CASE
Paramedics were recently called to a middle‑aged woman suffering profound shortness of breath. QAS Medical Director, Dr Stephen Rashford The patient had been well before bed, waking two hours later with severe dyspnoea. The only background history was very mild intermittent asthma and allergy – neither of which caused any issue previously. The Advanced Care Paramedics (ACPs) and Critical Care Paramedics (CCP) arrived.
36
The paramedics were confronted with a patient in extremis – profoundly dyspnoeic, hypoxic complicated by a reduced level of consciousness. The initial treatment was intramuscular (IM) adrenaline x3 and then progression to an adrenaline infusion. The High Acuity Response Unit (HARU) was also responded. Prior to HARU arrival, the paramedics administered hydrocortisone and commenced a magnesium infusion, in addition to high flow oxygen and continuous nebulised salbutamol. The HARU arrived to find a patient in a periarrest scenario, despite very prompt, aggressive therapy. GCS 4 HR 90 Palpable BP SpO2 <50%, Cyanosed, Respiratory Rate 40-50/ min with maximal accessory muscle movements The HARU paramedic contacted me to discuss the potential for a rapid sequence induction (RSI) as the next escalation point for therapy. The provisional diagnosis was either anaphylaxis or acute hyperfulminant asthma, both having similar presentations. This patient was critically unwell, with a great risk of deteriorating into cardiac arrest. A FaceTime video consultation into the scene was performed.
Autumn 2022
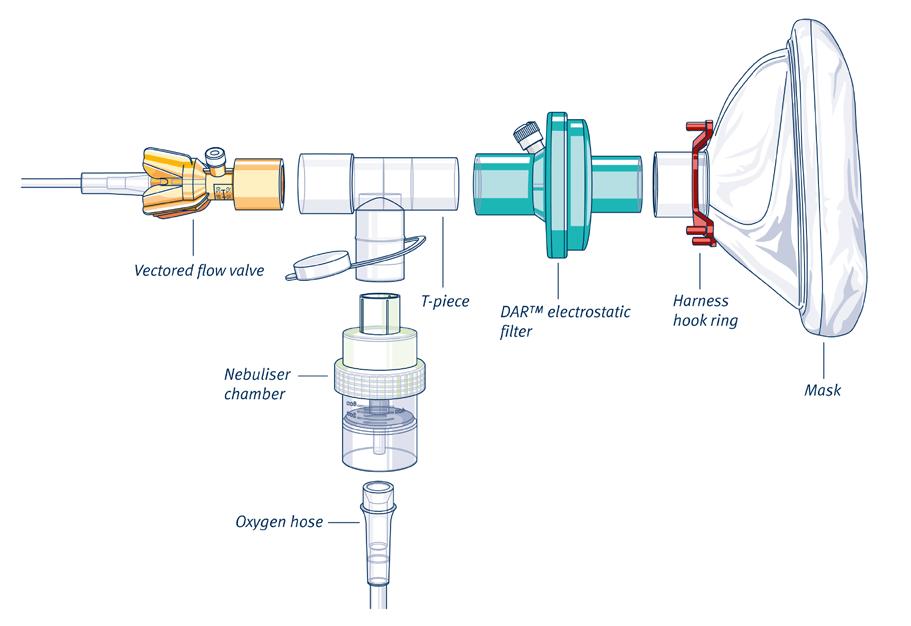
I was particularly concerned by the level of respiratory embarrassment and hypoxia, coupled with the inability to mount a tachycardic response despite this level of stress and being treated with 50mcg/min of intravenous (IV) Adrenaline. The risk of precipitating cardiac arrest with an RSI and positive pressure ventilation was also extremely high. This patient was on a clinical precipice – not a good scenario to be in. In discussion with the crews, we decided the next most appropriate step was improve mechanics for the work of breathing, rather than attempt an RSI. I requested that CPAP with continuous nebulised salbutamol be applied to the patient and the patient be sat upright, despite being deeply unconscious. Both of these measures improve work of breathing and optimise ventilation. It was important to remove the CPAP immediately if further deterioration occurred. The paramedics then in a very novel fashion sat the patient up ‘back-to-back’ with a paramedic, as she was still on the floor in her bedroom. Thankfully, over the next 20 minutes, the patient relatively improved. The SpO2 rose to 80%, the respiratory distress eased somewhat and the conscious level improved. At this point the patient was extricated from the house. Upon arrival at hospital, the patient was conscious, had been weaned off CPAP and the adrenaline infusion had also been weaned, now at 10mcg/min – quite an amazing result.