

WELCOME TO Neuro Transmitter
Welcome to Rice Neuro Transmitter (RNT), Rice’s first undergraduate neuroscience journal! The RNT team is very excited to share Issue 3 with you today, and if you like what you see, you’ll probably want to read Issues 1 and 2 too!
Our journal aims to share neuroscience-themed articles written by undergrads with the Rice community and greater Houston area about any topic that may promote in terest in neuroscience. These articles can range from case studies, to opinion piec es, to interviews and more!
In this issue, our writers focused on bringing to light new and encouraging treat ments that are being developed for the most severe neurological disorders and dis eases. Furthermore, we discuss how COVID-19 has unfortunately led to more inter personal violence in the US. Finally, our writers have included articles on careers in neuroscience that include an interview with a physician and the perspective of some Rice neuroscience students exploring options outside of medicine.
In addition, we’ve included a list of neuroscience clubs on campus and courses for next semester for you to view at your convenience to make it easier for you to get involved in neuroscience at Rice!
In our next issue, we will include an article written by a high school student whose article was determined to be the best out of dozens submitted in our high school competition we held this semester! We hope you will look forward to reading what the next generation of neuroscience students have on their minds.
If you enjoy our journal, share it with your friends so they can enjoy it too! We appreciate all the support.
Nick Gonzalez President Thank you,3-4 5-6 7-10 11-14 15-18 19-20 21-22 23-26 27-30 31-34
TABLE OF CONTENTS
Faculty Address
Meet some of our amazing faculty, their current research at Rice, and their involvement in neuroscience!
Clubs Courses
Find out about various neuroscience clubs at Rice and get involved!
See what the different neuroscience courses here at Rice have to offer,their prerequisites, and more!
Brain Machine Interface in Neuromuscular Disorders
This article discusses the potential of brain machine interfaces and neuroprosthetics in leading patients to a more independent lifestyle.
Neuroscience Student Spotlight: Passion Outside of Medicine
This article shines light on the experiences of two neuroscience students pursuing careers outside of medicine.
The Psychology of Domestic Violence in COVID Times
Examines domestic violence through neuroscience, this article describes how events of the COVID-19 pandemic exacerbated domestic violence nation-wide.
Body Transplants Via Smart Materials
This article explores how the smart material of graphene nanoribbons can aid in spinal cord fusion after body transplants, providing hope for victims of neck-down paralysis.
The Opioid Crisis in Houston
This article details two new prevention and treatment options for opioid addiction.
Alzheimer’s Disease: From Prions to Palliative Care
From neurobiology to experimental treatments to empathetic palliative care, this article serves as an overview of Alzheimer’s disease.
Q&A with Dr. Nisha Gadgil
Faculty Address
Hello all,
Dr. Jonathan Flynn Neuroscience Faculty AdvisorIt has been another eventful year! Personally, I went on parental leave during the spring and returned this past fall. I had the privilege to see my daughter develop from an in fant to a toddler (making Piaget’s developmental phases much more interesting than a chapter in PSYC 203), and had to juggle the responsibilities of being a parent and a pro fessional. I also learned that children in daycare spread germs worse than plague rats/ freshmen, and spent more time being sick in the last three months than I had in the last decade. I offer that last bit as both a warning to future parents and as an apology to the students in my classes who had to suffer long delays for grades.

As for the overarching neuro community around Rice - we have continued to grow and have achieved a few milestones. First, we have increased our official presence at Rice. Prior to this last summer, decisions on the major and minor were made by a shifting hodgepodge of faculty. Now, the Biosciences department established the Neuroscience Undergraduate Curriculum Committee (NUCC), which has specific faculty from multi ple departments whose job now includes shepherding pedagogy around the major. As we make more substantial changes to the major (and some should be announced in the early spring!), we will be able to make material across classes more cohesive. We will have meetings every semester, and if you have any curricular suggestions that you would like for me to bring up to the committee, please email them to me at flynn@rice.edu.
The neuroscience courses have seen some shifts. Dr. Caprette and Dr. Dickman, the for mer instructors for BIOS 385 Fundamentals of Neuroscience and NEUR 380 Neurosys tems respectively, have happily retired. Dr. Cana Ross and Dr. Nele Lefeldt have taken over their roles and are working together to reduce the shared content in these courses. Dr. Fischer-Baum, former instructor for PSYC 362 Cognitive Neuroscience, has tempo rarily moved to a position at the NIH, with Dr. Moore staying and taking over the course.
Additionally, BIOS 212 Experimental Neuroscience has been changed to require either COMP 140 or CAAM 210, with the idea that small coding projects will be standard across the mid and higher level labs.
In terms of student organizations, we see continued expansion. The latest semester of BrainSTEM saw approximately 40 undergraduates mentoring over 100 local K-12 students four days of the week. We expect to be teaching at even more schools next semester. The Rice Neuroscience Society (RNS) has continued their usual wonderful productions, and created the first annual Rice Undergraduate Neuroscience Symposium (RUNS), a student run presentation and poster event. This event will reoccur bigger and better this spring, as they have received a substantial grant from the Creative Ventures Fund at Rice. Finally, an exciting new club called Rice Neurotech has been formed, and will be focusing on the de velopment of technology related to neuroscience. The faculty have agreed to allow ABL 123 (i.e., the teaching lab for BIOS 212) to be open after hours for students who will use the lab tools for club projects. As a general announcement, this is not limited to Neurotech - if your organization could use ABL 123 as an after hours space, let me know.
Finally, it is important to note that we have had some growing pains this past year. Most notably, many senior students in the neuroscience major attempted to finish their elective laboratory requirements and were initially stopped due to seating limits. To give an idea on the extent of the problem by describing its solution, Dr. Lefeldt had to increase the seat limit of the spring semester of BIOS 415 Experimental Physiology from 12 seats to 28. While things worked out thanks to Dr. Lefeldt’s plan and the Biosciences department’s willingness to financially support the expanded course, this is clearly not a feasible strategy for the long term. While I cannot talk about the details now, I can say that the administration is aware of this problem and has started working towards a solution. Keep an eye out on the NEUROPPS email list in the late spring for further announcements.
Neuroscience at Rice is clearly making its mark, and I am delighted to see all that we have accomplished in the past year. The community is thriving, and I hope that everyone keeps helping each other be the best they can. I look forward to seeing where everything is a year from now.
Neuro Transmitter
Rice Neuro Transmitter (RNT) is Rice’s first undergraduate neuro science journal. Started in Fall 2021, RNT aims to share interesting student-written articles on neuroscience to the Rice community. Rice Neuro Transmitter’s articles include a range of topics, such as neuroscience’s connection to law or art, and progressions in re search made by Rice’s neuroscience faculty. We also have exciting future plans such as a potential research article competition, and much more! If you want to be published, you may submit an article through our website and we will review them. If you want to join, please apply during the Fall semester!
Speculative Neuroscience
Best Buddies
Best Buddies is the Rice chapter of an international non profit organization that promotes the inclusion of people with intellectual and developmental disabilities (IDDs) by providing opportunities for one-to-one friendships. We are dedicated to our part in the movement to end the social, economic, and physical isolation of people with IDDs. Our chapter on campus works in partnership with the HEART Program located in Houston. In addition to monthly group parties (bowling, scavenger hunts, picnics), each Buddy pair is encouraged to meet on their own time and keep close con tact through letters, phone calls, and emails. You can contact Best Buddies at Rice at mv26@rice.edu. Also, like the Face book page to keep up with events: https://www.facebook. com/RiceBestBuddies/.
Neurotech @ Rice
Neurotechnology at Rice (N@R) aims to serve as a resource for Rice students to learn more about careers in neurotechnology, research in neuroengineering & Rice’s Neuroengineering Initiative (NEI), and other related neurotechnology resources and to make partnerships with various organizations in the Neurotechnology community! We meet every other Tuesday during lunch!
Speculative Neuroscience is a really chill neuroscience discussion group that talks about a variety of topics relating to neuroscience such as free will, advances in artificial intelligence, ethics of neural stem cell research and treatment, the cognitive aspect of emotion/memory/perception, theories of consciousness, and so much more!! You can also request specific topics you’d like to hold a discussion on. We meet every other Friday for lunch at the Martel PDR from 12-12:45PM :) please reach out if you want to join!
BrainSTEM is a group at Rice that teach es neuroscience to local high school stu dents in Houston, via hands-on activities and interactive small-group lessons. It also counts as a 1-credit hour Satisfacto ry/Non-Satisfactory class at Rice! Further, if you take this class for three semesters (not necessarily in a row), BrainSTEM can count as one of your four required elec tives for the neuroscience major. We meet every Friday 1-2PM at ABL 130, where we run through our lessons. BrainSTEM has numerous other projects to get involved in, such as creating neuroscience demon strations at Rice, creating a BrainSTEM textbook for middle-schoolers, creating video lessons on neuroscience topics, and developing a BrainSTEM manual.
President: Nick Gonzalez Vice Presidents: Kirim Kim & Autumn Hildebrandteach stu activities It Satisfacto Further, semesters can elec meet we has involved demon BrainSTEM creating and
Pancakes for Parkinson’s
Pancakes for Parkinson's (P4P) is a student-led organization that fundraises for Parkinson's disease research and supports Houston's PD community. We host an annual breakfast fundraiser, educational panels, and volunteer events, whose proceeds benefit the Michael J. Fox Foundation and the Houston Area Parkinson Society. One of our upcoming events is Pancakes Around the World, where students can sample pancakes from several Rice cultural clubs - think Indian dosas and Japanese okonomiyaki - while donating to support our organization! This past year, we hosted a number of virtual, hybrid, and in-person events, including a socially-distanced breakfast fundraiser in April. Being part of P4P has taught me a lot about being an advocate for people with PD, and I have enjoyed learning about Parkinson's through their perspectives. If you want to be involved in P4P, we will be sending out board member applications early this fall. In the meantime, please join our Owlnest group so we can reach out to you!
Rice Neuroscience Society Alzheimer’s Buddies
Rice Neuroscience Society (RNS) is dedicated to increasing interest in neuroscience at Rice Univer sity and beyond by putting together events that are educational and engaging. Some major events we host include the annual Brain Bee competition for high school students, summer NeuroCamp, Brain Awareness week, and the Neuroscience mentorship program. We also organize a variety of monthly events such as Halloween eyeball dissection, neu roscience career panel, and the Brain Trivia Night! Last year, we managed to transform many in-per son events into an online format and keep students engaged. In this upcoming semester, we will try to incorporate more hybrid events to make sure ev eryone can participate. A general body meeting will take place in September, as well as a Neuroscience Major/Minor Advising Session with Dr. Flynn and Dr. Lefeldt. We will also be sending out committee applications soon, so definitely be on the lookout for that if you are interested in getting involved!
Alzheimer’s Buddies is a response to the profound isolation and social disengagement experienced by people in the intermediate-to-late-stages of Alz heimer’s disease or other dementia-related illness. Student volunteers will be able to form meaning ful relationships over the course of a semester or longer with the residents of the nursing homes (“Buddies”). Our initiative encourages students to take the mindset of a friend rather than of a care provider, to learn about their patients’ past and passions, to establish real friendships. This interac tion not only provides patients with social support, but also provides students with a formative clinical experience and formal training on this devastating disease.
Classes CORE CLASSES
Utilize this section to consider some neuroscience courses to take during your time at Rice
Cognitive Neuroscience: Exploring the Living Brain (NEUR362)
Survey of theory and research on how mental processes are carried out by the human brain, with an emphasis on relating measures of brain activity to cognitive functioning, methods surveyed included electro physiological recording techniques, functional imaging techniques and methods that involve lessoning or disrupting neural activity.
Prerequisites: PSYC 203
Minor Requirement — social sciences and humanities concentration
Fundamental Neurosystems (NEUR380)
This course will provide a broad overview of the brain’s neural systems that subserve perception, learning, and behavior. The course will be highly integrative with thematic content including func tional organization of the nervous system, neural encoding and decoding, sensory systems, motor systems, and high-level concept processing.
Minor Requirement - Core Requirement
LAB ORIENTED
Experimental Neuroscience (BIOS212)
Introduction to the scientific method, principles of experimental design, selected research strategies, record keeping, and technical communication as related to neuroscience. This course is restricted to Neuroscience majors.
Prerequisites: CAAM210
Experimental Physiology (BIOS415)
Laboratory studies in membrane, nerve, and muscle physiology, with emphasis on experimental de sign, data analysis, and data interpretation.
Prerequisites: BIOS 311 or BIOS 385 and BIOS 211 or BIOS 212
ELECTIVES
Introduction to Social and Affective Neuroscience(PSYC354)
Overview of social and affective neuroscience research, including examination of the neurobiologi cal mechanisms supporting social cognition; inter-personal processes; emotion and motivation; and emotion regulation. These topics will be examined in both healthy and affectively-disordered popu lations, with links made to the fields of health psychology and clinical neuroscience.
Minor Elective — social sciences and humanities concentration
Prerequisite: PSYC202
BrainSTEM (BIOS128)
BrainSTEM is a service organization that teaches STEM subjects through the lens of neuroscience. We perform hands-on, small-group activities with ~45 students per week. This course will prepare you to communicate science in a both effective and entertaining manner, as well as build your skills in managing small groups. More information can be found at ‘www.brainstem.club.’
Minor Requirement — social sciences and humanities concentration
Animal Behavior (BIOS321)
Evolutionary theory is used to evaluate behavioral adaptations of organisms to their environment
Minor Elective — social sciences and humanities concentration
Prerequisites: BIOS 201 and BIOS 202
Learning from Sensor Data (ELEC475)
The first half of this course develops the basic machine learning tools for signals images, and other data acquired from sensors. Tools covered include principal components analysis, regression, sup port vector machines, neural networks, and deep learning. The second half of this course overviews a number of applications of sensor data science in neuroscience, image and video processing, and machine vision.
Minor Requirement — natural sciences and engineering concentration Elective
The Sciences of the Mind (PHIL130)
An introduction to the scientific investigation of the mind, with special attention to topics of partic ular philosophical interest. Topics are likely to include: representation and computation, perception, cognition, action, and the neural implementation of mental states and processes. Previously offered as PHIL 103. Mutually exclusive with PHIL 103, credit cannot be earned for both classes.
Minor Elective — social sciences and humanities concentration
Animal Minds (PHIL231)
This course will examine various philosophical questions raised by the science of animal cognition: What is it to have a mind? How can we learn about animal minds? Are animals conscious? Do they have beliefs or concepts? What does this tell us about the nature and value of animal minds? Previ ously offered as PHIL 359 and is mutually exclusive. Credit cannot be earned for both PHIL 231 and PHIL 359. Distribution 1 credit effective Fall 2022.
Minor Elective - Humanities and Social Science
Psychology of Aging (PSYC310)
This course focuses on the psychology of aging through a biological, cognitive, and socio-emotional framework. Topics to be covered include how mental capacities change over time, especially memory processing, differences between normal and pathological aging, neurobiological changes with age, dementias such as Alzheimer’s disease, and individual differences in aging. There will be an emphasis on discussion of recent literature and developing research ideas in the field of psychology of aging.
Minor Requirement — social sciences and humanities concentration
Elective
The Sciences of the Mind (PHIL130)
This course focuses on the psychology of aging through a biological, cognitive, and socio-emotional framework. Topics to be covered include how mental capacities change over time, especially memory processing, differences between normal and pathological aging, neurobiological changes with age, dementias such as Alzheimer’s disease, and individual differences in aging. There will be an emphasis on discussion of recent literature and developing research ideas in the field of psychology of aging.
Minor Requirement — social sciences and humanities concentration
Elective
RESEARCH ORIENTED
Independent Research for Neuroscience (NEUR310)
Information on how to find a lab, apply to the course and what to expect can be found at www. neur310.rice.edu. This course gives credit for independent research in Rice Neuroscience faculty laboratories (or other Texas Medical Center laboratories.) Students spend at least 3 hours per week in the laboratory for each semester hour of credit. If taken for 3 or more hours, counts as one required 300+ level lab course within the neuroscience major. Can be repeated once for 3 hours or more to count towards an elective credit within the neuroscience major. Requires a proposal abstract, weekly reports, and a final project that summarizes your activities in the lab. Students wishing to perform their research in an off-campus lab must submit a completed application to the NEUR 310 instructor at least 2 weeks prior to the start of classes. Students are strongly advised to secure research advisors and register for the class well in advance of the start of classes. Repeatable for Credit.
Elective
Neural Computation (NEUR416)
How does the brain work? Understanding the brain requires sophisticated theories to make sense of the collective actions of billions of neurons and trillions of synapses. Word theories are not enough; we need mathematical theories. The goal of this course is to provide an introduction to the mathematical theories of learning and computation by neural systems. These theories use concepts from dynamical systems (attractors, oscillations, chaos) and concepts from statistics (information, uncertainty, inference) to relate the dynamics and functions of neural networks. We will apply these theories to sensory computation, learning and memory, and motor control. Students will learn to formalize and mathematically answer questions about neural computations, including “what does a network compute?”, “how does it compute?”, and “why does it compute that way?” Prerequisites: knowledge of calculus, linear algebra, and probability and statistics.
Minor Requirement — natural sciences/engineering concentration
Electives
Methods in Social Cognitive and Affective Neuroscience (PSYC366)
This course will give students hands-on training in the research methods of social cognitive and affective neuroscience. Students will learn about the theoretical underpinnings of these allied fields; acquire, preprocess, and analyze human functional neuroimaging data (i.e. using fMRI); and inter pret and write-up results.
Minor Requirement — social sciences and humanities concentration
Elective 09
Developmental Neurobiology (BIOS443)
An advanced undergraduate and graduate level course, dedicated to analysis and evaluation of scientific inquiry into animal development and neurodevelopment. Textbook based lectures and discussions based on primary scientific literature are used to exemplify and evaluate concepts and methodology. Writing assignments, quizzes, midterm and final exam will be used to evaluate per formance. Cross-list: BIOS 543.
Register for research credit before the spring semester begins.
Go to http://biosugresearch.rice.edu/ course-requirements/ for more information.

BRAIN MACHINE INTERFACE
IN NEUROMUSCULAR DISORDERS
Written By Abhishek Kona, Edited by Ryan WangImagine a child with quadriplegic ce rebral palsy — they are unable to walk in hallways, they have trouble talking with their classmates, and they cannot leave the sight of a supervisor. This lack of independence from neuromuscular disorders creates a dif ficult lifestyle for patients; in contrast, through brain machine interfaces (BMI), they are able to live unconstrained from caretakers. Using brain-machine interfaces, we can enable mo tor movement, essentially giving life to para lyzed or amputated limbs with individualized patient needs.
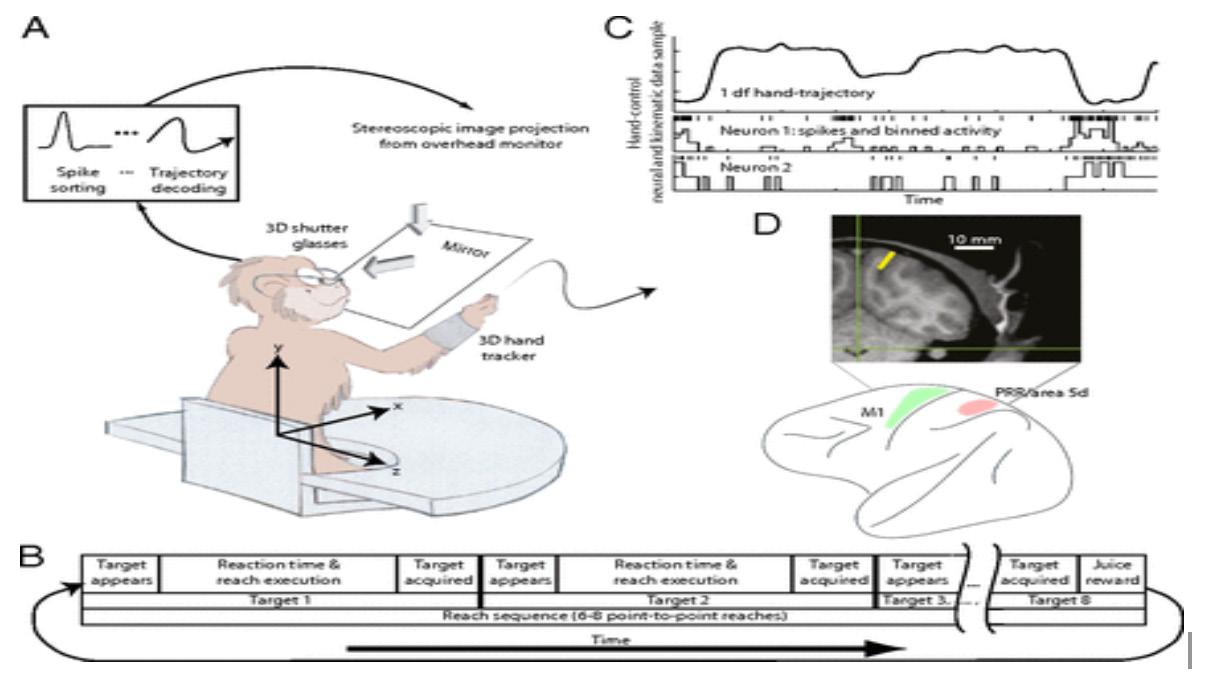
In order to implement brain machine inter faces, the Cortical Prosthetic, a device supple menting input and output of the nervous sys tem in the motor areas, must be used. Varying cortical areas have been proven to be places for Cortical Prosthetic to aid and help with para lyzed subjects. The motor cortex, where the in terface primarily affects, can emit spinal coor
dination signals, directly commanding circuits and the nerve system of the spinal cord. More cognitive variables such as memory capaci ty and mobility are now being extracted from the Posterior Parietal Cortex region (PPC) and the Parietal Reach Region (PRR) of the brain to create precise, accurate, and consistent signals from the interface that can be applied to the cortical prosthetics of regular patients. When precise and accurate trajectories are emitted from the PPC, the emissions can soon be coded as movement signals, expand ing the uses of cortical prosthetics and BMIs. These cortical prosthetics can generate ste reotypical movements that will be used on ge neric amputees or paralyzed patients who do not have specialized needs or care.

A Neuroprosthetic Experiment with Two Rhesus Monkeys:
Figure I. The hand trajectories from the neuroprosthet ics are at first inconsistent, but then get more precise and accurate after about six trials with the Kalman Filter.
To get an idea of the plausibility of sending co To get an idea of the plausibility of sending command signals from regions of the brain to the motor cortical prosthetic or the brain-machine interface, an experiment was done with two rhesus monkeys. Each per formed a test of moving a cursor in a 3D envi ronment. Electrodes were placed in the PPC of both monkeys, where continuous signals were extracted, unlike other experiments of a signal targeting the various motor areas. The mouse was then controlled by neural commands in stead of physical manipulations. In a week, de coders were made to exploit the features of the neural 3D hand movement. The Kalman filter, an algorithm providing estimates of unknown variables such as movement from activity in areas of the brain, gave the best data of recon struction position of the hand and average de termination factor given to the prosthetics. With more tests with increased com plexity in tasks and visual disturbances, the result was only a slight difference of decod ing messages from both monkeys. The exper
Design by Bryant Polancoiments prove that the PPC messages to the prosthetic were insensitive to visual pertur bations, and the neural signal represented the brain’s intention to move. This means that measuring intention to move, rather than in sert something here through the PPC could be used to control prosthetics.. Furthermore, the limbs were mostly used in a straight direction to reach goals rapidly, accurately, consistently, and precisely, although a few random and er roneous trajectories were displayed initially during the process. Just like a regular brain, the prosthetic improved in performance over time.
Application to Humans for Hand Function:
As exemplified with Rhesus Monkeys, brain in terface machines in coordination with neuro prosthetics can provide a new solution for pa tients in post-stroke rehabilitation therapies, suffering from loss of motor function in their
arms. Dr. Marcia O’ Malley, a professor and dean of the school of engineering here at Rice, focuses on the development of brain machine interfaces and new pilot projects for stroke survivors who are missing motor functions. Though current robot-assisted therapies exist, they have trouble ensuring patient engagement and motivation and have yet to match benefits of conventional therapies.
Dr. O’Malley specifically implemented a brain machine interface with non-invasive scalp EEG, an Electroencephalogram that measures electrical activity in areas of the brain be fore any major diagnosis: this enabled analy sis of neural activity and a returned feedback mechanism to the patient using the interface machine. If Malley and her team were able to detect motor intent from movement related cortical potentials, singlas detectable by the EEG, (MRCP) , then the motion of the upper limb exoskeleton would be triggered. The study tested for optimization and feasibility of the
brain machine interface in three different aspects: adaptive time window for extracting features, increased robustness, reduction of false positives by residual electromyography gating. Over the course of five days, in the latter of the experiment, Malley found con sistent results of strong BMI performance and low false positive rates considerably for the impaired arm. Her findings provided ev idence for the development of EEG based Brain Machine interface for stroke patients as a rehabilitative method, as it can sustain a strong performance without recalibration over several days.

of neuroprosthetics and brain machine in terface will pave the way for more advanced rehabilitative therapies for patients, leading to opportunities for increased independence for patients not only with strokes but more severe neuromuscular disorders such as quadriplegic cerebral palsy.
In Fig. 3, motor intents are being detected from an impaired stroke patient by the EEG.
Citations
Bhagat NA, Venkatakrishnan A, Abibullaev B, Artz EJ, Yozbatiran N, Blank AA, French J, Karmonik C, Grossman RG, O’Malley MK, Francisco GE and Con treras-Vidal JL (2016) Design and Optimization of an EEG-Based Brain Machine Interface (BMI) to an Up per-Limb Exoskeleton for Stroke Survivors. Front. Neurosci. 10:122. doi: 10.3389/fnins.2016.00122

Moreover, beyond this initial study of brain machine interfaces within robot ic therapies, O’Malley, in conjunction with Houston Methodist’s Dr. Dimitry Sayenko, is now currently directing the first pilot proj ect in restoring the upper limb exoskeleton, a suit designed to restore function to the upper limbs, as a continuation of the previous study. This project will combine Sayenko’s noninva sive stimulator that stimulates the spinal cord and her upper limb exoskeleton with BMI in order to create a more fast-paced recovery for patients. The work of Malley in the field
Markus Hauschild, Grant H. Mulliken, Igor Fineman, Gerald E. Loeb, and Richard A. Andersen (2012) Cog nitive signals for brain–machine interfaces in poste rior parietal cortex include continuous 3D trajectory commands. PNAS, 109 (42), 17075-17080.
JOSEPH
Sid Richardson senior Joseph Asfouri said. “[Rice] has one of the most well-known neuroengineer ing centers [and] initiatives going on with the in credible amount of innovative research here and across the street at the Texas Medical Center.”

Asfouri, who is pursuing a dual degree in Neuro science and Electrical Engineering, knew that he wanted to combine his passion for robotics and medicine since high school. Although he started college on the pre-med track, Asfouri made the switch to the pre-grad track after shifting his fo cus to research. In his career, he hopes to become a professor of neuroengineering and serve an in stitute like the Rice Neuroengineering Initiative with his research.
“I realized that human behaviors are at the source of many of the world’s problems at the same time neuropsychiatric diseases are on the frontier of medicine, and we have a great need for develop ing cures for these conditions. [I am] able to target these problems in medicine—these problems to society—with neuroengineering, combining electrical engineering and neuroscience together,” As fouri said. “The research is what drew me to the major.”
NEUROSCIENCE STUDENT SPOTLIGHT:
PASSIONS OUTSIDE OF MEDICINE
t most universities, neuroscience is among the majors most commonly associated with the pre-med track, and Rice is no excep tion—pre-med neuroscience students are plen tiful on campus. Non-pre-med neuroscience students, on the other hand, are uncommon, and those outside their circle lack knowledge of their involvement in the neuroscience community. But despite their limited presence amongst a sea of
written by Hayley Juepre-med peers, many have achieved their unique academic goals through participation in Rice’s neuroscience program.

Rice’s neuroscience opportunities first caught Sid Richardson senior Joseph Asfouri’s interest when he was deciding which college to attend.
“Neuroengineering is the reason I came to Rice,”
Asfouri said that he experienced no obstacles in classes or barriers to opportunities despite being one of a few neuroscience majors not pursuing medicine. Some of Asfouri’s favorite classes in clude Dr. Caprette’s Fundamentals of Neurosci ence, Dr. Lefeldt’s Advanced Cell and Molecular Neuroscience, Dr. Pitkow’s Theoretical Neurosci ence, Dr. Flynn’s Experimental Neuroscience, and Dr. Robinson’s Intro to Neuroengineering. He said that these classes confirmed his interest in the neuroscience major.
“I want to design medical devices for patients, so a firm understanding of cellular and molecular neuroscience, which are the courses I most en joyed taking from the neuroscience major at Rice, is absolutely necessary,” Asfouri said.
Because Rice’s core requirements are flexible, Asfouri suggests supplementing the neurosci ence curriculum with engineering and computer science courses that teach data analysis and ma chine learning skills.
“Don’t stay within the confines of the major. With the amount of data in neuroscience and genom ics in general, there needs to be a strong under standing of machine learning and data science,” Asfouri said.
In his summers, Asfouri put his practical neu roscience skills to use by seeking new research experiences. He has worked in the University of Washington’s National Primate Research Center on brain-computer interfaces, Weill Cornell Med icine in New York City on addiction and anxiety disorders, the Baylor College of Medicine on deep brain stimulation for treatment-resistant depres sion, and Rice’s Robinson Lab on non-invasive neural stimulation using magnetic fields.
“I was actively seeking these opportunities [during] the winter break before summer,” Asfou ri said. “I got rejected from most of them, I got ac cepted to a few, and that’s all you [need] to be able to actually study an incredible diversity of labs.”
Asfouri recommends that other pre-grad neuro science majors seek diverse research experienc es too.
“Get involved in research as early as you possi bly can,” Asfouri said. “If you’re really passionate about going to graduate school and becoming a PhD in academia or going into industry after wards, it’s important to have as much research experience as possible.”
DANTE KIENIGIEL
xchange student Dante Kienigiel from Insti tuto Tecnológico de Buenos Aires agrees that data skills and research experiences are use ful for neuroscience students interested in graduate programs.
“Build your own projects, even if they are small… Learn how to program because it will just make your life easier,” Kienigiel said. “And get involved in research as early as possible.”
Kienigiel is pursuing a five-year bioengineering de gree from his home university, with this year being his fifth and final in the program. Initially, Kienigiel only planned to study at Rice for the fall semester, but he has since extended his plans to include the spring semester.
“This semester, mainly, I’m taking 15 credits and auditing a bunch of stuff. But the final project for one of my courses is the beginning of the thesis and then I [will] keep working on it throughout the next semester,” Kienigiel said.
Under his thesis mentor Dr. Segarra, who teaches in the Electrical and Computer Engineering depart ment, Kienigiel intends to complete his thesis while finishing his degree requirements at Rice. Dr. Segarra, who graduated from Kienigiel’s university in 2011, and Dr. Pitkow, who researches computational neuroscience, were the two main reasons Kienigiel decided to study at Rice.
“[Dr. Pitkow] was one of the professors who taught some of the courses in the
Neuromatch Academy summer school, which got me into computational neuroscience in the first place,” Kienigiel said. While applying for the stu dent exchange program, Kienigiel “was talking to [Dr. Segarra] first because being from the same university, he’s more accessible…[Dr. Pitkow] was his office neighbor, so it ended up being a full cir cle from different places.”
Kienigiel said that there is a shortage of neuro science programs in Latin America. To address this disparity, Kienigiel and his friends founded Brainware, which educates high school students on neuroscience topics, at Instituto Tecnológico de Buenos Aires.
“The goal is to get people interested in neurosci ence, and if you’re into engineering, [to show] you can still do neuroscience…Just in general in Latin America, there are not many neuroscience op tions for undergrads. I believe there is a single neuroscience program in all of Latin America…in Mexico,” Kienigiel said.
At Rice, Kienigiel is a member of Rice Neurosci ence Society and Rice Undergraduate Neurosci ence Symposium committee. He is also excited for Rice’s new Neuro Tech student organization, which will start meeting late in the fall semester. Neuro Tech intends to bridge the gap between neuroscience and engineering, and Kienigiel hopes that students interested in both disciplines will join the organization.
Some of Kienigiel’s favorite Rice classes include Dr. Moore’s Computational Modeling of Cognitive Processes and Dr. Segarra’s Network Science and Analytics.

In Computational Modeling of Cognitive Process es, “it is interesting to be able to work at a higher level without having to go into neurons, and that’s my lifelong goal—working on artificial intelli gence. It’s always the debate of ‘how deep do we have to go?,’” Kiniegel said. In Network Science and Analytics, “It’s by far the most challenging
course I’ve taken in years, but I’m learning a whole entire field, and I love how it’s applicable to pretty much any area.”
In graduate school, Kienigiel wants to continue studying computational neuroscience and pur sue a PhD. This passion originally stemmed from the Neuromatch Academy online courses—in cluding those taught by Dr. Pitkow—he took in the summer of 2020.

“I didn’t know [computational neuroscience] was a whole field. This was everything I was actually looking for. I just didn’t know it was a thing,” said Kienigiel. “So since then, [my interest has] been definitely computational neuroscience.”
While most Rice neuroscience majors are pursu ing the pre-med path, both Asfouri and Kienigiel emphasized the wealth of opportunities available to students interested in other neuroscience top ics. From medicine to neuroengineering to com putational neuroscience, diverse students have found success in Rice’s neuroscience major.

The Psychology of Domestic Violence in COVID
Written by Lindsey Ran Copy Edited by Mira SrinivasaDomestic violence is defined as” a pattern of abusive behavior in any relationship that is used by one partner to gain or maintain power and control over another intimate partner” by the US Dept of Justice.
During the COVID-19 pandemic, mandatory stay-at-home orders were enforced. Psychological repercussions including fear, frustration, and boredom correlated with a drastic increase in reported cases of anxiety, post-traumatic stress, and depression. Do mestic violence is closely correlated to these mental health issues and saw an increase nationwide.
Specifically in Houston, from 2019 to 2020, domestic violence increase by 40% and became the leading county in Texas for domestic violence numbers. This increase can largely be owed due to lockdown during the pandemic where more stressors due to finances or health were placed on family units with little space to retreat to.
There are a variety of factors that have been found to be tied to domestic violence. Brain damage has reportedly led to violence where people suffering from a frontal lobe injury can become impulsive, violence, and lose control. Additionally, it was found that male batter ers tend to have issues with memory and cognitive flexibility, resulting in them processing negative emotional stimuli in a violent manner.

Certain regions of the brain have also been found to have altered functioning. In particular, the amygdala, cingulate gyrus, and parietal and prefrontal cortices were found to have the most difference. Respectively, these regions of the brain control processing of threats, emo tion regulation, and sensory perception.
During COVID-19, many families had to undergo much emotional stress from lost family members and reduced financial security. This, along with the inability to leave the house, combined poorly with the reduced emotional processing of perpetrators of domestic vio lence, resulting in numbers to increase.


Body Transplants Via Smart Materials
Written by Priyanka Patel Copy Edited by Audrey Arroyave
Copy Edited by Audrey Arroyave
Every year, upward of 250,000 spinal cord injuries occur around the world. Quadriplegia or neck-down paralysis is a debilitating, horrific condition that is a common symptom of traumatic spinal cord injury, happening in about 60% of cases. However, science has come a long way, and there is possibility for quadriplegics to regain function of their bodies. Head transplants or “full-body” transplants, as Rice professor Dr. James Tour likes to put it, may have life-saving implications for patients who are quadriplegic or termi nally ill when there is no other treatment available.

James Tour, a proponent of using smart materials to address real world prob lems, is well-renowned for his work with graphene. This smart material is composed of repeating hexagonal carbon cells, up to 50 nm wide and several dozens of micrometers long (Zakharova, 2021). Graphene possesses unique electrical, physical, and chemical properties that may offer significant po tential as a bioscaffold for neuronal regeneration after spinal cord injury.
In 2016, Sergio Canavero, an Italian neurosurgeon, was amidst conducting a head transplantation experiment in which the spinal cords of mice were transected and attempted to be reattached. For unknown reasons, the neu rons in the spinal cord would simply not fuse and there was a great deal of un warranted swelling which left the mice with little to no mobility after the trans plant. When Dr. Tour’s student read about this issue, he was struck by an idea to use graphene, which possesses conductive properties that would allow the neu rons to continue to communicate despite there being a severance in the nerve.
As a result of the student’s idea, Dr. Tour and his team decided to use graphene nanoribbons and work with Bae Hwan Lee and C-Yoon Kim from Konkuk University in South Korea who were also working to restore spinal cord function in rodents. To their surprise, they discovered the material greatly reduced swelling which prevented a significant amount of damage to the spinal cord. The material reliably allowed motor and sensory neuronal signals to cross the gap 24 hours after complete transection of the spinal cord. Dr. Tour says, “The [Schwann] cells grew all around the graphene,” and its conductive properties allowed it to mesh with the nerve cells effectively. The ro dent experienced almost complete recovery of motor control after two weeks! This is a major advance over previous work with PEG (polyethylene glycol) alone, which gave no recovery of sensory neuronal signals over the same period of time and only 10 percent motor control over four weeks (Tour, 2016)
Although the act of transplanting a human head sounds like something straight out of a sci-fi or horror novel, Dr. Tour says, “We are on the right path.” Of course, it may take years or even decades to successfully transplant a human head, which is exponentially more complex physically and ethically. Several patients who suffer from paralysis have reached out to Dr. Tour with heartfelt emails pleading to be a part of his translational research, but unfortunately, he had to turn them down as the treatment has only been tested on mice. However, even though it is still far from becoming an official treatment for human patients, the rapid rate of scientific advancement leads to a promising future.
Further applications of graphene within neuroscience are vast. Some paths his team studied but did not have the funding to pursue were “the repair of the optic nerve” and “peripheral nerve repair” using graphene nanoribbons. Another promising avenue of future research involves “stimulating growth of neuronal interconnections in the brain” by locally placing graphene na noribbons. This can not only repair lesions but also enhance cognitive func tion. “Could we make people superhuman, in other words, increase the level of interconnection?” he asks. He asserts it would be interesting to observe how the brain’s plasticity takes advantage of these materials to form new connections.
References
Bennett J, M Das J, Emmady PD. Spinal Cord Injuries. [Updated 2022 May 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560721/
Kim C, Sikkema WKA, Hwang I, Oh H, Kim UJ, Lee BH, Tour JM. Spinal cord fusion with PEG-GNRs (TexasPEG): Neurophysiological recovery in 24 hours in rats. Surg Neurol Int 13-Sep-2016;7:. Available from: https://surgical neurologyint.com/surgicalint-articles/spinal-cord-fusion-with-peg-gnrs-texaspeg-neurophysiological-recov ery-in-24-hours-in-rats/
“Quadriplegia (Tetraplegia): Definition, Causes & Types.” Cleveland Clinic, 10 Aug. 2022, https://my.clevelandclinic. org/health/symptoms/23974-quadriplegia-tetraplegia.
Rice University. (2016, September 20). Graphene nanoribbons show promise for healing spinal injuries. ScienceDaily. Re trieved November 23, 2022 from www.sciencedaily.com/releases/2016/09/160920101607.htm
Sahni, D., Jea, A., Mata, J. A., Marcano, D. C., Sivaganesan, A., Berlin, J. M., Tatsui, C. E., Sun, Z., Luerssen, T. G., Meng, S., Kent, T. A., & Tour, J. M. (2013). Biocompatibility of pristine graphene for neuronal interface, Journal of Neurosurgery: Pediatrics PED, 11(5), 575-583. Retrieved Nov 24, 2022, from https://thejns.org/pediatrics/view/journals/j-neuro surg-pediatr/11/5/article-p575.xml
Zakharova, O. V., Mastalygina, E. E., Golokhvast, K. S., & Gusev, A. A. (2021). Graphene Nanoribbons: Prospects of Application in Biomedicine and Toxicity. Nanomaterials (Basel, Switzerland), 11(9), 2425. https://doi.org/10.3390/ nano11092425
 COPY EDITED BY SONAKSHI BHALLA & MIRA SRINIVASA
COPY EDITED BY SONAKSHI BHALLA & MIRA SRINIVASA
Ten years ago, Julia Soloman was snorting OxyContin off the back of a toilet seat. Now, she’s a successful art director in Los Angeles. How did she become addicted, how did she recover, and what does the future look like for ad diction treatment?
Opioids are a class of drugs that were originally derived naturally from the opium poppy plant, but later cre ated synthetically en masse. They include drugs like oxycodone, hydrocodone, codeine, morphine, and fentanyl. These trigger the pleasure center of the brain, making the drugs highly addictive and lethal. Opioids become deadly as they interfere with the function of the locus coeruleus in the brain, which helps regulate neurotransmitters that control breathing. Thus, opioid overdose often results in death from respiratory suppression (1).
The opioid crisis’ origin began in the 1990’s, when pharmaceutical companies aggressively (and, often, dishon estly) advertised the efficacy and safety of opioids like OxyContin. In hopes of quickly and effectively managing pain, many doctors prescribed opioids to their patients. Due to overmedication, among other factors, some of these patients became addicted to painkillers. Continuing into the 2000’s, the opioid crisis became further exacerbated by the in creased availability of more potent opioids, namely heroin and fentanyl. Currently, fentanyl, a synthetic opioid, contin ues to grow in popularity and cause overdoses across the US (2).
Opioid overdose deaths in the US from 1999–2020. Data from the Center for Disease Control (3) Houston is experiencing a sharp uptick in opioid overdoses, primarily due to a heavy increase in fentanyl use. In 2017, Houston experienced 56 fentanyl overdose deaths; in 2020, that number jumped to over 300 (4). Between 2019 and 2021, fentanyl-related deaths more than tripled, from 104 to 459 (5). The city has often been criticized for refusing to provide adequate resources to combat the opioid epidemic; however, progress seems to be moving in the right direc tion.

Houston recently passed two pieces of important legislation regarding funding for the prevention and treat ment of opioid addiction. The first applied for a federal grant from the Substance Abuse and Mental Health Services Administration. The requested $2 million would be used to train first responders and provide funding to rehab and education centers. The second bill provided funding for a collaboration between UT Health and the Houston Police Department to create the Comprehensive Opioid Stimulant Substance Abuse program, which will train police officers to properly respond to opioid overdoses (5,6). Additionally, there is significant neuroscience research being conducted to create more effective treatment options f2or opioid addiction. The Houston-based J Flowers Health Institute uses neuroengineering to treat opioid addiction in inple like Julia. At the University of Houston, Dr. Therese Kosten is devel oping anti-fentanyl addiction vaccines that she hopes will soon help prevent overdoses nationwide.
Design by Kate HiltonNEUROENGINEERING AS A DIAGNOSTIC AND TREATMENT
METHOD
Julia Soloman became addicted to opioids at seventeen. After receiving a prescription of OxyContin to treat her lyme disease, Julia fell down a spiral. As her addiction worsened, she sought various treatments, all of which led to relapse after relapse. After many failed attempts to end her addiction, Julia traveled to the J Flowers Health Institute in Houston (7).
J Flowers specializes in treating complex neurological issues through neuroengineering. It treats a wide array of patients, including those with ADHD, OCD, PTSD, and drug addiction. J Flowers analyzes the brain through a variety of noninvasive imaging techniques, then uses these data to create an individualized care plan for its patients. The core of the treatment stems from the institute’s brain imaging technology, which is among the most advanced in the nation (7).
The primary difficulty in treating opioid addiction is combating changes in brain function and chemistry. Research suggests that opioid presence in the brain disrupts many neural pathways. Continued use can cause people to misattribute basic needs as drug cravings; for example, a patient may confuse a desire for social interaction with a need to use opioids. Changes such as this prevent patients from maintaining normal social relationships (8).
J Flowers’ primary goal is to use neuroimaging to identify areas of the brain that have been changed by contin uous drug use. There is extensive research detailing these changes to the brain, many of which can be mapped using EEG and fMRI (two methods of brain imaging) (9). For example, many patients experiencing drug addiction are found to have low impulse control. Julia Soloman fell into this category (7). Throughout treatment, patients meet with psychol ogists to treat these cognitive deficits and improve their abilities. This combination of neuroscience and psychology
J Flowers also uses neurofeedback in their novel addiction treatment plan. Patients’ brains are analyzed using EEG, a brain activity tracker. A pa tient may be presented with images related to drug use or asked to imagine scenarios in which opioids are involved (10). Depending on whether the patient processes these situations in a healthy or unhealthy way, they will receive a positive or negative stimulus in return (usually they will hear or see something desirable or undesirable). By “punishing” addictive behavior and “rewarding” normal, or non addictive, behavior, J Flowers helps retrain the brain to free itself of its reliance on opioids.
J Flowers successfully treated Soloman’s opioid addiction, and she is now happily living in Los Angeles addiction free. In reference to the treatment she received, Soloman said, “I’ve seen it help so many people, and it sounds like magic when you talk about it. I think we’re at a point now where science can re ally help addicts.” Julia Soloman is now an advocate for the life-changing power of brain mapping and neuroimaging. According to Soloman, she “wouldn’t trade [her] life right now for the world” (7).
 Julia Soloman now works as an art director in Los Angeles
Photo from LinkedIn
Julia Soloman now works as an art director in Los Angeles
Photo from LinkedIn
VACCINATION AS A SOLUTION TO FENTANYL ADDICTION
Fentanyl is a synthetic opioid that is “50 to 100 times more potent than heroin and morphine.” Frequently mixed with other drugs, even a small amount of fentanyl can result in accidental overdoses and related deaths. In Houston, the fentanyl crisis is rising rapidly as reportedly “four out of every 10 pills on Houston’s streets right now are laced with [fentanyl].” Because fentanyl is a current and critical issue, researchers are looking to vaccination as a way to prevent overdoses and psychoactive effects.
The National Institutes of Health (NIH) has created the Helping to End Addiction Long-term (HEAL) Initiative, under which some researchers are studying the effects of vaccination on fentanyl potency. With a $25 million grant, research has shown that vaccination looks promising in rhesus monkeys and rodents. Dr. Therese Kosten, the Head of the University of Houston’s Developmental, Cognitive, and Behavioral Neuroscience Program in Psychology, has joined the team developing the fentanyl vaccine in early 2021.
RAT TRIALS
In the Kosten lab, they previously created a fentanyl vaccine where a structure similar to fentanyl (FEN) is injected intramuscularly into the body. This structure combines with a carrier protein CRM197 and an adjuvant dmLT, which then triggers the body to create anti-FEN antibodies. These antibodies, when combined with FEN, create too large of a structure to pass the blood-brain barrier and instead will be excreted harmlessly through urine. When FEN cannot enter the brain, it is unable to affect the brain. This suppresses any psychological effects and respiratory rate effects that the drug would otherwise have, preventing deadly overdoses.
In the experiment, male and female rats were administered this vaccine and a control. Both groups were then tested for the effect of FEN through testing pain stimuli, changes in vital signs, and levels of FEN in the brain. The vac cinated groups in both male and female rats were found to have little effect due to FEN even when dosage and time of FEN administration changed, demonstrating that the vaccine was effective at preventing FEN from reaching the brain.
Overall, the animal trials for anti-fentanyl vaccines have been promising, and anti-fentanyl vaccines may be possible for distribution as a complete overdose preventative measure. These vaccines can be used in addition to the current method of treatment, opiate agonist therapy.
Works Cited (APA Style; in order of appearance)
1. Kosten, T. R., & George, T. P. (2002). The neurobiology of opioid dependence: implications for treatment. Science & practice perspectives, 1(1), 13–20. https://doi.org/10.1151/spp021113
2. Lopez, G. (2017). The opioid epidemic, explained. Vox. https://www.vox.com/science-and-health/2017/8/3/16079772/opioid-epidemic-drug-overdoses
3. Hedegaard H, Miniño AM, Spencer MR, Warner M (2021). Drug overdose deaths in the United States, 1999–2020. NCHS Data Brief, no 428. https://dx.doi.org/10.15620/cdc:112340
4. Goñi-Lessan, A., & Barned-Smith, S. J. (2021). People didn’t think the fentanyl crisis was Houston’s problem. But it’s here. Houston Chronicle. https://www.houstonchronicle.com/news/investigations/article/Fentanyl-crisis-people-think-it-can-t-16351791.php
5. Glover, C. (2022). ABC13 given rare access inside DEA lab fighting Houston’s fentanyl Crisis. ABC13 Houston. https://abc13.com/fentanyl-crisis-houston-crime-allison-scroggins-dea-dallas-lab/12240978/
6. Gonzalez, S. (2022). Houston passes ordinances to combat opioid epidemic with grant funding. Community Impact. https://communityimpact.com/houston/heights-river-oaks-montrose/government/2022/05/18/houston-passes-ordinances-to-combat-opioidepidemic-with-grant-funding/
7. Glover, C. (2021). How neuroengineering is helping people fight addiction in Houston. ABC13 Houston. https://abc13.com/neuroengineering-brain-mapping-neuroscience-j-flowers-health-institute/11033615/
8. Heilig, M., Epstein, D., Nader, M. et al. (2016). Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosci 17, 592–599. https://doi.org/10.1038/nrn.2016.67
9. Marzbani, H., Marateb, H. R., & Mansourian, M. (2016). Neurofeedback: A Comprehensive Review on System Design, Methodology and Clinical Applications. Basic and clinical neuroscience, 7(2), 143–158. https://doi.org/10.15412/J.BCN.03070208
10. What is Neurofeedback? J. Flowers Health Institute. (2022). https://jflowershealth.com/what-is-neurofeedback/
Alzheimer’s Disease: From Prions to Palliative Care

 written by Dheerj Jasuja
written by Dheerj Jasuja
group to tau proteins. The phosphate group addition causes a physical change in tau’s structure. While normal tau helps maintain neuron
hood that one develops a neurodegenerative disease by priming the immune system to deal with misfolded proteins. Müller-Schiffmann and Korth (2008) described a vaccine model in which they would inject an engineered antibody into an individual to knock out the prion-creating gene. However, they noted that based on experimental results, such a vaccine would be hard to deliver as it may not be able to cross the blood-brain barrier.
ith an air of distress, Mr. P turned to one of the memory care center’s nurses and asked: “Who pays my bills?” She quickly responded, “Your kids do, Mr. P.” Mr. P seemed placated, but then sadly asked, “Do my kids visit me?” The nurse kindly told Mr. P that his kids vis ited him last Tuesday. Again, Mr. P looked satis fied with her response. Yet thirty seconds later he frantically queried: “Who pays my bills?”
Mr. P is one of the 6 million patients who suffer from Alzheimer’s disease in the United States (Alzheimer’s Facts and Figures, 2022). These pa tients experience reduced memory, communica tion, balance, and mobility abilities as a result of their condition. Given this disease’s prevalence and debilitating nature, it is no wonder that sci entists around the world have been working to eradicate Alzheimer’s.
In the search for a cure, researchers have sought to meticulously document the ailment’s neurobiology. The disease starts at a subcellular level with pathological proteins, known as prions. There are two main prions involved in Alzheimer’s disease: amyloid-beta (AB) and tau. AB is formed as a byproduct of amyloid precursor protein breakdown and is normally recycled through cellular processes. The issue arises when misfolded AB accumulates into plaques outside of neurons. Small chains of AB proteins can bind to certain neuronal receptors. Depending on the receptor, binding can then induce a toxic calcium ion influx in a neuron, induce apoptosis, dysregulate energy generation pro cesses, and more (Chen et al., 2017). Further, the accumulation of AB plaque modifies the tau protein to its disease state. In essence, AB chains initiate cellular pathways that add a phosphate
Figure 1. A cartoon of the numerous cellular mechanisms that neurodegeranation affects. (Wood et al., 2015)
structure, “hyperphosphorylated” tau forms toxic neurofibrillary tangles which kill neurons through numerous cellular processes. (Medeiros et al., 2010; Gong & Iqbal, 2008). While a singular misfolded tau or AB peptide would not be harmful, prions are able to convert regular conformations of the protein into the prion conformation. Thus, they proliferate to the point that they affect millions of neurons and other supporting cells. As detailed in Figure 1, prion spread causes neuronal death, loss of signal transmission between neurons, and tears in the blood-brain barrier (Wood et al., 2015). As the disease progresses, this damage can result in the loss of brain function and eventually death.
Although there is still much to learn about neurodegeneration, scientists have identified AB and tau prions as potential therapeutic targets for Alzheimer’s given their causal role in the disease process. From a preventative perspective, a prion vaccine may significantly reduce the likeli-
To circumvent this problem, Fang et al. (2022) researched protein scaffolds as a way to train the body’s own immune system to target prions. A protein scaffold is a non-toxic protein that carries the surface antibody sites of the target prion. Unlike an antibody-based vaccine, the protein scaffold is small enough to readily cross the blood-brain barrier. Once the protein scaffold enters the brain, the immune system creates antibodies that will trigger an immune response to dangerous prions with the same surface anti-
body binding sites. In their study, Fang et al. engineered a protein scaffold to target prions that cause a neurodegenerative disease called Gerstmann-Sträussler-Scheinker (GSS) disease. The authors tested this vaccine in mice that were genetically modified to eventually develop GSS disease and found that the vaccinated mice took over three times as long to develop the illness than unvaccinated mice.
These results are groundbreaking and demonstrate that in theory a viable prion vaccine can be developed for any prion-based neurodegenerative disease. The widespread distribution of an Alzheimer’s vaccine would significantly increase the healthspan of individuals who are vulnerable to this disease.
However, a vaccine does not help those who currently have Alzheimer’s. While there is no cure for the disease, numerous drugs such as galantamine, rivastigmine, and donepezil are
used to manage Alzheimer’s physical symptoms and improve the patient’s quality of life (How is alzheimer’s disease treated?, n.d). However, an overlooked symptom of dementia is loneliness. Many patients often do not have family who vis it them. Like Mr. P, others do not remember their family visiting them. Victor et al. (2020) found that approximately 30% of dementia patients experienced loneliness and associated depres sion symptoms. Fortunately, numerous organi zations are dedicated to minimizing feelings of isolation among dementia patients, including the Rice Chapter of the National Alzheimer’s Buddies campaign. Rice students volunteer at various memory care facilities in Houston and do their best to make the residents feel loved and sup ported through conversations filled with laughter, thoughtful discussions about reading materials, and more.
As an avid member of Alzheimer’s buddies and the research community, I am constantly remin-
ded of how community engagement and scientific discovery work together to provide holistic care for patients. While we wait for the cures and vaccines for neurodegenerative diseases that researchers are tirelessly working on, it is essential that we do our part in supporting these patients like Mr. P.



Works Cited
Alzheimer’s Facts and Figures. (2022) Alzheimer’s Association. Retrieved November 6, 2022, from https://www.alz.org/alzheimers-dementia/facts-figures
Chen, G.-fang, Xu, T.-hai, Yan, Y., Zhou, Y.-ren, Jiang, Y., Melcher, K., Xu, H. E. (2017). Amyloid beta: Structure, biology and structure-based therapeutic development. Acta Pharmacologica Sinica, 38(9), 1205–1235. https://doi.org/10.1038/aps.2017.28
Fang, A., Fleming, M., Tancowny, B., Tang, X., Wille, H. (2022). A structure-based prion vaccine protects a transgenic mouse model of Gerstmann-Sträussler-scheinker disease from neurodegeneration. Biophysical Journal, 121(3). https://doi.org/10.1016/j.bpj.2021.11.1959
Gong, C.-X., Iqbal, K. (2008). Hyperphosphorylation of microtubule-associated protein tau: A promising therapeutic target for alzheimer disease. Current Medicinal Chemistry, 15(23), 2321–2328. https://doi.org/10.2174/092986708785909111
How is alzheimer’s disease treated? (n.d.) National Institute on Aging. Retrieved November 6, 2022, from https://www.nia.nih.gov/health/how-alzheimers-disease-treated Medeiros, R., Baglietto-Vargas, D., LaFerla, F. M. (2010). The role of tau in alzheimer’s disease and related disorders. CNS Neuroscience & Therapeutics 17(5), 514–524. https://doi.org/10.1111/j.1755-5949.2010.00177.x
Müller-Schiffmann, A., Korth, C. (2008). Vaccine approaches to prevent and treat prion infection. BioDrugs 22(1), 45–52. https://doi.org/10.2165/00063030-200822010-00005

Victor, C. R., Rippon, I., Nelis, S. M., Martyr, A., Litherland, R., Pickett, J., Hart, N., Henley, J., Matthews, F., Clare, L. (2020). Prevalence and determinants of loneliness in people living with dementia: Findings from the IDEAL programme. International Journal of Geriatric Psychiatry, 35(8), 851–858. https://doi.org/10.1002/gps.5305
Ways to Volunteer. (n.d.) Alzheimer’s Society. Retrieved November 6, 2022, from https://www.alzheimers.org.uk/get-involved/volunteering/ways-volunteer Wood, L. B., Winslow, A. R., Strasser, S. D. (2015). Systems biology of neurodegenerative diseases. Integrative Biology, 7(7), 758–775. https://doi.org/10.1039/c5ib00031a
Image 1. A snapshot of the positive impact one could have on the lives of patients with dementia. (Ways to Volunteer, n.d.)
Dr. Nisha Gadgil is an Assistant Professor of Pediatric Neurosurgery at Baylor College of Medi cine and the Director of Pediatric Neurosurgical Movement Disorders at Texas Children's Hos pital located within the Texas Medical Center. Dr. Gadgil's clinical interests include treating and caring for patients with movement disorders, spasticity, Chiari malformation, pediatric brain/ spine tumors, and more. Dr. Gadgil obtained her medical doctorate and completed her neurolog ical surgery residency and pediatric neurosurgery fellowship at Baylor College of Medicine.
What are three adjectives you would use to describe the typical pediatric neurosurgeon: Tenacious, Hard-working, Committed
What is the lifestyle of a pediatric neurosurgeon like? (usual working hours, how often you are on call, how hectic or stressful the day can be)
It’s very variable, but neurosurgery is a demanding field. We’re constantly dealing with emergencies that arise at any time of the day, week, or break. Training is particularly long for neurosurgery. For me, it took nine additional years after medical school. The hours are tough. You can be on-call every other day for 24 hrs at a time. Once training is over, the hours get better. Right now, as an at tending, I’m not on-call as frequently, and how often one may be on-call depends on how many partners are in their group. But being at a level one trauma center means that you are always prepared for any emergency. Pediatric neurosurgery’s definitely a challenging lifestyle, but it is one that I’ve seen many successfully balance with a personal or family life. Nonetheless, it’s rewarding, and you just have to re member why you’re doing what you’re doing. Often those moments really come to clarity when there’s a particular patient that you’ve helped or family that’s grateful for what you’ve done, and their conversa tions can really put those things into perspective and make it worth it.
How does your lifestyle match, or differ from, what you had envisioned?
I guess it depends on when I was envisioning it. I definitely didn’t go into medicine, knowing I wanted to become a pediatric neurosurgeon. But I went into medicine knowing that I was going to work hard and that the training years, as well as the years even after training, were going to be tough. It’s a profes sion where you really have to be committed to your
patients and be willing to sometimes put your personal life on the back burner. So, I did envision those things being the case. I guess it was surpris ing that you never really understood what it would be like until you went through it. Everyone talks about the rigor of surgical residency, but I think when you’re going through those nights of being on-call and just being so tired you feel like you can’t even function, you will finally understand what that experience is like.
How did you know you were interested in specializing in pediatric neurosurgery as opposed to adult neurosurgery? Were there any particular factors that heavily influenced your decision?
It was really my mentors in pediatric neurosurgery. I had the privilege of working with many great mentors at Texas Children’s, who showed me what an exciting field it is and then guided me. Rotating through the pediatric service at Texas Children’s and seeing the types of cases we could treat as pediatric neurosurgeons was really cool. Kids are unique in that their central nervous system has much more plasticity and ability to recover after a neurological injury than an adult, which was ap pealing to me. I saw a lot of cases where our inter ventions did make a massive difference in a kid’s life. Even within procedures that aren’t necessarily life-saving and are just quality-of-life improving, the results that we get are incredible. I appreciated the impact that we could have.
You can say, to a certain extent, I was a little jaded sometimes in the adult world where, of course, we do great things and help people, but there are many people we can’t help at times. Or we might save their life, but they live in a very compromised state following a devastating injury that they don’t recover as much because their brain and central
nervous system aren’t as plastic. I was disillusioned by this because sometimes I felt a sense of futility, like did I really help this person? It was really rewarding to see in the world of pediatrics many instances of kids who were devastated by their injury but recovered to a much greater extent than you might have expected. That really pushed me towards pediatrics. I also really love kids. That is a simple answer, but it’s true. They’re hilar ious and quirky, and they make the job fun.
Do various neurological disorders present differently in the pediatric population than in adults? Are there any barriers to treatment for the pediatric population? It’s a different set of pathologies you see in kids. Some things are similar, like, for example, trauma. Trauma may be similar in how we manage it with minor site differences compared to adults. But congenital disorders, which are disorders that they are born with or a result of a problem with the development of the nervous sys tem, are disorders of children and not adults. You also do see a different set of diseases. In terms of their pre sentation, it’s interesting, especially with young babies and children: they’re non-communicative. You have to really do a thorough neurological exam and question the parents, as they are the ones that are going to say, “Oh, Johnny’s not acting right.” You may not notice that there is an issue with Johnny when you see Johnny. In stead, you do have to talk to the parents and listen to what they say, as you may not be able to tell on your own. You have to play detective a little bit, learn to incorporate the vague symptomatology, and go off of that.
What are some of the most significant differences between non-pediatric & pediatric patients when it comes to surgeries or patient/family interactions?
It’s just a different set of pathologies that you tend to see in kids than adults. But in terms of family interac tions, you often catch the parents at their worst moment. Something unimaginably bad might be happening to their child. So we have to have empathy for that and put ourselves in their shoes and understand that they aren’t always going to act as they normally would. The best way to go about things is to have compassion and give them space. Often those families that were unpleasant to you just because they were stressed out come back to say thank you and are appreciative. I always try to keep that in mind when dealing with families and patients.

How do you keep updated with the front end of neuroscience, seeing as the field is rapidly evolving?
I’m lucky to be associated with an academic institution, Texas Children’s and Baylor College of Medicine. So a lot of being part of an academic institution is education, not only for residents or students but ourselves. We read journals, do journal clubs, and go over newly published articles. We have conferences and continuing medical education. For example, in our department, we have a conference every Wednesday, and it’s kind of like a sacred time. We all go to it if possible unless there’s an emergency. We talk about upcoming cases, complications, and new procedures, and it’s a beneficial form to learn what new procedures are being per formed, what people are doing, and what sort of new ideas there are on managing certain diseases because that changes over time. Even during my short time in neurosurgery, how we manage things has changed. We’re constantly students of the discipline and learning.
What kept you going during the journey of becoming a physician? My love for medicine and the field kept me going. The advice I would have going off of that is you want to make sure you are going into medicine and the field you decide to go into for the right reasons. If you’re go ing in for the wrong reasons, then you’re going to find along the way, you’re resolved, and your grit that you need to get you through those tough years is not going to be sufficient to push you through. It’s only if you’re going in for the right reasons that you enjoy the field and care about the kinds of patients you’re serving and getting satisfaction from what you’re doing. That pushes you forward because the other things will only get you so far before you find yourself lacking the motivation to keep going. I think nobody goes into the field and doesn’t at some point think, “I should quit.” At some point, you’re going to think that. But if you keep coming back to why you did it and went into it, that will keep you going. Questioning it along the way is normal. But if you come back to that why, why you did this and why are you’re doing this, that will keep you moving for ward.
Book recommendations for students interested in pediatric neurosurgery or just neurosurgery in general?


The Rice Neurotransmitter team would like to thank Dr. Flynn and Dr. L Lefeldt for their support in producing this issue, and the team for their contributions to the journal.

