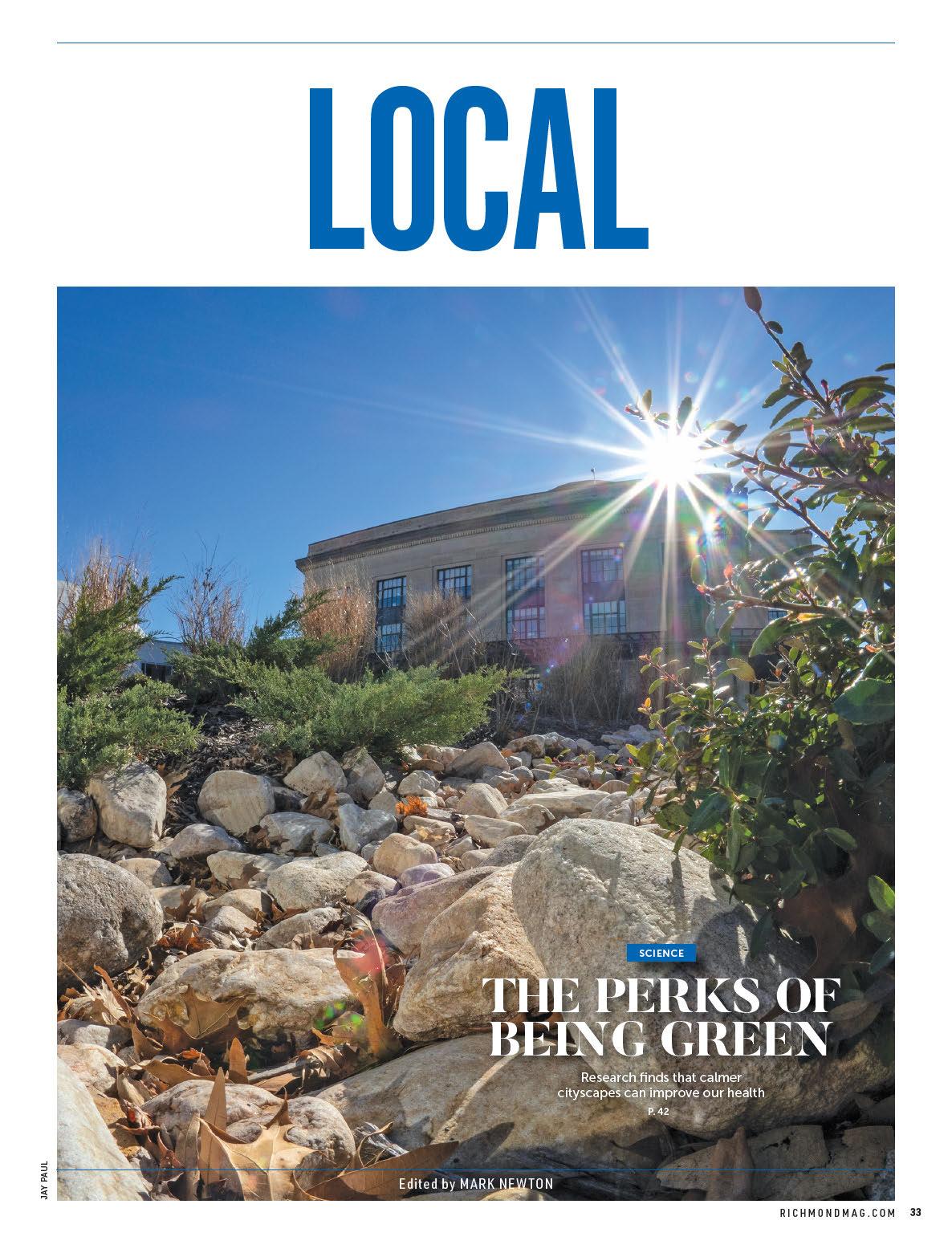
NOW & LATER
Richmond’s job market has made a strong rebound from the COVID-19 pandemic, but there’s work to be done if the city is to maintain its progress.
By Emily McCrary-Ruiz-EsparzaMeet four innovators working to advance cancer treatment; tour VCU’s new Children’s Tower; and explore the promise of ketamine in treating mood disorders. Plus, 492 top medical pros, as chosen by their peers.














students with disabilities.
For all the complaints and the fatigue surrounding face masks, one thing must always be unequivocally understood:
ere are students for whom catching COVID-19 represents a very real threat to their lives, and those same students are as entitled to a public education as any able-bodied child. We’d all like to put the last three years behind us, but we also have to try to put be er days ahead.
“I get that many people would like to be done with COVID,” says Christopher Seaman, a law professor at Washington and Lee University and the plainti for whom the suit was named, “but for families with a medically vulnerable child, ‘return to normalcy’ simply isn’t an option. My son has been a cancer patient for over four years, he was diagnosed with leukemia shortly a er starting kindergarten, and even though he’s

been in remission for over a year now, he is still immunocompromised.” Seaman’s son had never been able to a end a full school year until this year, when “peer masking,” he says, “allowed him to return safely.”
e thing everyone seems to agree on is that in-person learning, especially among younger children, is important. Seaman and the other parents involved in the lawsuit just want to make sure that everyone is a orded the opportunity to learn in person. Seaman said that his son “loves being back in class in person, which has helped him to thrive both educationally and socially. And there are hundreds, possibly thousands, of other children across the commonwealth who are similarly in need of accommodations like peer masking so they can have the same experience. No family should have to choose between
their child’s health and their education.” e way things were before is gone, and it’s not coming back. We’ve had three years to grieve, but now it’s time to stand up straight and face reality. Immunocompromised children are no longer safe in maskless in-person classrooms, yes. But the truth is they were never really that safe in schools before, either. Now the question is, where do we go from here? Do we strive for something be er? We’ve been given our wake-up call. It’s time to reconsider some things and do what we should have been doing from the beginning: taking care of our most vulnerable and giving every child the opportunity to grow up safely. R
David Le owitz is a reporter, freelance writer and Richmond-area native. You can find his work on reasonablyspeedy. substack.com and other websites.






















In February, Dr. Vanessa Sheppard was named the American Cancer Society’s 2022 Researcher of the Year. The honor recognizes her innovative research at Virginia Commonwealth University’s Massey Cancer Center where, for years, she and her team have worked to improve breast cancer outcomes for Black women.
“We focus on African American women because they’re the group that experiences the worst breast cancer mortality — 40% higher than their white counterparts,” says Sheppard, associate director for community outreach and engagement and health disparities research at VCU Massey Cancer Center and associate vice president for population and public health strategic initiatives at the VCU School of Medicine.
According to Sheppard, Black women are more prone to triple-negative breast cancer, which has fast-growing tumors and high recurrence rates. Biology plays a part, as do socioeconomic and behavioral factors. She’s found that Black women are less likely to complete chemotherapy or endocrine therapy and they also report communication issues with their doctors. To address this, she developed a Sisters Informing Sisters intervention that pairs newly diagnosed Black breast cancer patients with trained coaches who are also Black and are cancer survivors who have undergone similar therapies.
The coaches share stories from their experiences, using a patient guidebook, and help the patients learn how to be er communicate with their physicians, while stressing the importance of receiving treatment. Various therapies, survivor stories, and real patient-to-physician conversations are presented in a digital guidebook, which the pairs also discuss.
“The goal is that women will have be er communication
with their providers, because we know when there’s be er communication, then people are more likely to have recommended treatments [and] they’re more likely to complete those treatments,” says Sheppard, adding that these findings were discovered during her initial study.
Sheppard’s research team partnered with survivors and stakeholder groups like the African Women’s Cancer Awareness Association and members of the Sisters Network Inc. to develop the guidebook and ensure it was culturally relevant.
“At the time we were developing the tools, there weren’t any focused on African American women,” says Sheppard. “There weren’t even materials that had faces of brown people. So, we’ve come a long way over the last decade or so of this work.”
She is now overseeing a randomized clinical trial funded with a $1.5 million American Cancer Society grant in which participants either receive enhanced usual care or the Sisters Informing Sisters intervention. The trial is open to newly diagnosed Black women in Virginia and in metro Washington, D.C.

It will be one of the largest interventional trials to focus on Black women. The grant and recognition from the American Cancer Society will assist in expanding her platform to reach more patients.

“The goal is, ‘How do we reduce morbidity and mortality from breast cancer?’ ” Sheppard says. “We think that interaction between the patient and her clinician is critical.”
In his darkened office, radiologist Dr. Ryan Gabriel clicks through bright mammography images on a large monitor. On one 3D scan, no tumors are visible. But on the next scan of the breast, using a different technology, cancerous growths show up clearly as white spots. Such vivid images are the hallmark of a contrast-enhanced mammogram, or CEM.
“It’s really an amazing tool,” says Gabriel, director of breast imaging at the Sarah Cannon Cancer Institute at Henrico Doctors’ Hospital. He and his colleagues have analyzed more than 1,000 scans. Contrast imaging enables doctors to detect cancers at the earliest stage possible.
Patients are injected with an iodine-based dye prior to CEM imaging. The dye is later flushed out by the kidneys, but while in the body, it can light up tumors that escape 3D imaging.
“What we’re taking advantage of are those blood vessels that are growing in the cancer, and those blood vessels are not normal, they’re leaky,” Gabriel says. “The contrast that we inject through an IV leaks out into the tumor for a li le bit of time and we capture it, we take a picture at that time.”
Gabriel trained in CEM imaging during a breast imaging fellowship at the University of Virginia, which he completed in 2017. A passionate patient advocate, he lobbied to bring the technology to Henrico Doctors’ in 2019. The hospital
offers the only contrast-enhanced mammograms in metro Richmond. Henrico Doctors’ is also one of only a few facilities in the United States offering contrast-enhanced stereotactic biopsy machines, where tissue collections are guided by real-time contrast injection.
“It is important to know that MRI is still the most sensitive method to detect breast cancer and CEM doesn’t completely negate the need for MRI,” Gabriel says. “CEM has the potential to provide a quicker, more affordable way to identify breast cancers for those who can’t or don’t want to do MRI.”
At Henrico Doctors’, CEM patients also receive a 3D scan. The contrast dye can pick up tumors as small as 5 mm in diameter — about the size of a pencil eraser — buried deep within layers of tissue.
One of Gabriel’s patients, Melanie Crouch, 47, has dense breast tissue (which can easily hide tumors) but no family or personal history of breast cancer. In 2020, she had an abnormal mammogram and then biopsy findings of atypical ductal hyperplasia, which can sometimes lead to cancer. In 2021, she had a 3D mammogram. Though it came back normal, she says, “I decided I wanted something more in-depth in 2022,” and underwent a contrast-enhanced mammogram for her annual screening.
On the scans, Gabriel discovered “a subtle change on the 3D portion from her prior mammogram, but the tumors were dramatically obvi ous on the CEM. She had multiple tumors equating to a large cancer in her le breast.”
An ultrasound was also performed. It showed abnormal lymph nodes under her le arm. A er biopsy, she learned she had stage 2A breast cancer, which had spread to the lymph nodes.
She has since undergone a double mastectomy, four months
of chemotherapy and five weeks of radiation, which she recently completed. Now, “I can see the light at the end of the tunnel,” she says with a laugh. “It’s been a long year, but at the point it was caught it was still treatable and curable, so I’m very thankful for that.”
Crouch hopes her story encourages others to get mammograms. “If I would have put this off,” she says, “I don’t know how far it would have spread.”
Of the advanced imaging screening, Crouch says: “It saved my life.”
Dr. William “Billy” Irvin Jr. looks out his office window at Bon Secours Cancer Institute at St. Francis Medical Center and sees signs of a booming population — the foundations and frameworks of apartments and office buildings going up just across the street. Here in the growing suburbs of Chesterfield County, he sees a need to expand the reach of clinical trials.
“Eighty to 85% of patients with cancer are treated in a community hospital se ing such as ours. Having trials available in someone’s backyard is absolutely necessary to give them state-of-the-art care. We don’t want to limit it to only those who can drive or fly or have the means to get to a large academic center,” says Irvin, medical director of oncology for Bon Secours Richmond and director of clinical research for the Bon Secours Cancer Institute.
Since his arrival to Bon Secours in 2012 he’s sought to grow the clinical trial program — making sure patients have access to National Cancer Institute trials.

Dr. James Pellicane, a surgeon and director of breast oncology for Bon Secours Richmond, says, “I honestly don’t think we had a program before he took it over, at least not a very active one. He’s done a tremendous job with developing this — not just for breast cancer, but for all cancers.”

Irvin notes that the mortality rate from cancer has decreased 30% in his lifetime. “We’re at the point now where people with a lot of cancer diseases can live a long time, and that’s because of advancements in care,” he says.
Some cancers are still proving stubborn, like triple-negative breast cancer, the most aggressive subtype. Bon Secours patients can undergo trials for datopotamab deruxtecan (DatoDXd). “It’s a novel antibody-drug conjugate; think of a Trojan horse, in that it is a drug linked to another drug,” Irvin says.
As of press time, Bon Secours has 59 clinical cancer trials open. Trials are also offered at sites including Massey Cancer Center, Richmond VA Medical Center (formerly Hunter Holmes

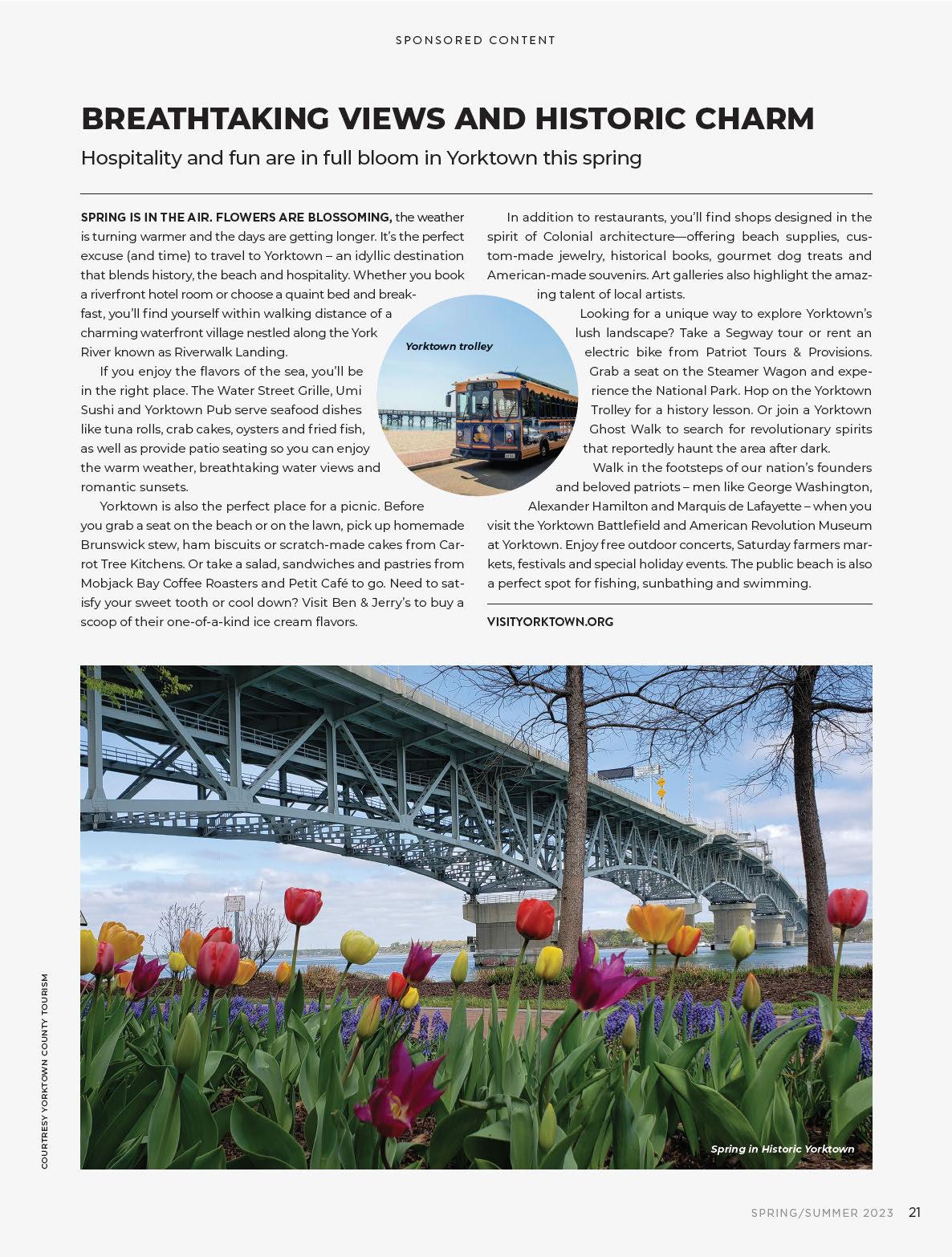
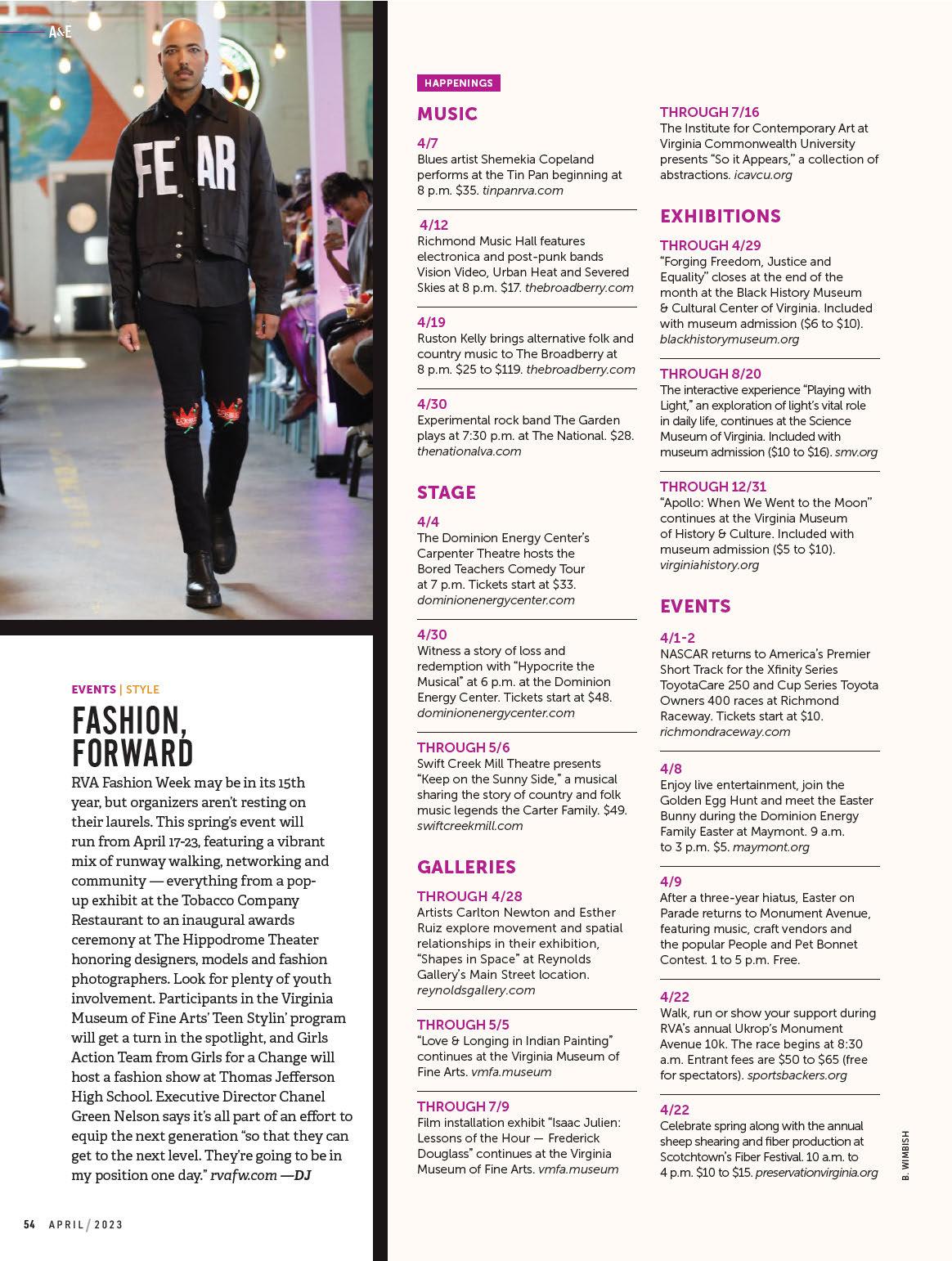
A new pediatric facility is giving rise to improved and expanded health care. Breaking ground in 2019, the Children’s Hospital of Richmond at VCU’s new tower is in the final stages of construction and is set to open on April 30. The 16-story, 500,000-square-foot building comprises an entire city block and is designed to consolidate pediatric care by connecting to the outpatient Children’s Pavilion (which opened in 2016) and housing emergency, trauma and inpatient care. It features 72 private rooms, an emergency department, helipad, expanded child life services, family amenities, additional operating rooms and imaging services. Located on Marshall Street between 10th and 11th streets, the $400 million project was playfully nicknamed the “Wonder Tower” during a fundraising campaign highlighting the creativity and imagination of children, who influenced design elements throughout the facility. Here’s a look inside the Children’s Tower.

Each level of the tower incorporates a design element drawn from nature, as well as a James River-inspired animal mascot for each floor. The blue jay pictured here is on the first level and is paired with some quick facts about the bird; other mascots include a turtle, dragonfly and fox. The bold colors of the walls are different on each level so it’s easier for children to identify their room by noting that it’s on the green floor or the blue level, etc. Fun fact: The height of the tower is equivalent to 13 giraffes.

Vivid colors are used throughout the facility, creating a more inviting and comfortable space for children and their families. Amenities such as playrooms, teen spaces and family lounges are on each floor except the intensive care unit. This playroom on the 12th level is one of four to accommodate bone marrow transplant patients and epilepsy monitoring unit patients, who require a separate space due to health and safety precautions. “Part of taking care of children is taking care of their development,” says Tracy Lowerre, a pediatric nurse clinician at the Children’s Hospital of Richmond and clinical liaison for the Children’s Tower. “Some stay for way longer than what we prefer and so we need to meet all of their needs.”

Seen from below via the cafeteria and above from the main entrance Sky Lobby, this artistic display is one of many colorful elements incorporated into the building’s design.

Murals (including a mural series created by Richmond-based artist Matt Lively), an indoor children’s garden and areas that offer views of the city are all designed to be mood-boosters to ease the stress of a hospital stay for patients and their families. The layout of the building is centered around meeting the needs of children and creating
a space conducive to healing. Jeniece Roane, a pediatric registered nurse and chief nursing officer and vice president of operations at the Children’s Hospital of Richmond, notes that the new tower is also a benefit for VCU Health employees.
“The children are at the center of everything we do, and for a long time we haven’t had an environment that really supports and is reflective of the great care that the children get from our teams,” she says. “So, to be able to do that, it really is an honor.”
The pediatric trauma bay is intended to support two patients at a time, but it’s designed with flexible monitoring capabilities to be able to serve multiple patients in the event of an emergency. “It would be tight, but we can do that,” Lowerre says.

Equipped with seating for about 75, the cafeteria will offer a hot and cold line, brick oven pizza options and grab-and-go items. Families are welcome to use the space, and patients can also request kid-friendly meals in their rooms. Lowerre says the tower will provide healthy vending fare, such as sandwiches and salads, for health-care workers on the night shift. The cafeteria will stay open for early evening diners, so later-shift team members have the opportunity to stop in for a meal prior to its closure. For parents who want to stay close to their child’s unit, lounges on each floor are equipped with amenities, including a refrigerator, ice machine and coffeemaker, and snacks are also available via Ronald McDonald House Charities of Richmond.

 BY PAULA PETERS CHAMBERS / ILLUSTRATION BY CATE ANDREWS
BY PAULA PETERS CHAMBERS / ILLUSTRATION BY CATE ANDREWS
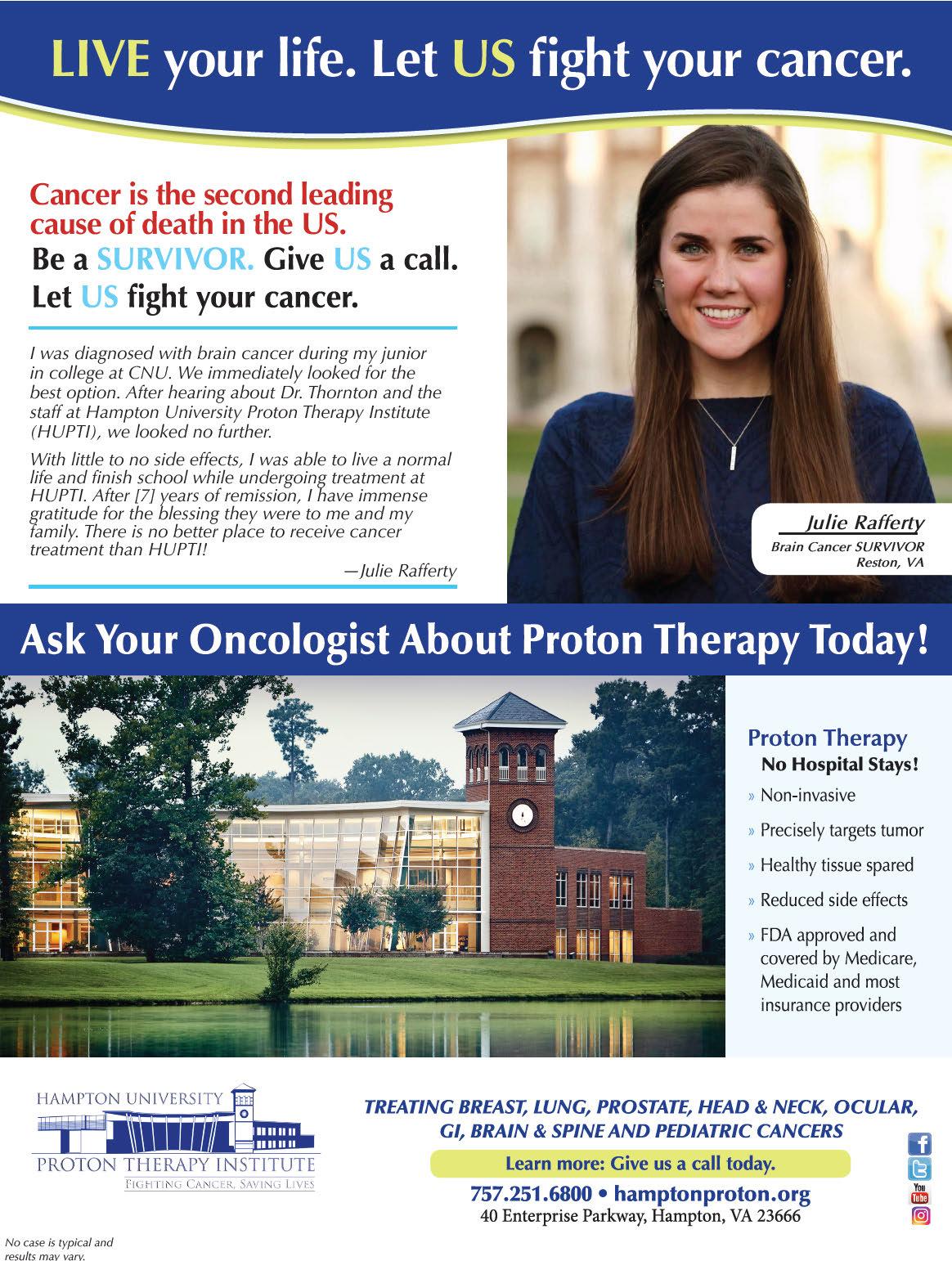
As a nation, we’re struggling with mental health. According to the Centers for Disease Control and Prevention, suicide rates declined in the United States in 2020 during the early days of the COVID-19 pandemic but rebounded in 2021 to 14.5 deaths per 100,000 people. That eclipsed a pre-pandemic peak in 2018 of 14.2. In general, 1 in 6 people will have depression at some time in life. Some will not respond to talk therapy or prescribed medication.
Results of a study published in the September 2022 Journal of Clinical Psychiatry show that regular infusions with the drug ketamine offer relief to people suffering the most with treatmentresistant depression and generalized anxiety symptoms and may also prevent suicidal ideation.
The study — a collaboration between Dr. Albert Arias, an associate professor of psychiatry at VCU Health, and Dr. Pat-
rick Oliver, founder and medical director of the MindPeace Clinic in Richmond — measured both symptom improvement and remission of symptoms. Patients received a low dose of ketamine over 40 minutes via IV drip.
Patients with suicidal ideation experienced dramatic improvement. “At six infusions over two weeks, 50% [of those in the study] were no longer suicidal,” Oliver says. “A er 10 infusions, 75% were no longer suicidal. That’s compared to [prescription] pills, which might take two months to work with less than half the efficacy. In two to three weeks, we’re fixing this problem.”
Study participants experiencing treatment-resistant depression and generalized anxiety also saw relief with 72% and 30% response rates, respectively.
Arias notes that while the study wasn’t a randomized clinical trial, the
large number of patients — 424 — lends weight to the results. “It’s technically a case series, so not as strong [as a clinical trial], but still a useful type of trial that tells us some information,” he says, noting that additional research will use a larger cohort to see if the results hold.
Developed in the 1960s, ketamine is used as an anesthetic for people and animals. Ketamine is structurally related to PCP and can produce hallucinations. It has been used as a party drug, o en referred to as “Special K.” Over the past two decades, research has increased in its use to relieve depression. In 2019, the Food and Drug Administration approved Spravato, a ketamine-based nasal spray, for use in treating depression.
The cost for ketamine infusions is about $500 per 40-minute session; they are offered locally at clinics including Oliver’s MindPeace Clinic and at Alchemy
Wellness in Henrico. Infusions aren’t covered by insurance because they haven’t yet been approved by the FDA. Spravato may be covered, depending on the individual’s health insurance plan.

A s interest has increased, so have businesses that offer ketamine delivered through lozenges or injections, which may not have the medical underpinning used in their study, Oliver and Arias say. “[These treatments] were done under the care of licensed physicians,” Arias says. “Patients aren’t given a supply to take home with them to take however they want.”
Oliver adds, “We have to give the medication in the right amount, in the right concentration, to get the right effect. The problem with oral delivery at home is that when you take it by mouth, it goes through the liver, and you have 10% to 20% absorption. And some people have reactions where they are spooked by it. Some people like the experience of roller coasters; others don’t.”
Grace, a patient of Oliver’s whose last name has been withheld to protect her privacy, found the MindPeace Clinic through an online search. She was diagnosed with major depressive syndrome in college. Over the years, she had tried various treatments, including SSRI medications and talk therapy. She was aware of ketamine’s use to alleviate symptoms but didn’t pursue it until she reached a breaking point in November 2021.
“I thought I wasn’t going to be able to make it through the holidays,” she says. “I was nearly bedridden, with feelings that I’d be better off dead. I’d spent 30-plus years dependent on multiple medications to control depression and anxiety, which were ineffective, but that’s all there was. My mindset was pure desperation. There was nothing le for me to try.”
Grace began treatments before Thanksgiving and had the last session in early December 2021. “I felt completely changed; it was amazing,” she says. “I was shopping, I was wanting to go to holiday parties. Words came easily, my brain fog li ed.”
Because of her anxiety, Grace takes anti-anxiety medication before an infusion, recalling how her first treatment was unsettling. “There is a moment where you begin to dissociate, when you feel like pu ing your foot on the floor to ground yourself,” she says. “When you relinquish that control, I find it to be incredibly peaceful. I can see why people would feel like this is a spiritual thing.”
Since her first round of infusions, Grace has returned to the clinic for four “boosters,” using a mood monitor app to identify when her mental health starts to decline. “Everybody’s different,” she says. “I had hoped that after the first six sessions, everything would be gone; I wasn’t considering that I might need more maintenance. I think because of the severity [of my condition] and where I started, it makes sense that [my issues] wouldn’t just go away.”
Arias says that the recent study doesn’t consider how long treatment effects will last. “We think the majority of people will need boosters, maybe monthly or every couple of months. It varies by person.”
One thing the study does is reassure both patients and prac-
titioners. “This is the type of scientific investigation that academics like to do,” he says. “The treatment remains somewhat controversial within the field. Some prominent psychiatrists on the national level have made statements cautioning about it. There are bits of wisdom in that. On the other hand, it’s an emerging treatment. This is something that adds to the evidence base.”
Oliver says he knew ketamine treatments were helping his patients. The benefit of the study is that it provides data that can be presented to skeptics in the psychiatric community.
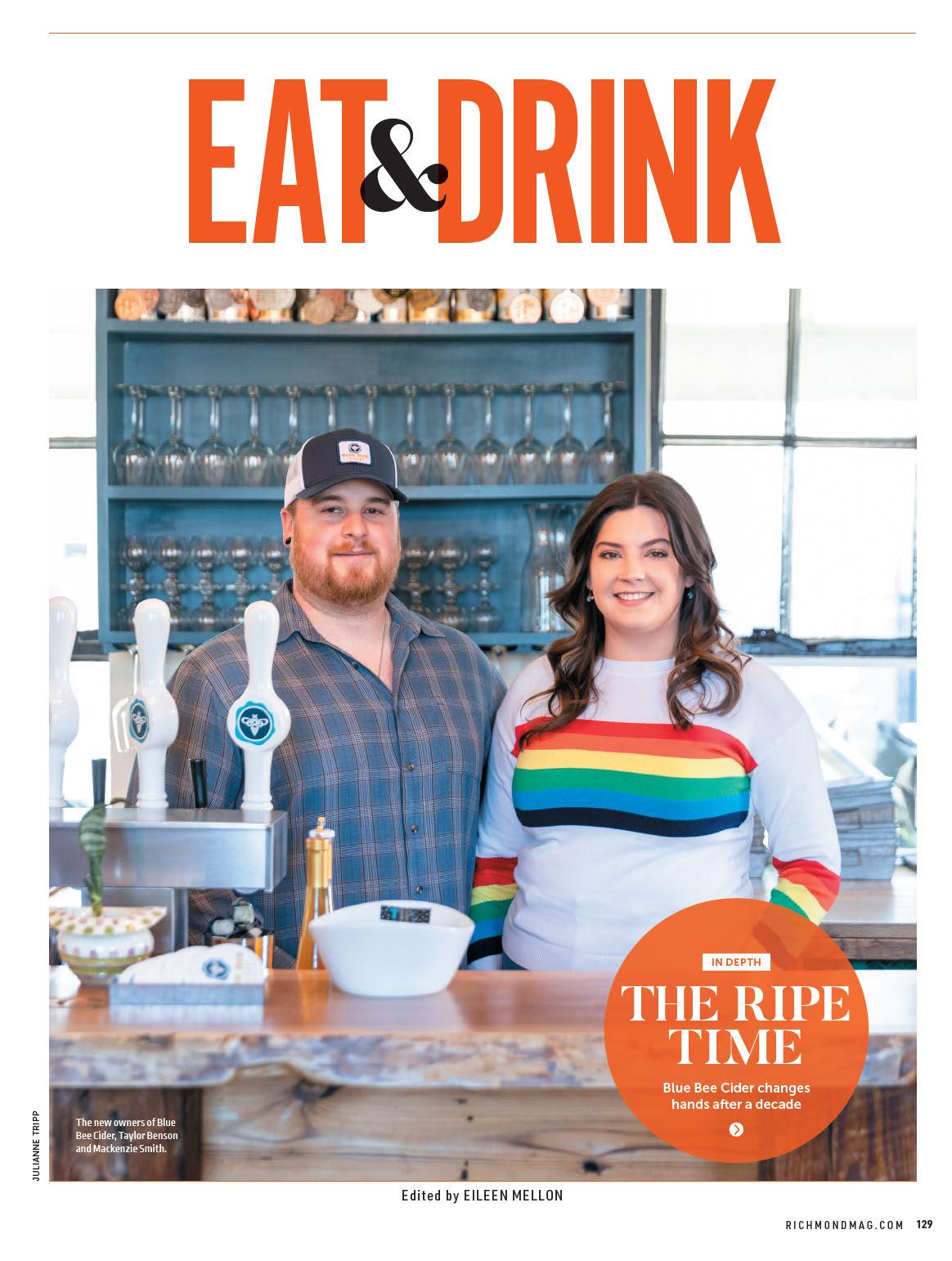
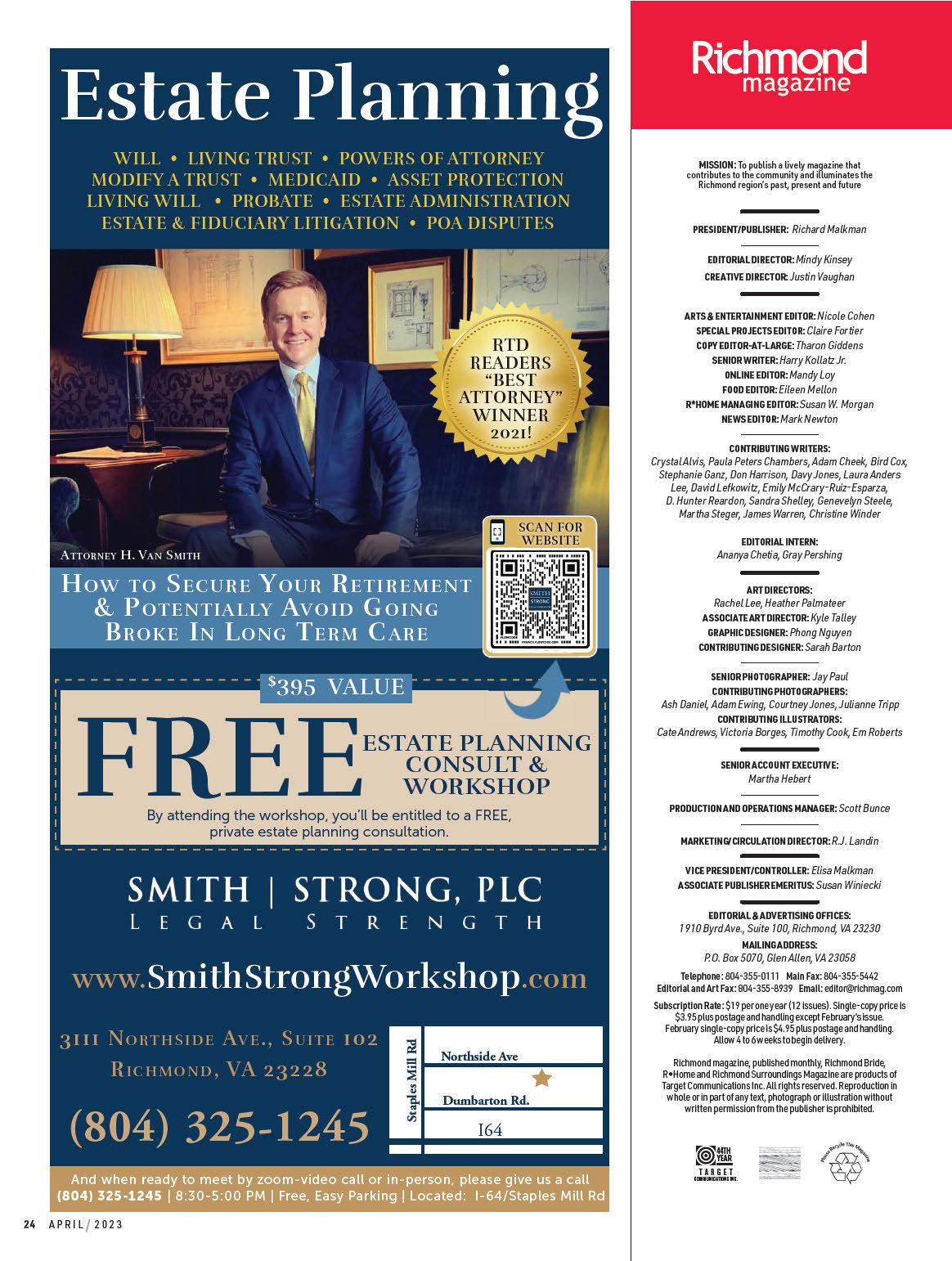
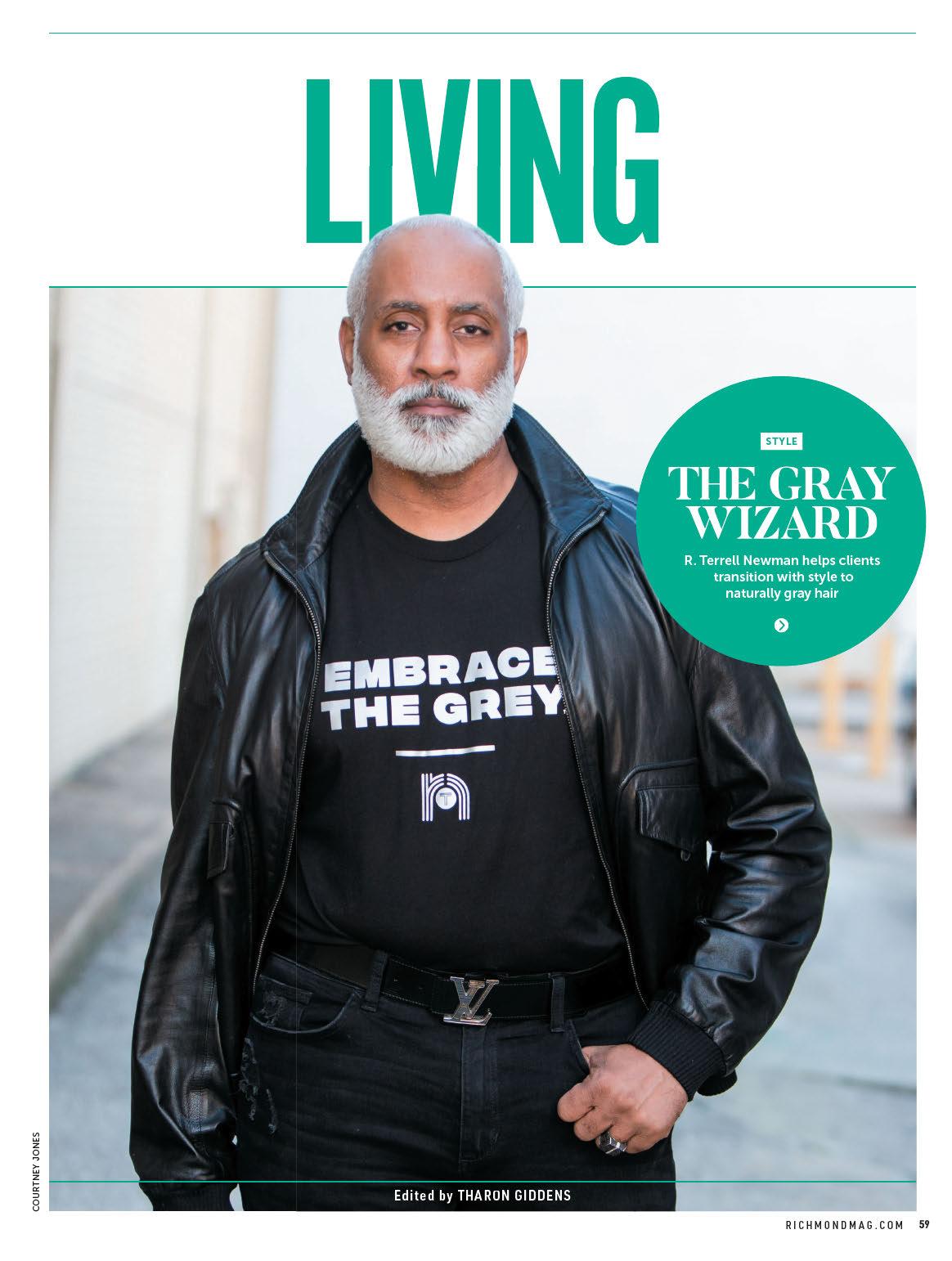
(From left) Registered Nurse Brittany Harding and Dr. Patrick Oliver with a patient, Sharon Nowak
“It’s a different key to the lock; or more accurately, a different set of transmi ers, GABA and glutamate,” he says. “These mood disorders are brutal. With [ketamine infusions], we are encouraging the nerve to release growth protein that tells the nerve to regrow connections, or synapses, amongst themselves. It’s neuroplasticity, regrowing dendritic spines so the nerves can communicate effectively. This is why we’re so excited. I’ve had patients suffering with depression for 40 years; they do treatments with us for two weeks, and they get be er.” R