IG10 1ET. Tel: 020 8532 0055 www.healthbusinessuk.net P ONLINE P MOBILE P FACE-TO-FACE E 3 Issue 23.3 | HEALTH BUSINESS MAGAZINE EDITOR Polly Jones PRODUCTION MANAGER & DESIGNER Dan Kanolik PRODUCTION DESIGNER Jo Golding PRODUCTION CONTROL Deimante Gecionyte ADMINISTRATION Enkelejda Lleshaj WEB PRODUCTION Freya Courtney ADVERTISEMENT SALES Lauren McGowan, Maziar Movassagh PUBLISHER Damian Emmins GROUP PUBLISHER Karen Hopps

▶

















1948 HMT Empire Windrush arrived in others who were part of the “Windrush generation” 1948 5th July the NHS founded on the principle 1949 Labour, the Colonial Office, Nursing begin recruitment recruit staff to the NHS 1956 programme begins by the 1957 The whooping cough immunisation programme 1958 By 1958, the polio and diphtheria vaccination 1960 The first kidney transplant takes place Edinburgh 1962 The first full hip replacement is carried out at 1968 introduced 1968 The first heart transplant carried out at the National Addenbrooke’s Hospital in Cambridge 1987 Princess Diana opens Britain’s first ever purpose1987 The world’s first heart, 1986 The first lung-only transplant 1983 UK liver transplant 1980 1979 The UK heart transplant 1978 Louise Brown, the world’s first test-tube baby born 1972 CT scans begin to be used, 1988 1992 1994 1999 vaccine against Group meningococcal disease 2000 access to range of services 2006 launched for those aged 60-69, and becomes the first 2007 Hospital Leeds 2008 aged 12 2010 out to provide hearing in both ears 2012 2023 2022 George Cross by Her Majesty The Queen at Windsor Castle 2022 net zero operation at Solihull Hospital 2021 The first climate-friendly baby born in Newcastle Hospitals NHS Trust 2020 health system in the world to commit to becoming carbon 2020 programme begins 2020 Covid-19 reported in the UK and The NHS launches call 2017 NHS England announces the world’s largest single PrEP implementation trial to Contents Health Business 23.3 Contents Health Business magazine www.healthbusinessuk.net NEWS NHS 75 NHS 75 NHS 75 CAREERS HEALTHCARE ESTATES LEGIONELLA IT TECHNOLOGY FIRE SAFETY WELLBEING LOCAL GOVERNMENT VOLUNTEERING 7 13 18 23 39 31 35 42 49 55 69 75 79 89 63 ENERGY NHS STAFF SURVEY Sponsored by 5 Issue 23.3 | HEALTH BUSINESS MAGAZINE
“REACH


RELIABLE + PRACTICAL.”


6 Issue 23.3 | HEALTH BUSINESS MAGAZINE Save Time On Installation
Wireless apollo-fire.co.uk FOR MORE INFORMATION VISIT: APOLLO-FIRE.CO.UK/REACH
to make installation and commissioning quicker and easier, REACH Wireless is Apollo’s latest hybrid-wireless solution.
the QR Code to explore how REACH Wireless can make installing a new fire detection system easier than ever.
With REACH
Designed
Scan
Wireless has been designed to make extending an Apollo wired loop effortless. With an easy-to-use survey kit, REACH Wireless is FLEXIBLE +
Government announces rebuild of five hospitals
The Department of Health and Social Care has announced that five hospitals that were built using mostly reinforced autoclaved aerated concrete (RAAC) will be rebuilt by 2030 as part of the New Hospital Programme.

According to the Department, patients and staff will benefit from safe, state-of-the-art new facilities and improved care.
The government has also announced that over £20 billion is expected to be spent on new hospital infrastructure.
The hospitals included are Airedale in West Yorkshire, Queen Elizabeth King’s Lynn in Norfolk, Hinchingbrooke in Cambridgeshire, Mid Cheshire Leighton in Cheshire and Frimley Park in Surrey, all of which have significant amounts of reinforced autoclaved aerated concrete (RAAC).
RAAC is a lightweight type of concrete used to construct parts of the NHS estate in the past. However, at the end of its limited lifespan, it deteriorates significantly.


West Suffolk Hospital in Bury St Edmunds and James Paget Hospital in Norfolk, which are also affected, have already been announced in the New Hospital Programme and these are set to be prioritised.
The government has a manifesto pledge to build 40 new hospitals in England by 2030. According to the government: “Two hospitals in the New Hospital Programme are already complete and five in construction. By the end of next year more than 20 will be underway or complete.”
Health and social care secretary Steve Barclay said: “These five hospitals are in pressing need of repair and are being prioritised so patients and staff can benefit from major new hospital buildings, equipped with the latest technology.
“On top of this I’m strengthening our New Hospital Programme by today confirming that it is expected to represent more than £20 billion of new investment in hospital infrastructure.
“As we approach the 75th anniversary of our fantastic NHS, this extra investment will ensure it can care for patients for decades to come and help cut waiting lists, so they get the treatment they need quicker.”
Patients to be offered choice to cut waiting times
The Department of Health and Social Care has announced that NHS patients will be given more choice and more control over their own care.
The NHS has issued a letter to local areas stating that patients should be offered choice when clinically appropriate.

After speaking to their GP, patients will be able to view information for up to five healthcare providers including distance, waiting times and quality of care and can then make a choice on where they would like to go for care.
Research has shown that giving patients choice can cut up to three months off their waiting time by selecting a different hospital in the same region.
Amanda Pritchard, NHS chief executive, said: “By giving patients greater choice and more information about their care through the convenience of the NHS app, we can change the way people access treatment options while also building on the fantastic work already being done by NHS staff across the country in bringing down the longest waits for care.
“Despite significant pressure, the NHS reduced 18 month waits for care by more than 90 per cent by April and alongside existing tools like elective hubs, surgical robots and ‘prehab’ checks, this is another way that we are continuing to embrace the latest innovations and tech for the benefit of patients.”
Health and social care secretary Steve Barclay said: “Every patient should be able to easily choose where they go to receive treatment and today’s package will put that power in their hands...
NEW HOSPITAL PROGRAMME
CONTINUE READING READ MORE News 7 Issue 23.3 | HEALTH BUSINESS MAGAZINE
BACKLOG
Compliant with the National Standards of Healthcare Cleanliness

IOS and Android complaint
Digital operation reduces errors and operator time
Meets growing demand for digital working
We have saved over 6 days per month of resource time having the ability to auto trigger emails direct to our users, as well as now having access to key electronic data on audits being completed for ease of reporting.

New NHS App features for hospital appointments
New features in the NHS App are set to improve patient experience and support elective care recovery, while at the same time help to reduce pressure on the NHS.
The updates will give patients more direct control over their care, including management of hospital appointments. Patients will be able to see all appointments and referrals in one place in the NHS App, as well as book, change and cancel hospital appointments.
The features are currently available across 28 acute trusts in England, with more expected to join in the next few months.
The Accelerated Capability Environment (ACE) has developed the new features.



Six new community diagnostic centres to open across the UK
NHS England and the Department of Health and Social Care have announced that six new community diagnostic centres (CDCs) will open across the UK to deliver more than 500,000 diagnostic checks a year.
The new centres will join the 106 that are already in operation, which have so far delivered over 3.8 million additional tests, checks and scans since July 2021.

The CDCs are intended to cut waiting lists and offer tests, checks and scans closer to home.
North Lincolnshire CDC will be in a car park in Scunthorpe town centre, and will offer more than 146,000 additional checks a year. This will include ultrasound checks, blood tests and CT and MRI scans...
Funding announced for zeroemission ambulances

The government has announced £77 million of funding for new zero-emission vehicle projects.
It is hoped the projects will support more than 4,400 jobs across the UK over the next ten years.
The emergency services are set to benefit from new zero-emission vehicles, thanks to the HYER POWER project to develop a hydrogen fuel-cell range extender for specialist electric vehicles in demanding roles like ambulances and fire engines.
The funding has been awarded through the Advanced Propulsion Centre (APC) Collaborative Research and Development programme. £38.4 million of the investment is from the government, and £38.7 million comes from the automobile industry.

Industry and economic security minister Nusrat Ghani said: “Zero-emission cars, vans and taxis are increasingly common, but this cutting-edge work is going to mean clean, green vehicles designed and built in the UK can increasingly take on the toughest jobs too, from life-saving emergency services to haulage and public transport.
“Our automotive industry keeps setting the pace globally and seizing the potential of new technologies. Today’s multi-million-pound boost will help them stay ahead of international competition, while delivering on our priority to grow the economy and support high-quality jobs.”
DIGITAL
FLEET READ MORE CONTINUE READING News CONTINUE READING
BACKLOG 9 Issue 23.3 | HEALTH BUSINESS MAGAZINE




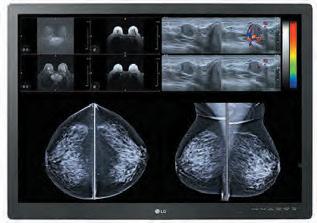
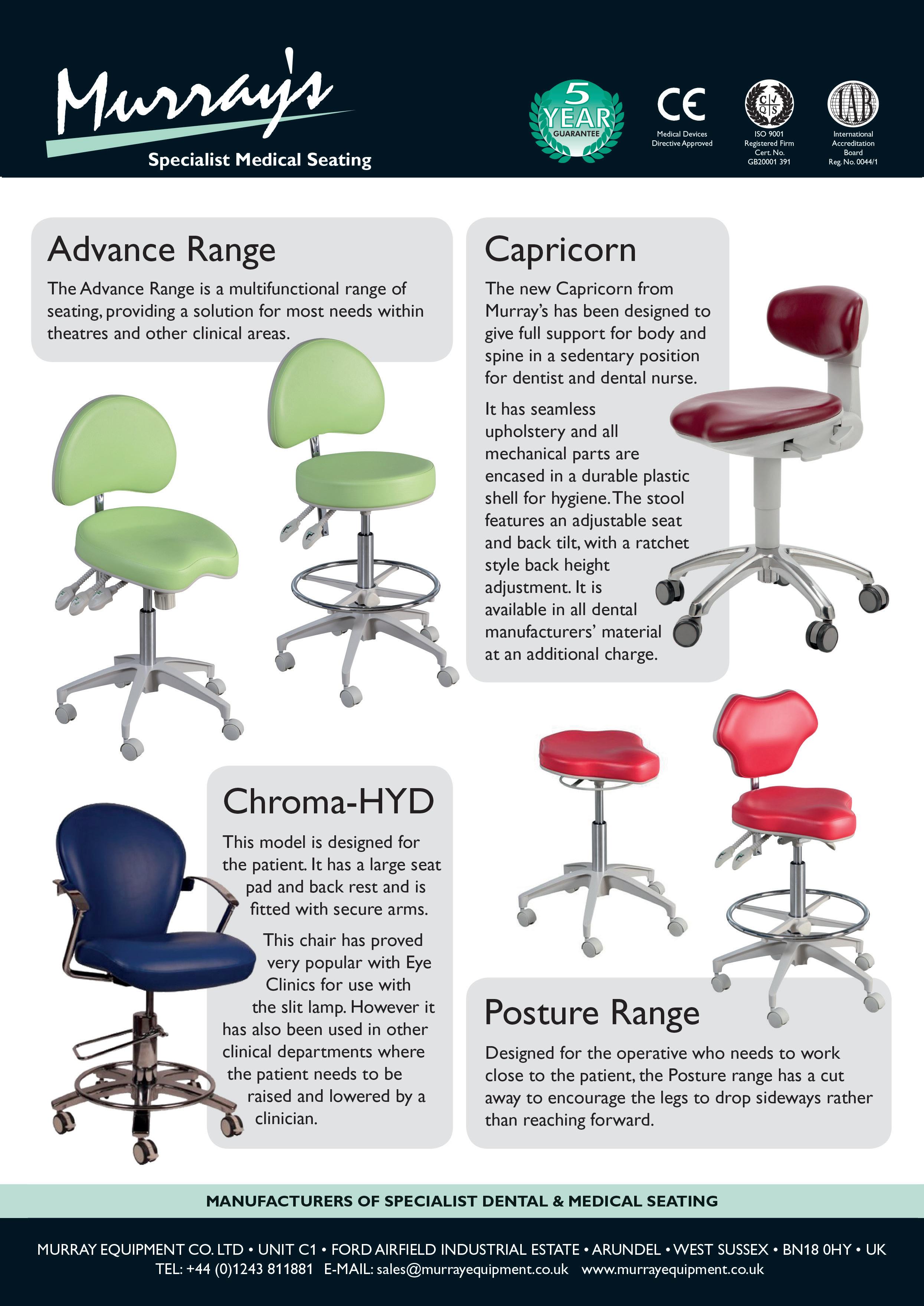
Our portfolio of surgical monitors comprises near-patient and large-screen displays for use in any surgical procedure, including the endoscopy, interventional or hybrid OR. Available in high definition or 4K ultra-high definition, and in 2D or 3D. High quality diagnostic and clinical review monitors ranging from 21” to 31.5” and up to 12MP resolution. Barco MDSC-8427 LED 27” 4K Surgical Monitor LG 32HL710S 31.5” 3G-SDI 4K Surgical Monitor LG 31HN713D 31’’ 12MP IPS Diagnostic Monitor for Mammography ...and many more. All our products and services are available now on the new NHS SBS framework Audio Visual Solutions and Integrated Operating Theatres Register to view the agreement and request access for free: https://www.sbs.nhs.uk/proc-framework-agreements-support Framework reference: SBS/18/CR/WCN/9343 0151-6750675 www.jonesav.co.uk info@jonesav.info Shop Surgical Monitors ONLINE No waiting Transparent Pricing SURGICALMONITORS.COM
UK encouraged to parkrun for the NHS

Sir Andy Murray OBE is calling on people across the country to ‘parkrun for the NHS’ to celebrate the health service’s 75th birthday and lead a more healthy and active lifestyle.
Thousands of people across the UK are expected to take part in parkrun events on Saturday 8 July and junior parkrun events on Sunday 9 July. The events are intended for for parkruns and their local communities to acknowledge the huge contribution that the NHS makes to the health of the nation. Participants are encouraged to wear NHS blue or fancy dress.
For the NHS’s 70th birthday in 2018, more than 146,000 people took park in a park run event. Participants can walk, run or jog the event. Volunteers to help run the event are also welcome.
Andy Murray said: “The NHS is one of our nation’s greatest institutions and I am honoured to support its 75th birthday. ‘Parkrun for the NHS’ is a great initiative and it’ll be amazing to see thousands of people from across the UK walking, running and volunteering at their local parkrun and junior parkrun events to mark this major milestone in the NHS’s history.
“Our nurses, doctors, paramedics, midwives and all of the other NHS staff and volunteers do an amazing job caring for us and the NHS’s 75th birthday is an opportunity to recognise their hard work and commitment. It’s also a fantastic way of encouraging more people across the UK to be active, together in the outdoors, no matter what their age, ability or background. I’d encourage everyone to head down to their local parkrun or junior parkrun and join in the 75th birthday fun...
NHS reaches record number of doctors and nurses: READ MORE
Chancellor announces life sciences growth package: READ MORE

New Heat-Health Alerting service launched: READ MORE
Online GP registrations hit 240,000: READ MORE
NHS testing pilot identifies thousands of HIV and Hepatitis cases: READ MORE
NHS England reports data breach: READ MORE
Medical device outcome registry launched: READ MORE


APPOINTMENTS
New chief executive of NHS Wales appointed
Judith Paget has been appointed as Chief Executive of NHS Wales. She had been in the post on an interim basis since November 2021. Paget was appointed after an international recruitment exercise chaired by the First Civil Service Commissioner.
Minister for health and social services, Eluned Morgan, said: “Judith has shown great leadership and oversight of the NHS in Wales through some of its most difficult times. I congratulate her on her appointment and look forward to continuing our work to deliver an NHS Wales to be proud of.”
Paget said: “I am honoured to be appointed to this important role and look forward to continuing to work with Ministers and NHS Wales organisations to deliver excellence in our health and care services.”
NHS 75 CONTINUE READING More top news stories from www.governmentbusiness.co.uk
CONTINUE READING News 11 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Revolutionising healthcare with mobile carts featuring Philips Monitors
The healthcare industry has seen a substantial shift in recent years, with digitalisation becoming increasingly vital due to the pandemic. To offer improved patient care and simplify medical processes, hospitals and medical centres are embracing technological advancements
In collaboration with Kinetic ID, a company specialising in mobility solutions such as ITintegrated carts, now more than 1000 medical carts equipped with top-quality Philips monitors have been introduced in the UK. These Kinetic-ID carts with Philips monitors are currently being utilised in numerous UK hospitals, helping to alleviate daily challenges faced by patients and healthcare professionals. Furthermore, Kinetic-ID is about to expand that reach by launching a range of patient booking kiosks, featuring Philips touchscreen monitors, which will enable patients with appointments to check-in by themselves in a quick and efficient manner. The mobile carts are designed to enhance patient experiences while streamlining medical operations. They can be used by patients and medical staff for various purposes, such as monitoring vital signs, accessing patient records, facilitating video calls with family members or serving as portable medication dispensers. Among the monitors integrated into these mobile carts is the Philips 242B9TN, a 24” touchscreen 1080p display without a base or
stand, ideal for embedding into stations like medical carts. The monitor boasts a vibrant IPS panel and 10-point projective capacitive touchscreen technology. It can be operated with a stylus or gloved fingers, and the front surface is water and dust resistant, meeting IP65 standards. With a 7H touch-glass hardness, the monitor is well-suited for the demanding healthcare environment, making it perfect for use in patient rooms, emergency rooms, and other clinical settings. The touchscreen allows healthcare professionals to effortlessly access medical records and input data without relying on a keyboard, which can be difficult to sanitise. Moreover, patients can use the touchscreen to watch movies, play games, or surf the internet, making their hospital stay more enjoyable.
Philips Monitors plays a crucial role in the healthcare industry by: Offering versatile, durable, and user-friendly technology as the sector embraces digitalisation; elevating patient care and boosting overall efficiency; providing advanced solutions like mobile carts with monitors that cater to diverse demands of healthcare professionals and patients, ensuring accessibility and user-friendliness; driving improvements in telemedicine, in-patient care, clinical workflows, and overall healthcare efficiency through their commitment to innovation; and investing in and supporting the healthcare sector to contribute to better patient care and shape the industry’s future. L
FURTHER INFORMATION philips.com/monitors
Adveretisement Feature BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 12
Celebrating the NHS at 75


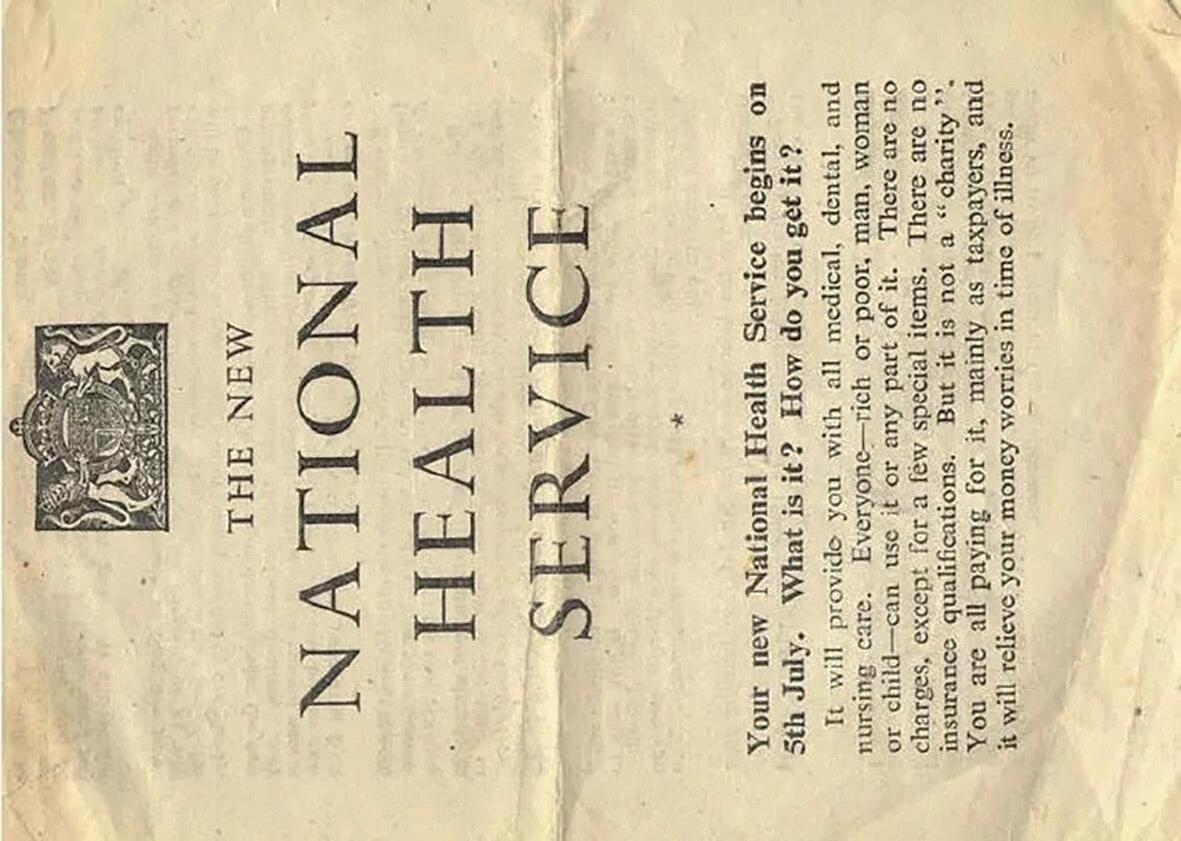
5 July 2023 marks 75 years of the NHS

In 1948, when it was founded, the NHS was the first universal health system to be available to all, free at the point of delivery. It is important to note, that 75 years later, there are still many people around the world who are not able to access free healthcare.
A lot has changed and progressed over the years, and now the NHS treats a million people a day, and 1,600 babies born every day.
Achievements
The NHS is a place of firsts: Britain’s first heart transplant in 1958, Europe’s first liver transplant in 1968, the world’s first CT scan on a patient in 1971, the world’s first test-tube baby born in 1978. Vaccination programmes also are an important part of the NHS, those which began years ago to protect against whooping cough, measles and
tuberculosis and the more recent protecting against meningitis C and Covid.
Since December 2020, the NHS has delivered 128 million vaccines as part of the NHS Vaccination Programme. According to the NHS, as of August 2021, 105,900 deaths and 24,088,000 infections have been prevented because of the NHS COVID-19 vaccination programme.
We cannot forget or underestimate what the NHS went through during the pandemic, with little to no recognition or renumeration, and the effect that this has had on staff. This should never be forgotten.
Today
Now the NHS is a world leader in adopting innovative medicines and pioneering new E

NHS 75 13 Issue 23.3 | HEALTH BUSINESS MAGAZINE

F technologies. Robotic surgery is no longer unusual, patients are routinely treated in virtual wards, we have recently seen the first new treatment for sickle cell disease in over two decades, and the 100th cancer drug was fast tracked to patients through the NHS Cancer Drugs Fund.
All of this is possible thanks to the skills, expertise and hard work of NHS staff. In August 2022, across Hospital and Community Healthcare Services, the NHS employed (fulltime equivalent): 130,398 doctors; 319,616 nurses and health visitors; 21,231 midwives; 157,098 scientific, therapeutic and technical staff; and 17,870 ambulance staff. But it’s not just the medical staff that are important. The NHS cleans an area the size of Gibraltar every day and provides up to 227 meals every minute for staff, patients, and visitors: 326,880 meals a day, the same as providing a meal to everyone in Shropshire.

Celebrations
Those who have worked in the NHS know that it is not easy, the hours are long, the pay is low, and the days can be difficult and upsetting. At the same time, you can see the enormous amount of good it does. The NHS delivers and saves lives and helps millions of people every day.
We have all been in contact with the NHS in some way, whether through receiving care or treatment or supporting loved ones through their own treatment. Every single one of us has benefitted from the NHS and we cannot take it for granted.
There has been a lot of negativity towards the NHS and particularly the staff recently, whilst many are striking for better pay and conditions. The NHS needs the support of the public and

the government to be able to continue what it is doing – that is delivering, improving and saving lives and doing so without cost to those who need the care.
On the 75th anniversary, we are celebrating and are grateful for the NHS and its staff doing what they are doing day in and day out, to the benefit of all of us. So, on the NHS’s 75th birthday, we say “congratulations”, “happy birthday” and “thank you”.
Health Business is taking part in activities and celebrations throughout the year, including this special issue of the magazine. Staff are also taking part in NHS 1000 miles and giving blood. The office will also be host to an NHS Big Tea event with all proceeds going towards NHS Charities Together. L
Find out more about the NHS’s 75th anniversary here.
FURTHER INFORMATION
NHS 75 15
Every single one of us has benefitted from the NHS and we cannot take it for granted
For over ten years, Radar Healthcare has been working with health and social care providers to help improve the quality and care of patients and residents with its all-in-one risk, quality and compliance solution. This summer we come together to celebrate one of our very treasured services, the National Health Service (NHS) who celebrate their 75 year anniversary.
In honour of this, we’ve launched #MyNHSStory. Over the next few months, we’ll be giving you the chance to share your stories and memories, as well as a host of other ways to celebrate 75 years of the NHS. Have a look at what we’ll be up to and how you can get involved at www.radarhealthcare.com/nhs-75-anniversary
ABOUT RADAR HEALTHCARE

At Radar Healthcare, we believe in making a difference. Combining digital innovation with hands-on experience in healthcare environments characterises our strategies, with the end goal always being to make healthcare safer. We’re not just selling risk, quality and compliance software, it’s the importance of care and safety. When we talk about user experience and engagement, our commitment to helping deliver our partners the best possible healthcare outcomes has been there since day one.



Compliance isn’t just ticking a box; it’s creating a safer experience. Spotting trends and analysing data isn’t just for board reporting, it’s learning how to prevent incidents and improve future outcomes. We understand the day-to-day pressures and challenges faced, which is why we are constantly evolving our software to stay on top of the latest requirements. We’re here to help healthcare providers make a real difference, now and in the future.
Risk Management
Business Compliance Action and Improvement Plans


SHARE

AND WE’LL DONATE
£75
It's time to celebrate 75 years of the Nation Health Service (NHS) and all the incredible stories that come with it! Share your #MyNHSStory with us and let's honour the amazing service that has kept our nation healthy and happy for generations. Whether you're a nurse, a doctor, a patient, or someone whose life has been touched by the NHS, we want to hear from you!
To thank you for sharing, we’re giving away £75 to a charity of the winners’ choosing - either NHS Charities Together or The Care Workers’ Charity. And that’s not all – we’ll also share your words on our social media platforms, spreading your message far and wide to inspire others to celebrate the NHS.
YOUR #NHSSTORY NEED SOM E I NSPIRATION FOR YOUR #NHSSTORY?
Entering is easy - just scan the QR code and submit your #NHSStory. Need some help getting started? Take a look at our inspiration tips and start crafting your masterpiece. Who knows, your story could be one of five winners that touch the hearts of people across the nation. Don't waitshare your #MyNHSStory today and make a difference!
SCAN TO ENTER
YOU COULD SHARE...
• Your experience of working in the NHS
• Your memories of receiving care from the NHS
• Your thoughts on the importance of the NHS
By sharing your story, you’ll be helping celebrate the 75th birthday of the NHS and all the incredible work that healthcare professionals do every day. Your story could inspire others and help raise awareness of the important role that the NHS plays in our lives.
P.S Don’t forget to follow us on social media @RadarHealthcare and use the hashtag #MyNHSStory to spread the message!
#NHS75 #NHSSTORY
*Read T&Cs for more details.
NHS turns 75: A timeline
1948
On 22 June 1948, HMT Empire Windrush arrived in the UK with 492 passengers from the West Indies. Many of those on board and others who were part of the “Windrush generation” would go on to work in the NHS
1948
On 5th July, the NHS is founded on the principle of providing healthcare services that are free for all at the point of delivery
1949
The ministries of Health and Labour, the Colonial Office, the General Nursing Council and the Royal College of Nursing begin a recruitment drive in the West Indies to recruit staff to the NHS
1956
Polio immunisation programme begins – by the end of the 1960s, polio cases had decreased significantly
1957
The whooping cough immunisation programme begins – by 1973, cases were almost zero
1987
Princess Diana opens Britain’s first ever purposebuilt AIDS ward at the Middlesex Hospital
1988
Free breast screening is introduced
1987
The world’s first heart, lung and liver transplant is carried out at Papworth Hospital in Cambridge
1992
Haemophilius influenzae type B (Hib) vaccine is introduced
1986
The first lung-only transplant in Europe is carried out at the Freeman Hospital in Newcastle
1994
The NHS Organ Donor Register is set up
1983
UK liver transplant programme begins
1999
The UK becomes first country in the world to use a vaccine against Group C meningococcal disease
2000
NHS walk-in centres are introduced to offer easy access to a range of services

2023
The NHS turns 75
2022
NHS staff are awarded the George Cross by Her Majesty The Queen at Windsor Castle
Source: https://www.england.nhs.uk/nhsbirthday/about-the-nhs-birthday/nhs-history/
2022
The NHS conducts the first net zero operation at Solihull Hospital
2021
The first climate-friendly baby is born in Newcastle Hospitals NHS Trust
NHS 75
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 18
1958
By 1958, the polio and diphtheria vaccination programmes ensured that everyone under 15 was vaccinated
1960
The first kidney transplant takes place at Edinburgh Royal Infirmary
1962
The first full hip replacement is carried out at Wrightington Hospital in Wigan
1968
The measles vaccine is introduced
1968
The first heart transplant is carried out at the National Heart Hospital in London and Europe’s first liver transplant is performed at Addenbrooke’s Hospital in Cambridge
1980
MRI scans are introduced
2006
The NHS Bowel Cancer Screening Programme is launched for those aged 60-69, and becomes the first ever screening programme to target both men and women
1979
The UK heart transplant programme begins at Papworth Hospital
2007
The first living donor in the UK donates part of his liver to his father at St James’ Hospital in Leeds
1978
Louise Brown, the world’s first test-tube baby is born
2008
The HPV vaccine is made available for all schoolgirls aged 12
1972
CT scans begin to be used, improving non-invasive diagnostics
2010
The UK’s first cochlear implant operation is carried out to provide hearing in both ears
2012
The 100,000 genomes project is announced
2020
The NHS becomes the first health system in the world to commit to becoming carbon net zero


2020
The Covid-19 vaccination programme begins
2020
The first known case of Covid-19 reported in the UK and the NHS launches a call for people to become NHS Volunteer Responders
2017
NHS England announces the world’s largest single PrEP implementation trial to prevent HIV infection
19 Issue 23.3 | HEALTH BUSINESS MAGAZINE NHS 75







We provide the TIME, RESOURCE and EXPERTISE that most in-house teams cannot justify resourcing internally. Benefits to your organisation from a review: Recoveries often provide a significant ‘unbudgeted’ windfall that can be used to fund: At the forefront of Spend Recovery Services Historical Overpayments, Supplier Overcharging and Outstanding Supplier Credits could be identified and recovered on your behalf. We take the risks around the ‘what if’ challenge for you and our recoveries demonstrate our success. VISUALISING THE INVISIBLE Spend Recovery - what could it mean to you? Jobs Treatments Essential Medicine Equipment Operations LOT 15 SPEND ANALYTICS AND RECOVERY SERVICES RM6226 DEBT RESOLUTION SERVICES FRAMEWORK twice2much.com I 0344 225 2090 I Duplicates / Overpayments: £100m Contract Compliance: £10m Statement Credits: £20m VAT: £10m ENQUIRE NOW Our Spend Recovery Reviews are carried out on a NO RECOVERY – NO FEE basis. What if ... Recoveries made to date from our reviews:
Spend Recovery Reviews to ease financial pressures
Twice2much discuss how Spend Recovery Reviews, based on a ‘share of recoveries’ only, can help ease current financial pressures
Many organisations have either not heard of Spend Recovery Reviews or do not consider that the recoveries and associated cash generated are likely to be applicable to them.

However, with so many financial pressures on every organisation as a result of the recent inflation, energy costs surges and the COVID pandemic, there has never been a more appropriate time to consider EVERY avenue for income generation. As the cost of a review is based on a ‘share of recoveries’ with no upfront costs and limited/no internal resource requirements, undertaking a review of this type should bear serious and urgent consideration.
Twice2much specialises in ‘Spend Recovery Services’ working with finance directors, accounts payable managers and heads of audit to provide a comprehensive review of accounts payable spend. Our recoveries made on behalf of clients to date demonstrate beyond doubt how we can help any client…
suppliers; and specialist expertise in reviewing supplier transactions and identifying anomalies.
Stage 2 - Verification/validation
Expert detailed analysis of transactions at individual supplier level to validate and investigate anomalies and evidence to support initial findings.
Stage 3 – Recovery/Reporting
Twice2much provide the system, processes and resources to recover the errors found on our clients’ behalf. Flexible but targeted reporting provides significant additional benefits to clients.

Who should be considering these reviews within your organisation?
Heads of audit, heads of fraud departments, heads of finance, and heads of accounts payable or procurement are the key individuals involved in considering and procuring these types of ‘specialised’ reviews.
As ‘all’ Twice2much Spend Recovery Reviews are undertaken on a ‘share of savings’ basis, they are in effect self-financing, and therefore no budget or funding is required, limiting the need for a protracted procurement exercise.
Benefits?
Recoveries from our reviews effectively represent an ‘unbudgeted financial windfall’ which can be used to directly address budgetary pressures, enable the provision of additional services and/ or fund additional resource requirements.
There are 3 stages to a Twice2much Spend Recovery review:
Stage 1 - Identification/detection
Access to £100,000’s of technology, including ‘bespoke’ analytic software and resources; access to dedicated experienced professionals; multiple-layer interrogation of transactions with
Twice2much would be happy to provide more details or discuss how we can help you generate these benefits quickly and efficiently. L
FURTHER INFORMATION
www.twice2much.com
Advertisement Feature
21 Issue 23.3 | HEALTH BUSINESS MAGAZINE
How trusts and ICSs can leverage communications Technology
Dave O’Shaughnessy, healthcare practice leader at Avaya explains how healthcare organisations can improve their communications technology

Imagine a patient management services manager concerned that the many communication channels between her hospital and its patients and primary caregivers are confusing, disjointed, and causing service delays spanning the whole organisation. She longs for a solution that unifies email addresses, phone and SMS numbers and new digital channels so that patients can communicate with a one-stop shop of healthcare services within the contact centre. Also, by enabling mobile service recording at the point of care, the organisation minimises patient data administration, which is carried out by suitable resources as opposed to medical staff. This is all entirely possible. So how can trusts and ICSs leverage communications technology to benefit patients and staff?
Rules-based triage
NHS 111 takes over 1 million calls a month That is 1 million instances in which GPs and A&Es are relieved of acting as first point of contact. This ‘outside the hospital’ approach needs emulating ‘inside the hospital.’ There is already potential for automated elements within hospital call centres, like chatbots and IVR (Interactive Voice Response) to catch the most common ‘no treatment needed’ or ‘logistical question answered’ enquiries before dialling-in an agent.
A rules-based triage, whereby the system would only ever allocate appropriate options according to myriad ‘If this then that’ conditions, would ensure
only relevant services are made available to the patient. This type of routing perfectly illustrates effective digital transformation through the connection of two or more intelligent systems which are taught to speak to one another.

Think connected
Change is a constant in the NHS. Workflows must be adaptable to how hospitals operate in the dayto-day. Open APIs (Application Programmable Interfaces) mean consultants, dev teams and IT departments can rapidly design and implement workflows as needs arise. A focus on connecting systems with communications and collaborations ensures effortless experiences for all by accelerating the introduction of new workflows and facilitating the automation of even the most rudimentary and time-consuming administrative tasks.
With the right technology partner, the patient and employee experience can be designed and integrated into a communications and collaboration solution platform. With an interoperable, highly resilient, and enterprise-grade architecture, building digital workflows to transform patient care is not only fast but frictionless, delivering experiences that ‘simply work’ for staff and patients alike. Digitalfirst experiences connect all devices and systems, empowering trusts, and ICSs to truly realise the foundational promise of digital transformation.
This quick and easy healthcare Innovation Maturity Model assessment, provides immediate recommendations to help trusts or ICSs overcome obstacles in providing first-class care and experiences for both staff and patients. L
BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
FURTHER INFORMATION www.avaya.com
Adveretisement Feature 22
Working in the NHS
HB heard from some of those working at NHSPS about their careers,
in
Janice Bentham
Estates coordinator | Joined NHS in 2008


Janice’s journey with the NHS has spanned two significant chapters in her career, reflecting her passion for making a difference in people’s lives. Janice’s initial encounter with the NHS began shortly after completing her A Levels. She joined a bustling GP Practice in Salford, a deprived area of Greater Manchester. Initially intending to work there only for the summer while awaiting her studies in Home Economics at Salford University, Janice quickly fell in love with the role. The allure of working for Good Housekeeping Magazine in the field of diet and nutrition took a back seat as she embraced her position wholeheartedly. This unexpected love for her job led her to stay for an incredible 10 years, foregoing her university plans.
In 2008, an opportunity presented itself, drawing Janice back into the NHS after
her time in facilities management. Janice joined NHSPS, bringing with her a wealth of knowledge and experience. For Janice, the best aspect of working in the NHS is the people. This encompasses both the colleagues she collaborates with and the individuals she serves through her work. The opportunity to make a positive impact on people’s lives is a rewarding and fulfilling experience that motivates Janice every day.
Throughout her journey in the NHS, Janice has learned valuable lessons. She emphasises the importance of listening to others, practicing patience, and treating individuals with the same kindness and respect she would expect for herself. Over the years, Janice has witnessed substantial changes within the NHS. From the absence of computers when she first started to the current emphasis on customer service and improving patient care, the evolution has been E
NHS 75 23 Issue 23.3 | HEALTH BUSINESS MAGAZINE
what has changed since they started and what working
the NHS means to them
MAINTENANCE
FREE means
HYGIENIC AND EASY TO CLEAN
Prevent everyday wear and tear with Yeoman Shield’s extensive range of easy-clean, wall and door protection.
Our attractive, maintenance free, hygienic products protect healthcare environments from costly impact damage, making repainting and repair a thing of the past.


Blending with decors, and available in primary dementia-friendly colours, our designs can include signage, to promote the well-being of patients and aid wayfinding.
For more information call 0113 279 5854 or email info@yeomanshield.com
cost effective wall and door protection www.yeomanshield.com
F profound. Within NHSPS, the focus has shifted beyond bricks and mortar to understanding how the condition of buildings impacts patient care and the delivery of services by the wider NHS.

The NHS holds a special place in Janice’s heart. As a user of NHS services herself, she deeply appreciates its accessibility and availability. Whether picking up the phone or walking down the high street, the NHS is always there, offering support during life’s most challenging times. Janice believes in making the NHS the best it can be through the collective efforts of individuals in their daily lives, ensuring exceptional care for all.
Matt Willis
Chef | 20 Years in the NHS
Matt’s journey with the NHS began unexpectedly. After a period of unemployment, he seized an opportunity through an agency and found himself at Clacton Hospital, ready to contribute to the team. Recognising his talent and dedication, the hospital offered him a contract as a pot wash boy, which became the stepping stone for him to pursue his passion for cooking and become a self-taught chef.
When asked about his favourite aspect of working for the NHS, Matt’s answer is clear: bringing smiles to patients’ faces and ensuring their hospital stay is as pleasant as possible. Through his culinary creations, he has the privilege of making a positive impact on patients’ lives. Matt cherishes the heartwarming moments when patients light up with joy, particularly on special occasions like Christmas, where he takes pride in preparing a delicious roast turkey meal.
Reflecting on the changes he has witnessed since joining the NHS, Matt highlights the
profound impact of the pandemic. The outbreak of Covid-19 emphasised the importance of maintaining rigorous cleanliness and adhering to strict procedures.
Notably, Matt achieved a personal goal he had nurtured since his early teens - acquiring his own chef’s jacket. His self-taught journey paved the way for him to become the first-ever chef apprentice in NHSPS. Currently, he is on track to successfully complete his apprenticeship this September.
The NHS holds immense significance in Matt’s life, extending beyond his professional endeavours. His family shares a deep connection with the NHS, as both his sisters are dedicated healthcare professionals, his mother works as a receptionist at a GP surgery, and his mother-in-law serves as a nurse in the community. Furthermore, the NHS has played a vital role in saving the lives of his loved ones, including his brother and nephew who E

NHS 75 25
His self-taught journey paved the way for him to become the first-ever chef apprentice in NHSPS






Read our whitepaper on how Powerstar supports NHS Trusts and healthcare providers to balance their energy priorities.
F overcame meningitis, and another nephew who triumphed over serious complications at birth. For Matt, the NHS symbolises an invaluable service that has positively impacted countless lives throughout the country.
Celebrating 50 years at the NHS Meet NHSPS chef, Irene Wallace, the Lancashire lass who simply can’t leave “In June this year, I’ll have worked for the NHS for 50 years. It’s a long time at the same company.

“I’m a chef at Longridge Community Hospital in Preston. I’m so lucky to have found my niche and was able to have a happy working life.
“These days I only work on Mondays, though I sometimes stand in for colleagues. I still love it –especially the baking!
“I started off as a kitchen assistant in a small psychiatric hospital. I heard about the vacancy, applied, and got the job. That’s how it happened then; it’s different now. I worked part-

time because of my two young boys. (We had childcare issues back then too!)
“I officially retired in 2001 aged 62. (Now you’ll be able to work out my age!) I had a huge party and they even wrote about me in the local rag.
But I just couldn’t leave. I said I’d go when I was 70. Then at 80. I suppose it’ll have to be 90 now! Every winter I say I’ll leave in the spring, so I can do more gardening and DIY. But spring comes and goes, and I’m still here.
“I’m blessed to be healthy and happy at 84 and still being useful in the workplace. But when I feel I can’t keep up, I’ll leave. I’m forthright and speak my mind. But I don’t think I’ve ever offended anyone. I’ve got on with everyone.
Why do I love the NHS? I suppose it’s all about the people. It’s always been like family to me. It’s given me a job I’ve been happy to go to every single day. I’ve made lifelong friends and I’ve learnt so much: things like tolerance, patience, and kindness.
“My NHSPS family calls me ‘Mum’, so I suppose I am a bit of a matriarch! (At least they don’t call me Grandma – even though I’ve got four grandchildren and two great grandchildren!)
I’ve never met any stars, royalty, or had any glittering career highlights. There’s no celebrity chef I look up to, or fancy cookbook I want to own. You may think my journey has been ordinary. That’s not the case.
“I can say that I’ve done my best. No one can do more than that. I’ve never shied away from hard work or clock watched. I’ve put my head down and contributed in my own small, but honest, way.
“So much has changed over 50 years. Everything has changed. And I’ve been a part of that. I’m as proud of the NHS/NHSPS today as I was when I started.” L
NHS 75
Why do I love the NHS? I suppose it’s all about the people. It’s always been like family to me.
27 Issue 23.3 | HEALTH BUSINESS MAGAZINE


When every message counts Multitone provide rapid, reliable, secure communications technologies to customers worldwide. With our suite of hardware, software and apps, we can deliver bespoke integration, automation and communications systems that make workplaces safer, more efficient and more resilient - with great results for the people that work in them and for the people that rely on them. Visit multitone.com/solutions/ to find out more. info@multitone.com | +44 (0)1256 320 292
Multitone and the NHS: a shared journey based on values, knowledge and experience
From the world’s first bleep paging system developed in partnership with St Thomas’ Hospital, through to cloud-based messaging solutions, Multitone has been a key partner to the NHS throughout its 75-year history
worker employees. Multitone’s award-winning EkoTek Staff Safety Solution is a good example, allowing employees to discreetly summon immediate assistance to their location at the touch of a button, should they feel unwell or unsafe.
Helping the NHS to meet the challenges of today
The UK’s healthcare needs and its society are changing. This requires the NHS to evolve further, to meet these new challenges and use its resources in more efficient and innovative ways. As the acceleration in the digital transformation gathers pace, Multitone is a partner within the NHS SBS Patient/Citizen Communications and Engagement Solutions Framework and is creating new leading-edge solutions and adapting existing ones to meet the demands of the adapting market, including:
Secure digital communications for the mid-2020s and beyond . Hospitals are upgrading their critical communications and building local resilience within their network systems. Multitone is working with many healthcare providers to replace legacy systems with the latest state-of-the-art digital technology such as the Multitone critical messaging platform and critical smart apps.
Protecting employees . Increasingly, employees in the NHS are working throughout the community as well as in various locations on healthcare sites. Multitone is using its technological expertise and experience to adapt solutions to support the needs of lone
Better patient care . Multitone’s innovative EkoCare nurse call solution for care homes, nursing homes and hospitals ensures that whether residents or patients are in bed or mobile, they can get help as quickly as possible at the push of a button.
Secure and robust infrastructure . The NHS and other organisations face multiple threats of hardware failure, internet outage, power cuts, cyber-crime, workplace floods, fires, and vandalism. Multitone’s Hybrid Cloud Service solution is providing almost certain continuity of critical communications for organisations across the UK.
Celebrating the NHS’s 75th –and looking to the future
Multitone is proud of its very special, deeprooted relationship with the NHS, which is based on values, experience, knowledge of what the organisation needs and how the organisation works. The team at Multitone congratulates the NHS on its 75th anniversary and looks forward to helping the service move forward as it evolves well into the future. L
Advertisement Feature
FURTHER INFORMATION www.multitone.com
29 Issue 23.3 | HEALTH BUSINESS MAGAZINE










BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net DOWNLOAD HERE 500K+ downloads 1 2K r ti (UK) Visit: www brainsparkerapp com Email: hello@brainsparker.com Call: 0207-096-1469 Unlock Innovation in Healthcare √ CREATIVE BRAINSTORMING TOOL √ BOOST PROBLEM-SOLVING SKILLS √ GENERATE BREAKTHROUGH IDEAS √ UPSKILL WITH BITE-SIZED TRAINING 30 www.glasdon.com Designs for a Cleaner, Safer & More Sustainable Environment GW655 Health Business Magazine Advert FINAL 2.23.indd 1 23/02/2023 15:26:11
Volunteers can help to tackle NHS staff burnout

The findings of NHS England’s latest annual staff survey are stark. Nearly three-quarters of NHS workers (73.6 per cent) said there aren’t enough staff at their organisation to do their job properly. Almost a fifth (17.3 per cent) said they will leave the NHS as soon as they find another job. Substantially less than half (42.9 per cent) said they’re able to meet all the conflicting demands on their time at work.

In the wake of the Covid-19 pandemic and a decade of cuts, the nation’s public sector health professionals are completely, and understandably, burnt out. With 124,000 vacant posts, including over 40,000 vacancies in nursing, and an unprecedented wave of industrial action over pay and conditions, morale is extremely low. The pressure on staff, however, remains unabated, with 7.2 million people waiting for routine operations at the last count.
Volunteers as a solution
Volunteers are one part of the solution to this huge problem. They can relieve the pressure
on staff and give them some breathing space by providing non-clinical care to patients. At Helpforce – a charity that partners with health and care organisations to transform the delivery of volunteer services – our work on-the-ground proves that volunteers are hugely beneficial for both healthcare staff and their patients.
Our Back to Health campaign aims to help one million people obtain more support in hospitals, their communities and at home, with the help of volunteers. Through the campaign, volunteers have already supported just under 40,000 NHS staff and nearly 60,000 patients. Statistics from the campaign provide strong evidence that volunteers free up clinical staff’s time. In fact, our research shows that 79 per cent of the NHS staff involved in this campaign believe volunteers improve their working lives.
Variety of tasks
Volunteers can help at every stage of a patient’s health and care journey and therefore, can relieve pressure on frontline staff as a result. E
Volunteering 31 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Mark Lever, CEO of Helpforce, explains how volunteers can be a helpful addition to the NHS workforce
F They provide practical support at home to people on waiting lists through giving them check-in phone calls, sharing with them useful information to prepare for their treatment, so that their appointments at the hospital can go smoothly. In hospitals, they can do pharmacy runs, deliver lab samples, help patients to move wards or stock up PPE cupboards, all can help staff from leaving their posts so they can focus on their patients or have breaks. Our research shows that by carrying out these in-hospital tasks, volunteers could save staff significant amounts of time – up to 93 minutes per interaction . As a result, 94 per cent of staff agree that volunteers support them to feel less stressed when they’re busy. Moreover, volunteers can also free up staff by helping patients with their meals and hydration needs. By ensuring they have enough food and water, they can help them recover more quickly. They are also able to offer companionship to patients who don’t have their own support network. By adding value to patients’ care in this way, volunteers help reassure clinical staff that patients and their families have the right support, giving them peace of mind. Meanwhile, they can focus on other priorities.
Back to Health campaign
For the Back to Health campaign, Helpforce has partnered with 45 organisations to design innovative volunteering roles that not only
make a big impact on patients, but also on staff. These include Emergency Department Response Volunteers, Falls Prevention Volunteers, Hand Holding Volunteers, Restraint Debrief Volunteers, Baby Clinic Volunteers, Dementia Volunteers and many others.
When it’s time for a hospital patient to go home, volunteers are especially useful. They can pick up people’s medication, help get them home and settle them back into their surroundings. Our research shows that their support speeds up the discharge process by 44 minutes. This undoubtedly eases pressure on staff.

Post-discharge, they can knit people into their community, by connecting them with local services, like physiotherapy or speech therapy. If patients receive support at home, they’re less likely to experience loneliness and social isolation, which could put them at greater risk of cognitive and physical decline. Emotional wellbeing is critical to physical recovery. Indeed, loneliness, in conjunction with living alone and poor social connections, is as bad for health as smoking 15 cigarettes a day. It is also linked to heightened risk of hospital admission , which means volunteers can help patients to avoid being readmitted – once again reducing the pressure on NHS staff.
Volunteer to career
Trained and experienced volunteers can also end up becoming NHS staff members, helping to fill vacancies and ease staff shortages. As a case in point, we run the Volunteer to Career programme , as part of our Back to Health campaign. It helps NHS recruitment and staffing levels by identifying pathways for volunteers to develop their careers in health and care. What makes the programme stand out is that the volunteers receive focussed support from workforce and clinical leads. They not only benefit from first-hand experience of working in the health and care environment – but also the right clinical, wellbeing and career support. Emerging results from the programme have shown that 73 per cent of volunteers who took
Volunteering
32 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
Volunteers help reassure clinical staff that patients and their families have the right support, giving them peace of mind
part in the programme secured a paid job or accessed further education in health and care. Clinical staff consistently tell us that they value volunteers’ contributions. As just one example, Muna Abdullahi, the lead pharmacy technician in Clinical Services & Operations Pharmacy Department at Moorfields Eye Hospital, London, said, “We can’t thank the volunteers enough for everything they have and continue to do. I want them to know we value and appreciate them and consider them part of our team.”
Positive feedback
After the successful implementation of the Response Volunteer service, Kristine Davies, head of Voluntary Services at the University Hospitals Coventry and Warwickshire NHS Trust, commented: “Within the first seven weeks of the service we can already see what an impact the Response Volunteers are having. We couldn’t have made this happen without the engagement from our clinical staff to help us to design the role and to train and support the volunteers. The staff are extremely grateful for the volunteers’ time and have felt that the volunteers have made a significant impact and are part of their team.”
Call to action
As NHS England’s staff survey attests, our public healthcare workers are at breaking point. While renowned for their high standards and compassionate care, the NHS’ professional health and social care teams are now stretched
to their limits. Record staff shortages are a burden they are struggling to bear. Morale is declining. An alarming number of essential staff are considering leaving to find less stressful employment elsewhere. We must do everything we can to stop this happening. We need to turn this situation around.
Healthcare staff’s stress and workloads could be eased by volunteer assistance, allowing them to focus on more urgent clinical care. In health and care, volunteering is a proven, yet massively underused, asset. Embedding volunteers into NHS services makes them more effective and resilient. And the will is there. As was demonstrated during the Covid19 pandemic, local communities are keen to support their NHS trusts. They want to help and many services stand to benefit.
What is stopping us from realising this potential?
We need the government, local authorities, health and care leaders, charities and community organisations to work together to put in place well-designed and properly managed volunteer initiatives. Only then will we unlock the huge potential of volunteers for people across the UK – and make a significant difference to reducing the incredible pressures on our NHS staff. L
https://helpforce.community/
FURTHER INFORMATION Volunteering
E33
P2 BY PINPOINT AVAILABLE NOW



Lee Smith, head of Cove Healthcare: “I’ve worked with all manner of safety systems, but none of them come anywhere near Pinpoint.”

34 Issue 23.3 | HEALTH BUSINESS MAGAZINE
AWARDWINNING STAFF SAFETY SYSTEMS
YOU
pinpointlimited www.pinpointlimited.com @PinpointLimited
PINPOINT’S
PROVIDE
WITH THE SAFEST ENVIRONMENT FOR YOUR STAFF.
High performance, effective and simple to use staff safety systems that enable your employees to call for assistance or emergency in any situation.
Looking ahead: NHS Staff Survey, a call to action
Chris Graham, CEO of Picker, a not-for-profit research charity working across health and social care, which helped to carry out the recent NHS staff survey, explains some of the results
Employee experience is an issue of increasing importance for employers. Studies across a variety of sectors have shown links between workforce experience and organisational success, creating a robust business case – as well as a clear moral case – for ensuring that individuals have positive experiences of work. Better employee experience is associated with higher engagement, productivity, and retention, as well as wider outcomes.
The NHS in England is frequently cited as one of the world’s largest employers. Indeed, its workforce numbers some 1.5 million people –more than one in thirty of all working age adults in England – and staffing accounts for the lion’s share of the service’s expenditure. It’s fitting, then, that the NHS can call itself a global leader on measuring and reporting staff experience.
The annual NHS Staff Survey, overseen by NHS England and coordinated on their behalf by Picker, is the largest published workforce survey in the world, now attracting more than 600,000 responses each year. Detailed results are available at national and local levels, along with a set of interactive dashboards. It is a remarkable and highly transparent collection that provides detailed evidence about the experiences of people working in the NHS.
The 2022 NHS Staff Survey
Results from the 2022 NHS Staff Survey were published earlier this year. The survey was conducted mainly in October and November 2022, prior to the current rounds of industrial action – but nevertheless in the context
of significant pressures on the workforce. There has been extensive discussion of the challenges the service faces around staffing levels, with high rates of vacancy in some key areas such as midwifery, and in dealing with an unprecedented backlog of care following the COVID pandemic.
Given the wider context, many readers will have jumped straight to the question on staff satisfaction with pay. Unsurprisingly, this had declined – only 26 per cent were satisfied with their pay in 2022, compared to 33 per cent in 2021 and 37 per cent in 2020. But in some ways, this is one of the less illuminating findings to be gleaned from a survey that includes more than one hundred questions and that allows significant disaggregation of data. After all, you don’t need a survey to tell you that staff are dissatisfied with pay when the same staff are on strike over their salaries.

Elsewhere, results from the survey show the quality of staff experience largely holding E

NHS Staff Survey
35 Issue 23.3 | HEALTH BUSINESS MAGAZINE
F steady since 2021, when results had fallen in many areas after the pandemic. Two thirds of staff (67 per cent) agreed that they were “enthusiastic about their job” and, as in 2021, slightly more than half (53 per cent) said that they look forward to going to work. Some of the most positive results were about teamworking: in many organisations, there seems to be a sense of camaraderie that supports working culture. There were also some encouraging signs of improvement in certain problem areas from the 2021 survey. For example, the proportion of staff who had felt unwell due to work related stress in the past year fell from 47 per cent to 45 per cent: still a worryingly high proportion, but a positive development in light of wider pressures. Despite these findings, one change stood out as particularly concerning. There was a steep drop in the proportion of staff who said that they are happy with the standard of care provided by their own organisation, which fell to 63 per cent in 2022 from 68 per cent in 2021, having peaked at 74 per cent during the first year of the COVID pandemic. By the standards of a survey of this scale, where question level results typically move by only one or two percentage points each year, this is an alarming drop.
A crisis of faith?
Back in 1992, the recently late Nigel Lawson remarked with evident frustration that “the NHS is the closest thing the English have to a religion, with those who practise it regarding themselves as a priesthood”. If that were to
be read literally, we might choose to interpret this finding about satisfaction with standards of care as indicating a collective crisis of faith –especially as confidence is lower still amongst front line staff, including doctors and nurses. Personally I find this rather too reactionary a viewpoint. The vast majority of NHS staff (87 per cent) still believe that their role makes a difference to patients and that patient care is their employer’s top priority (74 per cent). And although headlines have highlighted the finding that almost a third of staff (32 per cent) “often think about leaving” their organisation, the more detailed results suggest that a far smaller proportion of staff actively wish to leave the NHS as a whole.
Instead, we might look at staff experience as a bellwether of patient experience and clinical quality across the service. Perhaps unsurprisingly, there is good evidence that staff wellbeing should be seen as an antecedent of patient experience. If staff are reporting concerns about the standard of care in their organisations, then employers must take these concerns seriously; work with their staff to understand the causes for their concerns; and commit to doing what they can to remedy them.
Improving staff experiences

Despite the huge scale and scope of the NHS Staff Survey, it should be seen as simply one part of the puzzle of understanding and improving staff experience. Analysis of organisational results will allow employers to understand the areas of workforce experience where they have the greatest challenges, and to assess how they are progressing against their own people plans and staffing strategies. But the causes of problems, and their remedies, may resist simple explanations.
It would be all too easy to write off poor staff experience within an NHS organisation as a consequence of essentially external factors that are beyond local control. Dissatisfaction with pay is a national issue, subject to collective bargaining and agreement; similarly, the towering elective care backlog is best viewed as a consequence of whole system pressures following the pandemic. But such a simplistic reading of the complex causes of staff experience would serve only to negate organisations’ own agency in determining working conditions, workforce wellbeing, and wider outcomes.
In fact, the range of results for organisations within each sector – acute trusts, ambulance
NHS Staff Survey
36
issue
trusts, and so on – shows how variable workforce experience can be within different NHS employers and, by extension, indicates how much influence local employment practice does have. All employers would therefore be well advised to engage with their workforces to explore the detailed local factors contributing to staff experience, and to understand that changes that could be made that would have the greatest impact on improving people’s experiences. The range of results also provides opportunities for good practice to be shared and spread. With more than 200 organisations participating in the survey, NHS employers with specific challenges can often find a peer who has worked through the same issue. At Picker, we hold national workshop events each year to bring together organisations and we have seen first hand how this can help catalyse innovation.
Looking to the future
As an annual survey, the NHS Staff Survey can be relied upon to provide a robust timeline of data on workforce experience in the health service. This enables organisations to evaluate the success of their organisational development activities and test whether the changes they make are improving people’s work experiences. But it’s important to be realistic: meaningful change often takes time, and demands a strategic approach.
The best advice for organisations looking to improve workforce experience is, therefore, to create a strategic plan that is rooted in good
evidence about staff experience; to maintain this, taking a continuous improvement approach to building on change; and to critically evaluate progress over time. By retaining a strategic focus on improving staff experience, employers can demonstrate how they value their staff and continue to provide high quality care to those who need it most. L
About the author
ChrishasbeenPicker’sCEOsince2017,leadingthe organisationaswellascontributingtoitsresearch andpractice.
PriortobecomingCEO,ChrisledPicker’sresearch divisionfrom2011to2016.Inthispost,hewas responsibleforoverseeingthedevelopmentand coordinationoflarge-scaleresearchandevaluation projects,includingtheNHSPatientandStaff SurveyCoordinationCentres,runonbehalfofthe CareQualityCommission(CQC)andNHSEngland, respectively.HehasalsoworkedattheCQCandits predecessor,theHealthcareCommission,aswellas undertakingotherrolesatPickerfrom2004to2007. Chrishasparticularinterestsinpersoncentredcareandinresearchonstaff,patient,anduser experiencesofhealthandcare.Hehasundertaken researchandwrittenwidelyonthesesubjects.Chris readExperimentalPsychologyatPembrokeCollege, UniversityofOxford.
The results of the NHS staff survey are available here.

FURTHER INFORMATION
NHS
Staff Survey
37 Issue 23.3 | HEALTH BUSINESS MAGAZINE
NHS employers with specific challenges can often find a peer who has worked through the same
Drive change in healthcare through innovation

Managers working in the fast-evolving healthcare sector must wrestle with daily challenges caused by budget constraints, increased demand for services, workforce shortages, and rapid technological advancements. Creative thinking is crucial for overcoming these obstacles and continuing to deliver services that enhance patient care and community service
can empower their team members to come up with their own solutions to solve problems.
Organise cross-functional brainstorming sessions:
Facilitate brainstorming sessions between departments using interactive tools like the brainsparker app, which has thousands of random prompt cards designed to trigger fresh thinking and new ideas. Other tools like whiteboards, sticky notes, and mind maps help team members visualise and organise their ideas.

Here are five ways that healthcare managers can unlock innovative thinking in their teams:
Foster open communication: Create an environment where team members feel comfortable sharing ideas without fear of criticism. Encourage open dialogue and value everyone’s input, irrespective of their position or seniority. This atmosphere of trust and openness encourages a collaborative approach to problem-solving and can lead to unexpected insights.
Establish an idea-sharing forum. Set up suggestion boxes or chat rooms where team members can submit their ideas for consideration. This approach can foster a sense of ownership in improving service delivery and generate a wealth of potential solutions to overcome daily challenges.
Implement the GROW coaching model: Utilize the GROW coaching model (Goal, Reality, Options, and Way Forward) to help team members clarify their goals, assess the current situation, explore different options, and identify action steps. With this structured approach, managers
Encourage continuous learning: Provide opportunities for team members to learn and develop their creative thinking skills by offering training programs, workshops, or access to online courses. Encouraging continuous learning helps team members stay current with industry trends and develop the essential problem-solving skills they need for today and in the future.
Conclusion
In a world where change is the only constant, healthcare managers who champion creative thinking will empower their teams to overcome obstacles, drive positive change, and ensure the successful delivery of essential services to the communities they serve. By implementing strategies such as open communication, idea-sharing forums, the GROW coaching model, cross-functional brainstorming sessions, and continuous learning, healthcare managers and their teams can enhance patient care and community services. L
38 38 Issue 23.3 | HEALTH BUSINESS MAGAZINE BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
FURTHER INFORMATION https://www.linkedin.com/in/ gabriellagoddardinnovation/ www.brainsparkerapp.com
Adveretisement Feature
Gabriella Goddard is the CEO & Coaching Director at Brainsparker Ltd.
Tech careers in the NHS: addressing the gender gap

Roslyn Churchill, chief information officer, NHS Property Services (NHSPS) explores how to overcome the gender gap in NHS tech careers
Women make up 75 per cent of all NHS staff from clinicians, porters to admin roles and senior positions. The NHS is one of the largest employers of women in the world. However, figures show that in health technology specifically, only one woman in five people are working in the industry.
The COVID-19 pandemic has merely exacerbated this issue. In 2021, the Institute of Coding (IoC) has estimated the UK alone needs at least 1.5 million people with advanced computer science and data skills. With the current graduate pool being around 28,000 in this field, there is an urgent need to address this gap, as it is only going to grow.
What can be done to make up this gap?
Having a more diverse workforce – we need to be introducing more training and compulsory classes at an education level. Traditionally, computer science has always been seen as a man’s job. While this perception is slowly changing, and we are seeing more girls and women becoming interested in computer
science and data, much more needs to be done to not only encourage women into embarking on this career path, but also empower them to stay on and flourish.
Addressing the gender gap challenge
Having been an executive director in my organisation for over four years, my passion for data and technology is just as strong as it was when I studied IT at school. But technological advancements have skyrocketed since I first ventured into the field rather naively.
Women are still under-recruited, underretained and under-promoted, which is contributing to the widening technology skills gap. We are now in an age where digital data has become the essence of what we do, and with the continuous evolution in digital technology, we need to consider how information can be used to our advantage in all aspects of healthcare.
For digital transformation in healthcare to be truly successful, we need digital inclusion. E
Careers 39 Issue 23.3 | HEALTH BUSINESS MAGAZINE
F Women must be at the heart of healthcare technology, as their inclusion, perspective and experience can help improve patient outcomes. With existing technologies and data processes still heavily biased against women, having more women working in data and technology can help address this, as well as help tackle broader issues such as health inequalities.
Featuring role models
An important way to address the gender gap in healthcare technology is showcasing women who are already working in it, particularly spotlighting those who are in leadership positions. This can come from women networks within an organisation, networking events dedicated to women in tech, and mentoring programmes. It is crucial that we normalise the notion that women can be at the forefront of this sector and especially in leadership roles alongside men.
Research has shown that a ‘maternal-style’ leadership, which embraces an empathetic, open and caring approach to leadership, has led to higher levels of job satisfaction, staff retention, as well as improved company culture. By having different approaches in leadership, particularly one that allows employees to be more open and feel safe to do so, it can also help address the gender gap. Over my 20-year career, I must admit that I am proud to be working for an organisation that is truly walking the walk when it comes to improving diversity in digital and data. As of
2022, over 35 per cent of digital and data roles at NHS Property Services (NHSPS) are filled by women, a significant increase from 2018 when this figure was only 5 per cent. We have also improved representation of women in senior levels, with 80 per cent of senior technical roles now being undertaken by women.

Transforming health estates for the better
Data intelligence is becoming much more important and has become lifeblood of the healthcare setting. Looking at health estates specifically, we have data intelligence within the digital and data team and leverage these insights to inform the business on how our buildings are utilised and run, and therefore the strategies that can improve the way we manage the health estate.
By having that visibility, we have a more proactive approach to monitoring the health of our workforce. For example, many of the services that NHSPS support have women at the centre of their operations – social prescribing sites, community centres, childcare hubs and more. To ensure that our buildings are fit for purpose, we must have precise data on the needs of the women and people who use these facilities, how they are using them, and any areas for improvement. More importantly, we need to be able to interpret and analyse this data and turn insights into meaningful actions to improve the health and wellbeing of our site users. Having
Careers
40
It is crucial that we normalise the notion that women can be at the forefront of this sector
a diverse team on the ground and in the data teams will be critical to making this a success. To support the NHS now and in the future, we have to stay at pace with the ever-changing life cycle of technology. Beyond the usual constant upgrades and replacements, we need to look at our workforce and come up with tangible ways to ensure that they are equipped with the skills needed to keep up with these rapid changes. Having more women and diversity generally will be a critical component to this. By focussing on strategic investments in digital and data technologies, as well as solid training and recruitment, the NHS’ continuous change in a time of uncertainty, adapting and influencing to be able to deliver the quality of services that we continue to provide for the benefit of patients. L


About the author
Roslynisaccountableforthedigital,technologyand datastrategyandenablementthroughdeliveringto NHSPSplans.Roslynbringssignificanttechnology andpropertyexperiencetotherole,aswellasa strongtrackrecordofdirectingcomplex,operational environments.Shehasover20yearsofexperience deliveringstrategictransformationandsolutionsand hasakeeninterestincontinuousimprovementto meettheevolvingneedsofthebusiness.
Careers 41
Social enterprise backs call for free period products for NHS staff
A leading social enterprise is uniting with NHS staff across the country to raise awareness of period poverty in the healthcare sector
Musselburgh-based not-for-profit Hey Girls has made it their mission to raise awareness of the growing issue, which has worsened since the start of the cost-of-living crisis. The multi-award-winning social enterprise donates a box of period products to good causes for every one purchased by its corporate
and public sector partners, and currently works with hospitals, clinics and other healthcare units across almost 30 trusts nationwide. Its team work with organisations throughout the UK in introducing period dignity schemes, although no challenge is as unique as the NHS.
Long hours
Georgie Nicholson, contracts and partnerships manager at Hey Girls, was first approached by two nurses in Scotland looking for support, and has since helped build a strong sense of community among NHS staff raising awareness about the everyday struggles they face.
“Periods don’t stop for anything,” Georgie said. “It doesn’t matter where you are or what you’re doing. And in high-pressure jobs like in healthcare, where you need to remain constantly alert, your period unexpectedly starting can be incredibly stressful.
“That is especially true in fields like surgery, where we have heard stories of staff having to ‘double up’ or bleed through their scrubs for up to 12 hours as they have no other alternative.
“NHS staff aren’t robots, and while they continue to perform like superheroes under increased pressure – they are human beings.
“And they are human beings who through their devotion to caring for others, often overlook their own needs, health and wellbeing. And it shouldn’t have to be that way.”
Talking to staff
But the problem is not unique to those working in theatre. The sheer size and scale of hospitals, tied in with the constant demand for patient care, means it can be incredibly difficult for staff to access products when they need them.

Wellbeing 42
That reality has rung true in Georgie’s travels across the country, where conversations are beginning to grow among staff.
Georgie added: “We have heard similar messages from NHS staff nationwide – and that is that they often feel unseen and unheard.
“At every event we visit, we always ask attendees to raise their hands if they have ever been caught short while at work and not had access to period products.
“In our multiple talks with healthcare staff, everyone has raised their hand – and every time you can see the shock on people’s faces as they suddenly realise they are not alone.
“It is so important we have those conversations. Without them, nothing will ever change.”
Those conversations, Georgie said, are the first step towards achieving positive change – and help develop understanding among those in decision making roles.
Change is coming
Georgie said: “We know we cannot achieve change without getting men on our side too, so it is so important we have the support of men across the board.
“What we never want to be are preachers or to point the finger. We want to create an allyship, helping educate people while showing them how their simple acts can make a huge difference to their workforce.
“Staff turnover is high in the NHS, and while we know period dignity schemes aren’t going to magically fix that – they will help boost staff morale and can improve staff performance by taking away that stress.
“What we want to say is that introducing period dignity schemes is such a simple thing to do. And that staff deserve it.”
Feedback
Dr Rosie Baruah is an ICU consultant who has seen first-hand how healthcare staff have struggled through a lack of access to period products at work.
She said: “When we first started raising awareness in 2021 it was all about how unpredictable periods are and how they can start by surprise – and that staff needed access to products for when they were caught off guard.
“What we have seen in the last year with the cost-of-living crisis however is that some staff simply cannot afford to buy period products. E

Wellbeing
43 Issue 23.3 | HEALTH BUSINESS MAGAZINE
It is so important we have those conversations. Without them, nothing will ever change
F “This is a basic part of personal hygiene we are talking about, just like how your boss would always supply toilet roll, soap or hand towels.”
Rosie’s native Scotland became the first country in the world to make the access to free period products a legal right, although the NHS and its hospitals are not covered by the law.
Rosie added: “The introduction of the Period Products Act has been fantastic for Scotland, but the reality is that staff working in the NHS under significant time constraints or working irregular hours simply can’t access the pick-up points. They need the products available to them there and then.
“I like to see the introduction of period products as an omission rather than an addition – they are something that should have always been available.
“Periods are something that affect over half of NHS staff, and without them we don’t have a health service. Anything we can do to support them, and their wellbeing is money well spent.”
Resusable products
The introduction of reusable products such as period pants has also been touted as a solution to the NHS’ unique challenges, alongside disposable pick-up points in washrooms.
Hey Girls’ work with public sector organisations has included the introduction of home packs containing reusables for residents in numerous local authority areas in the UK.
Georgie said: “There should be options available depending on people’s role within the NHS. Yes, having disposable products like tampons, pads and panty liners available in staff washrooms would be a huge step forward – but what we would love to see is the introduction of reusable product packs.
“Those reusable products, like our cups and pants, can hold a significantly higher amount of liquid compared to disposables and are the perfect solution for theatre staff who face hours and hours of work without the chance to go to the bathroom.

Wellbeing 44
This is a basic part of personal hygiene we are talking about, just like how your boss would always supply toilet roll, soap or hand towels
“But regardless, we know introducing disposable products is a great place to start.”
Cost
Georgie added introducing a period dignity scheme is much cheaper than many expect.
She said: “While it might sound like a mountain of products would be required for every hospital that introduces a period dignity scheme, that isn’t really the case. In reality, we recommend two pads and two tampons per person, per month.

“That isn’t anything radical in the slightest. And it isn’t the expensive mass roll-out so many expect it to be.
“It would be brilliant to see period products made available to patients too, although we appreciate budgets in the NHS are incredibly tight.
“Our dream would be for patients to be sent home with a pack of products.
“Everyone deserves a dignified and safe period.”
Georgie said she hoped decision makers in the NHS will be swayed in future.
She added: “Like everyone else in this country, all of us at Hey Girls are proud
Take Control of Infectious Germs, Bacteria and Viruses...
Sanondaf are a specialist decontamination company ...





We provide Hospital Grade Disinfectant, with no need to rinse after application

Our hydrogen peroxide vapour treatments (HPV) have been clinically tested
We disinfect to 6 log kill in a highly efficient, effective and environmentally friendly manner
Rooms can be turned around in one hour
of the heroes who don their scrubs every day to look after us and our loved ones.
“We just think taking away the added stress their period can bring is the least they deserve.” L
NHS Trusts looking to introduce period dignity schemes at their hospitals can learn more by visiting the Hey Girls website: www.heygirls.co.uk
www.sanondaf.co.uk support@sanondaf.co.uk +44 (0) 1236 702028
FURTHER INFORMATION 45 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Upcycling plastic waste for the health service
Linda Ball, founder and CEO of Upcycled Medical explains how the company is fighting plastic waste with their products
How did Upcycled Medical come about? What problem are you trying to address?
Upcycled Medical started in 2019, and our mission is to end the problem of plastic pollution. Our oceans are filling up with plastic waste - over 14 million tons of plastic waste are dumped into our oceans every year, killing wildlife and leaching dangerous chemicals into the water. By collecting plastic waste and reusing it, upcycling it into sustainable and eco-friendly clothing, we can reduce the amount of plastic filling up the oceans and reduce the need for new plastic to be created at the same time. We aim to change the manufacturing industry for the better and inspire other businesses and organisations to follow in our footsteps by embracing more sustainable practices.
What does Upcycled Medical do? Can you explain the process?
Put simply, we turn plastic waste into fabric, which we then make into products for the medical and healthcare industry, including medical gowns, scrubs, coats, and even curtains and bedsheets. To collect plastic, we teamed up with the SeaQual Initiative and their network of partners - through an agreement endorsed by the Spanish government, they’ve incentivised fishermen to trawl the oceans and bring back plastic waste. We also collect plastic waste from our partners - this is all sorted and pelletised before being upcycled into polyester yarn, which we weave into textiles. All of this plastic would have otherwise ended up in landfills, but we ensure it’s given new life - around seven or nine plastic bottles go into each piece of medical clothing that we make. We don’t just collect plastic. We’ve teamed with ocean clean-up programs and plastic waste collectors to clean up plastic, metal, rubber, glass, wood, and other materials - for every kilogram of yarn that Upcycled Medical produce, we estimate that we’ve collected between 600 grams and 1 kilogram of marine litter from our oceans.
What is the difference between what Upcycled Medical does and other recycled products?
Most medical scrubs used by the NHS are made using plastic made in Saudi Arabia, which is then shipped to China to be turned into scrubs shipped to the UK. This process wastes fossil fuels, water, and energy - and we’ve made it our aim to change that. Unlike other companies, we make our products in the UK from recycled material - and the finished products are completely recyclable, too. Upcycled Medical has the lowest verifiable carbon footprint in the world. Our zero-waste production process reduces CO2 emissions by 34 per cent, water usage by 34 per cent, and energy consumption by 39 per cent.
What happens to the clothes at the end of their life? Can they be recycled again?
Every single Upcycled Medical piece is designed and manufactured with both sustainability and longevity in mind. Healthcare workers spend countless hours carrying out their important work across various hospitals, clinics, and dispensaries. It is crucial that the clothing they wear is comfortable, durable and can be worn over long periods of time - and that those items can be re-worn and used again and again, for as long as possible. It’s also crucial that when an item of clothing reaches the end of its life, it’s not simply thrown away, to end up in a landfill - and when an item of Upcycled Medical clothing reaches the end of its life, it can be recycled and upcycled into a brand new item of clothing. Production begins with treating and cleaning the ocean waste used to create the yarn we make our clothing from, ensuring it can be recycled over and over again. The collected waste is then transformed into flakes and pellets, which are subsequently sent to our factory in Spain. At the factory, the pellets are bound together to create high-quality yarn, forming the basis of our recycled clothing. Waste plastic - including discarded clothing - is
Advertisement Feature
46 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
collected from our clients, including Bupa, and then sorted and transformed into pellets, flakes, and chips so that they can be upcycled all over again.
What are Upcycled Medical’s goals and plans for the future?
Upcycled Medical is committed to our mission of ending plastic pollution. There’s an urgent need to address the irreparable damage caused by waste plastic pollution, and we aim to amplify our voice to raise awareness worldwide.
We want to educate and inspire the public to create change and learn new behaviours that are kinder to our earth. To do this, we plan to foster collaborations and partnerships with social groups, charitable organisations, and waste collection initiatives globally. By joining forces with like-minded entities, we can leverage our collective efforts, share knowledge, and maximise our impact on a global scale.
There are endless possibilities for what we can create from upcycled plastics. Our hope is that we will never need to create anything from new plastics and that we can prevent the inevitable build-up of these harmful plastics in our oceans and landfills around the world. We can create a collective movement that fosters a sustainable future and actively works towards the elimination of plastic pollution. L
upcycledmedical.com
LindaBallisavisionary entrepreneurandenvironmental advocate dedicated to revolutionisingthewaywe approachrecyclingand sustainability.AstheFounder andCEOofUpcycledMedical, Lindaisleadingatransformative movementinthemedicalindustrybyproviding eco-friendlyscrubsthatcombinestyle,comfort,and environmentalresponsibility.Drivenbyherpassion foracleanerandhealthierplanet,Linda’sdreamis tocreateatechnologythatenablestheproduction ofrecycledproductswithoutcompromisingon qualityoraddingharmfultoxinstotheenvironment. Throughherinnovativeapproach,Lindaaims tochangethefaceofmanufacturingandinspire otherindustriestoembracesustainablepractices. UpcycledMedicalsuppliesthemedicalindustrywith stylish,eco-friendlyscrubs,whileADifferentBall Gamefocusesonupcycledfootballkitsthatcombine sustainabilityandperformance.Additionally,Linda establishedUpcycledCorporateClothing,abrand dedicatedtotransformingdiscardedmaterialsinto environmentallyfriendlyattireforcompanies. Recognisingtheurgentneedtoaddressplastic waste,LindafoundedUpcycledPlastics,acompany specialisingindesigningandmanufacturingbins thatfacilitatetheproperrecyclingofdifferent plastics,ensuringtheyarerepurposedformultiple applications.ShealsodevelopedUpcyclingWarriors, anengaginggamethateducatesplayersaboutthe importanceofresponsiblewastemanagement. Bygamifyingrecycling,sheaimstoinspireanew generationtobecomeenvironmentalstewardsand makeapositiveimpactontheplanet.
Inherquesttoinspirewidespreadadoptionof upcyclingpractices,LindacreatedSupraCycling,an onlineplatformthatservesasavaluableresource hubforindividualsandbusinessesseekingto embracesustainablelivingandproductionmethods. CentraltoLinda’srevolutionaryinitiativesisFather Alterin,agroundbreakingtechnologythatpowersall hercompanies.Thisinnovativesolutioncombines cutting-edgeengineeringandadvancedmaterials science to transform waste into valuable resources, makingrecyclingmoreefficientandsustainablethan ever before.

LindaBall’sunwaveringcommitmentto sustainabilityandherpioneeringspirithave positionedherasatrailblazerinupcyclingand environmentaladvocacy.Throughhervisionary leadership,Lindaisactivelyreshapingindustries, onerecycledproductatatime,andpavingthe wayforamoresustainableandenvironmentally conscious world.

Advertisement Feature
FURTHER INFORMATION
47 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Linda Ball, Founder and CEO of Upcycled
30 Years of providing Health Care facilities with energy management systems engineered for sustainability

Keep sustainability and net zero building compliance on your facilities wish list, with Powell Systems. We’ll help get you the most from your budget as part of working with you, not just for you.
We work with you to stretch your budget without sacrificing sustainability and net zero building compliance. And we look forward to the next 30 years of serving Health Care using our in-house BEMS expertise and system knowledge
Powell Systems will support your team, to achieve cost optimisation in the building projects and upgrades of your facilities. Together we will apply technology to get the most out of your budget, improve reliability, manage costs and make delivering your services more achievable.

Whether it’s BEMS, Maintenance or Lighting controls for your next project, Powell Systems would welcome the opportunity of working with you. Visit our website for more information on the solutions we offer, or call +44 (0) 1689 879000 to book a consultation

Working in partnership with local government

Michael Laing, director of integrated community services, County Durham Care Partnership explains the collaboration between the NHS and local authorities

The most moving celebrations of the Coronation weekend for me were those which took place in our supported housing. Our extra care schemes, residential and nursing homes and specialist accommodation are a valued part of their communities. Schools, volunteers and faith groups all made an extra effort to include the people we care for in our supported housing. NHS Community staff, social care teams and primary care colleagues were all invited to join in. Most of the care we give happens in
someone’s home and is delivered by a team every day of the year not just on a special occasion such as the Coronation.
The Coronation Service was full of messages about relationships, symbols and tradition. The long lasting success of the County Durham Care Partnership is built on the relationships between individuals at all levels developed over many years. The Chief Officers meet fortnightly. We talk informally about a range of work related subjects but we also get to know and understand each E
Local Government 49 Issue 23.3 | HEALTH BUSINESS MAGAZINE
F other, share problems and find joint solutions. There is also some talk about favourite foods, holidays, dogs, horses and our families. This incidental chat is important. It shows that we are human and have interests beyond the formal work situation. It helps when we are facing pandemics, storms, floods and demand pressures to enhance and sustain our joint working. More importantly it helps us care for each other as unique individuals.
Many Coronation guests wore medals and the neck chains of the orders of chivalry. I’m told special permission is needed to wear the decorations of other nations. This may come from the time when the Earl of Leicester presumed to wear “foreign” symbols of office in front of Queen Elizabeth I. Her characteristic remark for all of the Court to hear was “My dogs wear my collars”. We are not quite so fussy in our Partnership. We give out our lanyard and badge pretty freely. We encourage people to wear it as an outward sign of being part of the Partnership. I always feel quietly proud when I see them being worn especially by people who are not members of the Partnership.
Durham Cathedral stands high above the River Wear and dominates the surrounding City especially when seen from the East Coast Mainline. It was illuminated red, white and blue for the Coronation. It began as a monastery in 995. One of the roles of the monks was to care for the sick. They were organised into groups of monasteries called provinces or congregations – similar to ICBs. Monasteries had infirmaries, dispensaries and alms-houses – not unlike acute hospitals. They also had parishes and “cells” outside of the Abbey caring for people in villages and towns – just like primary and community services. The monks’ health and care system is part of our tradition and perhaps our future.


“Integrated” care
Integrated care systems need more than relationships, symbols and traditions to be successful. They need structures, administration and money. In County Durham we are working with our ICB in the North East and North Cumbria to co-produce a Joint Committee. We have been operating as a Joint Executive for many years and have structures which work well, reach shared decisions and make the most of the skills of our workforce and get best value from every penny. The Joint Committee is the natural development for the County Durham Care Partnership – but it is “new territory” in terms of governance. We have some Government guidance from late 2022 but we are working through the details together drawing on the expertise of the ICB’s Head of Governance.
Our ambition is to co-produce a Joint Committee which has “everyone and everything” related to health and care in scope. We know that this will be achieved over time. This means the NHS, primary care, Public Health, Adult Care, Children and Young People’s Services, the voluntary and independent sector and Community Services. There is also an important role for housing and economic development. We want to jointly exercise
Local Government
50
County Durham, where their Care Partnership is built on the relationships between individuals at all levels developed over many years
our decision making capacity to commission services to meet needs, innovate, sustain and improve outcomes and support each other when we are under pressure. Above all we want to make it easier for our people to experience and deliver health and care services.


Funding
“Put not your trust in money but put your money in trust” said Oliver Wendell Holmes. Money and trust go together in the County Durham Care Partnership. How we spend and account for our money is key to all of our relationships. We can demonstrate that trust in our Better Care Fund, in the way we decide together how to invest money from the Discharge Fund and how we commission. We respect the different financial regimes of our partner organisations. However some of the important lessons from the Covid pandemic and austerity are about sharing our money to get better outcomes and supporting partners with financial troubles.
“While money can’t buy you happiness it certainly lets you choose your own form of misery” according to Groucho Marx. Agreeing the governance arrangements and culture for our money is essential in the development of the Joint Committee. We work on “open book” principles now and we want to keep them in the future. If we don’t get the governance and culture of the money right we will be at risk of choosing our own form of misery.
Children and young people’s services are “front and centre” of our Partnership
Children and young people
We often concentrate on adults when we integrate services. In County Durham, children and young people’s services are “front and centre” of our Partnership. We have appointed to some joint posts recently to lead our integration of children and young people and turn our ambitions into operational changes E
Local Government 51 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Joint
F and improved outcomes. The Association of Directors of Children’s Services (ADCS) President this year is John Pearce from Durham County Council. In his first speech as President he called for a Better Care Fund for children and young people and greater integration between health and care.
Joint posts across health and care have worked really well in County Durham. We have a Joint Head of Integrated Commissioning who is also our Director of Place. I am in a joint post between the Council and the Trust. We have joint posts in mental health and learning disabilities. Our aim is to have more joint posts in the future and more secondments between partners as recommended by the Hewitt and Messenger Reviews.

It seemed odd going to the North East and North Cumbria ICB “Winter Debrief” in bright spring sunshine. Our ICB is doing some great work in bringing us together and promoting good practice as well as listening to feedback from the “frontline”. They have put me in touch with North Cumbria who are doing some outstanding work on integration and our visit is already planned. Going to visit customers in their homes with “frontline staff” is a great privilege. I’m often greeted with the line “Hello, where do you belong?” Which is a County Durham way of asking where I live. It emphasises the strong sense of “belonging” to a place felt by our customers and workforce. We will do well to remember that sense of place and belonging as we develop our Joint Committee. L

Local Government
posts across health and care have worked really well in County Durham
52
Hospital Disposable Curtains
Yewdale is the only designer and manufacturer offering a complete privacy package for healthcare providers, plus a recycling programme for used disposable curtains.

Most environmentally friendly curtain available Smoothest to operate with our wheeled roller runner hooks
Available through the NHS Supply Chain
Scan this QR code to learn more about our disposable curtains.
Compliance Management Made Easy with Evidence-Based Software

The full annual inspection and load testing of all antiligature products in accordance to HTM66 and NHS Policies with transparent asset reporting via purposebuilt web-based software.
We demonstrate our offering and create a bespoke proposal for your needs and requirements to guarantee your environments are safer and more effective resulting in a more risk-free future.
Visit: protects-plus.co.uk Call: +44(0)345 646 0955 Email: enquiries@protects-plus.co.uk Evaluate Clarify
Engage We believe in agile partnerships built on
your requirements to deliver the best value. Certify Together with our consultants, we translate the evidence and data into our secure online portals providing you with total transparency that allows you to clearly interpret the results for full visibility
understanding
Call: +44 (0)1268 570900 Email: enquiries@yewdale.co.uk Visit: yewdale.co.uk


VISIT OUR VIRTUAL SHOWROOM
Healthcare Estates 2023
Healthcare Estates, the UK’s largest event for Healthcare Estates, Engineers and FM Professionals is coming to Manchester, 10-11 October 2023


This year’s event is expecting more than 4,500 visitors, delegates, speakers and dinner guests, with more than 240 companies exhibiting their latest products and services.
The event consists of the IHEEM Annual Conference, awards dinner and the UK’s largest trade exhibition for Healthcare Engineering and EFM.
The IHEEM Annual Conference
The IHEEM Annual Conference will see more than 50 expert presentations, addressing the key topics in the healthcare sector.
This year’s conference themes include: Health and Social Care Planning, which will focus on how the estates and facilities profession can effectively support & influence the delivery of the Integrated Health & Social Care System’s future strategic planning requirements; Governance, Assurance & Compliance of Healthcare Estates & Infrastructure, which will cover how we can ensure healthcare estate E
Healthcare Estates 2023 55 Issue 23.3 | HEALTH BUSINESS MAGAZINE
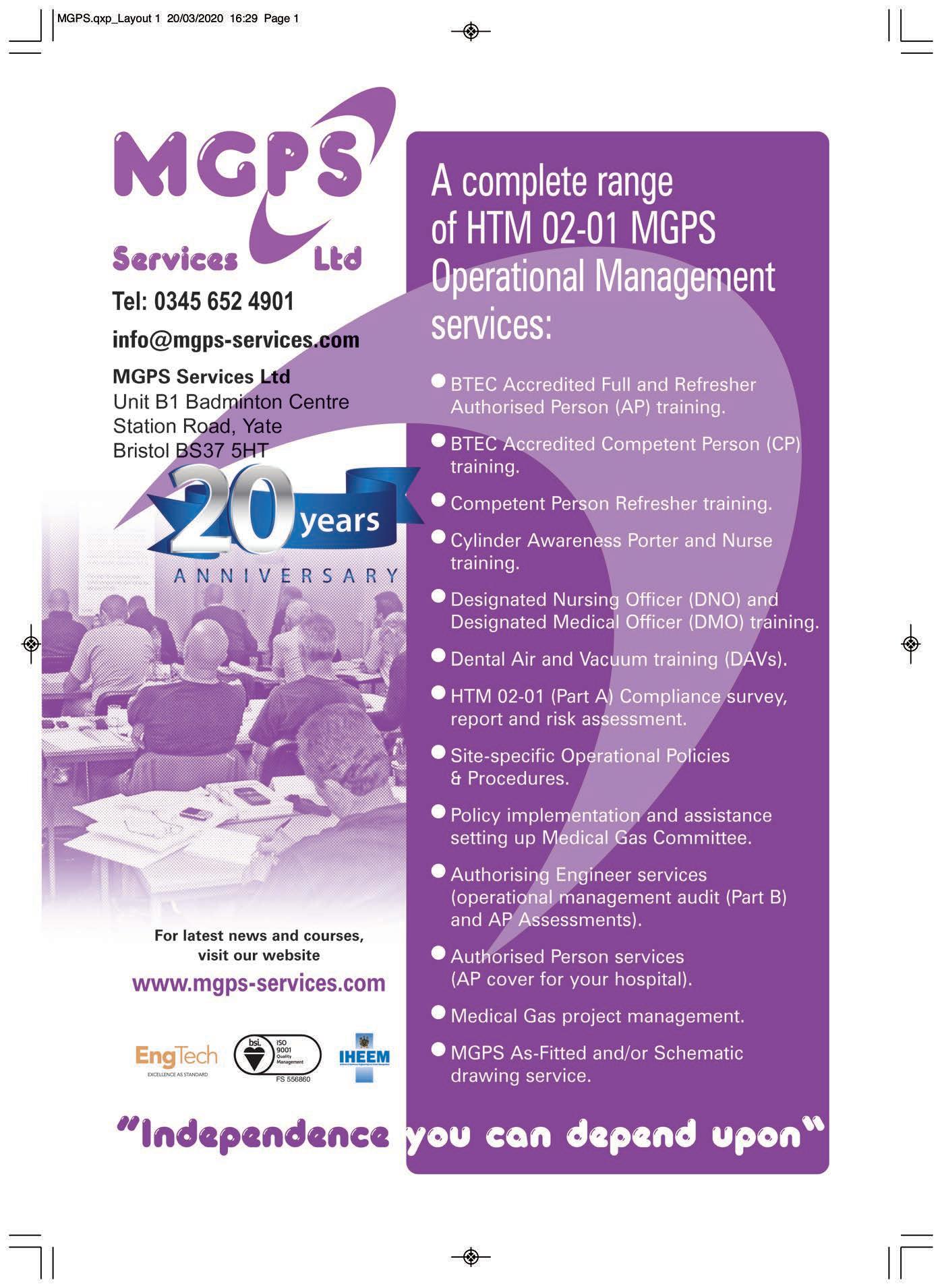
F services and critical functions relating to patient safety are compliant and appropriately managed to meet the increased governance in national policy and legislative requirements of governing bodies such as HES & CQC; and Implementing Digital Technology & Innovation into the Healthcare Estate, which centres on the key issues impacting the EFM profession in adopting and implementing digital technologies in both the existing estate and the healthcare-built environment of the
future. Medical Engineering and Healthcare Engineering will investigate the technical, specialist and scientific challenges that need to be addressed to ensure future healthcare engineering and medical engineering services are designed differently, particularly in the areas of ventilation, water safety, infection control and infrastructure resilience; and Operational Delivery of the Healthcare Estate will look at how the estates and facilities profession can continue to deliver high-quality healthcare services and functions to patients as they face increased & conflicting challenges of capability, capacity and efficiency particularly around workforce and the net zero carbon agendas.

Presentations that are confirmed for this year include Patient Safety - It Starts with Good Infrastructure, by David Jones, director of estates, facilities & capital development, University Hospital Southampton; Modular Builds - a Versatile Solution for Hospital Blocks by Angela Clarke, associate director for capital development, Kingston Hospital NHS Foundation Trust; and Unlocking the Power of Peer Knowledge Sharing: Insights from a Three-Year Study on NHS EFM Departments by Carl-Magnus von Behr, Doctoral Researcher, University of Cambridge. E
Exhibitor-led theatres will focus on HVAC & Engineering; Infection Control & Water; Energy & Sustainability

Healthcare Estates 2023
57
F Keynotes will be delivered by Simon Corben, director and head of profession at NHS Estates & Facilities, NHS England; Julie Critchley, director of NHS Scotland Assure, Procurement Commissioning and Facilities, NHS National Services Scotland; and Stuart Douglas, director specialist estates services, NHS Wales Shared Services Partnership.
Exhibit
The UK’s largest EFM zone will feature four industry zones and 200 exhibitors. Several exhibitors are already confirmed, who will be showcasing the products, equipment and services to create high-quality, patient-centred environments.

Exhibitor-led theatres will focus on HVAC & Engineering; Infection Control & Water; Energy & Sustainability; Design & Construction and Facilities Management. Organisations and companies will be discussing future challenges and opportunities; operational excellence and best practice; product and equipment innovations; cost control and asset management; legislation and compliance. For exhibitors, the event offers several benefits, including; the opportunity to meet
specifiers and decision-makers responsible for controlling built environment budgets and talk directly to those on the front line about the problems and challenges they face and how your products and services can help address them. Exhibitors will be able to present and demonstrate their expertise to a highly targeted and motivated audience and receive valuable feedback and insights that can feed into new product and business development processes.
Awards
There are 12 award categories celebrating excellence. The awards also offer the opportunity to network with more than 500 people. Entries for the awards are open now and close on 30 June. The Healthcare Estates IHEEM Awards recognise excellence in the latest innovations from the leading names in the healthcare engineering and EFM sector. The Awards are judged by experts with extensive experience and achievements within the NHS and commercial healthcare sector. Award categories include Apprentice of the Year, which invites entries from apprentices at intermediate, advanced, higher and degree level; the Estates & Facilities Champion of
Healthcare Estates 2023
58
Several exhibitors are already confirmed, who will be showcasing the products, equipment and services
Champions, which recognises a member of the Estates & Facilities team that has gone above and beyond their job specification to improve the patient environment; and the Staff Wellbeing Initiative of the Year, which recognises an initiative or programme introduced within a Trust to ensure the wellbeing and mental health of its team Register
now
Attendees can register online now as a Conference Delegate or Exhibition Visitor. Delegates will be able to access the full Conference Programme, as well as the Exhibition and Exhibition Theatres. Visitors will only be able to access the exhibition and exhibition theatres.
The event will take place in Manchester Central, which is in the city centre, easily accessible by public transport. There is also an NCP carpark nearby.
The event will be open Tuesday 10 October, 08:45-18.00 and Wednesday 11 October 08.4516.00.
https://www.healthcare-estates.com/
A solution for a net-zero future
BeaconMedaes is the sole UK supplier of Medclair’s unique Central Destruction Unit (CDU), helping hospitals reach net zero. The low-energy unit eliminates 99% of exhaled nitrous oxide, making the surrounding environment safer for staff and patients without any reduction in the level of pain relief provided.


CDU Explained
The CDU is a centrally installed nitrous oxide destruction unit that can handle up to 12 treatment rooms

The unit is compact and contains functionality for continuous real-time monitoring
• Exhaled air is passed from the face mask into a climate-smart catalytic purification system, where the environmentally hazardous nitrous oxide gas is decomposed into harmless nitrogen (N2) and air (O2) and can be safely vented into the atmosphere
Greaves Close, Markham Vale, Derbyshire S44 5FB
Office: 01246 474 242 | E-mail: gbn.sales@beaconmedaes.com www.beaconmedaes.com/en-uk | www.mymedgas.com/en-uk
L
Healthcare Estates 2023 FURTHER INFORMATION 59 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Modular solution reduces backlog at North Devon Hospital
In this interview, Marsh Pullen, capital contracts manager for the Royal Devon University Healthcare NHS Foundation Trust, explains the process of procuring a modular building from Wernick. This includes the benefits of the modular building method, the challenges of the project and the feedback from the end users

We required a new building to increase our elective bed capacity to assist with the backlog of elective surgical patients that the trust currently has. A modular building was chosen primarily because of speed of deployment, but also because it complemented the space that we had on site and it minimised disruption and the build time on the actual hospital site.
Procurement
We went out to the marketplace using the modular building framework and we had a specification of our requirements. Wernick were able to offer a very competitive package and they were a clear winner.

We raised an order with Wernick Buildings and 20 weeks later, we were delivered a fully compliant, completed building. One week after that, we were treating patients in it.
We asked Wernick to deliver a compliant ward. What they actually delivered was above and beyond that because although it is compliant, it also aligns with our standard specification for mechanical and electrical items, which means that our users, clinical users, are familiar right out the box of how all of the systems work.
Challenges
We had some logistical challenges with the install which the Wernick build team were able to overcome. The ward is in a bit of a tight corner of the hospital. It also needed to marry in with the existing
structure to allow patients to transit to and from the main building and it also had to be undertaken on the site of an acute care hospital which is at full capacity all of the time and the Wernick team were able to undertake the work with minimal disruption. Wernick and the design team on the clinical side worked really, really well together. There was a lot of harmony. Whenever we had a problem it was overcome collectively – and that proactive attitude shows through on the outcome that we’ve got a successfully delivered ward within the timeframe.
Feedback
The feedback from the end users is great. Everybody that’s looked at it so far absolutely loves it. It’s a 21st century ward with all of the mod cons and all of the elements that it requires to treat the patients we need it to. Our experience of working with the Wernick build team is very professional, they said they could deliver us a ward on time, on budget and they have, and that speaks volumes. I can’t speak highly enough, really, they’ve delivered us a fantastic ward which I’d put up against any ward in the UK for quality, speed of delivery, and affordability. L
www.wernick.co.uk
Advertisement Feature
FURTHER INFORMATION
60 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net



Specialists in modular construction CONTACT US TODAY 0800 18 18 22 | www.wernick.co.uk buildings@wernick.co.uk Scan the QR code our latest watch video 50+YEARS DESIGN LIFE SUSTAINABLE CONSTRUCTION FULL PROJECT MANAGEMENT MINIMUM ON-SITE TIME FLEXIBLE EXPANDABLE WERNICK MODULAR BUILDINGS DELIVER... Wernick Group’s commitment to a sustainable future
Honouring 75 Years of the NHS
Patient care is the number one priority. Working across 230 NHS customers and sites has strengthened our understanding of the solutions Veolia provides when offering sector-specific services that address environmental needs. To mark this milestone, we look at how we have done that across the sector’s water, waste and energy
Decarbonising and delivering lower-cost energy:
Operating large, complex, and energy-hungry facilities requires significant contributions to reducing carbon impact while creating a comfortable environment for patients and staff. We currently provide energy and facility management to over 100 hospitals around the UK. Our innovative projects, such as installing hydrogen-ready boilers, have helped hospitals cut carbon and achieve sustainability goals. Our unique service offering for clinical alternative treatment (AT) waste delivers carbon savings of up to 73% to support the NHS in significantly achieving its carbon reduction goals.
See how we helped decarbonise Eastbourne District General Hospital: https://www.youtube. com/watch?v=oYeMnPYVmFs

Taking care of critical services: Our facilities management teams ensure hospital facilities run smoothly and efficiently so that NHS teams can continue to focus on their duties. We service many hospitals, from safety and cleaning services to infrastructure, waste and energy management to reduce carbon emissions, increase recycling rates and improve the sustainability of the facilities.
Clinical waste:
Clinical waste must be responsibly collected and disposed of safely. Using information from pre-acceptance audits, we identify materials that are incorrectly classified as clinical waste
and which, with proper segregation, can be recycled. Working closely with our materials recycling team, we investigate solutions to capture identified streams for recycling, moving materials up the waste hierarchy. We divert offensive waste from landfill using our ERF facilities to process the waste. We have undertaken significant investment in our Tyseley and Sheffield ERF facilities enabling us to compliantly process orange bag waste via these ERFs as opposed to traditional autoclave routes avoiding the emissions generated from autoclaving and delivering carbon savings of up to 73%.
All waste streams processed through the ERF generate electricity to power local homes and businesses and heat for district heating networks used to heat local buildings, including some local hospitals, providing a unique and genuinely circular solution where the hospital’s clinical waste is effectively powering its electricity and heating. We look forward to following the progress of the NHS and continuing our partnerships in building a greener future for the healthcare sector. L
www.veolia.co.uk/sectors/healthcare

BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 62
FURTHER INFORMATION
▶ Advertisement Feature BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
Efficient energy use to reduce emissions
Wirral University Teaching Hospital NHS Foundation Trust has a Green Plan to cover 2022 to 2025, with a major focus on energy
In the foreword to the Green Plan, Matthew Swanborough, director of strategy & partnerships, recognises the need to ensure delivery of safe care, while at the same time recognising the responsibility to reduce impact on the environment.
The Wirral Peninsular, where the trust is located has already seen the effects of climate change, with longer dry spells and more frequent heat waves, warmer and wetter winters, more storms and floods, and a rise in sea levels – a worry being located on the coast. Swanborough said: “As most of us will be aware, reaching net-zero emissions is high on the agenda at present and while the Trust already incorporates sustainability in many aspects of its activities, we also recognise that more can be done, and we are committed to making the necessary changes to contribute to net-zero. This document will set out actions and targets for different areas of focus, these will be monitored annually to ensure we reach our netzero target by 2040/45.”
Sustainability and low carbon

The trust’s green plan aims to embed sustainability and low carbon practice in the

way that healthcare services are offered and at the same time, help the NHS to become the first health service in the world with net zero greenhouse gas emissions.
The trust recognises that the climate crisis is also a health crisis, with rising temperatures and extreme weather disrupting care and impacting the health of patients.
The Green Plan is to be reviewed annually.
Areas of Focus
The vision of the Green Plan has a focus on Net Zero and Resource consumption and Greenhouse Gas emission reductions that align with NHS net zero targets. Climate Resilience is a key factor, including reducing the environmental impact of the trust’s activities and providing a basis to become a climatechange-resilient organisation.
The Green Plan has nine Areas of Focus, with actions to be achieved within the three years covered by the plan. These areas include Workforce and Systems Leadership, Sustainable Models of Care, Digital Transformation, Travel and Transport, Estates and Facilities, Medicines, Supply Chain and Procurement, Food and Nutrition and Adaptation. E
Energy Sponsored by 63



Helping you meet your decarbonisation targets We’ll help you manage your energy costs, advise on your decarbonisation plans and meet your sustainability targets. Get in touch with us Electricity bill forecast A tailored, five-year electricity bill forecast to assist your strategic decision making. Energy Net Zero Regular insight on the energy market’s move to net zero, keeping you up to date on the latest developments. Energy Net Zero forum Bi-monthly forum on the latest policy and regulatory changes and the implications for businesses. Josh Bamsey j.bamsey@cornwall-insight.com +44 (0)7741 648285 www.cornwall-insight.com Find out more @CornwallInsight Click here to learn more
F The Green Plan links to NHS Net Zero, acknowledging the aim for the NHS Carbon Footprint for the emissions directly controlled to net zero by 2040 and the NHS Carbon Footprint ‘Plus’ for the emissions influenced, to be net zero by 2045.
Emissions
Wirral University Teaching Hospital (WUTH) commits to reduce greenhouse gas emissions to Net Zero to prevent the worst impacts of climate change and meet NHS Net Zero commitments and the plan outlines how it will do this.
As of 2020/21, WUTH’s carbon footprint was 29,451 tCO2e. This means that to reach the net zero goal, the trust needs to avoid around 1100 tCO2e from all sources each year until 2040/45.

After investigation, it was found that 72.8 per cent of the trust’s carbon emissions came from the supply chain and 9 per cent came from patient and visitor travel, areas which are harder to control.

However, 27.2 per cent of emissions are from sources which the trust can control, which include the operation of buildings and transport associated with the delivery of care – including staff travel. Building energy makes up 26.3 per
cent of the trust’s emissions – a great place to start when it comes to reducing emissions
Estates and facilities
Estates and Facilities in one of the nine Areas of Focus and this is where energy reduction comes in. The trust acknowledges that providing care 24 hours a day comes with high energy consumption. Therefore, energy use needs to be optimised and there needs to be a move away from the use of fossil fuels.
The trust recognises that energy consumption needs to be reduced by 182,000 kWh per year to achieve the emissions reduction target of 3,376 tCO2e in 2024/25. To achieve this the trust will be following the four-step approach within the NHS’ ‘Estates ‘Net Zero’ Carbon Delivery Plan’. This includes making every kWh count and investing in no-regrets energy-saving measures; preparing buildings for electricity-led heating and upgrading building fabric; switching to nonfossil fuel heating and investing in innovative new energy sources; and increasing on-site renewables and investing in on-site generation. The trust has provided detailed analysis of where its energy emissions come from and why this is.
As well as using renewable energy, the trust also commits to reducing energy consumption overall.

The trust says: “Moving away from fossil fuels is vital to achieve net zero targets: electrically powered heating systems, such as heat pumps and infrared heating, while using a 100 per cent renewable electricity tariff, will result in zero emissions (at point of use).”
The Green Plan concludes: “Climate Change poses many threats to our care population and how we deliver care. This Green Plan will enable us to become an adaptable and resilient organisation. It will help steer our direction of travel with other local anchor institutions, bolstering our ability to provide a continued critical service.
“Our dedicated workforce is core to our care provision and delivery of this Green Plan. With the necessary structures in place, it will be our people and service users who will drive the changes to make us a more sustainable organisation. We will continue an open dialogue with all stakeholders to improve our Green Plans and the care we deliver.” L
https://www.wuth.nhs.uk/media/19913/

wuth-green-plan-final-v10.pdf
FURTHER INFORMATION Sponsored by 65 Issue 23.3 | HEALTH BUSINESS MAGAZINE
As well as using renewable energy, the trust also commits to reducing energy consumption overall
Energy-efficient hospitals
Energy use in hospitals is a hot topic, with such a large carbon footprint, an energy pricing crisis and a goal of net zero, there is lots that can be done. HB spoke to Heather Foster, sector lead healthcare at Veolia UK about how hospitals can make their energy usage more efficient

How can hospitals go about saving carbon? Is it about turning things off, changing processes, small efficiency changes, something else entirely or a bit of everything?
The NHS is responsible for 40 per cent of the public sector’s emissions. Hospitals can save carbon through strategies, including turning things off, changing processes, and reducing their reliance on fossil fuel technology. By implementing these measures, hospitals can save carbon, improve the efficiency of their operations and make steps towards their decarbonisation targets. Getting a thirdparty energy audit of your estate can reveal a GreenPath towards carbon savings.
What is the best area to make changes in? Trusts have a limited budget, where can a small change make a big difference?
Veolia can support Trusts in England to apply for Public Sector Decarbonisation Scheme Funding, which is administered by Salix to the healthcare sector. This funding from the Government helps to reach the NHS Net Zero target of 2040. More than £409 million has already been awarded under this scheme. The window for applications to Phase 3C of this funding is expected to open in autumn 2023.
Many trusts have large sites, with big energy demands. However, how can

Q & A 66 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
Heather Foster, Sector Lead Healthcare, Veolia UK
this be used to their advantage to perhaps generate their own energy and reduce their carbon?
Veolia is focused on delivering Ecological Transformation, where historically hospitals have relied on large volumes of power from the grid, Veolia has adapted an energy mix. Balancing the needs to maintain power and heat for essential patient care with the benefits of cost management and environmental stewardship. Our approach is systemic and the larger and more complex the energy demands, the more of our solutions we can employ. We have over 120 products and services that decarbonise the operation of a building. Often these solutions are cumulative, meaning that the more we use in an integrated system, the greater the benefit.
We take a holistic approach and look at how we can reduce the demands before
implementing new technologies to provide a sustainable solution for generating energy. This can also help with the replacement of old equipment that is on the backlog maintenance list.
Can you provide any examples of a trust or hospital that has made large energy savings.

Veolia advances carbon reductions for two acute hospitals for the University Hospitals Birmingham NHS Foundation Trust, one of the largest teaching hospital trusts in England that treats over 2.8 million patients each year.
By applying heat pump and solar technologies, it will help the Trust achieve the NHS Net Zero goal by saving 3,847 tonnes of CO₂ each year. L
www.veolia.co.uk/sectors/healthcare
FURTHER INFORMATION
Q & A 67 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Fordingbridge are industry leaders in canopies and external builds designed to enhance healthcare and emergency service facilities throughout the year as weather protective solutions.




Maximise healthcare environments with a range of Fordingbridge canopy solutions offering excellent safeguarding measures, weather protection, and ensuring impressive canopy coverage, even in those seemingly inaccessible spaces.
We offer the design and build of:

• Bespoke canopies •
• Turnkey solutions •
• Optimised walkways •
• Sustainable buildings •
68 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net 68 Issue 23.3 | HEALTH BUSINESS MAGAZINE
01243 554455 | www.fordingbridge.co.uk | info@fordingbridge.co.uk | Arundel, West Sussex, BN18 0SD Ambulance bays | Entrance canopies | Staff breakout spaces | Emergency access
The life-saving role of fire doors in public sector buildings
Helen Hewitt, CEO of the British Woodworking Federation (BWF) explains best practice for fire doors in public sector buildings including healthcare settings
Day to day, a fire door is used in the same the way as for any other door. However, in the event of a fire, the fire door must then perform its primary role – to protect lives and prevent the spread of fire and/or smoke.
So, what part do fire doors play in ensuring a building’s safety? Who is responsible for them, and what measures need to be taken to ensure they perform as intended in the event of a fire?

What role do fire doors have in public buildings?
Fire doors are required in most public, commercial and multiple occupancy buildings
and they form a crucial part of a building’s passive fire protection strategy. Fire doors help hold back the spread of fire and/or smoke to allow for a safe means of escape for building occupants while enabling the emergency services to enter the building.
They consist of specialist components which have been designed and tested to control the passage of smoke and withstand fire for a defined period. They enable access between the compartments of a building that are used to contain a fire while preventing a fire spreading from one area to another, and are used to maintain vital escape routes. E
Fire Safety 69 Issue 23.3 | HEALTH BUSINESS MAGAZINE
F In public sector buildings such as care homes or houses of multiple occupancy, which often house vulnerable people, a safe route of escape is essential. In the case of healthcare buildings, protecting escape routes for as long as possible can be vital where the occupants of the building may have difficulty responding to a fire alarm or escaping from the building unaided.
The importance of fire door classifications

For escaping a building, the fire door classification - the period for which a fire door can resist fire, and whether the fire door is also a smoke control door – is vital. Fire doors can be classified under the National System or the European System. A fire door assembly that has been tested to BS 476: Part 22 for fire resistance and was found to resist fire for a minimum of 30 minutes can be classified under the National System as FD30. After further testing to BS 476-31.1 for smoke control a fire door can be classified as FD30S.
Alternatively, a fire door can be tested for fire resistance to BS EN 1634-1 and if it resists fire for a minimum of 30 minutes it can be classified under the European System as E30. If the door is also tested for smoke control to BS EN 1634-3 it can be classified as E30Sa.

Who is responsible for fire doors in public buildings?
The Regulatory Reform (Fire Safety) Order 2005 (FSO) states that every public building
Fire Safety 70
must have a ‘Responsible Person’, typically the building owner or a facilities manager. In addition to carrying out fire risk assessments, the Responsible Person must also take steps to reduce or remove any fire safety risks on an ongoing basis and ensure inspections of fire safety ‘assets’, such as fire doors, are carried out regularly.

How often should fire doors be inspected?
Public sector buildings such as hospitals, care homes and schools often have high levels of through-traffic, making fire doors vulnerable to inevitable wear and tear. This is particularly true for healthcare settings where fire doors can also be damaged by the transportation of beds and trolleys.
Cracks and dents in a door – and any gaps between the door and its frame – will not only reduce its effectiveness and ability to perform as designed in the event of a fire, but can also harbour bacteria, impacting vital hygiene standards. Frequency of inspection depends on many factors, including the age and condition of the door.
For example, the Fire Safety (England) Regulations 2022 requires that, for buildings that contain two or more domestic premises and are over 11 metres in height, the Responsible Person, “must use best endeavours to undertake checks of fire doors at the entrances of individual domestic premises in the building at least every 12 months,” and they, “must undertake checks of any fire doors in communal areas of the building at least every 3 months.” In addition, BS 999:2017 Fire Safety in the design management and use of buildings - code of practice, Annex I, contains guidance on the “routine inspection and maintenance of fire safety installation” for the daily, monthly and six-monthly checks on fire doors.
However, in buildings where fire doors are in high use and therefore more susceptible to damage, for example in hospitals and schools, best practice recommends that they are inspected as frequently as each week or each month based on the door’s usage. E

71 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Fire Safety
Fire door third-party certification is a robust process which involves the fire door manufacturer or processor being audited by an independent third party
F Visual inspections of fire doors can help quickly identify any obvious maintenance issues that need to be addressed. However, the role of fire door inspectors should not be overlooked. Qualified and experienced fire door inspectors can conduct a thorough inspection and highlight issues that may not be easily visible but that could prevent the door performing as intended in the event of a fire. However, everyone can play a role in maintaining the fire safety of the buildings they occupy - the BWF’s Five Step Fire Door Check highlights the key elements to look for when you suspect a fire door may be in need of maintenance. Also, the Government has developed a checklist to support the Responsible Person with their fire door checks.
Why is third-party certification important?
Knowing that a fire door will perform as stated in the event of a fire is crucial. A standalone fire test report can evidence the performance of a fire door, but it can only cover the actual

configuration of the fire door assembly that was tested and there is no oversight of the production of doors produced following the one-off test.
Fire door third-party certification is a robust process which involves the fire door manufacturer or processor being audited by an independent third party to provide evidence that the fire door is appropriately tested and produced to a consistent standard.
For members of the BWF Fire Door Alliance, this involves meeting the strict criteria of an initial programme of fire testing, and auditing of the manufacturing process and quality management systems, which are confirmed by ongoing, regular, product testing and auditing. This provides vital evidence of performance and ensures that the initial tests were not a one-off result, giving building owners, the Responsible Person, specifiers and building users peace of mind that the fire door will perform as designed in the event of a fire. It also offers traceability throughout the construction supply chain, allowing access to important
Fire Safety
The original fire certificate and specification can be sourced, enabling on-site checks to be carried out against the door’s original standards
72 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
information about the door’s component parts which is essential to maintaining the door’s certification should any components or maintenance be needed.


When a fire door is manufactured or modified by a member of the BWF Fire Door Alliance an identifying label or plug is applied to the door in accordance with the chosen certification scheme. This allows for full traceability of the door by the fire door manufacturer or licensed processor, enabling access to documentation related to its specification and production records. This means the original fire certificate and specification can be sourced, enabling on-site checks to be carried out against the door’s original standards. If it’s found that any components should be replaced, the documents will also outline the parts compatible with the original certification and test requirements to ensure compliance is maintained.
Best practice and advice
To support the Responsible Person and all building owners in meeting their obligations, the BWF and the BWF Fire Door Alliance has

FIRE ALARM & ELECTRICAL
produced a range of advice and e-learning materials covering fire door responsibilities and key knowledge, as well as best practice for inspections and maintenance. L
https://firedoors.bwf.org.uk/knowledgecentre/fire-door-inspection-maintenance/

T : 01727 860 657
www.tfinstallations.co.uk
info@tfinstallations.co.uk


Our mission is to provide exceptional Fire Alarm, Electrical and Emergency Lighting services from first contact until project completion and beyond. You can rely on our expertise to help design, install and maintain life protection systems.

Fire Safety FURTHER INFORMATION 73 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Hydrosense PRO Ultra Legionella test














The world’s rst ultra-rapid test to detect all the Legionella pneumophila serogroups 1-15
Really easy to use – anyone can carry out the tests with minimal training
*
98% CONFIRMED
Healthcare-associated Legionnaires’ disease cases caused by Legionella pneumophila
50% of hands-free taps are contaminated with Legionella **

RESULTS IN INU T E S hydrosense-legionella.com
ONE also
–
serogroup
Sources: *bit.ly/3XIOR8y ** bit.ly/3Pupl3n
Hydrosense
available
detects
1
Managing legionella in old buildings
The Water Hygiene Centre on taking action against legionella
Older properties can provide unique problems when trying to manage the water systems especially if the water systems were installed before any of the Water Supply (Water Fittings) Regulations 1999 were in place, as they should not be retrospectively applied, as long as the fittings were lawfully installed at the time. It may also be that the water systems have not been refurbished since the first install. Refurbishment works on older systems may lead to modifications that if improperly done can lead to redundant pipework, dead-legs and dead-ends . These can lead to water stagnation that can provide ideal conditions for bacterial growth such as Legionella.
Legionella risk assessment



All water systems need to be risk assessed and this includes older water systems, especially important if there is no current legionella risk assessment present. Your legionella risk assessment will assess the current installation as far as reasonably practicable but there may be issues with accessing the whole water system.
Access issues

Where there are access issues, there will likely be assumptions that need to be made which might limit the conclusions of the risk assessment. Limitations on the findings of the risk assessment can include: the presence of asbestos which must not be disturbed; a lack of boarding in a loft space meaning that the cold water storage tank cannot be safely accessed for inspection, routine monitoring or a clean and disinfection; and the presence of vermin (rats, pigeons etc.) where there are safety issues relating to excrement. Any assumptions or limitations should be clearly defined in the risk assessment along with recommendations on how to manage the risks identified taking these limitations into account.
What do you do if you cannot access parts of your water system to assess the risk or complete the required tasks in HSG274 Part 2?
Your site-specific legionella risk assessment will identify additional controls, based on the findings of the assessment. E
Legionella 75

One useful activity would be to undertake bacterial sampling, such as routine legionella sampling
F It is likely that additional control measures, above and beyond the minimum requirements of HSG274 Part 2, and/or HTM 04-01 in healthcare settings, may be required if you cannot undertake certain routine tasks. Additional controls might include tasks such as (but not limited to): additional sampling for legionella to ascertain the efficacy of the current regime; increasing the frequency of your Legionella flushing regime; and additional controls such as chemical additions to supplement the temperature controls, especially where temperature control proves to be ineffective. The application of any additional controls should be carefully considered with your independent advisor or Authorising Engineer [Water]
Legionella sampling
One useful activity would be to undertake bacterial sampling, such as routine legionella sampling, to gather more information on the performance of your control regime.
If unsatisfactory results are obtained then a review of your control measures should be undertaken, as your current regime could be ineffective. If satisfactory results are obtained then it can help you demonstrate that what you are doing is effective, especially if you have increased controls over the minimum requirements in HSG 274. It is important to remember though that a ‘not detected’ microbiological result does not mean that there is no risk, and you should focus on maintaining your control measures.
Cold Water Storage Tanks
If your cold-water storage tanks cannot be accessed for safety reasons to carry out the annual inspection then sampling for general bacterial level/TVCs may also provide additional information as to the quality of the water supplied from the tank. This can help reassure you that if bacterial results are satisfactory then it provides evidence that the water system is under control. Always seek access to competent help when planning Legionella sampling regimes and interpretation of results.
Susceptibility
An additional problem comes when there are susceptible populations present, such as healthcare environments where the additional requirements of HTM04-01 need to be implemented, where the risk is higher and possible additional tasks will be required.
In summary, careful risk assessment and application of your control measures, following HSG274 Part 2 (and HTM04-01 in healthcare environments) and any additional control advised in your legionella risk assessment will help you manage your water system. L

For more information about Water Hygiene Centre and our independent advisory services click here

FURTHER INFORMATION
77 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Legionella
Hospitals of the future: digital technology leads the way
2023 marks two significant anniversaries; the 75th birthday of the NHS in England and the 50th birthday of the iconic barcode. While the two may seem worlds apart, they are rapidly becoming more closely linked than many may realise
With more than 10 billion scans each day, the benefits brought by GS1 barcodes extend far beyond retail. When adopted and actively used in clinical settings, the barcode – or more importantly the data it carries – has the ability to transform patient care with a simple scan.
How does it work?
In 2016, the Department of Health and Social Care introduced the Scan4Safety programme1 which centred on the adoption of GS1 standards to uniquely identify every person, every product, and every place.
GS1 standards are most commonly captured in barcodes, and associated with specific data such as a batch number for a product, or NHS number for a patient.
When a barcode is scanned at the point of care or use, the information is captured electronically. This reduces manual processes, decreasing the risk of human error, improving patient safety and driving operational efficiencies.
Initial results show that if Scan4Safety was adopted across hospitals in England alone, more than 3.2 million hours of staff time and nearly £120 million could be saved and re-invested back into patient care.
What could Scan4Safety hospitals of the future look like?
A patient is issued with a GS1-barcoded patient wristband upon admission. The wristband is then scanned along with the room or department barcode used to identify the location they are to be treated in. This captures the patient information and records which ward, department, or bed bay the patient is in.
Each time a medication is administered the product barcode is scanned along with a barcode on the staff ID badge. The same is done for any procedures or interventions to track the implants, medical devices, or products used. All the
relevant data is captured in near real time and stored in the electronic patient record (EPR). This process is repeated at every touchpoint throughout the care pathway, keeping an accurate record and consistent audit trail of every patient intervention. This data can then be shared easily between systems and organisations, providing the transparency and traceability needed to support improved clinical decision making.
The bigger picture
GS1 standards are both system and device agnostic, making it easier to share data between systems and organisations. This can be pooled into national registries, such as the Surgical devices and Implants Information system2, to improve traceability on a national scale. Any patient, product or place identified using GS1 standards will not only be unique in England, but also globally. Should a patient receive care in different countries, their record could follow, supporting initiatives such as the International Patient Summary3. Widespread adoption can help create safer and more efficient hospitals around the world. Combining digital technologies and standardised data at scale is the first step in making this a reality.

www.gs1uk.org/healthcare
1. https://healthcare.gs1uk.org/scan4safety
2. https://digital.nhs.uk/data-and-information/ data-collections-and-data-sets/data-sets/nationalperioperative-data-standard-programme
3. https://www.healthit.gov/topic/global-digital-healthpartnership/international-patient-summary
INFORMATION
L FURTHER
Advertisement Feature 78 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
Written by Glen Hodgson, head of healthcare, GS1 UK
New Cyber Strategy for the NHS
In March, the government set out a new strategy to protect the NHS from cyber attacks. HB looks at what it involves
The government has announced that it will provide a plan to promote cyber resilience across the health and care sectors by 2030 and protect services and patients.
The plan aims to ensure that services are better protected from cyber threats, further securing sensitive information and ensuring patients can continue accessing care safely as the NHS continues to cut waiting lists.
The aim is for all health and social care organisations to achieve cyber resilience no later than 2030.
Through good cyber security, it is hoped that organisations are better able to manage their cyber risk; organisations are better able to protect their patient, service user and staff data: organisations can more quickly respond to and recover from a cyber attack; and people’s trust in the digital systems is increased, so technological innovations can be applied with confidence.
Cyber resilient health sector
In a foreword to the strategy, Phil Huggins, national chief information security officer and Mike Fell, executive director of national cyber operations said: “In an increasingly digitised health and social care service, patients and
service users remain at the core of our vital work helping create a cyber resilient health and social care sector to 2030. While every health and social care organisation must take responsibility for its own cyber security, with national cyber security teams setting direction and providing central support, we must work as one across the system to further cyber resilience to improve the safety of the people we care for.
“Although our cyber defences have improved over the past years and especially since WannaCry in 2017, we know we still have further to go. The 5 pillars in our strategy focus our approach on the most important risks to our most critical systems, while growing our cyber workforce so that we can better tackle threats in the long term.”

The strategy acknowledges that healthcare is more digital than ever before. Over 40 million people now have an NHS login and over 50 per cent of social care providers now use a digital social care record.
According to the Department of Health and Social Care, progress has been made in recent years, and the sector is now much better protected than it was at the time of the WannaCry cyber attack in 2017. E
IT 79 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Secure

I.T.

Environments

congratulates the NHS on its 75th anniversary
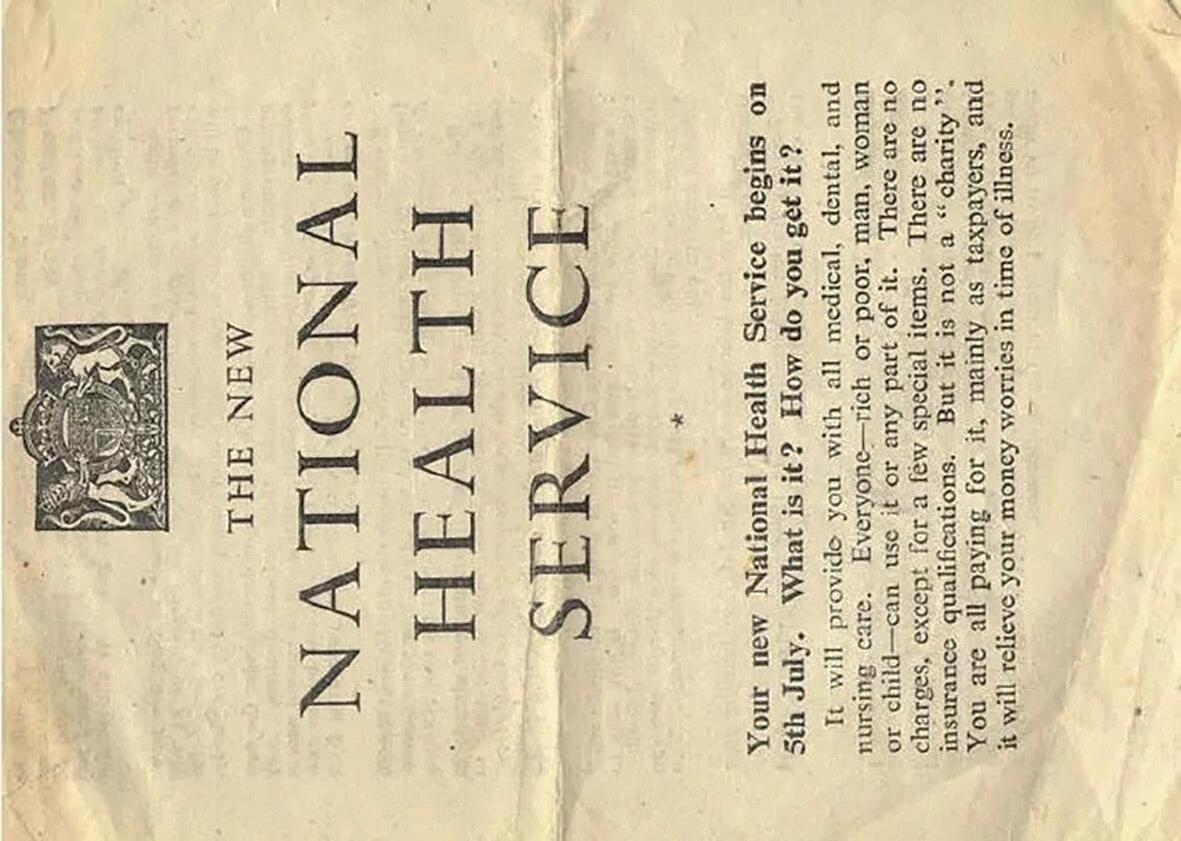
The NHS continually embraces how technology and data help to provide safe and compassionate care to patients and aid communication. We’re not quite 75, however with 20 years’ experience in the healthcare sector, Secure I.T. Environments is incredibly proud and honoured to be part of the digital transformation of the NHS. Here’s to the future. Learn more at www.siteltd.co.uk

SECURE I.T. ENVIRONMENTS LTD. UK-BASED INTERNATIONAL PROVIDER OF SECURE DATA CENTRE SOLUTIONS. OUR PROFESSIONAL SERVICES COVER ALL ASPECTS OF DATA CENTRE DESIGN, BUILD AND MAINTENANCE.
F Cybersecurity as part of care
The strategy also recognises that cybersecurity – protecting devices, services and networks and the information on them from theft or damage – is an essential enabler of providing care and ensures the safety of patients and their information.
In secondary care, devices and systems that need protection include diagnostic machines such as imaging scanners and systems that let hospitals know which beds are free, while in primary care this includes patient booking systems, call and recall facilities, and electronic prescription services.
NHS trusts now have a direct link to NHS England’s Cyber Security Centre (CSOC), which provides real-time protection of any suspicious activity to approximately 1.7 million devices across the NHS network. As well as this, around 21 million malicious emails are also blocked every month.

Health minister Lord Markham said: “We’re harnessing the power of technology to deliver better, safer care to people across the country - but at the same time it’s crucial we’re also bolstering the defences of our health and care services.
“This new strategy will be instrumental to ensure every organisation in health and adult social care is set up to meet the challenges of the future.
“This is an important step to ensure we’re building an NHS which is sustainable and fit for the future, with patients at the centre.”
The strategy sets out different areas of responsibility: health and social care organisations are responsible for their own cyber security; national cyber security teams are responsible for setting direction and providing central support; and ICSs are responsible for bolstering the cyber resilience across their area. However, a unified and collaborative approach is key to improving sector-wide cyber security.
Pillars
The new strategy includes 5 key pillars to minimise the risk of cyber attacks and other cyber security issues, as well as to improve response and recovery following any incidents across health and social care systems including for adult social care, primary and secondary care. The five strategies cover identifying the areas of the sector where disruption would cause the greatest harm to patients, such as through sensitive information being leaked or critical services being unable to function; uniting the sector so it can take advantage of its scale and benefit from national resources and expertise, enabling faster responses and minimising disruption; and building on the current culture to ensure leaders are engaged and the cyber workforce is grown and recognised, and relevant cyber basics training is offered to E
IT
81
However, a unified and collaborative approach is key to improving sectorwide cyber security






Serious games Change thinking & behaviour. www.FocusGames.com sales@focusgames.com Games and simulations that work face-to-face and online. · CPD & mandatory staff training · Diversity & Inclusion · Patient engagement 150+ games to improve education, training & engagement: · Engage, inform & enrich · Improve knowledge & confidence · Change thinking & behaviour If you wish to address a certain subject, we can create a new game for you. Please contact us to discuss your idea. Create your own game
F the general workforce. The remaining two are embedding security into the framework of emerging technology to better protect it against cyber threat and supporting every health and care organisation to minimise the impact and recovery time of a cyber incident.


The five pillars explained above are listed as: focus on the greatest risks and harms; defend as one; people and culture; build secure for the future; and exemplary response and recovery.
The desired outcomes for pillar 1 by 2030 are: a common understanding of risks and how they may vary is shared across the sector; visibility of the attack surface is increased; cyber security mitigations are proportionate to the threat and potential harm; and powers under NIS regulations are clearly understood and used proportionately to address cyber risk and improve resilience of the most critical
organisations. This will be achieved by creating a common language for measuring and recording cyber risk; developing and improving national capabilities to maximise sharing of information, services and products across the sector; and gathering data using national systems to build a system-wide threat picture, setting out proportionate mitigations for key risks and harms.
The desired outcomes for pillar 2 by 2030 are: health and social care organisations work in partnership on their cyber security, sharing data, learning and resources to improve sector-wide resilience; threat intelligence and detection across the NHS is co-ordinated nationally for rapid response and alerting; national teams set clear expectations of leaders and boards on the organisational risk they are held accountable for and implications for the wider sector if those risks are realised; and leaders and boards make full use of available services to respond to the greatest risks and harms to their organisation. This will be achieved by making clear roles and accountabilities to cyber risk across the sector; collaborating with partners across government, the care sector, commercial third parties and academia as well as across local organisations to ensure alignment and share learning and providing central support to cyber security initiatives aligned with national and government priorities.
For pillar 3, the desired outcomes by 2030 are: cyber security is recognised as a vital profession within health and social care; the NHS attracts and retains a diverse cyber security workforce; a ‘just culture’ for cyber regulation is championed across the system; and everyone understands their role in ensuring good cyber security E
IT 83 Issue 23.3 | HEALTH BUSINESS MAGAZINE
F and acts accordingly. To achieve this, national and regional cyber security teams will: clearly identify roles and responsibilities to manage cyber risk, making clear that cyber security is essential to patient and service user safety; embed cyber security decisions into multi-disciplinary national and regional forums to ensure a holistic cyber security culture; and deliver on a plan to grow the cyber workforce and embed a cyber profession across both the health and social care sectors, including in developing career pathways for cyber.
The desired outcomes for pillar 4 by 2030 are: organisations understand emerging risks and how to manage them; the critical supply chain risk is managed and resilience is increased across the critical health and social care supply chain; new services, support and standards are secure by design; and standards, underpinned by the CAF, are clear, understood and aligned. This will be achieved by working flexibly to adapt as new threats and requirements emerge, including developing horizon-scanning functions to anticipate future threats and opportunities; developing engagement with our most critical suppliers, not limited to software providers, to assure their cyber security; and developing pathways to improve communication with and across critical suppliers when responding to a cyber event or vulnerability.
Finally, the desired outcome for pillar 5 by 2030 is that national, regional and local responses to a cyber incident minimise the impact of a cyber attack on patient and service user care. To achieve this, national and regional cyber security teams will: publish expectations for incident response and reporting; lead on national incident response ‘dry run’ exercising, applying and developing plans for responding to and recovering from, a cyber attack; work with the NCSC to manage the technical response to a sector-wide attack.
The full implementation plan is set to be published in summer 2023 and will outline the detailed activities and defining metrics to build and measure resilience over the next two to three years.
National cyber security teams are also set to work with local and regional health and care organisations to achieve the visions and aims of the strategy. This includes enhancing the NHS England CSOC, publishing a comprehensive and data-led landscape review of cyber security in adult social care, and updating the Data Security and Protection Toolkit (DSPT) to empower organisations to own their cyber risk.

Threats
The strategy outlines the threats that the health and social care sector resists every day: phishing and other malicious emails; automated scanning for common software vulnerabilities; and attempted fraud.
The most significant cyber threat is identified as ransomware. The strategy explains that this is used in profit-seeking attacks, very often staged by organised criminal groups. However, the increasing proliferation and commercial availability of ‘ransomware as a service’ means that attacks are no longer limited to sophisticated groups.
Ransomware attacks can lead to the complete loss of clinical and administrative IT systems, which in turn, results in disruption to health and social care services, such as postponed operations, diverted ambulances and forcing staff to use paper-based contingency measures without access to electronic health records.
Research by the US Cybersecurity and Infrastructure Security Agency (CISA) showed that US hospitals that had suffered a ransomware attack were more likely to suffer worse health outcomes, including increased mortality.
IT
However, ransomware attacks are increasingly being used for data theft and extortion with the threat of data leaks.
Other potential threats include state actors seeking to access sensitive information, or people working in or near to the health and social care sector seeking to misuse their privileged access.
The listed threats pose a risk to patient and staff safety, as well as to public trust in the system.
Challenges
Though the NHS is in a better position to defend against cyber attacks than previously, some challenges still remain. Some challenges are the same as those faced by other sectors, including recruiting and retaining a workforce with the right skills, adapting to new technology and moving away from legacy devices. However, other challenges are particular to the health and social care sectors, including the size and complexity of the system, its geographic distribution across the nation and the layered nature of its governance.
High operational pressures mean it can be challenging to prioritise finite resources to address competing risks, priorities and pressures in a sector with varying working environments and high operational demand with many systems required to run 24/7. This has been exacerbated by pressures caused by the pandemic.
The size and diversity of the sector means it is difficult to set standards that can apply universally.
Supply chain vulnerabilities are also a factor that needs to be taken into account. Providers use many suppliers, and these suppliers have their own supply chains, creating multiple layers of risk.
Unclear accountability means health and social care leaders may find it difficult to dedicate time and resources to their organisation’s cyber security.
As well as this, a UK-wide shortfall of cyber professionals means it is difficult to hire and retain the experts needed to improve cybersecurity.
New digital, data and technology mean it can be challenging to ensure the cyber security of new products. On the other hand, legacy technology can be challenging to monitor and replace as it becomes outdated and more vulnerable to cyber attacks.

Lord Markham said: “Our vision and aims are ambitious and will require engagement at all
levels of the health and social care sector. We must build and maintain this engagement in the shared understanding that cyber security is a foundational business need that we must prioritise if we are to ensure patient and service user safety.”
Huggins and Fell added: “Our strategy to 2030 will allow us to work flexibly and adaptively in response to a changing world. Our Cyber Futures programme will take the lead, bringing forward important initiatives to make the 5 pillars of the strategy a reality. We are committed to publishing a detailed implementation plan to illustrate the progress. “This strategy and the operations underpinning it directly support and enable better health outcomes. Improved cyber resilience will assure availability of services, protect valuable data, and build patient and service user trust in our systems. This is an ambitious body of work, but working collaboratively across the system we can have a genuine impact on people’s safety and wellbeing in assuring the vast and varied digitised care and support services provided across the sector.” L
85 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Further information is found here and here.
FURTHER INFORMATION IT
Other potential threats include state actors seeking to access sensitive information
Innovative solutions for reducing paper use
SMS Technology is revolutionising the healthcare industry by developing software that improves workflows and eliminates the use of paper in hospitals
SMS Technology is a leading software company that has revolutionised the healthcare industry by developing innovative solutions that eliminate the need for paper in hospitals. Their cutting-edge software is designed to streamline workflows which leads to improved patient care, and enhance efficiency in healthcare institutions by reducing the time spent to collate and analysis data.
The problem
Traditionally, hospitals and healthcare providers have relied on paper-based systems to manage audits and other critical information. These systems have proven to be cumbersome, time-consuming, and error-prone, leading to a significant amount of paperwork that needs to be managed, stored, and archived. The use of paper in healthcare also poses a significant risk to key information, as important information can be easily misplaced or lost. Additionally, paper-based systems are often not easily accessible or shareable, leading to inefficiencies and redundancies in the healthcare system.
The solution
SMS Technology recognised the need for a more efficient, streamlined system to manage

information in hospitals and healthcare facilities. Their software solution provides a comprehensive, centralised platform for managing critical data whilst being able to be fully customisable, so it gives the ability to create new documents in minutes due to legislation or requests from the board. The SMS Technology software is designed to be user-friendly, with an intuitive interface that allows healthcare providers to access records and data quickly and easily. The system is customisable, allowing hospitals to tailor the software to their specific needs and requirements.
The benefits
The benefits of the SMS Technology software are numerous and significant. By eliminating paper-based systems, healthcare providers can improve patient safety, reduce the risk of errors, and increase efficiency in their operations. Here are some of the key benefits of the SMS Technology software.
Increased efficiency
A significant benefit of the SMS Technology software is the increase in efficiency. With paperbased systems, healthcare providers often spend significant amounts of time searching for and managing information. With the SMS Technology software, this information is easily accessible and can be quickly retrieved, allowing healthcare providers to spend more time with patients and providing quality care.
Cost savings
The SMS Technology software can also help healthcare providers to save money by reducing the costs associated with paper-based systems. By eliminating the need for paper-based records,
Advertisement Feature
86 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
healthcare providers can reduce the costs associated with printing, storing, and archiving paper records and also the time it takes to populate and duplicate the data recorded.
Enhanced data security
The SMS Technology software also provides enhanced data security, ensuring that patient information is protected from unauthorised access or theft. The system is designed with advanced security features, including encryption and multi-factor authentication, to ensure that information is kept confidential and secure.
Improved collaboration
The SMS Technology software also enables improved collaboration between healthcare providers, allowing for more efficient communication and information sharing. Healthcare providers can easily access information, facilitating faster and more effective decision-making.

The future
The SMS Technology software has already made a significant impact on the healthcare industry, with hospitals and healthcare providers adopting the system to improve operations, patient care and increase efficiency. The future of healthcare is increasingly digital, and the SMS Technology software is at the forefront of this digital revolution. With ongoing development and innovation, SMS Technology is committed to providing healthcare providers with the most advanced and effective solutions for managing hospitals information and data. By leveraging cuttingedge technology and a commitment to patient safety and efficiency, SMS Technology is helping to transform the healthcare industry for the better whilst also having strong corporate and social values. L FURTHER
sms-tech.org
Advertisement Feature
INFORMATION
87 Issue 23.3 | HEALTH BUSINESS MAGAZINE
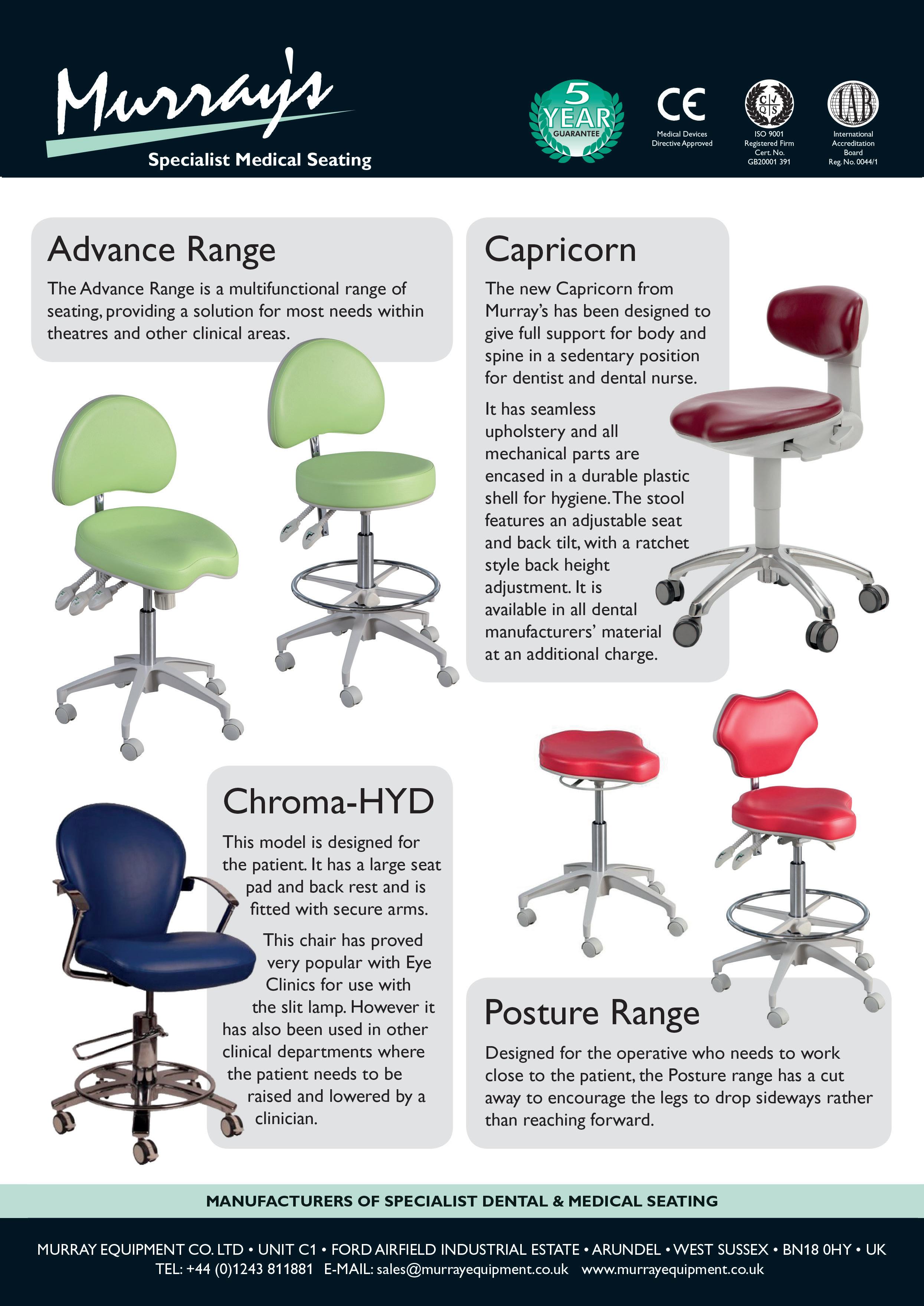
Boosting health data-enabled research
Dr Erik Mayer, director of the Digital Collaboration Space, on how this newly opened space in Paddington will play a vital role in boosting health data-enabled research
Health data routinely collected by the NHS is well understood to be a valuable asset for driving innovation in medical research and improving patient care. Ultimately, harnessing its power will not only transform our nation’s health but help shape the future of the NHS. While there is an increasing demand for health data-enabled research, there are longstanding barriers that are preventing researchers, clinicians and industry from realising its full potential. A key challenge is how to navigate the fragmented NHS data sets available and at a speed that helps us rapidly to translate research into better care.
At Imperial College Healthcare NHS Trust, we recently opened our Digital Collaboration Space – a dedicated facility for translating data-driven insights into person-centred care, while addressing the current challenges of dataenabled research. The space, next to St Mary’s Hospital in Paddington, houses our growing digital health team from the National Institute
for Health and Care Research (NIHR) Imperial Biomedical Research Centre, a partnership between the Trust and Imperial College London. This is the first new initiative within the Trust’s Paddington Life Sciences development. The vision for this new life sciences cluster is to improve health and reduce inequalities by connecting communities, healthcare, research and industry, centred around St Mary’s Hospital, to deliver health innovation and social and economic value. Through our new Digital Collaboration Space, we want to build awareness and understanding of the power of data to improve health and healthcare, bringing in additional funds and ideas to create even more benefits for patients in north west London. As a team, we provide state-of-theart analysis of the huge amount of health data routinely collected across Imperial College Healthcare’s five hospitals and collaborate with the wider North West London Integrated Care System on a complementary data set from a diverse population of 2.4 million people. Our digital health team provide secure and managed access to de-identified NHS data for industry and academic partners. Access to the data is carefully governed and is only granted for research that has a direct public health or care benefit. E

Technology
89


www.healthbusinessuk.net 90 Issue 23.3 | HEALTH BUSINESS MAGAZINE Turning plastic waste into ecoconscious clothing Tons of plastic dumped in the sea every year Of plastic is currently recycled Plastic takes hundreds of years to break down 14Million 9% 100Years
At Upcycled Medical, we make medical clothing and accessories from recycled plastic, which is sourced from our oceans and from landfills. We offer a sustainable alternative to other brands, and have the lowest verifiable carbon footprint in the world. Our zero-waste production process reduces energy usage by 39%, and CO2 emissions by 36%.
products are made from 65% recycled plastic post-consumer PET and 35% organic cotton, which means they last longer, and can be recycled at the end of their working life. Order now and find out more at: www.upcycledmedical.com T: 0330 133 4192 | E: info@upcycledmedical.com
We’ve made it our mission to change things
Our
F Real-world evidence
Our Trust has a long track record in research and innovation, and we undertake hundreds of clinical trials and gather data from well over a million patient contacts each year. But simply holding data isn’t enough to drive research. Our specialist data scientists curate and organise these complex, mixed data sets to answer research questions as effectively as possible. This offers a great advantage as using real-world evidence from clinical settings ensures our research has direct relevance to the health needs of our diverse communities. We can also tap into the extensive clinical research trial capacity of the North West London Clinical Research Alliance, within which our Trust has the highest patient recruitment to research trials.
We can also build an understanding of how clinical staff use new digital tools, which is important for testing and evaluating their effectiveness. For example, a recent study using real-world clinical data from more than 250,000 patients admitted to hospital with a suspected heart attack found that a simple blood test measuring levels of a protein linked to inflammation would better identify those at high risk of dying within three years, opening the door to more targeted treatment for heart attack patients. Our team also demonstrated that they can provide population health data monitoring across the 2.4 million north west London citizens in close to real-time, with the potential to improve diagnosis of conditions.
Public support for data use
All of this is dependent on the public’s confidence that their personal data is protected. This is why we only use completely anonymised data within our secure data environment, iCARE, and work closely with patient groups on scrutinising research projects. We also collaborate closely with patient groups to ensure we’re responding to the most pressing local health needs, such as respiratory disease, infection, pregnancy and premature births, and cancer. Public support for use of healthcare data is strengthened when people see the benefits of its use, as happened in the pandemic when routine de-identified healthcare data was used at scale to answer research questions and led to new treatment options for patients.
Embedded in the community
Our location in Paddington, close to St Mary’s Hospital, means we are well-placed to encourage and host research collaborations

between clinicians, academics, data scientists and partners from industry and local communities. St Mary’s is local to communities in north Westminster, north Kensington and south Brent, which are among the most deprived areas in the country and where over half the population come from a Black, Asian or minority ethnic background. These communities have significant disparities in health outcomes and life expectancy. There is a 14-year life expectancy gap between Westminster’s most and least deprived. The new Digital Collaboration Space, and Paddington Life Sciences more widely, will enable us to improve not just healthcare but also wider health and wellbeing. Our focus on social and economic value and inclusion is critical for meeting local needs, making our clinical research relevant, and inspiring our clinical and research staff. And with our local partners, including life sciences and technology businesses already located in Paddington, we are already working on wider initiatives to increase access to healthcare and clinical research, skills and job creation, and digital inclusion. We will ensure that data-driven insights and digital innovation are at the heart of our work, connecting communities to a future of better health. L
www.imperial.nhs.uk/paddington-life-sciences
Technology FURTHER INFORMATION
91 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Our Trust has a long track record in research and innovation
Overcoming communications challenges in healthcare facilities


Implementing new communication technologies in a business is not always straightforward. This could be for multiple reasons – for example, there might be a wide deployment area, a high number of employees that the technology needs to cater for, or safety standards that must be upheld
The latter applies particularly in healthcare settings. While communication is a key aspect for effective patient care, as well as ensuring medicines are handled safely, strict safety protocols must always be observed. Any tools and technologies need to be compliant with these regulations so that they can be deployed. There is no one-size-fits-all solution for healthcare facilities either – each deployment must meet the needs of the department, whether it’s patient-facing or ‘behind the scenes.’
Importance of hygiene
One challenge that healthcare companies share when implementing a new cordless telephony infrastructure is their ability to meet hygiene requirements. Usually, individual countries will have their own health and safety standards – NHS England, for instance, released its own national standards for cleanliness in 2021. Healthcare providers may also have classified premises, such as sterile workshops, within their facilities, where they need to avoid contamination. Upholding standards is important for their own safety, as well as that of their patients.
Dealing with different environments
Taking into account those high hygiene standards, technology has to be carefully selected to ensure it does not become a source of contamination and can control infection. Bacteria and viruses can be spread on equipment that is being
handled regularly – and it’s easy for staff to overlook phone hygiene during busy days. Moreover, new devices must be able to adapt to rapid changes of temperature and humidity – particularly in sterile environments where steam-sterilising temperatures will remain at either 121 degrees fahrenheit or 132 degrees fahrenheit to kill microorganisms. This is why phones with military grade certified robustness and an antibacterial finish that can withstand alcohol-based solutions required for disinfecting clean rooms, are the best option for healthcare providers.
Finding the right solution
When implementing new communications equipment, product availability and cost will always play an important part. Using a base station can also make deployments of phones across larger sites such as hospitals simpler, connecting multiple devices through a single point. Snom’s IP-DECT phones meet a range of needs and can be deployed throughout healthcare facilities, providing staff with state-of-the-art technology and functionality to make their day-to-day jobs easier. L


Advertisement Feature
FURTHER INFORMATION www.snom.com
92 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
Feel connected at work
The Snom M90 is specially designed for use in hospitals. For this purpose, it is equipped with a special protective cover certified according to JIS-Z2801, which provides no breeding ground for bacteria.



Hygiene environments




snom.com
Bringing technology to rural practices
Dispensing Doctors are integral to primary healthcare in rural communities. However, sometimes they can be a little bit behind the rest of the NHS when it comes to technology. HB spoke to Laura Wright at Stoneleigh Surgery in Milnthorpe, Cumbria, the first dispensing doctor in England to deploy end-to-end EPS for medicines management
Dispensing doctors are practices with an additional licence to dispense prescriptions on site. They are usually found in rural areas, with limited pharmacy provision. There are currently around 1,000 dispensing doctor surgeries in England, dispensing around 6.5 million prescriptions a month. That’s around 7 per cent of the national total of prescriptions. Dispensing doctors are different from pharmacies, in that they don’t have a pharmacist. However, the process for dispensing is similar – a prescription is generated, labelled and bagged in the same way.
Prescriptions
The software that dispensing doctors use is often an extension of the prescribing system and can be quite basic. Community pharmacies generally have better technology. Up until now, there has been no EPS (Electronic Prescription Service) system for

dispensing doctors, despite it being available for pharmacies for 18 years. Therefore, every prescription is written on paper. In comparison, 95.3 per cent of prescriptions from community pharmacies are issued electronically.
The NHS has a target of 100 per cent of prescriptions being issued electronically, but dispensing doctors are dragging down the figures.
New technology
A new independent dispensing system has been accredited by the NHS for Dispensing Doctors to process electronic prescriptions. Titan is not linked to any particular GP software and can operate in any site. The new system aims to improve efficiency, without the use of paper. Other benefits include barcode scanning, to reduce dispensing errors; artificial intelligence, to improve efficiency; and digital workflow, so everyone knows where everything is.
Laura Wright at Stoneleigh Surgery in Milnthorpe, Cumbria is the first dispensing doctor in England to use the new technology. She answered some of HB’s questions.
Dispensing doctors
We first asked about the importance of dispensing doctors and their benefit to rural communities. Laura said: “Dispensing doctors are more important to rural communities than ever before. With large chain community pharmacies closing their small rural shops and moving their dispensing into large hubs, dispensing doctors provide the personalised, local service that patients want and need.
We know all of our dispensing patients and our fantastic team go above and beyond every day to look after them. If there is ever
Technology 94
a query concerning a prescription, we have the patient’s clinical record at our fingertips and can resolve any issues, far quicker than a community pharmacy could.”

How it works
We asked how the new system works, how it is different to the old system and what benefits this brings. Laura replied: “Titan allows us to electronically nominate ourselves, enabling the dispensary to receive prescriptions from any of our six sites via EPS. This means that our GPs no longer have to sign prescriptions by hand which we believe saves the GPs on average between 20 and 30 minutes a day. Being able to nominate ourselves has also streamlined our processes for acute prescriptions issued at different branches. In terms of our dispensing processes themselves, using the new system has reduced the time taken to dispense a prescription by probably 50 per cent when compared with the system that was previously in place.
“The new system automatically detects the manufacturer, pack size, batch number and date of expiry from the FMD code which our previous system did not.
“It is also possible to dispense the items from the prescription in any order, which we could not do previously.
“We no longer need to manually count, package and post paper prescriptions for
NHSBSA submission at month end as these are sent electronically.”
WiFi problems
Change always comes with challenges, as Laura explains: “There haven’t been any real issues since its implementation in November 2022. The only issue that we have had is that, due to the poor WIFI signal in our practice, we are unable to use the ‘Edo’ handout facility which would further improve the patient experience by sending an email to them when their prescription is ready to collect. We are working with TITAN to find a work around for this problem though.”
On the other hand, there have been several benefits: “We are finding that both our workload and patient expectations are increasing. With the greater workload, we are encouraged to streamline our processes and make ourselves as efficient as possible. Titan is simple to use, has excellent safety features and saves time for our dispensary staff, clinicians and GPs.”
There has also been a noticeable difference for patients, as Laura explains: “Patients can benefit from their prescription being ready sooner and will benefit from the notification email once this facility is up and running.” L
https://digital.nhs.uk/services/electronic-
Technology FURTHER INFORMATION
prescription-service/for-dispensing-doctors
95 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Dispensing doctors are more important to rural communities than ever before
Using technology to tackle the backlog
HB spoke to Dr Patrick Davey, a cardiology consultant from Northampton on how remote consultations are being used to tackle the backlog
The National Consultant Network (NCN) service facilitates communication between health professionals and specialists. There are 200 NHS consultants in the NCN service who receive around 100,000 calls and messages a year from GPs looking for advice on their patients.
Can you explain how the NCN works?
“Imagine you’re visiting your GP with an issue and your GP is unsure about your symptoms. Previously they would probably refer you to a specialist, which might involve a long wait for a hospital appointment. Then Consultant Connect came along with tech that allows GPs to reach an NHS consultant quickly for specialist advice.
“The GP selects the relevant specialty and the tech will call through a list of numbers, bypassing the hospital switchboard. If they can’t answer it moves on to the next. On average calls are answered in 30 seconds.
“From the call, the GP can be advised on what the appropriate next steps are for their patient, often an unnecessary hospital visit is avoided, but if it is required, the patient is sent to the right department. Ultimately it means patients receive better, faster care.”

In what situations can it be used?
“The tech can be used for advice and guidance. I remember a call I had from a GP whose patient had ongoing chest pains. He’d been previously diagnosed with pericarditis, which is inflammation of the lining of the heart.
“Using Consultant Connect, the GP contacted me to check if the ongoing symptoms were compatible with the diagnosis. During the call I found out the patient had taken cocaine. I told the GP to refer the patient to the local cardiology department to be absolutely certain the cocaine had not damaged the patient’s heart, as this would have implications for the future.
“The patient was reassured that a specialist had been consulted and his GP was able to provide clear next steps for his treatment.”
What problems can this system help to address?
“Seven million people are currently waiting for treatment, and clearing those waiting lists can be daunting for those working in the NHS and frustrating for the patients left waiting. We know the pandemic put huge pressure on the system and has caused backlogs.
Technology 96 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
“What’s great is Consultant Connect is now helping ease some of those pressures, by limiting unnecessary visits and by getting patients seen by the right specialists.

“Once upon a time there was a disconnect between GPs and specialists in hospitals. If you had a question about your patient you’d have to call through to the switchboard, be put on hold while the person at the other end did their best to connect you to the right person. Consultant Connect has made this process far easier.”
What are the benefits for patients?
“Simply, it improves the patient’s experience.
“Often GPs will call me up when the patient is still in the room. The patient hears their GP speaking to a consultant about their symptoms. Immediately, they have more confidence in what is going on and feel that something is being done.
“When patients are referred to secondary care, they often have no idea for weeks or months whether that referral has been reached or what is happening. In the meantime, the patients’ anxiety goes up while they’re waiting for an appointment.
“By using Consultant Connect, patients can be seen quicker and get assurance on the decision that we’re making. If they don’t need to be referred they won’t be, and if they do they’re referred to the correct specialist. Overall, they’ll have a much better experience and won’t have to go through unnecessary stress.”
What are the benefits for the NHS?
“There are inevitably times when GPs are not sure about a patient’s symptoms - when they have to put their hand up and say ‘look, I have a problem. I don’t know the answer’. It is a mark of quality in GPs that they can ask for help when needed and seek advice for what to do next.
“So when GPs ring me up and start explaining the problem, I think to myself that this person really values my opinion. It’s not a long conversation, maybe a minute or a couple of
minutes. But when they have a problem and I can help, it’s the most wonderful interaction.
“GPs have been hammered with the message that they mustn’t send patients to hospital. When they call consultants, they’re seeking approval for what needs to be done. There are a lot of grey areas, so it’s often a question of managing uncertainty in a safe way. GPs are very grateful because a problem shared is a problem halved.”
Why did you decide to get involved in the project?
“When I started using the service, I actually found it really enjoyable. I’ve heard it said that at heart, we’re all in the Anglo Saxon hut telling stories and listening to stories. So when GPs call you, you’re just listening to the story. I found interacting with that service delightful - I felt I provided useful advice for GPs.
“I often say to colleagues: what’s not to like about the service. There tends to be initial resistance to new technology and changedifferent people had different perceptions of that, but I was very enthusiastic about change.” L
https://www.consultantconnect.org.uk/ what-we-do/national-consultant-network/
Technology FURTHER INFORMATION 97 Issue 23.3 | HEALTH BUSINESS MAGAZINE
Seven million people are currently waiting for treatment, and clearing those waiting lists can be daunting for those working in the NHS
New procurement framework for hospitalat-home technology
NHS SBS has a new technology framework, for the procurement of remote patient monitoring solutions

NHS Shared Business Services (NHS SBS) brings a new framework agreement to the market enabling health and social care providers to procure remote patient monitoring solutions that can reduce the burden on the NHS, at pace. Comprising lots endorsed as recommended buying channels by NHS England’s Central Commercial Function, it comes at a time that sees longer hospital waiting times, hospitals being fuller than pre-pandemic and a discharge crisis. Consequently, the use of technology like connected medical devices, monitoring apps and video consultations – which enable remote monitoring and treatment of people
with long term conditions at their place of abode, is being ramped up in a bid to create virtual wards and free up more hospital beds for those who most need them.
The coronavirus pandemic forced many hospitals and social care providers to suspend their routine and elective activities, creating a backlog of patient appointments. Longer hospital waiting times have been exacerbated by discharge difficulties. As many as one in three hospital beds in parts of England are occupied by patients who are well enough to be discharged but a chronic lack of social care means many do not have suitable places to go.
Technology 98
Given 19 out of 20 hospital beds are full, and 14,000 are being occupied by someone clinically ready to leave but unable to be discharged to the appropriate care setting, NHS England (NHSE) has, in its delivery plan for recovering urgent and emergency care services , stated “its ambition to improve to 76 per cent of patients being admitted, transferred or discharged within four hours by March 2024”.
Virtual wards
The plan also sees virtual wards (hospitallevel care at home) playing an important part in expanding capacity by joining-up health and care outside of the hospital. Virtual wards combine technology and remote monitoring and advice to allow hospital-level care, including diagnostics and treatment. They can also replace the need for admission and facilitate people being able to leave hospital sooner, safely. As such, NHSE is looking to deploy virtual ward beds to scale up capacity from 7,000 to 10,000 in autumn, ready for winter. Integrated Care Systems (ICSs) bring together providers and commissioners of NHS services like hospitals and GP practices, local authorities and other partners (including charities, voluntary, community and social

enterprise organisations), to collectively plan and deliver health and care services to meet the needs of their respective populations. As part of NHSE’s ambition, ICSs are expected to deliver virtual ward capacity equivalent to 40-50 virtual ward beds per 100,000 people by December 2023, with virtual ward services developed across ICSs and provider collaboratives, rather than individual institutions.
Framework
NHS SBS has designed the second iteration of its framework agreement, Technology Enabled Care Services, in response to the need within the NHS and social care sector to free up beds, reduce the backlog of appointments, speed up patient discharge, and reduce the burden on the stretched social care sector. Launched in January, the £150 million framework agreement was created in collaboration with NHSE’s Transformation Directorate, local authorities, national technology enabled care (TEC) policy makers like TEC Cymru, as well as industry bodies including the TSA (TEC Services Association). It focuses on three key themes; Remote Clinical Monitoring, Patient Empowerment and Social Care monitoring. E
Technology
ICSs are expected to deliver virtual ward capacity equivalent to 40-50 virtual ward beds per 100,000 people
99 Issue 23.3 | HEALTH BUSINESS MAGAZINE
F Organisations can choose to purchase goods and services from 19 carefully selected best-of-breed suppliers, each of whom have undergone a competitive and rigorous selection process in order to be included on the framework agreement.
The free-to-access framework agreement provides a convenient, compliant and costeffective method of purchasing technology enabled care for all publicly-funded organisations, including GP Practices, hospitals, health centres, emergency services, housing associations and local authorities. Suppliers can introduce any additional new products and services that meet the standards set out and are within scope throughout the framework agreement’s lifetime.
The framework agreement is categorised into 6 Lots (service types), each representing a combination of goods and/or services which can largely be defined as either clinical (for the NHS and healthcare organisations) or social care-based (for local authorities and housing associations).
The core elements include:
Remote Clinical Monitoring (including Virtual Wards)
Remote clinical monitoring platforms and services connect to vital sign devices that aid in the monitoring, reporting and analysis

of a patient’s acute or chronic condition from outside the hospital or clinical setting, for instance, blood pressure or blood glucose levels. They facilitate real-time understanding of a patient’s disease state, enabling clinical decisions to be made.
Alarm Receiving Centre Platforms
These software platforms allow the remote connection of telecare and telehealth devices like movement sensors which aid in the detection of falls, raising an alarm call if unusual activity is detected, or pill dispensers which release medication at the appropriate time, triggering an alarm if it is not removed from the dispenser.
Digital Alarm Services and Peripherals (social alarms)
Facilitate the automatic and remote nonclinical monitoring of individuals using a combination of behavioural and environmental sensors, alarms or other means linked to a communications device. Collectively, they help manage risk and support independence. Social alarms include pendants which users can activate to call for assistance in urgent situations, through to wireless systems which can detect possible problems with smoke or gas. Sensors automatically raise an alarm alerting a monitoring centre which contacts a carer.
Technology 100
Intelligent Activity Monitoring
A non-intrusive system of sensors, machine learning and automatic data communication to facilitate monitoring ‘activities of daily living’ and detect deviations from previous patterns - crucial to assessing the ability of an individual to live independently in their community and in the early detection of upcoming critical situations. The data generated can capture insights that pre-empt longer term subtle changes in behaviour.
Patient Controlled Personalised Healthcare Records


Allow individuals to access their healthcare record and related data in one place. The supplier solutions on offer are complementary to the NHS App and can empower the patient/citizen to add, access and share their health information with healthcare professionals in various settings.
Combined Solutions
Designed to enable procurement of a combination of digital solutions from suppliers on the framework agreement.
Routes to procurement
There are two routes to procuring services using the framework agreement – further competition or direct award. The direct award route allows the purchaser to award a contract directly to a supplier, enabling them to obtain goods and services at speed.
The further competition process (sometimes called mini-competition) re-opens competition under the framework agreement. Procuring parties can ask suppliers listed to submit proposals and costings to help select the most appropriate products and services and drive further efficiencies.
Adam Nickerson – head of category, digital & IT procurement frameworks at NHS SBS said: “The coronavirus pandemic added to waiting lists and the knock-on effects of a lack of beds in the NHS and social care sector. The Technology Enabled Care Service framework agreement enables ICSs and provider collaboratives - from housing authorities to local authorities, to strategically source and quickly buy a mixture of goods be it a single, bundled or a fully managed service, which works across a region. It means they can better plan and deliver joined up services and improve the health of the population across their regional wing of care.” L
For further information contact: sbs.hello@nhs.net
Social alarms include pendants which users can activate to call for assistance in urgent situations
Technology
FURTHER INFORMATION 101 Issue 23.3 | HEALTH BUSINESS MAGAZINE
ADVECO
01252 551540
enquiries@adveco.co
https://adveco.co
For award-winning specialist design, supply and service of sustainable water heating for new build or refurbishment projects. Adveco can advise and support gas, electric or hybrid applications with a complete range of heat pumps, solar thermal collectors, hot water cylinders, boilers, water heaters, packaged plant rooms and ancillaries.

HEALTHCARE ESTATES
MGPS SERVICES LTD

0345 652 4901
info@mgps-services.com
MGPS Services Ltd are an independent company accredited to ISO 9001:2015 and provide Medical Gas training, AE Services, AP Duties, Testing & Commissioning, Compliance Audits, System Validation & Schematic Drawing, writing of Operational Policies, Project Management and various other Medical Gas Consultancy services.
SIGNS
LASTING IMPRESSIONS (SIGNS) LTD

01308 456721
Lasting Impressions have been supplying health & safety signage to the NHS for over 20 years. With our large range of stock signs, or manufacturing your custom requirements, we can offer a fast turnaround at affordable prices. Call our sales team today.
Product Finders
sales@lastingimpressionsonline.co.uk www.lastingimpressionsonline.co.uk
ENERGY
102 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
TROJAN
01684 295 782 sales@trojanbins.co.uk

TROJAN BINS offers a comprehensive range of bins and sack holders covering recycling, the medical sector and external venues. An accredited ISO9001 and ISO14001 business and approved supplier to the NHS. We deliver your needs.
CleanEvent specialise in providing cleaning and other soft services for the Healthcare, Education, Leisure and Retail Sectors. We are a flexible supporting partner to the NHS with the ability to provide fully managed staffing solutions at short notice for short, medium and long-term placements.

D J HILL ENGINEERING


02920 790784 | 07725 947217
info@djhillengineering.co.uk
www.djhillengineering.co.uk
Welcome to the Hospital Bedstacker. The Bedstacker is available in 3, 4 and 5 Bed configurations for vertically stacking hospital beds. The Bedstacker has a small footprint with simple push button operation, full safety guarding and safety locking gates. D J Hill Engineering Services Ltd can supply and fit nationwide and also provide extended warranties and servicing.
103 Issue 23.3 | HEALTH BUSINESS MAGAZINE
BINS
WASTE & RECYCLING
www.trojanbins.com
CLEANEVENT SERVICES LIMITED 44 + (0) 333
0130 Info@ceworld.com www.CEworld.com
210
MISCELLANEOUS Product Finders
HOOPER SERVICES
023 9263 0276
sales@hooperservices.co.uk


With 30 years of expertise in cleaning and facility management solutions, Hooper Services have you covered. After a free site survey, we can recommend bespoke packages from our diverse range of application led cleaning machines, equipment, tools, and white goods. Quote? Maintenance? Free demo? PAT test? Get in touch today!
LANES GROUP PLC

0800 526 488
sales@lanesgroup.co.uk
Lanes Group can help the NHS by offering services such as CCTV drain surveys, which can identify any issues in the hospital’s drainage systems, such as blockages or leaks. We can then provide solutions such as drain unblocking, repairs, and maintenance to prevent any further damage or disruption to hospital operations. Effective drainage management can improve hygiene and reduce the risk of healthcare-associated infections.
01280 706640 | 07572 236044
info@quenelles.co.uk
www.quenelles.co.uk
We’re an independent market leading company who benchmark food prices across the industry. We’re impartial, accurate and confidential. Our data ensures you have more control over your catering budget and find opportunities towards improving efficiencies. We give you the assurance that you’re competitive or highlight your opportunities.
104 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
QUENELLES LIMITED
Product Finders
THE SAFER FOOD GROUP
0800 612 6784 info@thesaferfoodgroup.com
Leading online training company The Safer Food Group provides food safety training for catering professionals. As an existing preferred supplier to numerous NHS trusts, we provide food safety, allergy awareness, health & safety and HACCP courses at negotiated partnership prices. Existing infrastructure enables immediate access to flexible, learner driven courses, accessible management data and trusted teaching materials.
TOTAL CLEAN SERVICES LTD
020 7935 5088
Total Clean has a 35 year history of providing commercial cleaning services to the NHS, Hospitals, GP’s, Dental practices, Cosmetic Surgeries and Private practices. We would love to be of service too you too!


TWICE2MUCH
0344 225 2090
Kate.donnelly@twice2much.com www.twice2much.com
Twice2much specialise in Spend Recovery Auditing, involving the review of Client’s historical Accounts Payable spend, not just to identify and confirm anomalies and/or overpayments but also recover the monies from Suppliers. We work unobtrusively with Clients’ Finance, Audit, AP/Fraud Teams, utilising our own expert resources to generate unbudgeted financial windfalls.

105 Issue 23.3 | HEALTH BUSINESS MAGAZINE Product Finders
www.thesaferfoodgroup.com
enquiries@totalclean.co.uk www.totalclean.co.uk
ADVERTISERS INDEX
The publishers accept no responsibility for errors or omissions in this free service
© 2023 Public Sector Information Limited. No part of this publication can be reproduced, stored in a retrieval system or transmitted in any form or by any other means (electronic, mechanical, photocopying, recording or otherwise) without the prior written permission of the publisher. Whilst every care has been taken to ensure the accuracy of the editorial content the publisher cannot be held responsible for errors or omissions. The views expressed are not necessarily those of the publisher. ISSN 1470-0735
Health Business is a member of the Independent Press Standards Organisation (which regulates the UK’s magazine and newspaper industry). We abide by the Editors’ Code of Practice and are committed to upholding the highest standards of journalism. If you think that we have not met those standards and want to make a complaint please contact Polly Jones or Angela Pisanu on 0208 532 0055. If we are unable to resolve your complaint, or if you would like more information about IPSO or the Editors’ Code, contact IPSO on 0300 123 2220 or visit www.ipso.co.uk
106 BUSINESS INFORMATION FOR HEALTHCARE PROFESSIONALS | www.healthbusinessuk.net
Adveco (AWP) 102 Apollo UK 6 Asckey Data Services 8 Avaya 22 B Medical Systems Sarl IBC BeaconMedaes 59 Borg & Overström 54 Brainsparker 30, 38 Calomax 76 Clean Event Services 103 Clinisys UK 14 Cornwall Insight 64 D J Hill Engineering Services 103 Focus Games 82 Fordingbridge 68 Glasdon UK 30 GS1 UK 78 Hooper Services 104 Hydrosense 74 Jones AV 10 Lanes Group 104 Lasting Impressions Online 102 MGPS Services 56, 102 Multitone Electronics 28 Murray Equipment Co 88 Philips Monitors IFC, 12 Pinpoint 34 Powell System Engineering 48 Powerstar 26 preOx.RS GmbH BC Primed Halberstadt 4 Quenelles 104 Radar Healthcare 16 Sanondaf UK 45 Secure IT 80 SMS Technology 86 Snom 92 TF Installations 73 The Safer Food Group 105 Total Clean 105 Trojan Bins 103 Twice2much 20, 105 Upcycled Medical 46, 90 Veolia ES (UK) 62, 66 Wernick Buildings 60 Yeoman Shield 24 Yewdale Corporation 53

IAP-Adatper-Set






















New treatment kit for measurement of Intra Abdominal Pressure (IAP) during Abdominal Compartment Syndrome (ACS).
IAP-Adapter-Set includes IAP-Adapter, 3-way valve, double check valve, syringe, spike and tubes.
• easy & quick handling
• effective measurement

• reliable & replicable results




• Step by steps video instruction
Product page

preOx RS technology for health preOx.RS GmbH Obertiefenbacher Straße 16 D-65614 Beselich Tel. +49 (0) 6431-21579-0 Fax +49 (0) 6431-21579-10 E-Mail sales@preox.de www.preox.de
▶