PROFESSOR DEBORAH MCNAMARA

or 240 years, RCSI has been at the forefront of improving surgical care for patients, safeguarding standards of practice and providing leadership in the field of surgery. It is an honour to serve as President of RCSI and, with your support, I will endeavour to retain our College’s role as the voice of surgery. RCSI has prevailed over the last 240 years due to the commitment and leadership of surgeons across the centuries. Working together, we can ensure its relevance for generations to come.
Our new RCSI Council is already hard at work in areas as diverse as surgical training, best practice in surgical clinical governance, technology and digital medicine, and standards for cosmetic surgery, to name just a few. You can read more about our new Council (page 2). I am very grateful for Council’s work on behalf of RCSI, and their support for me personally.
During my first few months in post, I have worked closely with the team in our Fellows and Members Office to explore how we can better support surgeons at every career stage. We have launched the RCSI Fellows and Members Portal, a
new access point for surgeons to interact with RCSI, no matter where they live and work. Over the next year, you can expect greater integration of the RCSI Fellows and Members Portal with the Professional Competence Scheme. You can access the portal at www.rcsi.com/portal and I encourage you to have a look at the short ‘How To’ video if you have not already signed up. Over time, we hope to provide a more individualised experience for each Fellow and Member, tailored to your needs and interests.
The new portal has enabled us to complete our first Fellows and Members census, providing clear insights into where our Fellows and Members are practicing, your areas of specialty and career stage. With 10,944 Fellows and Members working in 103 countries worldwide, this data will assist us in planning for the future and help us to support you better.
As you know, a key focus of my term as President is to support early career surgeons in their first years of independent practice. In July, as President, I had the pleasure of welcoming 48 new Fellows to the RCSI community at our summer conferring. Our
The governing Council of RCSI is composed of 21 surgeons who are Fellows of the College – and two lay members – elected by the College’s Fellows and Members. Council meets regularly throughout the year and meetings are chaired by the President. Council delegates a number of key functions to various boards and committees, which report to Council on a regular basis. At a meeting of the College held on Wednesday, 5 June 2024 the following were elected to office (elected members listed in alphabetical order):









Professor Deborah McNamara
President of RCSI and Consultant General/Colorectal Surgeon at Beaumont Hospital.
Professor Michael Kerin Vice President of RCSI and Consultant General and Breast Surgeon at Galway University Hospital.
Professor Ronan Cahill General/Colorectal Surgeon at the Mater Misericordiae University Hospital and Professor of Surgery at University College Dublin.
Mr John Caird Consultant Paediatric Neurosurgeon at Beaumont Hospital, CHI at Temple Street and CHI at Crumlin.
Professor Camilla Carroll Consultant Otolaryngology Head and Neck Surgeon at the Royal Victoria Eye and Ear Hospital Dublin.
Professor Kevin Conlon Consultant General Surgeon at St Vincent’s University Hospital and Tallaght University Hospital, Professor of Surgery, Trinity College Dublin.
Ms Bridget Egan Consultant Vascular Surgeon at Tallaght University Hospital.

Mr James Geraghty
Consultant General Surgeon at St Vincent’s University Hospital and Senior Lecturer in Surgery at University College Dublin.
Ms Ann Hanly
Consultant General/Colorectal Surgeon at St Vincent’s University Hospital, and Director of National Pelvic Floor Centre, St Vincent’s University, St Michael’s and National Maternity Hospitals.






Professor David Healy
Consultant Cardiothoracic and Transplant Surgeon at St Vincent’s University Hospital and Mater Misericordiae University Hospital.
Mr Sean Johnston Consultant General Surgeon at Midland Regional Hospital Tullamore.
Mr Paddy Kenny Consultant Orthopaedic Surgeon at Connolly Hospital Blanchardstown and Cappagh National Orthopaedic Hospital.
Professor Carmel Malone Consultant General/Breast Surgeon and Clinical Lead at Galway University Hospital.
Mr David Moore Consultant Trauma and Orthopaedic Surgeon, CHI at Crumlin, Tallaght University Hospital and Blackrock Clinic.
Professor Michael O’Riordain Consultant General/Colorectal Surgeon/Chair of Division of Surgery at Mercy University Hospital, Cork.
Mr Barry O’Sullivan Consultant Plastic Surgeon, Beaumont and Connolly Hospitals, and Clinical Director of Surgical Directorate, Beaumont Hospital.

Professor John Quinlan Consultant Trauma and Orthopaedic Surgeon at Tallaght University Hospital.

Professor Paul Ridgway Consultant General Surgeon at Tallaght University Hospital and St Vincent’s University Hospital.

Mr Keith Synnott Trauma and Orthopaedic Surgeon at the Mater Misericordiae University Hospital.


Professor Laura Viani Consultant Otolaryngologist/ Neuro-Otologist at Beaumont Hospital and Director of the National Hearing Implant and Research Centre (NHIRC) at Beaumont Hospital.
Professor Kilian Walsh Consultant Urological Surgeon at University Hospital Galway and Bon Secours Hospital Galway.


Hon. Mr Justice Peter Kelly Former President of the High Court and former chair of the Commercial Law Centre in University College Dublin, Adjunct Professor of Law at Maynooth University.
Roderick Ryan
Chartered accountant, director of a number of companies including Glen Dimplex, formerly Managing Partner of Arthur Andersen.
Bed and theatre cancellations are a frequent reality. For surgeons, the introduction of new infrastructure for scheduled care such as surgical hubs and elective hospitals gives cause for hope.
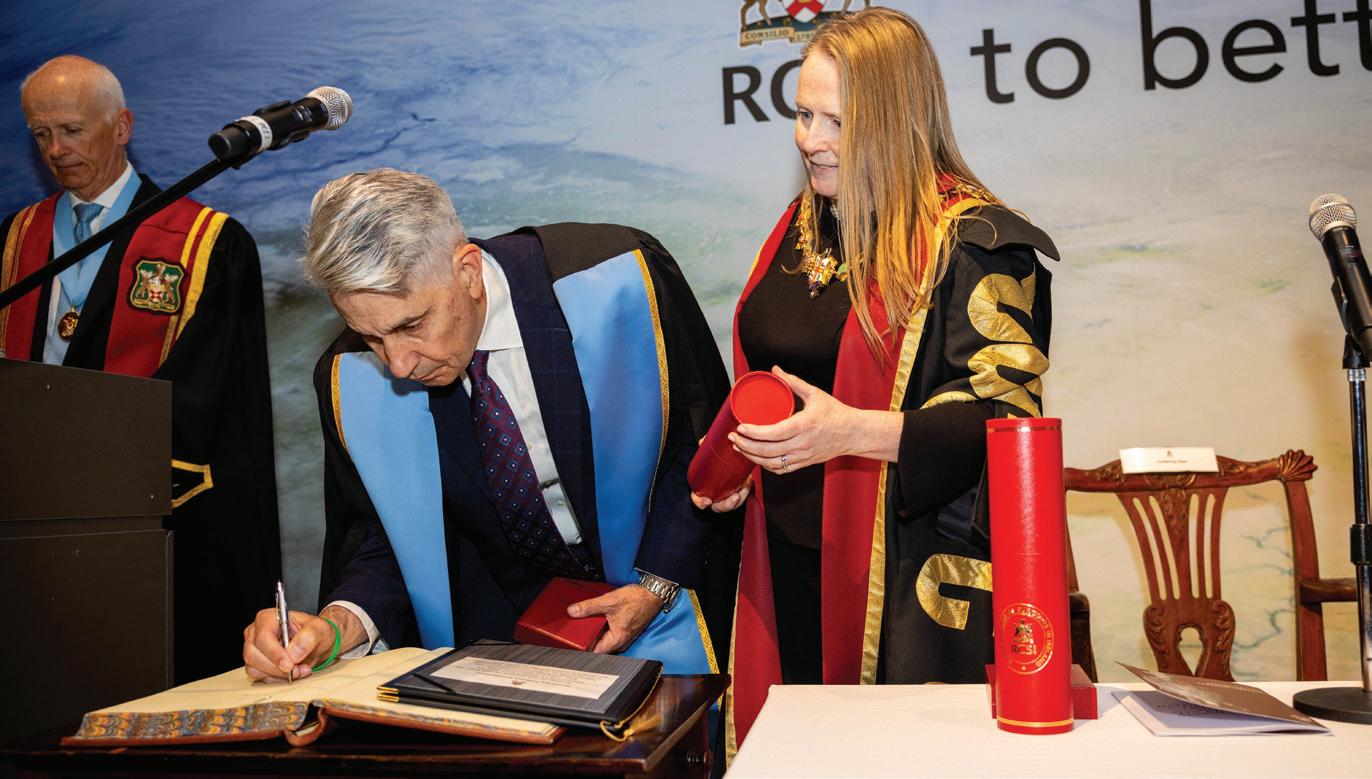


ABOVE Dr Michael T. Longaker is conferred with an Honorary Fellowship by Prof. Deborah McNamara. LEFT Prof. Laura Viani, Prof. Ronan Cahill and Prof. Deborah McNamara at the launch of the New Technologies for the Future of Surgery in Ireland Report. BELOW LEFT RCSI Fellows and Members Conferring in Penang. BELOW The launch of the new Model of Care for Paediatric General Surgery.

census shows that Fellows ratified since 2019 account for more than 12% of our active community. In many conversations over my term as Vice President, I heard much about the challenges faced by young surgeons. Completing surgical training is a cause for celebration, but taking the next steps – whether commencing an international fellowship or starting as a consultant surgeon – can be daunting. In early September, I hosted an informal gathering in Galway to begin building a network of early career surgeons. With the leadership of Christina Fleming FRCSI (Gen Surg), Greg Nason FRCSI (Urol), Emmeline Nugent FRCSI (Gen Surg) and others, we formally launched the RCSI Early Career Surgical Network at the Millin Meeting in November. David Healy FRCSI, RCSI Council member, will act as Council liaison for the new network. You can read more about the work and plans of the Early Career Surgical Network in the “Peer Support for Surgeons” feature on page 8 of this edition of Sugeons Scope. I hope that many of you will get involved.
Resources for Surgery
One of the key challenges reported by newly appointed consultants is difficulty accessing the resources they need to care for patients. As a result, patients face prolonged delays in accessing surgical care and surgeons become frustrated and disillusioned. Bed and theatre cancellations are a frequent reality. For surgeons working in Ireland, the introduction of new infrastructure for scheduled care such as surgical hubs and elective hospitals gives cause for hope.
The HSE’s Elective Surgical Programme promises ambulatory surgical facilities in Cork, Galway, Limerick, Waterford, North Dublin and South Dublin. Progress at each site is at a different stage, with the first hubs scheduled to open in the coming year. Through the National Clinical Programmes, RCSI is playing its part in areas including workforce development and clinical guidance, with RCSI Council member Bridget Egan FRCSI chairing an expert group to coordinate clinical input. Our Vice President, Professor Michael Kerin FRCSI, is leading efforts to improve clinical infrastructure in the West of Ireland. I encourage each of you to stay informed about developments in your own local region to ensure that surgical patients across Ireland benefit from greater access to care. In this regard, don’t forget the annual Health Service Quality Improvement and Innovation Conference at RCSI on 5 February 2025.
Of course, while surgical hubs are welcome, they form only one part of the solution to waiting lists due to their exclusive focus on ambulatory care and day cases. Expansion of inpatient surgical beds and upgrading of theatre infrastructure is critically required to ensure that patients can fully benefit from surgical innovation. Modern laparoscopic, robotic and image-guided minimally invasive surgery is difficult to perform in operating theatres designed and built in the last century. The recent RCSI publication of the short-life working group on technology, chaired by RCSI Council member Professor Ronan Cahill FRCSI, shows that practicing surgeons embrace the role of technology in enhancing surgical care. It’s time for our health service to do likewise. I look forward to discussing this and many other matters at Charter Week 2025 and invite you all to join us from 4-8 February in RCSI. ■






















RCSI SURGEONS SCOPE MAGAZINE is published annually by RCSI for surgical Fellows and Members. Issues are available online at www.rcsi.com. Your comments, ideas, updates and letters are welcome. Please contact the Fellows and Members Office, 111 St Stephen’s Green, Dublin 2; telephone: +353 1 402 2116; email: fellows@rcsi.ie. RCSI Surgeons Scope is posted annually to Fellows and Members in Good Standing. To ensure you continue to receive your copy, please update your contact details via www.rcsi.com/portal. RCSI Surgeons Scope is produced by Gloss Publications Ltd, The Courtyard, 40 Main Street, Blackrock, Co Dublin. Copyright Gloss Publications.

Ms Zahraa Al-Hilli FRCSI, Breast Surgery Specialist at
Clinic,
General Surgeon Mr Aongus Twomey FRCSI on
as
Professor Premnath Nagalingam FRCSI describes the healthcare system in
How Mr Keith Synnott FRCSI signed up for humanitarian work in Haiti and Ukraine
Surgeons can leverage LinkedIn to protect their online presence as well as create a personal brand
growing number of healthcare professionals at all career stages are joining the professional platform to network, learn new skills, build their personal brands and keep their nger on the pulse of industry news.
Jennifer Ryan, Careers Editor at LinkedIn Ireland, says that when it comes to your LinkedIn pro le, it’s important to make sure that it re ects your personality, while remaining professional.
Top tips on how to build a compelling LinkedIn pro le and get the most from the platform include:
Update your profile
Your LinkedIn pro le is a little like an online handshake and we all know rst impressions count. Take the time to add as much detail as you can to your pro le in terms of areas such as your specialty focus and education. Be clear, and use keywords to improve searchability.
Prepare a short introduction that tells your connections a little about yourself. Simple things can make a big di erence. For example, make sure to list your past positions. Users who include at least one position on their pro le receive up to twice as many pro le views and connection requests. Also, include your full educational background and all your certi cations.
Highlight your achievements, including research and publications, state your professional values and goals and invite readers of your pro le to get in touch with you regarding professional opportunities or potential collaborations. Add skills relevant to your eld and request endorsements from colleagues and peers. Be prepared to do the same for others.
Do include a picture, as pro les with images garner more engagement. Use a high quality, recent photo that embodies who you are as a professional –don’t forget to smile!
You can even upload an audio clip to your pro le, using LinkedIn’s name pronunciation tool, to
ensure connections know how to pronounce your name correctly. Considering how many healthcare professionals spend time working abroad, this can be an invaluable tool to avoid awkward situations.
LinkedIn is by its nature a professional network, so building a circle of colleagues, peers and friends is part and parcel of the experience. First and foremost, connect with people you know. When expanding your network beyond that, be sure to add a personalised note so that it’s clear why you are looking to add them to your network.
ere is also the option to follow people you want to learn from. at could include fellow healthcare professionals and other industry leaders – think about how their knowledge and insights can help you in your career. Look out for Top Voices on LinkedIn, who are industry leaders in their eld. Anyone with a Top Voices badge has been handpicked by LinkedIn in recognition of their e orts in helping fellow users uncover valuable knowledge relevant to them.
ink of your network like a garden, it will yield the best results if you give it attention and cultivate it. In this regard, engage with your fellow users by liking or commenting on their posts.
It is also worthwhile joining industry groups and participating in discussions – look out for tools such as the ‘Catch Up’ tab, which is focused on highlighting opportunities to spark conversations with people in your network.
Professional development
Everybody is time pressed these days, but professional development can be as simple as a few clicks on your laptop or phone. Lots of people are understandably nervous that they might be le behind, or not have the right skills. What’s important is that you give yourself an edge by focusing on improving the skills you already have or investing in learning new skills.
Healthcare professionals are no di erent, so it’s
important to keep developing skills that you are interested in, whether it’s improving your ability to give a presentation or becoming an expert in Excel. LinkedIn Learning gives access to over 16,000 online courses taught by real-world professionals.
Join the conversation
Status updates are an easy way to update your network on your professional development or to position yourself as a thought leader. Joining groups and sharing your opinions on current topics as well as videos or articles that interest you are both great ways of staying connected, both within the healthcare community and further a eld.
If you present a paper at a conference or publish an article, be sure to post it. Posting regularly, keeping your pro le up to date and engaging consistently are all key to making LinkedIn work for you. ■





www.linkedin.com/company/rcsifellowsandmembers/
RCSI alumnus and consultant radiologist Dr John Sheehan is active on LinkedIn, sharing articles and podcasts.
Preventive cardiologist Dr Paddy Barrett posts articles, engages with other members and shares videos.
In Dubai, consultant breast surgeon Ms Houriya Kazim FRCSI has an excellent LinkedIn profile with 3,000 followers.
In the UK, cardiac surgeon Mr Anthony H. Walker follows and engages with relevant professional networks.





RCSI University of Medicine and Health Sciences has announced that Blackrock Health is the lead partner for Ireland’s first public health gallery at RCSI’s new building on St Stephen’s Green. Blackrock Health, combining Hermitage, Blackrock, Galway and Limerick Clinics, is Ireland’s leading private hospital group, providing easy access for patients to 600 highly skilled consultants in 50 medical specialties. Dr Caroline Whelan, CEO of Blackrock Health said: “We are proud to support RCSI on this hugely important initiative.”

New surgical guidelines for the treatment of a rare cancer associated with breast impants – Breast Implant Associated-Anaplastic Large Cell Lymphoma (BIA-ALCL) – have been launched. Mr Padraic Regan, National Clinical Advisor for Plastic Surgery, National Clinical Programme for Surgery (NCPS), said: “It is reassuring for plastic and breast surgeons to have this document available as a framework for care. More importantly, it offers reassurance to people impacted by this cancer, that their care will be informed by these evidence-informed guidelines. Getting these guidelines published was a collaboration of many stakeholders and the NCPS is grateful to all those who contributed to this work.”






A new model of care for the sustainable delivery of paediatric general surgery in Ireland was launched by the National Clinical Programme for Surgery (NCPS) and the National Clinical Programme for Paediatrics and Neonatology (NCPPN). Speaking at the launch, Mr Ken Mealy FRCSI, Chair of the Working Group for the General Paediatric Surgery Model of Care and Co-lead of the National Clinical Programme in Surgery, said: “This launch represents a significant step forward in ensuring that every child in Ireland has access to safe, high-quality surgical care, no matter where they live. This model of care has an emphasis on safety, workforce planning, training, and quality assurance of service provision, to ensure that all children who require acute or elective general paediatric surgery are managed in an appropriate environment by staff with the requisite skills.”
INAUGURAL PROFESSOR SEAN TIERNEY TRAINING FELLOWSHIP GRANT
RCSI has awarded the inaugural Professor Sean Tierney Training Fellowship Grant to Zambian neurosurgeon Dr Peter Mushenya. Congratulating Dr Mushenya on his award, RCSI President Professor Deborah McNamara said:
“We are proud to make this award to Dr Mushenya in the memory of Professor Sean Tierney who made an incredible impact on the surgical workforce in Africa. The Fellowship Grant allows us to further sustain his legacy by increasing the specialist knowledge and skills of the surgeons who are providing vital surgical care in underserved communities in the east, central and southern African region. We wish Dr Mushenya every success and we look forward to seeing his progress during his fellowship and beyond.”





RCSI OPENS DOORS TO NEW ¤32M EDUCATION AND RESEARCH CENTRE AT CONNOLLY HOSPITAL
The new Education and Research Centre is an important addition to Connolly Hospital in Blanchardstown. Giving students a dedicated space to learn and hone their skills in a state-of-the-art facility as well as providing additional capacity for cutting-edge research, the building also includes new HSE pathology laboratories. Minister for Children, Equality, Disability, Integration and Youth Roderic O’Gorman TD said: “I am pleased to welcome the opening of the new RCSI Education and Research Centre at Connolly Hospital, Blanchardstown. The students who are educated here will go on to become the healthcare leaders of the future and they will have had the benefit of being educated in a world-class learning environment on the campus of a busy acute hospital.”

Multi-platform RoboStart and Robotic Assistants workshops were held at RCSI for the first time in September, giving surgical trainees across different specialties and surgical assistants the opportunity to enhance their skills in these emerging technologies. Professor Barry McGuire, Dean of Postgraduate Surgical Education and Academic Development, RCSI, said: “We hope to expand this next year, and ultimately it will form part of a formal curriculum pathway.”







A new report from RCSI, which was commissioned by Professor Laura Viani during her term of office as RCSI President, has heard from surgeons across a range of specialties and training stages about how technology is changing surgery.
Professor Ronan Cahill, RCSI Council Member and Chair of the Committee on New Technologies in Surgery in Ireland, described the work in the report as a first step in engagement. “Like everywhere else in society, technology is embedded in surgery with increasing capability coming on stream,” said Professor Cahill. “With advances in computing power alongside improved patient diagnostics, including imaging and genomic analysis, the role of technology in surgery is set to accelerate further into the 21st century. Such capabilities require consideration of training, working, implementation and administration.”
The New Technologies for Future of Surgery in Ireland RCSI Working Group Report 2024 also features a series of invited perspectives on surgical training and education, environmental impact, integrating innovation, the need for surgeons to adapt throughout their career, and the medtech industry.

Professor Eamonn Rogers FRCSI has been appointed co-lead of the National Clinical Programme for Surgery (NCPS). “This clinical programme plays a critical role in our health system, allowing the surgical community to work in collaboration to develop standardised care pathways, clinical guidelines and models of care for the patient journey,” said RCSI President, Professor Deborah McNamara.
“Eamonn is a very experienced surgeon who brings many years’ experience of policy development and quality improvement to his role. I look forward to working with him to support the delivery of safe, timely, accessible and efficient care for patients.”

RCSI President: “Every health service workaround takes time away from patient care.”
In her first interview with The Irish Times, in October, RCSI President Professor Deborah McNamara detailed to journalist Shauna Bowers the “considerable challenges” facing newly qualified surgeons. “The infrastructure in lots of areas is not as good as it could be, and it’s very easy for young surgeons to be isolated when they start clinical practice,” said Professor McNamara. “There are a lot of demands placed on them, and the public have an expectation of very high standards of care.”
Although the health service is undergoing a significant organisational and technological transformation, some elements remain largely unchanged, one being infrastructure. “Many of our operating theatres were designed and built decades ago, and they were built before innovations like laparoscopy or robotic surgery were even imagined,” she said. “There is a mismatch there between the services that surgeons can deliver and the ones that are enabled by the health service in which they’re working.”
Many staff have to think outside the box to counteract such difficulties; Professor McNamara said workarounds have become “a characteristic” of the health service. “Health staff generally work really hard to deliver the best care that is possible for a patient, and the less the infrastructure and systems support that, the more effort and energy health staff spend delivering workarounds as opposed to delivering care.” This is particularly the case in the area of IT, she says, due to largely paper-based systems leading to “duplication of effort” and “every workaround taking time away from patient care”.
However, efforts to change this are underway; the government recently published its digital framework, for example, which would see the introduction of electronic patient health records, and the roll-out of a patient app by the end of the year. Health service staffing is another topic that constantly arises. Unions say there still is not enough, while the Department of Health says the workforce has grown significantly in the past four years.
However, there is an ongoing recruitment challenge, with many recently qualified doctors emigrating for a number of years, particularly to Australia. There can be push factors for younger doctors to work abroad, Professor McNamara said, as “medicine is a 24-hour profession”.
Time spent working abroad can be a good thing for the State. Higher surgical trainees, for example, tend to complete a one- or two-year international surgical fellowship after their programme in Ireland. “That’s actually really enhanced our health service over the years, because the majority of surgeons who go abroad for training, at the end of their training actually come home and practice as consultant surgeons.” The most recent data, from the 2019 class, found 80 per cent returned to Ireland, she adds.
There is also the reverse, with more than 60 per cent of RCSI’s student population being international students. Those who come from within the EU can work in Ireland after obtaining their qualification if they so choose. For those from outside the bloc, however, the rules are different. “Some doctors who qualify in Ireland, and who we know have met the standards of Irish medicine, because of employment legislation don’t have the option to practice in Ireland,” she says. At the same time, she said, in the later stages of their healthcare careers, Ireland is “importing doctors from other countries, where they have studied in a language other than English”.
The State’s population is increasing, as well as becoming older and more diverse, which all changes the needs and demands on the health service. Emergency department overcrowding is at unsustainable levels, while waiting lists – though decreasing – remain above 700,000, with more than two-thirds waiting longer than target times. In light of this, Professor McNamara believes there is a need to think about the “separation of emergency and scheduled care”. The development of surgical hubs, for example, is being done “really efficiently”, and they’re going to be a “really important part of the solution”.
“But they are focusing on ambulatory [outpatient] surgery. So they’re focusing on lower-complexity work. But the hubs focus only on the ambulatory part of the waiting list, and so patients who need the services of bigger hospitals or specialist care, they [the hubs] aren’t going to address that part of it.
There tends to be a “variation across the year”, she says, in terms of elective surgeries being completed. Higher emergency presentations to hospitals during the winter period can result in cancellation of elective or scheduled procedures. “Until we have that [separation], it’s very hard to see how you can get rid of that variation, unless you have a very substantial increase in infrastructure.”
“We have very few hospitals in Ireland that focus on elective surgery or scheduled surgery. We know that the ones that do focus on scheduled surgery can do it really well,” she said.“So it is possible to separate scheduled and emergency care, but it does require action, and it requires what can sometimes be hard decisions.”



The Pan-African Paediatric Surgery e-Learning Programme (PAPSEP), the first ever pan-African training platform for children’s surgery, has just completed its first three-year cycle. The platform, developed in collaboration with RCSI’s Institute of Global Surgery, brings high-quality, free education to paediatric surgical trainees across the continent. Professor Juan Carlos Puyana, O’Brien Chair of Global Surgery at RCSI, said: “The RCSI Institute of Global Surgery is working towards a world where all children in need of surgery can access it when they need it. Surgical workforce remains a huge problem in the strengthening of global health systems, and we are committed to driving programmes which increase capacity through training.” ■



We’ve been protecting members in Ireland for more than 100 years. We have extensive experience of dealing with clinical negligence claims and our team of experts can support you through whatever legal or ethical challenges arise in your career.
medicalprotection.org/ireland




A new initiative to create a dedicated network to support early career Fellows aims to address challenges and barriers to those establishing consultant practice
he Early Career Surgical Network (ECSN) – launched at the Millin Meeting last month – follows on from the establishment of a working group in March of this year. The initiative is supported by RCSI and President Professor Deborah McNamara.
The launch of the network reflects the ongoing commitment of the College to building a supportive community for its newest Fellows as they complete surgical training, undertake fellowship training and transition into their careers as independent consultant surgeons.
Ms Christina Fleming FRCSI, Consultant General and Colorectal Surgeon at University Hospital Limerick, is Chair of the ECSN.
“Our intention,” explains Christina, “is to create a peer support community for people at that time of transition from training into the early years of independent consultant practice, when they are building their surgical practice and trying to figure out where they fit into things.

“The key thing is that this is a career stage-relevant group as opposed to a specialtyrelevant group.”
“It tends to be a time when we are clinically very busy. Building our practice, we are inclined to take on extra clinical sessions to continue to develop our craft and adjust to fully independent practice. But this can be a very challenging time with a lot of firsts experienced across all areas of delivery of surgical care, and it is hard to balance clinical commitments with academic and networking opportunities. So, at a time when we could probably do with the support of our surgical community the most, we don’t lean into it. Having a dedicated network allows us to put a structure around that and create a space for people at that specific stage.”
In her role as chair, Christina is supported by a committee representing a range of surgical specialties. The ECSN will provide opportunities for early career surgeons to network with peers and, as it develops, will provide practical information and resources available both online via a dedicated section on the RCSI Fellows and Members Portal and through organised events.
“Our plan is to invite people who’ve completed Part A of their fellowship exams,” explains Christina. “We envisage them benefiting from the network for approximately the first five years of their consultant practice, bearing in mind that five years of practice will take different people different amounts of time due to a
variety of reasons including maternity leave and sabbaticals. The timing is not strict, and it will become apparent to people whether it remains relevant to them or not.
“The key thing is that this is a career stage-relevant group as opposed to a specialty-relevant group. It’s open to anyone who is a Fellow of the College, whether they are practising in Ireland or not, and whether they came through a structured training scheme or an alternative pathway.”
The ECSN held an informal dinner prior to the Freyer meeting in Galway in September for early career surgeons working in the region or involved in the conference programme.
“That was an effective opportunity to brainstorm and garner informal feedback from people who weren’t involved in the initial working group as to where they would see the value for a group such as this,” says Christina.
One early career consultant who welcomes the establishment of the ECSN is Professor Jarlath Bolger FRCSI, Associate Professor of Surgery and Consultant Upper GI Surgeon at Beaumont Hospital. He was appointed in June of this year having spent almost three years in University Health Network in Toronto and University of Toronto on a fellowship in upper GI surgery, focusing on minimally invasive surgery for cancers of the oesophagus and stomach as well as a placement in bariatric and metabolic surgery and a research fellowship looking at treatment responses in oesophageal cancer. He currently has a 50 per cent academic commitment to RCSI and a 50 per cent clinical commitment to Beaumont.
“Having worked in the system in Ireland and spent time in Beaumont training has made the transition back to Ireland a little smoother,” he says. “But it’s taken a little time to set up access to theatre, endoscopy suites and to clinics and to build a clinical practice. On the academic side I’m still in the process of putting that aspect of my job together, and it will take a few months to get it up and running. Having trained here, I’ve seen enough people coming back from fellowship to know these things take time. One of the most helpful things to me since coming back has been talking to colleagues who returned in the last two or three years about the challenges they experienced. It’s slightly different for everyone, but a lot of the themes are common.”
Mr Andrew Hughes FRCSI, was appointed Consultant Orthopaedic Surgeon at St James’s Hospital and National Orthopaedic Hospital Cappagh in September, having recently returned from three years of fellowship in the US, where he spent a year each at the Rothman Orthopaedic Institute in Philadelphia, which is allied to the Thomas Jefferson University Network, as well as NYU Langone Orthopedics and the Hospital for Special Surgery, both in New York.
“We are very well trained as surgeons in Ireland,” says Andrew, “so I received fantastic hands-on experience in the US as the primary operator, earlier than I expected. When I returned to Ireland I was excited to deal with the surgical aspect of the job, after three years of intense operating and training. I am lucky to have been assigned a weekly trauma theatre slot in SJH, and a clinic every second week.”
While Andrew says he can see his referrals starting to accelerate, and is working with hospital administration to find a weekly outpatient location, it is things outside of the operating room – from making independent decisions, to speaking to family members, to relinquishing autonomy to registrars in theatre – that he says have posed unexpected challenges. He has found being able to turn to friends, co-Fellows and colleagues for advice hugely helpful.
“Andrew Moriarty and Robert Piggott, two early-career colleagues in SJH, have been generous with their time and advice on everything from indemnity issues to constructing and managing my work practice plan. Outside of SJH, Eoghan Pomeroy, Gerard Sheridan, Eamon Coveney, Peter Staunton and Robert Hurley are all former co-registrars of mine, who have been reliable and supportive.
or 20 years ago, and that having a younger voice represented by the ECSN should enable RCSI to support people in the early phase of their consultant career.
“Whether that’s through networking or research supports, there are lots of different ways it could happen,” he says. “Consultants today are expected to be strong clinicians and strong researchers, and then there’s the question of whether or not they want to work in private practice, given the new contract. The demands on consultants from patients and their families are different and increasing. That’s as it should be, but it’s important to figure out a way to support them through that.”
Both Jarlath and Andrew welcome the establishment of the ECSN and are hopeful that it will be an important voice within the surgical community.


He has found being able to turn to friends, co-Fellows and colleagues for advice hugely helpful.
“To formalise an early career group to get a handle on the challenges we are facing is a very important first step,” says Jarlath. “The group will need to be refreshed every couple of years because the challenges will change and the challenges for our cohort now might not be the same in five years’ time. Through my work with the Irish Surgical Research Collaborative I know that the senior leadership of the College is keen to engage on this and to support early consultants and mentor them. I’d be hopeful that this could be a very impactful forum.”



“One of the most helpful things to me since coming back has been talking to colleagues who returned in the last two or three years about the challenges they experienced.”
“Orthopaedic surgery as a specialty in Ireland manages a large national training scheme – there were twelve SpRs in my year – and we have formed quite a tight-knit group particularly over the past two or three years. My registrar colleagues, who I consider good friends, are now working as consultants in hospitals all over the country. We have been helping each other with advice and second/third opinions on a reciprocal basis since our time on the training scheme. I’d encourage surgeons training in all specialties to start to form those bonds as early as possible, as these friendships and professional connections will prove invaluable.”
Jarlath notes that starting out in consultant practice is not the same as it was. Today’s challenges and demands are different to those 15
“An Early Career Network will certainly benefit newly-appointed consultant surgeons in Ireland,” says Andrew. “In the US, specialty and even subspecialty support groups exist for new consultants, such as the Young Arthroplasty Group within the American Association of Hip and Knee Surgeons, so I am keen to get involved in the new network here.”
“The launch of the ECSN at the Millin Meeting in November was confirmation of the commitment on the part of the current leadership of RCSI to explore how best to amplify the voice and views of early career consultant surgeons” Christina says. The ECSN is next planning both a plenary session and a collaborative event with the Irish Surgical Training Group (ISTG) during Charter Week.
“From my previous leadership experience I know how important it is to have a formal group that represents the voice of those at specific stages of their career,” she says. “The ISTG is a fantastic example for surgical trainees in RCSI and I envisage the ECSN being a continuum of this, as trainees transition into independent consultant practice. Until now, I feel that early career consultant surgeons have been somewhat of a lost tribe. I think a younger voice can bring a fresh and diverse vision which can add significant value”. ■
Many factors make the experience of surgeons who are parents particularly difficult, but more flexibility and support ease the challenges. Here, surgeons explain how they balance their work and family priorities
he challenges of combining a career with being a parent are not unique to surgeons.
Everyone who works and has children knows that it is hard to find the balance between doing your job to the best of your ability and being a present and involved parent. But, starting a family during surgical training and raising your children away from your natural support networks while on fellowship abroad presents challenges beyond the norm, particularly for female surgeons who take breaks for maternity leave during training.
Understanding, empathy and flexibility ensure that great surgeons can also be great parents – the roles must not be mutually exclusive.
Mr Ian Reynolds FRCSI
International Colon & Rectal Surgery Fellow, Mayo Clinic
I am currently on fellowship at the Mayo Clinic in Rochester, Minnesota for a year. My wife, Emma, and I have a three-year-old son, Ronan, and a daughter, Harper, who was born on 31 July this year. Ronan was born when I was working as a specialist registrar, just as I was moving between St Michael’s and St Vincent’s Hospitals in Dublin. That was a big adjustment. It was a busy time as I was trying to hone my technical skills and clinical knowledge, and build up an academic portfolio. The call rota was frequent but the job was great and I was learning a lot. Ronan’s birth brought positive change, and made me focus on the more important things in life, and in work. I learned how to be more efficient with my time, to say no to certain things and to prioritise what was important so I could free up time to spend with my family.
Emma is the Communications Director for Aon. Her work is important and she has risen rapidly to a leadership role. As surgical trainees, we have a tendency to focus on ourselves and forget about the amazing things other people do at work. The hard part is trying to balance what I do and what she does with having children. She does a lot of the heavy lifting at home and I’m lucky she is willing to take all that on. She has a little more flexibility than me at work, but not much.

“If I’m involved in a complex resection I might not get home at all.”
Harper was born in Dublin. We had talked about whether Emma would move over with me and have the baby in the Mayo Clinic or whether she would stay in Ireland and have the baby there. For various personal and medical reasons,


she decided on Dublin as she was very happy with the obstetric care she was receiving and would have been moving over very late in the pregnancy when flying was not advisable. The due date was 6 August and I planned to fly home on 2 August. But I got a call on 31 July while I was in clinic to say that Emma had gone into labour. I rushed to the airport, but halfway between Rochester and Minneapolis I got a call from Emma’s mum to say that Harper had been born. I arrived 16 hours later having missed the birth, which was obviously very disappointing. We were lucky that Emma’s mum was around, and it was a happy occasion for her to be there for the birth of her granddaughter. Parental support on both sides has been hugely important. I was home for nine days, and it was very hard to leave. There was uncertainty about how long it would take to get passports and visas, and it was the first weekend in October when Emma moved over. We had been apart for August and September, which was hard.
Emma’s parents travelled over with her and stayed for a couple of weeks. Ronan has started preschool, which he loves; he’s a busy little boy who needs
to be stimulated. I worry that the days could be long for Emma, but she’s an outgoing person, and is doing everything she can to get out and meet people through mother and baby groups and the local athletic club.
Emma will be on maternity leave until my year at Mayo is finished in July 2025. Had we been back home, she might have gone back to work after six months because she loves her job so much, but she’s taking the year off so that we can all be together. She’s making big sacrifices. Transitioning back to work after having a child is much easier for a man, because the time off is short – for women it can be a challenge to find and re-establish their place after maternity leave, so that’s another thing she’s taking on.
Every week is different here, but I finish on time more often here than I did at home. If I’m involved in a complex resection I might not get home at all, or only for two or three hours in the middle of the night and then I’m gone again before anybody sees me. I do some colorectal-specific on-call and I cover one weekend in five, but I get both evenings off. So even when I work weekends, we still get to have dinner together.
This is an adventure for us. We know that if I’m fortunate enough to get a job back home when my training is finished, that’s going to be it for the next 30 years, so we’re making the most of our time away. Last week we took Ronan on a boat ride on the Mississippi River which he loved. It doesn’t really matter what we’re doing, just being together is important.
We are lucky as male trainees, our decisions around balancing work and family are very different. I think for female trainees it’s much more challenging because the complex decisions around starting a family tend to be made at some of the most critical points in their training. I haven’t had to take much time off work or consider extending my training. If someone had said to me, you have to take six months or a year off when your wife has the baby, that’s the rule, I think it would have made us rethink the timing of our family, because I’m not sure how easy it would have been for me to pause my training, or how willing I would have been to do that. I’m very conscious that for female trainees it is a tough personal and professional decision. It’s important we listen to female trainees and make changes to help them manage maternity leave and transition smoothly back into training.
Ms Catherine Gilliland FRCSI
Locum Consultant, Trauma & Orthopaedics, Northern Ireland
My husband, Conor Mullan, and I are both orthopaedic surgeons. We live in Belfast and have four children aged 7, 6, 5 and 7 months, all born in Northern Ireland while I was a registrar in surgical training, which I commenced in August 2013.
In 2014, I took a one-year out-of-programme career break to support my husband on his surgical fellowship abroad. Since then, I have taken three periods of maternity leave during training and a final maternity leave just after CCT. I reduced my training to 80 per cent during my third pregnancy. In total, it took me just over ten years to achieve my CCT.
Taking several periods of maternity leave during orthopaedic training is not a well-trodden path and, though most colleagues were encouraging, I did come up against occasional challenges. I found it hard to access accurate and up-to-

date information on issues surrounding pregnancy in surgical training such as around screening in theatre, exposure to potentially harmful substances, and limitations on some of the more physical aspects of the job. My worry was always that my training would be impacted negatively by adjusting how I worked and there was no one who could advise me. Few of my trainers had encountered a pregnant trainee before. It was rare that I came up against anyone who felt my chosen career clashed with my decision to be a mother, but I had one bad experience with an older surgeon in theatre when I had been scheduled in surgeries that were not reasonable for someone 30 weeks pregnant. Although it was distressing at the time, I was delighted to be shown support by other surgical and nursing colleagues. Other challenges came in the form of dealing with the hospital trust’s administration teams, as reducing my hours to 80 per cent inevitably led to incorrect banding and pay every six-month rotation.
“Some weeks there are balls dropped, deadlines missed and fish fingers again for dinner.”
I feel blessed to have had four mostly healthy pregnancies and appreciate that I was able to continue training to the best of my ability. I love being a mother and when I was sitting the FRCS exams it was a difficult time managing small children and seeing them less frequently to facilitate revision and attendance at multiple courses.
Conor is a few years ahead of me and had already been appointed a consultant when we had our first child. For the first few years, gaining confidence and expanding your surgical abilities through high exposure to diverse and complex cases is so important that we never considered him reducing his hours. I also
dearly wanted some balance between time with my children and training. We continue to support each other as both jobs, parenting and surgery, are fulltime. Some weeks it feels like it all falls apart and there are balls dropped, deadlines missed and fish fingers again for dinner.
In February, I am going on a one-year Fellowship in Paediatric Orthopaedics to Perth Children’s Hospital in Australia. Conor will take a career break from his NHS job in order to enable us to do this. I couldn’t realistically do a remote fellowship in the UK or Ireland as I want to be 100 per cent committed to the fellowship opportunity and not have to be thinking about getting home at weekends or worrying about being away from the children; it’s better for us all to be in the same place.
Conor may work in some capacity once we are settled but not full-time; he is going to take on the bulk of parental responsibility. Going back to Perth where he did his fellowship removes some of the unknowns for us and hopefully reduces some of the stress of the move – we know the schools and the areas we would like to live in, and still have some friends and colleagues out there.
As a two-medic family you just have to get on and do it. It is chaotic some of the time and the house is not as tidy as we might like it to be. Sometimes appointments get forgotten. We are lucky to have the help of our parents from time to time and we set up childcare as best we can. Until now, I have been the parent who can be available when one of the children is sick, but that will be difficult going forward when we are both consultants and have commitments to a clinic or theatre list. How will we cope? I don’t have the answer at the moment but I plan to outsource as much as I can and accept there will be a degree of unpredictability.
Sometimes I feel I have missed out career-wise. Occasionally, I have to remind colleagues not to confuse my inability to go to something with a lack of enthusiasm for my career. My husband has also had this experience as, in supporting me through my training and being an involved parent, especially taking on the lion’s share of parenting in the months before my FRCS, he has missed out on career opportunities. It has been disheartening to watch male colleagues go past me, and have people whom I taught have to sign me off on an operation. There are some courses and travelling fellowships in which I would have aspired to partake, but couldn’t. It has not always been an easy journey but mostly an enjoyable one. I am proud of making it through and have an adorable family I wouldn’t change.
I think that training schemes are beginning to adapt and develop to make surgical training more flexible for the next generation and I hope that we continue to make improvements. We need to be mindful that not everyone’s journey to parenthood is an easy one. Time out may be required to attend multiple appointments for assisted conception and parental leave will be requested by couples of the same sex, or people having children by surrogacy, not just women needing to take maternity leave. It is going to be challenging, but to retain and expand a workforce, and attract diverse and passionate individuals to the surgical disciplines we need to learn to be flexible while ensuring that the craft of becoming a surgeon is not diluted.

Ms Helen Mohan PhD FRCSI FRACS
Consultant Colorectal and Robotic Surgeon, Peter MacCallum Cancer Centre, Austin Health; Director of Clinical Research IMRA; Senior Lecturer, University of Melbourne.
When it comes to parenthood and surgery, there is never a perfect time and things don’t always work out to plan. I’ve been very lucky in that I have a family of four kids: a boy of 7, twins of 5 and a little girl, Siobhán, who has just turned one. Each of them was born at different stages of my training journey. I had my first in the middle of my SpR training, the twins as a final year SpR and Siobhán as a consultant, but I also lost a little girl, Fiona, at 18 weeks gestation when I was on fellowship here in Australia and had a previous miscarriage. Parenthood isn’t a given and it presents a lot of challenges. It’s very common for female surgeons to have fertility and pregnancy issues, as Dr Ailín Rogers has highlighted in her research, and I’m aware of many colleagues and friends who have had IVF or experienced pregnancy loss. It is important to be mindful that people may be struggling on their journey to have kids. I really appreciated good colleagues for both the happy and sad events along my training journey. I was lucky to be very well during my last pregnancy and, because I do a lot of robotic surgery, I was physically able to operate until quite late. However, I believe it is important to empower female surgeons to take whatever time they
“My husband and I are both doctors so if we have a sick child we end up negotiating.”
need to protect both their own health and that of their babies, and not champion working until super-late in pregnancy no matter what. In previous pregnancies, I ended up taking time off work with severe hyperemesis and finished up early with the twin pregnancy. It was a very small percentage of surgical and training time overall; we need to have enough flexibility and capacity within the workforce to accommodate pregnant surgeons.
I was lucky to get the PROGRESS Women in Surgery Award when I was coming to Melbourne on fellowship. The funding helped me maximise my fellowship experience, because at the time the twins were very small and we didn’t have our normal backup and support. Being able to get additional childcare to be able to fully embrace the fellowship and do a high case load was great.
One of the things that hasn’t been done as well as it could have been historically is supporting people with intentional training opportunities and encouragement as they return to the workforce after periods of leave. I notice in our trainees coming back from leave that while their skills are there, their confidence isn’t back to normal.
Improving efficiency in how healthcare organisations function can facilitate more family time. My husband and I are both doctors so if we have a sick child we end up negotiating. If it’s a theatre day for me, then my husband does the pick-up but if I am in clinic and can convert some to virtual consultations then I do it. Having a good electronic medical record system that I can use from home helps with this. We still rely on finding emergency childcare sometimes.
If starting again I would tell myself that ‘good enough’ is okay and not to be sucked into peer pressure about parenting non-essentials. I think you can put yourself under huge pressure over things that probably don’t matter in the long run; it doesn’t matter what other people are doing once your little family is happy.
Childcare is a huge issue. In Ireland I had lots of family support at home, whereas in Australia I had no regular family support until recently when my cousin moved here. It is very expensive to work the hours we work because we end up having to pay for out-of-hours and unpredictable childcare, particularly in training. When I was in training, all of my salary would go on our childcare, particularly since we had twins. I think there’s an argument for more statesubsidised out-of-hours childcare for healthcare workers.
While it is a huge joy to be a parent and a surgeon, it does have its challenges and there’s lots we can do to make it easier for those coming behind us.

“I would encourage all trainees and young consultants to use the flexibility to get stuck in as the kids will be gone in no time.”
Professor Brian J. Mehigan FRCSI FRACS
Consultant General & Colorectal Surgeon, St James’s Hospital
As a father of five – Ogie, 15, twins Michael and Claire, 12, and identical twins, Florence and Helen, 8 – I feel very lucky that my architect wife, Emily, gave up work to become a full-time stay-at-home mum when our eldest was born. I recently moved to a half-time role in my HSE job so I have some quiet weeks when I can do school runs with my three daughters and enjoy that. I never managed any school runs before and only realise now how the local national school is the cornerstone of the community. I meet lots of other dads as well as mums at the school and enjoy those interactions. I think less-than-fulltime commitment to HSE jobs will be the future and I would encourage all trainees and young consultants to use the flexibility to get stuck in as the kids will be gone in no time. No one on their deathbed wishes they spent more time at work! ■
The NSRSC is establishing itself as a go-to centre for national and international trials and studies. RCSI is the driving force
he purpose of the National Surgical Research Support Centre (NSRSC), established by RCSI in 2021, is to support, encourage and facilitate surgical trials, and to generate high-quality evidence-based research in surgery.
It aims to promote a culture of research in clinical practice and thereby improve patient outcomes.
Professor Stewart Walsh, Established Professor of Vascular Surgery at the University of Galway is the Clinical Director of the NSRSC.
“Surgical trials capacity in Ireland lags behind comparable nations in Europe and further a eld,” he explains. “Building trials capability requires a core team with knowledge and expertise in trials regulation, design and conduct to support surgeon investigators who wish to undertake their own trials or participate in major international trials.”
Dr Anne-Marie Byrne, Operations Director of the NSRSC, says that one of the reasons there are very few surgical trials done in Ireland is that the pressure to train surgeons to meet the needs of the health services has meant that there has not been su cient time or resources to support and develop multi-centre surgical trials and studies.

mainly of systematic reviews, clinical audits or single centre studies rather than high-quality research studies and trials.
“ e group also identi ed a perception that Ireland was a di cult place to do a surgical trial because of a lack of supports and training,” explains Dr Byrne. “ is combination of factors discouraged surgeons from getting involved in trials as they saw it as too onerous.”
e working group recommended the establishment of the NSRSC to help surgeons by encouraging them to collaborate to undertake multi-centre surgical trials and generate high-quality research.

“Building trials capability requires a core team with knowledge and expertise in trials regulation, design and conduct.”
RCSI Past President Professor P. Ronan O’Connell FRCSI recognised the importance of research in surgical training, and established a working group to examine what could be done. e working group found that some of the research being done by trainees to meet the four-publication requirement of their training consisted
“Trainees who have nished their eight-year training programme have to compete with international surgeons for fellowships in the top institutes around the world, where they will have to demonstrate their research skills and ability to publish,” says Kieran Ryan, Managing Director of Surgical A airs, RCSI. “ e NSRSC is part of RCSI’s investment in supporting this aspect of our trainees’ development.”
“ e driving motivation,” explains Professor O’Connell, “was the College’s ambition to provide the infrastructure necessary to facilitate engagement by surgical trainees and early career consultants such that clinical outcomes’ research and innovation would become integrated into training and daily clinical practice.
“Surgical trainees were nding it increasingly di cult to undertake research in the absence of a supportive infrastructure. Few hospital units had the resources to facilitate research protocol development, ethics application, grant application, secure data collection and statistical analysis.
“We felt there was a need for the College to promote clinical research as an integral component of training by providing the necessary infrastructure. If this could be achieved, I was sure our trainees would embrace the opportunity.”
Professor O’Connell’s ambition is to create a culture where involvement in research is the norm rather than the exception, and that this in time will percolate down to each new generation of consultants.
“In order to maximise the buy-in from the largest number of trainees possible,” he says, “we felt it important that the NSRSC fall under the aegis of the College of which they are all part, rather than any other institution.”
e NSRSC now provides permanent trial support resources for Irish surgical patients and investigators.
Dr Byrne, a scientist and former clinical project manager in Cancer Trials Ireland, has extensive experience in setting up and running trials in Ireland. She explains that while working on a trial is not yet mandatory for trainees, there is a growing awareness that work on multi-site trials generates better evidence and publications, and makes trainees more competitive in terms of fellowships and even consultancy posts in the future.
ree years on from the establishment of the NSRSC, she is seeing increased enthusiasm on the part of trainees to get involved.

is capacity to support we then further re ne and develop the methodology and statistical analysis plan. We help prepare patient information lea ets, consent forms, data protection impact assessment forms, ethics and regulatory submissions, and contracts. Once all approvals are in place we help the principal investigator open their study at multiple sites across Ireland.
“ e advantages of opening in lots of hospitals is, rstly, it gives patients access to a trial regardless of their geographical location and, secondly, the trial is more likely to recruit the necessary number of patients to provide data to answer the research question.”

“Surgical trainees were finding it increasingly difficult to undertake research in the absence of a supportive infrastructure.”
“We have harnessed connections, established collaborations and are very much working with the willing,” she says. “Within the University we have been able to leverage the support of the Data Science Centre and of the research, contracts, legal and sponsorship o ces. In terms of paperwork, it’s di cult to get trials o the ground in Ireland. e administrative workload is heavy, and issues around ethics approval and data protection are complex. Surgeons are not familiar with the processes involved nor do they have the capacity to deal with the major administrative workload as they lack su cient protected research time. e NSRSC can relieve them of that burden and provide training so surgeons can get on with recruiting patients and collecting data to answer important research questions.”
To encourage collaboration and engagement in trial activity, the NSRSC has provided bursaries to fund multi-centre feasibility trials. e NSRSC’s scienti c advisory board, comprising a surgeon from each specialty, reviewed the applications and awarded nine initial grants.
Each trial begins with a dra protocol from a principal investigator outlining the proposed research question and approach to be used to answer that question.
“Our role at the NSRSC is to sense-check that initial protocol from a scienti c, clinical and resource perspective,” explains Dr Byrne, “and if there
e Centre provides support for trials involving patients under the care of a surgeon from any surgical discipline. Professor Walsh explains that there is a deliberate focus on attempts to address research questions that are important for surgical patients but would not be addressed by commercial sponsors.
PROPEL-2, the rst investigator-led trial under the aegis of the NSRSC, led by Chief Investigator Ms Claire Donohoe FRCSI, with Co-Investigator Mr Noel Donlon FRCSI, is now open in ten sites in Ireland. is randomised controlled trial compares negative pressure wound therapy dressings to standard wound dressings in patients following midline laparotomy, to determine the best surgical outcomes in terms of surgical infections, patients’ quality of life and cosmetic appearance.
“To get the trial up and running we had to go to the ethics committees for each of the twelve hospitals, and then to their data protection, contracts and legal o ces, for review and approval,” explains Dr Byrne. “It took two years to get this trial open at all ten sites. If we had a single national ethics approval system in place in Ireland for surgical trials, we would have been able to open ten di erent trials in the same time frame. It is very frustrating as it ultimately sti es research, innovation and the enthusiasm of the surgeon trying to get their trial started. Somewhat counterintuitively, if you want to do a higherrisk regulated drug or medical device trial, you only need to go to one ethics committee to get approval to open in multiple hospital sites.
“ e training opportunity that working on a multi-centre trial o ers is invaluable, as the surgeons are learning by apprenticeship rather than theoretically. Having multi-centre trials also means that, when the surgeons nish their rotation in one hospital, they can continue the trial in their new hospital. at is fantastic for the trial, for the patients and for the surgeon, who can bring that experience to the new hospital team. In an ideal world, we’d have multiple surgical trials across all specialties open in every hospital in the country.”
Professor Walsh notes that “as the WHO estimates that by 2050 annual deaths from infection due to multiresistant organisms will equal deaths from cancer, this has profound implications for future surgical patients and the NSRSC is especially keen to support surgeon investigators evaluating novel non-pharmacological interventions to reduce the burden of surgical infection such as the PROPEL-2 trial.”
Other trials currently underway addressing the issue of surgical infections are the MetaMet Trial in conjunction with the HRB Diabetes Trials Network, which assesses two methods of dividing bone during digit amputation to assess the e ect on healing and surgical infections, PINTA – Prophylactic Incisional Negative Pressure Wound erapy (NPWT) for major amputations, and ENVELOP: Excision and Negative Pressure Wound erapy Versus Excision and Leaving Open with standard wound care for management of chronic pilonidal sinus disease.
In addition to these feasibility trials, the NSRSC also supports and encourages surgeons to open international trials and studies in Irish hospitals to give Irish patients access to cutting edge research.
Dr Anne-Marie Byrne.


“We have harnessed connections, established collaborations and are very much working with the willing.”
e award of an NSRSC International Collaborative Surgical Trial Award helped Professor Aoife Lowery FRCSI open the ATNEC breast cancer trial, led by Professor Amit Goyal of the University of Derby, in University Hospital Galway. ATNEC is a randomised controlled trial investigating whether armpit (axilla) treatment and associated side e ects can be avoided in breast cancer patients with no residual cancer in the lymph glands a er chemotherapy.
e trial is open in 78 sites across the UK, and Ireland is the rst country outside of the UK to open the trial.
“We are in the process of opening the study in a number of other Irish hospitals,” explains Dr Byrne. “Although it brought its challenges from a GDPR and contracts’ perspective, it is important to persevere so Irish patients can bene t.”
rough the NSRSC Surgical Trial Embark Award, the NSRSC are
supporting Dr Jessie Elliott FRCSI, and her SARONGII randomised controlled trial of intensive surveillance versus standard postoperative follow-up in patients undergoing surgical resection for oesophageal and gastric cancer.
Dr Elliott is the Chief Investigator and leading this international study from the Trinity St James’s Cancer Institute. In collaboration with Trinity College Dublin, which is the sponsor of the trial, the NSRSC is acting as the trial coordinating unit assisting Dr Elliott with opening the study in sites across Europe.
Since the establishment of the NSRSC, its team has expanded to include a statistician, a clinical project manager and a clinical trial coordinator. Initial funding has come from RCSI, and a sustainable funding model to support future trials is now being developed. Clinical investigator grants and the SPARK research innovation funding programme are also available to surgeons, and Dr Byrne and her team are available to help identify opportunities and encourage and support surgeons to apply.
“ e ultimate aim,” explains Dr Byrne, “is to establish a surgical trial network to promote collaboration amongst surgeon investigators for international and collaborative trials that can be open in hospitals across the island of Ireland. We want to showcase Ireland as an innovative, attractive place to do trials.”
“ anks to the funding and supports provided by the College,” says Professor O’Connell, “and the outstanding work of Kieran Ryan, Dr Anne-Marie Byrne and Professor Stewart Walsh, the NSRSC has already succeeded beyond all expectations in terms of the enthusiasm on the part of trainees and early career surgical investigators and the success of their research studies to date. ere is a great sense of momentum. I am looking forward to the NSRSC establishing itself as the go-to centre for national and international studies and trials, and I hope that in the future the national funding agencies such as the HRB will recognise the importance and support surgical research to improve outcomes for Irish patients.” ■
To find out further information and keep up to date with the NSRSC activities visit their website www.rcsi.com/nsrsc and social media channels



To get in touch with your idea for a trial email NSRSC@rcsi.com










For Ms Zahraa Al-Hilli, Cleveland has all the perks and none of the hassle of a big city, and is home for the foreseeable future

orn and raised in Bahrain, Ms Zahraa Al-Hilli is the second of four children. She always knew she wanted to study medicine and become a doctor, so she applied to RCSI and started her undergraduate degree in 1998 at the age of 17.
“I was nervous moving away from my home and family to start something new,” she recalls, “but I was also excited to meet fellow students from all around the world. I developed strong bonds and relationships with my classmates. During medical school I also started to develop an interest in surgery. I did several electives, some in Bahrain, which exposed me to the field. I was able to scrub into cases, work with surgeons, and develop that passion and love for surgery.”
Zahraa completed her internship at Beaumont Hospital, rotating through colorectal surgery, ENT, cardiology and GI. This was a great experience, which allowed her to build on the interest in surgery she had developed during her undergraduate years.
“I had the opportunity to get to know and work with some great female surgeons including Professor Deborah McNamara and Professor Laura Viani. These women are powerful role models and leaders, and I have been lucky to have them and other female surgeons as mentors throughout my career. Although surgery was a predominantly male specialty when I started, things are changing, which is great to see.”
After intern year, Zahraa stayed in Ireland for her SHO training, and worked with Professor McNamara and Professor Arnold Hill in Beaumont.
“As I got exposed to more specialties, I found myself drawn to the discipline of breast surgery. There was a lot of exciting research and innovation happening, and the experience of being part of a breast surgery patient’s journey drove me to do my research in that area.”
Zahraa subsequently did research with Professor Hill and Professor Leonie Young, working in the lab for two years and completing a doctorate in medicine by research. She was then a lecturer in surgery and worked as a registrar before being accepted for SpR training.
“As I neared completion of my training, I was looking to do a fellowship and specialise further, and my field of interest was breast surgery and endocrine surgery,” she explains. “Initially I had not intended to apply to the US. But my sister, Mariam, who is three years younger than me, a graduate of RCSI and a gynaecologic surgeon, was doing her training at Mayo Clinic and I thought it would be a good opportunity to explore some options. I completed my exams, and matched into the Breast Surgical Oncology Fellowship programme at Mayo Clinic. I had a fantastic year, with great mentors who are leaders in breast surgery. After the breast surgical oncology fellowship I did an endocrine surgery fellowship, also in Rochester. That provided me with the additional training, skills and tools I needed to go into practice in these areas.”
The extent of opportunities available to her in terms of clinical practice, academic research and innovation in the US influenced Zahraa to remain in the States after completing her fellowships.
“I’ve been at Cleveland Clinic for the past eight years. It has been a great privilege working as part of a great multidisciplinary team. We have a comprehensive programme that provides a wide range of services including screening, high risk management, management of benign breast disease, hereditary breast cancer risk management, breast cancer care and survivorship.”
Zahraa is currently the Interim Director of the Breast Center and Co-Director of the Comprehensive Breast Programme. It is, she says, a privilege and honour to hold these roles and be able to impact the care of the women under the care of her and her team.
As well as her days in the OR and in clinic, Zahraa is able to dedicate time to her administrative and leadership duties which include programmatic development, strategic planning, and the professional development and support of the staff.
The Cleveland Clinic’s Breast Programme spans several locations in Ohio as well as sites in Florida and Abu Dhabi. Zahraa and her colleagues work together to ensure aligned and consistent care across all locations.
“Our teams come together for tumour boards, journal clubs, staff meetings, programmatic meetings and education meetings. We also have an active research programme that includes clinical research and translational research, as well as clinical trials.”
On an OR day, Zahraa would typically start at 7.30am and work through until 5pm. Clinic days run from 8am until 5pm.
“A lot of what we do in breast surgery is outpatient work, so we usually don’t have many inpatients to see. Many of our patients are able to go home on the same day after surgery. We do surgeries such as excisions, wide excisions or lumpectomies, axillary lymph node surgery and mastectomies with or without reconstruction. We partner with our plastic surgery colleagues for reconstructive surgery and collaborate together on innovative procedures such as immediate lymphatic reconstruction for lymphedema prevention and nerve restoration after mastectomy. We are exploring the exciting world of robotics. My individual team includes a nurse care coordinator who helps take care of the patients and coordinate their cancer journey. We also have nurse practitioners, physician assistants and rotating general surgery residents. Sometimes we have medical students and visiting residents as well.”
For Zahraa, the biggest challenge in healthcare now is the speed of innovation and data.


Our goal is to deliver equitable quality care ... medical advances need to reach everyone
“There’s a lot to keep up with while at the same time managing the complexities of coordinating efficient patient care. We have to ensure we keep up with the increase in volume of patients while taking good care of them and reducing the cost of care. Being able to provide good access for patients to have their treatment in a timely fashion is one of our top priorities. It is important to me to work towards a seamless patient experience, and we try to address these issues through continuous improvement efforts. Thankfully, I’m part of a great institution and team and everybody keeps the patient at the centre of how we think and what we do. This makes partnering on these tasks more enjoyable.
“The US healthcare system is different to other healthcare systems in that it is predominantly a private system. Access to care varies based on insurance coverage and for that reason there is a significant population that faces barriers to care, out-of-pocket costs and limited access to some services. At my institution, we care for patients of different backgrounds; these are predominantly privately insured but also include government-funded, self-pay and international patients. Ultimately, our goal is to deliver equitable quality care. Innovations and medical advances need to reach everyone.”
Over the past two years, in addition to juggling her clinical and academic work with her research and leadership roles, Zahraa completed an MBA at the University of Chicago Booth School of Business.
“It required a lot of time and effort as I had to travel to Chicago for classes at weekends and it was quite a rigorous programme to complete alongside my busy clinical practice. Completing the MBA was a key goal for my own professional development; it was important to me to broaden and hone my skills as they

relate to healthcare and business. Acquiring business acumen has helped me think and approach problems in a different way, and has allowed me to gain skills in strategic planning, financial management, leadership, operations efficiency and understanding economics. Building on this, I hope to continue to grow in my career and my ability to impact patient care, through innovation and research.”
Zahraa lives in Downtown Cleveland, a 15-minute commute from the main campus of Cleveland Clinic. She finds Cleveland a very liveable city and, after eight years, considers it home for the foreseeable future.
Dr Prabhu Ramasamy and family.
“It was an easy place for me to settle and integrate in. It is quite spread out and has all the perks of a big city without the hassle of a big city; traffic is not a problem. There’s lots of of great food and events from sport to orchestra to theatre. Getting to the airport is straightforward, so it’s easy to get away for the weekend. One of the best things about Cleveland is having access to one of the Great Lakes, Lake Erie, and there are miles and miles of green space within a ten- or 15-minute drive. There’s a huge metro park system with trails for walking, cycling or running going from the Lake all the way south.”
Weather-wise, Cleveland is typical of the Midwest so the winters are cold and snowy, but the summer and fall are pleasant.
“Experiencing all four seasons is special, and it’s amazing to have all of that nature so close by. The summers here are beautiful, and to be able to spend time outdoors running or biking or just meeting up with friends on a patio is wonderful.”
Zahraa’s family – aside from her sister, Mariam, also in Cleveland – live in Bahrain, and they talk often. She visits Bahrain at least twice a year.
“One of the best things about being in Cleveland is having my sister here. I think if she was not here, I might not still be here! We are very close; not only is she my sister, she’s also my best friend. So we often travel together at weekends or go out for dinner or just catch up; we have a lot of friends in common and similar interests. We overlapped in RCSI and we were in Rochester together. We are here together. So I guess wherever we go in the future we will probably be in the same place.” ■
Mr Aongus Twomey FRCSI is a Consultant General Surgeon with a specific interest in urology. After six years in the UK, he worked for many years at Mercy University Hospital in Cork and outside of his clinical practice was, and still is, an active member of the Irish Surgical Travellers Club
orn in Cork City, Aongus Twomey grew up in Mallow where his father, Tadhg, a scientist with a PhD from University of Galway, was the manager of the town’s sugar factory. His mother, Maeve, was a doctor who had trained as an anaesthetist in the UK and worked part-time throughout his childhood.
Aongus is the middle child of five, though his younger brother, Feargal, sadly died as the result of an accident at the age of eight when Aongus was twelve. He initially attended Dromahane National School outside Mallow and later moved to the Patrician Brothers National School in the town. He attended Coláiste na Rinne at Ring, Co Waterford, for a year before boarding at Glenstal in Co Limerick.
“My parents’ priority for us was education,” he recalls. “All their money was invested in us. We had many happy summer holidays in Ballybunion where we made lifelong friends and great memories. They gave us the best possible education.”
Aongus remembers there being plenty of ‘medical speak’ in the house when he was growing up. His older brother, Cillian, who became a geriatrician, and sister, Fiodna, who became a public health doctor, went to medical school before he did. His younger sister, Aifric, is an advanced nurse practitioner in emergency medicine in Scotland.
“Growing up, I always wanted to be a doctor and in particular a GP,” says Aongus.
Aongus attended medical school at UCC graduating in 1973, and then completed his intern year at University Hospital Kerry, which was then called St Catherine’s.
“By that stage I had a yen to become a surgeon,” he says, “but the exams were very difficult, consultant posts were thin on the ground and it was all very competitive. I wasn’t sure that I would make it.”
Instead, he opted to do GP training and did a few GP locums in Cork and Kerry. While he found the work interesting, he had a sense of being very isolated, and became increasingly aware of the huge burden of responsibility borne by GPs, particularly those working in single doctor practices.
His years in general practice gave him an insight into that world, but Aongus eventually decided to pursue a career in surgery.


“At that time, the initial training took three years,” he says. “I spent the first two years doing basic training in neurosurgery, orthopaedics, general surgery and A&E at Cork University Hospital and its associated hospitals, and I followed that with a year as a junior registrar. I had very supportive mentors in Cork including Professor Michael Brady, the late Professor Liam Kirwan, Professor Gerald O’Sullivan and Mr Joe O’Donnell. They were very encouraging and maintained contact and involvement all the way through my career.
“There were very few higher training posts available in Ireland at that time and most of us went abroad. I had married Eileen Murphy from Cork City who had been a couple of years behind me in UCC. She had completed her membership in medicine but being a pragmatist, switched paths to radiology which she felt would offer us more options.”
The couple moved to London when Eileen secured a training post in radiology at Northwick Park Hospital in Harrow.
“I had no job when we travelled over,” recalls Aongus, “but after a few days I secured locum work at Northwick Park and after a short while my career took off. I was very fortunate. I also worked in the West Middlesex Hospital in Isleworth, and in the then-new Charing Cross Hospital. We had a wonderful time in London and spent six years there, during which time our sons Michael and Conor were born.
“In Northwick Park, there were four general surgeons, each with a specific interest. I held registrar and senior registrar posts in general surgery and subsequently in urology. At the time there were very few urologists in Ireland, but there were lots of patients with urological problems in Irish hospitals. Because of this, those with similar training to me were appointed as consultants to various hospitals around the country to meet this need. Subsequently, specialist training for urologists was introduced but that didn’t exist at the time.
“I do feel that surgery is very specialised now but that not every patient needs a specialist and our peripheral hospitals need to be staffed by well-trained general surgeons who know what they can do safely and what they can’t. When I interviewed for the job in Mallow the first question I was asked was: ‘What operations are you not going to do in Mallow?’ I said I wouldn’t do oesophageal, low rectal, elective vascular, reconstructive urology in children or cystectomy operations. I’d say that got me the job. I think knowing your limitations demonstrates good clinical judgement.”
“I do feel that
surgery is very specialised now but that not every patient needs a specialist and our peripheral hospitals need to be staffed by well-trained general surgeons who know what


they can do safely and what they can’t ...”
Interestingly, Aongus notes, there were 16 applicants for the Mallow job. “Different times indeed!”, he says.
Aongus, Eileen and their two sons returned to Mallow in 1986, and he worked there for the next 34 years. For the first 25 of his years at Mallow, Aongus was on a 1-in-2 call rota and for the remainder it was a 1-in-3, a huge improvement.
“We had no registrars and so all surgery was done by the consultants themselves, which was hard work for the consultants but very good for the patients,” says Aongus. “Working in a peripheral hospital on a 1-in-2 rota can be challenging. It was certainly very tough for my family. We lived in Mallow initially and then moved to Cork, 20 miles away. I liked the commute, because in the morning it gave me time to prepare for the day ahead, and on the way home it was an opportunity to debrief and process how the day had gone.”
During his time in Mallow, hardly a single day passed that he didn’t get a call from a GP concerned about a patient.


“Mentoring in surgery is very important and I think it is not as strong as it was in my day, it has been diluted in recent years. It’s still hugely important and should not be allowed to disappear.”
“I always took the calls and tried to help. If it was an emergency, I could advise the GP to send them in or, if it was less urgent I could see them in clinic. It was important to me that the GPs felt comfortable ringing and I was very conscious it was much easier for me with the hospital back-up than for the GP out on their own.”
In 2012, emergency surgery ceased in Mallow. Aongus was appointed to the Mercy University Hospital in Cork but continued to do non-emergency work in Mallow as well, retiring from Mallow in 2020.
“The Mercy asked me to stay on after that and I am still there,” he says. “I work part-time and have done no ‘on call’ since 2022. I do a full day list on a Monday, an outpatient clinic on a Tuesday and I visit inpatients on the other days. I also spend time teaching, mentoring and examining. It works out at two and a half days spread across the week and I find it very rewarding. The Mercy is a fantastic hospital and I have excellent colleagues in surgery, anaesthetics, radiology and ICU. In ways, starting at the Mercy was a new beginning for me and it has been an absolute joy. I very much enjoy the engagement with the trainees and students. I like structure in my life, and the fact that I can still make a contribution.”
Outside of his clinical practice, Aongus has been an active member of the Irish Surgical Travellers Club since 1998, serving as its president in 2012.
“The society was founded in 1954 and has about 30 members,” he explains. “We meet twice a year and each year we go abroad to visit a hospital overseas. Professor Gerald McGreal is this year’s President and recently we travelled to Toronto to visit Toronto General Hospital. When I was President in 2012 I brought the group to Boston visiting Massachusetts General, the Brigham and Women’s Hospital and Beth Israel Hospital. We were very well received and had a great time.”
“My membership of the Surgical Travellers Club has created fantastic connections with other specialists around the country and with colleagues who worked a 1-in-2 rota, as I did. The opportunity to visit operating theatres abroad and see different operations and new innovations has been wonderful. It’s reassuring when you see how people do things elsewhere and realise the way you’ve been doing things is not so bad. Surgery is a discipline of confidence and competence, and both are equally important.”
Reflecting on a long and fulfilling career, Aongus observes that he has seen very many changes over the years in the practice of surgery.

“I suppose the biggest was the change from open to laparoscopic surgery. Many of us were used to doing ‘oscopies’ already so that transition was not particularly difficult. Surgical instruments have improved and there have been enormous advances in intravenous nutrition, to the benefit of patients in recovery from surgery. I welcome the advent of the multi-disciplinary team and meetings and that most surgeons no longer work in isolation. Help is always available. The best piece of advice I could give a surgeon who is in a dilemma is to pick up the phone and ring a colleague. Mentoring in surgery is very important and I think it is not as strong as it was in my day, it has been diluted in recent years. It’s still hugely important and should not be allowed to disappear.”
Aongus is pleased to see more women joining the surgical training programmes in all disciplines.“In my experience they are very bright, hugely committed and hard working, they are very much part of the future of surgery and the College needs to help and support them in every way possible.”
Now that they have a little more free time, Aongus and Eileen, who retired a few years ago, enjoy walking, music and playing the odd round of golf. They travel often to visit their sons and their families – Michael is a solicitor in Dublin and has three children, and Conor works in AI in New York and has two children.
“I could not have had the career I have had without the support of Eileen, who worked part-time, and my children, siblings and mentors. We adore our sons, daughters-in-law and grandchildren and our life is all about them now. I wake up every day thinking how lucky I have been and I am very grateful. I have no regrets and would do everything exactly the same way again. I feel very privileged to be a surgeon.” ■
RCSI’s community of Fellows and Members is truly international with representation in 74 countries worldwide. Outside of Ireland, Malaysia features in the top three countries of practice for RCSI Fellows and Members. Professor Premnath Nagalingam FRCSI, former Dean and Head of Surgery at the RCSI + UCD Malaysia Campus (RUMC) in Penang, shares his thoughts on some of the hot topics facing surgeons practicing in Malaysia
believe that Malaysia’s healthcare system is one of the best, if not the best in the world, due to its equitable nature. e State provides universal healthcare for all citizens and legal residents, ensuring high levels of accessibility to quality care.
However, no healthcare system is without its challenges and the ipside of universal healthcare is the demand on the public sector, which has led to a gradual growth in private healthcare. From a surgical perspective, the movement of specialists from the public to private sectors has been a topic of discussion for a number of years. ere has been a discernible trend of surgeons, who are ten or more years quali ed, moving into the private sphere, which has higher pay and better working hours. As a result, the public hospitals are increasingly understa ed, and patient care is somewhat negatively impacted.

“No system is perfect, and the imperfections are often complex and multifactorial.”



A number of years ago, the government announced that senior surgeons working in public hospitals could undertake one day of private practice a week. While it sounded good in theory, I think it has done little to address the issues simply because it is impractical for a surgeon to only see certain patients once a week. My personal belief is that, in time, we will see a better balance restored and this may in part be due to market factors such as the growing demand for private insurance and associated increases in insurance premiums. Whether the market drives a better equilibrium will remain to be seen.
Demand is also an issue when it comes to specialist surgical training. e current practice is for those pursuing specialist training to travel abroad with nancial support from the State for a year, two years or indeed for the entirety of their training. ere is o en talk of increasing the number of training positions within Malaysia. My personal opinion is that it is bene cial for individuals and for our system overall. Travel broadens the mind. e opportunity to train in the UK, India, Australia or China provides exposure to di erent cultures, di erent communication styles, di erent ways of approaching surgery. Our surgical community bene ts greatly from those who return from training abroad with di erent knowledge and skillsets.
RCSI is taking a leading role in addressing another area where demand outweighs supply, namely through the delivery of surgical skills courses and the MRCS Part A and Part B exams. I have witnessed the growth in candidates sitting the exams in Penang and have been closely involved in the expansion and establishment of a second exam centre in Sabah, which is in East Malaysia. Over the years, I have met individuals who have travelled from Australia, Singapore, Brunei, New Zealand, Pakistan, Bangladesh, Sudan, India and the Middle East to participate in the courses or sit the exams. It is a testament to the international regard with which the MRCS examinations are held. ere is now a signi cant cohort of surgeons in Malaysia who take pride in their MRCSI and FRCSI postnominals and I believe there is great potential to build on RCSI’s excellent reputation, possibly putting arrangements in place to provide advanced surgical training, or replicating the courses and programmes being delivered in Dublin.
Surgery in Malaysia has its own unique challenges. However, in common with healthcare globally, the reality is that no system is perfect, and the imperfections are o en complex and multi-factorial. Solutions take time and patience while new challenges will always appear on the horizon. What I remain con dent of is the quality and calibre of the teaching, training and assessment of our surgeons here in Malaysia – the future is de nitely bright. ■
Consultant Trauma and Orthopaedic Surgeon at the Mater, Mr Keith Synnott FRCSI is National Clinical Lead for Trauma Services for Ireland. A committed humanitarian, he has worked in Haiti and across Africa, and teaches trauma team management and leadership skills in war-stricken Ukraine
A er completing the BST in 1997 and HST in 2003, Keith Synnott went on fellowship to the Hospital for Special Surgery in New York. In 2004 he was appointed Consultant Trauma and Orthopaedic Surgeon with a special interest in spine, and particularly spine trauma, in the Mater Misericordiae University Hospital in Dublin. Currently he spends half his time on clinical work in the National Spinal Injuries Unit and Major Trauma Centre at the Mater, and half as the National Clinical Lead for Trauma Services for Ireland with the responsibility for leading out on the implementation of the Trauma Strategy.
always had an interest in doing humanitarian work abroad, as do many people, but it’s more di cult to get into than you might imagine. For example, if you want to work with Médecins Sans Frontières you have to commit to one or even two years and the paperwork is quite onerous. In 2006, I was doing an ABC travelling fellowship in America, and in an airport bookshop a book caught my eye because it had an aeroplane on the cover and mentioned Africa, two things I was interested in. e book was by Scott Gri n, a Canadian businessman who ew his Cessna 172, the same aeroplane I y, from Toronto to Nairobi so he could work as a business consultant with AMREF, the charity which runs the Flying Doctors of East Africa.
I did some research and learned that AMREF ran a visiting physicians programme, so you could volunteer to spend a month working with them. ey have a doctor and a nurse on every mission, and if they have an overseas volunteer, it saves them paying a local. So, in 2008, I took a month’s leave of absence. e work in Nairobi involved pre-hospital care, critical care and transfers.
What they really needed was an anaesthetist or critical care doctor, but there wasn’t one available so they got me instead. A lot of what I did was straightforward, but sometimes I was out of my depth, so it was a bit uncomfortable. But it was interesting. On the one hand, the Flying Doctors did work for overseas insurance companies and tourists, so you might be sent to collect a tourist in Madagascar with chest pain, and bring them back to the private hospital in Nairobi. Or to collect an injured tourist in Ethiopia, and bring them back to Germany. On the other hand, was the work that funded the local missions, which might involve going to a rural bush hospital to collect someone injured in an industrial accident and bring them back to the public hospital in Nairobi.

My grandfather was a pilot in the RAF, and he flew in the Second World War. From him I have a sense of duty – if you’re able to do stuff, you have to do stuff.




While I was there, I met an orthopaedic surgeon based in Eldoret, in the east of Kenya, which is where all the runners do all their training. He told me they needed training in joint replacements, so we partnered with a company here in Ireland called PEI, and they agreed to pay for a mission, and to cover the cost of the surgeons, the instruments, and the implants. In 2010, I went with fellow surgeons Gerry McCoy and Fintan Doyle and we spent a couple of weeks doing clinics, identifying patients, performing hip replacements and training the local surgeons.
Later in 2010, I went to Haiti about a week a er the earthquake. On the news it all looked very bad with buildings collapsing and amputations being done in terrible conditions. I spoke to Kieran Ryan at RCSI and mentioned that it looked like they needed orthopaedic and trauma people. I was wondering if there was anything we could do to help. A couple of days later I got a call from someone saying that Denis O’Brien was ying to Haiti to visit his business there and did I want to get on the plane and go with him?
e prospect was scary but I went with surgeons John O’Byrne and Michael O’Sullivan. ings were chaotic. We ended up going to a hospital about 30 or 40 miles outside Port au Prince to replace an American team who had been working there. We spent a week operating there, and when we came back we set up a charity to raise funds. Over the course of about six months, we sent a series of teams – surgeons, nurses and physios – to work in the hospital. Conditions were very challenging. e steriliser was used half the time for sterilising instruments, and half the time for cooking people’s food. e scrub area was like the parlour of your granny’s kitchen.









Subsequently we worked with Boston Group Partners in Health, who ran a number of hospitals in Haiti, and I went to Haiti ve or six times over the following couple of years. As the acute need abated, we went on di erent missions. Seamus Morris and I went to do some spine xations, as there were no spinal surgeons in the country.
Generally, we stayed in the hospital compounds which had armed guards but the security situation got so bad in 2019 we had to stop going. It was chaotic and I o en felt in personal danger driving to the airport in a van, as you could get hijacked.
I got involved in Ukraine through my work as an instructor on the European Trauma Course (ETC), which is designed to teach trauma team leadership skills and trauma team management. e way in which the health services are organised in Ukraine is quite di erent to Ireland. Traditionally, they did not have emergency rooms, resuscitation bays and major trauma centres. Following the outbreak of the war, the Ministry for Health decided they wanted to reorganise the way in which healthcare was delivered with a particular focus on trauma, and emergency department trauma team response. ey approached the UN and WHO for help in identifying the best training, and they recommended the ETC. en the ETC organisation was seeking instructors to go to Ukraine. e way the course works is that you deliver the course and the instructors identify people who would make good instructors, and they then do three courses as a trainee instructor before they are quali ed to instruct themselves. e plan was to go out to Ukraine to run a course, identify potential Ukrainian instructors, and then run three more courses.
It was a ve-week mission to do all of that. But the UN has a rule that if you are ‘in country’ for more than a week, you need to do speci c threat training in terms of what to do if you are hijacked or in a mine eld etc. So we ran the course, then we did the UN threat training for a week, and then we ran three



courses. By the time we le , we had trained twelve full instructors in Ukraine. It was very worthwhile. In Haiti, I had done missions where I went and operated on the ground whereas this was more about training people to train. e ETC is not just about how to stop somebody bleeding to death, it incorporates teamwork, interactions and human factors. In a post-Soviet society, things can be very hierarchical and the ETC is not like that at all. e feedback we got from the locals was excellent, with senior surgeons noting they now felt they could listen to their juniors, and juniors saying they felt they could challenge their seniors and work better as a team. In Ukraine, we weren’t on the frontline and we weren’t operating, it was all teaching local Ukrainian doctors how to run trauma teams. At time of going to press, Дмитро Мясніков and Анна Анісімова were due to instruct on the ETC course in Dublin in late November.
In Ukraine we were in Ternopil in West Central Ukraine, which is very safe. e hospital has a big SIM centre, which is why it was chosen. We delivered another three courses in November in Kyiv. You don’t really know what it’s going to be like until you get there, and obviously you see on the news that there are a lot of bad things going on. I was apprehensive initially. e UN makes you do a lot of online training in advance so you are prepared for the worst. But Ternopil was only ever hit by a missile once, and that was when Ukraine won the Eurovision, and the person who won it was from Ternopil. In Lviv and Kyiv we spent a few nights in shelters because there were missile strikes.
My work at the moment is half-clinical, and half-administrative. A lot of my HSE Clinical Lead work is done remotely, so I am able to continue that while I am in Ukraine. e Mater gave me and Seamus Morris humanitarian leave, and our colleagues picked up the slack. ey were all very good. Without them, we couldn’t have gone. e hospital was very accommodating and so was the HSE.
I have a history of doing these mad things and disappearing o to funny places, so in terms of my family, it wasn’t unexpected. My wife and family were very supportive. My kids are all in college now, so it’s a bit di erent to when they were small. I’m fundamentally a chicken so when it came to going to Haiti I was looking for excuses not to go, but I felt that I had to go. My grandfather was a pilot in the RAF, and he ew in the Second World War. From him I have a sense of duty – if you’re able to do stu , you have to do stu . I suppose it sounds da , but that’s the way I’ve always thought of these things. People o en say to you, “Oh, I’d love to be able to do something to help.” And I was in a lucky situation, where I was able to do something, so I couldn’t really say no.” ■
Consultant General and Colorectal Surgeon at Galway University Hospital, Ms Emmeline Nugent
FRCSI ponders work, career, happiness and the good things in life

Outside of work, when and where are you happiest?
At big family gatherings where there is plenty of good food, company and wine.
What is your ideal evening?
Baking with my daughter, Isabel. She is most definitely the head chef and I am the sous-chef! Our repertoire is limited but the best part is enjoying the tasty treats with a large mug of tea. If you could research and write a book on any subject, what would it be?
Archaeology has always fascinated me. In particular, prehistoric monuments such as Newgrange. The feats of engineering, geometry and astronomy associated with this era are amazing.
What relaxes you most?
Cleaning. Nothing like a bit of elbow grease to make you feel better.
What is your greatest fear?
Heights – I would never in a million years do a bungee jump or a sky dive.
When did you decide you wanted to become a surgeon?
During final med. I did a vascular rotation with the late Professor Sean Tierney and Martin Feeley in Tallaght Hospital and loved the technical surgical aspects that I observed. It was clear also that they both had a passion for their craft.
Had you decided not to become a surgeon, what other career might you have chosen?
A professional ballet dancer – it nearly happened when I was in my early teens but I just wasn’t good enough.
What do newly appointed surgeons need?
Clearly the practical basics of infrastructure to do the job are what are needed as a minimum. Aside from this, I believe a support network is important as you become established in your new role. That is why I am delighted to be involved in the new Early Career Surgeons Network that has recently been launched by our president, Professor Deborah McNamara. I believe that it is a great initiative and hopefully newly appointed surgeons will find it helpful.
Were there mentors or sponsors who supported you on your career journey?
Absolutely! Too many to mention! I think that the balance between mentorship and sponsorship changes at various significant times in one’s career. Certainly some of the opportunities that I have been offered since being appointed wouldn’t have been feasible without serious sponsorship. I expect that I will continue to need both as time goes on and in a similar manner I hope to pay it forward!
What has been your proudest moment thus far in your career?
Seeing trainees that I worked with previously get appointed their job of choice and watching their stars rise.
How does a surgeon in 2024 cope with pressure?
There was a recent BMJ opinion piece titled “Medicine is difficult – there are no shortcuts” (BMJ 2024;387:q2163). Its focus was primarily on medical training and the importance of getting this right. However I think its central message is key –medicine as a whole is becoming more difficult to practice for many reasons. And it is probably going
“I think having a network of likeminded peers to bounce difficult scenarios off is helpful.”
to become more challenging in the future. I think having a network of like-minded peers to bounce difficult scenarios off is helpful. Aside from that, for me, regular exercise helps.
Do you believe that a psychological perspective in the surgeon's toolkit helps to improve the surgeon-patient relationship?
Absolutely. My mum, who does not have a medical background, has often reminded me how we meet patients and their families at their most vulnerable. I believe it is vital to always reflect on this and to remember that as surgeons we are in a position of privilege when looking after people at their most vulnerable.
Do you have a mantra to live by?
To borrow a quote from the eminent Patricia Numann, MD – “Laugh at closed doors”. What do you consider your greatest achievement?
Meeting my lovely husband. What living world figure do you admire?
Michelle Obama – she is an inspirational role model: “Be focused. Be determined. Be hopeful. Be empowered.”
What is your favourite memory?
Lots of favourite childhood memories but most treasured are those summers spent on my grandparents farm in Cavan – walking the fields counting cattle with my grandad and picking gooseberries and blackcurrants for my granny to make jam. I can still taste the blackcurrant jelly jam slathered on homemade soda bread with salty
butter. I had three always-hungry brothers so she had to be well stocked up in advance of our arrival – she could never seem to bake fast enough for us! What is your greatest extravagance?
The odd pair of designer shoes or handbag. I think every woman has a corner of her wardrobe where fancy items magically appear now and again. Your favourite writer?
Probably too many to pick from but one of my favourites has to be Edith Wharton, in particular The House of Mirth
If you could invite any historical figure to dinner, who would it be?
It would have to be someone like F. Scott Fitzgerald partly in the hope that he would bring with him some friends like Ernest Hemingway, James Joyce, Picasso. I’m not sure what my contribution would be but their company would certainly make for an interesting evening.
Which talent would you most like to have? Gardening – the main thing I seem to grow in abundance are weeds.
What is the best advice you have ever been given?
The importance of keeping things in perspective. I remember fondly a surgical trainer telling me once how important it was to remember that no matter how rough or tough your working day was that you always got to go home to something better. Certainly having kids has cemented this view – I get a great welcome coming through the door... most of the time.
How do you have fun?
Enjoying the simplest of outdoor activities with my girls. We especially love putting on wellies and grabbing a bucket and spade and digging holes in the sand and splashing in the sea, in spite of the west coast rain.
Name one virtue all surgeons ought to have.
A sound understanding of your limitations. Name one vice no surgeon should have. Impatience.
Name three things that you would like to have in your future.
Good health, plenty of laughter and time to spend with family. ■

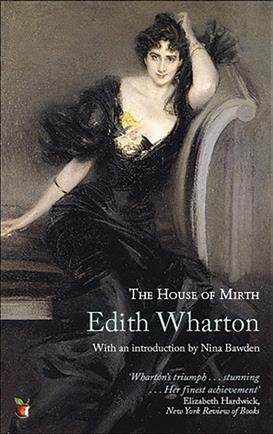



PENANG CONFERRING In June, RCSI President Professor Deborah McNamara travelled to Penang, Malaysia to recognise and celebrate the achievements of 38 newly conferred Members of RCSI and one recipient of an RCSI Fellowship at the RCSI Fellows, Members, and Diplomates Conferring.













PRESIDENT’S RECEPTION Prior to the conferring of 819 healthcare professionals at RCSI’s St Stephen’s Green campus in July, Professor Deborah McNamara, President of RCSI, hosted a reception in RCSI’s Board Room for the newest Fellows, their family members – including some very young guests – and friends. Professor McNamara emphasised RCSI’s commitment to building a supportive community for early career Fellows and congratulated them on this momentous achievement on their career journey.
and family.









CONFERRING CEREMONY The awards conferred at RSCI in July included surgical Fellowship and Memberships of RCSI, Fellowship in Urgent Care Medicine as well as Fellowship and Memberships of the Faculties of Radiologists and Radiation Oncologists, Dentistry and Sports and Exercise Medicine. Also awarded were Fellowship and Memberships of the Faculties of Dentistry, Fellowship and Memberships in General Dental Surgery and Diplomas in Primary Care Dentistry. The college also conferred Honorary Fellowships on Plastic Surgeon Dr Michael T. Longaker of Stanford Medicine, and General and Vascular Surgeon Professor David Nott, who volunteers to work in war zones.


























Fellows, Members and Affiliate Members of RCSI are warmly invited to mark your calendars for the year ahead and be sure to register for the following events.
RCSI Fellows, Members and Diplomates Conferring Ceremony, Dublin
Monday 9 December 2024 | RCSI Dublin | Free for eligible candidates.
RCSI President’s Reception for newly conferred Fellows of RCSI and their guests Monday 9 December 2024 | RCSI Dublin | Free for eligible candidates.
RCSI Charter Meeting
Tuesday 4 February 2025 – Saturday 8 February | RCSI Dublin | Paid event, registration not yet open.
Fellows and Members Family Event at RCSI Charter Meeting
Saturday 8 February | RCSI Dublin | Full details TBC.
RCSI Alumni, Fellows and Members London Reception Friday 28 February 2025 | Royal Society of Medicine | Free event for RCSI Alumni, Fellows and Members.
RCSI Alumni, Fellows and Members Lunchtime Talk
Friday 21 March 2025 | RCSI Dublin | Free event for RCSI Alumni, Fellows and Members.
RCSI Fellows and Members Social Mixer March 2025 | RCSI Dublin | Paid event, registration not yet open.
RCSI Alumni, Fellows and Members Kuala Lumpur Event
Friday 13 June 2025 | Kuala Lumpur | Full details TBC.
RCSI Alumni, Fellows and Members Penang Event
Saturday 14 June 2025 | Penang | Full details TBC.
RCSI Fellows and Members Conferring Ceremony, Penang Sunday 15 June 2025 | E&O Hotel, Penang | Free for eligible candidates.
RCSI Fellows, Members and Diplomates Conferring Ceremony, Dublin
Monday 7 July 2025 | RCSI Dublin | Free for eligible candidates.
RCSI President’s Reception for newly conferred Fellows of RCSI and their guests
Monday 7 July 2025 | RCSI Dublin | Free for eligible candidates.
RCSI Alumni, Fellows and Members Lunchtime Talk
Thursday 10 July 2025 | RCSI Dublin | Free event for RCSI Alumni, Fellows and Members.
RCSI Alumni Gathering 2025
Thursday 14 – Saturday 16 August 2025 | RCSI Dublin | Paid event for RCSI Alumni, by invitation only.
RCSI Alumni, Fellows and Members Lunchtime Talk
Thursday 11 September 2025 | RCSI Dublin | Free event for RCSI Alumni, Fellows and Members.
Chapter of Fellows Reception, American College of Surgeons (ACS) Clinical Congress
Saturday 4 October 2025 | Chicago, IL, USA | Open to RCSI Fellows and Members, cost associated.
RCSI Alumni, Fellows and Members Lunchtime Talk
Thursday 30 October 2025 | RCSI Dublin | Free event for RCSI Alumni, Fellows and Members.
RCSI Millin Meeting
Friday 7 November 2025 | RCSI Dublin | Paid event, registration not yet open.
RCSI Fellows, Members and Affiliate Members in Good Standing receive discounted attendance rates to RCSI events, or free attendance in some instances, as a benefit. You will be invited to each event and notified when registration opens by email. If you have any queries please contact fellows@rcsi.ie. | Please contact fellows@rcsi.ie to learn more. If you would like to arrange your own on-site meeting, those considered in Good Standing are also entitled to a discounted room booking rate. To avail of this, please contact us.
The Royal College of Surgeons is currently recruiting for clinical, basic, and lay examiners in Ireland, Bahrain, Malaysia, Egypt and the United Arab Emirates to examine in upcoming MRCS B OSCE examinations.
Members of the RCSI Court of Examiners are kept informed of developments and international best practice in clinical assessment at the Annual Court of Examiners Meeting and are awarded Professional Competence Scheme (PCS) credits for examining and attending our annual meeting. Members also receive a complimentary member’s pack with RCSI Court of Examiners merchandise.
If you’re interested in becoming an MRCS examiner with RCSI, please visit rcsi.com/coe, register your interest by scanning the QR Code or email courtofexaminers@rcsi.ie

Register your interest today