FIRST FEMALE Ms Houriya Kazim



The UAE’s First Female Surgeon

INTERNATIONAL FELLOWS WHERE ARE THEY NOW?
COLLES Q&A: Mr Morgan McMonagle + COLLABORATIVE INTENTIONALITY NEW THINKING: TRAUMA SURGERY

















































FIRST FEMALE Ms Houriya Kazim



The UAE’s First Female Surgeon

INTERNATIONAL FELLOWS WHERE ARE THEY NOW?
COLLES Q&A: Mr Morgan McMonagle + COLLABORATIVE INTENTIONALITY NEW THINKING: TRAUMA SURGERY
















































RCSI Fellows and Members,
As the key professional surgical membership organisation, our role is to drive the profession forward and support surgical Fellows and Members in achieving excellent surgical care for everyone. A recent census shows that there are more than 11,000 RCSI Fellows and Members and 1,700 A liate Members – a powerful community across 89 countries globally.
RCSI’s purpose is to educate, assess and develop surgeons and members of the wider surgical community at all stages of their career, and to set and safeguard standards for the optimisation of delivery of care to surgical patients. Earlier this year, the College launched the RCSI Surgery for Ireland Report, outlining a number of key recommendations on how to create a better working environment, and how to optimise the training, recruitment and retention of sta .

RCSI attracts the most highly committed candidates to surgical training. RCSI Fellows, of whom we are immensely proud, are dedicated to a lifetime in healthcare, and we are fortunate in maintaining a lifelong, career-long connection with them.
With that career-long connection in mind, this issue of Surgeons
Scope celebrates a number of internationally recognised Fellows who have maintained strong links with RCSI. ese include Dr Houriya Kazim, FRCSI 1993, the rst female surgeon in the UAE, and Professor Dhananjaya Sharma, FRCSI 2013, a champion of low-cost healthcare solutions in the developing world. eir service to the surgical community is inspirational.
Fellows can make an impact in so many di erent ways. In For ey are Good Fellows (page 10), it is wonderful to read about the various roads travelled by RCSI Fellows. ese roads have led to mentoring young surgeons, contributing to groundbreaking research, initiating pioneering surgical techniques and introducing innovative technology. In whatever sphere they operate, Fellows are committed to excellence.
And this starts early. Ms Evelyn Murphy, who will nish her higher surgical training in 2023, is a prime example of how we can help shape the future for RCSI Fellows. She is a recipient of the 2023 PROGRESS Women in Surgery Fellowship, which will take her to Sydney where later this year she will receive specialised training in Minimally Invasive Surgery and in Foot and Ankle Surgery. Also in this issue, Professor Paul Balfe (Fellow 2006) describes the competency-based approach to training in trauma surgery in Trauma Surgery: New inking (page 14). He emphasises that the onus lies squarely with the trainers to only sign o a trainee when satis ed that the trainee is capable of managing the breadth of undi erentiated emergency take as a day 1 consultant.
RCSI attracts the most highly committed candidates in surgical training.
Recently, I have had the great honour of bestowing Honorary Fellowships on surgeons who are making a di erence all over the world. During Charter Week, Dr Vivian McAlister received an Honorary Fellowship for his many distinctions, including the important role he played as a member of the Royal Canadian Medical Service in the Canadian Armed Forces. Dr Ajit K. Sachdeva received an Honorary Fellowship for his achievements as a surgeon, educator and scholar. Professor Maria B. Majella Doyle was awarded an Honorary Fellowship for her role in US national transplant surgery and her inspiring mentorship of surgical trainees. Professor Richard Irving received an Honorary Fellowship for the impressive scope of his clinical practice including his contributions to implantation otology, chronic ear disease, facial nerve surgery and vertigo. And Dr John G. Meara was recognised for his work in global surgery, including his roles as co-chair for the Lancet Commission on Global Surgery and commissioner on the Lancet Global Health Commission on High Quality Health Systems in the SDG era.

In April, I had the great personal honour to travel to Melbourne to present an Honorary Fellowship to Professor Graeme Clark AC, pioneer of the bionic ear or the multi-channel cochlear implant. I thank all of our Honorary Fellows for helping to transform the lives of so many people, through their dedicated work over recent decades and into the future. Print copies of Surgeons Scope are distributed without charge to Fellows and Members in Good Standing. Current articles and archives are made available to you online through Surgical Bulletin, the monthly newsletter sent to Fellows and Members. Please keep in touch with us and update us on your achievements so that we can share these with the rest of the community.


 Professor Laura Viani President, RCSI
Professor Laura Viani President, RCSI

I thank all of our Honorary Fellows for helping to transform the lives of so many people, through the work that they have done over recent decades and into the future.Professor Richard Irving, Professor Maria B. Majella Doyle and Dr John G. Meara Dr Ajit K. Sachdeva and Dr Vivian McAlister RCSI President, Professor Laura Viani and Professor Shirley Potter RCSI President, Professor Laura Viani and Professor Graeme Clarke













Earlier this year, RCSI launched the RCSI Surgery for Ireland Report. This proposes new networks for emergency surgery and sets out a series of recommendations aimed at ensuring equitable regional access to higherquality emergency surgical services, while ensuring smoother transitions of care for people who require complex emergency surgery. Key to the report are recommendations designed to help create a working environment that is optimal for the training, recruitment and retention of staff. Find the report on www.rcsi.com


In March, a significant and visible milestone was reached in our new Project Connect site at 118 St Stephen’s Green with the first of two tower cranes being erected just behind the Unitarian Church. This will remain in position for the duration of construction until completion of Project Connect in June 2025.


Professor Oscar Traynor, Professor of Postgraduate Surgical Training, and Brenda Farrell, Development Executive in RCSI’s Department of Surgical Affairs, along with representatives of four other postgraduate training bodies in Ireland, travelled to the Gulf in February 2023 for the formal launch of a new collaborative website promoting opportunities for postgraduate clinical training in Ireland.



Professor Juan Carlos Puyana has been appointed O’Brien Chair of Global Surgery at RCSI University of Medicine and Health Sciences. Professor Puyana will lead RCSI’s Institute of Global Surgery in its work to improve access to high-quality, essential surgical care for underserved populations. Professor Puyana joins RCSI from the University of Pittsburgh where he was Director of Global Health-Surgery.

Dr Niamh Keenan, Lecturer in Postgraduate Surgical Education, was delighted to welcome Professor Paul Ramphal of the University of the West Indies to RCSI, to facilitate a two-day cardiac surgical skills course for our cardiothoracic trainees. Professor Ramphal, a cardiothoracic surgeon, well known in the field of simulation, has developed the Ramphal Cardiac Surgery Simulator, a high-fidelity simulator allowing
trainees to practice complete cardiac operations in a realistic environment. Dr Keenan and many of our own cardiac surgeons and trainees were hugely enthusiastic about the experience of bringing cardiac surgical theatre to the RCSI wetlab, a wonderful learning and teaching experience. We are extremely grateful to Professor Ramphal, who has allowed us the use of his simulator for the next year.
RCSI conferred five new Honorary Fellows at ceremonies which took place during Charter Week 2023. The fellowships were awarded to Dr Vivian McAlister, Dr Ajit K Sachdeva, Professor Maria B. Majella Doyle, Professor Richard Irving and Dr John G. Meara. Honorary Fellowship is the highest distinction the College bestows, recognising outstanding achievement in surgery and other areas.

RCSI published guidance for patients travelling abroad for surgery, given the signi cant increase in the number of patients admitted through emergency departments in Ireland with complications of surgery undertaken abroad. “ e guidelines are aimed at helping people understand and manage the greater risk involved in having an operation in another country,” says RCSI Vice President, Professor Deborah McNamara. See www.rcsi.com for further details.

Ms Danielle McLaughlin, FRCSI and Dr Dawn Deacy, MRCSI have been announced by Operation Childlife and RCSI as the rst recipients of the Operation Childlife Fellowship. is prestigious bursary, awarded jointly by RCSI and Operation Childlife, aims at supporting surgical trainees or medical professionals in gaining additional expertise by participating in international paediatric healthcare missions, while also conducting research into the areas of altruism and global health in collaboration with local medical professional and Operation Childlife members.
Earlier this year, Professor P. Ronan O’Connell kindly donated a 28th Edition of Bailey and Love’s Short Practice of Surgery to RCSI Library Heritage Collection and the 2019 Hunterian Orator Gold Medallion to RCSI. Both the book and medallion are currently on display in RCSI.
RCSI President, Professor Laura Viani, Professor P. Ronan O’Connell, immediate past President RCSI, Ms Aíne Gibbons, Director of Development, RCSI and Ms Kate Kelly, Director of Library Services.



CSI was granted a Charter by George III on the 11 February 1784, and for the last 239 years, the College has celebrated the Charter on the Friday closest to that calendar date, falling on 3 February this year. But, in reality, the Charter programme begins the preceding Saturday, with meetings, presentations and parallel sessions held every day leading up to Charter Day itself.
So, it’s a week that sees the College brimming with activities, all focused on a theme chosen by the President. Charter Meeting 2023 commenced on Saturday, 28 January with the Annual Meeting of the Irish Surgical Training Group (ISTG), which included the Bosco O’Mahony Lecture delivered by RCSI Council Member, Professor Michael Kerin. The lecture is named in honour of Mr John Bosco O’Mahony, one of the longest serving members of the RCSI Council. Professor Kerin delivered the prestigious lecture on Irish surgery – A Discipline in Evolution: Implications for Training and Practice.
The National Office of Clinical Audit (NOCA) held its Annual Conference as part of the Charter Meeting on Tuesday, 31 January. NOCA is a publicly funded independent institution, based in and supported by RCSI. The meeting, on the theme of Audit Matters, looked at NOCA’s key achievements, as well as future objectives to develop a national clinical audit across our healthcare system.
Also on 31 January, RCSI hosted the 17th Annual Intercollegiate Case Presentations, an annual competition that brings together the surgical societies of Irish medical schools. The winner of the David Bouchier-Hayes Award was Meadhbh Ní Mhiochain from the School of Medicine, University of Galway.
The Annual Health Service Quality Improvement and Innovations Conference was held on Wednesday, 1 February, hosted by RCSI National Clinical Programmes. The conference’s invited speaker was Mary Dixon Woods, Director of The Healthcare Improvement Studies (THIS) Institute and the Foundation Professor of The Healthcare Improvement Studies in the Department of Public Health and Primary Care at the University of Cambridge. Wednesday afternoon also saw the Faculty of Surgical Trainers’ Meeting, parallel sessions from the RCSI Faculties of Dentistry and Nursing and Midwifery and the Irish Institute of Pharmacy, as well as the 33rd Annual VideoSurgery Meeting that evening.
Key symposiums were held across Thursday and Friday on the future of surgery and healthcare, including those related to technology, training, clinical audit and cancer care. The final symposium on the configuration and staffing of safe surgical services included the official launch of RCSI’s Surgery for Ireland report, which was presented to Dr Colm Henry, HSE Chief Clinical Officer.
With an impressive line-up of speakers this year we present just some of the key highlights:
Professor Paul Ridgway introduced a very interesting session by Consultant Haematologist Professor Siobhan Glavey on The Then, Now and When of Personalised Cancer Medicine. Professor Glavey described haematology as being the specialty at the frontline of cancer medicine. She explained the concept of precision medicine and how categorising patients into sub-groups of cancers that are completely different genomically means that precision therapeutics targeted to the tumour cells can be so effective. Genomics, she said, is the reason why Multiple Myeloma survival rates have improved. Professor Glavey’s lecture included observations on cancer immunotherapy, and how CAR-T treatment has benefited children who have been diagnosed with ALL (Acute Lymphocytic Leukemia).
Next up was Consultant Clinical Geneticist Dr Terri McVeigh who trained in Ireland and is now based at the Royal Marsden in London. Dr McVeigh presented a vivid snapshot of what is happening in the NHS in the UK in terms of genomic profiling. The priority is to establish if a patient has a heritable predisposition
The original Charter dates from 1784. It was revised in 1828, 1844, 1883, 1885 (‘And we do hereby, for us, our heirs and successors, grant, declare and appoint, that all provisions of the Charter, Bye-Laws, and Ordinances as to education, examination, and granting diplomas to Fellows or Licentiates shall extend to include women’). In the 20th century it was revised in 1965, when RCSI was designated a Charity. Early in the 21st century, it was amended again, in 2003, paving the way for RCSI to award its own degrees.

integral to characterising tumours. This is critical to treatment, and is shown to detect early relapse. Dr McVeigh said that “every specialist will have to upskill”. She outlined the challenges in cancer care and the development of liquid biopsy, which might lead to overdiagnosis. She observed that while genome sequencing is relatively inexpensive, the staff and infrastructure required to conduct the analysis is not. Dr McVeigh concluded by summarising the NHS Genomic Strategy priority areas in terms of the mainstreaming of services (to include those not trained in genetics), equity of access, data and digital transfer and research and innovation.



After lunch and an exhibition by industry partners Johnson & Johnson, Medtronic and Olympus among others, the O’Flanagan Lecture Theatre filled up when Professor Margaret O’Donnell gave the citation for internationally respected plastic surgeon Dr John G. Meara who delivered the Annual Johnson & Johnson Lecture. He chose the title of his lecture because he said he was “grappling with the neo-colonial aspects” in the world, namely in global surgery. Many people have benefited from serendipity and charity, he said, but “serendipity is not a good strategy, and charity is not a solution. They are seeds, but they don’t grow unless they sit in the soil of a health system.” Dr Meara talked about the key outcomes of the Lancet Commission on Global Surgery, namely the vision and key messages including the fact that five billion people lack access to healthcare, 81 million face catastrophe and $350 billion dollars are needed, but the positive impact of that spend would be $12 trillion dollars. He said that the idea of planetary health and the biosphere is now talked about by the UN and while it is hard to make predictions for surgery of the future, the Venn diagram for surgical care and climate change overlap and the world is finally breaking some ground in this regard. He described the Honorary Fellowship to be bestowed on him later that evening as an “intense honour”, referring to his Irish ancestry and his father’s pride at this accolade.




The 45th Millin Lecture, on the topic of Malignant Melanoma, An Unlikely Poster Child for Personalised Cancer Treatment, was delivered by Professor Shirley Potter, Consultant Plastic and Reconstructive Surgeon, Mater Misericordiae University Hospital. Professor Potter was the first plastic and reconstructive surgeon to have the honour, and only the seventh female surgeon. Ireland’s skin cancer problem outweighs all other cancers in terms of new cases, and is the fourth most common cancer in men and women, affecting women mainly on limbs and men on the trunk. Professor Potter’s fascinating lecture described the unique properties of melanoma and how immunotherapy has boosted survival rates, with the focus now on moving towards personalised management of the disease.

7 Brent Van Eccelpoel, Dr Ozanan Meireles and Professor Ronan Cahill.
8 Jack Logue and Mary Ellen McMahon.
9 Professor Conor Deasy.
10 Patrick Collins, John O’Kelly and Sarah Norton.
11 Professor Calvin Coffey, Professor Gutschow Christian and Professor P. Ronan O’Connell.


12, 13 An audience of more than 100 medical students, surgical trainees, interns, NCHDs, and junior and foundation doctors attended the Becoming a Standout Surgeon event.





14 Ms Jessica Ryan, Professor David Healy, Mr Dara Kavanagh, Professor Kevin Barry and Ms Ciara Tallon.

On Friday, the popular Becoming a Standout Surgeon session for Affiliate Members was followed by the 98th Abraham Colles Lecture, delivered by Luc Morris, Memorial Sloane Kettering Cancer Center. He designed his intriguingly titled presentation The Cobra Effect: How COVID-19, Immunolology and Surgical History Can Help Us Understand Indolent Cancers, he said, to interest the polymath Abraham Colles himself whose 250th anniversary of his birth is marked this year. Dr Morris drew a parallel between the tendency to overdiagnose indolent cancers with how colonial administrators offered a bounty on cobra heads, hoping to reduce the number of deadly snakes only to find that everyone started to breed cobras to avail of the cash, so that there were more at the end of the initiative than there were at the beginning. He said the incentive to find disease leads to more disease being discovered. He questioned if every human condition, including slow growing, highly prevalent indolent cancers, need to be found and treated?

15 RCSI Vice President, Professor Deborah McNamara and Professor Frank Keane.


16 Amit Kalra, outgoing President, RCSI Student Union and Lina Adil, outgoing Vice President and Education Officer, RCSI Student Union.

17 Dr Anna Clarke, Professor Emma Meagher and Professor Noel Williams.
18 Professor Richard Irving, Professor Maria B. Majella Doyle and Dr John G. Meara.
19 Mr Kenneth Mealy and Mr Dennis Lawlor.

20 Jack O’Grady, Dr Frank Kenny and Ailbhe Kenny.


21 Dr Luc Morris, Ms Victoria Rose and Professor Camilla Carroll.

RCSI invited Orla Tinsley, journalist, Cystic Fibrosis campaigner and multimedia artist, to give the 30th Carmichael Lecture. She was the first patient advocate to give the Carmichael Lecture and she proved to be most worthy of this honour. What Good Looks Like – From a Patient Perspective was a deeply moving and inspiring account of her decades-long patient journey and her experiences of patient/practitioner interactions. She highlighted the differences between her very positive experience in New York when undergoing a double lung transplant with her visits to a Dublin hospital during COVID-19 when there were no temperature checks, no name checks, no precautions to protect a vulnerable patient. She talked of how “being born in the kingdom of the sick and holidaying in the kingdom of the well” is somewhat dependent on how clinicians respond to their patients, not just in a treatment sense, but in an emotional sense, creating structure and safety. She urged healthcare professionals to think differently, to use language carefully, to “sit with your patients and spend time”.

As proceedings drew to a close, Professor Viani thanked the many colleagues and external faculty who contributed to this really excellent programme and the Surgical Specialties and RCSI Faculties who put together excellent parallel sessions. On Thursday and Friday evening, Professor Viani also conferred Honorary Fellowships on Dr Vivian McAlister, Dr Ajit K. Sachdeva, Dr Maria B. Majella Doyle, Professor Richard Irving and Dr John G. Meara, who have contributed greatly to the science and practice of surgery and society as a whole. Charter celebrations culminated in a most enjoyable Charter Dinner. ■

RCSI INTERNATIONAL FELLOWS ARE GLOBAL LEADERS IN SURGICAL PRACTICE AND IN GROUNDBREAKING RESEARCH. WE FOLLOW THE CAREERS OF EIGHT FELLOWS, AND FIND OUT WHERE THEY ARE NOW
MCh, PhD, FRCSI, FACS, FASCRS, FRCSI (Hon), MAMSE
Colorectal Surgeon; CEO and President, Cleveland Clinic Florida; President, American Society of Colon and Rectal Surgeons.
In his role as the CEO and President of Cleveland Clinic Florida, Conor Delaney oversees ve hospitals, a state-of-the-art research centre and numerous outpatient centres located across southeast Florida, and serves as a member of the Cleveland Clinic enterprise Executive Team. Previously, Professor Delaney was Chairman of Cleveland Clinic’s Digestive Disease and Surgery Institute, where he was responsible for a number of departments including the departments of colorectal surgery; gastroenterology; hepatology; nutrition; general and transplant surgery. Professor Delaney completed a residency through RCSI, a transplant immunology fellowship at the University of Pittsburgh and a colorectal surgery fellowship at Cleveland Clinic. He was a sta surgeon at Cleveland Clinic in the Departments of Colorectal and Minimally Invasive Surgery from 2000-2005 and was Chief of the Division of Colorectal Surgery, Chair of Digestive Health and Vice Chair of Surgery at University Hospitals Case Medical Center in Cleveland.
Professor Delaney currently serves as the President of the American Society of Colon and Rectal Surgeons. He is also Cleveland Clinic’s Robert and Suzanne Tomsich Distinguished Chair in Healthcare Innovation and a Professor of Surgery at the Cleveland Clinic Lerner College of Medicine. He has published 11 books, more than 420 original manuscripts and chapters and has given over 450 lectures nationally and internationally. His clinical interests include laparoscopic colorectal surgery; carcinoma of the colon, rectum and anus; Crohn’s disease and ulcerative colitis, sphincter-saving surgery; reoperative abdominal surgery and colonoscopy. His research interests include various aspects of colorectal surgery, surgical techniques, optimisation of postoperative recovery and optimisation of value in clinical care.
“My day-to-day work is primarily with the 11,000 caregivers on our Florida team, although I continue to have many enterprise level virtual meetings each week, as well as regular trips back to Cleveland where I was for 22 years. As we come out of the challenges of the pandemic and the healthcare sta ng crisis, our priorities are focusing on our mission of caring for life, researching for health and educating those who serve. It has been a privilege to partner with and add to the Florida team as we integrate new hospitals with the enterprise, bring the right scale of services to each hospital and submarket, and bring Cleveland Clinic care to our communities,” says Professor Delaney.
BSc, MB, FRCSI, PhD
Consultant Neurosurgeon with subspeciality interests of Neuro-Oncology and Traumatic Brain Injury, Queen Elizabeth Hospital, Birmingham.
Philip O’Halloran graduated from University College Cork in 2003 with a BSc (Physiology) before studying Medicine in RCSI where he also completed his Higher Surgical Training. During his neurosurgery training, Mr O’Halloran was the lead author and co-investigator of the Beaumont Brain Tumour Biobank. In 2017, he was awarded a PhD in Neuro-Oncology following research conducted at RCSI and the European Institute of Molecular Imaging in Germany.

In 2019, Mr O’Halloran was awarded the prestigious Neuro-Oncology/Skull Base surgical fellowship at Toronto Western Hospital. Subsequently, he became the rst Royal College of Surgeons in England approved Surgical Neurotrauma Fellow at the Royal London Hospital Major Trauma Centre.

In 2021, he was awarded the Dan Rooney Concussion Fellowship, during which he spent time at the UPMC Sports Medicine Concussion Program in Pittsburgh, Pennsylvania, to develop baseline clinical knowledge of concussions and their evaluation, and study clinical research methods. e academic position was also the research lead of UPMC Sports Concussion Network in Ireland.
Mr O’Halloran was appointed as a Consultant Neurosurgeon at Queen Elizabeth Hospital, Birmingham at the beginning of 2022 and has expertise in awake craniotomy, day case glioma surgery, laser interstitial thermal therapy (LITT), and uorescence guided surgery as well as intra-operative monitoring. He is an Honorary Senior Clinical Lecturer at RCSI and research interests include translational oncology incorporating orthotopic glioma models/patient-derived xenogra s. Mr O’Halloran is also an Associate Editor of the British Journal of Neurosurgery. An internationally recognised opinion leader in sports-related brain injury as well as an independent match day doctor of the English Rugby Gallagher Premiership and European Cup, he is also the principal investigator of the pioneering Rugby Headgear E ectiveness Study.
“My role is to independently assess the e ect of this new headgear design on brain injury using state-of-the-art blood and saliva biomarkers, neuroimaging, instrumented mouthguards and neurocognitive tests. We have assembled a world-leading, independent panel of scienti c and medical experts in brain health and brain injury to monitor the study; it represents an important piece of the jigsaw of what is an ongoing international collective e ort to protect amateur and professional players,” says Mr O’Halloran.
MB, BCh, BAO, MCh, FRCSI
Consultant Plastic and Reconstructive surgeon at Waikato Hospital, Middlemore Hospital and Gisborne Hospital, Private practice at Waikato Specialist Centre, Hamilton, New Zealand.
Deirdre Seoighe undertook specialist training in plastic and reconstructive surgery in Ireland, followed by a fellowship in burns surgery at Middlemore Hospital, Auckland. She has been working at Waikato Hospital in Hamilton, New Zealand since 2017. She is the clinical lead for burns surgery covering a vast area in the central North Island of New Zealand. is includes the Taupo Volcanic Zone and a very active geothermal region. Ms Seoighe is the clinical lead of a research group looking speci cally at geothermal and volcanic injuries. During her time at Waikato Hospital, she has served as head of department and also helped to set up a combined plastic surgery and dermatology medical laser unit. e plan is to provide a publicly-funded high quality and comprehensive laser treatment unit that will treat patients from all over New Zealand.
“New Zealand has one of the highest skin cancer rates in the world. is places huge demands on the plastic surgery department as we try to deliver services to almost one million people over a vast geographical distribution. Plastic surgery is a challenging and variable specialty. ere is always a new challenge; recently I had the opportunity to lead the plastic surgery component of New Zealand’s rst hemicorporectomy. Floods, cyclones, a volcanic eruption and a global pandemic have put pressure on the hospital system and our department. Despite setbacks and challenges, we continue to grow our department and try to improve the quality of care we deliver to our patients,” says Ms Seoighe.
MD, PhD,
Hon D Arts, FRCSIConsultant General Surgeon
Cleveland Clinic London, Chevalier de la Légion d’Honneur, President American College of Surgeons (UK Chapter), Membre de l’Academie Française de Chirurgie.

A specialist in bariatrics and kidney/pancreas transplantation surgery, Nadey Hakim started the rst Pancreas Transplant Programme in South East England. He was the British surgeon on the International team which performed the world’s rst successful arm transplant and was the rst surgeon to be awarded the prestigious Max orek Professorship of Surgery. With over 250 peer-reviewed papers and 24 textbooks, he is a proli c author and sought-a er international speaker.
Professor Hakim gained his medical degree from Paris Descartes University with the prestigious award of Laureate of the Faculty of Medicine. He trained in surgery at Guy’s Hospital London. At the University of London, he obtained his PhD a er completing a gastrointestinal fellowship at the Mayo Clinic and a transplant fellowship at the University of Minnesota.
Currently Professor of Transplantation Surgery at Imperial College London
and Professor of General Surgery at the Cleveland Clinic London, Professor Hakim’s academic awards and professional achievements are extensive.
ey include ve honorary professorships at universities worldwide including Baskent University and several international visiting professorships. In 2007, he was awarded the J. Wesley Alexander Prize for outstanding transplantation research.
Formerly World President of the International College of Surgeons, Vice President of the Royal Society of Medicine and Vice President of the British Red Cross, Professor Hakim is a member of several professional organisations, holds educational roles such as Assessor for the Royal College of Surgeons of England, Member of the International Relations Committee of the American College of Surgeons and President of the UK Chapter of the American College of Surgeons. His editorial roles include having been Editor in Chief of International Surgery for 11 years before becoming Emeritus Editor.
Currently Councillor for Europe of the e Transplantation Society and Vice President of the International Medical Sciences Academy. He was made Chevalier de la Légion d’Honneur in 2016.
“As a Member of the International Relations Committee of the American College of Surgeons I have o ered my transplant surgical skills to countries in the developing world, having regularly visited Nigeria to perform live related kidney transplants. I will very soon perform the rst kidney transplant in St Kitts and Nevis, having been invited by the Prime Minister of the country. As the Councillor for Europe of the Transplantation Society it gives me great pleasure to expand the eld of transplantation to less fortunate countries,” says Professor Hakim.
MBBS, FRCSI, MRCOphth
Consultant Ophthalmic Surgeon, Royal Victoria Eye and Ear Hospital; Tallaght University Hospital and Hermitage Clinic.
Rizwana Khan completed her Basic Surgical and Higher Surgical Training in Ireland, followed by a two-year fellowship in Orbits, Oculoplastics and Neuro-Ophthalmology at the Royal Victoria Eye and Ear Hospital, Dublin.
Orbits and oculoplastics is a subspecialty of ophthalmology dealing with eye socket and eyelid disorders and its management in the form of plastic and reconstructive surgery. It also includes the management of lacrimal system disorders, and eyelid and socket tumour reconstructive surgery.
Ms Khan has a keen interest in the use and development of innovative technology in her subspecialty, including the use of CO2 laser in oculoplastic surgery and image-guided navigation in orbital surgery. She also specialises in multifocal intraocular lens implantation.

She is the co-director of a fellowship programme in Orbits, Oculoplastics and Neuro-Ophthalmology in the Royal Victoria Eye and Ear Hospital, and is currently undertaking a doctorate with RCSI while guiding her trainees in surgical training and research.
“I have always been interested in the use of new innovative technology in ophthalmic surgery. I secured a state-of-the-art electromagnetic imageguidance technology for orbital surgery in the Royal Victoria Eye and Ear Hospital. I have been leading a clinical trial to explore its role in our surgical practice and have shown that this technology has potential to make complicated orbital surgery safer, faster and more e ective,” says Ms Khan.

MD, MCh, PhD, FACS, FASCRS, FRCSI (Hon)
Robotics Pioneer – Urology; Professorial Fellow, University of Melbourne; Consultant Urologist, Epworth Hospital, Richmond Campus, Melbourne; Director and CEO at Australian Medical Robotics Academy.
Tony Costello is one of the leading prostate specialists in Australia and a pioneer in the eld of robotic surgery in urology, performing the rst open radical prostatectomy using robotic surgery at Epworth Hospital in Australia in 2003. Since then, over 2,600 cases of robotic radical prostatectomy have been performed at Epworth. Professor Costello is an invited faculty member of the American Urological Association where he teaches aspects of robotic surgery to an international audience annually. He is also on the Editorial Board of the US publication Journal of Robotic Surgery, the British Journal of Urology and the Journal of Endourology.
Professor Costello is the only Australian member of the American Association of Genitourinary Surgeons. e AAGUS is an association of leading academic urologists from the US, Canada and around the world dedicated to the study of diseases of the genitourinary system. Active membership is limited to 75 of the world’s most distinguished academic urological specialists.
“I have had the great privilege to train a number of Irish urologists in the art of robotic surgery. I have always admired Irish surgery and in particular the talent in Irish urology. My recent collaboration with RCSI has reinforced my belief that RCSI is the most nimble College in its ability to deal with the complexities of providing a modern surgical pedagogy. As a proud Honorary Fellow of RCSI, it is wonderful now to be working in collaboration in the area of Education and Robotic Assisted Surgery. It gives me such pleasure to have teamed up with RCSI and to be launching the Foundation of RAS course developed at IMRA, which RCSI will deliver to Irish surgical trainees. is is such an important technological advancement and RCSI show great leadership in adding it to their surgical training programme. I really look forward to seeing this collaboration develop and to achieving great things together.”
MB, BCh, BAO, MCh, FRCSI, PROGRESS Women in Surgery Fellow 2023
Training in Trauma and Orthopaedics at RCSI, due for completion in 2023, and is currently posted at Galway University Hospital. She has four postgraduate quali cations, has published over 55 papers and has been awarded and shortlisted for more than 15 prizes, bursaries and research grants for her work.
Ms Murphy is the recipient of the 2023 PROGRESS Women in Surgery Fellowship. e prestigious bursary, awarded by RCSI and supported by Olympus Medical, promotes female participation in surgical training at

fellowship level. Ms Murphy will undertake a fellowship in Minimally Invasive Surgery and Orthopaedic Foot and Ankle Surgery in Sydney. It will incorporate percutaneous surgery, sports surgery, trauma and total ankle replacement, covering basic and complex fusions and osteotomies and forefoot reconstructions. Following the fellowship, Ms Murphy will be one of the pioneers in this eld in Ireland.
“I am actively involved in mentoring junior trainees completing research projects and supporting them in presenting at conferences and progressing to higher degrees. I was recently part of the faculty at the ATLS trauma provider course in Kilkenny and got to experience multidisciplinary teamwork in action. I am in the nal stages of preparing to move to Sydney to pursue my fellowship in minimally invasive foot and ankle surgery. I am delighted to receive the 2023 PROGRESS Women in Surgery Fellowship and honoured to be the rst Orthopaedic recipient of this award. During my fellowship I intend to develop key skills in minimally invasive foot and ankle surgery which will allow me to continue to innovate in the eld of orthopaedics. I recently was successful in my application for a consultant position in Cork University Hospital,” says Ms Murphy.


MB, BCh, BAO, LRCP/LRCS, FRCSI
Senior Consultant Neurosurgeon with a subspecialty in Spine Surgery; Medical Director at Oxford Spine and Neurosurgery Centre, Mount Elizabeth Novena Hospital, Singapore.
Colum Nolan graduated from RCSI and undertook comprehensive neurosurgery training in Ireland and at the Royal Melbourne Hospital in Australia. He pursued his interest in complex spine surgery as a spinal fellow at Addenbrooke’s Hospital in Cambridge, UK, gaining experience in the management of degenerative spine disorders, complex spinal tumours and fractures, and developing his skills in minimally invasive spine surgery. Dr Nolan was the former Spine Director at the National Neuroscience Institute (NNI) and was instrumental in growing the combined NNI-Tan Tock Seng Hospital (TTSH) spine service. He also started and headed the neurosurgery service at Sengkang General Hospital. He is currently a visiting consultant at NNI and the National University Hospital.
Dr Nolan has been published in many international journals and presented at many local, regional and international conferences. He was a member of the medical council, professional development committee and peer-review learning quality assurance committee at NNI, and a clinical physician faculty member for the integrated neurosurgery training programme. He was also an adjunct assistant professor at Duke-NUS Medical School. ■
Following the Fellowship, Ms Murphy will be one of the pioneers in this field in Ireland.













































t’s generally recognised that emergency surgery (both trauma and non-trauma) has in some ways played second ddle to other areas of surgical endeavour by way of resource investment, training etc. By its nature, it o en occurs out of hours, isn’t always consultant supervised and there may be signi cant interpersonal and interinstitutional variability in outcomes.
Recognising the imperative that surgical training should aim to equip practitioners with the knowledge and skills required to competently deal with the range of presentations that might reasonably be expected on emergency take, the four Royal Colleges of the UK and Ireland set about developing a new Higher Surgical Training (HST) curriculum which would once again put the acquisition of emergency surgical competencies front and centre of the HST programme.
e new surgical curriculum came into e ect in July 2021 and, in addition to the knowledge and competencies speci ed with respect to the trainee, the onus is now squarely on trainers only to sign o a trainee when they are satis ed that the trainee is capable of managing the breadth of undi erentiated emergency take as a Day 1 consultant. To that extent, the training programme is now rmly competency rather than time based.
e launch of the new curriculum followed closely on the launch by the Irish government of a comprehensive blueprint for ‘A Trauma System for Ireland’ which will see the rollout of what is hoped will be a top-quality trauma network over the next six to eight years. e network will comprise a ‘Hub and Spoke’ model involving two Major Trauma Centres (Mater Misericordiae University Hospital (MMUH) and Cork University Hospital (CUH) and
ten Trauma Units throughout the country. e core trauma team will comprise: general surgery, trauma and orthopaedics, emergency medicine and anaesthesia/critical care. is core team will be expected to handle the breadth of undi erentiated emergency take, calling on other specialties as available and as required.
To re ect the new curriculum requirements, trainees now sitting the FRCSI exam will be expected to have acquired the requisite knowledge and competencies in the area of emergency surgery. But while the College already had a good nontrauma emergency surgery training programme run in conjunction with the World Society of Emergency Surgery (WSES), until recently there was no corresponding programme for trauma surgery training.
Professor Paul Balfe
At the height of the pandemic, when it was unclear if and when it would ever end and travel restrictions would li , we decided to develop a trauma surgery skills course from the ground up for our Irish HSTs drawing on our own collective experience and the best of international practice. To date, two courses were successfully rolled out in 2022 with further courses scheduled for 2023. But regardless of how successful such stand-alone courses may be, they necessarily operate in something of a silo without connection to a wider trauma forum/community.
Following some preliminary discussions, in 2022 the then RCSI President, Professor P. Ronan O’Connell established a small working group with a view to exploring the possibility of adopting one of the existing internationallyaccredited training modules – either the De nitive Surgical Trauma Care (DSTC)/De nitive Anaesthetic Trauma Care (DATC) or De nitive Surgical Trauma Skills (DSTS) – into the College’s formal training programme. In

addition, there was recognition of the need to forge international relationships with a view to creating rotation and fellowship opportunities for our HSTs in the area of trauma surgery.
In November 2022, Mr Sean Johnston, Chair, General Surgery Training Committee (GSTC), Ms Caroline McGuinness and I travelled to Johannesburg where we had the opportunity to completely immerse ourselves in every aspect of the DSTC/DATC from both the surgical and operational perspective. We also visited two Level 1 trauma centres and had very positive discussions with relevant parties regarding the possibility of Irish ST8/ST8+ trainees rotating through such units. It was ironic, and in some ways hilarious, that when we arrived at the 4,000 bed Chris Hani Baragwanath Academic Hospital and walked into the Trauma Resuscitation Bay, the rst person we encountered was Dr Jimmy Lee from Ireland, who had just completed his training in emergency medicine and who was spending three months at the hospital before taking up a consultant post in UCHG.
It is planned to similarly assess the RCSE’s DSTS course in June 2023. Both courses will then be evaluated against a set of objective criteria and a formal recommendation made as to which should be adopted by the College in the best interests of our trainees/practitioners and ultimately our patients. Whichever course is chosen, it is envisaged that suitably credentialled Irish faculty would join international faculty in delivering the courses.
It is important we get this right given the changing practice landscape and the College is absolutely committed to doing so.
By Professor Paul Balfe, General Surgery Lead, Trauma Education and Training, RCSI; Mr Sean Johnston, Chair, GSTC, RCSI; Professor Kevin Barry, Dean of Postgraduate Surgical Training, RCSI. ■
The onus is now squarely on trainers only to sign off a trainee when they are satisfied that the trainee is capable of managing the breadth of undifferentiated emergency take as a Day 1 consultant.
AN ADVOCATE FOR COLLABORATIVE INTENTIONALITY, DR MARIE MORRIS’ WORK IS FOCUSED ON THE EMPOWERMENT OF MULTIDISCIPLINARY TEAMS
r Marie Morris PhD, Senior Lecturer in Postgraduate Surgical Education, RCSI has over 35 years’ experience in health sciences, holding both clinical and education posts.

For the rst half of her career she worked in acute and critical care as a clinical nurse specialist and postgraduate nurse educator in the UK. She then moved into undergraduate medical education in Ireland. A er over a decade of teaching undergraduate medical students, she completed a PhD in Surgical Education and led the masters degree in Surgical Science and Practice at RCSI Dublin in collaboration with the Programme Director, Professor Oscar Traynor.
e focus of Dr Morris’ work for many years has been on interdisciplinary team collaboration and she is an advocate for collaborative intentionality, the empowering of teams by instilling a mindset of deliberately seeking out collaboration.
“When I was working in intensive care,” says Dr Morris, “I noticed that the junior doctors starting their jobs were like ducks out of water. ere’s no doubt that anyone nishing a medical degree has expertise in medical information, but what was missing was translational transferability. Medical
school didn’t teach them how to be a doctor. ey had a head full of knowledge of respiratory disease and how to do a respiratory assessment and how to read arterial blood gases, but at two o’clock in the morning when they were standing in front of Mr O’Brien in acute respiratory distress they would freeze because suddenly they had to pull all this information together and do something fast. Observing this gap between the young doctors’ academic learning and how they were poorly prepared for stressful clinical situations, I set up an outreach programme where the senior nurses in intensive care started teaching and supporting the junior doctors in relation to the step down of ICU patients. I am a strong advocate for senior nurses crossing traditional hierarchical boundaries to share their expertise with junior doctors to ensure patient safety.”
On returning to Ireland, Dr Morris considered postgraduate entry to medicine but felt that she could make more of an impact by bringing her experience as a senior nurse into undergraduate medical education by reforming the medical curriculum to improve junior doctors’ preparation for clinical practice. A er a masters in Clinical Medicine in Trinity College Dublin, she was appointed to lead the undergraduate clinical skills programme in the School of Medicine there.
“I could see very quickly that what was missing was communication skills training. We know from all the human factors literature that doctors are generally very well trained, and don’t tend to make technical errors, but that major errors generally result from a breakdown in communication. My masters thesis therefore focused on the design and implementation of an undergraduate curriculum on communication skills training and assessment.
“I always feel that we train medical students as if they are only children. e system in medical school whereby medals and the choice of internships goes to those who perform best in exams makes them highly competitive, so that their peers are their competition, not their support network. And then we put them through an internship, and it’s as if mummy and daddy have suddenly adopted four children – a nurse, a physiotherapist, a pharmacist, and an dietician – and we tell them to go and play nicely. ey are suddenly expected to communicate and collaborate and become part of a ‘team’ with unfamiliar people, unsure of the exact roles and scope of knowledge of other disciplines.”
Dr Morris believes that training doctors and surgeons in isolation is wrong, and may lead to poorer outcomes for patients.
“Patient care is like a jigsaw or puzzle. As the junior medical/surgical person in the team, the doctor generally has the most pieces of the puzzle, but they won’t nish the puzzle properly if they don’t have a piece from the nurse, the physiotherapist, the pharmacist and the dietitian. And where they don’t get all those pieces to make the big picture, that’s where error happens and the patient su ers.”
Dr Morris designed and introduced a simulation-based module to her undergraduate teaching of clinical skills, so senior medical students could rst learn and come to understand their strengths and limitations in a psychologically safe environment.
“ ey need to know when to ask for help. To learn that even if it feels really uncomfortable, and even if the other person on the end of the phone says you should know the answer, their responsibility is to the patient and also to themselves is to ask for help early.”
When Dr Morris took up the role of leading the new masters degree in Surgical Science and Practice at RCSI in 2019, e ectively a one-year simulated intern job, it was an opportunity to introduce the missing interdisciplinary dimension to medical education and to implement a totally new way of doing things. In collaboration with Professor Walter Eppich, Chair, RCSI SIM Centre, she explored ways of promoting collaborative intentionality into simulation-based education.
With the support of the simulation team in 26 York Street, the students had their theatre practice, ward rounds and clinics, they undertook a simulated clinical post in a psychologically safe and supervised setting.

It was the optimal opportunity for instilling a mindset of intentional, deliberate interdisciplinary collaboration: “I reached out to the Schools of Physiotherapy, Pharmacy and Nursing and we worked together, taking a top down and bottom up approach. I wanted to instil the concept of deliberately, intentionally communicating and collaborating outside your own discipline into all the students. e support and involvement of cardiac surgeon consultant, Mr Simon MacGowan, legitimised the importance of and the essential contribution other disciplines make to clinical decision making and safe patient care.”
Each cohort of students shared the responsibilities of their role, so each group could better understand the other disciplines – learning with, from and about each other. ey were then placed in multidisciplinary groups. When they went to meet simulated patients, they observed each other take histories to gain a better understanding of the information required by each discipline. As a team they wrote up each case, and presented it to the consultant and received feedback from their discipline faculty.
“ e intention was to build a community of interdisciplinary learners,” explains Dr Morris. “ ey went to co ee together, stayed together and didn’t silo o into their own disciplines. It worked out very well in terms of starting to instil a new mindset or cultural change. It’s going to take time, but it’s about re-iterating to all disciplines that they each have accountability for patient safety and that by working together in collaboration they will achieve better outcomes for their patients, something they all obviously care deeply about as healthcare professionals.”
Feedback from the doctors revealed that, before commencing the masters, they had underestimated how much knowledge the nurses had, and they
Dr Fridah Bosire
“I am a strong advocate for senior nurses crossing traditional hierarchical boundaries to share their expertise with junior doctors to ensure patient safety.”Dr Marie Morris, winner of the National Teaching Hero Award for student mentorship and coaching, with Dr Zahra Khalaf, Ms Celine Sooknarine, Ms Abigail Tan and Dr Suhitha Mahadev.
also observed that in terms of discharge planning, if on Day 1 they had collaborated with a pharmacist and physiotherapist for their input, the patient probably would have gone home a lot sooner. Scholars of the programme have reported meeting physiotherapists and pharmacists in clinical posts since their training and are continuing their interdisciplinary collaboration in the workplace.
“ ey got to see the dynamics of the whole team in action,” explains Dr Morris. “And from the systematic review we published, we saw that nurses sometimes struggle to cross a traditional professional boundary and speak up either because it feels intimidating or unsafe. So we designed scenarios around courageous conversations to promote traditional boundary crossing to share discipline speci c expertise within the team. e development of advanced nurse practitioner roles also helps with the challenging of traditional boundaries.”
Simulated nights on call were part of the award-winning masters programme, with senior nurses from Dublin hospitals working unscripted as they would on an actual night shi .
“ is was really powerful learning,” says Dr Morris. “ e doctors reported the sense of being alone and isolated was petrifying. It was just them, the patient and the nurse, and they said that without the nurse, they wouldn’t have known what to do. ey just were lost. e exercise promoted nurses to be their authentic selves, step into their power and cross traditional boundaries for the better good, share their expert discipline knowledge to support their doctor and suggest when to escalate to senior sta in order to keep their patients safe.”
e masters programme is now paused as Dr Morris and her colleagues evaluate everything they have learned, to prepare to deliver this programme using a hybrid approach, and to explore how it could be integrated into the undergraduate curriculum.
“ e dream for me would be that from the start of health science education we train every discipline together as much as feasible. We instil a mindset of collaborative intentionality and build up this community of interdisciplinary learners. From this training, the professional identity of an inclusive team member can then be fostered to transfer into the clinical workplace. is team approach and mutual respect for one another then contributes to the best care of the patient.” ■
Limited yet encouraging evidence in the literature points to the positive effects of interdisciplinary surgical ward rounds on behaviour change, organisational practice and patient bene ts. The evidence from medical rounds suggests that this form of clinical practice can improve collaborative attitudes, perceptions, knowledge, and skills. Many healthcare disciplines support the bene ts of interdisciplinary surgical ward rounds to improve communication, collaboration and patient safety, however logistical and nancial barriers restrict planning and implementation.
Future research should focus on key aims as follows:
• to establish an evidence-based clinical and educational model for designing and implementing interdisciplinary surgical ward rounds to support clinicians and ensure patient safety; and
• to prioritise addressing the barriers in surgical rounds through implementation of deliberate interdisciplinary collaborative training to ensure the mandated clinical competencies and capabilities are achieved.
• Longstanding structures, with doctors teaching doctors and nurses teaching nurses, hamper learning across professional boundaries.
• Boundary-crossing between CoHP (Community of Healthcare Practitioners) represents particularly fertile ground for learning through occasional forays either across borders or through membership of two or more communities.
• Collaborative intentionality requires deliberate connectedness and thoughtful collaboration through adaptation, exibility and tolerance from all team members.
• We advocate for early introduction of a boundary-crossing approach in health professional education (HPE) to promote collaborative intentionality and deliberate team engagement.
• Cross-Professional Educators (CPEs), such as nurses teaching in medical schools, are uniquely positioned to challenge uni-professional siloed approaches to HPE and atten hierarchies.
M Morris, C Mulhall, PJ Murphy and WJ Eppich, ‘Interdisciplinary collaborative working on surgical ward rounds: reality or rhetoric?
A systematic review’, Journal of Interprofessional Care, 2022. DOI: 10.1080/13561820.2022.2115023.
To link to this article: https://doi.org/10.1080/13561820.2022.2115023
“The dream for me would be that from the start of health science education we train every discipline together as much as feasible. We instil a mindset of collaborative intentionality and build up this community of interdisciplinary learners.”

THE COUNTRY’S FIRST FEMALE SURGEON, MS HOURIYA KAZIM FOUNDED THE UAE’S WELL WOMAN CLINIC, A ONE STEP HEALTHCARE SERVICE FOR WOMEN
Ms Houriya Kazim, BSc, MPH, MB BCh, LRCP&SI, BAO, FRCSI, FRCS(Eng) RCSI Fellow (1993) and Alumna (Class of 1988) is a Consultant Breast Surgeon, Medical Director of the Well Woman Clinic, Adjunct Clinical Assistant Professor MBRU and Founder and President of Brest Friends.
orn in Dubai in 1959, Ms Houriya Kazim (Dr Kazim in the UAE) grew up in London, where her late father, Dr Ahmad Kazim, did his surgical training, and in the Caribbean, where he worked as an orthopaedic surgeon. She attended boarding school in Canada.
“I have only realised as an adult how lucky I was to have the parents I had,” she says via Zoom from her home in Dubai. “ ey had a traditional arranged marriage but my mother Sultana trained as a radiographer and later had her own fashion business, now she is an artist. I grew up with both parents working and did not see that as anything odd. ey were both very much into education, it didn’t matter if you were a boy or a girl. I remember telling my grandmother once that I was going to be a nun because I didn’t want to get married and have kids and she freaked out. ose things never bothered my parents, but if I got up one day and said, ‘I didn’t feel like going to school’, it was as if the world had stopped revolving on its axis. Other women in this country didn’t have the same kind of parents.”
Ms Kazim’s grandfather was a hakeem or faith healer, and her father’s siblings, and now their children and grandchildren, are all involved in medicine.
“ ere are now more than 70 doctors in the family,” she says. “And it was expected of me to study medicine. I don’t remember my parents ever saying, ‘You have to be a doctor’, but I also don’t remember them saying, ‘You have options’!”
A er boarding school, Ms Kazim completed a bachelor’s degree in Canada and a master’s in public health in Texas before enrolling in RCSI in 1982.
“My dentist and GP in Dubai were Irish,” she recalls, “and between them they decided that I was going to RCSI. ey turned out to be the best years of my life. I’m not sure how I ended up thinking about surgery, because there were no female surgeons that I knew, but I knew I liked cutting and sewing - I de nitely didn’t
consider the work life balance questions that young doctors do now! I remember mentioning I was considering a career in surgery to one of the scary surgeons on a ward round in Dublin. He said, ‘You’re very aggressive’. When I was re ecting on it a erwards, I thought, if I was a guy, he’d have used the word ambitious.”
A er graduating, Ms Kazim returned to the UAE to commence her internship.
“On my surgical rotation, I saw really advanced cases of breast cancer. I’d seen breast cancer in Ireland, but never anything like this. I remember pulling out my father’s general surgery textbooks from the 1940s and seeing the same things I was seeing in the 1980s. Arab women are modest, and we had no female
surgeons. ey didn’t want to show their breasts to a male surgeon. And because women were presenting late, they would end up succumbing to breast cancer. So in everybody’s mind, breast cancer equalled death. And here we are superstitious, we don’t even use the word ‘cancer’. We say ‘that disease’, or we mouth it without actually vocalising it, because if you say it, you’ll get it. I saw what happens to a tumour when you don’t do anything about it. It just keeps growing until it grows out of your body. And so this thing is right under your nose, you can smell it, you can see it, you can feel it. Obviously their deaths made me think, ‘ is is what I want to do’. But this was the late 1980s and there was no such thing as a breast surgeon.”
Ms Kazim moved to the UK to study for her Fellowship exams and obtained her Fellowship in General Surgery. She then sub-specialised in surgical oncology and, in particular, breast surgery and reconstruction at the Royal Marsden Hospital in London and the MD Anderson Cancer Centre in Houston, Texas.
“For me, the appeal of breast surgery is that as well as the actual surgery, a lot of the work is general practice because you get to know the patients and their families and you see them again and again. And if you’re like me, and you’ve been working long enough, you start taking care of their children too. ere’s a lot of psychiatry because, of course, everybody who comes to see you thinks they have cancer. And then there’s plastics as well, because we do breast reconstruction, so you are using a lot of your creative genes.”
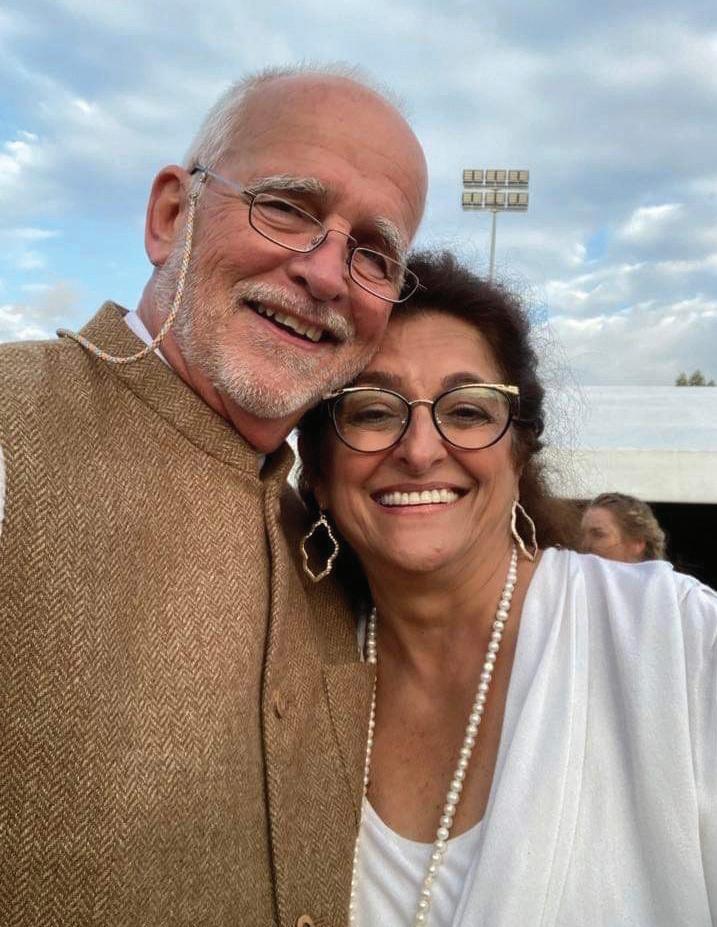
Ms Kazim returned to the UAE in 1998 to be appointed the country’s rst female surgeon, soon a er having married her ancé of nine years, American war journalist, Ron Bagnulo.

“I came back as a 39-year-old newlywed wanting to start a family,” she recalls. “And I wanted to nd part-time work, which was di cult. And nobody knew what a breast surgeon was, because it was not and is still not actually recognised as a standalone speciality. So I was making it up as I went along. It was interesting trying to get a licence.”
A er working at a hospital two hours away from her home for a few years, Ms Kazim established the UAE’s rst Well Woman Clinic. Her motivation was a desire to nd a way through the long waiting times women had to endure waiting for mammograms and biopsies.


“I didn’t want it to be scary,” she explains, “so it looks like a living room. It’s sta ed solely by women, we have radiology in the building and the lab is across the street. So I can have a diagnosis within 24 hours.”
In addition, Ms Kazim and her colleagues started an outreach programme to raise the national consciousness of breast cancer and to encourage women to be more proactive about their health, travelling to ladies clubs’, schools and colleges to give talks about breast cancer and teach women how to examine themselves.
She also started a charity to raise money to help people without medical insurance pay for their cancer treatment, and a support group for breast cancer patients. is evolved into the rst cancer drop-in centre in the Middle East, Majlis Al Amal – Lounge of Hope.
Ms Kazim has operating privileges at three hospitals in the UAE, and now her colleagues include other female surgeons, both local and foreign. ere are trained breast surgeons in all the major hospitals.
“Breast surgery is an emotive subject,” she says. “It’s not a hernia, it’s not a lump or bump. I nd it very hard to take time o or to go on holiday. ere are so many emotions involved. And even though I have another breast surgeon in the clinic who covers for me when I’m away and vice versa, I still work every single day even when I am away.”
As well as her clinical work, Ms Kazim is an adjunct professor at Mohammed Bin Rashid University of Medicine and Health Sciences (MBRU) and enjoys mentoring young female medical students, encouraging them to see surgery as a viable career option.
“Sadly things have again become di cult for women here in the UAE. In my time there were no universities here, so pretty much everybody went

She also started a charity to raise money to help people without medical insurance pay for their cancer treatment, and a support group for breast cancer patients.Ms Houriya Kazim Ms Houriya Kazim giving a lecture. Ms Houriya Kazim (the UAE’s first female surgeon) with her father, Mr Ahmad Kazim (the UAE’s first male surgeon).
away to school. Now, because we have universities and branches of major universities here, parents, the same parents who themselves went away to university, will choose to keep their children, especially their daughters, home. I think it’s important for a career in surgery to travel. I had that opportunity when I worked in the Caribbean before returning to the UAE and it was a great experience. Now the girls are kept home and there is a lot of pressure still to get married and have kids. I don’t think I could have combined my training with having small children, I am glad I waited until I was nished.”
Currently, Ms Kazim is engaged in research on the pattern of breast cancer in the UAE, Middle East, and North Africa region, where the median age for breast cancer diagnosis is 45, compared to 62 in Ireland, the UK, Western Europe and North America.

“I get women in their 20s and 30s with breast cancer,” she says. “ ey may have young families and be working hard at their careers. We have been auditing our patients along the way and now we are putting together a large study looking at genomic pro ling, to see if there is something genetic going on.”
Dubai is a notoriously expensive place to live; Ms Kazim lives in a small bungalow on the beach where she tries to get in a 5km walk each day.

“I work seven days a week, but two of those are from home. I do three days in the clinic, have one day for surgery, and then one day is for over ow, either clinic or surgery. My commute is an 18 minute drive if I’m early enough; the tra c is a big deal here.”

Ms Kazim knits and crochets to de-stress – a habit that got her through some tough modules in RCSI. “I found it just took my mind o things, especially if I had to do some kind of intricate pattern. I still have big u y mohair jumpers that I made in Ireland; my daughters pull them out sometimes.”
In her Dublin days Ms Kazim was voted queen of the cocktail party circuit but now prefers a quieter life.
“I socialised too much when I was young and now prefer to stay home with a cup of tea and a good book. My daughters, Tara and Gina, are at university in New York and Dublin, studying science and politics, respectively, and I visit as o en as I can. I love what I do. When I go on holiday, people ask, ‘Do you miss being in surgery?’ I say I don’t miss the actual cutting, but I do miss the people. I miss their stories.” ■

“Now, because we have universities and branches of major universities here, parents, the same parents who themselves went away to university, will choose to keep their children, especially their daughters, home. I think it’s important for a career in surgery to travel.”Ms Houriya Kazim and her husband, Ron Bagnulo.
PROFESSOR DHANANJAYA SHARMA (FRCSI 2013) HAS BEEN, FOR ALMOST 50 YEARS, A PIONEERING AND INSPIRATIONAL TEACHER AND CHAMPION OF LOW-COST SURGICAL SOLUTIONS FOR THE DEVELOPING WORLD. HIS ENTHUSIASM AND EXPERTISE HAS BEEN INTERNATIONALLY RECOGNISED, BUT HE SHOWS NO SIGNS OF STOPPING ...

Studying came easy to me. I came rst in the state in the higher secondary examination and did not struggle with exams in medical school. I did my internship in a small district hospital called Chhindwada – the workload was intense and there was very little in the way of modern equipment. en I returned to the medical school where I’ve been teaching for the last 40 years for my postgraduate quali cation in surgery. A er three years of my masters degree in surgery, I went to work in a Christian mission hospital. at gave me a new perspective. e patients were very poor, and I felt that my purpose as a doctor should be to do whatever I could for them and people like them.
I came back to my alma mater in 1986 as a young, idealistic lecturer and assistant professor. And I’ve been here ever since. My rst four years were all about mastering the technique and the skills. I wanted my technique to be perfect, because technique is freedom and enables you to focus on what you are doing, to nd the simplest and most e ective way of doing things.
Professor Dhananjaya Sharma, MBBS, MS, PhD (Doctor of Philosophy), DSc (Doctor of Science), is Head of the Department of Surgery at Government Medical College and Allied Hospitals, which are a liated to MP Medical Sciences University, Jabalpur, the largest teaching hospital in Central India. His work in innovating low-cost appropriate technology for healthcare in the developing world has been recognised with Ad Eundem Fellowships of all four Royal College of Surgeons of UK and Ireland, Honorary Fellowships of Royal College of Surgeons of ailand and Académie Nationale de Chirurgie France and visiting professorships/invited faculty at iconic Karolinska Hospital Stockholm and Oxford University.
come from a family of doctors. My grandfather was dean of one of the oldest medical schools in India, and as a child I used to accompany my father, the doctor-in-charge of the Government’s Rural Public Health Programmes, on his o cial tours. My interest in public health stems from this time; I remember my mother saying to me that it was not possible to be a good doctor without rst being a good person.
In 1988, I spent a couple of months as a visiting fellow at Vienna University where I was exposed to all the modern techniques of endoscopic surgery. When I came back I attended my rst international meeting in Delhi in 1990, and listened to people from all over the world talking about their work. I was frustrated. I didn’t have the equipment or the instruments about which they spoke. How could I do research? One evening, I found Professor Michael Hobsley of University College London Medical School sitting by himself on a lawn chair. I summoned up the courage to approach him and introduced myself. I asked for his advice. ‘Everyone talks about such futuristic instruments and techniques,’ I said, ‘how can I do research with my limited resources?’ And he told me I could do everything with the basics I had. I spoke with him for just a few minutes but those few minutes changed my life.
We remained in touch and he encouraged me to register for my PhD. I went on to get my PhD and DSc, all the time focusing on research which was clinically relevant for my poor patients. Simultaneously, I became interested in translating my knowledge into frugal surgical solutions. Gradually, I started getting published, and I had the opportunity to be a visiting fellow at Kurume University Japan and at Sloan Kettering Memorial Kettering Cancer Center New York, USA.
I could see that I was going to become a professor and head of the department in the future and I wanted to be ready. One of my favourite quotations is by Benjamin Franklin: ‘By failing to prepare, you are preparing to fail’. So I was ready when I was appointed.
e rst thing I did was to introduce a model of inclusive leadership. I told everyone that I would measure my own success by the number of successors I created. So everybody would have a say. When we were making a big decision, everyone sat together. And once we made that decision, everyone would stick
to it. So everyone was in it together. is means that when I’m away, I know my department is going to be run the way we have decided collectively.
I also made sure that I kept my ego in check, and I made this a rule for my students and doctors too. e hospital is for the patients, the college is for the students. Surgeons are egotistical and arrogant and I didn’t want that in my department. I was fortunate to become friends with and be mentored by Professor Daniel Jaeck, Professor Emeritus at Strasbourg University, former President of the European Surgical Association, and he taught me to keep my ambition in check, to practise humility and to learn the di erence between pride and arrogance.
As a young man I fell into the trap of becoming arrogant. But as I grew older and wiser, I realised that I came from a privileged background: my father was a doctor, my grandfather was a doctor, I was very good at studying, everything was on a silver platter for me. I realised that things were not as easy for people coming from very modest backgrounds. So I changed my arrogance to pride. If I think I’m good, that is pride. But if I think that only I am good, that is arrogance. As a teacher, it became my mission to help those students coming from very modest backgrounds. ey’re my favourites. I make sure I give a lot of my time to them to guide them along.

e next thing I learned was the di erence between knowledge and wisdom. It’s very easy to confuse the two. You can get knowledge from Google, but you cannot get wisdom from Google. How you apply the knowledge is wisdom, and knowledge is of no use unless it is used for the bene t of mankind.
In Hindi, we have a beautiful couplet, which translates as ‘ e peacock dances in the forest, but nobody sees it’. I decided that I had to publish extensively to let people know what I was doing. I wasn’t going to be like a beautiful peacock dancing in a forest, with nobody noticing.
We have now published over a hundred papers on low-cost surgical solutions, which can be practised on a large scale, even in a district hospital. All solutions which I have published require zero funding and just use local resources. You don’t really need a lot of money. You just need enough to survive. All solutions are shared on the Center for Global Surgical Innovations and low-cost solutions website www.surgicalinnovations.in.

Jonas Salk was the person who invented the rst successful polio vaccine and gave away its rights for $1. What he said about teaching was: ‘Be good ancestors’. My biological DNA goes to my family, but my trainees carry my surgical DNA. So I have to be a good ancestor. My mentees come to me with many limitations, and it is for me to help with their imperfections and improve
them, to give them con dence. I love teaching. Many of my students have gone on to become professors all over the world, but many return a er training and rejoin the department. e Government asked me to take on the roles of Dean and Vice Chancellor but I declined, because I want to be a teacher not an administrator. I didn’t want to be a boss; I wanted to be a leader.
As an academic leader, it is my duty to nd these low-cost surgical solutions. How do I go about it? I need global wisdom, learning from everyone, but using local resources. I combine the two, and call it ‘Glocal solutions’. My mentor in Strasbourg, Professor Jean-Marie Lehn, Nobel Laureate in Chemistry 1987, talks about creating science. ‘ ink outside the box,’ he says. ‘Don’t just read and follow science, create your own science.’ I made it a rule in the department: If you have a problem, you don’t have some machine or instrument, don’t complain, don’t come and cry on my shoulder. Come with a solution. I train my students that every di culty is an opportunity.
You can do research on what is interesting or what is important. When I was young, I wanted to do a heart transplant in the morning, go back home, have a nice lunch, come back and nd a vaccine for cancer. at was my dream. So that would have been interesting. But I had to deal with diseases of poverty, perforations and obstructions, with no ventilators, and no intensive care unit. So I had to do research on what is important for me and my patients. I couldn’t keep on dreaming, thinking, ‘One day, I’ll have that …’ and waste my life getting frustrated. So, we made a rule. Modify, simplify, and apply. Don’t wait for expensive things that may never come. Whatever is available, you modify it, you simplify it, and you apply it. And we started getting successful results. at is what I teach and preach and practise. e simplest solution is the best, so try to nd it. And more o en than not, it is the most economical one.
e next rule was: Don’t waste your time. Don’t discuss people, don’t discuss events, discuss ideas instead. I ask my trainees, ‘What do you talk about when you are having a cup of tea or co ee? Movie stars? Sports stars?

“We have now published over a hundred papers on low-cost surgical solutions, which can be practised on a large scale, even in a district hospital.”Professor Sharma with his grandparents in 1960. Professor Sharma, captain of the tennis team at Jabalpur University,1980. Professor Sharma with his mentor Professor Daniel Jaeck.
Why? You are scientists. Your job is to think science and discuss ideas.’ As Marie Curie said, ‘Be less curious about people and be more curious about ideas’. I tell my trainees to keep an open mind and, as Linus Pauling, [Nobel Laureate Chemistry, 1954, and Nobel Laureate Peace, 1962] said, ‘If you want to have good ideas, have plenty of them. Recognise which are the good ones, and throw the bad ones away.’ I tell my trainees that if they want mentors and sponsors they have to stand out in the crowd. How do they do that? By being prepared and doing their best every single day.
I love teaching. Teaching is synonymous with learning. e only thing which increases when you distribute is your knowledge. I feel very privileged to have had the opportunity to teach all over the world and to be recognised with so many awards and fellowships. Simultaneously, I have had the privilege of teaching in developing countries such as ailand, Bangladesh, Maldives, Bhutan, Pakistan, Mexico, Afghanistan, Myanmar and Nepal.


Our department is a General Surgery department. We have many specialties, – paediatric surgery, gastrointestinal surgery, kidney surgery, plastic surgery, and breast surgery, but we work together. ere are no silos, so there is a lot of cross-fertilisation of ideas. Ninety per cent of the surgeons have been trained by me. It’s like a family. So we sit together, and there’s a very healthy rivalry. If someone publishes two papers in a week, he has the bragging rights. at is our innovation ecosystem. Young fertile minds are the best for nding solutions. My job is to protect them from all those things which can go wrong in a government hospital – if their salary is late or they have problems at the bank. I am the father gure, I keep them protected and provide a healthy ecosystem so they can do their best. Of course we have had our share of failures, but we learn from them, and we move on.


I still put in 18 hours every day. I will retire from my o cial position next year, but I will continue to teach and write and travel. I don’t want to sit at home. Zoom has made it so easy – I can teach anywhere. I am ready to take

up more challenging work, and will continue to work on developing frugal surgical solutions and teaching people from very modest backgrounds. Unless I bring value to my patients and my students, I’m not doing my job. I have to do more for people who are less privileged than me because leadership is about serving, not ruling.
I have been married to my childhood sweetheart, Neeta, for almost 40 years now, a er a long courtship. She is a clinical psychologist and a counsellor and is now retired. Every day I tell her that she is the most beautiful girl I have ever seen. Yes, I am a diehard romantic. My son and his family live in Seattle, so that is where we spend all our holidays. My grandson is my hearthrob. Doting grandfather is an understatement. I’m absolutely crazy about him. In Hindi, the word for grandfather is Baba, and when he says ‘Baba’ my heart skips a beat.
ere was never anything else for me but being a doctor. I’d do the same thing all over again. When I was young, I refused a couple of lucrative o ers to work in the Middle East and in Europe. I was very clear in my mind that I have to look a er my patients here. It is my responsibility to do good for those who are less privileged than me. I had to provide leadership by serving my people and my students. And that I have done. I hope the people who take over from me will continue the same work. ■
“Unless I bring value to my patients and my students, I’m not doing my job. I have to do more for people who are less privileged than me because leadership is about serving, not ruling.”Professor Sharma with his family. Professor Sharma with Princess Sirindhorn of Thailand. Professor Sharma receiving an honorary degree from the Queen of Thailand. ‘Baba’ with his grandson . Professor Sharma and RCSEng President, Professor Clare Marx.










All Liz O’Riordan ever wanted was to help people – from the age of seven, she knew she was going to be a doctor. Surgical training was hard. e highs were life-changing, but the lows were worse. Surgery was a man’s world. Sexual harassment and bullying were commonplace. By the time she reached her 30s, she was ready to quit. e mild depression she’d had at medical school got worse and worse. Two things helped – antidepressants and alcohol.
Twenty years a er starting medical school, she became a consultant breast surgeon. She loved her job, but wasn’t prepared for the reality of telling ten women a day they had cancer. Her depression spiralled out of control with suicidal thoughts.
Six months later she was diagnosed with breast cancer herself. A er brosis and scarring caused a permanent reduction in shoulder movement, power and function, she was unable to operate and was forced to retire from surgery.
Liz began a new career, as a speaker and writer. She has authored two books, e Complete Guide to Breast Cancer, with Professor Trisha Greenhalgh, and Under e Knife, Life Lessons From e Operating eatre.

To be a successful surgeon you must have the eyes of a hawk, the heart of a lion and the hands of a lady.
Doctor in the House, 1954
s a trainee surgeon, it’s all about the hernia. e inguinal hernia, to be precise. e operation starts when I shave a man’s groin with a scalpel, and it always feels like a little bit of history. e original surgeons were barbers, and the red and white pole outside today’s high-street barbers represents the bloody bandages used a er the operation. I too am a barber surgeon. A er carefully removing any pubic hair, I become an artist. I paint his groin with a sponge soaked in Hibiscrub, a brown antiseptic solution, to sterilise his skin. I let it dry and then do it again before isolating the area with green cotton drapes.
But how did that man end up on my operating table? He came to see me with a lump in his groin. An inguinal hernia. ey were the bane of my life as a medical student. e anatomy is complex and there are many terms that had to be memorised parrot-fashion for oral exams. A hernia happens when something inside the body, like fat or a loop of small bowel, pushes through a weakness in the muscle or surrounding tissue.
ere’s a natural weakness in the groin called the inguinal canal. It’s a series of openings in the lower abdominal wall that the testicles travel down to reach the scrotum while a baby boy is still inside the womb. Trying to get my head around this three-dimensional canal from the at pages of a book was hard. I just couldn’t picture how everything tted together. Instead, I practised getting men to cough while I fumbled around in their groin trying to nd a lump.
But there’s an art to groin-fumbling. Although most hernias travel down the canal, called indirect hernias, sometimes the fat can push through a weakness in the back of the canal, causing a direct hernia. If I put my nger exactly halfway between their hip bone and the edge of their pubic bone and get a man to cough, I can tell which type of hernia they have. Either my nger controls the bulge, or the hernia pops out.
One of my bosses was a hernia expert. He would make me write down in the notes what kind of hernia I thought each man had. And then we would take him to theatre and see if I was right. To make things easier for the patient, I was taught to x them using local anaesthetic. e patient was awake but didn’t feel pain, only pressure. ey could walk out of theatre and go home shortly a erwards instead of the longer recovery needed a er a general anaesthetic. As great as it is for the patient, it is technically challenging for the surgeon. e rst time I in ltrated the canal with anaesthetic, the tissues bulged with the uid and the anatomy was distorted. And because the patient was awake, I had to watch what I said. No more asking the scrub nurse for a knife or a needle. We developed our own sign language instead.
In a few months I had done over 50 of them and was le to crack on by myself. Back to the man on my table. A er hanging a drape like a curtain in front of him to hide my handiwork, I pick up the blade and start to cut, gently dissecting through each individual layer, in ltrating with anaesthetic as I go.
Two of the other consultants wander into theatre to see what I’m up to. If it was any other operation, sweat would start to drip down the back of my legs at

the pressure of being watched, but this is a hernia repair. ey are teasing me, trying to put me o my game, but this is my eld. ey can’t rile me. Not here. Not in my place.
I open up the inguinal canal and everyone peers into the wound.
‘Yes!’ I whisper to myself. I was right. It’s a direct hernia. I smile under my mask as I carry on gently teasing out the hernia, pushing it back inside the abdomen where it belonged. e consultants leave to nd other trainees to tease.
e nurse hands me a sterile mesh that I carefully cut to size, taking care to round the edges of the rectangle so there are no spiky corners, cutting a curve to match the patient’s body, happy in my work. Like dressmaking, I tailor it to t his groin. A er a quick check on the patient to make sure he’s OK, I suture in the mesh with a Prolene thread. It’s bright blue and has a memory. It wants to curl up like it did in the suture packet, so I run it through my hand a few times to straighten it out. To coax it to behave. And then I tack the mesh to the underlying tissue with a simple running stitch, to keep it in place, before burying the knot.
I ask the man to cough to test my repair job. Not even a glimmer of a bulge. God, I’m good.
And then, my favourite bit. Closing up the wound. I carefully sew the layers of the canal back together. I start at either end, moving my way towards the middle so they are perfectly aligned.
I nish with the skin, pushing the needle just under the surface with a clear suture, taking little bites that can’t be seen. e skin comes together with the smallest of humps in the middle which I know will heal as a beautiful, at scar. My cra smanship will soon be hidden by his pubic hair, but that’s not the point. I remove the drapes. e scrub nurse hands me a large wet swab to clean the skin before applying a surgical dressing. It must be parallel to the wound. Nothing else is acceptable. I lower my mask, approach the end of the bed, and tell him it’s all over. He gives me a grin and says, ‘ ank you, nurse.’ ■ Liz O’Riordan’s book, Under e Knife, Life Lessons from the Operating eatre will be published in July. It is available to pre-order at www.liz.oriordan.co.uk.
The original surgeons were barbers, and the red and white pole outside today’s high-street barbers represents the bloody bandages used after the operation.
When and where are you happiest? In a stadium, front of the pit at the foot of the stage of a classic rock concert. Just for the sheer tribal experience which cannot be equalled anywhere else in a stadium. Or 25m under the ocean, scuba diving in splendid isolation. So much beauty and danger juxtaposed. Makes you realise we’re all just visitors. What is your ideal evening? Concert at the Royal Albert Hall in London with friends or family, followed by tapas at Casa Brindisa in South Kensington. I should have frequent yer points! If you could research and write a book on any subject, what would it be?
Morgan McMonagle, MB, BCh, BAO (Hons), MD, FRCSI, FRCPSGlas

FACS is a consultant vascular and trauma surgeon at University Hospital Waterford; Director, Trauma MSc, Imperial College, London; Director, Trauma Training RCSEng; Mass Casualty Planning Training Team, World Health Organization. A er graduating from UCD in 1997, Mr McMonagle undertook basic surgical training at RCSI Hospital Group and gained further trauma surgery experience at Westmead Hospital, Sydney, Australia. Following this he gained extensive experience working in prehospital care and aeromedical retrieval with Care ight and Care ight International, Australia and with MAGPAS air ambulance in the UK. He completed higher surgical training with the West Midlands surgical training programme, UK followed by
a Fellowship at the Royal Brisbane & Women’s Hospital, Brisbane, Australia and additional fellowship training in trauma, emergency surgery and surgical critical care at Penn-Trauma at the Hospital of the University of Pennsylvania and was awarded Fellowship of the American College of Surgeons (FACS). e rst trauma surgeon appointed at Imperial Healthcare as part of the new London Trauma Network, he was also a member of the steering group advising on A Trauma System for Ireland: Report of the Trauma Steering Group for the Department of Health, Ireland. A clinical lecturer in surgery at RCSI and an honorary lecturer in surgery at Imperial College, London, he is an Intercollegiate Examiner in vascular surgery, a published author and the national clinical lead for mass casualty planning for the HSE.
Route 66 and how it has weaved itself into modern American culture and music. What relaxes you most? Playing guitar, either acoustic or electric. I used to play in a group but haven’t been able to dedicate myself to that in a very long time. So now, it’s playing alone. Need to limit the decibels though! What is your greatest fear? at we, the human race, the most intelligent and progressive of our (or any) species that ever existed, as the current occupiers of this tiny speck of a rock called earth, suspended in the vast cosmic arena in a beam of sunlight, are slowly and deliberately destroying it. ere will be no planet to leave to our children. We are the worst tenants on a beautiful planet that we call home. Homo Sapiens will not be the rst species in history to become extinct, but we will be the rst species
wholly responsible for our own extinction. Knowledge and wisdom are clearly not synonymous. When did you decide you wanted to become a surgeon? Probably about age 15. One of my very good friends had a kidney transplant. I went to visit him in Beaumont Hospital and met the team looking a er him who were incredibly nice I recall. Would you have any advice for your younger self? Ignore the begrudgers and the nay-sayers. Be yourself. Follow your own path. at’s about as polite as I can make it! How do you have fun? So many ways, as long as I’m moving forward! Working hard in the gym or pool. Going scuba diving (esp. South West Donegal), skiing in the winter. Going to any live music, then trying (with di culty) to re-play the guitar parts. Travel, restaurants, wine (amateur oenophile). Where would you be if you decided not to become a surgeon? Probably a helicopter pilot. Preferably o -shore ying. I’ve met a lot of pilots over the years from my days doing pre-hospital care in Australia and the UK and I’ve NEVER met an unhappy one. ey have the best o ce in the world and just love to y! In what way do surgeons struggle/ what issues do surgeons today face? I think the health service is becoming very consumer and target driven, which naturally leads to micromanagement at every level. e ‘purpose’ (ie: the reason why we all get out of
MORGAN MCMONAGLE MADE HEADLINES RECENTLY WHEN HE AND OTHER INTERNATIONAL EXPERTS TRAVELLED TO CITIES IN UKRAINE TO TRAIN HEALTHCARE WORKERS DEALING WITH THE FALLOUT OF WARMr Morgan McMonagle
bed in the mornings to come and do the best job that we can) is easily distorted and lost in such an atmosphere. ere is a certain existential deafness regarding this, which is less about hard work or long hours. It’s about the loss of self-pride in the pursuit of a productive day. As a result, people vote with their feet and leave. What has been your proudest moment? Professionally travelling deep into Ukraine on the day the Crimea Bridge was destroyed. Despite the massive bombing campaign that followed, the resolve of the Ukrainian doctors and nurses was humbling to experience and the spirit amongst our team was inspiring! Having said that, I was happy to cross back into Poland two weeks later (very sleep deprived). Who have you learned the most from in your life? Personally, my kids, who are the best teachers of humility. Professionally, probably Bill Schwab at PennTrauma on leadership and David Nott on making the absolute most of your professional life! How does a surgeon in 2023 cope with pressure? Live every day with intent. Intention equates with purpose. at includes professional and personal. Once the purpose goes, your inner vibe quickly follows. at’s covert self-sabotage. Always look to better yourself in every way, which is a form of reconditioning for the soul. Look positively towards change and be progressive. is keeps the spirit free from dry-rot. What is the best thing about the system of training young doctors in Ireland? It’s a small country, but punches way above its weight when it comes to surgical expertise internationally. ere is still a deep commitment to surgical training in Ireland, which includes embracing international travel and fellowships. is makes up for the smaller population. As a result, there is a very high concentration of skill
and expertise on the island to learn from. is makes the ‘trainingdensity’ very rich indeed. What is your greatest extravagance?


Probably my 1959 Gibson Les Paul guitar. A soulful blend of handcra ed mahogany and Indian rosewood with a maple top. Beautiful tone unmatched by any other guitar. A small re-mortgage, but worth it! Do you have a mantra to live by? “Don’t say you don’t have enough time. You have exactly the same number of hours per day that were given to Helen Keller, Pasteur, Michaelangelo, Mother Teresa, Leonardo da Vinci, omas Je erson, and Albert Einstein”. - H. Jackson Brown Jr. What do you consider your greatest achievement? Personally, seeing my kids grow up with unique personalities and talents. Although it sounds trite, it is also a very grounding achievement. Professionally, getting nominated (twice) in the BMA Annual Book Awards. In your profession, a historical figure you admire?
Although not a surgeon, I admire what Henri Dunant (1828-1910) did to bring about the existence of the International Red Cross. A Swiss banker who happened to witness the devastation on the battle eld at Solferino in 1859 in the battle between the French – Italian allies and Austria. Not only did he use his in uence and leadership to convince the victorious to take care of all injured, regardless of their allegiances (tutti fratelli), but he also sparked numerous European leaders into action towards the concept of international humanitarianism. As a result, 16 nations signed the rst treaty to establish the International Red Cross. He established the concept of neutrality for healthcare workers in war (currently not respected in many con icts). He also used his banking credentials to raise funding necessary for such work. He was probably the rst logistician in

humanitarian healthcare. Anyone who has been on such a mission will know that the most useful and important people are in the logistics department! What is your favourite memory? Holidaying in South West Donegal as a child with my parents, then later going back to scuba dive at the foot of Glencolmcille with friends, then again later re-visiting with my kids. Have you a hobby and if not, why not? If you do have a hobby, what do you enjoy about it? I do quite a lot in my (limited) spare time. I used to do competitive judo and was All-Ireland and University National Champion when in College. Nowadays, I swim (typically 2-3km every 2nd day) and use the gym, scuba dive in the summer and ski in the winter. I also own 16 guitars, a drum kit and a piano. Can’t play them all, at least at the same time though. Name your favourite writer. I typically only read non- ction. Favourite is probably AA Gill. Smart and intellectually funny. But there are many others I love to read like Joe Klein, Atul Gwande and Carl Sagan. e one book I’d love to get my hands on is Fly Fishing by J R Hartley. If you could invite any historical figure to dinner, who would it be? Jesus. I’d like to ask him about his life between the ages of 12 and 30 years old, as there’s no historical record! I might even get a book out of it. Which talent would you most like to have? A great singing voice. at way you bring your instrument everywhere. What is the wisest thing you have ever said?
ere’s no such thing as an atheist
at the end of a winch! is occurred a er winching an injured patient out of the Blue Mountains near Sydney, Australia from 200M into a helicopter. It works on so many levels when things take an ‘unexpected’ turn during surgery. Every surgeon has had that sinking feeling, where you pray quietly, act professionally and hope for the best! Name one virtue all surgeons ought to have. Progression and change. Name one vice no surgeon should have. Self-righteousness. Good luck excising that one! ■
“Look positively towards change and be progressive. This keeps the spirit free from dry-rot.”Scuba diving. Favourite writer AA Gill. Red Cross founder, Henri Dunant.




We congratulate over 130 Fellows and Members who received FRCSI, MRCSI, and DO-HNS awards in December 2022 at RCSI Dublin. We look forward to welcoming them to our RCSI Membership community and surgical professional network and to supporting all of them throughout their careers.





Events during Charter Meeting 2023 began on 31 January and included meetings, presentations, parallel sessions, symposiums and lectures, all focused on the theme, ‘Shaping the Future’, and culminated on 3 February with the conferring of Honorary Fellowships and the Charter Dinner.











RCSI SURGICAL BOOTCAMP
19 June - 7 July 2023
RCSI Dublin and Virtual. Free, limited to CST Trainees.
‘DOING THE ROUNDS’ ROADSHOW - TULLAMORE
22 June 2023
RCSI Dublin. Free, registration now open.
RCSI FELLOWS, MEMBERS AND DIPLOMATES CONFERRING CEREMONY
3 July 2023
RCSI Dublin. Free for eligible candidates.
CONTINUOUS PROFESSIONAL DEVELOPMENT SUPPORT SCHEME ENROLMENT OPENS FOR NCHD’S
10 July 2023
Virtual. Free for eligible candidates.
LAUNCH OF THE CPD ACADEMIC PROGRAMME BROCHURE
August 2023
Virtual. Free.
RCSI ALUMNI GATHERING 2023
17-19 August 2023
RCSI Dublin. Paid event, register online.
SIR PETER FREYER MEMORIAL LECTURE AND SURGICAL SYMPOSIUM
1-2 September 2023
NUI Galway. €40-80.
MRCS PART B (OSCE) PREP COURSE
4-5 September 2023
RCSI Dublin. €640, limited capacity.
MRCS PART A EXAMINATION
12 September 2023
RCSI Dublin.
UEMS EBSQ GENERAL SURGERY EXAMINATION
13-15 September 2023
RCSI Dublin. Cost associated.
NATIONAL HUMAN FACTORS IN PATIENT SAFETY CONFERENCE
29 September 2023
RCSI Dublin. Registration will open soon.
MRCS PART B (OSCE) EXAMINATION
19-20 October 2023
RCSI Dublin.
AMERICAN COLLEGE OF SURGEONS (ACS) CLINICAL CONGRESS 2023
22-26 October 2023
Boston, USA. Cost associated.
CHAPTER OF FELLOWS, FELLOWS AND MEMBERS RECEPTION AT ACS 2023
23 October 2023
Boston, USA. Free, registration not yet open.
RCSI MILLIN MEETING
10 November 2023
RCSI Dublin. Paid event, registration not yet open.
‘DOING THE ROUNDS’ ROADSHOWNORTHERN IRELAND
16 November 2023
Northern Ireland. Free, registration not yet open
RCSI FELLOWS, MEMBERS AND DIPLOMATES CONFERRING CEREMONY
4 December 2023
RCSI Dublin. Free for eligible candidates
RCSI CHARTER WEEK 2024
6-9 February 2024
RCSI Dublin. Paid event, registration not yet open
REGISTRATION AND QUERIES:
RCSI Fellows, Members and Af liate Members in Good Standing receive discounted attendance rates to RCSI events, or free attendance in some instances as a bene t. You will be invited to each event and noti ed when registration is open for each event by email. If you have any queries, please contact fellows@rcsi.ie
and Affiliate Members of RCSI are warmly invited to register for the upcoming events and to save the dates
Approved Conditions & Approved Medical Device EN 14931 (chamber)




Recognized Medical HBOT Treatment Tables and Protocols - 2.4 ATA - 6ATA

- From 115 Minutes to 285 Minutes
100% Medical Oxygen (BOC Supplied) As a Prescribed Medication
On-site Hyperbaric Physicians and Nurses - Pre and Post Treatment Assessments



GDPR Compliant Data Handling and Communication with Referrers

Best Partner in Wound Care and Enhanced Healing



OUR PARTNERS
ACCREDITED WITH







