




















Before we head into the next winter period , to avoid experiencing repeat issues year on year regarding internal structural conditions Cornerstone are committed to providing an opportunity for all interested parties to learn more of the reasons behind these repetitive issues and how they can be readily adopted within any organisational policies plus landlord and manager procedures for a proactive solution.
With many years of expert, trusted, independent experience surveying properties following reports of damp, condensation and mould, Cornerstone remain committed to sharing their diagnostic findings and consequently, the reasons behind these issues alongside credible and understandable recommendations for long-term occupant health and engagement.
With a number of complaints relating to untimely responses, actions and guidance, there is a new opportunity to get ahead of these issues with a unique called-for framework aimed at delivering timely guidance aligned to the problem.
A new Property Health App lication has been developed however, before this exciting tool is available, Cornerstone are seeking key interested persons or organisations for complimentary use alongside defined feedback of its resultant success with a key alignment to receiving your opinions regarding its design and simple functionality. After all, this guidance mechansism is for you and your occupants to uphold a healthy structure for living, learning and working in.

The process will resonate with having key experts to hand with a timely convenience to suit you 24/7 365 days of the year. And, after resident access to onboard guidance and simplified measures undertaken, your complaint can be sent with supporting images to the landlord for immediate investigation. Suffice to add, only when a complex issue requires resolving or defined training and/or specific surveying guidance is required, will there be associated fixed fee s for Cornerstone to assist resulting in a transparent framework for all concerned with a known confidence level it will assist solving these ongoing issues.
To learn more and resgister your interest for complimentary use, contact Cornerstone now …
Email: info@cornerstone-ltd.co.uk Tel: 0345 846 0955
Web: www.cornerstone-ltd.co.uk
023 9200 9270

A £200 million funding package is set to benefit public health services, and is set to boost addiction recovery services, sexual health clinics, and local nurses, among other incentives.
Announced on 7th February, the investment is part of the government’s plan to shift healthcare away from secondary care and into the community, in a move to take pressure off of emergency services and hospitals. This is a key factor of the government’s Plan for Change.
This new funding will power essential services such as smoking cessation programmes, addiction recovery, family and school nurses, sexual health clinics, local health protection services and public health support for local NHS services. This investment is the biggest realterms increase in spending after nearly a decade of austerity and budget cuts from 2016-2024.
Funding for public health grants will be increased by a 5.4 per cent in cash terms (three per cent in real terms) compared to last year’s funding. This investment will focus on prevention and community care, building stronger, healthier communities more resistant to illness nationwide.
Then minister for public health and prevention, Andrew Gwynne, said: “Lord Darzi’s investigation into the NHS has found that children are sicker today than a decade ago, and adults are falling into ill-health earlier in life.
“Prevention is better than cure. If we can reach people earlier and help them stay healthy, this extra investment will pay for itself several times over in reduced demand on the NHS and by keeping people in work...


A report from the National Audit Office (NAO) has revealed that the government building maintenance backlog is at least £49 billion. This includes maintenance backlogs across hospitals, schools, prisons and more.
The NAO found that Ministry of Defence properties, schools and NHS properties have a backlog totalling more than £10 billion each and make up 88 per cent of the total backlog. The remaining 12 per cent is made up of sites including prisons, job and assessment centres, courts, and museums and galleries.
Due to limited government data, the true cost of full remediation is not known, but the Office of Government Property (OGP) believes it could be substantially higher than estimated.
Building failures are impacting delivery of public services. On average, between 201920 and 2023-24, approximately 5,400 clinical service incidents occurred in the NHS every year due to property and infrastructure failures. It can also affect productivity, staff retention, and the ability to meet environmental targets.
The data shows that maintenance backlogs have been rising for at least a decade; for instance, between 2013-14 and 2022-23, NHS England’s backlog increased steadily, at an average of £800 million per year (in 2023-24 real terms).
The NAO has recommended that the government implements measures to address the backlogs. This includes mandating to departments and arms-length bodies a standardised definition of the maintenance backlog, so the true figure across government can be calculated and including data on the ...
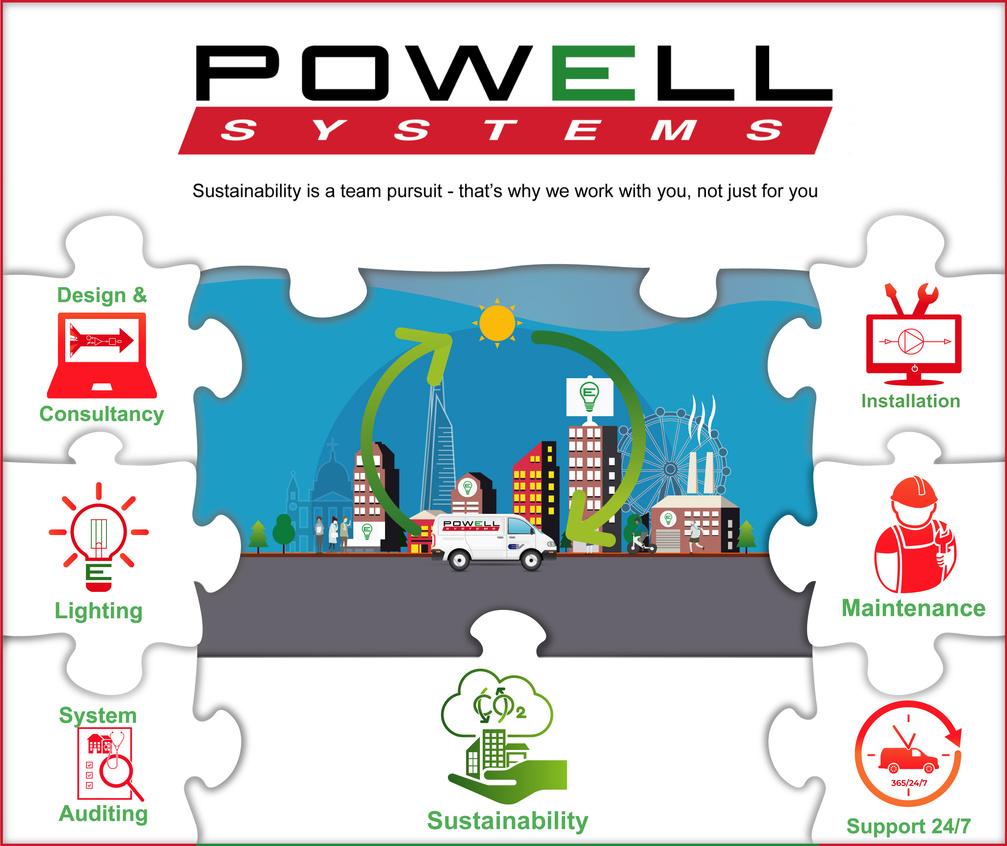
Every step of the way, Powell Systems offers you Services that are synonymous with sustainability covering a full range of close/tight control, lighting control and Building Energy Management Systems (BEMS).
We offer a full support service for any area of your business: from the more complex lab, operating theatre and sensitive facility areas to the everyday, office, industrial and community spaces
Because sustainability is a team pursuit, Powell’s aim is to work with you, not just for you.

The government has announced plans to leverage technology and AI tools to streamline public services, including the NHS, improve data sharing and reduce costs.
The plans come following the publication of a review that shows that the country relies on a poor system, with outdated methods of communication. For example, HMRC takes 100,000 calls a day and DVLA processes 45,000 letters.
The technology secretary has launched his department as the digital centre of government to overhaul digital services and target £45 billion in productivity savings every year.
The new plans include scrapping the need for people to register a death in person and removing the need to post an advert in the local paper before getting a license to drive a lorry.
There will also be changes to data sharing, which could help central government departments, like HMRC and the Department for Business and Trade, share data with each other and local councils more seamlessly to crack down on fraud.
A new team will be housed in the Department for Science, Technology and Innovation (DSIT) to join up public services and there will be training programmes to help civil service technologists become AI engineers.
Science secretary Peter Kyle said: “Sluggish technology has hampered our public services for too long, and it’s costing us all a fortune in time and money...


go ahead
The government has confirmed funding and a future roadmap of implementation for their New Hospital Programme, following a review that the government’s plan to build “40 new hospitals” by 2030 was behind schedule and without adequate investment.
The Infrastructure Project Authority (IPA) has also labelled the previous scheme “unachievable’” highlighting major issues with the schedule and budget.
In May 2023, the previous government announced that £20 billion would be funnelled into the project, but it was never delivered.
The new plan, affordable and transparent, aims to give £15 billion of new investment over consecutive five-year waves, averaging £3 billion a year. Now, the government has inherited buildings and equipment across the NHS that are in poor states, disrupting patient care and hindering staff.
Lord Darzi, in his investigation, found that the NHS was starved of funding throughout the 2010s, with £37 billion underinvestment, leaving hospitals with roofs fallen in and leaking pipes that freeze in winter.
Building a sustainable, long-lasting NHS estate is a key component of the government’s Plan for Change, which will see the health service revitalised and less time waiting for those needing an appointment. At the Budget, chancellor Rachel Reeves announced that health capital spending in the NHS is set to increase to record levels of £13.6 billion in 2025-26...
For any stakeholders you want to reach get people focussed insights you can act on


Our experienced team of researchers provide the personal touch during your project, at every point, from designing the questionnaire through to presenting the findings and helping you get the insight that you can take action on





£3 million investment is to go towards the Women’s Health Research Wales from Health and Care Research Wales, supported by the Welsh government, on top of the already-existing £750,000 for other dedicated women’s health research projects.
Published in December, the women’s health plan for Wales delivers plans for women’s health research, with a budget of £750,000 in April 2025. Welsh universities are also encouraged to bid for funding to create a Women’s Health Research Centre.
£3,013,936 has been secured, as part of a wider £49 million investment package announced by Health and Care Research Wales. This will support 17 research centres across the country.
Minister for mental health and wellbeing, Sarah Murphy, said: “This new research centre, the first for women’s health in Wales, will be crucial in helping us to better understand women’s experiences, develop more effective treatments, and ensure our health services truly meet women’s needs at every stage of their lives.
“I hope the centre will attract and retain leading researchers in the field and help ensure Welsh women’s experiences and needs drive our women’s health plan for Wales.”
The Women’s Health Network part of the NHS Executive, is to work with Health and Care Research Wales and the academic community in the future to improve the women specific health evidence available in Wales.
National clinical lead for Women’s Health, Dr Helen Munro, said: “The is an encouraging step towards achieving a more equal healthcare...

NHS care targets halved for faster patient access: READ MORE
New chief medical officer for Wales announced: READ MORE
Wales launches Social Care Workforce Partnership: READ MORE
AI to revolutionise cancer care: READ MORE
Social care reform for Scotland: READ MORE
Increase in NHS capacity planned for Scotland: READ MORE
NHS SBS launches new decarbonisation framework: READ MORE
The first event in which frontline NHS staff have the opportunity to put forward what they would like to see from the government’s 10 Year Health Plan has taken place in Liverpool. NHS staff were joined by NHS England directors to hear their views on what they think the future of the NHS should look like.
Joining NHS staff were NHS England’s chief nursing officer, Duncan Burton; chief midwifery officer, Kate Brintworth, primary care medical director Dr Clare Fuller, and North West medical director for primary care, Dr Paula Cowan.
Staff were nominated to attend across the board, including GPs, nurses, optometrists, consultants, porters, pharmacists, and more, to ensure any impact on local services is as minimal as possible.
This comes as part of the biggest listening event the NHS has ever seen, with seven nationwide public debates and a series of online staff events having already taken place, which were also about making a 10 Year Health Plan for the future. A further six listening events are scheduled through February and March, with Sheffield, Sutton, Coldfield, London, Reading, Peterborough, and Taunton to host these conversations...



Alpine Works Limited, established in 2002, has built a renowned reputation for it’s extensive expertise in the healthcare sector, particularly for delivering complex installations of specialist medical facilities across many major London hospitals.
As a leading mechanical and electrical building services company, Alpine Works also undertake building fabric projects and planned preventative maintenance, meeting client demand for a single-source partner through our 24/7, 365-day emergency helpdesk service.






Following the formation of a Labour government in July, Wes Streeting, the new secretary of state for health and social care, commissioned the peer and former surgeon Lord Ara Darzi to lead an independent investigation into the NHS in England. The report, published in September 2024, shed light into the “critical” state of the NHS, and shaped the government’s later allocation of funding towards health and social care in the Autumn Budget. HB takes a look at how this money is to be spent

The state of the NHS estate independent investigation of the NHS , Lord Darzi refers to the NHS as in “critical condition” in his detailed outlined of the challenges facing the NHS and its subsequent, often subpar, performance. Over a decade of severe austerity and public spending cuts, the NHS has been “starved of funding”, with a backlog maintenance bill of over £11.6 billion, a £37 billion shortfall, and productivity flagging. The effect of inadequate investment is palpable: the waiting list for elective treatment 7.6 million in June 2024, and ten per cent of A&E waits are longer than 12 hours. Lord Darzi’s report highlights the best courses of action for future funding and the forthcoming 10-Year Health Plan , which the government built into its Plan for Change and the Autumn Budget 2024
The Autumn 2024 Budget Rachel Reeves’ first budget as Chancellor was the biggest tax-raising budget since 1993 , and set aside huge increases in public sector investment. The Department for Health and Social care received an extra £22.6 billion for 2025-26 spending, bringing up the total to £214.10 billion, and providing the highest E
F growth rate (four per cent) since before 2010, excluding COVID-19 pandemic years. Of this, NHS England’s budget is set to increase from £171 billion in 2023-24 to £192 billion in 202526, and the capital budget is set to rise to over £13 billion next year, 80 per cent more than prepandemic spending (2028-19) in real terms. This is a particularly welcome investment as a report from the Institute for Government identified that the capital budget is often not spent effectively or in full, and has routinely been raided to plug day-to-day running costs, leading to a crumbling estate in dire need of upgrades.
Six months into governance and three months since the Autumn Budget, Labour have started to rollout their fiscal policies and changes to healthcare, but progress remains slow for plans that span up to decades to fully realise. With their Spending Review set to be published in the coming March , we take a look at where the Health and Social Budget has been delegated and what the government have already implemented.
Waiting lists for elective care have skyrocketed, with the record being 7.77 million in November 2023 compared to 2.4 million in 2010. In 2010, 200,000 people waited more than 18 weeks for care, with 20,000 of these waiting a year. By June 2024, over 300,000 people had waited over a year, which is 15 times as many. As it stands, one in nine people across England are on a waiting list.
In 2010, 94 per cent of people attending a type one or type two A&E were seen within four hours, but by May 2024, this figure had dropped to just over 60 per cent. In 2023, more than 100,000 infants waited more than six hours in A&E, and ten per cent of all patients were waiting for 12 hours or more. The Royal College of Emergency Medicine has estimated that these long waits for emergency care cause 14,000 deaths every year, more than double all of the British armed forces’ combat deaths since the NHS was founded in 1948.
The NHS constitutional right to care within 18 weeks from a GP referral was established in 2010, but the target has never been met, and it has clearly only gotten worse. The government have since reiterated the NHS pledge that 92 per cent of patients should start consultantled treatment within 18 weeks, and bolstered this with additional funding to deliver an extra two million NHS operations, scans, and appointments. This averages to 40,000 extra

£1.5
billion has been earmarked for over 30,000 NHS procedures, 1.25 million diagnostic tests, as well as new beds
appointments a week across England. £1.5 billion has been earmarked for over 30,000 NHS procedures, 1.25 million diagnostic tests, as well as new beds.
Another key part of reducing waiting lists is investment in surgical hubs, which are designated for elective care, and are protected from being used for emergency treatment, reducing waiting times for both departments. Research by the Health Foundation has found that in their first year, trusts in England with surgical hubs carried out 21.9 per cent more high-volume, low-complexity elective surgeries than they would have without a hub, amounting to around 29,000 more procedures.
£70 million will also go towards new radiotherapy machines for cancer treatment, which will be welcomed following Darzi’s findings that only around 60 per cent of genomic tests are being completed on time. More than 30 per cent of patients are waiting longer than 31 days for radical radiotherapy, and so more machines should help to streamline cancer treatment processes.
The 2023-24 Estates Returns Information Collection (ERIC) shows that the total cost to run the NHS estate is £13.6 billion, and yet the cost the eradicate maintenance backlog tops it by £0.2 billion. Maintenance backlog is the estimated cost of bringing NHS estates or buildings back to a minimum expected standard, and many necessary renovations have been put off due to focusing on eradicating dangerous reinforced autoclaved aerated concrete (RAAC).
With 90 per cent of the NHS budget going towards day-to-day costs, the capital budget necessary to get the NHS estate back up to standard has remained flat at around £5 billion, a decrease in real-terms. Lord Darzi described the NHS as suffering from “capital starvation”, with Charlotte Wickens from The King’s Fund drawing attention to: “the neglect of the NHS estate led to 751 incidents to patients and staff, such as through equipment failures or infection outbreaks.” In 2022-23, 13 hospitals each day were disrupted by failing or crumbling buildings.
The Autumn Budget puts £1 billion towards reducing the backlog of critical NHS maintenance, repairs, and upgrades, as well as £102 million towards upgrading dilapidated GP surgeries; 20 per cent of GP buildings are older than the NHS
Around 70 per cent of local authority spending goes towards treading water in adult and children’s social care provision
itself. A recent announcement in January 2025 saw the government reevaluating and committing to a revised New Hospital Programme, since its announcement under the previous government in May 2023 where £20 billion was pledged but never delivered. The government’s review of the scheme will deliver £15 billion of new investment over five consecutive years, starting with hospitals constructed using RAAC until 2030, and then moving onto deliver the rest of the 40 new hospitals promised.
Around 70 per cent of local authority spending goes towards treading water in adult and children’s social care provision, so the Budget’s £1.3 billion extra for local authorities this year was much appreciated. This included £600 million ringfenced exclusively for social care. Better social care keeps people out of hospitals and prevents illnesses and injuries before E


More than £2 billion has been earmarked for NHS technology and digital to run essential services and boost NHS productivity
F they happen, taking the pressure off secondary healthcare facilities. A further £86 million has been earmarked to increase the Disabled Facilities Grant which will support 7,800 more adaptions to homes for those with social care needs, again reducing hospitalisations and promoting communitybased care.

From April 2025, the carer’s allowance will increase its weekly payout from £151 to the equivalent of 16 hours at National Living Wage, recognising the work carers do behind the scenes in the community.
The Health Foundation, however, draws attention to an analysis that found that £1 billion extra would be needed to meet the growing demand for adult social care, meaning that £600 for both adult and child provision is unlikely to be sufficient. We are yet to find out whether more detailed provisions for adult social care will be laid out in the 10-Year Plan
Lord Darzi found that as of June 2024, more than one million people were waiting for community services, many being children and young people. Community services for mental health have been particularly affected by previous funding cuts : in April 2024, one million people were waiting for mental health services, with 345,000 people waiting more than a year. These waits disproportionately affect children and young people, as 109,000 of those waiting for more than a year are under 18.
The NHS budget, Lord Darzi found, had not been spent where it should be: too much money was thrown at hospitals, and not enough in the community. This forms a disastrous cycle where underfunded primary care pushes people to seek secondary care, further adding pressure to hospitals with too few beds and too long waiting times. The poor state of social care means that 13 per cent of NHS beds are occupied by people waiting for social care support or care that would be more appropriate outside of a hospital.

The UK, in comparison to other high-income countries, has almost 16 per cent fewer qualified GPs, and years of cuts have meant that the number of nurses working in the community fell by five per cent between 2009 and 2023, while the number of health visitors dropped by nearly 20 per cent between 2019 and 2023. It is a welcome relief, then, that a core pillar of the government’s plan to resuscitate the NHS involves greater focus – and investment – in shifting care from the hospital to the community. Alongside £1.5 billion towards specialised surgical hubs to triage patients, the Budget has promised to deliver £26 million to open new mental health crisis centres, which will reduce pressure on A&E services. Further funding to deliver 200 upgrades to GP surgeries across England has been announced, increasing productivity and allowing practices to deliver more patient appointments.
More than £2 billion has been earmarked for NHS technology and digital to run essential services and boost NHS productivity. This investment will work to free staff from administration burdens so they can focus on productive work, ensure all trusts have Electronic Patient Records, and improve cyber security. Lord Darzi identifies harnessing technology as a key factor in both reviving the NHS and also for the government to focus on in their upcoming 10-Year Health Plan, and finds that capital starvation is a leading cause of poor technological advancement in the NHS. By using capital funding as an effective reserve for daily spending costs, previous governments have had insufficient investment in digital technologies and too few medical scanners.
focuses on prevention through its £460 million towards pandemic preparedness
Recently, the UK has rolled out AI to predict those at risk of frequently attending A&E before they can join the waiting list.
The power of prevention is best showcased through the Diabetes Prevention Programme, which reduced the risk of type two diabetes by nearly 40 per cent. Type two diabetes costs the NHS £8.8 billion each year, which is almost nine per cent of its budget. Shifting the focus from sickness to prevention, then, cuts cost and also prevents illness and related deaths.
Alongside boosted funding towards GP practices, diagnostic equipment, and digital technology, the Budget focuses on prevention through its £460 million towards pandemic preparedness. The money will go towards replenishing personal protective equipment (PPE), vaccines, medicine stockpiles, as well as critical health infrastructure like high containment laboratories.
Lord Darzi’s report found that the COVID19 pandemic was one of the key factors contributing to its financial and productive burnout, and that following the most austere decade in the NHS’s history, the health service was too unequipped, underfunded and understaffed to deal with the colossal pressures of a global pandemic. The allocated funding strives to make sure this does not happen again.
The government’s pledges are ambitious, expensive and, for the most part, yet to be materialised. But such structural change to a system that has been progressively ransacked for over a decade does not happen overnight, or even over three months, especially when the majority of the government’s plans span beyond this parliament. The Autumn Budget set the precedent for their fiscal policies and overall attitudes towards health and social care, but we must look towards the Spending Review and the 10-Year Health Plan, both set to be published in the spring, for further finetuning of their financial policies, and hope that the government manage to meet their ambitious targets deploying investment where they highlighted it was most needed. L
The announcement follows news last year that Marlin Equity Partners had made significant investment in Radar Healthcare, which enabled the company to accelerate growth and expand its product offering


Radar Healthcare, a provider of digital risk management and quality compliance software, is excited to announce a strategic investment in EIDO Healthcare (“EIDO”), a leading provider of digital consent and patient information solutions. Together, these two established providers of healthcare solutions will combine their expertise to deliver high-quality tools for organisations across the health and care landscape, supporting safer and more effective care.
This exciting development brings together two highly complementary organisations with decades of knowledge and a shared vision for driving positive change in healthcare. By uniting Radar Healthcare’s innovative technology and EIDO’s trusted informed consent solutions, the combined organisation is poised to accelerate growth and enhance its offering for customers in the health and care markets across the globe.
“This is an exciting new chapter for Radar Healthcare,” said Paul Johnson, CEO of Radar Healthcare. “We are thrilled to have EIDO joining us to grow our ecosystem and enhance what we can offer to healthcare and care providers. Both organisations share a deep passion for improving healthcare, and together, we can address new challenges while continuing to deliver exceptional service and innovation to our customers.” The combination will enable broader functionality, deeper technical expertise, and more opportunities for healthcare and care teams to improve outcomes. Reflecting a commitment to customer-centric innovation, Radar Healthcare and EIDO will also engage with healthcare providers through customer forums, ensuring their feedback shapes future developments and supports the delivery of intuitive, impactful solutions.
“At EIDO, we are proud of our long-standing reputation for providing trusted patient information solutions,” said Matthew Ravenscroft, CEO of EIDO. “This strategic investment from Radar Healthcare allows us to build on this legacy, combining our strengths to better support healthcare providers and empower patients with clear, reliable information. This will allow us to enhance digital consent processes through our suite of resources designed to support healthcare professionals and reduce the risk of litigation as well as enhance the patient experience. We look forward to embarking on this transformative journey together.”
This news follows a significant investment in Radar Healthcare last year from Marlin Equity Partners, which backed the company to accelerate growth and expand its product offering. The integration with EIDO is another step forward in driving innovation within healthcare, and both companies are committed to delivering exceptional value to their customers.
“We are excited to work alongside EIDO following the strategic investment from Radar Healthcare,” said Chris Clasper, a principal at Marlin. “Both organisations have a proven commitment to excellence and are united in their passion to offer their customers the best possible digital solutions to achieve their goals.”
Further updates about this partnership and its benefits for customers will be shared in the coming months.

Radar Healthcare empowers health and social care organisations to make a meaningful impact on patient safety and quality of care. By blending digital innovation with real-world healthcare expertise, Radar Healthcare enables providers to not only meet regulatory standards but to actively spot trends, prevent incidents, and drive continuous improvement. Designed with flexibility and adaptability in mind, and with a deep understanding of the daily challenges in health and care, Radar Healthcare is dedicated to evolving alongside the industry, delivering a system that is valued for its role in shaping safer, more effective care.
EIDO is a trusted provider of digital consent and patient information solutions, specialising in creating clear, accurate, and accessible content to support informed consent in healthcare. With decades of experience, EIDO helps healthcare providers deliver safe, effective care by ensuring patients have the information they need to make well-informed decisions about their treatment. The modular digital informed consent solution supports deployment into the patient pathway, either as standalone modules or as a complete solution. Known for its commitment to quality and innovation, EIDO works with healthcare organisations globally to empower both patients and clinicians in achieving better outcomes.
Marlin Equity Partners is a global investment firm with over $9 billion in capital commitments. The firm is focused on providing corporate parents, shareholders and other stakeholders with tailored solutions that meet their business and liquidity needs. Marlin invests in businesses across multiple industries where its capital base, industry relationships and extensive network of operational resources significantly strengthen a company’s outlook and enhance value. Since its inception, Marlin, through its group of funds and related companies, has successfully completed over 250 acquisitions. The firm is headquartered in Los Angeles, California, with an additional office in London.

Designed as both a functional handrail and robust crash rail, all in one stylish design, it’s easy to install and maintain.
Available as two independent sections, each offered in a variety of colour options that can be mixed and matched. The Contour blends seamlessly into any interior designs, providing support for those in need, while also fending off impact damage from heavy wheeled equipment and people usage.
In this article, Simon Taylor, estates strategy director, NHS Property Services explores how NHS Property Services is optimising healthcare spaces, unlocking funding, and tackling maintenance challenges to create a more efficient and patient-focused NHS estate
Last December, a number of NHS Trusts declared their buildings unfit for purpose; this is nothing new and has been in and out of the media headlines for years.
The warning from these Trusts came months after the recommendations from Lord Darzi that singled out capital investment as a major area of concern identifying a £37 billion shortfall.
And the National Audit Office recently published their report revealing at least £49 billion maintenance backlog across government buildings. The NAO found that MoD properties, schools, and NHS properties have a backlog totaling more than £10 billion each, making up 88 per cent of the total backlog.
Added to the major financial constraints is the level of confusion around the many capital and revenue funding methods.
NHS Property Services looks after 10 per cent of the NHS estate – that is around 3,000 buildings.
In our recent funding report , estates, finance and strategy leaders shared their concerns and told us what the key barriers are to delivering an NHS estate for the future.
84 per cent of estate leaders surveyed stated that barriers to funding are due to a lack of understanding of the options and these have a real impact on the success of funding applications and total funding pots being leveraged.
So, we at NHS Property Services welcome that long-term estates funding is under the spotlight once again. We know there are ICBs and Trusts that are missing out right now on funding opportunities, through developer contributions. E






F Our approach is to provide better access to the funding opportunities on offer and to make informed financial choices to ensure the release of additional capital focuses by deepening NHS leaders’ understanding of their options and sharpening their skills.
As a strategic estates partner, we are helping many ICBs to deliver their estate infrastructure strategies. This includes helping them to make the most of their existing estate and different capital and revenue funding sources available –but we want to help many more.
We want to ensure our customers use every bit of the support and advice from our experts they can to get their property fully functioning and able to offer the best care to patients.
And we will do this by: optimising the existing NHS estate through better use of vacant space, improved utilisation and speed of decision making – all to improve pace of delivery of better facilities; introducing a new approach to estate investment decisionmaking, through a new funding settlement and simplified capital processes; and tackling backlog maintenance and ensuring statutory compliance to improve safety and productivity. We will also be rolling out existing property technology, such as NHS Open Space, property and facilities management CAFM platform and Smarter Building and investing and increasing collaboration between estates resources, keeping skills in-house.
D J Hill Engineering Ltd.
NHS Property Services has raised £541million from the sale of 596 properties for reinvestment
Since the change in Government, more focus has been put on waiting times and how to tackle them. The Prime Minster, Sir Keir Starmer wants three shifts: primary care to community services; analogue to digital; treatment to prevention.
The Institute of Fiscal Studies’ recent report noted the last time the NHS met its target of 92 per cent of patients receiving treatment within 18 weeks was 2015.
NHS Property Services is determined to help our customers achieve these three shifts.
Since our conception in 2013, NHS Property Services has raised £541million from the sale of 596 properties for reinvestment; and we have also delivered surplus land for 8,326 new homes in the past seven years alone, we have cumulatively saved the NHS £364 million.
There are many examples of our work to support the NHS. And our 5,500 colleagues across our organisation continue to work tirelessly to deliver great results. E
NHS Property Services has transformed underused indoor and outdoor spaces into wellbeing hubs and green spaces
F Our Healthy Places programme was expanded last year to increase focus on Community Diagnostic Centres, we announced our most recent construction in December at St Margaret’s Hospital in Epping.
A further Healthy Places project is the Chiswick Health Centre project , where we were able to rationalise inefficient land use and release latent value. The proceeds of the land sale were recycled back into the new health centre development. This was alongside section 106 planning contributions and a grant from the NHSE towards the temporary relocation costs for suppliers.
The new health centre will host three GP surgeries, two NHS Trusts, and the Chiswick PCN (Primary Care Network), delivering a range of primary care and out-of-hospital services to more than 60,000 patients locally.
A joint development with Hounslow Council also formed part of the project and will deliver 55 social-rented, affordable new homes on the surplus land.
Another great example of our work is at St James’ Hospital in Portsmouth. The former asylum was sold in January 2024 and will offer 209 new homes and community facilities in Portsmouth in the future.
One of our growing areas of support, which is particularly beneficial for GPs and hospitals that find patients coming to see them due to long-term stress affecting their health is social prescribing. GPs have told us that a lot of people visit them when they are feeling lonely or isolated and we have responded to their call to help tackle this problem.
Since 2019 we have been supporting the 47 per cent of our customers who are GPs by using our estate to provide social prescribing and green spaces in communities up and down the country. NHS Property Services has transformed underused indoor and outdoor spaces into wellbeing hubs and green spaces that can be used for gardening groups, cookery classes and other types of therapy.
We now have 100 of these across England that bring people together to improve health and wellbeing. One excellent example of these hubs is the Victoria Central Health Centre in Wallasey, Wirral. It helps people with anything from housing to getting back to work to caring for someone with dementia. It is a non-medical service supporting people with problems that can make us feel unwell and are caused by stress.
Pushing our role as a social prescribing facilitator alongside our property expertise means we provide better support to our customers to tackle what they see are the areas holding them back from delivering the best treatment for patients.
As we at NHS Property Services look to the future, we know we have an important role to play in supporting Trusts and GPs; the NHS faces challenging times ahead but working together we can deliver our vision. Because we are part of the NHS, every penny stays within the health system and is reinvested across it so we can continue to focus on delivering brilliant service and building an NHS estate that is fit for the future. M
A webinar run by our town planning experts to help our NHS colleagues learn how to speed up access to funding takes place on 25th February for more information click here. Our handbook which gives expert advice on how to draft business cases can also be found here.




The NHS estate backlog has become a critical issue, with aging infrastructure and delayed repairs posing significant challenges to patient safety and operational efficiency. The importance of Soft Facilities Management (FM) services like laundry, security, waste management, and general upkeep cannot be overstated
These non-clinical services are critical for ensuring the smooth day-to-day operations of healthcare facilities. By investing in effective Soft FM, NHS organisations can alleviate the pressure on their estates, creating safer, more efficient environments for both patients and staff. Three new procurement solutions from NHS Shared Business Services (NHS SBS) are helping them to do this.
As patient demand continues to rise, the NHS requires well-maintained, functional buildings to accommodate staff, treat patients, and support various administrative functions. These facilities, ranging from hospitals and clinics to offices and research centres, are under increasing pressure. Many are in dire need of refurbishment.
The growing backlog of maintenance work and the limited funding for upgrades have left NHS estates in a state of disrepair. The NHS now finds itself in a challenging position: existing buildings need substantial attention, but there’s also a need for new infrastructure to meet the demands of modern healthcare.
The findings from Lord Darzi’s independent investigation into the NHS have drawn attention to the poor condition of its estate, identifying it as a significant barrier to highquality care.
The maintenance backlog is disrupting the delivery of services, with deteriorating conditions affecting health and safety, undermining staff morale, and reducing productivity. These issues further compound E
The £150m linen and laundry services framework agreement provides a comprehensive solution for managing linen across NHS estates
F the NHS’s struggle to tackle patient backlogs and improve overall performance.
A key takeaway from Lord Darzi’s report is the urgent need to modernise the NHS estate to support enhanced patient care. This involves more than just patching up old buildings; it’s about creating environments that contribute to better health outcomes.
Modernising NHS estates is a critical priority, requiring investments in both physical infrastructure and new technologies that can improve the efficiency of healthcare delivery. These upgrades also need to be designed to improve the experience of both patients and staff - spaces that are not only functional but conducive to recovery and well-being.
NHS estate costs and government investment
The financial burden of maintaining the NHS estate is substantial. NHS England has estimated the total cost currently stands at £13.6bn. Of this, £1.5bn is allocated to cleaning and related services, while energy consumption across NHS facilities adds up to 11.1 billion kWh. This financial burden underscores the importance of making strategic investments to address long-term sustainability.
In the Autumn 2024 budget, the government recognised the need for increased investment in NHS infrastructure. A £1bn funding boost was announced to help address the existing backlog of essential repairs and upgrades. Additionally, £102million has been earmarked for the first phase of GP surgery upgrades, marking a significant step toward transforming the primary care estate.
The government is also committed to the New Hospital Programme , a long-term initiative aimed at modernising NHS buildings. Following a review and an update to the project timetable, all planned projects within this programme , backed by £15 billion of new investment, are set to be delivered over several phases, ensuring that NHS facilities across the country are transformed to meet the needs of modern healthcare.
Enhancing operational efficiency with Soft FM solutions
Effective Soft FM is crucial to ensuring the smooth day-to-day operation of NHS facilities. With services such as linen management, waste handling, security, and grounds maintenance, Soft FM plays a pivotal role in creating safe, clean, and welcoming environments for both patients and staff. These services not only help maintain hygiene standards but also support broader healthcare goals, such as improving patient recovery times and enhancing staff satisfaction.
NHS SBS’s three new Soft FM procurement framework agreements — designed to improve operational efficiency and reduce cost — are a response to these needs.
With a combined value of £375m, the framework agreements provide NHS trusts and public sector organisations with quick access to compliant, cost-effective solutions from fully vetted vendors, enabling them to buy solutions and services to manage the upkeep of their estates, at pace. The framework agreements cover essential services that directly impact the operational effectiveness of NHS facilities.
Linen and Laundry Services: supporting hygiene and infection control
The £150m linen and laundry services framework agreement provides a comprehensive solution for managing linen across NHS estates. This includes linen hire, decontamination, repair, and recycling. These services are crucial in maintaining hygiene standards and preventing healthcareassociated infections (HAIs), which continue to be a major concern in hospital settings.
In addition to infection control, it promotes sustainability by recycling old linen and using energy-efficient laundry practices, aligning with the NHS’s net-zero ambitions, helping reduce the environmental impact of hospital operations. The framework’s regional structure allows NHS buyers to source from local suppliers and SMEs, offering flexibility and promoting regional economic growth.
Grounds Maintenance: enhancing patient wellbeing and estate presentation
A well-maintained environment is essential for promoting patient recovery and staff wellbeing. NHS estates require constant attention, from landscaping and pest control to regular cleaning of outdoor spaces.
The £100m grounds maintenance framework agreement provides a range of services that ensure NHS facilities remain clean, attractive, and functional.
In addition to general upkeep, the framework supports sustainability goals. For example, green waste is recycled or composted, and electric-powered tools are used to reduce carbon emissions.
The framework also assists NHS trusts in meeting biodiversity targets as part of their broader Green Plans , ensuring that NHS estates are both environmentally friendly and conducive to health.
Ensuring the safety and security of patients, staff, and assets is a critical priority for NHS organisations. The £125m security services framework agreement solutions offer includes manned guarding, keyholding, and emergency response. This is vital for creating a secure environment that allows healthcare workers to focus on delivering care without concerns about safety.
Security services also protect valuable medical equipment and hospital assets, essential for maintaining high standards of patient care. By streamlining the procurement of these services, NHS organisations can ensure their facilities remain safe and secure, supporting the delivery of uninterrupted care.
One of the key advantages of the new framework agreements is the streamlined procurement process. By offering access to pre-approved suppliers, NHS trusts can avoid lengthy and complex tender processes. This reduces administrative burdens and speeds up the procurement process, enabling NHS organisations to quickly acquire the services they need at competitive rates.
The framework agreements also offer transparent pricing, making it easier for procurement teams to compare options and select the best value solutions. With inclusive access to a diverse range of suppliers — including SMEs — they promote fairness and ensure procurement processes are equitable.
The NHS is committed to sustainability, and the framework agreements align with that

By streamlining the procurement of these services, NHS organisations can ensure their facilities remain safe and secure
vision. From energy-efficient laundry practices to electric-powered equipment, the solutions offered through them reduce environmental impact while maintaining high service standards.
NHS SBS’s supplier evaluation process also included a focus on social value. Bidders were required to demonstrate how they address modern slavery in their supply chains and provide apprenticeships or training opportunities through the delivery of their services. This social value aspect ensures the framework agreements not only contribute to the NHS’s operational goals but also support broader societal and environmental objectives.
NHS SBS plans to roll out three more framework agreements soon, focusing on Building Safety and Fire Compliance, Cleaning and Associated Products and Services and Catering and Associated Services. The additions will enhance its range of Soft FM solutions, enabling it to provide the NHS and public organisations a comprehensive suite of tools to support them with estate maintenance and management. M
For further information contact: sbs.hello@nhs.net


We can cover for when you just need cover for a day / a week - no contracts necessary


Contracts ranging over a year/ multiple years for reliable and efficient servicing in any departments needed
Auxilium Medical Services offers decontamination services for sterilisers, washer disinfectors, endoscopy washers, laboratory & pharmacy ranging from validation servicing and maintenance to weekly testing on a flexible basis
For when you just need a service provider to cover for a few weeks/months we are happy to accommodate to your schedules

Although we do not provide parts, we can attend to any breakdowns to diagnose and fix issues. Let us know if you would like this included in the quote!
Almost 25 years after mandatory surveillance of the superbug methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections (BSIs) came into practice, the vigilant cleaning of hospitals and other healthcare environments is just as important as ever

Awareness and protocols put into place in the early 2000s raised attention towards the cleanliness, infection prevention control (IPC), and management of hospitals across the country, but this was only half the battle: healthcare-associated infections (HCAIs) – that is, infections contracted as a direct result of a treatment in a healthcare setting – are still a major concern in hospitals, care homes, and the wider healthcare landscape.
2023-24 government statistics show that 74 out of every 100,000 people will contract Escherichia coli (E. coli), with almost one fifth of these cases being diagnosed on the third day after hospital admission (hospital-onset). The good news is that up to 50 per cent of HCAIs are estimated to be preventable, and the application of effective IPC measures, such as cleaning, is paramount in reducing HCAIs.
A report by The Health Foundation (November 2015) tracks HCAIs in England from 2000-2015, as well as offering recommendations to further prevent the rise in infection spreading due to poor sanitation and infection prevention methods. Additional statistics by the European Centre for Disease Control (ECDC) estimate that each year 3.5 million patients develop infections within the European Union and European Economic Area (EU/EEA) as a result of healthcare, with 90,000 of these resulting in death. HCAIs are also expensive. The World Health Organisation estimates each year HCAIs cost €7 billion and 16 million extra days in hospitals for patients, which only increases the chance of infecting other patients and causing an outbreak. E


























F HCAIs that received much attention in the UK are MRSA BSIs, notorious in hospitals during the early-mid 2000s, and Clostriodioides difficile (C. difficile), an infection often brought on by antibiotic use that causes symptoms ranging from diarrhoea to life-threatening colon damage. Other common HCAIs include pneumonia and urinary tract infections (UTIs), as they are often correlated with use of invasive devices, like central lines, ventilators, and catheters. HCAIs comprise a wide variety of infections, from those spread through blood, those spread through bodily fluids, and others spread through respiratory droplets. The varied way in which infections can spread begs the need for a comprehensive, all-encompassing method to effective IPC and standardised cleaning protocols to ensure the spread of HCAIs is kept to a minimum, if not eradicated.
Rigorous surveillance, the installation of thorough cleaning practices, and mass media attention have meant that the UK has cracked down on the number of HCAIs. In 2020-21, the total number of E. coli infections decreased by 15 per cent , possibly down to interventions and changes in IPC practices following the COVID-19 pandemic. This number has increased slightly in 2022-23, with 38,757 E. coli infections reported, although 80 per cent of these emerged in the community, not in hospitals. This stands in comparison to 43, 294 E. coli infection s recorded in 2019-20.

All NHS trusts were also required to appoint a director of infection prevention and control to provide a direct line of accountability
The call for national cleaning regulations
Mandatory surveillance of MRSA recorded 7,249 cases in its first year, bringing further attention to more rigorous surveillance and mitigation of BSIs: the problem was now quantified, and action was clearly needed. In December 2003, the chief medical officer at the time published the report, ‘ Winning ways: working together to reduce Healthcare Associated Infection in England ,’ which gave guidance that would later become standard NHS practice and British law. The report emphasised strict aseptic technique when administrating catheters, tubes, and cannnulae to patients, the necessity of durable surfaces that can be easily cleaned, and high standards of hygiene in clinical practice. These are now the pillars of mandatory IPC protocols across the UK.
The following year, NHS England and Wales launched their Cleanyourhands campaign, which turned the tide on common handwashing practice. Rather than letting healthcare professionals assume their hands were clean if visibly so, the emphasis shifted to if hands were safe. When the campaign was launched, the global average rate of hand hygiene was estimated to be around 40 per cent; staff were thus washing their hands roughly half the number of times they should. The cost of the campaign was 0.1 per cent of the cost of HCAIs in England and Wales, and led to a threefold increase in procurement of soap and alcohol handrub. The effects of the campaign can still be seen in hospitals today through alcohol handrub dispensers at all points-ofcare.
All NHS trusts were also required to appoint a director of infection prevention and control to provide a direct line of accountability. It is especially important that IPC leadership is distributed throughout an organisation, with accessible managers in all areas: infection, after all, doesn’t just happen in hospitals, but any venue where healthcare is varied out, be that dentist surgeries, care homes, or GP clinics. E

A key milestone in effective IPC was the publication of the National infection prevention and control manual (NIPCM) for England
F Mandatory surveillances were introduced for Glycopeptide-Resistant Enterococci (GRE) (2003), orthopaedic surgical site infections (2004), C. difficile (2007), Methicillin sensitive s. aureus (MSSA) BSIs (2011), and E. coli (2011), as part of efforts to monitor levels of HCAIs in hospitals. Further campaigns that stressed the importance of healthcare hygiene and IPC to reduce HCAIs include ‘bare below the elbow ’ guidance to ensure hand decontamination (2007), the Safer Patients Initiative by the Health Foundation (2011), Matching Michigan) (2018) to decrease central line infections in over 200 intensive care units (ICUs) in England, as well as Sir Robert Francis’ report into Mid Staffordshire NHS Foundation Trust (2013). Following serious neglect of care and cleaning standards at Stafford hospital 2005-09, the report recommended reviewing staff training programmes and firmer standards of cleanliness and hygiene.
Recurrent outbreaks of HCAIs, differing levels of hygiene standards across trusts, and reports like the Francis inquiry highlighted the need for government legislation to standardise rigorous IPC by embedding it into the law. In 2008, the Department of Health published a report emphasising the importance of cleanliness to
prevention infection, stressing the lives lost and the cost of cure: the report estimated it cost between £4,000 and £10,000 more to treat a patient with a HCAI during their hospital stay. The Health and Social Care Act (2008) made the Care Quality Commission (CQC) the regulator of all health and adult social care services across England, and all providers of healthcare are required to register with the CQC to comply with their fundamental standards. The CQC’s fundamental standards, now revised and updated several times since 2008 (including in 2014 following changes proposed by Francis), detail 16 essential standards that care must never fall below, including principles on patient safety, the cleanliness of healthcare settings and their equipment, and that all treatment be appropriate: this is an important detail in the face of growing antimicrobial resistance (AMR).
A key milestone in effective IPC was the publication of the National infection prevention and control manual (NIPCM) for England (2022), which details the implementation and compliance with criteria set out in the Health and Social Act 2008, Code of practice on the prevention and control of infections and related guidance. The NIPCM is an adoption of a Scottish manual of the same name, published ten years prior, and details comprehensive cleaning protocols to ensure IPC in healthcare settings, providing a standardised approach for all the UK. The NIPCM details ten elements of standard infection control precautions (SICPs), and gives detailed
instructions on when to wash hands with soap and water and when to rub hands with alcohol gel, correct respiratory and cough hygiene, as well as appropriate use of personal protective equipment (PPE), which must always be close to the point of use and disposed of immediately if single-use.
Further instructions include the safe management of care equipment, which must be either sterilised or disposed of immediately, to prevent the spread of possible infections from one patient to another, as well as the safe management of the care environment. The NIPCM instructs that the care environment must be: “visibly clean, free from non-essential items and equipment to facilitate effective cleaning”, as well as “well maintained, in a good state of repair, and with adequate ventilation for the clinical speciality”.
Linen must be managed and sorted properly according to categories of cleanliness, and blood and other bodily spillages must be cleaned immediately by staff trained to undertake this safety to prevent the transmission of infection and viruses. Waste should be disposed quickly and safely, and in the correct bag: yellow stripe for offensive waste and orange for clinical infection waste. Following the Health and Safety (Sharp Instruments in Healthcare) Regulations in 2013, healthcare organisations must have arrangements for the safe use and disposal of sharps, such as sufficient provision of information and training to employees. This is especially impertinent when improper use of equipment such as needles could result in the transmission of bloodborne viruses like MRSA and human immunodeficiency virus (HIV).
The Royal College of Nursing offers further instruction on these principals, such as appropriate use of indwelling devices in patients, and maintaining accidental exposure to blood-borne viruses, both of which are key in both the prevention and mitigation of infections in patients, visitors, and healthcare staff. A report after 90 patients died in C. difficile outbreaks 2004-2006 found that, alongside poor cleaning standards , one of the failings in IPC was having patients’ beds too close together. C. difficle cannot be screened like MRSA, making cleanliness and correct IPC paramount.
The stakes of proper cleaning practices Without effective cleaning in healthcare settings, methods against IPC weaken, which increase the rate that HCAIs can spread through
Without effective cleaning in healthcare settings, methods against IPC weaken, which increase the rate that HCAIs can spread through hospitals
hospitals and other healthcare venues. One of the greatest risks of high HCAI rates is the increase of AMR infections, which are much harder and much more expensive to treat, as conventional antimicrobial courses are no longer effective. No new antibiotics have been discovered since the 1980s, and yet AMR infections cause an estimated 700,000 deaths per year. Due to overuse and abuse of antimicrobial treatments, one in three patients in hospitals in England are on antibiotics at any one time, yet 2019 figures revealed that 20 per cent of all antibiotic prescriptions in primary care were inappropriate.
The Royal College of Nursing estimates that 10 million lives each year could be lost as a result of AMR by 2050 if this problem remains unaddressed, alongside a cumulative cost of $100 trillion. Despite successes in decreasing the persistence of MRSA in hospitals, C. difficle and E. coli infections are still common , with 45,885 cases of E. coli BSIs diagnosed in 2015 rising to 50,400 in 2017.
In 2019, the UK was the first country to set an ambition to reduce the number of AMR infections, and published two reports: a fiveyear plan and a twenty-year plan , following the World Health Organisation’s Global Action Plan on Antimicrobial Resistance (GAP). Both plans stressed the root causes of the issue: preventing the infections themselves, and called for thorough decontamination of medical devices, proper training for health and social care workers in practices like hand hygiene and aseptic technique, and the use of surveillance systems to monitor and recognise infections.
The rollout of competent IPC knowledge, training, and boards is vital for hospitals to properly implement these procedures, and so the UK also recommended boardlevel leadership with a combined IPC and antimicrobial stewardship role, facilitating and supporting an open learning culture for all health and social cares staff. These, in turn, strive towards a vision ‘of a world in which antimicrobial resistance is effectively contained, controlled, and mitigated’ by 2040. L



The CCMA look at how call and contact centres are utilised across the NHS and how to make best use of them
Did you know that in 2023/24, the NHS managed an astounding 600 million patient interactions? This included 13.1 million ambulance calls and 21.8 million NHS 111 calls.
These staggering numbers actually make the NHS one of the UK’s largest contact centre operators. Even in our digital-first world, plenty of people’s interactions with the health system still begin with a phone call.
NHS contact centres and what they’re used for
The NHS operates several distinct contact centre services across the UK. In England, NHS 111 operates through multiple locations across the country, working closely with regional ambulance services. Scotland has its own service called NHS 24, which operates as a single nationwide service. Wales operates NHS 111 Wales, and Northern Ireland is currently looking to establish its own 111 service. Each of the countries operate their services quite differently. NHS England 111 is much more closely aligned with the Ambulance service and is split into regions. NHS 24 covers Scotland as whole.
The key services provided by NHS contact centres include NHS 111 (Non-emergency medical helpline), which includes 24/7 medical triage and advice; appointment booking with GPs, urgent treatment centres, and A&E; mental health crisis support with dedicated mental health professionals; emergency dental appointment arrangements; and assistance with repeat prescriptions.
There are also 999 Emergency Services which include: immediate response to life-threatening emergencies; fire, police and ambulance dispatch coordination; integration with emergency departments; and mental health crisis response teams.
Contact centres play a vital role in public health initiatives and patient education, helping to guide people to the most appropriate care pathways. They use sophisticated clinical assessment tools like NHS Pathways – which is owned by the Department of Health and Social Care and delivered by NHS England – to ensure consistent and safe triage of patients, with over 50 per cent of callers speaking directly to clinicians such as nurses, doctors, pharmacists, or paramedics. E
The NHS is famously one of the world’s largest organisations, so it has many other touchpoints with the public and patients
In addition to 111 and 999, other NHS contact centres include Shared Business Services which is focused on administrative functions that keep the healthcare system running smoothly. These centres manage support, procurement and invoicing for 45 NHS trusts and 150,000 suppliers.
John Murphy, head of customer excellence at NHS Shared Business Services notes: “NHS Shared Business Services is a joint venture with NHS to reduce transactional processing costs as part of the ongoing efficiency drive to allow more funds for front line care.”
While traditionally focused on calls, NHS SBS has transformed its operation with 80 per cent of traffic now handled via their portal with 24hour turnaround. John Murphy explains: “In partnership with NHS, a significant investment is being made in the next generation of services with an updated user design portal and increasing levels of self-service where this is more efficient for both parties.” The organisation is consolidating its various contact
centres into a single point of contact and maintains a separate dedicated contact centre handling payroll and pensions queries.
Another division, NHS Business Services Authority (NHS BSA) operates an award-winning Customer Contact Centre handling over 5 million contacts annually. With approximately 650 staff, this centre manages queries related to assistance with health costs, student services, dental services, pension schemes, NHS jobs, overseas healthcare services and prescription services.
NHS BSA also managed the NHS 119 COVID-19 service during the pandemic, offering support in 200 languages for COVID-19 testing, vaccination appointments, and NHS COVID Pass inquiries. This saw the introduction of video consultations on a massive scale, the deployment of tens of thousands of remote contact centre staff, and a huge increase in the use of digital channels. Many of those initiatives have since become permanent features, transforming the way the NHS communicates.
The NHS is famously one of the world’s largest organisations, so it has many other touchpoints with the public and patients. These include Blood & Transport which operates the blood donor programme and has recently implemented Salesforce Marketing Cloud to increase donor engagement through their contact centres – an initiative that other NHS centres are planning to follow. And of course, most hospitals and GP surgeries still handle calls and bookings from their own patients.

Recent data from October 2024 shows that NHS 111 achieved an 89.8 per cent answer rate, some way below its 95 per cent target. The core NHS 111 targets are: 95 per cent of calls answered within 60 seconds; maximum 5 per cent abandonment rate; minimum 30 per cent clinical intervention rate; 75 per cent warm transfer rate for clinical calls; and 75 per cent of callbacks completed within 10 minutes.
Enhanced Urgent Care KPIs (2023/24) include: average answer speed under 20 seconds; 95th percentile answer time within 120 seconds; at least 50 per cent of calls assessed by clinical staff; 90 per cent of callbacks were clinically assessed within the agreed timeframe: and minimum 15 per cent self-care recommendation rate after clinical input.
The 999 service, on the other hand, has to answer calls and find solutions much more quickly. The UK’s emergency response system employs a tiered approach to categorisation, with each level having specific response time targets, from initial call handling to hospital handover times.
This includes 95 per cent of emergency calls answered within 5 seconds; 30-minute total hospital turnaround time; 15-minute hospital handover window; and a 15-minute crew precise time target.
According to John Murphy of NHS SBS: “Our Key KPIs include 85 per cent of calls answered

NHS contact centres, particularly NHS 111, have evolved from telephone helplines to sophisticated multi-channel healthcare hubs
in 180 seconds, 5 per cent abandoned rate, 95 per cent+ digital channel response within one working day, with CSat averaging at over 90 per cent with the service.”
NHS contact centres, particularly NHS 111, have evolved from telephone helplines to sophisticated multi-channel healthcare hubs which act as gateways into the healthcare system for patients. Their primary function today is to optimise patient care pathways, ensuring patients who need urgent care are directly and quickly taken to the right place while reducing pressure on emergency and primary care services.
A primary goal of NHS contact centres is reducing unnecessary A&E (accident and emergency) visits through effective triage and providing appropriate alternatives. The service offers 24/7 mental health crisis support, with dedicated mental health professionals available through the 111 service. Contact centres also play a crucial role in public health initiatives, providing education and campaign support while enabling direct booking into GP practices and urgent treatment centres.
The NHS has embraced digital transformation through multiple channels centred around three main access points: the NHS app; NHS website portal; and NHS 111 online service. These platforms give patients comprehensive access to healthcare services. They can use them to complete symptom assessments, book appointments, access medical records, view test results, and order repeat prescriptions. Integrating these digital services with traditional call centres has created a more efficient and accessible healthcare system.
At the heart of NHS contact centre operations is a critical tool called the NHS Pathways clinical assessment tool. This sophisticated triage system supports contact centre and clinical E
F staff in making consistent, evidence-based decisions across all channels. The system integrates with real-time service directories and supports 111 and 999 services, facilitating accurate, appropriate care pathway selection.
The NHS continues to enhance its digital capabilities through advanced technologies, including AI-powered platforms for remote consultations, video consultation capabilities, and natural language processing for call routing. Real-time data analytics and predictive modelling help optimise resource allocation and service delivery, ensuring patients receive the proper care through the most appropriate channel at the right time.
The CCMA’s comprehensive study of customer service perceptions reveals fascinating insights about the levels of customer service offered by public sector services, including NHS contact centres.
The research uncovered what CCMA terms the ‘Category Effect’, where service perceptions vary dramatically across sectors. Public sector services, including the NHS, typically return lower satisfaction scores than commercial sectors.
This disparity isn’t simply about competence - it reflects fundamental differences in service complexity, public accountability, and emotional stakes.
The diagram below shows how the public rates the public sector (labelled Gov’t) compared to the commercial sector.
This pattern suggests that the public recognises the commitment of frontline NHS contact centre colleagues
The most revealing finding here is the disconnect between the public’s overall perception of the customer service they receive and their recognition of the effort those staff make. While government services scored -25 for overall service perception, they achieved a positive score (+1) for staff effort (see diagram opposite). This pattern suggests that the public recognises the commitment of frontline NHS contact centre colleagues, even when systemic challenges get in the way of overall service delivery.
The research and success stories point to clear opportunities for NHS contact centres to enhance patient experience while improving operational efficiency.
The first step is to integrate and optimise the use of digital channels. This doesn’t mean forcing patients onto digital platforms – instead, it’s about making digital interactions so efficient and user-friendly that they become the natural choice. This requires careful planning, clear communication, and, of course, maintaining phone access for those who need it.


NHS contact centres are already utilising sophisticated clinical assessment tools. The next step is integrating these with user-friendly digital interfaces that maintain clinical safety while improving accessibility. Recent implementations of systems like Salesforce by NHS operations show how modern technology can enhance efficiency and the patient experience.
The research done by the CCMA shows that NHS contact centre employees are already recognised for their commitment to helping patients. Lack of effort and care are not the problem. What the NHS needs to do is continue to support the dedication of their colleagues with more efficient systems and processes. These include: comprehensive training programs; sustainable workload management; clear career progression opportunities; and regular development and support.
Traditional contact centre metrics need to be balanced with healthcare-specific measures, including: time saved for patients; first contact resolution rates; patient satisfaction scores; clinical safety metrics; and staff wellbeing measures.
The future lies in balancing digital efficiency with human connection – using technology to handle routine interactions while preserving valuable colleague time for complex cases requiring personal attention. This isn’t just about operational efficiency – it’s about recognising that every minute saved for a patient is a minute they can spend on what
matters most to them. In healthcare, that time saving could be transformative. M
Formorethan30years,theCCMAhasbeen absolutelydedicatedtosupportingcontactcentre professionals.We’reconstantlypushingourselves todomoreforourthrivingcommunity,which happenstobethelargestcommunityofcontact centreprofessionalsintheUK.TheCCMAwas foundedwiththegoalofsharingbestpracticeand networkingtoimproveskillsandknowledgein ordertoprogresscontactcentreoperations–and welivebythattothisday.
Nomatterwhereyourcontactcentreisinits development,weareheretosupportyou.
Wegivethosethatworkincontactcentresthe chancetodiscussideasandshareexperiences throughmember-onlySpecialInterestGroups andonlineandin-personevents.Membersare invitedtobecomeAccreditedthroughtheContact CentreStandardsFrameworkandgetindependent guidanceonwheretofocusforimprovements. Thereisalsotheopportunitytobenchmarkthe operationagainst25+KPIs.TheCCMAAcademy giveseveryoneastructuredlearningopportunity tosupportbothpersonalandprofessional developmentforthebenefitoftheiroperation. Andofcourse,wecelebratetheprogressour industryismakingthroughtheUKNationalContact CentresAwards.Thosethatwingoontosharetheir storiesthroughchannelssuchastheUKNational ContactCentreConference,BestPracticeVisits andCareerTalk.Theyareinvitedtoinputintothe SpecialInterestGroupsandotherevents.
www.ccma.org.uk

Hospital food is widely criticised for its poor quality and lack of nutrition. As the NHS aims to become more sustainable, should hospitals switch to plant-based meals by default? Evidence suggests that a shift could benefit both patient health and the environment - but how feasible is it?
A 2020 survey by the Patients Association asked people who had spent at least a night in a hospital within the last six months their opinions of hospital food, which were less than favourable. Only 20 per cent said the food they were served improved their stay, while 44.6 per cent said hospital food had made their experience worse. Almost half (48 per cent) of respondents were unsatisfied with their meals, and a large majority of comments pointed towards the nutritional content of the food as being the source of discontent. “Healthy food please” demanded one participant, while another asked for “provide simply nutritious food.”
The current state of hospital catering This correlation is not surprising when compared with data from a 2016 survey of London hospital food, which revealed that only 30 per cent of hospitals cook food fresh on-site for adults (42 per cent for paediatric patients),

with 17 per cent of hospitals serving patient food in ready meal packaging. Only 13 per cent of hospitals have a Soil Association Food for Life Catering Mark for their patient food, a mark of fresh, environmentally sustainable, and ethical food. This raises concerns as the NHS Constitution says that every patient has ‘the right to receive suitable and nutritious food’. One Health is an integrated approach to health that recognises that human health, animal health, and ecosystem health are all interdependent on each other; that is, us, the animals, and the planet are all related via food and our consumption of it. Poor nutrition exacerbates ill health, climate change and the NHS’s already existing issues.
It is no secret that the NHS is in a critical state. Over a decade of ‘capital starvation’, understaffing , and budget slashes have left our health service deprived of the resources it needs to function properly, and as a result services often fall short of quality and efficiency targets. The NHS is particularly under stress as Britain faces two major challenges of decreasing public health and the climate crisis, exacerbated by poor funding and lifestyle factors that create a dangerous, expensive cycle.
In 2020, the NHS became the world’s first health service to commit to net zero , and published
Poor nutrition exacerbates ill health, climate change and the NHS’s already existing issues
a report where they outlined their roadmap to more sustainable future. In ‘Delivering a ‘Net Zero’ National Service’, the NHS acknowledge that food and catering services produce 1,543 ktCO2e each year, approximately six per cent of the NHS’s total emissions. Methods to rectify this include reducing food waste, ensuring suppliers have sustainable production and transportation practices, and locally sourcing produce. Despite mentioning that the “government’s EatWell plate recommends a diet with reduced processed foods high in sugar, salt and fats”, there is no mention of changing the food served in hospitals, even though a survey commissioned by Plant-Based Health Professionals UK (PBHP) revealed that 30 per cent of participants thought meat-free meals would be better for both the environment and health.
There is long-standing evidence that links animal farming with greenhouse gases, with 70 per cent of food-related emissions in the UK coming from red meat and dairy alone. Meat, specifically processed meat, is recognised as E


74 per cent believed it is important to make dietary and lifestyle changes to reduce the risk of developing chronic health conditions
F an International Agency for Research on Cancer (IARC) group one carcinogen – the same level as tobacco and gamma radiation – and poses a serious threat to health if consumed in large quantities, and yet a study by the PBHP looking at hospital food menus found that all of the menus analysed contained processed meat. Research found that if everybody were to adopt meat-free lunches just during the week, it would prevent over 7,000 deaths from cardiovascular disease each year. Reducing meat intake in countries with high-fat, high-protein diets (the ‘ Western Diet ’) is a crucial element to both public health and sustainability, and is particularly important in a hospital, an environment where wellness must take priority and where the national health system has made a pledge to be greener . Between 20 and 25 per cent of all deaths in adults have been associated with imbalanced diets, with one in ten Brits over 40 having type two diabetes.
In June 2024, PBHP’s survey to gauge the general public’s attitudes towards changes in hospital menus revealed 64 per cent believed that hospitals should prioritise offering healthy meals, 74 per cent believed it is important to make dietary and lifestyle changes to reduce the risk of developing chronic health conditions, and 35 per cent supported the switch to plant-based menus. This is a staggering number considering only two per cent of the respondents were vegan. Another survey by PBHP conducted in May 2024 involving the staff at King’s College Hospital, 74 per cent of respondents gave adding dishes with lentils, beans, mushrooms, or tofu to menus as their response to improve hospital menus.
61 per cent of respondents to this survey said they would be annoyed if they were unable to eat meat during their hospital stay, which is why a “plant-based by default” approach would be best, rather than outright banning meat in hospital catering. A plant-based by default method is not restrictive and uses choice architecture to encourage people to select plant-based meals during their hospital stays. Much like how vegans often need to ask to see a vegan menu in restaurants, a plant-based by default approach in hospitals would centre
plant-based options, making people need to ask for meat options should they wish to. By making plant-based options the norm, institutions like hospitals can nudge individuals towards more sustainable and healthier eating choices without taking away someone’s freedom of choice.
In New York City , 11 public hospitals implemented plant-based menus by default in 2022, leading to a 35 per cent reduction in foodrelated carbon emissions in just one year, as well as cost savings of 59 cents per meal in 2023. Most importantly, patients who ate plant-based meals in 2023 gave a 90 per cent satisfaction rate. In the UK, the Conservative Animal Welfare Foundation have calculated that a plant-based approach in NHS hospitals could save the NHS £74 million, and even further savings for patients should they also wish to modify their diets once out of care. A reduction in meat consumption would benefit the NHS even if it takes place outside its estate: the Office of Health Economics recently estimated that if England were to adopt a plant-based diet there would be a net total benefit to the NHS of £18.8 billion each year.
By making plant-based options the norm, institutions like hospitals can nudge individuals towards more sustainable and healthier eating choices
Should the UK consider the switch, it is paramount that choice still remains an option for those who still want to eat meat or fish, and that the plant-based meals on offer contain a full nutrient profile. Some people may find transitioning to a vegan diet near impossible, such as those with coeliac disease, those deficient in zinc or B12, and those with allergies to foods often used as substitutes, like soy or nuts. If these remain priorities and policymakers take these into consideration, trialling plantbased menus by default in hospitals could be a solution to three big issues in the NHS: sustainability, poor patient satisfaction, and health. L

This article, written by NHS Supply Chain, explores how standardising inventory management and point-of-care scanning across NHS trusts is improving patient safety, enhancing supply chain resilience, and delivering significant cost savings
With over £1 billion of shelf stock across the NHS in England, standardising inventory management capability and point-of-care solutions is a key way to release significant cost benefits to trusts while at the same time delivering benefits for patients.
In-trust inventory management has been identified as one of the biggest areas of opportunity for NHS Supply Chain to have a positive impact.
NHS Supply Chain manages the sourcing, delivery, and supply of healthcare products, services, and food for NHS trusts and healthcare organisations across England and Wales, processing more than 8 million orders per year, across over 129,000 order points, over 16,000 locations and consolidating orders from over 1100 suppliers.
NHS Supply Chain established their Inventory Management and Point of Care Scanning programme in line with the priorities set out by NHS England in their Operational Planning Guidance for 2023/24, NHS Supply Chain Head of Inventory Management Solutions, Mark Vallentine, said “Unlocking savings, improving patient care, and creating greater supply chain resilience has always been at the heart of our offering to the NHS,”
“By implementing inventory management and point of care scanning we can help NHS trusts to improve patient safety by scanning the product to the patient in real time and capturing the data about the product electronically, making it far more efficient to trace the patient in the case of a product recall.”
As part of a national programme managed by NHS Supply Chain, advanced IMS and Point of Care Scanning (PoC) solutions are being deployed to NHS trusts. These innovations enhance patient safety and deliver significant productivity improvements by reducing the time spent on administrative tasks, ultimately supporting better patient care and driving operational excellence.

The programme, managed nationally by NHS Supply Chain and funded by NHS England, is designed to improve patient care, and streamline operations in NHS trusts. The programme aims to deliver: cash-releasing savings; visibility of end-to-end supply chain data; scalability and a standardised turnkey deployment approach; enhanced patient safety and experience; and increased clinical productivity through reduced administrative tasks.
The scope of the programme can be segmented into four key components.
1. The system and module: this includes inventory management, Point of Care scanning and analytics functionality. The programme will focus on supporting trusts obtain visibility of high-value medical devices (Class III and IIb) up to 75 per cent by value.
2. Implementation delivery support: a small team of NHS Supply Chain colleagues will be deployed to provide technical and delivery expertise to trusts.
3. Licensing and hardware: licencing and hardware will be funded for the trust for the initial period.
4. Maintenance and support: ongoing programme support and training will be
These innovations enhance patient safety and deliver significant productivity improvements
provided via NHS Supply Chain’s team, as well as technical support via the system provider.
The programme is delivered by NHS Supply Chain’s In Hospital Services team which is comprised of a specialist deployment team, supported by subject matter experts in benefits realisation and change management, data standards and IT integration, and relies on robust project management.
The programme enables NHS Supply Chain to leverage a system-wide view to optimise visibility on national stock demand and consumption to improve supply chain resilience, while supporting upstream supplier stock management and demand planning. It also facilitates national initiatives such as Scan4Safety and GS1 standards adoption.
NHS Supply Chain Strategy executive director, Sara Ford said: “The rollout will bring supply chain and trust efficiency opportunities, E


As of January 2025, NHS Supply Chain has successfully implemented a digital inventory management system (IMS) across six NHS trusts
F as well as enabling significant patient safety benefits. By scanning once, uniting data on product, patient, clinician and location, we can bring both short term cash releasing savings, as well as longer term improvements in supply chain resilience and capture key information required by medical device outcome registries.”
As of January 2025, NHS Supply Chain has successfully implemented a digital inventory management system (IMS) across six NHS trusts, tackling challenges such as inaccurate stock tracking, inefficiencies, and resource wastage. By improving inventory accuracy, reducing costs, and streamlining operations, the system has delivered early measurable benefits and created a clear roadmap for wider rollout. The programme has been implemented through strong collaboration, creating a solid
foundation for continuous improvement and nationwide scalability. This teamwork highlights a shared commitment to improving patient outcomes and driving innovation.
The following trusts are now live, with implementations initially focused on specific hospital areas and potential for expansion: Dorset County Hospital NHS Foundation Trust; Newcastle upon Tyne Hospital NHS Foundation Trust; Northumbria Healthcare NHS Foundation Trust; Sandwell and West Birmingham NHS Trust; The Princess Alexandra Hospital NHS Trust; and West Suffolk NHS Foundation Trust.
Louise Brereton, head of procurement and logistics, Dorset County Hospital NHS Foundation Trust said: “At Dorset County Hospital, we are delighted to be part of the NHS Supply Chain IMS programme and working with Ingenica to implement i360. The system itself has been well received by our clinical teams and by our own team of Inventory Controllers.”
Simon Peck, team leader for vascular, The Princess Alexandra Hospital NHS Trust commented: “So far, the project has already made some really good changes to our theatre consumable cupboard, it already looks so much neater and easier to identify where our products are. It has highlighted to us just how much

excess stock we have and we are hoping the next stage of the project helps to condense our low turnover stock, and allow more room for our high turnover stock.”
The IMS deployment journey continues, with more trusts set to go live throughout 2025
Debbie Stevenson, head of procurement, West Suffolk NHS Foundation Trust added: “The NHS Supply Chain team on the ground supported the trust team to a high level with stocktakes, templates, engagement, training and support and were an invaluable resource.”
The IMS deployment journey continues, with more trusts set to go live throughout 2025. The team remain committed to supporting trusts by working closely with local teams to understand their unique requirements and provide tailored solutions.
NHS Supply Chain will be updating regularly on their website about the progress and positive changes IMS and PoC are bringing to NHS trusts nationwide. M
If you would like to learn more about the programme, please contact the In-Trust Inventory Management Systems (IMS) team at IMS@supplychain.nhs.uk

With the new Procurement Act 2023 legislation set to come into place this month, Crown Commercial Service provides guidance for healthcare organisations on how to prepare

The rules that govern how public money is spent on common goods and services in the UK are about to change.
The Procurement Act 2023 was made law in October 2023 and is currently expected to golive on 24 February 2025.
These new regulations will bring significant changes for everyone involved in public sector procurement and it’s important to understand what is happening, why, and how they can best prepare for the upcoming changes.
When the UK left the EU in 2020, it was decided that the UK needed a simpler, more flexible, commercial system that met our country’s needs better, while keeping us compliant with our international obligations.
This new set of regulations provides a number of benefits to suppliers and buyers, including: supporting innovation and removing red tape or barriers to progress; improving transparency by giving everyone access to public procurement data through a fully open and transparent system, enabling faster competition processes for emergency buying, giving buyers the tools to meet urgent needs quickly and efficiently; simplifying the process of working with the public sector, supporting more SMEs to bid for contracts.
The Procurement Act 2023 will apply to any commercial agreement created after the ‘golive’ date, and all activity carried out under these agreements will need to be compliant with these new regulations.
The NHS spends almost £22 billion on common goods and services each year and with tighter NHS budgets and resources, buying products and services is challenging. Working with Crown Commercial Service (CCS) can help take some pressure off your capital projects. Nationally, NHS trusts are tapping into our buying power to access sustainable solutions for their estates and facilities to help get the NHS back on its feet.
CCS has prepared for the implementation of the new regulations through five workstreams. Buyers can use a similar approach to assess readiness in their own organisation. The five workstreams are broken down as follows:
In advance of the new regulations, NHS organisations with existing contracts should review all current and planned commercial opportunities.
Understanding when these contracts will expire, if and how they will need to be renewed or replaced, and the agreements that will be available to do so is vital for future-proofing an organisation’s procurement strategy.
Reviewing the way an organisation works in terms of their procurement activity and ensuring these processes are robust and future-proofed for the new regime is vital to a smooth transition.

NHS organisations can help to ensure a smooth transition by creating appropriate guidance and resources around the Procurement Act for their staff. These should take particular account of the provisions and requirements introduced by the new regulations and highlight where particular changes have been introduced.
Organisations can also review the existing documents that their teams and suppliers use for training, guidance and information about the procurement process. Some of these documents can become outdated over time, so make sure they include the most up-to-date information.
New procurement regulations mean that some things in the process will need to be done differently in future.
Examining the readiness of an organisation’s systems and what changes may be needed in advance of the go-live can help contracting authorities preempt these changes and be ready to incorporate them.
Coordinate the training needs of your people and ensure they fully understand the new regulations through regular communication and necessary training.
What training resources are available?
Transforming Public Procurement (TPP) is the readiness programme for the new procurement regulations. This has been led by the Cabinet Office, which has developed a suite of official
training programmes to help the public sector prepare for the new regulations.
The primary training they have provided is the Transforming Public Procurement Knowledge Drops, aimed at anybody who interacts regularly with procurement. They provide a high-level overview of the changes the new regulations will bring, delivered through a series of short ondemand broadcast presentations.
There are different versions of these Knowledge Drops available for buyers and suppliers in the public sector, as well as a third adaptation aimed specifically at small and medium-sized enterprises (SMEs) and voluntary, community and social enterprises (VCSEs).
More detailed and specific training options are available for buyers who require more than a general overview of the new regime, including self-guided e-learning modules and more intensive ‘deep dive’ training courses. Visit the Cabinet Office Transforming Public Procurement webpage to find out more about these and to access more available resources around the TPP project.
Learn more about our healthcare services and commercial solutions to maximise your health estate by visiting our health webpage and viewing our digital brochure.
CCS has created a dedicated implementation guide to help public sector organisations prepare for the new procurement regulations. Download the guide now for more detailed information on steps that can be taken now to get ready. M

Starting a new job is daunting enough, let alone moving to another country. What can the NHS do to make sure overseas workers feel welcome?
For healthcare staff considering relocating to the UK for work or those newly arrived, the experience can often feel overwhelming and, at times, even unsafe.
Dr Salman Waqar, the president of the British Islamic Medical Association (Bima) told The Guardian: “I’ve seen some really terrible messages, particularly coming out from Belfast and in Greater Manchester, of people having to close up their GP surgery early, of people being trapped in their practices, of people having to take taxis back and forth from work, people not going on home visits, people working remotely from home, there’s too many to mention and to count.”
Following the tragic killings of three young girls in Southport, a wave of violence and anger was directed at migrants and asylum seekers.
The unrest quickly escalated into nationwide riots, resulting in over 1,000 people being charged in connection with the disorder.

International NHS staff also became targets of the violence and racism. In one incident, two Filipino NHS nurses travelling to work by taxi in Sunderland were attacked when rioters in the city centre pelted their vehicle with rocks.
The Filipino Senior Nurses Alliance UK said on X that they “strongly condemn” the attacks and added: “Our community has been an integral part of the NHS since 1969. We are united against racism and will continue to support our colleagues.”
Seeing these events in the news is understandably alarming for many overseas NHS workers.
Here, we explore ways NHS managers and staff can support them, fostering a welcoming and positive work environment.
Addressing bullying/ harassment effectively
Following the attacks on Filipino healthcare staff, health secretary Wes Streeting amended NHS guidance to list “when there is discriminatory behaviour, including racism” as one of the situations that may justify a nurse declining to give care.
This was in an effort to curb the amount of harassment and abuse that overseas or people of colour (POC) are subject to in healthcare.
Streeting said: “I will not tolerate, under any circumstances, NHS or social care staff in
A survey in April found that over three in four NHS staff said they have experienced a mental health condition in the last year
any health or care setting being subjected to intimidation, harassment or racist abuse.
“We have a zero-tolerance policy in the NHS and we’ll take a zero-tolerance approach in social care too.
“People who are abusing NHS staff can be turned away, and should be turned away, if that is the way that they are treating our staff.”
He went on to express his pride at the international staff working in NHS and social care services in the UK providing “great, compassionate care”.
While this is a step forward in terms of government action, there is much that NHS managers and staff can do to improve the workplace.
Making sure staff feel supported and like they belong should be one of the key priorities for managers.
A survey in April found that over three in four NHS staff said they have experienced a mental health condition in the last year. In addition, E


F more than one in two reported experiencing anxiety and a similar proportion had struggled with low mood. Over two in five respondents said they’d experienced exhaustion and 60 per cent said they were worried about their colleagues’ mental health.
While this is applicable for everyone working in the NHS, overseas healthcare workers can be hit with an extra dose of burnout and stress.
It’s not just harassment from patients and the public that can concern international NHS workers, but also the issue of burning out can loom larger.

Improving staff mental health is not an easy fix, but it is an essential aspect to consider
In 2021, Nuffield Trust estimated that based on an average joining age of 30, an overseas nurse not from the EU might work in the NHS for an average of 12 years, which is three years longer than an UK national and six years longer than a nurse from the EU.
Improving staff mental health is not an easy fix, but it is an essential aspect to consider. One way staff can feel more supported in their wellbeing is by setting up a buddy system for those who are new to the country.
Many sectors use this method to make their employees feel more comfortable in a new place with new people, particularly in education. Moving to a new country as well as starting a new job comes with even more worries for many. This includes finding somewhere to live, new bank accounts, national insurance numbers, registering with a GP, UK sim cards, access to schools, and navigating public transport.
Setting up a buddy system or having good pastoral care to help them make these arrangements can make a huge difference to their transition period. Coordinating social activities during those first crucial few months is another way to create a cohesive, welcoming team atmosphere with high staff retention. L
With over half of NHS staff experiencing anxiety and low mood, we examine what the health service can do to improve staff wellbeing
According to NHS Digital, mental ill health accounts for over 20 per cent of sickness absence in the NHS.
Working in the NHS can take its toll on the mental health of many, leading to burnout, anxiety, PTSD and many more issues.
A YouGov survey conducted last year found that over half of the staff surveyed reported experiencing anxiety, while half had struggled with low mood. Exhaustion was reported by 42 per cent while 60 per cent were worried about their colleagues’ mental health.
We take a look at what the NHS is doing so far to ease the mental health crisis in the workforce, as well as what other organisations are doing to build a support network.
The Blue Light Symphony Orchestra is the UK’s only orchestra for all Emergency Services personnel and includes people in the Police Force, Fire Brigade and Ambulance Service, the military and other emergency services such as Mountain Rescue, Cave Rescue and the RNLI.
They are a registered charity, and hold all sorts of events across the year to show off the hidden talents of the blue light industry.
Last Christmas season, for example, the orchestra performed in Soho Fire Station with the London Fire Brigade Choir to sing carols and fundraise for both charities.
They held a concert in October in central London, where members came together for a E


There are staff wellbeing support hubs in place across the NHS

F unique performance of some classical favourites, such as Beethoven’s overture ‘Egmont’, a stormy and dramatic rendition of Mozart’s Piano concerto No.20. in D minor and Tchaikovsky’s Symphony No. 5.
Surrey Police officer and acting conductor
Seb Valentine said: “This unique concert is a celebration of the musical talent that exists within the UK’s emergency services. It is a rare opportunity for these selfless individuals to show their human side and express themselves artistically.”
This orchestra is not the only musicorientated support for NHS workers. You may recognise the Lewisham and Greenwich Trust Choir from their various media appearances.
In 2016, they recorded and released their debut album; ‘Something Inside So Strong’. As well as lending their support to community and NHS events around the country they have also performed at high profile events including Glastonbury Festival, the FA Cup Final at Wembley Stadium, Christmas with the Stars at the Royal Albert Hall, and Stand Up To Cancer with Boy George.
In June last year, they also performed the national anthems at the Major League Baseball series in London.

Wellbeing support hubs
There are staff wellbeing support hubs in place across the NHS, too. Established in October 2020, with funding subsequently extended to March 2023, the hubs were funded on a nonrecurrent basis in response to the pressure on the workforce from the pandemic.
Now, they are still providing services for NHS staff to receive mental health support. These hubs across the UK, where staff can seek mental health support through the current staff wellbeing offers, including free access to a range of health and wellbeing apps, or through NHS talking therapies.
They can access help from a GP, as well as a free and confidential Check My Wellbeing self-check tool which can provide further information on the range of support.
For trainee healthcare staff, work can feel especially daunting and stressful.
The Trainee Doctors & Dentist Support Service (TDDSS) is a psychoeducation and support service which aims to offer a range of interventions to support trainees on programmes managed by HEE Local offices in London & the South East.
The service is delivered as part of the PH+ programme of work, hosted by the NHS Practitioner Health Service.
in six women from the workforce due to insufficient support
The NHS workforce employs over 1.3 million people, 76.5 per cent of them (over 1 million) women, of which women between the ages of 45 and 54 make up over 19 per cent of the entire NHS workforce.
Supporting women and people going through menopause in the workplace has been an overlooked aspect of mental health support until very recently. The Chartered Institute of Personnel and Development found that employers lose one in six women from the workforce due to insufficient support.
Menopause and perimenopause (the phase leading up to the menopause) can cause symptoms including anxiety, mood swings, brain fog, hot flushes and irregular periods. These changes can impact many people’s work lives, meaning it is even more essential the NHS provides support for their staff during this time.
NHS Employers said that leaders and managers need to understand menopause and how they can support their staff. They urged NHS Trusts and employers to integrate a variety of strategies to help people going through the menopause in the workplace.
One of these is to recognise the need for support from others going through the same thing, and make space for this in the workplace.
At Northern Lincolnshire and Goole NHS Foundation Trust, for example, they set up a closed Facebook group for staff to join, where colleagues support each other and share their menopausal experiences.
The Trust also implemented menopause network meetings, with guest speakers such as gynaecologists attending to educate and raise awareness, with an inclusive atmosphere welcoming all staff members.
Other ways to help staff going through menopause feel supported include following national menopause guidance, maintaining regular contact to support and connecting during their absence, and offering regular wellbeing conversations to check in. L

Internationally recognised for its pioneering staff alarm systems, Pinpoint Ltd ensures staff safety is a priority in healthcare settings. With increasing rates of violence toward healthcare staff, Pinpoint’s alarms stop abuse in its tracks.
Established in 1990, the family-owned business has a long history in designing and manufacturing safety alarm systems that cater to the particular needs and challenges
of those working in hospital environments.
The P2 System is the latest evolution of Pinpoint’s awardwinning product. Durable, unobtrusive and highly efficient, the P2 System seamlessly integrates into hospital settings, while providing a vital safety function for both staff and service-users.
A wearable, personal alarm enables staff to quickly and easily summon support when


needed. By clicking one of two buttons on the device, corresponding to assistance or emergency respectively, staff trigger the System, alerting colleagues to their exact location and the severity of the call.
This rapid process, taking just milliseconds seconds from activating the alarm to the information display, prevents the escalation of high-risk situations and ensures staff receive a response when they need it most. M
www.pintpoint.ltd.uk

and Ireland’s leading

NHS staff across the UK are facing an alarming rise in violence and abuse, with reports of physical assaults, threats, and verbal attacks reaching record levels. Recent investigations reveal that ambulance crews, call handlers, and hospital workers are increasingly at risk, prompting urgent calls for stronger protections and tougher penalties for offenders
NHS staff safety has been in the news recently, with reports of staff being spat at, hit and punched while on duty.
A recent investigation by the BBC found that more than 1,700 physical assaults have been recorded on hospital staff in Kent and Sussex over the course of a year. A 2022 staff survey found that more than 14 per cent of the NHS Sussex Trust workforce has experienced physical violence.
In January, the Association of Ambulance Chief Executives (AACE) said that UK ambulance services are on course for the highest rate of reported incidents of violence, aggression and abuse directed at their people ever recorded. Data from the association showed that there are 20,000 incidents expected across the fourteen
UK ambulance services in the 2024-25 financial year. This is an average of 55 a day. There has been a sharp increase in reported incidents of violence, aggression and abuse against ambulance staff over the past four years. In 2021/22 the total was 15,430, in 2022/23 it rose by 2.7 per cent to 15,857. In 2023/24 the figure rose by 23.8 per cent to 19,633.
Jason Killens, AACE chair and chief executive of the Welsh Ambulance Services University NHS Trust said: “It is with huge regret that we see the level of violence, aggression and abuse across all UK ambulance services increasing and that frontline clinical employees as well as call handlers are affected. This unacceptable behaviour has a major long-term impact on E
F the health and wellbeing of ambulance people who are simply trying to do their jobs and help save lives. This is why we are making a plea to the public to ensure that our staff are treated with the respect they deserve, especially during the busy festive period. We are also asking the judiciary to use their full powers under the Assaults on Emergency Workers Offences Act 2018 legislation to ensure appropriate sentences are handed out consistently to those found guilty of committing these crimes against our workforce.”
Meanwhile, attacks on crews and call handlers at London Ambulance Service have increased by more than 10 per cent in the last year. Recent figures show that there were around seven physical or verbal attacks on ambulance crews or those taking 999 calls in London every day. This is the highest rate ever recorded. These incidents include kicking, punching, slapping, spitting, verbal abuse, threats, and sexual assault.
An ITV News investigation last year found that there were at least 41,226 physical assaults on NHS staff working in hospitals in 2023. The number represented a 21 per cent increase since 2019. There was also a 142 per cent increase in reports to the police of violent assaults on hospital staff compared to 2019.
Berkshire Healthcare NHS Trust reported 800 physical assaults against its staff in 2023. There were also 925 non-physical assaults.
In June last year, University Hospitals Tees launched a violence against staff campaign after a 32 per cent increase in attacks over a 12-month period. More than 800 members of staff from across South Tees Hospitals NHS Foundation Trust and North Tees and Hartlepool NHS Foundation Trust (which make up University Hospitals Tees) reported some form of assault from patients, relatives or the public whilst carrying out their duties.
The campaign shows images of children of staff members alongside messages pleading to keep their parents safe at work.
Faye and Logan, children of Louise Michie, consultant obstetrician for South Tees Hospitals took part in the campaign. Louise Michie said: “All NHS workers have the right to feel safe at work to allow them to provide the best possible care to our patients.
“The campaign is incredibly important as it highlights the message that violent attacks against our staff will not be tolerated.”
East of England Ambulance Service NHS Trust (EEAST) launched its ‘Your Safety, Our Priority’ campaign last year after an increase in attacks on staff. Of the 1,455 attacks recorded, 362 were physical assaults, 522 were verbal in nature, and 571 were instances of non-physical abuse such as aggressive gestures and intimidating behaviour towards staff.
EEAST’s health, safety and security specialist Alistair Livingstone runs the campaign, he said: “We see too many incidents where our colleagues are attacked – either physically or

NHS
England has provided £8.4 million to all 11 ambulance services for the procurement and evaluation of a three-year body worn camera trial
verbally – when they are there doing their job in difficult circumstances to help people in their time of need. It is completely unacceptable.
“We’re doing all we can to support our staff if they are confronted or physically attacked. In the coming months we’re introducing a new training programme for our people to recognise and assess the risk of potentially dangerous situations, and how to get away to safety. We’re driving forward the delivery and use of bodyworn cameras, which are invaluable for staff if something happens.
“We’re reviewing how the Trust manages and responds to internal reports of violence and aggression, so our colleagues can see what action is being taken.
“Finally, we are being clear about how the Trust will support and help our colleagues through any process, including prosecution of those that choose to attack emergency workers, which can be really gruelling for all involved.”
NHS England has provided £8.4 million to all 11 ambulance services for the procurement and evaluation of a three-year body worn camera trial.

The Work without fear campaign has been developed in collaboration with the Association of Ambulance Chief Executives (AACE). The aim of the campaign is to portray ordinary people doing an extraordinary job and highlight the impact that violence and abuse can have on the everyday lives of ambulance staff.
Amanda Pritchard, NHS chief executive said: “It is horrific that in just one year, thousands of our hardworking ambulance staff have experienced unacceptable violence and abuse at work. Ambulance staff are already under huge pressure delivering urgent care to patients and they have a right to feel safe when they come to work.
“We know there is more to be done right across the NHS to ensure staff are protected and Work Without Fear is an important campaign which will highlight the horrendous impact this is having on the ambulance workforce and hopefully help towards preventing such violence from happening.”
NHS England’s Violence Prevention and Reduction Programme aims to support NHS organisations and systems to embed a culture where NHS colleagues feel supported, safe and secure at work.
NHS England encourages the use of the VPR standard as a framework and elements of it can be incorporated into pre-existing strategies and policies.
NHS England expects all parts of the NHS to commit to preventing and reducing the risk of violence towards staff and support health and wellbeing. L
Robust data infrastructure and language AI could transform the NHS, addressing the challenges of unstructured data and the critical need for ethical, transparent data governance in healthcare

The NHS sits on a goldmine of clinical data, but much of its value remains locked away behind clinical records software, or in unstructured form – buried within clinical notes, letters, and free-text fields. The data we have available nationally are a poor quality and shallow representation of patients, poorly suited for AI or detailed research.
While most medical journeys are recorded electronically, the suppliers that create clinical software often do allow analysts and researchers to access the data that is generated. To provide access, suppliers will often charge substantial amounts for the privilege.
In addition, more than 80 per cent of information is recorded in free text. While some companies have demonstrated the value of manually extracting insights from clinical notes, this approach isn’t scalable across a health system as vast as the NHS. The good news is that we now have the technology to automate this process through language AI, potentially unlocking unprecedented value from NHS data.
This isn’t just about operational efficiency; it’s about fundamentally improving patient care and research capabilities. By using improving access to deeper healthcare data, and properly utilising language AI at scale, we can accelerate patient access to clinical trials, enhance realworld evidence generation for life sciences research, and – perhaps most critically –address systematic biases in our healthcare data.
One of the most compelling arguments for leveraging language AI lies in its potential to address healthcare inequalities. Consider a typical GP consultation: when seeing a patient with multiple comorbidities from a deprived area, perhaps struggling with English, time constraints may mean only the most pressing conditions get properly coded. In contrast, simpler consultations allow time for comprehensive coding. The result? Patients with complex needs may end up with sparser coded records, creating a dangerous data bias that can perpetuate healthcare inequalities. This bias isn’t just a documentation issue – it has far-reaching implications for AI development in healthcare. When we train AI models on structured data alone, we risk embedding these biases into our algorithms. By incorporating unstructured data through language AI, we can build more complete patient profiles and develop more equitable AI solutions.
Looking beyond our borders, we can learn valuable lessons from other countries and industries. Singapore, Switzerland and Scandinavian countries have shown remarkable success in healthcare data management, largely due to their focus on system harmonisation and standardised EHR/EPR implementations. But perhaps the most important lesson comes from non-healthcare industries: the emphasis should be on infrastructure and data pipelines rather than algorithm development.
Healthcare has fallen into what I call the “algorithm fallacy” – developing countless algorithms on clean, curated datasets that fail to perform in real-world conditions. In contrast, successful industries build robust data pipelines and infrastructure, regularly retraining their models to adapt to changing
real-world conditions. This is especially crucial in healthcare, where patient conditions and care pathways are inherently dynamic.
The value proposition: an uncomfortable but necessary conversation
We need to have frank, open discussions about the value of NHS data. Currently, hospital data is being sold to private companies who clean it, extract value, and broker it onwards – all while the NHS sees little return on this valuable asset. This fragmented approach not only fails to maximise the potential of our data but also raises serious concerns about data governance and patient trust.
The value chain needs to be brought back into the NHS. While this might be an uncomfortable conversation, it’s essential for ensuring that any monetary value generated from NHS data directly benefits patient care and system improvement. By controlling and properly managing our data assets with continual patient engagement and maximum transparency, we can ensure both ethical use and financial sustainability.
Infrastructure before innovation
The path forward requires a fundamental shift in our approach. Rather than focusing solely on developing new algorithms, we need to invest in robust data infrastructure and pipelines. This means creating systems that can handle realworld data complexity, support regular model retraining, and ensure consistent data quality across the system. This also mean changing procurement practices and legislation, such that the NHS (not the systems supplier) is always in control of its data.
This infrastructure-first approach would enable us to achieve several critical objectives. By building robust data pipelines, we could extract deeper data, and more meaningful insights from unstructured data at scale, transforming millions of clinical notes into actionable intelligence. Such infrastructure would also allow us to maintain up-to-date, representative AI models that evolve with our patient population and clinical practices. It would ensure equitable representation in our healthcare data, addressing the current biases that risk perpetuating health inequalities. Perhaps most importantly, this approach would create sustainable value from NHS data assets, ensuring that the benefits of data-driven healthcare flow back into improving patient care and system efficiency.

Dr Joe Zhang, head of Data Science, London AI Centre & Secure Data Environment
Dr Zhang will take part in a Rewired 2025 session ‘NHS data architecture: where we are, where we need to get to’ exploring the size of the potential prize in securing data trust with the public and working with the wider life sciences community. He will be joined by speakers Ele Harwich, director at Newmarket Strategy and Will Browne, co-founder of Emrys Health.
At the AI Centre, we’re actively working to address these architectural challenges, developing scalable solutions for handling unstructured data and building the robust data pipelines necessary for sustainable AI deployment. Our focus in the London Secure Data Environment isn’t on creating more algorithms, but rather on establishing the foundational infrastructure that will allow existing AI solutions to work effectively in realworld clinical settings.
The road ahead
Success requires more than just technical solutions though. We need recognition of the challenge, appropriate funding, and strategic focus. Equally important is the governance framework that ensures public acceptability and ethical use of data.
As we move forward, we must maintain transparency in our objectives and be honest about both the challenges and opportunities. The NHS has a unique opportunity to lead in ethical, effective healthcare data utilisation, but this requires careful navigation of technical, cultural and governance challenges. M
FURTHER INFORMATION
www.digitalhealthrewired.com

Ahead of his talk at Rewired 2025, Andy Haywood, group chief digital officer at NHS Humber Health Partnership, shares his insights on how digital transformation is reshaping patient care and system-wide operations through innovative solutions and strategic deployment of technology
In healthcare we often talk about digital transformation, but what truly matters is how these changes impact patient care and experience. At the Humber Health Partnership, one of the new Group structures within the NHS, we’re embarking on an ambitious journey to revolutionise how patients interact with our services, starting with one of the most fundamental aspects - appointment booking.
Our upcoming patient-led booking system represents a significant shift from traditional methods. Currently, patients receive letters and face the often frustrating experience of making phone calls to arrange appointments, leading to high rates of non-attendance. By implementing smart booking solutions that integrate with the NHS app and use text messaging, we’re putting control back in patients’ hands while ensuring
we don’t digitally exclude those who prefer traditional communication methods.
This initiative goes beyond mere appointment scheduling. It’s about creating a comprehensive support system that provides patients with information about managing their health while waiting for procedures, ensuring they’re better informed and engaged in their healthcare journey.
One of our most exciting recent initiatives was a hackathon exploring the potential of Microsoft Copilot, which brought together over 150 staff members from various roles - clinical, operational, leadership, and frontline nursing.
The event generated remarkable insights into how AI could transform our operations while maintaining our commitment to responsible innovation.
We’re taking a measured but ambitious approach to AI implementation. While acknowledging the legitimate concerns around data protection and privacy, we’re also recognising AI’s immense potential to streamline administrative processes and enhance patient care. From generating initial drafts of discharge summaries to improving patient communication, AI presents
While acknowledging the legitimate concerns around data protection and privacy, we’re also recognising AI’s immense potential to streamline administrative processes and enhance patient care
opportunities to reduce administrative burden on clinical staff while maintaining safety and quality.
Digital transformation in healthcare isn’t just about implementing new technologies within hospital walls - it’s about creating a connected ecosystem that benefits the entire healthcare system. We’re expanding our virtual ward capabilities, looking at ways to prevent unnecessary hospital admissions and improve capacity management across the system. Our approach to digital transformation is guided by two key principles: focus on foundational improvements while planning E

Success in digital transformation requires more than just implementing new technologies
F for strategic change and deliver continuous improvement rather than waiting for perfection. This is exemplified in our Electronic Patient Record (EPR) programme. While we’re working towards procuring a new system, we’re simultaneously implementing improvements that can benefit patients and staff today. This dual approach ensures we maintain momentum while building towards larger strategic goals.
Understanding the critical role of data in modern healthcare, we’re investing in new data warehouse infrastructure to improve our analytical capabilities. This investment will enable better decision-making and support
our broader digital transformation initiatives, ensuring we can effectively measure and improve patient outcomes.
Success in digital transformation requires more than just implementing new technologies though. It demands careful alignment with organisational strategy while maintaining focus on immediate improvements. We’re ensuring that digital considerations are embedded in all strategic conversations, particularly when discussing new models of care delivery or system-wide changes.
Our group strategic framework, published in July, represents a comprehensive approach to digital integration across our healthcare system. At its core, we’re focused on eliminating system duplication and ensuring interoperability between our various platforms. This goes handin-hand with our vision of moving towards a single architecture that can support our entire organisation efficiently and effectively. We’ve made it a priority to engage users in setting these priorities, ensuring that our digital transformation reflects the real needs of those delivering and receiving care.

A key component of our strategy is enabling virtual hospital models, which we believe will be crucial in meeting future healthcare demands. As we look ahead,
The
our focus remains on delivering tangible benefits to patients while building the foundations for future innovation. The integration of AI, expansion of virtual care and implementation of patient-led booking systems are just the beginning of what promises to be an exciting period of digital evolution in healthcare.
As we continue this transformation journey, our focus remains on delivering tangible benefits to patients while building the foundations for future innovation.
Don’t miss the opportunity to hear more about our digital transformation journey and participate in the discussion about the future of healthcare technology. Join me at Digital Health Rewired 2025, where I’ll be sharing detailed insights about our experiences and the lessons learned along the way. M









SIGN UP FOR YOUR FREE DIGITAL SUBSCRIPTION



The publishers accept no responsibility for errors or omissions in this free service