scheie vision












celebrating
150 years





































Caring for Community and Country
Healthcare Heroes, Then and Now
The Role of UPenn Ophthalmology in the World Wars

Scheie and the British Royal Family Pioneering Advances in Science and Education
Looking Back: Early Inventions and Research
From my days as a medical student at the University of Pennsylvania (UPenn), and throughout the ensuing two decades, the Scheie Eye Institute and the Department of Ophthalmology at UPenn have been synonymous to me with excellence in research, clinical practice, and education. As you all know, without question, this continues to be the case. It is therefore an incredible and humbling honor for me to return to Scheie as the new Chair of the Department of Ophthalmology.
In just the very short time that I have been here, I have witnessed firsthand the delivery of outstanding and compassionate clinical care, the promise of groundbreaking and innovative research with translational impact for our patients, and the focus on first-rate education for learners at all stages, including medical students, residents, and fellows. All of this is possible because of the people; the dedicated faculty, trainees, and staff are a cohesive community that set this Department apart from all others.
Without question, the history of the Department and of the Scheie Eye Institute tells the story of some of the nation’s greatest achievements in ophthalmology, which you can read about in this publication. Under the stewardship of the former Chairs and Directors, the Department rose to and

Managing Editor: Rebecca Salowe | Research and Writing: Isabel Di Rosa, Kristen Mulvihill, Rebecca Salowe, Marquis Vaughn, Selam Zenebe-Gete Faculty Leads: Joan O’Brien, MD, Charles Nichols, MD | Faculty Editor: Benjamin Kim, MD | Chairman: Bennie Jeng, MD Design: Caren Goldstein | Printing: Quaker Printing Cover images courtesy of University of Pennsylvania Archives, Brian Holmes, Rui Ochoa (Champalimaud Foundation), Peggy Peterson, and Scott Spitzer
has held its place amongst the upper echelon of ophthalmologic institutions across the country. So where do we go from here?
As we enter into the second 50 years of the Scheie Eye Institute and approach the 150th anniversary of the Department, I see an unparalleled opportunity to build upon the foundation that has been established to further our mission. My vision is to create a supportive and nurturing culture of inclusiveness and diversity that will foster the successes of each member in their chosen areas of interest. This will not only help each individual to achieve their personal goals, but will also elevate the stature of the entire department to one that is recognized as a top program in every domain. With the support of colleagues and friends such as yourself, I have no doubt that we will see this happen, and I am pleased that you will be able to see us through in this exciting journey!
With best regards,

Established in 1874, the Department of Ophthalmology at the University of Pennsylvania (UPenn) proudly celebrates 150 years of excellence. The Scheie Eye Institute, opened in 1972, has remained at the forefront of innovation over the last 50 years, transforming the way that patient care, research, education, and community service are conducted. We are thrilled to present this special anniversary edition magazine, showcasing extraordinary moments from our past and remembering the inspiring individuals who made the last 150 years possible.
The Department of Ophthalmology has experienced immense change and growth over the last 150 years. Beginning with our original location in the basement of the Hospital of the University of Pennsylvania, we now offer eye care in six clinical facilities across Philadelphia and Delaware County. Our faculty currently consists of 68 brilliant individuals, including five members of the Academy of Master Clinicians and four UPenn Advisory Deans, representing 20% of our clinical faculty. The Department now offers every subspecialty of ophthalmic care and sees more than 130,000 patient visits each year.
With respect to our research mission, the Department has become a top recipient of National Eye Institute funding nationwide for the past five years. Our faculty consistently conduct transformative research, publishing results in high-impact journals each year. The Department remains a leader in research impact, with our H-index steadily increasing each year. We have also developed strong partnerships with foundations, non-profits, and industry, and have raised over $43 million in philanthropy since 2010.
Similarly, our educational mission has progressed over the years, increasing from two residents in 1937 to 15 residents in 2022. Our residency program receives more than 600 applications for five positions each year, and consistently matches with diverse, talented, and compassionate individuals. Surgical volumes for residents have increased by 88% since 2010 and the number of grants/trials per alumnus ranks in the top 1% of programs across the country. Our third-year residents consistently secure top choice fellowships at outstanding institutions.
Over the years, our faculty, staff, and trainees remain committed to making an impact through service initiatives in the community. Programs such as Penn Sight Savers and Puentes de Salud, staffed by volunteer physicians, residents, and medical students, provide comprehensive ophthalmic care to patients who are often uninsured and undocumented. Several times a year, our faculty and staff organize screening events across Philadelphia, providing free health and eye screenings. In the past decade, our faculty have traveled to more than 30 countries to provide eye care to desperately at-risk and underserved populations internationally.
We hope you enjoy reading through these pages celebrating the milestones and individuals who have made the Department of Ophthalmology and the Scheie Eye Institute a truly remarkable place.

Sincerely,
Bennie H. Jeng, MD Harold G. Scheie Chair and Professor Chairman, Department of Ophthalmology Director, Scheie Eye InstituteJoan O’Brien, MD Director, Penn Medicine Center for Ophthalmic Genetics in Complex Diseases Harold G. Scheie-Nina C. Mackall Professor of Ophthalmology Inducted Member, National Academy of Medicine
Charles W. Nichols, MD Associate Professor of Ophthalmology Chief of Ophthalmology, Hospital of the University of Pennsylvania
In 2024, the Department of Ophthalmology at the University of Pennsylvania (UPenn) will celebrate the 150th Anniversary of its founding in 1874. This milestone is the culmination of numerous achievements and contributions, many of which are commemorated below.
1871
1765
The Trustees of the College of Philadelphia (later called the University of Pennsylvania) establish the first medical school in the American colonies.


1784
Benjamin Franklin invents bifocal glasses.
1805
Philip Syng Physick, MD, becomes Penn’s first professor of surgery, separating surgery from anatomy and midwifery. He develops a novel method to extract cataracts.
Construction begins for the Hospital of the University of Pennsylvania (HUP), the first university-owned hospital in the United States built expressly for the purpose of teaching.
1787
The College of Physicians of Philadelphia is founded.
1874

The Department of Ophthalmology at HUP is founded. William F. Norris, MD is appointed the first Professor of Ophthalmology
1861-1865
The Civil War divides the medical school. Approximately 660 Penn medical alumni serve as Union army surgeons and 550 as Confederate army surgeons.

1751
Pennsylvania Hospital is founded by Benjamin Franklin and Dr. Thomas Bond.


Penn medical faculty and alumni support American troops fighting for independence during the Revolutionary War. John Morgan, founder of Penn’s medical school, serves as Director-General of the Continental Army’s hospital.
1855
Children’s Hospital of Philadelphia is founded by Francis West Lewis.

1897
The Agnew Wing of the University Hospital, which provides eye wards for men and women, is constructed.
More than 200 surgical procedures are performed in the eye clinic, which is more than any other department at the University Hospital.
Dr. de Schweinitz co-founds the American Board of Ophthalmology.
The Graduate School of Medicine is organized, which includes a program offering specialized training in ophthalmology.
The United States enters World War I. The Civilian Base Hospital No. 20 in France is staffed by Penn physicians and medical students, with a special ward for patients with ophthalmic injuries.


Dr. de Schweinitz is part of the medical care team that treats President Woodrow Wilson after a stroke.
Thomas B. Holloway, MD, becomes the third Chairman of Ophthalmology. A slit lamp microscope is installed in the eye dispensary and a laboratory of perimetry is established. Dr. Holloway advocates for greater endowment of ophthalmology departments and becomes one of the first ophthalmologists to use films for scientific and educational purposes.

The annual de Schweinitz Lecture and Dinner is founded as a memorial to Dr. de Schweinitz.


The influenza pandemic spreads through Philadelphia. The Ophthalmology Department, then located at HUP, refocuses effort on treating these patients.
George E. de Schweinitz, MD, becomes the second Chairman of the Department of Ophthalmology. He creates an operating room for eye surgery, renovates the eye dispensary and ophthalmic pathology laboratory, and forges important collaborations with other departments
Francis Heed Adler, MD, becomes the fourth Chairman of Ophthalmology. He moves and expands the clinic and eye ward, promotes innovative clinical research, and improves the training of eye specialists. Dr. Adler is later named the first William F. Norris and George E. de Schweinitz Professor of Ophthalmology.
The first residency program at Penn is established.
Harold G. Scheie, MD, becomes the first ophthalmology resident to complete the full three-year program.
The United States enters World War II. Penn physicians, including ophthalmologists, organize and run the US Army 20th General Hospital in Burma, India.

The Scheie Eye Institute is founded by Dr. Scheie at the Presbyterian Medical Center in Philadelphia.
Stuart Fine, MD, becomes the seventh Chairman of Ophthalmology. Dr. Fine expands the faculty threefold, increases the number of endowed chairs from three to eight, and sees considerable growth in the clinical practice and educational programs.
The Veterans Administration Hospital of Philadelphia opens, with the UPenn Ophthalmology Department designated as its sole ophthalmic provider.
The first female resident is appointed at Scheie.

Dr. Scheie becomes the fifth Chairman of Ophthalmology. He creates an elective five-year training program that includes two research years, pioneers glaucoma research and treatments, and develops affiliations with the new VA Hospital and Children’s Hospital of Philadelphia. He begins to raise funds for a new eye hospital at UPenn.
The Penn Vision Research Center is established.
Maureen Maguire, PhD, establishes the Center for Preventive Ophthalmology and Biostatistics (CPOB). The F.M. Kirby Center for Molecular Ophthalmology is established with a generous gift from the F.M. Kirby Foundation.
Alexander Brucker, MD, founds the scientific journal RETINA, which has become the world’s leading journal for retinal and vitreous diseases.
Myron Yanoff, MD, becomes the sixth Chairman of Ophthalmology. Dr. Yanoff establishes prosperous retina, cornea, and glaucoma services and recruits many skilled ophthalmologists. James Katowitz, MD, establishes a plastic surgery service.

The Center for Hereditary Retinal Degenerations is established by Samuel Jacobson, MD, PhD.



Presbyterian Medical Center becomes part of the University of Pennsylvania Health System.
The Ruth and Raymond Perelman Center for Advanced Medicine opens.


A formal, reciprocal agreement is reached with the Aravind Eye Hospital in Southern India. Scheie residents may visit Aravind during their elective time in the third year for four weeks.

2022
Bennie H. Jeng, MD is named the ninth Chairman of Ophthalmology.

2022
The Penn Medicine Center for Ophthalmic Genetics in Complex Diseases opens, with Chairman Emeritus Joan O’Brien, MD, as the Inaugural Director.

Joan M. O’Brien, MD, becomes the eighth Chairman of Ophthalmology and first female Chair. She expands the number of subspecialities to 17, conducts groundbreaking research on the genetics of glaucoma in African Americans, and forges powerful industry collaborations. Under her direction, the Department consistently ranks as a top recipient of NEI funding nationwide.
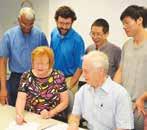
The first gene therapy for an inherited eye condition (Luxturna) is approved by the FDA. For this achievement, Drs. Jean Bennett, Samuel Jacobson, and Albert Maguire are awarded the 1 million euro Champalimaud Vision Award.

UPenn announces the creation of the Penn Center for Advanced Retinal and Ocular Therapeutics (CAROT), with Jean Bennett, MD, PhD and Albert Maguire, MD as co-directors.
Extensive renovations of the Scheie Eye Institute are completed.
Images courtesy of University of Pennsylvania Archives and Library of Congress.The Ophthalmology Department at the University of Pennsylvania (UPenn) was officially established in 1874, but its story began long before then. Below, we highlight the leaders, both before and after the founding of the Department, who pioneered advancements in clinical care, research, and education. The leadership of these remarkable individuals helped the Department grow into the renowned, internationally recognized institution it is today.
Key Contributors to the Birth of the Ophthalmology Department from 1700s-1874
Beginning in the early 1700s, innovations in ocular treatment and surgery, research, and teaching laid the groundwork for the founding of the Department. Below, we highlight several key individuals who pioneered these changes.
Benjamin Franklin (1706-1790)
Benjamin Franklin was a printer, inventor, and founding father of the United States. He is considered the primary founder and shaper of the University of Pennsylvania. Among his many inventions, he is credited with developing the first pair of bifocals in 1784.

Philip Syng Physick, MD (1768-1837)
Widely considered the “Father of American Ophthalmology,” Dr. Physick served as a Professor of Surgery (1805-1819) and Professor of Anatomy (1819-1831) at UPenn. He pioneered a number of surgical innovations, including the development of a novel method to extract cataracts. When the yellow fever epidemic struck Philadelphia in 1793, he was one of the few physicians to remain in the city and treat fever victims.
As the successor to Dr. Physick, Dr. Gibson served as the Professor of Surgery at UPenn for 36 years. He was considered the leading surgeon in Philadelphia in the earlyto mid-1800s. Dr. Gibson was uniquely skilled in eye surgery and became the first surgeon to operate for strabismus. He wrote the


Dr. Horner was a Professor of Anatomy at UPenn and the Dean of the Medical School from 1822 to 1852. He is credited with discovering and dissecting the tensor tarsi muscle (now called Horner’s Muscle), and was the first to explain how tears pass from the conjunctival sac to the nose.
 popular medical textbook The Institutes and Practice of Surgery, which included several detailed sections on eye diseases and treatments.
popular medical textbook The Institutes and Practice of Surgery, which included several detailed sections on eye diseases and treatments.
A Professor of Surgery at UPenn, Dr. Agnew was well-known for his teaching ability and his ambidextrous surgical skill. He wrote several volumes of The Principles and Practice of Surgery, which included sections on the eye. Dr. Agnew is the subject of the famous painting The Agnew Clinic, which was commissioned by students upon his retirement. He is often considered the last of the great general surgeon-ophthalmologists in Pennsylvania, ending an era when general surgeons operated on the eye.
Over the last 150 years, nine Chairmen of the Department of Ophthalmology committed their careers to fostering the growth of faculty, staff, patients, trainees, and alumni. Below, we take you on a journey through the Department, beginning with the first appointed chair, William F. Norris, MD, all the way to the current chair of the Department, Bennie H. Jeng, MD.

In 1870, William F. Norris, MD and George C. Strawbridge, MD were appointed to establish an eye and ear clinic at UPenn. Located at Ninth and Chestnut Street, the Eye Dispensary opened on October 6, 1870. In 1874, Dr. Norris became the first Professor of Diseases of the Eye at UPenn—only the fourth such appointment in the United States. During his time as Chairman, Dr. Norris was committed to teaching and research. He gave weekly lectures on ophthalmology to interested students in an anatomical amphitheater, which became a formal part of the curriculum in 1879. Dr. Norris contributed vastly to various ophthalmology texts, authoring one of the first nationally recognized textbooks in ophthalmology. He also pioneered the usage of photography for medical and surgical cases. Dr. Norris played an instrumental role in the founding of the Hospital of the University of Pennsylvania, one of the first university-owned hospitals that was dedicated to medical student education. During the Civil War, Dr. Norris served with distinction as a surgeon for the U.S. Army.

George E. de Schweinitz

succeeded Dr. Norris as Chairman in 1902. Under his leadership, the eye dispensary was remodeled and expanded, and both an ophthalmic pathology lab and an operating room for ophthalmological procedures were constructed. By 1924, the ophthalmology clinic was the third largest clinic at UPenn, behind only the medical and surgical clinics. Dr. de Schweinitz forged important collaborations with other departments for consultations and led lab projects in newly acquired lab space. His book Diseases of the Eye became the official handbook for the students in the clinic. To date, Dr. de Schweinitz is the first and only ophthalmologist to serve as President of the American Medical Association. Over the years, Dr. de Schweinitz sustained a large and impressive practice, with President Woodrow Wilson among his patients. His efforts helped to establish the nation’s first certifying board—the American Board of Ophthalmic Examination, now named the American Board of Ophthalmology. During World War I, Dr. de Schweinitz was appointed to the Council of Defense as Major and became Brigadier General in the Medical Reserve Corps in 1922.
The legacies of both Drs. Norris and de Schweinitz have been honored by the Department through the William F. Norris and George E. de Schweinitz Professorship of Ophthalmology.
William F. Norris, MD George E. de Schweinitz, MD David Hayes Agnew, MDThomas B. Holloway, MD followed Dr. de Schweinitz as Chairman of the Department in 1924. Dr. Holloway was sincerely committed to teaching, having previously led the development of an ophthalmology training program in the Graduate School of Medicine in 1916. He also contributed greatly to clinical studies in the field of ophthalmology and brought various clinical instruments and upgrades to the Department. He introduced a slit lamp in the eye dispensary, as well as a laboratory of perimetry, used for visual field testing. Dr. Holloway was also among the first ophthalmologists to use films for scientific and educational purposes.

Francis Heed Adler, MD succeeded Dr. Holloway as Chairman in 1937, a time when ophthalmology residency programs were emerging across the nation. In 1937, the Department introduced the first residency program at UPenn. Dr. Adler prided himself most on improving the training of eye specialists. Furthermore, he promoted innovative clinical research and advocated for expanding the ophthalmology clinic to provide necessary facilities for resident training. Dr. Adler received a generous gift to rebuild the eye wards and expand patient occupancy. Under his leadership, the eye clinic was moved to a more spacious area. In 1945, Dr. Adler was named the inaugural William F. Norris and George E. de Schweinitz Professor of Ophthalmology.
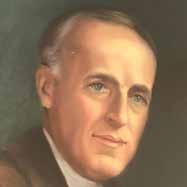
Among one of the first residents when the residency program was introduced, Harold G. Scheie, MD experienced a long history with the Department. Before becoming Chairman, he was the first resident to finish the full three-year program in ophthalmology at UPenn. During World War II, Dr. Scheie served active duty as a captain in the Army Medical Corps and was Chief of Ophthalmology at the 20th General Hospital in India. When Dr. Scheie became Chairman in 1960, the Department’s residency program excelled. He established an elective five-year training program to provide residents with research and basic science experience. Clinical research also flourished under his leadership, as Dr. Scheie pioneered novel glaucoma research and treatment methods. Dr. Scheie led the fundraising efforts to build a new $12.5 million eye hospital, opened in 1972 and named the Scheie Eye Institute. During his time as Chairman and beyond, Dr. Scheie maintained an international reputation and greatly contributed to literature. Even after he retired from active practice, Dr. Scheie remained involved in raising funds for the Institute’s endowments.

Myron Yanoff, MD succeeded Dr. Scheie and became the sixth Chairman in 1978. Among Dr. Yanoff’s many accomplishments as Chairman, he successfully promoted the growth of subspecialties within the Department. Dr. Yanoff established prosperous glaucoma, retina, corneal and external disease, oculoplastics, and comprehensive ophthalmology services. These subspecialties all aimed to provide innovative patient care and superior training to medical students and residents. Furthermore, Dr. Yanoff recruited many skilled ophthalmologists and promising trainees to Scheie during his time as Chairman.

Stuart L. Fine, MD
Stuart L. Fine, MD assumed the role of Chairman in 1991. Dr. Fine largely contributed to the fields of public health and epidemiology, namely establishing the Center for Preventive Ophthalmology, Biostatistics, and Epidemiology in 1994. Dr. Fine appointed Maureen Maguire, PhD, an internationally recognized researcher, as Director of the Center. The Center, now named the Center for Preventive Ophthalmology and Biostatistics, serves as the hub for coordinating multicenter studies. During his term as Chairman, Dr. Fine also established the F.M. Kirby Center for Molecular Ophthalmology. This Center aims to elucidate the mechanisms of blinding retinal diseases and to develop novel therapies for these diseases.
Joan M. O’Brien, MD
Joan M. O’Brien, MD joined the University of Pennsylvania in 2010 as the first female Chairman and Director of the Scheie Eye Institute. During her 12-year tenure, she led the expansion of the Department. The faculty grew from 24 to 68 individuals in all subspecialties, and the clinicians now see more than 130,000 patient visits per year. Under Dr. O’Brien’s leadership, the Department was continually a top five recipient of National Eye Institute funding, and the residency program consistently ranked in the top 5% nationwide for research output per alumnus. In 2014, Dr. O’Brien oversaw extensive renovations of the Scheie Eye Institute. In her 12 years as Chairman, she helped raise over $43M in philanthropy.

In addition to these contributions, Dr. O’Brien spearheaded the $17.9M Primary Open-Angle African American Glaucoma Genetics study. This study aims to find targeted treatments for glaucoma, which disproportionately affects the Black population, and has enrolled over 10,200 Black patients in Philadelphia. Dr. O’Brien has received numerous honors for her contributions to
ocular oncology and genetics, including induction into the National Academy of Medicine in 2013. Dr. O’Brien currently serves as the Inaugural Director of the Penn Medicine Center for Ophthalmic Genetics in Complex Diseases. This Center seeks to elucidate the genetics of diseases that overaffect African ancestry populations, with the long-term goal of developing personalized diagnostic and therapeutic strategies to address this unmet need.

Bennie H. Jeng, MD, current Chairman of the Department of Ophthalmology and Director of the Scheie Eye Institute, is a nationally recognized clinicianscientist and surgeon who specializes in cornea and external diseases. Before holding this position, Dr. Jeng served for nine years as Chairman of the Department of Ophthalmology and Visual Sciences at the University of Maryland School of Medicine. With a translational research interest in corneal wound healing and infectious keratitis, his more recent work in clinical trials includes serving as co-Chair of the NEI-funded Zoster Eye Disease Study. Dr. Jeng has a special interest in fostering the professional growth of young faculty members and trainees to become outstanding funded researchers and leaders in the field, and he has been very successful in this endeavor.
In his current role as Chairman, Dr. Jeng plans to continue his efforts in promoting the career development of the Scheie faculty and residents. He is also planning for a significant expansion of the basic and translational research enterprise, which will include increasing collaborative research with other groups on the UPenn campus. In addition, he is strategizing for a dramatic growth of the clinical enterprise, including further expansion into the suburbs to help provide better access for patients who live outside of the city. For the educational mission, Dr. Jeng looks forward to enhancing the existing outstanding programs in undergraduate and graduate medical education to provide the very best in ophthalmic education at UPenn. n
Albert, D. M., & Scheie, H. G. (1965). A history of ophthalmology at the University of Pennsylvania. Springfield, Illinois: Charles C. Thomas.
Frayer, W. C. (2002). An ophthalmic journey: 50 years at the University of Pennsylvania. William C. Frayer, M.D.
Note: Unless otherwise specified, headshots were retrieved from the University of Pennsylvania Archives.
 Stuart L. Fine, MD Courtesy of Dan M. Albert, MD
Joan M. O’Brien, MD
Courtesy of Peggy Peterson
Bennie H. Jeng, MD
Stuart L. Fine, MD Courtesy of Dan M. Albert, MD
Joan M. O’Brien, MD
Courtesy of Peggy Peterson
Bennie H. Jeng, MD
In 1874, the Hospital of the University of Pennsylvania opened, becoming the first teaching hospital in the nation. That same year, the Department of Ophthalmology was established. On February 3, William F. Norris, MD was appointed the first Professor of Diseases of the Eye at the University—only the fourth such appointment in the country.

The eye clinic was located in the lower level of the Hospital of the University of Pennsylvania (HUP), which was the original location of the Department of Ophthalmology. The first clinical records of the Department were found in leatherbound journals.


As the first Chairman of the Department, Dr. Norris was committed to research, contributing to many ophthalmology texts and initiating the study of ocular pathology within the Department. Dr. Norris became an expert in medical photography and greatly contributed to the rise of the usage of
the ophthalmoscope, an instrument used to observe the retina. During his time as Chairman, he also recruited distinguished faculty members to join the Department.
In 1897, construction of the Agnew Wing of the University Hospital was completed, providing additional eye wards for men and women. By 1901, more than 200 surgical procedures were performed in the eye clinic—more than any other department at the University Hospital at the time.
Following Dr. Norris’s unexpected death in 1901, George E. de Schweinitz, MD was selected as the second Chairman of the Department. Under Dr. de Schweinitz’s leadership, the ophthalmic pathology laboratory and the eye dispensary were renovated and expanded, tripling the number of patients seen. Additionally, an operating room for eye surgery was constructed in the Department.

At this time, no national standards existed for ophthalmic care. Dr. de Schweinitz, along with other leading ophthalmologists, set out to change this. In 1916, he helped to found the American Board of Ophthalmic Examination (later renamed the American Board of Ophthalmology), the nation’s first certifying board.


As the Department of Ophthalmology continued to advance, the
early 19th century brought global crises. In 1914, World War I began, a fatal conflict with lasting effects. In 1918, a deadly epidemic, known as “The Great Influenza,” spread rapidly across the globe. To read about how UPenn and the Department of Ophthalmology responded to these catastrophic events, turn to page 21, “Healthcare Heroes, Then and Now,” and page 25, “The Role of UPenn Ophthalmology in the World Wars.” n
Cataract knives used by William F. Norris, MD.

Reference
Albert, D. M., & Scheie, H. G.
Note: All images included in this article were taken from this text.
 (1965). A history of ophthalmology at the University of Pennsylvania. Springfield, Illinois: Charles C. Thomas.
Eye operating room (1907).
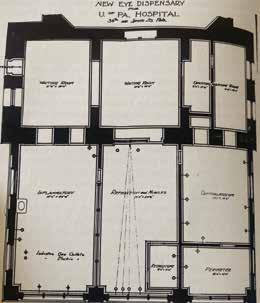
Plans for the new eye dispensary for the University of Pennsylvania Hospital (1903). Waiting room in remodeled clinic (1905).
(1965). A history of ophthalmology at the University of Pennsylvania. Springfield, Illinois: Charles C. Thomas.
Eye operating room (1907).
Plans for the new eye dispensary for the University of Pennsylvania Hospital (1903). Waiting room in remodeled clinic (1905).
Alongside the expansion of its clinical practice and research scope, the Department of Ophthalmology has undergone several changes in location over the past 150 years. Here, we walk through the history of physical spaces that have housed the Department over the years.
In 1874, architect Thomas Webb Richards designed the original building of the Hospital of the University of Pennsylvania. Richards was the University’s first professor of drawing and architecture. The plot of land on which the hospital was built was donated by the city of Philadelphia on the condition that 50 free beds were provided for low-income community members who were ill. Both State funds and private funds were used to finance the construction.
When the hospital opened in June of 1874, an eye clinic was nestled in the lower level of the building: the Department of Ophthalmology was born. William F. Norris, MD, the first Chairman of the Department, was one of 11 doctors on the medical staff of the hospital at the time of its opening.

Named for UPenn surgeon David Hayes Agnew, MD, the Agnew Wing of the Hospital was designed by Cope and Stewardson Architects and opened in 1897. The eye clinic moved to the Wing, which housed 160 beds and five wards, two of which were ophthalmic wards. Located on the second floor, one of the wards was for women and the other for men. Dr. Norris also opened an ocular pathology laboratory in the Agnew Wing. In 1902, George E. de Schweintz became the second Chairman of the Ophthalmology Department and advocated for an operating room for eye surgery. The eye dispensary and lab were also expanded and renovated in the Agnew Wing.
In 1937, a fire broke out, likely due to an electric short circuit. Engulfing much of the building, flames reportedly shot 20 feet in the air from the rooftop. In just 18 minutes, all 78 patients in the affected areas had been carried or led to safety. Thankfully, no one was seriously injured. Shortly after this fire, Francis

THE ORIGINAL BUILDING
Top image: The original building of the Hospital of the University of Pennsylvania, 1888 Retrieved from University of Pennsylvania Archives.

Bottom left image: “The New University Hospital,” September 1874. Retrieved from the Philadelphia Inquirer Archives.

THE AGNEW BUILDING
Middle image: The Agnew Wing, November 1904. Retrieved from University of Pennsylvania Archives
Bottom right image: The Agnew Wing fire, February 1937. Retrieved from the Philadelphia Inquirer Archives
Heed Adler, MD, Chair of the Department at the time, moved the eye clinic to a different part of the hospital, where the Gates Pavillion was eventually erected. The new clinic was located on the third floor, where it remained until the opening of the Scheie Eye Institute.

In 1960, Harold G. Scheie, MD became the fifth Chairman of the Department and subsequently founded the Scheie Eye Institute. The multimillion-dollar construction of the building began in 1969 at the Presbyterian University of Pennsylvania Medical Center (now Penn Presbyterian Medical Center). The new institute was funded in part by a $3 million anonymous donation.
Ground was broken on December 8, 1969. In May of 1971, a “Topping Out” ceremony was held to celebrate the halfway point of construction. Cutting the ribbon were Dr. Scheie, his wife Mary Ann Scheie, and Mabel Pew Myrin, Honorary Chairman of the Friends of the Scheie Eye Institute.

The Scheie Eye Institute opened in 1972. Designed by architect Dick Colville of the Kling Partnership, the building’s exposed structural concrete and brick are characteristics of the brutalist architecture style. The interior design matched the circular exterior. The waiting room featured rounded seating areas, circular paneless windows, and an oval-like reception desk. The formal dedication of the building was led by Lord Mountbatten of the British royal family, who had been treated by Dr. Scheie for an eye injury.
Images from top to bottom: CONSTRUCTION OF SEI ca. 1972. Retrieved from University of Pennsylvania Archives.
TOPPING OUT CEREMONY
May 1971. From left to right: Mary Ann Scheie, Harold G. Scheie, MD, Mabel Pew Myrin. Retrieved from the Philadelphia Inquirer Archives.
THE SEI COMPLETION
Exterior of the original SEI building, c. 1970-1980. Courtesy of the Department of Ophthalmology Archives.

ROUNDED EXTERIOR OF THE SEI

Bottom left image: Courtesy of Ralph C. Eagle.
THE LOBBY OF THE ORIGINAL SEI Bottom right image: c. 1970-1980. Courtesy of the Department of Ophthalmology Archives.

Images from top to bottom: Renovated lobby with new lighting and seating.

Courtesy of BBLM Architects
New banquet seating in the lobby. Courtesy of BBLM Architects

Renovated exam room. Courtesy of BBLM Architects

In 2014, the interior of the Scheie Eye Institute underwent extensive renovations under the leadership of Joan O’Brien, MD, eighth Chairman of the Department. The project, led by Brandon Sargent of BBLM Architects, aimed to improve the outpatient experience by reconfiguring and modernizing the lobby and first and fifth floor clinical spaces. Throughout the renovation, efforts were made to feature the architectural details of the original building, such as the exposed brick and the circular cutouts of the large concrete walls, which had been covered up over the years.
In the lobby, noise issues were addressed. Sargent explains: “[We] looked at every surface in the lobby to figure out how we could add some sound absorption quality.” This included the carpeting, the wood-paneled lower walls with sound insulation, and the upper walls with sound absorption plaster finish. In addition, Sargent emphasized the “suspended cloud in the top of the lobby,” used to interrupt sound travel throughout the lobby.
Indirect lighting, such as light-colored surfaces and illuminated cylinders in the ceiling coffers, was utilized to protect patients with dilated eyes while still brightening the once dark space. As part of the renovation, the first floor was also reconfigured to become more accessible, with decentralized check-in desks to allow for more privacy, custom banquet seating, large bathrooms, and an updated optical shop. The designs included rounded elements to match the building’s architecture.
In addition to these updates, 30 exam rooms were entirely renovated and fit with new, state-of-the-art technology. To evaluate the exam room design, physicians and technicians saw patients in a working mock-up room and made constructive comments about how to improve the layout. Because of this collaboration, the exam rooms continue to function well today, nearly a decade later.
The Department of Ophthalmology has now expanded to six clinical facilities across Philadelphia and Delaware County: the Scheie Eye Institute at Penn Presbyterian Medical Center, the Perelman Center for Advanced Medicine, the Scheie Eye Satellite in Radnor, the Scheie Eye Satellite in Media, the Children’s Hospital of Philadelphia, and the Veterans Affairs Medical Center of Philadelphia of Philadelphia. The Department is dedicated to providing superb eye care across the Philadelphia area. n

Historical giving: 1883-1995. (n.d.). Perelman School of Medicine at the University of Pennsylvania - Donor Recognition. Retrieved from https://www.med.upenn.edu/donorrecognition/historical-giving. html#DullesAgnew19414
History of Ophthalmology at Penn. (n.d.). Penn Medicine Department of Ophthalmology. Retrieved from https://www.pennmedicine.org/ departments-and-centers/ophthalmology/about-us/history
Hospital Evacuated as Firemen Battle Flames. (1937, February 25). The Philadelphia Inquirer, p. 3. Retrieved from https://www.newspapers.com/ image/176106409/
Hospital Memorial to Titanic Victim. (1931, April 19). The Philadelphia Inquirer, p. 75. Retrieved from https://www.newspapers.com/ image/173334477/
Leong, J. (2011, February 3). D. Hayes Agnew Memorial Pavilion. Penn Today. Retrieved from https://penntoday.upenn.edu/node/151694
Rain Goes Away for Topping Out at Eye Institute. (1971, May 18). The Philadelphia Inquirer, p. 3. Retrieved from https://www.newspapers.com/ image/180063213/?terms=scheie%20eye%20institute&match=1
Salowe, R., Mulvihill, K., & Laberee, N. (2019). Department Milestones: Looking Back on 145 Years of Ophthalmology. Scheie Vision. Retrieved from https://www.pennmedicine.org/-/media/academic%20departments/ ophthalmology/summer%202019/summer%202019.ashx?la=en
Sapega, S. (2020, February 28). Another “Look Back” at HUP. Penn Medicine News. Retrieved from https://www.pennmedicine.org/news/ internal-newsletters/hupdate/2020/march/another-look-back-at-hup
Sargent, B. (n.d.). Scheie Eye Institute Renovation. Archinect. Retrieved from https://archinect.com/bsargent/project/scheie-eye-instituterenovation
Scheie Eye Institute. (2018, March 16). BBLM Architects. Retrieved from https://www.bblm.com/project/scheie-eye-institute/
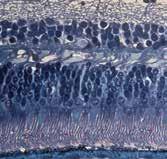
SCHEIE TODAY Modern image of the SEI. Courtesy of Ralph C. EagleA mole on the eye spontaneously grows into a large tumor, a doctor sacrifices his vision, and an infection is squeezed out of the eye. In this article, we look back at a small sample of noteworthy historical medical cases and surgeries in the Ophthalmology Department prior to the 1940s.
April 26, 1939: With blood dripping down her face from her left eye, a 50-year-old woman walked into the outpatient eye clinic at the Hospital of the University of Pennsylvania (HUP). When she was a teenager, she had noticed a dark spot on the sclera of her eye, on the nasal side of the cornea. The spot, called a nevus (like a mole on the eye), remained unchanged for over 30 years. When it suddenly began to grow, and then bleed, she knew it was time to seek help.
When she reached the clinic, her bloody eye was first irrigated with boric acid. The rinse dislodged a piece of black, hardened tissue the size of “the nail of the little finger,” which dropped from the upper eyelid, according to the treating physician Dr. W. E. Fry’s account of the case. After this, the bleeding stopped temporarily.
Unfortunately, the nevus—now a tumor—continued to grow. After her eye hemorrhaged again, the patient was admitted to HUP and underwent surgery. In surgery, Dr. Fry discovered that the tumor occupied most of the nasal portion of the orbit, and he was forced to perform an exenteration. In addition to the eyeball, the surrounding muscles, fat, nerves, and eyelids were removed to increase the chances that the entire malignant tumor was excised.
Microscopic examination of the tumor revealed malignant melanoma. Thankfully, Dr. Fry was able to remove the whole tumor, and the patient’s melanoma did not metastasize.
June 30, 1936: Julius Comroe, MD was finishing up the last day of his internship at UPenn. He was assigned to an outpatient with an eye infection, and Dr. Comroe advised the patient to return for a followup if his condition worsened.

The next day, the patient returned to the eye clinic, where he was admitted as an inpatient and diagnosed with conjunctivitis. Unfortunately, antibiotics, which are used
today to treat bacterial conjunctivitis, were not readily available in the mid-1930s. As a result, the contagious condition was particularly dangerous. The patient was strictly isolated.
Two days after his internship ended, Dr. Comroe, who had left Philadelphia and was now in Chicago, began experiencing similar symptoms. He promptly returned to UPenn to be treated by then-Chairman Thomas B. Holloway, MD.
Without viable treatment options, Dr. Holloway prescribed frequent irrigations of the eyes with boric acid and daily application of one percent silver nitrate. According to Harold G. Scheie, MD, who recalled this event in an interview with science historian Sally Smith Hughes, “The silver nitrate hurt like the devil but it was thought to be effective by causing so much irritation that the epithelial cells would slough off carrying the [bacteria] with them.”
Without the aid of antibiotics, Dr. Comroe lost one of his eyes in a matter of days. However, his other badly infected eye eventually fully recovered. Though he could no longer pursue surgery as he had hoped, he became an expert in physiology, cardiology, and pulmonology. He served as Chairman of the Department of Physiology and Pharmacology at UPenn from 1946 to 1957, then founded the Cardiovascular Research Institute at the University of California, San Francisco. Dr. Comroe passed away in 1984 after dedicating his life to his patients and research.
Late 1880s to early 1900s: Trachoma, a bacterial eye infection that causes blindness, was considered granular conjunctivitis in the mid to late 1800s. By 1897, the United States government had enacted a law that prohibited those with trachoma to enter the country.
Despite this law, the University of Pennsylvania (UPenn) continued to see cases of trachoma in the early 1900s, the cause of which was still unknown. In its acute form, the infection was treated primarily with topical medications like boric acid. In its chronic form, more extreme measures were taken; the use of caustics, astringents, and surgery were not uncommon.
George E. de Schweinitz, MD, the second Chairman of Ophthalmology at UPenn, credited Jacob Hermann Knapp, MD for the invention of forceps that revolutionized surgery for chronic trachoma at the time. In the operating room, for one such case, Dr. de Schweinitz everted the eyelids and used the Knapp forceps to squeeze the conjunctiva “until all the morbid material … had been thoroughly milked.” The forceps allowed for quick expression with less damage to the eye than previous manual methods of treatment.
Today, trachoma is the leading cause of infectious vision loss in the world, though extremely rare in the United States. In its early stages, it is treatable with antibiotics. n
Adler, F. H., & Reese, W. S. (1941). College of Physicians of Philadelphia: Section on ophthalmology. American Journal of Ophthalmology, 26. https://doi. org/10.1016/s0002-9394(43)91863-x
Albert, D. M., & Scheie, H. G. (1965). A history of ophthalmology at the University of Pennsylvania. C.C. Thomas.
Scheie, H. G. Ophthalmology Oral History Series. A Link with Our Past. Sally Smith Hughes Foundation of the American Academy of Ophthalmology, 1988. “Julius H. Comroe.” A History of UCSF https://history. library.ucsf.edu/comroe.html
World Health Organization. (n.d.). Trachoma. World Health Organization. Retrieved from https://www.who. int/news-room/fact-sheets/detail/trachoma
Over the years, the Department has seen many patients amaze with their incredible talents. Our care team provides high quality treatment to allow patients to continue to do what they love. In this article, we feature three patients who, despite the constraints of limited sight, found passion and success in musical and visual arts.
In 2013, just two weeks after receiving a novel gene therapy for Leber’s Congenital Amaurosis (LCA), Christian Guardino sang to a transfixed audience. That night, he saw the moon for the first time and gained the confidence to become a star.
As an infant, Christian was diagnosed with LCA, a rare retinal degeneration. When he was 11, his vision began to deteriorate rapidly. His concerned mother, Beth, attended an LCA conference in Philadelphia, where she learned the sobering prognosis of LCA: without intervention, Christian could lose all of his sight. The following year, at the age of 12, he did.
Then, Christian and his mom met Jean Bennett, MD, who is Co-Director of the Center for Advanced Retinal & Ocular Therapeutics at the University of Pennsylvania and an expert in gene
therapy for retinal degenerations. Dr. Bennett was conducting a clinical trial on patients with LCA using a gene therapy (now named Luxturna) targeting the RPE65 mutation. Christian was eligible for the trial, and soon found himself in treatment with great success. Just two weeks later, he was staring mesmerized at the giant rock in the sky, about to sing to a teary audience.
The following year, Christian won the Grand Prize at the Apollo Theater’s Amateur Night at the Apollo in the “Stars of Tomorrow” category. Two years later, in 2016, he welcomed ice hockey fans with the national anthem at a NY Islanders playoff game and performed a duet with Jordin Sparks for Michelle Obama’s “Fit 2 Celebrate” Gala.
In 2017, at the age of 16, Christian stood on the stage of a packed concert venue in front of the judges of America’s Got Talent. His performance of “Who’s Lovin’ You” by The Jackson Five brought the audience and judges to their feet, left Simon Cowell

speechless, and prompted Howie Mandel to press the Golden Buzzer, sending Christian immediately to the quarterfinals. Christian also performed in the semifinals, again receiving a standing ovation from all four judges.
Just this year, in 2022, Christian successfully auditioned for American Idol, a show he had followed his entire life. The judges were in awe of the range and depth of his voice, and of Christian himself. His performance of John Lennon’s “Imagine” brought Katy Perry to tears. “I didn’t hear anything but perfection,” raved Luke Bryan. The sheer power of Christian’s voice in his performance of “Circle of Life” from The Lion King was breathtaking.
Of over 100,000 auditioners, Christian was a Top 7 Contestant in Season 20 of American Idol.
Now, thanks to the research-scientists at the Scheie Eye Institute, Christian can see the gaping audience as he performs.
Christian Guardino performs on America’s Got Talent in 2017. Photo credit: Trae Patton/NBC/NBCU Photo Bank/Getty Images.98-year-old Hilda Friedman was born an artist. As a child, she gained practice drawing her favorite muse, her grandmother’s cat. Hilda grew up alongside her three sisters during the Great Depression, and she attended South Philly High School. After receiving a full scholarship, she earned her bachelor’s degree from William Smith College.
Despite initial doubts from her family,
Like Hilda Friedman, Bernice Paul was destined to be an artist. Born in Moscow in 1917, she immigrated to the United States in the 1930s. She settled in Philadelphia, where she studied at the Pennsylvania Academy of Fine Arts, the Philadelphia College of Art, the Barnes Foundation, and the Fleisher Art Memorial.
Bernice especially loved to paint flowers and landscapes in the summertime, and she enjoyed art as a social activity. “I rarely paint alone; I most enjoy painting with friends,” she told former medical writer Nora Laberee in an interview in 2020. She went with her daughter to art studios in Philadelphia to meet others
Hilda chose to pursue art after college, and studied drawing at the Tyler School of Art at Temple University in the 1950s. While at Temple, Hilda became interested in color and began working with watercolors and printmaking as media. Interested in furthering her education and honing her skills, Hilda studied lithography and printmaking at the Academy of Fine Arts in Philadelphia, silkscreening at the Fabric Workshop, and art history at the Barnes Foundation. While educating herself, she taught her own students in classes at the Philadelphia Museum of Art, Wayne Art Center, and St. Joseph’s University.
who liked to paint.
Do not be fooled: Bernice’s art was not simply a social pastime. She earned many awards, including a gold medal from the Philadelphia Sketch Club, gold and silver medals from the Plastic Club, first prizes at the Upper Merion Cultural Center, and Best in Show at the Main Line Center of the Arts.
As Bernice aged, she began to suffer from macular degeneration, the leading cause of vision loss in the United States in individuals over 65 years old. Bernice came to the Department as a patient under the care of Albert Maguire, MD and Ranjoo Prasad, MD.
Though she was losing her eyesight, Bernice’s passion for art was unfaltering.
Kikut, A. (July 2018). Like Watching a Miracle. Scheie Vision Laberee, N. (July 2019). Still Painting After 102 Years, Despite Vision Loss. Scheie Vision Salowe, R. (December 2020). 96-Year-Old Patient and Artist Donates Paintings to Scheie. Scheie Vision
Hilda became a patient of the Scheie Eye Institute in the 1970s when she suddenly lost half of her field of vision. She learned that she had melanoma in her right eye and came to Scheie for further evaluation under the care of Harold Scheie, MD and William Frayer, MD. The doctors advised surgery, as her eye had to be enucleated. After surgery, Hilda was persistent about continuing her art.
Hilda’s later work used metal, a symbol of grief in Mexico. She was drawn to this medium in response to the loss of her husband, whom she married young and loved deeply.
In 2020, she donated three tremendous watercolor paintings to Scheie, which are on exhibit today in the second floor waiting room. The abstract art is charged with emotion, and the enormous size of the paintings—particularly unusual for watercolors—makes the detail more visible to patients. In Hilda’s current phase of work, she uses wood as a medium.

Hilda’s work is available for sale or placement in galleries and museums. Her work can be viewed at hildafriedman.com
The late Bernice Paul sits next to one of her beautiful floral paintings, which she donated to UPenn.
“My eyes are going now, but I still paint,” she told Laberee in their interview.
“There is a joy in painting, I love it.”
Bernice Paul passed away in 2021 at the age of 103. She spent her entire life, even despite vision loss, painting. n

 By Isabel Di Rosa
By Isabel Di Rosa
Left: Ali Haasz prior to surgery.
Right: Ali Haasz four weeks after surgery. before after
Alexandra “Ali” Haasz had almost given up on her vision before seeking help at the Scheie Eye Institute. She had previously undergone four surgeries at other eye institutes with little improvement.
When she was born, Ali was diagnosed with strabismus, commonly referred to as crossed eyes. She underwent her first operation prior to her first birthday, which was unsuccessful and resulted in exotropia in both eyes. Exotropia is an eye misalignment that causes the eye to deviate outward.
While Ali was extremely insecure due to her condition, her parents were incredibly supportive of her. Her father drew eyes on the patches that Ali sometimes wore when she was not donning her glasses with prisms. Her parents took her to vision therapy and countless doctors’ appointments. Ali had three surgeries prior to entering high school.
The surgeries, while not as life changing as she had hoped, allowed Ali to learn to control each eye independently or both if she concentrated. “To use both of my eyes together, it felt like I was holding a dumbbell and I was halfway through a bicep curl,” Ali explained. This tension caused severe headaches.
“Everything from my sleep to my selfesteem was adversely affected [by strabismus].” Through young adulthood, Ali wore sunglasses and heavy eye
makeup, and she avoided cameras and eye contact. Explained Ali, “I have always had tremendous insecurity and shame over my lazy eyes.”
When she turned 30, she decided she was ready to pursue treatment again. She had a fourth surgery that was not only unsuccessful, but also caused significant regression. She could no longer move both eyes at the same time. “I was in a place of total devastation,” Ali remembered. When she returned home, she prayed. “These are my eyes. This is important!” she cried.
Ali wanted another opinion. She started researching and discovered the Scheie Eye Institute and Madhura Tamhankar, MD. “During my initial consult with her, she literally said those words: ‘These are your eyes. This is important!’ I almost cried,” Ali recalled.
After considering the risks of a fifth surgery, without knowledge of what she would discover until the operation began, Dr. Tamhankar was still willing to take on the case. She recognized the limiting effect strabismus had on Ali’s life.

Ali was impressed by Dr. Tamhankar’s diligence in gaining as much background information as possible to prepare for the operation. In August 2022, Dr. Tamhankar performed Ali’s fifth eye surgery.
“All I saw for the first 40 minutes of surgery was scar tissue,” Dr. Tamhankar recalled.
“I have never seen so much scar tissue in an eye surgery—to the point where it was completely covering the muscle.” Because eye muscle and scar tissue are sometimes intertwined, Dr. Tamhankar had to dissect the scar tissue with extreme precision. She considered stopping the surgery; with the muscle nowhere in sight, it might be too weak or too entangled within the scar tissue to safely operate on. However, Dr. Tamhankar continued to work, aware that after a fifth surgery, it would be difficult for Ali to find another surgeon willing to operate. “If I don’t fight for her, who is going to?” Dr. Tamhankar remembered thinking.
After 40 minutes of dissecting scar tissue, Dr. Tamhankar finally found the muscle: “That was my first glimmer of hope.” She was then able to complete the surgery successfully using adjustable sutures, which allowed her to tweak the alignment of Ali’s eyes immediately after surgery. This ensured perfect alignment.
At the time of the interview, it had been two and a half weeks since the surgery and the results had already increased Ali’s confidence tremendously. “I can connect with people in deeper ways… just in the past two weeks [since surgery],” Ali remarked. Eye contact played a large role in this.
“My eyes are straight,” Ali laughed with joy. “They’re completely straight. It surprises me every time I look in the mirror.” n
These are my eyes. This is important.”
On March 11, 2020, the World Health Organization declared the novel coronavirus (COVID-19) outbreak a global pandemic. Since then, the city of Philadelphia has experienced more than 350,000 cases and 5,200 deaths. Unfortunately, COVID-19 was not the first virus to wreak devastation on the city. Below, we examine the outbreaks of yellow fever in 1793 and influenza in 1918 in Philadelphia. Like COVID-19, both outbreaks led to swift and unprecedented responses from the University of Pennsylvania (UPenn)—including our ophthalmologists.


Called the “American Plague” at the time of its outbreak, yellow fever was an acute viral hemorrhagic disease caused by a virus in the family Flaviviridae. The virus caused symptoms such as high fever, internal bleeding, vomiting of blood, and jaundice (leading to the name “yellow” fever). Philadelphia, which was the nation’s capital at the time, had the highest death toll of all cities in the United States.
During the summer of 1793, yellow fever spread like wildfire throughout Philadelphia. The origins of the virus and its mode of transmission (mosquitoes) were unknown at the time, fueling fear and panic. More than 20,000 people fled the city and sought safety in the countryside, including Thomas Jefferson, George Washington, and Alexander Hamilton.
A 19th-century image depicting the final stages of yellow fever. Courtesy of Wellcome Images via Wikimedia Commons.
Those left behind (often without the means to travel) described the city as being eerily quiet and desolate. Mass graves were scattered around the city, with families buried together. Carriages were driven through the streets, with shouts for families to bring out their dead—a practice not seen widely since the Black Death of medieval Europe.
The mass exodus from Philadelphia during the epidemic included many of the city’s physicians. The few who remained were mystified and increasingly desperate to find effective treatments. Even the 16-member College of Physicians was divided on how to treat the virus, with some advocating for more aggressive therapies that bled and purged patients, and others supporting milder remedies such as cold baths.
Like all hospitals at that time, Philadelphia Hospital closed its doors to yellow fever victims to protect its existing inpatients. A temporary hospital was opened by the Guardians of the Poor at Bush Hill, an estate outside the city, but was desperately understaffed. In The Story of Philadelphia, author Lillian Rhoades commented: “The hospitals were in a horrible condition; nurses could not be had at any price . . . nearly every bed contained a dead body, and the floors reeked with filth.”
Benjamin Rush (1746-1813). Retrieved from University of Pennsylvania Archives.


Philip Syng Physick (1768-1837). Retrieved from University of Pennsylvania Archives.
The care of thousands of sick patients thus fell to the few physicians who valiantly refused to flee the city. Among these physicians were two professors from UPenn: Benjamin Rush, MD and Philip Syng Physick, MD. Both worked tirelessly with yellow fever victims, attempting to save as many lives as possible.
The Arch Street Ferry is believed to be the entry point of yellow fever into Philadelphia in 1793. Courtesy of Independence National Historical Park via Wikimedia Commons.Dr. Rush, Professor of Medical Theory and Clinical Practice at UPenn, was a signer of the Declaration of Independence and a founder of the College of Physicians of Philadelphia. He was among the first to identify the disease affecting city residents that summer as yellow fever. He worked closely with Dr. Physick, who had just returned from medical school in Edinburgh. Dr. Physick later became a Professor of Surgery and Anatomy at UPenn who specialized in ophthalmic procedures. Though the Ophthalmology Department was not officially founded for another 80 years, he was undoubtably a leader in the field at that time, earning the name “Father of American Ophthalmology.”
Drs. Rush and Physick worked closely with yellow fever victims, taking careful notes and performing frequent autopsies in the hopes of understanding this deadly virus. Both supported a controversial approach to treating yellow fever, including blood leeching and purging patients, as well as administration of mercury. They reported that this treatment regimen was highly effective if administered early. When Dr. Rush fell ill with the virus on two separate occasions, he applied this treatment method to himself and recovered. Similarly, when Dr. Physick contracted yellow fever, he later credited his survival to Dr. Rush’s treatment of bleeding and purging.
However, some colleagues believed that these treatments were applied too excessively and without discrimination. Dr. Rush also came under fire for his theory that the virus was spread by putrid exhalations in the atmosphere from unsanitary conditions and rotting food at city ports, angering proud Philadelphians. He was correct, however, that the virus did not spread through human-tohuman contact. His accounts on the fever in books and lectures, as well as private letters, were widely read and cited.
Today, many regard both physicians as heroes for their utter devotion to patients at a time when most physicians fled the city to protect themselves.
In late October 1793, the frost finally killed the mosquitoes in Philadelphia, bringing an end to the deadly epidemic. It is now estimated that more than 5,000 people in Philadelphia died between August and November of 1793 from yellow fever, which was 10% of the city’s population at the time.
Though an effective vaccine was developed in 1938, yellow fever still kills approximately 30,000 people each year. Ninety percent of these individuals live in Africa.
Philadelphia
Retrieved
Philadelphia had a staggering death toll from influenza. Retrieved from National Museum of Health and Medicine.

In 1918 and 1919, a deadly influenza pandemic spread worldwide, ultimately resulting in more deaths than World War I. This outbreak was caused by a H1N1 influenza A virus with genes of avian origin. Many individuals experienced relatively mild flu symptoms, especially during the first wave of disease. Later waves of a more virulent strain of the virus were far more deadly, with many individuals developing complications such as bacterial pneumonia. Unlike yellow fever, the virus was transmitted person to person through airborne respiratory droplets.
The influenza pandemic broke out in 1918 near the end of World War I. Though the exact origin of the virus remains unknown, it is believed that American troops returning from Europe inadvertently brought a more virulent form of influenza back to ports in Philadelphia and Boston. Within a matter of days, 600 sailors caught the disease. The virus soon spread from these port cities across the country.
On September 28, 1918, Philadelphia hosted the Fourth Liberty Loan Campaign rally to raise funds for the war effort, bringing together more than 200,000 Philadelphians. It is now believed that this rally contributed to the deadliest period of illness in the city.
With an unnerving similarity to the yellow fever pandemic, bodies began to pile up in makeshift morgues and in the streets. The frantic public stripped medications from the shelves of pharmacies, or resorted to buying folk remedies in the streets. Unlike most influenza strains, this outbreak had an unusually high mortality rate for healthy adults between the ages of 20 and 40, rather than the very young and old.
 Liberty Loan’s Parade on Broad Street gathered more than 200,000 Philadelphians, contributing to the rapid spread of the virus.
from U.S. Naval History and Heritage Command – Smithsonian.
Liberty Loan’s Parade on Broad Street gathered more than 200,000 Philadelphians, contributing to the rapid spread of the virus.
from U.S. Naval History and Heritage Command – Smithsonian.
The influenza epidemic overwhelmed city hospitals, with Philadelphia General Hospital and Hospital of University of Pennsylvania (HUP) receiving an unprecedented influx of patients. Beds were added to waiting rooms to accommodate the mounting number of patients. At this time, the Ophthalmology Department was located in HUP and thus was closely involved in treating patients.
Compounding the problem of hospital overcrowding was the severe shortage of health care professionals at HUP and throughout the city. More than 25% of physicians and nurses were called away to serve the war effort—and up to 75% of hospital medical and surgical staff were overseas. Among the physicians overseas was the then-Chairman of the Ophthalmology Department, George de Schweinitz, MD, who was serving in a field hospital in France.
This absence of vital medical personnel left the city unprepared to contain the virus and care for the sick. In addition to understaffing, there was also uncertainty about how to best treat the virus. There were no antiviral drugs or antibiotics for secondary bacterial infections, and the most common prescription filled for patients was whiskey.
The physicians who remained in Philadelphia were devoted to fighting the virus and saving lives. The Ophthalmology Department and other medical specialties at HUP re-focused all effort on treating influenza patients, with the exception of emergency surgeries. The entire hospital was put under strict quarantine with no visitors permitted. Even individuals without medical experience volunteered to clean facilities, dispose of dead bodies, or operate soup kitchens.

A significant portion of care also fell to medical students, nurses, and volunteers, who played a vital role in staffing hospitals. Penn medical students staffed 19 hospitals in Philadelphia, with only one lecture on influenza to guide them. The Student Army Training Corps, which had been established to provide trained officers for the war effort, also played a large role in curtailing the virus’s spread. They commandeered two fraternity houses at UPenn to use as emergency hospitals.
Nurses at HUP and other overflowing hospitals worked around the clock to care for patients. Many treated the thousands of sick who could not reach a hospital, describing horrors such as entering houses where every member of the family was dead. Many heralded the nurses and medical workforce as heroes and saviors, while others shunned them because they wore white gowns and masks.
Regardless of the public’s opinion, the medical workforce and volunteers risked their lives to care for influenza patients. Large numbers contracted the virus during their work. For example, first-year nursing students at UPenn were encouraged to return home rather than face the disease, but all chose to stay and work in hospitals. Six eventually died from the virus.

The

The severity of the influenza outbreak waned quickly in Philadelphia. By late October 1918, most quarantines at UPenn and in Philadelphia were lifted. A plaque was dedicated at HUP to all the nurses who died during the pandemic. However, the heroic efforts of the medical workforce and volunteers were largely overshadowed by the war.
Though estimates vary, it is believed that more than 50 million people died from the virus between 1918 and 1922, roughly half of whom were between the ages of 20 and 40. Philadelphia had approximately 500,000 cases and 16,000 deaths.
Influenza pandemics caused by novel influenza strains have occurred every 10 to 50 years since the late 1800s. Today, new versions of influenza vaccines are developed twice per year because the virus rapidly mutates. A universal flu vaccine that is effective against all influenza strains and does not require yearly modifications is currently the subject of much research. The first in-human trial with such a vaccine was launched in 2021.
Today, we know first-hand that pandemics remain a global threat. Almost three years have passed since the outbreak of the novel coronavirus (COVID-19) in March 2020. As in past pandemics, ophthalmologists and trainees at UPenn were quick to volunteer to help patients, working in triage tents and at testing sites throughout Philadelphia.
In 2022, an article was published in Clinical Ophthalmology outlining the successful recovery strategy of the UPenn Ophthalmology Department in response to the coronavirus pandemic. In this article, Joan O’Brien, MD, Benjamin Kim, MD, and Madhura Tamhankar, MD described the innovative metrics and initiatives developed by recovery ad hoc committees, allowing a safe recovery of patient and surgical volumes after seven months. The actions described in this article can help provide a blueprint for the response of academic departments and clinics to future pandemics.
Most of all, we must never forget to look to the self-sacrifice, courage, and innovation of ophthalmologists, physicians, and trainees during these pandemics. They serve as examples of the strong and compassionate approach needed in medicine in times of crisis. n
Armstrong, J. (2015). Philadelphia, nurses, and the Spanish influenza pandemic of 1918. Naval History and Heritage Command. Retrieved from https:// www.history.navy.mil/research/library/online-reading-room/title-listalphabetically/i/influenza/philadelphia-nurses-and-the-spanish-influenzapandemic-of-1918.html
Barry, J.M. (2004). The Great Influenza: the story of the deadliest pandemic in history. New York, New York: Viking Press.
Brodin AC, Tamhankar MA, Whitehead G, MacKay D, Kim BJ, & O’Brien JM. (2022). Approach of an Academic Ophthalmology Department to Recovery During the Coronavirus Pandemic. Clinical Ophthalmology (Auckland, NZ), 16, 695.
Crosby, M. C. (2006). The American plague: The untold story of yellow fever, the epidemic that shaped our history Berkley Books, New York: Berkley.
Gammon, K. (2018). Flu Forward 1918 | 2018. Penn Medicine Magazine.
Gum, S.A. (2010). Philadelphia under siege: the yellow fever of 1793. Retrieved from https://pabook.libraries.psu.edu/literary-cultural-heritage-map-pa/ feature-articles/philadelphia-under-siege-yellow-fever-1793
Hingston, S. (2016). 11 Things You Might Not Know About Philly’s 1793 Yellow Fever Epidemic. Philadelphia Magazine.
Lynch, E.A. (1998). The Flu of 1918. The Pennsylvania Gazette.
Rhoades, L. (1900). The Story of Philadelphia. New York, Cincinnati, Chicago: American Book Company.
University Archives & Records Center. (n.d.). Benjamin Rush. Retrieved from https://archives.upenn.edu/exhibits/penn-people/biography/benjamin-rush
University Archives & Records Center. (n.d.). Penn and the 1918 Influenza Epidemic. Retrieved from https://archives.upenn.edu/exhibits/penn-history/flu
University Archives & Records Center. (n.d.). Philip Syng Physick. Retrieved from https://archives.upenn.edu/exhibits/penn-people/biography/philip-syngphysick.
Since the Revolutionary War, physicians, nurses, and medical trainees from the University of Pennsylvania (UPenn) have served in most major conflicts in our nation’s history. Because the U.S. Armed Forces lacked a strong medical infrastructure of their own until the second half of the 20th century, the medical community at UPenn—including ophthalmologists—played a major role in providing care during conflict. Physicians and nurses led field hospitals, treated the wounded on battlefields, and developed new technologies on the home front. Nowhere were these contributions more impactful than during World Wars I and II.
World War I broke out among European nations on July 28, 1914. Though the United States officially maintained a neutral position for three more years, physicians and nurses at UPenn began to volunteer for service on behalf of the Allies. In 1915, a group of these physicians and nurses travelled to Europe and took over leadership of the American Ambulance Hospital in Paris.
Back on campus, the Hospital of the University of Pennsylvania (HUP) set aside 250 beds for special use by the Army and Navy. Medical students enrolled in courses that would prepare them to treat heavy combat injuries. They were also taught operative surgery on cadavers and neurological diagnostics to assess trauma and shock. Students and faculty formed battalions, and all male medical students were inducted into the Students’ Army Training Corps.
Medical faculty also pursued research projects to support the war effort during these years of neutrality. Eye surgeon Hunter Scarlett, MD (1911 Penn Medicine alumnus), along with Frenchman Dr. Georges des Jardins in the American Ambulance Service, discovered a microbe that caused gangrene to develop in bullet and shrapnel wounds. This discovery led to work at the Pasteur Institute to create a serum for injection of patients on the battlefield, which helped to prevent unnecessary amputations and death.
By the time the United States entered the war on April 6, 1917, approximately 40% of the medical faculty at UPenn had enlisted in the service. Their contributions were far-reaching and impactful. Over the course of the war, these physicians


Ambulance at Base Hospital No. 20.
Retrieved from University of Pennsylvania Archives.
and nurses led three Ambulance Units, several Red Cross units, and various detached units to support the war effort. Their largest contribution, however, was the organization and leadership of Civilian Base Hospital No. 20, which later became the largest field hospital in World War I.

UPenn began preparations to lead this field hospital back in 1916, working with the American Red Cross and War Department. In 1918, the members of Civilian Base Hospital No. 20 set sail for France when called into active service. All chief medical officers were from UPenn’s medical school and hospital, and many general staff members were Penn medical students.
The field hospital was operated out of hotels in France for a period of eight months, with patients continuously arriving from hospital trains. In total, they saw 75,000 patients, including 4,000 surgical cases and 3,500 medical and gas patients. Of note, only 65 patients died, which was an incredible feat for that time period.
When patients first arrived at the field hospital, they were classified by disease or injury and organized into separate wards, including a designated area for ophthalmic injuries. The majority of patients were American, but French soldiers and German prisoners were also seen. Though the field hospital mostly treated battle causalities and disease, they also became known as one of three observational hospitals for tuberculosis, and had unusual success dealing with the influenza pandemic.
There was a staggering number of eye injuries during World War I, necessitating the creation of an Eye Department at Civilian Base Hospital No. 20. It consisted of a ward of 40 beds, a dark room, an operating room, and an outpatient dispensary.
British soldiers temporarily blinded by mustard gas. Courtesy of Imperial War Museums (collection no. 1900-22).
The then-Chairman of the Ophthalmology Department at UPenn, George E. de Schweinitz, MD, served in this Eye Department. When the United States entered the war, he was appointed as lieutenant-colonel in the Medical Reserve Corps. Among his many contributions, Dr. de Schweinitz is credited with generously providing much of the ophthalmic equipment used in this field hospital. He also served on the Committee of the Office of the Surgeon General, which was responsible for introducing specialties into the Army Medical Corps, and founded the Army School of Ophthalmology at Fort Oglethorpe. He was the only ophthalmologist or otolaryngologist to attain the rank of colonel during World War I.
Dr. de Schweinitz and other ophthalmologists faced enormous challenges at the field hospitals. The quantity and severity of eye trauma was unlike anything seen in prior wars. New types of weapons such as grenades, shells, and shrapnel produced chips that often projected into the face and eyes, causing severe trauma. Combat eye protection was scarce during the war, leaving the eyes especially vulnerable. Treatment usually involved enucleation or palliative care, or plastics operations if patients did not require immediate transport back to the United States.
World War I was also marked by increased use of chemical agents, especially mustard gas. Affected soldiers suffered from photophobia, tearing, and kerato-conjunctivitis with temporary visual incapacity and blindness. Typically, only the most serious cases were sent to the eye ward, while the milder cases were treated in the general wards or outpatient dispensary.
As a result of his outstanding service during the war, Dr. de Schweintiz was appointed as Brigadier General in the Medical Reserve Corps in 1922. He was also part of the medical care team called to treat President Woodrow Wilson after a stroke.
The Allies signed an armistice with Germany on November 11, 1918. In total, it is estimated that over 116,000 American soldiers died during World War I. An additional 800,000 became blind in one or both of their eyes during the conflict.


As in World War I, faculty and students at UPenn were actively engaged in preparations for the war before the United States had officially entered the conflict. During this time of neutrality, the University created a number of training programs across schools and implemented extensive security and safety measures, including first aid stations across campus. The Reserve Officers’ Training Corps (ROTC) on campus, which had added a medical unit after the First World War, was very active in these preparations.
The medical school accelerated its curriculum from four years to three years to aid the war effort. Medical students served in the ROTC and underwent regimented military training. The students began their military service as privates and were promoted to private first class the following year.
During this time, a number of medical faculty were asked by the government to carry out war-related research projects. For example, the then-Chairman of the Ophthalmology Department, Francis Heed Adler, MD, directed an investigation at UPenn on the mechanisms and treatment of mustard gas injuries to the eye. In later years, Alfred Newton Richards, PhD, Chairman of the Pharmacology Department, spearheaded the mass production and distribution of penicillin, which saved countless lives.
In December 1941, the United States officially entered World War II following the Japanese attack on Pearl Harbor. Several medical alumni from UPenn led the treatment of the wounded on the Hawaiian Islands in the aftermath of this attack. Over the following years, more than 17,000 faculty, staff, students, and alumni from UPenn joined the armed forces. A total of 362 individuals never returned home.
In 1940, the U.S. Surgeon-General called upon UPenn to organize an overseas military hospital, after their success in World War I. The medical faculty organized the 20th General Hospital and began two years of preliminary preparations in Philadelphia. By the time the Japanese attacked Pearl Harbor, the hospital was already organized and well-trained. They entered active service on May 15, 1942, with an enthusiastic send-off from Philadelphians at 30th Street Station.
Around the same time, the Medical Specialists Unit No. 31 of the Navy Reserve was activated. This unit was organized by Richard Kern, MD, a physician at UPenn. Dr. Kern and several other UPenn physicians spent the majority of the war aboard the Solace, a hospital ship in the Pacific. The ship functioned as an ambulance transporting the wounded to hospitals and provided emergency care and surgeries.
After eight months of training in Louisiana, the 20th General Hospital unit journeyed to Ledo in the Assam region of northeast India. Here, they provided medical care to the American, British, and Chinese troops fighting the Japanese and building the Ledo Road (earning them the nickname of “league of nations”). This road was essential to reopening land communication between the Chinese and the Allies.

Operating room at the 20th General Hospital. Retrieved from University of Pennsylvania Archives.

Christmas activities in a ward of the 20th General Hospital. Retrieved from University of Pennsylvania Archives.

As in World War I, almost all staff at this field hospital came from UPenn, including 59 physicians, 120 nurses, and 600 enlisted men. They occupied 289 buildings and 162 tents, ultimately admitting 73,000 patients. However, the similarities between the field hospitals led by UPenn in the two world wars mostly end here.
The medical team at the 20th General Hospital served for a much longer period of time, under very different conditions. The location of the field hospital in India posed more dangers than the hotels that housed Civilian Base Hospital No. 20 in World War I. The staff and patients lived in native structures called “bashas” that had dirt floors, leaky roofs of palm leaves, and no lights. The area experienced heavy rainfall and monsoons, and had few outlets for water, contributing to malaria and bacillary and amoebic dysentery. Dangers were also posed by leeches, mites, poisonous snakes, tigers, elephants, bears, bison, and rhinoceroses. These conditions not only made the treatment of battle causalities difficult, but worsened the problems in many cases.
Despite all these obstacles, the overall mortality rate at the 20th General Hospital was only 0.4%, the same as for civilian hospitals at that time. Isidor Ravdin, MD, a UPenn Professor of Surgery who served as the Commanding Officer at the field hospital, stated that this success was largely due to their implementation of modern medical practices, such as antibiotics.
As in World War I, the sheer quantity of eye injuries led to the creation of a separate eye clinic and eye ward in the field hospital, as well as a special section of the operating room for ophthalmic surgeries. Major Harold Scheie, who was an Associate Professor of Ophthalmology at UPenn at the time, was asked to be the Chief of Ophthalmology at the field hospital.
In this leadership role, Dr. Scheie quickly realized that bamboo huts were not dark enough to use diagnostic instruments, and had a room built of plywood for eye exams. His team was constantly busy. The eye ward housed about 50 beds (with separate wards for the Americans/British and the Chinese), but there were often
more than 90 eye patients in the field hospital at a given time. More than 60% of the Chinese soldiers had active trachoma, many with advanced cases that required surgery.
There was also a shortage of essential equipment at the field hospital, making eye exams and surgery very challenging. When Dr. Scheie and others left the United States, they did not know their final destination or what instruments would be available. Thankfully, Dr. Scheie brought his ophthalmoscope with him to the field hospital, which was invaluable in the following months. He and his team were also creative and resourceful in designing equipment from the few supplies they had available. For example, Dr. Scheie designed his own visual field apparatus by buying a black muslin from a local bazaar to make a testing screen, and spent two days creating a magnet to remove metallic foreign bodies from the eye.
The humid climate also posed difficulties for eye surgery. Even when surgical instruments were sterilized and dry, the excessive moisture in the air would quickly lead to rust and mold. Again, Dr. Scheie and ophthalmologists developed creative solutions, such as drying the instruments in an oven and submerging them in paraffin oil to prevent air contact.
Of the many patients that Dr. Scheie treated during the war, Lord Louis Mountbatten may be among the most memorable. As the great-grandson of Queen Victoria and cousin of Queen Elizabeth II, Lord Mountbatten was a key member of the British royal family. On the day of a planned inspection of the 20th General Hospital, his eye was pieced by a piece of bamboo. Dr. Scheie led the treatment of Lord Mountbatten’s eye over the following days and months, and the two formed a lifelong friendship (see more detail in “Scheie and the British Royal Family” on the following page).
Over 70 million soldiers and civilians died during World War II, which was roughly 3% of the world’s population at that time. Roughly 15,000 soldiers were blinded from combat injuries. It is likely that many more would have lost their eyesight without the care of trained ophthalmologists, like Dr. Scheie, serving abroad. n
Berens C. (1939). In Memoriam–Dr. George Edmund de Schweinitz. Bull N Y Acad Med, 15(1), 58–60.
Doria C. (2016). The effects of World War I upon French ophthalmology. Hist Sci Med, 50(3), 311-323.
Harold Glendon Scheie, M.D. (1988) Ophthalmology Oral History Series. A Link with Our Past. Sally Smith Hughes Foundation of the American Academy of Ophthalmology.
Perloff, CB. (2015). To Spread the Light of Knowledge: 250 Years of the Nation’s First Medical School. Philadelphia, PA: Trustees of the University of Pennsylvania.
University of Pennsylvania, United States, & Surgeon-General’s Office. (1920). History of United States Army Base Hospital No. 20: organized at the University
of Pennsylvania. Philadelphia, PA: E.A. Wright Company.
University Archives & Records Center. (n.d.). A Brief History of Global Engagement at the University of Pennsylvania. Retrieved from https://archives.upenn.edu/exhibits/ penn-history/global-engagement/international-crises/wwi#
University Archives & Records Center. (n.d.). Penn in the Great War: The University’s Role in a Critical Time. Retrieved from https://archives.upenn.edu/exhibits/pennhistory/wwi
University Archives & Records Center. (n.d.). Penn’s Base Hospitals in World Wars I and II. Retrieved from https://archives.upenn.edu/exhibits/penn-history/basehospitals
University Archives & Records Center. (n.d.). U.S. Army 20th General Hospital Records. Retrieved from https://archives.upenn.edu/collections/finding-aid/ upc15
It was March 7, 1944 when Harold G. Scheie, MD met Lord Louis Mountbatten—Supreme Allied Commander of South East Asia, last viceroy of India, and member of the British royal family. At the onset of World War II in 1943, Dr. Scheie joined the 20th General Hospital as a captain in the Army Medical Corps. He traveled with the unit to Southeast Asia, where he would soon encounter the 1st Earl Mountbatten of Burma—great-grandson of Queen Victoria, second cousin of Queen Elizabeth, and uncle of Prince Charles.
While in India, Lord Mountbatten’s left eye was pierced by a bamboo branch while riding in a jeep through the jungle. He was rushed to Seagrave’s field hospital, where he was then air evacuated to the 20th General Hospital. Lord Mountbatten suffered superficial corneal lacerations, embedded foreign bodies, and an anterior chamber hemorrhage, which filled the chamber with blood. Vision in his injured eye was limited to light perception.
Later that same afternoon, Lord Mountbatten was scheduled to inspect the field hospital. Dr. Scheie recalled Lord Mountbatten arriving earlier than expected with a bandage covering his left eye. Lord Mountbatten was surrounded
by high-ranking, well-known generals, including General Henry Pownall, who had commanded the British troops during the Japanese siege in Singapore.
While in the hospital, Lord Mountbatten told Dr. Scheie, who was an unknown young captain at the time, that President Roosevelt, Prime Minister Churchill, and the royal family urged him to fly in a consultant to treat his eye. Lord Mountbatten refused and said, “I have faith in Captain Scheie, and if he wants help he will ask for it” (Scheie, 1988, p. 101).
Over the next six days, Lord Mountbatten remained in private quarters. On the sixth day, Lord Mountbatten had to leave to counter an invasion, as the Japanese forces were preparing to invade India. Dr. Scheie accompanied Lord Mountbatten to New Delhi, and stayed in his quarters at the embassy, home to several highranking officers. Once news spread that an ophthalmologist was staying at the embassy, Dr. Scheie was asked to examine several patients’ eyes.
“Lord Mountbatten treated me royally and took me nearly everywhere that he went, including staff briefings,” recounted Dr. Scheie (1988, p. 103).

Dr. Scheie routinely performed checkups on Lord Mountbatten’s eye. During these visits, Lord Mountbatten would insist that Dr. Scheie stay for a meal and occasionally spend the evening. Dr. Scheie recalls one such visit, in which Lord Mountbatten escorted him to tour the Viceroy’s Palace. During another visit, Dr. Scheie dined with Lord Mountbatten and his wife, Edwina Mountbatten, Countess Mountbatten of Burma.
In 1946, Dr. Scheie received an honorary membership in the Order of the British Empire for his care of the British and American troops of the South East Asia Command, including his care of Lord Mountbatten. Dr. Scheie left the Army as a Brigadier General and was awarded the Legion of Merit.
After the war, the two remained quite close. Dr. Scheie was informed whenever Lord Mountbatten visited the United States, and Dr. Scheie and his wife stayed in London at Lord Mountbatten’s estate, Broadlands, on several occasions.
During his time as fifth Chairman of the Department of Ophthalmology, Dr. Scheie led the fundraising efforts to construct a new $12.5 million eye hospital (equivalent to $81M in 2022). The formal dedication of the Scheie Eye Institute occurred on
October 12, 1972. The Institute dedication was led by Lord Mountbatten, who spoke at the ceremony. He stayed in the corner patient suite on the fourth floor of the Scheie Eye Institute.

Dr. Scheie and his wife planned a visit to stay with Lord Mountbatten at Broadlands in June 1980. However, Lord Mountbatten

was tragically assassinated on August 27, 1979 by members of the Provisional Irish Republican Army. The group of political terrorists planted a bomb in the World War II hero’s fishing boat in northwest Ireland. Dr. Scheie attended the funeral of Lord Mountbatten, held at Westminster Abbey.

To commemorate the 10th anniversary of
Albert, D. M., & Scheie, H. G. (1965). A history of ophthalmology at the University of Pennsylvania.

Frayer, W. C. (2002). An ophthalmic journey: 50 years at the University of Pennsylvania. William C. Frayer, M.D. Harold Glendon Scheie, M.D. (1988). Ophthalmology Oral History Series. A Link with Our Past. Sally
the opening of the Scheie Eye Institute, Dr. Scheie and Myron Yanoff, MD, the sixth chairman of the Department, organized a special series of events in November 1982. Patricia Knatchbull, 2nd Countess Mountbatten of Burma, daughter of the late Lord Mountbatten, spoke at the anniversary celebration. n
Kennedy, L. (2020, November 13). The IRA assassination of Lord Mountbatten: Facts and fallout. History. Retrieved from https://www.history.com/news/mountbattenassassination-ira-thatcher
 Springfield, Illinois: Charles C. Thomas.
Smith Hughes Foundation of the American Academy of Ophthalmology.
Dr. Scheie examining Lord Mountbatten’s eye at the Scheie Eye Institute Dedication in 1972. Courtesy of Ralph C. Eagle, Jr., MD.
Lord Mountbatten and Dr. Scheie at the Scheie Eye Institute Dedication in 1972. Retrieved from University of Pennsylvania Archives.
Lord Mountbatten led the Scheie Eye Institute Dedication in 1972 and spoke at the ceremony Courtesy of Ralph C. Eagle, Jr., MD.
From left to right: Lord Mountbatten, Dr. Scheie, and Isodor Ravdin at the retirement ceremony for Dr. Scheie, held in the Officers’ Club of the Defense Supply Agency. Retrieved from University of Pennsylvania Archives.
Lord Mountbatten and Dr. Scheie maintained a close friendship after the conclusion of World War II Courtesy of Ralph C. Eagle, Jr., MD.
Springfield, Illinois: Charles C. Thomas.
Smith Hughes Foundation of the American Academy of Ophthalmology.
Dr. Scheie examining Lord Mountbatten’s eye at the Scheie Eye Institute Dedication in 1972. Courtesy of Ralph C. Eagle, Jr., MD.
Lord Mountbatten and Dr. Scheie at the Scheie Eye Institute Dedication in 1972. Retrieved from University of Pennsylvania Archives.
Lord Mountbatten led the Scheie Eye Institute Dedication in 1972 and spoke at the ceremony Courtesy of Ralph C. Eagle, Jr., MD.
From left to right: Lord Mountbatten, Dr. Scheie, and Isodor Ravdin at the retirement ceremony for Dr. Scheie, held in the Officers’ Club of the Defense Supply Agency. Retrieved from University of Pennsylvania Archives.
Lord Mountbatten and Dr. Scheie maintained a close friendship after the conclusion of World War II Courtesy of Ralph C. Eagle, Jr., MD.
 By Isabel Di Rosa
By Isabel Di Rosa
The Department has a rich history of contributions to the field of ophthalmology. Clinician-scientists in the early years of the Department developed innovative operation techniques, invented surgical tools, and were pioneers in photographing the eye. Here is a small sample of some of the most groundbreaking research advancements through the year 1900.

In 1800, Philip Syng Physick, MD joined the Medical Department of the University of Pennsylvania (UPenn). As a Professor of Surgery, Dr. Physick was a well-respected general surgeon who earned his reputation by successfully operating on cataracts and the bladder. In his 1795 journal, Dr. Physick describes the case of a woman who lost her vision following cataract surgery. Most cataract surgeons in the 1700s applied the couching technique, in which a sharp instrument pierces the eye and dislocates the opaque lens from the central visual axis, pushing the opaque lens (the cataract) to the back of the eye to allow light to enter. Dr. Physick, however, was able to extract the cataract using methods that were unconventional at the time. Instead of using couching, which was largely unsuccessful, Dr. Physick corrected the woman’s botched surgery by using a knife to make an incision in the eye, and he then used a needle to tear the capsule of the cataract, drawing out the clouded lens. Today, cataracts can be removed through phacoemulsification, which uses a very thin probe to transmit ultrasound waves that emulsify the cataract for removal.
In the late 1700s, the smallpox epidemic ravaged the country. The infection had residual effects on the eye, including occluded pupils. To treat occlusion, Dr. Physick invented punch-forceps, which were used to remove a piece of the iris to create an artificial pupil. Later, George Strawbridge, MD, Professor of Diseases of the Eye and Ear at UPenn, also made strides in artificial pupil surgeries by inventing a pair of fine scissors to make a very small incision in the cornea and provide access to the iris.

William Gibson, MD, who succeeded Dr. Physick as Professor of Surgery at UPenn in 1819, noticed that the “dissolution” method used by Dr. Physick and other surgeons was flawed in that it would sometimes cause the lens to be pushed into the vitreous humor. To correct this issue, Dr. Gibson invented a pair of scissors with knife-like edges that could cut the cataract lens in-situ without damaging other parts of the eye. The shut blades of the scissors were used to force the pieces of the cataract into the anterior chamber of the eye to be absorbed.
Illustration of the tensor tarsi muscle in Dr. William Edmonds Horner’s article “Description of a Small Muscle of the Inner Commissure of the Eyelids.” Courtesy of King’s College London.

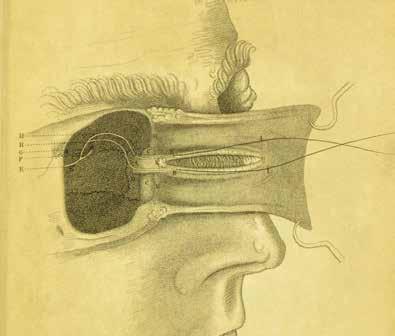
William Edmonds Horner, MD was appointed Adjunct Professor of Anatomy at UPenn in 1819 and later Professor of Anatomy in 1832. With a particular interest in the eye, Dr. Horner performed minute dissections and was the first to identify muscle fibers that extended along the lacrimal canal. These muscle fibers formed the tensor tarsi muscle, now called the Horner’s muscle. The discovery explained how tears traveled from the conjunctival sac to the nose.

While he did not receive credit because he was not the first to record the surgery, Dr. Gibson was the first surgeon to perform an operation to correct strabismus, colloquially known as “crossed eye,” by dividing the rectus internus muscle. The operation occurred in 1818. While Dr. Gibson’s method was later successful and commonly used by other surgeons, Dr. Gibson stopped performing the surgery after several failed attempts at curing strabismus and on the advice of Dr. Physick.
William F. Norris, MD, first Chairman of the Department, and his colleague William Thomson, MD were the first to reproduce objects seen in a microscope by using wet-plate photography. To do so, the physicians coated the microscope objective with oil in the days prior to photographing, then used a Welsbach gas burner with a diaphragm as the light source. The photographs of the retina were ready after 10 hours of exposure. Through this new technique, Dr. Norris was able to document his clinical cases using pictures.
Portrait of Dr. William Gibson. Retrieved from University of Pennsylvania Archives. Photograph of the retina taken by Dr. William F. Norris using wet-plate photography. Courtesy of Daniel Albert, MD.Samuel Doty Risley, AM, MD, LLD worked in the eye infirmary at UPenn as the Assistant Surgeon in the Dispensary of Diseases of the Eye and as Chief of the eye clinic in 1872. Dr. Risley was the first in Philadelphia to correct a case of mixed astigmatism. In 1899, he invented the rotary prism: an optometer with two overlapping prisms that rotated independently of each other and in opposite directions. The invention measured visual acuity as a function of distance using only two prisms—much more efficient than the previous method, which required a whole set of prisms of varying strengths. The Risley prism is still commonly used today, both in medicine and beyond. The prisms are used to stabilize motion in astronomical telescope photographs and can be found in barcode scanners and scanning spectrometers, among many other applications.

In 1890, George E. de Schweinitz, MD, second Chairman of Ophthalmology, was the first to prove that quinine produced toxic changes in the eye. These effects were termed quinine amaurosis. Dr. de Schweinitz’s study led to several others in the Department determining potential toxins, such as lead, methyl alcohol, salicylic acid, and mescal beans.
In the 1880s, Dr. Risley co-led a large-scale eye study on 1,200 Philadelphia public school children. During the study, Dr. Risley noticed several drawbacks of existing optometers and ophthalmoscopes. He made many suggestions on how to improve these tools, such as the addition of cylindrical lenses to the ophthalmoscope, which could be used to quickly identify and correct astigmatisms. Dr. Risley and his colleagues used data from their study to make recommendations on how to improve students’ eye health in school. They developed an equation to calculate the number of square feet of windows necessary for adequate lighting in the classroom, which Dr. Risley believed contributed to the development of myopic vision. After he lobbied state and local officials, schools across the country used the equation to ensure proper lighting. Dr. Risley also suggested that all children be screened for poor eyesight before entering school. These eye examinations are still required in schools today.

Read on to learn about the Department’s modern contributions to the field of ophthalmology! n
Albert, D. M., & Scheie, H. G. (1965). A history of ophthalmology at the University of Pennsylvania. Springfield, Illinois: Charles C. Thomas.
Carter, W., Shrestha, R., Slatton, C., Shrestha, K., & Cossio, T. (2005). Geodetic Laser Scanning: Refractive Optics Offer Wide Variety of Scan Patterns. AGU Fall Meeting Abstracts.
Frank, V. F. (1902). THE MEDICAL SOCIETY OF THE COUNTY OF NEW YORK: STATED MEETING, HELD APRIL 28, 1902. Medical Record (1866-1922), 61(20), 797. Mayo Clinic Staff. (n.d.). Cataract Surgery. Mayo Clinic. Retrieved from https://www.mayoclinic.org/tests-procedures/cataract-surgery/about/pac-20384765
Ring, G. O. (1920). SAMUEL DOTY RISLEY, A.M., M.D., LL.D. Trans Am Ophthalmol Soc. 1920;18:12.2–20. PMCID: PMC1318219.
University Archives & Records Center. (n.d.). George Strawbridge. Retrieved from https://archives.upenn.edu/exhibits/penn-people/biography/george-strawbridge/
Research has been a cornerstone of the Ophthalmology Department’s mission since its inception in 1874. Today, the Department is a uniquely translational research center. In addition to exhibiting a strong commitment to ocular research, nearly every scientist is also a practicing clinician.

Since 2010, the Department has conducted over 250 clinical trials and studies, allowing for the testing of novel diagnostics and treatments. Below, we highlight three major areas of research as examples of the Department’s diverse and impactful science today.
Established in 1994, the Center for Preventive Ophthalmology and Biostatistics (CPOB) is an internationally recognized leader in the design and execution of clinical trials in ophthalmology. The Center has led a number of multi-center clinical trials over the years. One of the most impactful
trials was the Comparison of Age-Related Macular Degeneration Treatment Trial (CATT).

The $26M CATT trial assessed the relative safety and efficacy of two treatments for neovascular age-related macular
degeneration (AMD). AMD is one of the largest causes of visual impairment in people over the age of 60 in the developed world. Neovascular AMD, which accounts for 90% of cases of severe vision loss, results from the growth of abnormal leaky blood vessels under the retina, partly
Jean Bennett, MD, PhD, Albert Maguire, MD, and Samuel Jacobson, MD, PhD are among the recipients of the 2018 €1M António Champalimaud Vision Award. Photo credit: Rui Ochoa. Researchers at the Center for Preventive Ophthalmology and Biostatistics (CPOB).35 due to excess amounts of the vascular endothelial growth factor (VEGF) protein. Within the United States alone, $10 billion is spent each year on the treatment of AMD.
In the early 2000s, two novel antiVEGF drugs emerged on the market. Ranibizumab (Lucentis) was approved by the FDA in 2006 for treatment of neovascular AMD. Prior to the drug’s approval, many ophthalmologists prescribed a very similar drug called bevacizumab (Avastin), which was approved by the FDA for the treatment of specific cancers. The biggest difference between the two drugs was not in efficacy but in cost: off-label Avastin cost $50-$100 per dose for AMD, while FDAapproved Lucentis cost $2000 per dose.
Launched in 2007 with the participation of 44 clinical centers, the CATT trial aimed to compare the safety and efficacy of Avastin and Lucentis for the treatment of neovascular AMD. The trial also explored the efficacy of a reduced dosing schedule in decreasing neovascularization activity at the macula. The study team included the Ophthalmology Department’s Maureen Maguire, PhD, Gui-shuang Ying, PhD, Juan Grunwald, MD, Ebenezer Daniel, PhD, and Stuart Fine, MD.
The study ultimately found that both Avastin and Lucentis were effective
and safe for treatment of neovascular AMD. The drugs provided equivalent visual outcomes for the treatment of neovascular AMD. These results were published in the New England Journal of Medicine and later replicated in five clinical trials conducted abroad.
The study’s findings greatly increased the confidence of ophthalmologists in prescribing off-label Avastin for treatment of neovascular AMD. Doing so resulted in enormous cost savings: using conservative estimates, the price differential between the treatments is roughly $26,800 per patient annually, leading to Medicare savings of up to $3 billion per year. In many countries, the affordability of Avastin has allowed for more patients to receive treatment for neovascular AMD.
The rich CATT dataset has led to a number of follow-up studies over the years. For example, a five-year follow-up study in 2016 evaluated the long-term effect of anti-VEGF drugs on patients’ vision. The study found that, following five years of anti-VEGF treatments, 50% of individuals increased to and/ or maintained 20/40 vision, while 20% decreased to 20/200 vision or worse. This demonstrates a significant improvement over outcomes of previous AMD treatments.
It is no surprise that the CATT trial was characterized by a New England Journal of Medicine editorial as “the most noteworthy in health outcomes research to date.”
Another growing area of research in the Ophthalmology Department is genetic studies, particularly with the inclusion of diverse populations in study cohorts. As of 2019, African ancestry populations made up only 2% of participants in genetic studies worldwide. One example of a large genetic study in the Ophthalmology Department that addresses this disparity is the Primary Open-Angle African American Glaucoma Genetics (POAAGG) study.

Primary open-angle glaucoma (POAG) disproportionately affects individuals of African descent. These individuals are five times more likely to be diagnosed with POAG and up to 15 times more likely to experience glaucomatous vision loss than other ethnic groups. However, the majority of genetic studies on POAG have been conducted in European populations.

The POAAGG study aims to address this unmet need. Led by Principal Investigator Joan O’Brien, MD, the study was funded for $11.25M by the NIH in 2014, with a $6.6M renewal in 2021. The main goal is to elucidate the genetics of POAG in African ancestry individuals, with the long-term aim of developing more targeted diagnostic and therapeutic interventions for these patients.
The study team enrolled over 10,200 individuals of African descent from the greater Philadelphia area. These subjects were recruited primarily from the Ophthalmology Department and satellites, as well as from several collaborating sites, including the Philadelphia VA Medical Center, Temple University, and a private practice of a Scheie Eye Institute alumnus (Windell Murphy, MD).
Community outreach was an essential part of recruitment for the study. The team collaborated with community leaders to host free glaucoma screenings at churches and schools throughout the city. Efforts were also made to raise awareness about glaucoma risk and to offer free screenings with glaucoma specialists through a citywide campaign, including a collaboration with WURD Radio. The successful recruitment of subjects in the study has been attributed to the development of a relationship with the Black community in Philadelphia over the years.
Currently, researchers are using a genome-wide association study, wholeexome sequencing, and whole-genome sequencing to understand how genetics
contribute to risk of developing POAG. The POAAGG team is also working closely with the Scheie Image Reading Center to conduct in-depth analysis of how optic disc features contribute to glaucoma incidence and progression.
The POAAGG team will continue to expand this research at the newly established Penn Medicine Center for Ophthalmic Genetics in Complex Diseases, of which Dr. O’Brien is the Director. The mission of the Center is to elucidate the genetics of diseases that overaffect minority populations.
Gene therapy has long been an area of enormous potential and promise, but until recently, was marked by years of failures and disappointments. These setbacks did not deter researchers in the Ophthalmology Department, who after several decades of research, received FDA approval for the first gene therapy for an inherited disease (Luxturna) in 2017. Gene therapy is now a burgeoning area of research in the Ophthalmology Department, with scientists developing similar products for other blinding diseases.
The research leading to Luxturna began back in the 1990s, when Jean Bennett, MD, PhD and Albert Maguire, MD began exploring the possibility of restoring vision through delivery of “normal” genes to correct a genetic mutation. In 2000, they had great success in testing a gene therapy procedure in dogs with retinal

disease caused by a RPE65 mutation. Over the following years, the team worked relentlessly to translate this finding to human clinical trials. The results of the clinical trials were nothing short of astounding, with dozens of blind patients gaining and maintaining vision.
Building off this success, the Penn Center for Advanced Retinal and Ocular Therapeutics (CAROT) was established in 2014, with Drs. Bennett and Maguire as Co-Directors. The goal of CAROT is to develop novel biologic and small molecule therapeutics for retinal and ocular diseases. Currently, there are more than 265 genes known to cause inherited retinal disease.
In December 2017, Luxturna received FDA approval. The therapy was developed in collaboration with Spark Therapeutics and is now available at designated treatment facilities throughout the country. As result of this breakthrough, Dr. Bennett, Dr. Maguire, and Samuel Jacobson, MD, PhD received the €1M António Champalimaud Vision Award in 2018, which is given to the scientists with the greatest contribution to vision research worldwide.
Luxturna has not only restored sight to many patients, but has also paved the way for similar products for other retinal degenerations. There are currently over a dozen gene therapy targets in the pipeline for clinical trials at CAROT. In 2021, the biotech startup called Opus Genetics was launched with $19M in seed funding, with the goal of developing new gene therapies to treat rare inherited retinal diseases. n
Jean Bennett, MD, PhD, and Albert Maguire, MD with the dogs that received the successful gene therapy. Photo credit: Peggy PetersonPhotos from left to right: The Medical School Building of the University of Pennsylvania from 1765 to 1802, located on the east side of Fifth Street between Liberty (Chestnut) and Walnut Streets. Courtesy of Albert, D. M., & Scheie, H. G. (1965). A history of ophthalmology at the University of Pennsylvania.
Important ophthalmology texts available to the American physician in 1850. Courtesy of Albert, D. M., & Scheie, H. G. (1965). A history of ophthalmology at the University of Pennsylvania.

Medical School lecture hall with students sitting at desks in 1920. Retrieved from University of Pennsylvania Archives.
Medical student Teja Alapati, class of 2020, conducting research during his gap year.

Scheie residents, early 1970s. Courtesy of Ralph C. Eagle, Jr., MD.
Residents in the operating room observing ophthalmic surgery. Courtesy of Ralph C. Eagle, Jr., MD.
The Department of Ophthalmology at the University of Pennsylvania (UPenn) has provided a legacy of outstanding medical education. With superior medical student, resident, and fellowship training, the Department continues to propel its educational mission to new, unmatched heights. This history of excellence began back in the late 1700s.
The first medical school in the American colonies was founded at UPenn in 1765. To further this pursuit of education, UPenn developed a number of professional schools, all of which are now highly regarded.
For the first one hundred years of the medical school, ophthalmology specialists and lectures were rare. The medical curriculum was divided into seven branches, including anatomy, physiology, chemistry, materia medica, therapeutics, institutes of medicine, obstetrics, and surgery. The only education on
ophthalmology came from the few professors of anatomy and surgery who chose to lecture on this field.
In 1874, the Hospital of the University of Pennsylvania (HUP) was founded at its current location to serve as a teaching hospital for medical students. The hospital is recognized as the oldest university-owned teaching hospital in the nation.
The Department of Ophthalmology at HUP was also founded in 1874, with William F. Norris, MD appointed the first Professor of Ophthalmology. Dr. Norris was committed to advancing ophthalmic education and began to present weekly ophthalmology lectures to interested students in an anatomical amphitheater. The lectures became a formal part of the curriculum in 1879.
The late 1800s experienced significant changes in the number of required years for both medical school and courses related to ophthalmology. In 1885, the first elective course in ophthalmology was offered to senior


students at UPenn, a time when students had very limited experience in ophthalmic surgery.
Succeeding Dr. Norris, George E. de Schweinitz, MD became the second Chairman of the Department in 1902. Dr. de Schweinitz advocated for ophthalmology to be taught to all medical students, as the eye is commonly affected in many diseases. During his term, Dr. de Schweinitz presented clinical lectures and demonstrations and offered students practical work in the eye dispensary. Students were also encouraged to observe surgeries and conduct research in the newly created pathology lab.
In 1937, Francis Heed Adler, MD, fourth Chairman of the Department, established the Ophthalmology Residency Program, the first program introduced at UPenn. There were only two residents in 1937, one of them being Harold G. Scheie, MD, who later became the fifth Chairman of the Department and founder of the Scheie Eye Institute. The program consisted of three years, in which the first year was mostly spent in the graduate school and the last two years spent completing clinical work.
The residency matching system was not yet created at this time. Instead, it was common for a committee within the residency program to review applications and select candidates.
At this time, the residents’ schedules were not as busy and demanding as they are today. Most afternoons were dedicated to independent study or research, and residents rarely performed surgery before their senior year.

With the help of the new hospital at the Philadelphia Veterans Affairs Medical Center (VAMC), which opened in 1952, the residency program continued to expand and mature. The Department of Ophthalmology was chosen as the sole ophthalmic provider for the new facility, providing more learning opportunities for medical students, residents, and fellows.
During Dr. Scheie’s time as Chairman (1960-1977), residents began to stray from the three-year program and pursue five- to six-year residency programs. Training included research and advanced study in a basic science field related to ophthalmology. Under Dr. Scheie’s leadership, the size of the program increased to 12 residents. In 1960, the first female resident was appointed by Dr. Scheie.
In the early 1960s, UPenn had a separate Graduate School of Medicine with departments headed by individual Chairmen. In 1964, the graduate school merged with the undergraduate school and became a formal division of the School of Medicine.
Dr. Scheie also helped to establish an alumni association for graduated residents to stay connected to and collaborate with peers and the Department. Initially called the Adler Society, the foundation was renamed the University of Pennsylvania Alumni Ophthalmological Association. Membership was soon made available to all graduates of UPenn who were practicing ophthalmology, regardless of where they completed their graduate training. Funds raised by the group contributed to the creation of the new Scheie Eye Institute, which officially opened in 1972.
In 1977, during the chairmanship of Myron Yanoff, MD, the Ophthalmology Residency Matching Program was established by the Association of University Professors of Ophthalmology (AUPO). The program requires medical students to submit an application, interview at various institutions, and rank their top residency programs. Based on the applicant’s and institution’s rankings, the individual will be matched to an ophthalmology residency program.

Consistently ranked among the top medical schools in the nation, the Perelman School of Medicine at UPenn has continued its tradition of preparing students with the necessary knowledge
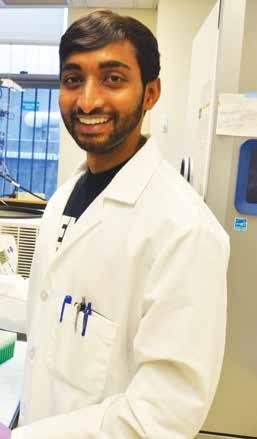
and skills to become experts in their respective fields. Currently, more medical students are pursuing ophthalmology than ever before. Over the years, Penn medical students continue to match at top ophthalmology residency programs across the country.
Perelman also offers students the opportunity to take a gap year during medical school. This year may be spent conducting research, exploring specialties, completing another degree program, and/or developing relationships with mentors. Over the years, many medical students have elected to take a gap year to pursue research projects related to ophthalmology. These projects span all 17 ophthalmic subspecialties offered by the Department.
Just as the number of medical students interested in ophthalmology has increased, the number of residents at Scheie has grown from just two residents in 1937 to 15 in 2022. Ophthalmology residents complete the program over three years, during which they progress from the general eye examination to subspecialty work. By year three, residents are involved in more surgeries and microsurgeries, particularly cataract surgeries.
The Department’s surgical experience for residents has significantly increased over the years. The Philadelphia VAMC played a large role, with the addition of an extra operating room at the facility contributing to increased surgical volumes. The operating room provided supplementary
educational opportunities, allowing for the addition of a second rotation for surgical senior residents.
Residents also have the opportunity to participate in the Department’s collaboration with Aravind Eye Hospital in Southern India. Scheie residents may visit Aravind during their elective time in the third year of residency for four weeks to gain further insight and experience in the field.
Penn Ophthalmology’s Residency Program has consistently ranked in the top ten in the nation for research output per alumnus and in the top 1% nationwide for the number of grants and trials per alumnus. These stats are a testament to the exceptional training and mentorship residents receive throughout the program.

Following graduation, residents may apply to fellowships in subspecialty areas such as cornea, glaucoma, retina, oculoplastics, pediatrics, and neuroophthalmology. Scheie residents have an impressive history of matching with highly competitive fellowship programs across the nation.
The Department offers fellowships in retina, glaucoma, neuro-ophthalmology, oculoplastics, and pediatric ophthalmology. Fellows work closely with faculty and are actively involved in patient care and surgery.
The Department of Ophthalmology is
committed to caring for underserved populations, a mission that is also prioritized by trainees. Penn Sight Savers is a student-run program that educates the Philadelphia community on the importance of regular eye exams, and offers free glaucoma screenings to patients across the city. Medical students collaborate with glaucoma specialists to host screening stations at local health fairs and community events.
Additionally, medical students and residents frequently volunteer their time at Puentes de Salud, a healthcare clinic that treats the Latino population of Philadelphia. Trainees and physicians provide comprehensive ophthalmic care to patients who are often uninsured and undocumented.
In July 2021, the Department received a $1 million grant from the Benjamin & Mary Siddons Measey Foundation to renovate and expand the Department’s existing ophthalmic surgery training laboratory. The renovated space will provide trainees the opportunity to learn and master techniques used in the operating room (read more about the laboratory in “The Measey Surgical Skills Center at the Widener Library” on page 42).
Over the last 150 years, the Department of Ophthalmology has become a global leader in patient care, research, and education. The Department provides the foundation for top minds in the field to prosper and become the next generation of experts in ophthalmology. n
Albert, D. M., & Scheie, H. G. (1965). A history of ophthalmology at the University of Pennsylvania. Springfield, Illinois: Charles C. Thomas. Frayer, W. C. (2002). An ophthalmic journey: 50 years at the University of Pennsylvania. William C. Frayer, M.D.
Friedman, S. M. (1996). A brief history of the University of Pennsylvania. University of Pennsylvania Archives and Record Center. Retrieved from https://archives. upenn.edu/exhibits/penn-history/brief-history/
Former Chairmen Francis Heed Adler, MD (left) and Harold G. Scheie, MD (right). Photo by Laurel M. Weeney. Retrieved from Harold Glendon Scheie, M.D. Ophthalmology Oral History Series. A Link with Our Past. Sally Smith Hughes Foundation of the American Academy of Ophthalmology, 1988.

“They were truly leaders and they convinced me that my future was in my own hands. Under their constant prodding, I began to do things I had never thought possible. These two men helped me to believe in myself,” wrote the late William C. Frayer, MD of his mentors Harold G. Scheie, MD and Francis Heed Adler, MD. Dr. Frayer, who joined the UPenn Ophthalmology faculty in 1952, was a resident at UPenn while Dr. Adler was Chairman.
Throughout the Department’s history, mentorship has played a large role in allowing physicians and researchers to achieve fulfillment and professional success, despite the inevitable obstacles of a rigorous medical career. Mentors, whether formal or informal, have used their experiences and perspective to guide those facing similar challenges. They have offered support when needed and given space for independence when not.
Drs. Scheie and Adler themselves had a strong working relationship built upon mentorship. Dr. Scheie joined the Department in 1937 as one of the first residents while Dr. Adler was Chairman. When Dr. Scheie was interviewed by science historian Sally Smith Hughes, he discussed how Dr. Adler allowed him space to flourish and encouraged his specific medical interests: “As I stayed in practice with him, I was given increasing responsibility in the department and the opportunity to build my own patient following and referral sources. He was not as interested in surgery as I was and delegated certain types to me. Later he recognized my interest in glaucoma and I saw most of the glaucoma patients.”
Decades later, senior faculty continue to work with junior faculty to involve them in both clinical cases and research projects that particularly interest them. Chairmen also continue to support faculty members
through mentoring. Joan O’Brien, MD, Chairman Emeritus, remarked, “The Chairman regularly meets with the junior faculty to facilitate requests, review grants, and provide advice and resources.” Senior faculty members, including Dr. O’Brien, agree that their mentors were instrumental in their successes, which makes them eager to provide their own support as mentors. And with the complex tenure track system of a teaching hospital, which requires reaching rigorous grant, publication, and other milestones, junior faculty are appreciative of this guidance.
“Mentorship can come in the form of providing guidance in day-to-day clinical practice and during surgeries, answering questions, and teaching,” noted Eydie Miller-Ellis, MD. “And then there is mentorship on how to progress up the academic ladder—how to make contacts in the field.”
Eydie Miller-Ellis, MD works with other glaucoma specialists and volunteers at an outreach event at a North Philadelphia Health Fair. Photo credit: Peggy Peterson.
Dr. Miller is the Chief of Glaucoma Services, as well as the Vice Chair for Faculty Affairs. She is known for the strong connections she has cultivated in the glaucoma group, and she goes out of her way to support the junior faculty and staff.
“I can suggest a mentee for a talk at an outside organization, opening the first door, and then the floodgates open— they are invited to speak at several more talks because they are recognized for their talent,” explained Dr. Miller.
Dr. Miller has also found it important to mentor other women in the Department: “There are a lot of challenges that women face along the way that men don’t necessarily face, and it’s nice to talk about it and use my insight to help guide other women.”
Due to similar sentiments, Prathima Neerukonda Atluri, MD, Assistant Professor of Clinical Ophthalmology, founded the Penn Ophthalmology Women’s Association (POWA) in 2018. The group’s aim is to provide a supportive environment for discussions among female ophthalmologists and

to foster mentoring among this group. POWA has hosted successful events such as a social get-together at the Continental Midtown in Center City and a symposium with invited speakers to discuss leadership and physician burnout. More recently, the COVID-19 pandemic has hindered in-person events, but the group is looking forward to re-starting in-person events soon.
The Department also offers more formal mentorship initiatives specifically with promotional goals in mind. These initiatives have allowed faculty to achieve continued professional success. Dr. O’Brien remarked: “Over the last 12 years, every faculty member has been promoted, due to young scientific talent and the very committed mentorship of young faculty by senior faculty mentorship committees. Maureen Maguire set up a formalized mentorship committee for the K12 program.”
The National Eye Institute funds K12 Clinical Scientist Institutional Career Development Program Awards, which aim to prepare newly trained clinicians for research roles.

“The K12 scientists and the young R01 scientists present formally on their progress, accompanied by their primary mentor,” Dr. O’Brien continued. “After the presentations, we have a 15-minute deep discussion and generate a formal report for each young scientist and their primary mentor.” The junior faculty is regularly provided constructive feedback and suggestions to further develop their research skills.
“The Department of Ophthalmology Committee on Appointments and Promotions (DCOAP) allows another opportunity to look at every reappointment and see where mentors can take on responsibilities to advance areas of junior faculty careers,” remarked Dr. O’Brien. DCOAP is the entity that approves promotions, so feedback from the committee is valuable.
The Department, throughout history and today, is invested in fostering a supportive environment that encourages personal and professional growth at every level. As expressed by Dr. O’Brien, “The ‘Scheie Family’ rejoices in every person’s individual success.” n
Frayer, W. C. (2002). An ophthalmic journey: Fifty years at the University of Pennsylvania. Philadelphia: Scheie Eye Institute.
Harold Glendon Scheie, M.D. (1988). Ophthalmology Oral History Series. A Link with Our Past. Sally Smith Hughes Foundation of the American Academy of Ophthalmology.
In July 2021, the Department of Ophthalmology received a $1 million grant from the Benjamin & Mary Siddons Measey Foundation to renovate and expand the Department’s existing ophthalmic surgery training laboratory. Located in the Widener Library in the basement of the Scheie Eye Institute, the new center will be named the Measey Surgical Skills Center at the Widener Library.
The new space will encompass both a wet lab and simulator training facility to allow medical students, residents, and fellows to learn and master techniques used in the operating room. With renovated space and state-of-the-art equipment, the lab will allow ophthalmology trainees to safely and efficiently practice basic and advanced surgical techniques. Because the space closely resembles an actual operating room, the skills acquired can be readily translated to patient procedures.
Given the complex nature of most ophthalmic procedures, the newly equipped center will augment medical student, resident, and fellow surgical training, and promote a collaborative learning environment. The Skills Center will also be a space for ophthalmologists— both within and outside of Scheie—to advance their expertise with access to the most sophisticated instrumentation and
By Kristen Mulvihilltechnologies in the field.
The new Skills Center will consist of approximately 10 workstations and will include equipment from distinguished ophthalmic vendors, including HaagStreit. The Skills Center will feature brand new microscopes and high-quality, durable instrument sets. State-of-theart video monitors and recorders will also be included, allowing instructors to engage with students and residents to record training for both review and documentation. The center will continue to serve as a library, with a vast medical education book collection and bookshelves lining the walls. The new space will also include a devoted instruction and lecture area for professorstudent learning.
This effort is led by Victoria Addis, MD, Assistant Professor of Ophthalmology and Associate Program Director for the Residency Program, and Christina Moon, MD, Assistant Professor of Clinical Ophthalmology.

“The future Measey Surgical Skills Center at the Widener Library will enable students, residents, and fellows at the Scheie Eye Institute to gain essential, unmatched surgical experience as well as create a platform for innovation and

collaboration within ophthalmic surgery and research,” said Dr. Addis.
“I would like to express my sincere gratitude to the Benjamin & Mary Siddons Measey Foundation for this extremely generous support to build a state-ofthe-art Surgical Skills Center to train our residents, medical students and colleagues on the most advanced surgical techniques in the field of ophthalmology,” said Joan O’Brien, MD, Chairman Emeritus of the Department.
The Benjamin & Mary Siddons Measey Foundation was founded in 1957 by William Maul Measey, a Philadelphiabased lawyer and philanthropist. The Foundation supports medical education in the Philadelphia area, funding various scholarships and fellowships. The foundation also provides support to cutting-edge programs at medical schools throughout the city.
The Measey Surgical Skills Center at the Widener Library will significantly propel the Department’s mission to train the next generation of world-class ophthalmic surgeons, as well as improve patient safety and outcomes. The well-resourced space will augment and enhance the tradition of excellence and mastery at the Scheie Eye Institute. n
Ophthalmology residents in the Department’s current wet lab.
Our faculty have traveled all over the world to care for underserved populations.
Historically, most academic and medical institutions have been occupied by white males. Although many strides have been made towards inclusion of diverse populations, there is still much room for improvement. As of 2020, approximately 51% of full-time professors at postsecondary institutions were Caucasian males, while Black and Hispanic males and females only made up 8% of that group.
Over the years, the number of women and minority faculty in the Ophthalmology Department has drastically increased (see infographic on page 43). The Department has become a place where people of different cultural, religious, and racial backgrounds can nurture and share their talents.
To further promote these goals, the Department created a Diversity, Equity, and Inclusion (DEI) Committee in 2021. This team of physicians and staff work together to promote staff development, address potential concerns voiced by employees, and serve as an unbiased liaison between staff and leadership. The committee evaluates suggestions about various departmental workflows and processes, and promotes the institution’s overall mission of creating a safe, inclusive, and positive work environment.
Eydie Miller-Ellis, MD, Vice Chair for Faculty Affairs, serves as one of the committee’s founding faculty members. “The Scheie DEI Committee promotes an equitable, supportive work

environment where the unique talents and contributions of individuals are appreciated and respected,” she said. “During COVID, our sense of community has declined. The inability to congregate in the workplace or have departmental social events left a lot of our staff feeling isolated and made it difficult for new staff to feel that they were part of Scheie. Thus, community building is also part of the committee’s mission.”
Below, we interview several ophthalmologists of color within the Ophthalmology Department. They explain their views and experiences surrounding race, equity, and diversity within the scope of healthcare and outside of it.
“Embracing core values related to inclusion, diversity, and equity is critical to the success of any organization, particularly those institutions which are focused on health care. Innovation is greatest when there are diverse perspectives that contribute to the solution of any strategic objective and it has been shown that organizations which have diverse boards and executive leadership are more profitable. What could be more important than a highly innovative and profitable organization? Well, in healthcare, it is critical that we deliver the highest quality care that is effective in ensuring the individuals and populations we serve. Therefore, having a diverse workforce ensures that we are reflecting the community we serve and delivering care with cultural humility. By delivering culturally relevant care, we can enhance our health outcomes, particularly when compliance is an important component of our patient’s healing and disease management process.”
EveQWhy is it important to promote diversity, equity, and inclusion within an organization?
–
J. Higginbotham, SM, MD, ML, Vice Dean for Penn Medicine’s Office of Inclusion, Diversity, and Equity, and Professor of Ophthalmology
“I think the better answer to the question is why you wouldn’t ensure diversity, equity, and inclusion within an organization, particularly healthcare or eye care? The argument should never be to sell an organization on this idea, but to outline how, by eliminating the smaller groups of people based on gender, race, sexual orientation, age, disability, etc. eliminates a population that might add depth to any element your organization wishes to study. Expanding your population opens the door for more talent and perspective and provides a more realistic sample of the population. (As an example, you can look at a working Black woman, Mary Kenner, who developed a wearable sanitary belt; by including the diversity of race, gender, and working class, they were able to revolutionize women’s health).
Fairless & Nwanyanwu et al (2021) addressed the importance of addressing disparities in eye care in a journal article. Even now, racial and ethnic minority groups are at greater risk of losing vision from eye diseases, such as glaucoma, cataracts, and diabetic retinopathy. Our ability to provide better care across populations means 1) identifying if there is a difference, 2) understanding why there is difference, and 3) finding the right equation to “treat” or “equilibrate” this difference. Additionally, the lack of DEI within any organization can absolutely influence how that organization operates. Vaughn & Elam et al (2021) outline that burnout, or emotional or psychological stress experienced by medical staff, is associated with medical errors, lower patient satisfaction, longer post-discharge recovery times, and decreased professional work effort. These are all endpoints that can affect the organization’s productivity.
Traditionally, DEI has been focused on the individual; however, I believe the more appropriate focus is on changing institutional perspectives. Elam et al and I agree that we consider the racialized character of medicine as an organization, shifting our focus away from individuals, to find solutions to the issues of health inequity and lack of diversity within ophthalmology and medicine.”
– Ahmara Ross, MD, PhD, Assistant Professor of Ophthalmology
“Pause – take a moment and look around the room and see if the room reflects a diverse group of opinions, experiences, and backgrounds. Also, pause to see if the atmosphere allows for diverse opinions to be expressed or is confined to group thinking. If the room is not diverse enough or safe enough for diverse opinions, but you are not in a position to change anything, at least think about how you would/ could improve the situation, because you never know when the opportunity to implement those ideas may arise.”
– Vivian Lee, MD, Assistant Professor of Ophthalmology
“I think listening is a good place to start. Sometimes we cannot identify a problem unless someone else brings it to our attention. Having a diverse workforce often means that more ideas are generated and more accurate solutions are discovered. This act can make good intentions even better.”
– Prithvi S. Sankar, MD, Professor of Ophthalmology, Director of Medical Student Education, and Advisory Dean of Perelman School of Medicine
QWhat can people do within their job scope to promote diversity and inclusion throughout their institution?
“I am a young, black, woman clinician-scientist at an Ivy League Institution. My education, training, surgical skills, and scientific knowledge is consistently called into question. I am often interrupted mid-sentence during meetings, told I am being too assertive to other colleagues, or I’m often asked to do additional things, such as developing aims for individuals for DEI initiatives. This plays into burnout or physical stress experienced by URM faculty, otherwise known as the ‘black tax.’”
– Ahmara MD, PhD, Assistant Professor of Ophthalmology“Diverse individuals offer more diverse viewpoints that in turn benefit more people. Organizations with broad
gender, and socioeconomic diversity are better equipped to address challenges. We must be sensitive to the needs of our patients, particularly those from underserved communities who often receive less from our system but need so much more. Health disparities and access to care continue to be a problem in America. We all need to be part of the solution. The reason all of us work at Scheie is to take care of patients. They trust us to do the best for them. We need to listen, treat people with respect regardless of socioeconomic status, and to do the best for them that we can. And we also have to do the best for each other.”
Fairless, E. A., Nwanyanwu, K. H., Forster, S. H., & Teng, C. C. (2021). Ophthalmology Departments Remain Among the Least Diverse Clinical Departments at United States Medical Schools. Ophthalmology, 128(8), 1129–1134. https://doi.org/10.1016/j.ophtha.2021.01.006

National Center for Education Statistics. (2022). Race/ethnicity of college faculty. IES/NCES Fast Facts. https://nces.ed.gov/fastfacts/display.asp?id=61
Scott, A. W., Elam, A. R., & Nwanyanwu, K. (2021). Addressing Disparities in Eye Care—The Time Is Now. Archives of Ophthalmology (1960), 139(9), 935-936.
Vaughn, D., & Elam, A. (2021). Addressing Structural Racism: Towards an Organization-Theoretical Approach. American Journal of Ophthalmology, 232, A1-A3.
QWhat has influenced your thinking around DEI and motivated you to be an advocate for change?
ethnic,
– Eydie Miller-Ellis, MD, Professor of Clinical Ophthalmology, Vice Chair for Faculty Affairs n
QWhat are some common biases that you have experienced or noticed within your individual field/specialty? How can we alleviate these biases?
Ross,Eydie Miller-Ellis, MD, screens patients at an outreach event. Photo credit: Peggy Peterson
The Primary Open-Angle African American Glaucoma Genetics (POAAGG) study aims to elucidate the underlying genetics of glaucoma in the overaffected African ancestry population. As part of this study, the team conducted a city-wide glaucoma awareness campaign to increase

awareness of the elevated risk of glaucoma in African ancestry populations and to provide free glaucoma screenings to these individuals.
In 2014, Principal Investigator Joan O’Brien, MD was awarded an $11.2M grant
from the National Eye Institute to enroll more than 10,000 subjects in the POAAGG study and to conduct genetic analyses on these individuals. In 2021, the research team received a $6.6M grant renewal to continue their work. The study recruits solely
African American participants The Department of Ophthalmology serves many diverse populations throughout Philadelphia and beyond. Community outreach and engagement have always been an integral part of the Department’s mission, and over the years, faculty, students, and staff have selflessly given their time and discovered creative ways to nurture this goal. In this section, we examine several key community outreach programs and discover one of the driving missions at the heart of this Department. A community member receives a free glaucoma screening at an event hosted by the POAAGG team and publicized by WURD radio. Photo credit: Peggy Petersonbecause primary open-angle glaucoma (POAG), the most common form of glaucoma, disproportionately affects African Americans compared to other ethnic groups. Despite being disproportionately affected by glaucoma and other diseases, the majority of clinical trials and genetic studies have been conducted in mostly European American populations. As of 2019, only 2% of participants in genetic studies were individuals of African descent.
When recruiting participants for the POAAGG study, it was important to consider the hesitation that people of color might have around participating in genetic research. In an October 2020 poll, 7 out of 10 Black Americans said that they are treated unfairly by the healthcare system and 55% percent said they distrusted it. The POAAGG study sought to disprove deepseeded stereotypes about the medical community by providing opportunities to receive quality care and be a part of innovative research.

In 2018, Dr. O’Brien and her team launched the Philadelphia-wide glaucoma awareness campaign. Their goals were to increase research participation in the POAAGG study, while also spotlighting the severity of glaucoma in the African American community. Most importantly, they offered free glaucoma screenings at the Scheie Eye Institute to any interested individuals.
The campaign was conducted in close
collaboration with major community leaders of Philadelphia. This helped to ensure that participants were treated with the utmost respect, properly informed about their treatment options, and given the opportunity to participate in meaningful research. At community outreach events, free glaucoma screenings were provided to all attendees.
The most impactful collaborator in this campaign was a well-established community representative for people of color in Philadelphia. WURD Radio, a pillar in the Philadelphia African American community, is the only Black-owned and -operated radio station in Pennsylvania, and one of few throughout the country. WURD Radio was founded by Dr. Walter Lomax, a respected and well-known physician who spent his career providing quality healthcare services to communities of color. His daughter and current CEO, Sara Lomax-Reese, is a graduate of the University of Pennsylvania’s Annenberg School of Communication. She has led WURD to become a multimedia powerhouse that provides access to support and information linked to health and wellness, community outreach, education, housing, finance, and business.
“We successfully connected hundreds of potential patients with information and resources that could improve the quality of their lives,” said Sara, describing the campaign with the POAAGG study.
“We learned that WURD can create
awareness within our community, and it is critical that the healthcare institutions be intentional about the treatments they provide once the patients are connected to them. Their systems must be fully fleshed out from the time the potential patient contacts the institution all the way through treatment and follow up. Every touch point must be handled with care, compassion, and cultural sensitivity.”
In addition to the collaboration with WURD Radio, the campaign also reached community members through strategically placed study flyers and postcards, promotion at health fairs, community meetings/events, and on internet platforms.
Many participants in the glaucoma awareness campaign have made renewed efforts to monitor their eye health. “The campaign allowed us to connect patients with ophthalmologists for glaucoma screenings, while recruiting subjects for our POAAGG study,” said Selam Zenebe-Gete, lead Clinical Research Coordinator for the POAAGG study. “Sometimes this was the springboard for getting patients set up with regular appointments at Scheie.”
The campaign placed a strong emphasis on providing high-quality individualized care, treating the patient compassionately, and alleviating barriers to healthcare. This was accomplished by providing free transportation and lunch vouchers and scheduling screening appointments around patient availability.
The Department of Ophthalmology hosts many outreach events throughout Philadelphia that provide free vision screenings and referrals to members of the community. Most of these screenings focus on glaucoma and low vision,


conditions that are more common in older and African ancestry populations.
At glaucoma screenings, physicians and staff transport all equipment to the event site in a mobile van. Community members cycle through a variety of
ocular and systems screenings, including measures of visual acuity, intraocular pressure, blood pressure, and a family and health history questionnaire. Attendees are then seen by a glaucoma specialist, and, if deemed necessary by
the physician, receive visual field testing, ocular coherence tomography imaging, and optic nerve fundus photography. If these tests show abnormal results, patients are given the option to be contacted and scheduled to be seen at the Scheie Eye Institute for a full visit. Up to 50% of people with glaucoma are unaware of their disease, so the screenings are essential for early diagnosis and treatment to prevent irreversible vision loss.
At some events, community members are provided with (and trained to use) free low vision devices, such as standing and handheld magnifiers, reading glasses and cases, and eye drops. Screenings are also often coupled with donated glasses giveaways, informational material distribution, and complimentary lunch. Some screenings are conducted in collaboration with other health care providers or existing health fairs, allowing
patients to access a variety of health resources and information in one place.
Another program, Penn Sight Savers, regularly provides free eye screenings and education throughout Philadelphia. Led by Prithvi Sankar, MD and medical student volunteers from the Perelman School of Medicine, the program aims to improve accessibility to eye care, raise awareness of eye conditions, and provide handson clinical ophthalmology experience to first- and second-year medical students. Screening events organized by Sight Savers are held across Philadelphia, often in community and religious centers in West Philadelphia. The team screens for diseases such as glaucoma and diabetic retinopathy. Glaucoma specialists then review findings with the students, providing a hands-on learning experience early in medical school. The specialists inform community members when they should
seek further testing and/or treatment at the Scheie Eye Institute.
These outreach events often serve individuals who are uninsured or without access to eye care. It is essential that these patients have access to vision screenings so that common eye diseases (glaucoma, age-related macular degeneration, diabetic retinopathy, etc.) are diagnosed as early as possible, when treatment can preserve vision.
Screening events also provide opportunities for social interactions among community members and a chance to circulate resources and information between long-time neighbors and friends. The screenings also introduce opportunities for healthcare systems and medical providers to establish trust with patients and to connect with one another in a familiar setting.
A Clinical Research Coordinator assesses a patient’s medical history at a free glaucoma screening hosted by Scheie. Scheie physicians and medical students volunteer at a Penn Sight Savers event, providing free vision screenings to patients.Puentes de Salud, or Bridges of Health, is a non-profit organization located in South Philadelphia that provides affordable healthcare services to the city’s expanding Latinx immigrant community members.

The Ophthalmology Department at UPenn continues to staff the eye clinic at this health organization despite challenges posed by the coronavirus pandemic.
Puentes has a sliding scale payment structure and collaborates with stakeholders, such as pharmaceutical companies and labs, to ensure pricing is affordable for patients. The health center has grown to include volunteer physicians across a wide range of sub-specialties.
The eye clinic is staffed monthly by Scheie physicians Tomas Aleman, MD, Irene HeinzGiven and John LaPorte Research Professor of Ophthalmology, and César Briceño, MD, inaugural Medical Director of Scheie at Penn Presbyterian and Associate Professor of Ophthalmology. Residents and medical students from UPenn also volunteer their time. The eye clinic provides preventative
screenings for diseases such as diabetic retinopathy and glaucoma, as well as refractions for eyeglass prescriptions.

Often, Drs. Briceño and Aleman take consultations over the phone to guide patients experiencing acute eye issues. They also place a heavy emphasis on educating patients on preventative care and treatment options. In rare emergency cases, they work with the city to obtain resources for patients requiring immediate surgical care. Patients are followed by the ophthalmologists for long-term care, which not only establishes a trusted relationship, but also permits patients to receive continuous healthcare services.
In 2019, Drs. Aleman and Briceño, with the support of then-Chairman Joan O’Brien, MD, submitted a grant proposal to the Board of Woman Visitors at UPenn to acquire much-needed equipment for the eye clinic at Puentes de Salud. Successful funding of this grant allowed for purchase of an autorefractor, a slit lamp, an indirect
ophthalmoscope, a tonometer, and a retinoscope. The new equipment has helped provide more efficient, accurate, and high-quality care.
The COVID-19 pandemic had a large impact on operations at Puentes de Salud. To follow social distancing requirements, the subspecialty clinics were forced to postpone healthcare delivery, which left patients without services for nearly two years.
“During this time, we weren’t physically able to see patients for logistical reasons,” said Dr. Briceño. “The only thing we could really do at the time was field it on the telephone and try to guide people to the appropriate emergency services.”
In the future, Drs. Aleman and Briceño hope to provide more surgical care to patients and to expand other health services for patients at Puentes. Partnering with local hospitals and other clinics to link patients to more resources and advanced care is another goal.
The Foundation Fighting Blindness (FFB) is an organization founded in 1971 by the families of individuals experiencing vision loss due to retinal diseases. These families were connected by their mission of supporting and advocating for research into prevention and treatment for inherited retinal diseases. Since its inception over 50 years ago, the FFB has raised over $856M to support research and treatment of blinding retinal diseases.
The VisionWalk, first held in 2006, is a nationally organized event coordinated by the FFB. In the past 15 years, VisionWalk events across the country have raised over $60M to support the FFB’s mission. In Philadelphia, the VisionWalk is held annually in the fall at the Independence National Historic
Park, with over 700 walkers, volunteers, and donors participating in person, virtually, or financially. Participants walk around the park after listening to speeches from the VisionWalk’s medical chairs and other leadership. Afterwards, they are encouraged to enjoy free food and socialize with fundraising team members and other attendees.
The Scheie Eye Institute has been a proud sponsor of the Philadelphia VisionWalk since 2011. Alan Laties, MD, Emeritus Professor of Ophthalmology, was an active member in the FFB for many years prior to the sponsorship. At Scheie, events leading up to the VisionWalk encourage the Scheie team to support FFB’s cause, including bake sales with homemade and donated
goods, raffles within the Department, and free Team Scheie gear for all walk participants. The Department has also been responsible for involving other large donors with the VisionWalk, such as the well-known medical supply company Bausch and Lomb.
In past years, more than 200 members of the Scheie community have attended the VisionWalk. Katharine Uyhazi, MD, Assistant Professor of Ophthalmology, has also served as one of the Medical Chairs for the Philadelphia VisionWalk in recent years. Although the event was held virtually during the COVID-19 pandemic, Team Scheie has continued to show their support for the FFB and enjoyed returning for the first in-person event this year. n

Friedman, D. S., Wolfs, R. C., O’Colmain, B. J., Klein, B. E., Taylor, H. R., West, S., Leske, M. C., Mitchell, P., Congdon, N., Kempen, J., & Eye Diseases Prevalence Research Group. (2004). Prevalence of open-angle glaucoma among adults in the United States. Archives of ophthalmology, 122(4), 532–538.
Gudiseva, H. V., Pistilli, M., Salowe, R., et al. (2019). The association of mitochondrial DNA haplogroups with POAG in African Americans. Experimental Eye Research, 181, 85-89. Guisti, K., Hamermesh, R. G. & Krasnow, M. (2021). Addressing Demographic Disparities in Clinical Trials. Retrieved from https://hbr.org/2021/06/addressing-demographicdisparities-in-clinical-trials
Hill, L., Artiga, S. & Haldar, S. (2022). Key Facts on Health and Health Care by Race and Ethnicity. Retrieved from https://www.kff.org/racial-equity-and-health-policy/ report/key-facts-on-health-and-health-care-by-race-and-ethnicity/ Hostetter, M., & Klein, S. (2021). Understanding and Ameliorating Medical Mistrust Among Black Americans. Commonwealth Fund. Labree, N. (2019). Puentes de Salud: Building Bridges of Health https://www.pennmedicine.org/departments-and-centers/ophthalmology/about-us/news/department-news/puentes-de-salud
Popejoy, A. B., & Fullerton, S. M. (2016). Genomics is failing on diversity. Nature, 538(7624), 161-164.
The Scheie Eye Institute participates in the 2019 Philadelphia VisionWalk to support the Foundation Fighting Blindness.No doubt we all recall with some awe the life of Queen Elizabeth II. Her steadfast leadership earned her an iconic status around the globe. Over her 70 years on the throne, the world changed around her in so many ways. Societal norms evolved, technology advancements skyrocketed, and 15 British Prime Ministers were under her watch, the most recent being elected in her final days. During her reign, Queen Elizabeth II showed a particular passion for philanthropy and was associated with more than 600 charities.
In the years since its inception in 1874, Penn Ophthalmology has also evolved, impacted the world, undergone changes in leadership, and made significant advancements. The Department currently sits at the conjunction of several milestones. In 2022, we welcomed our ninth Chairman. Dr. Bennie Jeng, like several Chairman before him, has his medical roots at the University of Pennsylvania. He brings back to Philadelphia much experience since he left our hallowed halls ready to leave his imprint over his coming tenure.
Next, the Scheie Eye Institute celebrated its 50th anniversary in 2022. Dr. Harold Scheie’s foresight and vision to establish a free-standing University facility dedicated to patient care and research has led to treatment of thousands of patients, impactful careers for trainees, and scientific discoveries that helped maintain or restore sight. And it cannot go without mention that Dr. Scheie treated and later befriended Lord Mountbatten, the great uncle of King Charles III, while serving in the U.S. Army during his time in Burma.
Finally, we prepare for the 150th anniversary of the Ophthalmology Department in 2024. The Department has grown innumerably since its founding in the 19th century. While the Ophthalmology Department was formally founded in 1874, it is important to note that several Penn general surgery faculty made progress in our field in the late 18th and early 19th century. These individuals included Dr. Philip Physick (the “Father” of American Ophthalmology, who went to Penn undergrad before obtaining medical training in Great Britain, then returning to Penn); Dr. William Gibson (the first surgeon to perform strabismus surgery); Dr. William Horner (anatomist who named Horner’s muscle); and Dr. David Hayes (the last of the great general surgeon ophthalmologists at Penn before our department founding). And since 1874, a multitude of giants have walked our halls, leaving their own mark in our field. This includes the publication of seminal textbooks, the modernization of surgery, and revolutionary research in ophthalmic physiology, ophthalmic pathology, molecular biology, and ocular genetics. This tradition continues today.
With this great alignment of our 9th Chairman, the Golden Anniversary of the Scheie Eye Institute, and the milestone of the founding of our Department, we hope that all of our alumni will join us as we embark on a great celebration of where we have been and the future yet to come. There will be opportunities to provide memories, photographs, and camaraderie with each other in Philadelphia this spring. We always welcome you home. n
Scott M. Goldstein, MD, Res ‘00, Fel ‘02 President, Penn Ophthalmology Alumni



Late 1960s: Tilman Ramsey Thorp, MD, Residency Class of 1970.
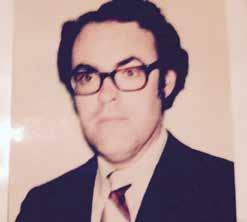

July 1972 - June 1975: Resident Teaching Schedule.


October 11-12, 1972: Outlines given to residents to use while giving tours at the Scheie dedication.building

Dec. 7, 1973: Typical O.R. schedule (“Yes, we started at 5:30AM” –Elliott Yolles, MD, Ward Chief on this rotation).

Courtesy of Elliott Yolles, MD
Early 1970s: From left to right: Smith F. Hogsett, MD, Elliott Yolles, MD, Judy Eagle, and Lai-Sung Leung, MD.

1971: Ralph C. Eagle, Jr., MD is all smiles as he observes an eyeball in the pathology lab.
Circa 1973: Elliott Yolles, MD, during his rotation as Chief Resident, aids Chairman Harold G. Scheie, MD in preparing for surgery.

1970s





 Photograph by Andy Warhol of Charles Nichols, MD, Residency Class of 1969 and Faculty Member since 1971.
Courtesy of Charles Nichols, MD
Photograph by Andy Warhol of Charles Nichols, MD, Residency Class of 1969 and Faculty Member since 1971.
Courtesy of Charles Nichols, MD
We asked faculty and alumni to submit their most cherished memories and photos from their time in the Department.Courtesy of Ralph C. Eagle, Jr., MD Courtesy of William Trattler, MD 1978-1979 Residents and Fellows. Circa : Senior residents gather outside of Dr. Scheie’s OR.
These were taken while we were having a blast rehearsing a skit-parody of ‘The Wizard of Oz’ that was presented to the Scheie faculty and families at the Residents Graduation Ceremony in May 1988. Fun times were had by all residents while first rehearsing and then performing the Resident’s Day skit ‘The Wizard of Scheie.’ I never cease to be grateful for everything I learnt at Scheie, especially how to play the role of Scarecrow.”




I am thankful for the outstanding teachers and mentors that formed my professional career. In particular there are lessons which I use today from a variety of attendings, particularly Irv Raber, Ralph Eagle, Myron Yanoff, Eliot Werner, Sandy Brucker, David Kozart, Ted Krupin, and my fellow residents. I really enjoyed my Assistant Chief of Service year as it gave me an opportunity to spend more time with the outstanding faculty, as well as getting to know the amazing residents who I was able to teach. Forever grateful to Scheie!!”
“The Wizard of Scheie” skit at Scheie Residency Graduation. Pictured: Robert “Bob” Weisenthal, MD, Director of the skit
1988: From left to right: Ira Wallace, MD, Jay Mulaney, MD (Scarecrow), Andrea “Andy” Freidberg, MD (Dorothy), Mark Schefkind, MD (Tinman), and Tom Stank, MD (Lion).
Circa Mid 1990s: Bill Trattler, MD (left) and Nicholas Volpe, MD (right) review notes.



Taken in July 1993: Residency Class of 1996. From left to right: Anitha Patel, MD, Bill Trattler, MD, Brad Simons, MD, PhD, Steve Thornquist, MD, and Maria Portellos, MD.

Circa 1994: Bill Trattler, MD in clinic.


Circa Mid 1990s: Residents gather at the Department’s holiday party. From left to right: Vivian Kim, MD, David Weissgold, MD, Bill Trattler, MD, Anitha Patel, MD, and Mary Chang, MD.
More photos from the mid 90s!







Circa mid 1990s. From left to right: Stuart Fine, MD, Michael Sulewski, MD, Juan Grunwald, MD, Dwight Stambolian, MD, PhD, Nick Volpe, MD, Stephen Orlin, MD, Janet Steinberg, OD, Samuel Jacobson, MD, PhD, David Kozart, MD, Richard Stone, MD, Michele Piccone, MD, Alexander ‘Sandy’ Brucker, MD.

 Circa Mid 1990s: Bill Trattler, MD (left) with Charles Nichols, MD, Residency Class of 1969 and Faculty Member since 1971 (right).
Albert Maguire, MD, Faculty Member since 1992, current Co-Director of the Center for Advanced Retinal and Ocular Therapeutics (CAROT).
Steve Orlin, MD and Mike Sulewski, MD.
All photos above courtesy of William Trattler, MD.
Three photos courtesy of Giacomina (‘Mina’) Massaro-Giordano, MD
Circa Mid 1990s: Bill Trattler, MD (left) with Charles Nichols, MD, Residency Class of 1969 and Faculty Member since 1971 (right).
Albert Maguire, MD, Faculty Member since 1992, current Co-Director of the Center for Advanced Retinal and Ocular Therapeutics (CAROT).
Steve Orlin, MD and Mike Sulewski, MD.
All photos above courtesy of William Trattler, MD.
Three photos courtesy of Giacomina (‘Mina’) Massaro-Giordano, MD
Great education and great friends and colleagues made during my times at Scheie.”1997: End-of-Year Photo. — Adam Scheiner, MD, Residency Class of 1998


AAO Event, 2012: Mina MassaroGiordano, MD (left) with Sepideh Tara Rousta, MD, Residency Class of 1997 (right).
AAO Event, 2018.
AAO Event, 2012: Nasreen A. Syed, MD, Prior Faculty (left) with Mina MassaroGiordano, MD (right).
AAO Event, 2015, from left to right: Mina Massaro-Giordano, MD, ‘98, Bill Trattler, MD, ‘96, Sepideh Tara Rousta, MD, ‘97.






My favorite memory at Scheie will always be the Scheie grand rounds that used to be in person. It was an opportunity to meet faculty and residents in person and discuss interesting cases in person! I hope we can have the grand rounds back in person by the time this appears in print!”
— Madhura Tamhankar, MD, Residency Class of 2007, Current Faculty
Two experienced readers Eli Smith and Candace Parker adjudicating grading discrepancies in the Scheie Image Reading Center, directed by Ebenezer Daniel, MBBS, MS, MPH, PhD.





Scheie residents, fellows, and faculty dress up for the annual George. E. de Schweinitz Memorial Lecture, for which then-Chairmen Joan O’Brien, MD was speaker. The event was held at the College of Physicians in Philadelphia.

From left to right: Mina MassaroGiordano, MD, Paul Tapino, MD, and Charles Nichols, MD.
 Courtesy of Charles Nichols, MD
Courtesy of Ebenezer Daniel, MBBS, MS, MPH, PhD
Courtesy of Mina Massaro-Giordano, MD
Courtesy of Mina Massaro-Giordano, MD
Residency Class of 2013. From Left to Right: Dina Gewaily, MD; Luxme Hariharan, MD, MPH; Ankoor Shah, MD; Deepika Nemani Shah, MD, MPH; Esther Bisker, MD.
From left to right: Jean Bennett, MD, PhD, Charles Nichols, MD, Mina Massaro, MD, and Lisa Schocket, MD attend an alumni event.
Courtesy of Esther Bisker, MD
Courtesy of Charles Nichols, MD
Courtesy of Ebenezer Daniel, MBBS, MS, MPH, PhD
Courtesy of Mina Massaro-Giordano, MD
Courtesy of Mina Massaro-Giordano, MD
Residency Class of 2013. From Left to Right: Dina Gewaily, MD; Luxme Hariharan, MD, MPH; Ankoor Shah, MD; Deepika Nemani Shah, MD, MPH; Esther Bisker, MD.
From left to right: Jean Bennett, MD, PhD, Charles Nichols, MD, Mina Massaro, MD, and Lisa Schocket, MD attend an alumni event.
Courtesy of Esther Bisker, MD
“Always document by taking images. Not only is a picture worth a thousand words, it is fundamental to ophthalmology research.”
“I would provide the same advice that my mentors told me. If you put the interest of the patient first, your care decisions will never be wrong.”
–
The field of vision science is at its helm with advances in gene therapy, cell therapy approaches using stem cell differentiation, transplantation approaches, and disease model studies.
Understanding the 3D human genome and lessons learnt from GWAS studies will bring precision medicine to diversified populations. Through innovation and cross-disciplinary research, our dream to prevent and cure blindness has just begun!”
– Murthy Chavali, PhDThis is such an exciting time to be an ophthalmologist. Always question the status quo. Many ophthalmic diseases that we never thought possible to treat, let alone cure, now can be. Always remember your patients and remember to treat them with compassion and to give them hope.”
– Victoria Addis, MDYou are in the most amazing field in medicine, but with that comes great responsibility. Always keep in mind the trust that many place in you. Each patient, trainee, student, and mentee provide an opportunity for you to grow and be a better version of yourself. With that, do not only surpass their expectations of you, but surpass the expectations you could never even dream of reaching.”
– Vivian Lee, MD“Stay curious, and by that I mean remain open to and actively seek out new ways of approaching a problem/finding a solution. This will help you to stay energized in your career. Also, never forget to take time for yourself to recharge along the way.”
“There will be many fantastic technical advances that will aid you in the care of your patients, but remember first and foremost, to be a caring, loving, and compassionate physician.”
– Brian Forbes, MD, PhD
“
What is one piece of advice that you would give the next generation of ophthalmologists and vision scientists?
Robert Avery, DO, MSCE
– Ebenezer Daniel, MBBS, MS, MPH, PhD
– Qi Cui, MD, PhD
“The impossible is possible when you work at a cutting-edge institution.”
– Giacomina Massaro-Giordano, MD
Do your very best at every opportunity that comes your way and then do your best not to worry about your efforts. Worry and anxiety really sap energy and you need that energy to move on and seek out the next opportunity. Take risks because the rewards are often great, and if you fail, move on without remorse. Failures are where we learn the most, although successes certainly feel much better.
Every life has uphill moments and moments where you then soar down the hill. Remember in those uphill moments, that in front of them an undoubted ability to soar exists.
Ask for help whenever you need it. The senior faculty will be glad to help. Develop scientific mentors, clinical mentors, and life advice mentors. Never let work replace time spent with family and friends. Joy comes from relationships with people. Everything else is just relief, not joy. Be joyful.”
“While we all know that learning ophthalmology (or anything in medicine for that matter) is a lifelong process, we cannot forget that this is also the case for mentorship and sponsorship: seek it when you are younger, and don’t forget to provide it when you are older…”
“Advances in understanding the biological mechanisms of eye disease and the potential to target interventions in a more precise manner with gene therapy and neuroprotection will revolutionize ophthalmology. We must remember that the goal is to provide superior care and achieve health equity for our patients. The opportunities are limitless!”
MD
“
“We are seeing remarkable new molecular and gene therapies enter the ophthalmology world. Keep on top of these as your careers progress so your patients can benefit from them once proven safe and effective. Also, remember to counsel patients to eat a diet rich in vegetables and fruits, as these are associated with better ocular (and general) health!”
– Joshua Dunaief, MD, PhD
– Bennie H. Jeng, MD
“New approaches to diagnosis and treatment are moving rapidly ahead in many different areas of eye disease –keep learning throughout your career!”
– Maureen Maguire, PhD
– Eydie Miller-Ellis,
“A healthy diet is a solution to many of our health care problems. It’s the most important solution…” n
– Madhura Tamhankar, MD– Joan O’Brien, MD
Allison Brucker, MD
Thomasine Gorry, MD, MGA
Diana Kim, MD
Charles Nichols, MD
Dwight Stambolian, MD, PhD
Paul Tapino, MD
Stephen Armenti, MD, PhD
Bennie H. Jeng, MD
Christina Moon, MD
Stephen Orlin, MD
Michael Sulewski, MD
Vatinee Bunya, MD, MSCE
Giacomina Massaro-Giordano, MD
Glaucoma
Victoria Addis, MD
Qi Cui, MD, PhD
Eve Higginbotham, SM, MD, ML
Eydie Miller-Ellis, MD
Prathima Neerukonda Atluri, MD
Prithvi Sankar, MD
Ali Hamedani, MD, MHS
Grant Liu, MD
Ahmara Ross, MD, PhD
Kenneth Shindler, MD, PhD
Madhura Tamhankar, MD
Joan O’Brien, MD
Vivian Lee, MD
César Briceño, MD
Sonul Mehta, MD
Sara Bierwerth, OD, FAAO
Stacey Cesarano, OD
Shelley Cutler, OD, FAAO, FSLS
Samantha Dougherty, OD
Alisha Fleming, OD
Mary Gerges, OD Li Lu, OD
Pediatric Ophthalmology (CHOP)
William Anninger, MD
Robert Avery, DO, MSCE
Gil Binenbaum, MD, MSCE
Stefanie Davidson, MD
Anne Jensen, MD
William Katowitz, MD
Priyanka Kumar, MD Monte Mills, MD
Julia Reid, MD Karen Revere, MD Drew Scoles, MD
Adele
Ophthalmology
Established in 2001
Current Chairholder: Joshua Dunaief, MD, PhD
Carolyn F. Jones
Professorship of Ophthalmology
Established in 1996
Current Chairholder: Gui-shuang Ying, PhD
Founder’s Professorship in Retinal and Vitreous Diseases in Ophthalmology
Established in 2018
Current Chairholder: Alexander Brucker, MD
F.M. Kirby Professorship of Molecular Ophthalmology
Established in 1996
Current Chairholder: Albert Maguire, MD
F.M. Kirby Professorship of Ophthalmology
Established in 2006
Current Chairholder: Kenneth Shindler, MD, PhD
Harold G. Scheie Chair and Professor Established in 2022
Current Chairholder: Bennie Jeng, MD
Retina & Vitreous
Tomas Aleman, MD
Alexander Brucker, MD
Samuel Jacobson, MD, PhD
Benjamin Kim, MD
Albert Maguire, MD
Katherine Uyhazi, MD, PhD
Brian VanderBeek, MD, MPH, MSCE
Nirali Bhatt, MD
Research Faculty
Artur Cideciyan, PhD
Ebenezer Daniel, MBBS, MS, MPH, PhD
Joshua Dunaief, MD, PhD Jessica Morgan, PhD Gui-shuang Ying, MD, PhD
Emeritus Faculty
Jean Bennett, MD, PhD
Stuart Fine, MD
Brian Forbes, MD, PhD Juan Grunwald, MD James Katowitz, MD Maureen Maguire, PhD Edward Pugh, Jr., PhD Graham Quinn, MD, MSCE Richard Stone, MD
2022-2023 Fellows:
Alexander F. Baten-Tschan, MD (Glaucoma)
Apoorv P. Chebolu, MD (Retina)
Gabriela M. Lahaie Luna, MD (CHOP Oculoplastics) Yoon H. Lee, MD (CHOP Pediatrics) David A. Ramirez, MD (CHOP Pediatrics) Jonathan C. Tsui, MD (Retina)
2022-2023 Residents:
First Year Residents
Lilian Chan, MD
Jason M. Keil, MD, PhD
Taylor J. Linaburg, MD
Nitya T. Rao, MD, MS Sabhyta Sabharwal, MD
Second Year Residents
Caroline W. Chung, MD
Devin C. Cohen, MD
Angela S. Gupta, MD, PhD Tejus Pradeep, MD Michael B. Wong, MD, MSc
Third Year Residents
Tomas Andersen, MD, MPH Tianyu Liu, MD
Samantha L. Marek, MD Brian J. Nguyen, MD Vivian L. Qin, MD
Harold G. Scheie-Nina C. Mackall Research Professorship of Ophthalmology
Established in 1983
Current Chairholder: Joan O’Brien, MD
Irene Heinz Given and John LaPorte Given Research Professorship of Ophthalmology
Established in 1970
Current Chairholder: Tomas Aleman, MD
William C. Frayer Professorship of Ophthalmology
Established in 1995
Current Chairholder: Samuel Jacobson, MD, PhD
William F. Norris and George E. de Schweinitz Professorship of Ophthalmology
Established in 1945
Current Chairholder: Vatinee Bunya, MD, MSCE
Niessen Chair ofThe David M. Kozart Memorial Lecturers (2007 – present)
2007 Peter S. Hersh, MD
2008 Randall J. Olson, MD
2009 Alan S. Crandall, MD
2010 Warren E. Hill, MD
2011 Garry P. Condon, MD
2012 John D. Gottsch, MD
2013 Thomas W. Samuelson, MD
2014 Daniel M. Albert, MD, MS
2015 Stephen E. Orlin, MD
2016 James C. Tsai, MD, MBA
2017 Alexander J. Brucker, MD
2018 Graham E. Quinn, MD, MSCE
2019 George A. Cioffi, MD
2020 Myron Yanoff, MD
2021 Irving M. Raber, MD
2022 Michael F. Chiang, MD
The Honored Alumni Lecturers (renamed to Alan M. Laties, MD, Lecturer in Ophthalmology) (2015 – present)
2015 J. Douglas Cameron, MD, MBA
2016 Dan S. Gombos, MD, FACS
2017 Donald S. Budenz, MD, MPH
2018 Michael Kazim, MD
2019 Jennifer E. Thorne, MD, PhD
2020 William B. Trattler, MD
2021 Raymond S. Douglas, MD, PhD
2022 Joseph W. Sassani, MD, MHA
The below resources informed much of the background research for this magazine. All are excellent references to learn more about the history of the Department of Ophthalmology.
A History of Ophthalmology at the University of Pennsylvania by Daniel M. Albert and Harold G. Scheie Highlights the birth and growth of the field of ophthalmology, as well as departmental history from 1870-1960.
An Ophthalmic Journey by William C. Frayer Provides a first-person account of departmental history from 1949 to 2000.
The Forever Fix: Gene Therapy and the Boy Who Saved It by Ricki Lewis Tells the story of gene therapy successes and failures over time, leading up to the first gene therapy for an inherited disease, which was developed by ophthalmologists at the Scheie Eye Institute.
To Spread the Light of Knowledge: 250 Years of the Nation’s First Medical School by Carol Perloff Chronicles the history of Penn Medicine in celebration of its 250th anniversary, including milestones in the Ophthalmology Department.
Ophthalmology Oral History Series: A Link with Our Past. An Interview with Harold Glendon Scheie, MD. Provides a transcript of a series of interviews with Dr. Harold Scheie, conducted by Sally Smith Hughes, about his career in ophthalmology.
Scheie Eye Institute Widener Library Displays and stores historical texts, journals, photos, portraits, artifacts, equipment, and more within the Scheie Eye Institute.
University Archives & Records Center
Provides a repository of historically significant artifacts, photos, and documents on departmental history.
Compiled by Rebecca Salowe

Scheie Eye Institute 51 N. Myrin Circle Philadelphia, PA 19104 find us on facebook at www.facebook.com/ScheieEye find us on twitter at www.twitter.com/ScheieEye
find us on linkedin at www.linkedin.com/company/scheie-eye-institute
EYE INSTITUTE
The Scheie Eye Institute is the Department of Ophthalmology at the University of Pennsylvania. Scheie has been a leader in the field of ophthalmic research, education, and patient care for nearly 150 years. Many of our greatest advancements in vision-saving therapy have been made possible by donations from individuals and organizations.
For more information contact us at 215.662.8415
Or by email: Rebecca.Salowe@pennmedicine.upenn.edu PennMedicine.org/supportscheie